Beruflich Dokumente
Kultur Dokumente
Applications of Telecounselling in Spinal Cord Injury Rehabilitation: A Systematic Review With Effect Sizes
Hochgeladen von
justin_saneOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Applications of Telecounselling in Spinal Cord Injury Rehabilitation: A Systematic Review With Effect Sizes
Hochgeladen von
justin_saneCopyright:
Verfügbare Formate
Clinical Rehabilitation
27(12) 1072 1083
The Author(s) 2013
Reprints and permissions:
sagepub.co.uk/journalsPermissions.nav
DOI: 10.1177/0269215513488001
cre.sagepub.com
CLINICAL
REHABILITATION
Introduction
Telecounselling the application of individual or
group-based counselling services using telecommuni-
cation technology, such as the telephone, video tele-
phone, videoconferencing, email correspondence, or
audio-video transmission via the internet
1
has the
potential to extend mental healthcare to community-
dwelling adults with spinal cord injuries. Specifically,
telecounselling offers the possibility of an equitable,
affordable and accessible mental health service to pro-
vide consultation, monitoring and treatment.
2,3
To date, however, research examining the
potential use of telecounselling in spinal rehabili-
tation has been limited in both quantity and
488001CRE271210.1177/0269215513488001Clinical RehabilitationDorstyn et al.
2013
School of Psychology, University of Adelaide, South Australia
Corresponding author:
D Dorstyn, School of Psychology, University of Adelaide,
North Terrace Campus, Adelaide, South Australia 5000,
Australia.
Email: diana.dorstyn@adelaide.edu.au
Applications of telecounselling
in spinal cord injury
rehabilitation: a systematic
review with effect sizes
Diana Dorstyn, Jane Mathias and Linley Denson
Abstract
Objective: To investigate the short- and medium-term efficacy of counselling services provided remotely
by telephone, video or internet, in managing mental health outcomes following spinal cord injury.
Data sources: A search of electronic databases, critical reviews and published meta-analyses was
conducted.
Review methods: Seven independent studies (N = 272 participants) met the inclusion criteria.
The majority of these studies utilized telephone-based counselling, with limited research examining
psychological interventions delivered by videoconferencing (N
study
= 1) or online (N
study
= 1).
Results: There is some evidence that telecounselling can significantly improve an individuals management
of common comorbidities following spinal cord injury, including pain and sleep difficulties (d = 0.45).
Medium-term treatment effects were difficult to evaluate, with very few studies providing these data,
although participants have reported gains in quality of life 12 months after treatment (d = 0.88). The main
clinical advantages are time efficiency and consumer satisfaction.
Conclusion: The results highlight the need for further evidence, particularly randomized controlled
trials, to establish the benefits and clinical viability of telecounselling.
Keywords
Spinal cord injuries, telecounselling, telerehabilitation, treatment outcome, systematic review
Received: 23 November 2012; accepted: 7 April 2013
Article
Dorstyn et al. 1073
quality. First, most telecounselling research has
examined other physical disabilities (e.g. stroke,
multiple sclerosis),
4
making it difficult to extrap-
olate the findings to spinal cord injury. Second,
these heterogeneous samples often include indi-
viduals with comorbid cognitive problems (e.g.
stroke, traumatic brain injury), who require dif-
ferent psychological assessments and interven-
tions.
5
Third, trials that have evaluated the
application of telecommunication technology
within spinal rehabilitation have incorporated
diverse treatment programmes, including tele-
medicine, telenursing and multidisciplinary
telerehabilitation, making it difficult to isolate
the effectiveness of counselling-only services.
6
Finally, there are very few qualitative or quantita-
tive reviews specific to this area.
4
Faced with
limited available research, we recently attempted
to address some of these problems by conducting
a meta-analysis of telecounselling research
involving people with chronic physical condi-
tions that have a significant disease burden,
7
namely spinal cord injury, limb amputation,
severe burn injury, stroke and multiple sclerosis.
4
While informative, this analysis was limited to
telephone-based counselling services only, was
not specific to the spinal cord injury population
and, moreover, pre-dated a number of recent tele-
counselling trials that can now be used to narrow
the focus of our analysis to this group.
The current study was therefore designed to con-
solidate the available evidence on the efficacy of
telecounselling in spinal rehabilitation by undertak-
ing a systematic review of this research. The specific
goals were to evaluate the clinical characteristics of
telephone-, video- and internet-based counselling
programmes, namely the: (1) treatment delivery
characteristics (e.g. duration, frequency); (2) short-
term treatment effects (defined as improvements
made from baseline to the period immediately after
telecounselling ceased), and medium-term effects
(defined as any maintenance effects observed after
telecounselling had ceased); and (3) process out-
comes (e.g. attrition rates and cost analyses, where
available). Given the very limited research in this
area, the magnitude of treatment change associated
with telecounselling could not be predicted.
Method
Eligible studies were sourced from six electronic
databases: PubMed, PsycINFO, CINAHL, Scopus,
Cochrane Library, Web of Science (see Appendix for
keywords). The search was restricted to full-text arti-
cles published in English in peer-reviewed journals
between January 1970 (empirical studies of telephone
counselling services dated from that year
8
) and
January 2013. Meta-analytic and systematic reviews
of the telerehabilitation and disability literature,
4,6,911
were also reviewed for additional published empirical
studies, as were the bibliographies of all retrieved
studies and the Spinal Cord Injury Rehabilitation
Evidence database (www.scireproject.com).
Eligible studies had to: (1) target an adult sample
with an acquired spinal cord injury (18 years); and
(2) conduct a telecounselling intervention that
involved healthcare professionals (nurses, social
workers or psychologists) directly interacting with
clients to facilitate psychological recovery follow-
ing injury.
1,4
This included the use of online inter-
ventions where real-time access to a clinician (e.g.
via telephone) was available.
1
Interventions also
had to (3) assess treatment efficacy using one or
more standardized measures of psychological out-
come (e.g. anxiety, depression, quality of life).
Given the very limited research in this area, quasi-
experimental designs that either used a standard-
care control group or no control condition (which is
often necessary in clinical settings),
12,13
were
included in this review.
Studies were excluded if: (1) the sample compo-
sition was heterogeneous and included participants
with a spinal cord injury in addition to those with
another chronic illness or disability (e.g. stroke,
multiple sclerosis), and where the data for spinal
cord injury patients could not be separately extracted;
(2) the telecounselling intervention focused on fam-
ily caregivers and not individuals with a spinal cord
injury; (3) the primary focus of the intervention was
not psychosocial (i.e. only entailed medical, nursing
or physical therapies); (4) the study had a multidisci-
plinary focus and did not specifically evaluate the
counselling component; or (5) treatment efficacy
was only assessed using non-standardized clinical
interviews (N.B. standardized interviews, such as
1074 Clinical Rehabilitation 27(12)
the Centre for Epidemiologic Studies Depression
Scale,
14
were eligible for inclusion).
Data extraction and analysis
The quality of each study meeting inclusion criteria
was evaluated using the Oxford Centre for Evidence
Based Medicine guidelines.
15,16
Accordingly, studies
with greater methodological rigor (e.g. randomized
clinical trials) received a higher rating (level 1 or 2,
depending on the number of participants and statisti-
cal power), meriting a higher grade of recommenda-
tion (grades A or B, respectively). In comparison,
studies received lower ratings (i.e. level 3), and a
lower grade of evidence (C), if they were non-ran-
domized or did not include a control or comparison
group (level 4 or 5). Methodological evaluation
involved consensus ratings by the first and second
authors (DD, JM).
For ease of data collection and interpretation, and
in accordance with the Cochrane Collaboration
17
and PRISMA
18
statements for reporting of system-
atic reviews, a data extraction sheet was used to
summarize key information from each study,
namely: sample demographics (e.g. sample size,
age, gender, race), methodological variables (e.g.
sample size, sampling method, control condition),
and characteristics of the implemented telecounsel-
ling programmes (e.g. programme aims, session fre-
quency and duration). Data extraction was completed
by the first author (DD).
Effect size estimation. To determine telecounselling
treatment effects, Cohens d effect sizes
19
were calcu-
lated for every outcome measure used by a study. Both
the short-term treatment effects (change in outcome
measures from pre- to post-telecounselling) and the
maintenance of treatment gains (post-telecounselling
to follow-up) were evaluated. Different Cohens d for-
mulae
20
were needed for studies that did and did not
use control groups. The direction of each effect size
was standardized across measures so that a positive
effect indicated that telecounselling was beneficial. A
negative d indicated either a worsening of symptoms
among the telecounselling participants, or signifi-
cantly more improvement in controls.
21
Cohens
d-values of 0.2, 0.5 and 0.8 equate to small, medium
and large treatment effects, respectively,
19
with statisti-
cally significant treatment effects having 95% confi-
dence intervals that do not span zero.
21
The original aim was to perform a meta-analysis
in which the data from multiple studies would be
averaged, however there was insufficient overlap in
the communication technologies (telephone, video
and internet); study designs (randomized controlled
trials vs. quasi-experimental); samples (i.e. inpatient
vs. outpatient); and treatment characteristics (e.g.
assessment intervals, outcome measures) of the
studies deemed eligible for inclusion.
21
Consequently,
the effect sizes from these studies were unsuitable to
pool.
22
Importantly, however, the calculation of
effect sizes for individual studies still provided a
standardized metric by which to compare the magni-
tude of treatment effects from different studies,
thereby providing a valuable contribution to the lit-
erature. Moreover, effect sizes provide the best
method by which to assess clinical, as opposed to
statistical, significance because unlike statistical
tests of significance they are not influenced by sam-
ple size.
