Beruflich Dokumente
Kultur Dokumente
Menstrual Physiology, Amenorrhea: Page 1 of 5
Hochgeladen von
seth10Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Menstrual Physiology, Amenorrhea: Page 1 of 5
Hochgeladen von
seth10Copyright:
Verfügbare Formate
Menstrual Physiology, Amenorrhea Dra.
Brion October 19, 2011
III-2
MENSTRUAL CYCLE Ideal 28 day cycle. Midcycle is marked by ovulation. Dependent on the interplay of pituitary and ovarian hormones. Predominant hormones involved: o GnRH from the hypothalamus. o FSH and LH from the anterior pituitary gland, secreted in response to GnRH. o Estrogen and Progesterone from the ovary, in response to FSH and LH. MENSTRUAL PHASE FSH Day 1 = 1st day of menses Ovarian Cycle changes during the cycle depends completely on the gonadotropic hormones FSH and LH. Folicular Phase / Endometrial Proliferation Phasepreovulatory:estrogen Luteal Phase / Secretory Phase postovulatory: progesterone Day 4: ovulation day LH surge happens to promote ovulation Estrogen has a rapid increase and then a sudden drop. Then a sudden surge of progesterone happens. Female menstrual cycle is determined by a complex interaction of hormones Predominant hormones involved in the menstrual cycle are GnRH, FSH, LH, estrogen and progesterone GnRH is secreted by the hypothalamus LH and FSH are secreted at the level of the ovary GnRH stimulates the secretion of LH and FSH from the anterior pituitary gland GnRH stimulates the secretion of LH and FSH from the anterior pituitary gland GnRH secreted from the hypothalamus in a pulsatile manner throughout the cycle. Early follicular phase is frequent of GnRH secretion: 1/90 minutes and 1/60 70 minutes Luteal phase decreases with increase in amplitude GnRH induces the release of both FSH and LH, but LH is much more sensitive to change in GnRH levels secreted by the anterior pituitary gland For follicular growth until antrum develops Secretion is highest and most crucial during the first week of the follicular stage of the menstrual cycle o time of follicle recruitment Negative feedback on GnRH. Induce estrogen and progesterone secretion at the level of the ovary. Induces the proliferation of granulose cell expression of LH reception on granulosa cells.
LH
secreted by the anterior pituitary gland required for the growth and preovulatory follicles; and the luteinization and ovulation of the dominant follicles Follicular phase-LH induces androgen synthesis by theca cells o stimulation, proliferation, differentiation and secretion of follicular theca cells and increase on granulose cells Preovulatory LH surge drives the oocyte into the 1st meiotic division and initiates luteinization of thecal and granulose cells. The resulting corpus luteum produces high levels of progesterone and some estrogen
ESTROGEN produced at the level of the ovary and is crucial for the development of the antrum and the maturation of the graafian follicle predominant at the end of the follicular phase directly preceding ovulation Estradiol, the most potent and abundant estrogen, is primarily derived from androgens migrating from the thecal cells to the granulose cells, where they are converted into estradiol by aromatase enzymes. Action of estradiol involves induction of FSH receptor on the granulose cells, proliferation and secretion of the follicular thecal cells At low circulatory levels, estrogen exerts negative feedback on FSH and LH secretion. Estrogen further induces proliferation of more estrogen-granulose cell and the synthesis of estrogen receptors establishing positive feedback loop on itself. In the uterine cycle, estrogen induces proliferation of endometrial glands. PROGESTIN secreted at the level of the ovary by luteinized follicles. first to be stimulated in progestin synthesis: requires p450 enzymes Levels increase prior to ovulation and peaks 5-7 days after. induce migration of blood vessels in the follicle walls and stimulate prostaglandin secretion on follicular tissues During the luteal phase, progesterone induces swelling and increase secretion of the endometrium
