Beruflich Dokumente
Kultur Dokumente
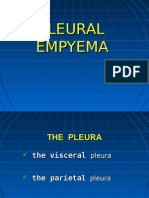
Pleura
Hochgeladen von
ameerabestCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pleura
Hochgeladen von
ameerabestCopyright:
Verfügbare Formate
DEFINITION
PLEURAL EFFUSION Abnormal collection of fluid in pleural space resulting from production , absorption. Normally contains fluid ; balance between 1.hydrostatic & oncotic forces (visceral & parietal pleural vessels) 2.extensive lymphatic drainage. **PE results from disruption of this balance. **PE classified as TRANSUDATE & EXUDATE. (refer table 1)
EMPYEMA Pus collection in pleural space. -maybe localized or involve entire pleural space. 1.Direct inoculation; penetrating injury / surgery 2. Contamination; -bronchopulmonary Infection. -Rupture of lung abscess, mediastinal abscess. -Transdiaphragmatic spread from subphrenic abscess. 3. Hematogenous spread (from distant sites) AEROBIC ANAEROBIC Gram +ve Bacteroids (strep, staph) Gram ve (coliforms, proteus, H.influenza) 1. Chest pain, purulent sputum, fever. 2. Dullness, air entry.
MESOTHELIOMA Tumor arising from mesothelial surfaces (pleura, peritoneum or pericardium).
ETIOLOGY
Types of PM: Localized -arises from mesothelial lining. -well-defined, encapsulated. -NOT ass. with ASBESTOS. -maybe BENIGN or MALIGNANT. -asymptomatic OR symptomatic (chest pain, cough) -Rx: surgical resection. Diffuse Always malignant, ass with ASBESTOS exposure.
CLINICAL PICTURE
INVESTIGATION
Small : ASYMPTOMATIC Large : dyspnea, cough, chest pain & low output syndrome if under tension. - breath sound & dullness to percussion. 1.Lab : ESR, CBC 2. CXR : Blunting of costophrenic angle (early sign) indicates accumulation more than 400 ml of fluid. 3. CT scanning & Ultrasound
1. Laboratory: Leucocytosis, high sedimentation rate. 2. Imaging : CXR : PE CT : Pleural collection, lung abscess, loculations, thickness of pleural peel,
1. Dyspnea 2. Chest wall pain 3. Weight loss 4. Weakness 5. Anorexia 6. Fever 1.Radiography (CXR, CT, MRI & PET scan): PE, Pleural thickening, mediastinal LN, distant metastases in advanced tumor. 2. Thoracocentesis. 3. Pleural needle biopsy. 4. Thoracoscopy & pleural biopsy.
TREATMENT
-assess PE, underlying lung, ass. Intrathoracic pathology. -localize fluid prior to thoracocentesis. -Plan biopsy or surgery. 4. Thoracocentesis: GROSS APPEARANCE: Bloody effusions malignancy after traumatic tap, with pulmonary embolus or TB. Milky fluid chylothorax Pus empyema ASPIRATE : 1.Microbiology 2. Cytology 3. Biochemistry -Total protein -LDH -Glucose -pH -Amylase -Triglycerides 4. Pleural biopsy -US guided percutaneous -CT guided percutaneous -VATS -Open (mini-thoracotomy) 1.Transudates & some exudates : RESOLVE 2.Moderate & massive effusions : Drainage with thoracocentesis or IC tube to an underwater seal. 3. Malignant PE : -pleurodesis
coexisting thoracic disease. US : pleural collections. 3. Thoracocentesis; Pus is examined for -Gross appearance. -Microbiology. Biochemistry; protein, glucose.
5. Open pleural biopsy. Pathologic types : Epithelial, sarcomatoid, mixed. Should be differentiated from metastatic adenocarcinoma with EM & Immunohistochemistry.
Causes of failure of empyema drainage Non-dependent drainage Tube inserted too far Tube too small Peel too thick dt late drainage Bronchoplueral fistula Presence of FB
1.General : Treat underlying cause, ass. Medical conditions(DM), physiotherapy, fluids & nutrition. 2. Antibiotics : systemic Ab 3. Surgery : a)Closed IC tube drainage : REMOVED when?
