Beruflich Dokumente
Kultur Dokumente
Sarcoidosis Lancet 2013
Hochgeladen von
Andreas IoannouOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Sarcoidosis Lancet 2013
Hochgeladen von
Andreas IoannouCopyright:
Verfügbare Formate
Seminar
Sarcoidosis
Dominique Valeyre, Antje Prasse, Hilario Nunes, Yurdagul Uzunhan, Pierre-Yves Brillet, Joachim Mller-Quernheim
Sarcoidosis is a systemic disease of unknown cause that is characterised by the formation of immune granulomas in various organs, mainly the lungs and the lymphatic system. Studies show that sarcoidosis might be the result of an exaggerated granulomatous reaction after exposure to unidentied antigens in individuals who are genetically susceptible. Several new insights have been made, particularly with regards to the diagnosis and care of some important manifestations of sarcoidosis. The indications for endobronchial ultrasound in diagnosis and for PET in the assessment of inammatory activity are now better specied. Recognition of unexplained persistent disabling symptoms, fatigue, small-bre neurological impairment, cognitive failure, and changes to health state and quality of life, has improved. Mortality in patients with sarcoidosis is higher than that of the general population, mainly due to pulmonary brosis. Predicted advances for the future are nding the cause of sarcoidosis, and the elucidation of relevant biomarkers, reliable endpoints, and new ecient treatments, particularly in patients with refractory sarcoidosis, lung brosis, and those with persistent disabling symptoms.
Published Online October 1, 2013 http://dx.doi.org/10.1016/ S0140-6736(13)60680-7 Department of Pneumology (Prof D Valeyre MD, Prof H Nunes MD, Y Uzunhan MD) and Department of Radiology (Prof P-Y Brillet MD), Assistance Publique Hpitaux de Paris, Avicenne University Hospital, Bobigny, France; University Paris 13, Sorbonne Paris Cit, Bobigny, France (Prof D Valeyre, Prof H Nunes, Y Uzunhan, Prof P-Y Brillet); and Department of Pneumology, University Hospital, Freiburg, Germany (Prof A Prasse MD, Prof J Mller-Quernheim MD) Correspondence to: Prof Dominique Valeyre, Service de Pneumologie, Hpital Avicenne, Bobigny 93009, France dominique.valeyre@avc.aphp.fr
Introduction
Sarcoidosis was recognised more than 120 years ago, and it remains a confusing disease with many grey areas.1 The cause of sarcoidosis is not known and diagnosis can be dicult and delayed from the diverse, nonspecic, unusual, or initially misleading presentations. Many advances have been made since the previous seminar on sarcoidosis in The Lancet,2 and the publication of other reviews.3,4 The indications for endobronchial ultrasound and for F-uorodeoxyglucose (F-FDG) PET have been elucidated further, and occurrence of persistent disabling symptoms such as fatigue, small-bre neuropathy, and cognitive dysfunction have been investigated further. Recognition of health status and quality-of-life impairments has improved. These advances and eorts to accurately assess the development of disease have provided a more comprehensive and personalised care for patients. However, important steps are still needed, such as more accurate biomarkers, improving diagnosis of some extrapulmonary localisations, validated endpoints, and treatments that are ecient in refractory cases. The most important step is to provide evidence on the cause of sarcoidosis.
increased rate of change in general health and extrapulmonary manifestations, particularly uveitis.7 The notion of environmental or transmissible agents having a causal role in sarcoidosis is lent support by temporal and spacetime clusters. Exposure to musty odours, insecticides, or to metal-processing industries are disease risk factors.8,9 A high incidence of sarcoidosis was reported in reghters and other responders after the attacks on the World Trade Center in 2001.10,11 By contrast, a decreased risk has been linked to cigarette smoking.9 Sarcoidosis is usually sporadic, but is familial in 3696% of cases.12 A patients siblings have a higher risk of sarcoidosis than do parents, suggesting a recessive inheritance mode with incomplete penetrance.12 An 80-times increase in risk in monozygotic twins lends support to the idea that genetic factors might account for two-thirds of disease susceptibility.13
Pathogenesis
Causes
The exact cause of sarcoidosis is still not known. Many studies suggest that genetic susceptibility and environmental factors contribute to disease development.2,9,14 Immunologically, sarcoidosis is an exaggerated immune response to so far unidentied antigens. Data for the clinical heterogeneity of sarcoidosis strongly suggest that pathogen-associated molecular patterns of microbial antigens can trigger or amplify
Epidemiology
Sarcoidosis is a global disease, with a prevalence of about 4764 in 100 000, and an incidence of 10355 in 100 000 per year. The highest rates are reported in northern European and AfricanAmerican individuals, particularly in women, and lowest in Japan.5,6 Dierences in prevalence and incidence are linked to age, sex, ethnic origin, and geographical location. The disease can occur in both men and women, with 70% of patients aged 2545 years; however, in Europe and Japan, a second peak of incidence occurs in women older than 50 years of age.5,6 Sarcoidosis is rare in people younger than 15 years or older than 70 years. The female to male ratio is 120:175. Clinical expression of sarcoidosis is aected by epidemiological and socioeconomic factors (appendix, p 1). Elderly-onset sarcoidosis is much more common in women, and in this disorder there is an
See Online for appendix
Search strategy and selection criteria We searched Medline and the Cochrane Library for reviews and original articles on sarcoidosis published in English from January 1, 2000, to January 1, 2013. We used the search term: sarcoidosis [MeSH] in combination with the following terms: diagnosis [MeSH], etiology [MeSH], epidemiology [MeSH], therapeutics [MeSH], or therapy [Subheading] or drug therapy [MeSH], follow-up studies [MeSH], or treatment outcome [MeSH]. We chose papers mainly from the past 5 years, although we did not exclude frequently referenced and highly regarded older reports. We also searched the reference lists of articles identied by this search strategy and selected those we judged to be relevant. We selected high-quality systematic reviews rather than individual studies.
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
inammation. There is no evidence that sarcoidosis is an infectious disease; rather, it is an exaggerated immune response to pathogen-associated molecular patterns of killed and partly degraded mycobacteria and propionibacteria. Other organic and inorganic substances might also trigger sarcoidosis.15 The pathogen-associated molecular patterns trigger pattern-recognition receptors such as Toll-like receptors 2 and 9, C-type lectins, and NOD-like receptors.16,17 Mycobacteria and propionibacteria persist in macrophage phagosomes because their high lipid content in membranes makes them acid-fast, and many of their glycolipoproteins are not very soluble and resist degradation. Chen and Moller15 used mass spectrometry to identify mycobacterial catalase-peroxidase as an antigen in Kveim test.18 Mycobacterial catalase-peroxidase was detected with immunoblotting in half of the tissue samples from patients with sarcoidosis, and further studies showed a mycobacterial catalase-peroxidase-specic T-cell response to the protein in a similar proportion of patients with sarcoidosis.15 The possible role of mycobacterial antigens in the development of sarcoidosis is supported by many studies that detected mycobacterial pathogen-associated molecular patterns in tissues from patients with sarcoidosis substantially more often than in tissues from healthy individuals. Moreover, several dierent pathogenassociated molecular patterns from mycobacteria, such as mycobacterial catalase-peroxidase, superoxide dismutase A, and cord factor, induce pulmonary granuloma in mice.19,20 Products from propionibacteria, including DNA, have been found in higher percentages of patients with sarcoidosis, and many patients show a specic T-cell response against propionibacterial-derived antigens.21 Notably, lysates from heat-killed propionibacteria can induce pulmonary granuloma in mice.22 Therefore, a microbial-induced host response promotes the aggregation and persistence of the non-degradable antigens, forming a nidus for granuloma formation.18 This formation causes sarcoid lesions through an exaggerated immune response from the close interaction between macrophages and T cells, which stimulate each other.23
pattern-recognition receptor ligands,24 and have an increased TNF response when stimulated by TLR4.25 There is also an inux of CXCR3-positive T-helper 1 (Th1) cells in organs with a sarcoid manifestation, which is triggered by increased pulmonary production of CXCR3 chemokines such as CXCL10.26 In-situ activation of T lymphocytes causes production of interferon-, TNF, and interleukin 2, resulting in a Th1 immune response.23 Furthermore, activated macrophages and dendritic cells shift the T-cell response towards Th1 dierentiation, and vice versa, Th1 cytokines activate antigen-presenting macrophages. Data suggest that although increased interleukin 17 production and Th17-positive cellular inltrates have been reported, the role of Th17 cells in sarcoidosis is still to be dened.27 Th1 immune response is exaggerated further because of the absence of negative immunological feedback signals deliveredeg, by regulatory T cells (Tregs). Low numbers of Tregs that have a reduced function have been reported in sarcoidosis, but their function could be restored by an experimental therapy with vasoactive intestinal peptide that leads to a reduction in the production of TNF by cells present in the bronchoalveolar lavage cells.28,29
Granuloma formation
Epithelioid-cell-rich granulomas that are non-necrotising are thought to trap remnants of causative agents that cannot be further degraded. The reasons why sarcoidosis spontaneously resolves in some patients and progresses in others are poorly understood. In the progressive disease, the antigen is postulated to persist, thereby inducing a chronic immune response.18,23 However, in patients with spontaneous resolution, an increased release of the immunosuppressive cytokine transforming growth factor (TGF) has been noted,30 which lends supports to treatments manipulating the cytokine network with monoclonal antibodies to stop exaggerated proinammatory cytokines such as TNF.31
Genetics
The immunological events we discussed above depend on a predisposing genetic background. Specic MHC-2 alleles can determine the course of the diseaseHLADRB1*03 predisposes to disease with spontaneous resolution and HLA-DRB1*14 or HLA-DRB1*15 are predisposing for a chronic course.32 Several studies on the MHC-2 genes show clear associations of the gene variations with sarcoidosis susceptibility, phenotype, and prognosis. An MHC-1 association is superimposed onto named MHC-2 associations, which aect disease resolution or persistence.3335 Immune-cell activation is regulated at several stages by costimulatory mechanisms and the cytokine network. Several candidate geneassociation studies have identied genetic loci and, most interestingly, many of these variant genes are involved in the regulation of the immune responseeg, Toll-like receptors,36 MHC-2 transactivators,33 and
Inammatory mechanisms
Whereas alveolar macrophages from healthy donors suppress eector T-cell responses, alveolar macrophages from patients with sarcoidosis have excellent antigenpresenting capacities. This increased response is caused by the upregulated expression and function of MHC-2 molecules and costimulatory molecules such as CD86, CD80, ICAM, and CD40.23 In the lung, these macrophages resemble dendritic cells,23 suggesting the ability to change from one type to another. In acute sarcoidosis, the number of CD14 positive macrophages increasessuggesting the inux of peripheral-blood monocyte-derived cells, which proliferate in situ.23 Notably, alveolar macrophages from patients with sarcoidosis are hyper-reactive to distinct
2
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
others. However, replication is still needed for many of those studies. Genome-wide association studies have identied previously unsuspected loci that increase sarcoidosis susceptibility: BTNL2,37 ANXA11,38 and others. Although these genes have a role in the immune system, the mechanisms that underlie the newly identied associations are often not obvious, but BTNL2 could function as a costimulatory molecule.39 These ndings show sarcoidosis is associated with a genetic risk prole made up of many variant genes. Each of the known susceptibility genes confers an increased sarcoidosis risk, with an odds ratio of between 11 and 18, but these genes will substantially aect disease predisposition when combined. New approaches such as transcriptome or miRNA analysis should be used to identify specic signatures of clinical usefulness. With these techniques, subphenotype-specic gene expression patterns have been identied for brotic sarcoidosis,40 and interactive gene networks have been discovered that include unexpected but important genes such as those for the matrix metalloproteinases.41 Signatures for protein expression, mRNA transcription, or miRNA obtained with these techniques might be useful for dierential diagnoses or to identify subphenotypes of prognostic relevance such as treatment resistance. Together, these data suggest the existence of several disorders that are diagnosed as sarcoidosis.
