Beruflich Dokumente
Kultur Dokumente
Composite Resin Layering and Placement Techniques
Hochgeladen von
enimaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Composite Resin Layering and Placement Techniques
Hochgeladen von
enimaCopyright:
Verfügbare Formate
C O N T I N U I N G
E D U C A T I O N
X X
COMPOSITE RESIN LAYERING AND PLACEMENT TECHNIQUES: CASE PRESENTATION AND S CIENTIFIC E VALUATION
Jeff T. Blank, DMD* Mark Latta, DDS, MS 17 6
Composite resin technology has evolved, providing clinicians with the ability to deliver more natural-looking restorations for their dental patients. The evolution of layering techniques and internal staining procedures has further improved composite resins potential for optimal results. This article discusses difficulties associated with traditional composite layering and staining, and it presents in vitro research that supports a novel layering approach. Specifically, the cut-back, etch, bond, and layer technique (CEBL) is introduced as an alternative to freehand layering.
Learning Objectives: This article presents current concepts for composite resin layering and bonding technology. Upon reading this article, the reader should: Understand the clinical protocol for resin layering and bonding. Recognize the scientific advantages associated with composite layering with the CEBL technique.
Key Words: composite, layering, bonding, cut-back, etch
*Private practice, Rock Hill, SC; Adjunct Instructor, Department of Operative Dentistry, Medical University of South Carolina College of Dental Medicine, Charleston, SC. Associate Dean for Research, Professor of General Dentistry, Creighton University School of Dentistry, Omaha, NE. Jeff T. Blank, DMD, 1318 Ebenezer Road, Rock Hill, SC 29732 Tel: 803-327-3240 E-mail: jblank@comporium.net
Pract Proced Aesthet Dent 2005;17(6):A-F
JULY
BLANK
1861_200506PPAD_Blank.qxd
6/9/05
3:10 PM
Page B
Practical Procedures & AESTHETIC DENTISTRY
he continued evolution of composite layering techniques has significantly enhanced clinicians deliv-
ery of predictable and natural-looking resin restorations. Dentists today are embracing the concept of composite stratification, and most contemporary composite systems include an assortment of opacities designed for use in advanced layering techniques. While the delivery of layered composite restorations remains a viable aesthetic option, many clinicians struggle with the technique sensitivity of placing several shades within a direct composite restoration.
1
Techniques for internally stratified, direct resin restorations are highly dependent on the clinicians skill, and care must be taken to ensure that the exact thickness and shape of each layer is accurately predicted. While the artistic capabilities of each clinician vary, appropriate restorative techniques can be learned. Pioneers in the field of operative dentistry have long advocated freehand placement of various opacious, body, and translucent materials onto the air-inhibited layer of the previously cured increment.
2,3
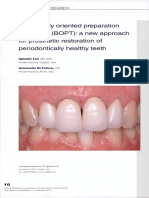
Figure 1A. Preoperative right buccal view demonstrating short, dark lateral incisors. 1B. Left buccal view of unaesthetic lateral incisors. The patient desired a more even smile line.
for internal anatomy (eg, mammelons) and receptacles to receive internal tints. This technique is used routinely in dental laboratories, where a single shade of ceramic ingot is pressed to full contour. The incisal third is then cut-back, and specialized tints and various shades of translucent enamel feldspathic porcelains are applied and fired. By adapting this same concept to direct composite veneers, clinicians may find the technique of reduction from full contour easier and less time-consuming than additive layering to accomplish the same goals. One concern with this technique, however, is the quality of the bond between layers of cured composite once the air-inhibited layer is removed following the cutback procedure. Intraoral repair of existing composite resin restorations has proven to be unreliable without extraordinary measures. Reportedly, this is due to the lack of chemical union of the layers.4,5 It has been reported, however, that in freshly cured composite resineven after the air-inhibited, resin-rich layer is removedradicals remain available for reaction in the body of the cured composite.6 The stability of these radicals is temperature- and formula-dependent, but it is reasonable to presume that in the time frame of a direct resin clinical procedure, they would be available for affecting a chemical union between a cut-back layer and freshly placed composite resin.
