Beruflich Dokumente
Kultur Dokumente
Self-Efficacy in Relation To Impairments and Activities of Daily Living Disability in Elderly Patients With Stroke: A Prospective Investigation
Hochgeladen von
UliuliauliaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Self-Efficacy in Relation To Impairments and Activities of Daily Living Disability in Elderly Patients With Stroke: A Prospective Investigation
Hochgeladen von
UliuliauliaCopyright:
Verfügbare Formate
J Rehabil Med 2003; 35: 202207
SELF-EFFICACY IN RELATION TO IMPAIRMENTS AND ACTIVITIES OF DAILY LIVING DISABILITY IN ELDERLY PATIENTS WITH STROKE: A PROSPECTIVE INVESTIGATION
Karin Hellstro m,1,2 Birgitta Lindmark,2 Birgit Wahlberg3 and Axel R. Fugl-Meyer1
From the 1Department of Neuroscience, Rehabilitation Medicine, Uppsala University, 2Department of Neuroscience, Section of Physiotherapy, Uppsala University, 3Geriatric Physiotherapy Section, University Hospital, Uppsala, Sweden
Objectives: The objectives of this prospective study, undertaken in elderly patients with stroke undergoing rehabilitation, were to determine to what extent fall-related selfefcacy changes over time, its relationships to objectively assessed functions and activities, and the predictive capacity of self-efcacy at discharge for activities of daily living 10 months after stroke. Methods: The study comprised 37 patients, aged 6689 years. Main outcome measurement instruments were the Falls Efcacy Scale (Swedish version), Berg Balance Scale and Functional Independence Measure. Results: Signicant improvements occurred in all these measures from admission to discharge, but patients with low self-efcacy at discharge showed less pronounced improvements than those with high self-efcacy. Falls Efcacy Scale (Swedish version) was closely associated with all other measures and was a more powerful predictor of activities of daily living than the observer-based measures of balance. Conclusion: To minimize dependence in activities of daily living, rehabilitation interventions should incorporate selfefcacy enhancement.
Key words: self-efficacy, fear of falling, stroke, balance, activities of daily living, motor function, ambulation. J Rehabil Med 2003; 35: 202207 Correspondence address: Karin Hellstro m, Section of Physiotherapy, University Hospital, Entrance 15, SE-751 85, Uppsala, Sweden. E-mail: karin.hellstrom@sjukgym.uu.se Submitted December 12, 2001; accepted January 31, 2003
decline, as fear may limit a persons function to an extent beyond that due to an underlying impairment of physical ability alone (4). Self-efcacy is a central concept in Banduras Social Cognitive Theory (5), and is dened as the degree of condence possessed by persons in their ability to perform specic acts successfully. Perceived self-efcacy is thought to be domainspecic; that is, it pertains to a specic behaviour in a particular context and cannot necessarily be generalized to other behaviours or other contexts (5). In Banduras perspective of the Social Cognitive Theory, behaviours most relevant to the domain of activity limitation consist primarily of self-care tasks, including personal activities of daily living (PADL) and instrumental activities of daily living (IADL). According to this theory, perceived self-efcacy beliefs regarding self-care behaviours should inuence the likelihood that such behaviours will be undertaken; thus low self-efcacy should predict greater disability. As an aid in preventing limitation of activity in elderly stroke victims, it would be useful to be able to identify factors contributing to decreased performance of routine activities of daily living (ADL). One of the specic aims of this prospective study was to determine, in elderly stroke patients, the extent to which fallsefcacy changes over time, and to assess the relationships of falls-efcacy to objectively assessed function (balance and motor function) and the ability to perform simple ADLs. A further aim was to estimate the extent to which the degree of self-efcacy at discharge from subacute geriatric rehabilitation can be a meaningful predictor for the level of gross ADL 10 months after the onset of stroke.
INTRODUCTION
The overall aim of this longitudinal study was to gauge the relevance of measuring perceived self-efcacy, in terms of fallsefcacy, in geriatric stroke rehabilitation. After stroke, many patients experience a decline in their dynamic and static balance. This can lead to an increased risk of falling, and in particular may result in fear of falling (1, 2). Fear of falling is common among elderly persons, both those who have and have not experienced a fall (3). Fall-related selfefcacy is a psychological characteristic, based on the selfefcacy concept, that can have an inuence on functional
2003 Taylor & Francis. ISSN 16501977 DOI 10.1080/16501970310000836 Subjects
SUBJECTS AND METHODS
A total of 146 patients with conrmed stroke were admitted consecutively for rehabilitation to a geriatric rehabilitation department between December 1, 1999 and January 31, 2001. Of these 146 patients, 60 (42%) met the following criteria for inclusion in the study: older than 65 years; rst ever stroke; interval since stroke of less than 8 weeks; able to communicate and understand instructions; no other severe disabilities that might hinder their training; and lived less than 50 kilometres from the participating hospital. Of these 60 patients, 12 declined and 7 were not asked to participate, leaving 41 patients. During the course of the investigation 4 further patients were lost to the study, giving a nal selected stroke sample of 37 subjects. Table I gives some pertinent descriptions of the population. J Rehabil Med 35
Self-efficacy in elderly patients with stroke
Table I. Characteristics of the patients (n = 37) Variable Age (years, mean (SD)) Days post onset on admission (mean (SD)) Length of in-patient stay (mean (range)) Female/male (n) Stroke types Stroke site Motor decits* Walking ability (n) Measurement
203
78 (5.5) 22 (6.6) 20 (15.0) (868 days) 15/22 CI 29, ICH 7, SH 1 Right 9, Left 25, Brainstem 2, Cerebellum 1 Massive 10, Marked 5, Moderate 11, Mild 9, None 2 None 12, With aid 19, Independent 6
* Classication according to Fugl-Meyer (12). Scores between 0 and 50 = massive hemiplegia, scores between 51 and 84 = marked motor impairment, scores between 85 and 95 = moderate impairment, scores between 96 and 99 = mild impairment, a score of 100 = normal motor function. CI = cerebral infarction; ICH = intracerebral haemorrhage; SH = subarachnoid haemorrhage.
