Beruflich Dokumente
Kultur Dokumente
Nursing Interventions CHF
Hochgeladen von
banyenye25Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nursing Interventions CHF
Hochgeladen von
banyenye25Copyright:
Verfügbare Formate
Nursing Interventions: a. Providing Oxygenation Administer oxygen therapy per nasal cannula at 2 to 6 L/ min as ordered.
. Evaluate arterial blood gas analysis results. Maintain semi-fowlers or high-fowlers position to maximize oxygenation by promoting greater lung expansion. b. Promoting rest and activity Bed rest or limited activity may be necessary during the acute phase. Provide an overbed table close to the patient to allow resting the head and arms. The arms may be supported on pillows to reduce the pull on the shoulder muscles when in high-fowlers position, which is most comfortable for the patient. Administer Diazepam (Valium) 2 to 10 mg. Three to four times a day as ordered to allay apprehension. Gradual ambulation is encouraged to prevent risk of venous thrombosis and embolism due to prolonged immobility. Activities should progress through dangling, sitting up in a chair and then walking in increased distances under close supervision. Assess for signs of activity intolerance such as dyspnea, fatigue and increased pulse rate that do not stabilize readily. c. Decreasing anxiety Identifying feelings and concerns related to these feelings. Identify strengths that can be used for coping. Learn what can be done to decrease anxiety. d. Facilitating fluid balance Control of sodium intake. Administer diuretics and digitalis as prescribed. Monitor intake and output, weight and vital signs. e. Providing skin care Edematous skin is poorly nourished and susceptible to pressure sores. Change position at frequent intervals. Assess the sacral area regularly. Use protective devices to prevent pressure sores.
f. Promoting nutrition Provide bland, low-calorie, low-residue with vitamin supplement during the acute phase. Frequent small feedings minimize exertion and reduce gastrointestinal blood requirements. There may be no need to severely restrict sodium intake of the client who receives diuretic. However, no added salt diet is prescribed. Salty foods must be omitted. g. Promoting elimination Advise the client to avoid straining at defecation which involves Valsalvas maneuver. Valsalva maneuver increases cardiac workload. Administer laxative as ordered e.g. Colace (docussate sodium) Encourage use of bedside commode. h. Facilitating learning Teach the client and his family about the disorder and self-care. Monitoring signs and symptoms of recurring CHF, e.g weight gain, loss of appetite, dyspnea, orthopnea, edema of the legs, persistent cough. Report these to the physician. Avoid fatigue, balance rest with activity. Observe prescribed sodium restrictions. Eat small, frequent meals rather than 3 large meals a day. Take prescribed medications at regular basis, e.g. digitalis, diuretics, vasodilators. Observe regular follow-up care as directed. i. If acute pulmonary edema occurs in the client with CHF, the following are the appropriate collaborative management: Place in high-fowlers position, with legs slightly lowered to facilitate breathing and to reduce preload. Morphine sulfate 10 to 15 mg/ IV as ordered. To primarily reduce preload and afterload, and to allay anxiety. Oxygen therapy at 40% to 70% by nasal cannula or face mask. Aminophylline/ IV as ordered. To relieve bronchospasm, increase urinary output and increase cardiac output. Rapid digitalization. Diuretic therapy.
Vasodilators. Dopamine or dobutamine. Monitor serum potassium. Diuresis may result to hypokalemia.
Imaging Assessment Chest X-rays- can be helpful in diagnosing left ventricular failure. Typically the heart is enlarged (cardiomegaly), representing hypertrophy or dilation. Pleural effusions develop less often and generally reflect biventricular failure. Echocardiography- is considered the best tool diagnosing heart failure. Cardiac valvular changes, pericardial effusion, chamber enlargement, and ventricular hypertrophy can be diagnosed using this non-invasive technique. The test can also be used to determine ejection fraction. Radionuclide studies (thallium imaging or technetium pyrophosphate scanning) - can also indicate the presence and causes of heart failure. Other Diagnostic Assessment Electrocardiogram (ECG) - is also performed. It may show ventricular hypertrophy, dysrhythmias, and any degree of myocardial ischemia, injury, or infarction. Pulmonary Artery Catheters- allow the assessment of cardiac function and volume status in acutely ill patients. These measurements can confirm the diagnosis and guide the management of heart failure.