Symptoms consistent with sarcoidosis
Dierences in genetic backgrounds, immunological responses, and causative agents that are so far unrecognised will lead to the denition of subsyndromes, which will probably need dierent therapeutic approaches. Studies of those targets are in progress.
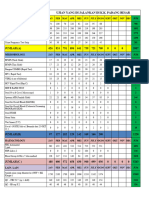
Diagnosis
There have been several new insights in the diagnosis of sarcoidosis (gure 1). Endobronchial ultrasound-guided transbronchial needle aspiration is a highly eective investigation for mediastinal and hilar lymphadenopathy, and can prevent the need for 87% of mediastinoscopies.42 Moreover, rapid on-site assessment by well trained cytologists provides sucient diagnostic information for the bronchoscopist about the need for additional lymphnode passes or transbronchial lung biopsy samples,43 and might be an alternative to doing endobronchial and transbronchial lung biopsy rst. F-FDG PET can be used to accurately assess inammatory activity4447 in patients with unexplained, persistent, disabling symptoms without serological inammatory activity, and can help to predict pulmonary deterioration at 1 year, and the pulmonary improvement expected after treatment. Inhibition of the physiological myocardial uptake with heparin injection or appropriate diets can enable the detection of cardiac sarcoidosis active lesions with F-FDG PET.48,49 Knowledge of pulmonary hypertension, cardiac involvement, small-bre neuropathy, fatigue,
Eliminate other diseases including tuberculosis; berylliosis Abnormal chest radiograph
Lfgrens and Heerfordts syndromes; BHL and uveitis; asymptomatic BHL
EPLs
Stage 3
Stage 2
Symptomatic BHL
Skin; lymph node; conjunctival nodule
Other EPLs
Endoscopy BB, BAL, TBB
Endoscopy BB, BAL
Follow-up
Normal chest radiograph
Yes
No
No
Yes
Minor salivary gland biopsy
No
BAL
Endobronchial ultrasound and ROSE
Yes
18
F-FDG PET
Biopsy sample with granulomas (or BAL-positive)
Sarcoidosis
Figure 1: Diagnosis of sarcoidosis Solid line indicates usual practice. Dotted line indicates alternative practice. BHL=bilateral hilar lymphadenopathy. EPL=extrapulmonary localisations. BB=bronchial biopsy. BAL=bronchoalveolar lavage. TBB=transbronchial biopsy. ROSE=rapid on-site cytological examination. F-FDG=F-uorodeoxyglucose.
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
cognitive failure, and impaired health status and quality of life has improved.5053 Initial manifestations of sarcoidosis vary with race, sex, and age (appendix p 1).1 The most common manifestations are persistent cough, localisation of disease in the skin, eye, and peripheral lymph nodes, erythema nodosum, fatigue, and incidental abnormal chest radiograph. Skin localisation of disease usually leads to a rapid diagnosis; however, diagnosis can be slow because persistent nonspecic respiratory symptoms and rare manifestations often do not prompt the need for a chest radiograph.54 The three criteria for diagnosis are: clinical and radiological presentation, evidence of non-caseating granulomas, and evidence of no alternative diseases.1 Condence in diagnosis can be strengthened with time. The respective weight of each criterion varies with presentation as noted in the following example scenarios. In our rst scenario, diagnosis relies exclusively on a specic presentation (eg, Lfgrens syndrome and Heerfordts syndrome), or it could match a few easily recognisable diagnoses (eg, bilateral perihilar masses on a chest radiograph where silicosis is dierentiated by history of reported occupation), making study of biopsy samples useless. In our second scenario, there is an initially isolated localisation or confusing element (eg, radiological pulmonary alveolar pattern) that is shared by other diseases, analysis of histological samples is crucial. In our third scenarioie, granulomatous disease that is conrmed easily with analysis of histological samples the elimination of all other granulomatoses (eg, tuberculosis or berylliosis) is crucial. The most common diagnostic signs are bilateral intrathoracic hilar lymphadenopathy or diuse micronodular pulmonary inltration at chest radiograph, associated with a typical lymphatic distribution or a galaxy sign on CT (gure 2),55 and the presence of some extrapulmonary localisations of diseaseeg, in the eye and skin (table 1, appendix p 1). If less characteristic clinical or radiological manifestations predominate, the combined presence of these signs substantially increases the amount of diagnostic condence.68
A
Diagnosis of sarcoidosis is improved by a biopsy sample that shows non-caseating epithelioid granulomas. One positive biopsy analysis result is usually sucient. Biopsy sample analysis is recommended before treatment. However, biopsy sampling is not needed for the diagnosis of Lfgrens syndrome and, according to many physicians, for typical bilateral hilar lymphadenopathy that is asymptomatic or associated with uveitis, or for advanced cases of sarcoidosis with no eect on treatment. The best biopsy site depends on accessibility, safety, and potential yield of the procedure according to presentation (gure 1). Biopsy samples of supercial lesionsskin lesions other than erythema nodosum, palpable peripheral lymph node, or visible conjunctival nodulesshould be considered before other sites. If none of these factors are present, then exible bronchoscopy with endobronchial and transbronchial lung biopsy and endobronchial ultrasound are cornerstone investigations. Bronchoalveolar lavage shows a moderate (2050%) lymphocytosis in 80% cases of sarcoidosis and a T lymphocyte CD4:CD8 ratio higher than 35 in 50% of cases, and this technique could be used to support sarcoidosis diagnosis.69 Analysis of a biopsy sample of minor salivary gland is useful when previous samples have failed, or when no target is easily accessible. Dierential diagnoses that should be considered are: infections, particularly tuberculosis; occupationally induced, environmentally induced, and drug-induced granulomatosis; common variable immune deciency; Blaus syndrome; sarcoid-like reactions in cancers and lymphomas, and other idiopathic granulomatosis (appendix p 3). Diagnosis of common variable immune deciency relies on hypogammaglobulinaemia,70 and the diagnosis of chronic pulmonary berylliosis is dependent on a focused questionnaire and on beryllium hypersensitivity.71 All specic manifestations of sarcoidosis, even when asymptomatic, should be recognised through diagnostic work-up (appendix p 2). General symptoms, health status, and quality of life should be assessed.
B
Figure 2: CT of typical features of lung sarcoidosis (A) Shows typical perilymphatic distribution of micronodules with ssural spreading. (B) Shows typical nodules with irregular margins and satellite micronodules known as the galaxy sign.
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
Prevalence (%) Skin56 Peripheral lymphadenopathy1,57 Eye58,59 Liver60 ~15 1020 1030 2030
Symptoms Papules, nodules, plaques, scar sarcoidosis, lupus pernio, subcutaneous sarcoidosis Mostly cervical or supraclavicular; inguinal, axillary, epitrochlear, or submandibular lymph node sites also possible; painless and mobile Anterior, intermediate, or posterior uveitis; retinal vascular change; conjunctival nodules; lacrimal gland enlargement Often symptom-free; abnormal liver function tests in 2030% of patients; hepatomegaly; rarely hepatic insuciency, chronic intrahepatic cholestasis, or portal hypertension Splenomegaly; rarely, pain or pancytopenia; very rarely, splenic rupture
Investigations Biopsy (except for in lupus pernio) Biopsy Systematic ophthalmologist examination, slit-lamp examination, uorescein angiography Systematic liver function tests, abdominal echography and CT, biopsy recommended if moderate or severe abnormalities on liver tests Echography and CT
Spleen57 Heart48,49,61,62
~10 25
Systematic electrocardiography, echocardiography, 24 h Atrioventricular or bundle branch block; ventricular tachycardia or brillation; congestive heart failure; pericarditis; impairment of sympathetic Holter monitoring, concentration of brain natriuretic peptide and pro-brain natriuretic peptide, MRI, perfusion nerve activity; sudden death scintigraphy, F-FDG PET, imaging of sympathetic innervation, biopsy is rarely done Facial nerve palsy, optic neuritis, leptomeningitis, diabetes insipidus, hypopituitarism, seizures, cognitive dysfunction, decits, hydrocephalus, psychiatric manifestations, spinal cord disease, polyneuropathy, small-bre neuropathy Rare symptoms; increased creatininemia sometimes associated with hypercalcaemia; nephrocalcinosis; kidney stones Symmetrical parotid swelling, Heerfordts syndrome when associated with uveitis, fever, and facial palsy Nasal stuness, nasal bleeding, crusting, anosmia Hoarseness, breathlessness, stridor, dysphagia Often asymptomatic; hands and feet classically most involved, also large bones and axial skeleton Proximal muscle weakness, amyotrophy, myalgia, intramuscular nodules All organs can be involved, including breast, uterus, epididymis, and testicle Most often symptom-free, but the oesophagus, stomach, small intestine, and colon can be involved CSF investigation, MRI, hormonal dose, electromyography, temperature-threshold testing; biopsy is rarely done
Nervous system6365
~5
Kidney66 Parotitis1 Nose57 Larynx57 Bones67 Skeletal muscles67 Genitourinary tract1,57 Gastrointestinal tract 1
052 4% 056 051 <5 1 1
Systematic renal tests, biopsy analysis Sinus CT, rhinoscopy, biopsy Laryngoscopy, biopsy Radiography, MRI, F-FDG PET, sometimes biopsy is done Creatine phosphokinase test, MRI, F-FDG PET, electromyography, biopsy Biopsy Endoscopy, biopsy
CSF=cerebrospinal fluid. F-FDG=F-uorodeoxyglucose.