Page 1 of 5
PHASES
AMENORRHEA Absence or cessation of menstrual blood flow during the reproductive period Categories: Physiologic Postpartum lactation Pregnancy Menopause Pathologic - absence of menses due to an anatomic or endocrinologic disorder o Primary Amenorrhea - failure of flow to commence before 16.5 years of age o Secondary Amenorrhea - absence of menses for at least 3 months in woman who previously had regular spontaneous menstrual period o Cases of investigation Primary amenorrhea at age 16 with normal secondary sexual development Primary amenorrhea at age 14 without normal secondary sexual development Amenorrhea for 3 months duration in previously menstruating female PRIMARY AMENORRHEA Grouping with primary amenorrhea with normal external genitalia as the basis of the presence or absence of secondary sexual characteristic (breast) and female external genitalia (uterus) o Breast = estrogen activity= intact HPO axis o Uterus = structurally intact reproductive tract
PROLIFERATIVE PHASE spans period from the end of menses until ovulation increase levels of estrogen induce proliferation in the zona functionalis from the stem cells of the basalis proliferation of the stromal glands and the stromal connective tissue endometrial glands are elongated with narrow lumen and their cells contain some glycogen. Glycogen however is not secreted during the follicular phase Spiral antrum elongate and stimulates the length of the endometrium SECRETORY PHASE from the ovulation and last until the menstrual phase of the next cycle progesterone induces the endometrial glands to secrete glycogen, mucus and other substances These glands become tortuous Without fertilization by day 23 of the menstrual cycle, corpus luteum begins to degenerate and consequently ovarian hormone levels decrease Estrogen and progestin levels decrease, the endometrium undergoes involution Day 25-26 menstrual cycle, endothelia and thromboxane begin to mediate vasoconstriction of the spiral arteries Resulting ischemia may cause early menstrual cramps. By day 28, intense vasoconstriction and subsequent ischemia cause mass apoptosis of the functionalis. MENSTRUAL PHASE spiral arteries rupture due to ischemia apoptosed endometrium is slough off and usually last for four days the functionalis is completely shed as menstrual flow (arterial and venous blood, remnants of endometrial stoma and glands, RBS and WBC).
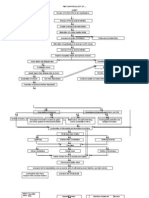
CATEGORY 1. BREAST ABSENT, UTERUS PRESENT Most common category Primary amenorrhea without breast development / uterus present Serum FSH
LOW / NORMAL Hypogonadotropic
HIGH Hypergonadotropic
Hypogonadism
Prolactin, CT-Scan NORMAL HIGH Pituitary Adenoma
Hypogonadism
BP
NORMAL
HIGH 17-Hydroxylase Deficiency
Non-Prolactin Secreting tumor, Inadequate GnRH
Karyotype Gonadal dysgenesis
Causes: 1.) Hypogonadotropic hypogonadism low FSH, LH; Low estrogen, progesterone CNS tumors o Non prolactin secreting tumor rare, chromophobe adenomas, pharyngiomas
Page 2 of 5
