Beruflich Dokumente
Kultur Dokumente
P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)
Hochgeladen von
fraditayyunusOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)
Hochgeladen von
fraditayyunusCopyright:
Verfügbare Formate
Diabetologia (2006) 49: 2528
DOI 10.1007/s00125-005-0057-7
SHORT COMMUNI CATION
A. Kerssen
.
H. W. de Valk
.
G. H. A. Visser
Do HbA
1
c levels and the self-monitoring of blood glucose levels
adequately reflect glycaemic control during pregnancy in women
with type 1 diabetes mellitus?
Received: 28 June 2005 / Accepted: 19 September 2005 / Published online: 9 December 2005
# Springer-Verlag 2005
Abstract Aims/hypothesis: Pregnancies of women with
type 1 diabetes mellitus are associated with maternal and
perinatal complications. These complication rates remain
elevated despite achievement of the treatment goals de-
scribed in the widely used guidelines of the American
Diabetes Association (i.e. HbA
1
c level 7.0%). Against this
background, we sought to answer two questions: (1) are
HbA
1
c levels within 1% above normal appropriate in preg-
nant women with type 1 diabetes or should treatment be
aimed at normal HbA
1
c levels; and (2) how many self-
monitored blood glucose (SMBG) levels are needed per day
to obtain an adequate image of glycaemic control in pregnant
women with type 1 diabetes? Materials and methods: We
asked 43 pregnant women with type 1 diabetes to use the
Continuous Glucose Monitoring System (CGMS) once in
each trimester of pregnancy, while continuing their SMBG
measurements. Glucose levels measured with the CGMS
were compared between patients with HbA
1
c levels of 4.0
6.0%, 6.07.0% and >7.0%. Self-monitored glucose levels
and those measured with CGMS were compared between
patients with four or five, six to nine and ten or more SMBG
determinations daily. Results: In patients with HbA
1
c lev-
els 6.0%, the glucose levels obtained by CGMS were sig-
nificantly better than in patients with HbA
1
c levels >6.0%. In
women with HbA
1
c levels 6.07.0%and >7.0%, these levels
did not differ. The detection rate of hyper- and hypogly-
caemic episodes was significantly higher in patients with ten
or more SMBG determinations daily than in patients with
fewer than ten. Conclusions/interpretation: Treatment of
diabetes in pregnant women should be aimed at achieving
HbA
1
c levels within the normal range, i.e. 6.0%. A min-
imum of ten SMBG determinations daily is necessary to
obtain adequate information of all daily glucose fluctuations.
Keywords Continuous Glucose Monitoring System
.
Glycaemic control
.
HbA
1
c level
.
Pregnancy
.
Self-monitoring of blood glucose levels
.
Type 1 diabetes mellitus
Abbreviations ADA: American Diabetes Association
.
CGMS: Continuous Glucose Monitoring System
.
SMBG: self-monitoring of blood glucose levels
Introduction
Pregnancy in women with type 1 diabetes mellitus is as-
sociated with an increased incidence of perinatal complica-
tions [1]. It is generally accepted that complication rates
decrease when glycaemic control during pregnancy is
tightened. The widely used guidelines of the American
Diabetes Association (ADA) state that in pregnancy HbA
1
c
levels within 1% above the upper limit of normal range are
desirable, as these are assumed to be associated with rates of
congenital malformations equal to those in healthy women
[2]. However, it has been shown that in patients with these
acceptable HbA
1
c levels, complication rates remain high-
er than in patients with normal HbA
1
c levels [1, 3]. The
most obvious explanation for this finding is that in patients
with HbA
1
c levels within 1% above normal, glucose levels
are not within an acceptable range [4].
Currently, self-monitoring of blood glucose (SMBG) is
the established and easiest way of observing daily glucose
levels in patients with diabetes. The frequency and timing of
SMBG should be dictated by the particular needs and goals
of the patients. During pregnancy, SMBG is recommended
at least three times per day in women with type 1 diabetes
[5]. SMBG, however, has its limitations and with the high
A. Kerssen (*)
.
G. H. A. Visser
Department of Perinatology and Gynaecology,
University Medical Centre Utrecht,
KJ.02.507.0/P.O. Box 85090,
3508 AB Utrecht, The Netherlands
e-mail: a.kerssen@umcutrecht.nl
Tel.: +31-30-2504913
Fax: +31-30-2505320
H. W. de Valk
Department of Internal Medicine and Dermatology,
University Medical Centre Utrecht,
Utrecht, The Netherlands
complication rates in pregnancies of women with type 1
diabetes, accurate reflection of glucose levels is important.