21
Results
Participant characteristics
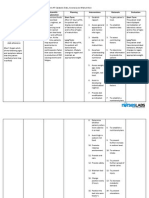
Seven independent clinical studies met all inclusion
criteria
2329
(Figure 1) and in combination they
comprised 272 participants with spinal cord injury
some (n = 52)
23,25
of whom commenced telecoun-
selling during their inpatient rehabilitation, and the
remainder (n = 220)
24,2629
in the community.
Injuries were acquired either recently or in the pre-
ceding 832 years (mean = 20.4; SD = 16.89 years).
The average age of participants was 41 years (SD =
12.2) and most were male (78%, n = 211). Five
studies recruited culturally and linguistically diverse
groups
23,25,26,28,29
(Caucasian: n = 184; 68%;
African-American: n = 75; 28%; Hispanic: n = 12;
4%). One study
29
examined the delivery of a tele-
counselling intervention that was jointly delivered
to individuals (n = 57) and family members (n =
57); however, consistent with the inclusion criteria
for this review, only the data for injured individuals
were considered here.
Dorstyn et al. 1075
Study evaluation
No study had the methodological rigor required for
the highest level of evidence (level 1). Two ran-
domly allocated participants to treatment and con-
trol conditions and were rated level 2.
28,29
Dorstyn
and colleagues
24
also used a randomized design,
but due to low statistical power this study was rated
at level 3. The remaining four studies
23,2527
were
assigned level 4 ratings due to non-randomized
treatment allocation or failure to use a control
group. Importantly, six of the seven studies
2328
were described as preliminary or pilot trials,
designed to evaluate the clinical feasibility of tele-
counselling and inform the power estimates of
subsequent research. The mean sample size was 27
participants per treatment (telecounselling) arm
(SD = 16.84) and 39 participants per control condi-
tion (SD = 20.5), although sample size varied con-
siderably across the seven studies (range: 3104).
Control conditions (N
studies
= 3)
24,28,29
included
standard outpatient care, which involved access to
multidisciplinary care (e.g. medicine, nursing, phys-
iotherapy) when needed (N
studies
= 2; N
participants
=
58),
24,28
and an information only control group
(N
studies
= 1; N
participants
= 60),
29
whereby the control
participants received the same written information
on spinal cord injury and access to community
resources as their telecounselling counterparts. In all
Potentially relevant studies identified
and screened
(n = 1084; duplicates removed)
Studies excluded off topic
(n = 43)
Telecounselling studies excludeddue
to sample characteristics, i.e. included
other chronic illness/disabilities,
>18 years (n = 39)
Studies included in systematic review
(n = 7)
Studies excluded due to intervention
characteristics, i.e. not
telecounselling
(n = 245)
Studies retrieved for more detailed
evaluation
(n = 1041)
Telecounselling studies excluded due to
design, i.e. qualitative or descriptive
stud with no treatment
evaluation (n = 7)
Studies excluded nil intervention
(n = 743)
Figure 1. Flowchart of study selection.
1076 Clinical Rehabilitation 27(12)
three studies,
24,28,29
check-in telephone or face-to-
face contact was available to control participants on
a needs basis.
Twenty different psychological and functional
measures were used to evaluate treatment effi-
cacy. These assessed depression, anxiety, stress,
quality of life, coping, hope, self-efficacy life sat-
isfaction, and aspects of community integration,
such as social and occupational functioning.
14,3046
Two studies
24,27
supplemented self-report mea-
sures with standardized clinical interviews,
namely the Mini International Neuropsychiatric
Interview
30
and Structural Clinical Interview for
Diagnostic and Statistical Manual of Mental
Disorders IV.
31
Clinical characteristics of telephone-
based counselling
While all seven studies used the telephone to some
degree, six utilized the telephone as a primary treat-
ment modality.
2326,28,29
In addition, Phillips and col-
leagues
28
compared the efficacy of two treatment
arms a telephone programme and an audio-video
counselling programme to each other and to a
usual-care control group (Table 1).
The six telephone programmes
2326,28,29
involved
preventative interventions designed to maximize
psychosocial adjustment in the early transition
period (i.e. 612 months) following injury (Table
1). In contrast, Schulz and colleagues
29
examined
the effectiveness of a telephone counselling inter-
vention 58 years following primary rehabilita-
tion. The telephone interventions were relatively
modest in scope, involving weekly or fortnightly
sessions (N
studies
= 5) or a graduated programme of
weekly, followed by fortnightly or monthly ses-
sions (N
studies
= 1) delivered over a 912 week
period (Table 1).
Telephone-based counselling offered flexible
treatment options, being utilized for different psy-
chological therapies, including supportive counsel-
ling (N
studies
= 3),
23,25,28
cognitive behaviour therapy
(N
studies
= 2)
26,29
and motivational interviewing
(N
studies
= 1),
24
and by various health professionals
(e.g. peers, nurses, social workers, psychologists)
(Table 1). The research predominantly involved
individual-based telephone interventions, with one
study
29
utilizing both individual and group formats
to deliver a psycho-educational and coping skills
programme.
Treatment efficacy and process
outcomes of telephone counselling
Cohens d effect sizes indicate that only one study
achieved a statistically meaningful treatment effect
(i.e. confidence intervals did not span zero) immedi-
ately following telephone counselling (Table 2
online).
29
This study found a moderate improve-
ment in participants ability to manage physical
health symptoms related to spinal cord injury (e.g.
muscle pain, poor sleep patterns).
29
The remaining
studies
2326,28
were associated with moderate to
large, but non-significant, short-term treatment
effects for a range of psychosocial measures.
Interestingly, based on their own calculation of
p-values, some of these studies had reported statisti-
cally significant improvements in coping skills,
24
hope,
26
social functioning
26
or cognitive ability.
23
This discrepancy (effect sizes versus statistical test-
ing: confidence intervals versus p-values) confirms
the importance of examining both clinical and sta-
tistical significance.
21
Very limited data were available to evaluate
medium-term treatment effects (i.e. 312 months
post-telecounselling). Only two studies addressed
this question,
24,28
and their effect sizes varied con-
siderably (range: d = 0.160.88; Table 2 online). In
fact, the telecounselling programme used by Phillips
et al.
28
produced the only significant positive change
in quality of life ratings that was maintained 12
months after treatment cessation. All other treat-
ment effects, although positive, were small to mod-
erate in size and non-significant when followed up
at 3 and 12 months.
Clinical outcomes were reported by five stud-
ies
2426,28,29
and were generally favourable. The
mean attrition rate was 28%, although the range was
broad (SD 23.3%; range: 335%). The cost analy-
ses provided by Dorstyn et al.
24
indicate that tele-
phone counselling is cost-efficient, with the total
treatment cost per participant estimated at AU$150.
Participants in some studies also commented that
Dorstyn et al. 1077
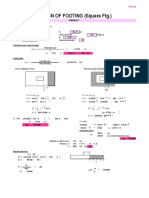
T
a
b
l
e
1
.
S
u
m
m
a
r
y
d
e
t
a
i
l
s
o
f
a
l
l
s
t
u
d
i
e
s
i
n
c
l
u
d
e
d
i
n
t
h
e
c
u
r
r
e
n
t
r
e
v
i
e
w
(
N
s
t
u
d
i
e
s
=
7
)
.
L
e
a
d
a
u
t
h
o
r
M
e
t
h
o
d
o
l
o
g
y
T
e
l
e
c
o
u
n
s
e
l
l
i
n
g
p
r
o
g
r
a
m
m
e
d
e
t
a
i
l
s
S
a
m
p
l
e
s
i
z
e
D
e
s
i
g
n
P
u
b
l
i
s
h
e
d
m
e
a
s
u
r
e
s
E
v
i
d
e
n
c
e
l
e
v
e
l
(
G
r
a
d
e
)
T
r
e
a
t
m
e
n
t
a
i
m
s
K
e
y
t
h
e
r
a
p
i
s
t
T
h
e
r
a
p
y
f
o
r
m
a
t
T
h
e
r
a
p
y
m
o
d
e
l
S
e
s
s
i
o
n
f
r
e
q
u
e
n
c
y
a
n
d
d
u
r
a
t
i
o
n
S
t
r
u
c
t
u
r
e
M
e
d
i
u
m
S
c
h
u
l
z
2
9
(
2
0
0
9
)
1
1
4
T
r
e
a
t
m
e
n
t
(
5
7
i
n
j
u
r
e
d
i
n
d
i
v
i
d
u
a
l
s
;
5
7
c
a
r
e
r
s
)
6
0
C
o
n
t
r
o
l
R
a
n
d
o
m
i
z
e
d
M
u
l
t
i
c
e
n
t
r
e
t
r
i
a
l
B
l
i
n
d
e
d
a
s
s
e
s
s
m
e
n
t
I
n
f
o
r
m
a
t
i
o
n
-
o
n
l
y
c
o
n
t
r
o
l
C
E
S
-
D
S
e
l
f
-
c
a
r
e
p
r
o
b
l
e
m
s
H
e
a
l
t
h
s
y
m
p
t
o
m
s
S
o
c
i
a
l
i
n
t
e
g
r
a
t
i
o
n
S
o
c
i
a
l
s
u
p
p
o
r
t
2
(
B
)
P
r
o
m
o
t
e
h
e
a
l
t
h
b
e
h
a
v
i
o
u
r
a
n
d
p
s
y
c
h
o
l
o
g
i
c
a
l
w
e
l
l
-
b
e
i
n
g
P
s
y
c
h
o
l
o
g
i
s
t
G
r
o
u
p
a
n
d
i
n
d
i
v
i
d
u
a
l
P
h
o
n
e
a
n
d
f
a
c
e
-
t
o
-
f
a
c
e
C
o
g
n
i
t
i
v
e
b
e
h
a
v
i
o
u
r
t
h
e
r
a
p
y
a
n
d
s
u
p
p
o
r
t
i
v
e
c
o
u
n
s
e
l
l
i
n
g
7
i
n
d
i
v
i
d
u
a
l
s
e
s
s
i
o
n
s
(
5
f
a
c
e
-
t
o
-
f
a
c
e
a
n
d
2
p
h
o
n
e
c
a
l
l
s
,
6
0
9
0
m
i
n
p
e
r
s
e
s
s
i
o
n
)
a
n
d
5
g
r
o
u
p
p
h
o
n
e
s
e
s
s
i
o
n
s
.
