Beruflich Dokumente
Kultur Dokumente
Responsive Documents - CREW: FTC: Regarding Indoor Tanning Association: 5/15/14 - Batch Two, Part One
Hochgeladen von
CREWOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Responsive Documents - CREW: FTC: Regarding Indoor Tanning Association: 5/15/14 - Batch Two, Part One
Hochgeladen von
CREWCopyright:
Verfügbare Formate
Kelly, Andrea
From:
Sent:
To:
Cc:
Subject:
Attachments:
Clark, Donald S.
Wednesday, March 20, 2013 1:38 PM
DeMartino, Laura; Engle, Mary Koelbel; Evans, Janet M.; Kohm, James A.
Bak, Patricia
Draft Response To California State Senator Ted LieuRe the American Suntanning
Association (A Possible Successor in Interest to the Indoor Tanning Association)
Bak.PDF; Letter To State Senator Ted LieuRe the American Suntanning Association.wpd
Everyone, I've drafted the attached response to the attached incoming letter from California State Senator Ted Lieu, in
which he argues that the American Suntanning Association is a successor to the ITA, and is therefore required to comply
with (but is failing to comply with) the Decision and Order against the ITA. I'd be happy to make any changes you'd like;
please let me know. Thanks!
Don
STAT E CAPITOL. ROOM 4090
SACRAMENTO,CA 95814
TEL (916) 6514028
FAX (916) 3236056
CHAI R
LABOR AND INDUSTRIAL
RELATIONS
DISTRICT OFFICE
2512 ARTESIA BLVD .. SUITE 320
REDONDO BEACH. CA 90278
TEL (3 1 0) 3186994
Qlalifnrnia t a t e ~ e n a t e
SENATOR
TED W. LI EU
TWENTY-EIGHTH SENATE DISTRICT
MEMBER
APPROPRIATIONS
EL ECTIONS AND
CONSTITUTIONAL AMENDMENTS
FAX (3 1 0) 3 186733
WWW.SEN .CA.GOV/LIEU
SENATOR.UEU@SENATE.CA.GOV
February 20, 2013
Patricia Bak, Executive Director
Federal Trade Commission
600 Pennsylvania A venue, NW
Washington, DC 20580
Via Fax and Mail
Dear Executive Director Bak:
INSURANCE
VETERANS AFFAIRS
I am writing to follow up on my letter sent to you on February 5, 2013 regarding the newly
formed American Suntanning Association (ASA). My letter documented several instances of the
ASA making statements that the Federal Trade Commission (FTC) had already ruled were false
.and misleading when the same statements were made by the Indoor Tanning Association (ITA).
The ASA is composed of many of the exact same members as the IT A and is essentially the
same organization, just with a different "name."
I now have concrete evidence the ASA is a direct successor organization of the IT A, which
means the prior FTC Order barring false statements about indoor UV tanning should also apply
to the ASA. In a recent Sun Tan Magazine article (Attachment 1) highlighting the ASA, the
organization's Legal Science/Research Board Member stated: "we especially want to thank John
Overstreet and the IT A for making such a smooth transition by getting us all of the state
lobbying history and contact information for the state lobbying battles."
By openly admitting to a "smooth transition," the ASA is showing itself to be nothing more than
a successor to the ITA and, therefore, in direct violation of the FTC's Order. The Order
(Attachment 2) specifically stated that any "respondent" be prohibited from making any false or
misleading statements regarding indoor tanning. The Order then goes on to define "respondent"
as the "Indoor Tanning Association, its successors and assigns" (emphasis added).
--.
It is unacceptable for the IT AI ASA to give false and misleading statements about the dangers of
indoor tanning and act as if the prior FTC Order did not exist. I urge the FTC to apply its prior.
Order, which protected consumers in the indoor tanning industry, to both the ITA and the ASA,
because they are essentially.the same entity. Thank you for reviewing this case and I look
forward to your response.
TEDW.LIEU
State Senator, District 28
Attaclunents:
I. Sun Tan Magazine article
2. FTC Decision and Order, Docket No. C-4290, "In the Matter of Indoor Tanning Association,"
dated May 13,2010
cc:
American Suntanning Association
..s :;':. . ; Salon .. Leaders Ann-o
, , Formation Of
:;A.merican Suntanning Ass.oc,.,.. . -.. ... ,
Promoting moderate uv exposure, combating
Professional sunbed solons in the United States finally hove a
national solon-lead association.
The United States' largest professional sunbed centers have formed
the American Suntanning Association, a values-based organization
dedicated to increasing public awareness about the facts associ-
ated with moderate ultraviolet exposure and spray"n tanning,
correcting misinformation about sunlight and sunbeds while raising
the professional standards in American suntanning centers.
The ASA launched in mid-December after its founders committed
seed money and began recrui ting charter members in October.
The association hit the ground running with o professional staff,
Washington, D.C., counsel, New York City publ ic relations firm
Global Strategy Group (www.globolstrotegygroup.com), and
is working with solons nationwide to retain state-level lobbying
counsel.
"It is time to hove a discussion about UV light from the
sun and from sunbeds," says Bart Bonn, ASA board president
and owner of Ashley Lynn's Tanning based in Omaha. "The ASA
is going to be a constructive party in that discussion, demanding
a consumer-first conversation differentiating. proper sun care from
blatant overstatements about the risks of UV exposure."
The ASA' s entire effort will be built on a solid foundation of cred-
ible scientific Funding research to counter the poorly
conceived International Association for Research on Cancer study
and all other studies that target our industry for unfair taxes and
regulations will be the most important priority for the.ASA. "For
the i ndustry to move forward, it i s critical that we hove solid sci;
ence created by highly credentialed researchers," says Allen
Miller, ASA' s research director.
The ASA took aim at the biggest core issue immediately; targeting
one specific significant concern in its first press statement: Many
ies about sunbed usage don' t actually study professional sunbed
solons, but rather include sunbeds used to treat cosmetic conditions
in doctors' offices and unmonitored home-based tanning units. When
home and medical sunbeds ore removed from these studies, the risk
connected to professional solons virtually disappears.
The ASA pointed out that organizations promoting these studies
haven't disclosed this critical distinction and hove ignored many
other confounding factors. The ASA will issue research and reports
to support an open and honest dialogue with the public, media, the
health core community and elected officials about the truth behind
responsible tanning.
63 SMART TAN MAGAZINE I ,,.,,.,
"Over the course of many years, our industry has been the forget
of misinterpretations and unfair attacks. What happens when these
statements ore not answered or refuted is they begin to be token
as fact or truths," says ASA Board Member James Oliver, CEO
of Beach Bum, based in New York. "With the correct information
and the guidance on the timing and content of our responses, we
con better protect the industry and our livelihood." why the
ASA has creoted on Immediate Response Team to respond to these
untrue statements in a very timely manner.
Another lop priority is to fund a notional public relations campaign
with a notional firm to spread the scientifically supported message.
For nearly a decode, the industry has been focused on crisis com-
munications and defensive the new long-term
effort will handle those concerns, but will also focus on building
relationships with reporters to creole positive press and expose the
anli-tonni.ng groups' mis-statements and financial agendas. " For so
many years, our industry has been forced to expend the majority
of its resources on legislative battles, and thus locked a more pro-
active voice/ says ASA Boord Member Doug McNabb, owner
of Calgary-based Fabuton Suntan Studios. "With the proper sci-
ence in handand the help of Global Strategy Group, the ASA has
already received a significant number of proactive inquiries in only
our first month of operation. We anticipate this only the beginning
of a significant shift in the UV light conversation."
POSITIVE PRESS
Star Player's Doctor Prescri bes Sun bed:
http:/ /www.foxnews.com/health/2013/0l /09/
new-jersey-teen-treats-skin-disorder-by-tanning-every-day/
Teens and tanning debate continues:
http://www.wtnh.com/dpp/news/new_london_cty/
teens-ond-tanning-debate-continues#.UOx3.TYnjmkl
Tanning Industry Tokes Measures To Police Itself:
http:/ /www.ctnewsjunkie:com/ ctnj.php/ archives/ entry/
lanning_industry_tokes_measures_to_police_ifself
Ferguson installed tanning booths so United players could
lop up their Vitamin D levels:
http:/ /www.dailymail.co.uk/ sport/football/
orticle-2250414/Sir-Aiex-Ferguson-instolled-tonning-
booths-Manchester-United.html#comments
ASA is already appealing to consumers and media through
its site - www.AmericanSuntanning.org - to balance the
message, and will work with state and federal regulators for con-
structive regulations that underscore operational protocol already
embraced by professional sun bed centers.
"Consumers who choose to ton - and it should be their choice -
need to be able to do so based on correct information about the
potential benefits and risks of UV exposure," says ASA member
Jon Meshon, owner of City Sun Tanning in New York City. "When
organizations who benefit by improperly vilifying all UV expo-
sure compare the manageable risks of sunlight to arsenic and
plutonium in public statements, something's seriously wrong. We
Med to correct that, and ASA is already working constructively
to do so."
The ASA has also engaged mCopitol, o Washington, D.C., lob-
bying group, to help us get the right message to our local, stole
and federal politicians. Promoting industry-supportive research
and statistics correctly to tell our industry's winning story can't be
accomplished effectively without the relationships and guidance
that mCapitol brings to our industry.
"We now hove a solid group of scientists working in harmony with
a notional PR firm and a Washington, D.C., lobbying. group," said
ASA Boord Member Diane Lucas, president of Dallas-based Palm
Beach Ton: "Our industry has used professional groups sporadi-
cally in the post, but this is the first time that these professionals ore
working together on a weekly and sometimes doily basis to put
together an extensive ond cohesive market growth plan."
"We especially want to thank John Overstreet and the ITA for mak-
ing such a smooth transition by getting us all of the state lobbying
history and contact information for the slate lobbying bottles,"
continues lucas. "The ASA is already working with many stole
lobbyists and solon advocates for what appears to be o pretty
big fight this year."
In 2013, on estimated 30 million Americans will visit a profes-
sional sun bed center- the vast majority of which ore family-owned.
Two-thirds of the 14,000 U.S. sun bed solons ore female-<iwned
businesses, employing about 150,000 people.
"The professional sunbed solon community is present in every
American community and has become on important port of
local small business economies as good employers," says ASA
Boord Member Rick Kueber, CEO of Sun Ton City, based in
Elizabethtown, Ky. " That's why it's important that the sunbed
salon market elevates the balanced conversation about UV expo-
sure and steps up to provide accurate education and information
about responsible indoor tanning to our clients."
As we've learned in the post, organizing and driving this major
effort can't be accomplished with volunteer labor. That's why
ASA has hired Nonprofit Management Services, o new organi-
zation mode up of Smart Ton staff created specifically for taking
on this task. "We knew that we needed on organization with an
experienced and extensive staff to coordinate and drive the ASA
plan," says ASA Boord Member Roger Holmes, owner of Celsius
Tannery, based in Kansas City. "Getting the years of experience
that Molt Russell, Joe levy and their staff bring to the table will be
on essential port of getting this done."
A volunteer-driven organization, ASA includes members from all
50 stoles. ASA members will be trained and supported so they
may work with legislators and health care officials at the local,
state and federal l evel to support constructive regulation that
underscores operational protocol already embraced by profes
sionol sun bed centers. "If you're in the indoor. tanning industry
for the long haul, you can't ignore what's happening around you.
You need to gel involved," says Oliver. "The ASA has a solid plan
of oclion and a team of professionals to put the plan .in effect. The
only thing missing .ore more salons that are willing to participate."
For more information about ASA visit www.omericonsuntanning.org
,;,-:: , ... : <\ .
. -:
.
.
.
Amor:can Sunl anninq Ass0cial.i on
FOUNDING BOARD
MEMBERS
President
Government Relations
Bart Bonn
Ashley Lynns Tanning
. .
Legal
Science/Research
Diane Lucas
Palm Beach Tan
Communications
James Oliver
Beach Bum Tanning
Public Relations
Doug McNabb
Fabutan
Treasurer
Rick Kueber
Sun Tan City
Membership
Roger Holmes
Celsius Tannery
I SMART TAN MAGAZINE 64
ASA MEMBERSHIP BENEFITS
-------------- ------------------------
The American Suntanning Association is focused on short and long-term efforts to secure the future of profes-
sional sun bed facilities based on redefining the standards of professionalism in the market and promoting a
balanced, scientifically supported message about UV exposure. The ASA' s plan includes:
MARKET GROWTH: F!Jndin'g a scientifically i_nitiatjve
. .. ; .. , _, , . : .. -.. -.
::- ' . . . . . ,: r: , : : .. '': . .- /. ' .
CREDIBLE RESEARCH: Funding research countering the poorly conceived IARC study on indoor tanning
and all other studies that target our industry for unfair taxes and regulations.
.. .:: ' I': "', ', ;: ,-,: ::,.:;=' .):.,> .. : ',, 'I ' ',> ' ... .':/.', ; '': ' ... ' :.:
. -i.EGALACTipN:raking legal steps to .. h919. antiUVspec.icil grgups fot
atfacks against the indoor tanning industry. ...
. . . :
HEALTH BENEFITS: Working with the federal government to properly address ways to substantiate and
claims regarding UV-induced vitamin D from indoor tanning equipment.
MEDIA AND PUBLIC RELATIONS: Funding a national PR campaign with a national firm to support the
scientifically supported message. This long-term effort will focus on building relationships with reporters to
create positive press and expose the anti-tanning groups' mis-statements and financi al agendas.
. ' . '
IMME.DIATE reac.tive qnline to :
... : ,- '.._::- .. - .._' ,_,. :. -::,. .. ...... , :-':' :._.,
.. _ : -'_:':. '.;: .::i .. .. ,:: . . ;. .. r # .:.'\ ' , : - ...... .
GRASSROOTS MOVEMENT: Building a grassroots salon initiative to educate and promote the benefits of
indoor tanning through the local media and local politicians. Developing regional salon advocates to carry
out a coordinated effort.
'
. :.
- SALOi'i .rRAINING to teach' regio.nal s_dlonadvocates h-ow.
toprbmote sunqed centers.witn local media support documents and handouts_-
PHONE AND ONLINE SUPPORT: Available any time for salon advocates.
- JOIN THE ASA TODAY
Visit www.AmericanSuntanning.org or
call 855-879-7678
65 SMART TAN MAGAZINE I .)-.,rl<:n,:.,n
UNITED STATES OF AMERICA
FEDERAL TRADE COMMISSION
In the Matter of )
)
INDOOR TANNING )
a corporation. )
File No. 082-3159
AGREEMENT CONTAINING
CONSENT ORDER
The Federal Trade Commission has conducted an investigation of certain acts and
practices of Indoor Tanning Association ("proposed respondent"). ProposedTespondent, having
been represented by counsel, is willing to enter into an agreement containing a consent order
resolving the allegations contained in the attached draft complaint. Therefore,
IT IS HEREBY AGREED by. and between Indoor Tanning Association and counsel for
the Federal Trade Commission that:
1. Proposed respondent Indoor Tanning Association is a Massachusetts corporation with its
principal office or place of business at 2025 M Street, N.W., Washington, D.C. 20036.
2. Proposed respondent admits all the jurisdictional facts set forth in the-draft complaint.
3. Proposed respondent waives:
A. Any further proce4ural steps;
B. The requirement that the Commission's decision contain a statement of findings
of fact and conclusions of law; and
C. All rights to seek judicial review or otherwise to challenge or contest the validity
of the order entered pursuant to this agreement.
4. This agreement shall not become part of the public record of the unless and
until it is accepted by the Commission. If this agreement is accepted by the Commission, it,
together with the draft complaint, will be placed on the public record for a period of thirty (30)
days and information about it publicly released. The Commission thereafter may either
withdraw its acceptance of this agreement and so notify proposed respondent, in which event it
will take such action as it may consider appropriate, or issue and serve its complaint (in such
form as the circumstances require) and decision in disposition of the proceeding.
5. This agreement is for settlement purposes only and does not constitute an admission by
proposed respondent that the law has been violated as in the draft complaint, or that the
Page 1 of 9
facts as alleged in the draft complaint, other than the jurisdictional facts, are true.
6. This agreement contemplates that, if it is.accepted by the Commission, an4 if such
acceptance is not subsequently withdrawn by the Commission pursuant to the provisions of
Section 2.34 of the Commission's Rules, the Commission may, without further notice to
proposed respondent, ( 1) issue its complaint corresponding in form and substance with the
attached draft complaint and its decision containing the following order in disposition of the
proceeding, and (2) make information about it public. When so entered, the order shall have the
same force and effect and may be altered, modified, or set aside in the same manner and within
the same time provided by statute for other orders. The order shall become final upon service.
Delivery of the complaint and the decision and order to proposed respondent' s address as stated
in this agreement by any means specified in Section 4.4(a) of the Commission's Rules shall
constitute service. Proposed respondent waives any right it may.have to any other manner of
service. The complaint may be used in construing the terms of the order, and no agreement,
understanding, representation, or interpretation not contained in the qrder or the agreement may
be used to vary or contradict the terms of the order.
7. Proposed respondent has read the draft complaint and consent order. It understands that
it may be liable for civil penalties in the amount provided by law and other appropriate relief for
each violation of the order after it becomes final.
ORDER
DEFINITIONS
For the purposes of this order, the following definitions shall apply:
1. Unless otherwise specified, "respondent" shall mean Indoor Tanning Association,
its successors and assigns, its officers when acting in active concert or
participation with Indoor Tanning A_ssociation, and its executive director.
2. "Covered product or service" shall mean any ultraviolet lamp or sunlamp. product, .
as defined in 21 C.F .R. 1 040 .20; and any commercial facility where consumers
may use ultraviolet lamps or sunlamp products.
3. "Clearly and conspicuously" means:
a. In pJ:int communications, the disclosure shall be presented in a manner
that stands out from the accompanying text, so that it is sufficiently prominent,
because of its type size, contrast, location, or other characteristics, for an ordinary
consumer to notice, read and comprehend it;
b. In communications made through an electronic medium (such as
television, video, radio, and interactive e i ~ such as the Internet, online
services, and software), the disclosure shall be presented simultaneously in both
Page 2 of 9
the audio and visual portions of the communication. In any communication
presented solely through visual or audio means, the disclosure shall be made
through the same means through which the communication is presented. In any
communication disseminated by means of an interactive electronic mediu,m such
as software, the Internet, or online services, the disclosure must be unavoidable.
Any audio disclosure shall be delivered in a volume and cadence sufficient for an
ordinary consumer to hear and comprehend it. Any visual disclosure shall be
presented in a manner that stands out in the context in which it is presented, so
that it is sufficiently prominent, due to its size and shade, contrast to the
background against which it appears, the length of time it appears on the screen,
and its location, for an ordinary consumer to notice, read and comprehend it; and
c. Regardless of the medium used to disseminate it, the disclosure shall be in
understandable language and syntax. Nothing contrary to, inconsistent with, or in
mitigation of the disclosure shall be used in any communication.
4. "Close proximity" means on the same print page, web page, online service page,
or other electronic page, and proximate to the triggering representation, and not
accessed or displayed through hyperlinks, pop-ups, interstitials, or other means.
5. "Commerce" shall mean as defined in Section 4 of the Federal Trade Commission
Act, 15 U.S.C. 44.
I.
IT IS HEREBY ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not represent, in any manner,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, that:
A. Tanning, including indoor does not increase the risk of skin cancer;
B. Tanning, including indoor tanning, is safe or poses no danger;
C. Indoor tanning is approved by the and
D. Indoor tanning is safer than tanning outdoorsbecause in indoor tanning facilities,
the amount of ultraviolet light is monitored and controlled.
