Beruflich Dokumente
Kultur Dokumente
Interpersonally Based Psychotherapies
Hochgeladen von
Nikko MelencionCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Interpersonally Based Psychotherapies
Hochgeladen von
Nikko MelencionCopyright:
Verfügbare Formate
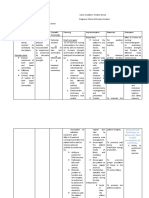
INTERPERSONALLY BASED PSYCHOTHERAPIES
PSYCHOTHERAPY any procedure that promotes the development of courage inner security
and self- confidence making the person more functional
- most important element is trust and communication
- a form of mental exploration should be individualized
General Types:
a. Supportive is indicated for the client with poor insight because he has fewer
resource and he is less intellectually capable. This includes guidance and
counseling, advising, education, etc
b. Uncovering or Insight includes exploring and bringing to consciousness the
source of repressed and suppressed conflict that operate unconscious level.
Forms of Psychotherapy:
a. One on one
Goal: to provide supportive relationship so that the individual is less threatened, help
client to function on higher level, to increase the individuals level of understanding of
himselfand his environment.
b. Group therapy - therapist with 10-12 clients in a group
Goal: to create sense of cohesiveness among group members to increase acceptance of
the group members and to increase social interaction
Focus : here and now, not the past
Group members should have similar problem
REMOTIVATION
Indication : repressed, long term hospitalized patients
Primary Aim: To stimulate thinking
Topics: Associated with the Real World, Topics should not touch the Wounded Areas of the
Patients Life
Steps;
a. Climate of Acceptance
-self introduction
-Objective: to establish rapport
b. Bridge of Reality
-start to select topic assisted with real world
-ask thought provoking questions
-use visual aid to motivate responses from members
-a poem may be read
c. Sharing the world we live in
d. Appreciation of the works of the world
-discussion is geared toward occupations Related to the main Topic
e. Climate of Appreciation
-Summary
-social amenities
-next meeting arrangements
THERAPEUTIC RELATIONSHIP
Therapeutic relationship
is a relationship that is established between a health care professional and a client for
the purpose of assisting the client to solve his problems
Components of a Therapeutic Relationship
a. Trust the nurse should be able to perceive and experience the feelings
of the patient to be able to understand the patient
develop when the trust is built in the nurse-client relationship. When
the nurse exhibits the following behavior: caring, openness, objectivity,
respect, interest, understanding, consistency, treating
the client as a human being, suggesting without telling, approachability,
listening, keeping promises, and honesty.
Congruence occurs when words and actions match.
b. Genuine Interest
this is manifested when the nurse is sincere and honest in her
relationship with the patient. Consistency conveys sincerity that in turn
foster the development of the patients trust. The nurse must maintain
an honest and open communication.
when the nurse is comfortable with himself or herself, aware of
His or her strengths and limitations, and clearly focused, the client
Perceives a genuine person showing genuine interest
self disclosure - the nurse willingness to share her own points of view
in a therapeutic manner can be an indication of genuineness, this
encourages the patient to become more open to the nurse in return.
c. Empathy
ability of the nurse to perceive the meanings and feelings
of the client and to communicate that understanding to client
Empathy is therapeutic but sympathy is not therapeutic because sympathy
is pity. Sympathy leads the patient to develop a poor me self concept.
therapeutic communication used are reflection, restatement and
Clarification.
d.Acceptance
the nurse who did not become upset or respond negatively to a
clientssoutbursts,anger, or acting out conveys acceptance to
the client. Avoiding judgments of the person, no matter what the
behaviour is acceptance.
e.Positive regard
the nurse who appreciates the client as a unique worthwhile human
being can respect the client regardless of his or behavior,
background, or lifestyle
Therapeutic use of self
By developing self awareness and beginning to understanding our
attitude, we can begin to use aspects of our personality, experiences,
values, feelings, intelligence, needs, coping skills, and perceptions to
establish relationships with clients.
Two Elements of Therapeutic Use of Self
1. Self-awareness
2. Self- disclosure
Self-Awareness
is the process of developing an understanding of ones own values, beliefs, thoughts,
feelings, attitudes, motivations, prejudices, strengths and limitations and how these
qualities affect others.
Nurses must clearly understand themselves to promote their clients growth and to
avoid limiting clients choices to those that nurses value.
One tool that is useful in learning more about oneself is the Johari window- which
creates a word portrait of a person in four areas and indicates how well that
person knows himself or herself and communicates with others.
Self Disclosure means revealing personal information such as biographical information and
personal ideas, thoughts and feelings about oneself to clients.
JOHARIs WINDOW: portrait of a self in 4 areas.
a. Open/Public Self qualities known by self and others
b. Blind/ Unaware Self qualities known only to others
c. Hidden/Private Self qualities known only to oneself
d. Area of the Unknown an empty quadrant to symbolize qualities as yet
undiscovered by oneself or others
Patterns of KNOWING:
Hildegard Peplau identified PRECONCEPTIONS, or ways one person expects
another to behave or speak, as a road block to the information of an authentic
relationship.
Patterns of Knowing accdng to Carper (1978)
i. Empirical Knowing (obtained from the science of nursing)
ii. Personal Knowing (obtained from life experiences)
iii. Ethical Knowing (obtained from the moral knowledge of nursing)
iv. Aesthetic Knowing (obtained from the art of nursing)
Types of Relationship:
1. Social Relationship initiated for the purpose of friendship, socialization,
companionship or accomplishment of task.
2. Intimate Relationship - involves two people who are emotionally committed to each
other. Include sexual or emotional intimacy as well as sharing of mutual goals.
3. Therapeutic Relationship focuses on the needs, experiences, feelings, and ideas of
the client only.
Therapeutic communication
Therapeutic Communication
is a process in which the nurse consciously influences a client or helps the client to a
better understanding through verbal or nonverbal communication. Therapeutic
communication involves the use of specific strategies that encourage the patient to
express feelings and ideas and that convey acceptance and respect.
a. Characteristics
1. Verbal >written/spoken
2. Non-verbal -> posture, tone of voice, facial expression
Types of Non-verbal communication:
a. Kinesis 1.body movement 2.eye contact 3.gestures
b. Paralanguage
1. voice quality
2. Non-language vocalization (crying, sobbing, moaning)
c. Proxemics law of space relationship
Intimate zone --- 0 to 18 inches
Personal zone ---- 18 to 36 inches
Social zone --------4-12 feet
Public zone --------12-25 feet
d. Touch
Types of Touch (Knapp,1980)
1. Functional-professional touch used to examinations or procedures
(assess skin turgor)
2. Social-polite touch used in greeting, such as a hand-shake and the air
kisses some womenuse to greet acquaintances, or when a gentle hand
guides someone in the correct direction.
3. Friendship-warmth touch hug in greeting, or the back slapping some men
use to greet friends and relatives
4. Love-intimacy touch - tight hugs and kisses between lovers or close
relatives.
5. Sexual arousal touch used by lovers
e. Cultural artifacts (bless, kiss the hand as expression of being thankful,
shake hands)
PHASES OF NPI or Nurse client Interaction:
1. Orientation Phase begins when the nurse and client meet and ends when the client begins
to identify problems to examine.
Nurse establish role, the purpose of meeting and the parameters of subsequent
meetings, identifies the client problem and clarifies expectations.
Before meeting,
reads the background materials available on the client;
be familiar with any medications the client is taking;
gathers necessary paper work and arranges for a quiet, private, and comfortable
position.
Consider his or her personal strengths and limitations
Nurse begins to build trust with the client.
Nurse should listen closely to the clients history, perceptions, and
misconceptions
Provide support and empathy of pts feelings
Major Task: to provide mutual agreement (contract)
2. Working Phase longest and most productive phase
identify perception to reality, support system and coping
mechanisms.
Two sub-phases :
a. identification the client identifies the issues or concerns causing the problems
b. exploitation the nurse guides the client to examine feelings and responses and to
develop better coping skills and a more positive image
Major Task: Identification and resolution of the patients problems.
Other Tasks:
a. maintaining the relationship
b. gathering more data
c. exploring perceptions of reality
d. developing positive coping mechanisms
e. promoting a positive self-concept
f. encouraging verbalization of feelings
g. facilitating behavior change
h. working through resistance
i. evaluating progress and redefining goals as appropriate
j. providing opportunities for the client to practice new behaviors
k. promoting independence
Problems:
Transference when the client unconsciously transfer to the nurse
feelings he or she has for significant others.
Countertransference occurs when the therapist displaces onto the
client attitudes or feelings from his or her past; process that can occur
when the nurse responds to the client based on personal, unconscious
needs and conflicts.
3. Termination Phase or the resolution phase (Final stage)
Begins when the problems are resolved, and it ends when the
relationship is ended.
Evaluate the summary of progress
Reinforce change and strength of the client
Give rewards for cooperation
Encourage about expression of feelings about termination of
relationship
Terminate the relationship without giving promises.
Roles of the nurse in Therapeutic Relationship
1.Teacher
2.Caregiver
3. Advocate ensuring privacy and dignity, promoting informed consent, preventing
unnecessary examinations and procedures, accessing needed services and benefits and
ensuring safety from abuse and exploitation and observant of other health care professionals.
Possible warnings or signals of abuse of the Nurse-Client Relationship (refer to Videbeck)
Therapeutic Techniques (Communication)
Technique Example
Accepting (conveys positive regard) Yes, that must have been difficult for you.
Broad openings (allows client to select the topic)
is there something youd like to talk about?
Acknowledge or giving recognition (acknowledging, indicating awareness)
I noticed that youve fixed your bed.
Asking direct questions How does your wife feel about you hospitalization?
Clarifying (striving to explain what is vague and searching for mutual understanding)
Im not sure that I understand what you are trying to say.
Confronting or presenting reality (clarifying misconceptions that client may be expressing)
I see no bats flying in this room.
Consensual validation (striving to explain what is vague and searching for mutual
understanding)
Tell me whether my understanding of it agrees with yours
Encouraging comparison (asking client to compare similarities and differences in ideas,
experiences, or interpersonal relationships)
Has this ever happened before?
Encouraging description (asking client to verbalize what is being perceived)
How do you feel when you take you medication?
Encouraging expression What are your feelings in regards to?
Encouraging evaluation Does participating in group therapy enable you
discuss your feelings?
Exploring (delving further into a subject, idea, experience, or relationship)
Tell me more about your job. Would you describe
your responsibilities?
Focusing (taking notice of a single idea or even a single word)
(assisting a patient to explore specific topic)
Giving broad openings (allows client to select the topic) or Asking open-ended questions
Is there something youd like to do?
Informing (giving needed facts) Ill be your nurse for today, from 7:00 until 3:00 this
afternoon.
Making observations (verbalizing what is observed or perceived)
You appear to be angry. / I noticed that youre trembling.
Offering general leads (encourages client to continue) Go on. / You were saying
Restating (lets client know whether an expressed statement has or has not been understood)
Client:I cant sleep, I stay awake all night.
Nurse:You cant sleep at night, (restating)
Summarizing During the past hour, we talked about your plans for
the future, they include...
Using silence (to induce thought, pacing, acceptance)
Validating (confirming ones observation)
So you mean.
Voicing doubt I find that hard to believe.
Non-Therapeutic Communication techniques
Agreeing and disagreeing (- implies that the nurse has the right to pass judgment on whether
clients ideas or opinions are right or wrong) I think you did the right thing.