The first aim of this study was to evaluate the
appropriateness of the limits of HbA
1
c levels currently
recommended in international guidelines during pregnan-
cy. The second aim was to assess how many SMBG
determinations have to be obtained daily to give an
accurate idea of glucose levels in pregnant women with
type 1 diabetes.
Subjects, materials and methods
The continuous glucose monitoring system
The Continuous Glucose Monitoring System (CGMS) is a
portable device (CGMS; MiniMed, Sylmar, CA, USA) that
measures glucose levels in the extracellular fluid of the
abdominal subcutaneous tissue for an uninterrupted period
of up to 72 h. With this device, ambulatory continuous
glucose monitoring is possible while patients maintain their
usual daily activities. The CGMS stores values within a
range of 2.2 to 22.2 mmol/l every 5 min, providing 288
readings in 24 h. The CGMS does not display glucose
values and the data saved in the monitor are downloaded
and printed after removing the sensor. Patients need to
calibrate the system by entering data from at least four
fingerstick glucose measurements each day.
The data of the CGMS are considered valid if three
criteria for optimal accuracy are met: (1) at least four paired
sensor glucose values and meter glucose readings per day;
(2) correlation coefficient between sensor glucose values
and meter blood glucose readings 0.79; and (3) average
value of differences between sensor glucose values and
meter glucose readings for a given day 28% [6]. It has
been shown that the CGMS is an accurate tool for glucose
monitoring in pregnant women with type 1 diabetes [7]. In
the present study glucose profiles measured with the
CGMS were used only if the accuracy criteria were met and
if none of the 288 glucose measurements per 24 h was
missing.
Materials and methods
The study was approved by the ethics committee of the
University Medical Centre Utrecht, The Netherlands. From
December 2001 through to June 2004, 43 pregnant women
with type 1 diabetes were recruited fromour obstetrical out-
patient clinic. All patients gave written informed consent to
participate in the study. The patients were asked to use the
CGMS once in each trimester of the pregnancy.
HbA
1
c levels were determined within 1 week after each
continuous glucose measurement. In 55% of the patients,
HbA
1
c levels were also obtained 68 weeks after the
CGMS measurement. Comparison of the two HbA
1
c levels
showed a correlation coefficient of 0.83 (p<0.001). A
paired t-test showed that HbA
1
c levels obtained 1 week or
68 weeks after the CGMS measurement were not sig-
nificantly different. HbA
1
c levels determined within 1
week after the CGMS measurement were therefore found
fit to use in the present study.
The patients were asked to maintain their regular SMBG
schedule on the days the CGMS was used, with a minimum
of four SMBG determinations per daythe amount needed
for calibration of the CGMS. All SMBG determinations
were performed through fingerstick measurement and were
determined with the MediSense Precision Xtra glucose
meter (Abbott, Bedford, MA, USA).
Analysis
Glucose levels measured with the CGMS were expressed
as mean and range per 24 h. Hyperglycaemia was defined
as a glucose level 7.8 mmol/l and hypoglycaemia was
defined as a glucose level 3.9 mmol/l. The number of
hyper- and hypoglycaemic episodes per 24 h measured
with the CGMS were counted. Glucose variability of the
glucose levels measured with the CGMS was expressed as
the CV (100SD/mean).
Mean glucose level, glucose range, number of hyper-
and hypoglycaemic episodes and CVof the CGMS glucose
levels were compared between patients with a normal
HbA
1
c level (6.0%), those with HbA
1
c levels within 1%
above normal range (6.07.0%) and those with not op-
timal HbA
1
c levels (>7.0%) using one-way ANOVA and
post hoc Bonferroni.
The measurement days were categorised into three
groups: (1) four or five SMBG determinations daily; (2)
six to nine daily; and (3) ten or more daily. For each mea-
surement day, the hyper- and hypoglycaemia detection rate
was calculated. The hyper- and hypoglycaemia detection
rates were compared between the three groups using one-
way ANOVA and a post-hoc Bonferroni correction. For
evaluation p<0.05 was considered significant.