II.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, trade name, or other device, in connection with the
Page 3 of 9
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce; shall not misrepresent, in any manner,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, that:
A: Research shows that vitamin D supplements may harm the body's ability to fight
disease; and
B. A study in the Proceedings ofthe National Academy of Sciences determined: (a)
that sun exposure does not cause skin cancer or melanoma, or that the risk of such
cancer is only hypothetical; (b) that getting a tan is healthy; (c) that the risks of
not getting enough ultraviolet light far outweigh the fisk of skin cancer; or (d) that
vitamin D has been linked to significantly decreasing the risk of contracting lung,
kidney, or liver cancer.
III.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not make any representation,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, about the safety, health-related efficacy or performance, or health-
related risks or benefits, of any covered product or or about the sources, performance,
efficacy, or health-related risks or benefits of vitamin D; unless the representation is non-
misleading, and, at the time it is made, respondent possesses and relies upon competent and
reliable scientific evidence that is sufficient in quality and quantity based on standards generally
accepted in the relevant scientific fields to substantiate that the representation is true. For the
purposes of this order, competent and reliable scientific evidence shall consist of tests; analyses,
research, studies, or other evidence that have been conducted and evaluated in an objective
manner by qualified persons, that are generally accepted in the profession to yield accurate and
reliable results, and whose results are consistent with the body of reliable scientific evidence
relevant to the representation.
IV.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not misrepresent, in any manner,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, the existence, contents, validity, results, conclusions, or interpretations
of any test, study, survey, or
Page 4 of 9
v.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not make any representation, in any
manner, expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, about the safety or health benefits of any covered product or service
unless it discloses, clearly and conspicuously, and within close proximity to that representation:
NOTICE: Exposure to ultraviolet radiation may increase the likelihood of developing
skin cancer and can cause serious eye injury.
Provided that, in lieu of the above, in the event that advertising for any covered product or
service makes any representation, expressly or by implication, including through the use of a
product name, endorsement, depiction, or illustration, that exposure to ultraviolet radiation
produces vitamin D _in the body, or otherwise about the effectiveness or usefulness of such
product for generation of vitamin D, the required disclosure shall be as follows:
NOTICE: You do not need to become tan for your skin to make vitamin D. Exposure
to ultraviolet radiation may increase the likelihood of developing_skin cancer and can
cause serious eye injury.
VI.
IT IS FURTHER ORDERED that respondent, directly or through any corp<:>ration,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not provide to any other person or
entity any means or instrumentalities that contain any representation or omission prohibited by
this order. For the purposes of this Part, "means or instrumentalities" shall mean any
information, including but not necessarily limited to any advertising, labeling, communications
guides, or t ~ r promotional material.
VII.
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall send as soon as practicable, but in no event later than thirty (30)
days after entry of this order, by first-class mail, postage prepaid and return receipt requested, an
exact copy of the notice attached hereto as Attachment A, showing the date of mailing, to all
Indoor Tanning Association members and all other entities to which Indoor Tanning Association
provided point-of-sale advertising on or after January 1, 2008. The notice required by this
paragraph shall not include any other document or enclosures and may be sent to the principal
place of business of each entity.
Page 5 of 9
VITI.
IT IS FURTHER ORDERED that, for a period of five (5) years after the last date of
dissemination of any representation covered by this order, respondent Indoor Tanning
Association and its successors and assigns shall maintain and upon make available to the
Federal Trade Commission for inspection and copying:
A. All advertisements and promotional materials containing the representation;
B. All materials were relied upon in disseminating the representation; and
C. All tests, reports, studies, demonstrations, or other evidence in its possession or
control that contradict, qualify, or call into question such representation,_ or the
basis relied upon for the representation, including complaints and other
communications with consumers or with. governmental or consumer protection
organizations.
IX.
'IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall deliver a copy of this order to all current and future principals,
officers, directors, and other employees with managerial authority having responsibilities with
respect to the subject matter of this order, and shall secure from each such person a signed and
dated statement acknowledging receipt of the order. Respondent shall deliver this order to
current personnel within thirty (30) days after the date of service of this order, and to future
personnel within thirty (30) days after the person assumes such position or responsibilities.
X.
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall notify the Commission at least thirty (30) days prior to any change
in the corporation that may affect compliance obligations arising under this order, including but
not limited to a dissolution, assignment, sale, merger, or other action that would result in the
emergence of a successor corporation; the creation or dissolution of a subsidiary, parent, or
affiliate that engages in any acts or practices subject to 'this order; the proposed filing of a
bankruptcy petition; or a change in the corporate name or address. Provided, however, that, with
respect to any proposed change in the corporation about which respondent learns less than thirty
(30) days prior to the date such action is to take place, respondent shall notify the Commission as
soon as is practicable after obtaining such knowledge.' All notices required by this Part shall be
sent by certified mail to the Associate Director, Division of Enforcement, Bureau of Consumer
Protection, Federal Trade Commission, Washington, D.C. 20580.
Page 6 of 9
XI.
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall, within sixty ( 60) days after the date of service of this order file with
the Commission a true and accurate report, in writing, setting forth in detail the manner and form
in which respondent has complied with this order. Within ten ( 1 0) days of receipt of written
notice from a representative of the Commission, respondent shall submit additional true and
accurate written reports.
XII.
This order will terminate twenty (20) years from the date of its issuance, or twenty (20)
years from the most recent date that the United States or the Federal Trade Commission files a
complaint (with or without an accompanying yonsent decree) in federal court alleging any
violation of. the order, whichever comes later; provided, however, that the filing of such a
complaint will not affect the duration of:
. .
A. Any Paragraph in this order that terminates in less than twenty (20) years; and
B. This order's application to any respondent that is not named as a defendant in
such complaint; and
C. This order if such complaint is filed after the order has pursuant to this
Paragraph.
Page 7 of 9
Provided, further, that if such complaint is dismissed or a federal court rules that the
respondent did not violate any provision of the order; and the dismissal or ruling is either not
appealed or upheld on appeal, then the order will terminate according to this Part as though the
complaint had never been filed, except that the order will not terminate between the date such
.complaint is filed and the later of the deadline for appealing such dismissal or ruling and the date
such dismissal or ruling is upheld on appeal.
Signed this _ day of _____ , 2009.
APPROVED:
MARY K. ENGLE
Associate Director
INDOOR TANNING ASSOCIATION
By: ________ _ _____ __ _
DAN HUMISTON
PRESIDENT
By: _______________ _
BRIDGET CALHOUN
CROWELL & MORlNG
Counsel for Respondent Indoor Tanning Association
FEDERAL TRADE COMMISSION
By: _________ _
JANET M. EVANS
Division of Advertising Practices
Division of Advertising Practices
DAVID VLADECK
Director
Bureau of Consumer Protection
Page 8 of 9
ATTACHMENT A
[ON INDOOR TANNING ASSOCIATION LETTERHEAp]
JMPORTANT NOTICE ABOUT GOVERNMENT ACTION
[insert addressee name]
[insert addressee address]
Dear ITA Member or Affiliate:
In a recent lawsuit, the Federal Trade Commission (FTC) charged the Indoor Tanning
Association (IT A) with making misleading representations in its advertising and marketing for
indoor tanning. Among_ other things, the FTC alleged that IT A falsely claimed that indoor
tanning poses no risk to health, including no risk of skin cancer. In addition, the FTC alleged
that when ITA represented that indoor tanning caused the skin to generate vitamin D, IT A failed
to disclose material facts about the risks of indoor tanning. IT A has agreed to send this
notification to you as part of its settlement with the FTC.
. .
IT A hereby requests that you immediately stop using all advertising and marketing
materials provided by to you by IT A. Among the materials you should no longer use
are all of the materials contained on the CD-ROM issued in 2008, including the following:
A. The "Melanoma Hype" print ad
B. .The "Overdose of Hysteria" video
C. . The "Communications: The Basics" guide and
D: The print ad with the tag line, "Time to rethink sun tanning?"
The FTC complaint alleges that these ads contain representations that are false and/or
misleading.
For further information about the FTC's complaint and order, go to www.ftc.gov and
search "Indoor Tanning
Very truly yours,
John Overstreet
Executive Director
Page 9 of 9
FEB- 05-2013 12 :13 From:SENATOR LIEU
9163275989
To : 2023262873
STATE CAPITOL.. ROOM 4090
SACRAMENTO CA
TC1.
.... 3236056 Qlalifornia:
C>ISTniCT
SENATOR
ZS\3 ARTESIA BLVO . SUITt!: 320
RF.OQNOO BEACH. C A 90278
TEL<310J 318-6994
"'"" <31013186?33
TE:O W. LI EU
TWENTY-EIGHTH SENATE DISTRICT"
WWW SEN CA C:OII
1
11Plr
CA GOV
February 5, 2013
Jon Leibowitz
Chairman, Federal Trade Commission
600 Pennsylvania Avenue, NW
Washington, DC 20580
Via Fax and Mail
Dear Chairman Leibowitz:
P.1"'13
CHAIR
L.ABOR ANO
REL.ATIONS
APPROPRIATIONS
t::I..ECTIONS ANO
CONSTITUTIONAL AMENOM!;NTS
INSURANCE
VETERANS At:"l'"AIRS
I commend the Federal Trade Commission (FTC) for itS May 2010 Order prohibiting the Indoor
Tanning Association (ITA) from making false statements regarding the purported safety and
health benefits of indoor UV tiUUling. Unfortunately, some members ofthis trade group have
now formed the American SWltanning Association (ASA) to mislead the public about the health
effects of dangerous indoor tanning. An organh:ation should not be able to escape an order of
the FTC by sjmply changing its name and some of its members. I respectfully request the
Federal Trade Commission apply its 2010 Order to the ASA.
Similar to the IT A. the newly formed ASA has aligned itself with j unk science that promotes the
aJleged safety and benefits of indoor tannjng. ln their efforts to deceive consumers into believing
indoor tanning is not only safe, but beneficial, the ASA cites studies that are not peer reviewed
and rely on cherry-picked data, have methodological flaws, or have been funded by the industry.
Rather than accepting the overwhelming medical evidence that indoor tanning is a cause of skin
cancer, the ASA fabricates its own false "science" in a blatant attempt to mislead consumers.
In the FTC' s previous order, the ITA was explicitly prohjbited from making any representation
that "Tanning, including indoor tanning, is safe Ol' poses no danger" or that "getting a tan is
(Attachment 1, Decision and Order of FTC In the Matter of IT A). The FTC Order
also prohibited the IT A, expressly or by implication, from making statements that "vitamin D has
been linked to significantly decreasing the risk of contracting lung, kidney, or liver cancer" or
that "vitamin D supplements may harm the body's ability to fight disease." (Attachment 1).
Unfortunately, the ASA has continued using the same statements that have already been
determined as being false and misleading by the FTC. For example, the ASA claims indoor
tanning provides "one ofthe safest ways for citizens to obtain adequate vitamin D." (Attachment
2, ASA statement). The ASA also states there are "health benefits to indoor tanning."
(Attachment 2). Both ofthese statements are false and would violate the FTC order if the ITA
FEB-05-2013 12:13 From: SENATOR LIEU 9163275989
To:2023262873
had made those statements. The ASA, comprised ofmany of the same members as the ITA,
should not be able to make these false statements.
The ASA refers to the overwbehning medical evidence that indoor UV tanning causes skin
cancer as "quasi-scientific reports." (Attachment 2). The entire thrust of the ASA mission is to,
in their words, "debunk the scientific reports being used against us." Both directly and by
implication, the ASA is making statements promoting the purported safety of indoor tanning and
the purported health_ benefits of indoor tarming, both of which the FTC fo\md f-alse in its order to
the ITC.
As the author of the first law in the nation to ban indoor UV tanning for all minors under 18, I
encountered all sorts of false and misleading statements bein.g made by the indoor tanning
industry. As the FTC knows, no level of indoor UV tanning is safe and, in fact, use oftanning
beds greatly increase the risk of deadly Melanoma. The ASA should not be allowed to
perpetuate blatant and dangerously false statements and mislead the public because their actions
will increase the number of people dying of deadly skin cancer.
It is not acceptable for the ASA to continue to deceive consumers by continuing with the same
narrative and same statements that were already ruled as having violated the Federal Trade
Commission Act, For the above reasons, I urge swift action by the FTC to prevent the further
spread of misguided infonnation by the ASA to consumers regarding indoor tanning.: '
Sincerely,
TEDW.LIEU
State Senator, District 28
. !":
Attachments:
1. FTC Decision and Order, Docket No. C4290, tiin the Matter oflndoor Tanning A$sociatio.n,'!
dated May 13,2010 ..
2. ASA Statement
cc:
American Suntanning Association
FEB-05-2013 12: 13 From: SENATOR LIEU
9163275989
To: 2023262873
UNJTED STATES OF AMERICA
FEDERAL TRADE COMMISSION
COMMISSIONERS; Jon Leibowitz, Chairman
William E. Kovacic
J. Thomas Rosch
Edith Ramirez
Julie BriU
Jn the Matter of )
)
INDOOR TANNING ASSOCIATION, ) DOCKET NO. C-4290
)
a corporation ) DECISION AND ORDER
082 3159
' .
The Federal Trade Commission having initiated an investigation of cenain acts and
practices of the respondent named in the caption hereof, and the respondent having been
furnished thereafter with a copy of s draft of complaint which the Bureau of Consumer
Protection proposed to present to the Commission for its consideration and which, if issued by
the Commission, would charge the respondent with violation of the Federal Trade Commission
Act; and
The respondent and counsel for the Commi:ssion having thereafter executed an agreement
containing "' consent order, an admission by the respondent of ull the jurisdictionul facts set fonh
in the aforesaid draft complajnt, a statement that the signing of the agreement is for settlement
purposes only and does not constitute an admission by the respondent tbat the law has beeo
violated as alleged in such complaint, or tbat any of the facts as a1leged in such complaint, other
than jurisdictional facts, are true, and waivers and otber provisions as required by the
Commission's Rules; and
The Commission having thereafter considered the matter and having determined that it
bad reason to believe that the respondent has violated the Act, and that complaint should issue
stating its charges in that respect, and having thereupon accepted the executed consent
agreement and placed such agreement on the public record for a period fo thirty (30) days for the
receipt and consideroition of public comments, and having ~ l y coosjdered the comments
received from interested persons, now in further conformity with the procedure described in .
Commission Rule 2.34, 16 C.F.R. 2.34, the Commission hereby issues its Complaint, makes
the following jurisdictional findings, and issues the followil\g Order:
FEB-05- 2013 12:13 From: SENATOR LIEU
9163275989 To:2023262873
1 . Respondent lndoor Tanrung Association ( .. IT A'.) is a Massachusetts corporation with its
principal office or place of business at 2025 M N.W., Washington, D.C. 20036.
2. The F.ederal "Trade Commission has jurisdiction of the subject matter of this proceeding
a,nd of the respondent and this proceeding is in the public interest.
ORDER
DEFINITIONS
For the purposes of this order, the following defini tions shall apply:
1. Unless otherwise specified, shall mean lndoor Tanning Assoc.iation,
its successors and assiiJlS, its officers when acting in coricert or ' ' '
participation with Indoor Tanning Association, and its executive director: :
2. "Covered product or service, shall mean any ultraviolet lamp or sunlamp product,
as defined in 21 C.F.R. 1040.20; and any commercial facility where consumers
may ultraviolet lamps or sunlamp products.
3. "Clearly and conspicuously" means:
: . . : . .
a. ln print communications, the disclosure shall be presented in a manner
that stands out from the accompanying text, so that it js sufficiently prominent,
because of its type size, contrast, location, or other characteristics, for an ordinary
consumer to notice, read and comprehend it;
b. In communications made through an ele'crronic medium (such as
television, video, radio, and interactive media such as the lntcmct, online
services, and software), the disclosure shall be presented simultaneously in both
the audio and visual portions of the communication. In any communication
presented solely through visual or audio means, .the shall be ' !
through the same means through which the is preseilted. In
communication disseminated by means of an electronic medium such
as software, the Internet, or online services, the disclosure must be unavoidable.
Any audio disclosure shall be delivered in a volume and cadence sufficient for' an
ordinary consumer to hear and comprehend it. Any vi sual disclosure shall be
presented in a manner that stands out in the context in which it is presented, so
that it is sufficiently prominent, due to its size and shade, contrast to the
background against which it appears, the length of time it appears on the screen,
and its location, for an ordinary consumer to notice, read and it; and
. . .
FEB-05-2013 12:14 From:SENATOR LIEU 9163275989 To:2023262873
c. Regardless of the medium used to disseminate it, the disclosure shaH be in
understandable language and syntax. Nothing contrary to, inconsistent with, or in
mitigation of the disclosure shall be used in any communication.
4. "Close proximity" means on the same print page, web page, online service page,
or other electronic page, and proximate to the triggering representation, and not
accessed or displayed through hyperlinks, pop-ups, interstitials, or other means.
5. "Commerce" shall mean as defined in Section 4 of the Federal Trade Commission
Act, 15 U.S.C. 44.
1.
IT IS HEREBY ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not represent, in any manner,
expressly or by implication, including through the use of a product name, endorsement,.
depiction, or illustration, that:
A. Tanning, including indo?r tanrung, does not increase the risk of skin cancer;
B. Tanning, including indoor tanning, is safe or poses no danger;
C. J.ndoor tanning is approved by the government; and
D. Indoor tanning is safer than tanning outdoors because in indoor tanning facilities,
the amount of ultraviolet llght is monitored and controlled.
n.
IT IS FURTHER ORDERED that respondent, directly or througb any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not misrepresent, in any manner,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, that:
A. Research shows that vitamin D supplements may harm the body's ability to fight
disease; and
B. A study in the Proceedings of the National Academy of Sciences determined: (a)
that sun exposure does not cause skin cancer or melanoma, or that the risk of such
cancer is only hypothetical; (b) that getting a tan is healthy; (c) that the risks of
not getting enough ultraviolet light far outweigh the risk of skin cancer; or (d) that
-3-
FEB-05-2013 12:14 From:SENATOR LIEU 9163275989 To:2023262873
vitamin D has been linked to significantly decreasing the risk of contracting lung,
kidney, or ljver cancer.
Ul.
11' IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not make any representation,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, about the safety, health-related efficacy or performance, or health-
related risks or benefits, of any covered product or service; or about the sources, performance.
efficacy, or health-related risks or benefits of vitamin D; unless the representation is non-
misleading, and, at the time it is made, respondent possesses and relies upon competent and
reliable scientific evidence tbat is sufficient in quality and quantity based on standards generally
accepted in the relevant scientific fields to substantiate that the representation is true. For the
purposes of t.b.is order, competent and reliable scientific evidc:nce shall consist of tests, analyses,
research, studies, or other evidence that have been conducted and evaluated in an objective
manner by qualified persons, tbat are generally accepted in the profession to yield accurate and
reliable results, and whose results are consistent with the body of reliable scientific evidence
relevant to the representation.
IV.
IT IS FURTHER ORDERED t.hat respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not misrepresent, in any manner,
expressly or by implication, inclu<ling through the use of a product name, endot'Sement, .
depiction, or illustration. the existence, contents, validity, results, conclusions, or interpretations
of any test. study, survey, or research.
v.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division. trade name, or otheT device, in connection with the
manufacturing, labeling, advertising, promotjon, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not make any representation, in any
manner, expressly or by implication, including thwugh the use of a product name, endorsement,
depiction, or illustration, about the safety or health benefits of any covered product or service
unless it discloses, clearly and conspicuously, and within close proximity to that representation:
NOTICE: Exposure to ultraviolet radiation may increase tbe likelihood of developing
skin cancer and can cause serious eye injury.
