Beruflich Dokumente
Kultur Dokumente
Extracorporeal Membrane Oxygenation For 2009 Influenza A (H1N1) Acute Respiratory Distress
Hochgeladen von
api-26851799Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Extracorporeal Membrane Oxygenation For 2009 Influenza A (H1N1) Acute Respiratory Distress
Hochgeladen von
api-26851799Copyright:
Verfügbare Formate
Extracorporeal Membrane Oxygenation for 2009
Influenza A(H1N1) Acute Respiratory Distress Syndrome
Online article and related content The Australia and New Zealand Extracorporeal Membrane Oxygenation
current as of October 13, 2009. (ANZ ECMO) Influenza Investigators
JAMA. published online Oct 12, 2009; (doi:10.1001/jama.2009.1535)
http://jama.ama-assn.org/cgi/content/full/2009.1535v1
Correction Contact me if this article is corrected.
Citations This article has been cited 1 time.
Contact me when this article is cited.
Topic collections H1N1 Influenza
Contact me when new articles are published in these topic areas.
Related Articles published in Critically Ill Patients With 2009 Influenza A(H1N1) in Mexico
the same issue Guillermo Domínguez-Cherit et al. JAMA. 2009;0(2009):20091536.
Critically Ill Patients With 2009 Influenza A(H1N1) Infection in Canada
Anand Kumar et al. JAMA. 2009;0(2009):20091496.
Preparing for the Sickest Patients With 2009 Influenza A(H1N1)
Douglas B. White et al. JAMA. 2009;0(2009):20091539.
Subscribe Email Alerts
http://jama.com/subscribe http://jamaarchives.com/alerts
Permissions Reprints/E-prints
permissions@ama-assn.org reprints@ama-assn.org
http://pubs.ama-assn.org/misc/permissions.dtl
Downloaded from www.jama.com by guest on October 13, 2009
CARING FOR THE JAMA-EXPRESS
CRITICALLY ILL PATIENT
Extracorporeal Membrane Oxygenation
for 2009 Influenza A(H1N1)
Acute Respiratory Distress Syndrome
The Australia and New Zealand
Context The novel influenza A(H1N1) pandemic affected Australia and New Zea-
Extracorporeal Membrane land during the 2009 southern hemisphere winter. It caused an epidemic of critical
Oxygenation (ANZ ECMO) Influenza illness and some patients developed severe acute respiratory distress syndrome (ARDS)
Investigators* and were treated with extracorporeal membrane oxygenation (ECMO).
I
N APRIL 2009, THE MEXICAN MIN- Objectives To describe the characteristics of all patients with 2009 influenza A(H1N1)–
istry of Health reported an in- associated ARDS treated with ECMO and to report incidence, resource utilization, and
patient outcomes.
crease in severe pneumonia cases
in young adults.1 The 2009 novel Design, Setting, and Patients An observational study of all patients (n=68) with
swine-origin influenza A(H1N1) vi- 2009 influenza A(H1N1)–associated ARDS treated with ECMO in 15 intensive care
units (ICUs) in Australia and New Zealand between June 1 and August 31, 2009.
rus was identified as its cause and rap-
idly led to a worldwide pandemic.2 This Main Outcome Measures Incidence, clinical features, degree of pulmonary dys-
pandemic began in the northern hemi- function, technical characteristics, duration of ECMO, complications, and survival.
sphere during late spring and early sum- Results Sixty-eight patients with severe influenza-associated ARDS were treated with
mer and appeared to decrease in inten- ECMO, of whom 61 had either confirmed 2009 influenza A(H1N1) (n=53) or influ-
sity within a few weeks.3 Shortly after, enza A not subtyped (n=8), representing an incidence rate of 2.6 ECMO cases per
at the start of the southern hemi- million population. An additional 133 patients with influenza A received mechanical
ventilation but no ECMO in the same ICUs. The 68 patients who received ECMO had
sphere winter, it spread to Australia and
a median (interquartile range [IQR]) age of 34.4 (26.6-43.1) years and 34 patients
New Zealand causing an approxi- (50%) were men. Before ECMO, patients had severe respiratory failure despite ad-
mately 8-fold greater number of con- vanced mechanical ventilatory support with a median (IQR) PaO2/fraction of inspired
firmed cases per head of population oxygen (FIO2) ratio of 56 (48-63), positive end-expiratory pressure of 18 (15-20) cm
than in the United States.4,5 H2O, and an acute lung injury score of 3.8 (3.5-4.0). The median (IQR) duration of
The spread of the virus to Australia ECMO support was 10 (7-15) days. At the time of reporting, 48 of the 68 patients
and New Zealand was also associated (71%; 95% confidence interval [CI], 60%-82%) had survived to ICU discharge, of
with a large number of patients admit- whom 32 had survived to hospital discharge and 16 remained as hospital inpatients.
Fourteen patients (21%; 95% CI, 11%-30%) had died and 6 remained in the ICU, 2
ted to intensive care units (ICUs) across
of whom were still receiving ECMO.
both countries.6 A proportion of these
patients presented with, or developed, Conclusions During June to August 2009 in Australia and New Zealand, the ICUs
severe acute respiratory distress syn- at regional referral centers provided mechanical ventilation for many patients with 2009
influenza A(H1N1)–associated respiratory failure, one third of whom received ECMO.
drome (ARDS). In some severe cases,
These young adults with severe hypoxemia had a 21% mortality rate at the end of
extracorporeal membrane oxygen- the study period.
ation (ECMO) was commenced for the JAMA. 2009;302(17):(doi:10.1001/jama.2009.1535) www.jama.com
treatment of refractory hypoxemia, hy-
percapnia, or both, which occurred de- tory failure, technical characteristics, *Authors/Management and Writing Committee and
spite mechanical ventilation and res- duration of extracorporeal support,
Investigators of the ANZ ECMO Influenza Investiga-
tors are listed at the end of this article.
cue ARDS therapies. complications, and survival in pa- Corresponding Author: Andrew R. Davies, MBBS,
We report herein on the incidence, tients with severe influenza-related FRACP, FJFICM, Intensive Care Unit, Alfred Hospi-
tal, Commercial Road, Melbourne, Victoria 3004, Aus-
clinical features, severity of respira- ARDS who were treated with ECMO. tralia (a.davies@alfred.org.au).
In addition, we discuss the relevance of Caring for the Critically Ill Patient Section Editor: Derek
See related article. C. Angus, MD, MPH, Contributing Editor, JAMA
our findings to the potential ECMO case (angusdc@upmc.edu).
©2009 American Medical Association. All rights reserved. (Reprinted) JAMA, Published online October 12, 2009 E1
Downloaded from www.jama.com by guest on October 13, 2009
EXTRACORPOREAL MEMBRANE OXYGENATION FOR INFLUENZA A(H1N1)
load in northern hemisphere coun- ["10 000/µL or "15% bands], C- ters during the winter of 2008 was ob-
tries during their 2009-2010 winter. reactive protein "3-fold the normal up- tained from each ICU’s registry of cases.
per limit, and a positive culture from
METHODS blood or pleural fluid). We identified Statistical Analysis
Study Design and Patient Eligibility the presumed infectious organism from Data analysis was descriptive using me-
We studied adult and pediatric pa- upper and lower respiratory tract speci- dian and interquartile range (IQR). We
tients who were treated with ECMO be- mens (polymerase chain reaction, vi- made no assumptions about missing
tween June 1 and August 31, 2009. We ral culture, or both), blood cultures, or data and adjusted proportions to the
contacted all 187 ICUs in Australia and urinary antigens obtained within the number of patients with available data.