Results
No adverse events were associated with the use of the
CGMS. A total of 212 measurement days were obtained, of
which 185 days (87%) fulfilled the predefined requirements
for analysis. The number of measurement days in the first,
Table 1 Mean glucose level, glucose range, number of hyper- and
hypoglycaemic episodes and CV per 24 h of CGMS glucose levels
in patients with different HbA
1
c levels
HbA
1
c level
4.06.0% 6.07.0% >7.0%
Mean glucose level (mmol/l) 5.6 7.0 7.8
Glucose range (mmol/l) 6.7 9.6 11.6
Hyperglycaemic episodes (n) 2.1 3.4 3.9
Hypoglycaemic episodes (n) 3.2 2.3 2.0
CV (%) 27 34 39
26
second and third trimester of pregnancy was 68, 59 and 58,
respectively. HbA
1
c levels ranged from 5.1 to 9.1%. The
HbA
1
c level was 6.0% in 58 (31%), 6.07.0% in 104
(56%) and >7.0% in 23 (12%) of the measurement days.
The HbA
1
c levels and CGMS glucose values are shown
in Table 1. In patients with HbA
1
c levels 6.0% all but one
of the glucose measures were significantly better (p<0.001)
than in patients with HbA
1
c levels of 6.07.0% or >7.0%.
Only the number of hypoglycaemic episodes was sig-
nificantly higher (p<0.05). Glucose measures in women
with HbA
1
c levels 6.07.0% and >7.0% did not differ
significantly, apart from mean glucose and glucose range
(p<0.05).
SMBG determinations were performed four or five, six
to nine and ten or more times per day on 92, 70 and
23 days, respectively. Mean HbA
1
c levels did not differ
significantly between the groups (6.5, 6.3 and 6.2%,
respectively), nor did the mean glucose values (Table 2).
The mean glucose level, glucose range and number of
hyper- and hypoglycaemic episodes measured with SMBG
and the CGMS are given in Table 2. Hyperglycaemia
detection rates increased significantly (p<0.05) with an
increase in the number of SMBG determinations (35, 59
and 100%, respectively). Hypoglycaemia detection rate
was significantly higher in the third group (73%) than in
the first (26%, p<0.01) and second (48%, p<0.05).
Discussion
This study shows that there is a significant difference in
glycaemic control between patients with HbA
1
c levels
within the normal range (6.0%) and patients with HbA
1
c
levels above the normal range (>6.0%). No difference in
glycaemic control was seen between patients with accept-
able HbA
1
c levels (6.07.0%) and those with not optimal
HbA
1
c levels (>7.0%). These results conflict with the
guidelines of the ADA, which state that in pregnancy
HbA
1
c levels 7.0% are acceptable [2]. This study also
shows that hyper- and hypoglycaemia detection rates
increase when patients measure their blood glucose levels
ten or more times daily. The hyperglycaemia detection rate
rises to 100%. The detection rate of hypoglycaemic epi-
sodes, however, did not exceed 73%. It is unlikely that
biochemical detection of hypoglycaemic episodes will ever
be 100%as these often occur in the night and early morning
hours when patients are sleeping [8].
Our findings indicate that the current guidelines might
not be accurate. However, before changing guidelines or
clinical practice, further research should be performed
evaluating the effects of the normalisation of HbA
1
c levels
and of a more frequent performance of SMBG determina-
tions on pregnancy outcome. Also the risk of normalising
HbA
1
c levels should be assessed. Normalisation of blood
glucose levels in pregnant women with diabetes is as-
sociated with an increased risk of hypoglycaemic episodes
[9]. This finding is confirmed in the present study, as the
number of hypoglycaemic episodes increased when HbA
1
c
levels were 6.0%. Thirdly, we should ask ourselves
whether, with the currently available insulins and proce-
dures, we are able to treat all glucose fluctuations that are
measured. In a previous study we have shown that treat-
ment adjustments are difficult to make in women whose
diurnal glucose profiles show large fluctuations [10]. In
some women, glucose fluctuations will persist despite the
extreme efforts of both doctors and patients. Finally, the
usefulness of HbA
1
c levels as a measure of glycaemic
control in pregnant women with diabetes should be reas-
sessed. Even in women with normal HbA
1
c levels, hyper-
and hypoglycaemic episodes were present. Is it a too gross
measure of glycaemic control or are there other, for ex-
ample, genetic or familial factors that cause the gap be-
tween actual glucose levels and HbA
1
c levels?
Acknowledgement This study was supported by Novo Nordisk
Farma BV, Alphen aan de Rijn, The Netherlands.
