Beruflich Dokumente
Kultur Dokumente
5.4 Febrile Neutropenia
Hochgeladen von
Ester Elisabeth WoworCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
5.4 Febrile Neutropenia
Hochgeladen von
Ester Elisabeth WoworCopyright:
Verfügbare Formate
1
Nottingham Paediatric Guideline Management of Febrile Neutropaenic Children Introduction
The most commonly encountered cause of neutropenia in the paediatric population is marrow suppression secondary to chemotherapy. Oncology patients are immunosuppressed due to a combination of: Neutropaenia Splenic dysfunction T and B-cell dysfunction quantitative and qualitative dysfunction Destruction of normal mucosal barriers Alteration of normal body flora Neutropenia can also be seen in non-malignant conditions (see table). Decreased Marrow Production Congenital Kostmanns syndrome, Reticular dysgenesis, Fanconis anaemia Acquired Sepsis, Post-viral, Drug suppression, Cyclical neutropaenia, benign chronic neutropaenia, myelofibrosis Associated with phenotypically abnormal syndromes Schwachmanns, Chediak-Higashi, Cartilage hair hypoplasia, Dyskeratosis congenita Increased destruction of neutrophils Sepsis, endotoxaemia, Autoimmune antibodies, Neonatal isoimmune haemolytic disease Sequestration of neutrophils Immune complexes Viral, SLE, Sjorgens syndrome Hypersplenism Associated with immunodeficiency X-linked hypogammaglobulinaemia Selective immunoglobulin deficiency states Metabolic Problems Propionic isovaleric, Methylmalonic acidaemia, Hyperglycinaemia
As the immune system is not working properly, the normal inflammatory responses are muted. This may lead to infection without fever and also a greater tendency to dissemination of pathogens. The initial management of a child with febrile neutropenia is the same irrespective of the cause of the neutropenia. The microbiological aetiology of the fever in febrile neutropaenic patients is found in only 30 40 % of cases (1). Bacteraemia is present in 10 20% of febrile neutropaenic patients with neutrophils below 0.1 (2). The most likely infective pathogens are endogenous bacteria from skin and gut flora with gram-positive organisms (Streptococci, coagulase-negative staphylococci, Staphylococcus aureus, Enterococci) now more common agents than gram-negative organisms (Escherichia coli, Klebsiella spp,
2 Pseudomonas aeruginosa) (3). Fungal infections are always a diagnostic possibility in immunosuppressed patients. These usually occur in patients with prolonged neutropaenia and those who have had a course of broad-spectrum antibiotics. Prior to empirical antibiotic regimens mortality rates with infections were as high as 80%. Aggressive and early broad-spectrum antibiotic policies have decreased these rates to less than 3%. All febrile neutropaenic patients should initially be considered infected, however non-infectious causes that also need to be considered are: Malignant process Cytotoxics cytosine, bleomycin Blood products Allergic reactions ANY CHILD SHOWING SIGNS OF INFECTION SHOULD BE STARTED ON ANTIBIOTICS AND REVIEWED BY A SENIOR STAFF MEMBER REGARDLESS OF THEIR NEUTROPHIL COUNT
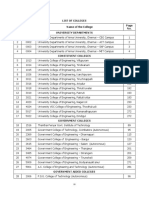
Normal range of neutrophils for children at different ages
AGE Birth 1 week 1 month 6 months 1 year 6 years 16 years TOTAL WBC Mean Range 18 9 30 12 5 21 10.8 5 19.5 11.9 6 17.5 11.4 6 17.5 8.5 5 14 7.8 4.5 13 NEUTROPHILS Mean Range 11 6 26 5.5 1.5 10 3.8 1.0 9 3.8 1.0 8.5 3.5 1.5 8.5 4.3 1.5 8 4.4 1.8 8 PERCENTAGE 61 45 35 32 31 51 57
Definitions
Neutropaenia: Absolute neutrophil count (ANC) less than 500/ml (< 0.5 x 109) ANC <1.0 and rapidly falling count after chemotherapy Fever: Temperature > 38.50 C on one occasion OR Temperature > 380C on 2 or more occasions recorded at least 1 hour apart
History on Admission
It is important to pay attention to the following: 1. Concomitant use of nephrotoxic drugs (e.g. Cisplatin, Ifosfamide, Vancomycin, Amphotericin, Amiloride). Gentamicin is not routinely used as a first line antibiotic if the patient is receiving ifosfamide or cisplatin as part of their chemotherapy regime unless the patient is shocked at presentation: 2. Relation of symptoms to central line flushing or usage Rigors associated within an hour of a line manipulation is strongly suggestive of a line infection 3. All patients that have received prolonged or intensive chemotherapy and repeated courses of antibiotics (e.g. patients with relapsed cancer) should be discussed with senior staff. More aggressive broad-spectrum antibiotic cover (e.g. Imipenem) may be required as first line therapy. 4. History of previous Gram Negative bacteria, e.g. gentamicin-resistant E Coli or Klebsiella, Enterobacter, Citrobacter, Morganella. Discuss these patients with Microbiology consider use of Imipenem or Meropenem. 5. History of other bacteria, e.g. history of MRSA, VRE or Clostridium difficile. Discuss patient with Microbiology.