The Ethical Committee of the Faculty of Medicine at the University of Uppsala approved the investigation. Procedures Assessments were made on entry into the study (admission), at discharge and 10 months after stroke. Follow-up assessment was conducted at home or at the rehabilitation department. Measurements were performed by one and the same physiotherapist, who was not involved in the treatment of the patients. Rehabilitative interventions were not standardized or in any way controlled. Each subject received all available interventions provided by the members of the geriatric rehabilitation unit team according to his or her individual needs. These interventions included medical, nursing, social and therapeutic interventions. The therapeutic interventions were designed by occupational therapists and physiotherapists following assessment of each individual and could include training in ADL, balance, mobility and low intensity strengthening. No specic training aimed at increasing self-efcacy was carried out. Assessment instruments In the present study only instruments with established reliability and validity were used. Falls-efcacy was measured with the FES(S) (6), a modied version of the Falls Efcacy Scale (7) described previously in our reports (6, 8, 9). FES(S) assesses an individuals perceived condence in task performance without falling in 13 items common in everyday life. The scale is divided into 2 subscales, 1 encompassing PADL (items 16) and 1 covering IADL (items 813). Item 7 (walking up and down stairs) is regarded as an intermediate item. The condence in performing each activity without falling was rated on a visual analogue scale from 0 to 10 varying from not at all condent to completely condent, giving a possible total score of 130. The maximal possible score for PADL and for IADL is 60. The FES(S) has a high test-retest reliability for the total scale (intra-class correlation, ICC = 0.97) and for the subscales PADL (ICC = 0.93) and IADL (ICC = 0.97) (20). The internal consistency of the instrument, expressed as Cronbachs alpha, is between 0.92 and 0.95 both for the subscales and for the overall scale (8). The FES(S) has been shown to be sufciently responsive to indicate changes during the subacute rehabilitation period (9). Balance was measured both with the Berg Balance Scale (BBS) (10) and with the balance subscale of the Fugl-Meyer Stroke Assessment Instrument (FMB) (11). The former encompasses 14 items. Each item is scored 04, giving a possible aggregated total score of 56. The latter, is a 7-item test for bedside use, particularly for assessment of sitting and standing balance after stroke. A 3-point scale (02) is applied to each item, providing a maximal possible aggregated score of 14. For evaluation of motor function, the Fugl-Meyer Stroke Assessment Instrument was used (11, 12). Each of 50 functions is rated on a 3-point scale (02). The minimum possible aggregated score is thus 0 and the maximum is 100. The Functional Ambulation Classication (FAC) (13, 14) was applied in order to document walking ability. The test includes 6 categories of walking ability. Level 0 describes a patient who cannot walk or requires
help of 2 or more people to walk. At level 5, the subject can walk independently anywhere. The Functional Independence Measure (FIMTM) (15), manual number 4.0 of the Swedish translation, was used to measure level of ADL disability. Each of 18 items is rated on a 7-point scale along a continuum from 1 (total assistance needed) to 7 (complete independence), yielding an aggregated score from 18 to 126. The areas measured are basic selfcare or ADL, sphincter control, transfers, locomotion, communication and social cognition. In the present investigation the areas of communication and social cognition were excluded; thus FIM motor comprised the sections of self-care, sphincter control, transfers and locomotion, giving a possible score ranging from 13 to 91. An FIM mobility score included only transfers and locomotion with a score between 5 and 35. Statistics The SPSSTM version 10.0 was used for all analyses. As all instruments in the study used ordinal scales, non-parametric statistics were generally applied, namely Spearmans rho to examine the associations between the FES(S) and the other measurements, the Mann-Whitney U test to assess differences between groups, and Wilcoxons signed-rank test to assess the level of signicance of changes. The level of statistical signicance was set at p < 0.01 for all tests, as a large number of independent tests were performed and this could lead to a relatively high risk of type I errors. Based on earlier research (16) regarding self-efcacy and disability, we decided to assign all patients retrospectively into 2 different groups on the basis of their falls-efcacy scores (FES(S) total) at discharge. Patients who scored above the group median were assigned to a high self-efcacy group, and those scoring below the median were assigned to a low self-efcacy group. The scores of the new groups were then analysed for differences on admission, at discharge and at 10-month follow-up. Linear multiple regression was performed to analyse the predictive effects of variables at discharge on ADL disability at follow-up as dened by the FIM motor and FIM mobility scores. Relationships between the predictive factors and outcome variables were rst explored by calculating the Pearson product-moment correlation coefcients. To select variables to include in the multivariate regression model the backward selection method was used. The following variables were screened: age, gender, stroke type, BBS, FMB, FES(S) total. FIM motor and FIM mobility were included in respectively model.
RESULTS
For all the objective motor and balance scores, the 2 FIM scores and all 3 FES(S) measures, Wilcoxons signed rank test showed signicant improvements from admission to discharge, and further signicant improvements from discharge to follow-up occurred for all measures except for FES(S) total, FES(S) PADL, motor function and FMB (Table II).
