Beruflich Dokumente
Kultur Dokumente
199 Full
Hochgeladen von
Ella Violettania STabilloOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
199 Full
Hochgeladen von
Ella Violettania STabilloCopyright:
Verfügbare Formate
Clinical Chemistry 45:2 199 205 (1999)
Enzymes and Protein Markers
Simultaneous Rapid Measurement of Whole Blood Myoglobin, Creatine Kinase MB, and Cardiac Troponin I by the Triage Cardiac Panel for Detection of Myocardial Infarction
Fred S. Apple,1* Robert H. Christenson,2 Roland Valdes, Jr.,3 Alexander J. Andriak,3 Amy Berg,1 Show-Hong Duh,2 Yue-Jin Feng,4 Saeed A. Jortani,3 Nancy A. Johnson,3 Brenda Koplen,1 Kristin Mascotti,1 and Alan H.B. Wu4
This multicenter study evaluated the Biosite Triage Cardiac Panel as a quantitative, multimarker, whole blood system for the detection of acute myocardial infarction (MI). Optimum cutoffs for the discrimination of acute MI (n 192 patients, 59 with MI) as determined by ROC curve analyses were as follows: 0.4 g/L for cardiac troponin I (cTnI); 4.3 g/L for the creatine kinase MB isoenzyme (CK-MB); and 107 g/L for myoglobin. The Triage Panel showed the following concordances for detection or rule-out of MI compared with established devices: cTnI >89%; CK-MB >81%; myoglobin >69%. No significant differences were present between methods for the same marker. Diagnostic efficiencies demonstrated comparable sensitivities and specificities for the diagnosis of MI in patients presenting with symptoms compared with the Dade, Beckman, and Behring CK-MB, cTnI, and myoglobin assays; the ratio of sensitivity to specificity for each marker was as follows: cTnI, 98%:100%; CK-MB, 95%:91%; myoglobin, 81%:92%. The areas under the ROC curves for the Biosite myoglobin, CK-MB, and cTnI were 0.818, 0.905, and 0.970, respectively; the areas were significantly different, P <0.05. In patients with skeletal muscle injury and renal disease, the Triage cTnI showed 94%
and 100% specificity, respectively. The Triage panel offers clinicians a whole blood, point-of-care analysis of multiple cardiac markers that provides excellent clinical sensitivity and specificity for the detection of acute MI. Serial measurement of biochemical markers is now accepted universally as an important determinant in ruling in or ruling out acute myocardial infarction (MI)5 (1, 2 ). Early markers such as myoglobin demonstrate excellent, early negative predictive value (approaching 100% within 2 h of admission) for ruling out MI (3, 4 ). The model described by the Heart Emergency Room (ER) Program (5 ) documented that serial testing for the creatine kinase MB isoenzyme (CK-MB, EC 2.7.3.2) mass on presentation and 3, 6, and 9 h later in patients with symptoms suggestive of acute ischemic coronary syndrome presenting with a nondiagnostic or equivocal electrocardiogram was more effective (100% sensitivity with 100% negative predictive value) than continuous serial electrocardiograms, echocardiography, and graded exercise testing. Recently, researchers have demonstrated that cardiacspecific troponin I (cTnI) and troponin T (cTnT) have similar usefulness for the detection of acute MI compared with CK-MB (4, 6 ), suggesting that serial testing of either cTnI or cTnT could replace CK-MB for the detection of acute MI (4, 79 ) In addition, although CK-MB has demonstrated significant benefit in risk stratification in patients presenting with unstable angina (10 ), the cardiac troponins have shown to be more powerful in identifying patients at risk (1114 ).