New Zealand and identified the 15 ICUs first 72 hours of admission, or from con- When acute lung injury score vari-
that provided ECMO support during valescent or paired serology testing. ables were missing, the modified score
this period. We excluded neonates or We obtained information on the tim- was calculated (dividing the sum of sub-
patients treated with ECMO for pri- ing of endotracheal intubation in rela- scores by the number of known vari-
mary cardiac failure, following heart tion to presumed onset of symptoms ables). To report our findings rapidly,
and/or lung transplantation or cardiac and hospital admission, the total du- we censored all outcomes at midnight
surgery. We applied these eligibility cri- ration of mechanical ventilation, and on September 7, 2009. Using current
teria to capture all confirmed or strongly administration of antiviral and antibi- Australia and New Zealand popula-
suspected cases of 2009 influenza otic medications. We documented tion data,10,11 we calculated the inci-
A(H1N1)–related respiratory disease. whether the ECMO treatment was com- dence of ECMO use per million people
We also identified and excluded pa- menced in the participating hospital or for Australia and New Zealand in total,
tients with an alternative diagnosis and whether the patient was retrieved and and for each jurisdiction (Australian
who had no virus isolated. transferred while receiving ECMO from states and New Zealand) that pro-
All members of the binational a referral center. vided ECMO support. We also calcu-
management committee approved We assessed severity of illness be- lated the incidence of ECMO use for
the study protocol. Trained research fore endotracheal intubation by docu- confirmed as well as the combination
coordinators or treating clinicians menting respiratory rate and mea- of confirmed and suspected 2009 in-
used a case report form to obtain rel- sures of oxygenation. We assessed fluenza A(H1N1). We also estimated
evant data. Approval was obtained severity of illness before commence- the ECMO burden by calculating the
from the hospital research ethics ment of ECMO by documenting total number of days on which ECMO
committees at all participating cen- nonpulmonary vital organ support, se- was provided to all patients and by cal-
ters. All committees waived the need verity of hypoxemia, hypercapnia, ven- culating the total number of patients
for informed consent. tilator settings, and use of rescue ARDS treated concurrently in all hospitals in
therapies in the 6 hours before ECMO Australia and New Zealand for each day
Data Collection commencement. We also obtained data of the winter period.
We collected data retrospectively on pa- to calculate a modified acute lung in- Comparisons of proportions were
tient demographics including age, sex, jury score (range, 0-4) during this made using #2 tests for equal propor-
height, weight, and ethnicity, as well as period.9 tion or Fisher exact tests when num-
the presence of a number of pre- We recorded duration of mechani- bers were small. Continuous vari-
defined comorbidities. We assessed cal ventilation, ECMO, ICU and hos- ables were compared using Wilcoxon
whether patients fulfilled criteria dur- pital stay, mortality, and destination at rank sum tests. All reported P values
ing the period before or at the time of hospital discharge. Information on are 2-sided and were not adjusted for
presentation to hospital for an influen- functional status at hospital discharge multiple comparisons. P$.05 was
zalike illness based on typical symp- in survivors included whether the pa- considered statistically significant.
toms7 (defined as !3 symptoms of sore tient was ambulant and the pulse ox- Analysis was performed using SAS
throat, cough, myalgia or arthralgia, res- imetry reading on room air. In pa- version 9.1 (SAS Institute Inc, Cary,
piratory distress, vomiting or diar- tients who died during hospital North Carolina).
rhea, and core temperature "38°C). We admission, we characterized the mode
also assessed whether they fulfilled cri- of death from a list of predefined RESULTS
teria for community-acquired pneu- options. Patient Characteristics
monia8 (defined as presence of a new Data on demographics, comorbidi- and Use of ECMO
or progressive infiltrate on chest radio- ties, treatment, and outcome were col- Between June 1 and August 31, 2009,
graph plus !2 symptoms of cough, spu- lected on patients with confirmed in- 72 patients were treated with ECMO
tum production, core temperature fluenza A who were not treated with and fulfilled eligibility criteria for the
"38°C, auscultatory findings consis- ECMO in the same ICUs. The use of study in the 15 participating ICUs. Four
tent with pneumonia, leukocytosis ECMO for ARDS in the ECMO cen- patients were excluded from analysis
E2 JAMA, Published online October 12, 2009 (Reprinted) ©2009 American Medical Association. All rights reserved.
Downloaded from www.jama.com by guest on October 13, 2009
EXTRACORPOREAL MEMBRANE OXYGENATION FOR INFLUENZA A(H1N1)
because 3 patients had alternative di- compared with the 133 treated with me- 2.6 (95% confidence interval [CI], 2.0-
agnoses (Wegener granulomatosis, con- chanical ventilation but without ECMO 3.2) cases per million people. When
nective tissue disease, and cystic fibro- in TABLE 1. only confirmed cases were consid-
sis) and 1 patient had 2009 influenza The estimated incidence of ECMO ered, the estimated incidence was 2.0
A(H1N1)–associated fulminant myo- use for the combination of confirmed (95% CI, 1.4-2.6) cases per million. In
carditis without ARDS. and suspected 2009 influenza A(H1N1) the jurisdictions where patients were
For the remaining 68 patients who during the winter influenza season was treated, the estimated incidence of
received ECMO, the median (IQR) age
was 34.4 (26.6-43.1) years and 34 pa-
Figure 1. Flow Diagram of Patients Receiving Mechanical Ventilation for Suspected 2009
tients (50%) were men. The most com- Influenza A(H1N1) Infection at ECMO Centers
mon associated comorbidities were obe-
sity (body mass index "30, calculated 201 Patients given mechanical ventilation
for confirmed or suspected influenza
as weight in kilograms divided by height
in meters squared), asthma, and dia-
betes mellitus in 34 patients (50%), 19 68 Received ECMO 133 Did not receive ECMO
patients (28%), and 10 patients (15%),
respectively. Six patients (9%) were
pregnant and 4 patients (6%) were post- 61 Confirmed 2009 7 Had suspected but 133 Confirmed 2009
influenza A(H1N1) unconfirmed influenza influenza A(H1N1)
partum ($28 days of delivery). Three or influenza A not or influenza A not
children (aged $15 years) and no el- subtyped subtyped
derly patients (aged "65 years) re-
ceived ECMO.