Das könnte Ihnen auch gefallen
- This Study Resource Was Shared Via: Template: SBAR - Postpartum Care SDokument2 SeitenThis Study Resource Was Shared Via: Template: SBAR - Postpartum Care SAira Leigh MoralesNoch keine Bewertungen
- The Infant Should Always Be in A Rear-Facing Car Seat From Birth To 9.1 KGDokument7 SeitenThe Infant Should Always Be in A Rear-Facing Car Seat From Birth To 9.1 KGSabhi Sandhu100% (1)
- NCP GeDokument14 SeitenNCP GeSuluhTriUtomoNoch keine Bewertungen
- Nursing Care Plans: Desired Outcome Interventions Impaired Physical MobilityDokument6 SeitenNursing Care Plans: Desired Outcome Interventions Impaired Physical MobilityNaomi MasudaNoch keine Bewertungen
- Nursing Diagnostic Reasoning for Otitis ExternaDokument5 SeitenNursing Diagnostic Reasoning for Otitis ExternaGino Al Ballano BorinagaNoch keine Bewertungen
- Care Plan FaringitisDokument63 SeitenCare Plan FaringitisEnerolisa ParedesNoch keine Bewertungen
- Cesarean Section PDFDokument9 SeitenCesarean Section PDFIeien MuthmainnahNoch keine Bewertungen
- Plan of Care For:: Nursing Diagnosis: Excess Fluid VolumeDokument3 SeitenPlan of Care For:: Nursing Diagnosis: Excess Fluid VolumeKenji CadizNoch keine Bewertungen
- ABDOMINAL ObjectiveDokument9 SeitenABDOMINAL ObjectiveXing-Jin RomeroNoch keine Bewertungen
- Oxytocin (Pitocin) : Slide 1Dokument16 SeitenOxytocin (Pitocin) : Slide 1Kalesha JonesNoch keine Bewertungen
- NCP NCM 109 Post Partum PeritonitisDokument2 SeitenNCP NCM 109 Post Partum PeritonitisHoney MacabuhayNoch keine Bewertungen
- EclampsiaDokument56 SeitenEclampsiagalihtrimuninggarNoch keine Bewertungen
- Valdez Reflective-Questions PDFDokument3 SeitenValdez Reflective-Questions PDFDexel Lorren ValdezNoch keine Bewertungen
- Pontine BleedingDokument99 SeitenPontine BleedingJeffrey Dela CruzNoch keine Bewertungen
- Electrolyte ImbalanceDokument4 SeitenElectrolyte ImbalanceDoneva Lyn MedinaNoch keine Bewertungen
- Disharge Plan Patient'S Outcome Criteria Nursing OrderDokument2 SeitenDisharge Plan Patient'S Outcome Criteria Nursing OrderDianne Loregas SanchezNoch keine Bewertungen
- Bowel IncontinenceDokument4 SeitenBowel IncontinenceprashanthNoch keine Bewertungen
- HISTORY TAKING - FINAL - Sumanyu258@gmail - Com - 01092014 PDFDokument111 SeitenHISTORY TAKING - FINAL - Sumanyu258@gmail - Com - 01092014 PDFRashmi RanjanNoch keine Bewertungen
- NANDA LIST of N.DiagnosesDokument3 SeitenNANDA LIST of N.DiagnosesHasan KasiNoch keine Bewertungen
- Renal CalculiDokument28 SeitenRenal Calculihailleyann33% (3)
- Nursing Diagnosis GuideDokument9 SeitenNursing Diagnosis Guidekhikmatul mu'jizahNoch keine Bewertungen
- LCPDDokument7 SeitenLCPDakoismeNoch keine Bewertungen
- Gordon'sDokument2 SeitenGordon'sCham Rafaela ConeseNoch keine Bewertungen
- Activity - PT - With - Fluid & Lyte ImbalanceDokument3 SeitenActivity - PT - With - Fluid & Lyte ImbalanceAngel Joy CatalanNoch keine Bewertungen
- Pico Question WatchornDokument5 SeitenPico Question Watchornapi-301725567Noch keine Bewertungen
- Assessing The IntegumentaryDokument73 SeitenAssessing The IntegumentaryHelena Meurial HilkiahNoch keine Bewertungen
- Assessing The Respiratory System (Thorax & Lungs)Dokument3 SeitenAssessing The Respiratory System (Thorax & Lungs)JENNA ELOISA UYNoch keine Bewertungen
- BS CareplanDokument11 SeitenBS CareplanJulia BrownNoch keine Bewertungen
- Dhan Chan NCPDokument3 SeitenDhan Chan NCPDhaneanne Marie ChanNoch keine Bewertungen
