Beruflich Dokumente
Kultur Dokumente
Effect of Glimepiride Compared With Glibenclamide On Post Prandial Blood Sugar in Type II Diabetes Mellitus Patients
Hochgeladen von
Khuriyatun NadhifahOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Effect of Glimepiride Compared With Glibenclamide On Post Prandial Blood Sugar in Type II Diabetes Mellitus Patients
Hochgeladen von
Khuriyatun NadhifahCopyright:
Verfügbare Formate
www.ijbcp.
com International Journal of Basic & Clinical Pharmacology | January-February 2014 | Vol 3 | Issue 1 Page 96
IJBCP International Journal of Basic & Clinical Pharmacology
Print ISSN: 2319-2003 | Online ISSN: 2279-0780
Research Article
Effect of glimepiride compared with glibenclamide on post prandial
blood sugar in type II diabetes mellitus patients
Meenu Rani
1
*, Shailesh Yadav
1
, Seema Choudhary
2
, Seema Sharma
2
, Surya Mani Pandey
3
INTRODUCTION
Diabetes mellitus is a chronic progressive metabolic
disorder characterized by hyperglycemia mainly due to
absolute or relative deficiency of insulin hormone.
1
According to the World Health Organization (WHO)
report, India today heads the world with over 32 million
diabetic patients and this number is projected to increase
to 79.4 million by the year 2030.
2
This multi-factorial
disease is hypothesized to damage cell membranes
resulting in elevated oxidative stress. The major concern
with diabetes clearly relates to marked increase of
neuropathy and series morbidity and mortality related to
the development of other complications.
3
New
recommendations for the classification and diagnosis of
diabetes mellitus include the preferred use of the terms
type 1 and type 2 instead of IDDM and NIDDM
to designate the two major types of diabetes mellitus.
4
Type 1 diabetes is results from a cellular-mediated
autoimmune destruction of the beta -cells of the pancreas.
Autoimmune destruction of beta-cells has multiple
genetic predispositions and is also related to
environmental factors that are still poorly defined.
5
Type
2 diabetes- There are probably many different causes of
this form of diabetes. Insulin secretion is defective in
these patients and insufficient to compensate for insulin
resistance. The risk of developing this form of diabetes
increases with age, obesity, and lack of physical activity.
5
ABSTRACT
Background: Diabetes mellitus is a major public health problem with
many complications. The Global Burden of Diabetes Study has projected
that there will be a 122% increase in the number of people with diabetes
mellitus worldwide in 2025 compared to 1995. Despite the availability of
new agents for the treatment of type 2 diabetes mellitus oral sulfonylureas
remain a cornerstone of therapy.
Glibenclamide and glimepiride are widely
used sulfonylurea antidiabetic drugs.
Methods: A randomized, open, parallel group study was conducted by the
Department of Pharmacology in association with Department of Medicine
at Maharishi Markandeshwar Institute of Medical Sciences & Research
(MMIMSR), Mullana, Ambala. Total 50 patients were divided into two
groups I & II. In Group I (n=25) glibenclamide (5-15 mg/day) & in Group
II (n=25) glimepiride (1-6mg/day) was administered for a period of 24
weeks and data analyzed by Students t- test.
Results: There was a significant improvement in the post prandial blood
sugar score (p<0.05) in both the study groups (I&II) after 24 weeks but post
prandial blood level did not differ significantly (p>0.05) between the two
groups.
Conclusions: Both the drugs glibenclamide and glimepiride were
effectively reduced post prandial blood sugar in both the groups. But these
sulfonylurea drugs lowered post prandial blood sugar to a similar degree
without significant difference between the two groups.
Keywords: Type II diabetes mellitus, Glimepiride, Glibenclamide, Post
prandial blood sugar, Sulfonylureas
doi: 10.5455/2319-2003.ijbcp20140210
1
Department of Pharmacology,
MMIMSR, Mullana-133203,
Ambala, Haryana, India,
2
Department of Community
Medicine, MAMC, Agroha-125047,
Hisar, Haryana, India,
3
Assistant Prof. (M.Sc., MCA),
MAMC, Agroha-125047, Hisar,
Haryana, India
Received: 19 November 2013
Accepted: 9 December 2013
*Correspondence to:
Meenu Rani,
Email: meenusaharan23@gmail.com
2014 Rani M et al. This is an
open-access article distributed under
the terms of the Creative Commons
Attribution Non-Commercial
License, which permits unrestricted
non-commercial use, distribution,
and reproduction in any medium,
provided the original work is
properly cited.
