Beruflich Dokumente
Kultur Dokumente
Misoprostol AJOG
Hochgeladen von
Oktaviana Sari DewiOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Misoprostol AJOG
Hochgeladen von
Oktaviana Sari DewiCopyright:
Verfügbare Formate
Misoprostol versus methylergometrine: Pharmacokinetics
in human milk
Danie`le Vogel,
a
Tilo Burkhardt, MD,
a
Katharina Rentsch, PhD,
b
Horst Schweer, PhD,
c
Bernhard Watzer,
c
Roland Zimmermann, MD,
a
Ursula von Mandach, PhD
a,
*
Department of Obstetrics
a
and Institute of Clinical Chemistry,
b
Zurich University Hospital, Zurich, Switzerland, and
Department of Pediatrics, Philipps University, Marburg, Germany
c
Received for publication January 17, 2004; revised May 1, 2004; accepted May 5, 2004
KEY WORDS
Misoprostol
Methylergometrine
Pharmacokinetics
Human
Lactation
Objective: The purpose of this study to compare breast milk pharmacokinetics between
misoprostol 200 mg and methylergometrine 250 mg after single oral dosing in women who require
postpartum uterotonic therapy.
Study design: Open prospective randomized phase I study measuring misoprostol and
methylergometrine on postpartum days 3 to 6 in milk 0.5, 1, 2, 3, 4, and 5 hours postdose,
and in maternal serum at 0.5 and 1 hours (misoprostol) and 1 and 2 hours (methylergometrine) in
10 lactating women per group.
Results: Milk misoprostol levels rose and declined rapidly, which gave a milk elimination half-life
of less than one half that of methylergometrine (mean GSE, 1.1 G0.3 hours [median, 0.6 hours]
vs 2.33 G0.3 hours [median, 1.9 hours]; P Z .003). Milk/plasma ratios for misoprostol were one
third of those for methylergometrine at 1 hour (P !.0001) and 2 hours (P ! .0015).
Conclusion: Misoprostol warrants further investigation as an alternative to postpartum
methylergometrine because it enters and leaves breast milk at twice the rate, with one third of the
milk/plasma ratio, whichsignificantly lowers infant exposure andfacilitates a timeddosing regimen.
2004 Elsevier Inc. All rights reserved.
Methylergometrine, the conventional postnatal ute-
rotonic, has several disadvantages: excessive uterine
contraction in some cases, inhibition of lactation, and
thermolability.
1-4
A potential alternative is the prosta-
glandin E1 analogue, misoprostol. It has proved an
eective uterotonic in the nal stage and directly after
delivery; it can be given by a variety of routes that
include orally; it has fewer systemic side eects, does not
inhibit lactation, and is heat stable.
1,5
Oral methylergometrine is rapidly absorbed in the
gut, with 60% of the dose entering the systemic circu-
lation.
6
Peak levels (maximum concentration [C
max
]) of
1.21 ng/mL appear 1 hour (time of maximum concen-
tration [T
max
]) after single oral dosing of 125 mg.
Because the plasma elimination half-life (t
b) is 1.4
hours, plasma levels of 0.2 ng/mL, with the use of high-
performance liquid chromatography, remain present 6
hours after the dose is administered.
7
Metabolism in the
liver is followed by excretion mainly in bile and feces.
* Reprint requests: Ursula von Mandach, PhD, Department of
Obstetrics, University Hospital Zurich, Frauenklinikstrasse 10, CH-
8091 Zurich, Switzerland.
E-mail: ursula.vonmandach@usz.ch
0002-9378/$ - see front matter 2004 Elsevier Inc. All rights reserved.
doi:10.1016/j.ajog.2004.05.008
American Journal of Obstetrics and Gynecology (2004) 191, 2168e73
www.ajog.org
Only 3% of an oral dose is excreted unchanged in the
urine.
6
After single oral dosing with 250 mg, the breast
milk C
max
, which is determined by radioimmunoassay
(RIA), is 1.3 ng/mL at a T
max
of 1 hour, with levels
becoming undetectable after 8 hours.
8
Oral misoprostol is 88% absorbed in the gut before
rapid and virtually total conversion by de-esterication
in the liver to its bioactive metabolite, misoprostol
acid.
