Beruflich Dokumente
Kultur Dokumente
Thrombotic Thrombocytopenic Purpura
Hochgeladen von
Ahsan Tanio DaulayOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Thrombotic Thrombocytopenic Purpura
Hochgeladen von
Ahsan Tanio DaulayCopyright:
Verfügbare Formate
Thrombotic Thrombocytopenic Purpura
http://emedicine.medscape.com/article/206598-overview
Medscape Reference Reference
News Reference Education MEDLINE
Thrombotic Thrombocytopenic Purpura
Author: Theodore Wun, MD, FACP; Chief Editor: Emmanuel C Besa, MD more... Updated: Feb 4, 2013
Practice Essentials
Thrombotic Thrombocytopenic Purpura (TTP) is a rare blood disorder characterized by clotting in small blood vessels of the body (thromboses), resulting in a low platelet count. In its full-blown form, the disease consists of the pentad of microangiopathic hemolytic anemia, thrombocytopenic purpura, neurologic abnormalities, fever, and renal disease.
Signs and symptoms
Patients with TTP typically report an acute or subacute onset of symptoms related to neurologic dysfunction, anemia, or thrombocytopenia. Neurologic manifestations include alteration in mental status, seizures, hemiplegia, paresthesias, visual disturbance, and aphasia Fatigue may accompany the anemia Severe bleeding from thrombocytopenia is unusual, although petechiae are common TTP can affect any organ system, but involvement of the peripheral blood, the central nervous system, and the kidneys causes the clinical manifestations. See Clinical Presentation for more detail.
Diagnosis
The exact etiology of TTP is unknown. Most sporadic cases of TTP appear to be associated with severe deficiency of ADAMTS13 activity due to autoantibodies against this protease.[1] Measuring ADAMTS13 activity level may aid in diagnosis. Laboratory studies for suspected TTP include a CBC, platelet count, blood smears, coagulation studies, BUN creatinine, and serum bilirubin and lactate dehydrogenase. Imaging studies and biopsies are not required for diagnosis. See Workup for more detail.
Management
The therapy of choice for TTP is plasma exchange with fresh frozen plasma. Only the minority of TTP patients (20-30%) present with the classic pentad. The presence of microangiopathic hemolytic anemia (schistocytes, elevated
1 dari 5
3/16/2013 6:21 AM
Thrombotic Thrombocytopenic Purpura
http://emedicine.medscape.com/article/206598-overview
LDH, and indirect hyperbilirubinemia) and thrombocytopenia in the absence of other obvious causes (DIC, malignant hypertension) is justification to begin total plasma exchange. Octaplas (Octapharma), a blood plasma product extensively used in Europe, was approved by the FDA in January 2013 for use in the United States. The product is a sterile, frozen solution of pooled human plasma from several donors. It is a viable alternative to single-donor plasma, and it is treated with a solvent detergent process, which reduces the risk of infection. The FDA based approval on clinical studies of patients with liver disease, liver transplant, heart surgery, and TTP. [2] In those patients refractory to plasma exchange, using cryopoor plasma (or cryosupernatant) has sometimes led to a response. This is fresh frozen plasma that has had the cryoprecipitate removed and is thus depleted of high-molecular-weight von Willebrand multimers, which have a pathogenic role in TTP. Corticosteroids may also be used in refractory patients. See Treatment and Medication for more detail.
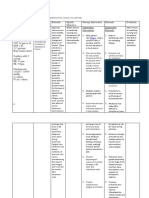
Image library
Peripheral smear from a patient with thrombotic thrombocytopenic purpura: Red blood cells are fragmented and appear as schistocytes. Certain schistocytes have the appearance of helmet cells (H). Spheroidal cells often are present (S). Occasional nucleated erythroid precursors may be present.
Background
In 1924, Eli Moschowitz, MD, described a girl who presented with an abrupt onset of petechiae and pallor followed rapidly by paralysis, coma, and death. Upon pathologic examination, the small arterioles and capillaries of the patient were found to have thrombi consisting mostly of platelets. Dr. Moschowitz hypothesized a "powerful poison which had both agglutinative and hemolytic properties" as the cause of the disease. The syndrome described by Moschowitz is now known as thrombotic thrombocytopenic purpura (TTP). See image below.
Peripheral smear from a patient with thrombotic thrombocytopenic purpura: Red blood cells are fragmented and appear as schistocytes. Certain schistocytes have the appearance of helmet cells (H). Spheroidal cells often are present (S). Occasional nucleated erythroid precursors may be present.
