Beruflich Dokumente
Kultur Dokumente
Metabolisme B-12 and Folate
Hochgeladen von
YeniOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Metabolisme B-12 and Folate
Hochgeladen von
YeniCopyright:
Verfügbare Formate
Cobalmin & Folate Metabolism
Cyanocobalamin (Vitamin B12) is one of a family of cobalamins consisting of 1) a corrin ring around a cobalt atom and 2) a nucleotide group of a base (5,6dimethylbenzimidazole) and a phosphorylated ribose with 1-amino,2-propanol. This complex is linked to a -group. The -group is: cyanide in cyanocobalamin (at right), an adenosyl group in adenosylcobalamin, a methyl group in methylcobalamin, and a hydroxyl group in hydroxocobalamin. Conversion between forms readily takes place in body tissues.
Cobalamin is synthesized exclusively by bacteria. Cobalamin is temporarily bound to R-binding proteins, but released by duodenal digestive enzymes. The newly freed cobalamin is bound by intrinsic factor (IF) secreted by gastric parietal cells. This IF-cobalamin complex binds to receptors on the brush border of the ileal mucosa and is absorbed over a period of several hours. Most absorbed cobalamin (90%) is transfered to transcobalamin II, the primary transport protein of cobalamin.
Total body stores of cobalamin measure 2-5 mg. The average daily diet in the US contains about 5-30 g, where as daily requirements are only 2-5 g/day. Cobalamin, in the form of adenosylcobalamin, is stored primarily in the liver. Adenosylcobalamin is key to conversion of methylmalonyl CoA to succinyl CoA (Krebs cycle). Methylcobalamin is an essential part of the folate-cobalamin reaction necessary for DNA synthesis. Folic acid (pteroyl monoglutamic acid) occurs in nature as relatively insoluble aggregates - polyglutamates.
Leafy vegetables (broccoli,spinach,asparagus,lettuce), fruit, milk, eggs, liver, and yeast contain folic acid. Some intestinal bacteria also form folic acid. The average US diet contains about 1,000 g of folate. The daily requirement is 100-200 g/day and body stores average 5,000g. Additional folate is required during pregnancy and growth. Liver is a major storage site, but releases folate only into the bile for reaborption in the jejunum and ileum. This process, refered to as the enterohepatic circulation, is necessary for maintainance of plasma folate levels. Alcohol interferes with the enterohepatic circulation of folate and can lower plasma folate levels within hours. Folate is absorbed in the proximal jejunum and ileum although the mechanism is unclear. Conjugases along the brush border break polyglutamates into monoglutamates for absorption. Folate circulates free or albumin bound in the plasma as N5-methyl FH4. Absorbed N5-methyl FH4 hands off a methyl group to synthesize methionine from homocysteine in a step requiring cobalamin and generates FH4 (tetrahydrofolate) which is reconjugated to N5,10-methylene FH4 or other FH4-(Glu)n for use in thymidilate and purine synthesis.
Vit B12
Cofactor for methionine synthase Methylcobalamin is required for the function of the folate-dependent enzyme, methionine synthase. This enzyme is required for the synthesis of the amino acid, methionine, from homocysteine. Methionine in turn is required for the synthesis of S-adenosylmethionine, a methyl group donor used in many biological methylation reactions, including the methylation of a number of sites within DNA and RNA (3). Methylation of DNA may be important in cancer prevention. Inadequate function of methionine synthase can lead to an accumulation of homocysteine, which has been associated with increased risk of cardiovascular diseases
S-adenosylhomocysteine is formed during Sadenosylmethionine-dependent methylation reactions, and the hydrolysis of Sadenosylhomocysteine results in homocysteine. Homocysteine may be remethylated to form methionine by a folatedependent reaction that is catalyzed by methionine synthase, a vitamin B12-dependent enzyme. Alternately, homocysteine may be metabolized to cysteine in reactions catalyzed by two vitamin B6-dependent enzymes.