9,10
It is detected in plasma within 2 minutes of
oral ingestion, reaches C
max
(approximately 300 pg/mL)
at 30 minutes, then declines rapidly.
5,11-13
Misoprostol
acid is 80% to 90% bound to serum protein, and its
t
b is approximately 30 minutes;
9,10
60% to 75% is
eliminated in the urine and 15% in the gut as inactive
polar metabolites.
9
No accumulation occurs even after
administration for several days.
14
After single oral
dosing with 600 mg, the breast milk C
max
, which is
measured by gas chromatography/mass spectrometry, is
21 pg/mL at 1 hour, with levels becoming virtually
unmeasurable after 5 hours.
15
The current data indicate that the more rapid distri-
bution and elimination of misoprostol results not only in
substantially lower exposure of the infant than with
methylergometrine but also allows an optimal time
window between dosing and breastfeeding, hence fur-
ther minimizing the risk of adverse infant eects. As
a preliminary to the major ecacy and tolerability study
required to test the clinical superiority of misoprostol as
a postpartum uterotonic, we decided to characterize its
pharmacokinetics versus methylergometrine in breast
milk using state-of-the-art analytics in a representative
clinical population.
Patients and methods
Patients
After approval from the institutional review board of
the Departments of Obstetrics and Urology at Zurich
University Hospital, 20 lactating well-being women (10
per group) in lactation stage II (milk volume, R30 mL
per feed after a 3-hour nursing interval; milk color,
white) with the postpartum problem of uterine atony
(putrid lochia, soft uterus !3 ngerbreadths below the
umbilicus) who were normally treated in our department
(2000 deliveries per year) with methylergometrine on
postpartum days 3 through 6 (depending on the day of
diagnosis) were recruited into the study, with informed
consent in March/April 2003. The noninclusion criteria
included multiple pregnancy, anemia (hemoglobin,
% 8.0 g/dL on postpartum day 2), inadequate lactation
(onset of lactation O48 hours after delivery; lactation
stage 1; requirement for infant supplementation with
Table I Patient characteristics (n = 10 per group)
Characteristic Misoprostol Methylergometrine
Age (y)* 31.2 G 1.9 31.9 G 1.9
Height (m)* 1.6 G 0.03 1.7 G 0.02
Weight (kg)* 66.6 G 3.1 73.2 G 3.4
Body surface area (m
2
)* 1.7 G 0.04 1.8 G 0.04
Gravidity (n)* 2.0 G 0.3 2.0 G 0.3
Parity (n)* 1.8 G 0.2 1.7 G 0.3
Gestational age at
delivery (wk)*
38.6 G 0.7 38.3 G 1.2
Vaginal delivery
or non-elective cesarean
delivery (n)
7 7
Elective cesarean
delivery (n)
3 3
Hemoglobin level,
day 2 after
delivery (g/dL)*
10.7 G 0.5 11.5 G 0.3
Study day after
delivery*
3.9 G 0.4 4.8 G 0.4
* Data are given as mean G SE; there were no signicant
differences between the groups.
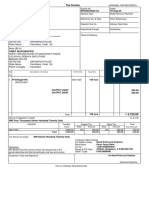
Figure A, Median milk misoprostol acid concentrations
(picograms per milliliter) over the 5 hours after single oral
dosing with misoprostol 200 mg in 10 lactating women. B,
Median milk methylergometrine concentrations (picograms
per milliliter) over the 5 hours after single oral dosing with 250
mg in 10 lactating women.
Vogel et al 2169
glucose or other liquids), vegan or similar extreme
diet, endometritis, essential hypertension, preeclampsia,
severe disease, concomitant uterotonic therapy or
medication likely to interfere with the study drugs, and
participation in another clinical study in the previous
4 weeks.
Protocol
According to the prospective open randomized design,
treatments were allocated in a computer-generated
random sequence with sealed opaque envelopes. After
conrmation of the clinical indication (uterine atony)
and before the rst dose of uterotonic, the patient chose
an envelope from the study box that allocated her to
either misoprostol 200 mg orally (one 200-mg tablet) or
methylergometrine 250 mg orally (two 125-mg tablets).
The dose of misoprostol was selected on the basis of
documented tolerability and uterine activity,
12
while the
dose of methylergometrine was approximated to the
standard regimen for uterine atony that has been used in
our Department for the past 20 years (250 mg, 3 times/d).