Advice (implies that the nurse knows what is best for client and that client is incapable of any
self-direction) You should.
Belittling (causes client to feel insignificant or unimportant)
Dont be concerned, everyone feels like that.
Challenging But how can you be president of the United States?
Defending (- to defend what client has criticized implies that client has no right to express
ideas, opinions, or feelings)
All doctors here are simply great.
Disapproving (implies that the nurse has the right to pass judgment on the goodness or
badness of clients behavior) Thats bad.
Giving approval (implies that the nurse has the right to pass judgment on the goodness or
badness of clients behavior) Thats good, Im glad that
False reassurance Dont worry, everything will be all right
Focus on caregivers feeling I feel that way too.
Judging Its your own mistake.
Probing (pushing for answers to issues the client does not wish to discuss causes client to feel
used and valued only for what is shared with the nurse)
Now tell me about this problem, you know I have to find out.
Reassuring (may discourage client from further expression of feelings if client believes the
feelings will only be downplayed or ridiculed I wouldnt worry about that
Rejecting ( refusing to consider clients ideas or behavior)
Lets not discuss
Requesting an explanation (asking why implies that client must defend his or her behavior or
feelings) Why do you think that?
Testing Do you know what kind of hospital this is?
Using Denial (blocks discussion with client and avoids helping client identify and explore areas
of difficulty) Client: Im nothing
Nurse: Of course youre something
Several nonverbal behaviors have been designed to facilitate attentive listening.
S Sit squarely facing the client.
O Observe an open posture.
L Lean forward toward the client.
E Establish eye contact.
R Relax.
Techniques fostering Description
Offering self making self available and showing interest and
concern
Active listening paying close attention to verbal and non verbal
communication
Silenceplanned absence of verbal remarks to allow patient to
Think and say more
Empathy - recognizing and acknowledging patients feelings
Questioning using open ended question
General lead using neutral expression to encourage patient to
continue talking
Restating repeating the exact words of patients to remind them
Of what they said, to let them know that they are heard
Verbalizing the implied - rephrasing patients words to highlight
An underlying message
Clarification asking patient to restate, elaborate or give examples
ideas or feelings
Techniques fostering Analysis and Conclusions
Making observation commenting on what is seen or heard to encourage
discussion
Presenting reality offering a view of what is real and what is not without
Arguing with the patient
Encouraging description of perceptions asking for patients views of the
situations
Voicing doubt expressing uncertainty about the reality
Placing an event in time or sequence asking for relationships among
events
Encouraging comparisons asking for similarities and differences among
Feelings, behaviors and thoughts
Identifying themes asking patients to identify recurrent patterns in
Thoughts, feelings and behaviors
Summarizing reviewing main points and conclusions
Techniques fostering Interpretation of Meaning and Importance
Focusing pursuing a topic until its meaning or importance is clear
Interpreting providing a view of the meaning or importance of
something
Encouraging evaluation asking for patients views of the meaning or
importance of something
Techniques fostering Problem Solving and Decisions
Suggesting collaboration offering to help patients solve problems
Encouraging goal setting - asking patient to decide of the type of change
needed
Giving information providing information that will help patients make
better choices
Encouraging consideration of options asking patient to consider the pros
and cons of possible options
Encouraging decisionsasking patient to make a choice among options
Encouraging the formulation of plan probing for step-by-step actions
that will be needed
Ineffective or Inappropriate Responses and Behaviors
Not fully listening, not paying attention
Looking too busy, ignoring the patient
Seeming uncomfortable with silence, fidgeting
Being opinionated, arguing with the patient
Avoiding sensitive topics; changing the topic
Being superficial or using clich
Having a close posture; avoiding eye contact with the patient
Making false promises or reassurances
Giving advice or talking too much
Laughing or smiling inappropriately
Showing disapproval or being judgmental
Belittling feelings or minimizing problems
Being defensive or avoiding the patient
Making flippant or sarcastic remarks
Lying or being insincere
4. Goals in the one-to-one relationship
* Establish rapport with the client by being empathetic, genuine, caring, and
unconditionally accepting of if a the client regardless of his behavior or beliefs
* Actively listen to the client to identify the issues of concern and to formulate
a client-centered goal for the interaction.
* Gain an in-depth understanding of the clients perception of the issue, and
foster empathy in the nurse-client relationship.
* Explore the clients thoughts and feelings.
* Facilitate the clients expression of thought and feelings
* Guide the client to develop new skills in problem-solving.
* Promote the clients evaluation of solutions
INTERACTIONS WITH SELECTED BEHAVIOR:
Violent Behavior:
o Stay out of striking distance ( this also reduces the threat to the patient
o Avoid touching the patient without approval
o Change the topic temporarily if a patients behavior is escalating.
o Suggest time out for the patient in a quiet area with fewer stimuli.
o Avoid entering a room alone with a patient who is not in control of his
or her behavior
o Leave temporarily if the patient is agitated and asking to be left alone.
o Call for staff assistance if the s losing control.
Hallucinations:
o The initial approach with patients to be listening or talking with voices is to
o Comment on their behavior: You look as if you are listening to something.
What do you hear?
o If the patient acknowledges hearing something that the nurse cannot hear,
The nurse can say, I dont hear anything, tell me what you hear.
o After knowing the content, focusing the hallucination is unnecessary.
I know the voices are important to you, but lets talk about your
loneliness
****exception****
Delusions:
o The initial approach with respect to delusions is clarification of meanings.
Who do you think is trying to hurt you? or Tell me about this power
you think you have.
Conflicting Values:
o Help the patient examine the effects or outcomes of their belief on their
lives relationships, and happiness.
Severe Anxiety and Incoherent Speech Patterns:
o Clarify the meaning of situations
o In severely ill and/or anxious patients, it is more effective to key into
their feelings and underlying themes than trying to make sense on the
content of their speech.
Manipulation:
Common manipulations are a means to gain attention, sympathy, control and
Dependence. Manipulation is not often recognized until it has already worked.
The initial approach is to address what is happening (or has happened)
o Im getting the impression that you would like me to tell you what
to do. What scares you about this decision?
o You are experiencing a lot of emotional pain and would like to relieve it
for you. Lets talk about what you can do to relieve it.
o I see you asking for a lot of attention. What is it that you really want?
o Limit setting is useful for manipulative client. A ppower struggle with
patient is useless. Helping patient to express their needs directly to others
is more productive.
Crying:
o Unless crying is manipulative gesture and is prolonged or unproductive,
it should be allowed and even encourage, verbally and nonverbally. By
saying, Its ok to cry or quietly offering a tissue, the nurse gives patients
permission to cry and relieve tension. Privacy should be provided. The nurse
should be as quiet as possible until the crying has ceased. The patient
is then offered an opportunity to discuss the circumstance that precipated
the tears.
Sexual Innuendos or Inappropriate Touch
o Patients generally stop these behaviors when asked and should be reminded
that the actions are inappropriate.
o If the the behavior continue, then setting limits can be stronger: I want
to talk to you but not if you continue to touch me. If you dont stop,
I will have to leave and come back later.
Suspiciousness
o Communicate clearly, simply and congruently. Misinterpretations by
patients are clarified, but argument over differences in opinion are avoided.
o Simple rationales or explanations for rules, activities, occurences, noises,
and requests are offered regularly.
o Patients participation is encouraged but not forced, thus avoiding an
increase in their fears.
Hyperactivity
o Place the patient in a quiet area with minimal auditory and visual
Stimulation. The nurse must remain calm, speak slowly and softly,
and respect patients personal space.
o Directions are given in kind, simple, but firm manner.
CRISIS -> Turning point in an individuals life that produces an overwhelming emotional
response; individual is confronting life circumstance or stressor that cannot be managed
through customary coping strategies
Crisis
Caplan (1964) identified the stages of crisis:
1. The person is exposed to a stressor, experiences anxiety, and tries to cope in a
customary fashion
2. Anxiety increases when customary coping skills are ineffective
3. The person makes all possible efforts to deal with the stressor, including attempts at
new methods of coping
4. When coping attempts fail, the person experiences disequilibrium and significant
distress.
Phases of crisis Development
1. Denial- initial reaction
2. Increased tension the person recognizes the presence of crisis and continues to do
activities of daily living.
3. Disorganized- the person is preoccupied with the crisis and is unable to do ADL
4. Attempts to reorganize the individual mobilizes previous coping mechanisms.
Characteristics of crisis
1. Highly individualized
2. Last for 4-6 weeks
3. Person affected becomes passive and submissive
4. Affects a persons support system
Crisis intervention includes a variety of techniques based on the assessment of the individual
in crisis, to assist in resolution or management of the stressor or circumstance.
A way of entering into the life situation of an individual, family, group, or community
to help them mobilize their resources and to decrease the effect of a crisis inducing
stress
The primary role of the nurse in crisis intervention is to be active and directive, she
has to assist the patient.
Concept of Anxiety
Defining characteristics of Anxiety
A vague feeling of dread or apprehension; it is a response to external or internal
stimuli that can have behavioral, emotional, cognitive, and physical symptoms.
H. Peplau described the four levels of anxiety: mild, moderate, severe and panic.
STRESS
- pressure of varying degrees
- a mental and physical response to stressor
- is a wear or tear that life causes on the body
- occurs when a person has difficulty dealing with life situations, problems and goals.
- Accdng to Hans Selye, a psychological and physical response of the body that occurs
whenever we must adapt to changing conditions, whether those conditions be real or
perceived.
Types of Stress:
1. Distress stress due to an excess of adaptive demands placed upon us. (this is the Bad
stress) it lead to bodily and mental damage.
2. Eustress the optimal amount of stress which helps promote health and growth.
3. Psychophysiological Stress mental upset that triggers a physiological stress response.
It leads to psychosomatic illness. This is the most common type of stress and is the
major factor in the onset of psychosomatic illness.
STRESSOR->According to Selye, it is a positive or negative occurrence, or any emotion requiring
response.
2 Classification of Stressor:
1. Maturational stressor experiences that are expected as a part of normal processes of
growth and development in a given society.
2. Situational stressor less predictable and specific action are taken only when the threat is
eminent or the event has occurred.
Characteristics of Stress:
1. It is recurring
2. It is normal
3. It is brought about by stressor
4. It cannot be avoided
Hans Selyes STRESS ADAPTATION THEORY
Stress is the major cause of disease because chronic stress causes long-term
chemical changes.
1. Alarm Reaction impingement of stressor on individuals activates the preparation for
FLIGHT or FIGHT.
a. The Flight or Fight pathway is composed of three major areas:
Amygdala, Hypothalamus, and Midbrain (Limbic system)
b. Electrical stimulation of these areas elicits rage behavior or flight. Bilateral lesioning
(destroying the three major areas can have a calming effect.
Individuals experience an increase in alertness in order to focus on the immediate
task or threat and to mobilize resources and defenses to concentrate on a particular
stressor.
Levels of Anxiety Mild to moderate
Learning and Problem Solving can occur.
Pathophysiology:
Factor of Stress Message (nervous system) stimulate adrenal glands to secrete adrenaline
and norepinephrine for fuel and organs (liver to convert glycogen stores to glucose for food ) to
prepare for potential defense needs.
Too much adrenaline results in a surge of blood pressure that can damage blood vessels of
the heart and brain a risk factor in heart attack and stroke.
