Beruflich Dokumente
Kultur Dokumente
Inverted Ductal Papilloma of The Oral Cavity
Hochgeladen von
Andi Sitti Hajrah YusufOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Inverted Ductal Papilloma of The Oral Cavity
Hochgeladen von
Andi Sitti Hajrah YusufCopyright:
Verfügbare Formate
J Clin Exp Dent. 2013;5(2):e112-6.
Traumatic inverted ductal papilloma of the oral cavity.
Journal section: Oral Medicine and Pathology Publication Types: Case Report
doi:10.4317/jced.51055 http://dx.doi.org/10.4317/jced.50950
Inverted ductal papilloma of the oral cavity secondary to lower lip trauma. A case report and literature review
Sergi Sala-Prez 1, Antoni Espaa-Tost 2, August Vidal-Bel 3, Cosme Gay-Escoda 4
DDS. Resident of the master of oral surgery and implantology. Barcelona University Dental School. MD, DDS, PhD. Associate professor of oral and maxillofacial surgery. Professor of the master of oral surgery and implantology. Barcelona University Dental School. Investigator of the IDIBELL Institute. 3 MD. Pathologist of Bellvitge University Hospital. Associate professor of the department of pathology and experimental therapeutics of the university of Barcelona. Investigator of the IDIBELL Institute. 4 MD, DDS, PhD. Chairman of oral and maxillofacial surgery. Director of the master of oral surgery and implantology. University of Barcelona Dental School. Coordinating investigator of the IDIBELL Institute. Head of the service of maxillofacial surgery, Teknon Medical Center. Barcelona, Spain.
1 2
Correspondence: Centro Mdico Teknon Instituto de Investigacin IDIBELL C/ Vilana 12 08022, Barcelona, Spain. E-mail: cgay@ub.edu Sala-Prez S, Espaa-Tost A, Vidal-Bel A, Gay-Escoda C. Inverted ductal papilloma of the oral cavity secondary to lower lip trauma. A case report and literature review. J Clin Exp Dent. 2013;5(2):e112-6. http://www.medicinaoral.com/odo/volumenes/v5i2/jcedv5i2p112.pdf
Article Number: 51055 http://www.medicinaoral.com/odo/indice.htm Medicina Oral S. L. C.I.F. B 96689336 - eISSN: 1989-5488 eMail: jced@jced.es Indexed in: Scopus DOI System
Received: 07/12/2012 Accepted: 10/01/2013
Abstract
Inverted ductal papilloma of the oral cavity is an infrequent benign neoplasm of papillary appearance that originates in the secretory duct of a salivary gland. The etiology is unknown, though some authors have related it to human papillomavirus (HPV) infection. We present the case of a 40-year-old woman with a tumor of the lower lip mucosa. Histopathological study of the lesion diagnosed inverted ductal papilloma of the oral cavity. Human papillomavirus DNA detection and typing based on tumor lesion DNA amplification and posterior hybridization, revealed no presence of viral DNA. The antecedents of trauma reported by the patient could have played an important role in the development of this tumor. Key words: Inverted ductal papilloma, intraductal papilloma, oral papilloma, papillary epidermoid adenoma.
e112
J Clin Exp Dent. 2013;5(2):e112-6.
Traumatic inverted ductal papilloma of the oral cavity.
Introduction
Oral papilloma is a benign tumor located in the oral mucosa. It normally shows exophytic growth with a polypoid or verrucous appearance. However, there have been reports of cases characterized by endophytic or inverted growth (1), most often located in the nasal and paranasal sinus mucosa, in the bladder, and in the lacrimal gland (2). Some papillary lesions of the secretory duct of a salivary gland, such as oncocytoma, papillary cystoadenoma, Warthins tumor, intraductal papilloma (IP), inverted ductal papilloma and sialoadenoma papilliferum can clinically manifest as tumors of the oral cavity (3). Inverted ductal papilloma of the oral cavity (IDPOC) is an infrequent benign neoplasm of papillary appearance that originates in the secretory duct of a salivary gland. It forms part of a group of ductal papillary neoplasms, together with intraductal papilloma and sialoadenoma papilliferum. The size of the lesion varies from 0.5-1.5 cm in diameter, and the most common location is in a minor salivary gland of the lip and lower cheek mucosa (2, 3). The etiology is unknown, though some authors have related it to human papillomavirus (HPV) infection, due to the detection of HPV sequences (subtypes 6/11) within the lesion (4, 5). Certain immunohistochemical and ultrastructural studies have suggested that IDPOC may originate in the transition zone between the distal extremity of the secretory duct of a salivary gland and the surface epithelium of the oral cavity (6). Surgical removal is the treatment of choice for IDPOC. No relapses or malignant transformations have been reported to date (3, 7).