- GRP 4 CLO 2 Concept Map PT 1 PDFDokument14 SeitenGRP 4 CLO 2 Concept Map PT 1 PDFMaria Lyn Ocariza ArandiaNoch keine Bewertungen
- Care of Pediatric Client With Dermatologic DisorderDokument3 SeitenCare of Pediatric Client With Dermatologic DisorderAraw GabiNoch keine Bewertungen
- Brief Description of The Disease/statistical IncidenceDokument2 SeitenBrief Description of The Disease/statistical IncidenceLeanne Princess Gamboa100% (1)
- Week 5 CareplanDokument2 SeitenWeek 5 CareplanRaenell Curry100% (1)
- Changing Fecal Pouching Colostomy)Dokument48 SeitenChanging Fecal Pouching Colostomy)Champola Pola Camille BernardoNoch keine Bewertungen
- Appendicitis: Symptoms, Diagnosis, and TreatmentDokument4 SeitenAppendicitis: Symptoms, Diagnosis, and TreatmentBanaag JayNoch keine Bewertungen
- Helping a client with leg traction and impaired mobilityDokument2 SeitenHelping a client with leg traction and impaired mobilityNikki GalveNoch keine Bewertungen
- Fabella NICUDokument4 SeitenFabella NICURoel Dominic BasilanNoch keine Bewertungen
- FNCP On Elevated Blood Pressure 2Dokument4 SeitenFNCP On Elevated Blood Pressure 2Aaron EspirituNoch keine Bewertungen
- St. Ferdinand College Provides Education on Musculoskeletal DisordersDokument12 SeitenSt. Ferdinand College Provides Education on Musculoskeletal DisordersSteve EstebanNoch keine Bewertungen
- National Guidelines On Management of Dengue Fever & Dengue Haemorrhagic Fever in Children and Adolescents - Sri LankaDokument53 SeitenNational Guidelines On Management of Dengue Fever & Dengue Haemorrhagic Fever in Children and Adolescents - Sri LankaNational Dengue Control Unit,Sri Lanka100% (1)
- Pediatric Nursing Care Plan Impaired Physical MobilityDokument5 SeitenPediatric Nursing Care Plan Impaired Physical Mobilityapi-3077327050% (1)
- Rheumatic Joint Disease Study GuideDokument18 SeitenRheumatic Joint Disease Study Guidechalinsammy1Noch keine Bewertungen
- Case Study 101: Abdominal Aortic Aneurysm With Acute Kidney InjuryDokument8 SeitenCase Study 101: Abdominal Aortic Aneurysm With Acute Kidney InjuryPatricia Ann Nicole ReyesNoch keine Bewertungen
- Pediatric Abdominal Assessment: Hind Al-SuwaisDokument20 SeitenPediatric Abdominal Assessment: Hind Al-SuwaisHINDNoch keine Bewertungen
- Ear, Nose and Throat (Ent) AssessmentDokument6 SeitenEar, Nose and Throat (Ent) AssessmentObama kindaNoch keine Bewertungen
- Fluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementDokument32 SeitenFluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementAcohCChaoNoch keine Bewertungen
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Dokument5 SeitenSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenNoch keine Bewertungen
- Activity Intolerance Care Plan For CFDokument8 SeitenActivity Intolerance Care Plan For CFapi-314197645Noch keine Bewertungen
- Concept Map Template NURS 3073Dokument4 SeitenConcept Map Template NURS 3073Savanna ChambersNoch keine Bewertungen
- Nursing Management Pancreatic CancerDokument2 SeitenNursing Management Pancreatic CancerKit NameKo100% (2)
- Fraktur NCP Surgery PDFDokument4 SeitenFraktur NCP Surgery PDFMuklis Al Fadlika100% (1)
- Types of Diagnosis:: Problem-Focused Nursing Diagnoses Have Three Components: (1) Nursing DiagnosisDokument4 SeitenTypes of Diagnosis:: Problem-Focused Nursing Diagnoses Have Three Components: (1) Nursing DiagnosisDaisy MellaNoch keine Bewertungen