The excess production of the cortisol hormone can cause damage to cells and muscle
tissues. Stress related disorders and disease from cortisol include cardiovascular conditions,
stroke, gastric ulcers, and high blood sugar levels.
At this stage everything is working as it should you have a stressful event, your body
alarms you with a sudden jolt of hormonal changes, and you are now immediately equipped
with enough energy to handle it.
2. Stage of Resistance
Individuals strive to adapt to stress
Increase use of coping and defense mechanisms
Problem solving and learning are difficult but can be accomplished with assistance.
Psychosomatic symptoms begin to develop.
Level of Anxiety Moderate to severe
If overwhelmed experience next stage
Pathophysiology Digestive system reduces function to shunt blood to areas
needed for defense. Lungs take in more air and the heart beats faster and harder so
it can circulate highly nourished blood/ oxygenated blood to the muscles to defend
the body by Fight, FLIGHT or freeze behaviors.
3. Stage of Exhaustion
Result from the stress that last too long or it is overwhelming, or may result from the
individuals total inability to cope.
Anxiety Level Severe to Panic
Chronic stress can damage nerve cells in tissues and organs. Particularly vulnerable is the
hippocampus section of the brain. Thinking and memory are likely to become
impaired, with tendency toward anxiety and depression.
There can also be adverse function of the autonomic nervous system that contributes to
high blood pressure, heart disease, rheumatoid arthritis, and other stress related illness.
Defenses are EXAGGERATED AND DYSFUNCTION and personality becomes
DISORGANIZED, thinking illogical decision making ineffective.
DELUSIONS AND HALLUCINATIONS can occur with sensory misperception and greatly
reduced orientation to reality.
Individuals may become Violent, Suicidal or may be completely IMMOBILIZED.
DEATH may occur Body stresses are depleted
PROCESS OF ANXIETY
Stressor
l
Anxiety
l
Neurochemical/Physiological Reaction
l
Coping Behavior
(Adaptive, Palliative, Maladaptive, and Dysfunction)
COPING WITH ANXIETY
Type of
Coping
Description
Adaptive Solves the problem that is causing the anxiety, so the anxiety is decreased. The
patient is objective, rational and productive.
Palliative Temporarily decreases the anxiety but does not solve the problem, so the anxiety
eventually returns. Temporary relief allows the patient to return to problem
solving.
Maladaptive Unsuccessful attempts to decrease the anxiety without attempting to solve the
problem. The anxiety remains.
Dysfunctional Not successful in reducing anxiety or solving the problem. Even minimal
functioning becomes difficult, and new problems begin to develop.
MALADAPTIVE RESPONSES
Anxiety
A subjective experience that can be detected only by the subjective behavior that result
from it.
Alternating individuals to prepare for self defense.
A warning sign that person perceived danger, loss or threat
a. health or the ability to perform the function
b. self-esteem or self-respect
c. self- control
d. control or power over ones life
e. status or prestige
f. loved ones
g. freedom or independence
h. needs, goals, desires and expectations
i. resources (emotional, physical, financial, spiritual, social and cultural.
Theories of Origin/ Predisposing Factors:
Psychoanalytic View
Sigmund Freud (1969) identified two types of Anxiety
1. Primary Anxiety the traumatic state begins in the infant as a result of sudden
stimulation and trauma of birth. It is a state of tension or drive produced by external
causes.
2. Subsequent anxiety is the emotional conflict between two elements of the
personality. This anxiety is due to the conflict between the ID and Superego.
Interpersonal Views-
> Sullivan (1953), believed that through the close emotional bond between the mother and the
child, anxiety is first convey by the mother to the infant who responds as if the mothering
person were one unit.
- He also believed that anxiety in later life arises when a person perceives that he or she will be
viewed unfavorably or will lose the love of a valued person.
Behavioral View
Some theorist proposed that anxiety is a product of frustration caused by anything
that interferes with attaining a desired goal.
Anxiety may also arise through conflict that occurs when the person experiences
two competing drives and may choose between them.
It drives from 2 tendencies:
1. Approach (fight) tendency to do something or more toward something.
2. Avoidance (flight) is the opposite tendency; not to do something or not to move
toward something.
LEARNING Theories:
Parental influence affects how a child responds to anxiety. The parents appropriate
emotional response gives the child security and helps him learn constructive way of
coping on his own.
BIOLOGIC Theories
Genetic Theory
- First degree relatives of clients with increased anxiety have higher rates of developing
anxiety.
Neurochemical Theory
- Gamma-amino butyric acid (GABA) is the amino acid neurotransmitter believed to be
dysfunctional in anxiety disorders.
- GABA, an inhibitory neurotransmitter
= anti anxiety agent that reduces cell excitability, thus decreasing the rate of neuronal firing.
= GABA reduces anxiety and Norepinephrine increases it.
LEVELS OF ANXIETY and its NURSING MANAGEMENT:
1. MILD ANXIETY (Alertness Level +1) is a sensation that something is different and
warrants special attention.
Psychological Responses Physiologic Responses
- wide perceptual field
- sharpened senses
- increased MOTIVATION
- effective problem solving
- increased learning activity
- irritability
- restlessness
- fidgeting
- GI butterflies
- Difficulty sleeping
- Hypersensitivity to noise
Key Nursing Interventions:
a. Recognize the anxiety by statements such as I notice you being restless today.
b. Explore causes of anxiety and ways to solve problems that cause anxiety by statements
such as Lets discuss ways to ..
2. MODERATE ANXIETY (Apprehension Level +2) is the disturbing feeling that something
is definitely wrong.
Psychological Responses Physiological Responses
- Perceptual field narrowed to immediate task
- Selectively attentive
- Cannot connect thoughts or events
independently
- Increased use of automatisms
- muscle tension
- diaphoresis
- pounding pulse
- headache
- dry mouth
- high voice pitch
- faster rate of speech
- GI upset
- Frequent urination
Key Nursing Interventions:
a. Speak in short, simple and easy-to-understand sentences
b. Redirect client back to the topic if the client goes off on unrelated tangent.
Nursing Interventions:
Long Term Goal: helping the patient understand the cause of the anxiety and learn new ways of
controlling it.
a. Education
Knowledge on predisposing and precipitating stressors, coping resource and adaptive
and maladaptive response.
Beneficial aspects of mild levels of anxiety in motivating learning and producing growth
and creativity.
Treatments
b. Recognition of Anxiety
Help the patient recognize anxiety by exploring underlying feelings.
E.g.
Are you feeling anxious today?, Are you comfortable.
I noticed you have smoked 3 cigarettes since we started talking with your husband, are you
feeling anxious. ------validating and relate feelings to anxiety.
Trusting relationship
- Nurse should be warm, responsive listeners, gives patient adequate time to
respond and support patients self-expression, they will be less threatening.
c. Insight to the anxiety
Precedent of anxiety
What coping mechanism did the patient use
Provide outlets for anxiety: crying, talking
d. Coping with threat
Anxiety reduction relaxation training, desensitization
Cognitive restructuring existing alternatives
- Helping patient cope with negative thoughts and beliefs and recognizing other
viewpoints that will help them cope to more realistic conclusions (changing
irrational belief to rational belief)
Learning new behavior role playing, social skills training (promote relaxation response)
e. Provide anti-anxiety oral medications
3. SEVERE ANXIETY (Freefloating +3)
- creates a feeling that something bad is about to happen, or feeling of an impending doom.
Psychological Responses Physiological Responses
- fight and flight response sets in
- perceptual field reduced to one detail or scattered details
- cannot complete task
- Cannot solve problems or learn effectively
-behavior geared toward anxiety relief and is usually
ineffective
- doesnt respond to redirection
- feels awe, dread, or horror
- cries
- Ritualistic behavior
- uses maladaptive coping mechanism
- severe headache
- nausea, vomiting, and diarrhea
- Trembling
- rigid stance
- vertigo
- pale
- tachycardia
- chest pain
- dilated pupils and fixed vision
Nurses Goal:
To lower the persons anxiety level to moderate or mild before proceeding with anyone else
Key Nursing Interventions: Remain with the client.
SEVERE TO PANIC STAGE:
Nursing Interventions:
1. Establish a trusting relationship open, trusting relationship
Listen to patient and encouraged to discuss their feelings of anxiety, hostility,
guilt and frustration.
Should answer patient questions directly and offer unconditional acceptance.
Nurse should remain available and respect to patients personal space.
6-foot distance in small room may create the optimum condition for openness
and discussion of fears.
2. Nurses self-awareness
3. Protecting and assuring the patient of his or her safety
Determine the amount the patient can handle her stress
Do not attack patients coping mechanism
Do not argue with the patient
4. Modify the environment
Assume a calm, quiet manner and lower environmental stimulation
Limits the patient interaction with other client to minimize the contagious
feelings of anxiety.
5. Encourage activity
6. Medication IM anti-anxiety medications
4. PANIC ANXIETY ( +4) feelings of helplessness and terror
Psychological Responses Physiological Responses
- perceptual field reduced to focus on self
- cannot process any environmental stimuli
- distorted perceptions
- Loss of rational thought
- doesnt recognize potential problem
- cant communicate verbally
- possible delusions and hallucination
- may be suicidal
- may bolt and run or totally immobile and mute
- dilated pupils
- increased blood pressure and pulse
- Flight, fight, or Freeze
Key Nursing Interventions:
a. clients safety is the primary concern
b. Talk in a comforting manner even though the client cannot process what the nurse is
saying.
c. Go to small, quiet and non stimulating environment.
d. Reassure the client that it is just anxiety and that it will pass, and that he or she is in safe
place.
e. Remain with the client until panic recedes. (last from 5 to 30 minutes)
f. Administer anxiolytics.
Nursing Intervention that could increase Anxiety:
1. Pressuring the patient to change prematurely.
2. Being judgmental.
3. Verbally disapproving patients behavior.
4. Asking the patient a direct question that brings defensiveness.
TREATMENT STRATEGIES:
Cognitive Behavioral Treatment
Aims:
1. Increasing activity.
2. Reducing unwanted behavior
3. Increasing pleasure
4. Enhancing social skills
Anxiety Reduction
1. Relaxation Training decrease tension and anxiety.
- Basic premise is that muscle tension is related to anxiety
- Involves rhythmic breathing.
2. Systematic Relaxation involves relaxing voluntary muscles in an orderly sequence until
the body as a whole, is relaxed
Techniques: patient seated in a comfortable chair with presence of soft music or
pleasant visual cues----explain how anxiety is related to muscle tension----procedure
should be described----deep breathing and exhaling slowly ---tension relaxation begins.
3. Meditation
Components:
A quiet environment A comfortable position
A passive attitude A word or scene to focus on
4. Biofeedback
- electrodes connected to the machine are attached to the patients forehead---brain
waves, muscle tensions, temp, HR and BP ----the changes are communicated with the
patient by auditory or visual means
5. Systematic Desensitization
Example:
Construct a hierarchy of provoking or feared situations from 1 to 10, 1 is evoking little
and 10 evoking intense or severe anxiety.
In vitro, or imagined, desensitization, the patient proceeds with the imagined pairing of
hierarchy items with the relaxed state, progressing from the least anxiety-provoking
item to the most anxiety provoking item. ..(implosion)
In vivo, exposes the patient to real rather than imagined life situations(flooding)
6. Interoceptive Exposure
- Hierarchy is made of the specific symptoms that increase the patients anxiety.