T
r
e
a
t
m
e
n
t
d
e
l
i
v
e
r
e
d
o
v
e
r
6
m
o
n
t
h
s
P
h
i
l
l
i
p
s
2
8
(
2
0
0
1
)
3
6
T
r
e
a
t
m
e
n
t
(
p
h
o
n
e
)
3
6
T
r
e
a
t
m
e
n
t
(
v
i
d
e
o
)
3
9
C
o
n
t
r
o
l
R
a
n
d
o
m
i
z
e
d
U
s
u
a
l
c
a
r
e
c
o
n
t
r
o
l
Q
W
B
C
E
S
-
D
2
(
B
)
P
r
o
m
o
t
e
h
e
a
l
t
h
b
e
h
a
v
i
o
u
r
a
n
d
p
s
y
c
h
o
l
o
g
i
c
a
l
w
e
l
l
-
b
e
i
n
g
N
u
r
s
e
I
n
d
i
v
i
d
u
a
l
P
h
o
n
e
a
n
d
v
i
d
e
o
P
s
y
c
h
o
-
e
d
u
c
a
t
i
o
n
a
n
d
s
u
p
p
o
r
t
i
v
e
c
o
u
n
s
e
l
l
i
n
g
7
s
e
s
s
i
o
n
s
(
3
0
4
0
m
i
n
p
e
r
s
e
s
s
i
o
n
)
o
v
e
r
9
w
e
e
k
s
(
5
w
e
e
k
l
y
a
n
d
2
f
o
r
t
n
i
g
h
t
l
y
D
o
r
s
t
y
n
2
4
(
2
0
1
2
)
2
0
T
r
e
a
t
m
e
n
t
1
9
C
o
n
t
r
o
l
R
a
n
d
o
m
i
z
e
d
B
l
i
n
d
e
d
a
s
s
e
s
s
m
e
n
t
U
s
u
a
l
c
a
r
e
c
o
n
t
r
o
l
D
A
S
S
-
2
1
M
D
S
S
M
I
N
I
S
C
L
F
I
M
3
(
C
)
P
r
o
m
o
t
e
h
e
a
l
t
h
b
e
h
a
v
i
o
u
r
a
n
d
p
s
y
c
h
o
l
o
g
i
c
a
l
w
e
l
l
-
b
e
i
n
g
P
s
y
c
h
o
l
o
g
i
s
t
I
n
d
i
v
i
d
u
a
l
P
h
o
n
e
M
o
t
i
v
a
t
i
o
n
a
l
i
n
t
e
r
v
i
e
w
i
n
g
7
s
e
s
s
i
o
n
s
(
a
v
e
r
a
g
e
1
9
m
i
n
/
s
e
s
s
i
o
n
)
o
v
e
r
3
m
o
n
t
h
s
L
u
c
k
e
2
6
(
2
0
0
4
)
1
0
T
r
e
a
t
m
e
n
t
C
o
n
v
e
n
i
e
n
c
e
s
a
m
p
l
e
N
o
c
o
n
t
r
o
l
P
A
N
A
S
H
H
S
M
H
S
L
S
S
S
F
-
3
6
4
(
C
)
P
r
o
v
i
d
e
i
n
f
o
r
m
a
t
i
o
n
a
l
a
n
d
p
e
e
r
s
u
p
p
o
r
t
N
u
r
s
e
a
n
d
p
e
e
r
m
e
n
t
o
r
I
n
d
i
v
i
d
u
a
l
P
h
o
n
e
C
o
g
n
i
t
i
v
e
b
e
h
a
v
i
o
u
r
t
h
e
r
a
p
y
3
s
e
s
s
i
o
n
s
(
s
e
s
s
i
o
n
t
i
m
e
s
n
o
t
s
p
e
c
i
f
i
e
d
)
o
v
e
r
6
w
e
e
k
s
M
i
g
l
i
o
r
i
n
i
2
7
(
2
0
1
1
)
3
T
r
e
a
t
m
e
n
t
M
u
l
t
i
p
l
e
c
a
s
e
s
t
u
d
y
d
e
s
i
g
n
N
o
c
o
n
t
r
o
l
S
C
I
D
D
A
S
S
-
2
1
S
C
L
P
W
I
4
(
C
)
M
a
n
a
g
e
s
y
m
p
t
o
m
s
o
f
d
e
p
r
e
s
s
i
o
n
a
n
d
a
n
x
i
e
t
y
P
s
y
c
h
o
l
o
g
i
s
t
I
n
d
i
v
i
d
u
a
l
I
n
t
e
r
n
e
t
a
n
d
p
h
o
n
e
C
o
g
n
i
t
i
v
e
b
e
h
a
v
i
o
u
r
t
h
e
r
a
p
y
a
n
d
p
o
s
i
t
i
v
e
p
s
y
c
h
o
l
o
g
y
1
0
m
o
d
u
l
e
s
(
C
o
n
t
i
n
u
e
d
)
1078 Clinical Rehabilitation 27(12)
L
e
a
d
a
u
t
h
o
r
M
e
t
h
o
d
o
l
o
g
y
T
e
l
e
c
o
u
n
s
e
l
l
i
n
g
p
r
o
g
r
a
m
m
e
d
e
t
a
i
l
s
S
a
m
p
l
e
s
i
z
e
D
e
s
i
g
n
P
u
b
l
i
s
h
e
d
m
e
a
s
u
r
e
s
E
v
i
d
e
n
c
e
l
e
v
e
l
(
G
r
a
d
e
)
T
r
e
a
t
m
e
n
t
a
i
m
s
K
e
y
t
h
e
r
a
p
i
s
t
T
h
e
r
a
p
y
f
o
r
m
a
t
T
h
e
r
a
p
y
m
o
d
e
l
S
e
s
s
i
o
n
f
r
e
q
u
e
n
c
y
a
n
d
d
u
r
a
t
i
o
n
S
t
r
u
c
t
u
r
e
M
e
d
i
u
m
B
a
l
c
a
z
a
r
2
3
(
2
0
1
1
)
2
8
T
r
e
a
t
m
e
n
t
N
o
c
o
n
t
r
o
l
C
H
A
R
T
4
(
C
)
P
r
o
v
i
d
e
i
n
f
o
r
m
a
t
i
o
n
a
l
a
n
d
p
e
e
r
s
u
p
p
o
r
t
P
e
e
r
m
e
n
t
o
r
s
u
p
e
r
v
i
s
e
d
b
y
s
o
c
i
a
l
w
o
r
k
e
r
I
n
d
i
v
i
d
u
a
l
P
h
o
n
e
a
n
d
f
a
c
e
-
t
o
-
f
a
c
e
P
s
y
c
h
o
-
e
d
u
c
a
t
i
o
n
a
n
d
s
u
p
p
o
r
t
i
v
e
c
o
u
n
s
e
l
l
i
n
g
W
e
e
k
l
y
c
o
n
t
a
c
t
f
o
r
1
h
o
u
r
o
v
e
r
1
2
m
o
n
t
h
s
6
1
%
p
h
o
n
e
c
o
n
t
a
c
t
a
n
d
3
9
%
f
a
c
e
-
t
o
-
f
a
c
e
L
j
u
n
g
b
e
r
g
2
5
(
2
0
1
1
)
2
4
T
r
e
a
t
m
e
n
t
N
o
c
o
n
t
r
o
l
G
S
E
F
4
(
C
)
E
n
h
a
n
c
e
s
e
l
f
-
e
f
f
i
c
a
c
y
a
n
d
p
r
o
v
i
d
e
p
e
e
r
s
u
p
p
o
r
t
P
e
e
r
m
e
n
t
o
r
s
u
p
e
r
v
i
s
e
d
b
y
p
s
y
c
h
o
l
o
g
i
s
t
I
n
d
i
v
i
d
u
a
l
P
h
o
n
e
a
n
d
f
a
c
e
-
t
o
-
f
a
c
e
P
s
y
c
h
o
-
e
d
u
c
a
t
i
o
n
a
n
d
s
u
p
p
o
r
t
i
v
e
c
o
u
n
s
e
l
l
i
n
g
W
e
e
k
l
y
c
o
n
t
a
c
t
f
o
r
3
m
o
n
t
h
s
,
f
o
l
l
o
w
e
d
b
y
b
i
w
e
e
k
l
y
c
o
n
t
a
c
t
f
o
r
3
m
o
n
t
h
s
,
a
n
d
m
o
n
t
h
l
y
c
o
n
t
a
c
t
f
o
r
6
m
o
n
t
h
s
.