-4-
FEB- 05-2013 12:14 From:SENATOR LIEU 9163275989 To:2023262873
Provided that, in lieu of the above, in the event that advertising for any covered product or
service makes any representation, expre:;sly or by implication, including through the use of a
product name, endorsement, depiction, or illustration, that exposure to ultraviolet radiation
produces vitamin Din the body, or otherwise about the effectiveness or usefulness of such
product for generation of vitamin D, the required disclosure shall be as follows:
NOTICE: You do not need to become tan for your skin to make vitamin D. Exposure
to ultraviolet radiation rnay increase the likelihood of developing skin cancer and can
cause serious eye injw-y.
VI.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other devjce, in connection with the
manufacturing, Jabelin:g. advertising. promotion, offering for sale, sale, or <listxibution of any
covered product or servjce, in or affecting conunerce, shall not provide to any other person or
entity any means or instrumentalities that contain any representation or omission prohibited by
this order. For the purposes of this Part, "means or instrumentalities" shall mean any .
informati.on, including but not necessarily limited to any advertising, labeling, communications
guides, or other promotional material.
VII.
IT IS FURTHER ORl>ERED that respondent Indoor Tanning Association it!;
successors and assigns shall send as soon as practicable, but in no event later than thirty (30)
days after entry of this order, by first-class mail, postage prepaid and return receipt requested, an
exact copy of the notice attached hereto as Attachment A, showing the date of mailing, to all
Indoor Tanning Association members and all other entities to which Indoor Tanning Association
provided advertising on or after January 1, 2008. The notice required by this
paragraph shall not include any other document or enclosures and may be sent to the principal
place of business of each entity.
VIII.
IT lS FURTHER ORDERED that, for a period of five (5) years after the last da.te of
dissemination of any representation covered by this order, respondent Indoor Tanning
Association and its successors and assigns shall maintain and upon request make available to the
Federal Trade Commission for inspection and copying: .
FEB-05-2013 12:15 From:SENATOR LIEU 9163275989 To:2023262873
A. All advertisements and promotional materials containing the
.B. All materials that were relied upon in disseminating the representation; and
C. All tests, reports, studies, demonstrations, or other evidence in its possession or
control that contradict qualify, or call into question such representation, or the
basis relied upon for the representation, including complaints and other
conununications with consumers or with governmental or consumer protection
organizations.
IX.
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall deliver a copy of this order to all current and future principals,
officers, directors, and other employees with managerial authority having responsibilities with
respect to the subject matter of order, and shall secure from each such person a signed and
dated statement acknowledging receipt of the order. Respondent shall deliver this order to
current personnel within thirty (30) days after the date of service of this order, and to future
personnel within thirty (30) days after the person assumes such position or responsibilities.
X.
IT IS FURTllER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall notify the Commission at least thirty (30) days prior to any change
in lhe corporation that may affect compliance obligations arisjng under this order, including but
not limited to a dissolution, assignment, sale, mer&er, or other action that would result in the
emergence of a successor corporation; the creation or dissolution of a subsidiary, parent, or
affiliate that engages in any acts or practices subject to this order; the proposed fi ling of a
bankruptcy petition; or a. change in the corporate name or address. Provided, howevC?,r, that, with
respect to any proposed change in the corporation about which respondent learns less than thirty
(30) days prior to the date such action is to take place, respondent shall notify the Commjssion as
soon as is practicable aftc.r obtaining such knowledge. All notices required by this Part shall be
sent by certified mail to the Associate Director, Division of Enforcement, Bureau of Consumer
Protection, Federal Trade Commission, Washington, D.C. 20580.
XI.
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall, within sixty (60) days after the date of service of this order file with
the Commission a true and accurate repon, in writing, setting forth in detail manner and form
in which respondent has complied with this order. Within ten ( 1 0) days of receipt of written
notice from a representative of the Commission, respondent shall submit additional true and
accurate written reports.
-6-
FEB-05-2013 12:15 From:SENATOR LIEU
9163275989
To:2023262873
XII.
This order will terminate on May 13, 2030, or twenty (20} years frotn the most recent
date that the United States or the Federal Trade Commission files a complaint (with or without
an accompanying consent decree) in federal court alleging any violation o( the order, whichever
comes later; provided, however, that the filing of such a complaint will not affect the duration of:
A. Any Paragraph in this order that terminates in less than twenty (20) years; and
B. Thjs order's application to any respondent that is not named as a defendant in
such complaint; and
C. This order if such complaint is filed after the order ~ terminated pursuant to this
Paragraph.
Provided, further, that if such complaint is dismissed or a federal court rules that the
respondent did not violate any provjsion of the order, and the dismissal or ruling is either not
appealed or upheld on appeal, then the order will terminate according to this Part as though the
complain! had never e ~ filed, except that the order will not terminate between the date such
complajnt is filed and the later of the deadline for appealing such dismissal or ruling and the date
such dismissal or ruling is upheld on appeal.
By the Commission, Commissioner Ramirez not participating.
ISSUED: May 13.2010
Donald S. Clark
Sectetary
-7-
FEB-05-2013 12:15 From: SENATOR LIEU
9163275989 To:2023262873
ATTACHMENT A
[ON INDOOR TANNING ASSOCIATION LETTERHEAD]
IMPORTANT NOTICE ABOUT GOVERNMENT ACTION
[insert addressee name)
[insert addressee address}
Dear IT A Member or Affiliate:
ln a recent lawsuit, the Federal Trade Commission (FTC) charged the
Indoor Tanning Association (ITA) with making misleading representations in its
advertising and marketing for indoor tanning. Among other things, the FTC
alleged that .IT A falsely claimed that indoor tanning poses no risk to health,
including no risk of sldn cancer. ln addition, the FTC alleged that when IT A
represented that indoor tanning caused the skin to generate vitamin D, 1T A fai led
to disclose material facts about the risks of indoor tanning. IT A has agreed to
send this notification to you as part of its senlernent with the FTC.
IT A ~ r e y requests that you immediately stop using all advertising and
marketing materials previously provided by to you by IT A. Amongthe materials
you should no longe:r use are all of the materials contained on the CD-ROM
issued in 2008, includin& the following:
A. The "Melanoma Hype .. print ad
B. The "Overdose of Hysteria" video
C. The "Communications: The Basics" guide and
D. The print ad with the tag line, "Time to rethink sun.tanning?' '
The FTC complaint alleges that these ads contain representations that are false
and/or misleading.
For further information about the FTC's complaint and order, go t.o
www.ftc.gov and search "Indoor Tanning Association!'
-8-
Very truly yours,
1 obn Overstreet
Executive Director
FEB-05-2013 12:15 From:SENATOR LIEU
9163275989
Federal Trade Commission
Protecting Am.erica's Consumers
For 01/26/2010
To: 2023262873
Indoor Tanning Association Settles FTC Charges That It Deceived
Consumers About Skin Cancer Risks From Tanning
The Federal Trade Commission today charged the Indoor Tanning Association with making false ttealth and safety claims
about Indoor tanning. Contrary to claims in the association's advertising, indoor tanning increases the risk of squamous cell
and melanoma skin cancers, according to the FTC complaint. The association has agreeo to a settlement that bars it from any
further deception.
"The messages promoted by the indoor tanning industry fly in the face of scientific evidence," said DavidC. Vladeck, Director
of tne FTC's Bureau of Consumer Protection. "The industry needs to do a better job of communicating the risks of tanning to
consumers."
The Indoor Tanning Association represents tanning facilities and suppliers of tannin9 equipment. The FTC complaint alleges
that in March 2008, the association launched an advertising campaign designed to portray indoor tanning as safe and
beneficial. The campaign include<! two national newspaper ads, television and video advertising, two Web sites, a
communications guide, and point-of-sale materials that were provided to members for distribution In local mar1<ets.
In addition to denying the skin C8ncer risks of tanning, ttto campaign allegedly also made these false claims:
- Indoor tanning Is approved by the government; . .
- Indoor tanning Is safer than tanning outdoors because the arnount of ultraviolet light received when tanning indoors
is monitored and controlled;
- Research shows that vitamin D supplements may harm the body's ability to. fight disease: and
- A National Academy of Sciences study that "the risks of not getting enough ultraviolet light far outweigh
the hypotl'letical risk of skin cancer."
The complaint also alleges that the asspciation failed to disclose material facts in its advertising.
Under its settlement with the Commission, the association is prohibited from making the
misrepresentations challenged in the complaint. from misrepresenting any tests or studies. and from providing deceptive
advertlsliments to members. The settlement also requires that future association ads that make safety or health benefits
claims for indoor tanning may not be misleading and must be substantiated. Further, the order requires that certain future
advertisements from the association contain disclosures. Ads that make claims about the safety or health benefits of indoor
tanning are required to olearly and prominently make this disclosure:
"NOTICE: Exposure to ultraviolet radiation may increase the likelihood of developing skin cancer and can cause serious eye
injury.H
Ads that claim exposure to ultravi olet radiation produces vitamin 0 In the body, or make other claims about the effectiveness
or usefulness of Indoor tanning products or seNlces for the body's generation of vitamin D, must clearl y and prominently make
this disclosure:
"NOTICE: You do not need to become tan for your skin to make vitamin D. Exposure to ultraviolet radiation may increase the
likelihood of developing skin cancer and can cause serious eye injury."
For more information about how indoor or outdoor tanning increases the risk of melanoma and other types of skin cancer. read
the FTC Consumer Alert Indoor T-anning at http:/lwww.ftc.gov/bcp/eduJpubs/consumer/aferts/alt174.pdf
The Commission vote to approve the administrative complaint and proposed consent agreement was 40. 'The FTC will publish
an announcement regardihg the agreement In the Federal Register shortly. The agreement will be subject to public comment
for 30 days, beginning today and continuing through Februery 26, 2010, after which the Commission will decide whether to
make it final. To file a public comment, please oliok on the following hyperl lnk:
http://www. ftc.gov/opa/20 1 0/0 1/ta.nning.shtm 6/24/2011
FEB-05-2013 12:16 Fr om:SENATOR LIEU 9163275989
To : 2023262873
...... - -- - .. -c ... ----------- --------- ----,.,-- --- --- -
https://public.commentworks.com/ftc/lndoortannlngassoc entffollow the instructions at that site.
Copi es of the complaint, the proposed consent agreement, and an analysis of the
agreement to aid In public comment lilre available from both the FTC's Web site at http://www.f\c.gov and the FTC's Consumer
Response Center. Room 130.600 Penn.sylvanla Avenue. N.W .. Washington. DC 20580.
NOTE: The Commission files a complaint when It has reason to that the law has been or is bei ng violated, and it
appears to the Commission that a proceeding is in the public interest. A consent agreement is for settlement purposes only
and does not constitute anadmission of a law violation. When the Commission issues a consent order on a final basis, it
carries the force of law with respect to future Each violation of such an order may result in a civil penalty of up to
$16,000. .
The Fed_eral Trade Commission works for consumers to prevent fraudulent, deceptive, and unfair business practices and to
provide 1nformat!On to help spot, stop, and avoid them. To file a complaint in English or Spanish. vi sit the FTC's online
Complaint Assistant or caii 1-877-FTC-HELP (1-877-382--4357). The FTC enters complaints into Consumer Sentinel, a secure.
online database available to more than 1,700 civil and criminal law enforcement agencies in the U.S. and abroad. The FTC's
Web site provides free information on a variety of consumQr topcs.
MEDIA CONTACT:
Betsy Lorden
Office of Public Affeiro
STAFF CONTACT:
Janet Evans
Buraau of Consumer Protection
202-326-2125
(FTC File No. 0623159)
(Indoor Tanning.wpd)
this News Release .
If you send this linK to someone else. the FTC will not collect any personal information about you or the reci pient.
I Related Items: 1 ..
In the Metter of Indoor Tanning Association, a corporation
/ FTC FHe No. 082 3159
; Consumer Information:
Indoor Tanni ng
Last Mo01f1eCI Frid11y. June 24. 1
http://www .ftc.gov/opa/20 10/0 1/tanning.sbtrn 6/24/201 1
FEB-05-2013 12: 16 From: SENATOR LIEU
9163275989
To: 2023262873
P . 13/13
American Suntanning Association
The ASA has been recently formed to promote the indoor tanning industry in the United
States and to protect it against attacks by the dermatological community and by governmental
authorities at the federal, state and local levels. Indoor tanning has been accused of causing
melanoma and other fonns of skin cancer by the World Health Organization and others based on
quasi-scientific reports that the ASA believes are flawed and biased. The dermatological
community appears to be united in their efforts to drive indoor tanning salons out of business,
and the ASA believes they are spending $5 million or more annually to this end. The money
appears to be coming from the cosmetic and sunscreen industries. We are all aware of the
extensive PR campaign that is being waged us, and of the increasing necessity of
estabhshing our own PR campaign to challenge the incorrect and misleading statements being
made against us.
Promoting the indoor tanning industry will require retention of scientists throughout the
world to help us debunk the scientific reports being used against us, and a major PR and
lobbying campaign to bring the truth about indoor tanning to the government and to the public at
large. We must do our best to convince the FDA that current regulations are adequate to protect
the public, to persuade the CDC to drop their anti-tanning stance, to persuade the NIH to spend
more money on vitamin D research, to prevent any more states or local government agencies
from initiating under-18 tanning bans or any other actions against our industry, and to get
government at all levels to permit the advertising of the health benefits of indoor tanning.
Additionally, the ASA would like to convince the government at all levels that vitamin D
deficiency is one of the country's most serious public health problems and that indoor tanning
plays an t"ole in providing one of the safest ways for citizens to obtain adequate
vitamin D. All of this needs to be accompanied by aPR campaign to bring the truth about
indoor tanning to the public.
1
02/ 05/ 2013 15:19 FAX 2023262873
RECEPTION OK
TX/ RX NO
RECIPIENT ADDRESS
DESTINATION ID
ST. TIME
TIME USE
PGS.
RESULT
OIA
*********************
*** RX REPORT ***
*********************
7179
9163275989
02/ 05 15:14
04'58
13
OK
la]001
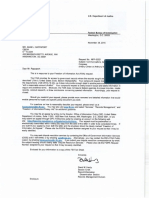
Office of the Secretary
The Honorable Ted W. Lieu
Twenty-Eighth Senate District
California State Senate
State Capitol, Room 4090
Sacramento, CA 95814
Dear Senator Lieu:
UNITED STATES OF AMERICA
FEDERAL TRADE COMMISSION
WASHINGTON, D.C. 20580
March 20, 2013
Thank you for your letters to the Federal Trade Commission expressing a number of
concerns about the newly formed American Suntanning Association ("ASA"). As you point out,
in 2010 - in In the Matter of Indoor Tanning Association, File No. 082 3159, Docket No. C-4290
(May 13, 2010)- the Commission issued a Decision and Order against the Indoor Tanning
Association ("ITA") , settling allegations in an accompanying Complaint that the ITA had made
false health and safety claims about indoor tanning. In particular, Paragraph 5 of the Complaint
alleged that IT A falsely represented, in violation of Section 5( a) and Section 12 of the Federal
Trade Commission Act, 15 U.S.C. 45(a), 52, that
A. Tanning, including indoor tanning, does not increase the risk of skin cancer;
B. Tanning, including indoor tanning, poses no danger;
C. Indoor tanning is approved by the government; and
D. Indoor tanning is safer than tanning outdoors because, in indoor tanning facilities,
the amount of ultraviolet light is monitored and controlled.
The Decision and Order, inter alia, prohibits the ITA from making these representations in the
future.
1
In your letter, you advise that the ASA is composed of many of the same members as the
IT A; that the ASA is arguably a successor to the IT A, and consequently required to comply with
the Commission Decision and Order against the IT A; and that the ASA appears to be making
many of the representations prohibited by the Decision and Order. You therefore request that
the Commission apply the Decision and Order to the ASA, as well as to the IT A.
1
The Commission Complaint, Complaint Exhibits, Decision and Order, and other
documents, including the news releases describing the case, can be found at the following URL:
http://www.ftc.gov/os/caselist/0823159/index.shtm.
The Honorable Ted W. Lieu -- Page 2
We appreciate receiving your correspondence, which has been forwarded to appropriate
members of the Commission staff for review, and I can assure you that the information you have
provided and the concerns you have expressed are being carefully considered. As you may
know, the Commission has been directed by Congress to act in the interest of all consumers to
prevent deceptive or unfair acts or practices, pursuant to the Federal Trade Commission Act, 15
U.S.C. 41-58. Under the FTC Act, a practice is deceptive if it is likely to mislead reasonable
consumers and affect their purchasing decisions? A practice is unfair if it causes or is likely to
cause substantial consumer injury which consumers cannot reasonably avoid, and which is not
outweighed by benefits to consumers or competition.
3
The Commission Complaint and
Decision and Order in the Indoor Tanning Association case are based upon these statutory
principles, and in determining whether a particular practice warrants enforcement or other action,
the Commission may consider a number of factors, including the type of violation alleged, the
nature and amount of consumer injury at issue, the number of consumers affected, and the
likelihood of preventing future unlawful conduct. However, I should note that a number of
statutory provisions and the Commission Rules of Practice prevent me from discussing what
actions, if any, the Commission may take in any particular situation.
We appreciate your interest in this matter, and hope that the foregoing information is of
assistance. Please let us know whenever we may be of assistance with respect to any other
matter.
Sincerely,
DonaldS. Clark
Secretary of the Commission
2
See, e.g., FTC v. Stefanchik, 559 F.3d 924, 928 (9th Cir. 2009); In the Matter of
Telebrands, Corp., 140 F.T.C. 278, 290 (2005), aff'd, 457 F.3d 354 (4
1
h Cir. 2006); see also
Federal Trade Commission Policy Statement on Deception, appended to In the Matter of
Cliffdale Assocs., 103 F.T.C. 110, 74-83 (1984).
3
15 U.S.C. 45(n); see also Federal Trade Commission Policy Statement on
Unfairness, appended to In the Matter of Int 1 Harvester Co., 104 F.T.C. 949, 1070-76 (1984).
Kelly, Andrea
Subject:
Start:
End:
Recurrence:
Organizer:
FDA webinar on indoor tanning
Wed 5/26/2010 2:00 PM
Wed 5/26/2010 3:00 PM
(none)
Evans, Janet M.
Kelly, Andrea
Subject:
Location:
Start:
End:
Show Time As:
Recurrence:
Meeting Status:
Organizer:
Required Attendees:
Indoor Tanning Assoc.
my office
Wed 10/8/2008 10:30 AM
Wed 10/8/2008 11:30 AM
Tentative
(none)
Not yet responded
Henry, Linda
Evans, Janet M.; Ducklow, William T.
When: Wednesday, Oct ober 08, 2008 10:30 AM-11:30 AM (GMT-05:00) East ern Time (US & Canada) .
Where: my office
To discuss findings, strat egy, et c.
Kelly, Andrea
Subject:
Location:
Start:
End:
Recurrence:
Meeting Status:
Organizer:
Required Attendees:
Indoor Tanning Association Meeting with Counsel Dan Mcinnis
H-340
Fri 11/20/2009 2:30 PM
Fri 11/20/2009 3:30 PM
(none)
Accepted
Matties, Deborah J.