1 Department of Laboratory Medicine and Pathology, Hennepin County Medical Center, Minneapolis, MN 55415. 2 Departments of Pathology and Medical Research Technology, University of Maryland School of Medicine, Baltimore, MD 21201. 3 Department of Pathology and Laboratory Medicine, University of Louisville, School of Medicine, Louisville, KY 40292. 4 Department of Pathology, Hartford Hospital, Hartford, CT 06102. *Address correspondence to this author at: Hennepin County Medical Center, Clinical Laboratories No. 812, 701 Park Ave., Minneapolis, MN 55415. Fax 612-904-4229; e-mail fred.apple@co.hennepin.mn.us. Received February 2, 1998; revision accepted November 17, 1998.
5 Nonstandard abbreviations: MI, myocardial infarction; ER, Emergency Room; CK-MB, creatine kinase MB isoenzyme; cTnI, cardiac troponin I; cTnT, cardiac troponin T; and CI, confidence interval.
199
200
Apple et al.: Simultaneous Whole Blood Measurement of Cardiac Markers
To date, all quantitative laboratory-based instrumentation provides measurement of biochemical markers of myocardial injury as discrete single tests after separation of serum or plasma from whole blood. The use of a panel of tests that includes an early marker such as myoglobin or CK-MB mass, and a cardiac-specific marker such as cTnI, may offer clinicians more information for ruling in or ruling out acute MI. The purpose of this study was to clinically evaluate the Triage Cardiac Panel (Biosite Diagnostics) for the quantitative simultaneous measurement of myoglobin, CK-MB mass, and cTnI in heparintreated whole blood and plasma in patients with chest pain to rule in or rule out acute MI.
Materials and Methods
This clinical evaluation, performed to collect data for submission to the Food and Drug Administration for 510K approval of the Triage Cardiac Panel (Triage), occurred at four clinical laboratory locations: Hennepin County Medical Center, Minneapolis, MN; Hartford Hospital, Hartford, CT; the University of Louisville Medical Center, Louisville, KY; and the University of Maryland Medical Center, Baltimore, MD. Modified WHO criteria were used to differentiate patients presenting with chest pain associated with acute MI from those presenting with other, noncardiac causes; two of the following criteria needed to be met: chest pain or discomfort for a duration of at least 20 min; electrocardiogram changes consistent with MI, defined as ST-segment deviation (ST-segment depression or elevation 0.1 mV on at least two contiguous leads) or new symmetric T wave inversions 0.1 mV or both; and changes in serial plasma or serum protein markers (CK-MB or cTnI) associated with MI (2, 7 ). Temporal changes in protein markers were defined as follows: increased concentrations above the decision thresholds limit or an increase of at least 50% over time if within the reference limits. Each of the four participating sites individualized their marker criteria, using the following preestablished decision thresholds: cTnI (Dade Stratus), 1.5 g/L (4, 15 ); cTnI (Behring Opus), 2.5 g/L (16 ); cTnI (Beckman Access), 0.15 g/L (15 ); CK-MB mass (Dade Stratus), 5.0 g/L (7, 15 ) or 4.0 g/L (8 ); CK-MB mass (Beckman Access), 7.5 g/L (15 ); and myoglobin (Dade Stratus), 110 g/L (recommended in manufacturers package insert). Clinicians were blinded to the results of the Triage Panel. Patients (n 192) experiencing symptoms of acute MI admitted through the ER were entered into the study. Specimens (n 170) were obtained from 59 (31%) patients diagnosed with acute MI, of which 37 were Q-wave MIs. The median (25th75th percentile) time for admission following onset of chest pain was 7.0 h (3.8 10.8 h). An additional 262 samples from the 133 patients excluded from MI were also obtained. Adequate specimens for the Triage analysis were not available in 50 patients for more than one sampling in the non-AMI patients, a limitation of the study. This group included patients with unstable
