Beruflich Dokumente
Kultur Dokumente
J Clin Pathol 2008 Edgar 988 93
Hochgeladen von
krimminal4802Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
J Clin Pathol 2008 Edgar 988 93
Hochgeladen von
krimminal4802Copyright:
Verfügbare Formate
Downloaded from jcp.bmj.com on February 28, 2014 - Published by group.bmj.
com
Review
T cell immunodeficiency
J D M Edgar
Correspondence to: J David M Edgar, Royal Hospitals, The Belfast Trust, Grosvenor Road, Belfast BT12 6BN, UK; david.edgar@ belfasttrust.hscni.net Accepted 16 May 2008
ABSTRACT T cell immunodeficiency can occur as one of a group of primary disorders or develop secondary to chronic infection, illness or drug therapy. Primary T cell disorders are rare, accounting for approximately 11% of reported primary immunodeficiencies, and generally present in infancy or early childhood. Early recognition is very important as many of these patients will require bone marrow transplantation prior to the onset of severe infection or other complications. Because of their rarity, these infants usually present to clinicians who have little or no prior experience of these conditions, and therefore laboratory-based clinicians with knowledge of the key laboratory/pathological abnormalities and clinical features have a valuable role in identifying the possibility of immunodeficiency. Secondary T cell deficiency is a cardinal feature of HIV infection and the specific susceptibility to infectious micro-organisms is highlighted. The possibility of T cell immunodeficiency should be considered in any patient presenting with unusual or severe viral, fungal or protozoal infection.
The purpose of this article is to alert clinicians in all pathology disciplines to the common clinical features and laboratory/pathological findings that should raise the possibility of T cell deficiency. Detailed molecular characterisation and extensive clinical management details of disorders are not included. T cells are lymphocytes that undergo post bone marrow maturation in the thymus and their major roles are in co-coordinating the immune response and fulfilling a cytotoxic function. Peripheral blood normally contains 7090% T cells, 510% B cells and approximately 110% natural killer (NK) cells. As T cells are the dominant type of lymphocyte in peripheral blood, it is to be expected that significant T cell deficiency frequently leads to total lymphopenia and this can be an important diagnostic clue. All T cells bear the CD3 surface antigen, which is associated on the cell surface with the T cell receptor. The two major T cell subsets are defined by the additional expression of either CD4 or CD8. CD8+ T cells are responsible for killing abnormal host cells (eg, virally infected, malignantly transformed or transplanted cells). CD4+ T cells provide signals and cytokines that are essential for effective B cell and macrophage activation, antibody production and the generation of effective CD8 T cell responses. T cell deficiency causes specific susceptibility to intracellular micro-organisms. These include mycobacteria, Salmonella, Listeria, Toxoplasma and other viral, fungal and protozoal diseases. Non-pathogenic micro-organisms such as the vaccine strain of mycobacterium (BCG) and other opportunistic infections such as Pneumocystis carinii/jirovecii can
988
also cause disease in severe T cell immune deficiency. Therefore, patients suffering from recurrent or severe infection with any of these micro-organisms should have T cell deficiency included in their differential diagnosis.1 2 In addition to defects of their cytotoxic function, there may also be defects in the co-coordinating role of T cells in the immune response. It is not surprising that primary defects in T cell function commonly give rise to secondary effects on antibody production, macrophage function and immunoregulation. Discrete combined B and T cell immunodeficiency syndromes also occur, and T cell disorders may be a part of wider developmental syndromes or conditions in which cellular repair mechanisms are disordered.3 4 As these are all uncommon conditions, they often present to clinicians who have no prior experience of diagnosing immune deficiency. Guidance on recognition of primary immunodeficiency by non-specialists has recently been published,1 2 and further assistance can be obtained using an online diagnostic tool.5 Laboratory-based clinicians, with knowledge of the characteristic clinicopathological features of primary immunodeficiency are therefore uniquely placed to assist colleagues in the recognition of these important disorders.
PRIMARY T CELL IMMUNODEFICIENCY
Primary immunodeficiency syndromes are usually the result of single gene disorders or other maturational abnormalities that typically result in a defective immune system from early in life. Specific T cell disorders account for approximately 11% of primary immunodeficiencies6 and detailed descriptions of diagnostic criteria,3 and classification and nomenclature4 are available. New primary immunodeficiencies and disease-related genes continue to be described.7 The most common forms and their characteristic presentations are summarised here.
