Beruflich Dokumente
Kultur Dokumente
Profilaxis Antiibiotica
Hochgeladen von
Andrés RezucOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Profilaxis Antiibiotica
Hochgeladen von
Andrés RezucCopyright:
Verfügbare Formate
The use of prophylactic antibiotics for the prevention of
postoperative infections
Daniel M. Laskin, DDS, MS
Department of Oral and Maxillofacial Surgery School of Dentistry, Virginia Commonwealth University,
Richmond, VA 23298-0566, USA
Despite use of the best surgical techniques, some
operations still carry a high risk of wound infection.
Basic and clinical studies have shown that this risk
can be reduced by the administration of prophy-
lactic antibiotics. There are certain inherent risks
associated with the use of these agents, however,
such as toxic and allergic reactions, emergence of
resistant bacteria, drug interactions, and superinfec-
tions. Moreover, prophylactic antibiotics do not
prevent all postoperative infections. For these reas-
ons, their use should be based on an understanding
of certain basic principles. This article reviews these
principles and discusses their application in specific
clinical situations.
Principles of prophylactic antibiotics
Antibiotic prophylaxis has been defined as the
preoperative use of antibiotics to prevent infection.
Prophylactic use of antibiotics is in contradistinction
to the therapeutic use of antibiotics, which are given
to treat an already existing infection. Not only are the
purposes different but also the manner in which the
drugs should be administered for an optimum effect
are different. A review of the literature clearly indi-
cates that, in many instances, antibiotics are given
postoperatively rather than preoperatively, although it
is still referred to as a prophylactic procedure. This
difference must be taken into consideration when
evaluating the conclusions that are reached and the
recommendations that are made by the authors. It also
may account for some of the contradictory findings
that have been reported in the literature.
As the result of the basic studies of Miles and
Burke et al [1,2] and several well-controlled clinical
studies, the principles of proper antibiotic prophylaxis
have been established for general surgery, and they
are applicable to the field of oral and maxillofacial
surgery. These principles are (1) that the intended
procedure must carry a significant risk of postoper-
ative infection, (2) that the correct antibiotic must be
selected, and (3) that the antibiotic is administered
properly. To these principles one may add a fourth
principle: not to rely solely on prophylactic anti-
biotics to prevent postoperative infections.
Risk of infection
Although such factors as age of the patient,
nutritional status, nature of any underlying disease,
presence of necrotic tissue, and a decreased blood
supply can increase the potential for postoperative
infection, perhaps the most important factor is wound
contamination. Altemeier et al [3] developed a clas-
sification of general surgical wounds relating con-
tamination to the risk of infection. In this
classification, operative wounds are categorized as
clean, clean-contaminated, contaminated, or dirty,
with contamination resulting from planned or
unplanned entry into the respiratory, gastrointestinal,
or genitourinary tracts. Because of the difference in
host response to such contamination and oral con-
tamination, this classification cannot be used for
intraoral wounds. It can be modified, however, to
1042-3699/03/$ see front matter D 2003, Elsevier Science (USA). All rights reserved.
PII: S1042- 3699( 02) 00067- 5
E-mail address: dmlaskin@vcu.edu
Oral Maxillofacial Surg Clin N Am 15 (2003) 155160
establish the indications for prophylactic antibiotics
in other forms of oral and maxillofacial surgery.
According to this modified classification, extraoral
wounds are still categorized in terms of increasing risk
of infection as clean, clean-contaminated, contami-
nated, and dirty. However, the definitions must be
altered to fit the regional differences. Clean surgical
wounds, which have a low infection rate, usually
involve no significant tissue trauma or inflammation,
the incision is closed primarily, the wound is not
drained, and there is no communication with the oral
cavity. Clean-contaminated surgical wounds are sim-
ilar to clean wounds except that there is a greater risk of
infection because communication with the oral cavity
occurs. Contaminated wounds are fresh traumatic
injuries that involve the oral cavity, whereas dirty
wounds are traumatic injuries with delayed treatment
that communicate with the oral cavity and contain
devitalized tissue or foreign bodies.
Clean surgical wounds do not require antibiotic
prophylaxis; however, it should be used in clean-
contaminated wounds. Contaminated wounds usually
can be managed with preoperative prophylactic anti-
biotics if there are no other significant risk factors.
Otherwise, patients with such wounds also should
receive postoperative prophylactic antibiotics. Patients
with dirty wounds, which are already infected, require
preoperative and postoperative therapeutic antibiotics.
The decision not to use antibiotics or to use only
preoperative prophylactic antibiotics is always based
on the assumption that the patient does not have any
significant medical risk factors that could affect the
bodys humoral and cellular defense mechanisms.
These risk factors include poorly controlled diabetes,
end-state renal disease and uremia, severe alcoholism,
an immunocompromising disease (eg, leukemia, lym-
phoma, or an advanced malignant neoplasm), and the
use of chemotherapeutic agents or other immunosup-
pressive drugs. In such patients, one is concerned not
only with preventing the initial contamination of the
wound but also with the possibility of recontamina-
tion during the postoperative period. Therefore, post-
operative prophylaxis is also indicated.