J Rehabil Med 35
204
K. Hellstro m et al.
Table II. Median values and ranges for condence in task performance (FES(S)), motor function, balance (BBS; FMB), ambulation (FAC) and ADL (FIM) on admission (A), on discharge (D) and at 10-months follow-up (F). Level of signicance given for differences between time points (n = 37) Variable FES(S) Total FES(S) PADL FES(S) IADL Motor function BBS FMB FAC FIM: Motor FIM: Mobility Admission median (Q1Q3) 47.0 32.0 15.0 91.0 36.0 10.0 3.0 58.0 18.0 (13104)*** (1153)** (045)*** (3397)*** (841)*** (810)* (04)*** (4075)*** (1330)*** Discharge median (Q1Q3) 79.0 45.0 27.0 96.0 40.0 10.0 4.0 85.0 32.0 (43113) (2853) (1354)**** (7599) (2149)**** (911) (45)***** (6690)***** (2635)***** Follow-up median (Q1Q3) 100.0 52.0 37.0 95.0 45.0 10.0 5.0 89.0 34.0 (44129) (2960) (1660) (80100) (2552) (1012) (45) (8091) (2835)
* p < 0.01, ** p < 0.001, *** p < 0.0001 admission vs discharge, **** p < 0.001, ***** p < 0.001 discharge vs follow-up. FES(S) = falls efcacy scale (Swedish version); BBS = Berg balance scale; FMB = Fugal-Meyer stroke assessment balance instrument; FAC = functional ambulation classication; ADL = activities of daily living; PADL = personal ADL; IADL = instrumental ADL; FIM = functional independence measure.
Neither on admission nor at discharge were there any signicant differences in scores in relation to age (dichotomized into 80 years of age or older vs those younger), gender or side of lesion. At follow-up the older group of patients had signicantly lower balance (BBS and FMB p < 0.001, and 0.01 respectively) than the younger group. Relations between perceived condence, balance, ambulation and ADL At all 3 assessment times all concurrent correlations between FES(S) and the other measures related signicantly, with rho ranging from 0.53 (p < 0.01) to 0.87 (p < 0.001). The BBS scores and the ambulation scores were relatively most closely correlated with FES(S) both on admission and at discharge, while at follow-up the total FIM score showed the greatest correlation with both FES(S) total and FES(S) PADL. All initial FES(S) scores correlated signicantly with both discharge and follow-up balance, ambulation and ADL scores (rho = 0.56 0.81). Discharge FES(S) scores were also correlated signicantly with follow-up scores (from rho = 0.49 between FES(S)
PADL at discharge and FMB at follow-up to rho = 0.82 between FES(S) IADL at discharge and FAC at follow-up).
Low and high self-efcacy Nineteen patients were assigned to the group with low selfefcacy, i.e. their FES(S) total scores at discharge were below the median score of 79, and 18 patients with scores above the median were assigned to the high self-efcacy group. The Mann-Whitney U test indicated that these 2 groups did not differ signicantly in age, gender, diagnosis or length of time since stroke onset (p > 0.05). Patients with low falls-efcacy at discharge had signicantly lower scores than those with high falls-efcacy concerning balance (p < 0.01) and locomotion (p < 0.01) on admission (Table III). At discharge and follow-up signicant and more pronounced differences were evident between the 2 groups with lower values for balance (p < 0.0001), locomotion (p < 0.0001), and both FIM motor and FIM mobility (p < 0.0001) in the group with low selfefcacy at discharge.
Table III. Median values and ranges for motor function, balance, locomotion and ADL in the groups with low and high self-efcacy at discharge. Low self-efcacy = FES(S) values below or at median (n = 19); high self-efcacy = FES(S) values above median (n = 18). p values are given for differences between groups Admission Self-efcacy Measure Motor function Balance (BBS) Balance (FMB) Locomotion (FAC) ADL total (FIM) ADL mobility (FIM) Low 60.0 21.0 8.0 2.0 47.0 17.0 (1699) (344) (410) (05) (1387) (532) High 95.0 39.0 10.0 4.0 71.0 27.0 (2591) (556)* (714)* (05)* (3291) (1235) Discharge Self-efcacy Low 90.0 28.0 10.0 4.0 75.0 27.0 (9100) (448) (414) (05) (2591) (635) High 95.0 48.0 10.0 5.0 87.0 34.0 (31100) (1356)*** (814) (45)*** (7291)** (2835) Follow-up Low 85.0 25.0 10.0 4.0 80.0 28.0 (3100) (351) (413) (05) (3891) (835) High 99.0 50.0 11.0 5.0 91.0 35.0 (47100) (1356)*** (714)* (45)*** (8491)*** (3335)***
* p < 0.01, ** p < 0.001 and *** p < 0.0001 for low vs high. ADL = activities of daily living; FES(S) = falls efcacy scale (Swedish version); BBS = Berg balance scale; FMB = Fugal-Meyer stroke assessment balance instrument; FAC = functional ambulation classication; FIM = functional independence measure.
J Rehabil Med 35
Self-efficacy in elderly patients with stroke
205
Table IV. Correlation coefcients between predictor variables measured at discharge and ADL disability 10 months post-stroke (n = 37) Outcome: FIM motor 10 months post-stroke Predictor variables Age Gender Diagnosis BBS FMB FES(S) total FIM motor FIM mobility Correlation coefcient 0.34 0.17 0.01 0.72 0.63 0.73 0.81 p-value 0.04 0.49 0.95 0.000 0.000 0.000 0.000 Outcome: FIM mobility 10 months post-stroke Correlation coefcient 0.39 0.16 0.03 0.72 0.67 0.74 0.85 p-value 0.02 0.34 0.87 0.000 0.000 0.000 0.000
ADL = activities of daily living; BBS = Berg balance scale; FMB = Fugal-Meyer stroke assessment balance instrument; FES(S) = falls efcacy scale (Swedish version); FIM = functional independence measure.