Examination On Admission
All patients with a temperature need a detailed and full examination. Areas that need special attention are: 1. Mouth teeth, gums, pharynx. 2. ENT especially examining for tenderness over the sinuses and mastoid sites. Consider NPA for patients with coryzal symptoms 3. Respiratory respiratory rate and oxygen saturations and requirements must be recorded and documented. Hypoxaemia and normal auscultation may be associated with Pneumocystis pneumonia (PCP). 4. Cardiovascular Blood pressure must be documented. 5. Upper gastrointestinal painful swallowing may be suggestive of herpetic or candidal oesophagitis. 6. Abdominal tenderness right lower quadrant pain may suggest typhilitis (neutropaenic caecal inflammation), as well as appendicitis discuss with
4 senior member of staff. 7. Perineum symptoms of perianal discomfort or pain should always be asked about. If there are symptoms, the perineum should be inspected. 8. Skin lesions look for petechiae and purpura (evidence of thrombocytopaenia or DIC), consider Pseudomonas, herpetic, fungal aetiology 9. Central venous line (CVL) sites erythema, swelling, tenderness are suggestive of infection tracking along the line 10. Procedure sites e.g. Gastrostomy sites, lumbar puncture, posterior superior iliac crests Patients with following signs/symptoms need antibiotics to be commenced immediately AND URGENT assessment by a senior staff member regardless of neutrophil count: Shock Respiratory distress Coagulopathy More than one organ system involvement
Investigations on Admission
All patients with a temperature on admission need: 1. Temperature/fever confirmed 2. Full blood count differential to confirm neutropaenia 3. Biochemistry U+Es, LFTs 4. Blood cultures each sample must be labelled from where it is taken (e.g. Waste red lumen) a. 1 Waste culture from each lumen of the CVL (red and white) b. 1 Systemic culture from the CVL c. If no CVL 1 peripheral culture Investigations to perform if any clinical indications: 1. CXR if signs or symptoms of respiratory disease 2. Nasopharyngeal aspirate if signs or symptoms of respiratory disease or coryza 3. Stool culture if diarrhoea MC+S, virology, Clostridium difficle toxin (discuss C difficile with microbiology if patient under 5 years) 4. Coagulation screen if septic APPT, INR, fibrinogen 5. Urine culture clean catch for urine dipstix and urgent MC+S 5. Throat swab bacterial and viral cultures (note that require different media) 6. Skin lesions: a. Bacterial skin swab b. CVL site c. Gastrostomy site 7. If CVL in situ consider septic embolic phenomena ECHO CVL
Subsequent Investigations
1. FBC repeated at least twice weekly 2. Biochemistry as clinically indicated 3. At 48 hours and still febrile Discuss patient with Consultant a. Repeat examination, including perianal region b. Repeat blood cultures 4. At 96 hours and still febrile Discuss patient with Consultant a. Repeat full clinical examination, including perineum b. Repeat blood cultures c. Discuss performing echocardiogram of heart and line tip d. Discuss abdominal ultrasound for fungal lesions in liver and spleen e. Discuss performing x-rays of sinuses if old enough
General measures
If the duration of neutropaenia is predicted to be prolonged, preventative measures need to be instituted: Do not routinely give any medication via PR route Support haematological requirements appropriately Do not routinely use NSAIDs as an anti-pyretic Good mouth care and dental hygiene with antiseptic mouthwashes (chlorhexidine) Prophylaxis against pneumocystis (Co-trimoxazole) in patients expected to have prolonged myelosuppression (particularly lymphopenia) except those on high dose methotrexate regimes to continue throughout treatment Prophylaxis against fungal infections (Fluconazole) Avoidance of inhaling building/construction dust because of the risk of acquiring Aspergillus. G cSF is not recommended in the acute situation institution of GcSF therapy is a consultant decision.