angina, coronary artery disease, and other causes for chest pain, but with MI ruled out. Serial whole blood or plasma specimens were collected at admission and at 6- to 8-h intervals for the first 12 to 24 h. In addition, collections were obtained randomly up to 72 h. Comparison diagnostic efficiency and correlation studies of the Triage device with the three other systems used the following number of patient samples: Dade Stratus, n 366; Beckman Access, n 252; and Behring OPUS, n 332. To investigate possible nonspecificity in patients with skeletal muscle disease or renal disease, we examined an additional 189 specimens from 117 patients with acute or chronic skeletal muscle injury or disease and 80 specimens from 80 patients with end-stage renal failure undergoing chronic hemodialysis. The device evaluated, the Triage Cardiac Panel, is a self calibrating fluorescence immunoassay system for the quantitative determination of myoglobin, CK-MB mass, and cTnI and is optimized for heparin-treated whole blood and plasma specimens (17, 18 ). Serum is not an acceptable specimen. Briefly as taken from the manufacturers package insert, after addition of the sample (six drops) to the sample port, the cells are separated from the plasma via a filter contained in the device. A predetermined quantity of plasma is allowed to react with fluorescent antibody conjugates within the reaction chamber. After incubation, the reaction mixture flows down the device detection lane. Complexes of the analytes and fluorescent antibody conjugates are captured on discrete zones, producing binding assays that are specific for each analyte. The concentration of each analyte, directly proportional to the fluorescence detected, is measured by the Triage meter. All results are available in 15 min. If whole blood or plasma testing was not performed within 24 h, plasma was stored frozen at 20 C until tested. No studies were performed to test for marker stability beyond 24 h in the present study. The external qualitycontrol solutions provided consist of a Cardiac Calibration Verification Control Set at three concentrations in a plasma pool and a Cardiac Control Set at two concentrations in an artificial matrix solution. In addition to the external quality-control sets, each Triage device contains two positive device controls, which are immunoassays and perform in the same manner as the specific assays being measured. The positive device control immunoassays comprise an antibody fluorescent conjugate and a ligand fluorescent conjugate. These conjugates bind to complementary ligand and antibody solid-phase zones, respectively, to provide specific fluorescence values at each zone. The device low-control assay is set to correspond approximately to the fluorescence signal generated at the analyte decision cutoff. The device high-control assay corresponds to a fluorescence signal at 75% of the maximum signal of the doseresponse curve. If either of the two internal controls fail, the test must be repeated. Furthermore, the meter has the following capabilities: quality-control requirements programmed into the instru-
Clinical Chemistry 45, No. 2, 1999
201
Fig. 1. ROC curves for cTnI (), CK-MB (), and myoglobin (f) plotted through decision intervals in the range of concentrations (g/L) representing peak values within 24 h after presentation for patients with acute MI.
The arrows indicate optimal decision cutoffs: myoglobin, 107 g/L; CK-MB, 4.3 g/L; and cTnI, 0.4 g/L.
ment, lock-outs for unauthorized personnel, and a laboratory information system interface (as stated by the manufacturer). The lowest detectable limits for the Triage were as follows: myoglobin, 2.7 g/L; CK-MB, 0.75 g/L; and cTnI, 0.19 g/L. Imprecision as determined in the present study of all analytes at the upper reference
limit/decision cutoff concentration, was as follows: 9.9% for myoglobin; 12% for CK-MB; and 12% for cTnI. Although not tested in this study, the manufacturer claims that all types of cTnI (free and complexed) are measured by the cTnI assay. The Triage decision cutoff concentrations were 107 g/L for myoglobin, 4.3 g/L for CK-MB,
Table 1. Clinical sensitivities and specificities for Triage Cardiac Panel markers, based on serial samplings for 192 patients grouped according to time after presentation to ER for MI detection.a