53 Confirmed 2009 8 Confirmed influenza A 6 Alive 116 Alive
Of the 68 patients who received influenza A(H1N1) not subtyped 1 Still in ICU 11 Still in ICU
ECMO for influenza-associated ARDS, 42 Alive 6 Alive 1 Died 17 Died
4 Still in ICU 1 Still in ICU
66 (97%) fulfilled criteria for pneumo- 11 Died 2 Died
nia and 64 (94%) fulfilled criteria for a
preceding influenzalike illness. Fifty- ECMO indicates extracorporeal membrane oxygenation; ICU, intensive care unit.
three patients (78%) had 2009 influ-
enza A(H1N1) detected by polymer-
Table 1. Comparison of Patients With Influenza A Who Received ECMO and Those Who
ase chain reaction or viral culture and Received Mechanical Ventilation But Without ECMO at ECMO Centers a
8 patients (12%) had serological evi- Mechanical Ventilation
dence of recent influenza A that was not ECMO But Without ECMO P
subtyped and was regarded as sus- Parameter (n = 61) (n = 133) Value
pected to be 2009 influenza A(H1N1) Age, median (IQR), y 36 (27-45) 44 (31-54) .02
Male sex 29 (48) 63 (47) .54
(FIGURE 1). The remaining 7 patients
BMI, median (IQR) 29 (23-36) 29 (24-37) .92
(10%) had preceding symptoms of in-
Chronic lung disease 18 (30) 35 (26) .64
fluenzalike illness and were also re-
APACHE III comorbidity b 5 (8) 30 (23) .02
garded as having suspected 2009 in-
Pregnancy or postpartum 10 (16) 12 (9) .21
fluenza A(H1N1). Seasonal subtypes of
Diabetes mellitus 9 (15) 23 (17) .64
influenza A were not detected in any
H1N1 positive 56 (92) 107 (80) .05
patient. Nineteen (28%) patients also
At ICU admission
had a secondary organism isolated from Mechanical ventilation 53 (87) 117 (88) .80
a respiratory tract specimen or blood Vasopressor 35 (57) 46 (34) .02
sample at the time of hospital presen- Renal replacement therapy 5 (8) 9 (7) .95
tation, the most common being Strep- Duration or length of stay,
tococcus pneumoniae (n = 10) and median (IQR), d
Mechanical ventilation 18 (9-27) 8 (4-14) .001
Staphylococcus aureus (n = 4).
ICU 22 (13-32) 12 (7-18) .001
During the study period, 252 pa-
Hospital 28 (15-43) 20 (13-31) .07
tients were admitted to the 15 partici-
Mortality
pating ICUs with influenza. Of these pa- in ICU 14 (23) 12 (9) .01
tients, 201 received mechanical in hospital 14 (23) 17 (13) .06
ventilation. Of the 194 patients with Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; BMI, body mass index (calculated as weight in
kilograms divided by height in meters squared); ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit;
either confirmed 2009 influenza IQR, interquartile range.
a Data are presented as No. (%) unless otherwise specified.
A(H1N1) or influenza A not sub- b The presence or not of at least 1 comorbidity.
typed, 61 treated with ECMO were
©2009 American Medical Association. All rights reserved. (Reprinted) JAMA, Published online October 12, 2009 E3
Downloaded from www.jama.com by guest on October 13, 2009
EXTRACORPOREAL MEMBRANE OXYGENATION FOR INFLUENZA A(H1N1)
ECMO use varied from 1.6 (95% CI, ter-hospital transfer to the ECMO- were 1.0 (1.0-1.0), 18 (15-20) cm H2O,
1.1-2.1) to 5.3 (95% CI, 4.3-6.3) cases providing site; of these, 38 (78%) were 5.6 (4.6-6.7) mL/kg, and 36 (33-38) cm
per million for confirmed and sus- started on ECMO at the referring site H2O, respectively. All but 2 patients had
pected 2009 influenza A(H1N1). The and successfully transferred while re- a PaO2/FIO2 ratio of 83 or less, and both
total ECMO burden for the cohort was ceiving ECMO. of these had a PaCO2 of 98 or more and
828 days of ECMO (32; 95% CI, 30-34 a pH of 7.07 or less. All patients had
ECMO days per million). The number Severity of Illness and Treatment either a modified acute lung injury score
of patients treated concurrently with Before Commencement of of 3.0 or more, or the combination of
ECMO in Australia and New Zealand Mechanical Ventilation and ECMO hypercapnia and a pH of less than 7.2.
peaked 8 weeks after the first patient Median (IQR) duration of mechanical Representative images of a chest radio-
was treated and then decreased dur- ventilation before commencement of graph and a computed tomogram for
ing the next 4 weeks, with the maxi- ECMO was 2 (1-5) days. Before me- these patients are shown in FIGURE 3.
mum number of 23 patients (34%) on chanical ventilation, the median (IQR) In cases with available data before
3 consecutive days in early August respiratory rate, arterial oxygen satu- commencement of ECMO, clinicians
(FIGURE 2). In the previous winter ration (SaO2), and PaO2 were 44 (31- used rescue ARDS therapies such as re-
(June 1-August 31, 2008), only 4 pa- 48)/min, 83% (77%-88%), and 53 (47- cruitment maneuvers in 38 patients
tients (estimated incidence of 0.15 cases 60) mm Hg, respectively. Details of (67%), prone positioning in 12 pa-
per million people) received ECMO for severity of illness in the 6 hours be- tients (20%), high-frequency oscilla-
ARDS in participating sites. fore ECMO commencement are shown tory ventilation in 3 patients (5%), in-
The median (IQR) interval between in TABLE 2. Overall, patients had a me- haled nitric oxide in 20 patients (32%),
the onset of influenzalike symptoms dian (IQR) lowest PaO2/fraction of in- or prostacyclin in 14 patients (22%).
and hospital admission, ICU admis- spired oxygen (FIO2) ratio of 56 (48- Overall, 55 patients (81%) received at
sion, and ECMO was 5 (3-6) days, 5 63), a lowest pH of 7.2 (7.1-7.3), a least 1 of these therapies. Further-
(3-7) days, and 9 (5-13) days, respec- highest PaCO2 of 69 (54-83) mm Hg, more, 46 patients (68%) received va-
tively. Oseltamivir (administered en- and a modified acute lung injury score soactive drugs and 16 patients (24%)
terally) was used as initial antiviral treat- of 3.8 (3.5-4.0). The median (IQR) received renal replacement therapy be-
ment in 64 patients (94%) for a median highest recorded FIO2, positive end- fore commencement of ECMO. Pa-
(IQR) duration of 8 (7-11) days. Forty- expiratory pressure, tidal volume (per tients with secondary bacterial infec-
nine of 68 patients (72%) who re- kg body weight), and peak airway pres- tion at the time of hospital presentation
ceived ECMO required retrieval and in- sure before ECMO commencement (n=19) were more likely to receive va-
Figure 2. Histogram of Number of Concurrent Patients Receiving ECMO Across Australia and New Zealand in 2009
25
20
15
No. of Patients
10
0
9 11 13 15 17 19 21 23 25 27 29 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 1 3 5 7
Jun Jul Aug Sep
Date
ECMO indicates extracorporeal membrane oxygenation.
E4 JAMA, Published online October 12, 2009 (Reprinted) ©2009 American Medical Association. All rights reserved.