References
1. Evers IM, de Valk HW, Visser GHA (2004) Risk of
complications of pregnancy in women with type 1 diabetes:
nationwide prospective study in the Netherlands. BMJ 328:915
2. ADA (2004) Preconception care of women with diabetes.
Diabetes Care 27[Suppl 1]:S76S78
3. Suhonen L, Hiilesmaa V, Teramo K (2000) Glycaemic control
during early pregnancy and fetal malformations in women with
type I diabetes mellitus. Diabetologia 43:7982
4. Kerssen A, Evers IM, Valk de HW, Visser GHA (2003) Poor
glucose control in women with type 1 diabetes mellitus and
safe hemoglobin A1c values in the first trimester of pregnan-
cy. J Matern Fetal Neonat Med 13:309313
5. ADA (2004) Standards of medical care in diabetes. Diabetes
Care 27(Suppl 1):S15S35
6. Mastrototaro J (1999) The MiniMed Continuous Glucose
Monitoring System (CGMS). J Pediatr Endocrinol Metab 12
(Suppl 3):751758
Table 2 Mean glucose
level, glucose range, number
of hyper- and hypoglycaemic
episodes per 24 h of SMBG
determinations and CGMS
glucose levels in patients
with different numbers
of SMBG determinations
Number of SMBG determinations
45 69 10
SMBG CGMS SMBG CGMS SMBG CGMS
Mean glucose level (mmol/l) 6.8 6.9 6.5 6.3 6.2 6.3
Glucose range (mmol/l) 5.1 9.6 6.4 8.1 7.8 8.9
Hyperglycaemic episodes (n) 1.2 3.4 1.7 2.9 1.8 1.8
Hypoglycaemic episodes (n) 0.6 2.3 1.2 2.5 2.7 3.7
27
7. Kerssen A, de Valk HW, Visser GHA (2004) The Continuous
Glucose Monitoring System during pregnancy of women with
type 1 diabetes mellitus; accuracy assessment. Diabetes Technol
Ther 6:645651
8. Rayburn W, Piehl E, Jacober S, Schork A, Ploughman L (1986)
Severe hypoglycemia during pregnancy: its frequency and
predisposing factors in diabetic women. Int J Gynaecol Obstet
24:263268
9. Rosenn B, Siddiqi TA, Miodovnik M (1995) Normalization of
blood glucose in insulin-dependent diabetic pregnancies and
the risks of hypoglycemia: a therapeutic dilemma. Obstet
Gynecol Surv 50:5661
10. Kerssen A, de Valk HW, Visser GHA(2004) Day-to-day glucose
variability during pregnancy in women with type 1 diabetes
mellitus: glucose profiles measured with the Continuous Glu-
cose Monitoring System. Br J Obstet Gynecol 111:919924
28
Das könnte Ihnen auch gefallen
- (ASRA) Guidelines Neuraxial and AnticoagulationDokument6 Seiten(ASRA) Guidelines Neuraxial and Anticoagulationfraditayyunus80% (10)
- 190 - Gestational Diabetes Mellitus AgogDokument16 Seiten190 - Gestational Diabetes Mellitus Agogjorge vergara100% (2)
- American College of Surgeons and Surgical Infection Society - Surgical Site Infection Guidelines, 2016 Update (SSI)Dokument16 SeitenAmerican College of Surgeons and Surgical Infection Society - Surgical Site Infection Guidelines, 2016 Update (SSI)Anonymous LnWIBo1GNoch keine Bewertungen
- Self-Monitoring of Blood GlucoseDokument3 SeitenSelf-Monitoring of Blood Glucosepasukan5jari100% (1)
- Artikel Aulia DyahDokument8 SeitenArtikel Aulia DyahproluvieslacusNoch keine Bewertungen
- March 2019 1551446825 124Dokument3 SeitenMarch 2019 1551446825 124Anjali Rahul AjmeriNoch keine Bewertungen
- Introduction: Diabetes Mellitus (DM) Is The Most Common Endocrine ProblemDokument6 SeitenIntroduction: Diabetes Mellitus (DM) Is The Most Common Endocrine ProblemHeribertus Andi WidagdoNoch keine Bewertungen
- tmp2475 TMPDokument7 Seitentmp2475 TMPFrontiersNoch keine Bewertungen
- An Evaluation of The Accuracy of A Flash Glucose Monitoring System in Children With Diabetes in Comparison With Venous Blood GlucoseDokument8 SeitenAn Evaluation of The Accuracy of A Flash Glucose Monitoring System in Children With Diabetes in Comparison With Venous Blood GlucosesovalaxNoch keine Bewertungen