1. Radiation: palliate symptomatic chest wall or mediastinal involvement. 2. Chemotherapy : Response is disappointing. 3. Immunotherapy: Promising response with Interferon 4. Surgery:
-surgery -Home management of indwelling pleural catheter.
<100 ml, sterile, lung re-expands. -Instillation of fibrinolytic enzymes (streptokinase, urokinase) ; helps drainage of thick pus. b) Open IC tube drainage. c) Rib resection. d) Decortication. e) Thoracoplasty. 3 stages; 1. Exudative. 2. Fibrinopurulent. 3. Organization. Untreated empyema: 1.Pulmonary fibrosis & chest wall deformities. 2. Spontaneous drainage of pus through chest wall & bronchial tree. 3. Local spread of infection to pericardium or mediastinum. 4. Distant infection ( osteomyelitis) 5. Amyloidosis.
Thoracoscopy & talc pleurodesis Pleurectomy & decortication Extrapleural pneumonectomy : En-bloc resection of pleura, lung, ipsilateral hemidiaphragm, pericardium. MORTALITY is HIGH. Combined modality therapy (Radio & chemo)
Pathogenesis
Complications
TRANSUDATE (imbalance in oncotic & hydrostatic pressure) Congestive Heart Failure Hepatic Failure Renal Failure Hypoalbuminemia
EXUDATE (result of inflammation of pleura or decreased lymphatic drainage Infections (bacterial, TB, fungal, parasitic, viral) Collagen vascular disease (rheumatoid, SLE) Malignancy Pulmonary Embolus Hemothorax Chylothorax Pseudochylothorax Abdominal disease Drug induced
Miscellaneous Idiopathic
DEFINITION
HEMOTHORAX Accumulation of blood in pleural space.
ETIOLOGY
1.Trauma (most common: chest trauma) -blunt/penetrating ++rib fractures -source of bleeding : ITA, IC vessel, lung, bronchial, pulmonary, heart & great v. 2. Iatrogenic -post-operative -thoracocentesis -needle lung biopsy 3. Spontaneous pneumothorax Tear of vascular adhesions. 4.Bloody effusion -Pulmonary embolus -Neoplasm -TB
CHYLOTHORAX Abnormal collection of thoracic duct lymphatic fluid (chyle) in pleural space. - TG, and chylomicron. - Usually right sided. Pseudochylothorax: cholesterol but no TG or chylomicrons. 1. Congenital -birth trauma or TD abnormalities. 2. Traumatic -Blunt: Spinal hyperextension -Penetrating: Above T5(left), Below T5(right) 3. Operative -during of aortic arch, SCA, esophagus, especially transhiatal esophagectomy. 4. Neoplastic -Intrinsic or extrinsic TD obstruction 2ry to malignancy(lymphoma) duct rupture -direct invasionwith lung & esophageal cancer. ++ benign tumors (lymphangioma & mediastinal hygroma) 5. Infections
PNEUMOTHORAX Air in the pleural space.
1. Spontaneous a) Primary : Ruptured apical bleb dt localized form of onterstitial empysema. b) Secondary : ++ -COPD -CF -Infection; TB, mycotic, parasitic, cavitating nonspecific bacterial. -Tumors; Rupture of ischaemic primary / metastatoc lung carcinoma, lymphoma, sarcoma -Catamenial; ++menstruation (focal pleural endometriosis) -Miscellaneous ; ++ CT & AID 2. Traumatic -Iatrogenic : lung biopsy, central line
CLINICAL PICTURE
-obstruction TB lympadenitis, filariasis, ascending lymphangitis. 6. Miscellaneous -spontaneous (violent cough, vomit) -venous thrombosis (SVC, Lt SC, JV) -idiopathic Post-operative: Milky chest tube drainage Non-operative: Dyspnea, physical & radiological evidence of PE 1.index of suspicion following trauma. 2.Physical signs of pleural fluid & pallor. 3.CXR: evidences of pleural collection 4. Thoracocentesis is DIAGNOSTIC. 1. Thoracocentesis &pleural fluid analysis -Gram stain : Lymphocytosis, no bact. -Sudan stain : Fat globules -Fat content>plasma -Lipid analysis : C/TG <1 -lipoprotein electrophoresis : chylomicrons. 2. Radionucleide scanning : 99Tc antimony sulfide colloidlevel of TD obstruction & site of leakage. 3. Lympahangiography : site of obstruction & leakage. 4. CT scanning: define ++pathology. Aim : - Drain pleural space - Lung expansion - Reduce volume of TD leakage
insertion, barotrauma. -Penetrating or blunt chest trauma : Disruption of TB tree, pulmonary parenchymal, esophageal perforation, open pneumothorax. -Asymptomatic -Symptomatic : dyspnea, chest pain, dry cough, severe RD with hypoxia, hypercarbia & acidosis. Signs: breath sound & hyperresonance.