Empirical Antibiotic Regime
AT ANY TIME DURING ADMISSION A CHILD APPPEARS SEPTIC, DISCUSS THE CONDITION WITH THE ONCOLOGY CONSULTANT ON-CALL. Decision to change antibiotics at any time will be a Consultant decision. First line antimicrobials: 1. IV Ceftazidime 50mg/kg every 8 hours (max 2 grams tds) 2. IV Gentamicin* (see below for exceptions) check inside cover of patients notes for advice regarding initial starting dose or commence dosing as below: a. < 12 years 2.5mg/kg every 8 hours b. > 12 years 1.5mg/kg every 8 hours (max 120 mg tds) c. Levels must be taken after the third gentamicin dose (pre + post) d. Adjust initial dose if patient requires gentamicin but has renal impairment and take earlier levels usually just give normal dose and take levels with second dose (must be taken). Wait for level before giving dose. 3. Oral fluconazole prophylaxis 3mg/kg once daily continue while neutropaenic * IV Flucloxacillin should be used instead of gentamicin in the following cases: Renal impairment discuss with senior staff member Renally toxic chemotherapy protocols, i.e. those containing cisplatin or ifosfamide Dose of flucloxacillin 25mg/kg every 6 hours (max 1 gram qds) If patient shows signs of septic shock contact a Senior member of staff as they may require gentamicin irrespective of renal impairment or treatment with renally toxic chemotherapy
Additional antibiotics 1. Consider adding glycopeptide as first line agent if: CVL related infection suspected Severe mucositis Previous MRSA isolate IV Teicoplanin 10mg/kg (max 400mg) every 12 hours for 3 doses, then once daily 2. If significant perianal inflammation or possible typhilitis (Neutropaenic colitis) add: IV Metronidazole 7.5mg/kg (max 500mg) every 8 hours Febrile at 48 hours Discuss possible second line antibiotics with Consultant: If patient is unwell add: IV Teicoplanin 10mg/kg (max 400mg) every 12 hours for 3 doses, then once daily
Febrile at 96 hours Discuss possible third line antibiotics with Consultant: Consider empirical treatment for possible fungal infection (Consultant decision only): IV Liposomal amphotericin (Ambisome) Dose 3mg/kg od (remember to prescribe test dose as per cBNF) Discuss change of antibiotic with Consultant on call: IV Imipenem* a. <12 years 15mg/kg qds (max 500mg qds) b. >12 years 12.5mg/kg qds (max1g qds) *Use Meropenem if evidence of renal impairment or history of CNS disorders
Discharge
Patients can be considered for discharge once 48 hour cultures are reported if ALL of the following criteria are met: 1. No signs of sepsis 2. Blood cultures negative at 48 hours 3. Temperature settling or afebrile 4. Consultant is aware of plan and agrees to discharge Discharge medications: 1. Fluconazole if still neutropaenic 3mg/kg/dose once daily Some children may be sent home on oral antibiotics. This is a Consultant decision only.
