Beruflich Dokumente
Kultur Dokumente
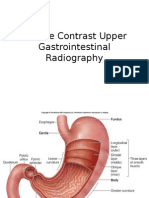
Detection of Ulcer Disease: Peptic Ulcers Gastric Ulcers Gastric Carcinomas
Hochgeladen von
Yannah Mae EspineliOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Detection of Ulcer Disease: Peptic Ulcers Gastric Ulcers Gastric Carcinomas
Hochgeladen von
Yannah Mae EspineliCopyright:
Verfügbare Formate
Detection of ulcer disease Endoscopy is the most accurate diagnostic test for peptic
ulcer disease (PUD). Sensitivity of endoscopy depends in part upon the location of the
ulcer, the experience of the endoscopist, and the "gold" standard used. Experienced
endoscopists detect about 90 percent of gastroduodenal lesions found by a second
endoscopist, by radiography, or at surgery
Peptic ulcers are mucosal breaks of 3 mm or greater and are common, occurring in about
10% of adults in Western countries.
[1]
Gastric ulcers account for about one third of peptic
ulcers, and duodenal ulcers account for the remainder. Because a small percentage (< 5%)
of gastric ulcers are caused by ulceratedgastric carcinomas, all gastric ulcers must be
carefully assessed to differentiate benign lesions from malignant lesions. Radiologic
characteristics of gastric ulcers are seen in the images below.
Image from an upper gastrointestinal series. A 5-cm ulcer crater in the lesser curve of the stomach is
depicted en face. The filling defects in the ulcer crater are caused by a blood clot from recent bleeding.
This lateral view (same patient as in the previous image) shows poor mucosal coating caused by recent
bleeding.
Hemorrhage
Hemorrhage occurs in 20-30% of ulcers.
[1]
Endoscopy is the modality of choice for the
investigation of hemorrhages, having a sensitivity of more than 90% in the detection of the
bleeding site.
Double-contrast barium studies are limited by poor mucosal coating in the presence of
bleeding. Nevertheless, the bleeding site may be detected in as many as 75% of cases. A
filling defect caused by a blood clot may be seen at the base of the barium-filled ulcer (as
seen in the images below).
Image from an upper gastrointestinal series. A 5-cm ulcer crater in the
lesser curve of the stomach is depicted en face. The filling defects in the ulcer crater are caused by a
blood clot from recent bleeding. This lateral view (same patient as in the
previous image) shows poor mucosal coating caused by recent bleeding.
Perforation
Perforation occurs in as many as 10% of patients with peptic ulcer disease but is less
common in gastric ulcers.
[1]
Most perforations arise from ulcers in the anterior aspect of the duodenal cap and, less
commonly, from the anterior aspect of the lesser curve of the stomach.
In 75% of cases, free gas is present in the peritoneum; this is best shown on an erect chest
radiograph (as demonstrated in the first image below) rather than on an erect or supine
abdominal radiograph.
This supine abdominal radiograph shows a pneumoperitoneum.
An upper GI series performed with water-soluble contrast agent may demonstrate the
presence and site of the perforation and whether it has sealed.
Subphrenic collections are common sequelae of a perforated peptic ulcer. They may be
depicted on plain radiographs (see the first image below), but they are best assessed with
ultrasonography
[5, 6]
or computed tomography (CT) scanning (see the second image below).
This radiograph depicts a subphrenic collection resulting from a perforated gastric ulcer.
Computed tomography scan. Subphrenic collection with gaseous and liquid
components. Note the interface between the edge of the liver and the collection.