JDL; Evans, Janet M.; Engle, Mary Koelbel; Harwood, Charles A.; Eichorn, Mark; Lupovitz,
Joni
When: Friday, November 20, 2009 2:30PM-3:30PM (GMT-05:00) Eastern Time (US & Canada).
Where: H-340
Counsel for proposed respondent Indoor Tanning Association will tentatively meet with the Chairman to discuss st affs
recommendation to issue. an administrative. complaint .. Daniel Mcinnis of Akin Gump is. representing ITA; I do. not yet
know if individual. proposed respondent John Overstreet will. be. attending and whether Mr. Overstreet will. have.
separate counsel..
Kelly, Andrea
Subject:
Location:
Start:
End:
Recurrence:
Meeting Status:
Organizer:
Required Attendees:
Meeting w/Outside counsel - re: Indoor Tanning Association
H385 - Conference Room
Mon 11/30/2009 4:00 PM
Mon ll/30/2009 5:00 PM
(none)
Accepted
Harbour, Pamela Jones
Davis, Tawana E.; Tom, Willard K.; Atleson, Michael; Hippsley, Heather; Evans, Janet M.
When: Monday, November 30, 2009 4:00PM-5:00PM (GMT-05:00) Eastern Time (US & Canada).
Where: H385 - Conference Room
Confirmed attendees to date for the. meeting:
Staff
Michael Atleson- Bureau
Heather Hippsley-Ad Practices
Janet Evans- Ad Practices
Counsel for Indoor Tanning
Dan Mclnnis- Akin Gump, Washi ngton, DC
OGC
Will Tom
Kelly, Andrea
Subject:
Start:
End:
Recurrence:
Organizer:
Read aditi's indoor tanning results; tw Vaishali
Wed 9/22/2010 10:30 AM
Wed 9/22/2010 11:00 AM
(none)
Evans, Janet M.
Kelly, Andrea
Subject:
Location:
Start:
End:
Recurrence:
Meeting Status:
Organizer:
Required Attendees:
Updated: Indoor Tanning Association -- outside counsel meeting with Comm. Rosch
Comm. Rosch's office (enter at H-524)
Mon 11/30/2009 2:00 PM
Mon ll/30/2009 3:00 PM
(none)
Accepted
Hann, Carolyn Lee
Hann, Carolyn Lee; Atleson, Michael; Evans, Janet M.; Murphy, R. Dennis
Kelly, Andrea
Subject:
Location:
Start:
End:
Recurrence:
Meeting Status:
Organizer:
Required Attendees:
Updated: Indoor Tanning Association 0823159 -doc scanning prep meeting
NJ 3213
Thu 10/22/2009 1:30 PM
Thu 10/22/2009 2:30 PM
(none)
Accepted
Dykstra, Peter
Izzard, Walter; Evans, Janet M.; Henry, Linda; Ducklow, William T.
Indoor Tanning Association 0823159 has approximately 18 boxes of docs ( -53k pages) that need to be scanned
and placed into a concordance database. The following are more details:
al most all pages are 8.5 x 11
almost all are B&W
almost all pages are single sided
all docs are "in good shape"
There may also be a disk or two.
I advised Janet that the docs would need to be organized/unitized before we send them to our contractor for
scanning. I briefed Janet on a couple of options for unitization (eg slipsheets, folders, etc.), but told her to hold
off on this until I could get one of our experts to speak with her. Janet mentioned that the pages were already
bates stamped, and that she had an "index" that roughly identifies the ranges for some of the docs. However,
Janet related that her index might need work, and she thought that her team would need to unitize the whole
collection.
Kelly, Andrea
Subject:
Start:
End:
Recurrence:
Meeting Status:
Organizer:
Required Attendees:
Updated: Indoor Tanning Association
Wed 12/2/2009 11:00 AM
Wed 12/2/2009 12:00 PM
(none)
Accepted
Kovacic, William
Kovacic, William; Winerman, Marc; Murphy, R. Dennis; Wagman, Lawrence; Hippsley,
Heather; Evans, Janet M.; Atleson, Michael
I understand that David Vladeck may join us as well
Spiegel, David R.
From:
Sent:
To:
Gorman, Frank
Tuesday, June 08, 2010 5:24PM
Spiegel, David R.
Subject: FW: Press inquiry
Attachments: AACR.Response- Jtrhd.doc
________ , _________ _
From: Evans, Janet M.
Sent: Wednesday, May 26, 2010 10:45 AM
To: Gorman, Frank
Cc: Hippsley, Heather
Subject: FW: Press inquiry
- ~ - - - - - - - - - - - -
From: Weinstock, Martin [mailto:Martin_Weinstock_MD@brown.edu]
Sent: Tuesday, May 25, 2010 6:12PM
To: Evans, Janet M.
Subject: FW: Press inquiry
Janet,
Page 1 of2
------- ------
J received the foll owing news release from the Indoor Tanning Association (ITA) via Liz Szabo, a reporter for USA
Today who was doing a story on a study being published (this week, I think) confirming the link between indoor
tanning and melanoma. Does this violate the agreement between the FTC and the ITA?
Marty Weinstock
From: Szabo, Liz [mai lto:lszabo@usatoday.com]
Sent: Tuesday, May 25, 2010 3:16PM
To: Weinstock, Martin
Subject: FW: Press inquiry
HI Dr. Weinstock,
Here is a response to the study from the Indoor Tanning Association. Is the literature on tanning and melanoma
really contradictory?
Liz Szabo
USA TODAY
Address: 7950 Jones Branch Drive, McLean, VA 22108
Phone: 703-854-5455
Twitter @LfzSzabo
Email: Jszabo@usatoday.com
Web: health.usatodaY..com I Story index I USA TODAY ~
----- .. - - - - - - - - - - ~ - - - - - - - - - - - - - - - - - - . ' - - - - - ~ - - - - - - -
From: Overstreet, John [mailto:joverstreet@theita.com]
6/9/2010
sent: Tuesday, May 25, 2010 2:18PM
To: Szabo, Liz
SUbject: FW: Press inquiry
Dear Ms. Szabo, Please see attached.
John Overstreet
Executive Director
From: Szabo, Liz [mailto:lszabo@usatoday.com]
sent: Monday, May 24, 2010 6:12 PM
To: ITAmailbox
SUbj ect: Press inquiry
Page 2 of2
- -----
I'd like to get the ITA's response to this new study (embargoed until Thursday) on tanning and melanoma. My
deadline is Wednesday at 2 p.m. Thanks.
Liz Szabo
USA TODAY
Address: 7950 Jones Branch Drive, Mclean, VA 22108
Phone:703-854-5455
Twitter @lizSzabo
Email: lszabo@usatoday.com
Web: health.usatoday.com 1 Story index I USA O D Y ~
6/9/2010
'llj T AI'
. r\. ASSOCIATI ON
Rt tpoulbl 31111 Car "'-" $u11
20::!5 M Strl'Cl, .t-:\V Suite 800
DC 20036
Phon<:: 881!-377-0477
riax:
www.theita.com
Response to inquiry about melanoma study published in American Association for Cancer
Research journal May 27, 2010
Overview
The latest science is contradictory. A study out just two weeks ago from the MD Anderson
Cancer Center found that UV A light does not cause melanoma. i
Another study out this week claims that most sunscreens could actually promote the growth of
skin cancers because they contain Vitamin A. ii
A study from a research affiliate of the Harvard medical school found that tanning offers
protection against melanomas. iii
And, a number of other studies and experts also tout the benefits of Vitamin D,
which is produced by the skin with moderate UV exposure.v
So clearly, lots of studies are reaching far different conclusions. These other findings may not be
promoted to the media as actively as those who may have a specific agenda, but they show that
science is still wrestling with this issue and there's certainly still more to learn. We welcome a
more complete body of research that will allow us to advise our customers how to achieve their
goals without unnecessary risk of overexposure.
AACR Article
As for the study published in the AACRjoumal, the researchers averaged a group of people with
the highest risk of melanoma (very fair skin and those with moles) with the general population
and then concluded the risk applies to everyone. But it doesn't. Independent scientists have
reviewed this study and noted that when you remove the high risk groups, there may be a
reduced ri sk for tanning bed users.
When you look at the greatest risk factors identified in this study, tanning isn't even one of the
top factors noted. The number of moles a subject had, bow fair their skin was, and the color of
their hair were all stronger indicators of their risk of melanoma
And even if you were to accept their risk factors, their study says the risk is about 1 in 5,000 that
someone might develop a melanoma. Other scientists believe the risk actually is far lower than
that.
Conclusion
When reputable researchers are coming to vastly different conclusions, it's clear that a lot more
research is needed. As various legislative bodies consider this issue, the science on both sides of
the question needs to be weighed before consideration is given to any sweeping policy changes.
Any potential regulation that would affect millions of people who have tanned for years with no
ill effects needs to consider all of the risk factors in a completely unbiased manner.
i http:/ /www. laboratQI):'.!tCUJ.iP.men,L(!Q_U.JlJiews-UV A-J .I 0 .aspx
ii http://www.aolnews.comlhealtl_l/article/study-many-sunscreens-may-be-acceleratfllg-cancer/19488158
iii http://www.dana-farber.org/abo/newslpress/2007/guardian-of-the-genome-protein-found-to-underlie-skin-
tanning.html
iv http://www.nmltiplesclerosishelp.net/abc-news-vitamin-d-from-uv-exposnre-can-decrease-cancer-by-l!p:to-80
http://abcnews.go.com/video/playerlndex?id=8794501
http:/Labcnews.go.com/videojpJayerlndex?id=8780395
!.!..ttP-://abcnews.go.com/GMA/9nCall/video/fight-cancer-vitamin-d-9907543
htrn://www.cMcer.rnQ.nthly.com/iNPiview.aso?ID=244
Spiegel, David R.
From: Gorman, Frank
Sent: Wednesday, June 16, 2010 3:44PM
To: Spiegel, David R.
Subject: RE: Indoor Tanning Association
e.g. - we have not made any claims of x; we stopped making y claims on such and such date, etc.
From: Spiegel, David R.
Sent: Wednesday, June 16, 2010 3:41PM
To: Gorman, Frank
Subject: Indoor Tanning Association
Page 1 of l
Their executive director says they sent out the letters required by Section VII of the Consent Order
several weeks ago and will supply me with an email confirmation.
I raised with him the requirement in Section XI requiring ITA to submit w/1 60 days (e.g. by mid-July) "a
true and accurate report, in writing, setting forth in detail the manner and form in which respondent has
complied with this order." He said he didn't know what that meant, beyond complying with the letter
notification requirement, and asked for guidance. I told him I would get back. Should I raise this with
Janet?
David R. Spiegel
Federal Trade Commission
Bureau of Consumer Protection
Division of Enforcement
202-326-3281
611612010
-i
!
SOLICITATION/CONTRACT/ORDER FOR COMMERCIAL ITEMS
P-'(;E 1 OF
Offet'or to Complm Blocks 12, 17, 23, U, & 3Q
b\(6\.Cbl I
11
\ 3A--Oata , 4. Onlet NUIT1bet S. N""be' 6. s-.._o ...
llbH6 bli7H I
s.-, 17, :root
1. For ScMicitetion
, . N...,. Crys,.l n.o.._. b. TelephoneN.,..,_ (No cOIIflclcolts) a . Oller OUo Oo<aii.<QI Tme .
tnfonneton Colt
<tho"''''Oo@ll< . ..,. 20V>U-2691 I
!I.IUuec!By Code 0617-04 10, Tt'is Acqu;s;tion Is
11. a....ty tor Foe unless
12.DiscoUntTonna
8locl< 1$ M;>rked.
-
- Un ... l1cl.., Oiu:tut: 0')(.
'-- Sec-Asl<lo %for
OfFICE OF ACQL1SITION Sinal susn..sa Nct ... :)O
FEOERAt ll\AOECO!>IMISSION
600 PENN. AVENUE li.W. ROOM ""l
;=: E"""gi"!l Small8uoinew
WASHlNGTOI#. OC.lOlto HI.IIIZotw s ...... 8..-iftH& w 13o conttaCJis a rate<!""* undo< Ill' AS (IS CFR 700)
... .....O....od
f-
'-- S(a)
NAICS:
- -
14. Mot.od o1 SolialaUon
SizoSIOnd- flRFa nlf8 nRFP
15. 0t-To Code 1141 I Ul . ...,-.,...,By CocM 0611.00
ADVERTISING PRACTICES ,omct: or ACQUismON
f'EDRAt TIIAOE COMMISSION
600PWN AVeNlJE,t.'W ROOM Nlll>
WASHINGTON, OC lOSIO
FeolltyCOcle
I
f'EOEli.At 'D. AI> COMMISSION
o00Pf:NN. AVMIEN,W. l\00M 102
WASI<INOTON. D.C. 21n10
FTC PAVMEIIT UNIT()Ol),69l170
CIO NATIONAL BUSINESS CNTER
P.O. IIOX 27)000
DENY D. CO 102l11000
181>. SUitmil .,..,.,.u.-..s-ln BIOd< aa Un .... Baa_ ;.c-.
X
... ,.,.._
28. c-.-;.leQ......, 10 o9lltlit <loeu ...... olld - I lo X
'loouing Com<oclot avroto lumlsll and- ol...,. sec Iotito or
-. ider.tilled al>crYe and on any ad<11Uonal.,_ta tullt<lo h termo and
...,...,... tpec:JIIA!d '-*"
(b)(6),(b)(7)(C)
0 and C..Wrms lolhe Controct. Eacopt os
321>. Signall;o of Aulhonzed Go..,..,_. R..-lalive
132e. D.to
32d, Pnnle<l Name ond Tife cl. Aulh:>tUed Gov..-
32o. IAaiino A<lclress oi Aultorizod Go__,t R-llv
321. Totephono N...,ber al Authori:zect R_....IIYe
32g. e....,;l oi A.Jihorized Goernmetll ...........
33. St>pN...,.,.,r 34. Voudlet N...-r 35. Amo41nt Veolftod Con-eel r 38, Paynent
137. Che<:kNumbot
For
l lFinot
38. SIR Acc;.otJnt Number 39. SIR VOUdler Nln>ber 40 Paid By
lc.er\ityiN,:
1b Signature <a Tille or C.rtilyirlg Oftlcot
r,
Ooto
I
42a. Rcoc:eived By (Ptlnl)
R_.,ad /4l (loc.otion)
42<;. Data Roc;'O (YYIMMIOO)
0 Par!iol OFinal
12o. Totai C,..ainers
ST ANOARO FORM 1-'49 (REV 312005)
Presaibed by GSA FAA (48 CFR) 53.212
SOLICITATION/CONTRACT/ORDER FOR COMMERCIAL ITEMS
1. Requisition Number
PAGE 1 OF
Offeror to Complete Blocks 12, 17, 23, 24, & 30 (b)(6),(b) 1
12
2. Contract No. J 3. Award/Effective Date 14. Order Number 5. Solicitation Number 6. Solicitation Issue Date
1 Sep 17. 2008
7. For Solicitation I a. Name
Crystal Thompson b. Telephone Number (No co/feel calls) 8. Offer Due Dale/Local Time
Information Call:
cthompson@flc.gov 2021326-2691 I
9. Issued By Code 0617-04 10. This Acquisition is
11. Delivery for FOB Destination Unless
12. Discount Terms
- .
Block is Marked.
_ Unrestnc\ed Discount: 0%
Set-Aside %for
-
0 See Schedule OFFICE OF ACQUISITION Small Business Net due: 30
FEDERAL TRADE COMMISSION
-
Emerging Small Business
600 PENN. AVENUE N.W. ROOM 702
WASI{(NGTON, D.C. 20580 HUBZone Small Business U 13a. This contract is a rated order under DPAS (15 CFR 700)
-
Service-Disabled Veteran-Owned
-
'-- 8(a)
13b. Rating
NAICS:
- -
14. Method of Solicitation
Size Standard:
- -
nRFQ niFB nRFP
15. Deliver To Code 1145 16. Administered By Code 0617-04
ADVERTISING PRACTICES OFFICE OF ACQUISITION
FEDERAL TRADE COMMISSION FEDERAL TRADE COMMISSION
600 PENN A VENUE, NW ROOM NJ-2243 600 PENN. AVENUE N.W. ROOM 702
WASHINGTON, DC 20580 WASHINGTON, D.C. 20580
17a. Contractor/Offeror Code 070516161 Facility Code 18a. Payment Will Be Made By Code0617
(b)(6),(b)(7)(C)
FTC PAYMENT UNIT (303) 969-5770
CIO NATIONAL BUSINESS CENTER
P.O. BOX 272040
DENVER, CO 80227-2040
Telephone No.l (b)(6),(b)(7) I TIN:I(b )(6),(b)( I
n Check if Remittance is Different and Put Such Address in Offer. 18b. Submit Invoices to Address Shown in Block 18a Unless Box Below is Checked.
X See Addendum.
19. 20. 21. 22. 23. 24.
J
ITEM NO. SCHEDULE OF SUPPLIES/SERVICES QUANTITY UNIT UNIT PRICE AMOUNT
25. Accounting and Appropriation Data 26. Total Award Amount (For Govt. Use Only)
l <b)(6),(b)(7)(C)
I
us 28,000.00
x
27a. Solicitation incorporates by reference FAR 52.212-1,52.212-4. FAR 52.212-3 and 52.212-5 are attached. Addenda U are U are not attached
27b. ContracVPurchase Order incorporates by reference FAR 52.212-4. 52.212-5 is at1ached. Addenda JXl are Dare not attached
X 28. Contractor is reQuired to sign this document and return I copies to 29. Award of Contract: Reference. Offer
__.J Issuing Office. Contractor agrees to furnish and deliver aU items set forth or Dated Your offer on Solicitation (Block 5), including
otherwise identified above and on any additional sheets subject to the terms and
any additions or changes which are set forth herein, is accepted as to items:
conditions specified herein.
30a. Signature of OfferoriContrador 31a. United States of America (Signature of Contracting Officer)
'lOb. Name and Title of Signer (Type or Print)
X
30c. Date Signed 31 b. Name of Contracting Officer (Type or Print) 31c. Date Signed
Crystal Thompson
cthompson@ftc.gov
32a. Quantify m Column 21 Has Been
D Received D Inspected D Accepted, and Confonms to the Centrad. Except as Noted:----- - - - - -
32b. Signature of Authorized Government Representative
132c Date
32d. Printed Name and Title of Authorized Government Representative
32e. Maili ng Address of Authorized Government Representative
32f. Telephone Number of Authorized Government Representative
32g. E-mail of Authorized Government Representative
33. Ship Number 34. Voucher Number 35. Amount Veri fied Correct 36. Payment 37. Check Number
For
0 Complete
0
0 Final Partial
l
l Partial
l
I Final
38. SIR Account Number 39. S/R Voucher Number 40. Paid By
41a. I certify this account is correct and proper for payment 42a. Received By (Print)
41b. Signature and Title of Certifying Officer 41c. Date 42b. Received At (Location)
42c. Date Rec'd (YYIMMIDD) 142d. Total Containers
STANDARD FORM 1449 (REV 3/2005)
Prescribed by GSA FAR (48 CFR) 53.212
SCHEDULE Continued
Item No. Supplies/Services Quantity Unit Unit Price Amount
This time-and-materials based contract for expert
services includes two attachments:
I) "FTC' Clauses and Special Provisions Applicable
to the Contract" (six pages); and
2) "NONDISCLOSURE AGREEMENT FOR
CONTRACTORS" (one page).