Severe combined immune deficiency
Severe combined immune deficiency (SCID) comprises a group of disorders characterised by severe T cell deficiency, with or without abnormal B cell differentiation.3 4 SCID may be caused by reticular dysgenesis in which both myeloid and lymphoid cell lines are affected, or it may be caused by specific deficiencies affecting lymphocytes (eg, X linked SCID; Online Mendelian Inheritance in Man (OMIM) #300400). Most of these affect the development of lymphoid stem cells into pre T cells (fig 1). The major subtypes of SCID, their characteristic lymphocyte profile and underlying causes are listed in table 1. There may be a family history of unexplained infant deaths. Autosomal
J Clin Pathol 2008;61:988993. doi:10.1136/jcp.2007.051144
Downloaded from jcp.bmj.com on February 28, 2014 - Published by group.bmj.com
Review
recessive variants occur much more commonly in consanguineous partnerships and therefore family relationships should be clarified. While there are an increasing number of different genetic causes, the major clinical features are common to all types. SCID typically presents early (in the first weeks and months of life) with a history of failure to thrive, oral candidiasis, unexplained diarrhoea, interstitial pneumonitis and other recurrent bacterial, viral, fungal or protozoal infection. Hepatosplenomagaly may be a feature. Specific micro-organisms commonly encountered include P carinii/jirovecii and Aspergillus species. Certain micro-organisms, when detected, are associated with particularly poor prognosis in babies with SCID; these include respiratory syncytial virus, parainfluenza viruses, Listeria, Legionella, Epstein-Barr virus (EBV) and cytomegalovirus (CMV). Live vaccines, particularly BCG can cause disseminated disease. Typically there is profound hypoplasia of secondary lymphoid organs and the thymus is abnormal with absence of the lymphoid component and failure of normal epithelial differentiation. There may be no Hassals corpuscles. Unexplained lymphopenia is often present and may be the first detected abnormality. A lymphocyte count ,2.86109/l in an infant should always prompt investigation for immune deficiency8; however total lymphocyte counts may be misleadingly normal in B cell positive variants of SCID, T cell activation deficiencies and graft versus host disease (GVHD). If SCID is suspected, lymphocyte subset analysis is essential to determine the percentage and absolute T, B and NK cell numbers. This provides valuable information as to the most likely underlying defect at presentation (table 1). Confirmation of the specific molecular defect is usually undertaken during the detailed investigation, prior to transplantation. Serum immunoglobulin is usually very low and isohaemagglutinins absent; however transplacentally acquired maternal IgG may mask this feature in the early weeks of life. Neonatal screening for SCID using T cell lymphopenia in dried blood spots has been proposed but not yet adopted.9 Incidence of SCID is not well defined, but a recent Australian study suggested that classical SCID occurred in one in every 69 000 live births.10 GVHD in SCID typically presents as jaundice, beginning after the first 2 weeks of life, rash affecting the palms and soles of the feet, diarrhoea and deranged liver function. Early GVHD is caused by materno-fetal transfusion of maternal lymphocytes
to the infants circulation in the perinatal period. These cells proliferate within the circulation and while low maternal cell numbers may be asymptomatic, 3040% of cases are symptomatic. GVHD may alternatively occur late, as a complication of blood transfusion with non-irradiated blood. In transfusion related GVHD, symptoms begin 24 weeks after transfusion; however the outlook is much worse, with most cases proving fatal. The diagnosis of SCID is a paediatric emergency and once the diagnosis is suspected the priority is to stabilise the infants clinical condition and transfer them swiftly to an appropriate tertiary paediatric bone marrow transplant unit. Long-term outlook in SCID is directly related to speed of diagnosis and successful bone marrow transplantation prior to the onset of severe infection or other complications. Stem cell transplantation has proven successful11 and further success has been achieved in the use of somatic gene therapy for both adenosine deaminase (ADA)-SCID (OMIM *608958) and X linked SCID.12 Although limited in scale to date, and complicated by the development of lymphoproliferative disease in a percentage of cases, it is likely that the use of gene therapy will continue to increase in these disorders. The need for rapid diagnosis and treatment of SCID make it imperative that when hypogammaglobulinaemia, lymphopenia, deranged liver function, hypoplastic lymphoid tissue or histological features of GVHD are identified in the first year of life, the possibility of SCID is considered and the case discussed with a local immunologist.
X linked lymphoproliferative syndrome
X linked lymphoproliferative syndrome (XLP; Duncan/Purtilo syndrome; OMIM #308240) is characterised by fulminant infectious mononucleosis, lymphoma and/or dysgammaglobulinaemia. It is usually only identified after the affected boys have become infected with EBV.13 14 The condition is inherited in an X linked recessive manner and the defective gene is identified as signalling lymphocyte-activation molecule associated protein (SAP/SH2-D1A) located at Xq25.15 16 Until EBV exposure, affected boys demonstrate no obvious signs of immune deficiency, in particular they have no excess of viral or fungal infections. EBV infection has severe consequences for them with severe hepatitis, lymphohistiocytic activation and bone marrow failure. They may then develop B cell lymphoma (NB, the cell surface receptor for EBV (CD21) is B cell specific) and/or severe hypogammaglobulinaemia, which may be fatal. Typically they do not mount a detectable antibody response to EBV nuclear antigen, or occasionally virus capsid antigen and early antigen. Early identification of EBV infection by PCR, lymphocyte subset analysis and screening for SAP expression are all essential in confirmation of the diagnosis. Affected boys require bone marrow transplantation, and therefore it is imperative that they are appropriately identified.
