Beruflich Dokumente
Kultur Dokumente
Pediatric Antibiotic Dosing Card 2012
Hochgeladen von
yoshilimsiacoshigyoCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pediatric Antibiotic Dosing Card 2012
Hochgeladen von
yoshilimsiacoshigyoCopyright:
Verfügbare Formate
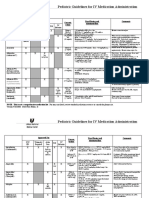
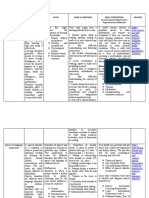
UCSF Benioff Childrens Hospital Pediatric Antimicrobial Dosing Guideline for Infants and Children > 1 Month of Age
Approved by the Antibiotic Advisory Subcommittee and the Pharmacy and Therapeutics Committee (11/98) Rev 5/2012
For assistance in antimicrobial dosing and selection, contact Infectious Diseases Pharmacy (443-9421). For diagnosis and management recommendations or formal consultation, contact Pediatric ID fellow (443-2384).
Shaded boxes indicate ID-Restricted agents (ID-R). Call ID Pharmacy (443-9421) for prior approval 8am-10pm. Orders will NOT be processed without approval (exceptions for certain agents noted in APEX). 10pm to 8am a single dose will be released; further doses require approval. Creatinine Clearance Creatinine Clearance Creatinine Clearance >50ml/min/1.73m2 10-50ml/min/1.73m2 <10ml/min/1.73m2 (ESRD not on dialysis) MAXIMUM DRUG OR OR OR DAILY DOSE Renal Function > 50% of Renal Function = 10-50% of Renal Function <10% of Normal Normal Normal
25-50% of normal clearance 5-10 mg/kg/dose q12h Non-CNS HSV infection: 5-10 mg/kg/dose q8h 10-25% of normal clearance 5-10 mg/kg/dose q24h 25-50% of normal clearance 10-20 mg/kg/dose q12h Herpes Zoster 10-20 mg/kg/dose q8h
Immunocompromised Host: Immunocompromised Host:
2.5-5 mg/kg/dose q24h
Acyclovir IV
500 mg/m2/dose q8h
500 mg/m2/dose q12h 10-25% of normal clearance 10-20 mg/kg/dose q24h
Immunocompromised Host:
5-10 mg/kg/dose q24h
Immunocompromised Host:
250 mg/m2/dose q24h
500 mg/m2/dose q24h 25-50% of normal clearance 20mg/kg/dose q12h HSV encephalitis, all neonatal infections: 20mg/kg/dose q8h
Immunocompromised Host: Immunocompromised Host:
500 mg/m2/dose q12h 10-25% of normal clearance 20mg/kg/dose q24h
Immunocompromised Host:
10mg/kg/dose q24h
Immunocompromised Host:
250 mg/m2/dose q24h
500 mg/m /dose q8h
500 mg/m2/dose q24h Amphotericin B Liposomal* (AmBisome)
*ID-R except for HemeOnc
Invasive yeast infections 3mg/kg/dose IV q24h Invasive mold infections 5mg/kg/dose IV q24h 50mg/kg/dose q6h Meningitis: 100mg/kg/dose q6h LD 70mg/m2 x1 Then 50mg/m2 q24h 25 mg/kg/dose q8h 10 mg/kg/dose PO q6-8h Otitis Media 20-25 mg/kg/dose PO q6h Osteomyelitis 25-30 mg/kg/dose PO q6h 50mg/kg/dose q12h
No change
No change
Dosage reductions in renal disease are not necessary. However, due to the nephrotoxic potential of the drug, reducing the dose or holding the drug in the setting of a rising serum creatinine may be warranted. 25mg/kg/dose q6h 50mg/kg/dose q6h No change 25 mg/kg/dose q12h 10 mg/kg/dose PO q8h-q12h 25mg/kg/dose q8-12h 2gm q4h 25mg/kg/dose q8-12h No change 25 mg/kg/dose q24h 10 mg/kg/dose PO q12-24h 70 mg 2gm q8h 4gm/day
