Beruflich Dokumente
Kultur Dokumente
2
Hochgeladen von
najmulCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
2
Hochgeladen von
najmulCopyright:
Verfügbare Formate
Report and Opinion 2013;5(10)
http://www.sciencepub.net/report
CIN In Upper Egypt LEEP Excision Edessy M.S *, Aldarwish A *, Hala Naguib Hosni **, Galal M **, and Ali F ***. Professor*, lecturer*** of Obstetrics and Gynecology Al Azhar University and Ass professor of pathology Cairo university** Abstract: The present study was To evaluate the effectiveness and safety of the loop electrosurgical excision procedure (LEEP) in the treatment of cervical intraepithelial neoplasia (CIN), Women participating in a cervical screening study with histologically confirmed cervix were visually inspected with acetic acid, followed by coloposcopy and biopsy taken from abnormal areas, Cure was defined as no clinical or histologic evidence of CIN. Factors influencing cure rates were evaluated by 2 tests Out of the 1000 screened women 126 were found to be CIN positive (12.6%), 120 underwent LEEP. Six months follow up of 114 cases showed complete cure of 108 women (94.7%), LEEP Cure rates were 96.7%, 88.9%, and 80% for CINI, CINII and CINIII respectively. Single Pass and Multiple Pass cure rates were 97% and 90% respectively. Minor adverse effects were observed in 15 women and complications were seen in 5 women, LEEP was associated with minimal complications and good cure rates especially in those with CINI even in cases with large lesions. [Edessy M.S, Aldarwish A, Hala Naguib Hosni, Galal M, and Ali F. CIN In Upper Egypt LEEP Excision. Rep Opinion 2013;5(10):34-40]. (ISSN: 1553-9873). http://www.sciencepub.net/report. 6 Keywords: effectiveness; safety; loop electrosurgical excision procedure (LEEP); cervical intraepithelial neoplasia (CIN); histology; biopsy; lesion
1.Introduction Cervical cancer is the second most common cancer among women.(1). A womans risk of developing cervical cancer by age 65 years ranges from 0.8% in developed countries to 1.5% in developing countries(2) Some cervical intraepithelial neoplasia (CIN) lesions progress to cervical cancer. Most of them, particularly CIN 1 and 2 lesions, regress spontaneously without treatment (3). Current consensus guidelines recommend follow up with cytology for up to 2 years for some women with CIN (4). LEEP, the out-patient surgical procedure to evaluate and treat CIN, is widely used in cervical screening programs in high-income countries. Electrically activated tungsten wire loop electrodes are used to excise the entire transformation zone and provide tissue samples for histologic assessment of the disease and excised margins. The procedure's effectiveness, adverse effects, complications, and long-term morbidity have been widely reported in high-income settings [5-11], and it has been found to be an effective and simple outpatient treatment for women with CIN. Similar cure rates for CIN have been found with LEEP and alternative surgical treatments, such as laser ablation and conization [1]. However, the effectiveness, safety, and acceptability of LEEP have not been widely investigated in low-
resource settings [12], and it is unclear whether similar cure rates and safety profile can be achieved. The aim of the present study was to evaluate the effectiveness of LEEP following confirmation of CIN and any adverse effects or complications associated with the procedure.
