Beruflich Dokumente
Kultur Dokumente
Bone Aging: Anatomy and Physiology of Bone
Hochgeladen von
Harun NasutionOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Bone Aging: Anatomy and Physiology of Bone
Hochgeladen von
Harun NasutionCopyright:
Verfügbare Formate
Chapter 2
Bone Aging
Arthur N. Lau and Jonathan D. Adachi
Abstract The aging musculoskeletal system has a profound effect on the health of an individual. In this chapter, the author outlines some of the key changes in bone physiology during aging and explains how they contribute to osteoporosis and the increased fracture risk in the elderly. Keywords Anatomy Osteoporosis Fracture Osteomalacia Elderly
Anatomy and Physiology of Bone
Bone is a unique structure made up of cells and extracellular matrix (ECM). This ECM is composed of collagen and non-collagen proteins. The collagen bers are arranged in bundles, which, in turn, are arranged in specic orientations. These bers are further mineralized with calcium phosphate and hydroxyapatite. The skeleton serves as the stores for 99% of the total body calcium and 80% of the total body phosphate. The bone organic matrix is predominantly composed of type I collagen (95%) along with sulfated proteoglycans, acidic glycoproteins, and osteocalcin. The cell types found in bone include osteoblasts, osteoclasts, osteocytes, and stromal cells. Bone continuously undergoes a remodeling process throughout life, where resorption and formation are continuously occurring. This process is known as bone turnover, and it occurs at discrete sites all throughout the skeleton. As a result, 510% of the total adult skeleton is replaced each year [1]. This process is closely regulated by the actions of osteoblasts (which are responsible for bone formation) and osteoclasts (which are responsible for bone resorption). The osteoblasts and osteoclasts build basic multicellular units (BMUs), which are under the control of various systemic hormones and local growth factors. As a result, these factors regulate the activity
J.D. Adachi(*) McMaster University/St. Josephs Healthcare, 501-25 Charlton Ave. E., Hamilton, ON L8N 1Y2, Canada e-mail: jd.adachi@sympatico.ca
and number of osteoclasts and osteoblasts through controlling the replication rate of undifferentiated cells and the differentiation of these cells [2]. This balance between for mation and resorption determines the total body bone mass. In the skeleton, two types of bone can be observed. Cortical or (compact) bones make up about 80% of the total skeleton and are present in the shafts of long bones. Trabecular (or cancellous) bone accounts for the remaining 20% of the total skeleton and is present in the end of long bones, vertebrae, and ribs. In the adolescence, there is net bone formation, as bone formation exceeds the rate of resorption, thus leading to an increase in total bone mass. However, this rate of growth ceases when linear growth stops, and at this point, the persons peak bone mass is achieved. This usually occurs by age 1525 [3]. The total bone mass usually remains constant for about 10 years, as the rates of bone formation and resorption are balanced during this time. By the third to fourth decade of life, total bone mass will begin to decrease. By age 80, it is estimated that the bodys total bone mass will be about 50% of its peak value [3]. This process is known as senile osteoporosis, which describes a process of age-related bone loss. Furthermore, women have an accelerated period of bone loss shortly postmenopause. This phenomenon will be discussed in subsequent chapters in this book.
Senile Osteoporosis
Osteoporosis is a disease leading to progressive decreases in bone mineral density (BMD), decreased bone strength, and increased risk of skeletal fractures [4]. Approximately 30% of women will have sustained at least one vertebral fracture by the age of 75 [5]. There are over 1,500,000 total fractures each year in the USA related to osteoporosis, and 700,000 of these were incident vertebral [5] (see Chap.19). Although the process of bone turnover is normally in equilibrium, the aging process has involuntary changes on the process of bone formation and resorption [3]. Two types of osteoporosis have been described. Type I which is seen in women
11
Y. Nakasato and R.L. Yung (eds.), Geriatric Rheumatology: A Comprehensive Approach, DOI 10.1007/978-1-4419-5792-4_2, Springer Science+Business Media, LLC 2011
12
A.N. Lau and J.D. Adachi
and is believed to be estrogen-dependent accelerated bone loss shortly after menopause. In a state of estrogen deciency, a high bone turnover state results from increased numbers of osteoblasts and osteoclasts. In type I osteoporosis, resorption exceeds the rate of bone formation, thus leading to an accelerated bone loss state. The exact cellular mechanism by which estrogen deciency exerts its effects on bone turnover is not entirely understood. However, increased cytokine production clearly plays an essential role in promoting osteoclast production and activity in the estrogen-decient state (vide infra). Type II, also known as senile osteoporosis, affects both men and women and is associated with aging. Unlike in type I, this form of osteoporosis has a decreased rate of bone turnover. The pathophysiology is due to a decrease in osteoblast numbers and activity, thus leading to a decrease rate of bone formation with subsequent net decrease in total bone mass. The mechanism by which this occurs will be discussed later on.
Age-Related Changes in Bone Cytokines
Chronic inammation secondary to the aging process plays a signicant role in the bone remodeling process though the actions of proinammatory cytokines. The immunosenescence process involves a chronic inammatory state with subsequent hyperproduction of proinammatory cytokines [6] (see Chap.1). Numerous studies have shown that interleukin (IL)-6, tumor necrosis factor alpha (TNF-a), IL-1, among other cytokines are elevated during the aging process [7, 8]. As previously mentioned, many of these cytokines and growth factors have a role in the regulation of bone metabolism and subsequent rate of bone turnover. IL-6 is a prominent example, as it increases steadily with aging. IL-6 is also a potent promoter of osteoclast differentiation and activation, thus favoring net bone resorption. IL-1 is another potent stimulator of osteoclast differentiation and activation, and its levels also rise steadily with aging. Parathyroid hormone (PTH) levels also increase with aging, and PTH has downstream effects of inducing IL-6 production. TNF-a has the effects of stimulating bone resorption and inhibits new bone formation [9]. Furthermore, the inducible nitric oxide synthesis pathway (iNOS) is activated through the effects of TNF-a and IL-1. In vitro studies have shown that iNOS pathway activation inhibits the production of new osteoblasts and can induce osteoblast apoptosis.