Fig. 1. Zone affected without signs of inflammation or suppuration.
Case report
A 40-year-old caucasian woman was reported to our service of Oral Surgery for evaluation and treatment of a tumor located in the lower left lip mucosa. She had the habit of nibbling her lower lip, and had suffered trauma in this same region, upon impacting with the head of her young child. After three months the patient noticed slight changes in the size of the lesion. She appeared to be in good health, and no maxillary asymmetries or tumors, or neck adenopathies were detected. At clinical exploration, the lesion showed a nodular aspect, of soft consistency, with no adherence to deep layers, and no pain in response to palpation (Fig. 1). There were no signs of inflammation or suppuration in the affected zone. The rest of the orofacial structures (teeth, upper lip, mucosal membranes, gums, tongue, floor of the mouth and mandible) were normal. The panoramic X-ray study likewise showed no alterations. - Differential diagnosis Based on the location, the history of trauma and the clinical characteristics of the lesion, a lower lip mucocele was initially diagnosed. However, the differential diage113
nosis also included other conditions such as pleomorphic adenoma, traumatic fibroma and lipoma. - Diagnosis and treatment Complete removal of the lesion was carried out with the CO2 laser under local anesthesia using 4% articaine with 1:100.000 adrenalin (Laboratorios Inibsa, Barcelona, Spain). The specimen sent to the pathology laboratory was of a pinkish color, rounded and measured 1 x 0.5 cm in size. The following postoperative medication was prescribed: ibuprofen 600 mg in tablets, one every 8 hours for 5 days (Ibuprofeno 600 mg, Zambom, Barcelona, Spain) and chlorhexidine gel, three applications a day for 10 days (Clorhexidina Gel Bioadhesivo 50 ml, Lacer, Barcelona, Spain). The postoperative course was free of complications, and the patient is presently subjected to periodic controls to detect possible relapse. - Histological study The surgical specimen was stained with hematoxylineosin (HE) and examined under an Olympus CX31RBSF light microscope (Olympus Corporation, Tokyo, Japan). The histological study revealed an endophytic lesion with extensive, rounded and regular margins, exhibiting an expansive growth pattern. The lesion was located in the transition zone between the secretory duct of a minor salivary gland and the surface epithelium of the oral cavity (Fig. 2). The tumor was composed of basaloid squamous cells without cytological atypia and included isolated mucosecretory cells (Fig, 3). Based on these findings, inverted ductal papilloma of the oral cavity was diagnosed. - Detection of HPV DNA extraction was carried out from the sample fixed in formalin solution and embedded in paraffin, based on
J Clin Exp Dent. 2013;5(2):e112-6.
Traumatic inverted ductal papilloma of the oral cavity.
Fig. 2. lesion located between the secretory duct of a minor salivary gland and the surface epithelium of the oral cavity.
(16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68, 69 and 82), and 19 of low risk (6, 11, 40, 42, 54, 55 , 61, 62, 64, 67, 70, 71, 72, 73, 81, 83, 84, IS39 and CP6108). The procedure for typing HPV DNA was carried out based on the same methodology as described above, and using the primers PGMY 09/11 for viral DNA amplification, and the primers PCO3, PCO4 and PCO5 for amplifying the -globin gene, which was used as internal control. The biotinylated amplicons were denaturalized with 0.4 N NaOH and hybridized in an immobile matrix with probes corresponding to 37 different HPV subtypes, according to the protocol recommended by the manufacturer (Roche Molecular Systems Inc., Los Angeles, CA, USA). Hybridization positivity was detected by streptavidin horseradish peroxidase precipitation onto the probe membrane. The sample DNA was correctly amplified, though no HPV DNA was detected.
Discussion
Fig. 3. A. Tumor composed of basaloid squamous cells without cytological atypia; B. Included isolated mucosecretory cells.