ASSESSMENT OF FEBRILE PATIENTS WITH NEUTROPHILS > 0.5
All patients should have the same history and examination and initial investigations instituted as per Febrile Neutropaenic Guideline. ADMISSION AND ANTIBIOTIC THERAPY SHOULD BE INSTITUTED IN ANY PATIENT WHO SHOWS SIGNS OF INFECTION REGARDLESS OF THEIR NEUTROPHIL COUNT (Coryza alone is not an indication for starting iv antibiotics) Identifiable source of infection treat with appropriate antibiotics, can discharge home if well No obvious source of infection careful observation. Antibiotics may not be necessary. If in doubt, contact Consultant.
FEBRILE NEUTROPAENIA MANAGEMENT ALGORITHM
8
IF ANY PATIENT SHOWS SIGNS OF INFECTION COMMENCE ANTIBIOTICS AND ARRANGE FOR URGENT SENIOR REVIEW Confirm neutropaenia and fever: Neutro&("ls 0 123 Te!&er#ture 4 56231 o$ce OR 4 561 ' 7+ 8 (our #&#rt
Relevant immediate investigations: Blood cultures s ste!"c #$d %#ste Ur"$e d"&st"' #$d culture T(ro#t s%#) )#cter"#l #$d *"r#l B"oc(e!"str UE+ ,FT+ CRP H#e!#tolo- DIC scree$ ". se&t"c
First line antibiotics: Ce.t#/"d"!e Ge$t#!"c"$ see )o' .or e'ce&t"o$s
Blood Culture : ;61
General measures: Sto& "!!u$osu&&ress"*e #-e$ts Fluco$#/ole %("le $eutro&#e$"c A$t"& ret"cs $o PR !ed"c#t"o$s Mout( c#re9 #$t"se&t"c !out( %#s(
Pos"t"*e
Ne-#t"*e Fe)r"le
Co$t"$ue #&&ro&r"#te #$t")"ot"cs d"scuss le$-t( %"t( !"cro)"olo-
Yes
Discuss with senior staff Re&e#t FBC Re&e#t )lood cultures
No
Discharge: WE,, CHI,D D<W Co$sult#$t Fluco$#/ole
Blood Culture : @A1 Ne-#t"*e #$d .e)r"le Ne-#t"*e #$d #.e)r"le 4 ;61
mportant 'oints to Consider: D"scuss #$t")"ot"c c(o"ce .or #ll rel#&sed &#t"e$ts %"t( se$"or st#.. Fluclo'#c"ll"$ .or &#t"e$ts rece"*"$".os.#!"de or c"s&l#t"$ CV, "$.ect"o$ sus&ected d"scuss #dd"t"o$ o. Gl co&e&t"de S"-$"."c#$t &er"#$#l "$.ect"o$ co$s"der #dd"t"o$ o. Metro$"d#/ole A,WAYS CHEC? INSIDE COVER OF GREEN FO,DER FOR SUGGESTED FIRST ,INE DRUG THERAPY OR ?NOWN RESISTANCE
I$*est"-#te .or s ste!"c .u$-#l "$.ect"o$
Sto& #$t")"ot"cs
D !C"!! # $% CON!"&$AN$ Re&e#t FBC #t le#st t%"ce %ee=l Re&e#t )lood culture C>R Poss")le9 A)do!"$#l ultr#sou$d (e&#t"c #$d s&le$"c !#sses ECHO c#rd"#c *#l*e #$d l"$e t(ro!)"