In its full-blown form, the disease consists of the pentad of microangiopathic hemolytic anemia, thrombocytopenic purpura, neurologic abnormalities, fever, and renal disease. A closely related disorder, hemolytic-uremic syndrome (HUS), shares many clinical characteristics of TTP but is more common in children. Renal abnormalities tend to be more severe in HUS. Although once considered variants of a single syndrome, recent evidence suggests differing pathogenic mechanisms of TTP and HUS. The mortality of TTP is greatly reduced with the routine use of aggressive high-volume total plasma exchange (TPE). The effect of TPE on the outcome of patients with HUS is more controversial.
Pathophysiology
2 dari 5
3/16/2013 6:21 AM
Thrombotic Thrombocytopenic Purpura
http://emedicine.medscape.com/article/206598-overview
TTP can affect any organ system, but involvement of the peripheral blood, the central nervous system, and the kidneys causes the clinical manifestations. The classic histologic lesion is one of bland thrombi in the microvasculature of affected organs. These thrombi consist predominantly of platelets with little fibrin and red cells compared to thrombi that occur secondary to intravascular coagulation. The ultimate cause of TTP is unknown; however, recent research has uncovered some clues about the pathophysiology. Patients with TTP have unusually large multimers of von Willebrand factor (vWF) in their plasma. Patients with TTP lack a plasma protease that is responsible for the breakdown of these ultralarge vWF multimers. In the congenital form of TTP, mutations in the gene encoding this protease have been described. In the more common sporadic form, an antibody inhibitor can be isolated in most patients. This protease has been isolated and cloned and is designated ADAMTS13 (a disintegrinlike and metalloprotease with thrombospondin type 1 motif 13). The activity of this protease is normal in most patients with classic HUS suggesting differing pathogenesis of these closely related entities.[3]
Frequency
United States
Exact incidence figures are not available, although TTP is thought to be a rare disease. One series showed the frequency was 1 in approximately 50,000 hospital admissions. In a 25-year period in the Sacramento, California region (population at risk 1.2 million), at least 176 documented cases of TTP were reported. In another 1-year study, 20 institutions reported 115 patients with TTP.
International
International incidence figures are not available.
Mortality/Morbidity
Untreated, TTP has a mortality rate of as high as 90%. With plasma exchange, the mortality rate is reduced to 10-20%. Acute morbidities include ischemic events such as stroke, transient-ischemic attacks, myocardial infarction and arrhythmia, bleeding, and azotemia. In general, survivors have no long-term sequelae, with the exception of residual neurologic deficits in a minority of patients. However, relapses are not uncommon, occurring in 13-36% of patients.
Race
An ethnic predisposition to TTP is not established.
Sex
In the larger series reported, a female predominance of approximately 2:1 was noted.
Age
In several large studies, the median age at diagnosis is approximately 40 years. However, in the authors' series of 126 consecutive patients, the median age was 52 years. In general, HUS is diagnosed in children and TTP is diagnosed in adults. Ninety percent of cases of HUS occur in children. Bouw et al recently presented a review article of TTP in children.[4]
Contributor Information and Disclosures
Author Theodore Wun, MD, FACP Professor of Medicine, Professor of Pathology and Laboratory Medicine, University of California Davis School of Medicine; Chief of Hematology/Oncology, Program Director, Veterans Affairs Northern California Health Care System; Medical Director, University of California Davis CCRC Theodore Wun, MD, FACP is a member of the following medical societies: American Association of Blood Banks, American College of Physicians, American Federation for Medical Research, American Society for Blood and