Antibiotic selection
Once it has been determined that prophylactic
antibiotics are indicated in a particular patient, the
second principle involves making the appropriate
selection. The choice of antibiotic is determined
largely by its effectiveness against the pathogens
commonly encountered at the specific surgical site.
It need not be able to eradicate every potential
pathogen that may be encountered. Expanded anti-
biotic coverage serves only to increase the rate of
bacterial resistance and the development of super-
infections. The most commonly encountered orga-
nisms from oral contamination are the streptococci,
anaerobic gram-positive cocci, and anaerobic gram-
negative rods, whereas contamination from the sinus
and nose may include Haemophilus influenzae, dip-
theroids, and peptostreptococci [4]. When the skin is
involved, the presence of Staphylococcus aureus and
epidermidis also must be considered.
Although the first consideration is that the anti-
biotic selected is effective against the major contam-
inating organisms, it also must be nontoxic and
relatively nonallergenic, bactericidal, capable of
achieving therapeutic tissue concentrations, and have
a long half-life so that redosing is generally not
required during the procedure. The antibiotic that
currently still fulfills these requirements best is peni-
cillin. When skin contaminants are a concern, how-
ever, a first-generation cephalosporin, such as
cefazolin, can be used because of its effectiveness
against most staphylococci.
Antibiotic administration
Although one selects the appropriate antibiotic for
prophylaxis, its ultimate effectiveness in preventing
infection still depends on proper administration. This
decision varies according to whether one is dealing
with normal patients, in whom there is only concern
about the initial bacterial contamination that can
occur during the operation, or patients with other
significant risk factors that decrease the bodys
defenses and retard healing, which makes them more
susceptible to recontamination during the healing
period. In the first instance, the antibiotic must be
administered intravenously or intramuscularly within
30 minutes of the incision time at twice the thera-
peutic dose [5]. For penicillin, the dose is 2 million
U, and for cefazolin it is 1 g. This dose generally
provides adequate coverage for up to 4 hours. If the
procedure is prolonged, however, it is advisable to
administer additional doses every 4 hours until the
operation is completed. In patients who are medically
compromised or immunosuppressed, it may be advis-
able to continue prophylactic oral antibiotics until
biologic sealing of the wound has occurred. No data
exist on how long this period should be or even if it
prevents postoperative infections. In fact, one must be
concerned about promoting the emergence of resist-
ant strains and causing superinfections. In a wound
that is healing by primary intention, the period should
D.M. Laskin / Oral Maxillofacial Surg Clin N Am 15 (2003) 155160 156
probably be no longer than 48 hours postoperatively
and in a wound healing by secondary intention it
should be no longer than 3 to 5 days, at which time a
biologic seal should have occurred.
Adjunctive procedures
Although the correct use of prophylactic anti-
biotics significantly reduces the incidence of post-
operative infections, their occurrence can be reduced
further by careful attention to proper surgical tech-
nique. Proper technique involves adequate cleansing
of the surgical site, strict adherence to sterile tech-
nique, avoiding tissue trauma, and minimizing oper-
ating time. In general, the risk of infection has been
shown to increase with each hour of surgery. Shav-
ing the skin in the surgical site with a razor the
evening before the operation also has been shown to
increase the infection rate, probably because of
bacterial proliferation in the areas of minor trauma
produced by shaving [6]. When shaving is neces-
sary, it should be done just before preparation of the
surgical site.
The use of drains also may contribute to post-
operative infections. When drains are necessary in
noninfected wounds, the closed-suction type is prefer-
able to open drains. They should not be placed through
the operative incision and should be removed as soon
as possible. Paying proper attention to these details
during management of the surgical patient greatly
improves the effectiveness of antibiotic prophylaxis.
Specific applications in oral and
maxillofacial surgery (Table 1)
Exodontia and dentoalveolar surgery
Although intraoral surgical wounds are contami-
nated by the oral flora, the ability of patients
normally to tolerate this bacterial population and
the excellent blood supply to the oral tissues allow
such wounds to be managed similarly to clean
wounds. It is unnecessary to use prophylactic anti-
biotics to prevent infection when performing most
types of exodontia and dentoalveolar surgery unless
there are other contributing risk factors (Table 1). If
the procedure involves the maxillary sinus or nasal
cavity, however, this can result in cross-contamina-
tion with new organisms, and prophylactic antibi-
otics should be used except when there is already
infection in these areas. In the latter instance, thera-
peutic antibiotics are indicated.
Impacted third molar surgery
Although many practitioners routinely prescribe
antibiotics for patients who have impacted third
molars removed [7,8], they are generally prescribed
postoperatively. This practice does not accomplish
the true purpose of using prophylactic antibiotics:
having a high tissue concentration present at the
time of surgery when the wound is exposed to
bacterial contamination. It is not surprising that no
convincing data show a significant reduction in
postoperative infections after third molar removal
when antibiotics are used in this manner [7,9]. The
fact that such infections are relatively uncommon
also may be a contributing factor to such findings
[10,11]. Most studies that report high postoperative
infection rates [12] include alveolar osteitis (dry
socket) and fascial space infections. In such stud-
ies, however, there is still not a significant reduc-
tion in either type of problem, whether the
antibiotics are given postoperatively or preopera-
tively [1315].