Table 1: Extrapulmonary localisations of sarcoidosis
The most common symptom of mediastinalpulmonary manifestations of sarcoidosis is a persistent cough. Dyspnoea, which is rare in the early stages of the disease, becomes more frequent later on. Wheezing and haemoptysis are infrequent. Crackles are rare. Chest radiographs, abnormal in 90% of cases, show lymphadenopathy in 2565%, diuse pulmonary inltration in 40%, and pulmonary brosis in 5% of patients at presentation. Scadding radiographical staging classies disease as stage 1 (lymphadenopathy alone), stage 2 (pulmonary inltration with lymphadenopathy), stage 3 (pulmonary inltration without lymphadenopathy), and stage 4 (pulmonary brosis), although this scale shows poor interobserver agreement, particularly for stage 4 disease.1,72 Thoracic CT, although not always needed, helps when there is a dicult diagnosis or complications, particularly pulmonary brosis.55,73 CT can show the eects of granulomatous and brous lung lesions respective contributions on disease (gure 3A),74 and can be used to reliably assess disease severity. F-FDG PET accurately shows active inammation in stage 4.44 Volume restriction or airow limitation indicates lung
and airway involvement, while a decreased diusion capacity of carbon monoxide and an abnormal ow volume curve are most typical. The 6 min walk distance is often reduced in sarcoidosis and is correlated with results from the St Georges respiratory questionnaire and forced vital capacity assessments.75 Bronchial endoscopy is used to access granulomas and to visualise proximal airways. In particular situations, cardiopulmonary exercise testing could help to detect impaired pulmonary gas exchange during exercise in patients with unexplained disabling symptoms, and normal results for spirometry and diusion capacity of carbon monoxide.76,77 Cardiopulmonary exercise testing can also help investigators to understand mechanisms behind dyspnoea of unclear origin and assess overall disease eect,76,77 and can be a predictor for the decline in pulmonary function and for prolonged immunosuppressive treatment.78,79 The combination of pulmonary function tests, endoscopy, and CT allow the assessment of causes of airow limitationsbronchial mucosal nodules, bronchial distortion and narrowing
5
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
secondary to lung brosis, localised bronchial stenoses, extrinsic compression, bronchiolitis, and airway hyperreactivity.68 Pulmonary hypertension is caused by many mechanisms,80 and should be suspected when there are persistent dyspnoea insensitive to corticosteroids, pulmonary brosis, abnormal 6 min walk distance, reduced diusion capacity of carbon monoxide, a need for supplementary oxygen, or echocardiographic results suggestive of cor pulmonale. Denite diagnosis of pulmonary hypertension and exclusion of left ventricular dysfunction can only be conrmed with right heart catheterisation.52 Contrast CT is used to rule out pulmonary embolism, and helps to specify the mechanisms in pulmonary hypertension.80 3050% of patients show extrapulmonary disease localisations, which can sometimes be the major disease manifestation (table 1).57 Extrapulmonary localisations can be initial or occur later, and can be isolated symptoms or not. Extrapulmonary localisations should be detected with a thorough physical examination, in a systematic ophthalmological examination with a slit lamp, and with an electrocardiogram (ECG)61 and blood tests. The sarcoid origin of extrapulmonary localisations should then be assessed. Published criteria help to classify extrapulmonary
A
localisations as denite, probable, or possible.57 Diagnosis is most dicult when only one organ is initially involved in uncommon localisations or when a biopsy is not possible.63 An occult localisation for biopsy sample might be found with the use of F-FDG PET.81 An international consensus58 has dened categories for ocular manifestations from denite to possible ocular sarcoidosis on the basis of presentation. The diagnosis of cardiac sarcoidosis, a potentially life-threatening localisation, is the most challenging without consensus.61 Manifestations include atrioventricular block, ventricular arrhythmias, congestive heart failure, sudden death, and consequences of impairment in sympathetic nerve activity. The presence of fragmented QRS or a bundle branch block pattern is associated with cardiac involvement.82 A myocardial biopsy sample that is positive is hard to obtain. Despite a revision in 2006, the Japanese Ministry of Health and Welfare guidelines do not include the most recent imaging investigations. Delayedenhancement cardiovascular magnetic resonance identies many more patients with cardiac sarcoidosis than do the Japanese Ministry of Health and Welfare guidelines for diagnosing cardiac sarcoidosis, and damage detected might be associated with future adverse
B
Figure 3: Imaging of various organ localisations in sarcoidosis (A) Fibrotic pattern of pulmonary sarcoidosis at CT. Characteristic features of severe architectural distortion with posterior volume loss and central traction bronchiectasis. (B) Cardiac sarcoidosis diagnosed on cardiac MRI shows subepicardial and transmural delayed enhancement on gadolinium-enhanced T1-weighted sequence. (C) FDG-PET and CT fusion image after dietary modications in the same patient reveals extensive focal uptake of the left ventricle. (D) Neurological involvement in sarcoidosis; typical involvement of hypothalamus, pituitary gland and optic chiasm seen on a sagittal gadolinium-enhanced T1-weighted sequence MRI (small arrow). Abnormal nodular enhancement of the fourth ventricle is also seen (arrow).
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
cardiac events (gure 3B).72 However, F-FDG PET could be the most reliable method for the detection of granulomatous myocardial lesions (gure 3C).48,49 Neurosarcoidosis can involve all parts of the nervous system. However, central nervous system (CNS) diagnosis is denite only in a minority of cases since neural biopsy is dicult to do.83 Features at presentation, MRI (gure 3D), CSF analysis, ophthalmological examination, biopsy of extraneural organs, and other tests, often allow a probable diagnosis. Infections, multiple sclerosis, and neoplasms should be excluded.83 Diagnosis of spinal-cord sarcoidosis is dicult with discreet extraneurological signs in most cases.64,65 Small-bre neuropathy is recognised as a frequent, chronic, and disabling disorder.51,84 Peripheral pain, dysaesthesia, and various autonomic disturbances are the most common symptoms.84 Without a diagnostic gold standard for diagnosis of small-bre neuropathy, a screening list is useful.51 Another disabling symptom is fatigue, which occurs in up to 70% of patients, and can be measured and monitored with a validated fatigue assessment scale.85 This symptom is independent of disease activity, and is increased by dyspnoea, 6 min walk distance reduction, and muscular pain. Fatigue is multifactorial and can be caused by granuloma burden, weight gain and diabetes due to corticosteroid therapy, depression, sleeping disorders, hypothyroidism, and unknown factors.50 Cognitive failure is also a common problem in patients with sarcoidosis, irrespective of disease severity.86 Eventually, quality of life might be impaired,87 with fatigue, sleep, day-to-day activities, and working capacity all being aected. Tests of serum angiotensin-converting enzyme concentrations even after correction for a genetic insertion or deletion polymorphism that aects serum concentrations,88 are not accurate for diagnosis of sarcoidosis. Chitotriosidase might be a better option for diagnosis.89 Reliable biomarkers of inammatory activity are needed to manage patients with unexplained persistent symptoms that are disabling.46 Serum interleukin-2 receptor, neopterin, chitotriosidase,89 lysozyme, KL-6 and amyloid A90 are interesting biomarkers for assessing activity. Interleukin-2 receptor and neopterin predict F-FDG PET uptake, but they do not have a 100% sensitivity.46 Moderate and severe liver test abnormalities are associated with advanced histopathological changes.60 Abnormal creatininaemia should prompt searches for a renal localisation or nephrocalcinosis.66 The cause of thrombocytopeniaeg, splenomegaly, bone-marrow localisation, or immune should be investigated.91 Hypercalcaemia is most common in white men older than 40 years of age; during the summer; and hypercalcaemia is less common than hypercalciuria, a cause of kidney stones.66 Assessments of the concentrations of plasma N-terminal pro-brain natriuretic peptide and troponin T are useful for the diagnosis of cardiac sarcoidosis.92,93
Monitoring
Clinical course and prognosis
The clinical course for sarcoidosis varies (appendix p 3). In half of cases, disease resolves spontaneously within 2 years, and does so in many other cases within 5 years. After 5 years, remission is much less likely.1,31,94 These dierent outcomes have led to the classication of sarcoidosis into acute (2 years) and chronic (35 years) phenotypes.1,31,94 Refractory sarcoidosis refers to patients progressing despite treatment.3 The main concerns with chronic sarcoidosis are brosis (pulmonary and extrapulmonary), pulmonary hypertension, and persistent disabling symptoms and impaired quality of life. Several indicators of prognosis have been reported (appendix p 4).1,31,94 There is an inverse relation between radiographical stage at presentation and the probability of spontaneous recovery. Several investigators have attempted to devise a comprehensive scoring system to assess severity of disease.3,95,96 Two scores have been reported that integrate whether treatment is needed, and whether the treatment should last for more than 12 months.3,95 However, neither score has been prospectively validated. Serum concentrations of interleukin-2 receptor, neopterin, and chitotriosidase might be markers of sarcoidosis activity and progression,88,97 but their value in routine practice has not been dened clearly.98
Follow-up
The modalities and duration for monitoring patients with sarcoidosis during follow-up have not been standardised. A general guide should be: clinical examination and chest radiograph every 36 months, pulmonary function tests, ECG and blood tests that include serum creatinine and calcium concentrations measurements every 6 months. An accurate denition of change in pulmonary sarcoidosis might be dicult.99 Changes in chest radiographs can help to diagnose pulmonary exacerbations,99,100 and to exclude any complications or comorbidities; however, pitfalls with this technique72 can be countered with the simultaneous use of pulmonary function tests and taking into account symptoms. Measurement of serial serum angiotensinconverting enzyme has no established role in the monitoring of sarcoidosis.98 Although disease relapse in patients with spontaneous remission is rare (8%), 3774% of treated patients have exacerbation or relapse when corticosteroids are tapered or discontinued.101 Relapses mostly occur 26 months after corticosteroid withdrawal, and are rare after 3 years without symptoms.101 This fact justies a minimum 3 year follow-up after the end of treatment before recovery can be conrmed,101 consequently, the involvement of originally unaected organs should raise the possibility of an associated comorbidity. Pregnancy does not usually interfere with sarcoidosis, but a are up is not uncommon shortly after delivery.102
7
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
Morbidity and mortality
About 20% of patients have permanent clinical symptoms because of irreversible brosis, mainly pulmonary brosis.1 Around 12% of all stage 4 patients need longterm oxygen therapy, and many develop diverse complications, including pulmonary hypertension (297%) and aspergilloma (113%).103 Patients with sarcoidosis have a lower survival rate than do the general population.103105 Premature death is most often due to sarcoidosis itself. Strikingly, in the previous two decades, sarcoidosis-related mortality has increased, particularly in patients aged 5574 years.105 Mortality is reported to be up to 76%.105 In western countries, most fatalities from sarcoidosis are due to advanced pulmonary brosis and less commonly, cardiac, CNS and hepatic involvement.1 Most decedents with stage 4 disease (687%) die from respiratory failure or pulmonary hypertension or both. Other causes of death include haemoptysis from aspergilloma.103 Pulmonary hypertension is the most robust predictor of mortality in patients who are candidates for lung transplantation106 and in unselected stage 4 patients.103 Precapillary pulmonary hypertension is associated with increased mortality compared to no pulmonary hypertension or pulmonary hypertension with left-ventricular dysfunction.52 In Japan, the main cause of mortality is cardiac involvement, which is accountable for 77% of deaths in people with sarcoidosis. Sarcoidosis can also be associated with increased incidence of lymphoma, and be a risk factor for pulmonary embolism.107