7. Flooding patient is immediately exposed to the most anxiety-provoking stimulus
instead of exposing gradually or systematically to a hierarchy of feared stimuli.
Implosion imaginary event instead of a real life event.
8. Response Prevention
- This technique is based on the concept that repeated exposure to an anxiety-
producing stimulus without the presence of the anxiety reducing response will
lead to anxiety reduction because the feared consequence does not occur.
- Example: use of public restroom and engage in hand washing up to 20 times.
9. Eye Movement Desensitization --- Hypnosis
LEARNING NEW BEHAVIOR:
Modeling strategy used to form new behavior patterns, increase existing skills, or
reduce avoidance behavior in which the patient observes a person modeling adaptive
behavior and is then encourage to imitate it.
Shaping introduces new behaviors by reinforcing behaviors that approximate the
desired behavior.
Token Economy a form of positive reinforcement in which patients are rewarded for
performing desired target behavior with tokens that they can use for desired purchases
or activities.
Role Playing acting out of a particular situation.
Social Skills Training teaching smooth social functioning to those who do not manifest
social skills, using the principles of guidance, demonstration, practice, feedback,
resulting the acquisition of behaviors that will support community living.
Aversion Therapy reduces unwanted but persistent maladaptive behaviors by
applying an aversive or noxious stimulus when that maladaptive behavior occurs.
EX: Snap a rubber band on the wrist when being bothered by intrusive thoughts
Contingency Contracting a formal contract between the patient and the therapist
defining what behaviors are to be changed and what consequences follow the
performance of these behaviors.
ANTIANXIETY DRUGS:
Benzodiazepines are CNS depressant
Ex: a. Alprazolam (Xanax)
b. Chlordiazepoxide (Librium) f. Flurazepam (Dalmane) j. Triazolam (Halcion)
c. Clonazepam (Klonopin) g. Lorazepam (Ativan)
d. Chlorazepate (Tranxene) h. Oxazepam (Serax)
e. Diazepam (Valium) i. Temazepam (Restoril)
Pharmacologic Effect:
Side Effects: Dry Mouth, Ataxia, Dizziness and Drowsiness, Nausea, Withdrawal
symptoms (increased anxiety, flu-like symptoms and tremors)
ANXIETY DISORDERS
Anxiety disorders are diagnosed when anxiety no longer functions as a signal of danger or a
motivation for needed change but becomes chronic and permeates major portions of the
persons life, resulting in maladaptive behaviors and emotional disability.
- have many manifestations but anxiety is the key feature of each.
Prevalence:
- More prevalent in women, people younger than 45 years, people who are
divorced or separated and people of lower socioeconomic status.
Types of Anxiety Disorders:
Phobia
Panic Disorder
Obsessive-Compulsive Disorder (OCD)
Generalized Anxiety Disorder (GAD)
Acute Stress Disorder (ASD)
Post- Traumatic Stress Disorder (PTSD)
RELATED DISORDERS:
1. Anxiety Disorder due to a general medical condition.
2. Substance-induced Anxiety Disorder directly caused by drug abuse, a medication, or
exposure to a toxin.
3. Separation Anxiety Disorder- excessive anxiety concerning separation from home or from
persons/parents/caregivers to whom he is attached. ( occurs when it is no longer
developmentally appropriate and before 18 years of age).
4. Adjustment Disorder
GENERALIZED ANXIETY DISORDER
A person with GAD worries excessively and feels highly anxious at least 50% of the time
for 6 months or more
Has three or more of the following symptoms:
1. uneasiness 4. fatigue
2. irritability 5. difficulty thinking
3. muscle tension 6. sleep alterations
TREATMENT:
Buspirone (BuSpar)
SSRI antidepressants
POST TRAUMATIC STRESS DISORDER
Post traumatic Stress Disorder
Disturbing pattern of behavior demonstrated by someone who has experienced a
traumatic event.
Example: natural disaster, combat or an assault, threat or death or serious injury and
responded with intense fear, helplessness or terror.
3 Cluster of Symptoms:
1. Reliving the event persistently re-experiences the event through memories, dreams,
flashbacks or reactions to external cues about the event.
2. Avoiding the reminders of event.
3. Being on guard or hyper-arousal signs of increased arousal are the
following: insomnia, hyperarousal or hypervigilance, irritability or angry
outburst.
Symptoms occur 3 months or more after the trauma.
Can occur at any age including childhood
Dissociation is a subconscious defense mechanism that helps a person protects his or
her emotional self from recognizing the full effects of some traumatic event by allowing
the mind to forget or remove itself from the painful situation or memory.
Types of Dissociative disorders:
a. Dissociative Amnesia the client cannot remember important personal information
usually of a traumatic stressful nature.
b. Dissociative fugue the client has episodes of suddenly leaving the home or place at
work without any explanation, traveling to another city, and being unable to
remember his or her past or identity. He or she may assume a new identity.
c. Dissociative Identity Disorder (formerly, multiple personality disorder). The client
display two or more distinct identities or personality states that recurrently take
control of his/her behavior. This is accompanied by inability to recall important
personal information.
d. Depersonalization disorder the client has persistent or recurrent feelings of being
detached from his or her mental processes or body. This is accompanied by intact
reality testing; the client is not psychotic or out of touch with reality.
APPLICATION OF THE NURSING PROCESS:
Assessment:
A) Background:
Reveals that the client has the history of trauma or abuse
B) General Appearance and Motor Behavior:
Often appears hyper-alert and react to even small environmental noises with a startle
response.
Maybe very uncomfortable is the client too close physically and may require greater
distance or personal space.
May appear anxious or agitated and may have difficulty sitting still or may sit very still,
seemingly to curl up with arms around knees.
C) Mood and Affect
Nurse must remember that a wide range of emotions is possible, e.g. from passivity to
anger.
May appear frightened or scared, or agitated and hostile depending on his or her
experience.
When experiences a FLASHBACK, the patient appears terrified and may cry, scream or
attempt to hide or runaway.
When the client is DISSOCIATING, he or she may speak in different tone of voice or
appear numb with a vacant stare.
Report intense rage or anger or feeling dread inside and unable to identify any feelings
or emotions.
D) Thought Process and Content
Report reliving the trauma nightmares or flashbacks
Intrusive, persistent thought about the trauma interfere on client focus on ADL.
Report hallucinations or buzzing voices in their head
Report fantasies in which they take revenge on their abuser.
E) Sensorium and Intellectual Processes
Oriented to reality except if the client is experiencing flashback or dissociative episodes.
With Memory Gaps period for which they have no clear MEMORIES. May be short or
extensive and are usually related to the time of abuse or trauma.
F) Judgment and Insight
Clients ability to make decisions or solve problems may be impaired.
G) Self- Concept
Low Self-Esteem
Believe they are bad people who somehow deserve or provoke the abuse.
Think they are unworthy and damage
Think they are going crazy and are out of control with no hope of regaining control.
See themselves as helpless, hopeless, and worthless.
H) Roles and Relationships
Great deal or difficulty with all types of relationships.
Problems with authority figures- being unable to make directions from another or have
another monitor her performance.
Close relationship are difficult- because clients ability to TRUST is severely
compromises.
Avoidant behavior.
I) Physiologic Consideration
Difficulty sleeping
Overeating or lack of appetite
Use alcohol or other drugs.
DATA ANALYSIS
Risk for Injury
Anxiety
Situational Low Self Esteem (during Panic Attack)
Ineffective Coping
Poswerlessness
Ineffective Role Performance
Disturbed Sleep pattern
OUTCOME IDENTIFICATION
1. The client will be physically safe.
2. The client will distinguish between ideas of self harm and taking action on those ideas.
3. The client will demonstrate healthy, effective ways of dealing with stress.
4. The client will express emotions nondestructively.
5. The client will establish a social support system in the community.
INTERVENTION:
1. Promoting the clients safety priority.
Assess the client potential for self harm and suicide and take action accordingly.
Nurse and treatment team must provide safety measures when the client cannot do so.
Nurse can talk with the client about the difference between having self harm thoughts
and taking action on those thoughts
Help the client develop plan for going to safe place when having destructive thoughts or
impulses so that he or she can calm down and wait until they pass.
2.Helping the client cope with stress and emotions.
Use GROUNDING TECHNIQUE to help client who is dissociating or experiencing a
flashbacks.
Reorient the client by saying John, Im here with you, my name is Roland, Im the nurse
working with you today. You are in the hospital?, today is Monday, July 2, 2007. Can
you open your eyes and look at me? John, my name is Roland
Validates clients feeling of fear but try to increase contact to reality:
I know this is frightening to you, but you are safe now
What are you feeling?
What are you touching?
do you feel your feet on the floor?
During dissociative experience or flashback, help client change body position but do not
grab or force client to stand up.
Use supportive touch when client responds well to it.
Teach deep breathing and relaxation techniques
Use distraction techniques such as physical exercises, listening to music, talking with
others to engaging in a hobby or enjoyable activities.
Help to make a list of activities and keep materials client on hand to engage client when
feelings are intense.
1. Help the client promote in self-esteem.
Refer to client as survivor rather than a victim allows the client to think they are
strong enough to survive their ordeal.
Establish social support system in the community- local hotline crisis, friends and family.
Medication:
Paroxetine (Paxil)
Sertraline (Zoloft)
ACUTE STRESS DISORDER
Is similar to PTSD in that the person experienced a traumatic situation but the
response is more dissociative.
Onset is within 4 week after event and duration is 2 days to 4 weeks
Assessment:
History of exposure to traumatic event
Avoidance of stimuli related to trauma ( feelings, thoughts, people, conversations,
places, activities) and distress when exposed to reminders of the traumatic event.
Increased arousal or anxiety: sleep disturbance, hypervigilance, startle response,
irritability, decreased concentration.
Flashbacks re- experiencing and relieving the event through dreams, nightmares,
illusions.
Impairment in functioning occupational, social, family.
Dissociative symptoms:
a. absence of emotions, numbing, detachment- may not be able to show emotions
such as affection.
b. Daze decreased awareness of surroundings
c. Amnesia
d. depersonalization
Cross sensitization overreaction to other stimuli that resemble the original
traumatic event.
Defense Mechanism: denial, suppression, and repression.
Nursing Intervention:
1. Desensitization through gradual exposure to stressful stimuli.
2. Medications:
3. Nursing Interventions:
a. Strengthen survivors sense of control over their lives.
>Familiarizing the individuals with the symptoms of PTSD and their basis.
>Teaching coping skills that channel anger and manage stress.
>Assisting with activities of daily living (ADL) and basic self- care skills.
>Allowing the survivors to make as many decisions as possible, based on their ability.
b, Create a sense of safety.
c. Provide support. Help survivor to grieve over their losses so they can move forward in their
lives.
d. Assist in forming meaningful goals and connections with other people.
PANIC DISORDER
Composed of discrete episodes of panic attacks, that is 15-30 minutes of rapid, intense,
escalating anxiety in which the person experiences great emotional fears as well
physiologic discomfort.
Displays four or more of the following symptoms: palpitations, sweating, tremors,
shortness of breath, sense of suffocation, chest pain, nausea, abdominal distress,
dizziness, paresthesias, chills or hot flashes.