X linked immune deficiency with associated hyper IgM
Hyper IgM syndrome (OMIM #308230) describes a group of conditions in which low serum IgG is typically and paradoxically associated with high serum IgM. These disorders reflect a failure of class switching of the humoral immune response (ie, in response to infectious stimuli, IgM is produced normally; however this does not progress to the normal production of antigen-specific IgG). Switching to IgA and IgE production is also usually defective. The most common underlying defect is abnormal expression of the T cell surface antigen CD40 ligand
989
Figure 1 T cell development and the stages at which primary and secondary immune deficiencies affect development or function. Purine nucleoside phosphorylase (PNP) deficiency, A-T and HIV infection all affect mature, normally developed T cells. ADA, adenosine deaminase; BM, bone marrow; MHC, major histocompatibility complex; X-SCID, X linked severe combined immune deficiency.
J Clin Pathol 2008;61:988993. doi:10.1136/jcp.2007.051144
Downloaded from jcp.bmj.com on February 28, 2014 - Published by group.bmj.com
Review
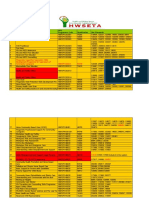
Table 1 Common forms of severe combined immune deficiency (SCID), their relative frequency, lymphoid cellular phenotype, mode of inheritance and underlying molecular lesions
Disease Reticular dysgenesis Alymphocytosis T cell deficiency Relative frequency ,1% 10% 10% 50% 10% 1% ,1% ,1% 1020% ,1% Deficient cells Leukocytes, platelets, B, T and NK cells T and B cells T and B cells T and NK cells T and NK cells T cells T cells T cells T, B and NK cells Progressive loss of T cells Inheritance AR AR AR XL AR AR AR AR AR AR Molecular lesion/deficiency Unknown RAG1/RAG2 DCLRE1C (Artemis) IL-2R common c chain JAK-3 IL-7Ra CD45 CD3d/CD3e Adenosine deaminase deficiency Purine nucleoside phosphorylase
ADA deficiency PNP deficiency
ADA, adenosine deaminase; AR, autosomal recessive; NK, natural killer; PNP, purine nucleoside phosphorylase; XL, X linked.
(CD40L/CD154) on activated T cells. This prevents T cells delivering essential signals to IgM-producing B cells (that express CD40) that would allow them to differentiate into IgG-producing plasma cells. The gene is located at Xq2627 and molecular confirmation of diagnosis and carrier status is possible. Other molecular variants exist (eg, OMIM 608184, #608186) but the clinical phenotype is reasonably consistent.17 18 Serum levels of IgG are usually less than 3 g/l but IgM levels may be up to 10 g/l (normally ,3 g/l). Associated with this failure of class switching, lymph node architecture is abnormal with failure/hypoplasia of germinal centres Affected boys (or occasionally adults) present with recurrent pyogenic infections or typically with P carinii/jirovecii pneumonia in early infancy. Neutropenia is common but T cell numbers and proliferative response to mitogens are normal. Affected boys have an increased susceptibility to Cryptosporidium infection which, in the long term, causes ascending cholangitis and chronic liver impairment. There is also an increased incidence of malignancy, particularly lymphoma and a range of autoimmune diseases. Once identified, commencement of immunoglobulin replacement therapy is very effective in preventing infection and usually results in normalisation of serum IgM and neutrophil counts. The particular susceptibility of those patients to P carinii/jirovecii pneumonia is an indication for primary/secondary prophylaxis with oral co-trimoxazole. However because of the susceptibility to progressive liver disease, malignancy and a range of autoimmune disorders, allogeneic bone marrow transplantation (usually before the age of 5 years) is the definitive treatment. In older patients with established liver disease, combined liver and bone marrow transplantation may be considered.