Rani M et al. Int J Basic Clin Pharmacol. 2014 Feb;3(1):96-99
International Journal of Basic & Clinical Pharmacology | January-February 2014 | Vol 3 | Issue 1 Page 97
If and when diet therapy fails, oral hypoglycemic agents
are the usual next step in the therapeutic armamentarium.
6
Glibenclamide & glimepiride both are second-generation
sulfonylureas.
7
The main effect of sulfonylurea (including
glimepiride) is increase in the beta cells insulin release as
a response to the serum glucose level. It is well
established that sulfonylureas produce insulin secretion
and improve tissue utilization of glucose at cellular level
which was responsible for lowering of blood glucose
level.
8
METHODS
This randomized, open, parallel group study was
conducted in the patients suffering from type 2 diabetes
mellitus by the Department of Pharmacology in
association with Department of Medicine at Maharishi
Markandeshwar Institute of Medical Sciences &
Research (MMIMSR), Mullana, Ambala. All the patients
visiting the Department of Medicine, MMIMSR, Mullana
were screened and 65 patients of both the sexes suffering
from type 2 diabetes mellitus were selected for the study.
15 patients were lost in the follow up period of the
patients and were declared as drop outs from the study
and thus 50 patients completed the study. All the patients
gave their written consent before enrolment in the study.
These patients were divided in group I & II. Group I (25
patients): This group included the eligible patients
diagnosed with type 2 diabetes mellitus and these patients
were administered glibenclamide in dose range of 5-15
mg/day, for 24 weeks. Group II (25 patients): This group
included the eligible patients diagnosed with type 2
diabetes mellitus and these patients were administered
glimepiride in dose range of 1-6 mg/day, for 24 weeks.
Patients with history of drug allergy, alcohol intake,
congestive cardiac failure, female patients who were
pregnant, lactating were excluded. Clinical evaluation of
all the patients was done by measuring blood sugar
before administration of drug. Efficacy of study drugs
evaluated by measuring the post prandial blood level at
start of pharmacotherapy, 2 weeks, 4 weeks and then
every 4 weeks up to 24 weeks. Data were collected and
the analysis of each variable was performed on the
change from baseline values using Students t- test. A
p value less than or equal to 0.05 was considered
statistically significant and p>0.05-non significant.
RESULTS
The mean of all the baseline characteristics and SD in
both groups were given (Table 1).
Table 1: Baseline characteristics in study groups.
Characteristic Group I Group II
Number of patients 25 25
Sex(Male/Female) 12/13 10/15
Mean Age 53.0013.55 54.0811.69
Post prandial blood
sugar(mg/dl)
264.4564.39 266.3764.04
Data shows that the patients in group I started improving
significantly with treatment as the mean scores of post
prandial blood sugar reduced significantly (p<0.05)
(Table 2).
Table 2: Mean scores of post prandial blood sugar in
group I patients with treatment over 24 weeks.
MeanSD p-value
Baseline 264.4564.39
Week 2 262.1363.84 <0.05
Week 4 260.2963.93 <0.05
Week 8 258.2964.29 <0.05
Week 12 256.8164.25 <0.05
Week 16 255.8164.49 <0.05
Week 18 251.9364.59 <0.05
Week22 252.8164.56 <0.05
Week 24 248.2569.29 <0.05
Data shows that the mean scores of post prandial blood
sugar reduced significantly (p<0.05) (Table 3).
Table 3: Mean scores of post prandial blood sugar in
group II patients with treatment over 24 weeks.
MeanSD p-value
Baseline 266.3764.04
Week 2 262.9364.09 <0.05
Week 4 260.5764.15 <0.05
Week 8 257.7364.08 <0.05
Week 12 255.2564.26 <0.05
Week 16 253.0964.68 <0.05
Week 18 252.1364.73 <0.05
Week22 250.0564.33 <0.05
Week 24 249.2164.23 <0.05
Data shows that change in post prandial sugar scores in
both the groups did not differ significantly (p>0.05)
(Table 4).
