Beruflich Dokumente
Kultur Dokumente
DEPRESI Pada Orang Turki
Hochgeladen von
Yuriko AndreCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
DEPRESI Pada Orang Turki
Hochgeladen von
Yuriko AndreCopyright:
Verfügbare Formate
Cult Med Psychiatry (2009) 33:412420 DOI 10.
1007/s11013-009-9139-1 ORIGINAL PAPER
Symptoms of Turkish Patients with Depression in Ankara and Berlin
Derya Iren Akbiyik Vildan Sumbuloglu Oguz Erkan Berksun Vesile Senturk Stefan Priebe
Published online: 11 June 2009 Springer Science+Business Media, LLC 2009
Abstract Numerous studies have investigated the potential impact of migration on psychiatric morbidity levels. Relatively little research has studied how the symptom proles of patients with similar disorders and similar backgrounds are linked to the culture in which they live. Such research requires comparisons of immigrant patient samples with samples of patient who remain in their country of origin. In this study we compared symptoms in Turkish patients with depression living in Ankara, Turkey, and Berlin, Germany. To understand symptoms of patients with depression, not only the culture of origin but also the cultural context in which patients have been living needs to be considered as an important factor. The new culture can be associated with distinct, and not necessarily more serious, symptom proles. Keywords Depression Immigrant mental health Turkish mental health Germany Symptoms
D. I. Akbiyik (&) Department of Psychiatry, Ankara Oncology Research and Training Hospital, Bulbulderesi Cad. 50/5, 06660 Ankara, Turkey e-mail: deryaakbiyik@yahoo.com V. Sumbuloglu Biostatistics Department, Zonguldak Karaelmas University, 67600 Kozlu-Zonguldak, Turkey O. E. Berksun V. Senturk Department of Psychiatry, Ankara University, Cebeci, Ankara, Turkey S. Priebe Unit for Social & Community Psychiatry, Newham Centre for Mental Health, Queen Mary University of London, London E13 8SP, UK
123
Cult Med Psychiatry (2009) 33:412420
413
Introduction: Migration and Mental Illness Migration is increasing throughout the world. As a consequence, mental health services everywhere must face the challenge of providing appropriate and effective care for immigrant populations who differ culturally from the host country (e.g., Gaines 1999; Nathan 1994; Vega et al. 2001; Westermeyer 1989). In general, mental illness is seen as an increasing burden on the worlds population, especially in low-income countries where economic and political issues are often prominent in their genesis (Desjarlais et al. 1995). Numerous studies have investigated morbidity levels in immigrant populations (e.g., LeTouze and Watters 2003; Watters 2003). Rates of mental disorders among immigrants are often higher than in the general population of the host country. Yet this is not consistently so, and does not apply to all immigrant populations. While much literature focuses on rates of disorders, less research has studied distinct symptom proles in immigrant populations. However, to understand the symptomatology of immigrant patients, clinicians should be in a position to consider what symptom patterns may be specic to the context in which the patients have been living (Akbiyik et al. 1999). This focus may lead to some novel ideas about afiction in immigrant contexts. It is widely accepted that the cultural background of a patient needs to be considered to understand the symptomatology, yet the cultural context for immigrant populations is different from that of the culture of origin. Immigrants experience a complex combination of factors that stem from the culture of origin, the culture of the host country and the interplay of those two cultures in a process of adaptation. Research to identify the specic cultural factors affecting the symptomatology of immigrant groups should therefore compare symptoms of immigrants with those of similar patients in the country of origin. Ideally, such comparisons should use the same methods for the assessment of the two groups so that differences found are not confounded by methodological inconsistencies. We attempt this effort by focusing on a major immigrant population in Europe, the Turkish people who moved to Germany, originally as so-called gastarbeiter or guest workers. The major movement began in the 1960s and has continued into the new millennium (Council of Europe 2003). Currently, more than 2.75 million Turkish people live in Germany. More than 200,000 live in Berlin alone, making it the fourth largest Turkish city. These Turkish immigrants did not necessarily aim at full assimilation in Germany, and many planned to return to Turkey sooner or later. Indeed, given the cultural ideology of identity in place in Germany, full assimilation would have been impossible (Kostoryano 2002; Yurdakul and Bodemann 2007). Given the exclusionary forces at work, Turkish people often settled in areas with high concentrations of immigrants with a similar background, for example, the Kreuzberg district in Berlin, and lived in quasi-Turkish communities replete with Turkish associations. This residential pattern kept somewhat intact many of the features of Turkish life and community as well as the use of the Turkish language. However, despite the fact that a large population of Turkish immigrants lives in Germanyand even though Turkish patients are a
123
414
Cult Med Psychiatry (2009) 33:412420
