Beruflich Dokumente
Kultur Dokumente
Diagnostico y Tratamiento de Lupus Eritematoso Sistemico Con Compromiso Visceral
Hochgeladen von
Franklin ArandaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Diagnostico y Tratamiento de Lupus Eritematoso Sistemico Con Compromiso Visceral
Hochgeladen von
Franklin ArandaCopyright:
Verfügbare Formate
REVIEW
Systemic Lupus Erythematosus: Emerging Concepts
Part 1: Renal, Neuropsychiatries, Cardiovascular, Pulmonary, and
Hematologic Disease
Dimitrios T. Boumpas, MD; Howard A. Austin III, MD; Barri J. Fessler, MD; James E. Balow, MD;
John H. Klippel, MD; and Michael D. Lockshin, MD
• Purpose: To review advances and controversies in Oystemic lupus erythematosus is an extraordinarily com-
the diagnosis and management of systemic lupus ery- plex autoimmune disease that touches on nearly all med-
thematosus with visceral involvement (renal, neuropsy- ical subspecialties (1). Evidence from a broad range of
chiatric, cardiopulmonary, and hematologic disease). basic science studies indicates that the pathogenesis of
• Data Sources and Study Selection: Review of the this disease is equally complex and may vary from patient
English-language medical literature with emphasis on to patient. The diverse expression of the common lupus
articles published in the last 5 years. More than 400 syndrome may result from variable abnormalities in inter-
articles were reviewed. secting genetic, immunologic, hormonal, and environmen-
• Dafa Synthesis: Recent debates pertaining to lupus tal pathways. Although many uncertainties about patho-
nephritis have focused on the value of kidney biopsy genic mechanisms remain, recent advances in diagnosis
data and the role of cytotoxic drug therapies. Many and treatment have substantially improved the prognosis
studies have shown that estimates of prognosis are of patients with systemic lupus erythematosus. As mortal-
enhanced by consideration of clinical, demographic, ity rates decrease, issues such as comorbidity, complica-
and histologic features. For patients with severe lupus tions of therapy, and overall quality of life are receiving
nephritis, an extended course of pulse cyclophospha- increased attention.
mide therapy is more effective than a 6-month course of We discuss recent advances in systemic lupus erythem-
pulse methylprednisolone therapy in preserving renal atosus. By necessity, this review is not comprehensive; we
function. Adding a quarterly maintenance regimen to focus on changing concepts and new information. In this,
monthly pulse cyclophosphamide therapy reduces the the first part, we review issues related to the diagnosis
rate of exacerbations. Plasmapheresis appears not to and management of systemic lupus erythematosus with
enhance the effectiveness of prednisone and daily oral visceral involvement. In the second part, to be published
cyclophosphamide. Small case series have shown in the 1 July issue, we examine selected topics related to
pulses of cyclophosphamide to be beneficial in patients dermatologic and joint disease, as well as issues related to
with lupus and neuropsychiatric disease refractory to the antiphospholipid antibody syndrome, pregnancy, hor-
glucocorticoid therapy, acute pulmonary disease monal therapy, and morbidity and mortality. We conclude
(pneumonitis or hemorrhage), and thrombocytopenia. with an overview of recent advances in the pathogenesis
Patients with systemic lupus erythematosus have an of the disease.
increased prevalence of valvular and atherosclerotic
heart disease, apparently because of factors related to
the disease itself and to drug therapy. Renal Disease
• Conclusions: Cytotoxic agents are superior to glu- The kidney is the viscus most commonly affected by
cocorticoid therapy for the treatment of proliferative systemic lupus erythematosus. With the use of sensitive
lupus nephritis, but the optimal duration and intensity light, electron, and immunofluorescence microscopy, at
of cytotoxic therapy remain undefined. Definitive stud- least modest abnormalities are seen in kidney biopsy spec-
ies of the treatment of autoimmune thrombocytopenia imens from almost all patients with lupus. Approximately
and acute pulmonary disease and of the diagnosis and 75% of renal biopsy specimens reported in several series
treatment of neuropsychiatric disease are not available. have been classified as focal proliferative, diffuse prolifer-
ative, or membranous glomerulonephritis (2).
Pathogenesis
Localization of immune complexes in the kidney ap-
pears to be the inciting event for the development of
lupus nephritis. Autoantibodies that react with DNA and
other cellular components are characteristic of human and
murine systemic lupus erythematosus, but only a subset of
Ann Intern Med. 1995;122:940-950. the resulting immune complexes seems to be nephro-
genic. Studies correlating the immunochemical properties
From the National Institutes of Health, Bethesda, Maryland. For of autoantibodies with the type and severity of nephritis
current author addresses, see end of text. have detected several features that may promote patho-
940 15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12
genicity, including quantity, charge, class, isotype, idio- Renal Biopsy
type, avidity for DNA, and efficiency of complement fix- A classic clinical syndrome (for example, rapidly pro-
ation (3). Furthermore, cross-reactivity of anti-DNA gressive glomerulonephritis) may, in some cases, obviate
autoantibodies with glomerular cell surface antigens, as the need for a kidney biopsy to establish the type of lupus
well as with normal components of basement membrane nephritis. Many patients, however, present with clinical
and mesangial matrix, probably promotes glomerular im- features compatible with several of the classes of lupus
mune complex formation and influences the location of nephritis for which different treatment strategies are usu-
these deposits within the glomerulus (4). Thus, factors ally recommended. In these patients, renal biopsy data
that lead to the deposition of many proinflammatory im- may clarify an ambiguous situation and help to justify
mune complexes in the subendothelial region of the glo- various therapeutic options. In the absence of significant
merular capillary wall, adjacent to the circulation, are proteinuria or urinary sediment abnormalities, we are
likely to induce (through release of complement compo- usually reluctant to recommend renal biopsy outside the
nents, cytokines, and other factors) cellular proliferation, context of a research protocol.
an inflammatory response, necrosis, and eventually fibro- Deliberations about treatment usually include an as-
sis (5). Furthermore, a subset of autoantibodies may pen- sessment of prognosis. Hypertension has been associated
etrate glomerular cells, bind to nuclei, and contribute to with renal disease progression and death (17). The con-
glomerular proliferation and proteinuria (6). tribution of kidney morphologic evaluation to estimates of
prognosis has been debated vigorously. Detailed records
The subepithelial immune deposits characteristic of lu-
of the duration of nephritis (18) or the rate of change of
pus membranous nephropathy probably evolve through
renal function (19) provide an indication of the balance of
the in situ interaction of autoantibodies with antigens,
reversible and irreversible injuries that may have oc-
such as DNA or histones, that bind to glomerular base-
curred. Kidney biopsy data provide a more direct ap-
ment membrane because of their affinity for basement
praisal of the type of renal disease and have enhanced
membrane components such as fibronectin, collagen,
outcome predictions based on clinical data in several ( 2 0 -
laminin, and heparan sulfate (7). Subepithelial immune
23), but not all (18, 24), studies. Variations in conclusions
complexes induce relatively little cellular proliferation or
may relate to the salutary effects of contemporary treat-
inflammatory response. Glomerular capillary wall injury ments as well as to differences in patient selection criteria,
appears to be induced by complement activation and for- prognostic factors, and outcome measures studied. Sev-
mation of the membrane attack complex, C5b-9, that has eral investigators have observed the prognostic effect of
been associated with this type of active immune complex- markedly active histologic features (such as cellular cres-
mediated injury (8). cents, fibrinoid necrosis, and subendothelial immune de-
posits) combined with chronic, irreversible morphologic
attributes (such as interstitial fibrosis, tubular atrophy,
Diagnostic Studies and glomerular sclerosis) (22, 25, 26).
Laboratory Evaluation
Serologic variables have been extensively evaluated as Treatment
indicators of the activity of lupus nephritis. Serum com- Glucocorticoids
plement abnormalities have correlated with the degree of A mainstay of the treatment of systemic lupus erythem-
renal histologic activity in several studies (9, 10). Persis- atosus, glucocorticoids are often used alone as initial ther-
tent C3 or CH 50 complement depression has been asso- apy for patients with lupus nephritis. Prednisone at low to
ciated with progression of kidney disease in some, but not intermediate doses is usually sufficient for patients with
all, groups of patients (10-12). Antinuclear and anti-DNA mesangial and mild focal proliferative glomerulonephritis.
antibody levels have been less consistently related to fea- Studies now in progress are evaluating the effectiveness
tures of active glomerulonephritis (13). Serologic abnor- and toxicity of prednisone therapy given on alternate days
malities may develop many months before evidence of and of other treatment strategies for patients with mem-
clinical renal involvement and should prompt close obser- branous lupus nephropathy (27).
vation to detect changes in urinary sediment and protein Patients with diffuse proliferative or severe focal prolif-
excretion rate, which are frequently considered stronger erative glomerulonephritis are candidates for vigorous im-
indications for modifications of therapy. munosuppressive treatments intended to control intrare-
Standard kidney function variables (such as serum cre- nal inflammation. In some cases, this control can be
atinine level and creatinine clearance) are insensitive in- achieved by using daily, high-dose prednisone (1 mg/kg of
dicators of change in glomerular filtration rate and are body weight daily) for approximately 2 months and then
likely to underestimate the severity of glomerulonephritis tapering the dose to reduce the risk for glucocorticoid-
(14). More accurate assessments of glomerular filtration associated toxicities. The systemic effects of glucocorti-
rate are obtained by using inulin or iothalamate clear- coids are well recognized. High-dose glucocorticoids may
ances or by using creatinine clearance after blocking tu- promote glomerular scarring by augmenting glomerular
bular secretion of creatinine by cimetidine (15). Nonethe- capillary perfusion pressures (28) and by elevating low-
less, even these measures of kidney function may fail to density lipoprotein (LDL) cholesterol levels, leading both
detect the extent of renal parenchymal injury because of to enhanced mesangial cell uptake of oxidized LDL cho-
intrarenal hemodynamic compensatory mechanisms that lesterol and to cellular injury (29).
have been shown in animal models to augment filtration Pulse intravenous methylprednisolone has been used as
in perfused glomeruli (16). an intensive initial therapy for patients with lupus nephri-
15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12 941
theless, it has been recognized that intravenous pulse
cyclophosphamide treatments are complicated, costly, in-
convenient, uncomfortable, and potentially toxic.
