Beruflich Dokumente
Kultur Dokumente
Ecg
Hochgeladen von
সাব্বির সালেকCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Ecg
Hochgeladen von
সাব্বির সালেকCopyright:
Verfügbare Formate
Introduction
Electrocardiography (ECG or EKG from Greek: kardia, meaning heart) is a transthoracic (across
the thorax or chest) interpretation of the electrical activity of the heart over a period of time, as detected
by electrodes attached to the surface of the skin and recorded by a device external to the body. The
recording produced by thisnoninvasive procedure is termed an electrocardiogram (also ECG or EKG).
An ECG is used to measure the hearts electrical conduction system. It picks up electrical impulses
generated by the polarization and depolarization of cardiac tissue and translates into a waveform. The
waveform is then used to measure the rate and regularity of heartbeats, as well as the size and position
of the chambers, the presence of any damage to the heart, and the effects of drugs or devices used to
regulate the heart, such as apacemaker.
Most ECGs are performed for diagnostic or research purposes on human hearts, but may also be
performed on animals, usually for diagnosis of heart abnormalities or research.
Principles
The ECG device detects and amplifies the tiny electrical changes on the skin that are caused when
the heart muscle depolarizes during each heartbeat. At rest, each heart muscle cell has a negative
charge, called the membrane potential, across its cell membrane. Decreasing this negative charge toward
zero, via the influx of the positive cations, Na
+
and Ca
++
, is called depolarization, which activates the
mechanisms in the cell that cause it to contract. During each heartbeat, a healthy heart will have an
orderly progression of a wave of depolarisation that is triggered by the cells in the sinoatrial node,
spreads out through the atrium, passes through the atrioventricular node and then spreads all over
the ventricles. This is detected as tiny rises and falls in the voltage between two electrodes placed either
side of the heart, which is displayed as a wavy line either on a screen or on paper. This display indicates
the overall rhythm of the heart and weaknesses in different parts of the heart muscle.
Usually, more than two electrodes are used, and they can be combined into a number of pairs (For
example: left arm (LA), right arm (RA), and left leg (LL) electrodes form the three pairs LA+RA, LA+LL,
and RA+LL). The output from each pair is known as a lead. Each lead looks at the heart from a different
angle. Different types of ECGs can be referred to by the number of leads that are recorded, for example
3-lead, 5-lead, or 12-lead ECGs (sometimes simply "a 12-lead"). A 12-lead ECG is one in which 12
different electrical signals are recorded at approximately the same time and will often be used as a one-
off recording of an ECG, traditionally printed out as a paper copy. Three- and 5-lead ECGs tend to be
monitored continuously and viewed only on the screen of an appropriate monitoring device, for example
during an operation or whilst being transported in an ambulance. There may or may not be any
permanent record of a 3- or 5-lead ECG, depending on the equipment used.
Figure: ECG Machine
Function
An ECG produces a pattern reflecting the electrical activity of the heart and usually requires a trained
clinician to interpret it in the context of the signs and symptoms the patient presents with. It can give
information regarding the rhythm of the heart (whether or not the electrical impulse consistently arises
from the part of the heart where it should and at what rate), whether that impulse is conducted normally
throughout the heart, or whether any part of the heart is contributing more or less than expected to the
electrical activity of the heart. It can also give information regarding the balance of salts (electrolytes) in
the blood (e.g. hyperkalaemia) or even reveal problems with sodium channels within the heart muscle
cells (Brugada syndrome). Modern ECG machines often include analysis software that attempts to
interpret the pattern but the diagnoses this produces may not always be accurate.
It is one of the key tests performed when a heart attack (myocardial infarction or MI) is suspected; the
ECG can identify whether the heart muscle has been damaged in specific areas, though not all areas of
the heart are covered. The ECG cannot reliably measure the pumping ability of the heart, for which
ultrasound-based (echocardiography) or nuclear medicine tests are used. It is possible for a human or
other animal to be in cardiac arrest, but still have a normal ECG signal (a condition known as pulseless
electrical activity).