widely investigated grouplittle research has been done on immigrants in Germany (Claassen et al. 2005). In this brief article, we report our clinical ndings on Turkish outpatients with depressive disorders. We used a baseline chronology for habitation, studying Turkish people who lived in Berlin and Ankara for a minimum of 10 years in each site. All individuals in this study were recruited and assessed in their native language and by the same Turkish-speaking interviewer to reduce the risk of variation. The assessment instruments employed included the Mini International Neuropsychiatric Interview (MINI), the Symptom Check List-90 Revised (SCL-90R), and the Beck Depression Inventory (BDI). Scores of the two groups of patients were then compared. We found that patients in Ankara (n = 52) and Berlin (n = 53) showed signicant differences in distinct symptom levels. It was interesting to note that patients in Berlin had more depressive symptoms while patients in Ankara had higher levels of obsessive-compulsive symptoms, anxiety, interpersonal sensitivity, hostility, phobic anxiety, and paranoid ideation as selfrated on the SCL-90-R. The present study aimed to establish and compare symptoms in Turkish patients with major depression or dysthymic disorders who have been living in the capital cities of Turkey and Germany, i.e., in Ankara and Berlin, for at least 10 years. Turkish patients in Berlin immigrated as adults. The same native Turkish researcher interviewed all patients in both cities, to minimize biases due to language barriers and/or different interview and assessment styles. This was a cross-sectional exploratory study. Inclusion criteria for all patients were (a) being of Turkish origin, (b) being diagnosed with major depression or dysthymic disorder by a psychiatrist within the previous 2 weeks, and (c) residing in Ankara or Berlin as an adult for a minimum of 10 years (resulting in a minimum age of 28 years). Patients in Berlin had to have immigrated to Berlin at or after the age of 18 years, and patients in Ankara had to have no history of internal migration. Patients in Ankara were recruited from the outpatient department of the psychiatric clinic at Ankara University. Patients in Berlin were recruited from two ofce-based practices of Turkish psychiatrists in central districts of Berlin. The patients were referred to the study by Turkish-speaking clinicians. The research interviewer, who was not involved in treatment in any of the settings, checked the inclusion criteria and administered a range of instruments. They included the MINI to establish the psychiatric diagnosis (Sheehan et al. 1997; Engeler 2004), the BDI for a self-rating of symptom levels of depression (Beck et al. 1974, 1988; Beck and Steer 1984; Hisli 1989) and the SCL-90-R for a self-rating of other psychological symptoms (Dag 1991; Derogatis 1977). All of the instruments have been validated previously in Turkish populations (Dag 1991; Engeler 2004; Hisli 1989). Referrals were based on clinical diagnoses of major depression according to the International Classication of Diseases (ICD)-10. The research interviewer conrmed the diagnosis using the MINI. All interviews were conducted in Turkish. All patients gave written informed consent, and this study received approval from the Ethics Research Community at Humboldt University at Berlin.
123
Cult Med Psychiatry (2009) 33:412420
415
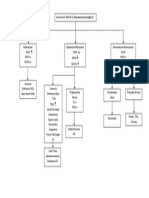
Statistical Analysis The study aimed to recruit a minimum of 50 patients in each group. This would provide limited statistical power to detect small and medium-sized differences between the two groups. Yet it was seen as appropriate for this exploratory study, as we were interested in identifying substantial differences. We summarized all data using descriptive statistics. Groups were compared using Chi-square and t-tests. (We did not compute multivariate tests in this analysis because of the risk that results based on the small sample size might not be sufciently robust.) The Sample Seventy-three patients in Ankara and 66 patients in Berlin were regarded as eligible by the clinicians and referred to the study. Figure 1 shows the subsequent selection process, resulting in a nal sample size of 52 patients in Ankara and 53 in Berlin. Mean ages were 49.4 8.4 years in the Berlin group and 44.7 9.2 years in the Ankara group. Demographic information on the groups is reported in Table 1. The diagnoses were First Major Depressive Episode (Ankara, 29; Berlin, 18), Recurrent Major Depressive Episode (Ankara, 14; Berlin, 23) and Dysthymic Disorder (Ankara, 9; Berlin, 12). None of the patients presented with current psychotic symptoms. Patients in both groups showed different degrees of anxiety symptoms, but they did not meet the full criteria for a comorbid anxiety disorder. Patients in Ankara had signicantly lower BDI scores (mean SD = 22.6 9.7 vs. 29.6 6.6; t = 4.233, p \ 0.001) but a higher Global Severity Index based on the SCL-90-R (mean SD = 52.0 18.4 vs. 43.4 11.5; z = -2.285, p = 0.002). Scores on the SCL-90-R subscales are reported in Table 2. Scores on the BDI and the subscale depression of the SCL-90-R were signicantly higher in Berlin. The Global Severity Index on the SCL-R-90 as well as subscale scores on obsessive compulsive symptoms, interpersonal sensitivity,
Fig. 1 Recruitment and selection of patients in Ankara and Berlin
123
416
Cult Med Psychiatry (2009) 33:412420
Table 1 Demographic and social characteristics of patients living in Berlin and Ankara: mean standard deviation or n (%) Berlin (n = 53) Sex Male Female Marital status Married Divorced Widowed With a partner Single Duration of marriage (years) Years in the city Total work years Household income (subjective) Very high High Moderate Low No income Number in household Note: ND not determined
a b c
Ankara (n = 52)
Total (n = 105)
p-value
19 (35) 34 (64) 43 (81) 7 (13) 2 (3) 1 (1) 23.9 10.5 26.8 7.8 20.0 10.0 3 (5) 6 (11) 14 (26) 29 (54) 1 (1) 2.8 1.4
14 (26) 38 (73) 41 (78) 4 (7) 3 (5) 1 (1) 3 (5) 20.4 10.8 30.3 10.7 12.3 12.5 1 (1) 43 (82) 7 (13) 1 (1) 3.4 1.2
33 (31) 72 (68) 84 (80) 11 (10) 5 (4) 1 (1) 4 (3) 22.2 10.7 28.5 10.5 16.2 11.1 3 (2) 7 (6) 57 (54) 36 (34) 2 (1) ND
0.325a
0.612b
0.046c 0.246c 0.001c \0.001b
0.006c
Chi-square test Fishers exact test (Monte Carlo) MannWhitney U
Table 2 SCL-90-R subscale scores of patients in Ankara and Berlin: mean standard deviation Symptom group Somatization Obsessive-compulsive Interpersonal sensitivity Depression Anxiety Hostility Phobic anxiety Paranoid ideation Psychoticism
a
Ankara 29.9 9.9 24.1 8.0 21.3 7.5 35.8 11.5 23.0 9.2 13.0 5.2 14.1 5.3 14.5 5.8 18.1 7.4
Berlin 30.5 9.2 16.6 5.4 16.5 4.2 39.6 7.5 17.9 5.3 8.6 2.8 8.9 2.7 8.4 2.6 16.7 4.1
t 0.304 -4.552 -4.073 1.994 -3.493 -5.321 -4.787 -6.907 -1.148
p-valuea 0.762 \0.001 \0.001 0.048 0.001 \0.001 \0.001 \0.001 0.251
Students t-test
anxiety, hostility, phobic anxiety and paranoid ideation were all signicantly higher in patients in Ankara. Only the SCL-90-R subscales somatization and psychoticism did not show any signicant difference between the two groups.