Treatment
There is no cure for sarcoidosis, and treatment only changes the granulomatous process and its clinical consequences. The mechanisms of action for drugs that are used in sarcoidosis are only partly understood (table 2). Most drugs target TNF, which has a crucial role in the initiation and perpetuation of the granulomatous response. Debate exists about whether treatment can change the outcome of sarcoidosis, particularly brosis.1 No rm guidelines exist on whether, when, and how treatment should be started.117 Between 20% and 70% of patients need systemic therapy.1,101,118 The decision to treat either immediately or during follow-up is guided by three broad factors: risk of severe dysfunction or irreversible damage to major organs, risk of death, or the presence of incapacitating, constitutional symptoms. The main indications for treatment are involvement of the cardiac, neurological, or renal systems; ocular sarcoidosis that does not respond to topical therapy; and symptomatic hypercalcaemia (appendix p 6).1,2 The best strategy would be to observe newly diagnosed patients that have a high probability of spontaneous resolution, and to decide on a treatment when the disease progresses with concordant radiographical and functional progression in the lung. In terms of evidencebased treatment for sarcoidosis, only a few randomised controlled trials have been done: 13 of corticosteroids,119
8
and ve of immunosuppressive and cytotoxic therapy,120 and ve other randomised controlled trials.31,121123 A pressing need exists for the denition of clinically appropriate endpoints for treatment response.98 Systemic corticosteroids remain the standard treatment (appendix p 6). No clear protocol has been validated for dose and treatment duration (table 2).124 Initial treatment is often prednisone 2040 mg daily for 612 weeks, with the dose reduced after this time. In some life-threatening situations such involvement of the heart, CNS, and kidney, or severe ophthalmological localisations, the initial dose is 1 mg/kg daily. Although a minimum of 12 months of maintenance therapy is often advised to prevent relapse, several investigators think that treatment should be stopped as early as 6 months after initiation.124 Adjustments to treatments should be made according to clinical presentation. Patients with chronic sarcoidosis might need low-dose treatment for many years, whereas treatment for 36 months might be adequate for patients with acute forms of disease. Although systemic corticosteroid treatment for symptomatic sarcoidosis has short-term benets, there is little evidence for long-term eect. Evidence from a metaanalysis119 supported that corticosteroid resulted in improvement signs on chest radiographs in patients with stage 2 and stage 3 disease after 624 months of treatment, and slightly improve the forced vital capacity by 42%, and diusion capacity of carbon monoxide by 57%. Whether or not asymptomatic patients with persistent lung inltration should be given systemic treatment is unresolved.2,118,125 The increased awareness of long term side-eects of corticosteroids, and the emergence of new drugs, has changed the treatment of sarcoidosis. Alternative or additional options to corticosteroids should be assessed under various circumstances: involvement of specic organs, contraindication for corticosteroids, a need for a corticosteroid-sparing therapy, and corticosteroid-resistant disease (table 2; appendix p 6). Antimalarial drugs or tetracyclines might be preferable to corticosteroids for mild skin involvement, and antimalarial drugs are preferred for mild hypercalcaemia.1,2 Conventional corticosteroid-sparing drugs are antimalarial drugs,125 methotrexate,126 or azathioprine.109 Methotrexate is more commonly used for corticosteroid-resistant disease than is azathioprine.2 In a Delphi survey,108 methotrexate was the second-choice treatment for most physicians specialising in sarcoidosis. However, because methotrexate has a delayed eect, it has to be used with corticosteroids when both a rapid eect is needed for sarcoidosis that involves vital organs and a prolonged course of disease is anticipated. Results of two retrospective uncontrolled studies suggest that leunomide might enable reduction of corticosteroid dose,110 and that it might be ecient alone or when used with methotrexate in pulmonary and other extrapulmonary localisations that have a poor response with therapy or if there are toxic eects from the previous treatment.110,127
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
About 10% of patients with chronic sarcoidosis will still have active disease despite being given at least one immunosuppressant drug.3 In the past 10 years, TNF antagonists were used increasingly as the treatment of chronic sarcoidosis. Iniximab showed ecacy in a randomised controlled trial compared with placebo in a population with pulmonary refractory sarcoidosis.31 However, the improvement in forced vital capacity was
Usual dose Corticosteroids Prednisone Unstable psychiatric 2040 mg/day initially*, 510 mg/day (or equivalent disorder alternate-day dosing) for maintenance treatment 1020 mg once per week orally or intramuscularly. Folate supplementation to prevent gastrointestinal toxic eects 50200 mg per day
only 25%, and there was no gain in St Georges Respiratory Questionnaire dyspnoea score, and 6 min walk distance.31 Post-hoc exploratory analyses report that patients with long-lasting disease, lower forced vital capacity, higher St Georges Respiratory Questionnaire total score, greater dyspnoea,31 or increased C-reactive protein,128 at baseline benet more from treatment than do those given placebo. Iniximab was also ecacious
Main side-eects Monitoring needed Comments
Main contraindications
Weight gain, hypertension, osteoporosis, diabetes, infection, neuropsychiatric reactions Gastointestinal eects, neutropenia, liver and renal toxicity, interstitial pneumonitis, alopecia Gastrointestinal eects, neutropenia, liver toxicity, photosensitivity, skin carcinoma
Weight, arterial blood pressure, glycaemia, bone density
The most eective, rapid-acting, and available drug. First-line treatment for severe sarcoidosis
Cytotoxic drugs Methotrexate Liver and severe renal failure; severe respiratory failure; alcohol abuse; pregnant or lactating women Lactating women; association with allopurinol Complete blood count liver function tests, and renal function every 412 weeks Preferred second-line therapy for corticosteroid-resistant sarcoidosis or as a corticosteroid-sparing drug.108 Delayed eect (up to 6 months) Similar comments as methotrexate but fewer data are available.109 can be used in men and women who want to have children, and used during pregnancy
Azathioprine
Complete blood count and liver function tests every 412 weeks; consider thiopurine S-methyltransferase genotyping Complete blood count and renal function tests every 412 weeks
Leunomide
1020 mg per day
Liver and renal failure; bone marrow dysfunction; pregnant or lactating women
Gastrointestinal eects, diarrhoea, liver toxicity, neutropenia, neuropathy, hypertension
Insucient data: might be useful in patients not responding well or who are intolerant to methotrexate or as a corticosteroid-sparing drug.110 Combination treatment with methotrexate is possible, fewer pulmonary toxic eects than with methotrexate Potentially serious side-eects that restrict its use; might be useful for refractory CNS83 and cardiac involvement; rapid eect
Cyclophosphamide
50150 mg per day orally; or 5001200 mg every 34 weeks intravenous pulse
Severe renal failure; bone marrow dysfunction; pregnant or lactating women
Neutropenia, gastrointestinal eects, haemorrhagic cystitis, possible irreversible sterility in both men and women, increased risk of malignancy, mostly bladder cancer Neutropenia, gastrointestinal eects, diarrhoea, photosensitivity, skin carcinoma Nausea, diarrhoea, gastrointestinal eects
Complete blood count liver function tests and renal function tests every 24 weeks
Mycophenolate mofetil
5003000 mg per day
Pregnant (insucient data on teratogenicity) or lactating women
Complete blood count and liver function tests every 412 weeks
Insucient data, might be useful as a corticosteroid-sparing drug.111 Fewer bone marrow toxic eects and infections than other immunosuppressant drugs Insucient and conicting data; might be useful as a corticosteroid-sparing drug.112 At the dose used, gastrointestinal toxic eects are very restraining112,113 Potentially serious side-eects; useful for severe skin sarcoidosis, particularly lupus pernio; not eective for pulmonary involvement;114 rapid eect; as early as 1 month Useful for chronic and refractory sarcoidosis particularly in lupus pernio, eye, and CNS disease.115 Ecacy for pulmonary disease,31 but whether improvement is clinically relevant is debated. Rapid eect; as early as 2 weeks. Possible loss of response due to antiiniximab antibody formation (Continues on next page)
Cytokine modulators Pentoxifylline 4002000 mg per day Acute myocardial infarction None
Thalidomide
50200 mg per day
Men refusing to wear a condom and women of childbearing age not using contraception; pregnant or lactating women; blood donation Pregnant (insucient data on teratogenicity) or lactating women; New York Heart Association class 3 or 4 heart failure; tuberculosis or other infection
Highly teratogenic; sleepiness, constipation, neuropathy, venous thrombosis, unexplained dyspnoea, bradycardia Allergic reaction. Increased risk of serious infections, mostly tuberculosis, and increased risk of cancer
Pregnancy testing every month and electromyography every 612 weeks
TNF antagonist
Iniximab 35 mg per kg intravenously at week 0, 2, 6, then every 48 weeks
Systematic assessment for tuberculosis before treatment
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
Usual dose (Continued from previous page) Antimicrobial drugs Antimalarial drugs Hydroxychloroquine 200400 mg/day||
Main contraindications
Main side-eects
Monitoring needed
Comments
Retinopathy, breastfeeding
Gastrointestinal eects, rash, retinopathy, neuromyopathy
Complete eye examination every 612 months
Inhibit antigen presentation by reducing degradation capacity of lysosomes; useful for moderate skin disease; hypocalcaemia, and fatigue, as well as a corticosteroid-sparing drug;116 delayed eect up to 6 months Few data: might be useful for moderate skin disease
Tetracycline
Minocycline 200 mg/day, doxycycline 200 mg/day
Pregnancy and breastfeeding, liver failure, sun exposure
Gastrointestinal eects, anaemia, skin photosensitivity
None
*1 mg/kg per 24 h of prednisone might be necessary to control cardiac and CNS disease. High-dose intravenous pulse methylprednisolone might be useful in patients with sarcoidosis that threatens life or organ function, such as in severe cardiac, CNS, laryngeal and renal involvement, or retrobulbar neuritis. All cytotoxic drugs are potentially teratogenic, with the exception of azathioprine. All drugs increase the risk of infection and malignancy. The risk of infection is especially increased with TNF antagonists, and the risk of malignancy with cyclophosphamide. The view that liver biopsy should be done after a cumulative dose of methotrexate of more than 12 g to exclude subclinical toxicity is controversial and non-invasive analysis of liver brosis might be replace liver biopsy. Although thiopurine S-methyltransferase (TPMT) deciency is rare, individuals can develop severe pancytopenia due to azathioprine not being correctly metabolised. Genotyping of TPMT is available and might be helpful to predict patients who will develop toxicity. This sensitivity to azathioprine needs to be identied with the introduction of the drug at 50 mg per day and close monitoring of complete blood count, and should be closely monitored, especially in the rst month of treatment. Iniximab is the preferred TNF antagonists. In some patients, the benet of iniximab is lost within 6 months of discontinuing the drug after 24 weeks of treatment, so most physicians prescribe the drug for a longer time. Adalimumab is another treatment, but much fewer data are available. Etanercept is not eective in sarcoidosis. ||Hydroxychloroquine is preferred to chloroquine because of the lower risk of ocular toxicity. TNF=tumour-necrosis factor-. CNS=central nervous system.