Table 4: Comparative mean scores of post prandial
blood sugar in group I and group II patients over 24
weeks.
Group I
(Mean)
Group II
(Mean)
p- value
Baseline 264.4564.39 266.3764.04 0.91
Week 2 262.1363.84 262.9364.09 0.96
Week 4 260.2963.93 260.5764.15 0.98
Week 8 258.2964.29 257.7364.08 0.97
Week 12 256.8164.25 255.2564.26 0.93
Week 16 255.8164.49 253.0964.68 0.88
Week 18 251.9364.59 252.1364.73 0.99
Week22 252.8164.56 250.0564.33 0.88
Week 24 248.2569.29 249.2164.23 0.96
Between group comparison [unpaired studentst test]
Rani M et al. Int J Basic Clin Pharmacol. 2014 Feb;3(1):96-99
International Journal of Basic & Clinical Pharmacology | January-February 2014 | Vol 3 | Issue 1 Page 98
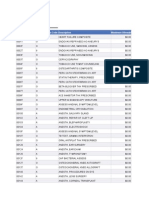
Figure showing comparative change in post prandial
blood sugar scores (Figure 1).
Figure 1: Comparative change in post prandial blood
sugar scores.
DISCUSSION
DM virtually affects every system of the body mainly due
to metabolic disturbances caused by hyperglycemia,
especially if diabetes control over a period of time proves
to be suboptimal.
9
Until recently it was believed to be a
disease occurring mainly in developed countries, but
recent findings reveal a rise in number of new cases of
type 2 DM with an earlier onset and associated
complications in developing countries
10
. Long-term
complications of diabetes include retinopathy with
potential loss of vision; nephropathy leading to renal
failure; peripheral neuropathy with risk of foot ulcers,
amputations, and Charcot joints; and autonomic
neuropathy causing gastrointestinal, genitourinary, and
cardiovascular symptoms and sexual dysfunction. Patients
with diabetes have an increased incidence of
atherosclerotic cardiovascular, peripheral arterial, and
cerebrovascular disease. Hypertension and abnormalities
of lipoprotein metabolism are often found in people with
diabetes.
11
The mean age of the patients in both the groups did not
differ significantly (p>0.05).The mean age and SD in
group A was 53.00 13.55 and in Group B 54.0811.69
(Table1).
The parameter used to assess the efficacy of drug therapy
was the post prandial blood sugar during the study. The
results showed that, in group I, the mean score of post
prandial blood sugar at baseline was 264.4564.39, at 4
weeks 260.2963.93 and at 24 weeks it dropped to
248.2569.29. In group II, the mean score of post
prandial blood sugar at baseline was 266.3764.04, at 4
weeks 260.5764.15 and at 24 weeks, it dropped to
249.2164.23. Therefore patients in both the study groups
started improving significantly with treatment by the end
of 2
nd
week as the mean scores of post prandial blood
sugar reduced significantly (p<0.05).The improvement
continued over time and mean scores were reduced
significantly at the end of 24 weeks(Table 2and Table 3).
Studies done by Groop et al.
12
Skrapari I et al.
13
and
Abdul B et al.
14
showed comparable results which were
similar to the present study.
While comparing the mean scores of post prandial blood
sugar in group I and group II patients over 24 weeks,
change in post prandial blood sugar scores in both the
groups also did not differ significantly (p>0.05) and over
the time both the groups maintained improvement which
was comparable throughout the study. Studies done by
Abdul B et al.
14
showed comparable results which were
similar to the present study.
CONCLUSION
During the study, it can be concluded that both
glibenclamide and glimepiride are equally effective in
reducing the post prandial blood sugar in type 2 diabetes
mellitus patients but there is no difference in their
efficacy as both the drugs lowered the post prandial blood
sugar to similar extent.
Funding: No funding sources
Conflict of interest: None declared
Ethical approval: The study was approved by the
Institutional Ethics Committee
REFERENCES
1. Bihari Lal Shrivastava SR, Shrivastava PS,
Ramasamy J. Role of self-care in management of
diabetes mellitus. J Diabetes Metab Disord.
2013;12:14.
2. Muninarayana C, Balachandra G, Hiremath SG,
Iyengar K, Anil NS. Prevalence and awareness
regarding diabetes mellitus in rural Tamaka, Kolar.
