Beruflich Dokumente
Kultur Dokumente
Bronchiolitis Case Study
Hochgeladen von
Tey HerreraOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Bronchiolitis Case Study
Hochgeladen von
Tey HerreraCopyright:
Verfügbare Formate
SCHOOL OF NURSING AND MIDWIFERY
Cover Sheet for Assignments and Clinical Evaluation Forms
Student Name: Student Number: Unit Name: Assignment: ut!r: Date Due:
Joselle J. Herrera 16435 41 !ursing "ractice #64 Case Stud$ Assessment Susan %o$len &th Se'tem(er # 1#
Date Submitted: Insert t"is #a$ t! date stam%
)))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))
Students Receipt !& Submissi!n'
Date Submitted: Insert t"is #a$ t! date stam%
Student Name: Joselle J. Herrera Unit Name: !ursing "ractice #64 Student !um(er* 16435 41
Assignment:
Case Stud$ Assessment
NOAH 3 months BRONCHIOLITIS Case Study (100 marks = 0!" #ord $u%de&%ne (1'00 ( )000 *ords " It is July and you are working in Emergency Department (ED). Noah is 3 months of age and his mother has brought him to the hospital at !"" hours as he is #breathing fast and not feeding#. $ou note immediately that Noah is tachypnoeic and is not interested in mother or surroundings. %e has thick nasal discharge. %is mother Jodie appears an&ious. 's Jodie is undressing Noah( to enable a full assessment( you elicit more information. Noah has a 3 year old sister )adison who attends kindy and has had a cold recently. Noah had a runny nose a few days ago but now has a thick( creamy nasal discharge. %e has been #hot# for the last day( and was feeding #alright# yesterday but has only breastfed for a minute or two at a time today and more fre*uently than usual. Jodie states Noah is sick and she continues to appear +ery an&ious. ,n e&amination of Noah you notice that he is not at all upset when you take him from )um and put him on the weighing scales. -he following ob.ecti+e data is obtained from your nursing assessment/ 0 1eight/ 2.3 kg 0 -o 4 3!.3o5 0 6ulse 4 7"" beats per minute 8 regular 0 9espiratory rate 4 !! breathes per minute 0 ,7 :aturations (,7 :ats) 4 !2; in room air 0 Noah has nasal flaring( intercostal( substernal and subcostal recession( 0 -hick creamy nasal discharge. 0 'udible e&piratory whee<e 0 ' fre*uent( tight( congested cough present 0 5hest has a barrel shaped appearance. 'nterior 6osterior ('6)/ trans+erse diameters e*ual. 0 1idespread e&piratory whee<e and prolonged e&piratory phase 0 :kin is pale and oral mucous membranes are dry( 0 :kin remains pinched when skin turgor tested 0 'nterior fontanelle sunken ' post=nasal aspirate specimen is collected and tested in the laboratory. -hespecimen tests positi+e to 9espiratory :yncytial >irus (9:>).
1+ Ho* %s RS, transm%tted- () marks" 9espiratory :yncytial >irus is highly contagious and is transmitted through direct contact with respiratory secretions and indirect inoculation from contaminated surfaces? which can li+e on for 3" hours and on clothes or hands for less than hour (5D5( 7"" ? @in<er 8 Authrie( 7""3). :uch sustainability enables the +irus to spread easily in households and daycare centers (5D5( 7"" ). )oreo+er( children who attend daycare( li+e in crowded conditions( li+e with a family member who smokes( ha+e a chronic illness( or were born premature are at highest risk for the de+elopment of 9:> infection (@in<er 8 Authrie( 7""3).