Given these concerns, additional studies have been
done to address several questions. First, could an initial
intensive immunosuppressive regimen shorten the dura-
tion of treatment? Second, is there an advantage to sus-
tained immunosuppressive therapy for lupus nephritis?
And third, what are the long-term toxicities of intermit-
tent pulse cyclophosphamide therapy?
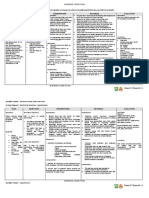
According to a recent study (39), exacerbations of ac-
tive renal and extrarenal disease are significantly more
likely to occur in patients receiving an intensive 6-month
course of pulse cyclophosphamide than in those receiving
a more sustained 30-month course (Figure 1). However,
pulse cyclophosphamide therapy may be associated with
substantial side effects. The risk for fatal opportunistic
infections of the pulmonary and central nervous systems
among patients with active systemic lupus erythematosus
treated with high-dose corticosteroids, cytotoxic drugs, or
both has been emphasized (40). Bladder cancer has been
seen in patients treated with daily oral cyclophosphamide
but has not been seen in our patients with lupus receiving
pulse cyclophosphamide therapy (35, 39), presumably be-
cause of the protective effects of hydration, a dilute di-
uresis, and mesna (2-mercaptoethanesulfonate). Hemato-
logic malignancies have been reported infrequently after
intravenous cyclophosphamide therapy for lupus nephritis
(41, 42). A large, multicenter study is needed to deter-
mine the effect of pulse cyclophosphamide therapy on the
risk for malignancy in patients with systemic lupus ery-
thematosus. Sustained amenorrhea was seen in 11 of 39
Figure 1. Treatment of severe lupus nephritis. Top. Probability of
not doubling serum creatinine levels in 65 patients with severe women younger than 40 years of age who were treated
active lupus nephritis randomly assigned to receive MP (intrave- with pulse cyclophosphamide therapy for systemic lupus
nous methylprednisolone, 1.0 g/m2 body surface area monthly for erythematosus (43). The risk for sustained amenorrhea is
6 months), CY-S (intravenous cyclophosphamide, 0.5 to 1.0 g/m2 significantly related to both the patient's age at the start
monthly for 6 months), or CY-L (intravenous cyclophosphamide, of pulse therapy and the number of doses of cyclophos-
0.5 to 1.0 g/m2 monthly for 6 months followed by quarterly
infusions for 24 months) (Gehan test comparing CY-L with MP, phamide received. These data, coupled with observations
P = 0.037). Bottom. Probability of no exacerbation of lupus about the risk for relapse after a short course of pulse
activity on completion of monthly pulses in groups randomly cyclophosphamide, pose a challenging problem. Recurring
assigned to receive CY-L and CY-S (Gehan test, P = 0.006). inflammation may result in sclerosing lesions that increase
Numbers of patients that remain at risk at various times are the risk for progressive renal failure during subsequent
shown along the abscissa. Reproduced with permission from
Boumpas and colleagues (39). episodes of active nephritis. A marked improvement in
renal status (resolution of initial elevations in serum cre-
atinine levels, low-grade proteinuria, and resolution of a
tis and other immune-mediated disorders. Favorable nephritic urinary sediment) favor a shortened course of
short-term results have been observed (19, 30), but this cytotoxic drug therapy (24). On the other hand, there is
therapy has been less extensively studied as a mainte- concern that discontinuing immunosuppressive therapy as
nance therapy for chronic disorders such as lupus nephri- soon as renal status is improved may increase the risk for
tis (31). The effectiveness and toxicity of daily high-dose relapse. Consequently, it has been recommended that pa-
oral prednisone and pulse intravenous methylpred- tients should receive quarterly pulse cyclophosphamide as
nisolone therapy have not been rigorously compared in maintenance therapy for approximately 1 year after
patients with lupus nephritis. achieving clinical renal remission, but this approach has
never been rigorously tested.
Cytotoxic Drugs
Immunosuppressive drug regimens that include cyto- Alternatives to this regimen of pulse cyclophosphamide
toxic drugs are more efficacious than prednisone alone in therapy are currently under investigation at the National
controlling clinical signs of active nephritis (32, 33), in Institutes of Health and other centers (44). That more
preventing renal scarring (34), and ultimately in reducing consistent and rapid responses could be achieved by com-
the risk for end-stage renal failure, but they have not bining pulse cyclophosphamide and pulse methylpred-
been shown to be more effective in reducing the risk for nisolone therapies or by synchronizing pulse cyclophos-
death (35, 36). Among cytotoxic drug regimens, intermit- phamide therapy and plasmapheresis has been suggested
tent pulse cyclophosphamide therapy appears to have one (45). Plasmapheresis appears not to enhance the effec-
of the most favorable therapeutic indexes (35-38). None- tiveness of prednisone and daily oral cyclophosphamide
942 15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12
(46). Other experimental immunosuppressive regimens, Table 2. Major Neuropsychiatric Manifestations of Sys-
including total lymphoid irradiation (47) and cyclosporine temic Lupus Erythematosus*
(48, 49), have been described but have not been prospec-
tively compared with other options. There is particular Diffuse cerebral dysfunction
Organic brain syndrome (20%)
interest in the development of more targeted treatments Psychosis (10%)
involving monoclonal antibodies and biologic-response Major affective disorder (< 1%)
modifiers; these are emerging as products of basic re- Focal cerebral dysfunction
search (50, 51). Seizures, all types (15%)
Cerebrovascular accidents (5%)
Transverse myelitis (1%)
Neuropsychiatric Disease Movement disorder
Chorea (3%)
Neuropsychiatric symptoms are common in patients Athetosis (rare)
with systemic lupus erythematosus and can be separated Parkinson-like (rare)
Cerebellar ataxia (rare)
into primary events, which result directly from immune- Peripheral neuropathy
mediated injury to the central nervous system, and sec- Symmetric sensorimotor (10%)
ondary events, which result from disease in other organs, Mononeuritis multiplex (rare)
complications of therapy, or both (Table 1) (52-55). Pri- Guillain-Barre syndrome (extremely rare)
mary neuropsychiatric events (neuropsychiatric lupus) typ- Autonomic neuropathy (extremely rare)
Miscellaneous
ically occur in a setting of clinical or serologic evidence of Aseptic meningitis (rare)
active systemic lupus erythematosus. Although relatively Pseudotumor cerebri (rare)
uncommon, systemic lupus erythematosus may first Cerebral venous thrombosis (extremely rare)
present with neurologic disease and should be included in
* Adapted from references 52-55. Numbers in parentheses indicate
the differential diagnosis of neuropsychiatric symptoms, approximate prevalence.
especially when these occur in young patients (54).
Pathogenesis many neuropsychiatric manifestations of systemic lupus
Multifocal cerebral cortical microinfarctions associated erythematosus; the organic brain syndrome has received
with microvascular injury are the predominant histopatho- increased attention in recent years and is discussed here
logic abnormalities attributed to neuropsychiatric lupus; briefly.
vasculitis is rare (56). The leading hypothesis about the
pathogenesis of neuropsychiatric lupus invokes vascular Organic Brain Syndrome
occlusion because of vasculopathy, vasculitis (in rare cas- This syndrome usually manifests with various degrees of
es), leukoagglutination or thrombosis, and antibody-medi- memory impairment, apathy, and loss of orientation, in-
ated neuronal cell injury or dysfunction. Antibodies may tellect or judgment, but agitation, delirium, stupor, or
be produced intrathecally or may gain access to the cen- coma may occur in severe cases. Symptomatic organic
tral nervous system from a blood-brain barrier disturbed brain syndrome has been reported in as many as 20% of
by the vascular injury (Table 1). patients with systemic lupus erythematosus (55). Limited
cognitive impairment has been reported in 20% to 70%
Clinical Presentation of these patients when examined using formal neuropsy-
chologic testing (55, 57) and may occur independently of
All parts of the nervous system (central, peripheral, or other manifestations of neuropsychiatric lupus or systemic
autonomic) may be involved (Table 2) (53). There are disease activity (58, 59). Slow but progressive deteriora-
tion may occur in a few patients and results in severe,
Table 1. Pathogenesis of Neuropsychiatric Events in Pa-
debilitating dementia. Dementia may be caused by active
tients with Systemic Lupus Erythematosus*
ongoing neuropsychiatric lupus or may result from previ-
Primary events ous insult to the central nervous system or from multiple
Vascular occlusion from immune-complex-mediated or infarctions caused by antiphospholipid antibodies (55, 60).
antibody (for example, antiphospholipid) -mediated
vasculopathy, vasculitis, leukoagglutination, or thrombosis.
Cerebral dysfunction from antibodies to brain tissue!
(antineuronal, antiribosomal P protein) or cytokines Diagnostic Studies
(interleukin-6, interferon-a).