The DiGeorge syndrome
DiGeorge syndrome (OMIM #188400), first described in the 1960s, is associated with a developmental abnormality of the third and fourth branchial arches. The clinical features of the fully expressed syndrome consist of (i) abnormal facies with low-set ears, fish-shaped mouth, hypertelorism, notched ear pinnae, micrognathia and a downward slant of the eyes; (ii) hypoparathyroidism (often presenting with neonatal hypocalcaemic tetany); (iii) congenital heart disease (particularly aortic arch defects: truncus arteriosus, interrupted arch or Fallots tetralogy); and (iv) cellular immune deficiency. The diagnosis
990
may therefore be first suspected in a wide range of clinical settings or from the incidental finding of hypocalcaemia. Partial forms of the condition exist. The most common presentation is with congenital heart disease. Significant immune deficiency is probably only present in a minority of cases and, interestingly, immune function in those children usually improves with time. Guidance on assessing the degree of immune deficiency is available.3 The occurrence of autoimmune disease in DiGeorge syndrome is increasingly recognised and may reflect abnormalities of T cell regulatory function.19 In very severe cases, the clinical presentation may be similar to SCID; however in such cases thymic transplant rather than bone marrow transplant is the treatment of choice.20 DiGeorge syndrome is now recognised a one of a group of related disorders that share a common genetic lesion. This is usually a deletion at 22q11 and the group of conditions is referred to as the CATCH 22 syndrome: (i) cardiac anomalies, (ii) abnormal facies, (iii) thymic hypoplasia, (iv) cleft palate and (v) hypocalcaemia.21 22 Other clinical syndromes that are within the broader CATCH 22 group include Velocardiofacial syndrome, Kallman syndrome and Schprintzen syndrome. The CHARGE syndrome (ocular coloboma, heart defects, atresia of choanae, growth retardation, genital abnormalities and ear abnormalities) (OMIM #214800) has some overlap in clinical features although the genetic defect is distinct. There may be B and T cell deficiency in CHARGE syndrome; however the T cell deficiency may be severe and the presentation very similar to DiGeorge syndrome.23 24 Diagnosis is based on the typical morphological features associated with recurrent viral or fungal infections such as oral and perineal candidiasis or viral pneumonia. Chest x ray may confirm an absent thymic shadow with abnormal cardiac outline. It is usual to find a reduced number of circulating T cells, but the degree of immunological deficiency is variable and is probably only significant in approximately 20% of cases identified by other criteria. Lymphocyte proliferation in response to mitogens (phytohaemagglutinin and phorbol myristate acetate) may be reduced. Antibody deficiency is rare. The chromosome 22q11 lesion is detectable by fluorescent in situ hybridisation (FISH). However as the range of clinical associations of 22q11 lesions is wide and the degree of immunodeficiency variable, the simple demonstration of a 22q11 deletion does not necessarily imply that there is clinically important immune deficiency.
J Clin Pathol 2008;61:988993. doi:10.1136/jcp.2007.051144
Downloaded from jcp.bmj.com on February 28, 2014 - Published by group.bmj.com
Review
Chronic mucocutaneous candidiasis
Chronic mucocutaneous candidiasis (CMC) is a rare condition that affects both men and women and presents with chronic candidal infection of skin and mucous membranes.25 It is believed to reflect a specific inability of T cells to respond to Candida antigens, and there is no generalised susceptibility to other viral, fungal or protozoal antigens. The condition may be inherited as an autosomal recessive (OMIM %212050) or more commonly a dominant trait (OMIM %114580). There may be an associated autoimmune endocrine deficiency, the endocrine features of which may precede the immune deficiency (type 1: autoimmune polyendocrinopathy candidiasis ectodermal dysplasia (APECED)) (OMIM #240300). The abnormal gene, termed autoimmune regulator, is located at 21q22.3. It is thought to have a normal role in modulating gene transcription.26 Patients affected by APECED have at least two of the following features: Addison disease, hypoparathyroidism or mucocutaneous candidiasis, and they may also have alopecia, vitiligo, ovarian failure, hypothyroidism, enamel hypoplasia or nail dystrophy. Investigation of such patients usually reveals normal numbers of T cell subsets and responses to non-specific mitogens but a specific failure of proliferative response to Candida antigens. Type II autoimmune polyendocrine syndrome involves Addison disease, autoimmune thyroid disease and type 1a diabetes; it is inherited as an autosomal dominant, but is not typically associated with immunodeficiency. It should be noted that heterozygotes for ATM gene mutations have an increased risk of developing a number of malignancies. ATM mutations are confirmed as breast cancer susceptibility alleles. Appropriate screening of family members (and other carriers) should be considered.30
Nijmegen breakage syndrome
Nijmegen breakage syndrome (OMIM #251260) is a very rare syndrome that is similar in some respects to AT but does not share the cardinal signs of ataxia or telangectasia formation and is genetically distinct. Similar chromosomal rearrangement occurs in T cells and there is impaired DNA repair following irradiation.29 Patients have microcephaly and developmental retardation. The immunodeficiency is more severe than in AT, with panhypogammaglobulinaemia, profound T cell cytopenia and reduced T cell responses to mitogens and antigens. Lymphoma development is very common in childhood.