Cofactor for L-methylmalonyl-CoA mutase 5-Deoxyadenosylcobalamin is required by the enzyme that catalyzes the conversion of L-methylmalonylCoA to succinyl-CoA. This biochemical reaction plays an important role in the production of energy from fats and proteins. Succinyl CoA is also required for the synthesis of hemoglobin, the oxygen carrying pigment in red blood cells (3). Symptoms of vitamin B12 deficiency Vitamin B12 deficiency results in impairment of the activities of B12-requiring enzymes. Impaired activity of methionine synthase may result in elevated homocysteine levels, while impaired activity of Lmethylmalonyl-CoA mutase results in increased levels of a metabolite of methylmalonyl-CoA called methylmalonic acid (MMA). Individuals with mild vitamin B12 deficiency may not experience symptoms, although blood levels of homocysteine and/or MMA may be elevated (12). Megaloblastic anemia Diminished activity of methionine synthase in vitamin B12 deficiency inhibits the regeneration of tetrahydrofolate (THF) and traps folate in a form that is not usable by the body (diagram), resulting in symptoms of folate deficiency even in the presence of adequate folate levels. Thus, in both folate and vitamin B12 deficiencies, folate is unavailable to participate in DNA synthesis. This impairment of DNA synthesis affects the rapidly dividing cells of the bone marrow earlier than other cells, resulting in the production of large, immature, hemoglobin-poor red blood cells. The resulting anemia is known as megaloblastic anemia and is the symptom for which the disease, pernicious anemia, was named (3). Supplementation with folic acid will provide enough usable folate to restore normal red blood cell formation. However, if vitamin B12 deficiency is the cause, it will persist despite the resolution of the anemia. Thus, megaloblastic anemia should not be treated with folic acid until the underlying cause has been determined (5).
Vitamin B12 and Nucleic Acid Metabolism
5,10-Methylene tetrahydrofolate (TH4) is required for the synthesis of nucleic acids, while 5-methyl TH4 is required for the formation of methionine from homocysteine. Methionine, in the form of S-adenosylmethionine, is required for many biological methylation reactions, including DNA methylation. Methylene TH4 reductase is a flavin-dependent enzyme required to catalyze the reduction of 5,10-methylene TH4 to 5methyl TH4.
Megaloblastic Anemia The normal proliferation of cells depends on adequate folate and vitamin B12. Folate is necessary for efficient thymidilate synthesis and production of DNA. B12 is needed to successfully incorporate circulating folic acid into developing RBCs; retaining the folate in the RBC. Review the metabolic mechanisms of B12 and folate (See Normal Hematopoiesis-B12 and Folate Metabolism) Pyrimidines: thymine, cytosine, and uracil Purines: adenine and guanine Lack of folate or B12 leads to decreased dTTP synthesis, resulting in a slowing of DNA synthesis. The role of folate is illustrated at right. The mechanism by which B12 leads to decreased DNA synthesis is unclear. Two likely explanations follow.
Methylfolate "trap" hypothesis. Lack of cobalamin slows the methyltransferase reaction resulting in increased N5-methyl FH4. Thus N5-methyl FH4 is "trapped" or unable to be metabolized to FH4. N5-methyl FH4 can convert to N5, 10-methylene FH4, but poorly without new FH4 other forms of folate diminish leading to slowed synthesis of dTMP. Formate "starvation" hypothesis. Lack of cobalamine slows the methyltransferase reaction deceasing methionine production and in turn depressing formate generation.
A deficiency of either vitamin Bl2 or folic acid results in megaloblastic erythroid cells-megaloblasts. These deficiencies result in a decrease in DNA synthesis which slows and inhibits DNA replication (nuclear division). Nuclear maturation is slowed whereas cytoplasmic maturation (largely dependent on RNA function and unaffected by failure of thymidilate synthesis) is relatively unimpeded. The impaired nuclear maturation is seen as open, loose, immature chromatin (cut-salami pattern).
In contrast to the nucleus, the cytoplasm of megaloblastic cells is abundant with normal hemoglobinization. This disparity between nucleus and cytoplasm is known as nuclear-cytoplasmic asynchrony.