Standardized milk sample collection (exactly 10 mL
in a graduated plastic tube) was performed with an
electric pump (Medela International, CH-6341, Baar,
Switzerland; www.medela.ch). The baseline milk sample
was taken 1 to 3 hours after a continental breakfast
(bread, butter, marmalade, and coee or tea) immedi-
ately after suckling the baby at the opposite breast, then
the allocated drug was given. Further milk samples (10
mL) at the same breast were taken 0.5, 1, 2, 3, 4, and 5
hours after the dose was administered. Each milk sample
was stored immediately at 4(C. Maternal blood samples
(5 mL) were taken0.5 and1 hours (misoprostol) and1 and
2 hours (methylergometrine) after the dose was adminis-
tered. Two-milliliter milk aliquots were pipetted into
polypropylene tubes and stored at 70(C until analysis,
along with 1-mL aliquots of centrifuged blood plasma
(milk and plasma samples from the methylergometrine
group were covered with aluminum foil). The sampling
schedule was based on the pharmacokinetic data that
were available in the literature that indicated that miso-
prostol levels in plasma and milk peak at around 1 hour,
somewhat earlier than methylergometrine. Suckling was
not allowed (at the opposite breast) until at least 4 hours
after the dose was administered.
Assays
All samples were analyzed after collection was complete
and were analyzed in duplicate. Each patients samples
were analyzed in the same run.
Misoprostol acid was quantied by gas chromatog-
raphy/negative ion chemical ionization tandem mass
spectrometry, with our published method.
16
Methylergometrine was determined in breast milk
and plasma with high-performance liquid chromatogra-
phy tandem mass spectrometry (Finnigan TSQ 7000;
ThermoQuest, San Jose, Calif). After the protein in the
milk was precipitated with acetone, methylergometrine
was extracted into dichloromethane/methanol by
liquid-liquid extraction, and the lipids were removed
from the organic phase by solid-phase extraction on
silica columns. Methylergometrine was extracted from
the plasma into ethyl acetate by liquid-liquid extraction.
Quantication was performed with calibration samples
that were prepared in the respective matrix.
8
Statistics
The data were entered into Excel (Microsoft Corpora-
tion, Redmond, Wash), analyzed with StatView 4.5
for Windows (SAS Institute Inc, Cary, NC), and ex-
pressed as means G SE (median). Misoprostol and
methylergometrine levels were also expressed as medians
in the Figures.
Pharmacokinetic analysis
Milk/plasma ratios were calculated from the respective
concentrations. Areas under the milk concentration-
time curve from 0 to 5 hours (AUC
0e5 h
) were calculated
by the trapezoidal rule; the C
max
was calculated from the
tted AUC
0e5 h
, along with the T
max
and the milk t
b
(Stata 8.0 for Windows; Stata Corp, College Station,
Tex).
Statistical tests
The Kolmogorov-Smirnov test was used for normality.
Mean within-group dierences were tested with the
Table II Pharmacokinetics in human milk of misoprostol 200 mg versus methylergometrine 250 mg orally
Misoprostol acid Methylergometrine
Mean G SE Median Range Mean G SE Median Range
AUC
0-5 h
(pg/mL ! h) 14.8 G 5.3 8.2 3.0-48.4 1774.0 G 139.5* 1686.3
y
1140.0-2477.5
C
max
(pg/mL) 7.6 G 2.8 3.6 1.9-30.7 657.0 G 38.9* 645
y
410-830
T
max
(h) 1.1 G 0.2 1.0 0.5-2.0 1.8 G 0.3 2.0 0.5-3.0
t
b (h) 1.1 G 0.30 0.6 0.4-2.2 2.3 G 0.3* 1.9
y
1.4-4.7
* Versus misoprostol: unpaired t test !0.0001 (AUC, C
max
) and !0.005 (t
b).
y
Versus misoprostol: Mann-Whitney U test !0.0005 (AUC, C
max
) and !0.05 (t
b).
2170 Vogel et al
Wilcoxon signed-rank test and a paired t test of log
values, and the mean between-group dierences was
tested with the Mann-Whitney U test and an unpaired
t test of log values. A probability value of ! .5 was
used in all tests. Bonferroni correction was used in the
nonparametric tests.