Das könnte Ihnen auch gefallen
- General Considerations: o o o o o o oDokument9 SeitenGeneral Considerations: o o o o o o ovitaNoch keine Bewertungen
- Imaging in Duodenal Ulcers: More..Dokument12 SeitenImaging in Duodenal Ulcers: More..Sulaiman NulhakimNoch keine Bewertungen
- Volvulus MedscapeDokument7 SeitenVolvulus MedscapeHanny Novia RiniNoch keine Bewertungen
- 004 Gastrointestinal TractDokument42 Seiten004 Gastrointestinal Tractنوال سائد عبداللطيف مسلماني نوال سائد عبداللطيف مسلمانيNoch keine Bewertungen
- Ca Coln - MinDokument46 SeitenCa Coln - Minminhaj_2086Noch keine Bewertungen
- C-Verheyden@chu-Montpellier - FR: Paper TitleDokument53 SeitenC-Verheyden@chu-Montpellier - FR: Paper TitleOttofianus Alvedo Hewick KalangiNoch keine Bewertungen
- CT of Colorectal CancerDokument35 SeitenCT of Colorectal CancerNader ElSayedNoch keine Bewertungen
- Case Based Surgery GuideDokument19 SeitenCase Based Surgery GuideGradestackNoch keine Bewertungen
- Case 70Dokument20 SeitenCase 70Ulfa DiyaNoch keine Bewertungen
- SESAP Abd HBPDokument90 SeitenSESAP Abd HBPLamisNoch keine Bewertungen
- Small Bowel ObstructionDokument17 SeitenSmall Bowel ObstructionXavi Diaz100% (1)
- GIT Raiological Signs1Dokument45 SeitenGIT Raiological Signs1Sharayu DhobleNoch keine Bewertungen
- Pancreatic Pseudocyst EDITEDDokument5 SeitenPancreatic Pseudocyst EDITEDLaura LatifaNoch keine Bewertungen
- 1 2019 Small Bowel ObstructionDokument15 Seiten1 2019 Small Bowel ObstructionPaúl AndradeNoch keine Bewertungen
- Surgery Pretest SummaryDokument9 SeitenSurgery Pretest SummaryPrince DuNoch keine Bewertungen
- Peptic and Other Benign UlcersDokument31 SeitenPeptic and Other Benign Ulcersmomi311Noch keine Bewertungen
- The Spleen: Splenic Trauma and Splenectomy: TrunkDokument3 SeitenThe Spleen: Splenic Trauma and Splenectomy: TrunkAsish GeiorgeNoch keine Bewertungen
- Radiografi AbdomenDokument55 SeitenRadiografi AbdomenadikNoch keine Bewertungen
- JURNALDokument27 SeitenJURNALLaily RosidaNoch keine Bewertungen
- Kamal Bani-Hani: Tumors of The EsophagusDokument38 SeitenKamal Bani-Hani: Tumors of The EsophagusHrineac FlorinNoch keine Bewertungen
- Causes of Sis and Management of A CaseDokument26 SeitenCauses of Sis and Management of A CaseEmmanuelLazarusNoch keine Bewertungen
- UntitledDokument49 SeitenUntitledkedas70Noch keine Bewertungen
- Endoscopic Management of Complications From Laparoscopic Cholecystectomy - UpToDateDokument16 SeitenEndoscopic Management of Complications From Laparoscopic Cholecystectomy - UpToDateLuis Miguel Díaz VegaNoch keine Bewertungen
- Abnormal Bowel Gas PatternDokument136 SeitenAbnormal Bowel Gas PatternEdward ElricNoch keine Bewertungen
- Pancreatic Pseudocyst EDITEDDokument5 SeitenPancreatic Pseudocyst EDITEDLaura LatifaNoch keine Bewertungen
- Otto Van Delden and Robin SmithuisDokument11 SeitenOtto Van Delden and Robin SmithuisSheila AnisaNoch keine Bewertungen
- Clinical Features, Diagnosis, and Staging of Gastric Cancer - UpToDateDokument41 SeitenClinical Features, Diagnosis, and Staging of Gastric Cancer - UpToDateTatiana CumbicosNoch keine Bewertungen
- Abd Trauma 1Dokument77 SeitenAbd Trauma 1mahak chaudharyNoch keine Bewertungen
- Abdominal Trauma-Solid Organ Injuries: Dr. Aakanksha GuptaDokument77 SeitenAbdominal Trauma-Solid Organ Injuries: Dr. Aakanksha Guptamahak chaudharyNoch keine Bewertungen
- EsophagusDokument187 SeitenEsophaguszaldi basalamahNoch keine Bewertungen
- ROBIN. Small Bowel ObstructionDokument25 SeitenROBIN. Small Bowel ObstructionRobin permadi100% (1)
- Findings of Acute Appendicitis of Ultrasound:: Barium Enema AnusDokument2 SeitenFindings of Acute Appendicitis of Ultrasound:: Barium Enema AnusAriana KimNoch keine Bewertungen
