Beruflich Dokumente
Kultur Dokumente
Major Report
Hochgeladen von
Princess PalakCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Major Report
Hochgeladen von
Princess PalakCopyright:
Verfügbare Formate
Anesthesia Machine
CHAPTER 1 INTRODUCTION
1.1 Biomedical Instrumentation Biomedical instrumentation is an extremely broad categoryessentially covering all health care products that do not achieve their intended results through predominantly chemical (e.g., pharmaceuticals) or biological (e.g., vaccines) means, and do not involve metabolism. A medical device is intended for use in: the diagnosis of disease or other conditions, or in the cure, mitigation, treatment, or prevention of disease, Some examples include pacemakers, infusion pumps, the heart-lung machine, dialysis machines, anesthesia machines, artificial organs, implants, artificial limbs, corrective lenses, cochlear implants, ocular prosthetics, facial prosthetics, somato prosthetics, and dental implants. Stereolithography is a practical example of medical modeling being used to create physical objects. Beyond modeling organs and the human body, emerging engineering techniques are also currently used in the research and development of new devices for
innovative therapies, treatments, patient monitoring, and early diagnosis of complex diseases. Medical devices are regulated and classified (in the US) as follows: Class I devices present minimal potential for harm to the user and are often simpler in design than Class II or Class III devices. Devices in this category include tongue depressors, bedpans, elastic bandages, examination gloves, and hand-held surgical instruments and other similar types of common equipment. Class II devices are subject to special controls in addition to the general controls of Class I devices. Special controls may include special labeling requirements, mandatory performance standards, and postmarket surveillance. Devices in this class are typically non-invasive and include x-ray machines, PACS, powered wheelchairs, infusion pumps, and surgical drapes. Class III devices generally require premarket approval (PMA) or premarket notification (510k), a scientific review to ensure the device's safety and effectiveness, in addition to the general controls of Class I. Examples include replacement heart valves, hip and knee joint implants, silicone gel-filled breast implants, implanted cerebellar stimulators, implantable pacemaker pulse generators and endosseous (intra-bone) implants.[1]
Mahant Bachittar Singh College of Engineering and Technology 1
Anesthesia Machine
[1]. http://en.wikipedia.org/wiki/Biomedical_engineering#Medical_devices 1.1.1 Anesthesia
Anesthesia or anaesthesia (from Greek -, an-, "without"; and , aisthsis, "sensation"),traditionally meaning the condition of having sensation (including the feeling of pain) blocked or temporarily taken away, is a pharmacologically induced and reversible state of amnesia, analgesia, loss of responsiveness, loss of skeletal muscle reflexes, decreased stress response, or all of these simultaneously. These effects can be obtained from a single drug which alone provides the correct combination of effects, or occasionally a combination of drugs (such as hypnotics, sedatives, paralytics and analgesics) to achieve very specific combinations of results. This allows patients to undergo surgery and other procedures without the distress and pain they would otherwise experience. An alternative definition is a "reversible lack of awareness", including a total lack of awareness (e.g. a general anesthetic) or a lack of awareness of a part of the body such as a spinal anesthetic. The pre-existing word anesthesia was suggested by Oliver Wendell Holmes, Sr. in 1846 as a word to use to describe this state.[2]
[2]. http://en.wikipedia.org/wiki/Anesthesia The purpose of anesthesiology was reduction of surgery-induced pain. However, the present goal of anesthesiology is control of excessive biological responses induced by a variety of stresses and protection of patients from stress-induced complications. Clinical activity is divided into anesthesia in the operation theater, pain control for a variety of diseases and critical care medicine. The aim is to protect a living body from stresses including surgical stresses, pain, injuries and inflammation for the benefit of patients. Anesthesia has many purposes including:
Pain relief (analgesia). Blocking memory of the procedure (amnesia). Producing unconsciousness. Inhibiting normal body reflexes to make surgery safe and easier to perform. Relaxing the muscles of the body.[3]