)+ .%s/uss the e0%dem%o&o$%/a& 1a/tors o1 th%s 2%rus %n re&at%on to aet%o&o$y3 %n/%den/e3 0re2a&en/e3 0re2ent%on and 0ro$nos%s s0e/%1%/ to Noah4s a$e $rou0+ (10 marks) 9espiratory :yncytial >irus is a +iral organism that can cause upper and lower respiratory tract infections. 9:> commonly causes bronchiolitis and pneumonia in children and infants during the first year of life with a peak incidence between 7=2 months of life (,renstein( 7"""). )oreo+er( 9:> symptoms can last se+eral days and be accompanied by fe+er and loss of appetite. 2"; of those diagnosed are boys (,renstein( 7"""). 9espiratory :yncytial >irus is more common in infants who are not breast fed( li+e in crowded conditions( attend daycare( and li+e with mother#s who smoke cigarettes and are socially disad+antaged (,renstein( 7"""). :usceptibility is also greater during the peak 9:> season( which typically begins in the fall and ends in the spring (@in<er 8 Authrie( 7""3). 'ccording to @in<er 8 Authrie (7""3)( prematurely born infants represent the largest population at risk for se+ere complications of 9:> infection. Burthemore( premature infants often lack sufficient maternal antibodies for protection and? therefore( more susceptible to 9:> infection early in life. -hus(
they ha+e less energy reser+e than full=term infants and? conse*uently( can progress to respiratory failure more *uickly. 3+ How do you think Noah got bronchiolitis? (2 mark) I think that Noah got bronchiolitis due to his surroundings and immunological immaturity. Initially( the 9:> causes an infection in the upper respiratory tract( and then spreads downward into the lower tract. 'ccording to ,renstein (7""")( the +irus can cause inflammation and e+en death of the cells inside the respiratory tract and leads to the obstruction of airflow in and out of the child#s lungs. In NoahCs case( his bronchioles are smaller and easier to plug thus causing bronchiolitis when the +irus was inhaled.
+ 560&a%n *hy Noah has 0resented *%th the res0%ratory s%$ns and sym0toms that he has+ Re&ate Noah4s man%1estat%ons o1 res0%ratory d%stress to the 0atho0hys%o&o$%/a& /han$es /aused 7y 7ron/h%o&%t%s- (10 marks" 'ccording to @in<er 8 Authrie (7""3)( 9:> in+ades the bronchiolar epithelial cells causing inflammation and edema. -he membranes of the infected cells fuse with ad.acent cells to form a large( multinucleated cell creating large masses of cells or syncytia (@in<er 8 Authrie( 7""3). Burthermore( the bronchiole mucosa ultimately begins to swell and the lumina fill with mucus and e&udates ()cIntosh( 7"""? 1ong et al.( 7""3). -hen( Inflammatory cells infiltrate the area resulting in the shedding of dead epithelial cells? which causes obstruction of small airway passages resulting in hyperinflation and areas of atelectasis (@in<er 8 Authrie( 7""3). -he inflammation and e&udate caused by the 9:> infection results in bronchiole obstruction during e&piration( air trapping( poor e&change of gases( increased work of breathing( and a characteristic e&piratory whee<e (:andritter 8 Draus( EEF? 1ong et al.( 7""3).
'+ What acid/base imbalance does Noah have? ( marks) Gncompensated 9espiratory 'cidosis is the acid=base disturbance initiated in NoahCs case.
8+ 560&a%n *hat %s ha00en%n$ *%th ea/h o1 the 1o&&o*%n$ /om0onents o1 the 7&ood $as resu&t and the rat%ona&e 1or ea/h /han$e s0e/%1%/ to Noah4s d%a$nos%s+ (9 marks" 9espiratory 'cidosis resulted from diminished or inade*uate pulmonary +entilation( which leads to an ele+ated partial pressure of carbon dio&ide (:aCO)"3 a normal le+el of bicarbonate content (HCO3"( and decreased o&ygenation (:aO)". -he hypo+entilation inhibits the e&cretion of carbon dio&ide( which conse*uently combines with water in the body to produce carbonic acid( thus reducing plasma 0H. ;n/om0ensated a/%dos%s results from compensatory mechanisms which unable to maintain the body p% le+el within the normal range.
<+ Noah is dehydrated! "ive at least # reasons why would Noah be dehydrated? (# marks) a) Decreased water or fluid intake. b) Bebrile illness/ fe+er causes increased insensible fluid losses. c) Insensible fluid losses such as discharges.