Int J Diabetes Dev Ctries. 2010Jan-Mar;30(1):1821.
3. Saumya SM, Mahaboob B. Antioxidant effect of
Lagerstroemia specicosapers (Banaba) leaf extract in
streptozotocin-induced diabetic mice. Indian J Exp
Biol. 2011;49 (2):125.
4. Mayfield J. Diagnosis and classification of diabetes
mellitus: new criteria. Am Fam Physian.
1998 Oct;58(6):1355-62.
5. American Diabetes Association. Diagnosis and
Classification of Diabetes Mellitus. Diabetes Care.
2012;35(1):64-71.
6. Miller LJ, Salman K, Shulman LH, Rose LI. Bed
time insulin added to daytime sulfonylureas
improves glycemic control in uncontrolled type 2
diabetes. Clin Pharmacol Ther. 1993Mar;53(3):380-
4.
7. Aquilante CL. Sulfonylurea pharmacogenomics in
type 2 diabetes: the influence of drug target and
diabetes risk polymorphisms. Expert Rev Cardiovasc
Ther. 2010Mar;8(3):35972.
8. Prashanth S, Kumar AA, Madhu B, Rama N, Sagar
JV. Pharmacokinetic and pharmacodynamic drug
235
240
245
250
255
260
265
270
0 2 4 8 12 16 18 22 24
Group A
Group B
M
e
a
n
S
c
o
r
e
Weeks
Rani M et al. Int J Basic Clin Pharmacol. 2014 Feb;3(1):96-99
International Journal of Basic & Clinical Pharmacology | January-February 2014 | Vol 3 | Issue 1 Page 99
interactions of carbamazepine and glibenclamide in
healthy albino wistar rats. J Pharmacol
Pharmacother. 2011Jan-Mar;2(1):710.
9. World health organization: Definition, diagnosis and
classification of diabetes mellitus and its
complications. Geneva: World health organization.
1999.
10. Chuang LM, Tsai ST, Huang BY, Tai TY: The status
of diabetes control in Asiaa cross-sectional survey
of 24 317 patients with diabetes mellitus in 1998.
Diabet Med. 2002;19(12):978-85.
11. American Diabetes Association. Diagnosis and
Classification of Diabetes Mellitus. Diabetes Care.
2009Jan;32:67.
12. Groop L, Wahlinboll E, Groop PH, Totterman KJ,
Melander A, Tolppaner EM, et al. Pharmacokinetics
and metabolic effects of glibenclamide and glipizide
in type 2 diabetics. Eur J Clin Pharmacol.
1985;28(6):697-704.
13. Skrapari I, Perra D, Ioanndis I, Karabina SA, Elisaf
M, Tselepis AD, et al. Glibenclamide improves
postprandial hypertriglyceridaemia in type 2 diabetic
patients by reducing chylomicrons but not the very
low-density lipoprotein subfraction levels. Diabetic
Medicine. 2001Oct;18(10):781-5.
14. Abdul B, Riaz M, Fawwad A. Glimepiride:
evidence-based facts, trends, and observations.
Vascular Health and Risk Management.
2012Aug;8:463-72.
doi:10.5455/2319-2003.ijbcp20140210
Cite this article as: Rani M, Yadav S, Choudhary S,
Sharma S, Pandey SM. Effect of glimepiride
compared with glibenclamide on post prandial blood
sugar in type II diabetes mellitus patients. Int J Basic
Clin Pharmacol 2014;3:96-9.