C'OTR: Janet Evans (202) 326-2125
Matter: Indoor Tanning Association
Matter#: 082-3159
Program Code: 102
EXPERT SERV1CES:I(b)(
6
),(b)(l )(C)
I
NTE
0001 1 LT 25,000.00 25,000.00
:ThJ
The Division of Advertising Practices (DAP)
requiresl(b)(6),(b)(7) ~ provide expert opinion
relating to me neann euccts of ultraviolet exposure,
as direct by the COTR, in connection with
advertising claims about the benefits of tanning,
including indoor tanning.
(b)(3):21 (f),(b)(5),(b)(6),(b)(7)(C)
NTE
0002 Associated travel and other miscellaneous expenses: I LT 3,000.00 3,000.00
Travel cost shall be reimbursed in accordance with
the Federal Travel Regulations.
The houri
rate forl(b)(6),(b)(7)(C)
is
(b)(6) to work approxm13te (b) 1nours.
This is a time-and-materials bas con act with a
cei ling price of $28,000.00.
The period of performance is from the date of award
through 06130/2009.
Page- 2
Table of Contents
Page
1. 52.212-4 CONTRACT TERMS AND CONDITIONS--COMMERCIAL ITEMS (FEB 2007) ................................ .4
2. 52.227-17 RIGHTS IN DATA--SPECIAL WORKS (DEC 2007) .................... ................ .......................................... 4
3. 52.212-4 I CONTRACT TERMS AND CONDITIONS--COMMERCIAL ITEMS (FEB 2007)--ALTERNATE I
(FEB 2007) ...... ....... ................. ............................ .................... .. .................................... .... .... .. ........ .... ..................... ........ 4
4. 52.212-5 CONTRACT TERMS AND CONDITIONS REQUIRED TO IMPLEMENT STATUTES OR
EXECUTIVE ORDERS--COMMERCIAL ITEMS (JUN 2008) ......................... ..... ................ .......... ........................ ... 11
(b)(6),(b)(7)(C)
Page - 3
1. 52.212-4 CONTRACT TERMS AND CONDITIONS--COMMERCIAL ITEMS (FEB 2007)
{Reference)
2. 52.227-17 RIGHTS IN DATA--SPECIAL WORKS (DEC 2007)
(Reference)
3. 52.212-4 I CONTRACT TERMS AND CONDITIONS--COMMERCIAL ITEMS (FEB 2007)--
ALTERNATE I (FEB 2007)
{a) "Inspection/Acceptance."
(1) The Government has the right to inspect and test all materials furnished
and services performed under this contract, to the extent practicable at all
places and times, including the period of performance, and in any event before
acceptance . The Government may also inspect the plant or plants of the
Contractor or any subcontractor engaged in contract performance. The Government
will perform inspections and tests in a manner that will not unduly delay the
work.
(2) If the Government performs inspection or tests on the premises of the
Contractor or a subcontractor, the Contractor shall furnish and shall require
subcontractors to furnish all reasonable facilities and assistance for the safe
and convenient performance of these duties.
(3) Unless otherwise specified in the contract, the Government will accept
or reject services and materials at the place of delivery as promptly as
practicable after delivery, and they will be presumed accepted 60 days after the
date of delivery, unl ess accepted earlier.
(4) At any time during contract performance, but not l ater than 6 months (or
such other time as may be specified in the contract) after acceptance of the
services or materials last delivered under this contract, the Government may
require the Contractor to replace or correct services or material s that at time
of delivery failed to meet contract requirements. Except as otherwise specified
in paragraph (a) (6) of this clause, the cost of replacement or correction shall
be determined under paragraph (i) of this clause, but the "hourly rate" for
labor hours incurred in the replacement or correction shall be reduced to
exclude that portion of the rate attributable to profit. Unl ess otherwise
specified below, the portion of the "hourly rate" attributable to profit shall
be 10 percent. The Contractor shall not tender for acceptance materials and
services required to be replaced or corrected without disclosing the former
requirement for replacement or correction, and, when required, shal l disclose
the corrective action taken.
(5)
(i) If the Contractor fails to proceed with reasonabl e promptness to
perform required replacement or correction, and if the replacement or correction
can be performed within the ceil ing price {or the ceiling price as increased by
the Government), the Government may--
(A) By contract or otherwise, perform the replacement or correction,
charge to the Contractor any i ncreased cost, or deduct such i ncreased cost from
any amounts paid or due under this contract; or
(B) Terminate this contract for cause.
(ii) Fai l ure to agree to the amount of i ncreased cost to be charged to the
Contractor shall be a dispute under the Disputes clause of the contract.
(6) Notwithstandi ng paragraphs (a) (4) and (5) above, the Government may at
any time require the Contractor to remedy by correction or replacement, wi thout
cost to the Government, any failure by the Contractor to comply with the
requirements of this contract, if the failure is due to--
(i) Fraud, lack of good fai th, or wi llful misconduct on the part of the
Contractor's managerial personnel; or
(ii) The conduct of one or more of the Contractor6S employees selected or
retai ned by the Contractor after any of the ContractorLS managerial personnel
has reasonable grounds to believe that the employee is habitually careless or
unqualified.
(b){6),(b)(7)(C)
Page - 4
(7) This clause applies in the same manner and to the same extent to
corrected or replacement materials or services as to materials and services
originally del i vered under thi s contract.
(8) The Contractor has no obligation or liability under this contract to
correct or repl ace materials and services that at time of delivery do not meet
contract requirements, except as provided in this clause or as may be otherwise
specified in the contract.
(9) Unless otherwise specified in the contract, the Contractor's obligation
to correct or replace Government-furnished property shall be governed by the
clause pertaining to Government property.
(b) "Assignment." The contractor or its assignee may assign its rights to
receive payment due as a result of perf ormance of this contract to a bank, trust
company, or o t her financing institution, including any Federal lending agency in
accordance with the Assignment of Claims Act (31 U.S.C. 3727). However, when a
third party makes payment (e.g., use o f the Governmentwide commercial purchase
card), the Contractor may not assi gn its rights to recei ve payment under thi s
contract.
(c) "Changes." Changes in the terms and conditions of this contract may be
made only by written agreement of the parties .
(d) "Disputes." This contract is subject to the Contract Disputes Act of 1978,
as amended (41 U.S.C. 601-613) . Failure of the parties to this contract to reach
agreement on any request f or equitable adjustment, claim, appeal or action
arising under or relating to this contract shall be a dispute to be resolved in
accordance with the clause at FAR 52 . 233-1, Disputes, which is incorporated
herein by reference. The Contractor shall proceed diligently with performance of
this contract, pending final resolution of any dispute arising under the
contract.
(e) "Definitions."
(1} The clause at FAR 52.202-1, Definitions , is incorporated herein by
reference. As used in this clause- -
(i) Direct materials means those materials that enter directly into the
end product, or that are used or consumed directly in connection with the
furnishing of the end product or service.
(ii) Hourly rate means the rat e( s } prescribed in the contract f or payment
for labor that meets the labor category qualifications of a labor category
specif i ed in the contract that are--
(A} Performed by the contractor;
(B) Performed by the subcontractors; or
(C) Transferred between divisions, subsidiaries, or affiliates of the
contractor under a common control.
(iii) Materials means--
(A) Direct materials, including suppl ies transf erred between divisions,
subsidiaries, or affi l iates of the contractor under a common control;
(B) Subcontracts for supplies and incidental services for which there is
not a labor category specifi ed in the contract;
(C) Other d i rect costs (e.g . , incidental services for which there is not
a labor category specified in the contract, travel, computer usage charges,
etc.) ;
(D) The followi ng subcontracts for services whi ch are speci f icall y
excluded from the hourly rate: [Insert any subcontracts for services to be
excluded from the hourly rates prescribed in the schedule.}; and
(E) Indirect costs specifically provided for in this clause.
(iv) Subcontract means any contract, as defined in FAR Subpart 2.1,
entered into with a subcontractor to furnish supplies or services for
performance of the prime contract or a subcontract including transfers between
divisions, subsidiaries, or affiliates of a contractor or subcontractor. It
includes, but is not limited to, purchase orders, and changes and modifications
t o purchase orders.
(f) "Excusable de l ays." The Contractor shal l be liable for default unless
nonperformance is caused by an occurrence beyond the reasonable control of the
Contractor and without its fault or negligence such as, acts of God or the
public enemy, acts of the Government in either its sovereign or contractual
capacity, fires, floods, epidemics, quarantine restrictions, strikes, unusually
(b}(6},(b}(7}(C}
Pag e - 5
severe weather, and delays of common carriers. The Contractor shall not ify the
Contracting Officer in writing as soon as it is reasonably possible after the
commencement of any excusable delay, setting forth the full particulars in
connection therewith, shall remedy such occurrence with all reasonable dispatch,
and shall promptly give written notice to the Contracting Officer of the
cessation of such occurrence.
(g) "Invoice."
(1) The Contractor shall submit an original invoice and three copies (or
electronic invoice, if authorized) to the address designated in the contract to
receive invoices. An invoice must include--
(i) Name and address of the Contractor;
(ii) Invoice date and number;
( iii) Contract number, contract line item number and, if applicable, the
order number;
(iv) Description, quantity, unit of measure, unit price and extended price
of the items delivered;
(v) Shipping number and date of shipment, including the bill of lading
number and weight of shipment if shipped on Government bill of lading;
(vi) Terms of any discount for prompt payment offered;
(vii) Name and address of official to whom payment is to be sent;
(viii) Name, title, and phone number of person to notify in event of
defective invoice; and
(ix) Taxpayer Identification Number (TIN) . The Contractor shall include
its TIN on the invoice only if required elsewhere in this contract.
(x) Electronic funds transfer (EFT) banking information.
(A) The Contractor shall include EFT banking information on the invoice
only if required elsewhere in this contract.
(B) If EFT banking information is not required to be on the invoice, in
order for the invoice to be a proper invoice, the Contractor shall have
submitted correct EFT banking information in accordance with the applicable
solicitation provision, contract clause (e.g., 52.232-33, Payment by Electronic
Funds Transfer- Central Contractor Registration, or 52.232-34, Payment by
Electronic Funds Transfer-Other Than Central Contractor Registration) , or
applicable agency procedures.
(C) EFT banking information is not required if the Government waived the
requirement to pay by EFT.
(2) Invoices will be handled in accordance with the Prompt Payment Act (31
U.S.C. 3903) and Office of Management and Budget (OMB) prompt payment
regul ations at 5 CFR part 1315.
(h) "Patent indemnity." The Contractor shall indemnify the Government and its
officers, employees and agents agai nst liability, including costs, for actual or
alleged direct or contributory infringement of, or inducement to infringe, any
United States or foreign patent, trademark or copyright, arising out of the
performance of this contract, provided the Contractor is reasonably notified of
such claims and proceedings.
(i) "Payments."
(1) Servi ces accepted. Payment shall be made for services accepted by the
Government that have been delivered to the delivery destination(s) set forth in
this contract. The Government will pay the Contractor as follows upon the
submissi on of commercial invoices approved by the Contracting Officer:
(i) Hourly rate.
(A) The amounts shall be computed by multiplying the appropriate hourly
rates prescribed in the contract by the number of direct labor hours performed.
Fractional parts of an hour shall be payable on a prorated basis.
(B) The rates shall be paid for all labor performed on the contract that
meets the labor qualifications specified in the contract. Labor hours incurred
to perform tasks for which labor qualifications were specified in the contract
will not be paid to the extent the work i s performed by individuals that do not
meet the qualifications specified in the contract, unless specifically
authorized by the Contracting Officer.
(C) Invoices may be submitted once each month (or at more frequent
intervals, if approved by the Contracting Officer) to the Contracting Officer or
the authorized representat ive .
(b)(6),(b)(7)(C)
Page - 6
(D) When requested by the Contracting Officer or the authorized
representative, the Contractor shall substantiate invoices (i ncludi ng any
subcontractor hours reimbursed at the hourly rate in the schedule) by evidence
of actual payment, individual daily job t i mecards, records that verify the
employees meet the qualifications for the labor categories specified in the
contract, or other substantiation specified in the contract.
(E) Unless the Schedule prescribes otherwise, the hourly rates in the
Schedule shall not be varied by virtue of the Contractor having performed work
on an overtime basis.
(1) I f no overtime rates are provided in the Schedule and the
Contracting Officer approves overtime work in advance, overtime rates shall be
negotiated.
(2) Failure to agree upon these overtime rates shall be treated as a
dispute under the Disputes clause of this contract.
(3) If the Schedule provides rates for overtime, the premium portion
of those rates will be reimbursable only to the extent the overtime is approved
by the Contracting Officer.
(ii) Materials.
(A) If the Contractor furnishes materials that meet the definition of a
commercial item at FAR 2.101, the price to be paid for such materials shall be
the contractor's established catalog or market price, adj usted to reflect the--
(1) Quantities being acquired; and
(2) Any modifications necessary because of contract requi rements.
(B) Except as provided for in paragraph (i) (1) (ii) (A) and (D) (2) of this
clause, the Government will reimburse the Contractor the actual cost of
materials (less any rebates, refunds, or discounts received by the contractor
that are identifiable to the contract) provided the Contractor - -
(1} Has made payments for materials in accordance with the terms and
conditions of the agreement or invoice; or
(2) Makes these payments within 30 days of the submission of the
payment request to the Government and such payment is in accordance
with the terms and conditions of the agreement or invoice.
(C) To the extent able, the Contractor shall--
(1) Obtain materials at the most advantageous prices available with
due regard to securing prompt delivery of satisfactory materials; and
(2) Give credit to the Government for cash and trade discounts,
rebates, scrap, commissions, and other amounts that are identifiable to the
contract.
(D) Other Costs. Unless listed below, other direct and indirect costs
will not be reimbursed .
(1) Other Direct Costs. The Government will reimburse the Contractor
on the basis of actual cost for the following, provided such costs comply with
the requirements in paragraph (i) (1) ( i i) (B) of this clause: TBD
(2} Indirect Costs (Material Handling, Subcontract Administration,
etc.). The Government will reimburse the Contractor for indirect costs on a pro-
rata basis over the period of contract performance at the following fixed price:
TBD
(2) Total cost. It is estimated that the total cost to the Government for
the performance of this contract shall not exceed the cei l ing price set forth in
the Schedule and the Contractor agrees to use its best efforts to perform the
work specified in the Schedule and all obligations under this contract within
such ceiling price. If at any time the Contractor has reason to believe that the
hourly rate payments and material costs that will accrue in performing this
contract in the next succeedi ng 30 days, if added to all other payments and
costs previously accrued, will exceed BS percent of the ceiling price in the
Schedule, the Contractor shall notify the Contracting Officer giving a revised
estimate of the total price to the Government for performing this contract with
supporting reasons and documentat i on. If at any time during the performance of
this contract, the Contractor has reason to believe that the total price to the
Government for performing this contract will be substantially greater or less
than the then stated ceiling price, the Contractor shal l so notify the
Contracting Officer, giving a revised estimate of the total price for performing
this contract, with supporting reasons and documentation. If at any time during
(b)(6},(b)(7)(C)
Page - 7
performance of this contract, the Government has reason to bel ieve that the work
to be required in performing this contract will be s ubstantial ly greater or less
than the stated ceiling price, the Contracting Officer will so advise the
Contractor, giving the then revised estimate of the total amount of effort to be
required under the contract.
(3) Ceiling price. The Government wil l not be obligated to pay the
Contractor any amount in excess of the ceiling price in the Schedule, and the
Contractor shall not be obligated to continue performance if to do so would
exceed the ceiling price set forth in the Schedule, unless and until the
Contracting Officer notifies the Contractor in writing that the ceiling price
has been increased and specifies in the notice a revised ceiling that shall
constitute the ceiling price for performance under this contract. When and to
the extent that the ceiling price set forth in the Schedule has been increased,
any hours expended and material costs incurred by the Contractor in excess of
the ceiling price before the i ncrease shall be allowable to the same extent as
if the hours expended and material costs had been incurred after the increase in
the ceiling price.
(4) Access to records. At any time before final payment under this contract,
the Contracting Officer (or authorized representative) will have access to the
following (access shall be limited to the listing below unless otherwise agreed
to by the Contractor and the Contracting Officer) :
( i) Records that verify that the employees whose time has been included in
any invoice meet the qualifications for the labor categories specified in the
contract;
(ii) For labor hours (including any subcontractor hours reimbursed at the
hourly rate in the schedule ), when timecards are required as substantiation for
payment--
(A) The original timecards (paper-based or electronic);
(B) The timekeeping procedures;
(C) Contractor records that show the distribution of labor between jobs
or contracts; and
(D) Employees whose time has been included in any invoice for the
purpose of verifying that these employees have worked the hours shown on the
invoices.
(iii) For material and subcont ract costs that are rei mbursed on the basis
of actual cost--
(A) Any invoices or subcontract agreements substantiating material
costs; and
(B) Any documents supporting payment of those invoices.
(5) Overpayments/Underpayments.
(i) Each payment previously made shall be subject to reduction to the
extent of amounts, on preceding invoices, that are found by the Contracting
Officer not to have been properly payable and shall also be subject to reduction
for overpayments or to increase for underpayments. The Contractor shall promptly
pay any such reduction within 30 days unless the parties agree otherwise. The
Government within 30 days will pay any such increases, unless the parties agree
otherwise. The payment will be made by check. If the Contractor
becomes aware of a duplicate invoice payment or that the Government has
otherwise overpaid on an invoice payment, the Contractor shall immediately
notify the Contracting Officer and request instructions for disposition of the
overpayment.
(ii) Upon receipt and approval of the invoice designated by the contractor
as the "completion invoice" and supporting documentation, and upon compliance by
the Contractor with all terms of this contract, any outstanding balances will be
paid within 30 days unless the parties agree otherwise. The completion invoice,
and supporting documentation, shall be submitted by the Contractor as promptly
as practicable following completion of the work under this contract, but in no
event later than 1 year (or such longer period as the Contracting Officer may
approve in writing) from the date of completion.
(6) Release of claims. The Contractor, and each assignee under an ass ignment
entered into under this contract and in effect at the time of final payment
under this contract, shall execute and deliver, at the time of and as a
condition precedent to final payment under this contract, a release discharging
(b)(6),(b)(7)(C)
Page - 8
the Government, its officers, agents, and employees of and from all liabilities,
obligations, and claims arising out of or under this contract, subject only to
the following exceptions.
(i) Specified claims in stated amounts, or in estimated amounts if the
amounts are not susceptible to exact statement by the Contractor.
(ii) Claims, together with reasonable incidental expenses, based upon the
liabilities of the Contractor to third parties arising out of performing this
contract, that are not known to the Contractor on the date of the execution of
the release, and of which the Contractor gives notice in writing to the
Contracting Officer not more than 6 years after the date of the release or the
date of any notice to the Contractor that the Government is prepared to make
final payment, whichever is earlier.
(iii) Claims for reimbursement of costs (other than expenses of the
Contractor by reason of its indemnification of the Government against patent
liability), including reasonable incidental expenses, incurred by the Contractor
under the terms of this contract relating to patents.
(7) Prompt payment. The Government will make payment in accordance with the
Prompt Payment Act (31 U.S.C. 3903) and prompt payment regulations at 5 CFR part
1315.
(8) Electronic Funds Transfer (EFT) . If the Government makes payment by EFT,
see 52.212 - 5(b) for the appropriate EFT clause.