2.Materials and Methods: In AlAzhar University Hospital- Assiut 1000 women aged 20-70 years old screened for CIN by pap. Smear. Women with positive pap smears results underwent coloposcopy (6x to 12x magnification) guided punch biopsies for further investigation. The biopsy specimens were processed and graded according to CIN nomenclature. Women diagnosed with CIN based on their punch biopsy results attended for LEEP. A detailed medical history was taken from each patient to exclude uncontrolled hypertension, diabetes mellitus, bleeding disorders, allergic reactions, exposure to diethylstilbestrol, pregnancy, and active genital tract infection. Each patient was counseled about the procedure and provided informed consent. LEEP was carried out as an outpatient procedure under local anesthetic and coloposcopic guidance. A speculum was used to expose the cervix, followed by application of 5% acetic acid and Lugol's iodine
34
Report and Opinion 2013;5(10)
http://www.sciencepub.net/report
solutions to assess the lesion. Local anesthesia was given by submucosal infiltration of 2% Xylocatine (AstraZeneca, London, UK). The appropriate loop electrode was used for excision of the transformation zone under colposcopic observation. The excision was initiated peripheral to the nonuptake area of iodine and single or multiple passes or 2-layer esxcisions were performed depending on the extent of the lesion. Bleeding was stopped by fulguration and application of ferric subsulfate solution. The excised specimens were sent for histopathological examination. As part of internal quality assurance, processing of specimens, laboratory manuals, and reporting procedures were periodically reviewed. After the procedure the women were advised not to use vaginal douches or tampons, nor to have sexual intercourse for 1 month after treatment, and to return to the clinic if they experienced any of the following within 4 weeks of the procedure: free for more than 2 days; severe lower abdominal pain; foul-smelling greenish-yellow discharge; bleeding with clots; or bleeding for more than 2 days. The women were informed that they may experience mild cramps and blood stained discharge in the following 2 weeks. A routine course of empirical antibiotics comprising doxycycline and metronidazole was prescribed, in addition to analgesics for pain. The women were advised to attend for follow-up 6 months later to rule out residual or recurrent cervical neoplasia. At follow-up the cervix was assessed with pap. semear colpscopy, and biopsy of abnormal areas observed colposcopically. Women with confirmed CIN underwent repeat LEEP, or simple hysterectomy depending on the lesion and the patient's preference. Women were considered disease free when no colposcopic features of CIN were observed or when no CIN lesions were established histologically if a biopsy sample was taken. The adverse effects of LEEP were defined as mild pain or mild cramps during or after treatment, vasomotor symptoms of fainting and flushing during or immediately after treatment, mild bleeding or
spotting immediately after treatment, foul smelling discharge, menorrhagia, and fever or chills after treatment; and these were used as the indicators of acceptability [13]. Anaphylactic reactions during LEEP, vaginal burns, severe pain, cramps or severe bleeding during or after LEEP that required further treatment, severe local cervical infections, unintended surgery within 4 weeks of LEEP, pelvic inflammatory disease, and functional cervical stenosis were assumed to be complications caused by the procedure and were used to assess its safety [14]. Cure rates, adverse effects, and complications were reported as frequency percentages. Cure rates categorized by age, menopausal status, extent of cervical lesion. Involvement of the endocervical canal, type of LEEP, margin involvement, and grade of CIN were compared using 2 tests.
3.Result analysis Total cure rate was 94.7% and that of CINI, CINII and CINIII were 96.7%, 88.9% and 80% respectively. The adverse effects observed were mild pain or mild cramps during or after treatment (3.3%), malodorous vaginal discharge following treatment (2.5%), mild bleeding (2.8%), menorrhagia (1.7%), and fever (1.7%). The complications recorded were PID (1.7%), severe bleeding that required suturing and blood transfusion (0.8%), severe pain (0.8%), and vaginal burns (0.8%). There were significant increase of cure rates with decrease of lesion area, decrease CIN grade, in non menopausal than menopausal women and in single than multiple pass LEEP (P<0.001, 0.001, 0.05 and 0.001 respectively. There were insignificant increase of cure rates wilth decrease of age and in cases without endocervical lesions.
35
Report and Opinion 2013;5(10)
http://www.sciencepub.net/report
Figure 1 show the schedule for management and follow-up after 6 months.
In Al-Azhar University Hospital (Assiut)1000 Women Aged 2070 Years old Screened for CIN
Colposcopic Guided Biopsy from Suspected Areas
874 (87.4%) no CIN
126 (12.6%) CIN
120 (95.2%) Treated by LEEP
2(1.6%) Treated by TAH
4(3.2%) Lost for treatment
114(95%) Followed 6 months
6(5%) Lost for follow-up
at 6
months
108(94.7%) cured 2 (1.8%) CINII No invasive cancer
3(2.6%) CINI
1(0.9%) CINIII
Fig. (2) Out of 1000 screened women 126 were found to be CIN positive. LEEP was allowed to 120 women, 114 were followed up for 6 months that resulted in cure rate of 94.7% and CINI, CINII and CINIII in2.6%, 1.8% and 0.9% of cases respectively.