Downloaded from www.jama.com by guest on October 13, 2009
EXTRACORPOREAL MEMBRANE OXYGENATION FOR INFLUENZA A(H1N1)
soactive drugs (90% vs 59%, respec- sion and hospitalization were 27 (16- ECMO, 1 had died and 52 (76%)
tively; P = .01). 37) and 39 (23-47) days, respectively. were still alive. Of the 52 patients still
Of the 68 patients, 53 (78%; 95% alive and weaned from ECMO, 4 were
Technical Details of ECMO Support CI, 68%-88%) had been weaned from still in the ICU and 48 (71%; 95% CI,
All centers provided ECMO with cen- ECMO, 13 had died while receiving 60%-82%) had survived to ICU dis-
trifugal blood pump driven circuit flow ECMO, and the other 2 were still charge. Of the 48 ICU survivors, 16
and polymethylpentene low-resis- receiving ECMO as of September 7, patients (24%; 95% CI, 13%-34%)
tance oxygenators. The initial mode of 2009. Of the 53 patients weaned from were still in the hospital and 32
ECMO was veno-venous in 63 pa-
tients (93%) and veno-arterial in 5 pa- Table 2. Severity of ARDS Before Commencement of ECMO
tients (7%). No arteriovenous (pump- 2009 Influenza A(H1N1)
less) support was used. The median
(IQR) duration of ECMO support was Confirmed Suspected
Infection Infection All Infections
10 (7-15) days. Median (IQR) circuit Characteristics (n = 53) (n = 15) (N = 68)
blood flow at 4 and 24 hours was 4.9 Ventilation parameters, median (IQR)
(4.0-5.9) and 4.9 (3.9-6.0) L/min, Lowest PaO2/FIO2 ratio 55 (48-65) 57 (45-62) 56 (48-63)
respectively. Highest FIO2 1.0 (1.0-1.0) 1.0 (1.0-1.0) 1.0 (1.0-1.0)
Highest PEEP, cm H2O 18 (15-20) 15 (14-18) 18 (15-20)
All adult patients had vascular can-
Highest peak airway pressure, 36 (34-40) 34 (29-36) 36 (33-38)
nulae inserted through a peripheral ap- cm H2O
proach into the femoral, jugular, or both Lowest pH 7.2 (7.1-7.3) 7.2 (7.1-7.3) 7.2 (7.1-7.3)
vessels, and 1 child had central cannu- Highest PaCO2, mm Hg 69 (54-86) 67 (61-73) 69 (54-83)
lae. In 33 patients (49%), a second ac- Highest tidal volume, mL/kg 5.6 (4.8-6.6) 5.7 (4.4-6.7) 5.6 (4.6-6.7)
cess cannula was needed to augment Quadrants of radiograph 4 (4-4) 4 (4-4) 4 (4-4)
ECMO support. Hemorrhagic compli- infiltrate, No.
cations occurred in 37 patients (54%) Acute lung injury score a 3.8 (3.3-4.0) 3.5 (3.3-3.8) 3.8 (3.5-4.0)
during ECMO therapy, with the most Pneumothorax pre-ECMO, No. (%) 9 (17) 1 (7) 10 (15)
common sources being ECMO cannu- Rescue ARDS therapies used, No. (%)
Recruitment maneuver 30 (66) 8 (66) 38 (67)
lation sites in 15 patients (22%), gas-
Prone positioning 11 (22) 1 (8) 12 (20)
trointestinal tract in 7 patients (10%),
High-frequency oscillation 3 (6) 0 3 (5)
respiratory tract in 7 patients (10%),
Nitric oxide 19 (38) 1 (8) 20 (32)
vaginal bleeding in 6 patients (9%), and
Prostacyclin 12 (23) 2 (15) 14 (22)
intracranial hemorrhage in 6 patients Abbreviations: ARDS, acute respiratory distress syndrome; ECMO, extracorporeal membrane oxygenation; FIO2, frac-
(9%). tion of inspired oxygen; IQR, interquartile range; PEEP, positive end-expiratory pressure.
a Data were missing in 4 cases for PaO /FIO ratio, in 4 cases for PEEP, in 17 cases for lung compliance, and in 5 cases
The median (IQR) amount of blood 2
for quadrants of radiograph infiltrate.
2
administered per patient was 1880
(904-3750) mL. Infective complica- Figure 3. Chest Radiograph and Computed Tomogram of 2 Patients Successfully Treated
tions occurred in 42 patients (62%) dur- With ECMO for Confirmed 2009 Influenza A(H1N1)
ing ECMO therapy, with the most com-
mon sites being respiratory tract in 30 Chest radiograph Computed tomogram
patients (44%), bloodstream in 14 pa-
R L R L
tients (21%), non-ECMO catheter-
related in 13 patients (19%), and ECMO
cannulae-related in 7 patients (10%).
Details of ICU Support
and Outcomes for Patients
Requiring ECMO
The median (IQR) duration of mechani-
cal ventilation was 25 (13-34) days (26
[14-34] and 14 [7-29] days for survi-
vors and nonsurvivors, respectively)
(T ABLE 3). Tracheostomy was per-
formed to assist weaning from mechani-
cal ventilation in 39 patients (57%). The ECMO indicates extracorporeal membrane oxygenation. The images demonstrate severe bilateral airspace dis-
ease with massive loss of normal aerated lung tissue.
median (IQR) durations of ICU admis-
©2009 American Medical Association. All rights reserved. (Reprinted) JAMA, Published online October 12, 2009 E5
Downloaded from www.jama.com by guest on October 13, 2009
EXTRACORPOREAL MEMBRANE OXYGENATION FOR INFLUENZA A(H1N1)
patients (47%; 95% CI, 35%-59%) influenza A(H1N1) or influenza A not lighted by the provision of a large num-
had survived to hospital discharge. subtyped (not all of whom had ARDS), ber of total days of ECMO support and
Of the 32 hospital survivors, 31 pa- patients treated with ECMO (n = 61) the use of ECMO support in approxi-
tients (97%) were ambulant. In 20 of were compared with those without mately one-third of all cases requiring
32 hospital survivors, pulse oximetry (n=133). The patients who were treated mechanical ventilation at these cen-
data on room air were available and all with ECMO had longer duration of me- ters. Affected patients were often young
patients had recordings of 92% or more chanical ventilation (median [IQR], 18 adults, pregnant or postpartum, obese,
(median [IQR], 97% [95%-98%]). In [9-27] vs 8 [4-14] days; P = .001), ICU had severe respiratory failure before
the 14 patients who died (21%; 95% CI, stay (median [IQR], 22 [13-32] vs 12 ECMO, and received prolonged me-
11%-30%), intracranial hemorrhage [7-18] days; P = .001), and greater ICU chanical ventilation and ECMO sup-
(n = 6), other hemorrhage (n = 4), and mortality (14 [23%] vs 12 [9%]; P=.01). port. Children and elderly persons were
intractable respiratory failure (n = 4) infrequently treated with ECMO. The
were the most common conditions con- COMMENT majority of patients underwent re-
tributing to death. Of the 10 pregnant Summary of Study Findings trieval to a specialist center for ECMO.