- Principles of Casting and SplintingDokument8 SeitenPrinciples of Casting and Splintingbobtaguba100% (1)
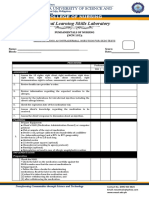
- Clinical Learning Skills Laboratory: College of NursingDokument3 SeitenClinical Learning Skills Laboratory: College of NursingBeverly DatuNoch keine Bewertungen
- Case 1Dokument2 SeitenCase 1Dinarkram Rabreca Ecul100% (1)
- Nursing Process Diagnosis Plan Implementation EvaluationDokument59 SeitenNursing Process Diagnosis Plan Implementation EvaluationYemaya84Noch keine Bewertungen
- Acute and Chronic GastritisDokument6 SeitenAcute and Chronic GastritisAnn CanNoch keine Bewertungen
- Nursing Care PlanDokument2 SeitenNursing Care PlanMiar QuestNoch keine Bewertungen
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideVon EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNoch keine Bewertungen
- Clinical Instructor Cover LetterDokument1 SeiteClinical Instructor Cover Letterbanyenye25Noch keine Bewertungen
- Pathophysiology of Congestive Heart Failure: Cardiovascular SystemDokument3 SeitenPathophysiology of Congestive Heart Failure: Cardiovascular Systembanyenye25Noch keine Bewertungen
- Virginia Henderson TheoryDokument6 SeitenVirginia Henderson Theorybanyenye25Noch keine Bewertungen
- Patho MIDokument2 SeitenPatho MIbanyenye25100% (2)
- Com Epi PaperDokument25 SeitenCom Epi Paperbanyenye25Noch keine Bewertungen
- A G E - PathoDokument1 SeiteA G E - Pathoranee dianeNoch keine Bewertungen
- Patho MIDokument2 SeitenPatho MIbanyenye25100% (2)
- NCP BurnDokument9 SeitenNCP Burnbanyenye2533% (3)
- Laboratory Assessment CHFDokument3 SeitenLaboratory Assessment CHFbanyenye25Noch keine Bewertungen
- Principles of BioethicsDokument5 SeitenPrinciples of Bioethicsbanyenye25Noch keine Bewertungen
- Acute Bronchitis PathoDokument3 SeitenAcute Bronchitis Pathobanyenye25Noch keine Bewertungen
- Philippines Population Pyramid For 2010Dokument4 SeitenPhilippines Population Pyramid For 2010banyenye25Noch keine Bewertungen
- Assessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation SubjectiveDokument6 SeitenAssessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation Subjectivebanyenye25Noch keine Bewertungen
- Nursing Care for Fracture PatientDokument2 SeitenNursing Care for Fracture Patientbanyenye25Noch keine Bewertungen
- Electro Cardiograph yDokument14 SeitenElectro Cardiograph ybanyenye25Noch keine Bewertungen
- NCPDokument4 SeitenNCPbanyenye25Noch keine Bewertungen
- EndometriosisDokument7 SeitenEndometriosisbanyenye25Noch keine Bewertungen
- Philippine healthcare laws overviewDokument5 SeitenPhilippine healthcare laws overviewbanyenye25100% (2)
- NURSING CARE PLAN For Myocardial InfarctionDokument13 SeitenNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- NCP Risk For InfectionDokument3 SeitenNCP Risk For Infectionbanyenye25Noch keine Bewertungen
- Pa Tho PhysiologyDokument2 SeitenPa Tho Physiologybanyenye25Noch keine Bewertungen
- NCP Risk For InfectionDokument3 SeitenNCP Risk For Infectionbanyenye25Noch keine Bewertungen
- Horowitz Taylor A Method of Tapering SSRI Treatment To Mitigate Withdrawal SymptomsDokument17 SeitenHorowitz Taylor A Method of Tapering SSRI Treatment To Mitigate Withdrawal SymptomsDonaNoch keine Bewertungen
- Magical thinking explainedDokument7 SeitenMagical thinking explaineds3m3staNoch keine Bewertungen
- Principles and Practice of Radiation Therapy PDFDokument939 SeitenPrinciples and Practice of Radiation Therapy PDFHala Yousef80% (10)