Results
The groups did not dier in demographic or obstetric
variables (Table I). Milk and plasma concentrations
were log-normally distributed in both groups.
Milk
Misoprostol acid levels rose rapidly, peaked at 7.6 G2.8
pg/mL (median, 3.6 pg/mL) at 1.1 G0.2 hours (Table II),
then rapidly declined to 0.20 pg/mL (median) at 5 hours
(Figure, A). Methylergometrine levels rose less rapidly,
peaked at 657.0 G 38.9 pg/mL (median, 645.0 pg/mL)
at 1.8 G 0.3 hours (Table II), then steadily declined to
0.20 pg/mL (median) at 5 hours (Figure, B). AUC
0e5 h
and t
b values diered signicantly between groups;
the t
b of misoprostol was less than one-half that
of methylergometrine (1.1 G 0.3 hours [median, 0.6
hours] vs 2.33 G 0.3 hours [median, 1.9 hours];
P =.003, unpaired t test; P =.02, Mann-Whitney U test;
Table II).
Milk/plasma ratios
C
max
with both drugs was signicantly lower in milk than
in plasma. Ratios for misoprostol acid (0.04 G0.02 [range,
0.001-0.198] at 0.5 hours and 0.06 G 0.01 [range,
0.02-0.16] at 1 hour) were one third of the ratios for
methylergometrine (0.18 G 0.03 [range, 0.08-0.40] at
1 hour and 0.17 G 0.01 [range, 0.12-0.25] at 2 hours;
P !.0001, t test; P !.0015, Mann-Whitney U test;
Table III).
Comment
Our data show that misoprostol enters and leaves breast
milk at twice the rate of methylergometrine and has one-
third the milk/plasma ratio, thus substantially lowering
infant exposure to the drug. To keep demands on
patients to a reasonable level (with respect to milk
output and adequate provision for the child) and to
maintain study feasibility, we could not investigate the
pharmacokinetics in milk at shorter intervals or outside
a 5-hour time frame. However, this time frame encom-
passed the pharmacokinetic prole of most women in
our population under the behavioral circumstances that
were described (clinical conditions, nutritional status,
standardized conditions of milk sampling). In the miso-
prostol group at least, values had declined towards
the detection limit after 5 hours, and in both groups the
information on the distribution and elimination of the
drugs in milk was sucient to permit the computation
of the milk/plasma ratio.
In the misoprostol group, the mean milk T
max
was
1.1 G0.2 hours. Because this included a T
max
of 2 hours
in 2 of the women, the mean concentration at 1 hour was
somewhat lower (4.8 G1.0 pg/mL) than mean C
max
(7.6
G 2.8 pg/mL); the medians (3.6 pg/mL) did not dier.
Similarly, the methylergometrine T
max
of 1.8 G0.3 hours
included 2 women with a T
max
at 3 hours, so that the
mean concentration at 2 hours (527 G 65.9 pg/mL) was
somewhat lower than the mean C
max
(657 G 38.9 pg/
mL); again, the medians (545 pg/mL) did not dier.
Table III Milk and maternal plasma levels (picograms per milliliter) and milk/plasma ratio after single oral dosing with misoprostol
200 mg versus methylergometrine 250 mg (n = 10 per group)
Misoprostol* Methylergometrine
Time post dose (h) Mean G SE Median Mean G SE Median
Milk (pg/mL) 0.5 5.2 G 2.9 2.4 d d
1 4.8 G 1.0 3.6 368 G 83.6 345
2 d d 527 G 65.9 545
Plasma (pg/mL) 0.5 174.3 G 53.5
y
123.7
z
d d
1 104.4 G 16.0
y
96
z
2594.4 G 588.7
y
2545
z
2 d d 3370 G 588.9
y
3140
z
Milk/plasma ratio 0.5 0.04 G 0.02 0.02 d d
1 0.06 G 0.01 0.04 0.18 G 0.03
x
0.16
k
2 d d 0.17 G 0.01 0.17
* The pharmacokinetics of misoprostol in breast milk suggest that it is a safer alternative to methylergometrine as a postpartum uterotonic in
lactating mothers.
y
Versus milk: P ! .0001, paired t test.
z
Versus milk: P ! .01, Wilcoxon signed rank test.
x
Versus misoprostol at 1 hour: P ! .0001, unpaired t test.
k
Versus misoprostol at 1 hour: P ! .01, Mann-Whitney U test.