Other rare T cell deficiencies
Several other rare conditions exist in which T cell immunity is impaired. These include (i) short limb dwarfism/cartilage hair hypoplasia (OMIM #250250), a condition most commonly reported in Finland and the Old Order Amish group in the USA; (ii) immunodeficiency, centromeric instability and facial anomalies (ICF) syndrome (OMIM #242860) is an autosomal recessive disorder characterised by facial abnormalities (micrognathia, hypertelorism, flat nasal bridge and epicanthic folds), mental retardation, malabsorption and failure to thrive; (iii) metabolic disorders including orotic aciduria (OMIM +258900), methionine synthetase deficiency and biotin-dependent multicarboxylase deficiency may all have T cell deficiency as part of their clinical presentation.3 4
NK cell deficiency
NK cells are not truly T cells as they do not express CD3. NK deficiency (OMIM #609981) is reported in the literature but is very rare in clinical practice.27 Patients have an increased susceptibility to herpes viruses including CMV and EBV. NK cells numbers are usually profoundly depressed.
SECONDARY T CELL IMMUNODEFICIENCY
Secondary immunodeficiency is a much more common phenomenon than primary immunodeficiency. Common causes of secondary immunodeficiency include drugs (eg, corticosteroids, cytotoxics, etc), infection (HIV, EBV, malaria etc), malignancy, (lymphoproliferative disease), malnutrition, and systemic disease (malignancy, diabetes, liver/renal failure). There are often multiple immunological mechanisms underlying secondary immune defects and it can therefore be difficult to demonstrate and quantify the degree of immunodeficiency by routine immunological laboratory testing. An important exception to this statement is however T cell deficiency resulting from HIV infection.
Ataxia telangectasia
Ataxia telangectasia (AT; OMIM #208900) is a progressive neurological and immunological disorder that is inherited in an autosomal recessive manner and usually presents in early childhood. Presenting features include cerebellar ataxia, nystagmus and oculomotor dyspraxia.28 Telangiectases are typically seen on the elbows, conjunctivae and ear lobes. Onset is typically gradual and therefore diagnosis can be delayed. The fundamental lesion is defective DNA repair caused by mutations in the protein kinase ataxia telangiectasia mutated (ATM) gene. This leads to increased radiosensitivity (as in other disorders, eg, Bloom syndrome, xeroderma pigmentosa, Nijmegen breakage syndrome).29 Chromosomal breaks, inversions and translocations are commonly seen at the T cell receptor and immunoglobulin gene complexes on chromosomes 7 and 14 respectively. The serum a-fetoprotein is often raised. There is a progressive, combined, immune defect that is variable in its immunological features. Peripheral blood T cell counts fall progressively, the thymus is often markedly hypoplastic and T cell cytotoxicity is impaired. The clinical manifestation of immune deficiency is usually mild and some patients require no preventative therapy. However many will require immunoglobulin replacement and some prophylactic antiviral and fungal agents. Patients ultimately develop lymphoid leukaemia/lymphoma in the second and third decades and this, with progressive combined immune deficiency, is the usual cause of death.
J Clin Pathol 2008;61:988993. doi:10.1136/jcp.2007.051144
HIV infection
HIV-1 and -2 express the surface protein gp120, which specifically binds to cell surface CD4 and thus HIV specifically infects and depletes T helper cells and macrophages/monocytes (which also express CD4). The importance of CD4 cells as central coordinators of the immune response is nowhere more evident than in HIV-related disease. As CD4 cells are lost, a profound immunodeficiency results with particular susceptibility to viral, fungal and other opportunistic pathogens. The relationship between the CD4 cell count and susceptibility to particular micro-organisms is well defined (fig 2).31 Interestingly, some coexistent autoinflammatory disorders (eg, psoriasis) improve in individual patients as CD4 counts fall. While acute infection with HIV is usually unnoticed, an acute seroconversion illness characterised by fever and flu-like symptoms may occur. Approximately 30% of patients develop persistent
991
Downloaded from jcp.bmj.com on February 28, 2014 - Published by group.bmj.com
Review
generalised lymphadenopathy (enlarged lymph nodes in two or more non-contiguous sites) prior to the development of AIDS.
CONCLUSION
It is clear that a wide range of clinical features and pathological findings may indicate the presence of an underlying T cell deficiency. Many of these patients will require urgent treatment and delay in diagnosis can have a very significantly adverse effect on prognosis. The role of the clinical pathologist in raising immunodeficiency as a possible differential diagnosis can play an important part in ensuring prompt accurate diagnosis and ultimately an improved patient outcome.
Acquired immunodeficiency syndrome
The definition of AIDS has developed over time but is generally accepted to have occurred if an HIV-positive patient develops one or more of a number of indicator infections or malignancies. The most common presenting conditions in the UK are P carinii/jirovecii pneumonia, oesophageal candidiasis, cytomegalovirus retinitis, Mycobacterium avium intracellulare infection, Kaposi sarcoma (caused by human herpes virus 8), central nervous system and other lymphomas (often EBV associated), or squamous cell carcinoma of the rectum or cervix. To date, approximately 25 million people are thought to have died of AIDS worldwide.32 The identification of any of the conditions in a patient not known to be HIV positive should therefore prompt clinicians to undertake further assessment. This should begin with a careful clinical history that identifies risk factors for infection and/or symptoms consistent with HIV infection. Focussing on highrisk groups alone is inappropriate as the epidemiology of the condition has changed significantly. HIV infection must be considered in all patients with unexplained illness irrespective of age, ethnicity, gender or sexual orientation. Unfortunately, it is all too common for such individuals to be investigated extensively for a variety of other illnesses before HIV infection is recognised. It is important to stress that if HIV is suspected, the measurement of T cell subsets is inappropriate until results of HIV antibody tests are known. Isolated CD4 counts and CD4:CD8 cell ratios are not a substitute for such testing.