Secondary events Analysis of the cerebrospinal fluid is one of the most
Infection (meningitis, abscess, discitis)
Cerebrovascular accidents due to accelerated atherosclerosis helpful diagnostic studies. Although elevated cell counts,
Hypertensive encephalopathy protein levels, or both are found in only about one third
Metabolic encephalopathy (uremia, electrolyte imbalance, of patients, analysis of the cerebrospinal fluid helps ex-
fever, hypoxia) clude acute or chronic infectious meningitis. Elevated in-
Hypercoagulable state due to the nephrotic syndrome
Drugs (glucocorticoids, nonsteroidal anti-inflammatory agents, trathecal IgG, IgM, or IgA indices (or a combination of
trimethoprim and sulfamethoxazole, hydroxychloroquine, these) and oligoclonal bands have been seen in patients
azathionrineV with diffuse neuropsychiatric disease but are not specific
to neuropsychiatric lupus (55). More specialized tests,
* Adapted from references 52-55.
t Intrathecal production or entrance through a blood-brain barrier dis- such as measurements of interleukin-6 and interferon-a,
turbed by vascular injury. are not readily available in most places (54).
15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12 943
features, including cerebrovascular accidents, multi-infarc-
tion dementia, seizures, intracranial arterial and venous
thrombosis, chorea, and acute transverse myelitis (60, 65).
With the exception of cerebrovascular accidents, the as-
sociation between these syndromes and antiphospholipid
antibodies has not been firmly established.
Neuroimaging Studies
Magnetic resonance imaging shows greater contrast and
detail than computed tomography, but it also shows more
clinically silent abnormalities and incidental findings (66).
Computed tomography is sufficient for the initial diagno-
Figure 2. Magnetic resonance imaging in neuropsychiatric lupus. sis of most mass lesions and of intracranial hemorrhage
Left. Axial T2-weighted scan of the brain in a woman 24 years of demanding immediate intervention, and it requires less
age with systemic lupus erythematosus. Small foci of increased patient cooperation than magnetic resonance imaging (67).
signal intensity are identified at the periventricular area of the The findings of magnetic resonance imaging in neuro-
white matter (arrows). These lesions are caused by microvascular
injury in the peripheral branches of the cerebral arteries resulting psychiatric lupus reflect the underlying histopathologic
in ischemia, edema, and infarction. If the underlying process findings of vascular injury and may involve the white
persists, these lesions may increase in number and coalesce, or gray matter of the brain parenchyma (Figure 2). In
forming larger lesions. In contrast to the smaller lesions, these general, patients with focal neurologic findings or focal
larger lesions may also be detected as hypodense areas on com-
puted tomographic scans. Right. Axial T2-weighted scan shows seizures are more likely than patients with diffuse involve-
increased signal intensity in the gray matter of the left basal ment to have abnormalities detected by magnetic reso-
ganglia. Abnormalities of the cortical or the deep gray matter are nance imaging. In most cases, this imaging cannot distin-
usually due to involvement of more proximal branches of the guish between primary and secondary neuropsychiatric
cerebral arteries, resulting in edema with high-signal intensity on
T2-weighted and proton density images. These lesions may re- events. It is also impossible to establish a diagnosis of
solve spontaneously or with therapy or may progress to infarc- neuropsychiatric lupus from neuroimaging studies in the
tion, in which case they may also be detected by computed absence of clinical history. Furthermore, in many cases,
tomographic scanning. In this patient, similar lesions were also the correlation between magnetic resonance imaging find-
seen in the left cerebral peduncle and in the cervical spinal cord. ings and clinical presentation is poor. For example, inter-
After treatment with oral glucocorticoids and pulses of cyclo-
phosphamide, these lesions resolved within approximately 6 pretation of white matter abnormalities (which are often
months (Reproduced with permission from Boumpas and col- clinically silent) is problematic because their prevalence in
leagues [71]). patients with nonsystemic lupus erythematosus increases
from 20% in persons younger than 50 years of age to
90% in persons older than 70 years of age (66).
Autoantibodies Single-photon emission computed tomography has been
Antineuronal antibodies are present in the serum of as used by several investigators to show a higher prevalence
many as 75% of patients with systemic lupus erythemato- of abnormal cortical perfusion in patients with neuropsy-
sus and neuropsychiatric lupus (53). Similarly, antiriboso- chiatric lupus than in patients with systemic lupus ery-
mal P protein antibodies have been found in 45% to 90% thematosus and no neuropsychiatric symptoms (68). Un-
of patients with systemic lupus erythematosus and psycho- fortunately, quantitative, rigorous assessments of the
sis or major depression in most (61), but not all (62), clinical utilities of magnetic resonance imaging and single-
studies. These autoantibodies may be found in as many as photon emission computed tomography have not been
25% of unselected patients with systemic lupus erythem- done in large case series or well-controlled comparison
atosus, and thus their presence must be interpreted with trials. Furthermore, data on the diagnostic accuracy of,
caution (55). Antineuronal antibodies and antiribosomal the diagnostic and therapeutic effect of, and the change in
P protein antibodies are more likely to be seen in patients patient outcomes attributable to these tests are not avail-
with diffuse rather than focal central nervous system in- able (66, 69).
volvement. This suggests that the former may be autoan-
tibody mediated (53, 55).
The specific antigens that induce the antineuronal an- Management
tibodies are beginning to be identified. Hanson and col-
leagues (63) described a 50-kd antigen in the plasma Therapy for neuropsychiatric lupus differs according to
membrane of brain synaptic terminals (neuronal compart- the type of presentation, its severity, and the nature of the
ments vital for normal brain function) that bound anti- underlying process (for example, inflammatory or throm-
bodies present in the sera of 19 of 20 patients with botic). Unfortunately, decisions about immunosuppressive
neuropsychiatric lupus. Antiribosomal P protein antibod- therapy must currently be made in the absence of data
ies were initially found to be directed to cytoplasmic from randomized controlled studies (54). Glucocorticoids
(ribosomal) proteins. More recently, however, reactive P remain the first line of therapy for the major manifesta-
peptides have also been found on the cell surface; this tions of neuropsychiatric lupus. In patients with severe
suggests that these autoantibodies may directly affect the disease or in those who do not respond to standard
function and viability of cells that express this antigenic prednisone therapy, pulse methylprednisolone therapy
target (64). In case-control studies, anticardiolipin anti- may be helpful. Small case series (45, 70-72) have shown
bodies have been associated with specific neuropsychiatric intravenous pulses of cyclophosphamide to be useful in
944 15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12
patients with very severe disease (for example, those with Table 3. Primary Respiratory System Involvement In Sys-
strokes, cerebritis, acute transverse myelitis, and coma), in temic Lupus Erythematosus*
those who fail to respond to glucocorticoids, and in those
who relapse while glucocorticoid therapy is being tapered. Upper airway disease
Epiglottitis
Plasmapheresis and intravenous immunoglobulin have Subglottic stenosis
also been proposed as adjunct therapies for life-threaten- Vocal cord paralysis
ing neuropsychiatric lupus, but only on the basis of case Laryngeal edema or ulceration
reports. In patients with thrombosis of intracerebral ves- Inflammatory mass lesions or nodules
sels (for example, cerebral vein thrombosis), and in the Cricoarytenoid arthritis
Necrotizing vasculitis
absence of generalized lupus activity or high-grade cere- Parenchymal disease
brospinal fluid abnormalities, therapy should be based Acute lupus pneumonitis
predominantly on anticoagulation (54). The role of im- Alveolar hemorrhage syndrome
munosuppressive therapy in these cases is not clear. Chronic lupus pneumonitis or interstitial lung disease
Lymphocytic interstitial pneumonia or pseudolymphoma
Bronchiolitis obliterans with or without organizing pneumonia
Cardiac Disease Respiratory muscle disease
Shrinking lung syndrome
Cardiovascular involvement has been receiving in- Pleural disease
creased attention in patients with systemic lupus erythem- Pleuritis with or without effusion
Vascular disease
atosus. Recent prospective studies using advanced diag- Pulmonary hypertension
nostic methods have allowed the delineation of the Pulmonary embolism
prevalence and significance of discrete cardiac manifesta- Acute reversible hypoxemia
tions such as valvular disease, myocardial dysfunction, and
* Adapted from references 93-98.
pericardial disease (73-77). In other studies (78, 79), cor-
onary artery disease has been found to have a substantial
effect on mortality and morbidity in patients with systemic 88); this has led to speculation about a possible causal
lupus erythematosus; it accounts for as many as one third relation (80). However, valvular abnormalities are also
of all deaths seen in this population (78, 79). seen in patients with systemic lupus erythematosus who
lack antiphospholipid antibodies; this suggests that addi-
Valvular Heart Disease tional pathogenetic factors may be operative in the devel-
opment of endocardial lesions in patients with systemic
The spectrum of lupus-related valvulopathies has been lupus erythematosus (76, 89).
expanded to include valve leaflet thickening with or with-
out valve dysfunction (regurgitation or stenosis) in addi-
tion to the more characteristic valve lesions of Libman- Accelerated Atherosclerosis
Sacks endocarditis (nonbacterial verrucous endocarditis) Atherosclerosis is emerging as a significant cause of
(73). The prevalence of lupus-associated valvulopathy death and illness in patients with systemic lupus erythem-
ranges from 18% to 74% depending on the cohort of atosus. The mortality rate from coronary artery disease in
patients studied, the duration of the disease, and the patients with systemic lupus erythematosus is estimated to
mode of diagnosis (for example, autopsy studies or trans- be ninefold greater than predicted population-based rates
thoracic or transesophageal echocardiography) (73, 76, (90). Severe atherosclerotic narrowing of coronary arter-
80). Valvular abnormalities may progress to hemodynam- ies has been well documented on autopsy studies, even in
ically significant lesions that require valve replacement patients younger than 35 years of age.