Sensitivity, % Sensitivity 0 to <6 h 6 to <12 h 12 to <24 h >24 to 72 h
cTnI 95% CI CK-MB 95% CI Myoglobin 95% CI Seriesb 95% CI Parallelc 95% CI
65.0 50.279.8 77.5 64.690.4 75.0 61.688.4 52.5 37.068.0 87.5 77.397.7
71.9 56.387.5 78.1 63.592.4 75.0 60.090.0 53.1 35.870.4 90.6 80.5100
Specificity, %
93.2 85.7100 79.5 67.691.5 72.7 59.685.9 61.4 47.075.8 97.7 93.3100
97.2 91.9100 94.4 87.0100 61.1 45.277.0 60.4 50.470.5 98.9 96.8100
cTnI 95% CI CK-MB 95% CI Myoglobin 95% CI Series 95% CI Parallel 95% CI
a b
100 100100 91.0 85.197.0 74.2 65.183.3 100 100100 67.4 57.777.2
97.0 92.8100 86.4 88.196.6 81.8 72.591.1 98.5 95.5100 72.7 62.083.5
94.4 89.799.2 82.2 74.390.1 67.8 58.177.4 97.8 94.7100 58.9 48.769.1
95.6 93.397.8 87.0 83.390.7 73.4 68.578.3 98.6 95.9100 64.8 53.775.9
Upper reference limits used for calculations were as follows: cTnI, 0.4 g/L; CK-MB, 4.3 g/L; myoglobin, 107 g/L. Series: myoglobin CK-MB TnI. c Parallel: myoglobin or CK-MB, or cTnI.
202
Apple et al.: Simultaneous Whole Blood Measurement of Cardiac Markers
and 0.4 g/L for cTnI, as determined by ROC curve analysis (see Results). Statistical comparisons of myoglobin, CK-MB, and cTnI between times and between analyzers were performed by one-way and two-way ANOVA. Statistical significance was set at P 0.05, using nonparametric MannWhitney statistics. ROC curve analysis was performed as described previously (19 ) using True Epistat, Ver. 5. The McNemar test was also used for comparison of diagnostic sensitivity and specificity data between markers or assays; P 0.05 was considered statistically significant. Diagnostic sensitivity and specificity data are presented with 95% confidence intervals (CIs), determined with the Epistat, Ver. 5. Spearman correlation coefficients were calculated between the Triage and comparison methods.
Results
The ROC curve analysis for myoglobin, CK-MB, and cTnI for determination of decision cutoff values for all 192 patients on the basis of peak concentrations over a 24-h period after admission are shown in Fig. 1; the cutoffs were 107 g/L for myoglobin, 4.3 g/L for CK-MB, and 0.4 g/L for cTnI. The areas under the ROC curves (with 95% CIs) for myoglobin, CK-MB, and cTnI were 0.819 (0.779 0.854), 0.905 (0.874 0.910), and 0.961 (0.931 0.979), respectively, and were significantly different, P 0.05. Regression analysis of Triage panel results across the dynamic range of each assay compared with established assay measurements showed the following correlations: Triage cTnI 0.40(Stratus cTnI) 0.06, r 0.952, n 56; Triage CK-MB 0.78(Access CK-MB) 2.96, r 0.957, n 65; Triage myoglobin 1.25(Stratus myoglobin) 38.8, r 0.943, n 119. Clinical sensitivities and specificities (with 95% CIs) are shown in Table 1 for serial samplings for all patients. The Triage device showed no significant clinical sensitivity differences for cTnI, as demonstrated in Table 1 and Fig. 2A, and for CK-MB, as demonstrated in Fig. 2B, over several time intervals when compared with the other established devices. However, the Triage device and the Beckman Access demonstrated a significantly increased sensitivity (P 0.05) for cTnI at 4 h when compared with the sensitivity for cTnI in the Dade and Behring devices (Fig. 2A). The Triage device demonstrated 89% concordance for cTnI, 81% concordance for CK-MB, and 69% concordance for myoglobin when compared with established devices, with no statistical differences in ruling in and ruling out MI. Because results for all three markers become available simultaneously on the Triage device, we examined whether the panel could provide improved early (4 h) diagnostic information when compared with individual test results. When clinical sensitivities were determined on peak concentrations or over the entire sampling period in serial (cTnI plus CK-MB plus myoglobin) or parallel (cTnI, CK-MB, or myoglobin), neither approach showed
Fig. 2. Sensitivity (with 95% CI bars) for cTnI (A) and CK-MB mass (B) for acute MI time intervals grouped according to time after onset of symptoms.