Das könnte Ihnen auch gefallen
- Diabetes Mellitus and Oral Health: An Interprofessional ApproachVon EverandDiabetes Mellitus and Oral Health: An Interprofessional ApproachNoch keine Bewertungen
- Role of Antioxidant Therapy in Management of Type - 2 Diabetes MellitusDokument6 SeitenRole of Antioxidant Therapy in Management of Type - 2 Diabetes MellitusDr_vishalvadgamaNoch keine Bewertungen
- Glibenclamide For Diabetic Tipe IIDokument5 SeitenGlibenclamide For Diabetic Tipe IIAnonymous A1qFGIXACNoch keine Bewertungen
- Practical Insulin: A Handbook for Prescribing ProvidersVon EverandPractical Insulin: A Handbook for Prescribing ProvidersBewertung: 5 von 5 Sternen5/5 (2)
- Kumamoto StudyDokument19 SeitenKumamoto StudyCarlosZamNoch keine Bewertungen
- Shalini Chawla, Nitin Kaushik, Narinder Pal Singh, Raktim Ghosh, Alpana SaxenaDokument41 SeitenShalini Chawla, Nitin Kaushik, Narinder Pal Singh, Raktim Ghosh, Alpana Saxena88AKKNoch keine Bewertungen
- Ass Knowledge and MaDokument1 SeiteAss Knowledge and MaB04-BALKIS SOLEHAHNoch keine Bewertungen
- JETIR1905867 - Reduction in Drug Dosage - DR - BiswaroopRoyChowdhury PDFDokument12 SeitenJETIR1905867 - Reduction in Drug Dosage - DR - BiswaroopRoyChowdhury PDFSudhir YadavNoch keine Bewertungen
- Efficacy of Metformin Versus Insulin in The Management of Pregnancy With DiabetesDokument5 SeitenEfficacy of Metformin Versus Insulin in The Management of Pregnancy With DiabetesRizky Agustian HadiNoch keine Bewertungen
- ESMON Study ArticleDokument7 SeitenESMON Study ArticleAhmedaref EzrinNoch keine Bewertungen
- 1 s2.0 S0149291803800930 MainDokument15 Seiten1 s2.0 S0149291803800930 Mainpepe_onetNoch keine Bewertungen
- The Study of Cumin On Blood Pressure in Patients With Diabeties Type IiDokument5 SeitenThe Study of Cumin On Blood Pressure in Patients With Diabeties Type IiBaru Chandrasekhar RaoNoch keine Bewertungen
- Article Wjpps 1444727958Dokument11 SeitenArticle Wjpps 1444727958CMargs ConceptsNoch keine Bewertungen
- Effect of Metformin As Adjunct Therapy With Insulin in Adolescent Pakistani People With Type 1 DiabetesDokument4 SeitenEffect of Metformin As Adjunct Therapy With Insulin in Adolescent Pakistani People With Type 1 DiabetesSundas EjazNoch keine Bewertungen
- Efektivitas Konseling DM Dalam Meningkatkan Kepatuhan Dan Pengendalian Gula Darah Pada Diabetes Melitus Tipe 2Dokument12 SeitenEfektivitas Konseling DM Dalam Meningkatkan Kepatuhan Dan Pengendalian Gula Darah Pada Diabetes Melitus Tipe 2AmmarForeverAjaNoch keine Bewertungen
- The Influence of Glucose Self-Monitoring On Glycaemic Control in Patients With Diabetes Mellitus in SudanDokument5 SeitenThe Influence of Glucose Self-Monitoring On Glycaemic Control in Patients With Diabetes Mellitus in SudanZam-zam RsiNoch keine Bewertungen
- Garlic AntidiabeticDokument6 SeitenGarlic AntidiabeticSalis MaghfurinaNoch keine Bewertungen
- Ias 25 2 40 49Dokument10 SeitenIas 25 2 40 49Erambaji NazNoch keine Bewertungen
- ANNALS-Diabetes Tipo IIDokument16 SeitenANNALS-Diabetes Tipo IIewb100% (2)
- 1110-Article Text-5889-2-10-20200229Dokument15 Seiten1110-Article Text-5889-2-10-20200229NavaaNoch keine Bewertungen
- Diabetes and Clinical Research: ClinmedDokument4 SeitenDiabetes and Clinical Research: ClinmedHerybert KiiNoch keine Bewertungen
- Https:/zero Sci-Hub Se/5089//boulet2016Dokument10 SeitenHttps:/zero Sci-Hub Se/5089//boulet2016Caroline QueirogaNoch keine Bewertungen