123
Cult Med Psychiatry (2009) 33:412420
417
Discussion Our study yielded clear and statistically signicant ndings. Turkish patients with major depression living in Berlin have higher levels of depressive symptoms but lower scores on obsessive-compulsive symptoms, interpersonal sensitivity, anxiety, hostility, phobic anxiety and paranoid ideation. Thus, we did not nd one of the two groups to have consistently higher levels of symptoms across all symptom scales, but distinct proles, with each group having signicantly higher scores for different types of symptoms. This is most interesting given the cultural system of identity in Germany. Our ndings suggest that looking at symptom proles comparatively may have important results for understanding immigrant experience that may go against conventional wisdom. The study has several methodological strengths. All patients met the same inclusion criteria and had a diagnosis of major depression or dysthymia. All patients had been living in Ankara or Berlin, respectively, for a minimum of 10 years, so that none was subjected to recent experiences of migration within or across countries or to possibly related adjustment problems. All had at least 10 years experience in a consistent cultural environment. In general, the Turkish immigrants in Berlin had originally not intended to stay in Berlin forever. Rather, they had plans, realistic or not, to return to Turkey at some point. Most of the Turkish patients in Berlin in this study did not have a very good command of German, and language was a serious barrier in all communications with German institutions, including health services. Because of this, all patients were interviewed by the same trained researcher in the native Turkish language so that there was neither interviewer bias due to different cultural backgrounds nor a language barrier. The initial diagnosis for including patients in the study had also been made by a native Turkish-speaking physician, to avoid possible misdiagnosis because of language problems. The study also has some limitations, which should be considered in the interpretation of the ndings. We assessed clinical samples, which do not allow conclusions on representative samples in the community. Since the health-care systems in Germany and Turkey differ, we could not use an identical recruitment processes and had to approach patients at services with slightly different functions. In this exploratory study we did not adjust the level of statistical signicance to multiple testing. Yet the level of statistical signicance for all the identied differencesother than the one on the SCL-90-R subscale depressionwere so high that a Bonferroni adjustment would still have left differences as statistically signicant. Most of the differences between the two groups are equivalent to a large effect size. Finally, because of the limited sample size we did not control for the inuence of potential confounders. The study was cross-sectional so that conclusions on causal relationships cannot be drawn. Different factors may have contributed to the different symptom proles. They include the selection processes of people who decided to migrate to Germany, experiences in the host culture over more than 10 years, selective pathways into specialized psychiatric care and various interactions with healthcare professionals at services in Germany. Whatever the exact explanation, the ndings demonstrate that the cultural context in which patients have been living
123
418
Cult Med Psychiatry (2009) 33:412420
is associated with specic symptom proles andsurprisingly, given the host country in this instancewith reduced symptoms of anxiety, hostility, phobic anxiety and paranoid ideation. These results are not consistent with those of a longitudinal study by Haefner (1980), which found that guest-workers from Turkey arriving in Germany initially suffered from depression and increasingly developed psychosomatic symptoms over the next 2 years. Those results suggested a decreasing focus on depressive symptoms after migration to Germany, while we found higher levels of depression in Turkish patients in Berlin compared to Ankara. Also, Haefner identied a tendency toward somatization, while in our study somatization was one of only two subscales with no statistically signicant differences between the two groups. However, the studies are difcult to compare. They were done at different times and in different settings, and Haefner studied younger people and psychosocial processes within the rst 2 years after migration, while we investigated patients more than 10 years after they had immigrated. One might speculate as to whether the health-care system in Germany is more responsive to the presentation of depressive symptoms, so that either patients with more depressive symptoms are more likely to receive treatment and stay in services or patients tend to focus on the presentation of depressive symptoms over time. In a similar vein, general aspects of the culture or specic responsiveness of health professionals might facilitate or reinforce the presentation of a wider range of symptoms including anxiety, but not specically depression, in Ankara. It is noteworthy that symptoms of hostility and paranoid ideation were higher in Ankara than in the patients in Berlin, although the latter were living in a foreign country where they commonly did not comprehend the language and did not enjoy the full entitlements of German nationals. However, these differences were identied only in clinical samples. There are no data suggesting that similar differences are to be found in representative community samples. Future research may explore whether the symptom proles of immigrant groups become more similar to those of indigenous patients in the host country or remain qualitatively different from those of both Turkish patients in Turkey and German patients in Germany. In addition to assessing immigrant patients in the country of origin and the host country, such research will require studying indigenous patients in the host country. A major challenge for such studies is the methodological consistency of assessments across groups, that is, how to guarantee consistency when different languages have to be used. What the ndings of this study clearly show is that specic symptom proles found in immigrant populations cannot necessarily be attributed to common symptom patterns in the culture of origin. Additionally, expected symptoms may not appear in an immigrant group, suggesting psychocultural adaptation or protective psychocultural processes. The current cultural context needs to be considered to understand patients presenting symptomatology in context, that is, in the host country. This is a challenge to clinicians and also to researchers, as in the future both will have to deal increasingly with immigrant populations with mental health disorders (Priebe et al. 2004).