(73, 81). Furthermore, an increased risk for infectious Although the pathogenesis of accelerated atherosclero-
endocarditis has been reported in retrospective reviews of sis is unknown, it is believed to be multifactorial. Tradi-
patients with systemic lupus erythematosus (82, 83). Be- tional cardiac risk factors, such as hypertension, obesity,
cause valvular lesions (such as Libman-Sacks endocardi- and hyperlipidemia, are observed with high frequency in
tis) may be overlooked by echocardiography and do not patients with systemic lupus erythematosus. Fifty-three
necessarily correlate with physical examination findings, percent of these patients have three or more risk factors;
some have suggested that antibiotic prophylaxis be con- this prevalence greatly exceeds the prevalence seen in a
sidered for all patients with systemic lupus erythematosus matched population (78). Glucocorticoid-induced dysli-
having dental or surgical procedures (84, 85), but this poproteinemia (91) and complications that result from
recommendation has not been widely accepted. disease involvement in other organ systems (for example,
The pathogenesis of valvular heart disease in systemic renal disease leading to hypertension and hyperlipidemia)
lupus erythematosus is unknown, but contributing factors may also potentiate the atherosclerotic process. Circulat-
may include verrucous vegetations, fibrinoid degeneration ing immune complexes may promote intracellular choles-
of valve cusps, valvulitis, fibrotic scarring (possibly wors- terol accumulation and therefore may be an additional
ened by glucocorticoids), vasculitis, or rupture of chorda compounding factor (92).
tendineae (81). The relation between antiphospholipid
antibodies and the development of cardiac valvular ab-
Pulmonary Disease
normalities is controversial. Valvular lesions have been
seen with increased frequency in patients with the primary The involvement of the respiratory system in systemic
antiphospholipid syndrome and in patients with systemic lupus erythematosus is relatively common, and its clinical
lupus erythematosus and antiphospholipid antibodies (86- manifestations are diverse (Table 3). Primary pulmonary
15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12 945
are high, ranging from 50% to 90% despite treatment (93,
102). However, a recent case series of patients with sys-
temic lupus erythematosus and pulmonary hemorrhage
suggested that the prognosis for these patients may not be
as grim as was previously thought and that early diagnosis
combined with aggressive immunosuppression may favor-
ably affect survival rates (102).
Acute Reversible Hypoxemia
A newly described syndrome of acute reversible hypox-
emia has been reported in a subpopulation of acutely ill
patients with systemic lupus erythematosus (94). The ex-
act pathogenesis of this syndrome is unclear. It has been
postulated that the elevated levels of complement split
products detected in the plasma of these patients may
activate circulating neutrophils, which aggregate within
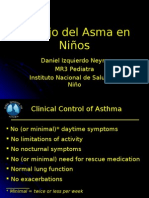
Figure 3. Computed tomographic scan of the lung in a patient the pulmonary vasculature, and partly account for the
with systemic lupus erythematosus and interstitial pneumonia.
This patient presented with several weeks of dry cough and observed diminished oxygenation capacity. In this series,
dyspnea on exertion. Note the bilateral ground-glass opacities hypoxemia resolved and the level of complement split
that do not obscure underlying vessels (6-mm axial section products decreased after treatment with glucocorticoids
through lung bases). Open lung biopsy showed lymphocytic in- for extrapulmonary disease manifestations.
terstitial pneumonia with numerous germinal centers situated
adjacent to bronchial epithelium and a less prominent inflamma-
tory background of lymphocytes and plasma cells within the Chronic Pulmonary Disease
alveolar septae. These abnormalities resolved after therapy with
high-dose glucocorticoids. Interstitial Lung Disease
Chronic interstitial lung disease may develop as a con-
sequence of acute pneumonitis or as an independent
involvement caused by systemic lupus erythematosus may manifestation of systemic lupus erythematosus (99, 103).
follow a variable course from incidental abnormalities Radiographic findings of interstitial lung disease may be
noted on chest radiography or pulmonary function testing more common than symptoms. Discriminating between
to acute or chronic disease. Acute pulmonary disease inflammatory alveolitis (which is treatable) and chronic
tends to develop in association with generalized lupus fibrosis is the primary difficulty in determining the appro-
activity, whereas chronic pulmonary involvement may priate therapeutic approach to chronic lupus pneumonitis.
progress independently of disease activity in other organs. Bronchoalveolar lavage and gallium scanning were used
to evaluate interstitial lung disease in the past, but their
correlation with disease activity or potential therapeutic
Acute Pulmonary Disease response has been questioned. High-resolution computed
Acute Lupus Pneumonitis and Alveolar Hemorrhage tomography is emerging as an important noninvasive tool
Alveolar hemorrhage and acute lupus pneumonitis are in the evaluation of idiopathic pulmonary fibrosis because
uncommon, life-threatening syndromes associated with high-resolution computed tomographic patterns (such as a
systemic lupus erythematosus; they result from acute in- ground-glass appearance that suggests active inflammation
jury to the alveolar-capillary unit (99). Acute lupus pneu- or a reticular pattern with honeycombing that suggests
monitis is characterized by the abrupt onset of fevers, irreversible fibrosis) have been shown to correlate with
dyspnea with hypoxemia, and patchy alveolar infiltrates on histologic findings on open lung biopsy and with response
chest radiography, without evidence of an underlying in- to therapy (104-106) (Figure 3). Although this has not
fection. The alveolar hemorrhage syndrome, which is less been critically examined in interstitial lung disease asso-
common than acute lupus pneumonitis, has a similar pre- ciated with systemic lupus erythematosus, high-resolution
sentation, except that it is associated with an acute de- computed tomographic scans with a pattern that suggests
cline in hemoglobin levels caused by bleeding within the chronic fibrosis may help to avoid unnecessary immuno-
lung (99). suppression.
Although they have not been the subject of prospective
controlled studies, glucocorticoids are generally accepted Pulmonary Hypertension
as the first line of therapy for acute immune-mediated Increasingly recognized as a complication of systemic
lung injury in patients with systemic lupus erythematosus. lupus erythematosus, pulmonary hypertension in this con-
Pulse methylprednisolone therapy seems to be effective in dition closely resembles primary idiopathic pulmonary hy-
treating various immune-mediated pulmonary hemorrhage pertension. The Raynaud phenomenon has been seen in
syndromes (100). The addition of azathioprine or cyclo- as many as 75% of patients with systemic lupus erythem-
phosphamide is generally advocated in patients who are atosus and pulmonary hypertension and in only 25% of
critically ill or unresponsive to glucocorticoids (101). Plas- the general population with systemic lupus erythematosus
mapheresis as an adjunct to immunosuppressive therapy (107). Serologic testing shows a high incidence of antiri-
has been used in rapidly deteriorating patients (45). Ther- bonucleoprotein antibodies, rheumatoid factor, and an-
apy must be initiated expeditiously because these syn- tiphospholipid antibodies (107). The pathogenesis of pul-
dromes can accelerate rapidly, leading to respiratory fail- monary hypertension associated with systemic lupus
ure and death. Overall mortality rates for both syndromes erythematosus is unknown, but the condition is believed
946 15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12
to result from vascular occlusion caused by vasoconstric- aggressive and severe disease and has a substantial nega-
tion, vasculopathy or vasculitis, platelet aggregation or tive effect on the prognosis of systemic lupus erythema-
thrombosis, and parenchymal lung disease (93, 107, 108). tosus (79).
Currently, no therapy has been proved efficacious for the
treatment of pulmonary hypertension associated with ei- Treatment
ther idiopathic or systemic lupus erythematosus. Prognosis
is poor, and a steady decline in pulmonary function, de- Randomized controlled studies of therapy for autoim-
spite treatment, is usual (109). Although it has been little mune thrombocytopenia are not available, and treatment
studied, heart-lung transplantation may be an option in is based on extrapolation from studies of patients with
patients with systemic lupus erythematosus, advanced pul- idiopathic thrombocytopenic purpura and small case se-
monary hypertension, and minimal disease activity in ries in patients with systemic lupus erythematosus. Ther-
other organs (109, 110). apy is aimed at attaining a complete and lasting response.
If this is unsuccessful, subsequent therapy should be di-
rected toward maintaining "safe" platelet counts (20 X
Hematologic Disease: Autoimmune Thrombocytopenia 109/L) (117). Therapy may not be necessary in patients
Autoimmune thrombocytopenia occurs in as many as with no evidence of systemic lupus erythematosus activity
25% of patients with systemic lupus erythematosus, and it in other organs, a platelet count of more than 20 to 30 X
may be severe (platelet count less than 20 X 109/L) in 109/L, and no evidence of coexisting coagulopathy or
approximately 5% of these patients. A positive test result platelet dysfunction. For all other patients, glucocorticoids
for antinuclear antibodies has been reported to occur in are usually recommended as initial treatment. A random-
as many as 30% of patients with chronic idiopathic ized clinical trial in children and adults with acute idio-
thrombocytopenic purpura, and this may present diagnos- pathic thrombocytopenic purpura showed similar efficacy
tic and therapeutic problems (111). The presence of high- for low-dose (0.25 mg/kg daily) and high-dose (1.0 mg/kg
titer antinuclear antibodies in combination with antibod- daily) glucocorticoids (prednisone or prednisolone) (119).
ies to extractable nuclear antigens (for example, Ro/SS-A, Patients who fail glucocorticoid therapy or relapse during
La/SS-B, ribonucleoprotein, or Smith) or anti-double- tapering may benefit from splenectomy, danazol, intrave-
stranded DNA antibodies increases the likelihood that nous immunoglobulin, vinca alkaloids, or intermittent
additional manifestations of systemic lupus erythematosus pulses of methylprednisolone, dexamethasone, or cyclo-
will develop at some future date (112). phosphamide (111, 120-123). Pulse cyclophosphamide
therapy is particularly attractive in patients with attendant
involvement of other organs (such as the kidneys, the
Pathogenesis and Clinical Presentation central nervous system, and the lungs) (123). For patients
Elevated platelet-associated IgG is found in patients with severe refractory idiopathic thrombocytopenic pur-
with systemic lupus erythematosus with and without pura, combination chemotherapy with cyclophosphamide
thrombocytopenia. It is not clear whether this indicates and prednisone combined with either vincristine, vincris-
platelet-specific antibody or adsorbed immune complexes tine and procarbazine, or etoposide has been reported to
(111). Antiplatelet autoantibodies bind to one or more be beneficial in a case series of 10 patients (124).