- Cud BdiabetesDokument10 SeitenCud BdiabetesShitanjni WatiNoch keine Bewertungen
- 737-Article Text-5178-1-10-20221104Dokument9 Seiten737-Article Text-5178-1-10-20221104Jeni FebroniaNoch keine Bewertungen
- 559-Article Text-2578-2-10-20230506Dokument4 Seiten559-Article Text-2578-2-10-20230506Uri CohenNoch keine Bewertungen
- 1 s2.0 S0002916523463010 MainDokument13 Seiten1 s2.0 S0002916523463010 MainsilviaNoch keine Bewertungen
- REVIEWDokument27 SeitenREVIEWRakhmat WabulaNoch keine Bewertungen
- The Relationship of Diabetes Mellitus Diet Knowledge With Blood Glucose Levels in Patients Diabetes Mellitus Type Ii in Hermana Hospital LembeanDokument5 SeitenThe Relationship of Diabetes Mellitus Diet Knowledge With Blood Glucose Levels in Patients Diabetes Mellitus Type Ii in Hermana Hospital LembeanIrene Hana HutagalungNoch keine Bewertungen
- HbA1C AS AN INDEX OF GLYCEMIC STATUS IN OBESE TYPE 2 DIABETICSDokument6 SeitenHbA1C AS AN INDEX OF GLYCEMIC STATUS IN OBESE TYPE 2 DIABETICSInternational Journal of Clinical and Biomedical Research (IJCBR)Noch keine Bewertungen
- Intensive InsulinDokument5 SeitenIntensive InsulinAndreea GherasimNoch keine Bewertungen
- Efficacy of Glyburide/Metformin Tablets Compared With Initial MonotherapyDokument7 SeitenEfficacy of Glyburide/Metformin Tablets Compared With Initial MonotherapyriphqaNoch keine Bewertungen
- ATTD 2011 Year Book: Advanced Technologies and Treatments for DiabetesVon EverandATTD 2011 Year Book: Advanced Technologies and Treatments for DiabetesNoch keine Bewertungen
- Meeting the American Diabetes Association Standards of Care: An Algorithmic Approach to Clinical Care of the Diabetes PatientVon EverandMeeting the American Diabetes Association Standards of Care: An Algorithmic Approach to Clinical Care of the Diabetes PatientNoch keine Bewertungen
- Artikel Daun SalamDokument12 SeitenArtikel Daun SalamernaaulianaNoch keine Bewertungen
- Efficacy of Vildagliptin and Metformin Combination in Type II Diabetes Mellitus PatientsDokument4 SeitenEfficacy of Vildagliptin and Metformin Combination in Type II Diabetes Mellitus PatientsDR.P.KALAI SELVINoch keine Bewertungen
- 1 SMDokument8 Seiten1 SMWanti WantiNoch keine Bewertungen
- 05 Iajps05062017Dokument6 Seiten05 Iajps05062017Baru Chandrasekhar RaoNoch keine Bewertungen
- Effect of Increasing Duration of Diabetes Mellitus Type 2 On Glycated Hemoglobin and Insulin SensitivityDokument5 SeitenEffect of Increasing Duration of Diabetes Mellitus Type 2 On Glycated Hemoglobin and Insulin SensitivityAlifLaelaNoch keine Bewertungen
- The Efficacy of A Health Program and A Food Diary in Blood Sugar Control of Patients With Type 2 DiabetesDokument7 SeitenThe Efficacy of A Health Program and A Food Diary in Blood Sugar Control of Patients With Type 2 DiabetesInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Insulin Therapy For Type 2 Diabetes Mellitus.Dokument11 SeitenInsulin Therapy For Type 2 Diabetes Mellitus.Clarissa CozziNoch keine Bewertungen
- Metformina y Estrés Oxidativo en Pacientes DiabéticosDokument14 SeitenMetformina y Estrés Oxidativo en Pacientes DiabéticosJesus D. Hernandez GuitianNoch keine Bewertungen
- Bismillah Fix Hba1c3Dokument8 SeitenBismillah Fix Hba1c3NsafifahNoch keine Bewertungen
- Nfs 774 Case StudyDokument37 SeitenNfs 774 Case Studyapi-533845626Noch keine Bewertungen
- Eqlima Aisch 2022Dokument10 SeitenEqlima Aisch 2022Wirda FaswitaNoch keine Bewertungen