3 dari 5
3/16/2013 6:21 AM
Thrombotic Thrombocytopenic Purpura
http://emedicine.medscape.com/article/206598-overview
Marrow Transplantation, American Society of Hematology, and Southwest Oncology Group Disclosure: Nothing to disclose. Coauthor(s) Wadie F Bahou, MD Chief, Division of Hematology, Hematology/Oncology Fellowship Director, Professor, Department of Internal Medicine, State University of New York at Stony Brook Wadie F Bahou, MD is a member of the following medical societies: American Society of Hematology Disclosure: Nothing to disclose. Specialty Editor Board Wadie F Bahou, MD Chief, Division of Hematology, Hematology/Oncology Fellowship Director, Professor, Department of Internal Medicine, State University of New York at Stony Brook Wadie F Bahou, MD is a member of the following medical societies: American Society of Hematology Disclosure: Nothing to disclose. Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference Disclosure: Medscape Salary Employment Marcel E Conrad, MD Distinguished Professor of Medicine (Retired), University of South Alabama College of Medicine Marcel E Conrad, MD is a member of the following medical societies: Alpha Omega Alpha, American Association for the Advancement of Science, American Association of Blood Banks, American Chemical Society, American College of Physicians, American Physiological Society, American Society for Clinical Investigation, American Society of Hematology, Association of American Physicians, Association of Military Surgeons of the US, International Society of Hematology, Society for Experimental Biology and Medicine, and Southwest Oncology Group Disclosure: No financial interests None None Rajalaxmi McKenna, MD, FACP Southwest Medical Consultants, SC, Department of Medicine, Good Samaritan Hospital, Advocate Health Systems Rajalaxmi McKenna, MD, FACP is a member of the following medical societies: American Society of Clinical Oncology, American Society of Hematology, and International Society on Thrombosis and Haemostasis Disclosure: Nothing to disclose. Chief Editor Emmanuel C Besa, MD Professor, Department of Medicine, Division of Hematologic Malignancies and Hematopoietic Stem Cell Transplantation, Kimmel Cancer Center, Jefferson Medical College of Thomas Jefferson University Emmanuel C Besa, MD is a member of the following medical societies: American Association for Cancer Education, American College of Clinical Pharmacology, American Federation for Medical Research, American Society of Clinical Oncology, American Society of Hematology, and New York Academy of Sciences Disclosure: Nothing to disclose.
References
1. Ferrari S, Mudde GC, Rieger M, Veyradier A, Kremer Hovinga JA, Scheiflinger F. IgG-subclass distribution of anti-ADAMTS13 antibodies in patients with acquired thrombotic thrombocytopenic purpura. J Thromb Haemost. Aug 11 2009;[Medline]. 2. Lowes R. FDA Okays Blood Plasma Product for Clotting Disorders. Medscape Medical News. January 17,
4 dari 5
3/16/2013 6:21 AM
Thrombotic Thrombocytopenic Purpura
http://emedicine.medscape.com/article/206598-overview