[3]. http://medical-dictionary.thefreedictionary.com/general+anesthesia 1.2 Branch of Science Anesthesiology is a medical specialty dealing with anesthesia and related matters, including resuscitation and pain. Originally concerned only with general anesthesia in the operating room, anesthesiology now includes epidural anesthesia (injection of local anesthetics into the spinal fluid, cutting off feeling below the point of injection); artificial respiratory support during
Mahant Bachittar Singh College of Engineering and Technology 2
Anesthesia Machine
operations requiring paralyzing drugs that render patients unable to breathe; clinical management of all unconscious patients; management of pain relief and cardiac and respiratory resuscitation problems; respiratory therapy; and treatment of fluid, electrolyte, and metabolic disturbances. Progress in anesthesiology has made possible more complex operations and surgery for more critically ill patients. The anesthesiologist's role has become increasingly important and complex.[4] [4].http://www.merriam-webster.com/dictionary/anesthesiology 1.3 Types of Anesthesia Types of anesthesia include local anesthesia, regional anesthesia, general anesthesia, and dissociative anesthesia. Local anesthesia is any technique to induce the absence of sensation in part of the body, generally for the aim of inducing local analgesia, that is, local insensitivity to pain, although other local senses may be affected as well. It allows patients to undergo surgical and dental procedures with reduced pain and distress. It inhibits sensory perception within a specific location on the body, such as a tooth or the urinary bladder. It numbs only a small, specific area of the body. With local anesthesia, a person is awake or sedated, depending on what is needed. Local anesthesia lasts for a short period of time and is often used for minor outpatient procedures (when patients come in for surgery and can go home that same day). For someone having outpatient surgery in a clinic or doctor's office (such as the dentist or dermatologist), this is probably the type of anesthetic used. The medicine used can numb the area during the procedure and for a short time afterwards to help control post-surgery discomfort. In many situations, such as cesarean section, it is safer and therefore superior to general anesthesia. It is also used for relief of non-surgical pain and to enable diagnosis of the cause of some chronic pain conditions. Anesthetists sometimes combine both general and local anesthesia techniques. [5] [6] [5]. http://en.wikipedia.org/wiki/Local_anesthesia [6]. http://kidshealth.org/teen/your_body/medical_care/anesthesia_types.html Regional anaesthesia is anaesthesia affecting a large part of the body, such as a limb or the lower half of the body by blocking transmission of nerve impulses between a part of the body and the spinal cord. Regional anaesthesia is generally used to make a person more comfortable during and after the surgical procedure. Regional anaesthetic techniques can be divided into
Mahant Bachittar Singh College of Engineering and Technology 3
Anesthesia Machine
central and peripheral techniques. The central techniques include so called neuraxial blockade (epidural anaesthesia, spinal anaesthesia). The peripheral techniques can be further divided into plexus blocks such as brachial plexus blocks, and single nerve blocks. Regional anaesthesia may be performed as a single shot or with a continuous catheter through which medication is given over a prolonged period, e.g. continuous peripheral nerve block (CPNB). Regional anaesthesia can be provided by injecting local anaesthetics directly into the veins of an arm (provided the venous flow is impeded by a tourniquet.) This is called intravenous regional techniques (Bier block). This differs from Local anaesthesia, which, in a strict sense, is anaesthesia of a small part of the body such as a tooth or an area of skin, and Conduction anaesthesia is a comprehensive term which encompasses a great variety of local and regional anaesthetic techniques.[7] [7]. http://en.wikipedia.org/wiki/Regional_anaesthesia General anaesthesia is a medically induced coma and loss of protective reflexes resulting from the administration of one or more general anaesthetic agents. It refers to inhibition of sensory, motor and sympathetic nerve transmission at the level of the brain, resulting in unconsciousness and lack of sensation. It can be given through an intra-venous (which requires sticking a needle into a vein, usually in the arm) or by inhaling gases or vapors by breathing into a mask or tube. A variety of medications may be administered, with the overall aim of