- Eficiencia y Tolerabilidad Glimepirida y MetfomrinaDokument7 SeitenEficiencia y Tolerabilidad Glimepirida y MetfomrinaMarioA.VelascoCórdobaNoch keine Bewertungen
- Journal Medicine: The New EnglandDokument11 SeitenJournal Medicine: The New EnglandYancy Erazo DoradoNoch keine Bewertungen
- Estudio PRODIACORDokument10 SeitenEstudio PRODIACORNatalia FernandezNoch keine Bewertungen
- Type 2 Diabetes Literature ReviewDokument7 SeitenType 2 Diabetes Literature Reviewdoawpfcnd100% (1)
- Silimarina ArticuloDokument6 SeitenSilimarina ArticuloArturo MarcialNoch keine Bewertungen
- Dia Care 2002 Pastors 608 13Dokument6 SeitenDia Care 2002 Pastors 608 13Isnar Nurul AlfiyahNoch keine Bewertungen
- Diabetes MellitusDokument8 SeitenDiabetes Mellitusi_anitaNoch keine Bewertungen
- Insulin ResistanceDokument48 SeitenInsulin ResistanceLavina JainNoch keine Bewertungen
- Promosi Kesehatan Dengan Model Sesama Berpengaruh Terhadap Kepatuhan Makan Pasien DM Tipe 2Dokument14 SeitenPromosi Kesehatan Dengan Model Sesama Berpengaruh Terhadap Kepatuhan Makan Pasien DM Tipe 2Ash RoryNoch keine Bewertungen
- Efficacy and Safety of Biosimilar Glargine-IMGDokument8 SeitenEfficacy and Safety of Biosimilar Glargine-IMGSiddiq MohammedNoch keine Bewertungen
- Paper DM NutritionDokument10 SeitenPaper DM NutritionyinvilllNoch keine Bewertungen
- Clinical Study Antidiabetic Effect of Fenugreek Seed Powder Solution (Trigonella Foenum-Graecum L.) On Hyperlipidemia in Diabetic PatientsDokument9 SeitenClinical Study Antidiabetic Effect of Fenugreek Seed Powder Solution (Trigonella Foenum-Graecum L.) On Hyperlipidemia in Diabetic Patientssartaeva.aigul1Noch keine Bewertungen
- 7979 12179 1 SMDokument2 Seiten7979 12179 1 SMRobert DwitamaNoch keine Bewertungen
- Glucose Intake and Utilization in Pre-Diabetes and Diabetes: Implications for Cardiovascular DiseaseVon EverandGlucose Intake and Utilization in Pre-Diabetes and Diabetes: Implications for Cardiovascular DiseaseBewertung: 4 von 5 Sternen4/5 (1)
- DM TyroidDokument10 SeitenDM TyroidKhuriyatun NadhifahNoch keine Bewertungen
- Pi Is 0020729205002377Dokument1 SeitePi Is 0020729205002377Khuriyatun NadhifahNoch keine Bewertungen
- JBR 26 04 235Dokument6 SeitenJBR 26 04 235Khuriyatun NadhifahNoch keine Bewertungen
- Risk Factors For Macrosomia in Infants Born To Latina Women: Original ArticleDokument7 SeitenRisk Factors For Macrosomia in Infants Born To Latina Women: Original ArticleKhuriyatun NadhifahNoch keine Bewertungen
- Adverse Maternal Outcomes Associated With Fetal Macrosomia: What Are The Risk Factors Beyond Birthweight?Dokument6 SeitenAdverse Maternal Outcomes Associated With Fetal Macrosomia: What Are The Risk Factors Beyond Birthweight?Khuriyatun NadhifahNoch keine Bewertungen
- Macrosomia Risk Factors and Labor Outcome Methal-A. Alrubae, Klood JaferDokument8 SeitenMacrosomia Risk Factors and Labor Outcome Methal-A. Alrubae, Klood JaferKhuriyatun NadhifahNoch keine Bewertungen
- Risk Factors For Fetal Macrosomia: The Importance of A Positive Oral Glucose Challenge TestDokument7 SeitenRisk Factors For Fetal Macrosomia: The Importance of A Positive Oral Glucose Challenge TestKhuriyatun NadhifahNoch keine Bewertungen
- Maternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyDokument7 SeitenMaternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyKhuriyatun NadhifahNoch keine Bewertungen
- OSPE DU MedicineDokument101 SeitenOSPE DU MedicinesaifNoch keine Bewertungen