Pituitary adenomas- MC, elevated prolactin, respond well to bromocripitine, increase PRL inhibit estrogen Congenital anatomic defect Insufficient GnRH secretion due to neurotransmitter defect Inadequate GnRH release or secretion o Eg. Kallmans syndrome (amenorrhea + anosmia) o Normal ovaries but lack gonadotropin-stimulating development o When pregnancy id desired may give pulsating GnRH or HMG stimulate ovulation 2.) Hypergonadotropic Hypogonadism Gonadal failure 60% primary amenorrhea Increased FSH and LH Decrease estrogen and progesterone Result to different syndromes: o Turners syndrome 45X MC chromosomal abnormality causing gonadal failure and primary amenorrhea o 46X, abnormal X (deletional disorder) o Mosaicism (X/XX,X/XX/XXX) structurally abnormal x may be due to deletions in the long or short arms, ring formation or minute fragmentations. short like turners syndrome but with somatic abnormalities o 46XX or 46XY pure gonadal dysgenesis Absent secondary sexual characteristics Gonads are fibrous commonly have Y chromosomes o 46XX with 17-hydroxylase deficiency extremely rare Impaired cortisol production Cortisol and sex steroid replacement Hypertension Lethal when left untreated - hypernatremia and hypokalemia hypertension Early electrolyte intervention MANAGEMENT: o All indications in this category are hypoestrogenic due to CNS abnormalities o Treatment: estrogen/progesterone replacement for withdrawal bleeding and enhance breast development o CATEGORY 2. BREAST PRESENT, UTERUS ABSENT
Absence of androgen receptor synthesis leading to failure of differentiation of male external and internal genitalia o Pubic and axillary hair fail to develop o Abnormal sexual differentiation and a Y chromosome mandates gonadal extirpation because of high risk for malignant degeneration of the dysgenetic gonad; about 20% among AI/TF after 20yo o In this case, gonadectomy done after puberty for endogenous hormonal stimulation of breasts and long bone epiphyses followed by E/P replacement therapy. Congenital absence of uterus (Rokitansky-Kuster_hauser syndrome) o Agenesis, mullerian problem o Uterus and outflow tract fail to develop o Ovaries remain anatomically and endocrinologically functional o Renal and skeletal anomalies - need urogram and skeletal x-ray o Treatment: surgical construction and progressive vaginal dilation - done at sexual debut o
CATEGORY 3. BREST ABSENT, UTERUS ABSENT Karyotype XY Laparoscopy
Testes PRESENT
Testes ABSENT
17,20 Desmolase Deficiency 17-Hydroxylase Deficiency
Agonadism
Testosterone
NORMAL
HIGH
Rare, not enough androgen production Least common Male karyotype: phenotypically female (FSH, testosterone in female range) Estrogen therapy to induce development of breast and enhance female features o 17,20 desmolase deficiency o 17-hydroxylase deficiency with 46XY karyotype leads to inadequate testosterone synthesis and testicular development o Agonadism Gonadectomy: to diminish remaining male hormone effect Probably occurs after MIF elaboration because no female ductal structures are seen Vanishing testes syndrome during embryonic life 46XY but no gonadal tissue laparoscopy
Congenital absence of Uterus
Androgen insensitivity (testicular feminization)
Causes: Androgen insensitivity (testicular feminization) o XY but phenotypically female o X-linked recessive, sex autosomal dominant disorder o Testosterone level normal range for males o Receptor present but insensitive to testosterone
Page 3 of 5
CATEGORY 4. BREAST PRESENT, UTERUS PRESENT
Prolactin
NORMAL
INCREASED
Hypothalamic, Pituitary, Ovarian, Uterine outflow