ensuring sleep, amnesia, analgesia, relaxation of skeletal muscles, and loss of control of reflexes of the autonomic nervous system. The optimal combination of these agents for any given patient and procedure is typically selected by an anaesthesiologist or another provider such as an anaesthesiologist assistant or nurse anaesthetist, in consultation with the patient and the medical or dental practitioner performing the operative procedure.[6] [8] [8]. http://en.wikipedia.org/wiki/General_anaesthesia Dissociative anesthesia uses agents that inhibit transmission of nerve impulses between higher centers of the brain (such as the cerebral cortex) and the lower centers, such as those found within the limbic system. It reduces anxiety and produces a trancelike state. The person is not asleep, but rather feels separated from his or her body.[6] 1.4 History After anaesthesia was invented and introduced with the public demonstration of ether anaesthesia by WTG Morton in 1846, for many years an anaesthesia machine was not required for providing
Mahant Bachittar Singh College of Engineering and Technology 4
Anesthesia Machine
anaesthesia to the patients until oxygen (O2) and nitrous oxide (N2O) were introduced as compressed gases in cylinders by the late 19th century.[7] A metal skeleton was required for mounting these cylinders. Boyles machine was invented by Henry Edmund Gaskin Boyle in 1917. His machine was a modification of the American Gwathmey apparatus of 1912 and became the best known early continuous flow anaesthetic machine. The Boyles apparatus was first made by Coxeter and Sons, under the direction of Lord George Wellesly, which was later acquired by the British Oxygen Company (BOC). Boyle was the trade name of BOC. It was named so to respect the inventor, Boyle. However, Boyle was not the pioneer in manufacturing anaesthesia machines. Two other great men had done excellent work before him. One was James Taylor Gwathmey who was practicing in New York who invented the Gwathmey machine in 1912. Later, Geoffrey Marshal developed a machine during the First World War (1914 1918) based on the Gwathmey machine. Boyle, who developed his machine from Gwathmeys basic model in 1917, presented his invention at the Royal Society of Medicine in London in 1918. Even though Marshal had developed his machine much before Boyle, he presented his machine before the medical community in 1919, much later than Boyle. All the credit had gone to Boyle, although Gwathmey and Marshal had developed their machines before him.[10,11] 1921 Waters to and fro absorption apparatus was introduced.[9] 1927 Flow meter for carbon dioxide was included, the volatile controls were of the lever type and the familiar back bar made its first appearance.[9] 1930 The plunger of the vaporiser appeared in the 1930 model.[9] 1930 Circle absorption system was introduced by Brian Sword.[9] 1933 Dry bobbin flow meters were introduced.[12] 1952 Pin index safety system (PISS) by Woodbridge.[12] 1958 Introduction of Bodok seal.[12] [9]. Thompson PW, Wilkinson DJ. Development of anaesthetic machines. Br J Anaesth 1985;57:640 8. [10]. Abraham A. Trade names that have become generic names in anaesthesia. Indian J Anaesth 2012;56:411 3. [11]. Ball C, Westhorpe R, Kaye G. Museum of anaesthetic history. Anaesth Intensive Care 1999;27:129. [12]. Watt M. The evolution of the Boyle apparatus 1917 67. Anaesthesia 1968;23:103 18.
Mahant Bachittar Singh College of Engineering and Technology 5
Anesthesia Machine
1.5 Anesthesia Machines The most important piece of equipment that the anaesthesiologist uses is the anesthesia machine. Safe use of anesthesia machine depends upon an interaction between the basic design of the machine with its safety features and the knowledge and skills of the anaesthesiologist. The basic function of an anaesthesia machine is to prepare a gas mixture of precisely known, but variable composition. The gas mixture can then be delivered to a breathing system. Anaesthesia machine itself has evolved from a simple pneumatic device to a complex array of mechanical, electrical and computer controlled components. Much of the driving force for these changes have been to improve patient safety and user convenience.[13] Though many modifications have been brought out still the basic design has not much changed. Hence, knowledge of the basic design of the anaesthesia machine is must for all the practicing anaesthesiologists to understand the modern anaesthesia workstation. [13]. Brockwell RC, Andrews GG. Understanding Your Anaesthesia Machine. ASA Refresher Courses. Vol. 4. Philadelphia, Pennsylvania: Lippincott Williams and Wilkins; 2002. p. 41 59.