DIAGNOSIS
INVESTIGATION
1. CXR : Expiratory films accentuates small pneumothorax 2. CT : -diff lung cysts & bullae in presence of subcutaneous emphysema. -quantitates degree of penumothorax
TREATMENT
1.General; maintain airway, IV access, define blood group.. 2.ICT : 5th & 6th space MAL 3.Thoracotomy is indicated if:
1.Observation -asymptomatic & small pneumothorax 2. ICTD
-initial ICTD >1500ml blood OR >1000ml +hypotension -ICTD >300ml/hour for 3 hours. -drainage is inadequate with persistent collection on CXR. -manage associated intrathoracic injuries or pathology. -Evacuation of clotted hemothorax. After 4-6 weeks, clot organization requires DECORTICATION.
- Treat underlying cause. 1.Conservative: (within 2 weeks; 50 % close spontaneously) -ICTD -NPO -TPN with correction of fluid & electrolyte imbalance. 2. Operative Indication surgical : daily drainage of 1000ml (adults) OR 100ml/year of age (children) . 7 days -Right thoracotomy & mass ligation of TD above Rt hemidiaphragm in azygoesophageal recess. -Direct ligation at site of leak. -Anastomosis of TD to azygous vein, fibrin glue, radiotherapy, pleurodesis with talc.
-underwater seal & suction 3. Pleurodesis 4. Surgery (Open or VATS) -to resect bullae or blebs, close BP fistula, & obliterate pleural space to prevent recurrence. Indications of Surgery : Prolonged air leak Failure of lung to re-expand Tension pneumothorax Single large bullae Bilateral pneumothorax Hemopneumothorax Recurrent pneumothorax.
COMPLICATION
1.Persistent air leak 2. Recurrence 3. Tension pneumothorax 4. Hemothorax 5. Pneumomediastinum
Das könnte Ihnen auch gefallen
- Cardio Block 3Dokument62 SeitenCardio Block 3Maya LaPradeNoch keine Bewertungen
- Neuro Written II TablesDokument10 SeitenNeuro Written II TablesSolomon Seth SallforsNoch keine Bewertungen
- Neuro Written III TablesDokument5 SeitenNeuro Written III TablesSolomon Seth SallforsNoch keine Bewertungen
- Haematology-Summary My NotesDokument24 SeitenHaematology-Summary My NotesToria053Noch keine Bewertungen
- Concise SEO-Optimized Title for Clotting DocumentDokument3 SeitenConcise SEO-Optimized Title for Clotting DocumentRyan TurnerNoch keine Bewertungen
- ENDOCRINE PATHOLOGY WebpathDokument35 SeitenENDOCRINE PATHOLOGY Webpathapi-3766657Noch keine Bewertungen
- Hi Stop Hath Ology 2Dokument22 SeitenHi Stop Hath Ology 2vivek govardhanamNoch keine Bewertungen
- GI + Renal OSCE: AMSA Edinburgh X IMU Y4Dokument41 SeitenGI + Renal OSCE: AMSA Edinburgh X IMU Y4Abby LiewNoch keine Bewertungen
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDokument4 Seiten4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaNoch keine Bewertungen
- Handouts Integumentary Sys Sp11 B201Dokument7 SeitenHandouts Integumentary Sys Sp11 B201Kelly TrainorNoch keine Bewertungen
- Anatomy and Physiology MnemonicsDokument7 SeitenAnatomy and Physiology MnemonicsLalajimNoch keine Bewertungen
- Diseases - BiochemDokument4 SeitenDiseases - BiochemJay FeldmanNoch keine Bewertungen
- Pathology B - Gastrointestinal Tract (Esguerra, 2015) PDFDokument18 SeitenPathology B - Gastrointestinal Tract (Esguerra, 2015) PDFJem QuintoNoch keine Bewertungen