Although most noticeable in erythroid cells failure of DNA synthesis also affects myeloid and megakaryocytes. Giant bands (right) and hypersegmented polymorphonuclear neutrophils (below) are common.
Even megakaryocytes (right) may be hypersegmented.
The impaired RBC production and destruction of defective RBCs in the marrow before release into the peripheral blood (ineffective erythropoiesis) results in the anemia. A bone marrow biopsy and aspirate reveal erythroid hyperplasia. Erythrocytic precursors (promegaloblasts with open, immature chromatin) are increased.
Bone marrow biopsy from patient with megaloblastic anemia. Arrowheads point to megaloblasts and arrow to RBC undergoing apoptosis.
Inhibition of thymidylate synthetase leads to decreased dTTP synthesis and formation of excess dUTP. The dUTP is incorporated into DNA. Repair of this abnormal DNA is blocked by lack of thymidine residues; the DNA breaks apart (karyorrhexis) and the cell dies.
The megaloblastic changes are most apparent in the polychromatophilic and orthochromatophilic stages. Multinucleate RBCs, abnormal karyorrhexis, increased pyknosis, and Howell-Jolly bodies ( right) may be seen.
The peripheral blood reveals a pancytopenia (decreased RBCs, white cells, and platelets), hypersegmented neutrophils (> five lobes), and oval macrocytes.
Once a macrocytic anemia is identified (MCV >100) and medications excluded, a PBS should be examined. Round macrocytes suggest possible thyroid or liver disease, while oval macrocytes suggest B12 or folate deficiency. The reticulocyte count is usually normal or low (if increased: hemolysis or blood loss are likely).
Megaloblastic anemia is most often due to a B12 or folate deficiency, but the cause of the deficiency must be determined for proper treatment. Megaloblastic anemia due to vitamin B12 deficiency caused by a lack of intrinsic factor is specifically referred to as pernicious anemia.
Laboratory testing of B12 and folate are critical to establishing the cause of a megaloblastic anemia.
B12 Absorption involves a series of several proteins and receptors. Antibodies against the proteins of cells involved can be helpful in the diagnosis of macrocytic anemia. Anti-intrinsic factor antibodies, are fairly specific, but unfortunately, not sensitve. Antiparietal cell antibodies while sensitive, are not specific as they are seen in a number of other diseases.
The Schilling test tests for evidence of impaired vitamin B12 absorption correctable by intrinsic factor. The Schilling test Radioactive cobalamin (Cbl*) is taken orally; followed by injection of a saturating dose of non-radioactive cobalamin. The level of Cbl* is measured in the urine. In pernicious anemia the excreted levels of Cbl* are low. If intrinsic factor is given with the Cbl* the Cbl* levels will correct in PA, but not in ileal malabsorption.
Clinical findings include a yellowish- lemon skin, glossitis (smooth tongue) and stomatitis in severe cases. Neurologic abnormalities, secondary to defects in myelination, are seen in Vitamin B12, but not folate deficiencies. The mechanism for the demyelination is believed to be lack of methyl-B12 for conversion of homocysteine to methionine. This results in decreased production of S-
Posterior and lateral degeneration typical of late stage disease.
adenosylmethionine (SAM) needed for methylation of phosphatidylethanolamine to phosphatidylcholine for incorporation into myelin. Degeneration of the posterior columns and peripheral nerve damage leads to numbness; "pins and needles" feeling; loss of position and vibratory sense. Later, lack of coordination; weakness of the legs can be seen. In long standing disorders an ataxic gait; +Babinski sign (lateral columns) may be found. Today neurologic manifestations are relatively rare (<20% of patients) and usually mild.