- Jurnal 2Dokument5 SeitenJurnal 2Rizqi Fauzi Nurul AwalinNoch keine Bewertungen
- Bismillah Fix Hba1c2Dokument7 SeitenBismillah Fix Hba1c2NsafifahNoch keine Bewertungen
- Fatimah Azzahra - Endocrin SystemDokument7 SeitenFatimah Azzahra - Endocrin SystemFatimah AzzahraNoch keine Bewertungen
- Monitoring Glucose Levels and KetonesDokument19 SeitenMonitoring Glucose Levels and KetonesLeonilyn Dagoplo RNNoch keine Bewertungen
- Factor Associated With Long-Term Control Blood Glucose Based On Hba1C Level in Type 2 Diabetes Mellitus PatientsDokument5 SeitenFactor Associated With Long-Term Control Blood Glucose Based On Hba1C Level in Type 2 Diabetes Mellitus PatientsYuswandi Satya PermanaNoch keine Bewertungen
- The Influence of Glucose Self-Monitoring On Glycaemic Control in Patients With Diabetes Mellitus in SudanDokument5 SeitenThe Influence of Glucose Self-Monitoring On Glycaemic Control in Patients With Diabetes Mellitus in SudanZam-zam RsiNoch keine Bewertungen
- A Deep Learning Approach of Blood Glucose Predictive Monitoring For Women With Gestational DiabetesDokument18 SeitenA Deep Learning Approach of Blood Glucose Predictive Monitoring For Women With Gestational Diabetes21bit20Noch keine Bewertungen
- Diagnosis of Gestational DiabetesDokument7 SeitenDiagnosis of Gestational DiabetesAl Hasyr SarminNoch keine Bewertungen
- Glycated Haemoglobin As A Stable Indicator Of: Hba C Type 2 DiabetesDokument4 SeitenGlycated Haemoglobin As A Stable Indicator Of: Hba C Type 2 DiabetesfamtaluNoch keine Bewertungen
- Bismillah Fix Hba1c1Dokument23 SeitenBismillah Fix Hba1c1NsafifahNoch keine Bewertungen
- Disease The British Journal of Diabetes & VascularDokument6 SeitenDisease The British Journal of Diabetes & VascularEstiPramestiningtyasNoch keine Bewertungen
- Correlation of Fasting and Postprandial Plasma Glucose With Hba1C in Assessing Glycemic Control Systematic Review and Meta-AnalysisDokument9 SeitenCorrelation of Fasting and Postprandial Plasma Glucose With Hba1C in Assessing Glycemic Control Systematic Review and Meta-AnalysisRodas GetachewNoch keine Bewertungen
- 1 s2.0 S0168822703002201 MainDokument7 Seiten1 s2.0 S0168822703002201 MainaasdaNoch keine Bewertungen
- Assessment and Treatment of Hyperglycemia in Critically IllDokument6 SeitenAssessment and Treatment of Hyperglycemia in Critically IllYousif ElmasryNoch keine Bewertungen
- Paper 2 HighlightedDokument9 SeitenPaper 2 HighlightedVaishnavi YacheNoch keine Bewertungen
- Point: Yes, It Is Necessary To Rely Entirely On Glycemic Values For The Insulin Treatment of All Gestational Diabetic WomenDokument2 SeitenPoint: Yes, It Is Necessary To Rely Entirely On Glycemic Values For The Insulin Treatment of All Gestational Diabetic WomenGeorge Tirta DihatmoNoch keine Bewertungen
- Intermittently Scanned Continuous Glucose Monitoring For Type 1 DiabetesDokument12 SeitenIntermittently Scanned Continuous Glucose Monitoring For Type 1 DiabetesClaudia NgNoch keine Bewertungen
- Nutritional Status in Patients With Diabetes and Chronic Kidney Disease: A Prospective StudyDokument6 SeitenNutritional Status in Patients With Diabetes and Chronic Kidney Disease: A Prospective StudyHenry HadiantoNoch keine Bewertungen
- Glycemic Targets: American Diabetes AssociationDokument8 SeitenGlycemic Targets: American Diabetes AssociationHelenaNoch keine Bewertungen
- Gestational Diabetes Mellitus DiagnosedDokument5 SeitenGestational Diabetes Mellitus DiagnosedMutia AgustriaNoch keine Bewertungen
- Scientific Advisory Committee Opinion Paper 23: 1. BackgroundDokument5 SeitenScientific Advisory Committee Opinion Paper 23: 1. BackgroundNatia DemetradzeNoch keine Bewertungen