(9) Discount. In connection with any discount offered for early payment,
time shall be computed from the date of the invoice . For the purpose of
computing the discount earned, payment shall be considered to have been made on
the date that appears on the payment check or the specified payment date if an
electronic funds transfer payment is made.
(j) "Risk of loss." Unless the contract specifically provides otherwise, risk
of loss or damage to the supplies provided under this contract shall remain with
the Contractor until, and shall pass to the Government upon:
(1) Delivery of the supplies to a carrier, if transportation is f.o.b.
origin; or
(2} Delivery of the supplies to the Government at the destination specified
in the contract, if transportation is f.o.b. destination.
(k) "Taxes." The contract price includes all applicable Federal, State, and
local taxes and duties .
(1} "Termination for the Government's convenience." The Government reserves
the right to terminate this contract, or any part hereof, for its sole
convenience. In the event of such termination, the Contractor shall immediately
stop all work hereunder and shall immediately cause any and al l of its suppliers
and subcontractors to cease work. Subject to the terms of this contract, the
Contractor shall be paid an amount for direct labor hours (as defined in the
Schedule of the contract} determined by multiplying the number of direct labor
hours expended before the effective date of termination by the hourly rate(s) in
the contract, less any hourly rate payments already made to the Contractor plus
reasonable charges the Contractor can demonstrate to the satisfaction of the
Government using its standard record keeping system that have resulted from the
termination. The Contractor shall not be required to comply with the cost
accounting standards or contract cost principles for this purpose. This
paragraph does not give the Government any right to audit the Contractorls
records. The Contractor shall not be pa id for any work performed or costs
incurred that reasonably could have been avoided.
(m} "Termination for cause." The Government may terminate this contract, or
any part hereof, for cause in the event of any default by the Contractor, or if
the Contractor fails to comply with any contract terms and conditions, or fails
to provide the Government, upon request, with adequate assurances of future
performance. In the event of termination for cause, the Government shall not be
liable to the Contractor for any amount for supplies or services not accepted,
and the Contractor shall be liable to the Government for any and all rights and
remedies provided by law. If it is determined that the Government improperly
terminated this contract for default, such termination shall be deemed a
termination for convenience.
(b}(6},(b}(7}(C}
Page - 9
1n) "Title . " Unless specified elsewhere in this contract, title to items
furnished under this contract shall pass to the Government upon acceptance,
r egar dless o f when o r whe r e the Gov ernment takes physical possession.
(o) "Warranty." The Contractor warrants and implies that the items delivered
hereunder a r e merchantable and fit for use for the particular pur pose described
in this contract .
(p) "Limitation of liability." Except as otherwise provided by an express
warranty, the Contractor will not be liable to the Government for consequential
damages resul t ing f r om any defect or deficiencies in accepted items.
(q) "Other compliances." The Contractor shall comply with all applicable
Federal, State and local laws, executive orders, rules and regulations
applicable to its performance under this contract.
(r ) "Compl i ance with laws unique to Government contr acts." The Cont r actor
agr ees to comply with 31 U.S.C. 1352 rel ating to l imitations on the use of
appr opriated funds to infl uence certain Federal contracts; 18 U.S.C. 431
relating to officials not to benefit; 40 u.s.c. 3701, et seq., Contract Work
Hours and Safety Standards Act; 41 U. S.C. 51 - 58, Anti-Kickback Act of 1986; 41
U.S.C. 265 and 10 U.S.C. 2409 r elating to whi stlebl ower protections; 49 u.s.c.
40118, Fly American; and 41 U.S.C. 423 r elating to procur ement integri ty.
(s) "Or der of p r ecedence." Any inconsistencies in this solicitation or
contract shal l be resol ved by giving precedence in the fol l owing order:
(1) The schedule of supplies/services.
(2) The Assignments, Disputes, Payments, Invoice, Other Compliances, and
Compliance with Laws Unique to Gover nment Contracts par agr aphs of this clause.
(3 ) The clause at 52 . 21 2 - 5.
(4) Addenda to this solicitati on or contr act , including any license
agreements for computer software.
(5) Solicitation provisions if this is a solicitation.
(6) Other paragr aphs of this clause.
(7) The Standard Form 1449 .
(8) Other documents, exhibits, and attachments.
(9) The specification.
(t) "Central Contractor Registration (CCR) ."
(1 ) Unl ess exempted by an addendum to this contract, the Contr actor is
responsibl e dur ing perfor mance and thr ough final payment of any contract for the
accuracy and completeness of the data within the CCR database, and for any
liability resulting from the Government's rel i ance on inaccurate or incomplete
data. To remain register ed in the CCR database after the initial registration,
the Contr actor i s required to review and update on an annual basis from the date
of initial registration or subsequent updates i ts infor mat i on in the CCR
database to ensure it is current, accurate and complete. Updat i ng i nformation in
the CCR does not alter the terms and conditions of this contract and i s not a
substitute for a properly executed contractual document.
(2)
(i) I f a Contractor has legally changed i ts business name, "doi ng busi ness
as" name, or division name (whichever is shown on the contr act), or has
transferred the assets used in performi ng the contract, but has not completed
the necessary requirements regardi ng novation and change - of-name agreements in
FAR Subpart 42.12, the Contractor shall provide the responsible Contracting
Of ficer a minimum of one bus i ness day's wr itten not i fication of its intention to
(A) change the name in the CCR database;
(B) comply with the requirements of Subpart 42 . 12; and
(C) agree in wri ting to the timeline and procedures specified by the
responsible Contracting Officer. The Contractor must provide with the
notification suff icient documentation to suppor t the legally changed name.
(ii ) If the Contractor f ails to compl y with the r equi r ements of paragraph
(t) (2) (i) of this clause, or fails to per form the agr eement at paragraph
(t} (2) (i) (C) of this clause, and, in the absence of a properly executed novation
or change-of - name agreement, the CCR information that shows the Contractor to be
other than the Cont r actor indi cated in the contr act will be consider ed to be
inc o rrect i nformation wi thin the meaning of the "Suspension o f Payment"
paragraph of the electr onic funds t r ansfer (EFT) clause of this contract.
(b)(6),(b)(7)(C)
Page - 10
(3) The Contractor shal l not change the name or address for EFT payments or
manual payment s, as appropr iate, in t he CCR record to reflect an ass ignee f or
the purpose of a ssignment of c l aims (see Sub part 32.8, Assignment of Claims).
Assignees shall be separately registered in the CCR database. Information
provided to the Contractor's CCR record that indi c ates payment s, i ncluding those
made by EFT, to an u l timate recipient other tha n that Contract or will be
conside red to be i nc orr e ct information withi n the meaning of the "Suspension of
payment " para g r aph of the EFT clause of thi s contract.
(4) Offerors and Contractors may obtain information on registration and
annual confirmation requirements via the internet at http://www.ccr.gov or by
call i ng 1 - 888-227 - 2423 or 269 - 961-5757 .
(End of Cl ause)
4. 52. 2 12-5 CONTRACT TERMS AND CONDITIONS REQUIRED TO IMPLEMENT STATUTES OR
EXECUTIVE ORDERS - -COMMERCIAL ITEMS (JON 2008 )
(a) The Contrac tor shal l comply with the following Federa l Acqui sition
Regulation (FAR) clause, which is incorporat ed in this contract by refer ence, to
implement provisions of law or Executive orders applicable to acquisitions o f
commercial items:
(1 ) 52.233-3, Protest after Award (Aug 1996) (31 U.S.C. 3553) .
(2) 52 . 233 - 4, Applicabl e Law for Breach o f Cont r a c t Claim (Oct 2004)
(Pub. L . 10 8 - 7 7 , 10 8-7 8) .
(b) The Contra ctor shall comply wi th t he FAR clauses in this paragr a ph (b)
that t he Contracting Officer has indicat ed as being incorporated i n this
contract by reference to implement provisions of law or Executive orders
applicable to acquis i tions of commerci al items:
XX (i) 52.222 - 50, Combating Trafficking i n Persons (Aug 2007)
(Applies t o a l l contract s) .
XX (36) 52.232-33, Payment by Electroni c Funds Transfer-Central
Contractor Registration (Oct 2003) (31 u . s.c. 3332).
(c) The Contractor shall comply with t he FAR clauses in this p a r agraph (c),
applicable to commercial servi c es, that the Contracting Officer has indicat ed as
being i ncorporated in this contract by reference to implement provisions of l aw
or Executi ve orders applicable to acquisitions o f commercial items:
(May
Act -
Act-
Contract
Contr act
l(b)(6),(b)(7)(C)
(1) 52.222-41 , Service Contract Ac t o f 1965 (Nov 2007)
(4 1 U.S.C. 351, et seq . ).
(2) 52.222 - 42, Statement of Equivalent Rates for Federal Hires
1989) (29 U.S.C. 206 and 41 U.S.C. 351 , et seq. ).
(3) 52.222 - 43, Fair Labor St andards Act and Servi ce Contract
Price Adjustment (Multiple Year and Option Contracts) (May 1989)
(29 u. s.c. 206 and 41 u.s.c. 351, et seq.).
(4) 52.222-44, Fair Labor Standards Act and Service Contract
Price Adjustment (Feb 2002) (29 U.S.C. 206 and 41 U. S.C. 351,
et seq . ) .
(5) 52.222 - 51, Exemption f rom Application of the Servi ce
Act to Contracts for Maintenance, Calibration, or Repair of
Certain Equipment - - Requirements (Nov 2007)
(41 U.S.C. 351, et seq.).
(6) 52 . 222 - 53, Exempt i on f r om App lication of the Service
Act Contracts fro Certain Services--Requirements (Nov 2007)
(41 U. S.C. 351, et seq.).
(7) 52.237-11 , Accepting and Di spensing o f $1 Coin (Aug 2007)
(31 u.s.c. 5112 (p) (1)).
Page - ll
(d) Comptrol l er General Examination of Record. The Cont r actor shall comply
with t he provisions of this paragraph (d) i f this contract was awarded using
o t her than sealed bid, is in excess of the s i mpl ified acquisition threshol d, and
does not contain the clause at 52.215 - 2, Audit and Records - Negotiat i on.
(1) The Comptroller General of the United States, or an authorized
representative of the Comptroller General, shall have access to and right to
examine any of the Contractor's directly pert inent record s involving
transactions related to t his contract .
(2) The Contractor shall make available at its offices at all reasonable
times the records, mater ials, and other evidence for exami nation, audit, or
reproduction, until 3 years after final payment under this contract or for any
shorter period specif i ed in FAR Subpart 4.7, Co ntractor Records Retention, of
the other clauses of this contract. If thi s contract i s completely or partially
terminated, the records relating to the work terminated shal l be made available
for 3 years after any resulting final termination settlement. Records relating
to appeals under the disputes clause or to litigation or the settlement of
c l aims a r i sing under or relating to this contract shall be made availabl e until
such appeal s, l itigation, or claims are final l y resol ved.
(3) As used in this clause, records inc lude books, documents, account i ng
procedures and practices, and other data, regardless of t ype and regardless of
form. This does not require the Contractor to create or maintain any r ecord that
the Contractor does not maintai n in the ordinary course of business or pursuant
to a provision of law.
(e)
(1) Notwithstanding the requirements of the clauses in paragraphs (a), (b),
(c), and (d) of this clause, the Contractor is not required to flow down any FAR
clause, other than those in paragraphs (i) through (vii of this paragraph in a
subcontract for commercial items. Unless otherwise indicated below, the extent
of the flow down shall be a s required by the c l ause--
(i) 52 . 219 - 8, Utilization of Small Business Concerns (May 2004) (15 U.S.C.
637(d) (2) and (3)), in a l l subcontracts that o f fer further subcontracting
opportunities. If the subcontract (except subcontracts to small business
concerns) exceeds $550,000 ($1,000,000 for construction of any publ ic fac i lity),
the subcontract or must include 52 . 219-8 in lower tier s ubcontracts that offer
subcontracting opportunities.
( i i) 52.222 - 26, Equal Opportunity (Mar 2007) (E . O. 11246) .
(iii) 52.222-35, Equal Opportunity for Special Disabled Veterans, Veterans
of the
Vietnam Era, and Other Eligible Veterans (Sept 2006) (38 U.s.c. 4212).
(iv) 52.222-36, Affirmative Action f or Workers with Disabilities (June
1998) (29 u.s.c. 793).
(v) 52.222-39, Notificat i on of Employee Rights Concerning Payment o f Union
Dues or Fees (DEC 2004) (E.O. 13201).
(vi) 52.222 - 41, Service Contract Act of 1 965 (Nov 2007) (41 U.S.C. 351, et
seq.).
(vii) 52.222 - 50, Combating Traf ficking in Persons (Aug 2007) (22 u.s.c.
7104(g)) . Flow down requi red in accordance wi th paragraph ( f ) of FAR c l ause
52 . 222-50.
(viii) 52.222- 51, Exemption from Application of t he Service Contract Act
to Contracts for Maintenance, Calibration, or Repair of Certain Equipment - -
Requi rements (Nov 2007) (41 U.S . c. 351, et seq.) .
(ix) 52.222 - 53, Exemption from Application of the Service Contract Act to
Contracts for Certain Services- - Requi rements (Nov 2007) (41 U.S.C. 351, e t
seq.).
(x) 52.247-64, Preference for Privately Owned U.S. - Flag Commercial Vessels
(Feb 2006) (46 U.S . C. Appx 1241 (b) and 10 U.S.C. 2631). Fl ow down required in
acc ordance with paragraph (d) of FAR clause 52.247-64 .
(2) Whi l e not requi red, the contractor may include in its subcontract s for
commerci al items a minimal number of addi t i onal clauses necessary to satisfy i ts
contractual obligat i ons .
(End of Clause)
(b)(6),(b)(7)(C)
Page - 12
FTC Clauses and Special Provisions Applicable to this Contract
ORDER OF PRECEDENCE: The following clauses and provisions shaU take precedence over any conflicting
terms and conditions included within the Contractor's quotation, proposal, or elsewhere.
l. Release of Information: No FTC data shall be divulged to any unauthorized person for any purpose. The
contractor shall clear with the Contracting Officer any public release of information on this contract/order, to
include news stories, articles, sal.es literature, advertisements, radio-tv spots, etc. Any request for public
release of information should be addressed to:
Federal Trade Commission
Office of Public Affairs
News Director
600 Pennsylvania Avenue, N.W.
Washington, D.C. 20580
2. F.T.C. Non-Disclosure: The unauthorized use of Federal Trade Commission files or information contained
therein is a violation of the Federal Criminal Code and is punishable by a fine of up to$ I 0,000 imprisonment
of up to ten years, or both. The Contractor agrees to have each person who uses the materials relating
to this contract/order execute the "NONDISCLOSURE AGREEMENT FOR CONTRACTORS"
attached hereto and return these documents to the Contracting Officer.
3. COTR. The contractor may accept technical direction, during the period of performance from the
Contracting Officer's Technical Representative (COTR), providing such direction is within the scope of the
contract/ order.
A. The COTR is not authorized to change the scope of work as stated in the contract/order or
obligate the Government (FTC) in any way. The Contracting Officer is the only agent for the FTC
who has the authority to obligate the FTC or change the contract/order terms and conditions. Any such
revision or obligation shaH be authorized in writing only by the Contracting Officers. Any monies
incurred beyond the dollar amount specified in this contract/order or its modifications may not be
paid and does not warrant interest payments as offered under the Prompt Payment Act.
B. COTR Responsibilities: A Contracting Officer's Technical Representative, (COTR) has been named
herein. The COTR is responsible for:
( l) monitoring the contractor's technical progress, including the assessment of performance and
recommending to the Contracting Officer changes in scope of work, contract/order schedules and/or
specifications to meet changes in requirement;
(2) advising on technical matters within the scope of work ;
(3) performing technical evaluation as required;
(4) performing technical inspections and acceptances required by this contract/order; and
(5) assisting the contractor in the resolution of technical problems encountered during performance.
JANUARY 2008 REV03 Page 1 of6
4. Payment: Original invoices are to be submitted to the billing office identified below. For purposes of
this contract/order the designated payment office is:
Re2ular Mail:
FTC Payment Unit
c/o National Business Center
PO Box 272040
Denver, CO 80227-2040
E-mail:
Express Mail:
DOI - National Business Center- FTC
7301 W. Mansfield Ave.
Accounting Operations Branch, D-2730
Denver, CO 80235-2230
FTCPayment_NBCDENVER@NBC.GOV (do not include banking information as the e-mail address is
not a secure site).
NOTE: A duplicate invoice shall be provided to the COTR and the Contracting Officer as listed on the
award documents. Mail to Washington D.C. is still being processed through special irradiation
processes thereby delaying delivery times. It is advised that documents sent to FfC
personnel in Washington D.C. be submitted either electronicaiJy via email or by use of a
delivery service (ex: FedEx, UPS, DHL, Courier, etc.).
5. Invoice Requirements: All Invoices must include the following information:
A. Name and address of contractor.
B. Invoice Date.
C. FTC Contract/Order Number
D. Line Item(s) being invoiced. [When applicable, Name, title, hourly rate and hours charged to each
labor category for each contractor staff for the current month for the applicable sub-part.]
E. Any corrections to previous month's charges for an applicable sub-part will be reported separately and
clearly with a narrative.
F. Any information or documentation required by provision of the contract/order.
NOTE: Contractor payment/financial information is obtained through the Central Contractor
Registration (CCR) Database. It is the contractor's responsibility to ensure that the CCR contains
accurate payment information. Invoices paid late because of inaccurate CCR information are not subject
to interest payments under the Prompt Payment Act.
6. Packaging and Marking
A. Packing for all deliverable items shall be in accordance with the best commercial practices to insure safe
delivery at destination.
B. Distribution and Marking shall be as follows:
Federal Trade Commission
Attention: Janet Evans, NJ-3212
600 Pennsylvania Avenue, N.W.
Washington, DC 20580
JANUARY 2008 REV03 Page 2 of6
C. Deliveries to the FTC Warehouse:
Address: 8405-8407 Ardmore Ardwick Road, Landover, Maryland 20785
Delivery Days/Hours are Monday- Friday from 7:00am- 4:00pm (Eastern Standard Time)
Phone (301) 583-7820, or 301-583-7822. The number for the loading dock is (301) 583-7823. The
FAX number is (301) 583-7821
NOTE: All deliveries must be palletized.
7. Inspection and Acceptance: Inspection and Acceptance will be accomplished by the COTR for services
performed and/or products delivered.
8. FTC Observance of Legal Holidays - Facility Closures:
A. The Federal Trade Commission observes the following days as holidays: New Year's Day, Martin Luther
King's Birthday, Washington's Birthday, Memorial Day, Independence Day, Labor Day, Columbus Day,
Veterans Day, Thanksgiving Day, Christmas Day, and any other day designated by Federal law,
Executive Order, or Presidential Proclamation.
B. When any such day falls on a Saturday or Sunday, the following Monday is observed.
9. Contractor Personnel Security Requirements
**SPECIAL NOTICE** Contractor Orientation takes place on Wednesdays only. It is the COTRs
responsibility to coordinate with the FTC Administrative & Security staff and work with the Contractor to
ensure that all contractor personnel are sent through orientation.