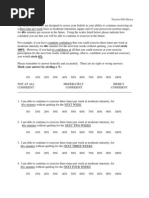
Prediction of disability of ADL Table IV summarizes the correlation coefcients of background and predictor variables, measured at discharge, with the outcome 10 months post-stroke. To adjust for potential non-
linear associations, second-order term FES(S)**2 of the independent variables FES(S) total were included (see Fig. 1). The model which best predicted the level of ADL total at 10 months post-stroke included the variables FE(S) total, FES(S)**2 and FIM motor at discharge. This combination explained 77% of the variance of the outcome measure (Table V). FES (S) total accounted for the largest proportion of the variance. FIM mobility at 10 months was best explained by the combination of 4 predictor variables: FES motor, FES(S)**2, age and FIM mobility. This model accounted for 84.3% of the explained variance (Table V). Again, FES(S) total showed the highest unique contribution.
DISCUSSION
First it must be said that in this investigation the selected sample of elderly stroke patients should not be regarded as representative. However, the major nding in this study was that the independent variable FES(S) had the highest explanatory value for ADL disability 10 months after stroke. Furthermore, the ndings in the univariate analyses that there were close concurrent correlations at all points of measurement between the FES(S) and its subscales and all other types of measurement, and that the FES(S) measurements showed prospective (or predictive) close correlations with the other measures indicate that, although demonstrated in a small sample, FES(S) has acceptable predictive validity. The fact that the second order term of FES(S) was the major predictor indicates a non-linear correlation. This may perhaps best be explained by a ceiling effect of the dependent variable FIM motor. In most studies on predictors of ADL improvement, early predictors are identied in the acute stage. In a cross-validation study Lo fgren et al. (17) failed to identify a sufciently accurate model for predicting chances of late ADL improvement in stroke patients. Feys et al. (18) found that very early predictive accuracy diminished as predictions were made to a later stage in the recovery process, while assessments of variables at 2 and 6 months increased the percentage of explained variance at 12 months. Thus, accuracy in predicting ADL performance at follow-up can be improved substantially by using predictors obtained from discharge. Prediction variables such as admission disability, urinary
J Rehabil Med 35
Fig. 1. Scatterplot of the relation between the predictor variable: Falls Efcacy Scale Swedish FES(S) total at discharge and the outcome variables (a) FIM motor and (b) FIM mobility.
206
K. Hellstro m et al.
Table V. Selected models of regression analyses for the prediction of disability: FIM motor and FIM mobility at 10 months post-stroke from a clinical examination at discharge from geriatric rehabilitation (n = 38) FIM motor 10 months follow-up Model: R = 77.0% Predictors Constant FES(S) total FES(S)**2 FIM motor Beta 29.26 0.67 0.003 0.33 p-value <0.000 <0.000 0.002 0.008
2
FIM mobility 10 months follow-up Model: R2 = 84.3% Predictors Constant FES(S) total FES(S)**2 Age FIM mobility Beta 26.61 0.30 0.003 0.20 0.29 p-value 0.002 <0.000 <0.000 0.034 0.008
FIM = functional independence measure; FES(S) = falls efcacy scale (Swedish version).
continence, degree of motor impairment, age, orientation and level of consciousness, balance and perceived social reports have all been found to predict recovery after stroke (19) but we have located no studies in which the ability of self-efcacy to predict degree of independence in activities of daily living after stroke has been addressed. In community-residing elderly persons, Mendes de Leon et al. (20) found a signicant interaction between self-efcacy and change in physical performance. Female gender has been reported (3, 21) to be a signicant risk factor for developing fear of falling. However, we did not observe any differences in falls-related self-efcacy between men and women. Nor did we nd that patients with right hemispheric strokes, who are likely to have difculties in perception, had a particularly great fear of falling. It is well known that sub-acute improvement is common even in very elderly patients after stroke (22, 23), but the question of self-efcacy has been less well studied. However, the present ndings substantiate those of Robinson-Smith et al. (24), who, using another self-efcacy measure in a sample of 77 patients with a mean age of 71 years, demonstrated that self-care selfefcacy improved with time after stroke. In our study generally signicant improvements were found between discharge and follow-up with the exceptions of FES(S) total and FES(S) PADL. The absence of signicant improvements in FES(S) PADL may be explained by the fact that during the course of rehabilitation the patients had been trained in PADL to such a degree that they perceived adequate condence in these tasks at discharge. The present nding that at follow-up the low self-efcacy group showed a decline in motor function and balance, while the high self-efcacy group had increased their motor function and balance and the observation that the differences between the low and high self-efcacy groups increased over time, substantiate previous reports indicating that activity is related to level of selfefcacy (20). It may be argued that relatively more serious stroke would lead to a lower level of falls-efcacy. Although we cannot postulate with certainty that there were no differences in the severity of stroke, there were, in fact, no signicant differences in motor function between the 2 groups at any of the assessment times. It appears that older stroke patients with
J Rehabil Med 35
low condence in task performance are likely to have a poorer functional outcome and make less improvements than patients with high self-efcacy. After an acute event, high self-efcacy may help patients to regain their ability to perform activities of daily living, resulting in less ADL decline from their premorbid levels compared with individuals with low self-efcacy. This view is consistent with other observations on the inuence of self-efcacy in the recovery process (25, 26). It therefore seems that identication and treatment of low condence in task performance need to be considered in preventing decline and boosting further improvements.
CONCLUSION
Stroke patients admitted for geriatric rehabilitation made signicant overall improvements in measures of functions and abilities from admission to discharge, but patients with low selfefcacy at discharge showed less improvement than those with high self-efcacy. Self-efcacy, as measured by the FES(S) scale at discharge, was a powerful predictor of ADL performance 10 months post-stroke, indicating that the benet from rehabilitation interventions may increase by incorporation of self-efcacy into assessment and treatment.
ACKNOWLEDGEMENTS
The authors would like to thank the patients who participated in rdal the study. This study was funded by grants from the Va Foundation.