123
Cult Med Psychiatry (2009) 33:412420
419
References
Akbiyik, I.D., E.G. Mendel, M.E. Onder, and C. Cording 1999 The Effects of Being Immigrant on Depression and Somatic Symptoms in Turkish Immigrants in Germany. Crisis Journal 7: 2529 (in Turkish). Beck, A.T., and R.A. Steer 1984 Internal Consistencies of the Original and Revised Beck Depression Inventory. Journal of Clinical Psychology 40: 13651367. Beck, A.T., W.Y. Rial, and K. Rickets 1974 Short Form of Depression Inventory: Cross Validation. Psychological Report 34: 11841186. Beck, A.T., R.A. Steer, and M.G. Garbin 1988 Psychometric Properties of the Beck Depression Inventory; 25 Years of Evaluation. Clinical Psychology Report 8: 77100. Claassen, D., M. Ascoli, T. Behre, and S. Priebe 2005 Research on Mental Disorders and Their Care in Immigrant Populations: A Review of Publications from Germany, Italy and the UK. European Psychiatry 20: 540549. Council of Europe 2003 Demographic Year Book Glossary. Available at: http://www.coe.int/t/e/social_cohesion/popu lation/demographic_year_book/-2003_Edition/Default.asp#TopOfPage. Accessed November 17, 2007. Dag, I. 1991 Validity and Reliability of Symptom Check List-90 Revised (SCL-90R) for University Students. Turkish Journal of Psychiatry 2: 512 (in Turkish). Derogatis, L.R. 1977 SCL-90: Administration, Scoring, and Procedure Manual-I. Baltimore, MD: Johns Hopkins University Press. Desjarlais, Robert, Leon Esenberg, Byron Good, and Arthur Kleinman, eds. 1995 World Mental Health: Problems and Priorities in Low-Income Countries. New York: Oxford University Press. Engeler, A. 2004 M.I.N.I. Instruments, Turkish Adaptation. Istanbul: GlaxoSmithKline (in Turkish). Gaines, A.D. 1999 Culture, Aging and Mental Health. In Serving Minority Elders in the 21st Century. May Wykle and Amasa Ford, eds., pp. 180199. New York: Springer. Haefner, H. 1980 Psychiatric Morbidity among Immigrant Workers in Mannheim. Nervenarzt 51: 672683 (in German). Hisli, N. 1989 The Validity and Reliability of Beck Depression Scale for University Students. Turkish Journal of Psychology 7: 313 (in Turkish). Kostoryano, Riva 2002 Negotiating Identities: States and the Immigrants in France and Germany. Princeton, NJ: Princeton University Press. LeTouze, D., and C. Watters 2003 Good Practices in Mental Health and Social Care Provision for Refugees and Asylum Seekers. Report on the United Kingdom. In Final Report on Good Practices in Mental Health and Social Care Provision for Asylum Seekers and Refugees. C. Watters and D. Ingleby, eds. Brusselles, Belgium: European Commission (European Refugee Fund). Nathan, T. ditions Odile Jacob. 1994 LInuence Qui Guerit. Paris: E Priebe, S., T. Behre, V. Iannibelli, and D. Claassen 2004 Migration and Mental Health Care. In Proceedings of the 14th International Conference of Psychosomatic Obstetrics and Gynaecology, Edinburgh, Scotland, May 1619. I.C. Allen, B. Alder, and M. Pawson, eds., pp. 179186. Bologna, Italy: Medimond International Proceedings. Sheehan, D.V., Y. Lecrubier, S.K. Harnett, J. Janavs, E. Weiller, L.I. Bonara, A. Keskiner, J. Schinka, E. Knapp, M.F. Sheehan, and G.C. Dunbar
123
420
Cult Med Psychiatry (2009) 33:412420
1997 Reliability and Validity of the MINI International Neuropsychiatric Interview (MINI): According to the SCID-P. European Psychiatry 12: 232241. Vega, W.A., K. Bohdan, and S. Aguilar-Gaxiola 2001 Help Seeking for Mental Health Problems among Mexican Americans. Journal of Immigrant Health 3(2): 133140. Watters, M. 2003 The 12 Steps to Rehab Health Care. Revolution 4(5): 1017. Westermeyer, J. 1989 Psychiatric Care of Migrants: A Clinical Guide. Washington, DC: American Psychiatric Press. Yurdakul, Gokce, and Y. Michal Bodemann 2007 Citizenship and the Immigrant Incorporation: Comparative Perspectives on North America and Western Europe. New York: Palgrave/Macmillan.