Table 2: Drugs used in sarcoidosis
for extrapulmonary sarcoidosis assessed as a secondary endpoint of the trial, but improvements during the 24 weeks of treatment were lost in the subsequent 24 week washout. Data from retrospective studies lend support to the expectation that a response with iniximab is valuable for some patients, mainly those with CNS115,129 or eye115 recalcitrant involvement, and lupus pernio.115,130 However, the advantage with biological therapy should be tempered by potentially serious toxic eects. By contrast, etanercept is ineective in progressive pulmonary131 and ocular disease.121 Adalimumab is ecacious in uveitis, as well as other disabling symptoms related to sarcoidosis.132 Rituximab is ecacious in refractory ocular lesions.133 Apremilast has been ecient in dicult-to-treat skin localisations.134 Dexmethylphenidate is superior to placebo for the treatment of fatigue, which is an otherwise dicult therapeutic issue.123 However, dexmethylphenidate is an amphetamine psychostimulant that should be prescribed with caution. Combination treatments might act at several levels of disease pathogenesis and have fewer toxic eects. Topical corticosteroids are helpful for the treatment of eye and skin involvement. Although useful for cough and bronchial hyper-reactivity, treatment with inhaled corticosteroids alone do not objectively improve the results in pulmonary function tests or radiograph images.119 Sequential treatment with 3 months of oral prednisone followed by 15 months of inhaled budesonide resulted in a signicant, but small, long-term, functional improvement in patients with recent stage 2 or stage 3 disease.125 In addition to specic treatments, symptomatic and supportive measures are crucial, including reducing intake of calcium and sun avoidance for hypercalcaemia,
10
drugs and implantable devices for cardiac involvement, hormonal substitution for hypothalamicpituitary involvement, and supplemental oxygen.1 Pulmonary rehabilitation has not been assessed. The benet and safety of drugs used for sarcoidosis-related pulmonary hypertension are not established, and might depend on an underlying primary mechanism.135 Endobronchial stenosis can necessitate mechanical dilatation. Antifungal treatment for aspergilloma is controversial, and surgical removal might be problematic in patients with severe pulmonary brosis. In patients with corticosteroid-induced osteoporosis, it is sensible to measure serum and urinary calcium concentrations before and periodically after the start of calcium and vitamin D supplementation. Bisphosphonate treatment should be chosen as the initial strategy for primary prevention of corticosteroid-induced osteoporosis.136 Despite disease-specic issues, transplantation of the lung, liver, heart, or kidney is a reasonable option for endstage sarcoidosis, with results generally matching those of other diagnoses.137 Referral should be made only after medical treatment options have been exhausted, and the disease extent, severity, and activity must be carefully assessed. The presence of aspergilloma should not disqualify potential transplant candidates.137 Recurrence of sarcoidosis in the allograft is 1435%, and is usually not dicult to control with medical treatment.137,138
Conclusions
Sarcoidosis has many manifestations, its prognosis is dicult to predict, and its evolution and severity vary hugely from case to case. A personalised and multidisciplinary approach might be needed to address these challenges and prevent quality-of-life impairment and potential adverse eects of treatment.
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
Contributors DV outlined the Seminar, collected and edited the dierent sections of the draft, and wrote the diagnosis section. AP and JM-Q wrote the pathogenesis section. HN wrote the monitoring and treatment sections. YU, DV, HN, JM-Q, and AP searched for clinical aspects and pathophysiology. P-YB provided the gures. All the authors reviewed the Seminar and approved the nal version. Conicts of interest DV has received scientic advisor consultancy fees from Sano, InterMune, and Actelion; travel and accommodation expenses to attend the American Thoracic Society conference and European Respiratory Society congress, the Congrs de Pneumologie de langue Franaise, and international meeting for orphan diseases 2011 from GlaxoSmithKline, AstraZeneca, Boehringer Ingelheim, Mundipharma, and Actelion; as well as academic grants from Direction de la Recherche Clinique and the Chancellerie des universits de Paris. DV has served as investigator or member of the steering committee for INSPIRE, CAPACITY, BUILD 1, and BUILD 3, and was an investigator in the Centocor (Jansen Biotech)funded trial evaluating golimumab versus placebo in severe sarcoidosis. The other authors declare that they have no conicts of interest. Acknowledgments We thank Emmanuelle Blondet (Haute Autorit de Sant, Saint-Denis, France) for assistance with the search strategy and selection criteria, and thank Gabrielle Kaufman and Sven Lord for assistance with English language editing. References 1 Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med 1999; 160: 73655. 2 Baughman RP, Lower EE, du Bois RM. Sarcoidosis. Lancet. 2003; 361: 111118. 3 Baughman RP, Culver DA, Judson MA. A concise review of pulmonary sarcoidosis. Am J Respir Crit Care Med 2011; 183: 57381. 4 Iannuzzi MC, Fontana JR. Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. JAMA 2011; 305: 39199. 5 Hillerdal G, Nou E, Osterman K, Schmekel B. Sarcoidosis: epidemiology and prognosis. A 15-year European study. Am Rev Respir Dis 1984; 130: 2932. 6 Morimoto T, Azuma A, Abe S, et al. Epidemiology of sarcoidosis in Japan. Eur Respir J 2008; 31: 37279. 7 Varron L, Cottin V, Schott AM, Broussolle C, Seve P. Late-onset sarcoidosis: a comparative study. Medicine (Baltimore) 2012; 91: 13743. 8 Deubelbeiss U, Gemperli A, Schindler C, Baty F, Brutsche MH. Prevalence of sarcoidosis in Switzerland is associated with environmental factors. Eur Respir J 2010; 35: 108897. 9 Newman LS, Rose CS, Bresnitz EA, et al. A case control etiologic study of sarcoidosis: environmental and occupational risk factors. Am J Respir Crit Care Med 2004; 170: 132430. 10 Crowley LE, Herbert R, Moline JM, et al. Sarcoid like granulomatous pulmonary disease in World Trade Center disaster responders. Am J Ind Med 2011; 54: 17584. 11 Perlman SE, Friedman S, Galea S, et al. Short-term and medium-term health eects of 9/11. Lancet 2011; 378: 92534. 12 Rybicki BA, Iannuzzi MC, Frederick MM, et al. Familial aggregation of sarcoidosis. A case-control etiologic study of sarcoidosis (ACCESS). Am J Respir Crit Care Med 2001; 164: 208591. 13 Sverrild A, Backer V, Kyvik KO, et al. Heredity in sarcoidosis: a registry-based twin study. Thorax 2008; 63: 89496. 14 Mller-Quernheim J, Schurmann M, Hofmann S, et al. Genetics of sarcoidosis. Clin Chest Med 2008; 29: 391414. 15 Chen ES, Moller DR. Etiology of sarcoidosis. Clin Chest Med 2008; 29: 36577. 16 Baca A, Scanga CA, Feng CG, Leifer C, Cheever A, Sher A. TLR9 regulates Th1 responses and cooperates with TLR2 in mediating optimal resistance to Mycobacterium tuberculosis. J Exp Med 2005; 202: 171524. 17 Kalis C, Gumenscheimer M, Freudenberg N, et al. Requirement for TLR9 in the immunomodulatory activity of Propionibacterium acnes. J Immunol 2005; 174: 4295300.