REFERENCES
1. Legters K. Fear of falling. Phys Ther 2002; 82: 264272. 2. Forster A, Yong J. Incidences and consequences of falls due to stroke: a systematic inquiry. BMJ 1995; 311: 8386. 3. Maki B, Holiday P, Topper A. Fear of falling and postural performance in the elderly. J Gerontol 1991; 46; 4: M123131. 4. Tinetti ME, Mendes de Leon CF, Doucete JT, Baker DJ. Fear of falling and fall related efcacy in relationship to functioning among community-living elders. J Gerontol 1994; 49: M140147. 5. Bandura A. Self-efcacy: the exercise of control. New York: WH Freeman and Co.; 1997.
Self-efficacy in elderly patients with stroke
6. Hellstro m K, Lindmark B. Fear of falling in patients with stroke: a reliability study. Clin Rehabil 1999; 13: 509517. 7. Tinetti ME, Richman D, Powell L. Falls efcacy as a measure of fear of falling. l J Gerontol 1990; 45: P239P243. 8. Hellstro m K, Nilsson L, Fugl-Meyer AR. Relationship of condence in task performance with balance and motor function after stroke. Physiother Theory Pract 2001; 17: 5565. 9. Hellstro m K, Lindmark B, Fugl-Meyer A. The falls efcacy scale, Swedish version: does it reect clinically meaningful changes after stroke? Disabil Rehabil 2002; 9: 471481. 10. Berg K, Wood-Dauphine e S, Williams SI. The balance scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med 1995; 27: 2736. 11. Fugl-Meyer AR, Ja a sko L, Leyman I, Olsson S, Steglind S. The poststroke hemiplegic patient. I: a method for evaluation of physical performance. Scand J Rehabil Med 1975; 7: 1331. 12. Fugl-Meyer AR. Post stroke hemiplegia assessment of physical properties. Scand J Rehabil Med Suppl 1980; 7: 5660. 13. Holden MK, Gill KM, Magliozzi MR. Clinical gait assessment in the neurologically impaired: reliability and meaningfulness. Phys Ther 1984; 64: 3540. 14. Holden MK, Gill KM, Magliozzi MR. Gait assessment for neurologically impaired patients: standards for outcome assessment. Phys Ther 1986; 66: 15301539. 15. Granger CV, Hamilton BB, Keith RA, Zielezny M, Sherwin FS. Advances in functional assessments for medical rehabilitation. Top Geriatr Rehabil 1986; 1: 5974. 16. So derlund A, Lindberg P. Cognitive behavioural components in physiotherapy management of chronic whiplash associated disorders (WAD)a randomized group study. Physiother Theory Pract 2001; 17: 229238. 17. Lo fgren B, Nyberg L, Mattson M, Gustafson Y. Three years after in-
207
18.
19. 20.
21. 22. 23. 24. 25. 26.
patient stroke rehabilitation: a follow-up study. Cerebro Vasc Dis 1999; 9: 163170. Feys H, De Weerdt W, Nuyens G, Van de Winckel A, Selz B, Kiekens C. Predicting motor recovery of the upper limb after stroke rehabilitation: value of clinical examination. Physiother Research Int 2000; 5: 118. Kwakkel G, Wagenaar RC, Kollen BJ, Lankhorst GJ. Predicting disability in strokea critical review of the literature. Age Ageing 1996; 25: 479489. Mendes de Leon C, Seeman T, Baker D, Richardson E, Tinetti E. Self-efcacy, physical decline, and change in functioning in community-living elders: a prospective study. J Gerontol: Soc Sci 1996; (51B); 4: S183190. Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age Ageing 1997; 26: 189193. Kong K-H, Chua KSG, Tow AP. Clinical characteristics and functional outcome of stroke patients 75 years and older. Arch Phys Med Rehabil 1998; 79: 15351539. sterlind PO, Gustafson Y. In patients Lo fgren B, Nyberg L, O rehabilitation after stroke: outcome and factors associated with improvement. Disabil Rehabil 1998; 20: 5561. Robinson-Smith G, Johnston MV, Allen J. Self-care self-efcacy, quality of life, and depression after stroke. Arch Phys Med Rehabil 2001; 81: 460464. Bandura A. Self-efcacy mechanisms in physiological activation and health-promotion behavior. In: Madden J, Matthysse S, Brchas J, eds. Adaptation, learning and affect. New York: Raven Press; 1992. Allegrante JP, Kovar PA, Mackenzie CR, Peterson M, Gutin B. A walking education programme for patients with osteoarthritis of the knee: theory and intervention strategies. Health Education Quarterly 1993; 20: 6381.