Figure: ECG Electrode Placing
Medical Uses
General symptoms indicating use of electrocardiography include:
Symptoms of myocardial infarction
Symptoms of pulmonary embolism
Cardiac murmurs
Syncope or collaps
Seizures
Perceived cardiac dysrhythmias
It is also used to assess patients with systemic disease, as well as monitoring during anesthesia and
critically ill patients.
Screening for coronary heart disease
The U.S. Preventative Services Task Force do not recommend either the ECG or any other cardiac
imaging procedure as a routine screening procedure in patients without symptoms and those at low risk
for coronary heart diseases. This is because overuse of the procedure is more likely to supply incorrect
supporting evidence for a nonexistent problem than to detect a true problem. Tests that falsely indicate
the existence of a problem are likely to lead to misdiagnosis, the recommendation of invasive procedures,
or overtreatment, and the risks associated with managing false information are usually more troublesome
than not using ECG results to make a health recommendation in low-risk individuals.
Persons employed in certain critical occupations, such as aircraft pilots, or in certain environments, such
as high altitudes, may be required to have an ECG as part of a regulatory regime.
Myocardial infarction
Characteristic changes seen on electrocardiography in myocardial infarction is included in the WHO
criteria as revised in 2000. According to these, a cardiac troponin rise accompanied by either typical
symptoms, pathological Q waves, ST elevation or depression or coronary intervention are diagnostic of
myocardial infarction.
Pulmonary embolism
In pulmonary embolism, an ECG may show signs of right heart strain or acute cor pulmonale in cases of
large PEsthe classic signs are a large S wave in lead I, a large Q wave in lead III and an inverted T
wave in lead III (S1Q3T3). This is occasionally (up to 20%) present, but may also occur in other acute
lung conditions and has, therefore, limited diagnostic value. This S1Q3T3 pattern from acute right heart
strain is termed the "McGinn-White sign" after the initial describers. The most commonly seen signs in the
ECG is sinus tachycardia, right axis deviation, and right bundle branch block. Sinus tachycardia was
however still only found in 869% of people with PE.
Design considerations
TI's new ADS1298 provides eight channels of PGA plus separate 24-bit delta-sigma ADCs, a Wilson
center terminal, the augmented Goldberger terminals and their amplifiers, provide for a full, standard 12-
lead ECG integrated analog front end. The ADS1298 reduces component count and power consumption
by up to 95 percent as compared to discrete implementations, with a power efficiency of 1 mW/channel,
while allowing customers to achieve the highest levels of diagnostic accuracy [view video]
ECG System Functionality and Evolution
Basic functions of an ECG machine include ECG waveform display, either through LCD screen or printed
paper media, and heart rhythm indication as well as simple user interface through buttons. More features,
such as patient record storage through convenient media, wireless/wired transfer and 2D/3D display on
large LCD screen with touch screen capabilities, are required in more and more ECG products. Multiple
levels of diagnostic capabilities are also assisting doctors and people without specific ECG trainings to
understand ECG patterns and their indication of a certain heart condition. After the ECG signal is
captured and digitized, it will be sent for display and analysis, which involves further signal processing.
Signal Acquisition challenges:
Measurement of the ECG signal gets challenging due to the presence of the large DC offset and various
interference signals. This potential can be up to 300mV for a typical electrode. The interference signals
include the 50-/60-Hz interference from the power supplies, motion artifacts due to patient movement,
radio frequency interference from electro-surgery equipments, defibrillation pulses, pace maker pulses,
other monitoring equipment, etc.
Depending on the end equipment, different accuracies will be needed in an ECG:
o Standard monitoring needs frequencies between 0.05-30 Hz
o Diagnostic monitoring needs frequencies from 0.05-1000 Hz
Some of the 50Hz/60Hz common mode interference can be cancelled with a high-input-impedance
instrumentation amplifier (INA), which removes the AC line noise common to both inputs. To further
reject line power noise, the signal is inverted and driven back into the patient through the right leg by an
amplifier. Only a few micro amps or less are required to achieve significant CMR improvement and stay
within the UL544 limit. In addition, 50/60Hz digital notch filters are used to reduce this interference
further.