Ampicillin IV Caspofungin Cefazolin
Cephalexin PO
>30% of normal clearance 50mg/kg/dose q12h 10-30% of normal clearance 25mg/kg/dose q24h >30% of normal clearance 50mg/kg/dose q12h 10-30% of normal clearance 50mg/kg/dose q24h Not documented 50mg/kg/dose q8h-12h 50mg/kg/dose q8h 50mg/kg/dose q12h Not documented No change No change 50mg/kg/dose q12h 10-30% of normal clearance 7.5 mg/kg/dose q12h Not documented No change No change
12.5mg/kg/dose q24h
2gm q12h
Cefepime
Febrile neutropenia: 50mg/kg/dose q8h Cystic Fibrosis: 50mg/kg/dose q8h 50mg/kg/dose q8h Meningitis: 50mg/kg/dose q6h 50mg/kg/dose q8h Cystic fibrosis: 50mg/kg/dose q8h 50mg/kg/dose q24h Meningitis: 50mg/kg/dose q12h 50mg/kg/dose q8h >30% of normal clearance 15mg/kg/dose q12h Cystic fibrosis: 15 mg/kg/dose q12h 10 mg/kg/dose IV q8h 2-8mg/kg/dose q6-8h Osteomyelitis 10-12 mg/kg/dose PO q6q8h 5-10mg/kg/dose q6h 15 mg/kg/dose q12h 13 years old: 1 gram daily 6-12mg/kg/dose q24h Fungal prophylaxis: 3mg/kg/dose q24h >80% of normal clearance 5mg/kg/dose q12h 79-50% of normal clearance 2.5mg/kg/dose q12h 2.5mg/kg/dose q8h
25mg/kg/dose q24h
2gm q8h
Not documented 25 mg/kg/dose q12h 50mg/kg/dose q12h 50mg/kg q24-48h Not documented No change No change 50mg/kg/day q24h 7.5mg/kg/dose q12h
Cystic Fibrosis: 2gm q8h 2gm q6h 2gm q8h Cystic fibrosis: 2gm q8h 1gm q24h Meningitis 2gm q12h 1.5gm q8h 400mg q12h Cystic fibrosis: 600mg q12h 900mg q8h 450mg q6h
Cefotaxime
Ceftazidime
Ceftriaxone Cefuroxime IV
Ciprofloxacin IV Not documented No change No change
Clindamycin IV
Clindamycin PO
Erythromycin IV Ertapenem Fluconazole IV/PO
No change < 30ml/min/1.73m2 Decrease dose 50% 3-6mg/kg/dose q24h 3-6mg/kg/dose q24h No change 25-50% of normal clearance 2.5mg/kg/dose q24h 10-25% of normal clearance 1.25mg/kg/dose q24h 2.5mg/kg/dose q12h No change 1.25mg/kg/dose q24h
No change
1gm q6h
400mg q24h
Ganciclovir IV
2.5mg/kg/dose q24h
Gentamicin
Imipenem Linezolid IV/PO
**consult with pharmacist for dose adjustment/level assessment** 20 mg/kg/dose q6h < 5 yo: 10mg/kg/dose q8h > 5 yo: 10mg/kg/dose q12h 20mg/kg/dose q8h
10 mg/kg/dose q6-8h No change 25-50% of normal clearance 20mg/kg/dose q12h 10-25% of normal clearance 10mg/kg/dose q12h 25-50% of normal clearance 40mg/kg/dose q12h 10-25% of normal clearance 20mg/kg/dose q12h No change
10 mg/kg/dose q12h No change 10mg/kg/dose q24h
1gm q6h 600 mg q 12h 1gm q8h
Meropenem Meningitis: 40mg/kg/dose q8h
20mg/kg/dose q24h
Meningitis: 2gm q8h
Metronidazole IV/PO
10mg/kg/dose q8h
10mg/kg/dose q12h
500mg q6h
Nafcillin
25-50mg/kg/dose q6h
No change
No change
2gm q4h
DRUG
Creatinine Clearance >50ml/min/1.73m2 OR Renal Function > 50% of Normal
Creatinine Clearance 10-50ml/min/1.73m2 OR Renal Function = 10-50% of Normal
Creatinine Clearance <10ml/min/1.73m2 (ESRD not on dialysis) OR Renal Function <10% of Normal
MAXIMUM DAILY DOSE
Penicillin G IV
Piperacillin/ Tazobactam (Zosyn )