It is the pres-
ence of this 3-m to 5-m layer of unpolymerized resin on the surface that provides the organic coupling sites for the additional increments. While layering composites in this fashion is optimal, the complexities of predetermining the exact thickness, placement, and shape of each layer and opacity complicate freehand layering for some clinicians. In the event that the previous layer was found to be too thick, clinicians have two options. The first is to cut-back the anatomically incorrect layer to the appropriate shape and contour with a rotary instrument and continue with layering. The second option is to remove the entire restoration and begin again. The former is a more practical approach as it saves valuable chairtime and effort. Another practical consideration that would warrant cutting back of a polymerized layer of composite prior to additional layering is the concept of building an entire direct veneer to full contour in a single shade, and then deliberately cutting back the incisal third to create space
Vol. 17, No. 6
1861_200506PPAD_Blank.qxd
6/9/05
3:10 PM
Page C
Blank
ing the occlusion and aesthetic form prior to the placement of internal tints and translucency was initiated. The lateral incisors were built out of a body shade of microhybrid composite (ie, EsthetX, Dentsply Caulk, Milford, DE) to full contour utilizing a freehand technique (Figure 2). Contemporary resin systems such as Premise (Kerr/Sybron, Orange, CA) or Filtek Supreme (3M Espe, St. Paul, MN) represented similar restorative material options. By building the tooth to full contour, the clinician could visualize the final contours in comparison to
Figure 2. The lateral incisors were initially built to full contour with a body shade of composite resin to confirm final anatomic contour prior to cut-back.
the adjacent teeth and be assured that the final restoration would be of appropriate length in relation to the aesthetic objectives and limitations of the patients occlusion. The initial buildup was light cured. The incisal third of the fully contoured, polymerized restoration was then cut-back using a diamond bur to create anatomic developmental lobes and dentin mammelons. Since the final facial and incisal contours had been approved prior to cut-back, the complications sometimes associated with failing to leave enough space for the subsequent layering of internal tints and the overlying translucent enamel layer were avoided (Figure 3). The polymerized buildup was re-etched using a phosphoric acid gel etchant to provide a clean, active surface for bonding the final buildup (Figure 4). A lightcurable, self-priming adhesive (ie, Prime & Bond NT, Dentsply Caulk, Milford, DE) was applied and polymerized for 20 seconds (Figure 5). Internal characterization was then applied using soft brown and yellow tints (ie, Effect Color, Heraeus Kulzer, Armonk, NY) to match the maverick stains present in the surrounding natural dentition (Figure 6). The tints were then polymerized. The final translucent incisal layer was subsequently applied over the cut-back lobes and the incisal tints (Figure 7). The restoration was then light cured, finished, and polished (Figure 8).
This article presents an in vitro analysis that supports the practice of cutting back, etching, bonding, and continued layering (CEBL); it also demonstrates a clinical protocol consistent with these findings.
Case Presentation
A 26-year-old female patient presented with short, dark, lateral incisors and the desire to eliminate her buck teeth (Figure 1). The patient desired a more even smile line, which would involve lengthening the clinically short crowns of teeth #7(12) and #10(22). Since the lateral incisors were unrestored healthy teeth, aesthetic restoration with a minimally invasive approach was desirable. Noting the preoperative presence of maverick tints, incisal edge translucency, and varying degrees of opacity in the surrounding dentition, two polychromatic, internally stained, stratified direct veneers were prescribed for teeth #7 and #10. Freehand layering with multiple shades and opacities of directly placed composite was considered. This approach would be complicated, however, by the need to preoperatively determine the correct length and contour of these teeth and to eliminate the potential for undesirable, nonworking, excursive interferences. The novel CEBL approach of building the entire veneer of a polymerized base shade to full contour and evaluat-
Evaluation of Sheer Bond Strength of Layered Composite
The following in vitro evaluation was performed to deter-
PPAD
1861_200506PPAD_Blank.qxd
6/9/05
3:10 PM
Page D
Practical Procedures & AESTHETIC DENTISTRY
Figure 3. An incisal cut-back was performed to create dentin lobes and the framework for incisal translucency.
Figure 4. The incisor was isolated with a metal strip and a phosphoric acid gel etchant was applied to acidify and cleanse the prepared surfaces.
mine the bond strengths of composites placed using a simulated layering approach. The sheer bond strengths (SBS) for layering two different composite materials were established. Determining SBS is a widely used screening test to evaluate adhesive materials and techniques using a variety of materials and substrates including enamel, dentin, metals, and other restorative materials. While bond testing alone is not completely discriminating among materials and techniques, the numerical values and the pattern of bond failures can be helpful in screening. Higher bond strengths and failure patterns of a cohesive nature would suggest that the CEBL technique would be durable clinically.
Figure 5. A light cured primer/adhesive agent was applied and subsequently polymerized.