36
Report and Opinion 2013;5(10)
http://www.sciencepub.net/report
Figure 2: Cervical Intraepithelial neoplasia (CIN). A) CIN grade I showing dysplastic squamous cells in the lower one-third of the epithelium . B) CIN grade II showing dysplastic squamous cells in the basal two-thirds of the epithelium. C) CIN grade III showing dysplastic squamous cells marked throughout the full thickness of the epithelium.
Figure 3: A) Cervical smear showing normal squamous cells. B) Cervical smear with CIN grade I showing dysplastic cells with mild degree of cellular and nuclear pleomorphism and enlargement. C) Cervical smear showing CIN grade II with dysplastic cells with moderate degree of cellular and nuclear pleomorhism and enlargement. D) Cervical smear showing CIN grade III showing dysplastic cells with marked cellular and nuclear pleomorphism and enlargement and increased nucleocytoplasmic ratio and scanty cytoplasm.
37
Report and Opinion 2013;5(10)
http://www.sciencepub.net/report
Table (1): Cure rates at 6 month follow-up according to characteristics of women at screening. Characteristics Cure rate (%) OR 95% CI P Age: (73/76) 96% 1.0 20 39 year < 0.742 (35/38)92% 0.9 (0.3-2.7) 40 70 year Area of lesion involved (%): < 25 (58/60)96.7% 1.0 < 0.001 25 50 (37/39)94.8% 0.2(0.1-0.6) > 50 (13/15)86% 0.1(0.0-0.4) endocervical canal involvement: No (96/99)96.9% 1.0 < 0.058 Yes (12/15)80% 0.5(0.2-1.0) Menopausal status: Not attained (90/94)95.7% 1.0 Attained (18/20)90% 0.3(0.1-1.0) < 0.050 Type of LEEP: Single Pass (68/70)97% 1.0 < 0.001 Multiple Pass (40/44)90% 0.4(0.2-0.9) Grade of CIN: CINI (88/91)96.7%) 1.0 < 0.001 CINII (16/18)88.8% 0.4(0.2-1.1) CINIII (4/5) 80% 0.2(0.1-0.5) 0.001 Table (2) Cure rates after 6 months. Punch LEEP biopsy Cases LEEP histology followed before cases LEEP CINI 96 91 CINII 19 18 CINIII 5 5 Total 120 114
Followup after 6 months Cured (%) 88(96.7) 16(88.9) 4(80) 108(94.7) CINI (%) 1(1.1) 1(5.6) 0(0) 2(1.8) CINII (%) 2(2.2) 1(5.6) 0(0.0) 3(2.6) CINIII (%) 0(0.0) 0(0.0) 1(20) 1(0.9) Invasive 0 0 0 0 Lost cases 5(5.2) 1(5.3) 0(0.0) 6(5.0)
4. Discussion: Cervical cancer is the second most common cancer among women. (1). A womans risk of developing cervical cancer by age 65 years ranges from 0.8% in developed countries to 1.5% in developing countries (2). Adequate treatment of CIN is vital for the success of cervical screening to prevent invasive cervical cancer. Cervical screening programs in lowand medium-resource countries have been less successful in reducing cervical cancer, partly because of the inadequate treatment coverage of women with CIN [15,16]; in addition, the lack of well-trained medical staff to perform colposcopy and treatment of the disease is a major resource constraint in many low-income countries [16]. LEEP has emerged as the most widely used CIN excision method in high-
income countries and results from well-conducted randomized clinical trials suggest that there is no difference in residual disease following LEEP, laser ablation, laser or cold knife conization [5]. From a practical perspective, LEEP is a superior excision treatment approach given the cheaper equipment and shorter duration of operative training. The present study showed that LEEP is an effective and safe procedure in a low-resource setting and also reflect the treatment outcomes reported by investigators in high-income countries. The discrepancy between colposcopically-directed biopsy and LEEP histology has been widely reported, and the agreement in the present study is in the higher range (46%-90%) of concordance reported in other studies [10, 17-18]. Clearance of small lesions by punch biopsy and the resulting inflammatory reaction
38
Report and Opinion 2013;5(10)
http://www.sciencepub.net/report