the conventional technique. HPV detection was carried out with the HPV LA genotyping test (Roche Molecular Systems Inc., Los Angeles, CA, USA). This process involves amplification of the viral DNA sequence via polymerase chain reaction (PCR) and posterior hybridization using probes corresponding to a total of 37 HPV subtypes 18 of which are considered to be of high risk
Inverted ductal papilloma of the oral cavity (IDPOC) was first described in 1982 by White et al. (2) as a benign tumor located in the secretory duct of a salivary gland, though the year before Basatkis et al. (8) had published three cases of an identical lesion which they referred to as papillary epidermoid adenoma. Due to its histological similarity to intraductal papilloma (IP) of the sinusal, nasal, bladder and oral mucosa, White et al. (2) coined the term inverted ductal papilloma of the oral cavity in reference to this lesion. IDPOC is an infrequent tumor of uncertain incidence (3). Regezi et al. (9) detected four of these lesions in a series of 238 minor salivary gland tumors. This has been the first and the only case of IDPOC diagnosed out of a total of 90 minor salivary gland biopsies performed in our service of Oral Surgery in the period 2003-2009. Since 2001, then there have been reported 10 new cases of IDPOCs, thus representing a total of 44, including the present case (Table 1). The patient age at appearance of the lesion is usually between the fourth and fifth decade of life and no particular gender predilection has been observed (1, 5). In our review of the literature, the mean age was found to be 44 years, with a range of 27-65 years. Clinically, IDPOC manifests as a submucosal tumor of nodular appearance and with a smooth or verrucous overlying surface, where dilatation of the salivary gland secretory duct outlet is generally noted (3). The lesion normally communicates with the mucosal surface (6), though a separating fibrous connective tissue band may be present. In our case the patient reported changes in the size of the lesion due to the internal accumulation of mucoid material. The oral structures most commonly affected by these lesions are the minor salivary glands particularly those of the lower lip mucosa, cheek mucosa and floor of the mouth(3, 5). The etiology is of IDPOC unknown, though some authors have related it to human papillomavirus (HPV)
e114
J Clin Exp Dent. 2013;5(2):e112-6.
Traumatic inverted ductal papilloma of the oral cavity.
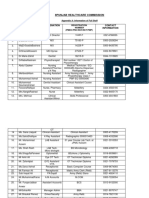
Table 1. New cases of inverted ductal papilloma of the oral cavity published since 2001 and up to the present case. F = female; M = male; HPV = human papillomavirus; NK = not known. No. cases 1 1 Haberland-Carrodeguas et al. (4) (2003) 1 1 1 1 Cabov et al. (7) (2004) Kubota et al. (6) (2006) Jurgens (3) (2004) Infante-Cosso et al. (5) (2008) Present case 1 1 1 1 1 Sex F F F M M M M M F F F Age 27 57 39 39 41 54 41 49 65 38 40 Origin/etiology NK NK NK HPV (6/11) HPV (6/11) HPV (6/11) NK NK NK HPV (11) Traumatism Location Soft palate Upper lip mucosa Cheek mucosa Floor of the mouth Floor of the mouth Cheek mucosa Cheek mucosa Cheek mucosa Lower lip mucosa Lower lip mucosa Lower lip mucosa
infection. Haberland-Carrodeguas et al. (4) were able to isolate HPV subtypes 6/11, while Infante-Cosso et al. (5) detected HPV subtype 11 in an HIV-infected female. In our case HPV DNA was not detected in the lesion, and no cytopathic changes suggestive of viral infection of the epithelial cells were observed. The antecedents of recurrent trauma reported by the patient in the affected zone possibly could have played an important role in the development of this tumor. In the latest cases reported in the literature, the mean evolution of the lesion has been 3-6 years, with a location in areas habitually exposed to trauma, such as the lip mucosa (as in our patient), the cheek mucosa and floor of the mouth. Macroscopically, IDPOC is an organized, non-encapsulated lesion presenting papillary crests that can form multicystic internal spaces. Growth is towards the lumen, and the tumor can even spread in an organized manner beneath the underlying connective tissue. Based on the location of the lesion, its growth pattern and papillary appearance, the histological differential diagnosis must be established with sialoadenoma papilliferum and intraductal papilloma (IP). However, from the histopathological perspective, the presence of mucosecretory cells among the basaloid squamous cells requires a differential diagnosis with mucoepidermoid carcinoma (6, 7). Sialoadenoma papilliferum is distinguished from IDPOC by its exophytic growth. This papillary lesion presents inflammatory connective tissue projections with acanthosis and parakeratosis at the surface of the epithelium. The gland stroma component also forms papillary prolongations with columnar or cuboid cells and mucosal cells. On the other hand, intraductal papilloma (IP) is an endophytic tumor that grows inwards within the duct, though in contrast to IDPOC, it forms a unicystic cavity. Mucoepidermoid carcinoma in turn is characterized by the presence of basal squamous cells and mucosal cells. The
e115
low grade lesions may present scant cytological atypia and pose differential diagnostic problems with IDPOC particularly in the case of incisional biopsies, where the characteristic structural pattern of the disease cannot be appreciated. A complete lesion sample is thus required in order to avoid diagnostic error (8). The treatment of choice is complete surgical removal, followed by histological analysis. In our case we used the CO2 laser for resection due to report fewer complications and relapses than the cold scalpel. The postoperative course in our patient was free of complications, and she is presently subjected to periodic controls to detect possible relapse. No relapses or malignization of IDPOC have been documented though a squamous cell carcinoma in an IP of the cheek mucosa has been identified (1). In most cases these complications are a consequence of an incomplete resection of the lesion.