or postpartum patients, 7 (70%) were We identified all patients who re- Despite the disease severity and the in-
alive. Of the 3 children treated with ceived ECMO for severe ARDS during tensity of treatment, the mortality rate
ECMO, all 3 were alive; however, 1 the 2009 influenza A(H1N1) winter was low.
child remained in the ICU. pandemic in Australia and New Zea-
land. Although there are almost 200 Comparison With Previous Studies
Details of Outcomes for Patients ICUs across these 2 countries, all To our knowledge, this is the first mul-
With and Without ECMO ECMO was provided at just 15 special- ticenter study on the use of ECMO for
From the group of 194 mechanically ist centers. Within these centers, the 2009 influenza A(H1N1)–associated
ventilated patients with confirmed 2009 burden was substantial, as high- ARDS. Publications from an interna-
tional ECMO registry12 and from cen-
ters experienced in the use of ECMO
Table 3. Patient Outcomes a
for ARDS of heterogeneous etiology
2009 Influenza A(H1N1)
have reported mortality rates between
Confirmed Suspected 30% and 48%.13-15 Although our pa-
Infection Infection All Infections tients had a mortality rate of 21% (95%
Outcome Measure (n = 53) (n = 15) (N = 68)
Length of stay, median (IQR), d
CI, 11%-30%), several patients re-
ICU 26 (16-35) 31 (15-38) 27 (16-37) mained in the ICU at the time of
Hospital 35 (24-45) 40 (27-54) 39 (23-47) reporting.
Duration, median (IQR), d Several factors may have contrib-
Mechanical ventilation 24 (13-31) 28 (13-34) 25 (13-34) uted to the observed mortality rate.
ECMO support 10 (7-14) 11 (10-16) 10 (7-15) First, our patients were young and had
Survival at ICU discharge 38 (72) 10 (67) 48 (71) ARDS secondary to viral pneumonia,
Still in ICU 4 (8) 2 (13) 6 (9)
which when managed with ECMO has
Survival at hospital discharge 22 (42) 10 (67) 32 (47)
been associated with higher survival
Still in hospital b 14 (26) 2 (13) 16 (24)
rates than other causes of ARDS.12-14
Ambulant at hospital discharge c 21 (95) 10 (100) 31 (97)
Second, improvements in ECMO tech-
SaO2 on room air at hospital 97 (95-98) 97 (95-98) 97 (95-98)
discharge, median (IQR), % c nology (eg, heparin-bonded cannulae,
Discharge destination rotary pumps, and small efficient long-
Died 11 (21) 3 (20) 14 (21) lasting oxygenators) and staff training
Home 18 (34) 4 (27) 22 (32) have occurred since previous publica-
Other hospital 0 1 (7) 1 (1) tions, leading to safer and more effec-
Rehabilitation facility 4 (8) 5 (33) 9 (13) tive ECMO application. All of the pa-
Cause of death d tients fulfilled the ARDS severity criteria
Hemorrhage 3 (27) 1 (33) 4 (29)
for enrollment in a recently reported
Intracranial hemorrhage 4 (36) 2 (66) 6 (43)
randomized controlled trial (the CESAR
Infection 1 (9) 0 1 (7)
study16) of ECMO treatment.
Intractable respiratory failure 3 (27) 1 (33) 4 (29)
Abbreviations: ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit; IQR, interquartile range; SaO2,
arterial oxygen saturation. Implications for Policy Makers
a Data are presented as No. (%) unless otherwise specified.
b Not including patients still in the ICU. and Clinicians
c For survivors only.
d Data are shown as No. (% of deaths) and patients could have more than 1 cause contributing to death.
Our findings have implications for
health care planning and the clinical
E6 JAMA, Published online October 12, 2009 (Reprinted) ©2009 American Medical Association. All rights reserved.
Downloaded from www.jama.com by guest on October 13, 2009
EXTRACORPOREAL MEMBRANE OXYGENATION FOR INFLUENZA A(H1N1)
management of patients with 2009 in- tients tested positive for 2009 influ- lowing ICU discharge was uncom-
fluenza A(H1N1) during the 2009- enza A(H1N1), the remainder had mon. In addition, we are unable to com-
2010 northern hemisphere winter. Our confirmed influenza A during an out- ment on the long-term outcome of our
results indicate that the incidence of break in which the dominant strain of patients, particularly in relation to the
ARDS sufficient to warrant consider- laboratory-confirmed influenza A has degree of pulmonary dysfunction and
ation of ECMO, based on the criteria been 2009 influenza A(H1N1)19 or had quality of life. Finally, our estimates of
used for the CESAR study,16 exceeds 2.6 features of a preceding influenzalike ill- ECMO use may be affected by changes
per million inhabitants. Given the out- ness complicated by pneumonia. In ad- in virulence of the virus or the devel-
comes reported in the CESAR study and dition, their clinical characteristics were opment and deployment of an effec-
in our study, other clinicians may also similar to those with confirmed 2009 tive and safe vaccine.
choose to treat these patients with influenza A(H1N1). As the diagnostic
ECMO. Approximately 15% of our pa- sensitivity of microbiological tests for CONCLUSION
tients were pregnant or postpartum, the 2009 influenza A(H1N1) is unknown, In Australia and New Zealand, during
largest case series of such patients in the many of these patients are likely to have the 2009 influenza A(H1N1) winter
literature.17,18 Most of these patients been infected with the virus. pandemic, there was a large increase in
survived. We are unable to report on the pos- the use of ECMO for ARDS in patients
Despite the additional disease bur- sible outcome of our patients if ECMO compared with the winter of 2008. De-
den, ECMO capacity was never ex- had not been used, because allocation spite their illness severity and the pro-
ceeded; however, information on the re- to receive ECMO was not conducted in longed use of life support, most of these
source utilization should facilitate the context of a randomized con- patients survived. This information
planning in the northern hemisphere. trolled trial. In our study, approxi- should facilitate health care planning
With a similar incidence of ECMO mately 30% of patients who were me- and clinical management for these com-
use for 2009 influenza A(H1N1)– chanically ventilated with 2009 plex patients during the ongoing pan-
associated ARDS, rough estimates are influenza A(H1N1) were treated with demic.
that the United States and the Euro- ECMO. This compares to an ECMO
pean Union might expect to provide treatment rate for patients who were Published Online: October 12, 2009 (doi:10.1001
/jama.2009.1535).