9+ Is the amount ordered reasona7&e 1or Noah- :&ease demonstrate understand%n$ o1 1&u%d re=u%rements %n your ans*er+ (3 marks" Bormula/ 1eight & mlHkgH7Ih J 7I 2.3 kg & 33 mlHkgH7Ih J 7I4 32.3 or 3F mlHhr $es( the amount is reasonable.
9. What mani$estations would contribute to insensible loss in Noah%s case and how would these $actors contribute! (# marks) Runny nose and other d%s/har$es can also be causes of fluid loss and it is difficult for a person to replace water by drinking it if they are unable to tolerate li*uids. -he body can lose significant amounts of water when it tries to cool itself by s*eat%n$. 1hether the body is hot because of the en+ironment or because a fe+er is present due to an infection? the body uses a significant amount of water in the form of sweat to cool itself (Nettina( 7""2). Ina7%&%ty to dr%nk 1&u%ds+ -he inability to drink ade*uately is the other potential cause of dehydration. 'ccording to 6illitteri (7""F)( whether it is the lack of a+ailability of water or the lack of strength to drink ade*uate amounts? this( coupled with routine or e&traordinary water losses can compound the degree of dehydration.
10+ Noah %s dehydrated+ #hat
/&%n%/a& man%1estat%ons 1rom the data you
ha2e 7een $%2en %nd%/ate th%s- ( marks" a) :kin is pale. b) ,ral mucous membranes are dry. c) :kin remains pinched when skin turgor tested. d) 'nterior fontanelle sunken.
11+ #hat ty0e o1 dehydrat%on %s Noah most &%ke&y to ha2e and *hy- ( marks"
Isotonic dehydration is mostly likely to occur. Due to electrolyte and water deficits occurring in appro&imately balanced proportions (Nettina( 7""2). 1)(13+ State the nurs%n$ %nter2ent%ons and mat/h these *%th s/%ent%1%/ rat%ona&e 1rom the e2%den/e 7ased &%terature (' marks ea/h" a"Ineffective breathing pattern evident by hypoxia, tachypnoea, nasal flaring, intercostal, substernal and subcostal recession, cough, expiratory wheeze. NURSING INTEVENTION Institute contact isolation. 6romote proper hand hygiene. RATIONALE 6re+ent the spread of infection for patient with highly contagious disease (Nettina( 7""2). Infants are obligate nose breathers (Nettina( 7""2). 5orrect positions promote easier +entilation? and occasional side or abdominal position will aid drainage of li*uefied secretions (6illitteri( 7""F 5hanging positions fre*uently minimi<e spasm and sudden blockage of airway (6illitteri( 7""F).
Deep nasal passages free from secretions. Gse a bulb syringe to clear nares and oropharyn&. 6lace child in a comfortable position such as semi=fowlerCs or side lying.
5hange position fre*uently and allow the infant to assume a position of comfort.
7"
Fluid
volume
deficit
evident
by
pale
skin,
dry
mucous
membranes, poor skin turgor, sunken anterior fontanelle. NURSING INTEVENTION 'ssess for further signs of dehydration. 'dminister oral rehydration therapy. 9ecord the childCs intake and output( and daily weights. RATIONALE Intra+enous fluids help restore and maintain ade*uate hydration for the patient (Nettina( 7""2).
'dminister I.>. fluids at the prescribed rate.
9eplacement with I.>. fluids is re*uired whene+er a child is unable to meet daily losses( replace deficits( or ongoing losses (6illitteri( 7""F). 5ontrol of fe+er reduces respiratory rate and fluid loss (6illitteri( 7""F).
5ontrol fe+er e.g. Ai+e antipyretics prescribed( increase e+aporation from skin with tepid sponges.
c) Sleep pattern disturbance characterized by Noah s lethargy, listlessness and irritability. NURSING INTEVENTION Encourage the parents to stay with the infant as much as possible and pro+ide a *uiet( stress=free en+ironment. 6ro+ide fre*uent changes of clothing and linen for the infant. @oosen tight clothing. RATIONALE 6arents must pro+ide comfort and security to promote ade*uate rest for the infant (Nettina( 7""2). 6arents must promote comfort and reduce infantCs restlessness? which is a sign of increasing respiratory distress or obstruction (6illitteri( 7""F). ' caregi+erCs cuddling and warmth can ease fears and infants commonly seek comfort from a security ob.ect during times of uncertainty or stress (Nettina( 7""2).