Original anesthesia machine was made by the firm COXTERS. There are several differences between newer and older anesthesia machines. Advanced ventilators are the biggest difference between newer and older gas machines. The differences between older gas machines -such as the Ohmeda modulus, Excel, or Aestiva and the DrgerNarkomed GS, Mobile, MRI, 2B, 2C, 3 or 4are less than their similarities. While the differences between new models from GE Healthcare (ADU, Aisys, Aespire, Avance) and Drger (Fabius GS, Narkomed 6000/6400, Apollo) are more than their similarities.[14] [14]. http://www.slideshare.net/imran80/anaesthesia-machine Some specifications of various older and newer anesthesia machines are discussed here. 1.5.1 Ohmeda Modulus IITM Anesthesia Machine The Ohmeda Modulus II Anesthesia Machine provides oxygen and volume monitoring and has optional pulse oximetry and endtidal CO2 modules. This high-end anesthesia machine is great for university and research facilities. DRE Veterinary also has available the Ohmeda Modulus II Plus.[15]. Fig1.1 shows the Ohmeda Modulus II Anesthesia Machine.[16]
Mahant Bachittar Singh College of Engineering and Technology
Anesthesia Machine
Fig1.1 Ohmeda Modulus II Anesthesia Machine
[16]. http://www.wemed1.com/catalog/an-mod.htm Features: Double Flowmeter Tubes (O2 & N2O) Flowmeter Protection Shield Link-25 Hypoxic Guard Touch-Coded Oxygen Knob Oxygen Supply Pressure Sensor / Alarm Oxygen Supply Pressure Failure Device A.C. Line Power Sensor / Alarm D.C. Power Sensor / Indicator Selectatec 3 Vaporizer SM Manifold Minimum Oxygen Flow Anti-Disconnect Fresh Gas Outlet 3 Drawer Lockable Cabinet Integral Footrest Integrated D.I.S.S. Pipeline Inlets Modular Oxygen & Nitrous Oxide Yokes High Pressure Regulator and Gauges
Mahant Bachittar Singh College of Engineering and Technology 7
Anesthesia Machine
Pneumatic / Electric Interface Main Switch O2 and N2O (Standard) Air (Optional) Hypoxic Guard (Standard) Oxygen and Volume Monitoring (Standard) Optional integrated Pulse Oximetry, Endtidal CO2 GMS CO2 Absorber (Standard) E-Cylinder and Central Gas Connections (Standard) Guarded Oxygen Flush Middle Shelf Tilt Adjustable Top Shelf Monitor Swivel Pod 5400 Volume Monitor 5100 Oxygen Monitor Electrical Outlet Panel Oxygen Power Outlet High-Pressure Hose Hanger Centralized Patient Interface Panel Shelf-Mounted Utility Hooks Anesthetic Bottle Holder Telescoping Absorber Arm Lockable Front Casters Monitor Securing Straps Battery Back-Up of the Ventilator Specifications: Dimensions: 61"H x 34.5"W x 25.2"D | 155 H x 88 W x 64 D (cm) Weight: Without Monitors or Shelves - 360 lbs| 163 kg With Monitors on Shelves - 477 lbs | 217 kg Absorber Swivel Arm Length: 14" | 35.5 cm
Mahant Bachittar Singh College of Engineering and Technology 8
Anesthesia Machine
Push Button Vertical Adjustment (from floor): 10" to 26" | 25.4 to 66 cm Range of Horizontal Adjustment: 5.5" Minimum 11" Maximum[13] [15]. http://www.dreveterinary.com/veterinary-equipment/veterinary-anesthesia/anesthesia-
machines/ohmeda-modulus-ii-anesthesia-machine 1.5.2 Drager Narkomed GS Anesthesia Machine One of the more popular machines on the market, the durable Narkomed GS machine features the familiar-style flow head, visible bellows, and reliable performance. It is intuitive, and easyto-use. Its built-in monitor displays volume, pressure and oxygen monitoring, and is available in 2 or 3 vaporizer configurations. With its simplistic approach, versatility, and reliability, the Narkomed GS provides next-level technology in a user-friendly machine, and offers a large 3drawer cabinet, writing tray and auxiliary flow meter. The machine comes standard with the dependable AV2+ ventilator, which is pressure-limited, time-cycled and volume-preset. Features include pneumatic circuitry, electronic timing, breathing rate controls, inspiratory to expiratory ratio, tidal volume, inspiratory flow and inspiratory pressure limit for flexible ventilation. Additional features include inverse I:E ratios with its built-in safety mechanism which allows for an assortment of conditions.[17]. Fig1.2 shows the Drager Narkomed GS Anesthesia Machine.[18]