followed by application of ferric subsulfate solution may partly explain this discrepancy. Treating women with low-grade disease has been a policy priority in this setting because women are likely to receive only one treatment in their lifetime and there are considerable difficulties in ensuring follow-up. A possible limitation of the present study is that only colposcopy and directed biopsies some women with residual disease because the transformation zone may not have been fully visible after LEEP. However, this figure is likely to be small. The overall cure rate of 95% found in the present study is in the lower range of the 90%-95% cure rates reported in nonrandomized studies in the literature [5-11, 21-24], but comparison of treatment results from nonrandomized case series can be limited by biases arising from case treatment failures following LEEP in both randomized and nonrandomized case series are similar and, in most settings, LEEP has around a 90% cure rate for CIN. A cure rate of 95.3% was reported for 149 patients with CIN treatment by LEEP in a study from Lima, Peru [8]; and the variables that correlated with failure included the grade of lesion and operator's expertise, in the present study, adverse effects and complications following LEEP were observed in a negligible proportion of women and none were major or life threatening. The frequency of adverse effects and complications favorably compares with those reported from other studies in both high- and lowincome countries [5-11, 24, 25]. The findings of the present study and those from other low-income country settings [12, 24, 25] reinforce that LEEP can be performed effectively in these settings with a low frequency of complications and high rates of disease control. The widespread use of LEEP to treat CIN that requires excision should be an important integral component of screening programs in low-income countries. It is vital that adequate resources are available and doctors and nursing personnel are trained to perform LEEP as part of screening programs. References: 1. Globocan N, Ferlay J, Bray F, Pisani P, Parkin DM. Cancer Incidence, Mortality and Prevalence Worldwide.IARC CancerBase No. 5, version 2.0. IARCPress, Lyo. 2. Iarc, Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB. Cancer Incidence in Five Continents. IARC Scientific Publication No. 155, Lyon 2002; Vol. Volume VIII 3. Castle PE, Schiffman M, Wheeler CM, Solomon D. Evidence for frequent regression of cervical intraepithelial neoplasia-grade 2. Obstet Gynecol. 2009;113:1825.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
Wright TC, Jr, Massad LS, Dunton CJ, Spitzer M, Wilkinson EJ, Solomon D. 2006 consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ. J Low Genit Tract Dis. 2007;11:22339. Martin-Hirsch PL, Paraskevaidis E, Kitchener H. Surgery for cervical intraepithelial neoplasia. Cochrane Database Syst Rev 2002(2): CD18. Prendiville W, Cullimore J, Norman S. Large loop excision of the transformation zone (LLETZ). A new method of management for women with cervical intraepithelial neoplasia. Br J Obstet Gynaecol 1989; 96(9): 1054-60. Luesley DM, Cultimore J, Redman CW, Lawton FG, Emens JM, Rollason TP, et al. Loop diathermy excision of the cervical transformation zone in patients with abnormal cervical sinners. BMJ 1990; 300(6741): 1690-3. Bigrigg MA, Codling BW, Pearson P, Read MD, Swingler GR. Colposcopic diagnosis and treatment of cervical dysplasia at a single clinic visit. Experience of lowvoltage diathermy loop in 1000 ptients. Lancet 1990; 336 (8709); 229-31. Wright Jr TC, Gagnon S, Richart RM, Ferenczy A. Treatment of cervical intraepithelial neoplasia using the loop electrosurgical excision procedure. Obstet Gynecol 1992; 79(2): 173-8. Ferris GD, Hainer BL, Pfenninger JL, Zuber TJ, DeWitt DE, Line RL. Electrosurgical loop excision of the cervical transofmraiton zone: the experience of family physicians. J Fam Pract 1995; 41(4): 337-44. Whiteley PF, Olah KS. Treatment of cervical intraepithelial neoplasia: experience with the low-voltage diathermy loop. Am J Obstet Gynecol 1990; 162(5): 1272-7. Santos C, Galdos R, Alvarez M, Velarde C, Arrriga O, Dyer R, et al. One-session management of cervical intraepithelial neoplasia: a solution for developing countries. A prospective randomized trial of LEEP versus laser excisional conization. Gynecol Oncol 1996; 61(1): 11-5. Sellors J, Sankaranarayanan R. Colposcopy and treatment of cervical intraepithelial neoplasia: A beginner's manual. Lyon: IARC Press; 2003. Alliance for Cervical Cancer Prevention. Effectiveness, safey, and acceptability of cryotherapy: a systematic literature review.