100,000 - 250,000 units/kg/day q4-6h Severe Infection: 250,000-400,000 units/kg/day q4-6h 80mg piperacillin/kg/dose q6h-8h Cystic fibrosis: 100mg piperacillin/kg/dose q6h 10-20mg/kg/day in 1-3 divided doses see gentamicin Cystic fibrosis: Once daily dosing: 10mg/kg/dose q24h Mild to moderate systemic bacterial infection: 5mg/kg/dose TMP q12h Serious systemic bacterial infection: 5mg/kg/dose TMP q6-8h Pneumocystis carinii pneumonia prophylaxis: 2.5mg/kg/dose TMP q12h three days per week. 15mg/kg/dose q6h*
*Cardiac Dysfunction/CICU consider q8-12h
70,000-160,000 units/kg/day q8h 160,000-260,000 units/kg/day q8h 80mg piperacillin/kg/dose q8h
50,000-125,000 units/kg/day q12h 4 million units q4h 125,000-200,000 units/kg/day q8h 80mg piperacillin/kg/dose q12h Not documented No change see gentamicin Not documented
4.5gm q6h
Not documented No change see gentamicin Not documented
4.5gm q6h 600mg qday
Rifampin IV/PO
Tobramycin
TMP/SMX (Septra ) SS Tablet: 80 mg TMP DS Tablet: 160 mg TMP Oral Suspension: 40 mg TMP / 5 mL
2.5mg/kg/dose TMP q12h
2.5-5mg/kg/dose TMP q24h
5mg/kg/dose TMP q8-12h
5mg/kg/dose TMP q12-24h
2.5mg/kg/dose TMP q12h three days per week 15mg/kg/dose q8-12h
2.5mg/kg/dose TMP q24h three days per week. 15mg/kg/dose q12-24h
Prophylaxis: 160mg TMP bid 1 gram IV q8h
Vancomycin CNS/Osteo/Serious Infections: 20mg/kg/dose q6h 20mg/kg/dose q8h 20 mg/kg/dose q12h 1 gram IV q6h
Voriconazole * IV/PO
*ID-R except for HemeOnc
Peak levels are not recommended. Trough levels ( 30 min before next dose) should be 10-20 mg/L depending on the severity of infection. Specifically, 15-20 for meningitis, sepsis and pneumonia No change No change Documented infections
LD = 7mg/kg q12h x 2 doses MD = 5-7mg/kg* q12h
PO should be used when possible, as oral bioavailability > 95%.
Presumed/Empiric infection
LD = 6mg/kg q12h x 2 doses MD = 4mg/kg* q12h
The use of IV should be avoided if possible in patients with CrCl<50 mL/min due to the accumulation of the IV vehicle
*Higher doses may be required based on therapeutic drug monitoring (consultation with Pedi-ID recommended)
Estimate of Creatinine Clearance using Schwartzs equation:
CLcr = K x L/Scr (Creatinine clearance in ml/minute/1.73m 2) L = Length or height in cm K = Constant of proportionality that is age specific Scr = Serum creatinine concentration in mg/dL Age K_ Preterm infants up to 1year 0.33 Full-term infants up to 1 year 0.45 1-12 years 0.55 13-21 years female 0.55 13-21 years male 0.7 1-16 years with Chronic Kidney Disease 0.413
UCSF PEDIATRIC SUSCEPTIBILITY DATA 2011
N/A-testing NOT APPLICABLE to organism. CZOL-cefazolin, CTRX-ceftriaxone, CTAZ-ceftazidime, CFPM-cefepime, GEN-gentamicin, TOB-tobramycin, T/S-trimethoprim/sulfamethoxazole, CIP-ciprofloxacin, MER- meropenem, P/T-piperacillin-tazobactam, PCN-penicillin, NAF-nafcillin, ERY-erythromycin, CLIN-clindamycin, DOX-doxycycline, VANC-vancomycin
Total isolates include Floor Isolates and ICU Isolates from UCSF Childrens Hospital (Does not include Outpatient)