B12 deficiency resulting in megaloblastic anemia may also be caused by a complete gastric resection [remember parietal cells (IF) are found in the gastric fundus]. Similarly, the IF-B12 complex is absorbed in the distal ileum, thus intestinal malabsorption syndromes or ileal resection can result in B12 deficiency. Antibiotics can allow cobalmin dependent bacterial over growth in the intestine resulting in vitamin B12 depletion. [Similarly any intestinal malformation (congenital or surgical) ie. blind loop syndroms, will decrease peristalsis leading to statis; bacterial overgrowth and vitamin B12 deficiency.] As B12 is found solely in foods of animal origin, individuals on strict vegetarian diets are susceptible to B12 deficiency. Megaloblastic anemia secondary to folate deficiency can be caused in several ways. Most common is severe dietary deprivation of folate from chronic alcohol abuse or malnuroishment. Similarly, the demands of the fetus and poor maternal diet may combine to produce folate deficiency in pregnancy. Folate deficiency may also be caused by malabsorption secondary to intestinal infection by Giardia or intestinal sprue. Chemotherapy for malignancy such as methotrexate, a folic acid antagonist, will cause megaloblastic anemia and requires "rescue" with citrovorum (N5-formyl THF). Dilantin and oral contraceptives may also cause folate deficiency. A relative folate deficiency may occur when the demand for folate increases due to accelerated erythropoiesis (ie. as a compensatory erythroid hyperplasia in hemolytic anemia).
Das könnte Ihnen auch gefallen
- 7 - Nursing Service Floating and Pull OutDokument4 Seiten7 - Nursing Service Floating and Pull Outakositabon100% (3)
- Group 3 Team 1 - Case AnalysisDokument14 SeitenGroup 3 Team 1 - Case AnalysisLaureen CordovaNoch keine Bewertungen
- Ultimate Final CoachingDokument79 SeitenUltimate Final CoachingCarlo Montejo100% (1)
- (Current Clinical Urology) Pat F. Fulgham, Bruce R. Gilbert (Eds.) - Practical Urological Ultrasound-Humana Press (2017) PDFDokument360 Seiten(Current Clinical Urology) Pat F. Fulgham, Bruce R. Gilbert (Eds.) - Practical Urological Ultrasound-Humana Press (2017) PDFIon VasianNoch keine Bewertungen
- 6.megaloblastic AnaemiasDokument34 Seiten6.megaloblastic AnaemiasWissam AlwazaniNoch keine Bewertungen
- Kuliah Macrocytic Anemia 2017Dokument40 SeitenKuliah Macrocytic Anemia 2017igus696Noch keine Bewertungen
- Megaloblastic Anemia Causes, Symptoms, Tests & TreatmentDokument14 SeitenMegaloblastic Anemia Causes, Symptoms, Tests & TreatmentMatt McAndrew GarciaNoch keine Bewertungen
- 3 - Metabolisme Vitamin B12 B9 CDokument49 Seiten3 - Metabolisme Vitamin B12 B9 CPaulinNoch keine Bewertungen
- Chemistry Lec.2 (Vitamins 2)Dokument6 SeitenChemistry Lec.2 (Vitamins 2)Muhammed AbdulsamadNoch keine Bewertungen
- AnemiaDokument26 SeitenAnemiaIrtiza ChohanNoch keine Bewertungen
- Macrocytic Anemia - Megaloblastic AnemiaDokument42 SeitenMacrocytic Anemia - Megaloblastic AnemiaDarien LiewNoch keine Bewertungen
- Metabolism - HW2 - Anemia Vitamins - SP24Dokument4 SeitenMetabolism - HW2 - Anemia Vitamins - SP24raybuaNoch keine Bewertungen