At 0 to 4 h, the Biosite () and Beckman () results for cTnI were significantly different compared with the Dade (f) and Behring (E) results; (), P 0.05 .
significant improvement compared with individual test results for either cTnI or CK-MB (Table 1). Table 1 also shows that the Triage cTnI demonstrated 95100% specificity over the entire 24-h period after admission. In comparison, CK-MB demonstrated 8291% specificity, and myoglobin demonstrated 67 81% specificity. Fig. 3 shows time vs concentration profiles for acute MI patients, comparing the Triage cTnI assay with the Dade and Behring cTnI assays. Although serial specimen patterns demonstrated the parallel rise after acute MI, the absolute concentrations showed differences between as-
Clinical Chemistry 45, No. 2, 1999
203
Fig. 3. cTnI concentrations for specimens collected from four MI patients having samples collected over a 24-h period after onset of chest pain.
(A), patient 1; (B), patient 2; (C), patient 3; (D), patient 4. Data presented are absolute concentrations for the Dade (f) and Behring (E) cTnI assays compared with the Biosite () cTnI assay.
says, underlying the need to validate each system independently. Fourteen patients (10.5% of all non-MI patients) with a non-MI final discharge diagnosis had at least one increased Triage cTnI concentration after admission, with cTnI ranging from 0.42 to 5.40 g/L. These included patients with the following diagnoses: unstable angina (n 4), coronary artery disease (n 3), congestive heart failure (n 3), and noncardiac chest pain (n 4). In patients with skeletal muscle injury, cTnI showed a clinical specificity of 94% compared with 44% for CK-MB and 21% for myoglobin. The nine samples that demonstrated an increased Triage cTnI without documented cardiac injury were from patients admitted after skeletal muscle trauma caused by automobile accidents and noncardiac
surgery. In patients with renal disease, cTnI showed a clinical specificity of 100%, compared with 79% for CK-MB and 16% for myoglobin.
Discussion
This study demonstrated that the rapid, whole blood Triage device, which simultaneously quantifies several biochemical markers of myocardial injury, was comparable to established devices for the detection of acute MI. Our data show that simultaneous measurement of myoglobin, CK-MB mass, and cTnI in patients presenting with chest pain has excellent concordance for cTnI and CK-MB when compared with each individually measured marker for both ruling in and ruling out acute MI. Sensitivity
204
Apple et al.: Simultaneous Whole Blood Measurement of Cardiac Markers
calculations for the Triage Cardiac Panel demonstrated the expected temporal increases over the 24-h period after admission, with 90% sensitivity for cTnI and CK-MB at peak concentrations. cTnI, a cardiac-specific protein that is challenging CK-MB mass as a new reference marker for MI detection, demonstrated absolute concentration differences when compared with cTnI measurements performed on the Dade Stratus, Beckman Access, and Behring Opus (Fig. 3). The two- to fourfold differences between assays substantiate the need to compare relative increases above respective reference limits for individual cTnI assays until appropriate standardization can be obtained. This lack of standardization also underlines the need for individual laboratories and hospitals to establish their own decision cutoff concentrations for cTnI as well as for CK-MB, as was done for this study. The diagnostic specificity of the Triage Cardiac Panel was also highly concordant with the other systems in this comparison study, demonstrating maximum clinical specificities for CK-MB and cTnI of 91% and 100%, respectively. When non-MI populations, including patients with skeletal muscle injury and patients with chronic renal disease, were evaluated, cTnI specificity was substantially improved compared with CK-MB. Of the non-MI patients with underlying cardiac pathologies, 14 patients showed increased cTnI concentrations. In this population, which included patients with unstable angina and congestive heart failure, increased concentrations of cTnI have become a risk stratification tool, prompting clinicians to consider a more aggressive management regimen because of poor prognostic outcomes at 30 42 days after presentation (1114 ). It should be noted that some of these studies use admission serum values