Analog front end options:
Optimizing the power consumption and the PCB area of the analog front end is critical for portable
ECG's. Due to technological advancements, there are now several front end options:
o Using a low resolution ADC (needs all filters)
o Using a high resolution ADC (needs fewer filters)
o Using a sigma-delta ADC (needs no filters, no amplifier aside from INA, no DC offset)
o Using a sequential Vs simultaneous sampling approach.
When a low resolution (16 bit) ADC is used, the signal needs to be gained up significantly (typically 100x
- 200x) to achieve the necessary resolution. When a high resolution (24bit) sigma delta ADC is used, the
signal needs a modest gain of 4 - 5x. Hence the second gain stage and the circuitry needed to eliminate
the DC offset can be removed. This leads to an overall reduction in area and cost. Also the delta sigma
approach preserves the entire frequency content of the signal and gives abundant flexibility for digital
post processing.
With a sequential approach the individual channels creating the leads of an ECG are multiplexed to one
ADC. This way there is a definite skew between adjacent channels. With the simultaneous sampling
approach, a dedicated ADC is used for each channel and hence there is no skew introduced between
channels.
Summary
ECG is a transthoracic interpretation of the electrical activity of the heart over time captured and
externally recorded by skin electrodes.It is a noninvasive recording produced by an ECG device. In
English speaking countries, medical professionals often write EKG.
The ECG works mostly by detecting and amplifying the tiny electrical changes on the skin that are
caused when the heart muscle "depolarises" during each heart beat. At rest, each heart muscle cell
has a charge across its outer wall, or cell membrane. Reducing this charge towards zero is called
de-polarization, which activates the mechanisms in the cell that cause it to contract. During each
heartbeat a healthy heart will have an orderly progression of a wave of depolarisation that is
triggered by the cells in the sinoatrial node, spreads out through the atrium, passes through
"intrinsic conduction pathways" and then spreads all over the ventricles. This is detected as tiny
rises and falls in the voltage between two electrodes placed either side of the heart which is
displayed as a wavy line either on a screen or on paper. This display indicates the overall rhythm of
the heart and weaknesses in different parts of the heart muscle.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Toxic Epidermal NecrolysisDokument13 SeitenToxic Epidermal NecrolysisHend AbdallaNoch keine Bewertungen
- CKD Pocket GuideDokument2 SeitenCKD Pocket GuideLutfi MalefoNoch keine Bewertungen
- Case Presentation On Wilms TumorDokument25 SeitenCase Presentation On Wilms TumorDeepika100% (1)
- Esthetic Posterior Inlays OnlaysDokument5 SeitenEsthetic Posterior Inlays OnlaysDentalBoardNoch keine Bewertungen
- LeptospirosisDokument35 SeitenLeptospirosisJep ValentinNoch keine Bewertungen
- Dialog Percakapan Bidan Tugas Bahs Inggris DedeDokument5 SeitenDialog Percakapan Bidan Tugas Bahs Inggris DedeSardianto TurnipNoch keine Bewertungen
- Casilan, Ynalie Drug Study (Morphine)Dokument5 SeitenCasilan, Ynalie Drug Study (Morphine)Ynalie CasilanNoch keine Bewertungen
- Routine 4-2Dokument1 SeiteRoutine 4-2সাব্বির সালেকNoch keine Bewertungen
- Final DraftDokument2 SeitenFinal Draftসাব্বির সালেকNoch keine Bewertungen
- Final DraftDokument2 SeitenFinal Draftসাব্বির সালেকNoch keine Bewertungen