39
Report and Opinion 2013;5(10)
http://www.sciencepub.net/report
15.
16.
17.
18.
19.
20.
Cervical Cancer Prevention Issues in Depth No. 1. January 2003. Lee KE, Koh CF, Watt WF. Comparison of the grade of CIN in colposcopically directed biopsies with that in out patient loop electrosurgical excision procedure (LEEP) specimens-a retrospective review. Sing Med 1999; 40(11): 694-6. Sankaranarayanan R, Buddukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bull World Health Organ 2001; 79(10): 954-62. Lee KE, Koh CF, Watt WF. Comparison of the grade of CIN in colposcopically directed biopsies with that in outpatient loop electrosurgical excision procedure (LEEP) specimens-a retrospective review. Sing Med 1999; 40(11): 694-6. Buxton EJ, Luesley DM, Shafi MI, Rollason M. Colposcopically directed punch biopsy: a potentially misleading investigation. Br J Obstet Gynaecol 1991; 98(12): 1273-6. Bonardi R, Cecchini S, Grazzini G, Clatto S. Loop electrosurgical excision procedure of the transformation zone and colposcopically directed punch biopsy in the diagnosis of cervical lesions. Obstet Gynecol 1992; 80(6): 1020-2. Howe DT, Vincentl AC. Is large loop excision of the transformation zone (LLETZ) more accurate than colposcopically directed
21.
22.
23.
24.
25.
punch biopsy in the diagnosis of cervical intraepithelial neoplasia? Br J Obstet Gynaecol 1991; 98(6): 588-91. sarian LO, Derchain SF, Andrade La, Tambascia J, Morais SS, Syrjanen KJ. HPV DNA test and Pap smear in detection of residual and recurrent disease following loop electrosurgical excision procedure of highgrade cervical intraepithelial neoplasia. Gynecol Oncol 2004; 94(1): 181-6. Brockmeyer AD, Wright JD, Gao F, Powell MA. Persistent and recurrent cervical dysplasia after loop electrosurgical excision procedure. Am J Obstet Gynecol 2005; 192(5): 1379-81. Kreimer AR, Guido RS, Solomon D, Schiffman M, Wacholder S, Jeronimo J, et al. Human papillomavirus testing following loop electrosurgical excision procedure identifies women at risk for posttreatment cervical intraepithelial neoplasia grade 2 or 3 disease. Cancer Epidemniol Biomark Prev 2006; 15(5): 908-14. Lee KE, Koh CF, Watt WF. Outpatient procedures for cervical dysplasia: a 3 years review of laser vaporization and LEEB. Med J Malys. 1999; 54(1): 47-51. Kletpeerahoiol c, Sriombon J, Khobjai A, Chandacham A. complication of loop electrosurgical excision procedure for cervical neoplasia: a prospective study. J Med Assoc. Thait 2006; 89(5): 583-7.