Pituitary lesion Prolactinoma
Decrease GnRH Hypothalamic etiology Pituitary etiology Ovarian etiology Uterine ouflow tract cause Causes: o Hyperprolactenimia about 25% cases o Normal prolactin hypothalamic pituitary Management: manage like secondary amenorrhea
Stress and strenuous exercise (self-limiting) o Catecholestrogen levels rises which reduce rate of catecholamine degradation and increase its availability for dopamine synthesis which suppresses GnRH release o Endorphin levels increase during exercise negative action on GnRH secretion and enhance dopamine secretion amenorrhea o Menses return when stress or exercise abates Weight loss o Amenorrhea induced in those with Weight loss in whom Body weight is >15% below Ideal Body Weight o Relatively small proportion of body fat shifts peripheral estrogen metabolism to formation of more catecholestrogen inhibit GnRH release amenorrhea (e.g. anorexia nervosa) Hypothalamic dysfunction o No cyclic pulsatile LH secretion because of abnormal GnRH pulsatility due to transmitter dysfunction o Circulating estradiol level > 40pg/ml (+) progesterone withdrawal bleeding o No bleeding < estrogen pituitary failure o differentiate from hypothalamic-pituitary failure where estradiol levels are <40 pg/ml
SECONDARY AMENORRHEA Definition: absence of menses for at least 3 months in a woman who previously had regular spontaneous menstrual periods Causes: o HPO axis causes, uterus outflow disorder
Pituitary Causes Neoplasms CT scan/MRI o prolactin secreting bromocriptine o nonprolactin secreting surgical Non-neoplastic conditions o excessive hemorrhage, anoxia, thrombotic episodes which cause destruction of Pituitary cells o Sheehans syndrome - related to pregnancy o Simmonds disease unrelated to pregnancy o Due to treatment hormonal replacement, low FSH, LH, ACTH, TSH adrenal insufficiency Note: American Congress of Obstetricians and Gynecologists (ACOG) PITUITARY DYSFUNCTION Hyperprolactinemia Prolactinomas account for 20% of secondary amenorrhea Pituitary adenomas Prolactin-secreting lactotroph-adenomas Non-functional adenomas Functional thyrotroph adenomas (secreting TSH and causing hyperthyroidism) Somatotroph adenomas (secreting GH and causing acromegaly) Corticotroph adenomas (secreting ACTH and causing Cushings disease) Other pituitary masses (craniopharyngiomas, meningiomas, cysts) Pituitary infarct/infiltration Sheehans syndrome, radiation, infiltration (hemachromatosis, lymphocytic) Ovarian causes ovaries unable to secrete estrogen for uterine priming Infections Decreased blood supply after surgery Depletion of follicles after cystectomy Irradiation Systemic Chemotherapy Autoimmune disease
Note: American Congress of Obstetricians and Gynecologists (ACOG) Etiology: o Dont forget PREGNANCY! Most common cause of secondary amenorrhea Rule out with a urine or serum hcg before proceeding o Consider each level of the control of menstrual cycle: Hypothalamus endocrine regulation of the Pituitary menstrual cycle Ovary Uterus responds to endocrine cues from the HPO axis Cervix involved structurally in the Vagina outflow of menstrual blood
Hypothalamic Causes CNS lesions that interfere with GnRH release craniopharyngiomas, granulomatous disease (TB, sarcoidosis) Drugs: o Phenothiazines, Reserpine - cause hyperprolactinemia and inhibit gonadotropin release o OCPs prevent ovulation by suppressing GnRH and Gn action and may persist up to 6 months after stopping the pills post-pill amenorrhea
Page 4 of 5