Mahant Bachittar Singh College of Engineering and Technology
Anesthesia Machine Fig1.2 Drager Narkomed GS Anesthesia Machine
[17].http://www.metropolitanmed.com/products/drager-narkomed-gs-anesthesia-machine.php [18]. System/ Features: Includes AV2+ Ventilator, featuring pressure-limited, volume-preset, and time-cycled controls Ventilator also measures breathing rate, inspiratory to expiratory (i:e) ratios, inverse i:e ratios, inspiratory flow and pressure limit, and tidal volume Designed for durability and flexibility Absorber O2, volume, pressure monitor 3-gas delivery system Active scavenge reservoir Latex-free goods Electronic spirometry 3-tier alarm system Next-level technology Open architecture Scavenging system Sphygmomanometer[17] 1.5.3 Aestiva 7900 Anesthesia Machine The Aestiva 7900 is a balance of advanced ventilation and exceptional capabilities, delivering a cost-effective approach to anesthesia therapy. The Aestiva with the 7900 SmartVent provides sophisticated ventilation capabilities that support the needs of a broad patient range. Aestiva's open architecture allows you to use your current monitors and data management systems, or purchase a fully integrated anesthesia system with GE CARESCAPE Monitors and Centricity Perioperative Anesthesia information management systems.[19]. Fig1.3 shows the Aestiva 7900 Anesthesia Machine.[20] http://www.buckeyemedical.com/North-American-Drager-Narkomed-GS-Anesthesia-
Mahant Bachittar Singh College of Engineering and Technology
10
Anesthesia Machine
Fig 1.3 Aestiva 7900 Anesthesia Machine
[20]. http://www.medwow.com/i_preview.php?sale_number=454468925 Integrated Breathing System The Aestiva breathing circuit is integrated, which helps protect the components from damage and disconnection. Smart sensors and switches link communication between the breathing circuit and the SmartVent ventilator. Confidence. Control. Comfort. Get close to your patient with monitors that are easily viewed and controls that are conveniently located, whether you are sitting or standing. Open Architecture Aestivas open architecture means it can fit easily with your existing equipment, monitors and accessories included. Enhanced Workflow Aestiva offers a cost-effective approach to anesthesia therapy and workflow through: o Low planned maintenance requirements and durable components to improve uptime. o An effective system for the practice of low-flow anesthesia, helping to minimize agent consumption to help save on anesthetic agent costs.
Mahant Bachittar Singh College of Engineering and Technology 11
Anesthesia Machine
Aestiva includes a selection of product options: Standard: SmartVent ventilator patient breathing system with circle module O2 and N2O gas delivery Lockable drawer Light strip Supports up to three in-line vaporizers Optional: Additional gases: air and heliox or CO2 Air-flow tube: single or dual Cylinder Yokes: up to five Auxiliary common gas outlet Integrated auxiliary O2 flowmeter[19] [19].http://www3.gehealthcare.com/en/Products/Categories/Anesthesia_Delivery/Aestiva/Aestiv a_7900#tabs/tab8A426481213F4317AFE3A58160CDF71E 1.6 Idea of Project We all have a great interest in biomedical field and wanted to make our project related to this field only. As we all know, deaths are taking place due to excess amount of anesthesia delivered to patient before any surgery. And this happens due to the mistake of anesthesiologists. To overcome this excess amount of anesthesia, we all decided to make an anesthesia machine which will give the proper mixture of gases in accurate amount. In case of excess amount of mixture of gases the machine automatically shuts down and the alarm gets activated. This machine is not a fully developed anesthesia machine, its just a basic machine to monitor the proper amount of anesthesia to be deliver to the patient. By using it number of deaths can be reduced. 1.7 Objective of the Project The objective of our project is to design an automatic anesthesia machine for controlled administration of global anesthesia in pre-opreative measures. The main objective of our project is to deliver accurate quantity of anesthesia to the patient before the operation. If overdose takes place the alarm activates. 1.7.1 Key Features The key features of our anesthesia machine are as follows: 1. Inlet Gas Pressure Sensing and Monitoring