10/9/2013
40
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- TCGRX BullsEye Tablet SplitterDokument2 SeitenTCGRX BullsEye Tablet SplittermalucNoch keine Bewertungen
- Baby DedicationDokument3 SeitenBaby DedicationLouriel Nopal100% (3)
- 11Dokument4 Seiten11najmulNoch keine Bewertungen
- 16Dokument49 Seiten16najmulNoch keine Bewertungen
- 13Dokument5 Seiten13najmulNoch keine Bewertungen
- Comparison Between Visual Inspection of Cervix and Cytology Based Screening Procedures in BangladeshDokument5 SeitenComparison Between Visual Inspection of Cervix and Cytology Based Screening Procedures in BangladeshnajmulNoch keine Bewertungen
- 12Dokument8 Seiten12najmulNoch keine Bewertungen
- Comparison Between Visual Inspection of Cervix and Cytology Based Screening Procedures in BangladeshDokument5 SeitenComparison Between Visual Inspection of Cervix and Cytology Based Screening Procedures in BangladeshnajmulNoch keine Bewertungen
- 3Dokument7 Seiten3najmulNoch keine Bewertungen
- 7Dokument6 Seiten7najmulNoch keine Bewertungen
- 9Dokument7 Seiten9najmulNoch keine Bewertungen
- Case in Ovarian CystsDokument4 SeitenCase in Ovarian CystsAde Gustina SiahaanNoch keine Bewertungen
- Malignant Transformation in An Ovarian Mature Cystic Teratoma: A Case ReportDokument4 SeitenMalignant Transformation in An Ovarian Mature Cystic Teratoma: A Case ReportnajmulNoch keine Bewertungen
- CIMA Syllabus PDFDokument80 SeitenCIMA Syllabus PDFMuhammad AshrafNoch keine Bewertungen
- 8Dokument6 Seiten8najmulNoch keine Bewertungen
- Kanker OvariumDokument4 SeitenKanker OvariumRizna SaidNoch keine Bewertungen
- Umi Umd 3091Dokument120 SeitenUmi Umd 3091najmulNoch keine Bewertungen
- ProfileDokument3 SeitenProfilenajmulNoch keine Bewertungen
- SynopsisDokument15 SeitenSynopsisnajmulNoch keine Bewertungen
- Centre For Continuing Education (Cce)Dokument2 SeitenCentre For Continuing Education (Cce)najmulNoch keine Bewertungen
- Retailing, Clothing and Textiles Production in Australia: Sally WellerDokument18 SeitenRetailing, Clothing and Textiles Production in Australia: Sally WellerMallesh MalluNoch keine Bewertungen
- 4Dokument6 Seiten4najmulNoch keine Bewertungen
- 951 44 5752 8Dokument114 Seiten951 44 5752 8najmulNoch keine Bewertungen
- Kamau GraceDokument44 SeitenKamau GracenajmulNoch keine Bewertungen
- Dissertation Psychosocial Effects of Cervical CancerDokument69 SeitenDissertation Psychosocial Effects of Cervical CancernajmulNoch keine Bewertungen
- How To Start An Export/Import BusinessDokument18 SeitenHow To Start An Export/Import Businesscontactway1Noch keine Bewertungen
- 1113-19 CM University Brochure - FA3 - LRDokument20 Seiten1113-19 CM University Brochure - FA3 - LRnajmulNoch keine Bewertungen
- AttachmentDokument2 SeitenAttachmentnajmulNoch keine Bewertungen
- Nottingham MBA Scholarship Application Form 2014/15Dokument2 SeitenNottingham MBA Scholarship Application Form 2014/15najmulNoch keine Bewertungen
- Part 01 (A)Dokument12 SeitenPart 01 (A)najmulNoch keine Bewertungen
- StuDokument17 SeitenStunajmulNoch keine Bewertungen
- Dummy 13 Printable Jointed Figure Beta FilesDokument9 SeitenDummy 13 Printable Jointed Figure Beta FilesArturo GuzmanNoch keine Bewertungen