Materials and Methods
A total of 48 cavities (6 mm 4 mm) were prepared in aluminum molds. A base layer of composite resin was then placed and flattened. The samples were light cured for 40 seconds from all sides. Four experimental groups represented different conditions prior to simulated layering (Table 1). The positive control (ie, the intact air-inhibited layer) represents the best possible condition for layering. The negative control removes this layer and bonds to an untreated ground surface. The CEBL groups included the cut-back, followed by the removal of debris with a phosphoric acid conditioner, application of a
Figure 6. Internal characterizations were added to the buildup in order to provide the appearance of natural dentition that matched the surrounding shade nuances.
Vol. 17, No. 6
1861_200506PPAD_Blank.qxd
6/9/05
3:10 PM
Page E
Blank
dentin/enamel adhesive, and then application of an uncured composite resin. The Co-Jet (3M Espe, St. Paul, MN) group was added as reference since excellent bond strengths have been reported with this system.5 The following composite resins and adhesives were used in this investigation: EsthetX composite resin (Dentsply Caulk, Milford, DE) Substrate Shade A2 Veneer Enamel GE
Figure 7. A final translucent shade was then layered and sculpted using a composite instrument.
Adhesive Prime & Bond NT Venus composite resin (Heraeus Kulzer) Substrate Shade A2 Veneer Enamel T1 Adhesive Comfort Bond Following specimen preparation, one half of the assemblies in each group were stored in water at 37C for 24 hours; the remaining specimens were prepared for immediate testing. The assemblies were then loaded to failure in an Instron 1123 test frame at a cross-head speed of 5 mm/min. Mean SBS was calculated in Megapascals (MPa) and fracture sites were evaluated to determine if they were adhesive, ie, at the interface between the ground layer and the added composite, or cohesive with the fracture occurring in the substrate composite. Both ANOVA and Tukeys post-hoc test were used for data analysis.
Figure 8A. Postoperative buccal view of the restored lateral incisor. 8B. Left lateral incisor after buildup. Note the harmonious integration with the surrounding dentition.
Table 1
Experimental Groups Prepared for Simulated Layering
Group (12 Specimens Each) 1. Positive Control 2. Negative Control no additional treatment 3. Etch and Adhesive (CEBL Technique) 4. Co-Jet (3M Espe, St. Paul, MN) Base Layer Treatment Air-inhibited layer left intact Ground with 320 grit; Ground with 320 grit; etched, adhered, light cured Ground with 320 grit; sandblasted with Co-Jet sand, silanated, adhered, light cured Application of Layering Resin Gelatin capsule loaded with layering resin, applied, and light cured Gelatin capsule loaded with layering resin, applied, and light cured Gelatin capsule loaded with layering resin, applied, and light cured Gelatin capsule loaded with layering resin, applied, and light cured
PPAD
1861_200506PPAD_Blank.qxd
6/9/05
3:10 PM
Page F
Practical Procedures & AESTHETIC DENTISTRY
Table 2
Mean Sheer Bond Strength for EsthetX
Surface Ground 320 grit Air-inhibited layer Etch and Adhesive (CEBL Technique) Co-Jet Debond Immediate 13.6 2.1 19.7 1.8 19.0 1.8 19.4 2.4 Debond 24 Hours 21.9 3.4 35.0 3.5 34.2 4.1 33.9 3.8
Table 3
Mean Sheer Bond Strength for Venus
Surface Ground 320 grit Air-inhibited layer Etch and Adhesive (CEBL Technique) Co-Jet Debond Immediate 13.6 3.1 16.9 1.6 17.1 2.4 16.6 2.1 Debond 24 Hours 29.3 6.7 33.2 4.7 32.8 3.1 31.5 2.3
Table 4
Failure Rates for the Resin Materials
Surface Ground 320 grit Air-inhibited layer Etch and Adhesive (CEBL Technique) Co-Jet EsthetX Immediate All adhesive All cohesive All cohesive All cohesive EsthetX 24 Hours All adhesive All cohesive All cohesive All cohesive Venus Immediate All adhesive All cohesive All cohesive All cohesive Venus 24 hours All adhesive All cohesive All cohesive All cohesive
Results
The mean SBS were tabulated for both EsthetX and Venus. In the former (Table 2), ground values were significantly lower (p<0.05) than in the air-inhibited layer, CEBL, or Co-Jet groups. In the latter (Table 3), no statistical difference in bond strength was observed for any group. The failure patterns for each group were also calculated (Table 4).
Conclusion
Even after removing the air-inhibited layer, the CEBL technique generated similar bond strengths and fracture patterns as those for bonding to the air-inhibited layer. After long-term water storage, the CEBL technique was successful for bonding to EsthetX but not to Venus. The results of this study support an immediate cut-back and rebonding placement technique for layering these two multishaded composite resin systems.