- Hema Chapter 21Dokument6 SeitenHema Chapter 21EMETERIO TUTOR IIINoch keine Bewertungen
- Megaloblastic Anaemia: Folic Acid and Vitamin B12 MetabolismDokument9 SeitenMegaloblastic Anaemia: Folic Acid and Vitamin B12 MetabolismStephan CanoNoch keine Bewertungen
- Water-Soluble VitaminsDokument32 SeitenWater-Soluble VitaminsHomed OpriNoch keine Bewertungen
- Vitamin B12 and Folic AcidDokument43 SeitenVitamin B12 and Folic AcidErin HillNoch keine Bewertungen
- Macrocytic AnemiasDokument28 SeitenMacrocytic AnemiasDeepankar SrigyanNoch keine Bewertungen
- Megaloblastic AnemiasDokument37 SeitenMegaloblastic AnemiasL3mi DNoch keine Bewertungen
- Vitamin 21 JulyDokument35 SeitenVitamin 21 JulySafura IjazNoch keine Bewertungen
- Vitamin b12Dokument18 SeitenVitamin b12api-3770131100% (1)
- Macrocytic Anemias: Defective DNA SynthesisDokument17 SeitenMacrocytic Anemias: Defective DNA SynthesispallavberiNoch keine Bewertungen
- Folate and Cobalamin MetabolismDokument5 SeitenFolate and Cobalamin MetabolismheyahroxNoch keine Bewertungen
- Cobalamin: A Critical Vitamin in The ElderlyDokument11 SeitenCobalamin: A Critical Vitamin in The ElderlyLuis ÓnidasNoch keine Bewertungen
- Megaloblastic AnemiaDokument11 SeitenMegaloblastic AnemiaThuvija DarshiniNoch keine Bewertungen
- Topic 9 - Anemia 4Dokument27 SeitenTopic 9 - Anemia 4Vince Martin ManaigNoch keine Bewertungen
- Obat Antianemia Warmadewa 2012 DrugsDokument30 SeitenObat Antianemia Warmadewa 2012 DrugsChandra ShinodaNoch keine Bewertungen
- Folic Acid.Dokument35 SeitenFolic Acid.M.PRASAD NAIDUNoch keine Bewertungen
- Or Deamination PLP Also Participates in Reactions in Which An Amino Group IsDokument5 SeitenOr Deamination PLP Also Participates in Reactions in Which An Amino Group IsNissa zuzulNoch keine Bewertungen
- Vitamin B12 and FolateDokument12 SeitenVitamin B12 and FolateAllessandria DimaggioNoch keine Bewertungen
- Solomon B12 2006Dokument18 SeitenSolomon B12 2006Erwin K EdisonNoch keine Bewertungen
- Macrocytic Anemia May Be Classified As MegaloblasticDokument5 SeitenMacrocytic Anemia May Be Classified As MegaloblasticOjambo FlaviaNoch keine Bewertungen
- Lec. B12Dokument94 SeitenLec. B12Arshad Mehmood MinhasNoch keine Bewertungen
- DNA Metabolism Disorders in Hematology: Vitamin B12 and Folate DeficiencyDokument1 SeiteDNA Metabolism Disorders in Hematology: Vitamin B12 and Folate DeficiencyPeter JosephNoch keine Bewertungen
- Introduction To MacrocyticDokument9 SeitenIntroduction To MacrocyticSalim UddinkhanNoch keine Bewertungen
- Treating Blood Cell Deficiencies and AnemiasDokument11 SeitenTreating Blood Cell Deficiencies and AnemiasVaishali PrasharNoch keine Bewertungen
- Megaloblastic Anaemia: Folic Acid and Vitamin B12 MetabolismDokument9 SeitenMegaloblastic Anaemia: Folic Acid and Vitamin B12 MetabolismLuna100% (1)
- Hematinic AgentsDokument89 SeitenHematinic AgentsHussain Rizvi50% (2)
- Folate Deficiency Presentation for MBChB Year 3Dokument6 SeitenFolate Deficiency Presentation for MBChB Year 3BISHOP MBILINoch keine Bewertungen
- Agents Used in Anemias 2Dokument25 SeitenAgents Used in Anemias 2Raboha TawilNoch keine Bewertungen