18
19 20
21
22
23 24
25
26
27 28 29
30
31
32
33
34
35
36
37
38
39
40
41
Chen ES, Song Z, Willett MH, et al. Serum amyloid A regulates granulomatous inammation in sarcoidosis through Toll-like receptor-2. Am J Respir Crit Care Med 2010; 181: 36073. Chen ES, White ES. Innate pathways shape sarcoidosis signaling: from bugs to drugs. Am J Respir Crit Care Med 2011; 183: 42527. Swaisgood CM, Oswald-Richter K, Moeller SD, et al. Development of a sarcoidosis murine lung granuloma model using Mycobacterium superoxide dismutase A peptide. Am J Respir Cell Mol Biol 2011; 44: 16674. Ishige I, Usui Y, Takemura T, Eishi Y. Quantitative PCR of mycobacterial and propionibacterial DNA in lymph nodes of Japanese patients with sarcoidosis. Lancet 1999; 354: 12023. McCaskill JG, Chason KD, Hua X, et al. Pulmonary immune responses to Propionibacterium acnes in C57BL/6 and BALB/c mice. Am J Respir Cell Mol Biol 2006; 35: 34756. Zissel G, Prasse A, Mller-Quernheim J. Immunologic response of sarcoidosis. Semin Respir Crit Care Med 2010; 31: 390403. Rastogi R, Du W, Ju D, et al. Dysregulation of p38 and MKP-1 in response to NOD1/TLR4 stimulation in sarcoid bronchoalveolar cells. Am J Respir Crit Care Med 2011; 183: 50010. Wiken M, Grunewald J, Eklund A, Wahlstrom J. Higher monocyte expression of TLR2 and TLR4, and enhanced pro-inammatory synergy of TLR2 with NOD2 stimulation in sarcoidosis. J Clin Immunol. 2009; 29: 7889. Pignatti P, Brunetti G, Moretto D, et al. Role of the chemokine receptors CXCR3 and CCR4 in human pulmonary brosis. Am J Respir Crit Care Med 2006; 173: 31017. Facco M, Cabrelle A, Teramo A, et al. Sarcoidosis is a Th1/Th17 multisystem disorder. Thorax 2011; 66: 14450. Miyara M, Amoura Z, Parizot C, et al. The immune paradox of sarcoidosis and regulatory T cells. J Exp Med 2006; 203: 35970. Prasse A, Zissel G, Lutzen N, et al. Inhaled vasoactive intestinal peptide exerts immunoregulatory eects in sarcoidosis. Am J Respir Crit Care Med 2010; 182: 54048. Zissel G, Homolka J, Schlaak J, Schlaak M, Mller-Quernheim J. Anti-inammatory cytokine release by alveolar macrophages in pulmonary sarcoidosis. Am J Respir Crit Care Med 1996; 154: 71319. Baughman RP, Drent M, Kavuru M, et al. Iniximab therapy in patients with chronic sarcoidosis and pulmonary involvement. Am J Respir Crit Care Med 2006; 174: 795802. Berlin M, Fogdell-Hahn A, Olerup O, Eklund A, Grunewald J. HLA-DR predicts the prognosis in Scandinavian patients with pulmonary sarcoidosis. Am J Respir Crit Care Med 1997; 156: 160105. Grunewald J, Idali F, Kockum I, et al. Major histocompatibility complex class II transactivator gene polymorphism: associations with Lofgrens syndrome. Tissue Antigens 2010; 76: 96101. Sato H, Woodhead FA, Ahmad T, et al. Sarcoidosis HLA class II genotyping distinguishes dierences of clinical phenotype across ethnic groups. Hum Mol Genet 2010; 19: 410011. Rossman MD, Thompson B, Frederick M, et al. HLA-DRB1*1101: a signicant risk factor for sarcoidosis in blacks and whites. Am J Hum Genet 2003; 73: 72035. Veltkamp M, van Moorsel CH, Rijkers GT, Ruven HJ, Grutters JC. Genetic variation in the Toll-like receptor gene cluster (TLR10-TLR1TLR6) inuences disease course in sarcoidosis. Tissue Antigens 2012; 79: 2532. Valentonyte R, Hampe J, Huse K, et al. Sarcoidosis is associated with a truncating splice site mutation in BTNL2. Nat Genet 2005; 37: 35764. Hofmann S, Franke A, Fischer A, et al. Genome-wide association study identies ANXA11 as a new susceptibility locus for sarcoidosis. Nat Genet 2008; 40: 110306. Nguyen T, Liu XK, Zhang Y, Dong C. BTNL2, a butyrophilin-like molecule that functions to inhibit T cell activation. J Immunol 2006; 176: 735460. Lockstone HE, Sanderson S, Kulakova N, et al. Gene set analysis of lung samples provides insight into pathogenesis of progressive, brotic pulmonary sarcoidosis. Am J Respir Crit Care Med 2010; 181: 136775. Crouser ED, Culver DA, Knox KS, et al. Gene expression proling identies MMP-12 and ADAMDEC1 as potential pathogenic mediators of pulmonary sarcoidosis. Am J Respir Crit Care Med 2009; 179: 92938.
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
11
Seminar
42
43
44
45
46
47
48
49
50 51
52
53
54 55
56 57 58
59 60 61
62 63 64 65
66
Navani N, Lawrence DR, Kolvekar S, et al. Endobronchial ultrasound-guided transbronchial needle aspiration prevents mediastinoscopies in the diagnosis of isolated mediastinal lymphadenopathy: a prospective trial. Am J Respir Crit Care Med 2012; 186: 25560. Plit ML, Havryk AP, Hodgson A, et al. Rapid cytological analysis of endobronchial ultrasound-guided aspirates in sarcoidosis. Eur Respir J 2012; published online Nov 22. DOI:10.1183/09031936.00128312. Mostard RL, Voo S, van Kroonenburgh MJ, et al. Inammatory activity assessment by F FDG-PET/CT in persistent symptomatic sarcoidosis. Respir Med 2011; 105: 191724. Sobic-Saranovic D, Grozdic I, Videnovic-Ivanov J, et al. The utility of F-FDG PET/CT for diagnosis and adjustment of therapy in patients with active chronic sarcoidosis. J Nucl Med 2012; 53: 154349. Mostard RL, Van Kuijk SM, Verschakelen JA, et al. A predictive tool for an eective use of F-FDG PET in assessing activity of sarcoidosis. BMC Pulm Med 2012; 12: 57. Keijsers RG, Verzijlbergen EJ, van den Bosch JM, et al. F-FDG PET as a predictor of pulmonary function in sarcoidosis. Sarcoidosis Vasc Diuse Lung Dis 2011; 28: 12329. Youssef G, Leung E, Mylonas I, et al. The use of F-FDG PET in the diagnosis of cardiac sarcoidosis: a systematic review and metaanalysis including the Ontario experience. J Nucl Med 2012; 53: 24148. Soussan M, Brillet PY, Nunes H, et al. Clinical value of a high-fat and low-carbohydrate diet before FDG-PET/CT for evaluation of patients with suspected cardiac sarcoidosis. J Nucl Cardiol 2013; 20: 12027. Drent M, Lower EE, De Vries J. Sarcoidosis-associated fatigue. Eur Respir J 2012; 40: 25563. Hoitsma E, De Vries J, Drent M. The small ber neuropathy screening list: construction and cross-validation in sarcoidosis. Respir Med 2011; 105: 95100. Baughman RP, Engel PJ, Taylor L, Lower EE. Survival in sarcoidosis-associated pulmonary hypertension: the importance of hemodynamic evaluation. Chest 2010; 138: 107885. Patel AS, Siegert RJ, Creamer D, et al. The development and validation of the Kings Sarcoidosis Questionnaire for the assessment of health status. Thorax 2013; 68: 5765. Judson MA, Thompson BW, Rabin DL, et al. The diagnostic pathway to sarcoidosis. Chest 2003; 123: 40612. Criado E, Sanchez M, Ramirez J, et al. Pulmonary sarcoidosis: typical and atypical manifestations at high-resolution CT with pathologic correlation. Radiographics 2010; 30: 156786. Mana J, Marcoval J. Skin manifestations of sarcoidosis. Presse Med 2012; 41: e35574. Judson MA. Extrapulmonary sarcoidosis. Semin Respir Crit Care Med 2007; 28: 83101. Herbort CP, Rao NA, Mochizuki M. International criteria for the diagnosis of ocular sarcoidosis: results of the rst international workshop on ocular sarcoidosis (IWOS). Ocul Immunol Inamm 2009; 17: 16069. Bodaghi B, Touitou V, Fardeau C, Chapelon C, LeHoang P. Ocular sarcoidosis. Presse Med 2012; 41: e34954. Cremers J, Drent M, Driessen A, et al. Liver-test abnormalities in sarcoidosis. Eur J Gastroenterol Hepatol 2012; 24: 1724. Hamzeh NY, Wamboldt FS, Weinberger HD. Management of cardiac sarcoidosis in the United States: a Delphi study. Chest 2012; 141: 15462. Patel MR, Cawley PJ, Heitner JF, et al. Detection of myocardial damage in patients with sarcoidosis. Circulation 2009; 120: 196977. Nozaki K, Scott TF, Sohn M, Judson MA. Isolated neurosarcoidosis: case series in 2 sarcoidosis centers. Neurologist 2012; 18: 37377. Hoitsma E, Faber CG, Drent M, Sharma OP. Neurosarcoidosis: a clinical dilemma. Lancet Neurol 2004; 3: 397407. Cohen-Aubart F, Galanaud D, Grabli D, et al. Spinal cord sarcoidosis: clinical and laboratory prole and outcome of 31 patients in a case-control study. Medicine (Baltimore) 2010; 89: 13340. Mahevas M, Lescure FX, Boa JJ, et al. Renal sarcoidosis: clinical, laboratory, and histologic presentation and outcome in 47 patients. Medicine (Baltimore) 2009; 88: 98106.