surface glycoproteins (usually the glycoprotein Ilb-IIIa Acknowledgments: The authors thank Drs. John L. Decker, Alfred D.
complex). The antibody-coated platelets are ingested by Steinberg, and Paul H. Plotz for their leadership in planning and imple-
macrophages of the spleen, liver, lymph nodes, and bone menting studies of systemic lupus erythematosus at the National Institutes
of Health; Dr. Nicholas J. Patronas for invaluable assistance and useful
marrow, which carry receptors for the Fc region of im- comments in the discussion of neuroimaging studies in patients with sys-
munoglobulin. Phagocytosis is more efficient when the temic lupus erythematosus; Dr. Catherine K. Chow for useful discussions
antiplatelet antibodies belong to the IgGx and IgG 2 sub- on the role of computed tomography in the diagnosis of pulmonary
disease; Drs. W. Travis and C.L. Phillips for their assistance with the
types (113). Antibodies to specific target antigens (other interpretation of the pathology of Figure 3; and Ms. Lisa A. Miller and
than the glycoprotein Ilb-IIIa complex) on platelets of Mr. Andrew S. Lerner for manuscript preparation.
patients with systemic lupus erythematosus and thrombo- Requests for Reprints: Dimitrios T. Boumpas, MD, National Institutes of
cytopenia have also been described (114). Several studies Health, Building 10, Room 3N-112, Bethesda, MD 20892.
have documented an association between the develop- Current Author Addresses: Drs. Boumpas, Austin, and Fessler: National
ment of thrombocytopenia and the presence of antiphos- Institutes of Health, Building 10, Room 3N-112, Bethesda, MD 20892-
pholipid antibodies (115). Other case reports (116) have 1268.
Dr. Balow: National Institutes of Health, Building 10, Room 9N-222,
suggested an association between systemic lupus erythem- Bethesda, MD 20892-1818.
atosus and a syndrome similar to thrombotic thrombocy- Dr. Klippel: National Institutes of Health, Building 10, Room 9S-205,
topenic purpura. It is difficult to differentiate between Bethesda, MD 20892-1828.
Dr. Lockshin: National Institutes of Health, Building 31, Room 4C-32,
thrombotic thrombocytopenic purpura and the cata- Bethesda, MD 20892-2350.
strophic occlusion syndrome in patients with antiphospho-
lipid antibody. Patients with thrombocytopenia are at in-
References
creased risk for bleeding either spontaneously or after 1. Tan EM. Foreword. In: Lahita RG, ed. Systemic Lupus Erythema-
trauma. Spontaneous bleeding is rare unless the platelet tosus. New York: Churchill Livingstone; 1992:xv-i.
count is less than 5 X 109/L, an associated congenital or 2. Golbus J, McCune WJ. Lupus nephritis. Classification, prognosis,
immunopathogenesis, and treatment. Rheum Dis Clin North Am.
acquired defect in platelet function is present, or a co- 1994;20:213-42.
agulopathy is present (117, 118). Although thrombocyto- 3. Hahn BH, Tsao BP. Antibodies to DNA. In: Wallace DJ, Hahn BH,
penia rarely causes a fatal hemorrhage in patients with eds. Dubois' Lupus Erythematosus. 4th ed. Philadelphia: Lea &
Febiger; 1993:195-201.
systemic lupus erythematosus, it may be a marker of more 4. Foster MH, Cizman B, Madaio MP. Nephritogenic autoantibodies in
15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12 947
systemic lupus erythematosus: immunochemical properties, mecha- 31. Harisdangkul V, Rockhold L, Myers A. Lupus nephritis: efficacy of
nisms of immune deposition, and genetic origins. Lab Invest. 1993; monthly pulse therapy with intravenous methylprednisolone. South
69:494-507. Med J. 1989;82:321-7.
5. Couser WG. Pathogenesis of glomerulonephritis. Kidney Int Suppl. 32. Donadio JV Jr, Holley KE, Ferguson RH, Ilstrup DM. Treatment of
1993;42:S19-26. diffuse proliferative lupus nephritis with prednisone and combined
6. Vlahakos D, Foster MH, Ucci AA, Barrett KJ, Datta SK, Madaio prednisone and cyclophosphamide. N Engl J Med. 1978;299:1151-5.
MP. Murine monoclonal anti-DNA antibodies penetrate cells, bind to 33. Dinant HJ, Decker JL, Klippel JH, Balow JE, Plotz PH, Steinberg
nuclei, and induce glomerular proliferation and proteinuria in vivo. AD. Alternative modes of cyclophosphamide and azathioprine ther-
J Am Soc Nephrol. 1992;2:1345-54. apy in lupus nephritis. Ann Intern Med. 1982;96:728-36.
7. Termaat RM, Assmann KJ, Dijkman HB, van Gompel F, Smeenk 34. Balow JE, Austin HA 3d, Muenz LR, Joyce KM, Antonovych TT,
RJ, Berden JH. Anti-DNA antibodies can bind to the glomerulus via Klippel JH, et al. Effect of treatment on the evolution of renal
two distinct mechansisms. Kidney Int. 1992;42:1363-71. abnormalities in lupus nephritis. N Engl J Med. 1984;311:491-5.
8. Kerjaschki D. The pathogenesis of membranous glomerulonephritis: 35. Austin HA 3d, Klippel JH, Balow JE, le Riche NG, Steinberg AD,
from morphology to molecules. Virchows Archiv B Cell Pathol Incl Plotz PH, et al. Therapy of lupus nephritis. Controlled trial of pred-
Mol Pathol. 1990;58:253-71. nisone and cytotoxic drugs. N Engl J Med. 1986;314:614-9.
9. Hill GS, Hinglais N, Tron F, Bach JF. Systemic lupus erythematosus. 36. Steinberg AD, Steinberg SC. Long-term preservation of renal func-
Morphologic correlations with immunologic and clinical data at the tion in patients with lupus nephritis receiving treatment that includes
time of biopsy. Am J Med. 1978;64:61-79. cyclophosphamide versus those treated with prednisone only. Arthri-
10. Pillemer SR, Austin HA 3d, Tsokos GC, Balow JE. Lupus nephritis: tis Rheum. 1991;34:945-50.
association between serology and renal biopsy measures. J Rheuma- 37. McCune WJ, Golbus J, Zeldes W, Bohlke P, Dunne R, Fox DA.
tol. 1988;15:284-8. Clinical and immunologic effects of monthly administration of intra-
11. Appel AE, Sablay LB, Golden RA, Barland P, Grayzel AI, Bank N. venous cyclophosphamide in severe systemic lupus erythematosus.
The effect of normalization of serum complement and anti-DNA N Engl J Med. 1988;318:1423-31.
'antibody on the course of lupus nephritis: a two year prospective 38. Lehman TJ, Sherry DD, Wagner-Weiner L, McCurdy DK, Emery
study. Am J Med. 1978;64:274-83. HM, Magilavy DB, et al. Intermittent intravenous cyclophosphamide
12. Laitman RS, Glicklich D, Sablay LB, Grayzel AI, Barland P, Bank therapy for lupus nephritis. J Pediatr. 1989;114:1055-60.
N. Effect of long-term normalization of serum complement levels on
39. Boumpas DT, Austin HA 3d, Vaughan EM, Klippel JH, Steinberg
the course of lupus nephritis. Am J Med. 1989;87:132-8.
AD, Yarboro CH, et al. Controlled trial of pulse methylprednisolone
13. Garin EH, Donnelly WH, Shulman ST, Fernandez R, Finton C, versus two regimens of pulse cyclophosphamide in severe lupus ne-
Williams RL, et al. The significance of serial measurements of serum
phritis. Lancet. 1992;340:741-5.
complement C3 and C4 components and DNA binding capacity in
patients with lupus nephritis. Clin Nephrol. 1979;12:148-55. 40. Hellmann DB, Petri M, Whiting-O'Keefe Q. Fatal infections in sys-
14. Shemesh O, Golbetz H, Kriss JP, Myers BD. Limitations of creati- temic lupus erythematosus: the role of opportunistic organisms. Med-
nine as a filtration marker in glomerulopathic patients. Kidney Int. icine (Baltimore). 1987;66:341-8.
1985;28:830-8. 41. Gibbons RB, Westerman E. Acute nonlymphocytic leukemia follow-
15. Roubenoff R, Drew H, Moyer M, Petri M, Whiting-O'Keefe Q, Hell- ing short-term, intermittent, intravenous cyclophosphamide treatment
mann DB. Oral cimetidine improves the accuracy and precision of of lupus nephritis. Arthritis Rheum. 1988;31:1552-4.
creatinine clearance in lupus nephritis. Ann Intern Med. 1990;113: 42. Vasquez S, Kavanaugh AF, Schneider NR, Wacholtz MC, Lipsky PE.
501-6. Acute nonlymphocytic leukemia after treatment of systemic lupus
16. Wilson CB, Blantz RC. Nephroimmunopathology and pathophysiol- erythematosus with immunosuppressive agents. J Rheumatol. 1992;
ogy. Am J Physiol. 1985;248:F319-31. 19:1625-7.