- Update On: Diabetes MellitusDokument37 SeitenUpdate On: Diabetes MellitusDr. Mamunul Abedin100% (1)
- Standards of Medical Care in Diabetes - 2010: Iii. Detection and Diagnosis of GDMDokument4 SeitenStandards of Medical Care in Diabetes - 2010: Iii. Detection and Diagnosis of GDMAnamarina Güette VianaNoch keine Bewertungen
- Desantis 2006Dokument15 SeitenDesantis 2006Hoàng ThôngNoch keine Bewertungen
- J of Diabetes Invest - 2020 - Mo - Defining The Target Value of The Coefficient of Variation by Continuous GlucoseDokument10 SeitenJ of Diabetes Invest - 2020 - Mo - Defining The Target Value of The Coefficient of Variation by Continuous Glucosesaurav kannilakandiNoch keine Bewertungen
- Diabetes Mellitus Management of Gestational Diabetes - 280720Dokument12 SeitenDiabetes Mellitus Management of Gestational Diabetes - 280720AddisNoch keine Bewertungen
- STATEMENTS ADIPS GDM Management GuidelinesDokument10 SeitenSTATEMENTS ADIPS GDM Management Guidelineskitten garciaNoch keine Bewertungen
- Karl Kristensen, Anne-Marie Wangel, Anastasia Katsarou, Nael Shaat, David Simmons, Helena Fadl, and Kerstin BerntorpDokument10 SeitenKarl Kristensen, Anne-Marie Wangel, Anastasia Katsarou, Nael Shaat, David Simmons, Helena Fadl, and Kerstin BerntorpSeven NightNoch keine Bewertungen
- Normal Glucose Levels - The Ultimate Guide From LDokument2 SeitenNormal Glucose Levels - The Ultimate Guide From LAgha Muhammad RazaNoch keine Bewertungen
- Blood GlucoseDokument5 SeitenBlood Glucoseediting visualsNoch keine Bewertungen
- Sistemik CaranzaDokument9 SeitenSistemik CaranzawulanNoch keine Bewertungen
- Flash Glucose MonitoringDokument9 SeitenFlash Glucose MonitoringAneed AnandNoch keine Bewertungen
- 134 2021 Article 6526Dokument13 Seiten134 2021 Article 6526Eyal RobinsonNoch keine Bewertungen
- DMG Diagnosis and ManagementDokument6 SeitenDMG Diagnosis and ManagementCésar MonjarásNoch keine Bewertungen
- Standards of Medical Care in Diabetesd2021: 6. Glycemic TargetsDokument12 SeitenStandards of Medical Care in Diabetesd2021: 6. Glycemic TargetsFajar NugrahantoNoch keine Bewertungen
- Insulin Detemir and Basal Insulin TherapyDokument7 SeitenInsulin Detemir and Basal Insulin Therapymayrapp16Noch keine Bewertungen
- P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokument4 SeitenP ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)fraditayyunusNoch keine Bewertungen
- ESMON Study ArticleDokument7 SeitenESMON Study ArticleAhmedaref EzrinNoch keine Bewertungen
- Full TextDokument8 SeitenFull TextJeNeth RevilNoch keine Bewertungen
- Continuous Glucose Monitoring: A Review of Recent Studies Demonstrating Improved Glycemic OutcomesDokument13 SeitenContinuous Glucose Monitoring: A Review of Recent Studies Demonstrating Improved Glycemic OutcomesguillermocochaNoch keine Bewertungen
- Gestational Diabetes Mellitus, Diagnostic Approaches and Maternal Offspring ComplicationsDokument12 SeitenGestational Diabetes Mellitus, Diagnostic Approaches and Maternal Offspring ComplicationsSaraid RuizNoch keine Bewertungen
- Diabetes & Metabolic Syndrome: Clinical Research & ReviewsDokument5 SeitenDiabetes & Metabolic Syndrome: Clinical Research & ReviewsRizaldi FirdausNoch keine Bewertungen
- Ajtr0014 4757Dokument20 SeitenAjtr0014 4757Eyal RobinsonNoch keine Bewertungen
- Research ArticleDokument12 SeitenResearch ArticleRodas GetachewNoch keine Bewertungen
- GDM Full PresentationDokument37 SeitenGDM Full PresentationDanielleMajorGalassoNoch keine Bewertungen
- High Maternal Hba Is Associated With Overweight In Neonates: Dan Med Bul Ϧϫ/ϪDokument6 SeitenHigh Maternal Hba Is Associated With Overweight In Neonates: Dan Med Bul Ϧϫ/ϪHerry SasukeNoch keine Bewertungen