Note: American Congress of Obstetricians and Gynecologists (ACOG) OVARIAN DYSFUNCTION Ovarian failure (menopause): 1 year of amenorrhea due to depletion of oocytes Spontaneous: typically occurs at age 52 in American women Premature: < 40 years old Autoimmune conditions o lymphocytic infiltrate in theca cells of ovarian follicles Chemotherapy/radiation Fragile X premutation Karyotypic abnormalities o Turner Syndrome, loss of small portion of X chromosome, mosaic Turner Syndrome, presence of Y chromatin material Surgical Hyperandrogenism Polycystic Ovary Syndrome (PCOS) Accounts for 20% of cases of amenorrhea Manifestations include: o Hirsutism o Acne o Menstrual irregularities o Obesity o Acanthosis nigricans o Premature pubarche, and/or precocious puberty To diagnose, any 2 of 3: o Oligomenorrhea/amenorrhea o Signs of androgen excess o Presence of polycystic ovaries on ultrasound ( 12 follicles)
Uterine and Outflow tract Ashermans syndrome o intrauterine adhesions that interfere with endometrial growth due to D&C pospartum curettage, endometritis esp. TB, myomectomy, metroplasty o adhesiolysis by hystereocopy or D&C indwelling pedia FC for 10 days, AB and high dose estrogen (2.5mg daily for 3 wks with MPA 10 mg OD during the 3rd wk) o Transverse vaginal septum septum at any level of the vaginal canal o Imperforate hymen septum located in the introitus o Cervical stenosis congenital or s/p cautery or conization Note: American Congress of Obstetricians and Gynecologists (ACOG) ASHERMANS SYNDROME Results from acquired scarring of endometrial lining Secondary to postpartum hemorrhage or endometrial infection, followed by instrumentation (i.e. D & C) Diagnosis suggested by: absence of normal uterine stripe on pelvic ultrasound Absence of withdrawal bleeding after sequential administration of estrogen, then progestin. Can confirm diagnosis by Hysteroscopic evaluation
*MPA - medroxyprogesterone acetate
MPA 5-10mg BID X 5days Uterine Bleeding LH High (>25mL) PCOS (LH:FSH = >3) Normal LH FSH Hypothalamic dysfunction Normal to Low High (>30 mIU/mL) Premature Ovarian Follicle (POF) <35 24 hour urine free cortisol NO Uterine Bleeding Pituitary lesion Prolactinoma
Testosterone (ovarian), DHEAS (adrenal)
Normal Induce bleeding, dexamethasone, spironolactone
Prolactin
HypothalamicPituitary Failure
High PRL, CT-Scan, ACTH Reserve test
MPA 10mg/day x 12days
Work-up for Hyperprolactinemia
A gynecologist had become fed up with malpractice insurance and was on the verge of being burned out. Hoping to try another career where skillful hands would be beneficial, he decided to become a Mechanic. He found out from the local technical college what was involved, signed up for evening classes, attended diligently, and learned all he could. When the time for the practical exam approached, the gynecologist prepared carefully for weeks and completed the exam with tremendous skill. When the results came back, he was surprised to find that he had made a score of 150%. Fearing an error, he called the instructor, saying, I dont want to appear ungrateful for such an outstanding result, but I wondered if there had been an error which needed adjusting. The instructor said, During the exam, you took the engine apart perfectly, which was worth 50% of the total mark. You put the eng ine back together again perfectly, which is also worth 50% of the mark. After a pause, the instructor added I gave you an extra 50% because you did all of it through the muffler.
Page 5 of 5
Das könnte Ihnen auch gefallen
- Maternal Health Review of Female Pelvis AnatomyDokument80 SeitenMaternal Health Review of Female Pelvis AnatomyHayes Clover100% (6)