Discussion
Similar bond strengths and fracture patterns were evident using the CEBL technique, even when the air-inhibited layer was removed. Even more important than the numerical values, however, the fracture patterns evident with the CEBL technique were identical to those of composite resin layered to the unaltered, air-inhibited layer. This suggests that the chemical union is similar to that achieved with the air-inhibited layer intact, and a restoration layer using the CEBL method should have the durability of a conventionally layered restoration.
References
1. Fortin D, Vargas MA. The spectrum of composites: New techniques and materials. J Am Dent Assoc 2000;131(Suppl): 26S-30S. 2. Fahl N Jr. Optimizing the esthetics of Class IV restorations with composite resins. J Can Dent Assoc 1997;63(2):108-115. 3. Jackson RD. Understanding the characteristics of naturally shaded composite resins. Pract Proced Aesthet Dent 2003;15(8): 577-585. 4. Kupiec KA, Barkmeier WW. Laboratory evaluation of surface treatments for composite repair. Oper Dent 1996;21(2):59-62. 5. Denehy G, Bouschlicher M, Vargas M. Intraoral repair of cosmetic restorations. Dent Clin North Am 1998;42(4):719-737. 6. Burtscher P. Stability of radicals in cured composite materials. Dent Mater 1993;9(4):218-221.
Vol. 17, No. 6
1861_200506PPAD_Blank.qxd
6/9/05
3:10 PM
Page G
CONTINUING EDUCATION (CE) EXERCISE NO. X
CE
X
CONTINUING EDUCATION
To submit your CE Exercise answers, please use the answer sheet found within the CE Editorial Section of this issue and complete as follows: 1) Identify the article; 2) Place an X in the appropriate box for each question of each exercise; 3) Clip answer sheet from the page and mail it to the CE Department at Montage Media Corporation. For further instructions, please refer to the CE Editorial Section. The 10 multiple-choice questions for this Continuing Education (CE) exercise are based on the article Composite resin layering and placement techniques: Case presentation and scientific evaluation, by Jeff T. Blank, DMD, and Mark Latta, DDS, MS. This article is on pages 000-000.
1. The best reason for layering modern composite resin systems in anterior restorations is: a. To generate maximum strength of the resin mass. b. To enhance the delivery of predictable, natural looking restorations. c. To best replicate the shape of adjacent teeth. d. To promote adhesion to tooth structure. 2. Bonding between layers of composite is most often facilitated by: a. Mechanical retention between the resin layers. b. Chemical bonding between the new resin layer and the air-inhibited layer of the previously cured increment. c. An adhesive agent placed on the resin surface. d. Acid etching the cured composite. 3. The chief reason to cut-back a cured layer of composite is to: a. Provide mechanical retention for bonding. b. To strengthen the bond between the resin layers. c. To remove the air-inhibited layer. d. To better control the thickness of the layered resin shade. 4. The laboratory process that is imitated in layering an anterior Class IV restoration using the CEBL technique is: a. Waxing a restoration to full contour. b. Placing surface stain on a porcelain crown. c. Cutting back a cast ceramic ingot and layering tints and shaded porcelains for characterization. d. Using diamond pastes for polishing the porcelain surface. 5. The most obvious clinical example concerning the quality of the bond between layers of composite placed after a cut-back is: a. The unreliability of intraoral repair of older composite restorations. b. Microleakage and stain between composite layers. c. Lack of retention of layers in posterior composite restorations. d. Color change of the composite placed in layers.
6. The proposed mechanism for the CEBL technique is: a. Mechanical retention between the resin layers. b. Polymerization shrinkage compressing the new resin layer to the old resin layer. c. Use of the air-inhibited layer for bonding. d. Remaining free radicals are available for reaction in freshly cured composite even once the air-inhibited layer is removed. 7. Which of the following are the sequence and steps for the CEBL technique? a. Place adhesive/layer composite/cure composite. b. Cut-back cured layer/place adhesive/layer composite/ cure composite. c. Cut-back cured layer/etch and rinse/layer composite/ cure composite. d. Cut-back cured layer/etch and rinse/place adhesive/layer composite/cure composite. 8. In the laboratory study, the negative control was: a. The air-inhibited layer surface. b. The ground surface with no treatment. c. The Co-Jettreated surface. d. The CEBL-treated surface. 9. Compared to the bond values achieved with the airinhibited layer: a. The Co-Jet and CEBL technique generated similar bond values. b. The negative control generated similar bond values. c. The negative control generated better bond values. d. No difference was seen with any group. 10. The pattern of fracture failures observed for the CEBL and air-inhibited groups: a. Were both cohesive supporting the use of the CEBL technique for layering. b. Were cohesive for the air-inhibited group and adhesive for CEBL, indicating CEBL does not work. c. Were the same as the adhesive group. d. Do not contribute to the interpretation of the study.