Although isolated cases of severe fascial space
infections after third molar removal have been
reported [16], the incidence is too low to justify the
routine use of prophylactic antibiotics. Such treat-
ment should be reserved only for patients with
significant medical risk factors for infection [1,17].
In these cases it should be given immediately before
surgery and for 3 to 5 days after surgery to provide an
adequate period of coverage.
Dental implants
Few studies have been conducted on the effect of
antibiotics on the infection rate after implant place-
ment. Two studies in which no control group was
used [18,19] concluded that preoperative prophylactic
antibiotics were effective in preventing postoperative
infections. In a subsequent, better controlled study
[20], however, no difference in postoperative infec-
tions or implant failure was found between the
two groups.
In a more recent, large, multicenter study, Dent et
al [21] analyzed implant failures (which probably
included some cases with infection) and found sig-
nificantly fewer failures up to stage 2 surgery, when
high-dose preoperative antibiotics (penicillin in 69%
of cases) were administered. These findings were
confirmed in a follow-up study at 36 months in the
same patient population (4.6% versus 10% failure)
[22]. Thus, there seems to be a benefit in using
prophylactic antibiotics in dental implant patients.
D.M. Laskin / Oral Maxillofacial Surg Clin N Am 15 (2003) 155160 157
Orthognathic surgery
Orthognathic surgery performed via an extraoral
approach is considered a clean procedure and pro-
phylactic antibiotics should not be necessary unless
communication with the mouth is anticipated [23].
Intraoral procedures and procedures that involve the
maxillary sinus and nasal passages are clean-contam-
inated operations, and short-term prophylactic anti-
biotics have been shown to reduce the postoperative
infection rate [24,25]. There seems to be no advan-
tage in prolonged postoperative antibiotic administra-
tion [25,26]. In one study in which a 5-day regimen
was shown to be better than a 1-day regimen [27], as
pointed out by Abubaker [24], the difference was
caused by the difference in the criteria used to
establish wound infection.
Mandibular fractures
Patients with condylar process fractures treated
by either open or closed reduction require no pro-
phylactic antibiotics. The same is true for fractures in
other nontooth-bearing areas that are not in com-
munication with the mouth, because these are all
clean wounds. In patients with compound man-
dibular fractures, however, which are contaminated
wounds, studies have shown that the use of anti-
biotics is effective in reducing postoperative infec-
tions [28,29]. In most of these studies, however, the
antibiotics were given not only preoperatively but
also for a long period postoperatively. More recent
investigations [28,30] have shown that prophylactic
antibiotics given preoperatively and for no longer
than 12 hours postoperatively are just as effective as
long-term use in preventing postoperative infections.
These findings apply only to fractures that are treated
shortly after the injury has occurred. Fractures for
which there is delayed treatment should be consid-
ered dirty wounds, and such patients should receive
therapeutic antibiotics postoperatively.
Facial bone fractures
Although it has been suggested that any mid-
facial fracture compounded into the mouth, nose,
or paranasal sinuses requires antibiotic coverage
[31,32], other studies [28,33] have shown that it
may not be necessary. Because one of these studies
[33] was not well controlled and the other [28] had a
relatively small number of cases, the issue remains
unresolved. Based on the fact that such compound
fractures communicate with a contaminated cavity,
they should be considered as clean-contaminated
wounds and preoperative prophylactic antibiotics
should be used.
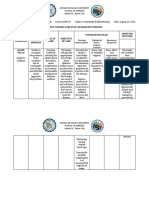
Table 1
Indications for prophylactic antibiotics
Procedure Antibiotic regimen Exceptions
a
Exodontic and dentoalveolar surgery None High risk for infection; communication
with sinus or oral cavity
Impacted third molar surgery None High risk for infection
Dental implants Preoperative Also postoperative prophylaxis when
high risk of infection
Orthognathic surgery (extraoral approach) None Preoperative when anticipate possible
oral contamination
Orthognathic surgery (intraoral approach) Preoperative and
1-day postoperative
None
Mandibular fractures (no oral communication) None None
Mandibular fractures (oral communication) Preoperative and
12 hours postoperative
Use prophylactic antibiotics 35 days
postoperatively when treatment delayed
Facial bone fractures Preoperative None
Soft tissue trauma (oral injuries) None Preoperative when high risk for infection
Soft tissue trauma (clean extraoral lacerations) None Preoperative when high risk for infection
Soft tissue trauma (blunt trauma, gunshot wounds,
bites, orocutaneous communication)
Preoperative Postoperative prophylaxis for 35 days
when high risk for infection
Major head and neck surgery Preoperative Postoperative prophylaxis 35 days when
packs or drains used; lack of watertight
closure; high risk for infection
a
High risk for infection refers to such factors as poor nutritional status, complicating medical problems, presence of necrotic
tissue or foreign bodies, and decreased blood supply to the region.