- GI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyDokument11 SeitenGI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyTony LeeNoch keine Bewertungen
- Prezentare AromaDokument56 SeitenPrezentare AromaMamaliga LizaNoch keine Bewertungen
- The Effects of Caffeine On Voice A Systematic ReviewDokument13 SeitenThe Effects of Caffeine On Voice A Systematic ReviewChrisNoch keine Bewertungen
- Nursing Care For ElderlyDokument7 SeitenNursing Care For ElderlyNeenu Rajput83% (12)
- 2nd Quarter Exam Science 10Dokument11 Seiten2nd Quarter Exam Science 10Brille Anthony BunielNoch keine Bewertungen
- 1st Summative Test Grade 9Dokument4 Seiten1st Summative Test Grade 9Jane Limsan Paglinawan87% (61)
- 2 - Megaloblastic Anaemia EssayDokument2 Seiten2 - Megaloblastic Anaemia EssayLefteris ChatzidoukasNoch keine Bewertungen
- ChickenpoxDokument5 SeitenChickenpoxShan MunozNoch keine Bewertungen
- RAD RLE MCN 6 Case StudyDokument9 SeitenRAD RLE MCN 6 Case StudyCathleen Nasis Forrosuelo100% (2)
- Hand Tool ReportDokument6 SeitenHand Tool ReportD.k. Asad100% (1)
- Autism Longitudinal StudyDokument10 SeitenAutism Longitudinal Studychristschool1440Noch keine Bewertungen
- DS - Aseptoman® Plus - Pif - en - 1711Dokument2 SeitenDS - Aseptoman® Plus - Pif - en - 1711Serbanica RazvanNoch keine Bewertungen
- Jurnal MigrainDokument6 SeitenJurnal MigrainReksyNoch keine Bewertungen
- Active Transport by ATP-Powered Pumps - Molecular Cell Biology - NCBI BookshelfDokument10 SeitenActive Transport by ATP-Powered Pumps - Molecular Cell Biology - NCBI BookshelfMuhammad KhanNoch keine Bewertungen
- Does The Behaviour of Using Electronic Cigarette Correlates With Respiratory Disease Symptoms?Dokument6 SeitenDoes The Behaviour of Using Electronic Cigarette Correlates With Respiratory Disease Symptoms?Ninuk KurniawatiNoch keine Bewertungen
- Nursing Selection TestDokument3 SeitenNursing Selection TestHarshita GuptaNoch keine Bewertungen
- Performing Chest PhysiotherapyDokument14 SeitenPerforming Chest PhysiotherapyDivya Chauhan100% (1)
- CREW: Department of Veterans Affairs: Regarding PTSD Diagnosis: Quick Referenec To Laws and Regulatinos Relating To Psychiactric DisordersDokument30 SeitenCREW: Department of Veterans Affairs: Regarding PTSD Diagnosis: Quick Referenec To Laws and Regulatinos Relating To Psychiactric DisordersCREWNoch keine Bewertungen
- PsychoticismDokument14 SeitenPsychoticismMahrukhNoch keine Bewertungen
- Anchor Speech On WorkshopDokument6 SeitenAnchor Speech On WorkshopPabhat Kumar100% (2)
- Bracha - 2004 - Freeze Flight FrightDokument7 SeitenBracha - 2004 - Freeze Flight FrightCK MawerNoch keine Bewertungen
- Pharmacology of Drugs For PPHDokument55 SeitenPharmacology of Drugs For PPHFaye CagayanNoch keine Bewertungen
- Chemical MediatorsDokument7 SeitenChemical MediatorsBlaze 69Noch keine Bewertungen
- 2009 Fee ScheduleDokument1.123 Seiten2009 Fee ScheduleNicole HillNoch keine Bewertungen
- Dr. Anas Yasin - MDDokument58 SeitenDr. Anas Yasin - MDMahfouzNoch keine Bewertungen
- Handbook of Poultry DiseasesDokument22 SeitenHandbook of Poultry DiseasesSoufian CherkiNoch keine Bewertungen
- Nephrotic SyndromeDokument32 SeitenNephrotic SyndromeMelati Putri SitorusNoch keine Bewertungen
- Post-Traumatic Stress Disorder (PTSD) Guidelines Review: July 2013Dokument86 SeitenPost-Traumatic Stress Disorder (PTSD) Guidelines Review: July 2013liamel salyaNoch keine Bewertungen
- Key Components of Industrial HygieneDokument2 SeitenKey Components of Industrial HygieneCharlotte LibreroNoch keine Bewertungen