2013. Available at http://www.medscape.com/viewarticle/777822. Accessed January 31, 2013. 3. Sauna ZE, Okunji C, Hunt RC, et al. Characterization of conformation-sensitive antibodies to ADAMTS13, the von Willebrand cleavage protease. PLoS One. Aug 5 2009;4(8):e6506. [Medline]. [Full Text]. 4. Bouw MC, Dors N, van Ommen H, Ramakers-van Woerden NL. Thrombotic thrombocytopenic purpura in childhood. Pediatr Blood Cancer. Jun 18 2009;53(4):537-542. [Medline]. 5. Marn Pernat A, Buturovic-Ponikvar J, Kovac J, et al. Membrane plasma exchange for the treatment of thrombotic thrombocytopenic purpura. Ther Apher Dial . Aug 2009;13(4):318-21. [Medline]. 6. Jhaveri KD, Scheuer A, Cohen J, Gordon B. Treatment of refractory thrombotic thrombocytopenic purpura using multimodality therapy including splenectomy and cyclosporine. Transfus Apher Sci . Aug 2009;41(1):19-22. [Medline]. 7. Scully M, McDonald V, Cavenagh J, et al. A phase 2 study of the safety and efficacy of rituximab with plasma exchange in acute acquired thrombotic thrombocytopenic purpura. Blood. Aug 18 2011;118(7):1746-53. [Medline]. 8. Bell WR, Braine HG, Ness PM, Kickler TS. Improved survival in thrombotic thrombocytopenic purpurahemolytic uremic syndrome. Clinical experience in 108 patients. N Engl J Med. Aug 8 1991;325(6):398-403. [Medline]. 9. Fakhouri F, Vernant JP, Veyradier A, et al. Efficiency of curative and prophylactic treatment with rituximab in ADAMTS13-deficient thrombotic thrombocytopenic purpura: a study of 11 cases. Blood. Sep 15 2005;106(6):1932-7. [Medline]. 10. Furlan M, Robles R, Galbusera M, et al. von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolytic-uremic syndrome. N Engl J Med. Nov 26 1998;339(22):1578-84. [Medline]. 11. Lara PN, Coe TL, Zhou H, et al. Improved survival with plasma exchange in patients with thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Am J Med. Dec 1999;107(6):573-9. [Medline]. 12. Lau DH, Wun T. Early manifestation of thrombotic thrombocytopenic purpura. Am J Med. Nov 1993;95(5):544-5. [Medline]. 13. Moake JL. Haemolytic-uraemic syndrome: basic science. Lancet. Feb 12 1994;343(8894):393-7. [Medline]. 14. Neild GH. Haemolytic-uraemic syndrome in practice. [published erratum appears in Lancet 1994 Feb 26;343(8896):552]. Lancet. Feb 12 1994;343(8894):398-401. [Medline]. 15. Rock GA, Shumak KH, Buskard NA, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian Apheresis Study Group. N Engl J Med. Aug 8 1991;325(6):393-7. [Medline]. 16. Shumak KH, Rock GA, Nair RC. Late relapses in patients successfully treated for thrombotic thrombocytopenic purpura. Canadian Apheresis Group. Ann Intern Med. Apr 15 1995;122(8):569-72. [Medline]. 17. Tsai HM, Lian EC. Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura. N Engl J Med. Nov 26 1998;339(22):1585-94. [Medline]. 18. Vesely SK, George JN, Lammle B, et al. ADAMTS13 activity in thrombotic thrombocytopenic purpurahemolytic uremic syndrome: relation to presenting features and clinical outcomes in a prospective cohort of 142 patients. Blood. Jul 1 2003;102(1):60-8. [Medline]. Medscape Reference 2011 WebMD, LLC
5 dari 5
3/16/2013 6:21 AM
Das könnte Ihnen auch gefallen
- 2014 - Trombotic MicroangiopathiesDokument23 Seiten2014 - Trombotic MicroangiopathiesLuis Fernando Morales JuradoNoch keine Bewertungen
- Idiopathic Thrombocytopenic Purpura (ITPDokument11 SeitenIdiopathic Thrombocytopenic Purpura (ITPMelDred Cajes BolandoNoch keine Bewertungen
- Thrombotic Thrombocytopenic Purpura PDFDokument6 SeitenThrombotic Thrombocytopenic Purpura PDFDany EdyNoch keine Bewertungen
- Thrombotic Thrombocytopenic Purpura and Hemolytic Uremic SyndromeDokument9 SeitenThrombotic Thrombocytopenic Purpura and Hemolytic Uremic SyndromeRex RuthorNoch keine Bewertungen
- 1 s2.0 S0899588513000701 Main PDFDokument8 Seiten1 s2.0 S0899588513000701 Main PDFRicki HanNoch keine Bewertungen
- Acquired TTP - Clinical Manifestations and Diagnosis - UpToDateDokument17 SeitenAcquired TTP - Clinical Manifestations and Diagnosis - UpToDatepradeep danielNoch keine Bewertungen
- Disorder of PlateletsDokument27 SeitenDisorder of PlateletsRoby KieranNoch keine Bewertungen
- Why Does My Patient Have Thrombocytopenia PDFDokument22 SeitenWhy Does My Patient Have Thrombocytopenia PDFElena Villarreal100% (1)