Vol. 17, No. 6
PPAD
Das könnte Ihnen auch gefallen
- Treatment Planning Single Maxillary Anterior Implants for DentistsVon EverandTreatment Planning Single Maxillary Anterior Implants for DentistsNoch keine Bewertungen
- Aesthetic Layering TechniqueDokument0 SeitenAesthetic Layering Techniqueatul_singh2001Noch keine Bewertungen
- 25 All Ceramic RestorationsDokument31 Seiten25 All Ceramic RestorationsJúliaJulie100% (2)
- Digital Smile DesignDokument14 SeitenDigital Smile DesignSahana RangarajanNoch keine Bewertungen
- EW Step by Step Veneer enDokument5 SeitenEW Step by Step Veneer enVipul SrivastavaNoch keine Bewertungen
- Layering Technique On Anterior Resin CompositeDokument7 SeitenLayering Technique On Anterior Resin CompositeDentisia RealNoch keine Bewertungen
- TMP F643Dokument20 SeitenTMP F643FrontiersNoch keine Bewertungen
- Sclerotic Dentin-Clinical Implications in Restorative DentistryDokument2 SeitenSclerotic Dentin-Clinical Implications in Restorative Dentistrydentace1100% (1)
- Rethinking Deep Marginal Extension (DME) : Pasquale VenutiDokument7 SeitenRethinking Deep Marginal Extension (DME) : Pasquale VenutiTheDessleyNoch keine Bewertungen
- Castingprocedure 141012113403 Conversion Gate01Dokument103 SeitenCastingprocedure 141012113403 Conversion Gate01joephinNoch keine Bewertungen
- Smile Design IIDokument68 SeitenSmile Design IIkastiel730% (1)
- InLine PoM Edition GruebelDokument28 SeitenInLine PoM Edition GruebelFabio WenoNoch keine Bewertungen
- Guide To Complete Dentures VitaDokument150 SeitenGuide To Complete Dentures VitaFrederico Diego Medeiros Lima67% (3)
- Biologically Oriented Preparation Technique (BOPT) : A Ne/a/ Approach For Prosthetic Restoration of Periodontically Healthy TeethDokument15 SeitenBiologically Oriented Preparation Technique (BOPT) : A Ne/a/ Approach For Prosthetic Restoration of Periodontically Healthy TeethDr. Marica Ramona Elena100% (1)
- Seminar 8 Smear LayerDokument100 SeitenSeminar 8 Smear LayerHari PriyaNoch keine Bewertungen
- Advance in MaterialsDokument10 SeitenAdvance in Materialssami robalinoNoch keine Bewertungen
- Laminate VeneerDokument51 SeitenLaminate VeneerZiad OthmanNoch keine Bewertungen
- Delivery of Complete Dentures, Prostho Lec 11Dokument19 SeitenDelivery of Complete Dentures, Prostho Lec 11JustDen09100% (4)
- DSD From 2d To 3dDokument14 SeitenDSD From 2d To 3dHugoRoCkstar100% (1)
- Dental Dialogue 07 2011 ENDokument16 SeitenDental Dialogue 07 2011 ENJames LinNoch keine Bewertungen
- Clarks Cavity PreparationDokument10 SeitenClarks Cavity PreparationVinisha Vipin SharmaNoch keine Bewertungen
- HTTP WWW - Styleitaliano.org Mobile Dental Photography Part IDokument7 SeitenHTTP WWW - Styleitaliano.org Mobile Dental Photography Part IAmee PatelNoch keine Bewertungen
- How To Bulk A Posterior Cavity: Giuseppe Marchetti Direct Posteriors - Cases - Shadeguides - Tips and TricksDokument23 SeitenHow To Bulk A Posterior Cavity: Giuseppe Marchetti Direct Posteriors - Cases - Shadeguides - Tips and Tricksmaroun ghaleb100% (1)
- Class I and II Indirect Tooth-Colored Restorations (4,5)Dokument133 SeitenClass I and II Indirect Tooth-Colored Restorations (4,5)Samah SakerNoch keine Bewertungen
- 12 RESTORATION OF THE ENDODONTICALLY TREATED TOOTHmic PDFDokument43 Seiten12 RESTORATION OF THE ENDODONTICALLY TREATED TOOTHmic PDFIonut Cristian OpreaNoch keine Bewertungen
- Irrigation in EndodonticsDokument142 SeitenIrrigation in EndodonticsArmanThaman100% (2)