Vogel et al 2171
As expected, the plasma misoprostol levels that are
foundinthis study were somewhat lower thanthose meas-
ured by the same method after an oral dose of 400 mg
(287.6 pg/mL [C
max
] at 27.5 minutes).
16
In the only
previous study that, to our knowledge, has investigated
the pharmacokinetics of misoprostol in parallel breast
milk and maternal plasma, with a single oral dose of 600
mg and our gas chromatography/mass spectrometry
assay,
16
the plasma C
max
was 344 pg/mL at 20 minutes;
the milk C
max
was 21 pg/mL at 1 hour, and the milk
AUC
1e5 h
was 51.4 pg/mL !hour.
15
The present study,
which used a dose of 200 mg, naturally found lower
values for all 3 parameters.
Misoprostol has been used widely, o-label, as an
uterotonic (eg, as an abortifacient in the rst and second
trimesters, for induction at term or after intrauterine
fetal death, and for the prevention and therapy of
atonicity-related postpartum hemorrhage). Dosing
has been tested between the vaginal, rectal, sublingual,
and oral routes.
11-13,17-20
Plasma C
max
occurs later, and
at a lower level, after vaginal versus oral dosing, but
the drug remains detectable for longer in plasma.
11,17
Sublingual dosing produces a Tmax similar to that of
oral dosing, but a higher C
max
.
17
Thus, the oral route
is clearly ideal in lactating mothers because it generates
rapidly declining levels, not only in maternal plasma,
but also, as our present data conrm, in milk.
The levels of methylergometrine that we found in
plasma and milk were only marginally lower than those
measured in 1978 by Erkkola et al,
8
who used radioim-
munoassay, in what to our knowledge is the only
previous parallel pharmacokinetic study. After single
oral dosing with 250 mg, they found C
max
values at 1
hour of 4.4 ng/mL in maternal plasma and 1.3 ng/mL in
breast milk, which provided a milk/plasma ratio of 0.3.
The adverse a-receptor and dopaminergic eects of
methylergometrine (abdominal pain because of gut
smooth muscle contraction, nausea, vomiting, diarrhea,
headache, tachycardia
1,2,8,20,21
) often prevent its wider use.
Convulsions and dyspnea have occurred on accidental
administration in newborn infants.
22,23
Thermolability is
a further restriction in tropical developing countries.
3,4
These substantial disadvantages make the identication of
a safe and eective alternative a matter of some urgency.
The lower drug levels that we have demonstrated in
maternal plasma and milk, combined with the faster
elimination from milk, are powerful pharmacokinetic
arguments that favor the use of misoprostol in the special
circumstances of the lactating mother. We estimate that
the maximum amount of drug that is delivered in breast
milk (108 pg in a nursing volume of 30 mL [3.6 pg/mL])
represents a dose of 3 !10
5
mg/kg in a 3.5-kg neonate
(ie, 1/100 that in the mother [0.2 mg/60 kg or 1 ! 10
3
mg/kg]). In recommending a safe dosing regimen for
lactating women, we can say that, on the basis of the
present data, misoprostol should be taken immediately
after a feed and that the next feed may safely be given
after 4 hours, or even at the earliest after 3 hours, by
which time misoprostol levels in milk have fallen below
1 pg/mL. Further advantages, such as absent cardio-
vascular eects
5,24,25
(no hypertensive eects, which
makes it an ideal oral drug for women with continuing
postpartum hypertension) and stability even at fairly high
temperatures
5,17,26
are additional reasons for undertaking
a large ecacy and tolerability study of misoprostol as
a postpartum uterotonic in lactating women.
References
1. Gru nberger W. Postpartum uterus involution and lactation levels in
randomized comparison between prostin E2 tablets and methergine
dragees [in German]. Gynakol Rundsch 1983;23:100-7.
2. Arabin B, Ru ttgers H, Kubli F. Eects of routine administration
of methylergometrin during puerperium on involution, maternal
morbidity and lactation [in German]. Geburtshilfe Frauenheilkd
1986;46:215-20.