- 1642497170754_Family Health 1 - CopyDokument20 Seiten1642497170754_Family Health 1 - CopyGoogle MediaNoch keine Bewertungen
- Female HormoneDokument43 SeitenFemale Hormoneامجد حسين جواد كاظمNoch keine Bewertungen
- Oxytocin, ADH Lecture For 2nd Year MBBS by DR Waeem KausarDokument28 SeitenOxytocin, ADH Lecture For 2nd Year MBBS by DR Waeem KausarIMDCBiochemNoch keine Bewertungen
- Problem No.1Dokument34 SeitenProblem No.1ayesha bgNoch keine Bewertungen
- Reproductive SystemDokument32 SeitenReproductive SystemEdwin OkonNoch keine Bewertungen
- MCN Menstrual Cycle LatestDokument8 SeitenMCN Menstrual Cycle LatestsophienNoch keine Bewertungen
- Female Physiology 1Dokument2 SeitenFemale Physiology 1JayricDepalobosNoch keine Bewertungen
- PHYSIOLOGY OF THE MENSTRUAL CYCLE بحث دكتوره ميDokument22 SeitenPHYSIOLOGY OF THE MENSTRUAL CYCLE بحث دكتوره ميSoma Al-otaibyNoch keine Bewertungen
- Fisiologi MenstruasiDokument3 SeitenFisiologi MenstruasiSyahnaz Mardiah AlkatiriNoch keine Bewertungen
- Reproductive HormonesDokument43 SeitenReproductive HormonesMunchkin CelinaNoch keine Bewertungen
- Hormonal Cycles: Ovarian CycleDokument5 SeitenHormonal Cycles: Ovarian CycleashuNoch keine Bewertungen
- IntroDokument7 SeitenIntroibrahim.21hm32Noch keine Bewertungen
- The complete guide to understanding the menstrual cycle and causes of amenorrheaDokument9 SeitenThe complete guide to understanding the menstrual cycle and causes of amenorrheaDista ArifanyNoch keine Bewertungen
- Normal Menstrual Cycle The ProcessDokument6 SeitenNormal Menstrual Cycle The ProcessBrett StevensonNoch keine Bewertungen
- Physiology of Female Reproductive SystemDokument57 SeitenPhysiology of Female Reproductive SystemIshaqNoch keine Bewertungen
- TP Anglais FinalDokument7 SeitenTP Anglais FinalGift NgongoNoch keine Bewertungen
- Stages of Puberty - Sundhed - DKDokument6 SeitenStages of Puberty - Sundhed - DKPavel BerlinschiNoch keine Bewertungen
- Menstrual CycleDokument41 SeitenMenstrual CyclesharimileeratnamNoch keine Bewertungen
- Fisiologi HaidDokument3 SeitenFisiologi HaidAndi Farid ANoch keine Bewertungen
- Physiology of The Menstrual Cycle 2Dokument22 SeitenPhysiology of The Menstrual Cycle 2anoy judeNoch keine Bewertungen
- NEW Physiology PAP 2 Ovarian and Uterine CyclesDokument33 SeitenNEW Physiology PAP 2 Ovarian and Uterine CyclesbhumeekakhadayatNoch keine Bewertungen
- MCN Cover To Cover ?Dokument247 SeitenMCN Cover To Cover ?Elsid Nathaniel S. MartinNoch keine Bewertungen
- Pregnancy Preparation: The Menstrual CycleDokument4 SeitenPregnancy Preparation: The Menstrual CycleTobias GummNoch keine Bewertungen
- MK Disorders of Menstruation (OBGY)Dokument76 SeitenMK Disorders of Menstruation (OBGY)Moses Jr KazevuNoch keine Bewertungen
- The Female Reproductive System: Paul F. Terranova, PH.DDokument17 SeitenThe Female Reproductive System: Paul F. Terranova, PH.DMekuriya BeregaNoch keine Bewertungen
- ENDO #6 - Reproductive Endocrinology of The Female - 13.10.23Dokument22 SeitenENDO #6 - Reproductive Endocrinology of The Female - 13.10.23sbobine.imsNoch keine Bewertungen
- Menstrual Cycle HormonesDokument3 SeitenMenstrual Cycle HormonesAine GrahamNoch keine Bewertungen
- Physiology of MenstruationDokument52 SeitenPhysiology of Menstruationmahirad001100% (2)
- Notes Infertility Delayed PubertyDokument9 SeitenNotes Infertility Delayed PubertyTONY GO AWAYNoch keine Bewertungen
- Ovarian CycleDokument78 SeitenOvarian CyclefasicaregroupNoch keine Bewertungen