D.M. Laskin / Oral Maxillofacial Surg Clin N Am 15 (2003) 155160 158
Soft tissue trauma
Patients with traumatic injuries that involve the
oral mucosa, gingiva, or tongue do not require
prophylactic antibiotics because such wounds,
although contaminated, generally heal without infec-
tion. Simple extraoral lacerations from relatively
clean objects that are closed within 4 hours also have
a low infection rate and do not require prophylactic
antibiotics [34]. Extraoral soft tissue injuries, such as
those caused by blunt trauma, gunshot wounds, and
bites and injuries that involve orocutaneous commu-
nication, fall into either the category of clean-con-
taminated or contaminated wounds, and the patient
should receive pretreatment antibiotic prophylaxis.
If the wounds are extremely dirty, the patient also
should receive postoperative therapeutic antibiotics.
Major head and neck surgery
Researchers generally agree that patients who
undergo major surgical procedures in the head and
neck region, such as oncologic and reconstructive
surgery, should receive preoperative prophylactic
antibiotics [31,3539]. There is a question regarding
how long they should be used postoperatively. Sev-
eral studies [31,35,36,38,39] that have shown that
there is no advantage in extending the prophylactic
antibiotics beyond 1 day after surgery in such cases
unless there are packs or drains in the wound or it is
not possible to obtain a watertight closure and there is
prolonged leakage of saliva into the wound [40].
Summary
Although prophylactic antibiotics do not prevent
all postoperative infections, they can reduce the
incidence significantly when administered correctly.
However, they should be used only in patients in
whom the surgical procedure or the medical condition
puts them at a high risk of developing such infec-
tions. As a general rule, the anticipated risk should
exceed 10% [41]. Use of antibiotics in low-risk cases
in an attempt to prevent postoperative infections,
especially when used for prolonged periods, can
result in adverse drug effects, superinfections, and
the emergence of resistant strains without providing
any significant benefits. As Furstenburg [42] stated so
succinctly more than 50 years ago: With the dis-
covery of penicillin, its allied agents, and their mass
production, clinicians have employed them in differ-
ent forms and by various methods for almost every
illness in the category of medicine. The urge to
administer appears to transcend therapeutic rationale
and provokes the use of antibiotics for purposes often
obscure and irrelevant. It is only natural that great
inventions and discoveries should gain wide acclaim
and enthusiastic endorsement and enjoy universal
acceptance far in excess of which they merit.
References
[1] Miles AA, Miles EM, Burke J. The value and duration
of defense reaction of the skin to primary lodgment
of bacteria. British Journal of Experimental Pathology
1957;38:7986.
[2] Burke JF. The effective period of preventive antibiotic
action in experimental incisions and dermal lesions.
Surgery 1961;50:1618.
[3] Altemeier WA, Burke JF, Pruitt Jr BA, et al. Manual on
control of infection in surgical patients. 2
nd
edition.
Philadelphia: JB Lippincott; 1984. p. 269.
[4] Gagliano NC, Leisure GS. Perioperative pharmacol-
ogy. In: Stone OJ, Bogdonoff DL, Leisure GS, et al,
editors. Perioperative care: anesthesia, medicine, and
surgery. St. Louis: Mosby; 1998. p. 486.
[5] Peterson LJ. Principles of antibiotic therapy. In: Topa-
zian RG, Goldberg MH, editors. Oral and maxillofacial
infections. 3
rd
edition. Philadelphia: WB Saunders;
1994. p. 16097.
[6] Cameron JL. Current surgical therapy. 7
th
edition.
St. Louis: Mosby; 2001. p. 1281.
[7] Capuzzi P, Montebugnoli L, Vaccaro MA. Extraction
of impacted third molars: a longitudinal, prospective
study. Oral Surg Oral Med Oral Pathol 1994;77:
3413.
[8] Piecuch JF, Arzadon J, Lieblich SE. Prophylactic anti-
biotics for third molar surgery: a supportive opinion.
J Oral Maxillofac Surg 1995;53:5360.
[9] Chiapasco M, Cicco LD, Marrone G. Side effects and
complications associated with third molar surgery. Oral
Surg Oral Med Oral Pathol 1993;76:31220.
[10] Goldberg MA, Nemarich AN, Marco WP. Complica-
tions after mandibular third molar surgery: a statistical
analysis of 500 consecutive procedures in private prac-
tice. J Am Dent Assoc 1985;111:2779.
[11] Osborn TP, Frederickson G, Small IA, et al. A prospec-
tive study of complications related to mandibular third
molar surgery. J Oral Maxillofac Surg 1985;43:7679.
[12] Mitchell DA. A controlled clinical trial of prophylactic
tinidazole for chemoprophylaxis in third molar surgery.
Br Dent J 1986;160:2846.
[13] Curran JB, Kennett S, Young AR. An assessment of
the use of prophylactic antibiotics in third molar sur-
gery. Int J Oral Surg 1974;3:16.
[14] Happonen R-P, Backstrom A-C, Ylipaavalniemi P.
Prophylactic use of phenoxy-methylpenicillin and tini-
dazole in mandibular third molar surgery: a com-
parative placebo controlled clinical trial. Br J Oral
Maxillofac Surg 1990;28:125.
D.M. Laskin / Oral Maxillofacial Surg Clin N Am 15 (2003) 155160 159
[15] Thomas DW, Hill CM. An audit of antibiotic prescrib-
ing in third molar surgery. Br J Oral Maxillofac Surg
1997;35:1268.