Panic disorder is diagnosed when a person has recurrent unexpected panic attack
followed by a least 1 month of persistent concern or worry about future attacks
Onset of panic disorder peaks in late adolescence and the mid-30s.
A person with panic disorder experiences this emotional and physiologic responses
without this stimulus.
TREATMENT:
Treated with COGNITIVE-BEHAVIORAL techniques deep breathing and relaxation and
medication such as:
e. SSRIs antidepressants (Selective Serotonin Reactive Inhibitors)
f. Tricyclic antidepressant
g. Benzodiazepines
h. Antihypertensive drugs (cataprespropanolol)
APPLICATION OF THE NURSING PROCESS:
Assessment
History:
Client usually seeks treatment for panic disorder after he or she has experienced several
panic attacks.
Client may report, I feel like Im going crazy, I thought I was having a heart attack, but
the doctor says its anxiety.
Usually the client cannot identify any trigger for these events.
General Appearance and Motor Behavior:
May appear entirely normal
Automatism automatic, unconscious mannerism, may be apparent..
Examples: tapping fingers, twisting hair- geared towards anxiety relief.
Moods and Affect
Anxious, worried, tense, depress, serious or sad.
Express anger at his or herself
Derealization (sensing that things are not real)
Thought Processes and Content
During a panic attack, the client may become overwhelmed, believing that he or she is
dying, losing control or going crazy.
May even consider suicide
Worry about the next panic attack
Sensorium and Intellectual Processes
May become confused and disoriented during the panic attack.
Self Concept
Client often make self-blaming statements such as I cant believe Im so weak and out
of control or I used to be a happy well-adjusted person.
Roles and Relationships
Typically avoids people, places and events associated with previous panic attack
Physiologic and self Care Concerns
With problems on sleeping and eating
Experience loss of appetite or eat constantly
OUTCOME IDENTIFICATION
1. The client will be free from injury.
2. The client will verbalize feelings
3. The client will sleep at least 6 hours per night.
4. The client will demonstrate use of effective coping mechanism.
5. The client will demonstrate effective use of methods to manage anxiety response
6. The client will verbalize a sense of personal control.
7. The client will establish adequate nutritional intake.
INTERVENTION:
Provide a safe environment and ensure clients privacy during the attack- if the
environment is over stimulating, the client should move into a less stimulating place (a
quiet place reduces anxiety and provides privacy for the client)
Remain in the client during a panic attack- to calm her down and to assess client
behaviors and concern.
Talk to client in a calm reassurance voice
Teach the client to use relaxation technique- deep breathing exercises, guided imagery
Help the client to use cognitive restructuring techniques.
Engage client to explore how to decrease stressors and anxiety-provoking situations.
OBSESSIVE-COMPULSIVE DISORDER
OBSESSION are recurrent, persistent intrusive and unwanted thoughts, images, or impulses
that cause markedly anxiety and interfere with interpersonal, social or occupational function.
COMPULSION are realistic or repetitive behaviors or mental acts that a person carries out
continuously in an attempt to neutralize anxiety.
Obsessive-compulsive disorder (OCD) is diagnosed only when these thoughts, images
and impulses consume the person or he or she is compelled to act out the behavior to a
point at which they interfere with personal, social and occupational function.
OCD can start in childhood especially in males
TREATMENT:
A. Behavior Therapy
Exposure- involves assisting the client to deliberately confront the situations and stimuli
that he or she usually avoids.
Response Prevention focuses on delaying or avoiding performance of rituals.
MEDICATION:
Clomipramine (Anafranil) a drug of choice, it decrease obsession and alleviate rituals.
APPLICATION OF THE NURSING PROCESS:
Assessment:
A. History:
Client usually seeks treatment only when obsession becomes too overwhelming,
compulsions interfere with daily living or both.
Most treatment is outpatient.
The client reports that rituals began many years before; some begin early as childhood.
B. General Appearance and Motor Behavior
Client seems tense, anxious, worried, and fretful.
Overall appearance is unremarkable; that is, nothing observable seems to be out of the
ordinary
C. Mood and Affect
Clients report ongoing, overwhelming feelings of anxiety is response to obsessional
thoughts, images, or urges.
Look sad and anxious.
D. Thought Processes and Content
Client describes the obsessions as arising from nowhere during the middle of normal
activities.
E. Sensorium and Intellectual Processes
There is intact intellectual functioning
The client may describe difficulty concentrating or paying attention when obsessions are
strong.
No impairment of memory or sensory functioning.
F. Judgment and Insight
Recognizes that obsession is irrational but he or she cannot stop them
Client can make sound judgment (I know the house is safe) but cannot act on them.
When anxiety overwhelms, client will engage in ritualistic behavior
G. Self Concept
Clients voices concern that he or she is going crazy.
There is feeling of powerlessness to control the obsession or compulsion that
contributes to low self-esteem.
H. Roles and Relationship
Relationship suffers as family and friends tire of repetitive behavior, and the client is less
available to them.
I. Physiologic and Self-Care Considerations
Have trouble sleeping
Loss of appetite or unwanted weight loss
Personal hygiene may suffer
OUTCOME IDENTIFICATION:
1. The client will complete daily routine activities within a realistic time frame.
2. The client will demonstrate effective use of relaxation techniques.
3. The client will discuss feelings with another person.
4. The client will demonstrate effective use of behavior therapy techniques.
5. The client will spend less time performing rituals.
INTERVENTION:
1. Offer encouragement, support, and compassion.
2. Be clear with the client that you believe he or she change.
3. Encourage the client to talk about feelings, obsessions and rituals.
4. Gradually decrease time for the client to carry out ritualistic behavior.
5. Assist the client to use exposure and response prevention behavioral techniques.
6. Encourage client to use techniques to manage and to tolerate anxiety responses.
7. Assist client to complete daily routine and activities.
PHOBIAS
Is an illogical, intense, persistent fear of a specific object or social situation that cause
extreme distress and interferes with normal functioning.
Usually do not result from past, negative experiences
3 Categories of phobia
1. Agoraphobia Acute anxiety on crowd and fear of being alone.
2. Specific phobia irrational fear of an object or situation
3. Social phobia anxiety provoked by certain social or performance situations.
Diagnosis of phobic disorder is made only when the phobic behavior significantly
interferes with the persons life by creating marked distress or difficulty in interpersonal
or occupational functioning.
Categories of Specific phobia:
1. Natural environmental phobias fear of storm, water, height, or other natural
phenomena.
2. Blood-injection phobia fear of seeing ones own or others blood, traumatic injury, or
an invasive medical procedure such as an injection.
3. Situational phobia- fear of being in a specific situation such as a bridge, tunnel, elevator,
small room, hospital or airplane.
4. Animal phobia fear of animal or insects (usually a specific type). Often this fear
develops in childhood and can continue through adulthood in both men and women.
Cats and dogs are the most common phobic objects.
5. Other types of specific phobias: for example, fear of getting lost while driving if not able
to make all right turns (and no left turns) to get to ones destination.
usually occur in childhood or adolescent.
Social Phobia is also known as social anxiety disorder.
Person becomes severely anxious to the point of panic or incapacitation when
confronting situations involving people.
Example: Making speech, attending a social engagement alone, interacting with the opposite
sex or with strangers, and making complaints.
Fear is rooted in low self esteem and concern about others judgment.
Fears on looking socially inept, appearing anxious, or doing something embarrassing
such as burping or spilling food.
Other social phobias: fear of eating in public, using public bathrooms, writing in public,
or becoming the center of attention.
Peak age of onset is middle adolescence.
TREATMENT:
1. Behavioral Therapy
Systematic Desensitization- in which the therapist progressively exposes the client to
the threatening object in a safe setting until the clients anxiety decreases.
Example: fear of flying, airplane, walk in the airport, taking a short ride in a plane.
Flooding form of rapid desensitization in which a behavioral therapist confronts the
client with phobic object (either a picture or the actual object) until it no longer
produces anxiety.
= Because the clients worst fear has been realized and the client did not die, there is a little
reason to fear the situation anymore.
= This method is highly anxiety producing and should be conducted only by a trained
psychotherapist under controlled circumstances and with the client consent.
2. MEDICATION:
No pharmacological intervention
PSYCHOPHYSIOLOGIC RESPONSES
Psychosomatic Disorders (Psychophysiologic Disorders)
= refer to disorders characterized by somatic complaints for which the organic
cause could be demonstrated and are the result of emotional conflict.
General Characteristics
1. Involves organ system innervated by the ANS.
2. Physiologic changes involved are those that usually accompany emotional response but
more intense autonomic nervous system sustained.
3. Symptoms are thus physiologic rather than symbolic, the effect being expressed through
the viscera.
4. May produce structural organic changes if psychosomatic symptoms persist.
5. Somatic symptoms afford generous secondary gains.
The nurse and other health team must never assume that patient with PPD are not sick.
Theories of psychopathology
1. Repressed conflict/events and leads to increase in the patients level of anxiety.
2. A certain personality type (type A) is particularly prone to the development of certain
physical illness.
3. This theory places emphasis on the symbolism of illness.
4. Organ weakness theory: All humans have one body system that is relatively less
healthy than the other.
5. Patient with psychophysiologic disorder often have needs for dependency, attention,
love and security.
* When these needs cannot be met the person clings unconsciously to this disability as means of
achieving satisfaction.
6. Psychophysiologic Disorders:
ORGAN/SYSTEM DISORDER
G.I.T - Peptic Ulcer
Cardiovascular - Essential hypertension
Respiratory - Bronchial asthma
Integumentary - ALLERGIC Dermatitis
Musculoskeletal - Arthritis
Masochistic Behavior
Concept in Giving Nursing Care
1. Persons who develop psychophysiologic disturbances have unconscious emotional
conflict that increases their anxiety and interferes with their effectively meeting their
needs.
2. The physical illness is the result of an expression of this unconscious conflict and serves
as a means of lowering anxiety level.
3. The physical illness is real in that those are demonstrable organic changes that may be
life-threatening.
Nursing Care:
1. The nurse must fully understand and accept the fact that these people are physically ill
and that these symptoms may reach in life-threatening proportion.
2. During the acute episode of illness meeting the physical needs of the client is for
primary importance.
3. It must be understood that many of the clients feelings unacceptable to him and
therefore acceptance of him and his feelings by the nurse is of primary importance.
4. The nurse carries out attitude that she believes the individual will get better if he merely
exerted more control over his emotion.
SOMATOFORM DISORDERS
= Expression of needs through body language: Symbolic repressed feeling is related with over-
excited organ. It is characterized as the presence of physical symptoms that suggest a medical
condition without a demonstrable organic basis. These are chronic and recurrent, so progress
toward treatment outcomes can be slow and difficult.
Coping Technique:
To gain attention * Punishing of self and others
Rationalization
3 Central features of Somatoform disorders:
1. Physical complaints suggest major medical illness but have no demonstrable organic basis.
2. Psychologic factors and conflicts seem important initiating, exacerbating, and maintaining
the symptoms.
3. Symptoms or magnified health concerns are not under the clients conscious control.
ETIOLOGY:
Psychosocial theorists believe that people with somatoform disorders keep stress,
anxiety, or frustration inside rather than expressing them outward. This is called
internalization.
When clients express these internalized feelings and stress through physical symptoms
is called Somatization
Internalization and Somatization are both unconscious defense mechanism
Physical symptoms worsen when they experienced another conflicts or emotional stress
The worsening of physical symptoms helps them to meet psychological needs for
security, attention, and affection through primary and secondary gains.