- All Ceramic RestorationsDokument13 SeitenAll Ceramic RestorationsMobarak NoorNoch keine Bewertungen
- ROUTES - For Excellence in Restorative Dentistry - Mastery For Beginners and Experts - Volume 2Dokument106 SeitenROUTES - For Excellence in Restorative Dentistry - Mastery For Beginners and Experts - Volume 2Игорь СидоренкоNoch keine Bewertungen
- ImplantDokument37 SeitenImplantazizNoch keine Bewertungen
- IPS E-Max CAD - Dental TechniciansDokument9 SeitenIPS E-Max CAD - Dental TechniciansHồ Đức100% (1)
- Clinical Photography: A Picture Can Tell A Thousand WordsDokument4 SeitenClinical Photography: A Picture Can Tell A Thousand WordsKalyana ChakravarthiNoch keine Bewertungen
- Custom Trays: The KeyDokument28 SeitenCustom Trays: The KeyKriti MalhotraNoch keine Bewertungen
- 3) All Ceramic RestorDokument26 Seiten3) All Ceramic RestorAboodMAlhandoodiNoch keine Bewertungen
- Denture AdhesiveDokument11 SeitenDenture AdhesiveAmniAzmiNoch keine Bewertungen
- Computer-Aided Designing and Computer-Aided Manufacturing in ProsthodonticsDokument60 SeitenComputer-Aided Designing and Computer-Aided Manufacturing in Prosthodonticsreshma shaikNoch keine Bewertungen
- A Modification of The Altered Cast TechniqueDokument2 SeitenA Modification of The Altered Cast TechniqueChirag Gorasiya100% (1)
- Try in FPDDokument40 SeitenTry in FPDharshini100% (1)
- Margin Elevation Technique PDFDokument6 SeitenMargin Elevation Technique PDFUsman SanaNoch keine Bewertungen
- Clinical Photography Part - 2 PDFDokument3 SeitenClinical Photography Part - 2 PDFsonal agarwalNoch keine Bewertungen
- VeneersDokument50 SeitenVeneersDr FarhatNoch keine Bewertungen
- Veneering Teeth With Porcelain: WWW - Dent.osu - edu/ddscurriculum/Students/Webr EsourcesDokument56 SeitenVeneering Teeth With Porcelain: WWW - Dent.osu - edu/ddscurriculum/Students/Webr EsourcesannisaNoch keine Bewertungen
- Composite Resin RestorationDokument9 SeitenComposite Resin RestorationSawsan Z. JwaiedNoch keine Bewertungen
- Finishing and Polishing Materials.9Dokument8 SeitenFinishing and Polishing Materials.9Eman Azmi OmarNoch keine Bewertungen
- All Ceramics - Dr. YashendraDokument32 SeitenAll Ceramics - Dr. YashendranjucyNoch keine Bewertungen
- Impression TechniquesDokument115 SeitenImpression Techniquesandrian_10Noch keine Bewertungen
- Direct Composites and Their Prosthodontic ApplicationDokument119 SeitenDirect Composites and Their Prosthodontic ApplicationTavleen KaurNoch keine Bewertungen
- VeneerDokument38 SeitenVeneerDRPRIYA007Noch keine Bewertungen
- Ada Guide To Digital Dental Photography and Imaging PDFDokument53 SeitenAda Guide To Digital Dental Photography and Imaging PDFLynda M. Naranjo100% (1)
- GolDen ProportIon in ProsthoDontICs Part-1Dokument6 SeitenGolDen ProportIon in ProsthoDontICs Part-1Jonathan Jaramillo100% (2)
- Metal Ceramic RestorationDokument48 SeitenMetal Ceramic RestorationZy Hoe75% (4)
- Composite ResinDokument46 SeitenComposite Resintj_sweetgirl100% (1)
- Management of Badly Broken Down Teeth IIDokument63 SeitenManagement of Badly Broken Down Teeth IIAhmad Zuhdi Aljedi100% (7)
- Color and Shade Matching in Operative DentistryDokument19 SeitenColor and Shade Matching in Operative DentistryMarco Antonio García LunaNoch keine Bewertungen
- IPR - Class II MO Preparation Restoration of 36Dokument14 SeitenIPR - Class II MO Preparation Restoration of 36kiranvarma2u50% (2)
- Smile Analysis Part 2Dokument11 SeitenSmile Analysis Part 2Mircea Ilie100% (1)