Gram-negative isolates (% strains susceptible, tested from all sites)
Organism Acinetobacter baumannii Citrobacter freundii Enterobacter aerogenes Enterobacter cloacae Escherichia coli* EColi-URINE EColi-NON URINE Klebsiella oxytoca Klebsiella pneumoniae Proteus mirabilis Pseudomonas aeruginosa** PICU+ICN PEDS Serratia marcescens Total isolates CZOL CTRX CTAZ CFPM GEN TOB T/S CIP P/T MER
4 5 5 31 68 47 25 15 19 6 34 12 23 8
N/A N/A N/A N/A 69 68 76 67 84 50 N/A N/A N/A N/A
50 40 60 56 90 91 88 100 95 100 N/A N/A N/A 88
100 40 40 55 96 98 92 100 100 100 85 83 87 100
75 100 80 100 97 98 96 100 100 100 88 83 91 100
100 80 100 91 93 96 88 100 89 100 100 100 100 100
100 80 100 91 91 94 88 93 95 100 97 100 96 100
100 80 80 78 71 74 60 100 79 50 N/A N/A N/A 100
100 80 80 91 85 89 80 100 95 100 97 100 96 100
75 60 60 72 99 98 100 100 95 100 91 83 88 88
100 100 100 100 100 100 100 100 100 100 94 92 96 100
** Pseudomonas aeruginosa isolates do not include isolates from cystic fibrosis patients
*Escherichia coli Haemophilus influenzae Stenotrophomonas maltophilia
Outpatient cefazolin/cephalexin susceptibility is 85%. Outpatient TMP/SMX susceptibility is 69%. Outpatient ciprofloxacin susceptibility is 95%. Nitrofurantoin susceptibility is 98% and should only be used for uncomplicated UTIs in patients with CrCl >60 mL/min. National incidence of -lactamase production is 37% (2010). Routine antimicrobial susceptibility testing is performed on sterile sites and cystic fibrosis isolates. TMP/SMX is the most active agent versus this organism.
Total isolates include Floor Isolates and ICU Isolates from UCSF Childrens Hospital (Does not include Outpatient)
Gram-positive isolates (% strains susceptible, tested from all sites)
Organism Staphylococcus aureus* MRSA MSSA Staphylococcus epidermidis Streptococcus pneumoniae *Staphylococcus aureus Enterococcus spp. Total Isolates 121 26 95 46 6 PCN 5 NAF 79 ERY 59 15 71 30 50 CLIN 78 64 82 57 83 CIP 83 73 73 74 DOX 94 96 93 85 67 T/S 95 92 96 65 83 VANC 100
2 See below
26
100 100
Outpatient Nafcillin susceptibility is 77% (Nafcillin resistance predicts cephalosporin resistance).
Enterococcus faecalis species are 100% ampicillin susceptible. Of 23 enterococcal bacteremias in 2011, 8 were due to Enterococcus faecium, and 5 isolates (63%) were vancomycin resistant (ie 5/23 [22%] of enterococcal bacteremias were VRE). The addition of gentamicin (1 mg/kg Q8h) is required for bactericidal activity in serious systemic enterococcal infections (e.g. endocarditis). Streptococcus pneumoniae 50% (3/6 isolates) were PCN non-susceptible. 83% (5/6) isolates were susceptible to CTRX. All isolates were susceptible to levofloxacin.
NOTE: For the treatment of meningitis, pending susceptibilities VANCOMYCIN empirically should be added to the regimen since failures (due to highly resistant isolates) have been reported with ALL third generation cephalosporins.