C
E
S
-
D
,
C
e
n
t
r
e
f
o
r
E
p
i
d
e
m
i
o
l
o
g
i
c
S
t
u
d
i
e
s
D
e
p
r
e
s
s
i
o
n
S
c
a
l
e
1
4
;
S
e
l
f
-
c
a
r
e
p
r
o
b
l
e
m
s
3
6
;
H
e
a
l
t
h
s
y
m
p
t
o
m
s
3
6
;
S
o
c
i
a
l
i
n
t
e
g
r
a
t
i
o
n
3
6
;
S
o
c
i
a
l
s
u
p
p
o
r
t
3
6
;
C
H
A
R
T
,
C
r
a
i
g
H
a
n
d
i
c
a
p
A
s
s
e
s
s
m
e
n
t
a
n
d
R
e
p
o
r
t
i
n
g
T
e
c
h
n
i
q
u
e
3
4
;
D
A
S
S
-
2
1
,
D
e
p
r
e
s
s
i
o
n
A
n
x
i
e
t
y
S
t
r
e
s
s
S
c
a
l
e
s
h
o
r
t
f
o
r
m
3
2
;
F
I
M
,
F
u
n
c
t
i
o
n
a
l
I
n
d
e
p
e
n
d
e
n
c
e
M
e
a
s
u
r
e
3
7
;
M
D
S
S
,
M
u
l
t
i
d
i
m
e
n
s
i
o
n
a
l
M
e
a
s
u
r
e
o
f
S
o
c
i
a
l
S
u
p
p
o
r
t
3
8
;
M
I
N
I
,
I
n
t
e
r
n
a
t
i
o
n
a
l
N
e
u
r
o
p
s
y
c
h
i
a
t
r
i
c
I
n
t
e
r
v
i
e
w
3
0
;
S
C
L
,
S
p
i
n
a
l
C
o
r
d
L
e
s
i
o
n
Q
u
e
s
t
i
o
n
n
a
i
r
e
s
3
3
;
Q
W
B
,
Q
u
a
l
i
t
y
o
f
W
e
l
l
-
B
e
i
n
g
S
c
a
l
e
3
9
;
P
A
N
A
S
,
P
o
s
i
t
i
v
e
a
n
d
N
e
g
a
t
i
v
e
A
f
f
e
c
t
S
c
a
l
e
4
0
;
H
H
S
,
H
e
r
t
h
H
o
p
e
S
c
a
l
e
4
1
;
M
H
S
,
M
i
l
l
e
r
H
o
p
e
S
c
a
l
e
4
2
;
L
S
S
,
L
i
f
e
S
i
t
u
a
t
i
o
n
S
u
r
v
e
y
4
3
;
S
F
-
3
6
,
M
e
d
i
c
a
l
O
u
t
c
o
m
e
s
S
t
u
d
y
S
h
o
r
t
-
F
o
r
m
H
e
a
l
t
h
S
u
r
v
e
y
4
4
;
S
C
I
D
,
S
t
r
u
c
t
u
r
a
l
C
l
i
n
i
c
a
l
I
n
t
e
r
v
i
e
w
f
o
r
D
S
M
D
i
s
o
r
d
e
r
s
3
7
;
P
W
I
,
P
e
r
s
o
n
a
l
W
e
l
l
b
e
i
n
g
I
n
d
e
x
;
4
5
G
S
E
F
,
G
e
n
e
r
a
l
i
s
e
d
P
e
r
c
e
i
v
e
d
S
e
l
f
-
E
f
f
i
c
a
c
y
S
c
a
l
e
.
4
6
T
a
b
l
e
1
.
(
C
o
n
t
i
n
u
e
d
)
Dorstyn et al. 1079
the intervention increased their sense of interper-
sonal support and reduced isolation.
23,26,28
Also interesting are the findings relating to tele-
counselling for diverse cultural groups. Participants
in Lucke and colleagues trial,
26
which targeted
Hispanics and African-Americans, reported that
telecounselling provided much-needed social sup-
port following primary spinal cord injury rehabilita-
tion. Similarly, Balcazar and colleagues
23
claimed
that matching their peer-mentors to mentees (n =
28) on the basis of race maximized improvements in
community integration (e.g. social roles and rela-
tionships). However, these qualitative data need to
be interpreted cautiously, given that both studies
examined small samples and were uncontrolled
(Table 2 online).
Clinical characteristics of video-based
counselling
Only one study examined the specific application of
video technology to counseling services in spinal
rehabilitation.
28
This study utilized videoconferenc-
ing to provide a nine-week nurse-led supportive
counselling programme to individuals with a newly
acquired injury who were not otherwise accessing
mental health services (Table 1).
Treatment efficacy and process
outcomes of video counselling
The short-term efficacy of video-based counsel-
ling could not be determined from this single trial,
because only post-intervention assessments were
conducted.
28
At 12-month follow-up, d-values
indicated that participants who completed the vid-
eocounselling programme reported significantly
more depression symptoms than those in the tele-
phone-only or standard-care conditions (Table 2
online).
28
Medium-term improvements were, however,
noted in relation to videoconferencing. Specifically,
these participants reported the lowest rehospitaliza-
tion rates, averaging 3 hospital-days per year, com-
pared with participants who received telephone
counselling (5 days per year) or standard care (8
days per year).
28
Thus, although there did not appear
to be any sustained psychological benefits from vid-
eocounselling, there appear to have been some
broader medical benefits. The authors
28
also
reported that videoconferencing was cost effective,
although formal costings were not included.
Clinical characteristics of internet-
based counselling
The study by Migliorini et al.
27
was the only evalu-
ation of an internet-delivered psychological pro-
gramme. Unlike the programmes reviewed above,
this intervention targeted a very small number of
adults (n = 3) in the chronic stage of spinal rehabili-
tation (mean time since diagnosis = 32.3 years, SD
= 11.9; range: 2745 years) but has informed a
larger scale randomized controlled trial that is cur-
rently underway.
27
The online programme, known
as ePACT, involved 10 self-administered modules,
addressing symptoms of depression and anxiety
using cognitive behavioural therapy and positive
psychology (Table 1). In addition to the standard-
ized intervention, email and telephone access to a
therapist were available, as needed.
Treatment efficacy and process
outcomes of internet counselling
Although the short-term treatment gains associated
with ePACT were moderate to large, they were not
statistically significant across the measures of
depression, anxiety and stress (Table 2 online).
27
Similarly, large to very large but non-significant
improvements were noted for injury-specific coping
strategies, including participants attitude towards
their disability and reduced sense of helplessness
(Table 2 online). Notably, these results were associ-
ated with large confidence intervals, indicating wide
variation in the treatment effects for individual cases
and rendering otherwise important treatment effects
non-significant. Nevertheless, the findings from this
study are promising, with all three participants
reporting non-clinical levels of depression, anxiety
and/or stress at the end of the intervention compared
to baseline.
27
Whether these clinical gains were
maintained over time remains unanswered because
follow-up assessments were not conducted.
1080 Clinical Rehabilitation 27(12)
Qualitative data from this study indicated that
participants considered the intervention to be con-
venient and acceptable, commenting that they
would not have otherwise accessed psychological
therapy due to the perceived stigma associated with
mental health services and/or transport access issues
related to physical disability.
27
Furthermore, partici-
pants reported that the availability of a therapist by
telephone contributed to the programmes appeal.
27
However, there was a high attrition rate, with 63%
(n = 5) of eligible participants withdrawing from the
programme due to conflicting time commitments or
a perception that they did not require psychological
support.
27
Consequently, these results should be
treated with caution.
Discussion
Results from the seven independent clinical stud-
ies
2329
included in this review are clinically promis-
ing, with telecounselling contributing to significant
short-term improvements in health symptoms for
individuals with spinal cord injuries.
29
However, the
longer term impact of telecounselling has yet to be
adequately evaluated. The few trials
24,28
that report
this data suggest that early treatment gains may not
be maintained.
Where available, the clinical outcome data sug-
gest that telecounselling can improve psychological
outcomes of this population in a time- and cost-
efficient way, with the majority of treatments (N
studies
= 5)
2326,28
delivered within the first three months
post discharge from primary rehabilitation.
However, these findings can only be considered ten-
tative: based on a small number of studies, most of
which utilized non-randomized and uncontrolled
trials (N
studies
= 4)
23,2527
with highly variable sample
sizes (sample size range: 3104).
Our results are largely consistent with those of
other telecounselling trials within chronic illness and
disability groups, which report that telephone- and
video-based counselling services provide an effec-
tive and efficient treatment option for managing
mood disorders in individuals with traumatic brain
injuries
47
or chronic medical conditions.
48,49
Telecounselling may facilitate routine psychological
follow-up of individuals with a newly acquired
injury, who often experience increased apprehension
and distress during the transition from primary reha-
bilitation.
4,28
However, additional information on the
delivery-related outcomes of telecounselling is
needed, with very few cost analyses currently avail-
able. These cost analyses need to include the total
amount of therapist contact time per participant, and
investigate clinician and patient attitudes towards the
different technology-assisted counselling services.
4
Given these potential clinical benefits, it may
be argued that telecounselling can provide com-
munity-based practitioners more opportunity to
efficiently monitor patients long-term psychologi-
cal health.
50
This is consistent with current models
of mental healthcare, favouring a biopsychosocial
approach in which periodic maintenance sessions
allow psychological problems to be monitored and
treated before they become more serious and
established.
1,50,51
Although the findings of this review are both
interesting and important, some limitations need to
be considered. First, the research designs that were
used by the current studies limit any causal state-
ments that can be made about the effectiveness of
telecounselling.
21
In particular, Balcazar et al.,
23
Ljungberg et al.,
25
Lucke et al.
26
and Migliorini
et al.
27
did not use control groups, consequently
spontaneous recovery/decline and the impact of hav-
ing some on-going contact (regardless of its content)
could not be assessed. A suitable control condition
might involve delivering the same tele-programme
in a face-to-face setting, which would control for
both of these effects while also enabling an evalua-
tion of whether the intervention content can be suc-
cessfully delivered via telecommunication
technology. Indeed this design has been adopted
among other telecounselling trials targeting, care-
givers of individuals with a spinal cord injury,
52
but
was only adopted by one reviewed study.