- Physiology of The Menstrual Cycle 1Dokument22 SeitenPhysiology of The Menstrual Cycle 1annonymousNoch keine Bewertungen
- Female PubertyDokument24 SeitenFemale PubertyHeba Khalid Al-HashmeyNoch keine Bewertungen
- Female HormonesDokument28 SeitenFemale HormonesmujahidalmakiNoch keine Bewertungen
- Menstrual Irregularities: Causes and Tracking ChangesDokument6 SeitenMenstrual Irregularities: Causes and Tracking ChangesLioraNoch keine Bewertungen
- Menstrual Cycle: The Ovarian and Uterine CyclesDokument10 SeitenMenstrual Cycle: The Ovarian and Uterine Cyclesfitrah fajrianiNoch keine Bewertungen
- SBM Reproduction NotesDokument73 SeitenSBM Reproduction NotesAhra100% (2)
- Ovulation and Menstration: Hormone ActionDokument4 SeitenOvulation and Menstration: Hormone ActionPaolo QuezonNoch keine Bewertungen
- Menstrual Cycle Stages and Hormone RegulationDokument6 SeitenMenstrual Cycle Stages and Hormone RegulationNida RidzuanNoch keine Bewertungen
- Mammalian Reproductive SystemDokument50 SeitenMammalian Reproductive SystemLeena MuniandyNoch keine Bewertungen
- OBGYN End of Rotation Exam OutlineDokument35 SeitenOBGYN End of Rotation Exam OutlinehevinpatelNoch keine Bewertungen
- Hormonal Cycles: Presented By: Miss. M.K.Kaku Nursing TutorDokument23 SeitenHormonal Cycles: Presented By: Miss. M.K.Kaku Nursing TutorKaku ManishaNoch keine Bewertungen
- RATHNADokument30 SeitenRATHNAhaisuresh100% (1)
- EndocrinologyDokument7 SeitenEndocrinologyVijith.V.kumarNoch keine Bewertungen
- Gonad Overview 2023 ADokument103 SeitenGonad Overview 2023 AElena Borş MorariNoch keine Bewertungen
- Imported FileDokument18 SeitenImported Fileg8pn6pt8nhNoch keine Bewertungen
- Tog 12665Dokument13 SeitenTog 12665saeed hasan saeed100% (1)
- Reproductive SystemDokument30 SeitenReproductive SystemmfaizchejamriNoch keine Bewertungen
- BIO ProjectDokument17 SeitenBIO ProjectHârsh V ÎshwãkårmāNoch keine Bewertungen
- Menstrual Cycle and Fertility by Neville Mvo NgumDokument7 SeitenMenstrual Cycle and Fertility by Neville Mvo Ngumlovelyc95Noch keine Bewertungen
- Female HormonesDokument28 SeitenFemale Hormonesİlbey Kayra Özçelik100% (1)
- MENSURATION: Understanding the Female Menstrual CycleDokument24 SeitenMENSURATION: Understanding the Female Menstrual Cyclesanjeev kumarNoch keine Bewertungen
- Gyne - Physiology of MenstruationDokument66 SeitenGyne - Physiology of MenstruationonijinoNoch keine Bewertungen
- Ovarian and Menstrual CyclesDokument7 SeitenOvarian and Menstrual CyclesMohamed FarahatNoch keine Bewertungen
- Physiology of The Menstrual CycleDokument17 SeitenPhysiology of The Menstrual Cyclezianab aliNoch keine Bewertungen
- Test #5 Notes 2Dokument29 SeitenTest #5 Notes 2api-3723612Noch keine Bewertungen
- Menstrual CycleDokument66 SeitenMenstrual CycleMelizza Fajardo Bañano100% (1)
- Physiology of MenstruationDokument3 SeitenPhysiology of MenstruationMIKAELA DAVIDNoch keine Bewertungen
- Endocrine PhysiologyDokument42 SeitenEndocrine PhysiologyNabila BaharNoch keine Bewertungen
- Hormone Replacement 101: A Guide for Evaluation and ManagementVon EverandHormone Replacement 101: A Guide for Evaluation and ManagementNoch keine Bewertungen
- Introduction to Clinical Reproductive EndocrinologyVon EverandIntroduction to Clinical Reproductive EndocrinologyBewertung: 1 von 5 Sternen1/5 (1)
- Ecv AsiaDokument8 SeitenEcv Asiaseth10Noch keine Bewertungen
- Score en SicaDokument11 SeitenScore en Sicaseth10Noch keine Bewertungen
- AmenorreaDokument9 SeitenAmenorreapenelopey39291Noch keine Bewertungen
- Acth 1Dokument7 SeitenActh 1seth10Noch keine Bewertungen