- Cerebral Blood FlowDokument39 SeitenCerebral Blood FlowRajat ThakurNoch keine Bewertungen
- Genetic Disorders-Www - Qworld.co - inDokument13 SeitenGenetic Disorders-Www - Qworld.co - inQworld100% (1)
- Less than 40 characters Key aging disorders and their genetic causesDokument3 SeitenLess than 40 characters Key aging disorders and their genetic causesvivek govardhanamNoch keine Bewertungen
- Kidney NewDokument4 SeitenKidney NewParth BhayanaNoch keine Bewertungen
- Gyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesDokument8 SeitenGyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesVon HippoNoch keine Bewertungen
- Table of Genetic DisordersDokument3 SeitenTable of Genetic DisordersEliNoch keine Bewertungen
- Anastomosis Left Anterior Cerebral Artery BlockageDokument5 SeitenAnastomosis Left Anterior Cerebral Artery BlockagemcwnotesNoch keine Bewertungen
- Brainstem StrokesDokument4 SeitenBrainstem StrokesChandniNoch keine Bewertungen
- DNA Viruses: P P P A H H PDokument2 SeitenDNA Viruses: P P P A H H PKimberly KanemitsuNoch keine Bewertungen
- Anat 6.3 GSA Appendix - EsguerraDokument4 SeitenAnat 6.3 GSA Appendix - Esguerralovelots1234Noch keine Bewertungen
- Disorders of Cho MetabolismDokument4 SeitenDisorders of Cho MetabolismJohn Christopher LucesNoch keine Bewertungen
- CerebellumDokument14 SeitenCerebellumapi-508474347Noch keine Bewertungen
- Dr. A. Samy TAG Bone Diseases - 1Dokument2 SeitenDr. A. Samy TAG Bone Diseases - 1Herato MenaNoch keine Bewertungen
- Abdominal Wall, Omentum, Mesentery, Retroperitoneum Anatomy and ConditionsDokument6 SeitenAbdominal Wall, Omentum, Mesentery, Retroperitoneum Anatomy and ConditionsMon Ordona De GuzmanNoch keine Bewertungen
- Nephrotic Syndrome WikipediaDokument10 SeitenNephrotic Syndrome WikipediaJohn KevlarNoch keine Bewertungen
- Structural Biology of HIVDokument31 SeitenStructural Biology of HIVLaura TapiaNoch keine Bewertungen
- Spinal Cord LesionsDokument1 SeiteSpinal Cord Lesionsnpatelmd14Noch keine Bewertungen
- Pathoma 2087m (34h47) : 1) Growth Adaptations, Cell Injury 154 MinsDokument11 SeitenPathoma 2087m (34h47) : 1) Growth Adaptations, Cell Injury 154 Minsgreen mateNoch keine Bewertungen
- Chapter 3 Genetic VariationDokument21 SeitenChapter 3 Genetic VariationAbdulkarimNoch keine Bewertungen
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Dokument18 SeitenPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiNoch keine Bewertungen
- Mediastinum and Its ContentsDokument11 SeitenMediastinum and Its ContentsPap YeeNoch keine Bewertungen
- Accordion Sign-Appearance (C. Difficile)Dokument41 SeitenAccordion Sign-Appearance (C. Difficile)Andra HijratulNoch keine Bewertungen
- The Basal Ganglia Mashehabat@just - Edu.joDokument62 SeitenThe Basal Ganglia Mashehabat@just - Edu.joSaddamix AL OmariNoch keine Bewertungen
- DISC, Drugs, Infection, Thick Basal MembraneDokument5 SeitenDISC, Drugs, Infection, Thick Basal MembraneHOPENoch keine Bewertungen
- Kidney Physiology (Q & A)Dokument28 SeitenKidney Physiology (Q & A)ramadan100% (1)