Take-home messages
c
Drug-induced T cell immunodeficiency
Drug-induced immunodeficiency is a predictable side effect of a range of medications in common usage for malignant and inflammatory disorders. Immunodeficiency may result from non-specific bone marrow suppression or specific interference with T cell function. The major drugs implicated include corticosteroids, cytotoxic (cyclophosphamide), antimetabolite (methotrexate), antiproliferative (azathioprine, mycophenolate mofetil) and anti-T cell activation (ciclosporin, tacrolimus) drugs. Well-established protocols are available for the monitoring of patients taking these drugs, including regular lymphocyte counts, but it is crucial that the possibility of significant immune deficiency is considered should they present with symptoms of unusual infection or pyrexia of unknown origin. The ever increasing use of biological agents including cytokines, anticytokines and other monoclonal antibody therapies should be kept under review for their potential immunosuppressive side effects.
T cell immunodeficiency typically manifests as recurrent viral, fungal or protozoal infection. Primary T cell immunodeficiencies commonly present in early childhood. Infants of consanguineous parents are at greater risk of autosomal recessive disorders. If severe combined immune deficiency (SCID) is suspected, avoid all live vaccines (eg, BCG) and ensure any blood products are irradiated and cytomegalovirus negative. All infants with total lymphocyte count ,2.86109/l should be investigated for SCID. Infants with recurrent infection, with or without failure to thrive, and with or without hypogammaglobulinaemia, should be investigated for SCID. Normal total lymphocyte count, lymphocyte subsets and serum immunoglobulin virtually outrules SCID. If HIV infection is suspected, ensure appropriate viral antibody and PCR studies are undertaken. In the face of unusual infection, consider if the patient is on long-term immunosuppressive therapy that may require modification.
Competing interests: None.
REFERENCES
1. Sewell WAC, Khan S, Dore PC. Early indicators of immunodeficiency in adults and children: protocols for screening for primary immunological defects. Clin Exp Immunol 2006;145:2013. De Vries E. For the Clinical Working Party of the European Society for Immunodeficiencies (ESID). Patient-centred screening for primary immunodeficiency: a multi-stage diagnostic protocol designed for non-immunologists. Clin Exp Immunol 2006;145:20414. Conley ME, Notarangelo LD, Etzioni A. Diagnostic criteria for primary immunodeficiencies. Clin Immunol 1999;93:1907. Geha RS, Notarangelo LD, Casanova JL, et al. Primary immunodeficiency diseases: an update from the International Union of Immunological Societies Primary Immunodeficiency Diseases Classification Committee. J Allergy Clin Immunol 2007;120:77694. UK Primary Immunodeficiency Network. http://www.ukpin.org.uk (accessed 13 June 2008). Eades-Perner AM, Gathmann B, Knerr V, et al. The European internet-based patient and research database for primary immunodeficiencies: results 200406. Clin Immunol 2006;117:88396. Marodi L, Notarangelo LD. Immunological and genetic bases of new primary immunodeficiencies. Nature Rev 2007;7:85161. Hague RA, Rassam S, Morgan G, et al. Early diagnosis of severe combined immunodeficiency syndrome. Arch Dis Child 1994;70:2603. Huang H, Manton KG. Newborn screening for severe combined immunodeficiency (SCID): a review Front Biosci 2005;10:102439. Yee A, De Ravin SS, Elliot E, et al. Severe combined immunodeficiency: A national surveilance study. Pediatr Allergy Immunol 2008;19:298302. Slatter MA, Gennery AR. Umbilical cord stem cell transplantation for primary immunodeficiencies. Expert Opin Biol Ther 2006;6:55565. Cavazzana-Calvo M, Lagresle C, Hacein-Bey-Abina S, et al. Gene therapy for severe combined immunodeficiency. Annu Rev Med 2005;56:585602. Gilmour KC, Gaspar HB. Pathogenesis and diagnosis of X-linked lymphoproliferative disease. Expert Rev Mol Diagn 2003;3:54961.
2.
3. 4.
5. 6.
7. 8. 9. 10. 11. 12.
Figure 2 Correlation between declining CD4 (T4) count and the development of specific conditions in AIDS.
992
13.