- Immune Thrombocytopenic Purpura (ITP) :: A New Look at An Old DisorderDokument6 SeitenImmune Thrombocytopenic Purpura (ITP) :: A New Look at An Old DisorderAsri Alifa SholehahNoch keine Bewertungen
- Guide To Anticoagulant Therapy: Heparin: AHA Scientific StatementDokument26 SeitenGuide To Anticoagulant Therapy: Heparin: AHA Scientific StatementIkeBundaAdellulaNoch keine Bewertungen
- Polisitemia VeraDokument4 SeitenPolisitemia VeraJicko Street HooligansNoch keine Bewertungen
- ThrombocytopeniaDokument9 SeitenThrombocytopeniaamjad_muslehNoch keine Bewertungen
- Anemias Aplastic Anemia Is A Condition Where Bone Marrow Does Not Produce Sufficient NewDokument15 SeitenAnemias Aplastic Anemia Is A Condition Where Bone Marrow Does Not Produce Sufficient NewZoreyca RiveraNoch keine Bewertungen
- Thrombotic Thrombocytopenic Purpura: Serena Ezzeddine Morning Report September 8, 2008Dokument22 SeitenThrombotic Thrombocytopenic Purpura: Serena Ezzeddine Morning Report September 8, 2008Yeni Chie Aneuk TuleutNoch keine Bewertungen
- Thrombocytopenic Disorders: Damanhour University Faculty of PharmacyDokument9 SeitenThrombocytopenic Disorders: Damanhour University Faculty of Pharmacyزياد محمدNoch keine Bewertungen
- DR Prakash Nag MD Medicine NGMCDokument70 SeitenDR Prakash Nag MD Medicine NGMCSamjhana NeupaneNoch keine Bewertungen
- Diagnostic Approach To Thrombocytopenia in Adults - UpToDateDokument81 SeitenDiagnostic Approach To Thrombocytopenia in Adults - UpToDateWidya MentariNoch keine Bewertungen
- 3032 Full PDFDokument12 Seiten3032 Full PDFcinosure1Noch keine Bewertungen
- Approach To The Adult With Unexplained Thrombocytopenia - UpToDateDokument36 SeitenApproach To The Adult With Unexplained Thrombocytopenia - UpToDateBhargav YagnikNoch keine Bewertungen
- Kappler 2017Dokument23 SeitenKappler 2017Alex CroNoch keine Bewertungen
- Trombocytopenia Uniba 16-1-13Dokument32 SeitenTrombocytopenia Uniba 16-1-13Dwiki Surya PrayogaNoch keine Bewertungen
- (Stasi) How To Approach Thrombocytopenia PDFDokument7 Seiten(Stasi) How To Approach Thrombocytopenia PDFrodtobingNoch keine Bewertungen
- Platelet Disorders: Autoimmune ThrombocytopeniasDokument6 SeitenPlatelet Disorders: Autoimmune ThrombocytopeniasShī Fu KoNoch keine Bewertungen
- Guidelines On The Diagnosis and Management of Thrombotic Thrombocytopenic Purpura and Other Thrombotic MicroangiopathiesDokument13 SeitenGuidelines On The Diagnosis and Management of Thrombotic Thrombocytopenic Purpura and Other Thrombotic Microangiopathiescitometria clinicaNoch keine Bewertungen
- Von Willebrand Factor, ADAMTS13, and Thrombotic Thrombocytopenic PurpuraDokument9 SeitenVon Willebrand Factor, ADAMTS13, and Thrombotic Thrombocytopenic PurpuraPaola TabaresNoch keine Bewertungen
- Thrombocytopenia: An Update: K. J. Smock, S. L. PerkinsDokument10 SeitenThrombocytopenia: An Update: K. J. Smock, S. L. PerkinsRevathy GunaseelanNoch keine Bewertungen
- In Brief: Thrombotic DisordersDokument5 SeitenIn Brief: Thrombotic DisordersalfredoibcNoch keine Bewertungen
- 10.21.09 Jenkins TTPDokument16 Seiten10.21.09 Jenkins TTPOdiliaDeaNovenaNoch keine Bewertungen
- Trombocitopenia en El IntensivoDokument9 SeitenTrombocitopenia en El IntensivoEstuardo Aguilar RuizNoch keine Bewertungen
- Blood 2013 Gernsheimer 38 47Dokument11 SeitenBlood 2013 Gernsheimer 38 47Nur Rahmat WibowoNoch keine Bewertungen
- Managing bleeding disorders during pregnancyDokument7 SeitenManaging bleeding disorders during pregnancyKharismaNisaNoch keine Bewertungen
- Ojim 2016091213324550Dokument10 SeitenOjim 2016091213324550rianmg21Noch keine Bewertungen
- Itp TTP Pic DXNDokument4 SeitenItp TTP Pic DXNmaryminNoch keine Bewertungen
- Bleeding DisorderDokument56 SeitenBleeding DisorderPriya Singh100% (1)