- Homocystinuria: Causes, Symptoms and TreatmentDokument4 SeitenHomocystinuria: Causes, Symptoms and TreatmentARyiam GtpNoch keine Bewertungen
- Megbl, Pernicious ADokument23 SeitenMegbl, Pernicious Aacs.pathNoch keine Bewertungen
- Water-Soluble Vitamins: Essential Nutrients for Metabolism and HealthDokument32 SeitenWater-Soluble Vitamins: Essential Nutrients for Metabolism and HealthannisaNoch keine Bewertungen
- Macrocytic AnemiaDokument48 SeitenMacrocytic AnemiaMONoch keine Bewertungen
- MetaScreen 100+ Conditions DeckDokument115 SeitenMetaScreen 100+ Conditions DeckLab Brawijaya HospitalNoch keine Bewertungen
- Chapter 4 Notes: Megaloblastic AnaemiaDokument7 SeitenChapter 4 Notes: Megaloblastic Anaemiamjamie12345Noch keine Bewertungen
- Aminomutase Which Converts B-Leucine Into L-Leucine and Vice-VersaDokument4 SeitenAminomutase Which Converts B-Leucine Into L-Leucine and Vice-VersaYohana MariaNoch keine Bewertungen
- Topic 12. Porphirin Metabolism.Dokument7 SeitenTopic 12. Porphirin Metabolism.Manar BehiNoch keine Bewertungen
- Anemia Defisiensi Asam FolatDokument15 SeitenAnemia Defisiensi Asam FolatKertiasihwayanNoch keine Bewertungen
- Haematinics & ErythropoietinDokument30 SeitenHaematinics & ErythropoietinManikanta GupthaNoch keine Bewertungen
- Vitamin B12 Properties and MetabolismDokument7 SeitenVitamin B12 Properties and Metabolismkalaiarasi ravichandranNoch keine Bewertungen
- Haematinic DeficienciesDokument7 SeitenHaematinic DeficienciesFrancesca Li100% (1)
- Nutrition in Anemia: Dr. Marlina Dewiastuti MkesDokument37 SeitenNutrition in Anemia: Dr. Marlina Dewiastuti MkesPrimarini RiatiNoch keine Bewertungen
- Anti-Anemic Drugs - 210619200800Dokument40 SeitenAnti-Anemic Drugs - 210619200800Yohannes MeridNoch keine Bewertungen
- Water Soluble Vitamins1Dokument9 SeitenWater Soluble Vitamins1kim mimiNoch keine Bewertungen
- Folate and Vitamin B12Dokument10 SeitenFolate and Vitamin B12KubilNoch keine Bewertungen
- Vitamin b12, Folic Acid, and TheDokument4 SeitenVitamin b12, Folic Acid, and TheFAZRI MONoch keine Bewertungen
- Folate Metabolism and Macrocytic Anaemia: by DR (MRS) Baulch E.KDokument49 SeitenFolate Metabolism and Macrocytic Anaemia: by DR (MRS) Baulch E.KPrincewill SeiyefaNoch keine Bewertungen
- Ow Q 1-50 (20 - 28.10.09)Dokument90 SeitenOw Q 1-50 (20 - 28.10.09)PradeepNoch keine Bewertungen
- VitaminDokument32 SeitenVitaminmohammed aliNoch keine Bewertungen
- Biochemical Basis of Phenylketonuria and Maple Syrup SyndromeDokument5 SeitenBiochemical Basis of Phenylketonuria and Maple Syrup SyndromeLauraTomicNoch keine Bewertungen
- Causes and Early Diagnosis of Vitamin B12 DeficiencyDokument7 SeitenCauses and Early Diagnosis of Vitamin B12 DeficiencytoobaziNoch keine Bewertungen
- Macrocytic AnemiasDokument49 SeitenMacrocytic Anemiasdr_asr100% (1)
- Lac operon regulation and polyol pathway in diabetesDokument38 SeitenLac operon regulation and polyol pathway in diabetesAnonymous lLiWgjFiNoch keine Bewertungen
- Antihipertension Drugs Revise 2010Dokument71 SeitenAntihipertension Drugs Revise 2010YeniNoch keine Bewertungen