123
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Das könnte Ihnen auch gefallen
- BCJ582 Final Exam 100% Correct AnswersDokument49 SeitenBCJ582 Final Exam 100% Correct AnswersHomeworkhelpbylance0% (3)
- Schizophrenia PaperDokument21 SeitenSchizophrenia PaperBagoes Ario BimoNoch keine Bewertungen
- One Blue Child: Asthma, Responsibility, and the Politics of Global HealthVon EverandOne Blue Child: Asthma, Responsibility, and the Politics of Global HealthNoch keine Bewertungen
- Phobia ListsDokument5 SeitenPhobia Listskatts4uNoch keine Bewertungen
- Prevalence of Migraine, Probable Migraine and Tension-Type Headache in The Croatian PopulationDokument8 SeitenPrevalence of Migraine, Probable Migraine and Tension-Type Headache in The Croatian PopulationmarcelliawharsonoNoch keine Bewertungen
- The Pathoplastic Effect of Culture On Psychotic Symptoms in SchizophreniaDokument7 SeitenThe Pathoplastic Effect of Culture On Psychotic Symptoms in SchizophreniaOftee Major GeneralNoch keine Bewertungen
- Epidemiology of SchizophreniaDokument13 SeitenEpidemiology of SchizophreniaSri AgustinaNoch keine Bewertungen
- The Association Between Age and Depression in The General Population: A Multivariate ExaminationDokument10 SeitenThe Association Between Age and Depression in The General Population: A Multivariate ExaminationNadiraNoch keine Bewertungen
- PerspectivesinPsychiatricCare Mentalpages 1Dokument2 SeitenPerspectivesinPsychiatricCare Mentalpages 1Ngọc PhanNoch keine Bewertungen
- CG in A Representativ PopulationDokument6 SeitenCG in A Representativ PopulationAdriana Turdean VesaNoch keine Bewertungen
- 2001 Kyol Goeu in CambodiaDokument6 Seiten2001 Kyol Goeu in CambodiaLuana SouzaNoch keine Bewertungen
- The Psychological Effects of MigrationDokument15 SeitenThe Psychological Effects of MigrationSe-lei Oi100% (1)
- ENg 101Dokument8 SeitenENg 101BiniamNoch keine Bewertungen
- Swinkels PscychopathologieDokument16 SeitenSwinkels PscychopathologiesezalwickNoch keine Bewertungen
- Suicide Attempts in First-Episode PsychosisDokument6 SeitenSuicide Attempts in First-Episode PsychosisAdam García BuenoNoch keine Bewertungen
- Keski Rahkonenetal2008Epidemiologyofeatingdisorders AnupdateDokument12 SeitenKeski Rahkonenetal2008Epidemiologyofeatingdisorders AnupdateHelena OliveiraNoch keine Bewertungen
- Cultural Distress Complex PTSDDokument14 SeitenCultural Distress Complex PTSDCesia Constanza Leiva GonzalezNoch keine Bewertungen
- Omics Publishing Group/OmicsDokument9 SeitenOmics Publishing Group/OmicsDr. Kaushal Kishor SharmaNoch keine Bewertungen
- Epidemiological Surveys of Autism and Other Pervasive Developmental Disorders: An UpdateDokument18 SeitenEpidemiological Surveys of Autism and Other Pervasive Developmental Disorders: An UpdatepipejaramilloNoch keine Bewertungen
- One Size Fits All Cultural Sensitivity in A Psychological Service For Traumatised RefugeesDokument8 SeitenOne Size Fits All Cultural Sensitivity in A Psychological Service For Traumatised RefugeesKnud PedersenNoch keine Bewertungen
- HD Psychiatry 1Dokument6 SeitenHD Psychiatry 1annaNoch keine Bewertungen
- DNB Vol33 NoSuppl 2 190Dokument2 SeitenDNB Vol33 NoSuppl 2 190Anel BrigićNoch keine Bewertungen
- Brinkmann - Mad or NormalDokument15 SeitenBrinkmann - Mad or NormalMaria EduardaNoch keine Bewertungen
- Child and Adolescent PsychiatryDokument8 SeitenChild and Adolescent PsychiatryEdl ZsuzsiNoch keine Bewertungen
- Pattern of Psychiatric Illness Among Tuberculosis Patients (AHMED TANJIMUL ISLAM)Dokument5 SeitenPattern of Psychiatric Illness Among Tuberculosis Patients (AHMED TANJIMUL ISLAM)AHMED TANJIMUL ISLAMNoch keine Bewertungen
- Affective Disorders in Cultural Context: Laurence Kirmayer, and Danielle Groleau, PHDDokument14 SeitenAffective Disorders in Cultural Context: Laurence Kirmayer, and Danielle Groleau, PHDvarhanNoch keine Bewertungen
- Epidemiiology SeminarDokument15 SeitenEpidemiiology SeminarMugu 123Noch keine Bewertungen
- BMC MedicineDokument22 SeitenBMC MedicineCharles FestoNoch keine Bewertungen
- Is Culture An Independent Variable in Psycho Geriatrics. The Case of Brazilian and Japanese ElderlyDokument4 SeitenIs Culture An Independent Variable in Psycho Geriatrics. The Case of Brazilian and Japanese ElderlyGeriatric_NeurologyNoch keine Bewertungen
- Acarturk Et Al 2016Dokument11 SeitenAcarturk Et Al 2016290971Noch keine Bewertungen