Das könnte Ihnen auch gefallen
- Ped Med HandbookDokument27 SeitenPed Med HandbookSoad Shedeed0% (1)
- Pediatric Cardiology and Pulmonology: A Practically Painless ReviewVon EverandPediatric Cardiology and Pulmonology: A Practically Painless ReviewNoch keine Bewertungen
- Stanford Hospital & Clinics Antimicrobial Dosing Reference Guide 2013Dokument3 SeitenStanford Hospital & Clinics Antimicrobial Dosing Reference Guide 2013SANCHOSKYNoch keine Bewertungen
- Idiot NotesDokument53 SeitenIdiot NotesRay PerezNoch keine Bewertungen
- Pediatrics Protocols - Pediatric Handbook 3rd EditionDokument25 SeitenPediatrics Protocols - Pediatric Handbook 3rd Editionklteng85Noch keine Bewertungen
- Congenital Heart Diseases, A Simple Guide to these Medical ConditionsVon EverandCongenital Heart Diseases, A Simple Guide to these Medical ConditionsNoch keine Bewertungen
- Pocket PediaeditedDokument9 SeitenPocket Pediaeditedjandale100% (1)
- NICU Standing Orders KFAFHDokument36 SeitenNICU Standing Orders KFAFHallysonviernes100% (1)
- Pharmacology of Cardiac Function: Section of Pharmacology of the International Union of Physiological SciencesVon EverandPharmacology of Cardiac Function: Section of Pharmacology of the International Union of Physiological SciencesOtto KrayerNoch keine Bewertungen
- NICU Protocol 100Dokument76 SeitenNICU Protocol 100Catherine Lee100% (1)
- Fast Dose PediatricsDokument15 SeitenFast Dose PediatricsNick Amonsull PhanuwatNoch keine Bewertungen
- Manual of Pediatric Emergency MedicineDokument28 SeitenManual of Pediatric Emergency MedicineRabi Dhakal100% (2)
- Pediatric Mechanical VentilationDokument49 SeitenPediatric Mechanical VentilationNirubhana ArunthavasothyNoch keine Bewertungen
- Pediatric Doses For Commonly Used OTCsDokument7 SeitenPediatric Doses For Commonly Used OTCsCharles Xavier KimNoch keine Bewertungen
- Quick Reference Guide Corrections 2021Dokument6 SeitenQuick Reference Guide Corrections 2021Prashin RocharamNoch keine Bewertungen
- UNC ED Pediatric Asthma ProtocolDokument2 SeitenUNC ED Pediatric Asthma ProtocolAhmed BekhetNoch keine Bewertungen
- Elsharnoby Pediatric Made Easy Up Load Waheed Tantawy 2014Dokument160 SeitenElsharnoby Pediatric Made Easy Up Load Waheed Tantawy 2014Emad AdelNoch keine Bewertungen
- Kuwait Pediatric GuideLinesDokument124 SeitenKuwait Pediatric GuideLinesemicurudimov100% (1)
- Peds Handbook 2017 - 2018Dokument25 SeitenPeds Handbook 2017 - 2018Michael MangubatNoch keine Bewertungen
- Pediatric Guidelines For MedicationsDokument24 SeitenPediatric Guidelines For MedicationsjonatasmartinezNoch keine Bewertungen
- Admitting OrdersDokument4 SeitenAdmitting OrdersRommel OliverasNoch keine Bewertungen
- PICU Protocol 1 Ain Shams UniversityDokument52 SeitenPICU Protocol 1 Ain Shams UniversityAhmad ElgazzarNoch keine Bewertungen
- Pocketbook WHO PediatricsDokument398 SeitenPocketbook WHO PediatricsNashria RusdhyNoch keine Bewertungen
- Pedia NotesDokument97 SeitenPedia NotesChristian Dave DoctoNoch keine Bewertungen
- PICU BookletDokument98 SeitenPICU BookletTufail MemonNoch keine Bewertungen
- Surgical Adult Critical Care Ref SheetDokument3 SeitenSurgical Adult Critical Care Ref Sheetsgod34100% (1)
- Common TreatmentsDokument5 SeitenCommon TreatmentsRaj MandumulaNoch keine Bewertungen