29
Moreover,
the four quasi-experimental studies
23,2527
all used
relatively small samples, limiting their statistical
power to detect significant effects.
19,21
Future trials
should therefore compute post-hoc power analy-
ses.
53
Estimates of treatment effects (i.e. Cohens d),
and tests of statistical significance (i.e. confidence
intervals for d-values), should also be routinely
Dorstyn et al. 1081
Clinical messages
Telecounselling has potential to provide a
community-based method by which to man-
age and treat a range of psychological issues
following spinal cord injury; thus reducing
depression and improving quality of life.
Telecounselling is practical to deliver and
generally accepted by consumers.
Further research using randomized controlled
trials and well controlled case studies are
needed to confirm the efficacy of telecounsel-
ling in the psychosocial care of people with
spinal cord injury and to define the minimum
requirements needed to achieve efficacy (e.g.
number and duration of sessions).
Conflict of interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
References
*References with an asterisk are those included in the systematic
review
1. Campos B. Telepsychology and telecounselling: counsel-
ling conducted in a technology environment. Counsel Psy-
chother Health 2009; 5: 2659.
2. Bloemen-Vrencken JH, de Witte LP and Post MWM.
Follow-up care for persons with spinal cord injury living
in the community: a systematic review of interventions
and their evaluations. Spinal Cord 2005; 43: 462475.
3. DeJong G, Hoffman J, Meade MA, et al. Post-rehabilitation
health care for individuals with SCI: extending health care
in the community. Top Spinal Cord Inj Rehabil 2011; 17:
4658.
4. Dorstyn DS, Mathias JL and Denson LA. Psychosocial out-
comes of telephone-based counselling for adults with an
acquired physical disability: a meta-analysis. Rehabil Psy-
chol 2011; 56: 114.
5. Krause JS, Saunders LL and Newman S. Posttraumatic
stress disorder and spinal cord injury. Arch Phys Med Reha-
bil 2010; 91: 11821187.
6. Bloemen-Vrencken JH, de Witte LP and Post MWM. Fol-
low-up care for persons with spinal cord injury living in the
community: a systematic review of interventions and their
evaluations. Spinal Cord 2005; 43: 462475.
reported.
21
As was apparent here, effect sizes may be
better measures of clinical significance than
P-values.
Second, unreported confounding variables may
have mediated and moderated study outcomes.
Specifically, variables known to have a positive
impact on the effectivenesss of psychological inter-
ventions in spinal rehabiliation, such as concurrent
pharmacotherapy, were not always reported.
54
Similarly, some variables known to affect post-
injury depression or functional outcomes (e.g. pre-
existing psychiatric illness
5,54
or injury-related
neuropathic pain
55
) were largely unreported. The
single trial
28
that compared telephone- and video-
counselling reported an increase over time in
depression symptoms among videoconferencing
participants, compared to participants in telephone-
only or standard-care conditions. The authors
argued that between-group differences in psychiat-
ric comorbidities and antidepressant medications
may have impacted on patients responses to the
two interventions.
28
Likewise, Dorstyn et al.
24
sug-
gested pain as a possible moderator, because the
majority of their telephone-counselling sample used
long-term prescription medication for neuropathic
pain.
Third, the timing of assessments may have influ-
enced the estimated treatment effects. Balcazar
et al.,
23
Ljungberg et al.
25
and Schulz et al.
29
obtained
baseline data during an initial treatment phase involv-
ing face-to-face therapy. Similarly Phillips et al.
28
did
not include baseline assessments administered pre-
telecounselling in their study. Consequently, their
results may not accurately reflect the effectiveness of
telecounselling alone.
Finally, future trials need to examine longer
treatment durations and extended service delivery,
to determine treatment efficacy for more severe
psychopathology. The trials evaluated by Dorstyn
et al.
24
and Migliorini et al.
27
included individuals
with clinical levels of depression or anxiety at
baseline, but both interventions were relatively
short-term (three months). Consequently, the
small and non-significant treatment effects may
reflect the fact that short-term interventions can-
not meet or resolve more complex mental health
needs.
4
1082 Clinical Rehabilitation 27(12)
7. World Health Organization. The global burden of disease:
2004 update. Geneva: World Health Organization, 2008.
8. Hornblow AR. The evolution and effectiveness of tele-
phone counselling services. Hosp Community Psychiatry
1986; 37: 731733.
9. Kairy D, Lehoux P, Vincent C and Visintin M. A systematic
review of clinical outcomes, clinical process, healthcare uti-
lization and costs associated with telerehabilitation. Disabil
Rehabil 2009; 31: 427447.
10. Hersh WR, Helfand M, Wallace J, et al. Clinical outcomes
resulting from telemedicine interventions: a systematic
review. BMC Med Inform Decis Mak 2001; 1: 512.
11. Rogante M, Grigioni M, Cordella D and Giacomozzi C. Ten
years of telerehabilitation: a literature overview of technol-
ogies and clinical applications. NeuroRehabilitation 2010;
27: 287304.
12. Schwartz SM, Trask PC, Shanmugham K and Townsend
CO. Conducting psychological research in medical settings:
challenges, limitations and recommendations for effective-
ness research. Prof Psychol Res Pract 2004; 35: 500508.
13. Kerstein P, Ellis-Hill C, McPherson KM and Harrington R.
Beyond the RCT: understanding the relationship between
interventions, individuals and outcome. Disabil Rehabil
2010; 32: 10281034.
14. Radloff LS. The CES-D Scale: A self report depression
scale for research in the general population. Appl Psychol
Meas 1977; 1: 385400.
15. Oxford Centre for Evidence Based Medicine Levels of
Evidence Working Group. The Oxford 2011 Levels of Evi-
dence, 2011. www.cebm.net/index.aspx?o=5653 (accessed
1 November 2012).
16. Sackett DL, Rosenberg WM, Gray JA, Haynes RB and
Richardson WS. Evidence-based medicine: what it is and
what it isnt. BMJ 1996; 312: 7172.
17. Higgins JPT and Green S (eds). Cochrane handbook for
systematic reviews of interventions, version 5.0.2. The
Cochrane Collaboration, 2009. www.cochrane-handbook.
org (accessed 1 November 2012)
18. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA state-
ment for reporting systematic reviews and metaanalyses of
studies that evaluate health care interventions: explanation
and elaboration. PLoS Med 2009; 6: e1000100.
19. Cohen J. A power primer. Psychol Bull 1991; 112: 155
159.
20. Morris SB and DeShon RP. Combining effect size estimates
in meta-analysis with repeated measures and independent-
groups designs. Psychol Meth 2002; 7: 105125.
21. Lipsey MW and Wilson DB. Practical meta-analyses. Lon-
don: Sage, 2001.
22. Sharpe D. Of apples and oranges, file drawers and garbage:
why validity issues in meta-analysis will not go away. Clin
Psychol Rev 1997; 17: 881901.
23. *Balcazar FE, Kelly EH, Beys CB and Balfanx-Vretiz K.
Using peer mentoring to support the rehabilitation of indi-
viduals with violently acquired spinal cord injuries. J Appl
Rehabil Counsel 2011; 42: 311.
24. *Dorstyn DS, Mathias JL, Denson LA and Robertson TM.
Effectiveness of telephone counselling in managing psy-
chological outcomes following spinal cord injury: a prelim-
inary study. Arch Phys Med Rehabil 2012; 93: 21002108.
25. *Ljungberg I, Kroll T, Libin A and Gordon S. Using peer
mentoring for people with spinal cord injury to enhance
self-efficacy beliefs and prevent medical complications. J
Clin Nurs 2011; 20: 351358.
26. *Lucke KT, Lucke JF and Martinez H. Evaluation of a pro-
fessional and peer telephone intervention with spinal cord
injured individuals following rehabilitation in South Texas.
J Multicult Nurs Health 2004; 10: 6874.
27. *Migliorini C, Tonge B and Sinclair A. Developing and
piloting ePACT: a flexible psychological treatment for
depression in people living with chronic spinal cord injury.
Behav Change 2011; 28: 4554.
28. *Phillips VL, Vesmarovich S, Hauber R, Wiggers E and
Egner A. Telecounselling: reaching out to newly injured
spinal cord patients. Public Health Rep 2001; 116: 94102.
29. *Schulz R, Czaja SJ, Lustig A, Zdaniuk B, Martire LM and
Perdomo D. Improving the quality of life of caregivers of
persons with spinal cord injury: a raandomised controlled
trial. Rehabil Psychol 2009; 51: 115.
30. Sheehan DV, Lecrubier Y and Sheehan KH. The MINI
International Neuropsychiatric Interview: the development
and validation of a structured diagnostic psychiatric inter-
view. J Clin Psychiatry 1998; 59 (suppl 20): 2223.
31. First MB, Spitzer RL, Gibbon M and Williams JBW. Struc-
tured clinical interview for DSM-IV-TR Axis I disorders,
research version, non-patient edition (SCID-I/NP). New
York: Biometrics Research New York State Institute, 2002.
32. Lovibond SH and Lovibond PF. Manual for the Depression
Anxiety Stress Scales, second edition. Sydney: Psychology
Foundation of Australia, 2001.
33. Migliorini C, Elfstrm ML and Tonge BL. Translation and
Australian validation of the spinal cord lesion related cop-
ing strategies and emotional well-being questionnaires. Spi-
nal Cord 2008; 46: 690695.
34. Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD
and Richardson GN. Quantifying handicap: a new measure
of long-term rehabilitation outcomes. Arch Phys Med Reha-
bil 1992; 73: 519526.
35. Burton L, Schulz R, Jackson S, Hirsch C and Zdaniuk B.
Transitions in spousal caregiving: experience from the
caregiver health effects study. Gerontologist 2000; 43:
230241.
36. Belle SH, Burgio L, Burns R, et al., for the Resources for
Enhancing Alzheimers Caregiver Health (REACH) II
Investigators. Enhancing the quality of life of dementia
caregivers from different ethnic or racial groups. Ann Intern
Med 2006; 145: 727738.
37. Hamilton BB, Granger CB, Sherwin FS, Zeilezny M and
Tashman JS. Uniform national data system for medi-
cal rehabilitation. In: Fuhrer MJ (ed.) Rehabilitation out-
comes: analysis and measurement. Baltimore, MD: Paul H.
Brookes Publishing, 1987, pp. 137147.
Dorstyn et al. 1083
38. Winefield HR, Winefield AH and Tiggeman M. Social sup-
port and psychological well-being in young adults. J Pers
Assess 1992; 58: 198210.
39. Kaplan BJ, Bush JW and Berry CC. Health status: types of
validity for the index of well-being. Health Serv Res 1976;
11: 478507.
40. Watson D, Clark LA and Tellegen A. Development and
validation of brief measures of positive and negative
affect: The PANAS scales. J Pers Soc Psychol 1988; 54:
10631070.
41. Herth K. Development and refinement of an instrument to
measure hope. Schol Inq Nurs Pract 1991; 5: 3951.
42. Miller JF and Power MJ. Development of an instrument to
measure hope. J Nurs Res 1988, 37: 610.
43. Chubon RA. Manual for the Life Satisfaction Survey.
Columbia, SC: University of South Carolina, School of
Medicine, Department of Neuropsychiatry and Behavior
Science, Rehabilitation Counseling Program, 1995.
44. Ware JE and Sherbourne CD. The MOS 36-item short-
form health survey (SF-46). Med Care 1992; 30:
473483.
45. International Wellbeing Group. Personal wellbeing index.
Melbourne, Australia: Australian Quality of Life, Deakin
University, 2006. www.deakin.edu.au/research/acqol/
instruments/wellbeing_index.htm (accessed 1 November
2012).
46. Jerusalem M and Schwarzer R. Self-efficacy as a resource
factor in stress-appraisal process. In: Schwarzer R (ed.)
Self-efficacy: thought control of action. Washington, DC:
Hemisphere, 1992: 195211.
47. Bombardier C, Bell KR, Temkin A, Fann JR, Hoffman JM
and Dikmen S. The efficacy of a scheduled telephone inter-
vention for ameliorating depressive symptoms during the
first year after traumatic brain injury. J Head Trauma Reha-
bil 2009; 24: 230238.
48. Bombardier C, Cunniffe M, Wadhwani R, Gibbons LE,
Blake KD and Kraft GH. The efficacy of telephone counsel-
ling for health promotion in people with multiple sclerosis:
a randomised controlled trial. Arch Phys Med Rehabil 2008;
89: 18491856.
49. Mohr DC, Likowsky W, Bertagnolli A, et al. Telephone-
administered cognitive behavioral therapy for the treatment
of depressive symptoms in multiple sclerosis. J Consult
Clin Psychol 2000; 68: 356361.
50. Kazdin AE and Blase SL. Rebooting psychotherapy
research and practice to reduce the burden of mental illness.
Perspect Psychol Sci 2011; 6: 2137.
51. Mozer E, Franklin B and Rose J. Psychotherapeutic inter-
vention by telephone. Clin Interv Aging 2008; 3: 391396.
52. Elliott TR and Berry JW. Brief problem solving training for
family caregivers of peresons with recent-onset spinal cord
injuries: a randomised controlled trial. J Clin Psychol 2009;
65: 406422.
53. Abdul Latif L, Daud Amadera JE, Pimentel D, Pimentel T
and Fregni F. Sample size calculation in physical medicine
and rehabilitation: a systematic review of reporting, char-
acteristics and results in randomised controlled trials. Arch
Phys Med Rehabil 2011; 92: 306315.
54. Tuszyinski MH, Steeves JD, Fawcett JW, et al. Guidelines
for the conduct of clinical trials for spinal cord injury as
developed by the ICCP panel: clinical trial inclusion/exclu-
sion criteria and ethics. Spinal Cord 2007; 45: 222231.
55. Nicholson Perry K and Middleton J. Comparison of a pain
management program with usual care in a pain management
centre for people with spinal cord injury-related chronic
pain. Clin J Pain 2010; 26: 206216.
Das könnte Ihnen auch gefallen
- Occupational Therapy and Physiotherapy Benefit The Acute Patient Pathway: A Mixed-Methods StudyDokument12 SeitenOccupational Therapy and Physiotherapy Benefit The Acute Patient Pathway: A Mixed-Methods StudyIlvita MayasariNoch keine Bewertungen
- A Telehealth Approach To Oropharyngeal Dysphagia TherapyDokument5 SeitenA Telehealth Approach To Oropharyngeal Dysphagia TherapyHeriberto Aguirre MenesesNoch keine Bewertungen
- Example of PHD Research ProposalDokument2 SeitenExample of PHD Research ProposalMuhammad Khurram ShahzadNoch keine Bewertungen
- Telehealth in Audiology: An Integrative ReviewDokument8 SeitenTelehealth in Audiology: An Integrative ReviewRUBÉN TOMÁS CRUZNoch keine Bewertungen
- Content ServerDokument14 SeitenContent ServerDilfera HermiatiNoch keine Bewertungen
- Prelim Exam Block 2 Group 3Dokument5 SeitenPrelim Exam Block 2 Group 3Sufina AnnNoch keine Bewertungen
- Metaanalisis Castro Et Al. 2019Dokument37 SeitenMetaanalisis Castro Et Al. 2019LauraNoch keine Bewertungen
- Bommersbach (2021) - Mental Health Staff Perceptions of Improvement Opportunities Around Covid 19Dokument14 SeitenBommersbach (2021) - Mental Health Staff Perceptions of Improvement Opportunities Around Covid 19Maximiliano AzconaNoch keine Bewertungen
- Martino, D. (2023) - Treatment Failure in Persisten Tic Disorders...Dokument15 SeitenMartino, D. (2023) - Treatment Failure in Persisten Tic Disorders...cuautzinNoch keine Bewertungen
- Evaluation of An Interdisciplinary Screening Program For People With Parkinson Disease and Movement DisordersDokument10 SeitenEvaluation of An Interdisciplinary Screening Program For People With Parkinson Disease and Movement DisordersAbu Faris Al-MandariNoch keine Bewertungen
- BMC Pediatrics: Effectiveness of Physical Therapy Interventions For Children With Cerebral Palsy: A Systematic ReviewDokument10 SeitenBMC Pediatrics: Effectiveness of Physical Therapy Interventions For Children With Cerebral Palsy: A Systematic ReviewERICKNoch keine Bewertungen
- Yjmt 30 1992090Dokument13 SeitenYjmt 30 1992090Luis Sebastian Arango OspinaNoch keine Bewertungen
- A Treatment Schedule of Conventional Physical Therapy Provided To Enhance Upper Limb Sensorimotor Recovery After Stroke Expert Criterion Validity and Intra-Rater ReliabilityDokument10 SeitenA Treatment Schedule of Conventional Physical Therapy Provided To Enhance Upper Limb Sensorimotor Recovery After Stroke Expert Criterion Validity and Intra-Rater ReliabilityGeraldo MoraesNoch keine Bewertungen
- Impact - Ijranss-1. Ijranss - Length of Stay Reporting in Forensic Secure Care Can Be Augmented by An Overarching Framework To Map Patient Journey in Mentally Disordered Offender Pathway ForDokument38 SeitenImpact - Ijranss-1. Ijranss - Length of Stay Reporting in Forensic Secure Care Can Be Augmented by An Overarching Framework To Map Patient Journey in Mentally Disordered Offender Pathway ForImpact JournalsNoch keine Bewertungen
- Disfagia OFDokument13 SeitenDisfagia OFSebastián Contreras CubillosNoch keine Bewertungen
- Telehealth RirinDokument12 SeitenTelehealth RirinririnsityalfiahNoch keine Bewertungen
- Effects of Internet-Based Psycho-Educational Interventions On Mental Health and Quality of Life Among Cancer PatientsDokument12 SeitenEffects of Internet-Based Psycho-Educational Interventions On Mental Health and Quality of Life Among Cancer PatientsflorgilNoch keine Bewertungen
- NGC 8208Dokument12 SeitenNGC 8208Alvaro Carlos Calvo ValenciaNoch keine Bewertungen
- Investigating The Preferences of Older People For Telehealth As A New Model of Health Care Service Delivery: A Discrete Choice ExperimentDokument13 SeitenInvestigating The Preferences of Older People For Telehealth As A New Model of Health Care Service Delivery: A Discrete Choice Experimenttherese BNoch keine Bewertungen
- Health Care Professionals' Experiences and Perspectives On Using Telehealth For Home-Based Palliative Care: Protocol For A Scoping ReviewDokument7 SeitenHealth Care Professionals' Experiences and Perspectives On Using Telehealth For Home-Based Palliative Care: Protocol For A Scoping Reviewshaza ameliaNoch keine Bewertungen
- Complementary Therapies in Clinical PracticeDokument18 SeitenComplementary Therapies in Clinical PracticeNgaWa ChowNoch keine Bewertungen
- Homebasedtelehealth PDFDokument6 SeitenHomebasedtelehealth PDFdaniel serraniNoch keine Bewertungen