- All Ceramic Materials and SystemsDokument6 SeitenAll Ceramic Materials and SystemsMahaAhmedNoch keine Bewertungen
- Advantages of Adhesive in DentistryDokument29 SeitenAdvantages of Adhesive in DentistryAnonymous CY62A9Noch keine Bewertungen
- A Clinical Overview of Removable Prostheses - Introduction 1.factors To Consider in Planning A Removable Partial DentureDokument6 SeitenA Clinical Overview of Removable Prostheses - Introduction 1.factors To Consider in Planning A Removable Partial DentureCristi PapandopolNoch keine Bewertungen
- 1 s2.0 S002234682200834X MainDokument7 Seiten1 s2.0 S002234682200834X MainenimaNoch keine Bewertungen
- 24Dokument11 Seiten24enimaNoch keine Bewertungen
- Fernando 2015Dokument7 SeitenFernando 2015enimaNoch keine Bewertungen
- 24Dokument11 Seiten24enimaNoch keine Bewertungen
- Topical Application of Antibiotics in Primary Teeth PDFDokument10 SeitenTopical Application of Antibiotics in Primary Teeth PDFenimaNoch keine Bewertungen
- 1 s2.0 S0022346822006893 MainDokument4 Seiten1 s2.0 S0022346822006893 MainenimaNoch keine Bewertungen
- Prevalence of Musculoskeleal Disorders Among Dentists in Al-Madinah Kingdom of Saudi ArabiaDokument5 SeitenPrevalence of Musculoskeleal Disorders Among Dentists in Al-Madinah Kingdom of Saudi ArabiaenimaNoch keine Bewertungen
- Filippi 2016Dokument12 SeitenFilippi 2016enimaNoch keine Bewertungen
- 00010Dokument11 Seiten00010enimaNoch keine Bewertungen
- (1)Dokument10 Seiten(1)enimaNoch keine Bewertungen
- Feng 2016Dokument2 SeitenFeng 2016enimaNoch keine Bewertungen
- Fractured Incisors: A Judicious Restorative Approach - Part 1Dokument6 SeitenFractured Incisors: A Judicious Restorative Approach - Part 1enimaNoch keine Bewertungen
- Pulmonary Pharmacology & Therapeutics Volume 33 Issue 2015 (Doi 10.1016/j.pupt.2015.05.005) Jyoti, Md. Anirban Zerin, Tamanna Kim, Tae-Hyun Hwang, Tae-Se - In Vitro Effect of Ursolic Acid On TheDokument2 SeitenPulmonary Pharmacology & Therapeutics Volume 33 Issue 2015 (Doi 10.1016/j.pupt.2015.05.005) Jyoti, Md. Anirban Zerin, Tamanna Kim, Tae-Hyun Hwang, Tae-Se - In Vitro Effect of Ursolic Acid On TheRifQy Praristiya SHindyNoch keine Bewertungen
- 00022Dokument11 Seiten00022enimaNoch keine Bewertungen
- Cbo9780511735011a009 PDFDokument33 SeitenCbo9780511735011a009 PDFenimaNoch keine Bewertungen
- Oral Manifestations of Chronic Renal Failure Complicating A Systemic Genetic Disease: Diagnostic Dilemma. Case Report and Literature ReviewDokument7 SeitenOral Manifestations of Chronic Renal Failure Complicating A Systemic Genetic Disease: Diagnostic Dilemma. Case Report and Literature ReviewenimaNoch keine Bewertungen
- Content ServerDokument6 SeitenContent ServerenimaNoch keine Bewertungen
- 10.2341@1559 2863 29 2 1Dokument124 Seiten10.2341@1559 2863 29 2 1enimaNoch keine Bewertungen
- Lorenzo VaniniDokument0 SeitenLorenzo Vaniniflaviuspopa27100% (2)
- Content ServerDokument9 SeitenContent ServerenimaNoch keine Bewertungen
- bjd12820 PDFDokument3 Seitenbjd12820 PDFenimaNoch keine Bewertungen
- ContentServer PDFDokument6 SeitenContentServer PDFenimaNoch keine Bewertungen
- Path o IntroductionDokument16 SeitenPath o IntroductionenimaNoch keine Bewertungen
- The Oral SideDokument12 SeitenThe Oral SideenimaNoch keine Bewertungen
- Mock UpDokument4 SeitenMock UpenimaNoch keine Bewertungen
- Johny GorengDokument33 SeitenJohny GorengMuhammad Bagus SetyawanNoch keine Bewertungen
- Lorenzo VaniniDokument0 SeitenLorenzo Vaniniflaviuspopa27100% (2)