when assessing outcomes, whereas others use peak serum values after serial sampling of cardiac markers. The present study was not designed to assess outcomes, and no patient follow up was obtained. In addition to CK-MB mass and cTnI, myoglobin concentrations are also obtained on the Triage Panel. Although not cardiac specific, myoglobin is one of the very early markers to increase after acute MI (3, 4, 20 ). Although studies have demonstrated 95% sensitivity within 4 h after admission for ruling in acute MI (13, 17 ), the sensitivity of the Triage Panel for myoglobin only approached 75 80%. The most likely explanation for the lower sensitivity of the Triage myoglobin assay (as well as for the Dade Stratus myoglobin assay, data not shown) in this study might be related to the patient population studied and the accuracy of the length of time from onset of chest pain to admission, which was estimated on the basis of histories taken at admission, always a confounding issue. However, we have no definite explanation for the lower sensitivities observed. The poor specificity for myoglobin in large populations of chest pain patients presenting with noncardiac chest pain (3, 20 ) was substantiated in the present study with a specificity of 80%. Several patients in our study experienced skeletal muscle
trauma and injury concomitant with chest pain. Furthermore, we are unable to explain the concordance of only 70% for the Triage myoglobin assay. This study does not address either the role of cardiac markers in reinfarction patients or in patients with acute MI presenting more than 72 h after the onset of chest pain. Clinical trials need to be designed to address both of these issues to determine whether a multiple-marker approach would offer cost benefits for improved patient diagnosis and treatment. The Triage Cardiac Panel and device (both Food and Drug Administration approved) offer clinicians quantitative whole blood analysis of multiple cardiac markers and can serve as a point-of-care testing device in the ER, the coronary care unit, or at the bedside. The Triage Panel will compete directly with qualitative positive/negative bedside tests for cTnI and cTnT that have demonstrated high sensitivity for the detection of acute MI after 6 h, with negative results associated with low risk and safe discharge of patients with an episode of acute chest pain (21 ). Neither serial nor parallel analysis of the multiple markers provided increased sensitivity or specificity for detection or ruling out of MI (Table 1). However, this study was not designed to address this issue. Outcome studies should be conducted to confirm whether the multiple marker approach or noncentralized laboratory measurements of these markers will be cost-effective or time-saving devices that will assist clinicians in more rapid or appropriate management and patient therapy.
This study was funded in part by Biosite Diagnostics, San Diego, CA.
References
1. Adams JE III, Abendschein DR, Jaffe AS. Biochemical markers of myocardial injury. Circulation 1993;88:750 63. 2. Tunstall-Pedoe H, Kuulasmaa K, Annouyel P, Arveiler D, Rajakangas AM, Pajak A. The WHO MONICA project. Myocardial infarction and coronary deaths in the World Health Organization MONICA project. Circulation 1994;90:588 612. 3. Montague C, Kircher T. Myoglobin in the early evaluation of acute chest pain. Am J Clin Pathol 1995;104:472 6. 4. Tucker JF, Collins RA, Anderson AJ, Hauser J, Kalas J, Apple FS. Early diagnostic efficiency of cardiac troponin I and troponin T for acute myocardial infarction. Acad Emerg Med 1997;4:1321. 5. Gibler WB, Runyon JP, Levy RC, Sayre MR, Kacich R, Hattemer CR, et al. A rapid diagnostic and treatment center for patients with chest pain in the Emergency Department. Ann Emerg Med 1995; 25:1 8. 6. Muller-Bardorff M, Hallermayer K, Schroder A, Ebert C, Gerhardt W, Katus HA. Improved troponin T ELISA specific for cardiac troponin T isoform: assay development and analytical and clinical validation. Clin Chem 1997;43:458 66. 7. Apple FS, Falahati A, Paulsen PR, Miller EA, Sharkey SW. Improved detection of minor ischemic myocardial injury with measurement of serum cardiac troponin I. Clin Chem 1997;43:204751. 8. Brogan GX, Hollander JE, McCuskey CF, Thode HC, Snow J, Sama A, et al. Evaluation of a new assay for cardiac troponin I vs creatine
Clinical Chemistry 45, No. 2, 1999
205
9.