[16] Indresano AT, Haug RH, Hoffman MJ. The third molar
as a cause of deep space infections. J Oral Maxillofac
Surg 1992;50:335.
[17] MacGregor AJ. Reduction in morbidity in the surgery
of the third molar removal. Dent Update 1990;17:
4114.
[18] Larsen P, McGlumphy E. Antibiotic prophylaxis for
placement of dental implants. J Oral Maxillofac Surg
1993;51:194.
[19] Peterson L, McGlumphy E, Halikas L. Long-term anti-
biotic prophylaxis is not necessary for placement of
dental implants. J Oral Maxillofac Surg 1996;54:76.
[20] Gynther G, Kondell P, Moberg L, et al. Dental implant
installation without antibiotic prophylaxis. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod 1998;85:
50922.
[21] Dent CD, Olson JW, Farish SE, et al. Influence of
preoperative antibiotics on success of endosseous im-
plants up to and including Stage 2 surgery: a study
of 2,641 implants. J Oral Maxillofac Surg 1997;55:
1924.
[22] Laskin DM, Dent CD, Morris HF, et al. The influence
of preoperative antibiotics on success of endosseous
implants at 36 months. Ann Periodontol 2000;5:
16674.
[23] Zallen RD, Strader RJ. The use of prophylactic anti-
biotics in extraoral procedures for mandibular prog-
nathism. J Oral Surg 1971;29:1789.
[24] Abubaker AO. Antibiotic prophylaxis in orthognathic
surgery: a 1-day versus 5-day regimen [discussion].
J Oral Maxillofac Surg 1999;57:2302.
[25] Ruggles JE, Hann JR. Antibiotic prophylaxis in intrao-
ral orthognathic surgery. J Oral Maxillofac Surg
1984;42:797801.
[26] Fridrich KL, Partnoy BE, Zeitler DL. Prospective anal-
ysis of antibiotic prophylaxis for orthognathic surgery.
Int J Adult Orthod Orthognath Surg 1994;9:12931.
[27] Bentley KC, Head TW, Aiello GA. Antibiotic prophy-
laxis in orthognathic surgery: a 1-day versus 5-day regi-
men. J Oral Maxillofac Surg 1999;57:22630.
[28] Chole RA, Yee J. Antibiotic prophylaxis for facial
fractures: a prospective, randomized clinical trial. Arch
Otolaryngol Head Neck Surg 1987;113:10556.
[29] Zallen RD, Curry JT. A study of antibiotic usage in
compound mandibular fractures. J Oral Surg 1975;33:
4314.
[30] Abubaker AO, Rollert MA. Postoperative antibiotic
prophylaxis in mandibular fractures: a preliminary
randomized, double-blind, and placebo-controlled clin-
ical study. J Oral Maxillofac Surg 2001;59:14159.
[31] Eschelman LT, Schleuning AJ, Brummett RE. Prophy-
lactic antibiotics in otolaryngologic surgery: a double-
blind study. Transactions of American Academy Op-
thalmology and Otolaryngology 1971;75:38794.
[32] Zallen RD, Black SL. Antibiotic therapy in oral and
maxillofacial surgery. J Oral Surg 1976;34:34951.
[33] Paterson JA, Cordo Jr VA, Stratigas GT. An examina-
tion of antibiotic prophylaxis in oral and maxillofacial
surgery. J Oral Maxillofac Surg 1970;28:7539.
[34] Dellinger ED. Antibiotic use. In: Trunkey DD, Lewis
Jr FR, editors. Current therapy of trauma. 3
rd
edition.
St. Louis: Mosby; 1991. p. 47.
[35] Conover M, Kaban LB, Mulliken JB. Antibiotic pro-
phylaxis for major maxillocraniofacial surgery. J Oral
Maxillofac Surg 1985;43:86570.
[36] Fee Jr WE, Glenn M, Handen C, et al. One day versus
2 days of prophylactic antibiotics in patients under-
going major head and neck surgery. Laryngoscope
1984;94:6124.
[37] Johnson JT, Myers EN, Thearle PB, et al. Antibiotic
prophylaxis for contaminated head and neck surgery.
Laryngoscope 1984;94:4651.
[38] Johnson JT, Schuller DE, Silver E, et al. Antibiotic
prophylaxis in high-risk head and neck surgery: one-
day vs five-day therapy. Otolaryngol Head Neck Surg
1986;95:5547.
[39] Mombelli G, Coppens I, Dor P, et al. Antibiotic pro-
phylaxis in surgery for head and neck cancer: com-
parative study of short and prolonged administration
of carbenicillin. J Antimicrob Chemother 1987;7:
66771.
[40] Shapiro M. Prophylaxis in otolaryngologic surgery
and neurosurgery: a critical review. Rev Infect Dis
1991;13(Suppl 10):S85868.
[41] Burkett HG, Quick RG, Gott DT. Essential surgery:
problems, diagnosis and management. 2
nd
edition. Ed-
inburgh: Churchill-Livingstone; 1998. p. 70.
[42] Furstenburg AC. Antibiotics in the treatment of disease
of the ear, nose, and throat. Ann Otol 1949;58:517.