- The Association Between Estimated Average Glucose Levels and Fasting Plasma Glucose LevelsDokument4 SeitenThe Association Between Estimated Average Glucose Levels and Fasting Plasma Glucose LevelsRina MachdalenaNoch keine Bewertungen
- Limitations of Conventional Methods of Self-Monitoring of Blood GlucoseDokument5 SeitenLimitations of Conventional Methods of Self-Monitoring of Blood GlucoseMohammed ElnaggarNoch keine Bewertungen
- Metabolic ControlDokument9 SeitenMetabolic ControlRommanah AzmiNoch keine Bewertungen
- What Are The Existing Diagnostic Criteria?Dokument6 SeitenWhat Are The Existing Diagnostic Criteria?Utkarsh AbhilashNoch keine Bewertungen
- Diabetes Spectr 2007 Langer 101 5Dokument5 SeitenDiabetes Spectr 2007 Langer 101 5salijanstarNoch keine Bewertungen
- GlucoseDokument5 SeitenGlucosebagsouravNoch keine Bewertungen
- Continuous Glucose MonitoringVon EverandContinuous Glucose MonitoringWeiping JiaNoch keine Bewertungen
- Pediatric Notes: Nutrition and Metabolic DiseaseDokument33 SeitenPediatric Notes: Nutrition and Metabolic DiseasefraditayyunusNoch keine Bewertungen
- Abstrak DR Jeffri FK UNHAS MakasarDokument1 SeiteAbstrak DR Jeffri FK UNHAS MakasarfraditayyunusNoch keine Bewertungen
- Perioperative Myocardial Ischaemia in Non-Cardiac Surgery: General Anaesthesia Tutorial375Dokument7 SeitenPerioperative Myocardial Ischaemia in Non-Cardiac Surgery: General Anaesthesia Tutorial375Halim SudonoNoch keine Bewertungen
- Igd ManDokument1 SeiteIgd ManfraditayyunusNoch keine Bewertungen
- Profopol Vs KTMDokument7 SeitenProfopol Vs KTMAuliaRusdiAllmuttaqienNoch keine Bewertungen
- Upload 8Dokument2 SeitenUpload 8cingyaNoch keine Bewertungen
- AanDokument1 SeiteAanfraditayyunusNoch keine Bewertungen
- Poed APN: Jadwal Jaga Kepaniteraan Klinik Rsud Labuang Baji Periode 7 - 14 Desember 2014Dokument2 SeitenPoed APN: Jadwal Jaga Kepaniteraan Klinik Rsud Labuang Baji Periode 7 - 14 Desember 2014fraditayyunusNoch keine Bewertungen
- Morning Report: Emergency Room Wahidin Sudirohusodo General Hospital Makassar July 9th, 2014Dokument20 SeitenMorning Report: Emergency Room Wahidin Sudirohusodo General Hospital Makassar July 9th, 2014fraditayyunusNoch keine Bewertungen
- Victoria Secret Body (A Month On December !) : Step 1 60 Dumbell Side LungesDokument5 SeitenVictoria Secret Body (A Month On December !) : Step 1 60 Dumbell Side LungesfraditayyunusNoch keine Bewertungen
- Koran Bedah Saraf TGL 1 Oct 2014Dokument9 SeitenKoran Bedah Saraf TGL 1 Oct 2014fraditayyunusNoch keine Bewertungen
- TreatmentDokument1 SeiteTreatmentfraditayyunusNoch keine Bewertungen
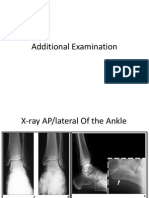
- Ankle Trauma TreatmentDokument3 SeitenAnkle Trauma TreatmentfraditayyunusNoch keine Bewertungen
- Ni Hms 39248Dokument8 SeitenNi Hms 39248fraditayyunusNoch keine Bewertungen
- TreatmentDokument1 SeiteTreatmentfraditayyunusNoch keine Bewertungen
- Tugas Hikmah Additional ExamDokument15 SeitenTugas Hikmah Additional ExamfraditayyunusNoch keine Bewertungen
- Mechanism of Trauma Lauge-Hansen Classification: Acute Fractures and Dislocations in Netter's and Sport MedicineDokument4 SeitenMechanism of Trauma Lauge-Hansen Classification: Acute Fractures and Dislocations in Netter's and Sport MedicinefraditayyunusNoch keine Bewertungen
- Initial AssesmentDokument30 SeitenInitial Assesmentfraditayyunus0% (1)
- P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokument4 SeitenP ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)fraditayyunusNoch keine Bewertungen
- P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokument4 SeitenP ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)fraditayyunusNoch keine Bewertungen