J Rehabil Med 35
Das könnte Ihnen auch gefallen
- Self-Care Self-Efficacy Correlates With Independence in Basic Activities of Daily Living in Individuals With Chronic StrokeDokument7 SeitenSelf-Care Self-Efficacy Correlates With Independence in Basic Activities of Daily Living in Individuals With Chronic StrokeSitti Rosdiana YahyaNoch keine Bewertungen
- Risk Factors Related To Falling in Stroke Patients: A Cross-Sectional StudyDokument3 SeitenRisk Factors Related To Falling in Stroke Patients: A Cross-Sectional StudyZilbran BerontaxNoch keine Bewertungen
- 3 158 1 PBDokument6 Seiten3 158 1 PBViista GiriNoch keine Bewertungen
- High Intensity Exercise For Walking Competency in Individuals With Stroke - A Systematic Review and Meta-AnalysisDokument16 SeitenHigh Intensity Exercise For Walking Competency in Individuals With Stroke - A Systematic Review and Meta-AnalysisSusana RodriguezNoch keine Bewertungen
- Comparison of Mini-Bestest and Dynamic Gait Index For Prediction of Fall Susceptibility in Old IndividualsDokument5 SeitenComparison of Mini-Bestest and Dynamic Gait Index For Prediction of Fall Susceptibility in Old IndividualsElahe SadeqiNoch keine Bewertungen
- Predicting The Probability For Fall Incidence in Stroke Patients Using The Berg Balance ScaleDokument8 SeitenPredicting The Probability For Fall Incidence in Stroke Patients Using The Berg Balance ScaleElahe SadeqiNoch keine Bewertungen
- Correlation Between Self-Efficacy With Activity of Daily Living On Post-Stroke Patients in TMS Clinic RSUD Dr. R. Koesma of TubanDokument7 SeitenCorrelation Between Self-Efficacy With Activity of Daily Living On Post-Stroke Patients in TMS Clinic RSUD Dr. R. Koesma of TubanIsmunandar wahyu KNoch keine Bewertungen
- Stroke Examination and InterventionDokument36 SeitenStroke Examination and InterventionMarikit2012Noch keine Bewertungen
- Functioning of Stroke Survivors - A Validation of The ICF Core Set For Stroke in SwedenDokument9 SeitenFunctioning of Stroke Survivors - A Validation of The ICF Core Set For Stroke in SwedenMuhammadMusa47Noch keine Bewertungen
- Physiotherapy Intervention in Alzheimer'sDokument12 SeitenPhysiotherapy Intervention in Alzheimer'sRestu AryaNoch keine Bewertungen
- Acl Rehab ProtocolDokument6 SeitenAcl Rehab ProtocolPricy DevNoch keine Bewertungen
- Review of Effects of Physical Activity On Strength, Balance, Mobility and ADL Performance in Elderly Subjects With DementiaDokument11 SeitenReview of Effects of Physical Activity On Strength, Balance, Mobility and ADL Performance in Elderly Subjects With DementiaAlejandra VasquezNoch keine Bewertungen
- Ms. Neelam Nayak Pranali Mahajan: BackgroundDokument6 SeitenMs. Neelam Nayak Pranali Mahajan: BackgroundYho Ghi GusnandaNoch keine Bewertungen
- Gye Yeop Kim Et Al 2014Dokument6 SeitenGye Yeop Kim Et Al 2014maria.castiyo2002Noch keine Bewertungen
- JIKSH: Jurnal Ilmiah Kesehatan Sandi HusadaDokument6 SeitenJIKSH: Jurnal Ilmiah Kesehatan Sandi HusadaIra ismawatiNoch keine Bewertungen
- Adobe Scan 02 Mar 2023Dokument18 SeitenAdobe Scan 02 Mar 2023ciptakarwanaNoch keine Bewertungen
- Body Weight-Supported Gait Training For Restoration of Walking in People With An Incomplete Spinal Cord Injury: A Systematic ReviewDokument7 SeitenBody Weight-Supported Gait Training For Restoration of Walking in People With An Incomplete Spinal Cord Injury: A Systematic ReviewInterSocial LinkNoch keine Bewertungen
- Headache YesterdayDokument7 SeitenHeadache Yesterdayaahmad87Noch keine Bewertungen
- Stroke 32Dokument8 SeitenStroke 32pokharelriwaj82Noch keine Bewertungen
- Kristenen, NeckmusclebalanceDokument9 SeitenKristenen, NeckmusclebalancePhooi Yee LauNoch keine Bewertungen
- Reliability of Gait Performance Tests in Men and Women With Hemiparesis After StrokeDokument8 SeitenReliability of Gait Performance Tests in Men and Women With Hemiparesis After StrokeKaniNoch keine Bewertungen
- Daily Living Self Efficacy ScaleDokument8 SeitenDaily Living Self Efficacy Scalespamemail00Noch keine Bewertungen
- Modified Rood's Approach and Ability of Independent Selfcare in Haemorrhagic Stroke Patients of Assam, IndiaDokument6 SeitenModified Rood's Approach and Ability of Independent Selfcare in Haemorrhagic Stroke Patients of Assam, Indianandhini raguNoch keine Bewertungen
- 2020 - Gait RehabilitationDokument8 Seiten2020 - Gait RehabilitationMargarida FonsecaNoch keine Bewertungen
- 1 KowalczykDokument6 Seiten1 KowalczykLuis Diego Verastegui LeguaNoch keine Bewertungen
- Krajewski Et Al, 2018Dokument6 SeitenKrajewski Et Al, 2018Rahmi LubisNoch keine Bewertungen
- Zimmerman 2008Dokument10 SeitenZimmerman 2008jgomezgNoch keine Bewertungen
- The Swedish Occupational Fatigue Inventory in People With Multiple SclerosisDokument7 SeitenThe Swedish Occupational Fatigue Inventory in People With Multiple SclerosisikrambahariNoch keine Bewertungen
- Ijerph 19 15199 v3Dokument13 SeitenIjerph 19 15199 v3soylahijadeunvampiroNoch keine Bewertungen