D.M. Laskin / Oral Maxillofacial Surg Clin N Am 15 (2003) 155160 160
Das könnte Ihnen auch gefallen
- Surgical Antibiotic ProphylaxisDokument7 SeitenSurgical Antibiotic ProphylaxisRony Rony100% (1)
- Dmso Natures Best HealerDokument2 SeitenDmso Natures Best HealerJan Pran100% (1)
- Antibiotic Prophylaxis PDFDokument3 SeitenAntibiotic Prophylaxis PDFPadmanabha GowdaNoch keine Bewertungen
- Antibiotic 4 SurgicalDokument3 SeitenAntibiotic 4 SurgicalNanaDinaWahyuniNoch keine Bewertungen
- Bpad 051822Dokument32 SeitenBpad 051822Shubhrima KhanNoch keine Bewertungen
- (Contemporary Clinical Neuroscience) Giuliana Grimaldi, Mario Manto (auth.), Giuliana Grimaldi, Mario Manto (eds.)-Mechanisms and Emerging Therapies in Tremor Disorders-Springer-Verlag New York (2013).pdfDokument490 Seiten(Contemporary Clinical Neuroscience) Giuliana Grimaldi, Mario Manto (auth.), Giuliana Grimaldi, Mario Manto (eds.)-Mechanisms and Emerging Therapies in Tremor Disorders-Springer-Verlag New York (2013).pdfDanalachi Adrian100% (2)
- FNCP - Inadequate Exercise & Breeding Site For MosquitoesDokument2 SeitenFNCP - Inadequate Exercise & Breeding Site For MosquitoesGwyneth Fisher100% (1)
- Biofilms in Infection Prevention and Control: A Healthcare HandbookVon EverandBiofilms in Infection Prevention and Control: A Healthcare HandbookBewertung: 1 von 5 Sternen1/5 (1)
- Adult ENT Antibiotic Surgical Prophylaxis Guidelines: Full Title of Guideline: AuthorDokument7 SeitenAdult ENT Antibiotic Surgical Prophylaxis Guidelines: Full Title of Guideline: Authorai naNoch keine Bewertungen
- Antimicrobialstewardship Approachesinthe Intensivecareunit: Sarah B. Doernberg,, Henry F. ChambersDokument22 SeitenAntimicrobialstewardship Approachesinthe Intensivecareunit: Sarah B. Doernberg,, Henry F. ChambersecaicedoNoch keine Bewertungen
- Use of Prophylactic AntibioticsDokument6 SeitenUse of Prophylactic AntibioticsDavid ArévaloNoch keine Bewertungen
- Laskin The Use of Prophylactic AntibioticsDokument6 SeitenLaskin The Use of Prophylactic Antibioticsapi-265532519Noch keine Bewertungen
- Preoperative Antibiotic Prophylaxis - StatPearls - NCBI BookshelfDokument6 SeitenPreoperative Antibiotic Prophylaxis - StatPearls - NCBI BookshelfAshen DissanayakaNoch keine Bewertungen
- Antibiotic SsiDokument6 SeitenAntibiotic Ssim8wyb2f6ngNoch keine Bewertungen
- Prophylactic Antibiotic TRT in ImplantDokument9 SeitenProphylactic Antibiotic TRT in ImplantEdu EduNoch keine Bewertungen
- A Review of Use of AntibioticsDokument15 SeitenA Review of Use of AntibioticsInternational Medical Publisher0% (1)
- Antibiotic in Obstetric and GynecologyDokument36 SeitenAntibiotic in Obstetric and GynecologyDrAbdi YusufNoch keine Bewertungen
- First Page PDFDokument1 SeiteFirst Page PDFmpaivaecostaNoch keine Bewertungen
- Aae Systemic AntibioticsDokument8 SeitenAae Systemic AntibioticsIulia CiobanuNoch keine Bewertungen
- Preoperative Antibiotic Prophylaxis StatPearls NCBI BookshelfDokument1 SeitePreoperative Antibiotic Prophylaxis StatPearls NCBI BookshelfJEAN BAILEY RAMOS ROXASNoch keine Bewertungen
- Antibiotic Prophylaxis in Blepharoplasty - Review of The Current Literature 2017Dokument5 SeitenAntibiotic Prophylaxis in Blepharoplasty - Review of The Current Literature 2017María Alejandra Rojas MontenegroNoch keine Bewertungen
- Antibiotic ProphylaxisDokument6 SeitenAntibiotic ProphylaxisTayyaba RafiqNoch keine Bewertungen
- Rational Use of Antibiotics in SurgeryDokument4 SeitenRational Use of Antibiotics in SurgerydaNoch keine Bewertungen
- Guidelines For Abx Prophylaxis o Surgical Wounds - AFPDokument16 SeitenGuidelines For Abx Prophylaxis o Surgical Wounds - AFPyusmaniqistinaNoch keine Bewertungen
- ANTIBIOTICS V (Basics)Dokument32 SeitenANTIBIOTICS V (Basics)Anamta AshfaqNoch keine Bewertungen
- Journal Surg Ward BorjaDokument4 SeitenJournal Surg Ward BorjaYana PotNoch keine Bewertungen
- Chemo ProphylaxisDokument13 SeitenChemo ProphylaxisSaket DaokarNoch keine Bewertungen
- Antibiotic TreatmentDokument25 SeitenAntibiotic TreatmentNailil khusnaNoch keine Bewertungen