- Zinoide To Indicate The Carcinoma-Like Appearance and The PreDokument4 SeitenZinoide To Indicate The Carcinoma-Like Appearance and The PreKarim SupanovaNoch keine Bewertungen
- Surgery - Oral ExamDokument37 SeitenSurgery - Oral ExamShidev100% (1)
- 008 Plain X-Ray AbdomenDokument7 Seiten008 Plain X-Ray AbdomenAthul GurudasNoch keine Bewertungen
- Appendicitis - US FindingsDokument37 SeitenAppendicitis - US FindingsAnonymous FCOOcnNoch keine Bewertungen
- Case ReportDokument5 SeitenCase Report260778Noch keine Bewertungen
- Colectomia Izquierda, Anastomosis Termino-TerminalDokument11 SeitenColectomia Izquierda, Anastomosis Termino-TerminalWildor Herrera GuevaraNoch keine Bewertungen
- Pneumo PeritoneumDokument35 SeitenPneumo PeritoneumDepinNoch keine Bewertungen
- Carcinomaoesophagus 120403111516 Phpapp02Dokument59 SeitenCarcinomaoesophagus 120403111516 Phpapp02Koushik Reddy PodduturiNoch keine Bewertungen
- RADIOLOGI JURNAL CampurDokument58 SeitenRADIOLOGI JURNAL CampurderpNoch keine Bewertungen
- 5th Year Git LectureDokument75 Seiten5th Year Git Lecturekasilat574Noch keine Bewertungen
- Jurnal Double Kontras FIXDokument33 SeitenJurnal Double Kontras FIXWisnuHeriPurwantoNoch keine Bewertungen
- Anorectal Abscess: Principles of Internal Medicine, 18E. New York, Ny: Mcgraw-Hill 2012Dokument7 SeitenAnorectal Abscess: Principles of Internal Medicine, 18E. New York, Ny: Mcgraw-Hill 2012Irene SohNoch keine Bewertungen
- Carcinoid Tumor of The Appendix: A Case ReportDokument3 SeitenCarcinoid Tumor of The Appendix: A Case ReportrywalkNoch keine Bewertungen
- Cholecystectomy (: Laparoscopic GallstonesDokument4 SeitenCholecystectomy (: Laparoscopic GallstonesAlexia BatungbacalNoch keine Bewertungen
- 04 Esophageal TumorsDokument36 Seiten04 Esophageal TumorsDetty NoviantyNoch keine Bewertungen
- Ileal Atresia ReferenceDokument50 SeitenIleal Atresia ReferenceOvamelia JulioNoch keine Bewertungen
- Volvulus of The Gastrointestinal Tract: X-Ray and CT ImagingDokument17 SeitenVolvulus of The Gastrointestinal Tract: X-Ray and CT ImagingFbihansip bancelNoch keine Bewertungen
- Sigmoid VolvulusDokument10 SeitenSigmoid Volvulusbengdubi100% (2)
- Rectal Carcinoma Imaging: More..Dokument13 SeitenRectal Carcinoma Imaging: More..Priyanka Neeraj AroraNoch keine Bewertungen
- UntitledDokument56 SeitenUntitledkedas70Noch keine Bewertungen
- Achalasia CardiaDokument10 SeitenAchalasia CardiaAshish AgarwalNoch keine Bewertungen
- Imaging in Diverticulitis of The ColonDokument7 SeitenImaging in Diverticulitis of The ColonHaryo Chandra KusumosariNoch keine Bewertungen
- Crohn ' S Disease (Regional EnteritisDokument26 SeitenCrohn ' S Disease (Regional EnteritisRasti AmediNoch keine Bewertungen
- Samphire2003 PDFDokument9 SeitenSamphire2003 PDFYacine Tarik AizelNoch keine Bewertungen
- APENDICITIS Fischers Mastery of Surgery 7th ING PDFDokument33 SeitenAPENDICITIS Fischers Mastery of Surgery 7th ING PDFMichel RamirezNoch keine Bewertungen
- Small Nowel Emergency SurgeryDokument8 SeitenSmall Nowel Emergency SurgerySurya Nirmala DewiNoch keine Bewertungen
- Colorectal Surgery: Clinical Care and ManagementVon EverandColorectal Surgery: Clinical Care and ManagementBruce GeorgeNoch keine Bewertungen
- Pathophysiology - HypokalemiaDokument1 SeitePathophysiology - HypokalemiaYannah Mae Espineli33% (3)
- Ventricular Septal DefectDokument6 SeitenVentricular Septal DefectYannah Mae EspineliNoch keine Bewertungen
- Brogada SyndromeDokument19 SeitenBrogada SyndromeYannah Mae Espineli100% (1)
- Medical Management 1. Approach ConsiderationsDokument10 SeitenMedical Management 1. Approach ConsiderationsYannah Mae EspineliNoch keine Bewertungen
- Pathophysiology of DiseaseDokument7 SeitenPathophysiology of DiseaseYannah Mae EspineliNoch keine Bewertungen
- Nursing Care PlansDokument5 SeitenNursing Care PlansYannah Mae EspineliNoch keine Bewertungen