- Assessment of Antibiotic Utilization in Sepsis Order Sets Initiated in The Emergency Department Draft 2Dokument45 SeitenAssessment of Antibiotic Utilization in Sepsis Order Sets Initiated in The Emergency Department Draft 2api-652562554Noch keine Bewertungen
- Clark IndigestionDokument50 SeitenClark IndigestionRaveendra MungaraNoch keine Bewertungen
- West Bengal Health Recruitment Board: WWW - Wbhrb.inDokument4 SeitenWest Bengal Health Recruitment Board: WWW - Wbhrb.inSouvik Basu RnsNoch keine Bewertungen
- Food Data Chart - Dietary FibreDokument10 SeitenFood Data Chart - Dietary FibreSabina AlicNoch keine Bewertungen
- Recent Advancement in Complete Denture PDFDokument7 SeitenRecent Advancement in Complete Denture PDFNoor MuhammadNoch keine Bewertungen
- Abdominal Wall Learning ObjectivesDokument7 SeitenAbdominal Wall Learning ObjectivesMadison KommorNoch keine Bewertungen
- How To Start A Homestead No Matter Where You LiveDokument41 SeitenHow To Start A Homestead No Matter Where You LiveAndrea MarendaNoch keine Bewertungen
- Exam 2018, Questions and Answers: Dentistry (University of Perpetual Help System DALTA)Dokument23 SeitenExam 2018, Questions and Answers: Dentistry (University of Perpetual Help System DALTA)tsukiyaNoch keine Bewertungen
- Understand and Meet The Nutritional Requirements of Individuals With DementiaDokument22 SeitenUnderstand and Meet The Nutritional Requirements of Individuals With DementiaJovana Ognenovska BakalovskaNoch keine Bewertungen
- Brachioradial PruritusDokument3 SeitenBrachioradial PruritusDan JohnstonNoch keine Bewertungen
- ParestesiDokument1 SeiteParestesiYolanda YiNoch keine Bewertungen
- PSS Siquijor TeamFAZ MCMFDokument21 SeitenPSS Siquijor TeamFAZ MCMFMadelaine Soriano PlaniaNoch keine Bewertungen
- Panacea Photonics User ManualDokument36 SeitenPanacea Photonics User Manualliterarysh1980Noch keine Bewertungen
- Frustrated Homicide CaseDokument6 SeitenFrustrated Homicide CaseJerome Morada100% (2)
- Roc and Auc: Receiver Operating CharacteristicDokument4 SeitenRoc and Auc: Receiver Operating CharacteristicJoe1Noch keine Bewertungen
- Sop Gram StainDokument6 SeitenSop Gram Staindavid mchembeNoch keine Bewertungen
- 6-1 Warm Up and StretchingDokument7 Seiten6-1 Warm Up and StretchingRam SyistNoch keine Bewertungen
- Lesch-Nyhan SyndromeDokument4 SeitenLesch-Nyhan Syndromeapi-209017848Noch keine Bewertungen
- Cornell Notes TemplateDokument3 SeitenCornell Notes Templateapi-385916500100% (1)
- James Levine, M.D., PH.D.,: The New Science of SedentarinessDokument56 SeitenJames Levine, M.D., PH.D.,: The New Science of SedentarinessNational Press FoundationNoch keine Bewertungen
- Iodine: A Support Against Infections and Emerging As An AntibioticDokument5 SeitenIodine: A Support Against Infections and Emerging As An Antibioticdhwanit31Noch keine Bewertungen
- 4 349560477619060786Dokument38 Seiten4 349560477619060786Masali MacdonaNoch keine Bewertungen
- AUBDokument45 SeitenAUBJBNoch keine Bewertungen
- DAFTAR HARGA TGL. 04 JANUARI 2022Dokument52 SeitenDAFTAR HARGA TGL. 04 JANUARI 2022lllaelaNoch keine Bewertungen
- Dictionary of HaematologyDokument293 SeitenDictionary of Haematologyansab6857Noch keine Bewertungen
- Actualizing TherapyDokument12 SeitenActualizing Therapyadieisidro100% (1)
- Daftar PustakaDokument8 SeitenDaftar PustakaRachel VictorianaNoch keine Bewertungen