PRIMARY GAINS is the direct benefit clients experience such as relief from anxiety, conflicts,
or distress.
e.g. If the client is physically sick, she doesnt have to deal with problems with the children
SECONDARY GAINS is the personal benefit derived from illness, such as special attention or
comfort received from others.
e.g.receiving back rub, being brought tea or breakfast in bed.
Types of Somatoform:
1. Body Dysmorphic Disorder
-Preoccupation with an imagined or exaggerateddefect in physical appearance in a
normal appearing person. E.g. Nose is too large or the teeth
- common in both gender
2. Conversion Disorder (Conversion reaction)
- An unconscious process through which the anxiety is converted into physical and
physiologic symptoms. Usually unexplained sudden deficit of sensory or motor
function (blindness, paralysis)
- Key feature: la belle indifference - a seeming lack of concern or distress.
- tends to develop during adolescence or early adulthood but may occur at any
age.
- More common among women and occurs between 10 and 35 years of age
- Patients with this disorder may have feelings of guilt, unexpressed anger,
frustrations and low self esteem.
Nursing Intervention:
a. Focus on anxiety reduction symptoms will be relieved when anxiety is relieved.
- diversional activities and administration of anti-anxiety medications.
b. Matter of fact attitude.
c. Relaxation training
d. Psychotherapy
e. Hypnotherapy
c. Hypochodriasis
- Morbid preoccupation with body functions or fear of serious disease. Motive is
unrecognizable or unconscious. They may interpret normal body sensations as signs of
disease. Also known as Disease phobia
- fear that one has a serious disease (disease conviction).
- fear that one will get a serious disease (disease phobia)
- common in both gender
- occur at any age
Six Major Criteria:
1. Preoccupation with having a serious disease based on misinterpretation of
physical symptom.
2. This conviction that he is ill is maintained despite medical reassurance that
nothing is wrong.
3. Preoccupation that is not as intense or distorted as delusional disorder or as
restricted as body dysmorphic disorder.
4. Preoccupation that causes significant distress and impaired social and
occupational functioning.
5. Disorder duration of at least 6 months; and
6. The symptoms are not caused by anxiety, somatoform, and major depressive
disorders.
Nursing Intervention:
1. Establish trust and show empathy.
2. Reassure client and family that there is no medical illness by showing laboratory results,
x-ray findings, and other tangible evidence but acknowledge the symptoms as real for
the person and discuss with the patient that they are caused by a disease fear.
3. Exposure techniques.
4. Explore alternative coping skills-identity stressors.
5. Set limits on the time spent with the client because of the tendency of the client to
manipulate.
6. Do not provide secondary gain, do not focus on the symptoms during interaction with
the patient but encourage verbalization of feelings.
7. Diversional activity.
8. Medications SSRI (fluoxetine {prosac}, paroxetine {paxil}, and fluvoxamine maleate
{luvox}).
d. Somatization disorder (Briquets Syndrome)
Somatization
- is defined as the transference of mental experiences and states into bodily
symptoms.
Somatization Disorder
- Somatic complaints of several years duration for which medical attention has
been sought but that are apparently not due to any physical disorder.
- Occurs before age 30 and runs a chronic course.
- Common in women
- Characterized by multiple physical symptoms which includes a combination of
pain, gastrointestinal, sexual and pseudoneurologic symptoms.
DIAGNOSTIC Criteria:
onset of physical complaints before age 30
a history of pain affecting at least four different body parts
two or more GI symptoms
at least one sexual or reproductive system
at least one neurologic symptom (excluding pain)
the diagnosis is supported by the dramatic nature of the complaints and the patients
exhibitionistic, dependent, manipulative, and sometimes suicidal behavior.
***Undifferentiated somatoform disorder
Symptoms: Nausea and vomiting, intolerance to several different food, erectile/ejaculation
problems, irregular menses, excessive menstrual bleeding, blindness, seizures, deafness,
paralysis, difficulty swallowing/breathing, dissociative symptoms such as amnesia, Dizziness,
Shortness of breath, Dysmenorrhea and chest pain, headache, sexual intercourse
(dyspareunia), painful urination (dysuria).
Key Feature: La belle indifference
Nursing Intervention:
a. Usually, the treatment is calm, firm, supportive relationship.
b. Avoid judgmental approach and such comments as There is nothing wrong with
you, or Everything is alright.
c. Matter of fact manner about the diagnosis but acknowledge the symptoms as
real and distressing to the patient. Provide symptomatic care.
d. Provide empathy. Reassure that although he has an impairing condition, it is not
life threatening and inform the patient of the different therapies available
e. Set limits.
e. Pain disorder (Psychalgia)
- Primary physical symptom of pain, which generally is unrelieved by analgesics
and greatly affected by psychological factors in terms of onset, severity,
exacerbation, and maintenance.
- Commonly seen in medical practice, which occur in 4% to 9%
- Common in women
- Occur at any age
General Characteristic:
1. Physical symptoms without organic basis.
Examples: blindness, seizures, paralysis, anosmia, aphonia,
Coordination disturbance, Anesthesia or paresthesia
2. La Belle indifference Lack of concern regarding the severity of the above symptoms.
3. Doctor hopping
4. Excessive use of analgesic with minimal relief from pain
5. Assumption of an invalid role.
6. Impairment in social and occupational functioning due to pre-occupation with physical
complaints.
Nursing Intervention: Same as Conversion Disorder
Somatization = is defined as the transference of mental experiences and states into bodily
symptoms.
Somatization Disorder
- Somatic complaints of several years duration for which medical attention has
been sought but that are apparently not due to any physical disorder.
- Occurs before age 30 and runs a chronic course.
Symptoms: Nausea and vomiting, intolerance to several different food,
erectile/ejaculation problems, irregular menses, excessive menstrual bleeding, blindness,
seizures, deafness, paralysis, difficulty swallowing/breathing, dissociative symptoms such as
amnesia, Dizziness, Shortness of breath, Dysmenorrhea and chest pain, headache, sexual
intercourse (dyspareunia), painful urination (dysuria)
RELATED DISORDERS:
a. Malingering is the intentional production of false or grossly exaggerated
physical or psychological symptoms.
- motivated by external incentives such as avoiding work, evading criminal
prosecution, obtaining financial compensation, or obtaining drugs.
b. Factitious Disorder(Munchausen syndrome) occurs when a person
intentionally produces or feigns physical or psychological symptoms solely to
gain attention.
- People with factitious disorder may even inflict injury on themselves to receive
attention.
- A variation of factitious disorder is Munchausen syndrome by proxy, occurs when a
person inflicts illness or injury on someone else to gain the attention of emergency
medical personnel or to be a hero for saving the victim.
Coping Strategies:
a. Emotion-focused coping strategies
- Help clients relax and reduce feelings of stress
- Includes progressive relaxation, deep breathing, guided imagery, and distractions
such as music or other therapies
- (does not eliminate their pain or physical symptoms; rather, the focus is helping
them to manage or diminish the intensity of the symptoms.)
b. Problem-focused coping strategies
- Help to resolve or solve the clients behavior or situation or manage life
stressors.
- Includes learning problem-solving methods, applying the process to identified
problems, and role playing interactions with others
SLEEP DISORDERS
- Is a medical disorder of the sleep patterns of a person or animal. Some sleep
disorders are serious enough to interfere with normal physical, mental and
emotional functioning.
- Polysomnography is a test commonly ordered for some sleep disorders.
PHYSIOLOGY OF SLEEP:
NREM stage 1: This is a stage between sleep and wakefulness. The muscles are active,
and the eyes roll slowly, opening and closing moderately.
NREM stage 2: theta activity In this stage, it gradually becomes harder to awaken the
sleep
NREM stage 3: Formerly divided into stages 3 and 4, this stage is called slow-wave sleep.
The sleeper is less responsive to the environment; many environmental stimuli no
longer produce any reactions.
REM: The sleeper now enters rapid eye movement (REM) where most muscles are
paralyzed. REM sleep is turned on by acetylcholine secretion and is inhibited by neurons
that secrete serotonin. This level is also referred to as paradoxical sleep because the
sleeper is harder to arouse than at any other sleep stage. Vital signs indicate arousal and
oxygen consumption by the brain is higher than when the sleeper is awake. An adult
reaches REM approximately every 90 minutes, with the latter half of sleep being more
dominated by this stage. The function of REM sleep is uncertain but a lack of it will
impair the ability to learn complex tasks.
TYPES OF SLEEP DISORDERS
1.Primary insomnia: Chronic difficulty in falling asleep and/or maintaining sleep when no other
cause is found for these symptoms.
2.Bruxism: Involuntarily grinding or clenching of the teeth while sleeping.
3. Delayed sleep phase syndrome (DSPS): inability to awaken and fall asleep at socially
acceptable times but no problem with sleep maintenance, a disorder of circadian rhythms.
(Other such disorders are advanced sleep phase syndrome (ASPS), non-24-hour sleep-wake
syndrome (Non-24), and irregular sleep wake rhythm, all much less common than DSPS, as well
as the transient jet lag and shift work sleep disorder.)
4. Hypopnea syndrome: Abnormally shallow breathing or slow respiratory rate while sleeping.
5. Narcolepsy: Excessive daytime sleepiness (EDS) often culminating in falling asleep
spontaneously but unwillingly at inappropriate times.
6. Cataplexy: a sudden weakness in the motor muscles that can result in collapse to the floor.
7. Night terror: Pavornocturnus, sleep terror disorder: abrupt awakening from sleep with
behavior consistent with terror.
8. Parasomnias: Disruptive sleep-related events involving inappropriate actions during sleep;
sleep walking and night-terrors are examples.
9. Periodic limb movement disorder (PLMD): Sudden involuntary movement of arms and/or
legs during sleep, for example kicking the legs. Also known as nocturnal myoclonus. See also
Hypnic jerk, which is not a disorder.
10. Rapid eye movement behavior disorder (RBD): Acting out violent or dramatic dreams while
in REM sleep, sometimes injuring bed partner or self (REM sleep disorder or RSD)
11. Restless legs syndrome (RLS): An irresistible urge to move legs. RLS sufferers often also
have PLMD.
12. Situational circadian rhythm sleep disorders: shift work sleep disorder (SWSD) and jet lag.
13. Sleep apnea, obstructive sleep apnea: Obstruction of the airway during sleep, causing lack
of sufficient deep sleep, often accompanied by snoring. Other forms of sleep apnea are less
common. When air is blocked from entering into the lungs, the individual unconsciously gasps
for air and sleep is disturbed. Stops of breathing of at least ten seconds, 30 times within seven
hours of sleep, classifies as apnea.
14. Sleep paralysis: is characterized by temporary paralysis of the body shortly before or after
sleep. Sleep paralysis may be accompanied by visual, auditory or tactile hallucinations. Not a
disorder unless severe. Often seen as part of narcolepsy.
15. Sleepwalking or somnambulism: Engaging in activities that are normally associated with
wakefulness (such as eating or dressing), which may include walking, without the conscious
knowledge of the subject.
16. Nocturia: A frequent need to get up and go to the bathroom to urinate at night. It differs
from Enuresis, or bed-wetting, in which the person does not arouse from sleep, but the bladder
nevertheless empties.[3]
17. Somniphobia: A cause of sleep deprivation. Somniphobia is a dread/ fear of falling asleep or
going to bed. Signs of illness include anxiety and panic attacks during attempts to sleep and
before it.