BIBLIOGRAPHY:
1. Pizzo PA. Dug Therapy: Management of fever in patients with cancer and Test dose t(e$ 5!-<=- OD treament-induced neutropenia. NEJM (1993); 328(18): 1323 - 1332 2. Schmipff SC. Empiric antibiotic therapy for granulocytopenic cancer patients. Am J Med (1986); 80 (suppl 5C): 13 20 3. Zinner SH. Changing epidemiology of infections in patients with neutropenia and cancer: emphasis on gram positive and resistant bacteria. Clin Infect Dis (1999); 29: 490 494 4. Alexander SW, Walsh TJ, Freifeld AG, et al. Infectious complications in Pediatric Cancer Patients. Section V. Principles and Practice of Pediatric Oncology 4th Edition (2002); p 1239 1285 5. Febrile neutropenia policy. Royal Childrens Hospital Melbourne, Australia 6. Pizzo P. Current concepts: Fever in Immunocompromised Patients. NEJM (1999); 341(12): 893 900 7. Garcia-Carbonero R, Paz-Ares L. Antibiotics and growth factors in the management of fever and neutropenia in cancer patients. Curr Opin Hem (2002); 9(3): 215 221 8. Ozer H, Armitage JO, Bennett CL, et al. 2000 update of recommendations for the use of haematopoietic colony-stimulating factors: Evidence-based, clinical practical guidelines. J Clin Oncol (2000); 18:3558 9. Link A, Bohme A, Cornely OA, et al. Antimicrobial therapy in unexplained fever in neutropenic patients. Ann Hematol (2003); 82 (suppl 2): S105 117 10. Estrada B. Treatment of Febrile Neutropenia: The Next Frontier. Infect Med (1999); 16(11): 699 700 11. Hughes WT, Armstrong D, Bodey GP, et al. 2002 Guidelines for the use of antimicrobial agents in neutropenic patients with cancer. IDSA Guidelines. Clin Infect Dis (2002): 34: 730 751 12. Alexander SW, Wade KC, Hibberd PL, et al. Evaluation of risk prediction criteria for episodes of febrile neutropenia in children with cancer. J Pediatr Hematol Oncol (2002); 24(1): 38 42 13. Levine JE, Boxer LA. Clinical applications of hematopoietic growth factors in pediatric oncology. Curr Opin Hem (2002); 9(3): 222 27 14. Auletta JJ, ORiordan MA, Nieder ML. Infections in children with cancer: A continued need for the comprehensive physical examination. J Pediatr Hematol Oncol (1999); 21(6): 501 08 15. Renoult E, Buteau C, Turgeon N, Moghrabi A, et al. Is routine chest radiography necessary for the initial evaluation of fever in neutropenia children with cancer? Pediatr Blood Cancer (2004) Sep; 43(3n): 224 - 8 16. Viscoli C, Castagnola E. Treatment of febrile neutropenia: what is new? Opin Infect Dis (2002); 15(4): 377 382 17. Mullen CA, Petropoulos D, Roberts WM, et al. Outpatient treatment of fever and neutropenia for low risk pediatric cancer patients. Cancer (1999); 86: 126 13
E!&"r"c#l A!)"so!e
Das könnte Ihnen auch gefallen
- Vancomycin Nephrology Preferred Dosing StrategyDokument2 SeitenVancomycin Nephrology Preferred Dosing StrategyEster Elisabeth WoworNoch keine Bewertungen
- COPD GuideDokument69 SeitenCOPD GuideEster Elisabeth WoworNoch keine Bewertungen
- Accepted Manuscript: Diabetes & Metabolic Syndrome: Clinical Research & ReviewsDokument30 SeitenAccepted Manuscript: Diabetes & Metabolic Syndrome: Clinical Research & ReviewsEster Elisabeth WoworNoch keine Bewertungen
- Ureteral Duplication and UreterocelesDokument8 SeitenUreteral Duplication and UreterocelesEster Elisabeth WoworNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- TNEA Participating College - Cut Out 2017Dokument18 SeitenTNEA Participating College - Cut Out 2017Ajith KumarNoch keine Bewertungen
- Green Campus Concept - A Broader View of A Sustainable CampusDokument14 SeitenGreen Campus Concept - A Broader View of A Sustainable CampusHari HaranNoch keine Bewertungen