- 1 s2.0 S0002939414001883 MainDokument11 Seiten1 s2.0 S0002939414001883 MainenimaNoch keine Bewertungen
- Animal Welfare in Bangladesh and The Role of Obhoyaronno CaseDokument11 SeitenAnimal Welfare in Bangladesh and The Role of Obhoyaronno CaseZarin Tanjim WoyshorjoNoch keine Bewertungen
- Churches That Have Left RCCG 0722 PDFDokument2 SeitenChurches That Have Left RCCG 0722 PDFKadiri JohnNoch keine Bewertungen
- MC Donald'sDokument30 SeitenMC Donald'sAbdullahWaliNoch keine Bewertungen
- Caregiving Learning Activity Sheet 3Dokument6 SeitenCaregiving Learning Activity Sheet 3Juvy Lyn CondaNoch keine Bewertungen
- 40+ Cool Good Vibes MessagesDokument10 Seiten40+ Cool Good Vibes MessagesRomeo Dela CruzNoch keine Bewertungen
- Hydraulics Experiment No 1 Specific Gravity of LiquidsDokument3 SeitenHydraulics Experiment No 1 Specific Gravity of LiquidsIpan DibaynNoch keine Bewertungen
- Pa Print Isang Beses LangDokument11 SeitenPa Print Isang Beses LangGilbert JohnNoch keine Bewertungen
- RESO NO. 4 - LANYARD FinalDokument1 SeiteRESO NO. 4 - LANYARD FinalsharonleefulloNoch keine Bewertungen
- Steven SheaDokument1 SeiteSteven Sheaapi-345674935Noch keine Bewertungen
- ListeningDokument2 SeitenListeningAndresharo23Noch keine Bewertungen
- Dummies Guide To Writing A SonnetDokument1 SeiteDummies Guide To Writing A Sonnetritafstone2387100% (2)
- Togaf Open Group Business ScenarioDokument40 SeitenTogaf Open Group Business Scenariohmh97Noch keine Bewertungen
- Adverbs Before AdjectivesDokument2 SeitenAdverbs Before AdjectivesJuan Sanchez PrietoNoch keine Bewertungen
- Chain of CommandDokument6 SeitenChain of CommandDale NaughtonNoch keine Bewertungen
- Nandurbar District S.E. (CGPA) Nov 2013Dokument336 SeitenNandurbar District S.E. (CGPA) Nov 2013Digitaladda IndiaNoch keine Bewertungen
- Performance MeasurementDokument13 SeitenPerformance MeasurementAmara PrabasariNoch keine Bewertungen
- MCS 033 NotesDokument7 SeitenMCS 033 NotesAshikNoch keine Bewertungen
- Trần Phương Mai - Literature - Irony in "Letter to a Funeral Parlor" by Lydia DavisDokument2 SeitenTrần Phương Mai - Literature - Irony in "Letter to a Funeral Parlor" by Lydia DavisTrần Phương MaiNoch keine Bewertungen
- Intro To EthicsDokument4 SeitenIntro To EthicsChris Jay RamosNoch keine Bewertungen
- DMSCO Log Book Vol.25 1947Dokument49 SeitenDMSCO Log Book Vol.25 1947Des Moines University Archives and Rare Book RoomNoch keine Bewertungen
- Samsung LE26A457Dokument64 SeitenSamsung LE26A457logik.huNoch keine Bewertungen
- Roman Roads in Southeast Wales Year 3Dokument81 SeitenRoman Roads in Southeast Wales Year 3The Glamorgan-Gwent Archaeological Trust LtdNoch keine Bewertungen
- Tour Guiding and Escort Services - 301Dokument95 SeitenTour Guiding and Escort Services - 301Zane 19531Noch keine Bewertungen
- Logic of English - Spelling Rules PDFDokument3 SeitenLogic of English - Spelling Rules PDFRavinder Kumar80% (15)
- FIREXDokument2 SeitenFIREXPausNoch keine Bewertungen
- Matthew DeCossas SuitDokument31 SeitenMatthew DeCossas SuitJeff NowakNoch keine Bewertungen
- Weill Cornell Medicine International Tax QuestionaireDokument2 SeitenWeill Cornell Medicine International Tax QuestionaireboxeritoNoch keine Bewertungen
- InnovationDokument19 SeitenInnovationPamela PlamenovaNoch keine Bewertungen
- DHBVNDokument13 SeitenDHBVNnitishNoch keine Bewertungen
- Scientific Errors in The QuranDokument32 SeitenScientific Errors in The QuranjibranqqNoch keine Bewertungen