- Mental Hygiene & Soc. EnvDokument22 SeitenMental Hygiene & Soc. Envandi lilisNoch keine Bewertungen
- Angermeyer-The Stigma of Mental Illness-Patients' Anticipations and ExperiencesDokument11 SeitenAngermeyer-The Stigma of Mental Illness-Patients' Anticipations and Experiencesstraton_elena755Noch keine Bewertungen
- Non Experimental EpidemologyDokument16 SeitenNon Experimental EpidemologyKrishnaveni MurugeshNoch keine Bewertungen
- SdarticleDokument2 SeitenSdarticleadela_adelaNoch keine Bewertungen
- European PsychiatryDokument7 SeitenEuropean PsychiatryBianca CaterinalisendraNoch keine Bewertungen
- Diarrhoea Morbidity and Mortality in Older Children Adolescents and AdultsDokument12 SeitenDiarrhoea Morbidity and Mortality in Older Children Adolescents and AdultsDelia KrisnasariNoch keine Bewertungen
- 2 Epidemiology by Farwa TahirDokument27 Seiten2 Epidemiology by Farwa TahirAli AkhtarNoch keine Bewertungen
- Post Stroke Aphasia in Spanish Language The Effect of Demographic Variables RG MR AA 2020 OriginalDokument11 SeitenPost Stroke Aphasia in Spanish Language The Effect of Demographic Variables RG MR AA 2020 OriginalGonzaloSebastianRojasFaúndezNoch keine Bewertungen
- Quin Et Al (2011) - Allergy Is Associated With Suicide Completion With A Possible Mediating Role of Mood Disorder - A Population-Based StudyDokument12 SeitenQuin Et Al (2011) - Allergy Is Associated With Suicide Completion With A Possible Mediating Role of Mood Disorder - A Population-Based StudymaelisonNoch keine Bewertungen
- Bronstein, Montgomery. Psychological Distress in Refugee Children - A Systematic ReviewDokument13 SeitenBronstein, Montgomery. Psychological Distress in Refugee Children - A Systematic ReviewAna Isabel PereiraNoch keine Bewertungen
- Essay 3 Draft 1 - 11 03Dokument5 SeitenEssay 3 Draft 1 - 11 03api-643551204Noch keine Bewertungen
- Descriptive Epidemiology: Submitted by Nirmal Varghese KDokument26 SeitenDescriptive Epidemiology: Submitted by Nirmal Varghese KHAMID100% (1)
- Fpsyg 14 1281878Dokument10 SeitenFpsyg 14 1281878dr.joneidiNoch keine Bewertungen
- An Investigation of Irrational Beliefs and Death Anxiety As A Function of Hiv StatusDokument18 SeitenAn Investigation of Irrational Beliefs and Death Anxiety As A Function of Hiv StatusDana PascuNoch keine Bewertungen
- Trends in Alzheimer's Disease and Dementia in The Asian-Pacific RegionDokument4 SeitenTrends in Alzheimer's Disease and Dementia in The Asian-Pacific RegionJeffrey Ramos GironNoch keine Bewertungen
- Lecture-3 - Three - Study Design SelectDokument80 SeitenLecture-3 - Three - Study Design Selectbirtukankassa99Noch keine Bewertungen
- Calidad de Vida 03Dokument7 SeitenCalidad de Vida 03RosarioBengocheaSecoNoch keine Bewertungen
- Acute Asthma Among Adults Presenting To The Emergency DepartmentDokument10 SeitenAcute Asthma Among Adults Presenting To The Emergency DepartmentbedeskahericosNoch keine Bewertungen
- Homoeopathic Intervention in PsoriasisDokument25 SeitenHomoeopathic Intervention in PsoriasisAnil Subhash RathodNoch keine Bewertungen
- CanadcapDokument39 SeitenCanadcapVietrrie SyuhadaNoch keine Bewertungen
- Mental Health TrendDokument8 SeitenMental Health TrendAkhmad RidhaniNoch keine Bewertungen
- Introduction To EpidemiologyDokument25 SeitenIntroduction To EpidemiologyReza Alfitra MutiaraNoch keine Bewertungen
- Outpatient Art Therapy With A Suicidal AdolDokument16 SeitenOutpatient Art Therapy With A Suicidal AdolEsteban Ferrandez MirallesNoch keine Bewertungen
- Managing Depression Among Ethnic Communities: A Qualitative StudyDokument6 SeitenManaging Depression Among Ethnic Communities: A Qualitative StudyCSilva16Noch keine Bewertungen
- Lesson 4 - Mental Health Across The Lifespan: Disaster and Mental Health/ Compiled By: Minera Laiza C. AcostaDokument5 SeitenLesson 4 - Mental Health Across The Lifespan: Disaster and Mental Health/ Compiled By: Minera Laiza C. AcostaCala WritesNoch keine Bewertungen
- How Psychotic Are Individuals With Non-Psychotic Disorders? Soc Psychiatry Psychiatr EpidemiolDokument7 SeitenHow Psychotic Are Individuals With Non-Psychotic Disorders? Soc Psychiatry Psychiatr EpidemiolKKN 11 UMY 2017Noch keine Bewertungen
- Alexis Celis - Final Draft Essay 3Dokument5 SeitenAlexis Celis - Final Draft Essay 3api-643551204Noch keine Bewertungen