(IGF) axis is also altered. GH plays a role in regulating somatic growth, while IGFs serve as mediators of GHs actions and also serve as regulators of connective tissue cell function [10]. As humans age, there is a progressive, yet gradual fall in GH secretion, and this is correlated with a concurrent drop in circulating IGF-1 levels [11]. Furthermore, the serum levels of IGF-binding proteins have been found to increase in the elderly population. This compounds the problem, since IGF-binding proteins decrease the bioavailable level of IGFs and antagonize the actions of IGF [12]. The GHIGF axis plays a pivotal role in regulating bone metabolism and subsequent BMD. IGF-1 is a potent bone anabolic factor through directly stimulating osteoblast activity [13]. IGFs also increase the number of active osteoblasts through its effects on stimulating the rate of bone marrow stem cell proliferation, and differentiation of mesenchymal cells into osteoblasts [13]. Through these actions, the activation of the GHIGF axis promotes bone formation and has a net anabolic effect when stimulated. Studies have shown a correlation between the age-dependent decline in circulating GH/IGF levels with an increased risk of osteoporosis and increased incidence of fragility fractures [14]. Studies which investigated the therapeutic use of GH in osteoporotic patients revealed a clear correlation between GH dosage and serum IGF-1 levels, with increases in BMD [15]. Furthermore, pulsatile injections of PTH (teriparatide/Forteo) also increase the circulating levels of IGF-1 which accounts for teriparatides therapeutic use as an anabolic bone agent [16]. Although chronically high levels of PTH will lead to signicant reductions in BMD, it has anabolic effects when given in a pulsatile manner. The reason for this paradoxical effect is due to different signaling mechanisms activated under the different two conditions. The exact mechanism is still uncertain, but it is believed that when PTH is given in a pulsatile fashion, the Wnt-b catenin pathway is activated, which has subsequent effects on increasing IGF-1 levels. Therefore, the age-dependent reduction in circulating GH and IGF-1 levels may play a signicant role in the development and progression of senile osteoporosis.
Fracture Healing in the Elderly
Aging is a complex physiological process with multiple involvements on the molecular, cellular, and systemic levels. The aging process and osteoporosis are intimately intertwined. Osteoporosis has a serious impact on the morbidity and mortality of elderly, if they sustain an osteoporotic fracture. Approximately 30% of women will have sustained at least one vertebral fracture by the age of 75 [5]. The lifetime risk for sustaining a hip fracture is 17% in Caucasian women and 6% in men above age 50. There are over 1,500,000 total fractures each year in the USA related to osteoporosis, and
GH-IGF Axis
In addition to changes in circulating cytokine levels with aging, the growth hormone (GH) and insulin-like factor
2 Bone Aging
13
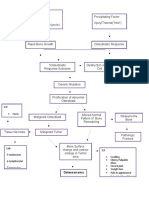
700,000 of these were incident vertebral [5]. Patients who have suffered an osteoporotic fracture, especially a vertebral or hip fracture has signicant impacts on their mortality and morbidity [17]. Both clinical and radiographic fractures are associated with an increase mortality rate. One study identied a 16% reduction in expected 5-year survivability. Approximately 75% of patients who present with a clinical vertebral fracture will experience chronic pain [5]. The number and severity of vertebral fractures also increases the risk of developing chronic back pain. Aside from the physical limitations suffered by these patients, chronic back pain has a signicant impact on the patients quality of life. Patients suffering from vertebral fractures often have impaired physical functioning, limited activities of daily living, limited leisure and recreational activities, and signicant emotional distress. There is a signicant difference in the fracture healing process when comparing the elderly to younger patients. The elderly with osteoporosis most likely sustain fractures in the femoral neck, vertebrae, and distal radius secondary to falls and low-energy trauma [18]. The femoral neck and vertebral bodies are at greater risk of an osteoporotic fracture because these sites contain a high percentage composition of trabecular bone, and it is more affected by the age-related shift on bone remodeling, which favors a net bone resorption. A decrease in BMD certainly has signicant contributions to increasing the risk of fractures, as a drop in one standard deviation in BMD (T-scores) increases the relative risk for a fracture by two- to threefolds [19]. However, there are other factors to consider aside from BMD values alone when assessing for fracture risks. Irrespective of BMD value, increasing age alone signicantly increases the risk of sustaining a fracture [20]. The repair mechanism is compromised with increasing age, and this also increases the risk of suffering a fracture in the elderly [21]. A disruption in the regulation of osteogenic differentiation, which subsequently disrupts angiogenesis, likely plays an important role in compromising the fracture healing mechanism [22]. In the normal physiology of fracture repair, angiogenesis plays a pivotal role. When a fracture occurs, platelets accumulate, which in turn form a brin-rich extracellular matrix. Chemoattractants are released to recruit neutrophils, macrophages, and lymphocytes. Granulation tissue is then formed as blood vessels begin to sprout into the clot along with undifferentiated mesenchymal cells. In stable conditions, intramembranous ossication is able to occur as the mesenchymal progenitor cells differentiate into osteoblasts, which in turn begin to form woven bone. The woven bone spans the fracture site and forms a hard callus. If the fracture is unstable, where angiogenesis is impaired or limited, another mechanism is activated. In this scenario, endochondrial ossication occurs with concurrent penetration of blood vessels and mesenchymal progenitor cells into the newly formed chondrogenic tissue. In either scenario of intramembranous or endochondrial
ossication, the newly formed matrix is remodeled into lamellar bone to conclude the fracture repair process. In this complex sequential repair process, the role of angiogenesis and the action of mesenchymal cells are critical. The aging process has profound effects on angiogenesis [23]. This results from a decrease in endothelial cells, activity of the hemostatic pathway, growth factors, and neurochemical mediators that are required for angiogenesis [23]. Aging also has an effect on mesenchymal progenitor cells numbers and activity. The mitotic rate of these progenitor cells decline with aging, and there are fewer the number of progenitor cells in the bone marrow show an age-related decrease [24]. However, it is unclear if the decrease is signicant enough to affect fracture healing [25]. Furthermore, in vitro experiments utilizing rat mesenchymal precursor cells showed samples from elderly rats had a signicantly lower responsiveness to 1,25 dihydroxyvitamin D3 and TGF-b, when compared with cells from non-elderly rats [26]. Although there are numerous age-related changes to normal physiology which contribute to impaired fracture healing, there is no yet enough evidence to conclude how great an impact these changes at the cellular and molecular level have on clinical disease development.