- Paediatric DosesDokument2 SeitenPaediatric DosesEdio PathicNoch keine Bewertungen
- BWH Hyperglycemia GuidelinesDokument7 SeitenBWH Hyperglycemia Guidelinespmahesh107100% (1)
- Nurse PicuDokument5 SeitenNurse PicuDitto RezkiawanNoch keine Bewertungen
- Neonatal Drugs Section Fifth Edition2012 PDFDokument163 SeitenNeonatal Drugs Section Fifth Edition2012 PDFAhmed MohammedNoch keine Bewertungen
- Pedia NotesDokument7 SeitenPedia NotesBonnyong MaNoch keine Bewertungen
- Pediatrics - Michael GrantDokument78 SeitenPediatrics - Michael GrantPappitha RajaNoch keine Bewertungen
- The Kids Are Alright Pediatric Trauma PearlsDokument21 SeitenThe Kids Are Alright Pediatric Trauma PearlsDaniel Torres CutivaNoch keine Bewertungen
- PHC EmergencyDokument42 SeitenPHC Emergencyمحمداحمد محمدنور ابايزيدNoch keine Bewertungen
- Techniques of Calculation and Prescribing Drug Dosage in Pediatric PracticeDokument25 SeitenTechniques of Calculation and Prescribing Drug Dosage in Pediatric PracticeJanarth Nan100% (1)
- Nicu ProtocolsDokument111 SeitenNicu ProtocolsJoão Paulo PatoNoch keine Bewertungen
- Mechanical Ventilation in Pediatric PatientDokument11 SeitenMechanical Ventilation in Pediatric PatientHandris YanitraNoch keine Bewertungen
- HFOV High-Frequency-Oscillatory-VentilationDokument22 SeitenHFOV High-Frequency-Oscillatory-VentilationJZNoch keine Bewertungen
- Clinical Protocol in Pediatrics, 2012Dokument96 SeitenClinical Protocol in Pediatrics, 2012floare de colt100% (1)
- Neonatal and Pediatric Guidelines Arrhythmia ManagementDokument16 SeitenNeonatal and Pediatric Guidelines Arrhythmia ManagementAkhmad HidayatNoch keine Bewertungen
- Persistent Pulmonary Hypertension in Newborn: By: Dr. Abhay Kumar Moderator: Dr. Akhilesh KumarDokument31 SeitenPersistent Pulmonary Hypertension in Newborn: By: Dr. Abhay Kumar Moderator: Dr. Akhilesh KumarAbhay BarnwalNoch keine Bewertungen
- Normal Values HR RR BPDokument28 SeitenNormal Values HR RR BPKthrine CrronNoch keine Bewertungen
- Trust Guideline For The Newborn and Infant Physical Examination (NIPE)Dokument37 SeitenTrust Guideline For The Newborn and Infant Physical Examination (NIPE)Clara CarneiroNoch keine Bewertungen
- Critical Care Drugs 2Dokument23 SeitenCritical Care Drugs 2Asri Ernadi100% (1)
- Pediatrics 5 Minute ReviewDokument206 SeitenPediatrics 5 Minute ReviewMarius CreangaNoch keine Bewertungen
- Handbook Peads SurgDokument88 SeitenHandbook Peads Surgsedaka26Noch keine Bewertungen
- Basic Practice of Anesthesiology FinalDokument70 SeitenBasic Practice of Anesthesiology FinalAfiqah So JasmiNoch keine Bewertungen
- Continuous Positive Airway Pressure (CPAP)Dokument53 SeitenContinuous Positive Airway Pressure (CPAP)indiamahesh100% (1)
- Pediatric TransfusionDokument82 SeitenPediatric TransfusionMia Lesaca-Medina100% (2)
- 10-Critical CareDokument3 Seiten10-Critical CareIbrahimFikryNoch keine Bewertungen
- Pediatric DosesDokument17 SeitenPediatric DosesIris MambuayNoch keine Bewertungen
- Multidrug-Resistant - Organisms (MDROsDokument59 SeitenMultidrug-Resistant - Organisms (MDROsTariq100% (2)
- Approach in Children With SeizuresDokument26 SeitenApproach in Children With SeizuresMD Luthfy LubisNoch keine Bewertungen
- 2014 SHC ABX Dosing GuideDokument4 Seiten2014 SHC ABX Dosing GuideisnaeniNoch keine Bewertungen