10.
11.
12.
13.
14.
15.
kinase MB for the diagnosis of acute myocardial infarction. Acad Emerg Med 1997;4:6 12. Mair J, Dienstl F, Puschendorf B. Cardiac troponin T in the diagnosis of myocardial injury. Crit Rev Clin Lab Sci 1992;29: 3157. Ravkilde J, Nissen H, Horder M, Thygesen K. Independent prognostic value of serum creatine kinase isoenzyme MB mass, cardiac troponin T, and myosin light chain levels in suspected acute myocardial infarction. J Am Coll Cardiol 1995;25:574 81. Galvani M, Ottari F, Ferrini D, Ladenson JH, Destro A, Baccos D, et al. Prognostic influence of elevated values of cardiac troponin I in patients with unstable angina. Circulation 1997;95:20539. Ohman EM, Armstrong PW, Christenson RH, Granger CB, Katus HA, Hamm CW, et al. Cardiac troponin T levels for risk stratification in acute ischemia. N Engl J Med 1996;335:133 41. Stubbs P, Collinson P, Moseley D, Greenwood R, Noble M. Prognostic significance of admission troponin T concentrations in patients with myocardial infarction. Circulation 1996;94:12917. Antman EM, Tanasijevic MJ, Thompson B, Schactman M, McCabe CH, Cannon CP, et al. Cardiac specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996;335:13429. Christenson RH, Apple FS, Morgan DL, Alonsozana GL, Mascotti K, Olson M, et al. Cardiac troponin I measurement with the
16.
17.
18.
19.
20.
21.
ACCESS immunoassay system: analytical and clinical performance characteristics. Clin Chem 1998;44:52 60. Wu AHB, Feng YJ, Copntois JH, Pervaiz S. Comparison of myoglobin, creatine kinase MB and cardiac troponin I for the diagnosis of acute myocardial infarction. Ann Clin Lab Sci 1996;26:291300. Buechler KF, Dwyer BP, Noar B, Tadesse L, Moi S. A fluorescence energy transfer detection system for immunoassays of biological samples [Abstract]. Clin Chem 1997;43:5136. McPherson PH, Anderberg JM, Lesefko SM, Fiechtner MD, Sundquist AR, Dwyer BP, et al. A rapid, quantitative point-of-care assay system for the simultaneous measurement of CK-MB troponin I, and myoglobin in blood [Abstract]. Clin Chem 1998; 44:A116. Beck JR, Shultz EK. The use of relative operating characteristic (ROC) curves in test performance evaluation. Arch Path Lab Med 1996;110:1320. Davis CP, Barrett K, Torre P, Wacasay K. Serial myoglobin levels for patients with possible myocardial infarction. Acad Emerg Med 1996;3:590 7. Hamm CW, Goldmann BU, Heeschen C, Kregmann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T on troponin I. N Engl J Med 1997;337:1648 53.