Pathophysiology of Osteoporosis in Males and Females
Based on comparisons with male database of BMD measurements, the World Health Organization estimates that 12million men in the USA have osteoporosis (dened as T-scores <2.5), and there are 813 million men with osteopenia (dened as BMD between 1.0 and 2.5). Like in women, there is an exponential increase in the risk of hip fractures with advancing age, yet this increase begins 510years later than in women [27]. It is estimated that one in ve men over the age of 50 will incur an osteoporosisrelated fracture in their lifetime. Therefore, although it is often overlooked, there is little doubt that osteoporosis is a very real and signicant medical problem in the elderly male population. Although BMD measurements are not as well standardized for men as they are for women, there are a few prospective studies investigating BMD values with fracture risks in men. The Rotterdam Study in 2004 reported that men older than 55 showed a relationship between their absolute BMD value and risk of hip and other non-vertebral fractures. This study also showed that the rates of non-vertebral fractures occurred at a rate that was comparable with women of the same age group [28]. In a prospective study done by the Osteoporotic Fractures in Men (MrOS) Study research group, a cohort of 5,000 men were followed, and this study showed a stronger relationship between hip BMD values and hip fracture risk in men, when compared with women
14
A.N. Lau and J.D. Adachi
relative risk of 3.2-fold in men vs. 2.1-fold in women for ( each SD decrease in hip BMD) [29]. Aside from hip fractures, osteoporotic men are also at risk of suffering from vertebral fractures. The European vertebral osteoporosis study (EVOS) was a large multinational survey which aimed to determine the prevalence of vertebral involvement in osteoporosis. They found the prevalence of vertebral deformities in males (15.1%) was similar to that seen in females (17.2%) [30]. The implications of the increase in fracture risk is very signicant, since the mortality rate associated with hip fractures and vertebral fractures is higher in men than in women [31]. In men, their BMD values increase signicantly during puberty in response to sex steroid production, and peak spinal bone density is reached by about age 20, and the peak density in long bones are reached several years later. After reaching their peak bone mass, men lose about 30% of their trabecular bone and 20% of their cortical bone mass during their lifetimes; loss begins shortly after peak bone mass is achieved [32]. In men after the age of 30, it is estimated that the BMD in their proximal and distal radius declines by about 1% per year [33]. At certain sites, including the femoral neck, the rate of decline in BMD may increase with advancing age [34]. During the years where females typically incur a rapid decline in BMD, males have several factors which protect them, which help account for the difference in incidence rates between men and women. Men do not suffer from a loss in sex steroid production during midlife, as seen in women. During menopause, there is an abrupt drop in serum estrogen levels, and this has signicant implications on bone metabolism. Estrogen inhibits bone resorption and when estrogen production declines after menopause, there is a marked increase in the rate of bone resorption. The exact mechanism by which estrogen regulates the rate of bone turnover is not entirely clear. However, in states of estrogen deciency, there is an upregulation of selected cytokines [especially IL-6 and macrophage colony-stimulating factor (M-CSF)]. These cytokines have an essential role in regulating osteoclast genesis and also regulate osteoclast function. IL-6 is a cytokine produced by many different cell types including the osteoblasts, and its production increases during states of estrogen deciency [35]. IL-6 acts as a mediator to stimulate osteoclastogenesis and bone resorption through a prostaglandin-dependent mechanism. Monocyte colony stimulating factor (M-CSF) levels also increase markedly in estrogen-decient states, and it is essential for the activation of osteoclasts through a cytokine-mediated mechanism. In addition to IL-6 and M-CSF, a number of other cytokines and growth factors are involved in a very complex process by which estrogen deciency leads to a marked rise in the rate of bone resorption and overall net bone loss. This rate then slows with time after menopause, but still progresses at a steady rate.
About 50% of osteoporotic men are diagnosed with a form of secondary osteoporosis, where there is a specic underlying cause. This leaves the other 50% of men with a primary form of osteoporosis, which encompasses idiopathic osteoporosis and senile osteoporosis. As in females, genetic factors play an essential role, as the rates of bone loss are correlated within twin pairs [36]. Serum concentrations of testosterone decreases with advancing age and this factor has been proposed to have effects on increasing bone resorption or decreasing the rate of bone formation. However, most cross-sectional studies investigating the relationship between serum testosterone concentrations and bone density have failed to nd a correlation, especially when adjusting for age body weight and serum estrogen levels [37]. However, low estrogen levels may also be an important factor leading to male osteoporosis. In older men, serum estrogen concentrations are correlated with their BMD, independent of serum testosterone levels [38]. It is still unclear whether estrogen levels have their benecial effects primarily by maximizing peak bone mass in adolescent men or have a major effect on determining the rate of bone loss in elderly men. In men, low serum estradiol levels are also associated with an increase risk of hip fractures. In addition, men with concurrently low levels of estradiol and testosterone have the greatest risk for future hip fractures.
Other Age-Related Factors
Vitamin D is an essential factor in the regulation of calcium metabolism. 1,25-Dihydroxy vitamin D3, the active form of vitamin D has effects on increasing intestinal calcium absorption, decreasing serum PTH levels through both a direct inhibition of PTH secretion, and also indirectly, through inhibiting PTH secretion through increased serum calcium levels. Therefore, vitamin D has overall effects of decreasing PTH-mediated bone resorption. Vitamin D deciencies often occur with advanced aging, and this may be another contributor to the pathogenesis of senile osteoporosis. Although severe vitamin D deciency will result in the development in osteomalacia in an adult person, a mild deciency could lead to a state of secondary hyperparathyroidism, with resultant development of osteoporosis. Both primary (due to deciency of vitamin D) and secondary vitamin D deciency (reduced level of 1,25-dihydroxy vitamin D3 resulting from renal impairment or a lack of target tissue responsiveness) could occur with aging. Serum levels of 1,25-dihydroxy vitamin D3 are seen at lower levels in those above the age of 65, and it is believed that the aging kidneys inability to synthesize 1,25-dihydroxy vitamin D3 at an optimal level contributes to this observation [39].