- Picu PocketbookDokument7 SeitenPicu Pocketbookandrahlyn100% (1)
- Hypertension: Are You Safe?: Keeping It Under ControlDokument2 SeitenHypertension: Are You Safe?: Keeping It Under ControlyoshilimsiacoshigyoNoch keine Bewertungen
- Pharmacy Industry Award Ma000012 Pay GuideDokument20 SeitenPharmacy Industry Award Ma000012 Pay GuideyoshilimsiacoshigyoNoch keine Bewertungen
- Ulipristal or Levonorgestrel As Emergency Contraception: AvailabilityDokument4 SeitenUlipristal or Levonorgestrel As Emergency Contraception: AvailabilityyoshilimsiacoshigyoNoch keine Bewertungen
- Ulipristal or Levonorgestrel As Emergency Contraception: AvailabilityDokument4 SeitenUlipristal or Levonorgestrel As Emergency Contraception: AvailabilityyoshilimsiacoshigyoNoch keine Bewertungen
- Work Health and Safety PolicyDokument4 SeitenWork Health and Safety PolicyyoshilimsiacoshigyoNoch keine Bewertungen
- Brekky Menu 5Dokument2 SeitenBrekky Menu 5yoshilimsiacoshigyoNoch keine Bewertungen
- Pharmacy Industry Award Ma000012 Pay GuideDokument20 SeitenPharmacy Industry Award Ma000012 Pay GuideyoshilimsiacoshigyoNoch keine Bewertungen
- Study Notes New Drugs 2012 and 2013Dokument9 SeitenStudy Notes New Drugs 2012 and 2013yoshilimsiacoshigyoNoch keine Bewertungen
- Pharma MCQDokument0 SeitenPharma MCQFoysal Sirazee0% (2)
- CephalosporinsDokument16 SeitenCephalosporinsAvrajit BhattacharjeeNoch keine Bewertungen
- Pharmacology Exam PDFDokument10 SeitenPharmacology Exam PDFyoshilimsiacoshigyoNoch keine Bewertungen
- Pediatric Antibiotic Dosing Card 2012Dokument2 SeitenPediatric Antibiotic Dosing Card 2012yoshilimsiacoshigyoNoch keine Bewertungen
- Policy For Administration of Intravenous Antibiotic Therapy To Adults in The Community and Community HospitalDokument24 SeitenPolicy For Administration of Intravenous Antibiotic Therapy To Adults in The Community and Community HospitalyoshilimsiacoshigyoNoch keine Bewertungen
- Electrolytes TutorialDokument3 SeitenElectrolytes TutorialyoshilimsiacoshigyoNoch keine Bewertungen
- Electrolytes TutorialDokument3 SeitenElectrolytes TutorialyoshilimsiacoshigyoNoch keine Bewertungen
- Milimolar CalculationsDokument17 SeitenMilimolar CalculationsMuhammad SafdarNoch keine Bewertungen
- Electrolytes TutorialDokument3 SeitenElectrolytes TutorialyoshilimsiacoshigyoNoch keine Bewertungen
- A Combined Patient and Provider Intervention For Management of Osteoarthritis in VeteransDokument13 SeitenA Combined Patient and Provider Intervention For Management of Osteoarthritis in VeteransHarshoi KrishannaNoch keine Bewertungen
- Mini Clinical Examination (Mini-CEX)Dokument21 SeitenMini Clinical Examination (Mini-CEX)Jeffrey Dyer100% (1)
- Physiological Changes Postpartum PeriodDokument2 SeitenPhysiological Changes Postpartum PeriodEurielle MioleNoch keine Bewertungen
- Requirements Specification For Patient Level Information and Costing Systems (PLICS) Mandatory Collections Continued ImplementationDokument40 SeitenRequirements Specification For Patient Level Information and Costing Systems (PLICS) Mandatory Collections Continued ImplementationAbidi HichemNoch keine Bewertungen
- Company Name: Aims Industries LTDDokument40 SeitenCompany Name: Aims Industries LTDkishoreNoch keine Bewertungen
- ESI ER CompleteDokument45 SeitenESI ER Completetammy2121Noch keine Bewertungen