ECMO to approximately 800 and 1300 mechanically ventilated with 2009 in- Authors/Management and Writing Committee: An-
patients during the 2009-2010 winter, fluenza A(H1N1) of only 10% from all drew Davies, MBBS, FRACP, FJFICM (chair), Austra-
lian and New Zealand Intensive Care Research Cen-
respectively. ICUs in 1 Australian state.20 Of the 187 ter, Monash University, and Alfred Hospital,
ICUs in Australia and New Zealand, Melbourne, Australia; Daryl Jones, MD, BSc(Hons),
Study Strengths and Limitations FRACP, FJFICM, Australian and New Zealand Inten-
only 15 provided ECMO services; how- sive Care Research Center, Monash University, and
Our study is the first to report, to our ever, these centers were often referred Austin Hospital, Melbourne, Australia; Michael Bailey,
knowledge, the ECMO experience for patients with severe respiratory fail- PhD, MSc(statistics), BSc(Hons), Australian and New
Zealand Intensive Care Research Center, Monash Uni-
2009 influenza A(H1N1)–related ARDS ure despite advanced mechanical ven- versity, Melbourne, Australia; John Beca, MBChB,
using a population-based method in 2 tilatory support through semiformal re- FRACP, FJFICM, Auckland City Hospital, Auckland,
New Zealand; Rinaldo Bellomo, MD, FRACP, FJFICM,
developed countries, with well- ferral networks. Australian and New Zealand Intensive Care Research
established and nationally coordinated Of the approximately 4950 patients Center, Monash University, and Austin Hospital, Mel-
bourne, Australia; Nikki Blackwell, BSc, FRCP, FRACP,
critical care systems. To our knowl- requiring hospitalization for 2009 in- DTMH, FAChPM, FJFICM, Prince Charles Hospital,
edge, this is the complete experience of fluenza A(H1N1) in Australia and New Brisbane, Australia; Paul Forrest, MBChB, FANZCA,
ECMO in our region during winter. We Zealand as of September 7, 2009 (4561 Royal Prince Alfred Hospital, Sydney, Australia; David
Gattas, MBBS, MMed(ClinEpi), FRACP, FJFICM, Royal
report important aspects of the epide- in Australia21 and approximately 400 in Prince Alfred Hospital, Sydney, Australia; Emily Granger,
miology, disease burden, and resource New Zealand based on a similar pro- FRACS, St Vincent’s Hospital, Sydney, Australia; Rob-
ert Herkes, MBBS, FRACP, FJFICM, Royal Prince Al-
utilization for ECMO. We confirm pre- portion of confirmed cases22), the ICUs fred Hospital, Sydney, Australia; Andrew Jackson,
vious findings of severe respiratory fail- at the 15 ECMO centers received 252 MBBS, FANZCA, St Vincent’s Hospital, Sydney, Aus-
tralia; Shay McGuinness, MBChB, FRCA, FANZCA,
ure in a subset of patients with 2009 in- patients, 68 of whom received ECMO. Auckland City Hospital, Auckland, New Zealand; Priya
fluenza A(H1N1),3 and also demonstrate Of the 252 patients, 31 died, represent- Nair, MD, FJFICM, St Vincent’s Hospital, Sydney, Aus-
tralia; Vincent Pellegrino, MBBS, FRACP, FJFICM, Al-
that most patients survived. ing 17% of all 2009 influenza A(H1N1) fred Hospital, Melbourne, Australia; Ville Pettilä, MD,
Our study has the inherent limita- deaths in Australia21 and New Zealand.22 PhD, Australian and New Zealand Intensive Care Re-
tions of a case series. To improve ac- With the requirement to inform the search Center, Monash University, Melbourne, Aus-
tralia; Brian Plunkett, MBChB, Royal Prince Alfred Hos-
curacy, we used systematic methods of northern hemisphere for the upcom- pital, Sydney, Australia; Roger Pye, FRACP, FJFICM,
data collection, such as a case report ing winter, we censored our data col- FANZCA, St Vincent’s Hospital, Sydney, Australia; Paul
Torzillo, MBBS, FRACP, FJFICM, Royal Prince Alfred
form, trained research coordinators, lection on September 7, 2009. Accord- Hospital, Sydney, Australia; Steve Webb, MPH, PhD,
predefined data field definitions, and a ingly, final hospital outcomes were not FRACP, FJFICM, Royal Perth Hospital, and School of
Population Health and School of Medicine and Phar-
prospectively constructed data analy- available for some patients. However, macology, University of Western Australia, Perth, Aus-
sis plan. Although only 78% of pa- death after weaning from ECMO or fol- tralia; Michael Wilson, BScMed, FRACS, Royal Prince
©2009 American Medical Association. All rights reserved. (Reprinted) JAMA, Published online October 12, 2009 E7
Downloaded from www.jama.com by guest on October 13, 2009
EXTRACORPOREAL MEMBRANE OXYGENATION FOR INFLUENZA A(H1N1)
Alfred Hospital, Sydney, Australia; Marc Ziegenfuss, Bird, Simon Finfer, Carole Foot, Richard Piper, Ray- 10. Australian Bureau of Statistics. Australian demo-
MBBCh, BSc, Dip(PEC), FRCS, FJFICM, Prince Charles mond Raper, Elizabeth Steel); Monash Medical Cen- graphic statistics. http://www.abs.gov.au/ausstats
Hospital, Brisbane, Australia. tre, Melbourne, Australia (Pauline Galt, Craig Walker); /abs@.nsf/mf/3101.0/. Accessed September 10,
Author Contributions: Dr Davies had full access to all Royal Perth Hospital, Perth, Australia (Andree Gould, 2009.
of the data in the study and takes responsibility for Geraldine McEntaggart, Steve Webb). 11. Statistics New Zealand. Population Indicators.
the integrity of the data and the accuracy of the data Project Support: Siouxzy Morrison, Belinda Howe http://www.stats.govt.nz/methods_and_services
analysis. (Australian and New Zealand Intensive Care Research /access-data/tables/pop-indicators.aspx. Accessed Sep-
Study concept and design: Davies, Jones, Beca, Centre). tember 10, 2009.
Bellomo, Gattas, Granger, Jackson, Nair, Pellegrino, Additional Contributions: We thank Simon Finfer, 12. Conrad SA, Rycus PT, Dalton H. Extracorporeal
Plunkett, Pye, Torzillo, Webb, Wilson, Ziegenfuss. FRACP, FJFICM (George Institute for International Life Support Registry Report 2004. ASAIO J. 2005;
Acquisition of data: Davies, Jones, Beca, Bellomo, Health, University of Sydney, Sydney, Australia), for his 51(1):4-10.
Blackwell, Forrest, Gattas, Granger, Herkes, Jackson, advice and comments during the preparation of the 13. Peek GJ, Moore HM, Moore N, Sosnowski AW,
McGuinness, Nair, Pellegrino, Plunkett, Pye, Torzillo, manuscript; and Ian Seppelt, FANZCA, FJFICM (Nepean Firmin RK. Extracorporeal membrane oxygenation for
Webb, Ziegenfuss. Hospital, Sydney, Australia), for assisting with the eth- adult respiratory failure. Chest. 1997;112(3):759-
Analysis and interpretation of data: Davies, Jones, ics committee approval process. We also thank all the 764.
Bailey, Bellomo, Blackwell, Gattas, Jackson, physicians, nurses, and perfusionists who cared for these 14. Hemmila MR, Rowe SA, Boules TN, et al. Extra-
McGuinness, Pettilä, Torzillo, Webb. complex patients. Drs Finfer and Seppelt did not re- corporeal life support for severe acute respiratory dis-
Drafting of the manuscript: Davies, Jones, Bellomo, ceive any compensation for their contributions. tress syndrome in adults. Ann Surg. 2004;240(4):
McGuinness, Nair, Pye, Torzillo, Webb, Ziegenfuss. 595-605.