A. Clearance Requirements for Contractor Personnel:
l) Authority: Because Contractor personnel may have access under this contract to sensitive agency data
and computer equipment subject to strict security controls, and/or may have access to a Federal
facility/building, the clearance procedures set forth in this section are necessary and shall be used to
determine the suitability of such individuals for such purposes, under the following authorities: the
Federal Information Security Management Act, Title III of Pub. L. No. 107-347, which requires agencies
to develop security plans for the operation of Federal computer systems that contain systems that contain
sensitive information, and NIST Publication SP 800-4 ( 1992) (Computer Security Considerations in
Federal Procurements); the Privacy Act, 5 U.S.C. 552a, which requires agencies to establish procedures
and safeguards to protect agency systems of records pertaining to individual; and Office of Personnel
Management (OPM) regulations, relating to background investigations of contractor personnel, 5 C.F.R.
Part 736. Contractor badging occurs every Wednesday. Contractor employees may begin work on
any day of the week, as directed by the COTR, but will not have access to information technology (e.g.,
usemame and password) until processed through the Security Office.
2) Applicability: The procedures in this section shall apply to all individuals fulfilling any of the
requirements set forth in this contract.
B. Procedures: The COTR shall provide each such individual with a copy of the procedures set in this
section before or at the time that such individual applies for clearance.
1) Fingerprinting and Forms submission: Each individual employed or otherwise retained by the Contractor
to perform work under this contract shall be fingerprinted at the FTC's Security Office, and shall also
submit to the Contracting Officer's Technical Representative ("COTR") one completed Optional Form
("OF") 306 ("Declaration for Federal Employment," answer Questions 1,7-12, 15, and 16a only). The
JANUARY 2008 REV03 Page 3 of 6
Contractor shall be responsible for all costs associated with completing the forms required by the FTC's
Security Office. Completed forms shall be submitted to the COTR, without alteration or changes to said
forms, at least 10 working days before the individual may begin work or be given access to any agency
records, data, or information in connection with this contract. Contractor processing occurs on
Wednesdays only. Contractor employees may begin work on days other than Wednesdays but
will not be issued contractor badges nor will be granted unlimited access to FTC facilities and
systems.
2) Additional Forms: In addition to the above forms, individuals employed or retained by the Contractor to
fulfill contract positions or duties for 180 days or more, and any individual designated to fulfill certain
sensitive contract positions or duties as determined by the FTC's Security Officer, shall be required to
submit to the COTR, one SF85 or SF85P (and any additional investigative forms) based on a risk
determination by the FTC Security Officer that shall take into account the sensitivity level of the contract
position or duties assigned to the individual, the individual's access, if any, to nonpublic or confidential
information, and any other relevant considerations. The individual must submit these additional forms to
the COTR at least 5 working days before such individual is scheduled to start work or to obtain access to
agency records, data, or information under the contract.
3) Background investigations: The FTC Security Office shall screen all forms for any adverse or derogatory
information, as denoted, for example, by a "yes" to questions 8-12, by additional information in Block 15
on the OF306, or by information on any additional forms that may be required, as discussed above. If the
individual has any adverse or derogatory information, the FTC shall conduct a background investigation
before s/he is permitted to begin work or be given access to agency records, data, or information under
this contract. The background investigation may be conducted in cooperation with or with the assistance
of other relevant government agencies or entities, including, but not limited to, OPM, including referral
to appropriate law enforcement authorities in the event of material falsification or other evidence of
unlawful conduct. To the extent agency records pertaining to these background investigations are subject
to the Privacy Act, such records shall be maintained and used in accordance with the applicable Privacy
Act system notice(s) pertaining to the agency's personnel background investigations. (Note: Neither the
maintenance of such records in the above-described system(s), nor the fact that this contract requires
individuals to complete certain forms or submit to background investigations that may also apply to FTC
employees, shall be deemed to render such an individual a Government or FTC employee in any
manner).
If, as a result of a background investigation, significant adverse or derogatory information is found that
may result in an unsuitability determination, the FTC Security Officer shall notify the COTR and the
relevant individual. The individual will be notified in writing (Statement ofReasons) of the derogatory
information and shall have 30 days to respond or dispute the results of the investigation. If the FTC
Security Officer, after receiving the individual's response, still determines that the individual is
unsuitable to fulfill the contract position or duties in question, the individual will be notified in writing of
that final determination and disqualification.
4) Suitability Determinations: The Government shall have and exercise full and complete control over these
suitability determinations. The Government may, as it deems appropriate, authorize and grant temporary
access and/or interim clearance to employees of the Contractor. However, the granting of temporary
access and/or interim clearance to any such individual shall not be considered as assurance that a fully
favorable suitability determination will follow as a result or condition thereof, and the granting of either
temporary access and/or interim clearance shall in no way prevent, preclude or bar the withdrawal or
termination of any such access or clearance by the Government. Failure of an individual to follow the
JANUARY 2008 REV03 Page 4 of 6
required procedures by this contract may result in suspension/termination of such individual's FTC
clearance/access.
5) A minimum of ten business days prior to the arrival of the contracted staff to the work site the
contractor shall provide the following information to the Federal Trade Commission for each staff
member:
Full legal name
Current address
Gender
Social security number
Date of birth
Place of Birth
Country of Citizenship
Height
Weight
Eye Color
Race
This information may be faxed to 202.326.2945
or mailed to: Federal Trade Commission
600 Pennsylvania Avenue, NW
Washington, DC 20580
ATTN: Security
6) In accordance with Executive Order 12989, as amended on June 9, 2008, it is the contractor's
responsibility to verify their employee's legal status and their eligibility to work. The only approved system is E-Verify,
the Department of Homeland Security tool. The system is available at http://www.uscis.gov/portal/site/uscis.
Verification must be provided with the information required under subparagraph 4) above.
10. Additional Contract Requirements
A. Contractor information systems subject to the Federal Information Security Management Act of 2002
{FISMA). A11 agency information systems, see 44 U.S.C. 3505(c), operated by or on behalf of the
Government by a Contractor or subcontractor containing Federal data shall be subject to the requirements of
the FISMA, including routine testing without advance notice to or approval of the Contractor or its
subcontractors. See 44 U.S.C 3544(b).
B. Handling of third-party requests for access to records. In the event that the Contractor receives any subpoena
or other voluntary or mandatory request for access to data first produced under this Contract, the Contractor
shall immediately notify the COTR and the CO, so that the Government may intervene or take any other steps
it deems necessary to protect its interests.
C. Data Breaches. As part of the requirement explained elsewhere in this document for the contractor to
comply with all contractual and Federal information security, privacy and confidentiality requirements
applicable to the operation, maintenance or support of a Federal information system, the contractor shall be
required to to prevent and remedy data breaches and to provide the FTC with all necessary information and
cooperation, and to take all other reasonable and necessary steps and precautions, to enable the FTC to satisfy
its data breach reporting duties under applicable law, regulation, or policy in the event, if any, that a breach
occurs. Special attention should be paid to OMB Memorandum 06-19 (July 12, 2006), particularly the
extremely urgent reporting time frames included therein for certain breaches, as well as to any other
JANUARY 2008 REV03 Page 5 of 6
subsequent laws, regulations, or policy governing data breaches that may arise during the performance of the
contract. The Information System Security Plan required elsewhere in this document shall include policies
and procedures necessary to ensure the timely detection of and reporting to the FTC of data breaches, as well
as safeguards to prevent and mitigate the risk of, as well as to remedy, such breaches, if any.
D. Use of FTC computer equipment by contractors is limited to what is necessary to accomplish the
work identified under the contract. All contractors or his/her employees or subcontractors are
subject to Internet access monitoring and auditing, and discoveries of inappropriate internet access
or activity not directly related to the contract, will be reported to the COTR and CO, and the
contractor shall be held in default of the contract. Contractors or his/her employees or
subcontractors found accessing inappropriate web sites while using an FTC computer, may be
grounds for initiating disbarment procedures.
E. TRAVEL:
Any authorized travel permitted under this contract must be in accordance with the General Services
Administration (GSA) and associated Federal Travel Regulations (FTR) (41 Code of Federal
Regulations (CFR) chapters 300-304) located at: http://www.gsa.gov. The FTR and associated GSA
websites will be utilized to determine all allowances for per diem and transportation costs. Travel
costs will be paid at actual cost within the FTR with no markup. Note: As a general rule all travel
within the continental United States (CONUS) shall be at coach cost with advance purchase fares and
associated lodging reservations utilized to the maximum extent practicable by all contractors. Travel
costs above those authorized by GSA including travel and per diem must be pre-approved by the
Contracting Officer's Technical Representative (COTR). It is the contractor's responsibility to make
every reasonable effort to book tickets and lodging that falls within the per diem rates. The contractor
shall submit copies of any airline, train, bus tickets and any other travel invoices in excess of $75.00
with their invoice.
Travel will only be paid where the contract or order, as applicable, contains a Contract Line Item for
travel expenses.
(End of Text)
JANUARY 2008 REV03 Page 6 of6
UNITED STATES OF AMERICA
FEDERAL TRADE COMMISSION
WJISHINGTON. D.C. 20580
NONDISCLOSURE AGREEMENT FOR CONTRACTORS
(1) Disclosure of FTC materiiJls and information. I will not divulge FTC materials and infonnation
for any purpose to any person other than an authorized person.
uFTC materials and information" includes both materials and information provided to me
by the FTC (whether the FTC received such materials and information from a submitter
or generated them internally) and me pursuant to my work for the FTC. It
includes materials and information in any form, including, for example, electronic form,
and it includes information identifying the existence of a nonpublic FTC investigation.
All "authorized person" is
(I) a member of the FTC staff, or
(2) other contractor personnel from whom the Contracting Officer has
received a signed FTC "Nondisclosure Agreement for Contractors."
(2) Use of FTC tltUi illfonlftllf.oll. I will not directly or indirectly use, or allow the use of,
FTC materials and information for any purpose other than that directly associated with my
officially assigned duties. I will not reveal the nalllre or content of FTC materials and
information to any unauthorized person, either by direct action, counsel, recommendation or
suggestion.
{3) Retunr of FTC llfllleriab tmd ilrformtltWII. At the conclusion of my work under this contract, I
will return to the FTC (or destroy, at the request of the Contracting Ollker's Technical
Representative) all FTC materials, including copies, and all records containing FTC materials and
information.
Consistent with the above, I understand that all reports or dati first produced during my contract
with the FTC and in connection with that contract shall be the sole property of the government.
None of these provisions shall limit disclosures: (I) at and consistent with directions of FTC staff,
during an adjudicative or judicial proceeding to which the FTC is a party; or (2) with the written consent
of the FTC General Counsel, or the General Counsel's delegate, which consent can only be given if
consistent with the FTC Act. the FTC's Rules of Practice, and any other applicable laws, regulations, or
orders.
typed or printed name)
,;;;:;;;::;;:;;;;;;;::::::::;------ (company)
l
(b)(6),(b)(7)(C)
L. ------If-- - - (contract number)
(At the time of contract award, the Contracting Officer is _ _ ___ _ _ ...: CR "' Y:.::ST.:;.AL.::;..;cn;.;;toM """ PSO:.:.;..w_ ____ _ _
!he Contracting Officer's Technical RcprcsentaJive is
IANETEVANS
FTC Fom1 X33 (rev. <11061
;;R>
- ------- - ----------------"""11'..,-..,....-------------------...
F41: 7?J Cry s
zoc_-z -
)c) l p
Fom1 W-9 Request for Taxpayer Give form to the
(Rev. October 2007)
Identification Number and Certification
requester. Do not
Oep<trtrnent of the Tren5lJry send to the IRS.
Internal Revenue Sarvic:e
C\i
Jb)(6),(b)(7)(C)
I a>
Cl
Business name, If different from above
"'
a.
c
/
0
CIJ ..
appropriate box; 131 Individual/Sole proprietor 0 Corporation 0 Partnership
a.C
O Exempt
>o.2
0 Umlted liability company. Enter the tax classification (D=disregarded entity, C=corporation. P=partnership) I>- -- ... ;:;
0 Other (sec instructions) .,.
payee
cw A ....
Requester's name and address (optionaQ
-c
l(b )(6),(b )(7)(C)
J
.__
O.o
It:
'i:i r.... ""'" ... 71C
l(b )(6),(b )(7)(C)
I
a>
(b )(6),(b )(7)(C)
I
a.
1/)
Q)
List account number(s) here foplional) Q)
[/)
I :F.Tii
Taxpayer Identification Number (TIN)
Enter your TIN in the appropriate box. The TIN provided must match the name given on Line 1 to avoid
backup withholding. For individuals, this is your social security number (SSN). However, for a resident
alien, sole proprietor, or disregarded entity, see the Part I instructions on page 3. For other entities, it is
your employer identification number (EIN). If you do not have a number, see How to get a TIN on page 3.
(b)(6)
or
Note. If the account is in more than one name, see the chart on page 4 lor guidelines on whose
number to enter.
Certification
Under penalties of perjury, I certify that:
1. The number shown on this form is my correct taxpayer identification number (or I am waiting for a number to be Issued to me), and
2. I am not subject to backup withholding because: (a) I am exempt from backup withholding, or (b) I have not been notified by the Internal
Revenue Service (IRS) that I am subject to backup withholding as a result of a failure to report all Interest or dividends, or (c) the IRS has
notified me that I am no longer subject to backup withholding, and
3. I am a U.S. citizen or other U.S. person (defined below).
Certification instructions. You must cross out item 2 above if you have been notified by the IRS that you are currently subject to backup
withholding because you have failed to report all interest and dividends on your tax return. For real estate transactions, item 2 does not apply.
For mortgage interest paid, acquisition or abandonment of secured property, cancellation of debt, contributions to an Individual retirement
arrangement (IRA), and generally, payments other than interest and dividen , you are not required to sign the Certification, but you must
provide your correct TIN. See the instructions on page 4.
Sign
Here
(b )(6),(b )(7)(C)
General Instructions
Section references are to the Internal Revenue Code unless
otherwise noted.
Purpose of Form
A person who is required to file an infannation return with the
IRS must obtain your correct taxpayer Identification number {TIN)
Ia report, for example, Income paid to you, real estate
transactions, mortgage interest you paid, acquisiti on or
abandonment of secured property, cancellation of debt, or
contributions you made to an IRA.
Use Fonn W-9 only if you are a U.S. person (including a
resident alien}, to provide your correct TIN to the person
requesting it (the requester) and, when applicable, to:
1 . Certify that the TIN you are giving is correct (or you are
waiting for a number to be issued),
2. Certify that you are not subject to backup withholding, or
3. Claim exemption from backup withholding if you are a U.S.
exempt payee. If applicable, you are also certifying that as a
U.S. person, your allocable share of any partnership income from
a U.S. trade or business is not subject to the withholding tax on
foreign partners' share of effectively connected income.
Note. If a requester gives you a fonn other than Fonn W-9 to
request your TIN, you must use the requester's fonn if it is
substantially similar to this Fonn W-9.
Definition of a U.S. person. For federal tax purposes, you are
considered a U.S. person if you are:
An individual who is a U.S. citizen or U.S. resident alien,
A partnership, corporation, company, or association created or
organized in the United States or under the laws of the United
States,
An estate (other than a foreign estate), or
A domestic trust (as defined in Regulations section
301 .7701-7).
Special rules for partnerships. Partnerships that conduct a
trade or business in the United States are generally required to
pay a withholding tax on any foreign partners' share of income
from such business. Further, In certain cases where a Form W-9
has not been received, a partnership is required to presume that
a partner is a foreign person, and pay the withholding tax.
Therefore, if you are a U.S. person that is a partner in a
partnership conducting a trade or business in the United States,
provide Form W-9 to the partnership to establish your U.S.
status and avoid withholding on your share of partnership
income.
The person who gives Fonn W-9 to the partnership for
purposes of establishing its U.S. status and avoiding withholding
on its allocable share of net income from the partnership
conducting a trade or business in the United States is in the
following cases:
The U.S. owner of a disregarded entity and not the entity,
Cat. No. 10231X Form (Rev. 10-2007)
AMENDMENT OF SOLICITATION/MODIFICATION OF CONTRACT ,
1
.contractlocooe I
of Pages
12
2. Amendment/Modification No. J 3. Effective Date 4. Reauisition/Purchase Req. No.
15.
Project No. (if applicable)
01 Oct24,2008
I
6. Issued By Code 0617-04 7. Administered By (If other than Item 6) Code 1145
OFFICE OF ACQUISITION ADVERTISING PRACTICES
FEDERAL TRADE COMMISSION FEDERAL TRADE COMMISSION
600 PENN. AVENUE N.W. ROOM 702 600 PENN A VENUE, NW ROOM NJ-2243
WASHINGTON, D.C. 20580 WASHINGTON, DC 20580
Crystal Thompson 202/326-2691
8. Name and Address of Contractor (No., Street, County, and Zip Code) (X) 9A. Amendment of Solicitation No.
___;_
(b)(6),(b)(7)(C)
Vendor rn- l (b)(B),(b)(?) I
96. Date (See Item 11)
DUNS: (b)(o),(b)(7)(C) r
10A
..
, nf Contract/Order No.
CAGE (b)(6),(b) I
(b)(6),(b)(7)(C)
I
. (7)(C)
X
10B. Date (See Item 13)
Sep 17,2008
Code I Facility Code
11. THIS ITEM ONLY APPLIES TO AMENDMENTS OF SOLICITAliONS
0 The above numbered solicitation is amended as set forth in item 14. The hour and date specified for receipt of Offers 0 is extended lUJ is not extended.
Offers must acknowledge receipt of this amendment prior to the hour and date specified in the solicitation or as amended, by one of the following methods:
(a) By completing items 8 and 15, and returning copies of the amendment; (b) By acknowledging receipt of this amendment on each copy of the offer
submitted; or (c) By separate letter or telegram which includes a reference to the solicitation and amendment numbers. FAILURE OF YOUR ACKNOWLEDG
MENT TO BE RECEIVED AT THE PLACE DESIGNATED FOR THE RECEIPT OF OFFERS PRIOR TO THE HOUR AND DATE SPECIFIED MAY RESULT
IN REJECTION OF YOUR OFFER. If by virtue of this amendment you desire to change an offer already submitted; such change may be made by telegram or
letter, provided each telegram or letter makes reference to the solicitation and this amendment, and is received prior to the opening hour and date specified.
12. Accounting and Appropriation Data (if required)
not applicable $ US 0.00
13. THIS ITEM APPLIES ONLY TO MODIFICATIONS OF CONTRACT/ORDERS.
IT MODIFIES THE CONTRACT/ORDER NO AS DESCRIBED IN ITEM 14.
(x) A. This change order is issued pursuant to: (Specify authority) The changes set forth in item 14 are made in the Contract Order No. in item 10A.
-'-'--
X
B. The above numbered Contract/Order is modified to reflect the administrative changes (such as changes in paying office, appropriation date, etc.)
Set fourth item 14 pursuant to the authority of FAR 43.103 (b)
C. This supplemental agreement is entered into pursuant to authority of:
D. Other (Specify type of modification and authority)
E. IMPORTANT: Contractor I X I is not, I I is required to sign this document and return copies to the issuing office.
14. Description of Amendment/Modification (Organized by UCF section headings, including solicitation/contract subject matter where feasible.)
The purpose of this no-cost modification is to change the COTR From Janet Evans To Bonnie Pulley.
Except as provided herein, all terms and conditions of the document referenced in item 9A or ,OA, as heretofore changed, remains unchanged and in full force and effect.