- 2021 - QoL in MSisdominated by Fatigue - Disability - Sefl-EfficacyDokument7 Seiten2021 - QoL in MSisdominated by Fatigue - Disability - Sefl-EfficacySM199021Noch keine Bewertungen
- How Often Should Sitting and Rising From A Chair Be Evaluated in Patients With Duchenne Muscular Dystrophy?Dokument6 SeitenHow Often Should Sitting and Rising From A Chair Be Evaluated in Patients With Duchenne Muscular Dystrophy?JoNoch keine Bewertungen
- 10 5923 J Stroke 20170501 01Dokument9 Seiten10 5923 J Stroke 20170501 01Cristian Florin CrasmaruNoch keine Bewertungen
- Effects of Exercise On Quality of Life in Stroke Survivors: A Meta-AnalysisDokument12 SeitenEffects of Exercise On Quality of Life in Stroke Survivors: A Meta-AnalysisNoor KameliaNoch keine Bewertungen
- 10.1093 PTJ Pzac153Dokument13 Seiten10.1093 PTJ Pzac153evelyn.minichNoch keine Bewertungen
- An 2016Dokument10 SeitenAn 2016fernando_a_gonzalezNoch keine Bewertungen
- Assessment of A Disease-Specific Muscular Impairment Rating Scale in Myotonic DystrophyDokument5 SeitenAssessment of A Disease-Specific Muscular Impairment Rating Scale in Myotonic DystrophyLovadi Emese IldikóNoch keine Bewertungen
- ArtikelDokument6 SeitenArtikeljeinzen14Noch keine Bewertungen
- The Effect of Task-Oriented Activities Training On UpperLimbDokument10 SeitenThe Effect of Task-Oriented Activities Training On UpperLimbbagasNoch keine Bewertungen
- Measurement Tools of StrokeDokument42 SeitenMeasurement Tools of StrokeDharam PandeyNoch keine Bewertungen
- 5 - Yadav Sunita. Correlation of Balance Tests Scores With Modified Physical Performance Test in Indian Community-Dwelling Older AdultsDokument19 Seiten5 - Yadav Sunita. Correlation of Balance Tests Scores With Modified Physical Performance Test in Indian Community-Dwelling Older AdultsDr. Krishna N. SharmaNoch keine Bewertungen
- tmp6E6F TMPDokument10 Seitentmp6E6F TMPFrontiersNoch keine Bewertungen
- Jurnal 1Dokument5 SeitenJurnal 1Fila IdieNoch keine Bewertungen
- Research in Developmental DisabilitiesDokument12 SeitenResearch in Developmental DisabilitiesRun CapNoch keine Bewertungen
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodVon EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNoch keine Bewertungen
- Ffects of Physical Exercise On Balance andDokument19 SeitenFfects of Physical Exercise On Balance andAlfiana ApriliaNoch keine Bewertungen
- Stroke RehabilitationDokument10 SeitenStroke RehabilitationPethuel Pomaloy100% (1)
- Lin 2012Dokument9 SeitenLin 2012Luis Briones Lau.LiNoch keine Bewertungen
- Jurnal Srs SkoliosisDokument5 SeitenJurnal Srs SkoliosisDhiny RatuNoch keine Bewertungen
- Effects of Schroth Method and Core Stabilization Exercises On Idiopathic Scoliosis: A Systematic Review and Meta AnalysisDokument12 SeitenEffects of Schroth Method and Core Stabilization Exercises On Idiopathic Scoliosis: A Systematic Review and Meta AnalysisAsmaa SalamaNoch keine Bewertungen
- Gum Mess On 2003Dokument6 SeitenGum Mess On 2003fajarcolzzzNoch keine Bewertungen
- 1471 2318 13 105Dokument13 Seiten1471 2318 13 105ANoch keine Bewertungen
- Leg Exercise: Effect On Reducing Fatigue and Improving Activities of Daily Living For Hemodialysis PatientsDokument9 SeitenLeg Exercise: Effect On Reducing Fatigue and Improving Activities of Daily Living For Hemodialysis PatientsriadesnitaNoch keine Bewertungen
- Effectiveness of Manual Perturbation Exercises inDokument7 SeitenEffectiveness of Manual Perturbation Exercises inSabarie PNoch keine Bewertungen
- Journal of Science and Medicine in SportDokument6 SeitenJournal of Science and Medicine in SportAlvaro FernandoNoch keine Bewertungen
- Jurnal 2 Stroke LinggaDokument9 SeitenJurnal 2 Stroke LinggaLingga Dewi SaraswatiNoch keine Bewertungen
- Rega Sugianto - J120190031 - EJHD Article Review 1Dokument20 SeitenRega Sugianto - J120190031 - EJHD Article Review 1j130235024Noch keine Bewertungen
- Registry of Outcome Measures With MDC 2010Dokument125 SeitenRegistry of Outcome Measures With MDC 2010bdesai48100% (1)
- Stump C Lit Reivew FinalDokument8 SeitenStump C Lit Reivew Finalapi-621438645Noch keine Bewertungen
- The General Function Score: A Useful Tool For Measurement of Physical Disability. Validity and ReliabilityDokument8 SeitenThe General Function Score: A Useful Tool For Measurement of Physical Disability. Validity and ReliabilityLatifatus SirriyahNoch keine Bewertungen
- Exercise Physiology for the Pediatric and Congenital CardiologistVon EverandExercise Physiology for the Pediatric and Congenital CardiologistNoch keine Bewertungen
- Osteoarthritis PDFDokument1 SeiteOsteoarthritis PDFUliuliauliaNoch keine Bewertungen
- Emd166 Slide Acute Coronary PDFDokument40 SeitenEmd166 Slide Acute Coronary PDFUliuliauliaNoch keine Bewertungen
- Manajemen OrganisasiDokument39 SeitenManajemen OrganisasiUliuliauliaNoch keine Bewertungen
- The Effect of Education On Knowledge, Self Management Behaviours and Self Efficacy of Patients With Type 2 DiabetesDokument9 SeitenThe Effect of Education On Knowledge, Self Management Behaviours and Self Efficacy of Patients With Type 2 DiabetesUliuliauliaNoch keine Bewertungen