- Analytical and Hortatory ExpositionDokument3 SeitenAnalytical and Hortatory ExpositionChie TjeeNoch keine Bewertungen
- Public Health Internship Cover LetterDokument8 SeitenPublic Health Internship Cover Letterf5dct2q8100% (2)
- Knowledgeand Beliefson Mental Illnessamong Church Leaders Basisfor Trainingand DevelopmentDokument15 SeitenKnowledgeand Beliefson Mental Illnessamong Church Leaders Basisfor Trainingand DevelopmentG Asilo, Jynelle A.Noch keine Bewertungen
- 2021 IWBF Classification Rules Version 202110 1Dokument108 Seiten2021 IWBF Classification Rules Version 202110 1Sebastian Alfaro AlarconNoch keine Bewertungen
- Azibact MMDokument37 SeitenAzibact MMરહીમ હુદ્દાNoch keine Bewertungen
- Smart and Sustainable Built Environment: Article InformationDokument14 SeitenSmart and Sustainable Built Environment: Article Informationmikky jayNoch keine Bewertungen
- ComplaintDokument28 SeitenComplaintLia TabackmanNoch keine Bewertungen
- Assess PDFDokument9 SeitenAssess PDFJov'z GuerreroNoch keine Bewertungen
- Lecture in Geriatrics Physical Therapy 1Dokument27 SeitenLecture in Geriatrics Physical Therapy 1S.ANoch keine Bewertungen
- CV Petrangolini enDokument8 SeitenCV Petrangolini enTeresa PetrangoliniNoch keine Bewertungen
- Cerad Total ScoreDokument6 SeitenCerad Total ScorecoconitaNoch keine Bewertungen
- 2008 04 Lecture 1 Interface Dermatitis FrishbergDokument6 Seiten2008 04 Lecture 1 Interface Dermatitis FrishbergYudistra R ShafarlyNoch keine Bewertungen
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDokument2 SeitenNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comNoch keine Bewertungen
- Disability MatrixDokument21 SeitenDisability MatrixAngelika MendozaNoch keine Bewertungen
- SR - Hse Officer (8104)Dokument5 SeitenSR - Hse Officer (8104)Nijo Joseph100% (1)
- Ug Epidemiological Bulletin 2023Wk19Dokument8 SeitenUg Epidemiological Bulletin 2023Wk19JACKLINE ONZIANoch keine Bewertungen
- Pro-Oxidant Strategies - Cancer Treatments ResearchDokument71 SeitenPro-Oxidant Strategies - Cancer Treatments ResearchSpore FluxNoch keine Bewertungen
- Set C QP Eng Xii 23-24Dokument11 SeitenSet C QP Eng Xii 23-24mafiajack21Noch keine Bewertungen
- Advanced Cardiovascular Life SupportDokument16 SeitenAdvanced Cardiovascular Life SupportSarah Mohd YusofNoch keine Bewertungen
- The Impact of Longitudinal Studies On Understanding Development From Young Adulthood To Old AgeDokument11 SeitenThe Impact of Longitudinal Studies On Understanding Development From Young Adulthood To Old AgeLana PeharNoch keine Bewertungen
- Urtikaria Pada Perempuan Usia 39 Tahun: Laporan Kasus: Moh. Wahid Agung, Diany Nurdin, M. SabirDokument5 SeitenUrtikaria Pada Perempuan Usia 39 Tahun: Laporan Kasus: Moh. Wahid Agung, Diany Nurdin, M. SabirZakia AjaNoch keine Bewertungen
- Therapeutic Relationship Is Between Therapist and Patient and Has Always Been Viewed As SacredDokument3 SeitenTherapeutic Relationship Is Between Therapist and Patient and Has Always Been Viewed As Sacredcbargrad100% (1)
- Tea and Industrial RevolutionDokument4 SeitenTea and Industrial RevolutionPhuong NguyenNoch keine Bewertungen
- Shoulder Pain and Disability Index (SPADI) PDFDokument2 SeitenShoulder Pain and Disability Index (SPADI) PDFIvro Linda cahyaniNoch keine Bewertungen