3. de Groot AN. The role of oral (methyl)ergometrine in the pre-
vention of postpartum haemorrhage. Eur J Obstet Gynecol
Reprod Biol 1996;69:31-6.
4. Hogerzeil HV, Walker GJ. Instability of (methyl)ergometrine in
tropical climates: an overview. Eur J Obstet Gynecol Reprod Biol
1996;69:25-9.
5. el Refaey H, OBrien P, Morafa W, Walder J, Rodeck C. Use of
oral misoprostol in the prevention of postpartum haemorrhage.
BJOG 1997;104:336-9.
6. Ma ntyla R, Kleimola T, Kanto J. Methylergometrine (methyler-
gonovine) concentrations in the human plasma and urine. Int J
Clin Pharmacol Biopharm 1978;16:254-7.
7. de Groot AN, Vree TB, Hekster YA, van den Biggelaar
Martea M, van Dongen PW, van Roosmalen J. Comparison of
the bioavailability and pharmacokinetics of oral methyler-
gometrine in men and women. Int J Clin Pharmacol Ther
1995;33:328-32.
8. Erkkola R, Kanto J, Allonen H, Kleimola T, Mantyla R. Excre-
tion of methylergometrine (methylergonovine) into the human
breast milk. Int J Clin Pharmacol Biopharm 1978;16:579-80.
9. Arns PA. Misoprostol. Am J Med Sci 1991;301:133-7.
10. Davies NM, Longstreth J, Jamali F. Misoprostol therapeutics
revisited. Pharmacotherapy 2001;21:60-73.
11. Zieman M, Fong SK, Benowitz NL, Banskter D, Darney PD.
Absorption kinetics of misoprostol with oral or vaginal adminis-
tration. Obstet Gynecol 1997;90:88-92.
12. Danielsson KG, Marions L, Rodriguez A, Spur BW, Wong PY,
Bygdeman M. Comparison between oral and vaginal administra-
tion of misoprostol on uterine contractility. Obstet Gynecol
1999;93:275-80.
13. Goldberg AB, Greenberg MB, Darney PD. Misoprostol and
pregnancy. N Engl J Med 2001;344:38-47.
14. Garris RE, Kirkwood CF. Misoprostol: a prostaglandin E1
analogue. Clin Pharm 1989;8:627-44.
15. Abdel-Aleem H, Villar J, Gu lmezoglu MA, Mostafa SA,
Youssef AA, Shokry M, et al. The pharmacokinetics of the
prostaglandin E1 analogue misoprostol in plasma and colostrum
after postpartum oral administration. Eur J Obstet Gynecol
2003;108:25-8.
16. Watzer B, Seyberth HW, Schweer H. Determination of misopros-
tol free acid in human breast milk and serum by gas chromatog-
raphy/negative ion chemical ionization tandem mass spectrometry.
J Mass Spectrom 2002;37:927-33.
2172 Vogel et al
17. Tang OS, Schweer H, Seyberth HW, Lee SW, Ho PC. Pharma-
cokinetics of dierent routes of administration of misoprostol.
Hum Reprod 2002;17:332-6.
18. Bamigboye AA, Merrell DA, Hofmeyr GJ, Mitchell R. Randomized
comparison of rectal misoprostol with syntometrine for management
of third stage of labor. Acta Obstet Gynecol Scand 1998;77:178-81.
19. Abdel Aleem H, el Nashar I, Abdel Aleem A. Management of
severe postpartum hemorrhage with misoprostol. Int J Gynaecol
Obstet 2001;72:75-6.
20. Zu st S, Ho sli I, Surbek D, Holzgreve W. Adverse eects of
misoprostol in pregnancy [in German]. Z Geburtshilfe Neonatol
2001;205:43-8 .
21. Ma ntyla R, Kanto J. Clinical pharmacokinetics of methylergome-
trine (methylergonovine). Int J Clin Pharmacol Ther Toxicol
1981;19:386-91.
22. Donatini B, Le Blaye I, Krupp P. Inadvertent administration of
uterotonics to neonates. Lancet 1993;341:839-40.
23. Baum CR, Hilpert PL, Bhutani VK. Accidental administration of
an ergot alkaloid to a neonate. Pediatrics 1996;98:457-8.