- Heart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesDokument3 SeitenHeart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesPrarthana Thiagarajan100% (3)
- Nose & Paranasal Sinuses 2018Dokument63 SeitenNose & Paranasal Sinuses 2018yasrul izadNoch keine Bewertungen
- Dermatology Resident Roundup Histologic BodiesDokument2 SeitenDermatology Resident Roundup Histologic BodiesAreg JosephsNoch keine Bewertungen
- Schematic Diagram Wilson'S DiseaseDokument2 SeitenSchematic Diagram Wilson'S DiseaseAmira CharmaineNoch keine Bewertungen
- Gastrointestinal Tract PathologyDokument12 SeitenGastrointestinal Tract PathologyTurinawe Bin ByensiNoch keine Bewertungen
- Patho CA - Acute PancreatitisDokument1 SeitePatho CA - Acute PancreatitisKNoch keine Bewertungen
- 1 Ge Stimulations Mast Cell Degeneration Asthma AttackDokument4 Seiten1 Ge Stimulations Mast Cell Degeneration Asthma Attacknebbie06Noch keine Bewertungen
- Kidney Functions and Renal FailureDokument6 SeitenKidney Functions and Renal FailureEn ConejosNoch keine Bewertungen
- Salmonela Thyposa: Disease Etiology Unique S&S Brief Patophysiology Diagnostic Treatment / Plan OthersDokument8 SeitenSalmonela Thyposa: Disease Etiology Unique S&S Brief Patophysiology Diagnostic Treatment / Plan OthersNatalia_WiryantoNoch keine Bewertungen
- Gastro ExamDokument2 SeitenGastro ExamJessica Brittain-GeorgeNoch keine Bewertungen
- Abdo Exam TableDokument2 SeitenAbdo Exam Tableapi-195986134Noch keine Bewertungen
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDokument3 SeitenVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNoch keine Bewertungen
- Nephrotic Nephritic SyndromsDokument4 SeitenNephrotic Nephritic SyndromsKimiwari100% (2)
- Lichen Planus, Nitidus, Striatus, Sclerosus (Dr. Cruz)Dokument9 SeitenLichen Planus, Nitidus, Striatus, Sclerosus (Dr. Cruz)Riena Austine Leonor NarcillaNoch keine Bewertungen
- Diseases Link To Chromosomal Abnormalities: Chromoso Me Abnormality DiseaseDokument7 SeitenDiseases Link To Chromosomal Abnormalities: Chromoso Me Abnormality Diseasenreena aslamNoch keine Bewertungen
- Skin Structure and Function GuideDokument10 SeitenSkin Structure and Function GuideyassrmarwaNoch keine Bewertungen
- Important Terms - Tropical InfectionDokument8 SeitenImportant Terms - Tropical InfectionTimothy JordanNoch keine Bewertungen
- Radiology - Imaging of The ThoraxDokument69 SeitenRadiology - Imaging of The ThoraxOrlando Daniel SitompulNoch keine Bewertungen
- Lung AbscessDokument26 SeitenLung AbscessPrajwal Rao KNoch keine Bewertungen
- Yingyu 1Dokument31 SeitenYingyu 1api-19916399Noch keine Bewertungen
- EmpiemaDokument19 SeitenEmpiemaArrol Iswahyudi100% (1)
- Pleural EffusionDokument3 SeitenPleural EffusionRafahiah HaronNoch keine Bewertungen
- @acute Nephrotic SyndromeDokument1 Seite@acute Nephrotic SyndromeameerabestNoch keine Bewertungen
- @ovary Cyst ComparisonDokument2 Seiten@ovary Cyst ComparisonameerabestNoch keine Bewertungen
- Cme Bronchial AsthmaDokument28 SeitenCme Bronchial AsthmaameerabestNoch keine Bewertungen
- Burn Injuries GuideDokument53 SeitenBurn Injuries GuideHusna NadiaNoch keine Bewertungen