- Thrombocytopenia in CirrhosisDokument4 SeitenThrombocytopenia in Cirrhosismy accountNoch keine Bewertungen
- Thrombotic Thrombocytopenic Purpura, Heparin-Induced Thrombocytopenia, and Disseminated Intravascular Coagulation 2020Dokument21 SeitenThrombotic Thrombocytopenic Purpura, Heparin-Induced Thrombocytopenia, and Disseminated Intravascular Coagulation 2020Cris TobalNoch keine Bewertungen
- Pathology Bleeding DisordersDokument67 SeitenPathology Bleeding DisordersMarcelliaNoch keine Bewertungen
- Bloodbook 2017 660 PDFDokument7 SeitenBloodbook 2017 660 PDFSambit DashNoch keine Bewertungen
- Kuliah Platelets DisordersDokument22 SeitenKuliah Platelets DisordersDesi AdiyatiNoch keine Bewertungen
- Bleeding Disorder (Paediatrics)Dokument95 SeitenBleeding Disorder (Paediatrics)Nurul Afiqah Mohd YusoffNoch keine Bewertungen
- Hypertension: Pathophysiology and Diagnosis - CPD Article - Pharmaceutical JournalDokument8 SeitenHypertension: Pathophysiology and Diagnosis - CPD Article - Pharmaceutical JournalOrion JohnNoch keine Bewertungen
- Hematology 2012 Falanga 571 81Dokument11 SeitenHematology 2012 Falanga 571 81Zikry AuliaNoch keine Bewertungen
- TTP vs HUS: Distinguishing Features and TreatmentDokument21 SeitenTTP vs HUS: Distinguishing Features and TreatmentHanif ullahNoch keine Bewertungen
- 10 1038@nrdp20156Dokument17 Seiten10 1038@nrdp20156Desi DwiNoch keine Bewertungen
- Defining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsDokument7 SeitenDefining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsZikry AuliaNoch keine Bewertungen
- Diagnosis and Clinical Manifestations of Essential ThrombocythemiaDokument27 SeitenDiagnosis and Clinical Manifestations of Essential ThrombocythemiaValeria GamboaNoch keine Bewertungen
- Approach To The Adult With Unexplained Pancytopenia - UpToDateDokument28 SeitenApproach To The Adult With Unexplained Pancytopenia - UpToDatesusanaNoch keine Bewertungen
- Hema 2 5th Ed SummaryDokument9 SeitenHema 2 5th Ed Summarymonzon.mika1801Noch keine Bewertungen
- Diagnosis and Management of PNHDokument12 SeitenDiagnosis and Management of PNHapi-26302710Noch keine Bewertungen
- Etiology and Significance of Thrombocytopenia in Critically Ill PatientsDokument13 SeitenEtiology and Significance of Thrombocytopenia in Critically Ill PatientsSambit DashNoch keine Bewertungen
- HP Jan05 BleedDokument5 SeitenHP Jan05 BleedSyahanim IsmailNoch keine Bewertungen
- Jurnal MikroDokument9 SeitenJurnal MikroVina SalsabilaNoch keine Bewertungen
- Manejo TrombocitopeniaDokument7 SeitenManejo TrombocitopeniaJenniferLanda'Noch keine Bewertungen
- Aplastic Anemia - An Overview: DR Aniruddh Shrivastava Guided By: DR S.H. Talib SIRDokument42 SeitenAplastic Anemia - An Overview: DR Aniruddh Shrivastava Guided By: DR S.H. Talib SIRdoctoranswerit_84161Noch keine Bewertungen
- Hematologic Disorders: JeffreyDokument582 SeitenHematologic Disorders: JeffreyPalak GuptaNoch keine Bewertungen
- How I Treat TTPDokument10 SeitenHow I Treat TTPGhazal KangoNoch keine Bewertungen
- Bod Cerebrovasculardiseasestroke PDFDokument67 SeitenBod Cerebrovasculardiseasestroke PDFMax Laban SeminarioNoch keine Bewertungen
- Fast Facts: Thrombotic Thrombocytopenic Purpura: Prompt action saves livesVon EverandFast Facts: Thrombotic Thrombocytopenic Purpura: Prompt action saves livesNoch keine Bewertungen
- Secondary HypertensionVon EverandSecondary HypertensionAlberto MorgantiNoch keine Bewertungen
- Essential Thrombocytosis, (Excess Platelets) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandEssential Thrombocytosis, (Excess Platelets) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBewertung: 4 von 5 Sternen4/5 (1)
- GeriatriDokument10 SeitenGeriatriAhsan Tanio DaulayNoch keine Bewertungen