- Kleinman, Suffering and Its Professional TransformationDokument18 SeitenKleinman, Suffering and Its Professional Transformationrachel.avivNoch keine Bewertungen
- Personality Traits AsthmaDokument10 SeitenPersonality Traits AsthmaAnna DiaconuNoch keine Bewertungen
- Epidemiology of Primary and Secondary Headaches in A Brazilian Tertiary-Care CenterDokument4 SeitenEpidemiology of Primary and Secondary Headaches in A Brazilian Tertiary-Care CenterVinicius SpazzapanNoch keine Bewertungen
- Background of The Study and SOP - Quali Research2-1Dokument3 SeitenBackground of The Study and SOP - Quali Research2-1Maricris I. AbuanNoch keine Bewertungen
- Religious Convictions in Patients With Epilepsy-Associated Affective Disorders: A Controlled Study From A Psychiatric Acute DepartmentDokument8 SeitenReligious Convictions in Patients With Epilepsy-Associated Affective Disorders: A Controlled Study From A Psychiatric Acute DepartmentgreenanubisNoch keine Bewertungen
- Midgut VolvulusDokument2 SeitenMidgut VolvulusYuriko AndreNoch keine Bewertungen
- Reseach Poster Handout PrintDokument1 SeiteReseach Poster Handout PrintYuriko AndreNoch keine Bewertungen
- EnchantmentanaDokument50 SeitenEnchantmentanamealecsandraNoch keine Bewertungen
- Lampiran A (IKA) PDFDokument1 SeiteLampiran A (IKA) PDFYuriko AndreNoch keine Bewertungen
- How Are We: PresentingDokument44 SeitenHow Are We: PresentingMuhammad Zufar Bin MarwahNoch keine Bewertungen
- Surat LaborDokument2 SeitenSurat LaborYuriko AndreNoch keine Bewertungen
- Apa (Ton) Broeders, Ma PHD University of Leiden NL Netherlands Forensic Institute, Rijswijk NLDokument10 SeitenApa (Ton) Broeders, Ma PHD University of Leiden NL Netherlands Forensic Institute, Rijswijk NLYuriko AndreNoch keine Bewertungen
- Encoded Evidence: Dna in Forensic Analysis: PerspectivesDokument1 SeiteEncoded Evidence: Dna in Forensic Analysis: PerspectivesYuriko AndreNoch keine Bewertungen
- TB Statistics and Key Facts Feb 2014Dokument3 SeitenTB Statistics and Key Facts Feb 2014Yuriko AndreNoch keine Bewertungen
- Review Of: Equivocal Child AbuseDokument1 SeiteReview Of: Equivocal Child AbuseYuriko AndreNoch keine Bewertungen
- Jfo 12275Dokument4 SeitenJfo 12275Yuriko AndreNoch keine Bewertungen
- Eviden BAsed Medicine For PBLDokument33 SeitenEviden BAsed Medicine For PBLamiruddin_smartNoch keine Bewertungen
- Midgut VolvulusDokument2 SeitenMidgut VolvulusYuriko AndreNoch keine Bewertungen
- Jfo 12273Dokument2 SeitenJfo 12273Yuriko AndreNoch keine Bewertungen
- Uillain Arré Yndrome: L A. M, MDDokument4 SeitenUillain Arré Yndrome: L A. M, MDYuriko AndreNoch keine Bewertungen
- Apa (Ton) Broeders, Ma PHD University of Leiden NL Netherlands Forensic Institute, Rijswijk NLDokument10 SeitenApa (Ton) Broeders, Ma PHD University of Leiden NL Netherlands Forensic Institute, Rijswijk NLYuriko AndreNoch keine Bewertungen
- Forensic Art Guidelines SGFAFI1 ST EdDokument24 SeitenForensic Art Guidelines SGFAFI1 ST EdYuriko AndreNoch keine Bewertungen
- Matriks KegiatanDokument1 SeiteMatriks KegiatanErni Yessyca SimamoraNoch keine Bewertungen
- Withholding or Withdrawing LifeDokument5 SeitenWithholding or Withdrawing LifeYuriko AndreNoch keine Bewertungen
- P ('t':'3', 'I':'669120784') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokument14 SeitenP ('t':'3', 'I':'669120784') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Yuriko AndreNoch keine Bewertungen
- 772980Dokument14 Seiten772980Yuriko AndreNoch keine Bewertungen
- Movement DisorderDokument37 SeitenMovement DisorderFalcon DarkNoch keine Bewertungen
- KP 1.1.15 Teknik Presentasi IlmiahDokument21 SeitenKP 1.1.15 Teknik Presentasi IlmiahfitriahendricoNoch keine Bewertungen
- Book Review Forensic Testimony: Science, Law and Expert EvidenceDokument4 SeitenBook Review Forensic Testimony: Science, Law and Expert EvidenceYuriko AndreNoch keine Bewertungen
- P ('t':'3', 'I':'669097626') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokument5 SeitenP ('t':'3', 'I':'669097626') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Yuriko AndreNoch keine Bewertungen
- 3 (Problem-Based Learning)Dokument36 Seiten3 (Problem-Based Learning)Ayu AzlinaNoch keine Bewertungen
- Leadership and Teamwork: Rahmatina B. Herman Bagian Pendidikan Kedokteran Fk-UnandDokument22 SeitenLeadership and Teamwork: Rahmatina B. Herman Bagian Pendidikan Kedokteran Fk-Unandsandurezu100% (1)