6ro+ide comfort and warmth e.g. blanket or a stuffed toy.
d" !ltered nutrition less than body re"uirements manifested by Noah s disinterest in breastfeeding prior to presenting to hospital NURSING INTEVENTION Discuss to the mother the importance of good nutrition. e.g. breast or bottle=feeding( feeding schedules( using syringes( cups. Emphasi<e on how breast feeding is +ery important to the RATIONALE Encourage the mother to follow recommendations for age= appropriate well childcare health promotion (Nettina( 7""2). Kreast milk or formula remains the primary source of nutrition
infantCs growth. -each the proper ways of breastfeeding e.g. positioning and? pumping to help stimulate the motherCs milk supply.
and it pro+ides an immunological boost for infants (6illitteri( 7""F). :tress of new motherhood or illness in the infant or mother may decrease the motherCs milk supply and inhibit her Llet= downC refle&( as well as increase or decrease the infantCs desire to suckle (Nettina( 7""2).
1 + >od%e *%shes to /udd&e Noah4s and 7reast1eed h%m+ A&ter your /are 0&an to su%t Noah4s /urrent status+ (9 marks"+ NURSING INTEVENTION Kegin breast=feeding in a *uiet( comfortable place that is free from interruption. Gse a pillow and a footstool. )ake sure infant is awake and hungry. 6osition infant at the breast by placing the infant in a semi= sitting position with face close to the breast and supported by one of the motherCs arms and hand. -he mother may need to support her breast with the other hand. Kurp the infant during and at the end of the feeding. RATIONALE 6illow help support the infant and a footstool to ele+ate the motherCs leg? and If awake and comfortable( the infant will settle down and feed better (Nettina( 7""2). 6roper positioning will pro+ide the infant with comfort and security and make it easier for the infant to suck and swallow? this makes the nipple more easily accessible to the infantCs mouth and pre+ents further obstruction of nasal breathing (6illitteri( 7""F). Kurping pre+ents abdominal distention or regurgitation from air swallowed during the feeding (6illitteri( 7""F). 5hanging soiled diapers lessen skin irritation (Nettina( 7""2). 9ight side lying pre+ents infants from aspiration and facilitates comfort when breathing (Nettina( 7""2).
1hen infant has finished feeding( change the diaper if it is wet or soiled. 6osition infant on the right side in bed.
1'+ 560&a%n *hat you *ou&d te&& >od%e a7out the mode o1 transm%ss%on o1 RS, and ho* she /an de/rease the /han/es o1 Noah $ett%n$ 7ron/h%o&%t%s a$a%n+ (3 marks"+ Kecause the +irus causing bronchiolitis can be spread to others +ia contact or inhalation( I would e&plain to her the importance of/ Deeping the infant away from people who are infected with cold. Deeping her baby warm thus reducing chances of a cold attack. Deeping the baby away from densely populated common places and the mother not allowing anyone to smoke near the baby. E+eryone going in and out of the room must wash hisHher hands. %ands must also be washed after pro+iding direct care to the child? whene+er hands are soiled by secretions or e&cretions? and after touching toys( medical e*uipment and furniture. %and washing is the best way to pre+ent the spread of infection.
18+ #hat 1urther %n1ormat%on *ou&d you %n/&ude %n Noahs d%s/har$e 0&an- (10 marks" E&plain to the parents or family members the prescribed medications included in the physicianCs order prior discharge. Discuss proper techni*ues for suctioning the nose and making breathing easier for the baby. 6rior discharge( parents must state that they understand the gi+en home management plan for the Noah. Ai+e Kronchiolitis parentHcaregi+er education leaflet. 6arents must ha+e a copy of Kronchiolitis education leaflet for further gain of knowledge. Immuni<ations gi+en before discharge if not up to date. Inform the parents that +accination is a+ailable to pre+ent 9:>.