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- BIO 211 Chapter 18 AssignmentDokument20 SeitenBIO 211 Chapter 18 Assignmentf1l2o3r4e5n6Noch keine Bewertungen
- Ok - Effect of Melatonin On Broiler ChicksDokument12 SeitenOk - Effect of Melatonin On Broiler ChicksOliver TalipNoch keine Bewertungen
- Feeling GreatDokument243 SeitenFeeling GreatSunny LamNoch keine Bewertungen
- AQ4PDokument3 SeitenAQ4PAhmed GaberNoch keine Bewertungen
- The Role of Radiotherapy in Cancer TreatmentDokument9 SeitenThe Role of Radiotherapy in Cancer TreatmentarakbaeNoch keine Bewertungen
- Congestion Pelvica 2020Dokument6 SeitenCongestion Pelvica 2020Cristian RodríguezNoch keine Bewertungen
- Urtricaria SDokument8 SeitenUrtricaria SpalNoch keine Bewertungen
- LaparotomyDokument36 SeitenLaparotomydenekeNoch keine Bewertungen
- Cholera (5 5)Dokument1 SeiteCholera (5 5)Celestial, Maybelle MarieNoch keine Bewertungen
- All About Rabies Health ScienceDokument28 SeitenAll About Rabies Health SciencetototoNoch keine Bewertungen
- Energy Drinks Are Bad RealDokument4 SeitenEnergy Drinks Are Bad RealMadihi NorhadiNoch keine Bewertungen
- HSBDokument4 SeitenHSBCarlos WebsterNoch keine Bewertungen
- Radiotherapy in Prostate Cancer Innovative Techniques and Current ControversiesDokument288 SeitenRadiotherapy in Prostate Cancer Innovative Techniques and Current ControversiesStirNoch keine Bewertungen
- Etamsylate DS Meppo2010 PDFDokument3 SeitenEtamsylate DS Meppo2010 PDFAqmarlia PutriNoch keine Bewertungen
- Basic Math Ability Exam A Relias Graded ADokument6 SeitenBasic Math Ability Exam A Relias Graded ADebs MaxNoch keine Bewertungen
- Acid Fast StainDokument3 SeitenAcid Fast StainMartina MicicNoch keine Bewertungen
- Hypopyon in Acute Lymphoblastic Leukemia A Case ReportDokument2 SeitenHypopyon in Acute Lymphoblastic Leukemia A Case ReportInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- XXXXXX 121Dokument11 SeitenXXXXXX 121AndriantkNoch keine Bewertungen
- Teaching Plan SampleDokument3 SeitenTeaching Plan SampleSoleil MaxwellNoch keine Bewertungen
- PhobiaDokument4 SeitenPhobiaZeba QuadiriNoch keine Bewertungen
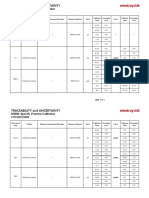
- Specific Proteins Calibrator-150721009-BS600Dokument2 SeitenSpecific Proteins Calibrator-150721009-BS600S6b2Noch keine Bewertungen
- NephrologyDokument9 SeitenNephrologyEliDavidNoch keine Bewertungen
- Gastroenterology Evaluation TemplateDokument2 SeitenGastroenterology Evaluation Templatee-MedTools86% (7)
- F Buski 111003095909 Phpapp01Dokument15 SeitenF Buski 111003095909 Phpapp01Ashik MajumdarNoch keine Bewertungen
- LESSON 3: Exercise Variables and PrinciplesDokument31 SeitenLESSON 3: Exercise Variables and PrinciplesCapulong Kimberly100% (1)
- Communicable DiseasesDokument24 SeitenCommunicable DiseasesJanus de LeonNoch keine Bewertungen
- Cancer Ozone Therapy Treatment A DiscussionDokument13 SeitenCancer Ozone Therapy Treatment A DiscussionjpgbfNoch keine Bewertungen
- Patient Information Leaflet: (Etonogestrel)Dokument4 SeitenPatient Information Leaflet: (Etonogestrel)A VHRSENoch keine Bewertungen
- An Unconscious Patient With A DNR TattooDokument2 SeitenAn Unconscious Patient With A DNR TattoonadaNoch keine Bewertungen
- Chronic Kidney DiseaseDokument22 SeitenChronic Kidney DiseaseAchmad ZainudinNoch keine Bewertungen