- Antibiotic Prophylaxis-An EssayDokument12 SeitenAntibiotic Prophylaxis-An EssayGokul RamakrishnanNoch keine Bewertungen
- Current Concepts Profilaxis CMFDokument11 SeitenCurrent Concepts Profilaxis CMFEliseo ValdezNoch keine Bewertungen
- Antibiotic Prophylaxis For Traumatic Facial FracturesDokument10 SeitenAntibiotic Prophylaxis For Traumatic Facial FracturesMaria Camila Castiblanco MolinaNoch keine Bewertungen
- Clasificacion de HeridasDokument11 SeitenClasificacion de HeridasSaul SilvaNoch keine Bewertungen
- Antimicrobial StewardshipDokument7 SeitenAntimicrobial StewardshipJohn TusselNoch keine Bewertungen
- Antibiotics AngeleDokument12 SeitenAntibiotics Angeleyehouenou carineNoch keine Bewertungen
- Audits For Monitoring The Quality of Antimicrobial PrescriptionsDokument2 SeitenAudits For Monitoring The Quality of Antimicrobial PrescriptionsRetno Dwi HartantiNoch keine Bewertungen
- 3avijeet EtalDokument9 Seiten3avijeet EtaleditorijmrhsNoch keine Bewertungen
- Practices: in Patient CareDokument5 SeitenPractices: in Patient Careahmad nuril hidayatNoch keine Bewertungen
- Idsaintraabdom2003 PDFDokument9 SeitenIdsaintraabdom2003 PDFluckevNoch keine Bewertungen
- Antimicrobial ProphylaxisDokument2 SeitenAntimicrobial ProphylaxisbournvilleeaterNoch keine Bewertungen
- Antibiotics 13 00272 With CoverDokument14 SeitenAntibiotics 13 00272 With CoverJoe Christopher Olivares LopezNoch keine Bewertungen
- Practice Bulletin ACOG Antibiotic Prophylaxis For LabourDokument12 SeitenPractice Bulletin ACOG Antibiotic Prophylaxis For LabourLorenzo TzuNoch keine Bewertungen
- General Principles of Antimicrobial Therapy - 1619693890521Dokument14 SeitenGeneral Principles of Antimicrobial Therapy - 1619693890521DicksonNoch keine Bewertungen
- Medical Therapy in Equine Wound ManagementDokument13 SeitenMedical Therapy in Equine Wound ManagementDanahe CastroNoch keine Bewertungen
- When To Stop Antibiotics in The Critically IllDokument13 SeitenWhen To Stop Antibiotics in The Critically IllJhoselyn De La Torre OnofreNoch keine Bewertungen
- Bacterial Impact On Wound Healing: From Contamination To InfectionDokument17 SeitenBacterial Impact On Wound Healing: From Contamination To InfectionLouis MushaikeNoch keine Bewertungen
- Medical Problem That Needs Antibiotic ProphylaxisDokument6 SeitenMedical Problem That Needs Antibiotic ProphylaxisPing KyNoch keine Bewertungen
- ATB ProfilaxisDokument10 SeitenATB Profilaxiscristopher_ahcNoch keine Bewertungen
- 01 Chapter Anti InfectiveDokument90 Seiten01 Chapter Anti InfectiveMSKCNoch keine Bewertungen
- St. Louis University Institute of Health and Biomedical SciencesDokument39 SeitenSt. Louis University Institute of Health and Biomedical SciencesMind BlowerNoch keine Bewertungen
- Antibiotics in Periodental TreatmentDokument29 SeitenAntibiotics in Periodental TreatmentJana AliNoch keine Bewertungen
- BP AntibiotictherapyDokument4 SeitenBP AntibiotictherapyDebasmita Datta GuptaNoch keine Bewertungen
- Preoperative Antibiotic Prophylaxis - StatPearls - NCBI BookshelfDokument7 SeitenPreoperative Antibiotic Prophylaxis - StatPearls - NCBI BookshelfMikaela l100% (1)
- Guideline Antibiotic RationalDokument35 SeitenGuideline Antibiotic RationalIstianah EsNoch keine Bewertungen
- G AntibiotictherapyDokument3 SeitenG AntibiotictherapyJavangula Tripura PavitraNoch keine Bewertungen
- The Ethics of Prophylactic Antibiotics For Neurosurgical ProceduresDokument6 SeitenThe Ethics of Prophylactic Antibiotics For Neurosurgical ProceduresBahtiar ArasNoch keine Bewertungen
- Intra-Abdominal Sepsis - Newer Interventional and Antimicrobial TherapiesDokument16 SeitenIntra-Abdominal Sepsis - Newer Interventional and Antimicrobial TherapiesDaniel Lumban GaolNoch keine Bewertungen
- Pharma JournalDokument3 SeitenPharma JournalAiMaoRuiNoch keine Bewertungen
- 4.AMS Uso ATM De-Escalar 2020Dokument56 Seiten4.AMS Uso ATM De-Escalar 2020christian mezaNoch keine Bewertungen
- Mayoclinproc 86 2 013 PDFDokument12 SeitenMayoclinproc 86 2 013 PDFMagdy Ali ELsherbenyNoch keine Bewertungen