Mahant Bachittar Singh College of Engineering and Technology 12
Anesthesia Machine
The Inlet Gas Pressure Sensing and Monitoring System consists of three pressure sensors attached to three different gas sources i.e. gas cylinders so as to check and maintain the delivery pressure of source gases used namely Oxygen(breathing essential), Oxide(anesthetic agent) and Air(mixture of gases and water vapor for humidification) 2. Outlet Gas Pressure Sensing and Monitoring The Outlet Gas Pressure Sensing and Monitoring System consists of one pressure sensor attached to output gas mixture delivery chamber in order to check and maintain the delivery pressure of final anesthetic gaseous mixture to the patient. 3. Inlet Valve Control System Inlet Valve Control System consists of three valves which control the delivery of source gases according to the desired pressure values. 4. Outlet Valve Control System Outlet Valve Control System consists of one valve which control the delivery of final anesthetic gaseous mixture to the patient according to the desired pressure values. 5. Microcontroller Microcontroller is the control unit of the system and controls all the valve actions of inlet Nitrous
and outlet systems with respect to the real-time inputs from the pressure sensors and preset delivery values. It also helps us to display the real-time pressure changes with help of a LCD. It controls all the system parameters and activates different the alarm systems available. 6. Inlet and Outlet Pressure Value Display The set pressure values and the real-time pressure changes are displayed on an LCD. 7. Cylinder Empty Alarm This is activated when atleast one of the three cylinders are close to empty point. 8. Overdose Alarm This is activated when the anesthesia is delivered over a preset time interval. 9. Emergency Shut Down or Auto-Shut Down This system is activated immediately if no corrected action is performed on the other alarms generated or the systems faults in any other situation e.g. power failure, valve malfunction etc.. 10. Power Supply A DC regulated Power supply is designed for different active and passive components of the system along with different actuators controls e.g. valves.
Mahant Bachittar Singh College of Engineering and Technology 13
Anesthesia Machine
CHAPTER 2 BLOCK DIAGRAM AND CIRCUIT DIAGRAM
2.1 Block Diagram of Anesthesia Machine Block diagram of the Anesthesia Machine is as shown in Fig 2.1.
Pressure Sensor PIC DC motor with H-bridge- Valve 1 DC motor with H-bridge- Valve 2 16F73
Buzzer
LCD Display
Fig 2.1 Block Diagram of Anesthesia Machine
2.1.1 Description of Block Diagram In this project one pressure sensor, two valves, PIC 16F73 microcontroller, LCD Display and a buzzer is used. Small description of each component is as given below: Pressures sensor: In this project we have used pressure sensor MPX5700DP manufactured by Free scale. This sensor interfaced with Inbuilt ADC of PIC16F73. It shows final pressure maintained in outlet chamber on LCD. Valve Control: There are two valves shown to control outlet of two cylinders. To control the valve automatically with pressure monitoring a motorside mechanism is fitted on the both valve knob. When motor move clock wise it open the valve. When motor moves anti-clock wise it closes the valve. To control the direction of dc motor Relay based H-bridge circuit is used with motors. Whenever there is low pressure or over pressure an alarm is generated using buzzer.