67
68
69
70
71
72
73 74
75 76
77
78
79
80 81
82
83 84 85
86
87
88
89
90
91
Sweiss NJ, Patterson K, Sawaqed R, et al. Rheumatologic manifestations of sarcoidosis. Semin Respir Crit Care Med 2010; 31: 46373. Nunes H, Uzunhan Y, Gille T, Lamberto C, Valeyre D, Brillet PY. Imaging of sarcoidosis of the airways and lung parenchyma and correlation with lung function. Eur Respir J 2012; 40: 75065. Costabel U, Bonella F, Ohshimo S, Guzman J. Diagnostic modalities in sarcoidosis: BAL, EBUS, and PET. Semin Respir Crit Care Med 2010; 31: 40408. Park MA, Li JT, Hagan JB, Maddox DE, Abraham RS. Common variable immunodeciency: a new look at an old disease. Lancet 2008; 372: 489502. Mller-Quernheim J, Gaede KI, Fireman E, Zissel G. Diagnoses of chronic beryllium disease within cohorts of sarcoidosis patients. Eur Respir J 2006; 27: 119095. Baughman RP, Shipley R, Desai S, et al. Changes in chest roentgenogram of sarcoidosis patients during a clinical trial of iniximab therapy: comparison of dierent methods of evaluation. Chest 2009; 136: 52635. Nunes H, Brillet PY, Valeyre D, Brauner MW, Wells AU. Imaging in sarcoidosis. Semin Respir Crit Care Med 2007; 28:10220. Erdal BS, Crouser ED, Yildiz V, et al. Quantitative computerized twopoint correlation analysis of lung CT scans correlates with pulmonary function in pulmonary sarcoidosis. Chest 2012; 142: 158997. Baughman RP, Sparkman BK, Lower EE. Six-minute walk test and health status assessment in sarcoidosis. Chest 2007; 132: 20713. Marcellis RG, Lenssen AF, de Vries GJ, et al. Is there an added value of cardiopulmonary exercise testing in sarcoidosis patients? Lung 2013; 191: 4352. Wallaert B, Talleu C, Wemeau-Stervinou L, Duhamel A, Robin S, Aguilaniu B. Reduction of maximal oxygen uptake in sarcoidosis: relationship with disease severity. Respiration 2011; 826: 50108. Lopes AJ, Menezes SL, Dias CM, Oliveira JF, Mainenti MR, Guimaraes FS. Cardiopulmonary exercise testing variables as predictors of long-term outcome in thoracic sarcoidosis. Braz J Med Biol Res 2012; 45: 25663. Kollert F, Geck B, Suchy R, et al. The impact of gas exchange measurement during exercise in pulmonary sarcoidosis. Respir Med 2011; 105: 12229. Nunes H, Uzunhan Y, Freynet O, et al. Pulmonary hypertension complicating sarcoidosis. Presse Med 2012; 41: e30316. Treglia G, Taralli S, Giordano A. Emerging role of whole-body 18 F-uorodeoxyglucose positron emission tomography as a marker of disease activity in patients with sarcoidosis: a systematic review. Sarcoidosis Vasc Diuse Lung Dis 2011; 28: 8794. Schuller JL, Olson MD, Zipse MM, et al. Electrocardiographic characteristics in patients with pulmonary sarcoidosis indicating cardiac involvement. J Cardiovasc Electrophysiol 2011; 22: 124348. Zajicek JP, Scolding NJ, Foster O, et al. Central nervous system sarcoidosisdiagnosis and management. Q JM 1999; 92: 10317. Hoitsma E, Marziniak M, Faber CG, et al. Small bre neuropathy in sarcoidosis. Lancet 2002; 359: 208586. De Vries J, Michielsen H, Van Heck GL, Drent M. Measuring fatigue in sarcoidosis: the fatigue assessment scale (FAS). Br J Health Psychol 2004; 9: 27991. Elerich MD, Nelemans PJ, Ponds RW, De Vries J, Wijnen PA, Drent M. Everyday cognitive failure in sarcoidosis: the prevalence and the eect of anti-TNF-alpha treatment. Respiration 2010; 80: 21219. De Vries J, Lower EE, Drent M. Quality of life in sarcoidosis: assessment and management. Semin Respir Crit Care Med 2010; 31: 48593. Biller H, Zissel G, Ruprecht B, Nauck M, Busse Grawitz A, Mller-Quernheim J. Genotype-corrected reference values for serum angiotensin-converting enzyme. Eur Respir J 2006; 28: 108590. Bargagli E, Bennett D, Maggiorelli C, et al. Human chitotriosidase: a sensitive biomarker of sarcoidosis. J Clin Immunol 2013; 33: 26470. Bargagli E, Magi B, Olivieri C, Bianchi N, Landi C, Rottoli P. Analysis of serum amyloid A in sarcoidosis patients. Respir Med 2011; 105: 77580. Mahevas M, Chiche L, Uzunhan Y, et al. Association of sarcoidosis and immune thrombocytopenia: presentation and outcome in a series of 20 patients. Medicine (Baltimore) 2011; 90: 26978.
12
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
Seminar
92
93
94
95
96 97
98 99
100
101
102 103
104
105
106
107
108
109
110
111
112
113
114
115
Handa T, Nagai S, Ueda S, et al. Signicance of plasma NT-proBNP levels as a biomarker in the assessment of cardiac involvement and pulmonary hypertension in patients with sarcoidosis. Sarcoidosis Vasc Diuse Lung Dis 2010; 27: 2735. Baba Y, Kubo T, Kitaoka H, et al. Usefulness of high-sensitive cardiac troponin T for evaluating the activity of cardiac sarcoidosis. Int Heart J 2012; 53: 28792. Neville E, Walker AN, James DG. Prognostic factors predicting the outcome of sarcoidosis: an analysis of 818 patients. Q JM 1983; 52: 52533. Prasse A, Katic C, Germann M, Buchwald A, Zissel G, Mller-Quernheim J. Phenotyping sarcoidosis from a pulmonary perspective. Am J Respir Crit Care Med 2008; 177: 33036. Was YS, Rose CS, Murphy JR, et al. A new tool to assess sarcoidosis severity. Chest 2006; 129: 123445. Ziegenhagen MW, Rothe ME, Schlaak M, Mller-Quernheim J. Bronchoalveolar and serological parameters reecting the severity of sarcoidosis. Eur Respir J 2003; 21: 40713. Keir G, Wells AU. Assessing pulmonary disease and response to therapy: which test? Semin Respir Crit Care Med 2010; 31: 40918. Zappala CJ, Desai SR, Copley SJ, et al. Optimal scoring of serial change on chest radiography in sarcoidosis. Sarcoidosis Vasc Diuse Lung Dis 2011; 28: 13038. Judson MA, Gilbert GE, Rodgers JK, Greer CF, Schabel SI. The utility of the chest radiograph in diagnosing exacerbations of pulmonary sarcoidosis. Respirology 2008; 13: 97102. Rizzato G, Montemurro L, Colombo P. The late follow-up of chronic sarcoid patients previously treated with corticosteroids. Sarcoidosis Vasc Diuse Lung Dis 1998; 15: 5258. King TE Jr. Restrictive lung disease in pregnancy. Clin Chest Med 1992; 13: 60722. Nardi A, Brillet PY, Letoumelin P, et al. Stage IV sarcoidosis: comparison of survival with the general population and causes of death. Eur Respir J 2012; 38: 136873. Gribbin J, Hubbard RB, Le JI, Smith CJ, West J, Tata LJ. Incidence and mortality of idiopathic pulmonary brosis and sarcoidosis in the UK. Thorax 2006; 61: 98085. Swigris JJ, Olson AL, Huie TJ, et al. Sarcoidosis-related mortality in the United States from 1988 to 2007. Am J Respir Crit Care Med 2011; 183: 152430. Shorr AF, Davies DB, Nathan SD. Predicting mortality in patients with sarcoidosis awaiting lung transplantation. Chest 2003; 124: 92228. Swigris JJ, Olson AL, Huie TJ, et al. Increased risk of pulmonary embolism among US decedents with sarcoidosis from 1988 to 2007. Chest 2011; 140: 126166. Schutt AC, Bullington WM, Judson MA. Pharmacotherapy for pulmonary sarcoidosis: a Delphi consensus study. Respir Med 2010; 104: 71723. Mller-Quernheim J, Kienast K, Held M, Pfeifer S, Costabel U. Treatment of chronic sarcoidosis with an azathioprine/prednisolone regimen. Eur Respir J 1999; 14: 111722. Sahoo DH, Bandyopadhyay D, Xu M, et al. Eectiveness and safety of leunomide for pulmonary and extrapulmonary sarcoidosis. Eur Respir J 2011; 38: 114550. Kouba DJ, Mimouni D, Rencic A, Nousari HC. Mycophenolate mofetil may serve as a steroid-sparing agent for sarcoidosis. Br J Dermatol 2003; 148: 14748. Park MK, Fontana JR, Babaali H, et al. Steroid-sparing eects of pentoxifylline in pulmonary sarcoidosis. Sarcoidosis Vasc Diuse Lung Dis 2009; 26: 12131. Zabel P, Entzian P, Dalho K, Schlaak M. Pentoxifylline in treatment of sarcoidosis. Am J Respir Crit Care Med 1997; 155: 166569. Judson MA, Silvestri J, Hartung C, Byars T, Cox CE. The eect of thalidomide on corticosteroid-dependent pulmonary sarcoidosis. Sarcoidosis Vasc Diuse Lung Dis 2006; 23: 5157. Baughman RP, Lower EE, Drent M. Inhibitors of tumor necrosis factor (TNF) in sarcoidosis: who, what, and how to use them. Sarcoidosis Vasc Diuse Lung Dis 2008; 25: 7689.
116 Baltzan M, Mehta S, Kirkham TH, Cosio MG. Randomized trial of prolonged chloroquine therapy in advanced pulmonary sarcoidosis. Am J Respir Crit Care Med 1999; 160: 19297. 117 Bradley B, Branley HM, Egan JJ, et al. Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax 2008; 63 (suppl): v158. 118 Gibson GJ, Prescott RJ, Muers MF, et al. British Thoracic Society Sarcoidosis study: eects of long term corticosteroid treatment. Thorax 1996; 51: 23847. 119 Paramothayan NS, Lasserson TJ, Jones PW. Corticosteroids for pulmonary sarcoidosis. Cochrane Database Syst Rev 2005 2: CD001114. 120 Paramothayan S, Lasserson TJ, Walters EH. Immunosuppressive and cytotoxic therapy for pulmonary sarcoidosis. Cochrane Database Syst Rev 2006; 3: CD003536. 121 Baughman RP, Lower EE, Bradley DA, Raymond LA, Kaufman A. Etanercept for refractory ocular sarcoidosis: results of a double-blind randomized trial. Chest 2005; 128: 106267. 122 Rossman MD, Newman LS, Baughman RP, et al. A double-blinded, randomized, placebo-controlled trial of iniximab in subjects with active pulmonary sarcoidosis. Sarcoidosis Vasc Diuse Lung Dis 2006; 23: 20108. 123 Lower EE, Harman S, Baughman RP. Double-blind, randomized trial of dexmethylphenidate hydrochloride for the treatment of sarcoidosis-associated fatigue. Chest 2008; 133: 118995. 124 Judson MA. An approach to the treatment of pulmonary sarcoidosis with corticosteroids: the six phases of treatment. Chest 1999; 115: 115865. 125 Pietinalho A, Tukiainen P, Haahtela T, Persson T, Selroos O. Early treatment of stage II sarcoidosis improves 5-year pulmonary function. Chest 2002; 121: 2431. 126 Baughman RP, Winget DB, Lower EE. Methotrexate is steroid sparing in acute sarcoidosis: results of a double blind, randomized trial. Sarcoidosis Vasc Diuse Lung Dis 2000; 17: 6066. 127 Baughman RP, Lower EE. Leunomide for chronic sarcoidosis. Sarcoidosis Vasc Diuse Lung Dis 2004; 21: 4348. 128 Sweiss NJ, Barnathan ES, Lo K, Judson MA, Baughman R. C-reactive protein predicts response to iniximab in patients with chronic sarcoidosis. Sarcoidosis Vasc Diuse Lung Dis 2010; 27: 4956. 129 Sodhi M, Pearson K, White ES, Culver DA. Iniximab therapy rescues cyclophosphamide failure in severe central nervous system sarcoidosis. Respir Med 2009; 103: 26873. 130 Stagaki E, Mountford WK, Lackland DT, Judson MA. The treatment of lupus pernio: results of 116 treatment courses in 54 patients. Chest 2009; 135: 46876. 131 Utz JP, Limper AH, Kalra S, et al. Etanercept for the treatment of stage II and III progressive pulmonary sarcoidosis. Chest 2003; 124: 17785. 132 Erckens RJ, Mostard RL, Wijnen PA, Schouten JS, Drent M. Adalimumab successful in sarcoidosis patients with refractory chronic non-infectious uveitis. Graefes Arch Clin Exp Ophthalmol 2012; 250: 71320. 133 Lower EE, Baughman RP, Kaufman AH. Rituximab for refractory granulomatous eye disease. Clin Ophthalmol 2012; 6: 161318. 134 Baughman RP, Judson MA, Ingledue R, Craft NL, Lower EE. Ecacy and safety of apremilast in chronic cutaneous sarcoidosis. Arch Dermatol 2012; 148: 26264. 135 Corte TJ, Wells AU, Nicholson AG, Hansell DM, Wort SJ. Pulmonary hypertension in sarcoidosis: a review. Respirology 2011; 16: 6977. 136 Burke RR, Rybicki BA, Rao DS. Calcium and vitamin D in sarcoidosis: how to assess and manage. Semin Respir Crit Care Med 2010; 31: 47484. 137 Shah L. Lung transplantation in sarcoidosis. Semin Respir Crit Care Med 2007; 28: 13440. 138 Collins J, Hartman MJ, Warner TF, et al. Frequency and CT ndings of recurrent disease after lung transplantation. Radiology 2001; 219: 50309.