- AmenorreaDokument9 SeitenAmenorreapenelopey39291Noch keine Bewertungen
- Baby Fae CaseDokument6 SeitenBaby Fae Caseseth10Noch keine Bewertungen
- Tocoliticos en RPMDokument91 SeitenTocoliticos en RPMseth10Noch keine Bewertungen
- Compare and Contrast Plant and Animal Reproduction and DevelopmentDokument145 SeitenCompare and Contrast Plant and Animal Reproduction and DevelopmentAuxidyNoch keine Bewertungen
- The Menstrual CycleDokument18 SeitenThe Menstrual CycleSakshi Halve100% (1)
- 3 AE85 C4 CD 01Dokument131 Seiten3 AE85 C4 CD 01Troey X MezciastNoch keine Bewertungen
- The Female Reproductive Anatomy GuideDokument10 SeitenThe Female Reproductive Anatomy GuideBurni GuevaraNoch keine Bewertungen
- KittenzDokument89 SeitenKittenztrina sircarNoch keine Bewertungen
- Hsslive-xii-Zoology Focus Area Note 2023-By-SunilDokument26 SeitenHsslive-xii-Zoology Focus Area Note 2023-By-Sunilmurshida murshida cNoch keine Bewertungen
- Placenta and Placental Hormones: PDVDokument156 SeitenPlacenta and Placental Hormones: PDVMikeeeNoch keine Bewertungen
- Physiology of The Menstrual Cycle 1Dokument22 SeitenPhysiology of The Menstrual Cycle 1annonymousNoch keine Bewertungen
- Reproductive Health and ManagementDokument10 SeitenReproductive Health and ManagementWinnie PillyNoch keine Bewertungen
- 2021.2 - Exam Q&ADokument203 Seiten2021.2 - Exam Q&ALucas Victor AlmeidaNoch keine Bewertungen
- Disorders of The Female Reproductive System PDFDokument4 SeitenDisorders of The Female Reproductive System PDFSeff CausapinNoch keine Bewertungen
- Endometrial BiopsyDokument72 SeitenEndometrial BiopsySatish TatamiyaNoch keine Bewertungen
- Progresterone Assay InsertDokument7 SeitenProgresterone Assay InsertYogaswara AdiputroNoch keine Bewertungen
- Ain Shams MCQDokument84 SeitenAin Shams MCQمعتز حرارةNoch keine Bewertungen
- Reproduction System NotesDokument18 SeitenReproduction System NotesmorganicalNoch keine Bewertungen
- CK-12 Biology Chapter 25 WorksheetsDokument32 SeitenCK-12 Biology Chapter 25 WorksheetsDEEBANNoch keine Bewertungen
- Lecture Reproductive - Glands FinalDokument32 SeitenLecture Reproductive - Glands FinalerikaquitaraaaNoch keine Bewertungen
- Female Reproductive System Part 2 - SPC MLS 2F - Histo Lec PDFDokument13 SeitenFemale Reproductive System Part 2 - SPC MLS 2F - Histo Lec PDFCesmaine SanchezNoch keine Bewertungen
- 3 Human Reproduction-Entrance QuestionsDokument3 Seiten3 Human Reproduction-Entrance QuestionsStreet Dancer9.2Noch keine Bewertungen
- 613 Case Study EssayDokument13 Seiten613 Case Study EssaysheemalNoch keine Bewertungen
- Normal Menstrual CycleDokument20 SeitenNormal Menstrual CycleTrevor UratelNoch keine Bewertungen
- TNV 321Dokument202 SeitenTNV 321Principal PolytechnicNoch keine Bewertungen
- Pa Tho Physiology of Cesarean2Dokument2 SeitenPa Tho Physiology of Cesarean2sorryandreosayanisalreadytakenNoch keine Bewertungen
- Men CycDokument90 SeitenMen CycBrendon MuriraNoch keine Bewertungen
- Mother and Child Health: Theories of Procreation and Human ReproductionDokument390 SeitenMother and Child Health: Theories of Procreation and Human ReproductionJeonghwa Park100% (1)
- Ovarian Cysts Overview: Menstrual Cycle Pregnancy UltrasoundDokument13 SeitenOvarian Cysts Overview: Menstrual Cycle Pregnancy Ultrasoundzerocoolz123Noch keine Bewertungen
- Teaching LessonDokument13 SeitenTeaching LessonRizky AmaliaNoch keine Bewertungen
- Maternal Ob NotesDokument103 SeitenMaternal Ob NotesBoris OrbetaNoch keine Bewertungen
- Fisiologi HaidDokument3 SeitenFisiologi HaidAndi Farid ANoch keine Bewertungen