- Levemir Flex PenDokument2 SeitenLevemir Flex PenDika FrantikoNoch keine Bewertungen
- Tutuwaa Final of Finals2Dokument69 SeitenTutuwaa Final of Finals2gideon A. owusuNoch keine Bewertungen
- Exercise in DiabetesDokument77 SeitenExercise in DiabetesAkshay BangadNoch keine Bewertungen
- Insulin For Glycaemic Control in Acute Ischaemic Stroke (Review)Dokument46 SeitenInsulin For Glycaemic Control in Acute Ischaemic Stroke (Review)Talitha PuspaNoch keine Bewertungen
- Medicinus JournalDokument68 SeitenMedicinus JournalDian Rosdiani FajrinNoch keine Bewertungen
- LEADING ARTICLE Inlacin Therapy in Patients With Type-2 Diabetes MellitusDokument10 SeitenLEADING ARTICLE Inlacin Therapy in Patients With Type-2 Diabetes MellitusBabanx Reigncary100% (1)
- Recovery?: Home: CorrespondenceDokument19 SeitenRecovery?: Home: CorrespondenceMahmoud El MohamdyNoch keine Bewertungen
- Diabetes Spectr 2004 Aronoff 183 90Dokument8 SeitenDiabetes Spectr 2004 Aronoff 183 90Bodea DoruNoch keine Bewertungen
- Avances en DiabetesDokument11 SeitenAvances en DiabetesDayan Princess WyNoch keine Bewertungen
- Hypoglycemia in Adults With Diabetes MellitusDokument25 SeitenHypoglycemia in Adults With Diabetes MellitusEsra AljafferNoch keine Bewertungen
- Diabetes CareDokument156 SeitenDiabetes CaresahebjuNoch keine Bewertungen
- Probiotics For Children With Type 1 DiabetesDokument9 SeitenProbiotics For Children With Type 1 DiabetesMahesh JayaramanNoch keine Bewertungen
- امتحان برومترك بكالوريوس صيدلة محلول بالكاملDokument10 Seitenامتحان برومترك بكالوريوس صيدلة محلول بالكاملعزالدين الطيارNoch keine Bewertungen
- ISPAD 2022 NutritionDokument71 SeitenISPAD 2022 NutritionsuNoch keine Bewertungen
- DCMNT PDFDokument36 SeitenDCMNT PDFOh HudaNoch keine Bewertungen
- Gliclazide Modified Release.10Dokument8 SeitenGliclazide Modified Release.10Sowbhagya LaxmiNoch keine Bewertungen
- Garber 2007Dokument6 SeitenGarber 2007Diana SamuezaNoch keine Bewertungen
- Nhanes IiiDokument9 SeitenNhanes Iiiannaafia69969Noch keine Bewertungen
- Diabetes Self-Management Education For Adults With Type 2 DiabetesDokument18 SeitenDiabetes Self-Management Education For Adults With Type 2 DiabetesNicole Sofia Martinez TovarNoch keine Bewertungen
- 342 MCQDokument4 Seiten342 MCQRAJESH SHARMA100% (1)
- Awareness of Diabetic Children Care Givers About Complications of Type 1 Diabetes Mellitus in Dhahran, Saudi ArabiaDokument7 SeitenAwareness of Diabetic Children Care Givers About Complications of Type 1 Diabetes Mellitus in Dhahran, Saudi ArabiaInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Diabetes Flow ChartDokument8 SeitenDiabetes Flow ChartNicky ChhajwaniNoch keine Bewertungen
- Diabetes Complication LectureDokument63 SeitenDiabetes Complication LectureDoni MarthenNoch keine Bewertungen
- Safety and Efficacy of Once-Weekly Semaglutide Vs Additinal Oral Antidiabetic Drugs in Japanese People With Inadequately Controlled Type 2 DMDokument11 SeitenSafety and Efficacy of Once-Weekly Semaglutide Vs Additinal Oral Antidiabetic Drugs in Japanese People With Inadequately Controlled Type 2 DMRizky Putri Agustina RumapeaNoch keine Bewertungen
- AAHA Diabetes Guidelines - FinalDokument21 SeitenAAHA Diabetes Guidelines - FinalKátia SouzaNoch keine Bewertungen
- Seminar: DiagnosisDokument14 SeitenSeminar: DiagnosisyenyenNoch keine Bewertungen
- ADA Type 2 Diabetes in ChildrensDokument10 SeitenADA Type 2 Diabetes in ChildrensCho Maharani Rijhigo BaeNoch keine Bewertungen
- Diamicron MRDokument50 SeitenDiamicron MROmar Kamel Rayyan33% (3)
- Health, Jurnal Bhs Inggris Bu Titin OkeDokument26 SeitenHealth, Jurnal Bhs Inggris Bu Titin OkePrast PratamaNoch keine Bewertungen