www.thelancet.com Published online October 1, 2013 http://dx.doi.org/10.1016/S0140-6736(13)60680-7
13
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- ARDS New Definition - Berlin ConsensusDokument8 SeitenARDS New Definition - Berlin ConsensusAndreas IoannouNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Pulmonary Embolism - European Heart Journal 2012Dokument12 SeitenPulmonary Embolism - European Heart Journal 2012Andreas IoannouNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Asthma Lancet 2013Dokument13 SeitenAsthma Lancet 2013Andreas IoannouNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- COPD GOLD Guidelines 2012Dokument67 SeitenCOPD GOLD Guidelines 2012Andreas IoannouNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- GiftasupDokument50 SeitenGiftasupFizza SiddiquiNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- ARDS New Definition - Journal of Thoracic Diseases 2013Dokument9 SeitenARDS New Definition - Journal of Thoracic Diseases 2013Andreas IoannouNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Ats-Ers Iip Statement Ajrccm 2013Dokument16 SeitenAts-Ers Iip Statement Ajrccm 2013Andreas IoannouNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- ACG Guideline AcutePancreatitis September 2013Dokument16 SeitenACG Guideline AcutePancreatitis September 2013gorditomaloNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Histoplasmosis Guidelines 2007Dokument19 SeitenHistoplasmosis Guidelines 2007Andreas IoannouNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Defining Opportunistic Invasive Fungal Infections-ConssnsusDokument8 SeitenDefining Opportunistic Invasive Fungal Infections-ConssnsusAndreas IoannouNoch keine Bewertungen
- Sporotrichosis Guidelines 2007Dokument11 SeitenSporotrichosis Guidelines 2007Andreas Ioannou100% (2)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Guidelines For The Management of Intravascular Catheter Related InfectionsDokument24 SeitenGuidelines For The Management of Intravascular Catheter Related InfectionsAndreas IoannouNoch keine Bewertungen
- Invasive Fungal Infections - Diagnostic CriteriaDokument37 SeitenInvasive Fungal Infections - Diagnostic CriteriaAndreas IoannouNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Coccidioidomycosis GuidelinesDokument7 SeitenCoccidioidomycosis GuidelinesAndreas IoannouNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- IDSA Clinical Practice Guideline For Acute Bacterial Rhino Sinusitis in Children and AdultsDokument41 SeitenIDSA Clinical Practice Guideline For Acute Bacterial Rhino Sinusitis in Children and AdultsKarina ParedesNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Cryptococcus GuidelinesDokument9 SeitenCryptococcus GuidelinesAndreas IoannouNoch keine Bewertungen
- Blastomycosis Guidelines 2008Dokument12 SeitenBlastomycosis Guidelines 2008Andreas IoannouNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Aspergillosis IDSA GuidelinesDokument34 SeitenAspergillosis IDSA GuidelinesAndreas IoannouNoch keine Bewertungen
- 2012 Diabetic Foot Infections GuidelineDokument42 Seiten2012 Diabetic Foot Infections GuidelineFadilLoveMamaNoch keine Bewertungen
- Candidiasis Guidelines 2009Dokument33 SeitenCandidiasis Guidelines 2009Andreas IoannouNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Streptococcal PharyngitisDokument13 SeitenStreptococcal PharyngitisAndreas IoannouNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Skin and Soft Tissue InfectionsDokument34 SeitenSkin and Soft Tissue InfectionsAndreas IoannouNoch keine Bewertungen
- ATS GuidelinesDokument46 SeitenATS Guidelinesapi-3847280100% (1)
- MrsaDokument38 SeitenMrsahahmed78Noch keine Bewertungen
- Idsa 2010Dokument32 SeitenIdsa 2010Monica S. SuarezNoch keine Bewertungen
- FN 2011 IdsaDokument38 SeitenFN 2011 IdsaNuttawath UngwichanpunyaNoch keine Bewertungen
- Bacterial Meningitis PDFDokument18 SeitenBacterial Meningitis PDFZulaicha MumarridzohNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- EncephalitisDokument25 SeitenEncephalitisAndreas IoannouNoch keine Bewertungen
- Uncomplicated Urinary Tract InfectionsDokument18 SeitenUncomplicated Urinary Tract InfectionsAndreas IoannouNoch keine Bewertungen
- Applications of Blockchain Technology in Medicine and Healthcare: Challenges and Future PerspectivesDokument16 SeitenApplications of Blockchain Technology in Medicine and Healthcare: Challenges and Future PerspectivesGeorgianaNoch keine Bewertungen
- ICAI HS360 WithoutDuductibleDokument52 SeitenICAI HS360 WithoutDuductiblepadiNoch keine Bewertungen
- Wco Global Competency Model 2015-1Dokument73 SeitenWco Global Competency Model 2015-1CHIMA ONWUKA MONGNoch keine Bewertungen
- Psychiatry Research: Steve S. Lee, Avital E. Falk, Vincent P. AguirreDokument7 SeitenPsychiatry Research: Steve S. Lee, Avital E. Falk, Vincent P. AguirreludilozezanjeNoch keine Bewertungen
- Final Clinical Evaluation FormDokument4 SeitenFinal Clinical Evaluation Formapi-301424065Noch keine Bewertungen
- Nursing Minimum Data Set SystemDokument4 SeitenNursing Minimum Data Set SystemHenry Roque Tagalag100% (3)
- HematospermiaDokument7 SeitenHematospermiaDanielDimandNoch keine Bewertungen
- PAPER 1 Wildan CompleteDokument19 SeitenPAPER 1 Wildan CompleteWiha GamingNoch keine Bewertungen
- Medical ErrorsDokument13 SeitenMedical ErrorsSyeda Wardah NoorNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Focusing On Success: Teaching Students With Attention Deficit/Hyperactivity DisorderDokument192 SeitenFocusing On Success: Teaching Students With Attention Deficit/Hyperactivity Disorder2009tamerNoch keine Bewertungen
- AppendicitisDokument36 SeitenAppendicitisPetro MyronovNoch keine Bewertungen
- VARC RT99 Gejo'sAnnotationDokument66 SeitenVARC RT99 Gejo'sAnnotationyamansinghrajput1234Noch keine Bewertungen
- Internship Duties and Expectations 2022Dokument15 SeitenInternship Duties and Expectations 2022Luma MaxNoch keine Bewertungen
- Anxiety AmbossDokument8 SeitenAnxiety AmbossShrests SinhaNoch keine Bewertungen
- Personal Development ReviewerDokument8 SeitenPersonal Development Reviewercelina odon100% (5)
- Medical Nemesis Illich PDFDokument19 SeitenMedical Nemesis Illich PDFIamJmlingconNoch keine Bewertungen
- Clinical Case Scenarios For Generalised Anxiety Disorder For Use in Primary CareDokument23 SeitenClinical Case Scenarios For Generalised Anxiety Disorder For Use in Primary Carerofi modiNoch keine Bewertungen
- Case Studies Diagnostic LabDokument3 SeitenCase Studies Diagnostic LabAngad AnandNoch keine Bewertungen
- Aapc Whitepaper Cic Coc Ccs Comparison 2 1 IntDokument6 SeitenAapc Whitepaper Cic Coc Ccs Comparison 2 1 IntamruthkiranbabujiNoch keine Bewertungen
- 1047 82 Articles The Psychological Health of Shamans A ReevaluationDokument24 Seiten1047 82 Articles The Psychological Health of Shamans A ReevaluationAndrás SzabóNoch keine Bewertungen
- ICD-11 RevisionDokument22 SeitenICD-11 RevisiondfriadyNoch keine Bewertungen
- The Use of Cerebrolysin and Citicoline in AutismDokument10 SeitenThe Use of Cerebrolysin and Citicoline in AutismAamir Jalal Al-MosawiNoch keine Bewertungen
- Bio Medical InstrumentationDokument5 SeitenBio Medical InstrumentationpearllineNoch keine Bewertungen
- ScriptDokument13 SeitenScript張水蛙Noch keine Bewertungen
- Interview Reflection PaperDokument3 SeitenInterview Reflection Paperapi-250740396Noch keine Bewertungen
- OCD Treatment GuideDokument8 SeitenOCD Treatment GuideAditi KirtaneNoch keine Bewertungen
- ComplaintDokument37 SeitenComplaintJustin BaxleyNoch keine Bewertungen
- Reten Bulanan BPKK KKPB 2023Dokument11 SeitenReten Bulanan BPKK KKPB 2023Kanageswaran GaneshNoch keine Bewertungen
- CMEmodlueforconsulatants NBEBedside TeachingDokument176 SeitenCMEmodlueforconsulatants NBEBedside TeachingShiv Narayan KaliaNoch keine Bewertungen
- What Is AutismDokument4 SeitenWhat Is Autismidno1008Noch keine Bewertungen
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (24)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (80)