- @non Neoplastic Non Inflammatory Lesions of The BreastDokument2 Seiten@non Neoplastic Non Inflammatory Lesions of The BreastameerabestNoch keine Bewertungen
- @histology of Male Genital SystemDokument6 Seiten@histology of Male Genital SystemameerabestNoch keine Bewertungen
- E.coli, Klebsiella, Proteus EtcDokument3 SeitenE.coli, Klebsiella, Proteus EtcameerabestNoch keine Bewertungen
- @acute Nephritic SyndromeDokument3 Seiten@acute Nephritic Syndromeameerabest100% (1)
- @ductal CarcinomaDokument1 Seite@ductal CarcinomaameerabestNoch keine Bewertungen
- @drugs Acting On Uterus and Erectile DysfunctionDokument2 Seiten@drugs Acting On Uterus and Erectile DysfunctionameerabestNoch keine Bewertungen
- @ovary Cyst ComparisonDokument2 Seiten@ovary Cyst ComparisonameerabestNoch keine Bewertungen
- Genitourinarybacteria Comparisons PDFDokument7 SeitenGenitourinarybacteria Comparisons PDFameerabest100% (1)
- @contraceptives DrugsDokument1 Seite@contraceptives DrugsameerabestNoch keine Bewertungen
- @hypothalamic HormonesDokument1 Seite@hypothalamic HormonesameerabestNoch keine Bewertungen
- @tumors of The Breast 1Dokument2 Seiten@tumors of The Breast 1ameerabestNoch keine Bewertungen
- @sex SteroidsDokument2 Seiten@sex SteroidsameerabestNoch keine Bewertungen
- Anatomy of Male GenitaliaDokument4 SeitenAnatomy of Male GenitaliaameerabestNoch keine Bewertungen
- @male PathoDokument8 Seiten@male Pathoameerabest100% (2)
- Nota Patho PDFDokument8 SeitenNota Patho PDFameerabestNoch keine Bewertungen
- Patho Male BreastDokument1 SeitePatho Male BreastameerabestNoch keine Bewertungen
- @ovarian Tumors ComparisonDokument6 Seiten@ovarian Tumors ComparisonameerabestNoch keine Bewertungen
- Semen AnalysisDokument3 SeitenSemen Analysisameerabest80% (5)
- Histology Female PDFDokument5 SeitenHistology Female PDFameerabestNoch keine Bewertungen
- Genitourinarybacteria Comparisons PDFDokument7 SeitenGenitourinarybacteria Comparisons PDFameerabest100% (1)
- Genital EmbryologyDokument6 SeitenGenital EmbryologyameerabestNoch keine Bewertungen
- Cardiac ExamDokument7 SeitenCardiac ExamameerabestNoch keine Bewertungen
- OSCE DermaDokument8 SeitenOSCE DermaameerabestNoch keine Bewertungen
- #Chest TraumasDokument4 Seiten#Chest Traumasameerabest100% (3)
- Virology of Hepatitis ADokument33 SeitenVirology of Hepatitis AameerabestNoch keine Bewertungen
- CXR InterpretationDokument3 SeitenCXR InterpretationNairobipaeds Madakitari WatotoNoch keine Bewertungen
- Jurnal Respirasi: Tutik Kusmiati, Winariani Koesoemoprodjo, Novita MaulidiyahDokument7 SeitenJurnal Respirasi: Tutik Kusmiati, Winariani Koesoemoprodjo, Novita MaulidiyahNiaNoch keine Bewertungen
- Drug Related Pleural Disease: Charis Moschos MD., Ioannis Kalomenidis MD E-Mail: Ikalom@Dokument11 SeitenDrug Related Pleural Disease: Charis Moschos MD., Ioannis Kalomenidis MD E-Mail: Ikalom@roland helmizarNoch keine Bewertungen
- Emphysema - Pleurisy - Pleural EffusionDokument17 SeitenEmphysema - Pleurisy - Pleural EffusionGEN ERIGBUAGASNoch keine Bewertungen
- Nursing Care Plan For HEMOTHORAX PNEUMOTHORAXDokument8 SeitenNursing Care Plan For HEMOTHORAX PNEUMOTHORAXHistory TechNoch keine Bewertungen