- SANDWICH Elisa (Procedure) - Immunology Virtual Lab I - Biotechnology and Biomedical Engineering - Amrita Vishwa Vidyapeetham Virtual LabDokument2 SeitenSANDWICH Elisa (Procedure) - Immunology Virtual Lab I - Biotechnology and Biomedical Engineering - Amrita Vishwa Vidyapeetham Virtual LabsantonuNoch keine Bewertungen
- The Philippine GovernmentDokument21 SeitenThe Philippine GovernmentChristel ChuchipNoch keine Bewertungen
- S4 Computer Sciences Exercises PDFDokument2 SeitenS4 Computer Sciences Exercises PDFHenriette Desanges UwayoNoch keine Bewertungen
- All Nobel Prizes in LiteratureDokument16 SeitenAll Nobel Prizes in LiteratureMohsin IftikharNoch keine Bewertungen
- NauseaDokument12 SeitenNauseakazakom100% (2)
- EDAG0007Dokument5 SeitenEDAG0007krunalNoch keine Bewertungen
- Kaun Banega Crorepati Computer C++ ProjectDokument20 SeitenKaun Banega Crorepati Computer C++ ProjectDhanya SudheerNoch keine Bewertungen
- Ims DB DCDokument90 SeitenIms DB DCpvnkraju100% (1)
- 1.classification of Reciprocating PumpsDokument8 Seiten1.classification of Reciprocating Pumpsgonri lynnNoch keine Bewertungen
- DC Generator - Construction, Working Principle, Types, and Applications PDFDokument1 SeiteDC Generator - Construction, Working Principle, Types, and Applications PDFGokul GokulNoch keine Bewertungen
- Banin Cawu 1: Panitia Ujian Perguruan Islam Mathali'Ul FalahDokument4 SeitenBanin Cawu 1: Panitia Ujian Perguruan Islam Mathali'Ul FalahKajen PatiNoch keine Bewertungen
- Unit 20: TroubleshootingDokument12 SeitenUnit 20: TroubleshootingDongjin LeeNoch keine Bewertungen
- Bullying Report - Ending The Torment: Tackling Bullying From The Schoolyard To CyberspaceDokument174 SeitenBullying Report - Ending The Torment: Tackling Bullying From The Schoolyard To CyberspaceAlexandre AndréNoch keine Bewertungen
- Collins Ks3 Science Homework Book 3Dokument5 SeitenCollins Ks3 Science Homework Book 3g3pz0n5h100% (1)
- The Ethics of Peacebuilding PDFDokument201 SeitenThe Ethics of Peacebuilding PDFTomas Kvedaras100% (2)
- Linux and The Unix PhilosophyDokument182 SeitenLinux and The Unix PhilosophyTran Nam100% (1)
- Very Hungry Caterpillar Clip CardsDokument5 SeitenVery Hungry Caterpillar Clip CardsARTGRAVETO ARTNoch keine Bewertungen
- VTB Datasheet PDFDokument24 SeitenVTB Datasheet PDFNikola DulgiarovNoch keine Bewertungen
- Cella Di Carico Sartorius MP77 eDokument3 SeitenCella Di Carico Sartorius MP77 eNCNoch keine Bewertungen
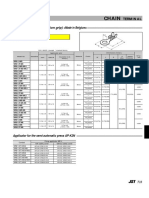
- Chain: SRB Series (With Insulation Grip)Dokument1 SeiteChain: SRB Series (With Insulation Grip)shankarNoch keine Bewertungen
- Chrysler CDS System - Bulletin2Dokument6 SeitenChrysler CDS System - Bulletin2Martin Boiani100% (1)
- BLG311 Cell Biology: Course Outline (Fall 2020)Dokument11 SeitenBLG311 Cell Biology: Course Outline (Fall 2020)Emilija BjelajacNoch keine Bewertungen
- 1 AlarmvalveDokument9 Seiten1 AlarmvalveAnandNoch keine Bewertungen
- Or HandoutDokument190 SeitenOr Handoutyared haftu67% (6)
- GNSS COrs SystemDokument20 SeitenGNSS COrs SystemKostPutriMalangNoch keine Bewertungen
- All About TarlacDokument12 SeitenAll About TarlacAnonymous uLb5vOjXNoch keine Bewertungen
- Pipe Freezing StudyDokument8 SeitenPipe Freezing StudymirekwaznyNoch keine Bewertungen