- Clinical Implication of Ageing Process and CGA - CZHDokument71 SeitenClinical Implication of Ageing Process and CGA - CZHAhsan Tanio DaulayNoch keine Bewertungen
- Perioperative Assessment in Elderly Surgical Patients: Geriatrics Point of ViewDokument43 SeitenPerioperative Assessment in Elderly Surgical Patients: Geriatrics Point of ViewAhsan Tanio DaulayNoch keine Bewertungen
- ICD-10 Trg. Tool User - GuideDokument15 SeitenICD-10 Trg. Tool User - Guidecckpo100% (1)
- Paper Obesity Is The Major Determinant of Elevated C-Reactive Protein in Subjects With The Metabolic SyndromeDokument6 SeitenPaper Obesity Is The Major Determinant of Elevated C-Reactive Protein in Subjects With The Metabolic SyndromeAhsan Tanio DaulayNoch keine Bewertungen
- Geriatric Medicine - Lally, Frank, Roffe, Christine (SRG)Dokument237 SeitenGeriatric Medicine - Lally, Frank, Roffe, Christine (SRG)pperutti100% (3)
- Antimicrobial Treatment Guidelines For Common Infections: June 2016Dokument56 SeitenAntimicrobial Treatment Guidelines For Common Infections: June 2016mario x.p.de araujoNoch keine Bewertungen
- 879 FullDokument7 Seiten879 FullAhsan Tanio DaulayNoch keine Bewertungen
- Adult Cardiac Life SupportDokument50 SeitenAdult Cardiac Life SupportAhsan Tanio DaulayNoch keine Bewertungen
- Adult Cardiac Life SupportDokument50 SeitenAdult Cardiac Life SupportAhsan Tanio DaulayNoch keine Bewertungen
- Check Your English Vocabulary For MedicineDokument65 SeitenCheck Your English Vocabulary For MedicineOlga Poleszak100% (1)
- Icd10cm Tabular Addenda 2017Dokument160 SeitenIcd10cm Tabular Addenda 2017Ahsan Tanio DaulayNoch keine Bewertungen
- Ijhoscr 7 034Dokument6 SeitenIjhoscr 7 034Ahsan Tanio DaulayNoch keine Bewertungen
- ICD 10 Diagnostic Codes for Dept of MedicineDokument4 SeitenICD 10 Diagnostic Codes for Dept of MedicineFern PeñarandaNoch keine Bewertungen
- ICD-10 Chapter I - Certain Infectious and Parasitic Diseases - WikipediaDokument84 SeitenICD-10 Chapter I - Certain Infectious and Parasitic Diseases - WikipediaAhsan Tanio DaulayNoch keine Bewertungen
- Effect of Dialysis On Bleeding Time in Chronic Renal FailureDokument5 SeitenEffect of Dialysis On Bleeding Time in Chronic Renal FailureAhsan Tanio DaulayNoch keine Bewertungen
- Antithrombin DeficiencyDokument11 SeitenAntithrombin DeficiencyAhsan Tanio DaulayNoch keine Bewertungen
- Factor XDokument6 SeitenFactor XAhsan Tanio DaulayNoch keine Bewertungen
- Battlefield AcupunctureDokument7 SeitenBattlefield AcupunctureAhsan Tanio DaulayNoch keine Bewertungen
- List of Antibiotics - Wikipedia, The Free EncyclopediaDokument13 SeitenList of Antibiotics - Wikipedia, The Free EncyclopediaAhsan Tanio DaulayNoch keine Bewertungen
- Acromegaly Testing: Click Here For Topics Associated With This AlgorithmDokument1 SeiteAcromegaly Testing: Click Here For Topics Associated With This AlgorithmAhsan Tanio DaulayNoch keine Bewertungen
- Drug Induce ATnDokument33 SeitenDrug Induce ATnAhsan Tanio DaulayNoch keine Bewertungen
- Jurnal 2 - AlbuminuriaDokument6 SeitenJurnal 2 - AlbuminuriaAhsan Tanio DaulayNoch keine Bewertungen
- Effect of Dialysis On Bleeding Time in Chronic Renal FailureDokument5 SeitenEffect of Dialysis On Bleeding Time in Chronic Renal FailureAhsan Tanio DaulayNoch keine Bewertungen
- Jadwal Jaga Azzakiah Jan 2013, Coba 1Dokument39 SeitenJadwal Jaga Azzakiah Jan 2013, Coba 1Ahsan Tanio DaulayNoch keine Bewertungen
- Unconjugated BilirubinDokument9 SeitenUnconjugated BilirubinAhsan Tanio DaulayNoch keine Bewertungen
- Factor IIDokument7 SeitenFactor IIAhsan Tanio DaulayNoch keine Bewertungen
- Factor VIIDokument8 SeitenFactor VIIAhsan Tanio DaulayNoch keine Bewertungen
- Factor VIIDokument8 SeitenFactor VIIAhsan Tanio DaulayNoch keine Bewertungen