J Clin Pathol 2008;61:988993. doi:10.1136/jcp.2007.051144
Downloaded from jcp.bmj.com on February 28, 2014 - Published by group.bmj.com
Review
14. 15. 16. 17. 18. 19. 20. 21. 22. Nichols KE, Ma CS, Cannons JL, et al. Molecular and cellular pathogenesis of Xlinked lymphoproliferative disease. Immunol Rev 2005;203:18099. MacGinnitie AJ, Geha R. X-linked lymphoproliferative disease: genetic lesions and clinical consequences. Curr Allergy Asthma Rep 2002;2:3617. Engel P, Eck MJ, Terhorst C. The SAP and SLAM families in immune responses and X-linked lymphoproliferative disease. Nat Rev Immunol 2003;3:81321. Notarangelo LD, Lanzi G, Toniati P, et al. Immunodeficiencies due to defects of class-switch recombination. Immunol Res 2007;38:6877. Etzioni A, Ochs HD. The hyper IgM syndrome-an evolving story. Pediatr Res 2004;56:51925. McLean-Tooke A, Spickett GP, Gennery AR. Immunodeficiency and autoimmunity in 22q11.2 deletion syndrome. Scand J Immunol 2007;66:17. Markert ML, Alexieff MJ, Li J, et al. Postnatal thymus transplantation with immunosuppression as treatment for DiGeorge syndrome. Blood 2004:104:257481. Hong R. The DiGeorge anomaly. Clin Rev Allergy Immunol 2001;20:4360. Sergi C, Serpi M, Muller-Navia J, et al. CATCH 22 syndrome: report of 7 infants with follow up data and review of the recent advancements in the genetic knowledge of the locus 22q11. Pathologica 1999;9:16672. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. Writzl K, Cale CM, Pierce CM, et al. Immunological abnormalities in CHARGE syndrome. Eur J Med Genet 2007;50:33845. Sanlaville D, Verloes A. CHARGE syndrome: an update. Eur J Hum Genet 2007:15:38999. Lilic D. New Perspectives on the immunology of chronic mucocutaneous candidiasis. Curr Opin Infect Dis 2002;15:1437. Ruan QG, She JX. Autoimmune polyglandular syndrome type 1 and the autoimmune regulator. Clin Lab Med 2004;24:30517. Orange JS. Human natural killer cell deficiencies. Curr Opin Allergy Clin Immunol 2006;6:399409. Taylor AMR, Byrd PJ. Molecular pathology of ataxia telangiectasia. J Clin Path 2005;58:10915. Gennery AR. Primary immunodeficiency syndromes associated with defective DNA double-strand break repair. Br Med Bull 2006;7778:7185. Ahmed M, Rahman N. ATM and breast cancer susceptibility. Oncogene 2006;25:590611. Lloyd A. HIV infection and AIDS. P N G Med J 1996 Sep;39:17480. Greene WC. A history of AIDS: looking back to see ahead. Eur J Immunol 2007;37(Suppl 1):S94102.
Raising the quality of academic journals
The Committee on Publication Ethics (COPE) is a charity that works to promote ethical conduct in scientific research and its publication in science journals. It was founded in 1997 by a group of medical journal editors concerned about research and publication misconduct. It now has over 3500 members, including many major medical and scientific journals. Its main activity is to advise the editors of academic journals on how to handle cases of suspected research and publication misconduct. COPE is looking for new members to join its Council, which is responsible for the charitys policy and management. They will be expected to attend four meetings a year (in London) as well as take part in sub-committees and other COPE-related tasks. There are also occasional strategy meetings and an annual seminar to attend. Council members may also be asked to take responsibilities as trustees of the charity. This is a voluntary position. The initial term of office is three years, but members may be reappointed for a further term of three years. Applications from journal editors are particularly welcome. Further details can be found on the website: www.publicationethics.org.uk Those who are interested should send a short CV (no more than 4 pages) plus a covering letter stating what they can contribute to COPE Council. Please email to the COPE Administrator, Linda Gough (cope_administrator@publicationethics.org) or by post to Linda Gough, PO Box 39, Harleston, IP20 9WR, UK. The closing date for applications is 30 September 2008.
Registered Charity No 1123023 Registered in England and Wales Company No 6389120
J Clin Pathol 2008;61:988993. doi:10.1136/jcp.2007.051144
993
Downloaded from jcp.bmj.com on February 28, 2014 - Published by group.bmj.com
T cell immunodeficiency
J D M Edgar J Clin Pathol 2008 61: 988-993
doi: 10.1136/jcp.2007.051144
Updated information and services can be found at:
http://jcp.bmj.com/content/61/9/988.full.html
These include:
References
This article cites 29 articles, 2 of which can be accessed free at:
http://jcp.bmj.com/content/61/9/988.full.html#ref-list-1
Article cited in:
http://jcp.bmj.com/content/61/9/988.full.html#related-urls
Email alerting service
Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article.