- 2007 Guidelines For The Management of Arterial European Heart AssossDokument75 Seiten2007 Guidelines For The Management of Arterial European Heart AssossYeniNoch keine Bewertungen
- Film Session Grey's AnatomyDokument4 SeitenFilm Session Grey's AnatomyYeniNoch keine Bewertungen
- Lo w1Dokument12 SeitenLo w1YeniNoch keine Bewertungen
- Physical Examination of Cardiovascular: DR - Ira Andaningsih SPJP Cardiovascular Block 2008Dokument89 SeitenPhysical Examination of Cardiovascular: DR - Ira Andaningsih SPJP Cardiovascular Block 2008YeniNoch keine Bewertungen
- Erythropoiesis and Bilirubin Metabolism: V. Sutarmo SetiadjiDokument16 SeitenErythropoiesis and Bilirubin Metabolism: V. Sutarmo SetiadjiYeniNoch keine Bewertungen
- History TakingDokument28 SeitenHistory TakingYeniNoch keine Bewertungen
- 2010 CHEP - RecommendationsDokument5 Seiten2010 CHEP - RecommendationsArdhito BudhijuwonoNoch keine Bewertungen
- The Overview of Hypertension 2009Dokument50 SeitenThe Overview of Hypertension 2009YeniNoch keine Bewertungen
- Rational Drug Treatment2011Dokument27 SeitenRational Drug Treatment2011YeniNoch keine Bewertungen
- Print-Slide DR DinaDokument4 SeitenPrint-Slide DR DinaYeniNoch keine Bewertungen
- Print-Slide DR DinaDokument4 SeitenPrint-Slide DR DinaYeniNoch keine Bewertungen
- Anemia UPHDokument24 SeitenAnemia UPHYeniNoch keine Bewertungen
- Appropriate Use of Tests For Folate and Vitamin B12 DeficiencyDokument4 SeitenAppropriate Use of Tests For Folate and Vitamin B12 DeficiencyYeniNoch keine Bewertungen
- Anemia ClinskillDokument15 SeitenAnemia ClinskillYeniNoch keine Bewertungen
- Erythrocyte Life Cycle: PathophysiologyDokument15 SeitenErythrocyte Life Cycle: PathophysiologyYeniNoch keine Bewertungen
- Anemia, Rhesus and Blood Group Incompatibility inDokument42 SeitenAnemia, Rhesus and Blood Group Incompatibility inYeniNoch keine Bewertungen
- Anemia FarmakoDokument28 SeitenAnemia FarmakoYeniNoch keine Bewertungen
- Dr. Haryanto - Kuliah Anemi Deff Fe 2011Dokument20 SeitenDr. Haryanto - Kuliah Anemi Deff Fe 2011YeniNoch keine Bewertungen
- Clinical Approach to AnemiaDokument23 SeitenClinical Approach to AnemiaYeniNoch keine Bewertungen
- Plenary Lecture Multiple Trauma by FredaDokument19 SeitenPlenary Lecture Multiple Trauma by FredaYeniNoch keine Bewertungen
- Syncope VonnyDokument41 SeitenSyncope VonnyYeniNoch keine Bewertungen
- Nosocomial Infection UphDokument77 SeitenNosocomial Infection UphYeniNoch keine Bewertungen
- Head InjuryDokument40 SeitenHead InjuryYeniNoch keine Bewertungen
- Tabel AntibiotikDokument5 SeitenTabel AntibiotikYeniNoch keine Bewertungen
- Week 4 - Fungi Effector Mechanism of IRDokument67 SeitenWeek 4 - Fungi Effector Mechanism of IRYeniNoch keine Bewertungen
- Syncope VonnyDokument41 SeitenSyncope VonnyYeniNoch keine Bewertungen
- Anti VirusDokument36 SeitenAnti VirusYeniNoch keine Bewertungen
- Nosocomial Infection UphDokument77 SeitenNosocomial Infection UphYeniNoch keine Bewertungen
- Assessment of The Thorax and LungsDokument108 SeitenAssessment of The Thorax and LungsJohn Martin Casihan100% (3)
- The Paleopathology of Specific Infectious Diseases From Southeastern Hungary: A Brief OverviewDokument6 SeitenThe Paleopathology of Specific Infectious Diseases From Southeastern Hungary: A Brief OverviewLucía Chavarría RíosNoch keine Bewertungen