2 Bone Aging
15
In addition to the vitamin D deciency, there is also an age-dependent decline in intestinal calcium absorption efciency, which may correspond with a Vitamin D decient state. Furthermore, there is also an age-related rise in serum biologically active PTH levels, which also would correspond to a vitamin D decient state [40]. Finally, there is a correlation between urine NTx levels (a marker for bone resorption) and serum PTH levels in postmenopausal women, thus a vitamin D decient state leading to an elevated serum PTH concentration may be a contributor senile osteoporosis. There are also a number of factors in the elderly population which may predispose them to falls, resulting in subsequent osteoporotic fractures. These factors include lack of physical activity, muscle weakness/atrophy, neuromuscular disease, impairment in gait, balance, and proprioception among other risk factors for falls. As a result, many of these low velocity falls may result in osteoporotic fractures in the elderly which will have a signicant impact on the patients quality of life and mortality rates, if a vertebral or hip fracture is sustained.
cirrhosis leading to defective 25-hydroxylation, vitamin D loss through nephritic syndrome, and defective 1-alpha 25-hydroxylation seen in chronic renal failure and hypoparathyroidism. Calcium deciency may also lead to osteomalacia, but it is an extremely rare cause. Osteomalacia can still occur in the setting of adequate mineral availability in the extracellular uid. This can occur in the setting of impaired matrix formation, as there is not a proper scaffolding onto which hydroxyapatite is deposited. Abnormal matrix formation is seen in conditions such as osteogenesis imperfecta, brogenesis imperfecta, chronic renal failure, and hypophosphatasia. Finally, there are a number of drugs and toxins which interfere with the mineralization of the osteoid. Bisphosphonates inhibit both bone resorption and formation and lead to impaired mineralization. Aluminum is another inhibitor of mineralization, especially in the setting of total parenteral nutrition use. Fluoride can also inhibit matrix mineralization, and osteomalacia is commonly found in the setting of endemic uorosis and in chronic uoride toxicity.
Osteomalacia
Osteomalacia is a relatively common metabolic bone disease leading to a reduced bone density. It is a disorder seen in the adult population, where there is defective mineralization of newly formed bone matrix. Rickets shares the same pathogenesis as osteomalacia, but by denition, it occurs in children with still open growth plates. Normal bone turnover occurs continually on trabecular and Haversian bone surfaces. This process begins as osteoclasts secrete protons, proteases, and proteoglycan digesting enzymes onto the bone surface, thus producing a tunnel in cortical bone. Osteoblasts then lay down a new bone matrix (osteoid), which serves as a scaffolding onto which mineral crystal hydroxyapatite can form. Bone mineral, in the form of amorphous calcium phosphate is deposited, which in turn undergoes conversion into hydroxyapatite. Given this normal physiological process necessary for bone turnover, the failure of mineralization seen in osteomalacia can occur due to a number of etiologies. Firstly, a normal concentration of minerals (calcium and phosphate) must be available in the extracellular matrix to form hydroxyapatite crystals in the osteoid. Phosphate deciency is the most common cause of osteomalacia. Causes of hypophosphatemia include decreased intake, antacid use, vitamin D deciency, secondary hyperparathyroidism, and phosphate wasting through renal tubular defects. Vitamin D deciency is another common cause of osteomalacia. Common etiologies of vitamin D deciency include decient intake, impaired gastrointestinal absorption, lack of sun exposure,
References
1. Partt AM. The coupling of bone formation to bone resorption: a critical analysis of the concept and its relevance to the pathogenesis of osteoporosis. Metab Bone Dis Relat Res. 1982;4:16. 2. Chan GK, Duque G. Age related bone loss: old bone, new facts. Gerontology. 2002;48:6271. 3. Kloss FR, Gassner R. Bone and aging: effects on the maxillofacial skeleton. Exp Gerontol. 2006;41:1239. 4. NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis and Therapy. Osteoporosis prevention, diagnosis and therapy. JAMA. 2001;285:78595. 5. Nevitt M, Chen P, Dore R, et al. Reduced risk of back pain following teriparatide treatment: a meta-analysis. Osteoporos Int. 2006;17:27380. 6. De Martinis M, Franceschi C, Monti D, etal. Inammation-ageing and lifelong antigenic load as major determinants of ageing rate and longevity. FEBS Lett. 2005;579:20359. 7. Bruunsgaard H. Effects of tumor necrosis factor-alpha and interleukin-6 in elderly populations. Eur Cytokine Netw. 2002;13:38991. 8. Nanes MSL. Tumor necrosis factor-alpha: molecular and cellular mechanisms in skeletal pathology. Gene. 2003;4:115. 9. Jilka RL, Hangoc G, Girasole G, etal. Increased osteoclast development after estrogen loss: mediation by interleukin-6. Science. 1992;257:8891. 10. Freemont AJ, Hoyland AJ. Morphology, mechanisms and pathology of musculoskeletal ageing. J Pathol. 2007;21:2529. 11. Sonntag WE, Lynch CD, et al. Pleiotrophic effects of growth hormone and insulin-like growth factor-1 on biological aging: inferences from moderate caloric-restricted animals. J Gerontol A Biol Sci Med Sci. 1999;54:52138. 12. Frystyk J. Aging somatropic axis: mechanisms and implications of insulin-like growth factor-related binding protein adaptation. Endocrinol Metab Clin North Am. 2005;34:86576. 13. Zofkova I. Pathophysiological and clinical importance of insulinlike growth factor-I with respect to bone metabolism. Physiol Res. 2003;52:65779.