- Jurnal BismillahDokument9 SeitenJurnal BismillahNavis ZhaFranNoch keine Bewertungen
- AAE Position StatementDokument5 SeitenAAE Position StatementCarlos San MartinNoch keine Bewertungen
- Tackling AB ResistenDokument4 SeitenTackling AB ResistenBedah Mulut UNAIRNoch keine Bewertungen
- Antimicrobial StewardshipDokument7 SeitenAntimicrobial StewardshipMehwish MughalNoch keine Bewertungen
- EAU Pocket On Paediatric Urology 2023Dokument54 SeitenEAU Pocket On Paediatric Urology 2023Andrea SzaszNoch keine Bewertungen
- Capgras' Delusion: A Systematic Review of 255 Published CasesDokument13 SeitenCapgras' Delusion: A Systematic Review of 255 Published CasesKaren RosasNoch keine Bewertungen
- Dengue Fever (Nepal) An Emerging Public Health Problem.Dokument13 SeitenDengue Fever (Nepal) An Emerging Public Health Problem.Bzay DhitalNoch keine Bewertungen
- Encefalitis LimbicaDokument11 SeitenEncefalitis LimbicaRandy UlloaNoch keine Bewertungen
- Stridor, Aspiration, and Cough in ChildrenDokument41 SeitenStridor, Aspiration, and Cough in ChildrenArif Rahman DmNoch keine Bewertungen
- Time in Time Out: Temperature Monitoring Log Sheet For The Month of February 2019Dokument6 SeitenTime in Time Out: Temperature Monitoring Log Sheet For The Month of February 2019Waqas VickyNoch keine Bewertungen
- Late Pregnancy Bleeding (LPB) : Antepartum Hemorrhage (Aph) Dr. A. MutungiDokument3 SeitenLate Pregnancy Bleeding (LPB) : Antepartum Hemorrhage (Aph) Dr. A. Mutungikhadzx100% (2)
- Eward SKDRDokument87 SeitenEward SKDRBasroni FaizalNoch keine Bewertungen
- Cataract: Health Education Library For PeopleDokument2 SeitenCataract: Health Education Library For PeopleNaidu VegiNoch keine Bewertungen
- Untitled PresentationDokument228 SeitenUntitled PresentationSafira WasimNoch keine Bewertungen
- Revathi Papsmear ProcedureDokument50 SeitenRevathi Papsmear ProcedureRevathi DadamNoch keine Bewertungen
- Dengue Fever: A Statistical Analysis Regarding Awareness About Dengue Among University Students in Azad KashmirDokument8 SeitenDengue Fever: A Statistical Analysis Regarding Awareness About Dengue Among University Students in Azad KashmirIm jungkook JUSTIN SEAGULL A.K.A jungshookNoch keine Bewertungen
- Kertas Kerja PinjamanDokument18 SeitenKertas Kerja PinjamanWan AzmanNoch keine Bewertungen
- Cerebral HemorrhageDokument2 SeitenCerebral HemorrhageGian TejadaNoch keine Bewertungen
- Moduleiii:Summativeevaluation: Pheochromocytoma. (2020) - N Ational Library of M EdicineDokument1 SeiteModuleiii:Summativeevaluation: Pheochromocytoma. (2020) - N Ational Library of M EdicineKashley DangliNoch keine Bewertungen
- Shutter Island Presentation For ArtifactDokument8 SeitenShutter Island Presentation For Artifactapi-478108843Noch keine Bewertungen
- Oral PathologyDokument31 SeitenOral PathologyAnonymous GyqTkXMwMNoch keine Bewertungen
- BPT 3rd Year General Surgery Lesson PlanDokument31 SeitenBPT 3rd Year General Surgery Lesson PlanKhushNoch keine Bewertungen
- COVID 19 RT PCR Screening (Nucleic Acid Amplification Qualitative)Dokument2 SeitenCOVID 19 RT PCR Screening (Nucleic Acid Amplification Qualitative)bawa sagguNoch keine Bewertungen
- Immunizations UAGDokument4 SeitenImmunizations UAGRafael G. Garcia SanchezNoch keine Bewertungen
- Removing Gallstones From Your Body: Recommended PracticeDokument1 SeiteRemoving Gallstones From Your Body: Recommended PracticeRyok DaysNoch keine Bewertungen
- TP3 Ingles II 19Dokument3 SeitenTP3 Ingles II 19Gustavo ArenaNoch keine Bewertungen
- Gynecology Adnexal MassDokument2 SeitenGynecology Adnexal MassgeNoch keine Bewertungen
- Caso 2Dokument78 SeitenCaso 2Khairul ScNoch keine Bewertungen
- I-Choose The Correct Answer of The Following Sentences:: Palestine College of NursingDokument9 SeitenI-Choose The Correct Answer of The Following Sentences:: Palestine College of NursingHasan A AsFourNoch keine Bewertungen
- Hospital Teams: Bahasa InggrisDokument6 SeitenHospital Teams: Bahasa InggrisIlhamNoch keine Bewertungen