'd+ice parents to consider nursing or other follow up in the community. 9ecommend Aeneral 6ractitioner follow up. hospital only if symptoms worsen or persist. 6atient must return to
Kreastfeed the baby+ Kreast milk helps the baby#s body fight infections( and may help pre+ent further health problems. 'd+ice the family to wash hands fre*uently. Deep the babyCs hands clean. -his is the most important thing a parent can do to pre+ent spreading germs( including those that cause bronchiolitis. 1ash often with soap and water to remo+e germs from your hands. ' germ=killing hand lotion or gel may be used when no water a+ailable.
1<+ R5?5R5NC5S@
5enters for Disease 5ontrol and 6re+ention. (7"" ). 9espiratory syncytial +irus. 9ock+ille( )D/ National 5enter for Infectious Diseases. 9etrie+ed 'pril " ( 7" " from www.cdc.go+HncidodHd+rdHre+bHrespiratoryHrs+feat.htm.
5enters for Disease 5ontrol. (7""7). 9espiratory syncytial +irus acti+ity K. 9etrie+ed 'pril 3( 7" "( from www.cdc.go+HmmwrHpre+iewHmmwrhtmlHmm3 "7a7.htm.
5urtin @ibrary and Information :er+ice. (n.d.). '6' referencing. 9etrie+ed 'pril " ( 7" "( from http/HHlibrary.curtin.edu.auHreferencingHinde&.html.
@in<er( J.B.( 8 Authrie( 5.5. (7""3). )anaging a 1inter :eason 9isk/ Kronchiolitis in children. Emergency Medicine Reports( !(7)( 3=77.
)cIntosh( D. (7"""). 9espiratory syncytial +irus. In 9.E. Kehrman( 9.). Dliegman( 8 %.K. Jenson (Eds.)( Nelson Textbook of Pediatrics (16th ed. ! EE =EE3.
,renstein( D.). (7"""). Kronchiolitis. In 9.E. Kehrman( 9.). Dliegman( 8 %.K. Jenson (Eds.)( Nelson Textbook of Pediatrics (16th ed. ! 7!3= 7!F.
6illitteri( '. (7""F). @ippincott 1illiams 8 1ilkins. Maternal " #hild $ealth N%rsing& #are of the childbearing and childrearing family! 7( 73=3".
Nettina( :.). (7""2). @ippincott 1illiams 8 1ilkins. Man%al of N%rsing Practice/ )aternity and childcare (!th ed.)( I7( 332= I3I
:andritter( -.@.( 8 Draus( D.). ( EEF). 9espiratory :yncytial >irus= Immunoglobulin Intra+enous (9:>=IAI>) for 9espiratory :yncytial >iral Infections/ 6art . 'o%rnal of Pediatric $ealth #are! ! 7!I=7E3.