16 14. Lombardi G, Tauchmanova L, Di Somma C, etal. Somatopause: dimetabolic and bone effects. J Endocriol Invest. 2005;28:3642. 15. Wuster C, Harle U, Rehn U, et al. Benets of growth hormone treatment on bone metabolism, bone density and bone strength in growth hormone deciency and osteoporosis. Growth Horm IGF Res. 1998;8:8794. 16. Canalis E, Giustina A, Bilezikian JP. Mechanisms of anabolic therapy for osteoporosis. N Engl J Med. 2007;357:90516. 17. Benhamou CL. Effects of osteoporosis medications on bone quality. Joint Bone Spine. 2007;74:3947. 18. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:17617. 19. Woodhouse A. BMD at varOsteoporos Intus sites for the prediction of hip fractures: a meta analysis. JBMR. 2000;15:1145. 20. Hui etal. JCI. 1988;81:18049. 21. Gruber R, Koch H, Doll BA, etal. Fracture healing in the elderly patient. Exp Gerontol. 2006;41:108093. 22. Lu C, Miclau T, Hu D, etal. Cellular basis for age-related changes in fracture repair. J Orthop Res. 2005;23:13007. 23. Brandes RP, Fleming I, Busse R. Endothelial aging. Cardiovasc Res. 2005;66:28694. 24. Bergman RJ, Gazit D, Khan AJ, et al. Age related changes in osteogenic stem cells in mice. J Bone Miner Res. 1996;11:56877. 25. Stenderup K, Justesen J, Clausen C, etal. Aging is associated with decreased maximal life span and accelerated senescence of bone marrow stromal cells. Bone. 2003;33:91926. 26. Shiels MJ, Mastro AM, Gay CV. The effect of donor age on the sensitivity of osteoblasts to the proliferative effects of TGF-beta and 1,25(OH(2)) vitamin D(3). Life Sci. 2002;70:296775. 27. Farmer ME. Race and sex differences in hip fracture incidence. Am J Public Health. 1984;74(12):137480. 28. Schuitt SC, Vander Klift M, Weel AE, etal. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone. 2004;34:195202. 29. Cummings SR, Cawthon PM, Ensrud KE, et al. Osteoporotic fractures in men (MrOS) Research Groups; Study of osteoporotic
A.N. Lau and J.D. Adachi fractures research group. BMD and risk of hip and non-vertebral fractures in older men: a prospective study and comparison with older women. J Bone Miner Res. 2006;21:15506. 30. Agnusdei D, Gerardi D, Camporeala A, et al. The European vertebral osteoporosis study in Siena, Italy. Bone. 1994;16:118S. 31. Center JR, Nguyen TV, Schneider D, etal. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:87882. 32. Nordstrm P, Neovius M, Nordstrm A. Early and rapid bone mineral density loss of the proximal femur in men. J Clin Endocrinol Metab. 2007;92:19028. 33. Orwell ES, Oviatt SK, McClung MR, etal. The rate of bone mineral loss in normal men and the effects of calcium and cholecalciferol supplementation. Ann Intern Med. 1990;112:2934. 34. Jones G, Nguyen T, Sambrook P, etal. Progressive loss of bone in the femoral neck in elderly people: longitudinal ndings from the Dubbo osteoporosis epidemiology study. BMJ. 1994;309:6915. 35. Bismar H, Diel I, Ziegler R, etal. Increased cytokine secretion by human bone marrow cells after menopause or discontinuation of estrogen replacement. J Clin Endocrinol Metab. 1995;80:33515. 36. Slemana CW, Christian JC, Reed T, etal. Long-term bone loss in men: effects of genetic and environmental factors. Ann Intern Med. 1992;117:28691. 37. Khosla S, Melton LJ, Atkinson EJ, etal. Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: a key role for bioavailable estrogen. J Clin Endocrinol Metab. 1998;83:226674. 38. Greendale GA, Edelstein S, Barrett-Conner E. Endogenous sex steroids and bone mineral density in older women and men: the Rancho Bernardo Study. J Bone Miner Res. 1997;12:183343. 39. Epstein S, Bryce G, Hinman JW, etal. The inuence of age on bone mineral regulating hormones. Bone. 1986;7:4215. 40. Landin-wilhelmsen K, Wilhelmsen L, Lappas G, etal. Serum intact parathyroid hormone in a random population sample of men and women: relationship to anthropometry, life-style factors, blood pressure, and vitamin D. Calcif Tissue Int. 1995;56:1048.
http://www.springer.com/978-1-4419-5791-7
Das könnte Ihnen auch gefallen
- Normal Bone Formation and RemodelingDokument4 SeitenNormal Bone Formation and RemodelingFernando AnibanNoch keine Bewertungen
- Nutritional Zinc Plays A Pivotal Role in Bone Health and Osteoporosis PreventionDokument14 SeitenNutritional Zinc Plays A Pivotal Role in Bone Health and Osteoporosis PreventionDewi HenssaNoch keine Bewertungen
- English IIIDokument10 SeitenEnglish IIIAyu Wulandari TrianggoNoch keine Bewertungen
- Primary Osteoporosis in Postmenopausal WomenDokument5 SeitenPrimary Osteoporosis in Postmenopausal WomenAzmi FarhadiNoch keine Bewertungen
- Chapter 23: Osteoporosis of The SpineDokument15 SeitenChapter 23: Osteoporosis of The SpineTraian UrsuNoch keine Bewertungen
- Update Osteoporosis Management (Listo)Dokument18 SeitenUpdate Osteoporosis Management (Listo)Jossie AcuñaNoch keine Bewertungen
- Alcohol and Other Factors Affecting Osteoporosis Risk in WomenDokument7 SeitenAlcohol and Other Factors Affecting Osteoporosis Risk in WomenRo KohnNoch keine Bewertungen