17. Ginzler EM, Felson DT, Anthony JM, Anderson JJ. Hypertension 43. Boumpas DT, Austin HA 3d, Vaughan EM, Yarboro CH, Klippel JH,
increases the risk of renal deterioration in systemic lupus erythema- Balow JE. Risk for sustained amenorrhea in patients with systemic
tosus. J Rheumatol. 1993;20:1694-700. lupus erythematosus receiving intermittent pulse cyclophosphamide
18. Esdaile JM, Levinton C, Federgreen W, Hayslett JP, Kashgarian M. therapy. Ann Intern Med. 1993;119:366-9.
The clinical and renal biopsy predictors of long-term outcome in 44. Houssiau FA, D'Cruz DP, Haga HJ, Hughes GR. Short course of
lupus nephritis: a study of 87 patients and review of the literature. weekly low-dose intravenous pulse cyclophosphamide in the treat-
Q J Med. 1989;72:779-833. ment of lupus nephritis: a preliminary study. Lupus. 1991;1:31-5.
19. Kimberly RP, Lockshin MD, Sherman RL, McDougal JS, Inman RD, 45. Schroeder JO, Euler HH, Loffler H. Synchronization of plasmaphere-
Christian CL. High-dose intravenous methylprednisolone pulse ther- sis and pulse cyclophosphamide in severe systemic lupus erythema-
apy in systemic lupus erythematosus. Am J Med. 1981;70:817-24. tosus. Ann Intern Med. 1987;107:344-6.
20. Nossent HC, Henzen-Logmans SC, Vroom TM, Berden JH, Swaak 46. Lewis EJ, Hunsicker LG, Lan SP, Rohde RD, Lachin JM. A con-
TJ. Contribution of renal biopsy data in predicting outcome in lupus trolled trial of plasmapheresis therapy in severe lupus nephritis. The
nephritis. Analysis of 116 patients. Arthritis Rheum. 1990;33:970-7. Lupus Nephritis Collaborative Study Group. N Engl J Med. 1992;
21. Esdaile JM, Federgreen W, Quintal H, Suissa S, Hayslett JP, Kash- 326:1373-9.
garian M. Predictors of one year outcome in lupus nephritis: the 47. Strober S, Farinas MC, Field EH, Solovera JJ, Kiberd BA, Myers
importance of renal biopsy. Q J Med. 1991;81:907-18. BD, et al. Treatment of lupus nephritis with total lymphoid irradia-
22. Austin HA 3d, Boumpas DT, Vaughan EM, Balow JE. Predicting tion. Arthritis Rheum. 1988;31:850-8.
renal outcomes in severe lupus nephritis: contributions of clinical and 48. Favre H, Miescher PA, Huang YP, Chatelanat F, Mihatsch MJ.
histologic data. Kidney Int. 1994;45:544-50. Ciclosporin in the treatment of lupus nephritis. Am J Nephrol. 1989;
23. McLaughlin JR, Bombardier C, Farewell VT, Gladman DD, Urowitz 9(Suppl l):57-60.
MB. Kidney biopsy in systemic lupus erythematosus. III. Survival 49. Tokuda M, Kurata N, Mizoguchi A, Inoh M, Seto K, Kinashi M, et
analysis controlling for clinical and laboratory variables. Arthritis al. Effect of low-dose cyclosporin A on systemic lupus erythematosus
Rheum. 1994;37:559-67. disease activity. Arthritis Rheum. 1994;37:551-8.
24. Levey AS, Lan SP, Corwin HL, Kasinath BS, Lachin J, Neilson EG, 50. Wacholtz MC, Lipsky PE. Treatment of lupus nephritis with CD5
et al. Progression and remission of renal disease in the Lupus Ne- PLUS, an immunoconjugate of an anti-CD5 monoclonal antibody
phritis Collaborative Study. Results of treatment with prednisone and and ricin A chain. Arthritis Rheum. 1992;35:837-9.
short-term oral cyclophosphamide. Ann Intern Med. 1992;116:114-23. 51. Stafford FJ, Fleisher TA, Lee G, Austin HA 3d, Balow JE, Klippel
25. Whiting-O'Keefe Q, Henke JE, Shearn MA, Hopper J Jr, Biava CG, JH. A pilot study of anti-CD5 ricin A chain immunoconjugate in
Epstein WV. The information content from renal biopsy in systemic systemic lupus erythematosus. J Rheumatol. 1994;21:2068-70.
lupus erythematosus. Ann Intern Med. 1982;96:718-23. 52. McCune WJ, Golbus J. Neuropsychiatric lupus. Rheum Dis Clin
26. Magil AB, Puterman ML, Ballon HS, Chan V, Lirenman DS, Rae A, North Am. 1988;14:149-67.
et al. Prognostic factors in diffuse proliferative lupus glomerulone- 53. Bluestein HG. The central nervous system in systemic lupus erythem-
phritis. Kidney Int. 1988;34:511-7. atosus. In: Lahita RD, ed. Systemic Lupus Erythematosus. New
27. Austin HA 3d, Antonovych TT, MacKay K, Boumpas DT, Balow JE. York: Churchill Livingstone; 1992:639-55.
NIH conference. Membranous nephropathy. Ann Intern Med. 1992; 54. Boumpas DT, Scott D, Balow JE. Neuropsychiatric lupus: a case for
116:672-82. guarded optimism [Editorial]. J Rheumatol. 1993;20:1641-3.
28. Garcia DL, Rennke HG, Brenner BM, Anderson S. Chronic glucocor- 55. West SG. Neuropsychiatric lupus. Rheum Dis Clin North Am. 1994;
ticoid therapy amplifies glomerular injury in rats with renal ablation. 20:129-58.
J Clin Invest. 1987;80:867-74. 56. Hanly JG, Walsh NM, Sangaland V. Brain pathology in systemic
29. Coritsidis G, Rifici V, Gupta S, Rie J, Shan ZH, Neugarten J, et al. lupus erythematosus. J Rheumatol. 1992;15:732-41.
Preferential binding of oxidized LDL to rat glomeruli in vivo and 57. Ginsburg KS, Wright EA, Larson MG, Fossel AH, Albert M, Schur
cultured mesangial cells in vitro. Kidney Int. 1991;39:858-66. PH, et al. A controlled study of the prevalence of cognitive dysfunc-
30. Mackworth-Young CG, David J, Morgan SH, Hughes GR. A double tion in randomly selected patients with systemic lupus erythematosus.
blind, placebo controlled trial of intravenous methylprednisolone in Arthritis Rheum. 1992;35:776-82.
systemic lupus erythematosus. Ann Rheum Dis. 1988;47:496-502. 58. Hay EM, Black D, Huddy A, Creed F, Tomenson B, Bernstein RM,
948 15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12
et al. Psychiatric disorder and cognitive impairment in systemic lupus 83. Luce EB, Montgomery MT, Redding SW. The prevalence of cardiac
erythematosus. Arthritis Rheum. 1992;35:411-6. valvular pathosis in patients with systemic lupus erythematosus. Oral
59. Hanly JG, Fisk JD, Sherwood G, Jones E, Jones VJ, Eastwood B. Surg Oral Med Oral Pathol. 1990;70:590-2.
Cognitive impairment in patients with systemic lupus erythematosus. 84. Zysset MK, Montgomery MT, Redding SW, Dell'Italia LJ. Systemic
J Rheumatol. 1992;19:562-7. lupus erythematosus: A consideration for antimicrobial prophylaxis.
60. Asherson RA, Mercey D, Phillips G, Sheehan N, Gharavi AE, Harris Oral Surg Oral Med Oral Pathol. 1987;64:30-4.
EN, et al. Recurrent stroke and multi-infarct dementia in systemic 85. Mitchell SR, Cupps TR, Nashel DJ, Katz P. Valvulitis in systemic
lupus erythematosus: association with antiphospholipid antibodies. lupus erythematosus. Am J Med. 1989;86:510.
Ann Rheum Dis. 1987;46:605-11. 86. Khamashta MA, Cervera R, Asherson RA, et al. Association of
61. Schneebaum AB, Singleton JD, West SG, Blodgett JK, Allen LG, antibodies against phospholipids with heart valve disease in systemic
Cheronis JC, et al. Association of psychiatric manifestations with lupus erythematosus. Lancet. 1990;335:1541-4.
antibodies to ribosomal P proteins in systemic lupus erythematosus. 87. Leung WH, Wong KL, Lau CP, Wong CK, Liu HW. Association be-
Am J Med. 1991;90:54-62. tween antiphospholipid antibodies and cardiac abnormalities in patients
62. van Dam A, Nossent H, de Jong J, Meilof J, ter Borg EJ, Swaak T, with systemic lupus erythematosus. Am J Med. 1990;89:411-9.
et al. Diagnostic value of antibodies against ribosomal phosphopro- 88. Vianna JL, Khamashta MA, Ordi-Rose J, Font J, Cervera R, Lopez-
teins. A cross sectional and longitudinal study. J Rheumatol. 1991; Soto A, et al. Comparison of the primary and secondary antiphos-
18:1026-34. pholipid syndrome: A European multicenter study of 114 patients.
63. Hanson VG, Horowitz M, Rosenbluth D, Spiera H, Puszkin S. Sys- Am J Med. 1994;96:3-9.
temic lupus erythematosus patients with central nervous system in- 89. Gleason CB, Stoddard MF, Wagner SG, Longaker RA, Pierangeli S,
volvement show autoantibodies to a 50-kD neuronal membrane pro- Harris EN. A comparison of cardiac valvular involvement in the
tein. J Exp Med. 1992;176:565-73. primary antiphospholipid syndrome versus anticardiolipin-negative
64. Koren E, Reichlin MW, Koscec M, Fugate RD, Reichlin M. Autoan- systemic lupus erythematosus. Am Heart J. 1993;125:1123-9.
tibodies to the ribosomal P proteins react with a plasma membrane- 90. Jonnson H, Nived O, Sturfelt G. Outcome in systemic lupus erythem-
related target on human cells. J Clin Invest. 1992;89:1236-41. atosus: a prospective study of patients from a defined population.