Das könnte Ihnen auch gefallen
- Case Study - BronchiolitisDokument4 SeitenCase Study - Bronchiolitisgojdsjdsjfis0% (1)
- Case Study Bronchiolitis UpdatedDokument23 SeitenCase Study Bronchiolitis UpdatedwokorowNoch keine Bewertungen
- Hyperbilirubinemia Case StudyDokument7 SeitenHyperbilirubinemia Case Studyr_ramos0759Noch keine Bewertungen
- Case Study TBDokument8 SeitenCase Study TBCesar Emmanuel Abigania100% (2)
- Case Study Neonatal SepsisDokument21 SeitenCase Study Neonatal SepsisLenjun0% (1)
- Acute Bronchitis - FinalDokument28 SeitenAcute Bronchitis - FinalJied100% (6)
- Neonatal SepsisDokument41 SeitenNeonatal Sepsisien100% (8)
- NCP For UrtiDokument40 SeitenNCP For UrtiEarl JamesNoch keine Bewertungen
- Hyaline Membrane DiseaseDokument31 SeitenHyaline Membrane DiseaseWeng RamojalNoch keine Bewertungen
- CASE REPORT Rhinitis AlergyDokument36 SeitenCASE REPORT Rhinitis AlergySiti MunirahNoch keine Bewertungen
- Case 5 SeizureDokument74 SeitenCase 5 SeizureGrace TanajuraNoch keine Bewertungen
- Case Study-PneumoniaDokument76 SeitenCase Study-PneumoniaArbie Jacinto80% (5)
- (DOC) 2015 - Pediatrics Case StudyDokument29 Seiten(DOC) 2015 - Pediatrics Case StudyEden CruzNoch keine Bewertungen
- Case Study PneumoniaDokument6 SeitenCase Study PneumoniaBrian CornelNoch keine Bewertungen
- Febrile SeizureDokument8 SeitenFebrile Seizureanon_944507650Noch keine Bewertungen
- Neonatal NCPDokument7 SeitenNeonatal NCPMaria Delia SalvadoNoch keine Bewertungen
- How Phototherapy WorksDokument4 SeitenHow Phototherapy WorksmaramNoch keine Bewertungen
- Febrile SeizuresDokument4 SeitenFebrile Seizuresmgonzalez_29Noch keine Bewertungen
- Session13 - Endometrial CaDokument27 SeitenSession13 - Endometrial CaCHALIE MEQUNoch keine Bewertungen
- Nursing Care Plan ExampleDokument9 SeitenNursing Care Plan ExampleJohn Sumallo Tegio75% (4)
- Power Point For The Case Study About PneumoniaDokument16 SeitenPower Point For The Case Study About PneumoniaJai - Ho86% (7)
- Gastroschisis Final PresentationDokument43 SeitenGastroschisis Final PresentationlhedavenNoch keine Bewertungen
- Case Study of Bronchial Asthma in Acute ExacerbationDokument19 SeitenCase Study of Bronchial Asthma in Acute ExacerbationEzra Dizon ManzanoNoch keine Bewertungen
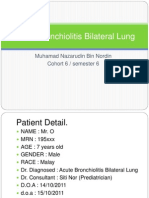
- Acute Bronchiolitis Bilateral Lung Case Study PresentationDokument36 SeitenAcute Bronchiolitis Bilateral Lung Case Study PresentationPyka Izzaty100% (1)
- Tuberculosis and Nephrotic Syndrome in A Child: Case ReportDokument34 SeitenTuberculosis and Nephrotic Syndrome in A Child: Case ReportAldo YustiantoNoch keine Bewertungen
- PEDIATRICS CaseDokument17 SeitenPEDIATRICS CaseCharles BayogNoch keine Bewertungen
- Acute Lobar PneumoniaDokument13 SeitenAcute Lobar PneumoniaICNoch keine Bewertungen
- Benign Febrile Seizure: Oris, Pamitan, Newberry 2NU06Dokument44 SeitenBenign Febrile Seizure: Oris, Pamitan, Newberry 2NU06Arthur Brian Panit100% (2)
- Febrile SeizureDokument16 SeitenFebrile SeizureRashed Shatnawi100% (1)
- Cough and Dyspnea Case StudyDokument4 SeitenCough and Dyspnea Case StudyAbigail Balbuena100% (1)
- Case of Febrile SeizuresDokument2 SeitenCase of Febrile SeizuresAzizan HannyNoch keine Bewertungen
- Pediatric Community-Acquired PneumoniaDokument60 SeitenPediatric Community-Acquired PneumoniaIkea Balhon100% (1)