- Putting Life in Years Pliny Telephone Friendship Groups Research Study Pilot Randomised Controlled TrialDokument12 SeitenPutting Life in Years Pliny Telephone Friendship Groups Research Study Pilot Randomised Controlled TrialMahmoud Abd ElazizNoch keine Bewertungen
- J Telemed Telecare 2011 Steel 109 17Dokument10 SeitenJ Telemed Telecare 2011 Steel 109 17LoguitosNoch keine Bewertungen
- Adherence Interventions and Outcomes of Tuberculosis Treatment in Low - and Middle-Income Countries (Lmic) : A Systematic Review ProtocolDokument6 SeitenAdherence Interventions and Outcomes of Tuberculosis Treatment in Low - and Middle-Income Countries (Lmic) : A Systematic Review Protocolijmb333Noch keine Bewertungen
- Applied Sciences: Post-Tuberculosis (TB) Treatment: The Role of Surgery and RehabilitationDokument18 SeitenApplied Sciences: Post-Tuberculosis (TB) Treatment: The Role of Surgery and Rehabilitationraja yasminNoch keine Bewertungen
- Acceptance and Commitment Therapy in Cancer: Review of Applications and FindingsDokument27 SeitenAcceptance and Commitment Therapy in Cancer: Review of Applications and FindingsJuan Alberto GonzálezNoch keine Bewertungen
- Comparing Digital To Conventional Physical Therapy For ChronicDokument18 SeitenComparing Digital To Conventional Physical Therapy For ChronickiranNoch keine Bewertungen
- Carlozzi-14 RS Outcomes HDDokument20 SeitenCarlozzi-14 RS Outcomes HDMARIA MONTSERRAT SOMOZA MONCADANoch keine Bewertungen
- A Study of Proactive Ethics Consultation For CriticallyDokument18 SeitenA Study of Proactive Ethics Consultation For CriticallyJENIFER KARINA PUTZ LORENZINoch keine Bewertungen
- Lung HN CancerDokument11 SeitenLung HN CancerFlorinaNoch keine Bewertungen
- Intensive & Critical Care Nursing: Ziad Alostaz, Louise Rose, Sangeeta Mehta, Linda Johnston, Craig DaleDokument11 SeitenIntensive & Critical Care Nursing: Ziad Alostaz, Louise Rose, Sangeeta Mehta, Linda Johnston, Craig DalecindyNoch keine Bewertungen
- Oropharyngeal and Tongue Exercises (Myofunctional Therapy) For Snoring: A Systematic Review and Meta-AnalysisDokument7 SeitenOropharyngeal and Tongue Exercises (Myofunctional Therapy) For Snoring: A Systematic Review and Meta-AnalysissirahNoch keine Bewertungen
- Journal Homepage: - : Introduction:-Objectives of The StudyDokument4 SeitenJournal Homepage: - : Introduction:-Objectives of The StudyIJAR JOURNALNoch keine Bewertungen
- Telepsiquiatria Meta Analisis 1Dokument11 SeitenTelepsiquiatria Meta Analisis 1daniel serraniNoch keine Bewertungen
- Wong Et Al-2015-Health & Social Care in The CommunityDokument13 SeitenWong Et Al-2015-Health & Social Care in The CommunityJoNoch keine Bewertungen
- HayesCAREER SharedDokument24 SeitenHayesCAREER SharedZhongxing YuNoch keine Bewertungen
- Effectiveness of Telemedicine: A Systematic Review of ReviewsDokument31 SeitenEffectiveness of Telemedicine: A Systematic Review of ReviewsaNoch keine Bewertungen
- NT and Conventional Medicine PDFDokument10 SeitenNT and Conventional Medicine PDFneuralterapianetNoch keine Bewertungen
- Case Study #3Dokument26 SeitenCase Study #3Reshma MohabeirNoch keine Bewertungen
- Artigo Mobilização PrecoceDokument9 SeitenArtigo Mobilização PrecoceLuciana AlexandreNoch keine Bewertungen
- The Pain, Agitation, and Delirium Practice Guidelines For Adult Critically Ill Patients: A Post-Publication PerspectiveDokument9 SeitenThe Pain, Agitation, and Delirium Practice Guidelines For Adult Critically Ill Patients: A Post-Publication Perspectivedebby claudiNoch keine Bewertungen
- 1 s2.0 S1201971214017214 Main PDFDokument5 Seiten1 s2.0 S1201971214017214 Main PDFYohanna ekasntNoch keine Bewertungen
- Severe Head Injury Clinical PathwayDokument7 SeitenSevere Head Injury Clinical PathwaytheodoruskevinNoch keine Bewertungen
- A Network Meta-Analysis On The Effects of Information Technology Application On Preoperative Anxiety of PatientsDokument7 SeitenA Network Meta-Analysis On The Effects of Information Technology Application On Preoperative Anxiety of PatientsInternational Journal of Application or Innovation in Engineering & ManagementNoch keine Bewertungen
- Summary of Purposes and ObjectivesDokument19 SeitenSummary of Purposes and Objectivesrodolfo opido100% (1)
- Effect of TelenursingDokument17 SeitenEffect of Telenursingirma nur amaliaNoch keine Bewertungen
- Nursing 440 - Nursing Leadership and Innovation Paper October 2014Dokument12 SeitenNursing 440 - Nursing Leadership and Innovation Paper October 2014api-242437021Noch keine Bewertungen
- Mobile Health (Mhealth) Versus Clinic-Based Group Intervention For People With Serious Mental Illness: A Randomized Controlled TrialDokument8 SeitenMobile Health (Mhealth) Versus Clinic-Based Group Intervention For People With Serious Mental Illness: A Randomized Controlled TrialOlivia NasarreNoch keine Bewertungen
- A Systematic Review of Telehealth Applications in Audiology: OriginalDokument20 SeitenA Systematic Review of Telehealth Applications in Audiology: Originalaimen_riyadhNoch keine Bewertungen
- Mental Health Services Research Methodology 2002Dokument8 SeitenMental Health Services Research Methodology 2002Kats CoelloNoch keine Bewertungen
- Cost-Effectiveness of Early Intervention in First-Episode Psychosis: Economic Evaluation of A Randomised Controlled Trial (The OPUS Study)Dokument8 SeitenCost-Effectiveness of Early Intervention in First-Episode Psychosis: Economic Evaluation of A Randomised Controlled Trial (The OPUS Study)Carlos A Luna CruzNoch keine Bewertungen
- 2019 Cognitive Rehabilitation For Cancer Related Cognitive DisfunctionDokument27 Seiten2019 Cognitive Rehabilitation For Cancer Related Cognitive DisfunctionAlba Sueiro DominguezNoch keine Bewertungen
- Neurologist Communicationg The Diagnosis of ELADokument9 SeitenNeurologist Communicationg The Diagnosis of ELAHabib G. Moutran BarrosoNoch keine Bewertungen
- Perez Mengual, M. - s0134775 (Verslag)Dokument61 SeitenPerez Mengual, M. - s0134775 (Verslag)Silvio MoralesNoch keine Bewertungen
- Telesalud - FisioterapiaDokument8 SeitenTelesalud - FisioterapiaManuel OlarteNoch keine Bewertungen
- Published Researches in The Year 2010Dokument16 SeitenPublished Researches in The Year 2010hsrimediaNoch keine Bewertungen
- A Survey of Practice Patterns For Rehabilitation Post Elbow FractureDokument11 SeitenA Survey of Practice Patterns For Rehabilitation Post Elbow Fracturejeremy1roseNoch keine Bewertungen
- Truijen2022 Article EffectOfHome-basedVirtualRealiDokument12 SeitenTruijen2022 Article EffectOfHome-basedVirtualRealiSM199021Noch keine Bewertungen
- IV GaugesDokument1 SeiteIV Gaugesjustin_saneNoch keine Bewertungen
- Peptic UlcerrDokument3 SeitenPeptic Ulcerrjustin_saneNoch keine Bewertungen
- Injection Site Cheat Sheet PDFDokument2 SeitenInjection Site Cheat Sheet PDFjustin_sane100% (2)
- Common Drug Stems Cheat SheetDokument2 SeitenCommon Drug Stems Cheat SheetCharis Mae DimaculanganNoch keine Bewertungen
- Improving Postoperative Pain Management What Are.40Dokument6 SeitenImproving Postoperative Pain Management What Are.40Luz Adriana Flores PalafoxNoch keine Bewertungen
- Risk For Infection Pneumonia Nursing Care PlanDokument1 SeiteRisk For Infection Pneumonia Nursing Care Planjustin_sane100% (1)
- Microsoft Word - Pneumonia Education EnglishDokument9 SeitenMicrosoft Word - Pneumonia Education Englishjustin_saneNoch keine Bewertungen
- HemodialysisDokument2 SeitenHemodialysisjustin_saneNoch keine Bewertungen
- DiagnosticDokument5 SeitenDiagnosticjustin_saneNoch keine Bewertungen
- Assessment Nursing Diagnosis Scientific Explanation Planning Interventions Rationale EvaluationDokument2 SeitenAssessment Nursing Diagnosis Scientific Explanation Planning Interventions Rationale Evaluationjustin_saneNoch keine Bewertungen
- 2 Acute Pain Chronic Renal Failure Nursing Care PlansDokument5 Seiten2 Acute Pain Chronic Renal Failure Nursing Care Plansjustin_saneNoch keine Bewertungen
- Hyperthermia Pneumonia Nursing Care PlanDokument1 SeiteHyperthermia Pneumonia Nursing Care Planjustin_saneNoch keine Bewertungen
- DMDokument10 SeitenDMjustin_saneNoch keine Bewertungen
- Physical AssessmentDokument29 SeitenPhysical Assessmentjustin_saneNoch keine Bewertungen
- PneumoniaDokument17 SeitenPneumoniajustin_saneNoch keine Bewertungen
- Ineffective Airway Clearance Pneumonia Nursing Care PlanDokument1 SeiteIneffective Airway Clearance Pneumonia Nursing Care Planjustin_sane100% (4)
- Other Possible Nursing Care PlansDokument1 SeiteOther Possible Nursing Care Plansjustin_saneNoch keine Bewertungen
- 2 Acute Pain Chronic Renal Failure Nursing Care PlansDokument5 Seiten2 Acute Pain Chronic Renal Failure Nursing Care Plansjustin_saneNoch keine Bewertungen