65. Lavalle C, Pizarro S, Drenkard C, Sanchez-Guerrero J, Alarcon- Medicine (Baltimore). 1989;68:141-50.
Segovia D. Transverse myelitis: a manifestation of systemic lupus 91. Ettinger WH, Goldberg AP, Applebaum-Bowden D, Hazzard WR.
erythematosus strongly associated with antiphospholipid antibodies. Dyslipoproteinemia in systemic lupus erythematosus. Am J Med.
J Rheumatol. 1990;17:34-7. 1987;83:503-8.
66. Kent DL, Haynor DR, Longstreth WT Jr, Larson EB. The clinical 92. Kabakov AE, Tertov W , Saenko VA, Poverenny AM, Orekhov AN.
efficacy of magnetic resonance imaging in neuroimaging. Ann Intern The atherogenic effect of lupus sera: Systemic lupus erythematosus-
Med. 1994;120:856-71. derived immune complexes stimulate the accumulation of cholesterol
67. Magnetic resonance imaging of the brain and spine: a revised state- in cultured smooth muscle cells from human aorta. Clin Immunol
ment. American College of Physicians. Ann Intern Med. 1994;120:872-5. Immunopath. 1992;63:214-20.
68. Rubbert A, Marienhagen J, Pirner K, Manger B, Grebmeier J, 93. Mulherin D, Bresnihan B. Systemic lupus erythematosus. Bailliere's
Engelhardt A, et al. Single-photon-emission computed tomography Clin Rheumatol. 1994;7:31-57.
analysis of cerebral blood flow in the evaluation of central nervous 94. Abramson SB, Dobro J, Eberle MA, Beuton M, Reibman J, Epstein
system involvement in patients with systemic lupus erythematosus. H, et al. Acute reversible hypoxemia in systemic lupus erythematosus.
Arthritis Rheum. 1993;36:1253-62. Ann Intern Med. 1991;114:941-7.
69. Holman BL. Functional imaging in systemic lupus erythematosus: an 95. Lynch JP, Hunninghake GW. Pulmonary complications of collagen
accurate indicator of central nervous system involvement? [Editorial]. vascular disease. Annu Rev Med. 1992;43:17-35.
Arthritis Rheum. 1993;36:1193-5. 96. Orens JB, Martinez FJ, Lynch JP. Pleuropulmonary manifestations
70. Boumpas DT, Patronas NJ, Dalakas MC, Hakim CA, Klippel JH, of systemic lupus erythematosus. In: McCune JW, ed. Systemic lupus
Balow JE. Acute transverse myelitis in systemic lupus erythematosus: erythematosus. Rheum Dis Clin North Am. 1994;20:159-93.
Magnetic resonance imaging and review of the literature. J Rheuma- 97. Teitel AD, Mackenzie CR, Stern R, Paget SA. Laryngeal involvement
tol. 1990;17:89-93. in systemic lupus erythematosus. Semin Arthritis Rheum. 1992;22:203-
71. Boumpas DT, Yamada H, Patronas NJ, Scott D, Klippel JH, Balow 14.
JE. Pulse cyclophosphamide for severe neuropsychiatric lupus. Q J 98. Martin L, Edworthy SM, Ryan JP, Fritzler MJ. Upper airway disease
Med. 1991;81:975-84. in systemic lupus erythematosus: a report of 4 cases and a review of
72. Barile L, Lavalle C. Transverse myelitis in systemic lupus erythema- the literature. J Rheumatol. 1992;19:1186-90.
tosus—The effect of IV pulse methylprednisolone and cyclophos- 99. Wiedemann HP, Matthay RA. Pulmonary manifestations of systemic
phamide. J Rheumatol. 1992;19:370-2. lupus erythematosus. J Thorac Imag. 1992;7:1-18.
73. Galve E, Candell-Riera J, Pigrau C, Permanyer-Miralda G, Garcia- 100. Leatherman JW. Immune alveolar hemorrhage. Chest. 1987;91:891-7.
Del-Castillo H, Soler-Soler J. Prevalence, morphologic types, and 101. Wiedemann HP, Matthay RA. Pulmonary manifestations of the col-
evolution of cardiac valvular disease in systemic lupus erythematosus. lagen vascular diseases. Clin Chest Med. 1989;10:677-722.
N Engl J Med. 1988;319:817-23. 102. Schwab EP, Schumacher Jr HR, Freundlich B, Callegari PE. Pulmo-
74. Leung WH, Wong KL, Lau CP, Wong CK, Cheng CH. Cardiac nary alveolar hemorrhage in systemic lupus erythematosus. Semin
abnormalities in systemic lupus erythematosus: a prospective Arthritis Rheum. 1993;23:8-15.
M-mode, cross-sectional and doppler echocardiographic study. Int J 103. Weinrib L, Sharma OP, Quismorio FP Jr. A long-term study of
Cardiol. 1990;27:367-75. interstitial lung disease in systemic lupus erythematosus. Semin Ar-
75. Cervera R, Font J, Pare C, Azqueta M, Perez-Villa F, Lopez-Soto A, thritis Rheum. 1990;20:48-56.
et al. Cardiac disease in systemic lupus erythematosus: Prospective 104. Muller NL, Miller RR. Computed tomography of chronic diffuse
study of 70 patients. Ann Rheum Dis. 1991;51:156-9. infiltrative lung disease. Am Rev Respir Dis. 1990;142:1206-15.
76. Roldan CA, Shively BK, Lau CC, Gurule FT, Smith EA, Crawford 105. Muller NL, Staples CA, Miller RR, Vedal S, Thurlbeck WM, Ostrow
MH. Systemic lupus erythematosus valve disease by transesophageal DN. Disease activity in idiopathic pulmonary fibrosis: CT and patho-
echocardiography and the role of antiphospholipid antibodies. J Am logic correlation. Radiology. 1987;165:731-4.
Coll Cardiol. 1992;20:1127-34. 106. Wells A, Hansell DM, Rubens MB, Cullman P, Black CM, Dubois RM.
77. Sturfelt G, Eskilsson J, Nived O. Cardiovascular disease in systemic The predictive value of appearances on thin section computed tomog-
lupus erythematosus: A study of 75 patients from a defined popula- raphy in fibrosing alveolitis. Am Rev Respir Dis. 1993;148:1076-82.
tion. Medicine (Baltimore). 1992;71:216-23. 107. Asherson RA, Oakley CM. Pulmonary hypertension and systemic
78. Petri M, Spence D, Bone LR, Hochberg MC. Coronary artery disease lupus erythematosus. J Rheumatol. 1986;13:1-5.
risk factors in the Johns Hopkins lupus cohort: prevalence, recogni- 108. Simonson JS, Schiller NB, Petri M, Hellmann DB. Pulmonary hy-
tion by patients, and prevention practices. Medicine (Baltimore). pertension in systemic lupus erythematosus. J Rheumatol. 1989; 16:
1992;71:291-302. 918-25.
79. Reveille, JD, Bartolucci A, Alarcon GS. Prognosis in systemic lupus 109. Asherson RA, Higenbottam TW, Dinh Xuan AT, Khamashta MA,
erythematosus: negative impact of increasing age at onset, black race, Hughes GR. Pulmonary hypertension a in lupus clinic: experience
and thrombocytopenia, as well as causes of death. Arthritis Rheum. with twenty-four patients. J Rheumatol. 1990;17:1292-8.
1990;33:37-48. 110. Levy RD, Guerraty AJ, Yacoub MH, Loertscher R. Prolonged survival
80. Nihoyannopoulos P, Gomez PM, Joshi J, Loizou S, Walport MJ, after heart-lung transplantation in systemic lupus erythematosus.
Oakley CM. Cardiac abnormalities in systemic lupus erythematosus. Chest. 1993;104:1903-5.
Circulation. 1990;82:369-75. 111. Laurence J, Wong JE, Nachman R. The cellular hematology of
81. Straaton KV, Chatham WW, Reveille JD, Koopman WJ, Smith SH. systemic lupus erythematosus. In: Lahita RG, ed. Systemic Lupus
Clinically significant valvular heart disease in systemic lupus erythem- Erythematosus. New York: Churchill Livingstone; 1992:771-806.
atosus. Am J Med. 1988;85:645-50. 112. Anderson MJ, Peebles CL, McMillan R, Curd JG. Fluorescent anti-
82. Lehman TA, Palmeri ST, Hastings C, Klippel JH, Plotz PH. Bacte- nuclear antibodies and anti-SS-A/Ro in patients with immune throm-
rial endocarditis complicating systemic lupus erythematosus. J Rheu- bocytopenia subsequently developing systemic lupus erythematosus.
matol. 1983;10:655-8. Ann Intern Med. 1985;103:548-50.
15 June 1995 • Annals of Internal Medicine • Volume 122 • Number 12 949
113. Schwartz RS. Treating chronic idiopathic thrombocytopenic purpura Group on Immune Thrombocytopenic Purpura. Low doses v conven-
[Editorial]. N Engl J Med. 1994;30:1609-10. tional doses of corticoids in immune thrombocytopenic purpura: re-
114. Jouhikainan T, Kekomaki R, Leirisalo-Repo M, Backlund T, Myllya sults of a randomized clinical trial in 160 children, 223 adults. Blood.
G. Platelet autoantibodies detected by immunoblotting in systemic 1988;71:1165-9.
lupus erythematosus: association with the lupus anticoagulant and 120. West SG, Johnson SC. Danazol for the treatment of refractory au-
with history of thrombosis and thrombocytopenia. Eur J Hematol. toimmune thrombocytopenia in systemic lupus erythematosus. Ann
1990;44:234-40. Intern Med. 1988;108:703-6.