Critical revision of the manuscript for important in- REFERENCES 15. Lindén VB, Lidegran MK, Frisén G, Dahlgren P,
tellectual content: Davies, Jones, Bailey, Beca, Bellomo, Frenckner BP, Larsen F. ECMO in ARDS: a long-term
Blackwell, Forrest, Gattas, Granger, Herkes, Jackson, 1. World Health Organization. Influenza-like illness follow-up study regarding pulmonary morphology and
McGuinness, Nair, Pellegrino, Pettilä, Plunkett, Pye, in the United States and Mexico. http://www.who function and health-related quality of life. Acta An-
Torzillo, Webb, Wilson, Ziegenfuss. .int/csr/don/2009_04_24/en/index.html. Accessed aesthesiol Scand. 2009;53(4):489-495.
Statistical analysis: Davies, Bailey. September 10, 2009. 16. Peek GJ, Mugford M, Tiruvoipati R, et al. Effi-
Obtained funding: Bellomo, Herkes. 2. Dawood FS, Jain S, Finelli L, et al; Novel Swine- cacy and economic assessment of conventional ven-
Administrative, technical, or material support: Jones, Origin Influenza A (H1N1) Virus Investigation Team. tilatory support versus extracorporeal membrane oxy-
Beca, Bellomo, Forrest, Gattas, Granger, Jackson, Emergence of a novel swine-origin influenza A (H1N1) genation for severe adult respiratory failure (CESAR):
McGuinness, Nair, Pellegrino, Pettilä, Plunkett, Pye, virus in humans. N Engl J Med. 2009;360(25): a multicentre randomised controlled trial [published
Webb, Wilson. 2605-2615. online September 16, 2009]. Lancet. doi:10.1016
Study supervision: Davies, Beca, Bellomo, Forrest, 3. Perez-Padilla R, de la Rosa-Zamboni D, Ponce de /S0140-6736(09)61069-2.
Gattas, Nair, Pye, Torzillo, Ziegenfuss. Leon S, et al; INER Working Group on Influenza. Pneu- 17. King PT, Rosalion A, McMillan J, Buist M, Holmes
Financial Disclosures: None reported. monia and respiratory failure from swine-origin influ- PW. Extracorporeal membrane oxygenation in
Participating Sites and Investigators (sites in order enza A (H1N1) in Mexico. N Engl J Med. 2009; pregnancy. Lancet. 2000;356(9223):45-46.
of largest number of patients): Royal Prince Alfred Hos- 361(7):680-689. 18. Cunningham JA, Devine PC, Jelic S. Extracorpo-
pital, Sydney, Australia (Paul Forrest, David Gattas, 4. Worldwide H1N1 (Swine Flu) Infection Data. http: real membrane oxygenation in pregnancy. Obstet
Robert Herkes, Brian Plunkett, Dorrilyn Rajbhandari, //www.flucount.org/. Accessed September 10, Gynecol. 2006;108(3 pt 2):792-795.
Caitlin Rees, Paul Torzillo, Michael Wilson); St Vin- 2009. 19. Australian Department of Health and Aging. Aus-
cent’s Hospital, Sydney, Australia (Emily Granger, An- 5. Webb SAR, Seppelt IM; ANZIC Influenza tralian National Influenza Surveillance 2009. http:
drew Jackson, Priya Nair, Roger Pye, Claire Rey- Investigators. Pandemic H1N1 2009 influenza (“swine //www.healthemergency.gov.au/internet
nolds); Auckland City Hospital, Auckland, New Zealand flu”) in Australian and New Zealand intensive care. /healthemergency/publishing.nsf/Content/ozflu2009
( John Beca, Nicola Gini, Shay McGuinness, Rachael Crit Care Resusc. 2009;11(3):170-172. .htm. Accessed September 10, 2009.
Parke); Prince Charles Hospital, Brisbane, Australia 6. Australian Department of Health and Ageing. Pan- 20. Lum ME, McMillan AJ, Brook CW, et al. Impact
(Nikki Blackwell, Angela McCosker, Dan Mullany, Marc demic (H1N1) 2009 update bulletins. http://www of pandemic (H1N1) 2009 influenza on critical care
Ziegenfuss); Alfred Hospital, Melbourne, Australia ( Jas- .healthemergency.gov.au/internet/healthemergency capacity in Victoria. Med J Aust. 2009;191:1-5. http:
min Board, Andrew Davies, Andrew Hilton, Vincent /publishing.nsf/Content/bulletins-13-19-july09. //www.mja.com.au/public/issues/191_09_021109
Pellegrino, Carlos Scheinkestel, Shirley Vallance); Sir Accessed September 10, 2009. /lum10916_fm.pdf. Accessed September 29,
Charles Gairdner Hospital, Perth, Australia (Stuart 7. Call SA, Vollenweider MA, Hornung CA, Simel DL, 2009.
Baker, Brigit Roberts, Paul Woods); Westmead Hos- McKinney WP. Does this patient have influenza? 21. Australian Department of Health and
pital, Sydney, Australia (Rowena Boyd, Peter Clark, JAMA. 2005;293(8):987-997. Ageing. Pandemic (H1N1) 2009 update bulletins.
Vineet Nayyar, Christina Skelly, Eddie Stachowski); St 8. Chow AW, Hall CB, Klein JO, Kammer RB, Meyer http://www.healthemergency.gov.au/internet
George Hospital, Sydney, Australia (Deborah Inskip, RD, Remington JS; Infectious Diseases Society of /healthemergency/publishing.nsf/Content
Doris Lam, John Myburgh, Rebecca Sidoli); Austin Hos- America and the Food and Drug Administration. Evalu- /2FBF38115CD98BB7CA25762A00121475
pital, Melbourne, Australia (Rinaldo Bellomo, Glenn ation of new anti-infective drugs for the treatment of /$File/h1n1-update-20090907.doc. Accessed Sep-
Eastwood, Daryl Jones); Liverpool Hospital, Sydney, respiratory tract infections. Clin Infect Dis. 1992; tember 29, 2009.
Australia (Sharon Micallef, Michael Parr); Princess Al- 15(suppl 1):S62-S88. 22. New Zealand Ministry of Health. Pandemic in-
exandra Hospital, Brisbane, Australia (Meg Harward, 9. Murray JF, Matthay MA, Luce JM, Flick MR. An fluenza (H1N1) 09 swine flu: update 148. http://www
Chris Joyce, Peter Kruger); Royal Children’s Hospital, expanded definition of the adult respiratory distress .moh.govt.nz/moh.nsf/indexmh/influenza-a-h1n1
Melbourne, Australia (Warwick Butt, Melissa Culka); syndrome. Am Rev Respir Dis. 1988;138(3):720- -update-148-070909. Accessed September 29,
Royal North Shore Hospital, Sydney, Australia (Simon 723. 2009.
E8 JAMA, Published online October 12, 2009 (Reprinted) ©2009 American Medical Association. All rights reserved.