- Neonatal Sepsis Case 2Dokument81 SeitenNeonatal Sepsis Case 2Joanne Bernadette Aguilar100% (1)
- Case Study Tonsil It IsDokument16 SeitenCase Study Tonsil It IsMuhammad FarhanNoch keine Bewertungen
- Case Study: Acute BronchitisDokument34 SeitenCase Study: Acute BronchitisJeffany Anne Rabaya Retirado0% (1)
- Pedia With LeukemiaDokument14 SeitenPedia With LeukemiaAlynna ValbuenaNoch keine Bewertungen
- Pulmonary Tuberculosis Case StudyDokument24 SeitenPulmonary Tuberculosis Case StudyKylie Golindang100% (3)
- Case Presentation HydrocephalusDokument48 SeitenCase Presentation HydrocephalusSu Osman50% (2)
- Pneumonia CaseDokument11 SeitenPneumonia CaseBrigette Molly LopezNoch keine Bewertungen
- Pneumonia Case StudyDokument14 SeitenPneumonia Case StudyMaryann LayugNoch keine Bewertungen
- Feliciano, Troy Ivan Silva, Queenie Rose V. BSN 3-C: Rationale: To Track The Changes of Client's ConditionDokument4 SeitenFeliciano, Troy Ivan Silva, Queenie Rose V. BSN 3-C: Rationale: To Track The Changes of Client's ConditionQueenie SilvaNoch keine Bewertungen
- PCAP FinalDokument28 SeitenPCAP FinalAmiebelle Naval0% (2)
- Hydronephrosis Fred LuceDokument69 SeitenHydronephrosis Fred LuceKMNoch keine Bewertungen
- Case AppendicitisDokument30 SeitenCase AppendicitisSarahNoch keine Bewertungen
- TAHBSO ReportDokument4 SeitenTAHBSO ReportsachiiMeNoch keine Bewertungen
- Neonatal Hypoglycemia APNECDokument26 SeitenNeonatal Hypoglycemia APNECyumicheongNoch keine Bewertungen
- Case Presentation Hepatitis A LuluDokument28 SeitenCase Presentation Hepatitis A LuluBrenda KarinaNoch keine Bewertungen
- GASTROSCHISISDokument4 SeitenGASTROSCHISISVin Custodio100% (1)
- Neonatal Pneumonia Case StudyDokument2 SeitenNeonatal Pneumonia Case StudyAngel Villamor0% (1)
- 1 Febrile Seizures DDokument30 Seiten1 Febrile Seizures DDorjee SengeNoch keine Bewertungen
- Ward Case PresentationDokument92 SeitenWard Case PresentationSuzette Rae TateNoch keine Bewertungen
- Clinical Log-5 Tibia #Dokument5 SeitenClinical Log-5 Tibia #Tahani KhalilNoch keine Bewertungen
- Pediatric Case StudyDokument29 SeitenPediatric Case Studyapi-296281683Noch keine Bewertungen
- I Can'T Breathe If Breathing Is Without: Bronchial AsthmaDokument33 SeitenI Can'T Breathe If Breathing Is Without: Bronchial AsthmaklamorenaNoch keine Bewertungen
- 1st Year-Pneumonia Case (Pedia Ward - Labrador)Dokument34 Seiten1st Year-Pneumonia Case (Pedia Ward - Labrador)parislove19Noch keine Bewertungen
- Case Study - OTITIS MEDIADokument9 SeitenCase Study - OTITIS MEDIAHasing Amado100% (1)
- Management of Tuberculosis: A guide for clinicians (eBook edition)Von EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Noch keine Bewertungen
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- Pathophysiology of Koch's Disease (Tuberculosis) : Primary InfectionDokument5 SeitenPathophysiology of Koch's Disease (Tuberculosis) : Primary InfectionYvylan Salino CasundoNoch keine Bewertungen
- Lung Toxicology Worksheet WordDokument4 SeitenLung Toxicology Worksheet Wordapi-236697820Noch keine Bewertungen
- Defient Fluid Volume Intake and Impaired Mobility NCPDokument6 SeitenDefient Fluid Volume Intake and Impaired Mobility NCPjordan aguilarNoch keine Bewertungen
- Screening Questionnaire: Dha Eligibility LetterDokument2 SeitenScreening Questionnaire: Dha Eligibility LetterDr. Emad Elbadawy د عماد البدويNoch keine Bewertungen