- 100%. However, If You Had No Confidence at All That You Could Exercise at Your ExerciseDokument2 Seiten100%. However, If You Had No Confidence at All That You Could Exercise at Your ExerciseUliuliauliaNoch keine Bewertungen
- Pain Self Efficacy QuestionnaireDokument2 SeitenPain Self Efficacy QuestionnaireUliuliauliaNoch keine Bewertungen
- Music Therapy Sangat Populer Saat Ini. Tapi Pada Saat Ini Jarang Di GunakanDokument6 SeitenMusic Therapy Sangat Populer Saat Ini. Tapi Pada Saat Ini Jarang Di GunakanElfanizar YusandiNoch keine Bewertungen
- Ambulance OperationsDokument36 SeitenAmbulance OperationsUliuliauliaNoch keine Bewertungen
- Attempts: Over Are AnDokument2 SeitenAttempts: Over Are AnSayed AbozeidNoch keine Bewertungen
- Clock Drawing Test PDFDokument6 SeitenClock Drawing Test PDFfissionmailedNoch keine Bewertungen
- Identifying A Cut-Off Point For Normal Mobility: A Comparison of The Timed Up and Go' Test in Community-Dwelling and Institutionalised Elderly WomenDokument6 SeitenIdentifying A Cut-Off Point For Normal Mobility: A Comparison of The Timed Up and Go' Test in Community-Dwelling and Institutionalised Elderly WomenCarolina SandovalNoch keine Bewertungen
- Geriatric Nursing: Feature ArticleDokument5 SeitenGeriatric Nursing: Feature ArticleBryan NguyenNoch keine Bewertungen
- DeliriumDokument12 SeitenDeliriumChrysi TsiouriNoch keine Bewertungen
- Curriculum Resource GuideDokument113 SeitenCurriculum Resource GuideAditya Dana IswaraNoch keine Bewertungen
- Bedridden Elderly: Factors and Risks: August 2020Dokument5 SeitenBedridden Elderly: Factors and Risks: August 2020ammarsalama997Noch keine Bewertungen
- Guidelines For The Falls Risk AssessmentDokument2 SeitenGuidelines For The Falls Risk AssessmentAnonymous tbJ24554Noch keine Bewertungen
- Geriatric SyndromeDokument16 SeitenGeriatric SyndromeJia Jia R'chelNoch keine Bewertungen
- MN Geriatric Nursing - SET2Dokument15 SeitenMN Geriatric Nursing - SET2dila punNoch keine Bewertungen
- Sas 3Dokument3 SeitenSas 3Dummy AccountNoch keine Bewertungen
- 0 The Timed Up and Go TestDokument9 Seiten0 The Timed Up and Go Testapi-593365151Noch keine Bewertungen
- Turquoise Heart Vector Medical BrochureDokument2 SeitenTurquoise Heart Vector Medical BrochureMAUREN DAZANoch keine Bewertungen
- Ageing Prisoners: An Introduction To Geriatric Health-Care Challenges in Correctional FacilitiesDokument24 SeitenAgeing Prisoners: An Introduction To Geriatric Health-Care Challenges in Correctional FacilitiesepraetorianNoch keine Bewertungen
- Hospital Project Proposal PDFDokument15 SeitenHospital Project Proposal PDFSatya Prakash SundramNoch keine Bewertungen
- Elective 2 2019 SyllabusDokument12 SeitenElective 2 2019 SyllabusMaria Rebecca CorazonNoch keine Bewertungen
- Scope of Community Health NursingDokument22 SeitenScope of Community Health NursingEli Zza Koirala85% (13)
- Dementia Types - Symptoms, Diagnosis, Causes, TreatmentsDokument6 SeitenDementia Types - Symptoms, Diagnosis, Causes, TreatmentsRatnaPrasadNalamNoch keine Bewertungen
- Moca Vs MMSEDokument2 SeitenMoca Vs MMSEYw LiuNoch keine Bewertungen
- Resume For LPNDokument8 SeitenResume For LPNafllwwtjo100% (1)
- New BoleanDokument3 SeitenNew BoleanSachi AnandNoch keine Bewertungen
- Geriatrics IntroDokument15 SeitenGeriatrics IntroAnanya KaurNoch keine Bewertungen
- Transitional Care For Older Adults With Chronic Illness - An Integrated ReviewDokument8 SeitenTransitional Care For Older Adults With Chronic Illness - An Integrated ReviewIJAR JOURNALNoch keine Bewertungen
- McMaster University Geriatrics Journal Club - Lecanemab in Early Alzheimers Disease - by ShanojanDokument35 SeitenMcMaster University Geriatrics Journal Club - Lecanemab in Early Alzheimers Disease - by ShanojanDr. Shanojan Thiyagalingam, FRCPC FACPNoch keine Bewertungen
- 3683263752english Annual Report 2010-11Dokument351 Seiten3683263752english Annual Report 2010-11srinivasanaNoch keine Bewertungen
- 2019 - High Levels of Polypharmacy in RheumatoidDokument7 Seiten2019 - High Levels of Polypharmacy in RheumatoidGustavo ResendeNoch keine Bewertungen
- Ageing, Geriatric Syndrome & Anthropometry - Ger.08.11.2021.dsnDokument10 SeitenAgeing, Geriatric Syndrome & Anthropometry - Ger.08.11.2021.dsnyudhi mdNoch keine Bewertungen
- Meeting Nutritional Needs ElderlyDokument25 SeitenMeeting Nutritional Needs ElderlyJustine PlazaNoch keine Bewertungen
- Association Between Frailty and Time Alive and at Home After Cancer Surgery Among Older Adults: A Population-Based AnalysisDokument19 SeitenAssociation Between Frailty and Time Alive and at Home After Cancer Surgery Among Older Adults: A Population-Based AnalysisJuan Camilo SánchezNoch keine Bewertungen
- Australian Dental Journal - 2015 - Ettinger - Treatment Planning Concepts For The Ageing PatientDokument15 SeitenAustralian Dental Journal - 2015 - Ettinger - Treatment Planning Concepts For The Ageing PatientLorri - Ann LamontNoch keine Bewertungen