- Final Test General English TM 2021Dokument2 SeitenFinal Test General English TM 2021Nenden FernandesNoch keine Bewertungen
- Curriculum Vitae: Personal InformationDokument2 SeitenCurriculum Vitae: Personal InformationtyasNoch keine Bewertungen
- Past Simple of BeDokument2 SeitenPast Simple of BeRoxana ClepeNoch keine Bewertungen
- 2's Complement Division C++ ProgramDokument11 Seiten2's Complement Division C++ ProgramAjitabh Gupta100% (2)
- A Practical Guide To Transfer Pricing Policy Design and ImplementationDokument11 SeitenA Practical Guide To Transfer Pricing Policy Design and ImplementationQiujun LiNoch keine Bewertungen
- Holophane Denver Elite Bollard - Spec Sheet - AUG2022Dokument3 SeitenHolophane Denver Elite Bollard - Spec Sheet - AUG2022anamarieNoch keine Bewertungen
- Filehost - CIA - Mind Control Techniques - (Ebook 197602 .TXT) (TEC@NZ)Dokument52 SeitenFilehost - CIA - Mind Control Techniques - (Ebook 197602 .TXT) (TEC@NZ)razvan_9100% (1)
- School Games Calendar Part-1Dokument5 SeitenSchool Games Calendar Part-1Ranadhir Singh100% (2)
- Kampfgruppe KerscherDokument6 SeitenKampfgruppe KerscherarkhoshNoch keine Bewertungen
- PsychometricsDokument4 SeitenPsychometricsCor Villanueva33% (3)
- The Neurology of Ageing: What Is NormalDokument11 SeitenThe Neurology of Ageing: What Is NormalEsther EunikeNoch keine Bewertungen
- Best Interior Architects in Kolkata PDF DownloadDokument1 SeiteBest Interior Architects in Kolkata PDF DownloadArsh KrishNoch keine Bewertungen
- IIT JEE Physics Preparation BooksDokument3 SeitenIIT JEE Physics Preparation Booksgaurav2011999Noch keine Bewertungen
- Queen of Hearts Rules - FinalDokument3 SeitenQueen of Hearts Rules - FinalAudrey ErwinNoch keine Bewertungen
- Contract of Lease (711) - AguilarDokument7 SeitenContract of Lease (711) - AguilarCoy Resurreccion Camarse100% (2)
- KV3000 Programming TutorialDokument42 SeitenKV3000 Programming TutorialanthonyNoch keine Bewertungen
- Digestive System LabsheetDokument4 SeitenDigestive System LabsheetKATHLEEN MAE HERMONoch keine Bewertungen
- Spice Processing UnitDokument3 SeitenSpice Processing UnitKSHETRIMAYUM MONIKA DEVINoch keine Bewertungen
- 6401 1 NewDokument18 Seiten6401 1 NewbeeshortNoch keine Bewertungen
- LEWANDOWSKI-olso 8.11.2015 OfficialDokument24 SeitenLEWANDOWSKI-olso 8.11.2015 Officialmorpheus23Noch keine Bewertungen
- CS 124/LINGUIST 180 From Languages To Information: Conversational AgentsDokument58 SeitenCS 124/LINGUIST 180 From Languages To Information: Conversational AgentsamanNoch keine Bewertungen
- Responsive Docs - CREW Versus Department of Justice (DOJ) : Regarding Investigation Records of Magliocchetti: 11/12/13 - Part 3Dokument172 SeitenResponsive Docs - CREW Versus Department of Justice (DOJ) : Regarding Investigation Records of Magliocchetti: 11/12/13 - Part 3CREWNoch keine Bewertungen
- Meditation For AddictionDokument2 SeitenMeditation For AddictionharryNoch keine Bewertungen
- CRM Final22222222222Dokument26 SeitenCRM Final22222222222Manraj SinghNoch keine Bewertungen
- AI in HealthDokument105 SeitenAI in HealthxenoachNoch keine Bewertungen
- Vickram Bahl & Anr. v. Siddhartha Bahl & Anr.: CS (OS) No. 78 of 2016 Casе AnalysisDokument17 SeitenVickram Bahl & Anr. v. Siddhartha Bahl & Anr.: CS (OS) No. 78 of 2016 Casе AnalysisShabriNoch keine Bewertungen
- 44) Year 4 Preposition of TimeDokument1 Seite44) Year 4 Preposition of TimeMUHAMMAD NAIM BIN RAMLI KPM-GuruNoch keine Bewertungen
- Lecture 4 PDFDokument9 SeitenLecture 4 PDFVarun SinghalNoch keine Bewertungen