Conflict of Interest
The authors declare that there are no conflicts of interest that could influence their work.
Acknowledgements
This study has been carried out by the consolidated research group in Dental and Maxillofacial Pathology and Treatment of the Institut dInvestigaci Biomdica de Bellvitge (IDIBELL), with financial support from the oral surgery teaching-healthcare agreement among the University of Barcelona, the Consorci Sanitari Integral and the Servei Catal de la Salut of the Generalitat de Catalunya.
J Clin Exp Dent. 2013;5(2):e112-6.
Traumatic inverted ductal papilloma of the oral cavity.
References
1. Boesen P, Laszewski M, Robinson R, Dawson D. Squamous cell carcinoma in an inverted papilloma of the buccal mucosa. Ann Otol Rhinol Laryngol. 1991;100:748. 2. White DK, Miller AS, McDaniel RK, Rothman BN. Inverted ductal papilloma: A distinctive lesion of minor salivary gland. Cancer. 1982;49:519-24. 3. Jurgens P. Inverted ductal papilloma of the lower lip: A case report. J Oral Maxillofac Surg. 2004;62:1158-61. 4. Haberland-Carrodeguas C, Fornatora ML, Reich RF, Freedman PD. Detection of human papillomavirus DNA in oral inverted ductal papillomas. J Clin Pathol. 2003;56:910-3. 5. Infante-Cosso P, Gonzalo DH, Hernndez-Gutirrez J, BorreroMartn JJ. Oral inverted ductal papilloma associated with condyloma acuminata and HPV in an HIV+ patient. Int J Oral Maxillofac Surg. 2008;37:1159-61. 6. Kubota N, Suzuki K, Kawai Y, et al. Inverted ductal papilloma of minor salivary gland: Case report with immunohistochemical study and literature review. Pathol Int. 2006;56:457-61. 7. Cabov T, Macan D, Manojlovic S, Ozegovic M, Spicek J, Luksic I. Oral inverted ductal papilloma. Br J Oral Maxillofac Surg. 2004;42:75-7. 8. Batsakis JG. Oral monomorphic adenomas. Ann Otol Rhinol Laryngol. 1991;100:348-50. 9. Regezzi J, Lloyd R, Zarbo R, McClatchey K. Minor salivary gland tumors. A histologic and inmunohistochemical study. Cancer. 1985;55:108-15.
e116
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Clinician's Guide To ADHD Comorbidities in Children and Adolescents Case Studies 2019 PDFDokument148 SeitenClinician's Guide To ADHD Comorbidities in Children and Adolescents Case Studies 2019 PDFfadel bilondatu100% (3)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Therapy With ChildrenDokument12 SeitenTherapy With Childrenantalmarialuana_67750% (1)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- ZSMU, Ukraine Pharmacology MCQs by Gankidi Raghavender Reddy,,,Used For Preparation of FMGE (Mci Screening Test) TooDokument117 SeitenZSMU, Ukraine Pharmacology MCQs by Gankidi Raghavender Reddy,,,Used For Preparation of FMGE (Mci Screening Test) Toogrreddy836100% (2)
- Case Presentation On GadDokument38 SeitenCase Presentation On GadBarjeesNoch keine Bewertungen
- Eric Berg CVDokument6 SeitenEric Berg CVHaralambicNoch keine Bewertungen
- Analgesics & Antibiotics in Pediatric DentistryDokument77 SeitenAnalgesics & Antibiotics in Pediatric DentistryJanani Gopalakrishnan100% (3)
- Injection TechniquesDokument7 SeitenInjection TechniquesLheo AngelesNoch keine Bewertungen
- Theories of Counseling and Psychotherapy A CaseDokument25 SeitenTheories of Counseling and Psychotherapy A Casedaffdg dsfNoch keine Bewertungen
- Access Consciousness The BARS - Nov11thDokument3 SeitenAccess Consciousness The BARS - Nov11thGinniNoch keine Bewertungen
- 1008cei Radiography WebDokument12 Seiten1008cei Radiography WebAndi Sitti Hajrah YusufNoch keine Bewertungen