18. Kleine-Levin syndrome or Sleeping Beauty syndrome is a neurological disorder
characterized by recurring periods of excessive amounts of sleeping and eating. At the onset of
an episode the patient becomes drowsy and sleeps for most of the day and night
(hypersomnolence), waking only to eat or go to the bathroom. When awake, the patients
whole demeanor is changed, often appearing spacey or childlike
Treatments for sleep disorders generally can be grouped into four categories:
Behavioral and psychotherapeutic treatment
Rehabilitation and management
Medication
Other somatic treatment
PERSONALITY DISORDERS
Personality
Includes perceptions, attitudes and emotions
Personality can be defined as an ingrained enduring pattern of behaving and relating to
self, others, and the environment.
Personality Disorders
Diagnosed when personality traits become inflexible and maladaptive and significantly
interfere with how a person functions in society or cause the person emotional distress.
Long standing because personality characteristics do not change easily
Diagnosis of PD is based on two or more deviations on the following
1. Ways of perceiving and interpreting self, other people, and events. (cognition)
2. Range, intensity, lability, and appropriateness of emotional response (affect)
3. Ability to control impulses or express behavior at the appropriate time and place
(impulse control)
Categories of Personality Disorders Based on DSM IV-TR
Cluster A includes people whose behavior appear odd or eccentric and includes
paranoid, schizoid, and schizotypal personality disorders.
Cluster B includes people who appear dramatic, emotional or erratic and includes
antisocial, borderline, histrionic, and narcissistic personality disorders.
Cluster C includes people who appear anxious or fearful and includes avoidant,
dependent, and obsessive-compulsive personality disorders.
Onset and Clinical Course:
- Common, occurring in 10% to 13% of the general population
- Higher in lower socioeconomic groups
- Treatment resistant
ETIOLOGY
Biologic Theories
Compose of temperament and character
Temperament refers to biologic processes of sensation, association, and motivation that
underlie the integration of skills and habits based on emotion.
- Temperament is about our habit systems (which roughly equates to the ancient
Greek concept of the "four humors") namely:
Traits :
1. Harm avoidance - The fear system that mediates responding to punishment and pain.
2. Novelty seeking - Looking for pleasure, which leads to rage when frustrated.
3. Reward dependence - Allows us to be sensitive to social cues that in turn allows social
intimacy.
4. Persistence - Allows us to deal with expectations about whether we will get rewarded
or not. We see it in very conscientious people.
FOUR TEMPERAMENT TRAITS
PSYCHODYNAMIC THEORIES
Character consists of concepts about the self and the external world.
THREE MAJOR CHARACTER TRAITS:
High: hardworking, and
ambitious overachievers who
respond to fatigue or frustration
as personal challenge,
perseverance
Low: inactive, indolent, unstable
and erratic
High : tender-hearted, sensitive,
sociable,, and socially dependent
Low : practical, tough minded, cold,
socially insensitive, and indifferent
to being alone. social withdrawal,
detachment, aloofness, and
disinterest
High: high tempered, curious,
easily bored, impulsive,
extravagant, disorderly. may be
easily bored abd distracted, prone
to angry outburst and fickle in
relationship
Low slow tempered, stoic,
reflective, frugal, reserved,
orderly, and tolerant of
monotomy
High: fear of uncertainty,
social inhibition, shyness with
strangers, rapid faigability
and pessimistic.
Low:carefree, energetic,
outgoing and optimistic
Harm
Avoidance
Novelty
Seeking
Persistence
Reward
Dependence
High: realistic and effective and can adapt their behavior to
achieve goals
Low: blaming, helpless,irresponsible, and unreliable
SELF DIRECTEDNESS
(is the extent to which a person is
realistic, reliable, resourceful, goal-
oriented and confident)
High: empathic, tolerant,compassionate, supportive, and
principled
Low: self-absorbed, intolerant, critical, unhelpful,revengeful, and
opportunistic
COOPERATIVENESS
(refers to the extent to which a person
sees himself or herself as an integral
part of human society)
High: spiritual, unpretentious, humble and fulfilled
Low: practical, self-conscious, materialistic and controlling,
difficulty accepting suffering, loss of control, personal and
material losses, and death
SELF-TRANSCENDENCE
(describes the extent to which a
person considers himself or herself to
be an integral part of the universe
Signs and symptoms of cluster A (odd, eccentric) personality disorders
Paranoid personality disorder
Suspiciousness and mistrust of people characterize the person with a paranoid disorder
Interpret the action of others as personal threats, which results in increase anxiety and
the need for defensiveness
Belief that others are lying, cheating, exploiting or trying to harm you
Perception of hidden, malicious meaning in benign comments
Inability to work collaboratively with others
Emotional detachment
Hostility toward others
Sometimes with ideas of reference, have a blunted affect
Capable of close relationships with a select few, however, they might be suspicious or
jealous of those close to them
Unique Causes: some evidence has suggested that it tends to occur in biologic relatives
of identified patients with schizophrenia.
More common in men than women
0.5%-2.5% of the general population
Defense Mechanism Used: Projection
Nursing Interventions:
Approach in a formal, business-like manner and refrain from social chitchat or jokes
Involve in formulating their plans of care
Teach client to validate ideas before taking action.
Schizoid personality disorder
People schizoid personalities do not want to be involved in interpersonal or social
relationships and keep people at an emotional distance.
Fantasizing rich and extensive
Extreme introversion self absorbed and loner
Emotional distance, even from family members lack of desire for involvement with
others in all aspects of life.
Solitary activities are more gratifying compared to real persons and social situations
Fixation on your own thoughts and feelings indecisive and lack future goals and
direction
Emotional detachment marked difficulty experiencing and expressing emotions
particularly anger and aggression
Occurs 0.5% - 7% of the general population
Nursing Interventions:
Improve clients functioning in the community
- Nurse can make referrals to social services or appropriate local agencies for assistance.
Assist client to find case manager that can help the client to obtain services and health
care, manage finances, and so on.
Schizotypal Personality Disorder
Appear similar to patients with mild schizophrenia and do not meet enough of the
criteria to be diagnosed with psychosis or schizophrenia
These patients have problems in thinking, perceiving, and communicating
Indifference to and withdrawal from others
"Magical thinking (experience transient psychotic episodes in response to stress) the
idea that you can influence people and events with your thoughts
Odd appearance, elaborate style of dressing (unkempt, clothes often ill-fitting, do not
match and stained and dirty), speaking (coherent but may be loose and bizarre) and in
interacting with others
Belief that messages are hidden for you in public speeches and displays
Suspicious or paranoid ideas anxious to strangers
Paranoid ideation, ideas of reference, and odd beliefs are some of the most prevalent
and unchangeable criteria for this disorder
3%-5% of the population; slightly common in men than women
Unique Causes: A family with Schizophrenia are at risk for developing this disorder
Nursing Interventions
Development of self-care skills
Improve community functioning
- Ask client to make a list of people in the community with whom they must have contact
(telephone or written)
Social skills training to help clients to talk clearly with others and to reduce bizarre
conversations.
Signs and symptoms of cluster B (dramatic, emotional) personality disorder
Histrionic personality disorder
2-3% of the gen.popul.
Excessive sensitivity to others' approval
Attention-grabbing, often sexually provocative clothing and behavior
- Speech is usually colorful and theatrical, full of superlative adjectives
Excessive concern with your physical appearance
False sense of intimacy with others refer almost all acquaintances as dear
Constant, sudden emotional shifts
Have variety of vague physical complaints or relate exaggerated versions of physical
illness
Nursing Interventions:
Teach social skills
Provide factual feedback about behavior should focus on appropriate alternatives, not
merely criticism
Narcissistic personality disorder
1-2% in general population; mostly in men
Inflated sense of and preoccupation with your importance, achievements and talents
(sense of entitlement)
Constant attention-grabbing and admiration-seeking behavior
Inability to empathize with others
Excessive anger or shame in response to criticism
Manipulation of others to further your own desires
Nursing Interventions:
Matter-of-fact approach
Teach client any needed self-care skills.
Antisocial (formerly, sociopathic, psychopathic or dyssocial personality disorder)
personality disorder
The main feature is a pattern of disregard for the rights of others, which is usually
demonstrated ny repeated violations of the law
Only 3% of the general population; common in men
Onset: is in childhood and adolescence
Hx: childhood= enuresis, sleep walking and syntonic act of cruelty
- adolescence engaged in lying, vandalism, sexual promiscuity
Chronic irresponsibility and unreliability and substance abuse
Lack of regard for the law and for others' rights
Persistent lying and stealing
Aggressive, often violent behavior
Lack of remorse for hurting others
Lack of concern for the safety
Unique Causes:
a. Influence of genetics and the environment
b. Biologic findings has a weak response to stress in the autonomic nervous system,
as evidenced by low heart rate and lack of increase level of anxiety.
c. Brain scan indicate dysfunction in the prefrontal cortex, frontal temporal
and amygdala-hippocampal regions of the brain
Nursing Intervention:
1. Stating the behavioral limit (describing the unacceptable behavior)
2. Identifying the consequences if the limit exceeded
3. Identifying the expected or desired behavior.
Confrontation (matter-of-fact)
- Point out problem behavior
- Keep client focused on self
Teach the client to solve problems effectively and manage emotions of anger and or
frustration
Problem Solving Skills:
1. Identifying the problem
2. Exploring alternative solutions and related consequences
3. Choosing and implementing alternatives
4. Evaluating the results.
Borderline personality disorder
Features include emotional dysregulation, anger, impulsivity, unstable relationships,
identity or self image disturbance, abandonment, fears, self mutilation, and suicidality
With history of childhood sexual abuse
About 2-3% of the general population, 3x common in women
8-10% commit suicide
Five times more common in those with first-degree relative
Difficulty controlling emotions or impulses
Frequent, dramatic changes in mood, opinions and plans
Stormy relationships involving frequent, intense anger and possibly physical fights (tend
to idealize and adore others)
Fear of being alone despite a tendency to push people away-tend to use traditional
objects
Feeling of emptiness inside
Tend to have psychotic features during intense stress
Suicide attempts or self-mutilation (cutting, burning, and severe skin scratching)
Unique causes:
a. Heriditary
b. Environmental factor (chaotic home environment such as emotional discord In the
family, neglect of the childs feelings and needs and verbal, emotional, physical and
sexual abuse.
c. Neuroimaging studies indicate a weakening of the pre-frontal cortex.