115. Alarcdn-Segovia D, Deleze M, Oria CV, Sanchez-Guerrero J, Gomez- 121. Maier WP, Gordon DS, Howard RF, Saleh MN, Miller SB, Lieber-
Pacheco L, Cabiedes J, et al. Antiphospholipid antibodies and the
man JD, et al. Intravenous immunoglobulin therapy in systemic lupus
antiphospholipid syndrome in systemic lupus erythematosus. A pro-
spective analysis of 500 consecutive patients. Medicine (Baltimore). erythematosus-associated thrombocytopenia. Arthritis Rheum. 1990;
1989;68:353-65. 33:1233-9.
116. Strieker RB, Davis JA, Gershow J, Yammamoto KS, Kiprov DD. 122. Andersen JC. Response of resistant idiopathic thrombocytopenic pur-
Thrombotic thrombocytopenic purpura complicating systemic lupus pura to pulsed high-dose dexamethasone therapy. N Engl J Med.
erythematosus. Case report and literature review from the plasma- 1994;330:1560-4.
pheresis era. J Rheumatol. 1992;19:1469-73. 123. Boumpas DT, Barez S, Klippel JH, Balow JE. Intermittent cyclo-
117. Berchtold P, McMillan R. Therapy of chronic idiopathic thrombocy- phosphamide for the treatment of autoimmune thrombocytopenia in
topenic purpura in adults. Blood. 1989;74:2309-17. systemic lupus erythematosus. Ann Intern Med. 1990;112:674-7.
118. Beutler E. Platelet transfusions: The 20,000/mL trigger. Blood. 1993; 124. Figueroa M, Gehlsen J, Hammond D, Ondreyco S, Piro L, Pomeroy
81:1411-13. T, et al. Combination chemotherapy in refractory immune thrombo-
119. Bellucci S, Charpak Y, Chastang C, Tobelem G, and the Cooperative cytopenic purpura. N Engl J Med. 1993;328:1226-9.
950 15 J u n e 1995 • Annals of Internal Medicine • V o l u m e 122 • N u m b e r 12
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Medical certificate from Pantalan SHSDokument2 SeitenMedical certificate from Pantalan SHSAngelo Villafranca67% (3)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Acute Kidney Injury W/ Hyperkalemia NCPDokument5 SeitenAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNoch keine Bewertungen
- Dental Public HealthDokument264 SeitenDental Public HealthCorina Manole DanielaNoch keine Bewertungen
- Erectile DysfunctionDokument145 SeitenErectile Dysfunctionluna palitoNoch keine Bewertungen
- C Anticholinergic Drugs PDFDokument53 SeitenC Anticholinergic Drugs PDFHitesh karnNoch keine Bewertungen
- Advanced Burn Life SupportDokument118 SeitenAdvanced Burn Life SupportIntan Noa100% (1)
- Historia de La Nutricion y Fluidoterapia (History of Pediatric Nutrition and Fluid Therapy)Dokument11 SeitenHistoria de La Nutricion y Fluidoterapia (History of Pediatric Nutrition and Fluid Therapy)Franklin ArandaNoch keine Bewertungen
- Factores de Virulencia Del Streptococcus PneumoniaeDokument7 SeitenFactores de Virulencia Del Streptococcus PneumoniaeFranklin ArandaNoch keine Bewertungen
- Satisfaccion y Burnout en PediatriaDokument6 SeitenSatisfaccion y Burnout en PediatriaFranklin ArandaNoch keine Bewertungen
- Visceral Larva Migrans (Toxocariasis)Dokument4 SeitenVisceral Larva Migrans (Toxocariasis)Franklin ArandaNoch keine Bewertungen
- Cat Scratch Disease, Microbiology, Epidemiology, Clinical Manifestations, Diagnosis and TreatmentDokument17 SeitenCat Scratch Disease, Microbiology, Epidemiology, Clinical Manifestations, Diagnosis and TreatmentFranklin ArandaNoch keine Bewertungen
- Clinica, Diagnostico y Manejo Del Sindrome de DownDokument23 SeitenClinica, Diagnostico y Manejo Del Sindrome de DownFranklin ArandaNoch keine Bewertungen
- Acute Infectious Purpura FulminansDokument15 SeitenAcute Infectious Purpura FulminansFranklin Aranda100% (2)
- Alopecia Androgenetica 2009Dokument9 SeitenAlopecia Androgenetica 2009Franklin ArandaNoch keine Bewertungen
- Deficit de Atencion Con Hiperactividad en Niños y AdolescentesDokument18 SeitenDeficit de Atencion Con Hiperactividad en Niños y AdolescentesFranklin ArandaNoch keine Bewertungen
- Tatuajes y Body PiercingDokument19 SeitenTatuajes y Body PiercingFranklin ArandaNoch keine Bewertungen
- Vascular Malformations of The Central Nervous SystemDokument9 SeitenVascular Malformations of The Central Nervous SystemFranklin Aranda100% (2)
- Revision Actualizada 2009 Sobre VasectomiaDokument12 SeitenRevision Actualizada 2009 Sobre VasectomiaFranklin ArandaNoch keine Bewertungen
- Convulsion No Epileptica PsicogenicaDokument19 SeitenConvulsion No Epileptica PsicogenicaFranklin Aranda100% (1)
- Muerte Cerebral: Criterios Diagnosticos Adultos y NiñosDokument16 SeitenMuerte Cerebral: Criterios Diagnosticos Adultos y NiñosFranklin ArandaNoch keine Bewertungen
- Neumonia Aspirativa en PediatriaDokument28 SeitenNeumonia Aspirativa en PediatriaFranklin Aranda100% (4)
- HEMORRAGIA Subaracnoidea No AneurismaticaDokument16 SeitenHEMORRAGIA Subaracnoidea No AneurismaticaFranklin Aranda100% (4)
- Manejo Del Asma en NiñosDokument84 SeitenManejo Del Asma en NiñosFranklin Aranda100% (1)
- Mini-implant molar intrusion caseDokument1 SeiteMini-implant molar intrusion caseVesna AndreevskaNoch keine Bewertungen
- Uncorrected Author ProofDokument15 SeitenUncorrected Author ProofindahNoch keine Bewertungen
- Bronchopulmonary Dysplasia (BPD)Dokument13 SeitenBronchopulmonary Dysplasia (BPD)Joan BuiNoch keine Bewertungen
- Type2 Diabetes HandoutDokument1 SeiteType2 Diabetes Handouthendra_darmawan_4Noch keine Bewertungen
- Rapid Pathogen Detection by Metagenomic Next-Generation Sequencing of Infected Body FluidsDokument26 SeitenRapid Pathogen Detection by Metagenomic Next-Generation Sequencing of Infected Body FluidsLuisNoch keine Bewertungen
- HEPATITIS B VACCINE NURSING RESPONSIBILITIESDokument14 SeitenHEPATITIS B VACCINE NURSING RESPONSIBILITIESJannine BensiNoch keine Bewertungen
- Femur and Pelvis Fracture (Trauma)Dokument20 SeitenFemur and Pelvis Fracture (Trauma)Ree YahNoch keine Bewertungen
- Thyroid: Cytopathology and Its Histopathological BasesDokument49 SeitenThyroid: Cytopathology and Its Histopathological BasesYuli Setio Budi PrabowoNoch keine Bewertungen
- Prostaglandins: An Overview of Structure and FunctionDokument33 SeitenProstaglandins: An Overview of Structure and FunctionMuhammad JamalNoch keine Bewertungen
- Assignment 1 Cs 0902Dokument4 SeitenAssignment 1 Cs 0902prince12Noch keine Bewertungen
- Understanding Traumatic Brain Injury (TBIDokument16 SeitenUnderstanding Traumatic Brain Injury (TBIdcNoch keine Bewertungen
- GROUP 10 Senstive Abt Food and Food AllergiesDokument16 SeitenGROUP 10 Senstive Abt Food and Food AllergiesLilis nopita SarryNoch keine Bewertungen
- Journal BalakrishnaDokument3 SeitenJournal BalakrishnafandheanayaNoch keine Bewertungen
- Hypokalemia and Hyperkalemia in Infants and Children: Pathophysiology and TreatmentDokument11 SeitenHypokalemia and Hyperkalemia in Infants and Children: Pathophysiology and TreatmentAnantaBenvenutoNoch keine Bewertungen
- Femoral Acetabular Impingement: RadiographyDokument9 SeitenFemoral Acetabular Impingement: Radiography杨钦杰Noch keine Bewertungen
- Obstetrics and GynacologyDokument14 SeitenObstetrics and GynacologykalkidanNoch keine Bewertungen
- Chest XrayDokument6 SeitenChest XrayAjit KumarNoch keine Bewertungen
- Hipertensi Portal Donny SandraDokument67 SeitenHipertensi Portal Donny SandrabobyNoch keine Bewertungen
- Congestive Heart Failure, Pulmonary Edema, and CPAPDokument35 SeitenCongestive Heart Failure, Pulmonary Edema, and CPAPSherwan R Shal100% (1)
- ACLS NotesDokument3 SeitenACLS Notessaxmanwrv0% (1)
- Diabetes Care GuideDokument14 SeitenDiabetes Care GuideadaezeNoch keine Bewertungen
- CLUSTERS LIST - (CHNCS) GO-209Dokument45 SeitenCLUSTERS LIST - (CHNCS) GO-209Gadde Srinivasarao67% (3)
- Kali Bichromicum 30C For COPD 2005Dokument8 SeitenKali Bichromicum 30C For COPD 2005Dr. Nancy MalikNoch keine Bewertungen
- KenyaEMR v17.3.1 Release Notes SummaryDokument3 SeitenKenyaEMR v17.3.1 Release Notes SummaryMigori Art DataNoch keine Bewertungen