- 1008cei Radiography WebDokument12 Seiten1008cei Radiography WebAndi Sitti Hajrah YusufNoch keine Bewertungen
- Traumatic Brain Injury PresentationDokument14 SeitenTraumatic Brain Injury Presentationapi-413607178Noch keine Bewertungen
- Pharmacology - Respiratory DrugsDokument61 SeitenPharmacology - Respiratory DrugsBenjamin Joel Breboneria100% (5)
- 4 Powerful Eye Exercises For Rapidly Improving Your VisionDokument8 Seiten4 Powerful Eye Exercises For Rapidly Improving Your VisionDoraemon Noby100% (1)
- Remotivation TherapyDokument2 SeitenRemotivation TherapyMelissa David100% (1)
- Nominal RollDokument11 SeitenNominal RollMuhammad FarooqNoch keine Bewertungen
- 1 The Influence of Parenting Style Towards Cooperatif Levels in ChildrenDokument23 Seiten1 The Influence of Parenting Style Towards Cooperatif Levels in ChildrenAndi Sitti Hajrah YusufNoch keine Bewertungen
- Muscle TrimmingDokument2 SeitenMuscle TrimmingAndi Sitti Hajrah YusufNoch keine Bewertungen
- PRD 12036Dokument12 SeitenPRD 12036Rolando Jorge TerrazasNoch keine Bewertungen
- X-Ray Analysis of Temporomandibular Joint in Totally Edentulous Patients With Symptoms of Temporomandibular DysfunctionDokument3 SeitenX-Ray Analysis of Temporomandibular Joint in Totally Edentulous Patients With Symptoms of Temporomandibular DysfunctionAndi Sitti Hajrah YusufNoch keine Bewertungen
- Kelompok 1a FKGDokument27 SeitenKelompok 1a FKGAndi Sitti Hajrah YusufNoch keine Bewertungen
- Responsi LimfadenitisDokument35 SeitenResponsi LimfadenitisSandra WirawanNoch keine Bewertungen
- DyslexiaDokument7 SeitenDyslexiaZumairi TaminNoch keine Bewertungen
- Gonzalez Lopez JL Cosmos Study 1Dokument10 SeitenGonzalez Lopez JL Cosmos Study 1Jose VegaNoch keine Bewertungen
- Peptic Ulcer DiseaseDokument3 SeitenPeptic Ulcer DiseasePhilip SimanganNoch keine Bewertungen
- Atrigel A Potential Parenteral Controlled Drug Delivery SystemDokument8 SeitenAtrigel A Potential Parenteral Controlled Drug Delivery SystemMaria RoswitaNoch keine Bewertungen
- Ezpap - Effects of EzPAP Post Operatively in Coronary Artery Bypass Graft PatientsDokument1 SeiteEzpap - Effects of EzPAP Post Operatively in Coronary Artery Bypass Graft Patientsjesushenandez_ftrNoch keine Bewertungen
- Early Features AutismDokument4 SeitenEarly Features AutismMonica AlexandruNoch keine Bewertungen
- CHBH Protocols 2004-1 PDFDokument161 SeitenCHBH Protocols 2004-1 PDFRagnah RantsNoch keine Bewertungen
- Ect BrochureDokument2 SeitenEct Brochureapi-283706202Noch keine Bewertungen
- Midazolam Injection: New Zealand Data SheetDokument14 SeitenMidazolam Injection: New Zealand Data SheetAlin AdelineNoch keine Bewertungen
- Blood Gases (Abgs) Interpretation Dr/Baha Eldin Hassan Ahmed Fellow Paediatric Critical CareDokument48 SeitenBlood Gases (Abgs) Interpretation Dr/Baha Eldin Hassan Ahmed Fellow Paediatric Critical Carehagir alhajNoch keine Bewertungen
- Session 6: Alcohol and Drug Use: E. E. Mccollum, and K. H. RosenDokument12 SeitenSession 6: Alcohol and Drug Use: E. E. Mccollum, and K. H. RosenLidiaMaciasNoch keine Bewertungen
- PredictiveDokument7 SeitenPredictiveAlbert VijayNoch keine Bewertungen
- Trauma 2Dokument10 SeitenTrauma 2rosenroseNoch keine Bewertungen
- HIPEC ProtocolDokument7 SeitenHIPEC ProtocolMariaNoch keine Bewertungen
- Neonatal Hyperbilirubinaemia 5.0Dokument25 SeitenNeonatal Hyperbilirubinaemia 5.0Anca AdamNoch keine Bewertungen