- Treatment of Postmenopausal OsteoporosisDokument8 SeitenTreatment of Postmenopausal OsteoporosisLaura_Puspita__9294Noch keine Bewertungen
- Love HormoneDokument4 SeitenLove HormoneNanda Nabilah UbayNoch keine Bewertungen
- Physiologicchangesofthe Musculoskeletalsystem Withaging:: A Brief ReviewDokument7 SeitenPhysiologicchangesofthe Musculoskeletalsystem Withaging:: A Brief ReviewRizqan Fahlevvi AkbarNoch keine Bewertungen
- ArtikelDokument13 SeitenArtikelAulia Rahma AgustianNoch keine Bewertungen
- Task Related To Muscles and Bone ProblemDokument6 SeitenTask Related To Muscles and Bone ProblemFOONG YI KUAN MoeNoch keine Bewertungen
- Ageing and OsteoarthritisDokument9 SeitenAgeing and OsteoarthritisHalim Muhammad SatriaNoch keine Bewertungen
- A Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthDokument17 SeitenA Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthErnest Gabriel Cruz AdvinculaNoch keine Bewertungen
- Articular Cartilage and Changes in Arthritis An Introduction: Cell Biology of OsteoarthritisDokument7 SeitenArticular Cartilage and Changes in Arthritis An Introduction: Cell Biology of OsteoarthritisBasheer HamidNoch keine Bewertungen
- ProjectDokument11 SeitenProjectChristian AndersonNoch keine Bewertungen
- Herbal Treatment For Osteoporosis: A Current Review: Ping Chung Leung, Wing Sum SiuDokument6 SeitenHerbal Treatment For Osteoporosis: A Current Review: Ping Chung Leung, Wing Sum Siusiska khairNoch keine Bewertungen
- Physiologic Processes in The Skeletal SystemDokument6 SeitenPhysiologic Processes in The Skeletal SystemAry Romeo ShakespeareNoch keine Bewertungen
- A Synopsis of The Article "The Cell Biology of Bone Metabolism "Dokument2 SeitenA Synopsis of The Article "The Cell Biology of Bone Metabolism "Julina AguirreNoch keine Bewertungen
- 1042 FullDokument9 Seiten1042 Fulloki harisandiNoch keine Bewertungen
- Stini-1990-American Journal of Physical AnthropologyDokument44 SeitenStini-1990-American Journal of Physical AnthropologyIsolda Alanna RlNoch keine Bewertungen
- Journal Review OADokument3 SeitenJournal Review OAAditya SatyawanNoch keine Bewertungen
- Sarcopenia Aging-Related Loss of Muscle Mass and FunctionDokument143 SeitenSarcopenia Aging-Related Loss of Muscle Mass and FunctionVictoria MNoch keine Bewertungen
- 2018 Update On OsteoporosisDokument16 Seiten2018 Update On OsteoporosisManel PopescuNoch keine Bewertungen
- Pathophysiology AssignmentDokument12 SeitenPathophysiology AssignmentBalqis HyoleeNoch keine Bewertungen
- Shoolar Ederly OsteoDokument9 SeitenShoolar Ederly OsteoBayu Surya AwalludinNoch keine Bewertungen
- Osteoporosis: How To Treat Osteoporosis: How To Prevent Osteoporosis: Along With Nutrition, Diet And Exercise For OsteoporosisVon EverandOsteoporosis: How To Treat Osteoporosis: How To Prevent Osteoporosis: Along With Nutrition, Diet And Exercise For OsteoporosisNoch keine Bewertungen
- Osteoporosis and OsteopeniaDokument29 SeitenOsteoporosis and OsteopeniaShruti Maroo - RathiNoch keine Bewertungen
- ASKEP OsteoporosisDokument41 SeitenASKEP OsteoporosisMaya PinteNoch keine Bewertungen
- Translational Endocrinology of Bone: Reproduction, Metabolism, and the Central Nervous SystemVon EverandTranslational Endocrinology of Bone: Reproduction, Metabolism, and the Central Nervous SystemGerard KarsentyNoch keine Bewertungen
- Cooper C, Campion G, Melton LJ, 3rd. Hip Fractures in The Elderly: A World-Wide Projection. Osteoporosis Int. 1992 2 (6) :285-289Dokument5 SeitenCooper C, Campion G, Melton LJ, 3rd. Hip Fractures in The Elderly: A World-Wide Projection. Osteoporosis Int. 1992 2 (6) :285-289Noor-E-Khadiza ShamaNoch keine Bewertungen
- Pathogenesis of Osteoporosis 2: Cli Ord J. RosenDokument13 SeitenPathogenesis of Osteoporosis 2: Cli Ord J. RosenRonald TejoprayitnoNoch keine Bewertungen
- Pathophysiology and Treatment of Osteoporosis: Challenges For Clinical Practice in Older PeopleDokument15 SeitenPathophysiology and Treatment of Osteoporosis: Challenges For Clinical Practice in Older PeopleDeddy ZulkarnaenNoch keine Bewertungen
- Nutrients 10 01103 v2Dokument21 SeitenNutrients 10 01103 v2Ida Ayu LitaNoch keine Bewertungen
- General - OsteoporosisDokument9 SeitenGeneral - OsteoporosisAsma NazNoch keine Bewertungen
- OsteoporosisDokument6 SeitenOsteoporosiskingNoch keine Bewertungen
- OsteoporosisDokument6 SeitenOsteoporosiskingNoch keine Bewertungen
- OsteoporosisDokument6 SeitenOsteoporosiskingNoch keine Bewertungen
- OsteoporosisDokument6 SeitenOsteoporosiskingNoch keine Bewertungen
- Metabolic Bone DiseaseDokument25 SeitenMetabolic Bone DiseaseSavin PetersNoch keine Bewertungen
- Pathophysiology and Etiology of OsteoarthritisDokument7 SeitenPathophysiology and Etiology of OsteoarthritisknikmahNoch keine Bewertungen
- Thiazolidinediones On PPARg The Roles in Bone RemoDokument9 SeitenThiazolidinediones On PPARg The Roles in Bone RemoNguyễn Hoàng Thiên TânNoch keine Bewertungen