- MT 1Dokument34 SeitenMT 1Vishal VnNoch keine Bewertungen
- And, As His Strength Failed Him at Length, He Met A Pilasasgrim Shadow-"Shadowsasas," Said He, "Whersasae Can It Be - This Land of Eldorado?" "Over The MountainsDokument1 SeiteAnd, As His Strength Failed Him at Length, He Met A Pilasasgrim Shadow-"Shadowsasas," Said He, "Whersasae Can It Be - This Land of Eldorado?" "Over The Mountainsসাব্বির সালেকNoch keine Bewertungen
- Final Project ReportDokument43 SeitenFinal Project Reportসাব্বির সালেকNoch keine Bewertungen
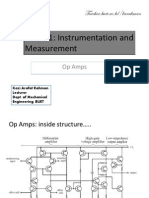
- ME 361: Instrumentation and Measurement: Teacher - Buet.ac - Bd/karahmanDokument11 SeitenME 361: Instrumentation and Measurement: Teacher - Buet.ac - Bd/karahmanসাব্বির সালেকNoch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care Plananon_984362Noch keine Bewertungen
- CRRT Cu CitratDokument35 SeitenCRRT Cu CitratAndreea MitranNoch keine Bewertungen
- The Clinical Significance of The Retromolar Canal and Foramen in DentistryDokument24 SeitenThe Clinical Significance of The Retromolar Canal and Foramen in Dentistryمحمد عبدالرحمنNoch keine Bewertungen
- Arero Primary Hospital Pain MGT ProtocolDokument9 SeitenArero Primary Hospital Pain MGT Protocolsami ketemaNoch keine Bewertungen
- Fluid Balance Case StudyDokument9 SeitenFluid Balance Case StudyAna BienneNoch keine Bewertungen
- Prumychild EngDokument12 SeitenPrumychild EngAmirol Ariff NazarudinNoch keine Bewertungen
- Tipos de SuturasDokument5 SeitenTipos de SuturasLeandro PeraltaNoch keine Bewertungen
- The Bidirectional Relationship Between Obstructive Sleep Apnea and Metabolic DiseaseDokument14 SeitenThe Bidirectional Relationship Between Obstructive Sleep Apnea and Metabolic DiseaseVenny SarumpaetNoch keine Bewertungen
- Epworth Sleepiness ScaleDokument1 SeiteEpworth Sleepiness ScaleSridhar ReddyNoch keine Bewertungen
- PrimaryCare JAWDA - Update 2022Dokument40 SeitenPrimaryCare JAWDA - Update 2022SECRIVINoch keine Bewertungen
- The Management of Patients With Acute Myocardial Infarction: Pocket GuidelinesDokument22 SeitenThe Management of Patients With Acute Myocardial Infarction: Pocket GuidelinesAhmad Yuliandri MustopaNoch keine Bewertungen
- Cytochemistry PrimerDokument2 SeitenCytochemistry PrimerMunish Dogra100% (1)
- Experiment #15: Screening Test For Low Titer Group "O" BloodDokument5 SeitenExperiment #15: Screening Test For Low Titer Group "O" BloodKriziaNoch keine Bewertungen
- Quisted en P Menopausicas Guias GTG - 34 PDFDokument32 SeitenQuisted en P Menopausicas Guias GTG - 34 PDFAdela Marìa P LNoch keine Bewertungen
- Diarrhea: On This PageDokument6 SeitenDiarrhea: On This PageKristine AlejandroNoch keine Bewertungen
- Mikrobiologi DiagramDokument2 SeitenMikrobiologi Diagrampuguh89Noch keine Bewertungen
- Diabetes Leader 2019 PDFDokument12 SeitenDiabetes Leader 2019 PDFArjun Kumar AdhikariNoch keine Bewertungen
- Knee Assessement FormDokument2 SeitenKnee Assessement FormLee Woo GuanNoch keine Bewertungen
- Diagnosis of Typhoid FeverDokument5 SeitenDiagnosis of Typhoid FeverpeterjongNoch keine Bewertungen
- Ambulance App - Book An Ambulance in A ClickDokument4 SeitenAmbulance App - Book An Ambulance in A ClickbloodforsureNoch keine Bewertungen
- Script Roleplay KonselingDokument4 SeitenScript Roleplay KonselingVella MerytaNoch keine Bewertungen
- Self Care Management and Puberty Health IssuesDokument10 SeitenSelf Care Management and Puberty Health IssuesIan Atienza0% (1)
- Fracture of The Upper HumerusDokument22 SeitenFracture of The Upper HumerusOlasinde AnthonyNoch keine Bewertungen