24. Ramsey PS, Hogg BB, Savage KG, Winkler DD, Owen J.
Cardiovascular eects of intravaginal misoprostol in the mid
trimester pregnancy. Am J Obstet Gynecol 2000;183:1100-2.
25. Amant F, Spitz B, Timmerman D, Corremans A, Van Assche FA.
Misoprostol compared with methylergometrine for the prevention
of postpartum haemorrhage: a double-blind randomised trial.
BJOG 1999;106:1066-70.
26. de Groot AN, van Dongen PW, Vree TB, Hekster YA, van
Roosmalen J. Ergot alkaloids: current status and review of clinical
pharmacology and therapeutic use compared with other oxytocics
in obstetrics and gynaecology. Drugs 1998;56:523-35.
Vogel et al 2173
Das könnte Ihnen auch gefallen
- Epinefrin UsesDokument7 SeitenEpinefrin UsesOktaviana Sari DewiNoch keine Bewertungen
- Properties of Wasp VenomDokument37 SeitenProperties of Wasp VenomOktaviana Sari DewiNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument9 SeitenNIH Public Access: Author Manuscriptimmortally89Noch keine Bewertungen
- Aafp Anaphylaxis Recognition and Management PDFDokument8 SeitenAafp Anaphylaxis Recognition and Management PDFOktaviana Sari DewiNoch keine Bewertungen
- Bee Stings Immunology Allergy and Treatment Marterre PDFDokument9 SeitenBee Stings Immunology Allergy and Treatment Marterre PDFOktaviana Sari DewiNoch keine Bewertungen
- Manajemen PWSDokument11 SeitenManajemen PWSOktaviana Sari DewiNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument9 SeitenNIH Public Access: Author Manuscriptimmortally89Noch keine Bewertungen
- Shock and Circulatory FailureDokument8 SeitenShock and Circulatory FailureOktaviana Sari DewiNoch keine Bewertungen
- Cerebral Palsy and EpilepsyDokument5 SeitenCerebral Palsy and EpilepsyOktaviana Sari DewiNoch keine Bewertungen
- Maternal Care UNICEF 2012 PDFDokument6 SeitenMaternal Care UNICEF 2012 PDFOktaviana Sari DewiNoch keine Bewertungen
- Peptic Ulcer Disease: Causes, Symptoms and TreatmentDokument24 SeitenPeptic Ulcer Disease: Causes, Symptoms and TreatmentOktaviana Sari Dewi100% (1)
- Cerebral Palsy and EpilepsyDokument5 SeitenCerebral Palsy and EpilepsyOktaviana Sari DewiNoch keine Bewertungen
- Ocular CorticosteroidDokument5 SeitenOcular CorticosteroidOktaviana Sari DewiNoch keine Bewertungen
- Peptic Ulcer DiseaseDokument17 SeitenPeptic Ulcer DiseaseHazel Anne Ison DumayasNoch keine Bewertungen
- Imaging in Acute Torticollis NXPowerLiteDokument41 SeitenImaging in Acute Torticollis NXPowerLiteOktaviana Sari DewiNoch keine Bewertungen
- Wound-Healing Outcomes Using Standardized Assessment and Care in Clinical PracticeDokument5 SeitenWound-Healing Outcomes Using Standardized Assessment and Care in Clinical PracticeOktaviana Sari DewiNoch keine Bewertungen
- C 050102Dokument8 SeitenC 050102Oktaviana Sari DewiNoch keine Bewertungen
- Faith For ToleranceDokument2 SeitenFaith For ToleranceOktaviana Sari DewiNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- All Over AgainDokument583 SeitenAll Over AgainJamie Kris MendozaNoch keine Bewertungen
- Brinker Insider Trading SuitDokument5 SeitenBrinker Insider Trading SuitDallasObserverNoch keine Bewertungen
- Modulo InglesDokument8 SeitenModulo InglesJames Mosquera GarciaNoch keine Bewertungen
- 6 Holly Fashion Case StudyDokument3 Seiten6 Holly Fashion Case StudyCaramalau Mirela-Georgiana0% (1)