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDokument1 SeiteIneffective Breathing Pattern Pneumonia Nursing Care Planjustin_saneNoch keine Bewertungen
- 5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care PlansDokument3 Seiten5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care Plansjustin_sane40% (5)
- Chilldeck KTV & Music Lounge: Free Five (5) Songs in Every Three (3) Buckets of DrinksDokument1 SeiteChilldeck KTV & Music Lounge: Free Five (5) Songs in Every Three (3) Buckets of Drinksjustin_saneNoch keine Bewertungen
- Risk For Infection Pneumonia Nursing Care PlanDokument1 SeiteRisk For Infection Pneumonia Nursing Care Planjustin_sane100% (1)
- Impaired Gas Exchange Pneumonia Nursing Care PlanDokument1 SeiteImpaired Gas Exchange Pneumonia Nursing Care Planjustin_saneNoch keine Bewertungen
- Air Passenger Bill of RightsDokument12 SeitenAir Passenger Bill of RightsAldan Subion Avila100% (1)
- High-Rise Climb V0.6a Smokeydots PDFDokument10 SeitenHigh-Rise Climb V0.6a Smokeydots PDFHer Lan ONoch keine Bewertungen
- X25Dokument10 SeitenX25RajNoch keine Bewertungen
- Service Bulletin: Service Bulletin NUMBER: 8.8/134A Caterpillar: Confidential Green Page 1 of 8Dokument8 SeitenService Bulletin: Service Bulletin NUMBER: 8.8/134A Caterpillar: Confidential Green Page 1 of 8GutsavoNoch keine Bewertungen
- Standard C4C End User GuideDokument259 SeitenStandard C4C End User GuideKanali PaariNoch keine Bewertungen
- Marketing Research ProjectDokument37 SeitenMarketing Research ProjectVijay100% (15)
- AKROLEN® PP ICF 30 AM Black (8344) - Akro-PlasticDokument3 SeitenAKROLEN® PP ICF 30 AM Black (8344) - Akro-PlasticalkhalidibaiderNoch keine Bewertungen
- Exit Exam Plan (New)Dokument2 SeitenExit Exam Plan (New)Eleni Semenhi100% (1)
- Table of Contents - YmodDokument4 SeitenTable of Contents - YmodDr.Prakher SainiNoch keine Bewertungen
- Calio Z: Type Series BookletDokument24 SeitenCalio Z: Type Series BookletDan PopescuNoch keine Bewertungen
- SS 531 2006 Code of Practice For Lighting of Work Places Part 1 PDFDokument13 SeitenSS 531 2006 Code of Practice For Lighting of Work Places Part 1 PDFEdmund YoongNoch keine Bewertungen
- DPS Ibak en PDFDokument9 SeitenDPS Ibak en PDFjsenadNoch keine Bewertungen
- EquisetopsidaDokument4 SeitenEquisetopsidax456456456xNoch keine Bewertungen
- Product Management GemsDokument14 SeitenProduct Management GemsVijendra GopaNoch keine Bewertungen
- 1.2 Server Operating SystemDokument20 Seiten1.2 Server Operating SystemAzhar AhmadNoch keine Bewertungen
- Design of Footing (Square FTG.) : M Say, L 3.75Dokument2 SeitenDesign of Footing (Square FTG.) : M Say, L 3.75victoriaNoch keine Bewertungen
- A Study of A Skirtless Hovercraft DesignDokument71 SeitenA Study of A Skirtless Hovercraft DesignSunil Kumar P GNoch keine Bewertungen
- Role of SpeakerDokument11 SeitenRole of SpeakerSnehil AnandNoch keine Bewertungen
- Bromate Prove Ulr en 2016-01-06 HintDokument3 SeitenBromate Prove Ulr en 2016-01-06 Hinttata_77Noch keine Bewertungen
- Exercises Service CostingDokument2 SeitenExercises Service Costingashikin dzulNoch keine Bewertungen
- Guide To Downloading and Installing The WebMethods Free Trial Version - Wiki - CommunitiesDokument19 SeitenGuide To Downloading and Installing The WebMethods Free Trial Version - Wiki - CommunitiesHieu NguyenNoch keine Bewertungen
- Reliability EngineerDokument1 SeiteReliability EngineerBesuidenhout Engineering Solutions and ConsultingNoch keine Bewertungen
- Plasticizers For CPE ElastomersDokument8 SeitenPlasticizers For CPE Elastomersbatur42Noch keine Bewertungen
- Vigi Module Selection PDFDokument1 SeiteVigi Module Selection PDFrt1973Noch keine Bewertungen
- Microstrip Antennas: How Do They Work?Dokument2 SeitenMicrostrip Antennas: How Do They Work?Tebogo SekgwamaNoch keine Bewertungen
- Series 90 100cc Pump Parts ManualDokument152 SeitenSeries 90 100cc Pump Parts ManualHernan Garcia67% (3)
- Solution Manual For Labor Relations Development Structure Process 12th Edition Fossum 0077862473 9780077862473Dokument16 SeitenSolution Manual For Labor Relations Development Structure Process 12th Edition Fossum 0077862473 9780077862473savannahzavalaxodtfznisq100% (27)
- Introduction To AccountingDokument36 SeitenIntroduction To AccountingRajnikant PatelNoch keine Bewertungen
- Termsconditions of JionetDokument3 SeitenTermsconditions of JionetskNoch keine Bewertungen
- (English) 362L Stereoselective Wittig Reaction - Synthesis of Ethyl Trans-Cinnamate (#7) (DownSub - Com)Dokument6 Seiten(English) 362L Stereoselective Wittig Reaction - Synthesis of Ethyl Trans-Cinnamate (#7) (DownSub - Com)moNoch keine Bewertungen
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeVon EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeBewertung: 4.5 von 5 Sternen4.5/5 (141)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsVon EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsBewertung: 4.5 von 5 Sternen4.5/5 (39)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisVon EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (9)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryVon EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryBewertung: 4.5 von 5 Sternen4.5/5 (157)
- Don't Panic: Taking Control of Anxiety AttacksVon EverandDon't Panic: Taking Control of Anxiety AttacksBewertung: 4 von 5 Sternen4/5 (12)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDVon EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDBewertung: 4.5 von 5 Sternen4.5/5 (167)
- An Autobiography of Trauma: A Healing JourneyVon EverandAn Autobiography of Trauma: A Healing JourneyBewertung: 5 von 5 Sternen5/5 (2)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveVon EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveBewertung: 4 von 5 Sternen4/5 (250)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeVon EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeBewertung: 4.5 von 5 Sternen4.5/5 (49)
- Redefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackVon EverandRedefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackBewertung: 4.5 von 5 Sternen4.5/5 (153)
- Breaking the Chains of Transgenerational Trauma: My Journey from Surviving to ThrivingVon EverandBreaking the Chains of Transgenerational Trauma: My Journey from Surviving to ThrivingBewertung: 4.5 von 5 Sternen4.5/5 (30)
- Feeling Great: The Revolutionary New Treatment for Depression and AnxietyVon EverandFeeling Great: The Revolutionary New Treatment for Depression and AnxietyNoch keine Bewertungen
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisVon EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisBewertung: 5 von 5 Sternen5/5 (5)
- The Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItVon EverandThe Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItBewertung: 4.5 von 5 Sternen4.5/5 (107)
- Happiness Hypothesis, The, by Jonathan Haidt - Book SummaryVon EverandHappiness Hypothesis, The, by Jonathan Haidt - Book SummaryBewertung: 4.5 von 5 Sternen4.5/5 (95)
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouVon EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouNoch keine Bewertungen
- Overcoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsVon EverandOvercoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsBewertung: 4.5 von 5 Sternen4.5/5 (48)
- A Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentVon EverandA Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentNoch keine Bewertungen
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionVon EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNoch keine Bewertungen
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesVon EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesBewertung: 5 von 5 Sternen5/5 (70)
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationVon EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationBewertung: 5 von 5 Sternen5/5 (9)
- It's All Too Much: An Easy Plan for Living a Richer Life with Less StuffVon EverandIt's All Too Much: An Easy Plan for Living a Richer Life with Less StuffBewertung: 4 von 5 Sternen4/5 (232)
- Taking Charge of Adult ADHD, Second Edition: Proven Strategies to Succeed at Work, at Home, and in RelationshipsVon EverandTaking Charge of Adult ADHD, Second Edition: Proven Strategies to Succeed at Work, at Home, and in RelationshipsBewertung: 4.5 von 5 Sternen4.5/5 (25)
- Beyond Thoughts: An Exploration Of Who We Are Beyond Our MindsVon EverandBeyond Thoughts: An Exploration Of Who We Are Beyond Our MindsBewertung: 4.5 von 5 Sternen4.5/5 (7)
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeVon EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeBewertung: 5 von 5 Sternen5/5 (560)