- OsteoporosisDokument2 SeitenOsteoporosisbiologoroger3637Noch keine Bewertungen
- Defining OsteoporosisDokument11 SeitenDefining OsteoporosisMelissa RosariNoch keine Bewertungen
- Osteoporosis Review of EtiologyDokument17 SeitenOsteoporosis Review of EtiologyClaudiaGuerreroNoch keine Bewertungen
- Death&Birth 00Dokument23 SeitenDeath&Birth 00kyz79Noch keine Bewertungen
- Fimmu 13 1005665Dokument14 SeitenFimmu 13 1005665sopha seyhaNoch keine Bewertungen
- Articular Cartilage and Changes in Arthritis and Introduction Cell Biology of OsteoarthritisDokument7 SeitenArticular Cartilage and Changes in Arthritis and Introduction Cell Biology of OsteoarthritisOscar NgNoch keine Bewertungen
- Osteoporosis For BonesDokument24 SeitenOsteoporosis For BonesRoking KumarNoch keine Bewertungen
- Osteoporosis: Screening, Prevention, and ManagementDokument20 SeitenOsteoporosis: Screening, Prevention, and ManagementBernardo RomeroNoch keine Bewertungen
- Effects of Glucosamine and Chondroitin Sulfate On Cartilage Metabolism in OA. Outlook On Other Nutrient Partners Especially Omega-3 Fatty AcidsDokument17 SeitenEffects of Glucosamine and Chondroitin Sulfate On Cartilage Metabolism in OA. Outlook On Other Nutrient Partners Especially Omega-3 Fatty Acidsharvestmoon.harvestingtimeNoch keine Bewertungen
- Molecular and Cellular Mechanisms of Skeletal Muscle Atrophy: An UpdateDokument17 SeitenMolecular and Cellular Mechanisms of Skeletal Muscle Atrophy: An UpdateBetzabé Irigoyen MoragaNoch keine Bewertungen
- Patogenesis of Bone MetastaseDokument7 SeitenPatogenesis of Bone MetastasekhairachungNoch keine Bewertungen
- Blok 16 Endocrinology of OsteoporosisDokument14 SeitenBlok 16 Endocrinology of OsteoporosisHasty WahyuniNoch keine Bewertungen
- 18-Unit 1 Anatomy and Physiology For Health and ExerciseDokument91 Seiten18-Unit 1 Anatomy and Physiology For Health and ExercisesamNoch keine Bewertungen
- Running Head: OSTEOPOROSIS 1Dokument7 SeitenRunning Head: OSTEOPOROSIS 1AssignmentLab.comNoch keine Bewertungen
- Review Article: Aging and Osteoarthritis: An Inevitable Encounter?Dokument7 SeitenReview Article: Aging and Osteoarthritis: An Inevitable Encounter?Iicha Phine'ToxicNoch keine Bewertungen
- A Comparative Survey On Supervised Classifiers For Face RecognitionDokument6 SeitenA Comparative Survey On Supervised Classifiers For Face RecognitionHarun NasutionNoch keine Bewertungen
- Ukhuwah Islamiyah Dan Ukhuwah InsaniyahDokument9 SeitenUkhuwah Islamiyah Dan Ukhuwah InsaniyahAbdurrohim NurNoch keine Bewertungen
- MmenuDokument8 SeitenMmenublanktropNoch keine Bewertungen
- Face Detection With The Faster R-CNN: Abstract - While Deep Learning Based Methods For GenericDokument8 SeitenFace Detection With The Faster R-CNN: Abstract - While Deep Learning Based Methods For GenericHarun NasutionNoch keine Bewertungen
- Deep Learning For Facial Expression Recognition - A Step Closer To A Smartphone That Knows You MoodsDokument4 SeitenDeep Learning For Facial Expression Recognition - A Step Closer To A Smartphone That Knows You MoodsHarun NasutionNoch keine Bewertungen
- Aquarium-Clownfish e I A4 1Dokument2 SeitenAquarium-Clownfish e I A4 1Ian ZackNoch keine Bewertungen
- Coo Vernal Kconj v10Dokument2 SeitenCoo Vernal Kconj v10schizodhiNoch keine Bewertungen
- AnnNuclMedSci05!18!143 (3 Huang)Dokument6 SeitenAnnNuclMedSci05!18!143 (3 Huang)Harun NasutionNoch keine Bewertungen
- 59 211 1 PBDokument5 Seiten59 211 1 PBHarun NasutionNoch keine Bewertungen
- Target Pressures in Glaucoma: Key WordsDokument5 SeitenTarget Pressures in Glaucoma: Key WordsHarun NasutionNoch keine Bewertungen
- Objectives:: Ahmed H. Al-SalemDokument4 SeitenObjectives:: Ahmed H. Al-SalemHarun NasutionNoch keine Bewertungen
- Chapter 14: Bone Disease and Calcium Abnormalities in Elderly Patients With CKDDokument5 SeitenChapter 14: Bone Disease and Calcium Abnormalities in Elderly Patients With CKDHarun NasutionNoch keine Bewertungen
- Vocals Guitar Mandolin Mandola Ukulele Keybo Ards The Remedy (I Won't Worry)Dokument1 SeiteVocals Guitar Mandolin Mandola Ukulele Keybo Ards The Remedy (I Won't Worry)Harun NasutionNoch keine Bewertungen
- Section 7Dokument11 SeitenSection 7Harun NasutionNoch keine Bewertungen
- Osteo RXDokument27 SeitenOsteo RXHarun NasutionNoch keine Bewertungen
- Vermiform AppendixDokument4 SeitenVermiform AppendixHarun NasutionNoch keine Bewertungen
- Alvorado ComparingDokument8 SeitenAlvorado ComparingHarun NasutionNoch keine Bewertungen
- Ajessp 2005 130 132Dokument3 SeitenAjessp 2005 130 132Harun NasutionNoch keine Bewertungen
- IndianJRadiolImaging164523-8683965 022443Dokument10 SeitenIndianJRadiolImaging164523-8683965 022443Harun NasutionNoch keine Bewertungen
- Acute Appendicitis - A 5-Year Review of Histopathology and Clinical PresentationDokument4 SeitenAcute Appendicitis - A 5-Year Review of Histopathology and Clinical PresentationJuan Carlos SantamariaNoch keine Bewertungen