Nursing Interventions
a. Promoting clients safety
- No-self-harm contract
- Safe expression of feelings and emotions
b. Helping the client to cope and control emotions
- identifying feelings
- Journal entries
- Delaying gratification
c. Cognitive restructuring techniques
- Thought stopping and decatastrophising
d. Limit setting and confrontation
Psychopharmacology:
Three Domains:
a. Cognitive- perceptual symptoms (include transitory hallucinations, suspiciousness,
paranoid thinking and delusions)
- Low dose, typical and atypical antipsychotics for 3 to 12 weeks to decrease symptoms
b. Affective or emotional dysregulation (
c. Impulsive-behavioral dyscontrol
Signs and symptoms of cluster C (anxious, fearful) personality disorders
Avoidant personality disorder
Hypersensitivity to criticism or rejection
Self-imposed social isolation (reluctant to anything perceived risky)
Extreme shyness in social situations, though you strongly desire close relationships
Nursing Interventions:
Support and reassurance
Cognitive restructuring
Reframing and decatastrophising
Promote self-esteem
Dependent personality disorder
15% of the population; 3x more often in female
Excessive dependence on others to meet your physical and emotional needs
Tolerance of poor, even abusive treatment in order to stay in relationships
Unwillingness to independently voice opinions, make decisions or initiate activities
Intense fear of being alone
Urgent need to start a new relationship when one has ended
Nursing Interventions:
Foster clients self-reliance and autonomy
Teach problem solving and decision making skills
Cognitive restructuring technique
Obsessive-compulsive personality disorder
Excessive concern with order, rules, schedules and lists
Perfectionism, often so pronounced that you can't complete tasks because your
standards are impossible to meet
Inability to throw out even broken, worthless objects
Inability to share responsibility with others
Inflexibility about the "right" ethics, ideas and methods
Compulsive devotion to work at the expense of recreation and relationships
Financial stinginess
Discomfort with emotions and aspects of personal relationships that you can't control
Nursing Interventions
Encourage negotiation with others
Assist client to make timely decisions and complete work
Cognitive restructuring technique
Depressive Personality Disorder
Char. by a pervasive pattern of depressive cognitions and behaviors in various contexts.
Occurs equally in both female and male
Similar behavior with MDD, but less severe
Nursing Interventions
Assess whether there is risk for self-harm
Encourage to involve in activities or engaged with others.
Provide factual feedback
Promote self esteem
Passive-Aggressive Personality Disorder
- 1-3% of the general population
- Slightly , prevalent in female than male
- Love procrastinate
- Express anger through passivity
Medications:
Antidepressants. Doctors commonly prescribe selective serotonin reuptake inhibitors
(SSRIs), such as fluoxetine (Prozac, Sarafem), sertraline (Zoloft), citalopram (Celexa),
paroxetine (Paxil), nefazodone, and escitalopram (Lexapro), or the related
antidepressant venlafaxine (Effexor) to help relieve depression and anxiety in people
with personality disorders. Less often, monoamine oxidase inhibitors such as phenelzine
(Nardil) and tranylcypromine (Parnate) may be used
Anticonvulsants. These medications may help suppress impulsive and aggressive
behavior. Your doctor may prescribe carbamazepine (Carbatrol, Tegretol) or valproic
acid (Depakote). Your doctor may also prescribe topiramate (Topamax), an
anticonvulsant that's being studied as an aid in managing impulse-control problems
Antipsychotics. People with borderline and schizotypal personality disorders are at risk
of losing touch with reality. Antipsychotic medications such as risperidone (Risperdal)
and olanzapine (Zyprexa) can help improve distorted thinking. For severe behavior
problems, doctors may prescribe haloperidol (Haldol).
Other medications. Doctors sometimes prescribe anti-anxiety medications such as
alprazolam (Xanax) and clonazepam (Klonopin) and mood stabilizers such as lithium
(Eskalith, Lithobid) to relieve symptoms associated with personality disorders.
Das könnte Ihnen auch gefallen
- Africa Case StudyDokument15 SeitenAfrica Case StudyNikko MelencionNoch keine Bewertungen
- TractionDokument19 SeitenTractionNikko Melencion0% (1)
- Americaa Case StudyDokument27 SeitenAmericaa Case StudyNikko MelencionNoch keine Bewertungen
- OxygenationDokument116 SeitenOxygenationCyndie Reyes LadladNoch keine Bewertungen
- CD Summer Review 1Dokument157 SeitenCD Summer Review 1Nikko MelencionNoch keine Bewertungen
- Meningioma Brain TumorDokument5 SeitenMeningioma Brain TumorNikko Melencion100% (1)
- Presentation For PROPOSALDokument12 SeitenPresentation For PROPOSALNikko MelencionNoch keine Bewertungen
- OxygenationDokument116 SeitenOxygenationCyndie Reyes LadladNoch keine Bewertungen
- Urinary 2Dokument44 SeitenUrinary 2Nikko MelencionNoch keine Bewertungen
- The patient's breathing has improved. She is able to take deep breaths without difficulty and her respiratory rate has decreased. Lung sounds are clearDokument42 SeitenThe patient's breathing has improved. She is able to take deep breaths without difficulty and her respiratory rate has decreased. Lung sounds are clearNikko MelencionNoch keine Bewertungen
- Concept On Oxygenation: Gas TransportDokument135 SeitenConcept On Oxygenation: Gas TransportNikko MelencionNoch keine Bewertungen
- Urinary 4Dokument22 SeitenUrinary 4Nikko MelencionNoch keine Bewertungen
- Liver Cirrhosis: Nikko G. MelencionDokument38 SeitenLiver Cirrhosis: Nikko G. MelencionNikko MelencionNoch keine Bewertungen
- N104semi Kenafafal FaDokument144 SeitenN104semi Kenafafal FaNikko MelencionNoch keine Bewertungen
- Acute BronchitisDokument38 SeitenAcute BronchitisNikko MelencionNoch keine Bewertungen
- AppendectomyDokument2 SeitenAppendectomyJoshua Triumfante De Vera IIINoch keine Bewertungen
- Grand Case EeDokument18 SeitenGrand Case EeNikko MelencionNoch keine Bewertungen
- Endocrine 3Dokument26 SeitenEndocrine 3Nikko MelencionNoch keine Bewertungen
- OxygenationDokument116 SeitenOxygenationCyndie Reyes LadladNoch keine Bewertungen
- Nursing Care Plan Nursing Diagnosis Anxiety (Mild)Dokument4 SeitenNursing Care Plan Nursing Diagnosis Anxiety (Mild)yvenette_kris871881% (27)
- NCP of Impaired MobilityDokument3 SeitenNCP of Impaired MobilityHazel Cabrera0% (1)
- Coping with breast cancer mastectomyDokument2 SeitenCoping with breast cancer mastectomyhaniehaehae93% (14)
- Nursing Care Plan Nursing Diagnosis Anxiety (Mild)Dokument4 SeitenNursing Care Plan Nursing Diagnosis Anxiety (Mild)yvenette_kris871881% (27)
- Digestive System5Dokument47 SeitenDigestive System5Nikko MelencionNoch keine Bewertungen
- Drug StudyDokument4 SeitenDrug StudyBobot Julius Oropeza100% (2)
- D Received Patient Sitting On Bed With Bottle # 1DDokument24 SeitenD Received Patient Sitting On Bed With Bottle # 1DMai Love100% (4)
- Concept On Oxygenation: Gas TransportDokument135 SeitenConcept On Oxygenation: Gas TransportNikko MelencionNoch keine Bewertungen
- Dengue Fever in The Philippines1Dokument23 SeitenDengue Fever in The Philippines1Nikko MelencionNoch keine Bewertungen
- Acute Abdominal Pain MS LectureDokument63 SeitenAcute Abdominal Pain MS LectureNikko MelencionNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Transkrip StressDokument26 SeitenTranskrip StressPrasetyo Hendy KurniawanNoch keine Bewertungen
- Fight & Flight ResposneDokument29 SeitenFight & Flight ResposneMohamed ElnadyNoch keine Bewertungen
- Academic Test3 PDFDokument13 SeitenAcademic Test3 PDFharry_potter3133% (3)
- CH 3 Stress and Its EffectsDokument7 SeitenCH 3 Stress and Its Effectscd_vyneNoch keine Bewertungen
- Child Abuse and Stress Disorders PDFDokument121 SeitenChild Abuse and Stress Disorders PDFFrescura1Noch keine Bewertungen
- PYC1501 Unit 9 Emotions OER 2022Dokument17 SeitenPYC1501 Unit 9 Emotions OER 2022aliiqsaanNoch keine Bewertungen
- Elc 501 - Outline For Forum Discussion - Latest RevisedDokument15 SeitenElc 501 - Outline For Forum Discussion - Latest RevisedMendung SimunjanNoch keine Bewertungen
- The Effects of Stress On Short-Term and Long-Term MemoryDokument12 SeitenThe Effects of Stress On Short-Term and Long-Term MemoryCarmen MihalachiNoch keine Bewertungen
- Occupational Stress - Causes and ConsequencesDokument4 SeitenOccupational Stress - Causes and ConsequencesVincent MosunalleeNoch keine Bewertungen
- Cortina Et Al 2023Dokument26 SeitenCortina Et Al 2023sabahrasheed1Noch keine Bewertungen
- The Psychological Impact of Architectural DesignDokument44 SeitenThe Psychological Impact of Architectural DesignmaygracedigolNoch keine Bewertungen
- 7 Steps To DestressDokument13 Seiten7 Steps To DestressArchy100% (1)
- Practice Test Academic ReadingDokument14 SeitenPractice Test Academic ReadingSenuja PasanjithNoch keine Bewertungen
- Panic AwayDokument102 SeitenPanic Awayzcrack100% (8)
- Energy Wheel White PaperDokument13 SeitenEnergy Wheel White PaperMohd NajmuddinNoch keine Bewertungen
- Phobias: What Is Your Problem ?! Hippopotomonstro-Sesquipedaliophobia ?!Dokument4 SeitenPhobias: What Is Your Problem ?! Hippopotomonstro-Sesquipedaliophobia ?!MarNoch keine Bewertungen
- Stress ManagementDokument80 SeitenStress ManagementJitendra Bhatia100% (1)
- Survival Stress in Law EnforcementDokument25 SeitenSurvival Stress in Law EnforcementFelipe PalmaNoch keine Bewertungen
- Academic Practice Test 3: IELTS Essential GuideDokument13 SeitenAcademic Practice Test 3: IELTS Essential GuideWahyu Ajh100% (1)
- HormonesDokument25 SeitenHormonesapi-309893409Noch keine Bewertungen
- EMDR E-Manual - 103pagsDokument103 SeitenEMDR E-Manual - 103pagsPaula Cruz100% (1)
- Box Breathing PDFDokument8 SeitenBox Breathing PDFScribd AnonNoch keine Bewertungen
- Perdev - Lesson 5 - 6Dokument7 SeitenPerdev - Lesson 5 - 6Mark Rigel Dayag ArnocoNoch keine Bewertungen
- Q3 - L1 - Health 7Dokument4 SeitenQ3 - L1 - Health 7Joyce Claire CasaneNoch keine Bewertungen
- Porn Addiction Recovery EbookDokument67 SeitenPorn Addiction Recovery Ebookfeedrightwolf88% (8)
- Module 5 Handout 5.3 PDFDokument21 SeitenModule 5 Handout 5.3 PDFAnonymous KOYPvPUNoch keine Bewertungen
- Module 2 - Theories and Treatment of AbnormalityDokument9 SeitenModule 2 - Theories and Treatment of Abnormalityxyryl ann mae capiliNoch keine Bewertungen
- Pat Ogden Sensorimotor Therapy PDFDokument16 SeitenPat Ogden Sensorimotor Therapy PDFEmili Giralt GuarroNoch keine Bewertungen
- A Rational Approach 2 ND EditionDokument125 SeitenA Rational Approach 2 ND Editionstephanie_bonner_2100% (2)
- Medical Surgical QuestionsDokument19 SeitenMedical Surgical QuestionsDebbie Meyer100% (2)