- Test Bank For Microbiology An Introduction 13th Edition Gerard J Tortora Berdell R Funke Christine L Case Derek Weber Warner BairDokument35 SeitenTest Bank For Microbiology An Introduction 13th Edition Gerard J Tortora Berdell R Funke Christine L Case Derek Weber Warner Bairshriekacericg31u3100% (37)
- Analysus of The Soft Tissue Profile in Croatians With Normal Occlusions and Well-Balanced FacesDokument6 SeitenAnalysus of The Soft Tissue Profile in Croatians With Normal Occlusions and Well-Balanced FacesIvanna H. A.Noch keine Bewertungen
- 2021 ASO Biology Exam Part 1Dokument20 Seiten2021 ASO Biology Exam Part 1Joshua DeathNoch keine Bewertungen
- Biology Bacteria Worksheet ANSWERSDokument2 SeitenBiology Bacteria Worksheet ANSWERSPsudopodNoch keine Bewertungen
- Msds Potassium Chloride 0.1MDokument5 SeitenMsds Potassium Chloride 0.1MNicholas Chan100% (1)
- DNA Profiling Gizmo Student Exploration SheetDokument5 SeitenDNA Profiling Gizmo Student Exploration SheetCarter BonesNoch keine Bewertungen
- Homeopathic Remedy Pictures Vicki Mathison Frans Kusse.11789 - 1 PDFDokument19 SeitenHomeopathic Remedy Pictures Vicki Mathison Frans Kusse.11789 - 1 PDFPrasanta ChatterjeeNoch keine Bewertungen
- Gene Therapy PDFDokument3 SeitenGene Therapy PDFJenny PastorNoch keine Bewertungen
- Introduction To ChemotherapyDokument28 SeitenIntroduction To ChemotherapyShivsharan B. DhaddeNoch keine Bewertungen
- Medical Technology Sections OverviewDokument3 SeitenMedical Technology Sections OverviewAlliah LorioNoch keine Bewertungen
- Antenatal Care and High Risk PregnancyDokument76 SeitenAntenatal Care and High Risk PregnancyLouis EkaputraNoch keine Bewertungen
- 705 FullDokument11 Seiten705 FullNguyễn HùngNoch keine Bewertungen
- Need To Know.: Self-Regulation: Science BackgrounderDokument3 SeitenNeed To Know.: Self-Regulation: Science BackgrounderRachelNoch keine Bewertungen
- Neuropsych Lec 5 Mental Status ExamDokument2 SeitenNeuropsych Lec 5 Mental Status ExamnkivcNoch keine Bewertungen
- Sensory Processing DisorderDokument9 SeitenSensory Processing Disorderapi-360330020Noch keine Bewertungen
- Mark Scheme (Results) November 2012: GCSE Biology 5BI2H/01Dokument16 SeitenMark Scheme (Results) November 2012: GCSE Biology 5BI2H/01RebeccaNoch keine Bewertungen
- Medical certificate conditions recurrent natureDokument1 SeiteMedical certificate conditions recurrent naturerajkmm36Noch keine Bewertungen
- Bacteria-Genetic TransferDokument57 SeitenBacteria-Genetic TransferKA AngappanNoch keine Bewertungen
- Medical Biochemistry Course SyllabusDokument6 SeitenMedical Biochemistry Course SyllabusSheryl ShohamNoch keine Bewertungen
- Rosenthal 2016Dokument10 SeitenRosenthal 2016RONALD. D VIERA .MNoch keine Bewertungen
- Stomatognathic SystemDokument129 SeitenStomatognathic Systemsurya kingsly100% (1)
- Microbiology NotesDokument3 SeitenMicrobiology NotesAthena Huynh100% (1)
- Ted Talk Reflection 1Dokument3 SeitenTed Talk Reflection 1api-242138662Noch keine Bewertungen
- Gene TherapyDokument36 SeitenGene TherapySukesh Potla100% (2)
- Cerebellar LesionsDokument3 SeitenCerebellar LesionsMary100% (1)
- NCP - FatigueDokument3 SeitenNCP - Fatigueitsmeaya100% (1)
- Argumentative Essay 1Dokument5 SeitenArgumentative Essay 1api-451529335Noch keine Bewertungen
- Directions: Each Question Below Contains Five Suggested Answers. Choose The One Best Response ToDokument3 SeitenDirections: Each Question Below Contains Five Suggested Answers. Choose The One Best Response ToTrottTamilNoch keine Bewertungen
- Quantitative Analysis of The Substrate Specificity of Human Rhinovirus 3C Protease and Exploration of Its Substrate Recognition MechanismsDokument14 SeitenQuantitative Analysis of The Substrate Specificity of Human Rhinovirus 3C Protease and Exploration of Its Substrate Recognition MechanismsLuís MiguelNoch keine Bewertungen
- HepatosplenomegalyDokument52 SeitenHepatosplenomegalySundar NatarajanNoch keine Bewertungen