- Acute Appendicitis - A 5-Year Review of Histopathology and Clinical PresentationDokument4 SeitenAcute Appendicitis - A 5-Year Review of Histopathology and Clinical PresentationJuan Carlos SantamariaNoch keine Bewertungen
- Clinical Correlation of Acute Appendicitis With Histopathological Diagnosis: A Prospective StudyDokument5 SeitenClinical Correlation of Acute Appendicitis With Histopathological Diagnosis: A Prospective StudyHarun NasutionNoch keine Bewertungen
- 94 FullDokument5 Seiten94 FullHarun NasutionNoch keine Bewertungen
- Imaging of Appendicitis A Cautionary NoteDokument4 SeitenImaging of Appendicitis A Cautionary NoteHarun NasutionNoch keine Bewertungen
- A Clinical Study of Acute Appendicitis and Role of Ultrasonography in Its DiagnosisDokument6 SeitenA Clinical Study of Acute Appendicitis and Role of Ultrasonography in Its DiagnosisMeva DowintaNoch keine Bewertungen
- Acute Appendicitis The Reliability of DiagnosisDokument6 SeitenAcute Appendicitis The Reliability of DiagnosisHarun NasutionNoch keine Bewertungen
- Manage Care 2012Dokument40 SeitenManage Care 2012Harun NasutionNoch keine Bewertungen
- 59 211 1 PBDokument5 Seiten59 211 1 PBHarun NasutionNoch keine Bewertungen
- Cowo Bmi N TinggiDokument1 SeiteCowo Bmi N TinggiAndi WirawanNoch keine Bewertungen
- Gel Polish and Dry Manicure Manual EDITABLEDokument56 SeitenGel Polish and Dry Manicure Manual EDITABLECristina Gradinari100% (1)
- "Sandwich" Bone Augmentation Technique-Rationale and Report of Pilot Cases PDFDokument14 Seiten"Sandwich" Bone Augmentation Technique-Rationale and Report of Pilot Cases PDFHector MurilloNoch keine Bewertungen
- Functionally Graded Materials Design ProDokument339 SeitenFunctionally Graded Materials Design Prosivakrishna nadakuduruNoch keine Bewertungen
- Group 10, VitaminsDokument12 SeitenGroup 10, VitaminsALCORUNoch keine Bewertungen
- Orthopedic NursingDokument19 SeitenOrthopedic NursingDa BondadNoch keine Bewertungen
- Skeletal SystemDokument5 SeitenSkeletal SystemWynne Michael David GogoNoch keine Bewertungen
- Final 1 (12TH June) - 230530 - 115919Dokument26 SeitenFinal 1 (12TH June) - 230530 - 115919Arda DumanNoch keine Bewertungen
- Animal Form and FunctionDokument18 SeitenAnimal Form and FunctionJerome Formaran100% (4)
- Naw TrainingDokument34 SeitenNaw Trainingganesh pNoch keine Bewertungen
- Multiapproach Orthopaedic ManagementDokument68 SeitenMultiapproach Orthopaedic ManagementDz PutraNoch keine Bewertungen
- Effective Functional Progressions in Sport Rehabilitation (2009) PDFDokument251 SeitenEffective Functional Progressions in Sport Rehabilitation (2009) PDFThunder Cracker100% (1)
- JC FMH Revisited 1 The Role of Mechano - TransductionDokument31 SeitenJC FMH Revisited 1 The Role of Mechano - Transductionchirag sahgalNoch keine Bewertungen
- Exsc 223 Practice Exam 2Dokument11 SeitenExsc 223 Practice Exam 2kimber brownNoch keine Bewertungen
- The Ultimate Guide FullDokument223 SeitenThe Ultimate Guide FullNBA ITALIANoch keine Bewertungen
- Miley Ped - RadiologyDokument52 SeitenMiley Ped - RadiologyLukasNoch keine Bewertungen
- Combined Effect of Nicotine and Caffeine On Orthodontic Tooth Movement in RatsDokument6 SeitenCombined Effect of Nicotine and Caffeine On Orthodontic Tooth Movement in RatsHusni mubarakNoch keine Bewertungen
- Paul Cavel - Cultivating SungDokument12 SeitenPaul Cavel - Cultivating SungConstanze Heringer100% (3)
- Chapter 4 Non Infectious DiseasesDokument32 SeitenChapter 4 Non Infectious DiseasesLove IsNoch keine Bewertungen
- Edith Jacobson Care PlanDokument10 SeitenEdith Jacobson Care PlanKarina Rodriguez100% (3)
- Shattered Lives and Broken Childhoods Ev PDFDokument12 SeitenShattered Lives and Broken Childhoods Ev PDFDiana Rocio Carvajal ContrerasNoch keine Bewertungen
- Haversian System (Osteon) : Basic Structural UnitDokument7 SeitenHaversian System (Osteon) : Basic Structural UnitJulius Matthew MarananNoch keine Bewertungen
- RefDokument6 SeitenRefanggitatriyurisworoNoch keine Bewertungen
- Patho (Osteosarcoma)Dokument1 SeitePatho (Osteosarcoma)Maan AdriculaNoch keine Bewertungen
- Physiology of BoneDokument32 SeitenPhysiology of BoneAnandhu GNoch keine Bewertungen
- Comprehensive Report Card: About The Probably Hidden ProblemsDokument2 SeitenComprehensive Report Card: About The Probably Hidden ProblemsShashikanth RamamurthyNoch keine Bewertungen
- Decalcification: MR G.P. Tiwari Technologist Tata Memorial HospitalDokument42 SeitenDecalcification: MR G.P. Tiwari Technologist Tata Memorial HospitalGulab Chand Tiwari Tiwari100% (5)
- 10 Amazing Facts About The Human Body - OSGDokument6 Seiten10 Amazing Facts About The Human Body - OSGprince christopherNoch keine Bewertungen
- Fracture On FemurDokument68 SeitenFracture On FemurHerwincaye100% (3)
- James Bruot Science Summative - Myp3Dokument6 SeitenJames Bruot Science Summative - Myp3api-512094211Noch keine Bewertungen
- Joints: Bones in The Shoulder and Chest: Types of Movable JointsDokument2 SeitenJoints: Bones in The Shoulder and Chest: Types of Movable JointsLloyd LagadNoch keine Bewertungen