- Evaluation and Management of Dyspepia (1999)Dokument14 SeitenEvaluation and Management of Dyspepia (1999)Yuriko AndreNoch keine Bewertungen
- Functional Dyspepsia - Past, Present, and Future (2008)Dokument6 SeitenFunctional Dyspepsia - Past, Present, and Future (2008)Yuriko AndreNoch keine Bewertungen
- Uninvestigated Dyspepsia Versus Investigated DyspepsiaDokument3 SeitenUninvestigated Dyspepsia Versus Investigated DyspepsiaYuriko AndreNoch keine Bewertungen
- SdsadaDokument9 SeitenSdsadaAnonymous KrfJpXb4iNNoch keine Bewertungen
- Second Draft2 8Dokument13 SeitenSecond Draft2 8api-533968411Noch keine Bewertungen
- Bipolar Check in PDFDokument2 SeitenBipolar Check in PDFAnonymous 830d2u2UNoch keine Bewertungen
- GRADE 10 MATH Research On The Effects of Stress To StudentsDokument5 SeitenGRADE 10 MATH Research On The Effects of Stress To StudentsJerica DagupenNoch keine Bewertungen
- Penyakit Obsesif Kompulsif: ReferatDokument11 SeitenPenyakit Obsesif Kompulsif: Referatmol3yNoch keine Bewertungen
- All About PhobiasDokument13 SeitenAll About PhobiasJharna MaheshwariNoch keine Bewertungen
- The Cowards of WarDokument9 SeitenThe Cowards of WarJess Willox100% (1)
- The Cardiff Anomalous Perceptions Scale (CAPS) : A New Validated Measure of Anomalous Perceptual ExperienceDokument12 SeitenThe Cardiff Anomalous Perceptions Scale (CAPS) : A New Validated Measure of Anomalous Perceptual ExperienceAngela EnacheNoch keine Bewertungen
- MCQ On Abnormal PsychologyDokument15 SeitenMCQ On Abnormal PsychologyjinimanxNoch keine Bewertungen
- NFNTSX Handbook eDokument122 SeitenNFNTSX Handbook eowaiskhan91Noch keine Bewertungen
- Personality Disorders Cluster CDokument19 SeitenPersonality Disorders Cluster CPahw BaluisNoch keine Bewertungen
- Help Your Child To Score More: Counselling For Better Life!Dokument1 SeiteHelp Your Child To Score More: Counselling For Better Life!ViseshNoch keine Bewertungen
- Overcoming Disordered Eating - 06 - Improving Low Self-EsteemDokument11 SeitenOvercoming Disordered Eating - 06 - Improving Low Self-EsteemYesha ShahNoch keine Bewertungen
- MSE Psychiatric InterviewingDokument26 SeitenMSE Psychiatric InterviewingZonny PatelNoch keine Bewertungen
- Clinical Psychology Thesis ListDokument42 SeitenClinical Psychology Thesis Listcriket jar100% (1)
- Cheek y Buss Shyness ScaleDokument9 SeitenCheek y Buss Shyness ScaleThomas JohnsonNoch keine Bewertungen
- Appendix A Books by Eric Berne: Editions Include: H A R M o N D S W o R T H: Penguin, 1968Dokument6 SeitenAppendix A Books by Eric Berne: Editions Include: H A R M o N D S W o R T H: Penguin, 1968Maiymona ShahNoch keine Bewertungen
- Antisocial Personality DisorderDokument9 SeitenAntisocial Personality Disordersandi_moore_1Noch keine Bewertungen
- Literature Review - Ali WeekleyDokument7 SeitenLiterature Review - Ali Weekleyapi-559220255Noch keine Bewertungen
- Literature ReviewDokument4 SeitenLiterature Reviewapi-549230420Noch keine Bewertungen
- Predisposing Factors: Precipitating Factors: Perpetuating Factors: Risk FactorsDokument3 SeitenPredisposing Factors: Precipitating Factors: Perpetuating Factors: Risk FactorsRein TamayoNoch keine Bewertungen
- 100321health Profile FormDokument2 Seiten100321health Profile FormmunafNoch keine Bewertungen
- Cynthia Perkins - Prep Assignments Spring 2021Dokument2 SeitenCynthia Perkins - Prep Assignments Spring 2021Haley Vest MustaficNoch keine Bewertungen
- A Comparison of Somatic Symptoms Between Depressive Disorder and Somatoform DisorderDokument8 SeitenA Comparison of Somatic Symptoms Between Depressive Disorder and Somatoform DisorderInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Psychiatric University Hospital Zurich, P.O. Box 1931, CH-8032 Zurich, Switzerland 27.12.2007Dokument4 SeitenPsychiatric University Hospital Zurich, P.O. Box 1931, CH-8032 Zurich, Switzerland 27.12.2007alaaNoch keine Bewertungen
- Chapter 3Dokument10 SeitenChapter 3WATI KAKINoch keine Bewertungen
- Franchie M. Hsu BSN-3 Movie Anlaysis/reflection: Howard Hughes Biography (OCD)Dokument1 SeiteFranchie M. Hsu BSN-3 Movie Anlaysis/reflection: Howard Hughes Biography (OCD)Marivic Yuson MalagarNoch keine Bewertungen
- Stress Management: 1. Self - Awareness and MindfulnessDokument3 SeitenStress Management: 1. Self - Awareness and MindfulnessyekiboomNoch keine Bewertungen