- Noncardiogenic Pulmonary EdemaDokument12 SeitenNoncardiogenic Pulmonary EdemaIrina DuceacNoch keine Bewertungen
- Chest TubeDokument21 SeitenChest TubeClaudio Nicolas Retamal YevenesNoch keine Bewertungen
- Pneumonia and TuberculosisDokument18 SeitenPneumonia and TuberculosisVincent QuitorianoNoch keine Bewertungen
- Pulmonary Tuberculosis 2017Dokument13 SeitenPulmonary Tuberculosis 2017GioNoch keine Bewertungen
- Chest Tube SizeDokument10 SeitenChest Tube SizeilpollolocoNoch keine Bewertungen
- LUNG ARTIFACTSreviewDokument13 SeitenLUNG ARTIFACTSreviewMayra ValderramaNoch keine Bewertungen
- Case Presentation Respiratory SystemDokument23 SeitenCase Presentation Respiratory SystemShubhamNoch keine Bewertungen
- Clinico Radiological ConferenceDokument67 SeitenClinico Radiological ConferenceSharmaine Margaret LeeNoch keine Bewertungen
- How the lungs work and functionDokument15 SeitenHow the lungs work and functionthenameisvijayNoch keine Bewertungen
- Acute Dyspnoea and Haemoptysis My Notes Add Jimmy's PDF Notes On & OrganiseDokument171 SeitenAcute Dyspnoea and Haemoptysis My Notes Add Jimmy's PDF Notes On & OrganisewwwrgrobinNoch keine Bewertungen
- Ecografia Pulmonar. Ficción o Realidad PDFDokument9 SeitenEcografia Pulmonar. Ficción o Realidad PDFAmilcar RomeroNoch keine Bewertungen
- Med Bio 349911 PDFDokument71 SeitenMed Bio 349911 PDFWen Jie LauNoch keine Bewertungen
- DK IPD 3 - Ogie AsitesDokument174 SeitenDK IPD 3 - Ogie AsiteshariogieNoch keine Bewertungen
- Pleural Effusion Case PresentationDokument78 SeitenPleural Effusion Case PresentationAnie Zacarias100% (3)
- NCP Pleural EffusionDokument7 SeitenNCP Pleural EffusionEjie Boy Isaga100% (2)
- MBChB Year 4 & 5 Past Papers + AnswersDokument170 SeitenMBChB Year 4 & 5 Past Papers + AnswersHariharan NarendranNoch keine Bewertungen
- Aubf Lec - Serous FluidDokument12 SeitenAubf Lec - Serous FluidColene MoresNoch keine Bewertungen
- Lung and Airway Ultrasound in Pediatric AnesthesiaDokument7 SeitenLung and Airway Ultrasound in Pediatric Anesthesiaema moralesNoch keine Bewertungen
- Unit 06 Assessment of Thorax and LungDokument55 SeitenUnit 06 Assessment of Thorax and Lunghuma100% (1)
- Efusi Pleura: Riana Sari Balai Besar Kesehatan Paru Masyarakat (BBKPM) SurakartaDokument34 SeitenEfusi Pleura: Riana Sari Balai Besar Kesehatan Paru Masyarakat (BBKPM) SurakartaSantiFaridKalukuNoch keine Bewertungen
- Approach To Pleural EffusionDokument46 SeitenApproach To Pleural EffusionBaskoro Tri LaksonoNoch keine Bewertungen
- 9 Topnotch Internal Medicine Superexampdf PDFDokument95 Seiten9 Topnotch Internal Medicine Superexampdf PDFSheryl Layne Lao-Sebrio100% (1)
- Case Study For Pleural-EffusionDokument10 SeitenCase Study For Pleural-EffusionGabbii CincoNoch keine Bewertungen
- Yield of Thoracoscopic Biopsy Truenat in The Diagnosis of Tubercular Pleural EffusionDokument7 SeitenYield of Thoracoscopic Biopsy Truenat in The Diagnosis of Tubercular Pleural EffusionThomas KurianNoch keine Bewertungen
- Surgery Songbook CompressedDokument69 SeitenSurgery Songbook CompressedBrandon HayashiNoch keine Bewertungen