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Principles of Immunochemical Techniques PDFDokument8 SeitenPrinciples of Immunochemical Techniques PDFdatitoxNoch keine Bewertungen
- Herpes Fact SheetDokument2 SeitenHerpes Fact SheetRebecca RichardsonNoch keine Bewertungen
- INFECTIONS IN DIALYSIS PATIENTS Basis & Prevention by Dr.T.V.Rao MDDokument48 SeitenINFECTIONS IN DIALYSIS PATIENTS Basis & Prevention by Dr.T.V.Rao MDtummalapalli venkateswara raoNoch keine Bewertungen
- Cholera Guidelines PresentationDokument17 SeitenCholera Guidelines PresentationhumphrangoNoch keine Bewertungen
- Counselling 101 For Kids 12 PDFDokument100 SeitenCounselling 101 For Kids 12 PDFShania SolomonNoch keine Bewertungen
- Chapter2 - Review of Related LiteratureDokument13 SeitenChapter2 - Review of Related LiteratureDiana Laura Lei57% (7)
- LymphomaDokument13 SeitenLymphomaRAJKUMARNoch keine Bewertungen
- Test List With Price Details For Web SiyeDokument11 SeitenTest List With Price Details For Web Siyeapi-172999234Noch keine Bewertungen
- Candida EsofagitisDokument5 SeitenCandida EsofagitisVina IsmawatiNoch keine Bewertungen
- PancharatnaDokument14 SeitenPancharatnajaynataNoch keine Bewertungen
- Skills Programme List 2016Dokument45 SeitenSkills Programme List 2016Christian Makande100% (1)
- Mind-Body Medicine - University of Maryland Medical CenterDokument17 SeitenMind-Body Medicine - University of Maryland Medical Centerjle_dlNoch keine Bewertungen
- FactSheet PseudomonasDokument3 SeitenFactSheet PseudomonasSmitha KollerahithluNoch keine Bewertungen
- Third Periodical Test in MAPEH 3 (Edited)Dokument5 SeitenThird Periodical Test in MAPEH 3 (Edited)kemsue1224Noch keine Bewertungen
- Eatern Equatoria State PresentationDokument24 SeitenEatern Equatoria State PresentationMayom MabuongNoch keine Bewertungen
- Thesis DoneDokument24 SeitenThesis DoneAmira SaidinNoch keine Bewertungen
- Abdul Wali Khan University, MardanDokument3 SeitenAbdul Wali Khan University, MardanMuhammad Ali ShahNoch keine Bewertungen
- Abdominal Pain: Right Upper AbdomenDokument4 SeitenAbdominal Pain: Right Upper AbdomenMohsin QayyumNoch keine Bewertungen
- Lymphatic SystemDokument70 SeitenLymphatic SystemNang Maizana Megat Yahya100% (1)
- "Beyond The Customary View" The Roles of Iddirs On Supporting Orphans Children's in EthiopiaDokument84 Seiten"Beyond The Customary View" The Roles of Iddirs On Supporting Orphans Children's in EthiopiaGetachew A.Noch keine Bewertungen
- WHO TRS 1003 Full-VersionDokument252 SeitenWHO TRS 1003 Full-VersionMechaheb MassinissaNoch keine Bewertungen
- NYCAHN Is Now VOCAL New York!Dokument3 SeitenNYCAHN Is Now VOCAL New York!VOCAL-NYNoch keine Bewertungen
- Question Bank For Mbbs Pediatrics: Long Essay - 20 MarksDokument17 SeitenQuestion Bank For Mbbs Pediatrics: Long Essay - 20 MarkspolluNoch keine Bewertungen
- CervikwqjqwnfpkqwnfpknasflkcnsalvknsdlbvowHT OIPHp93qn5evuhr92n38vicaqrfecal CancerDokument11 SeitenCervikwqjqwnfpkqwnfpknasflkcnsalvknsdlbvowHT OIPHp93qn5evuhr92n38vicaqrfecal CancerNicoh AvilaNoch keine Bewertungen
- 2nd Quarter Mapeh 10Dokument6 Seiten2nd Quarter Mapeh 10Donna VariasNoch keine Bewertungen
- Tratment of The Plaque-Induced GingivitisDokument10 SeitenTratment of The Plaque-Induced GingivitisPragita Ayu SaputriNoch keine Bewertungen
- Malawi 2009 STEPS Report PDFDokument131 SeitenMalawi 2009 STEPS Report PDFAnonymous 2oB60eU4Noch keine Bewertungen
- Bok 3A978 1 4614 5283 6 PDFDokument421 SeitenBok 3A978 1 4614 5283 6 PDFTeuku Akbar LazuArdiNoch keine Bewertungen
- Emerging Infectious Disease CDC 2016Dokument172 SeitenEmerging Infectious Disease CDC 2016Vera IndrawatiNoch keine Bewertungen
- Recombinant DNADokument6 SeitenRecombinant DNADiana Laura LeiNoch keine Bewertungen