Mahant Bachittar Singh College of Engineering and Technology 14
Anesthesia Machine
2.2 Circuit Diagram of Anesthesia Machine Fig 2.2 shows the circuit diagram of the Anesthesia Machine.
Fig 2.2 Circuit Diagram of Anesthesia Machine
Mahant Bachittar Singh College of Engineering and Technology
15
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- List of Anesthesia Library BooksDokument3 SeitenList of Anesthesia Library BooksSivaramakrishnan Dhamotharan100% (2)
- OB1 Lec - AnalgesiaDokument3 SeitenOB1 Lec - Analgesiaapi-3700579Noch keine Bewertungen
- Severe Pain in Chronic Pancreatitis PatientsDokument12 SeitenSevere Pain in Chronic Pancreatitis PatientsHernan Alfredo Argote VegaNoch keine Bewertungen
- Fibromyalgia and Neuropathic Pain - Differences and Similarities. A Comparison of 3057 Patients With Diabetic Painful Neuropathy and FibromyalgiaDokument9 SeitenFibromyalgia and Neuropathic Pain - Differences and Similarities. A Comparison of 3057 Patients With Diabetic Painful Neuropathy and FibromyalgiaErica Jade WilmesNoch keine Bewertungen
- Dance Therapy TortureDokument15 SeitenDance Therapy TortureeclatantNoch keine Bewertungen
- Flexilor RangeDokument31 SeitenFlexilor RangekurutalaNoch keine Bewertungen
- The Cost of PainDokument121 SeitenThe Cost of PainDavid IrelandNoch keine Bewertungen
- Final Paper Group 4 RevisedDokument93 SeitenFinal Paper Group 4 RevisedJeffrey marillaNoch keine Bewertungen
- SOP Akupresur MigrainDokument20 SeitenSOP Akupresur MigrainrachelNoch keine Bewertungen
- Case Note Question Sem 2-2022 (Official Version)Dokument9 SeitenCase Note Question Sem 2-2022 (Official Version)Thảo ThanhNoch keine Bewertungen
- Animal CrueltyDokument2 SeitenAnimal CrueltyJegathisan ViravelNoch keine Bewertungen
- Imperium SensusDokument10 SeitenImperium SensusmikeNoch keine Bewertungen
- Segmental Neuromyotherapy - Basic Concepts and Practical ApplicationsDokument4 SeitenSegmental Neuromyotherapy - Basic Concepts and Practical Applicationsweb3351Noch keine Bewertungen
- Vibroacoustic Apparatus Vitafon-T : Exploitation Manual AND User GuideDokument44 SeitenVibroacoustic Apparatus Vitafon-T : Exploitation Manual AND User GuideMax Smith0% (1)
- Pain Patom (Henny A. Sadeli, DR.,SPS)Dokument25 SeitenPain Patom (Henny A. Sadeli, DR.,SPS)Umar IslamiNoch keine Bewertungen
- Final Alternative MedicineDokument41 SeitenFinal Alternative MedicineKryzza LeizellNoch keine Bewertungen
- Centrally Mediated Abdominal Pain SyndromesDokument4 SeitenCentrally Mediated Abdominal Pain SyndromesPolo Good BoyNoch keine Bewertungen
- DR Sapna Ali Khan (PT) DPT, MSPTDokument32 SeitenDR Sapna Ali Khan (PT) DPT, MSPTCHANGEZ KHAN SARDARNoch keine Bewertungen
- Value Proposition CanvasDokument15 SeitenValue Proposition CanvasXyr Xys100% (2)
- Simple Technique For Lip and Nasolabial Fold Anesthesia For Injectable FillersDokument3 SeitenSimple Technique For Lip and Nasolabial Fold Anesthesia For Injectable FillersGina CastilloNoch keine Bewertungen
- Script Mindful BreathingDokument2 SeitenScript Mindful BreathingCeline CabadingNoch keine Bewertungen
- KSPAN Recognition and Treatment of Local Anesthetic Systemic ToxicityDokument39 SeitenKSPAN Recognition and Treatment of Local Anesthetic Systemic ToxicityAli AftabNoch keine Bewertungen
- Styles of Acupuncture in Current Practice - Martin WangDokument104 SeitenStyles of Acupuncture in Current Practice - Martin WangТом Вейцман100% (1)
- AAO FDM Indroduction 1994 PDFDokument12 SeitenAAO FDM Indroduction 1994 PDFHONGJYNoch keine Bewertungen
- Prioritization of Nursing Problems Rank Problem JustificationDokument2 SeitenPrioritization of Nursing Problems Rank Problem JustificationFia GregorioNoch keine Bewertungen
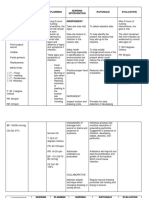
- NCP AppendectomyDokument6 SeitenNCP Appendectomymahmoud fuqahaNoch keine Bewertungen
- '05 Sullivan A.Dokument48 Seiten'05 Sullivan A.Geo NavarroNoch keine Bewertungen
- Heal Yourself NaturallyDokument204 SeitenHeal Yourself NaturallyKanjaFit100% (8)
- Renée Haynes - The Boggle ThresholdDokument6 SeitenRenée Haynes - The Boggle ThresholdKenneth AndersonNoch keine Bewertungen
- NCP - JaundiceDokument5 SeitenNCP - JaundiceQueen Shine0% (1)