- Reverse TsaDokument4 SeitenReverse Tsaprwill00Noch keine Bewertungen
- Mental Status ExamDokument10 SeitenMental Status ExamSrini VoruNoch keine Bewertungen
- Respiratory Failure in Children PDFDokument47 SeitenRespiratory Failure in Children PDFOxana TurcuNoch keine Bewertungen
- Benefits at A Glance: TexasDokument10 SeitenBenefits at A Glance: Texasakula_rupeshNoch keine Bewertungen
- LT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewDokument3 SeitenLT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewfatimaNoch keine Bewertungen
- Understanding Basics of EKG: by Alula A. (R III)Dokument37 SeitenUnderstanding Basics of EKG: by Alula A. (R III)sky nutsNoch keine Bewertungen
- Occupational Therapy - Kids Health Information: Scar ManagementDokument4 SeitenOccupational Therapy - Kids Health Information: Scar Managementmuambany1Noch keine Bewertungen
- T 1234029783 11845985 Nursing Crib Com Nursing Care Plan Dengue FeverDokument2 SeitenT 1234029783 11845985 Nursing Crib Com Nursing Care Plan Dengue Feversamantha cortezNoch keine Bewertungen
- J&J CompanyDokument127 SeitenJ&J CompanyRam TyagiNoch keine Bewertungen
- Branches of ZoologyDokument3 SeitenBranches of ZoologyVivek Morya100% (1)
- Final Abstract and Paper Edit 26 April 2020 อ เปรม แก้แล้ว PDFDokument22 SeitenFinal Abstract and Paper Edit 26 April 2020 อ เปรม แก้แล้ว PDFchanakarn Vipusmith100% (2)
- Catabolism of HemeDokument34 SeitenCatabolism of HemeGlen Jacobs Sumadihardja100% (2)
- Atlas of Gastrointestinal Endoscopy and Related PathologyDokument2 SeitenAtlas of Gastrointestinal Endoscopy and Related PathologyMaria PatituNoch keine Bewertungen
- 16-4 I The Truth About Physician Health ProgramsDokument5 Seiten16-4 I The Truth About Physician Health ProgramslbandrewNoch keine Bewertungen
- Multidisciplinary Management of Female Pelvic Floor DisordersDokument336 SeitenMultidisciplinary Management of Female Pelvic Floor DisordersJuan Jose Sardi100% (3)
- Wellness Check PrintableDokument2 SeitenWellness Check PrintablethubtendrolmaNoch keine Bewertungen
- Bio Availability Solved ProblemsDokument2 SeitenBio Availability Solved Problemsabdullah2020100% (1)
- Management Flabby RidgeDokument4 SeitenManagement Flabby RidgeNidya Patricia Sembiring100% (1)
- Strengthening Quality Midwifery Education For 2030 - Who Unfpa Unicef 20Dokument4 SeitenStrengthening Quality Midwifery Education For 2030 - Who Unfpa Unicef 20Sheilla Tania MarcelinaNoch keine Bewertungen
- Sports NutritionDokument78 SeitenSports NutritionnpurdonNoch keine Bewertungen
- Chapter 11 Occlusal Adjustment PDFDokument8 SeitenChapter 11 Occlusal Adjustment PDFDavid ColonNoch keine Bewertungen
- Ointment Box OutlineDokument1 SeiteOintment Box OutlineDon Nestor Razon Jr.Noch keine Bewertungen
- Hepatitis in Children: DR Hamza BawumiaDokument36 SeitenHepatitis in Children: DR Hamza BawumiaHamza BawumiaNoch keine Bewertungen
- Assignment 4: Genes & Cancer: NameDokument2 SeitenAssignment 4: Genes & Cancer: Namemiriam tidalNoch keine Bewertungen
- Aortic AneurysmDokument26 SeitenAortic Aneurysmchetanm2563100% (1)
- Apsy 603 Dual Relationship Assignment 4Dokument18 SeitenApsy 603 Dual Relationship Assignment 4api-161848380100% (1)
- Consenso Francês 2022Dokument20 SeitenConsenso Francês 2022larissa fernandesNoch keine Bewertungen
- BestDokument25 SeitenBestAlejandro Lopez OsorioNoch keine Bewertungen