- Career Map - DoctorDokument7 SeitenCareer Map - DoctorAdityaNoch keine Bewertungen
- Fixed Prosthodontic Ii: Department of Fixed ProsthodonticsDokument70 SeitenFixed Prosthodontic Ii: Department of Fixed Prosthodonticsعبد الرحمن خالد الزميليNoch keine Bewertungen
- The Privacy Isuues of AppleDokument7 SeitenThe Privacy Isuues of Applephysicser15Noch keine Bewertungen
- Impaired Gas Exchange NCPDokument1 SeiteImpaired Gas Exchange NCPCj AlconabaNoch keine Bewertungen
- SRJI 4-3-2015 Historical Roots of Acupressure Pillows PatentsDokument4 SeitenSRJI 4-3-2015 Historical Roots of Acupressure Pillows PatentsDr. Krishna N. SharmaNoch keine Bewertungen
- pg42-44 Aesthetic Layering PDFDokument2 Seitenpg42-44 Aesthetic Layering PDFAing MaungNoch keine Bewertungen
- Cardiac Case Study NDDokument11 SeitenCardiac Case Study NDapi-313165458Noch keine Bewertungen
- Antibiotic Pocket GuideDokument19 SeitenAntibiotic Pocket GuideNaomi Liang100% (1)
- Nursing Skills Checklist - RTDokument6 SeitenNursing Skills Checklist - RTapi-309674272Noch keine Bewertungen
- Nursing Care of a Patient with Hypovolemic ShockDokument46 SeitenNursing Care of a Patient with Hypovolemic ShockBianca MaeNoch keine Bewertungen
- Complete Genetics Disease ChartDokument14 SeitenComplete Genetics Disease ChartJames FlanneryNoch keine Bewertungen
- Basic ImmunologyDokument2 SeitenBasic ImmunologyadibwanNoch keine Bewertungen
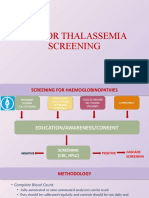
- Sop For Thalassemia Screening Wwith NbsDokument11 SeitenSop For Thalassemia Screening Wwith NbsUMMID WashimNoch keine Bewertungen
- Upper Extremity Venous Doppler Ultrasound PDFDokument12 SeitenUpper Extremity Venous Doppler Ultrasound PDFLayla Salomão0% (1)
- Ebp Picc Line - RevisedDokument6 SeitenEbp Picc Line - Revisedapi-234544335Noch keine Bewertungen
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDokument6 SeitenSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedNoch keine Bewertungen
- Brain injury patterns in hypoxiaDokument7 SeitenBrain injury patterns in hypoxiaDr.Deepak S MD,MRCPCHNoch keine Bewertungen
- NCP KoDokument1 SeiteNCP Kojiellianemae100% (1)
- Studies On The Stability of Chicken IgY in Different Sugars Complex Carbohydrates and Food MaterialsDokument12 SeitenStudies On The Stability of Chicken IgY in Different Sugars Complex Carbohydrates and Food MaterialsJohnrel SecretariaNoch keine Bewertungen
- Brain 101 Info (Merged) PDFDokument186 SeitenBrain 101 Info (Merged) PDFrosyuaNoch keine Bewertungen
- McGlamry's Forefoot SurgeryDokument629 SeitenMcGlamry's Forefoot SurgeryPourrielNoch keine Bewertungen
- Mcintyre, John 04/13/1990 Patient ReportDokument7 SeitenMcintyre, John 04/13/1990 Patient ReportJohn McIntyreNoch keine Bewertungen
- Effectiveness of Structured Teaching Program On Knowledge and Practice-FormatDokument7 SeitenEffectiveness of Structured Teaching Program On Knowledge and Practice-FormatAtul PrabhuNoch keine Bewertungen
- Skills Math WorksheetDokument4 SeitenSkills Math WorksheetBrennan MaguireNoch keine Bewertungen