- Some Definitions in Psychiatric NursingDokument9 SeitenSome Definitions in Psychiatric NursingYannah Mae EspineliNoch keine Bewertungen
- Videbeck Psychiatric Mental Health Nursing Chapter Work SheetDokument46 SeitenVidebeck Psychiatric Mental Health Nursing Chapter Work SheetYannah Mae Espineli100% (1)
- Discharge Plan For CADDokument2 SeitenDischarge Plan For CADYannah Mae EspineliNoch keine Bewertungen
- Qualitative Research 2009 Keats 181 95Dokument16 SeitenQualitative Research 2009 Keats 181 95Vratislav SlavíkNoch keine Bewertungen
- IPCMonitor User ManualDokument13 SeitenIPCMonitor User ManualUdo W. BachmannNoch keine Bewertungen
- Comparative Analysis of Short FilmDokument4 SeitenComparative Analysis of Short FilmjacobgeldardNoch keine Bewertungen
- Camera Kiev 88Dokument16 SeitenCamera Kiev 88Mariano RuffoNoch keine Bewertungen
- Sketch Roofing Guide (Sketching Roofs)Dokument5 SeitenSketch Roofing Guide (Sketching Roofs)Ronald Kahora100% (1)
- 1-AAA-The Bait Pumpers Bible !!-Adobe Acrobat PDF Version.Dokument15 Seiten1-AAA-The Bait Pumpers Bible !!-Adobe Acrobat PDF Version.Mike Sullivan100% (1)
- Newsletter TemplateDokument8 SeitenNewsletter TemplateFrans Eduardus FrancoisNoch keine Bewertungen
- Speedlite 420exDokument13 SeitenSpeedlite 420exchrisground2010Noch keine Bewertungen
- ParaNorman BookletDokument36 SeitenParaNorman BookletChavatt Bautista100% (1)
- WPB 2Dokument4 SeitenWPB 2api-239856554Noch keine Bewertungen
- LM-770 - Ome - ManualDokument40 SeitenLM-770 - Ome - ManualGabriel Gonçalves50% (4)
- Ap Project Presentation (Ankur Yadav) 2K20 B8 10Dokument20 SeitenAp Project Presentation (Ankur Yadav) 2K20 B8 10Rapid recordsNoch keine Bewertungen
- Intraoral RadiographyDokument18 SeitenIntraoral RadiographyAnonymous k8rDEsJsU10% (1)
- Ov2640 DS PDFDokument47 SeitenOv2640 DS PDFpiramidon100% (1)
- Rendezvous Rendezvous: Brca, Iit Delhi Presents Brca, Iit Delhi PresentsDokument16 SeitenRendezvous Rendezvous: Brca, Iit Delhi Presents Brca, Iit Delhi PresentsHimanshu GaurNoch keine Bewertungen
- Advanced Amateur Astronomy PDFDokument415 SeitenAdvanced Amateur Astronomy PDFSmilind100% (3)
- Inventions CambodiaDokument4 SeitenInventions CambodiaInah Quiniquini ManaleseNoch keine Bewertungen
- RockefellerCenter A4 USDokument5 SeitenRockefellerCenter A4 USfernandosurferNoch keine Bewertungen
- Title of My FilmDokument17 SeitenTitle of My FilmSuji JeevaNoch keine Bewertungen
- Quiz in MAPEH 1,2, and 3Dokument5 SeitenQuiz in MAPEH 1,2, and 3Nika BuzonNoch keine Bewertungen
- ICT Proposal 2Dokument17 SeitenICT Proposal 2raynaNoch keine Bewertungen
- Smiledesign 160716170541Dokument74 SeitenSmiledesign 160716170541Aya Ibrahim YassinNoch keine Bewertungen
- Assignment 1 (Lect. 1-2) : DMET501 - Introduction To Media Engineering Winter 2010/11Dokument3 SeitenAssignment 1 (Lect. 1-2) : DMET501 - Introduction To Media Engineering Winter 2010/11Amr EhabNoch keine Bewertungen
- Track 18.mp3Dokument1 SeiteTrack 18.mp3Nur RohimNoch keine Bewertungen
- Phottix Odin Instruction ManualDokument97 SeitenPhottix Odin Instruction Manualpeccavi808Noch keine Bewertungen
- Joy Schmidt (Pople) November 1973: Soviet Scientists Discover New EnergyDokument4 SeitenJoy Schmidt (Pople) November 1973: Soviet Scientists Discover New EnergyJack FooNoch keine Bewertungen
- Tariff Finder - SampleDokument4 SeitenTariff Finder - SampleTrinca DiplomaNoch keine Bewertungen
- Dual LED Flasher 2Dokument4 SeitenDual LED Flasher 2Denzel T. LanzaderasNoch keine Bewertungen
- D 1501 Service Manual: DevelopDokument229 SeitenD 1501 Service Manual: DevelopJoel RodriguesNoch keine Bewertungen
- 1c Basics Camera Training 2009Dokument49 Seiten1c Basics Camera Training 2009Art Del R Salonga100% (2)