- Recommendation Letter - One Young WorldDokument2 SeitenRecommendation Letter - One Young WorldNabeel K. AdeniNoch keine Bewertungen
- Jharkhand VAT Rules 2006Dokument53 SeitenJharkhand VAT Rules 2006Krushna MishraNoch keine Bewertungen
- Ramesh Dargond Shine Commerce Classes NotesDokument11 SeitenRamesh Dargond Shine Commerce Classes NotesRajath KumarNoch keine Bewertungen
- 5.2.1 1539323575 2163Dokument30 Seiten5.2.1 1539323575 2163Brinda TNoch keine Bewertungen
- Boeing 7E7 - UV6426-XLS-ENGDokument85 SeitenBoeing 7E7 - UV6426-XLS-ENGjk kumarNoch keine Bewertungen
- Kelainan Morfologi EritrositDokument19 SeitenKelainan Morfologi EritrositAdel shbelNoch keine Bewertungen
- 8086 ProgramsDokument61 Seiten8086 ProgramsBmanNoch keine Bewertungen
- Chinnamasta Sadhana PDFDokument1 SeiteChinnamasta Sadhana PDFSayan Majumdar100% (2)
- Orbit BioscientificDokument2 SeitenOrbit BioscientificSales Nandi PrintsNoch keine Bewertungen
- David Freemantle - What Customers Like About You - Adding Emotional Value For Service Excellence and Competitive Advantage-Nicholas Brealey Publishing (1999)Dokument312 SeitenDavid Freemantle - What Customers Like About You - Adding Emotional Value For Service Excellence and Competitive Advantage-Nicholas Brealey Publishing (1999)Hillary Pimentel LimaNoch keine Bewertungen
- HDFDJH 5Dokument7 SeitenHDFDJH 5balamuruganNoch keine Bewertungen
- Assignment 3-WEF-Global Competitive IndexDokument3 SeitenAssignment 3-WEF-Global Competitive IndexNauman MalikNoch keine Bewertungen
- ExpressionismDokument16 SeitenExpressionismRubab ChaudharyNoch keine Bewertungen
- Aaps Pronouns-ExplainedDokument2 SeitenAaps Pronouns-Explainedapi-277377140Noch keine Bewertungen
- Self Respect MovementDokument2 SeitenSelf Respect MovementJananee RajagopalanNoch keine Bewertungen
- Eun 9e International Financial Management PPT CH01 AccessibleDokument29 SeitenEun 9e International Financial Management PPT CH01 AccessibleDao Dang Khoa FUG CTNoch keine Bewertungen
- REBECCA SOLNIT, Wanderlust. A History of WalkingDokument23 SeitenREBECCA SOLNIT, Wanderlust. A History of WalkingAndreaAurora BarberoNoch keine Bewertungen
- PDFDokument2 SeitenPDFJahi100% (3)
- D2 Pre-Board Prof. Ed. - Do Not Teach Too Many Subjects.Dokument11 SeitenD2 Pre-Board Prof. Ed. - Do Not Teach Too Many Subjects.Jorge Mrose26Noch keine Bewertungen
- A Business Development PlanDokument90 SeitenA Business Development PlanRishabh Sarawagi100% (1)
- Effects of Violence On Transgender PeopleDokument8 SeitenEffects of Violence On Transgender PeopleAdel Farouk Vargas Espinosa-EfferettNoch keine Bewertungen
- Court Rules on Debt Collection Case and Abuse of Rights ClaimDokument3 SeitenCourt Rules on Debt Collection Case and Abuse of Rights ClaimCesar CoNoch keine Bewertungen
- Angel Turns 18 Debut ScriptDokument2 SeitenAngel Turns 18 Debut ScriptChristian Jorge Lenox100% (1)
- Risk Assessment: Act/Hse/Ra 001: Use of Suspended Access Cradles and Platforms (Temporary Works)Dokument2 SeitenRisk Assessment: Act/Hse/Ra 001: Use of Suspended Access Cradles and Platforms (Temporary Works)Saravana0% (1)
- Metabolic Pathway of Carbohydrate and GlycolysisDokument22 SeitenMetabolic Pathway of Carbohydrate and GlycolysisDarshansinh MahidaNoch keine Bewertungen
- Fiegel Kutter Idriss PDFDokument1 SeiteFiegel Kutter Idriss PDFAvaNoch keine Bewertungen