Downloaded from www.jama.com by guest on October 13, 2009
Das könnte Ihnen auch gefallen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- LCD For Abdominal and Pelvic Ultrasound (L28539) : Contractor Information Contractor NameDokument51 SeitenLCD For Abdominal and Pelvic Ultrasound (L28539) : Contractor Information Contractor Nameapi-26851799Noch keine Bewertungen
- FREQUENTLY ASKED QUESTIONS 1. What Documentation Is Necessary For TheDokument8 SeitenFREQUENTLY ASKED QUESTIONS 1. What Documentation Is Necessary For Theapi-26851799100% (1)
- Ultrasound Coding and Reimbursement Document 2009 Emergency Ultrasound Section AmericanDokument19 SeitenUltrasound Coding and Reimbursement Document 2009 Emergency Ultrasound Section Americanapi-26851799Noch keine Bewertungen
- Surgical Mask Vs N95 Respirator For Preventing Influenza Among HealthDokument8 SeitenSurgical Mask Vs N95 Respirator For Preventing Influenza Among Healthapi-26851799Noch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- CSIR NET Dec 2010 Life Sciences Solved Qiestion PaperDokument26 SeitenCSIR NET Dec 2010 Life Sciences Solved Qiestion PaperUdayanidhi RNoch keine Bewertungen
- Human Anatomy and Physiology II: Topic: Anatomy of The Blood Sub Topic: Introduction To Blood and Its CompositionsDokument28 SeitenHuman Anatomy and Physiology II: Topic: Anatomy of The Blood Sub Topic: Introduction To Blood and Its Compositionsngong ngong ametNoch keine Bewertungen
- 1 s2.0 S2451945621004384 MainDokument16 Seiten1 s2.0 S2451945621004384 Mainzeyneptozan136Noch keine Bewertungen
- DNA Microarrays: by Mohammed Mashik Kommareddy Krithik Yadu Krishnan Mubashir Deepak A SDokument30 SeitenDNA Microarrays: by Mohammed Mashik Kommareddy Krithik Yadu Krishnan Mubashir Deepak A SVipin GeorgeNoch keine Bewertungen
- NEJMNotable Articlesof 2021Dokument53 SeitenNEJMNotable Articlesof 2021Federico Ariel RodriguezNoch keine Bewertungen
- 1.01 PlateletsDokument9 Seiten1.01 PlateletsShiena ArchividoNoch keine Bewertungen
- Chemotherapy and Biotherapy GuidelinesDokument493 SeitenChemotherapy and Biotherapy GuidelinesMohammed GazoNoch keine Bewertungen
- (Zdenko Herceg, Toshikazu Ushijima) Epigenetics An (Book4You) PDFDokument411 Seiten(Zdenko Herceg, Toshikazu Ushijima) Epigenetics An (Book4You) PDFChristian MoscosoNoch keine Bewertungen
- Prevalence, Types and Treatment of Tuberculosis: A ReviewDokument25 SeitenPrevalence, Types and Treatment of Tuberculosis: A ReviewUMT JournalsNoch keine Bewertungen
- Science - July 8, 2022 USADokument144 SeitenScience - July 8, 2022 USASimej100% (1)
- Necrotizing Pneumonitis Caused by Mycoplasma Pneumoniae in Pediatric PatientsDokument4 SeitenNecrotizing Pneumonitis Caused by Mycoplasma Pneumoniae in Pediatric Patientswawa chenNoch keine Bewertungen
- Topic 11: The Aspects of Gene Therapy: Somatic Gene Therapy, Which Involves Introducing A "Good" Gene Into Targeted CellsDokument5 SeitenTopic 11: The Aspects of Gene Therapy: Somatic Gene Therapy, Which Involves Introducing A "Good" Gene Into Targeted CellsHannah Alvarado BandolaNoch keine Bewertungen
- Anticoccidial Drugs of The Livestock IndustryDokument18 SeitenAnticoccidial Drugs of The Livestock IndustryNofitra Dewi Suparno PNoch keine Bewertungen
- Scientia Horticulturae PotatoDokument8 SeitenScientia Horticulturae PotatoUMA MAHESWARINoch keine Bewertungen
- MycovirusDokument18 SeitenMycovirusMudasirAhmadDarNoch keine Bewertungen
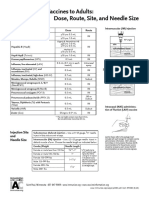
- Administering Vaccines To Adults: Dose, Route, Site, and Needle SizeDokument1 SeiteAdministering Vaccines To Adults: Dose, Route, Site, and Needle SizeAkashNoch keine Bewertungen
- Git, Liver & GB: by Dr. Thameem SaifDokument119 SeitenGit, Liver & GB: by Dr. Thameem SaifGirija VirkarNoch keine Bewertungen
- FinalthesisoftuberculosisDokument86 SeitenFinalthesisoftuberculosisOuaingar ngueadoumNoch keine Bewertungen
- Integrated Pest Management in WatermelonDokument42 SeitenIntegrated Pest Management in WatermelonGuruPrasadNoch keine Bewertungen
- RIBOZYMESDokument17 SeitenRIBOZYMESSharan GayathrinathanNoch keine Bewertungen
- 27 - Protein Trafficking - Nuclear TransportDokument12 Seiten27 - Protein Trafficking - Nuclear TransportHarry DouglasNoch keine Bewertungen
- FlashcardsDokument18 SeitenFlashcardsDaphne HernaezNoch keine Bewertungen
- Daftar Pustaka: Repository - Unimus.ac - IdDokument3 SeitenDaftar Pustaka: Repository - Unimus.ac - IdAri BudimanNoch keine Bewertungen
- Sanitation, Cleaning, and Disinfecting Poultry FacilitiesDokument4 SeitenSanitation, Cleaning, and Disinfecting Poultry Facilitiesronalit malintadNoch keine Bewertungen
- Family EnterobacteriaceaeDokument19 SeitenFamily EnterobacteriaceaeJisanieNoch keine Bewertungen
- 80 DIAGRAM BASED MCQS FOR AIIMS and NEET by Neetmedicalacademy Blog PDFDokument82 Seiten80 DIAGRAM BASED MCQS FOR AIIMS and NEET by Neetmedicalacademy Blog PDFAritraa SAHANoch keine Bewertungen
- Alfaa LabsDokument7 SeitenAlfaa LabsahmedgebalyNoch keine Bewertungen
- Journal - Antimicrobial ResistanceDokument12 SeitenJournal - Antimicrobial ResistanceTriLightNoch keine Bewertungen
- IgG4 Affected by Endotoxin in mRNA Jabs - by GeoffPainPhDDokument14 SeitenIgG4 Affected by Endotoxin in mRNA Jabs - by GeoffPainPhDbrunolacroix953Noch keine Bewertungen
- Current Research in Toxicology: Dawood Ghafoor, Zafran Khan, Asaf Khan, Daniya Ualiyeva, Nasib ZamanDokument10 SeitenCurrent Research in Toxicology: Dawood Ghafoor, Zafran Khan, Asaf Khan, Daniya Ualiyeva, Nasib ZamanjosetelhadoNoch keine Bewertungen