15A. Name and Title of Signer (Type or Print)
15B. Contractor/Offeror 15C. Date Signed
30-105
PREVIOUS EDITIONS UNUSABLE
16C. Date Signed
Nov 26, 2008
STANDARD FORM 30 (REV. 1083)
Prescribed by GSA FAR (48 CFR) 53.243
SCHEDULE
Item No. Supplies/Services Quantity Unit Unit Price Amount
COTR: Bonnie Pulley (202) 326-2356
Matter: indoor Tanning Association
Matter#: 082-3159
Program Code: 102
EXPERT SERVICES:I(b)(
6
),(b)(7)(C)
NTE
0001 1 LT 25,000.00 25,000.00
(b)(6),(b)(7) I
I(C)
The Division of Advertising Practices (DAP)
req uiresl<b ><6),(b )(7)(C)
o provide expert opinion
relating to the health ettects of ultraviolet exposure,
as direct by the COTR. in connection with
advertising claims about the benefits of tanning,
including indoor tanning.
(b)(3):21 (f),(b)(5),(b)(6),(b)(7)(C)
NTE
0002 Associated travel and other miscellaneous 1 LT 3,000.00 3,000.00
expenses:
Travel cost shall be reimbursed in accordance with
the Federal Travel Regulations.
The hourlv rate forl(b)(
6
),(b)(?)(C) _ I
Ph.D is (b)(6) Ito work
This is a ume-antl-materials based contract with a
ceiling price of $28,000.00.
The period of performance is from the date of
award through 06/30/2009.
1. CONTRACT ID CODE
l PAG:
OF PAGES
AMENDMENT OF SOLICITATION/MODIFICATION OF CONTRACT
I
AMENOWENTIMOOIFICATlON NO. 3. EFFECTIVE DATI; 4. REQUISITlDNIPURCHASE REO. NO. ,5. PROJECT NO. (II applicDblo)
03 Jun 24, 2009
l
ISSUED BY
CODE 0617-04
7. ADMINISTERED BY (tloll:er/llanl/em6)
CODE I
OFFICE OF ACQUISITION
SEE BLOCK 6
FEDEIU\L TIU\DE COMtHSSION
600 PENN. AVENUE N.W. ROOM 702
\oiASHING'l'ON, D.C. 20580
JOANNE COOPER 202/326-2257
NAME AND ADDRESS OF CONTRACTOR (No .. Slteel. Counly. StaiD alld ZIP Coda)
Vendor ID: I
DA. AMENDMENT OF SOLICITATION NO
DUNS: l(b)(6).(b)(7)(C) I
I
96. DATED (SEE ITEM II)
r XG),(bit?Xi:J CAGE: I
10A. MOOIFICATlON OF CONTRACTIORDER NO.
X
I
106. DATED (SEEITEM13)
)DE FACILITY CODE
sep 17, 2008
11. THIS ITEM ONLY APPLIES TO AMENDMENTS OF SOLICITATIONS
] The above nomberad saC-citation is amended as sol lo11111n Item 14. The hour and date specified for rocolpl of Offers 0 Is extended, 0 Is nol eX1ended.
Iars musl acknov.1odgo receipt or this amendment prior to the hour and data speciftad In the solicitation or as amended, by one of the fol'owing methods:
1 By completing Items Band 15, and rotumng copies of Uta amendment; (b) By acknow1edglng receipt of ttis amendment on each copy of tho offer submitted; or (c) By separate letter
telegram whk:h includes a reference to the soncitation and amendment numbers. F AlLURE OF YOUR ACKNOWLEDGMENT TO BE RECENED AT THE PLACE DESIGN A TED FOR THE RECEIPT
:OFFERS PRIOR TO THE HOUR AND DATE SPECIFIED MAY RESULT IN REJECTION OF YOUR OFFER. If by vlnue or this amendment you dcs!ro to change an otter submitted, such
ange may be rrodo by tolewam or totter, provided each telegram or letter makes reference to lhe soOcltaUon and this amendment, and Is received prior to lhe opening hour and dale specified
ACCOUNTING AND APPROPRIATION DATA (If reqtJited)
J(b)(6),(b)<')(C)
2
us 0.00
13. THIS ITEM APPLIES ONLY TO MODIFICATIONS OF CONTRACTS/ORDERS.
IT MODIFIES THE CONTRACT/ORDER NO. AS DESCRIBED IN ITEM 14.
(X) A. THIS CHANGE ORDER IS ISSUED PURSUANT TO: (Specffyau!hO<ity} THE CHANGES SET FORTH IN ITEM 14 ARE tMDE IN THE CONTRACT ORDER NO. IN rTEM 10A.
'-'-=--
X B. THE ABOVE NUMElERED CONTRACT/ORDER IS 1/.0DIFIEO TO REFlECT THE ADI.'JNISTRATlVE CHANGES SET FORTH IN ITEM 14, PURSUANT TO THE AUTHORITY OF FAR 43. 103 (bl.
(such as changes in paying office, apprcpriaUOn dalo, ole.)
C. THIS SUPPLEMENTAL AGREEMENT IS ENTERED INTO PURSUANT TO AUTHORITY OF:
D. OTHER (Specify lypa of modificatiOn and aulholily)
IMPORTANT: Contractor l.!J is not,
U Is required to sign this document and return
copies to the Issuing office.
DESCRIPTION OF AMENDMENT/MODIFICATION (Otpanl.rod by UCF sadion headings,lncludtlg sollcila/ionlcol11taa subjec.l maUor whore foasiblo.)
COTR: Bonnie McGregor (202)326-2356
The purpose of this modification to purchase order FTC-08-H-8234 is to extend the period performance
through December 31, 2009.
;ept as provided herein, all terms and cotuf;tlons of lhe document referenced in Item 9A or 10A, as heretofore changed, remains UO!:hanged and In flf.f force and effect
\. NAME AND TTTLE OF SIGNER (Type or Print} 16A. NAME AND TITLE OF CONTRACTING OFFICER (Type or Print)
JOANNE COOPER
Contracting Officer
3. CONTRACTOR/OFFEROR t5C. DATE SIGNED
om car)
16C DATE SIGNED
Jun 24 , 2009
30105 STANDARD FORM 30 (REV. 1003)
Prescribed by GSA FAR (49 CFR) 53.243
SUPPLIES OR SERVICES AND PRICES/COSTS
ITEM NO. SUPPLIES OR SERVICES
COTR: Bonnie Pulley (202) 326-2356
Matter: Indoor Tanning Association
Matter H: 082-3159
Program Code: 102
00 01 EXPERT SERVICES: fb)(6),(b){7)(C)
~ ~ ~ ~ ~ ~ 6 > I ......__ _____ ____.
The Division of Advertising Practices (DAP)
requires l<b)(6),(b)(7)(C) I to provide expert
opinion relating to the health e ffects of
ultraviolet exposure, as direct by the COTR,
in connection with advertising claims about
the benefits of tanning, including indoor
tanning.
Page - 2
QUANTITY UI
1 LT
UNIT PRICE
NTE
25,000.00
NTE
25,000 . 00
PR DATE PAGE
PURCHASE REQUEST FOR SUPPLIES/SERVICES
Jun 16,2009
1. PURCHASE REQUEST NO.
(b )(6),(b )(7)
C)
2. TYPE
SAP
3.AMOUNT
0.00
4. REQUIRED DELIVERY DATE 5. PROJECT
Dec 31, 2009 0823159
6. BUYER/CONTRACT SPECIALIST Name (Code) 7. AUTHORIZED BY
( ) Bonnie McGregor
1
8. FSC
R424
1
9. PRIORITY 110. FUND CODE
99 2008
11 . PURCHASE FOR 1145 12a. DELIVER TO
ADVERTISING PRACTICES
FEDERAL TRADE COMMISSION
600 PENN A VENUE, NW ROOM NJ-2243
WASHINGTON, DC 20580
DONNA K WOODS 202/326-2296
13. VENDOR
i(b)(6),(b)(7)(C)
ITEM OR
FORM NO.
(1 6)
DESCRIPTION
(17)
COTR: Bonnie McGregor (202) 326-2356
ADVERTISING PRACTICES
FEDERAL TRADE COMMISSION
600 PENN A VENUE, NW ROOM NJ-2243
WASHINGTON, DC 20580
12b. SUPPLEMENTAL ADDRESS
14. ACCOUNTING AND APPROPRIATE DATA
l(b)(6),(b)(7)(C)
I
15. PURPOSE. l (b)(
6
}.(b)(?)(C)
Mod to extend contract. I No change in funds
QUANTITY UNIT
(18) (19)
UNIT PRICE
(20)
000 1 The purpose of this modification to contract number I EA 0.00
(b)(6),(b)(7)(C) is to extend date of
deliverythru 12/31/22009.
COTR: Bonnie McGregor
1145
AMOUNT
(21)
0.00
AMENDMENT OF SOLICITATION/MODIFICATION OF CONTRACT 1
1
contractiD code I
of Pages
12
2. AmendmenUModificalion No.
13. Effective Date
4. Requisition/Purchase Req. No.
15.
Proj ect No. (if applicable)
04 Nov 6, 2009
6. Issued By Code 0617-04 7. Administered By (If other than Item 6} Code 1145
OFFICE OF ACQUISITION ADVERTISING PRACTICES
FEDERAL TRADE COMMISSION FEDERAL TRADE COMMISSION
600 PENN. A VENUE N.W. ROOM 779 600 PENN A VENUE, NW ROOM NJ-2243
WASHINGTON. D.C. 20580 W ASHlNGTON, DC 20580
Crystal Thompson 202/326-2691
8. Name and Address of Contractor (No., Street, County, and Zip Code) (X) 9A. Amendment of Solicitation No .
...:.....;...
. .
)(6),(b)(7)(C)
Vendor
98. Date (See Item 71)
I
DUNSt(b)(6),(b)(7)(C}
1 OA. Modification of ContracUOrder No.
I
(b)(6),(b)(7)(C)
I
7lici
X
10B. Date (See ttem 13)
Sep 17,2008
Code I Facility Code
11. THIS ITEM ONLY APPLIES TO AMENDMENTS OF SOLICITATIONS
0 The above numbered solicitation is amended as set forth in item 14. The hour and date specified for receipt of Offers 0 is extended WJ is not extended.
OHers must acknowledge receipt of this amendment prior to the hour and date specified in the solicitation or as amended, by one of the following methods:
(a) By completing items 8 and 15, and returning copies of the amendment; (b) By acknowledging receipt of this amendment on each copy of the offer
submitted; or (c) By separate letter or telegram which includes a reference to the solicitation and amendment numbers. FAILURE OF YOUR ACKNOWLEDG-
MENT TO BE RECEIVED AT THE PLACE DESIGNATED FOR THE RECEIPT OF OFFERS PRIOR TO THE HOUR AND DATE SPECIFIED MAY RESULT
IN REJECTION OF YOUR OFFER. If by virtue of this amendment you desire to change an offer already submitted, such change may be made by telegram or
letter, provided each telegram or letter makes reference to the solicitation and this amendment, and is received prior to the opening hour and date specified.
12. Accounting and Appropriation Data (if required)
"not applicable" $ US 0.00
13. THIS ITEM APPLIES ONLY TO MODIFICATIONS OF CONTRACT/ORDERS.
IT MODIFIES THE CONTRACT/ORDER NO. AS DESCRIBED IN ITEM 14.
(x) A. This change order is issued pursuant to: (Specify authority) The changes set forth in item 14 are made in the Contract Order No. in item 10A.
__;_;_
X
8. The above numbered Contract/Order is modified to reflect the administrative changes (such as changes in paying office, appropriation date, etc.)
Set fourth item 14 pursuant to the authority of FAR 43.103 (b)
C. This supplemental agreement is entered into pursuant to authority of:
D. Other (Specify type of modification and authority)
E. IMPORTANT: Contractor I X I is not, I I is required to sign this document and return copies to the issuing office.
14. Description of Amendment/Modification (Organized by UCF section headings, including solicitation/contract subject matter where feasible.)
The purpose of this no-cost modification is to assign Linda Henry as the Contracting Officer Technical Representative
(COTR) and extend the period of performance for another 6 months through June 30, 2010.
Except as provided herein, all terms and conditions ol the document referenced In Item 9A or lOA, as heretofore changed, remains unchanged and in full force and effect.
15A. Name and Title of Signer (Type or Print) 16A. Name and title of Contracting Officer (Type or Print)
Crystal Thompson 202/326-2691
Contract Support
ctholl)j:1Son@ftc.gov
15B. Contractor/Offeror 15C. Date Signed
16C. Date Signed
/...., . ..;02...
Nov 6, 2009
(Signature of person authorized to sign) ...- / (Signature of 'Contracting OHicer)
l(b)(6),(b}(7)(C)
I
30 105 STANDARD FORM 30 (REV. 1083)
PREVIOUS EDITIONS UNUSABLE Prescribed by GSA FAR (48 CFR) 53.243
SCHEDULE
Item No. Supplies/Services Ouanlily Unit Unit Price Amount
COTR: Linda Henry (202) 326-2542
Matter: Indoor Tanning Association
Matter#: 082-3159
Program Code: 102
NTE
0001
-o::: xt'cK SERVICES: l(b)(o),(b)(7)(C)
I
1 LT 25,000.00 25,000.00
I
The Division of Advertising Practices (DAP)
requiresl(b)(6),(b)(7)(C) Ito provide expert opinion
relating to me nemm enects of ultraviolet exposure,
as direct by the COTR, in connection with
advertising claims about the benefits of tanning,
including indoor tanning.
(b )(3):21 (f),(b )(5),(b )(6),(b )(?)(C)
NTE
0002 Associated. travel and other miscellaneous 1 LT 3,000.00 3,000.00
expenses:
Travel cost shall be reimbursed in accordance with
the Federal Travel Regulations.
The hourly rate forl(b)(6),(b)(7)(C) I
Ph.D is * b)(6) I to worK
This is a tJme-and-materials based contract with a
ceiling price of $28,000.00.
The period of performance is from the date of
award through 06/30/20 I 0.
AMENDMENT OF SOLICITATION/MODIFICATION OF CONTRACT 11. contract ID Code I
of Pages
12
2. Amendment/Modification No. 3. Effective Date 4. Requisition/Purchase Req. No.
15.
Project No. (if applicable)
05 Nov 9, 2009
I
6. Issued By Code 061 7-04 7. Administered By (If other than Item 6) Code 1145
OFFICE OF ACQUISITION ADVERTISING PRACTICES
FEDERAL mADE COMMJSSION FEDERAL TRADE COMMISSION
600 PENN. AVENUE N.W. ROOM 779 600 PENN A VENUE, NW ROOM NJ-2243
WASHINGTON, D .C. 20580 WASHINGTON, DC 20580
Crystal Thompson 202/326-2691
8. Name and Address of Contractor (No., Street, County, and Zip Code) (X) 9A. Amendment of Solicitation No.
b)(6),(b)(7)(C)
Vendor ID: l (b)(6),(b)(7) I 98. Date (See Item 11)
DUNSj (b)(6),(b)(7)(C) r
10A. Modification of Contract/Order No.
I
X
(b)(6),(b)(7)(C)
I
106. Date (See Item 13)
Sep 17,2008
Code I Facility Code
11. THIS ITEM ONLY APPLI ES TO AMENDMENTS OF SOLICITATIONS
0 The above numbered solicitation is amended as set forth in item 14. The hour and date specified for receipt of Offers 0 is extended lDJ is not extended.
Offers must acknowledge receipt of this amendment prior to the hour and date specified in the solicitation or as amended, by one of the following methods:
(a) By completing items 8 and 15, and returning copies of the amendment; (b) By acknowledging receipt of this amendment on each copy of the offer
submitted; or (c) By separate letter or telegram which includes a reference to the solicitation and amendment numbers. FAILURE OF YOUR ACKNOWLEDG-
MENT TO BE RECEIVED AT THE PLACE DESIGNATED FOR THE RECEIPT OF OFFERS PRIOR TO THE HOUR AND DATE SPECIFIED MAY RESULT
IN REJECTION OF YOUR OFFER. If by virtue of this amendment you desire to change an offer already submitted, such change may be made by telegram or
letter, provided each telegram or letter makes reference to the solicitation and this amendment, and is received prior to the opening hour and date specified.
12. Accounting and Appropriation Data (if required)
"not applicable" $US 0.00
13. THIS ITEM APPLIES ONLY TO MODIFICATIONS OF CONTRACT/ORDERS.
IT MODIFIES THE CONTRACT/ORDER NO. AS DESCRIBED IN ITEM 14.
(x) A. This change order Is issued pursuant to: (Specify authority) The changes set forth in item 14 are made in the Contract Order No. in item 10A.
-'-'--
X
B. The above numbered ContracVOrder is modified to reflect the administrative changes (such as changes in paying office, appropriation date, etc.)
Set fourth ftem 14, pursuant to the authoritv of FAR 43.103 (bl
C. This supplemental agreement is entered into pursuant to authority of:
D. Other (Specify type of modification and authority)
E. IMPORTANT: Contractor I X I is not, I lis required to sign this document and retum copies to the issuing office.
14. Description of Amendment/Modification (Organized by UCF section headings, including solicitatfonlcontract subject matter where feasible.)
The purpose of this no-cost modification is to correct the extended period of performance for another 6 months
through July 1, 2010.
COTR: Linda Henry, 202-326-2542
Except as provided herein, all tenns and conditions of the document referenced in item 9A or lOA, as heretofore changed, remains unchanged and in full force and effect.
15A. Name and Title of Signer (Type or Print)
156. Contractor/Offeror 15C. Date Signed
30105
16C. Date Signed
Officer)
Nov 9, 2009
STANDARD FORM 30 (REV. 10-83)
Prescribed by GSA FAR (48 CFA) 53.243
SCHEDULE
Item No. Supplies/Services Quantity Unit Unit Price Amount
CO'fR: Linda Henry (202) 326-2542
Matter: Indoor Tanning Association
Matter#: 082-3159
Program Code: 102
NTE
0001
EXPERT SERVICES: l (bX6),(b){7XC)
I
1 LT 25,000.00 25,000.00
I
The Division of Advertising Practices (DAP)
provide expert opinion
reJatingo eea t eftects of ultraviolet exposure,
as direct by the COTR, in connection with
advertising claims about the benefits of tanni ng,
includjng indoor tanning.
l(b)(3):21 (f),(b)(5),(b)(6),(b)(7)(C)
NTE
0002 Associated travel and other miscellaneous I LT 3,000.00 3,000.00
expenses:
Travel cost shall be reimbursed in accordance with
the Federal Travel Regulations.
The I
(bX6) s (bX to work approximately H[Jhours.
1s 1s a ttme-and-materials based contract with a
ceiling price of $28,000.00.
The period of performance is from the date of
award through 07/01/2010.
1. CONTRACT 10 CODE
I PAG:
OF PAGES
AMENDMENT OF SOLICITATION/MODI FICATION OF CONTRACT
I
2. AMENDMENT/MODIFICATION NO. 3. EFFECTIVE DATE 4. REOUISITIONIFURCHASE REO. NO. ,5. PROJECT NO. (If oppticable)
06 Nov 3, 2010
l(b)(6),(b)(7)(C) I
6. ISSUED BY
CODE 0617-04
7. ADMINISTERED BY (If other than Item 5)
CODE 11145
OFFICE OF ACQUISITION
ADVERTISING PRACTICES
FEDERAL TRADE COMI'I!SSION
FEDERAL COMMISSION
600 PENN. AVENUE N.W. ROOI1 779
600 PENN AVENOE, NW NJ-2243
D.C. 20580
NASHINGTON, DC 20580
Benaiah Grimes 202-326-2713
6. NAME AND ADDRESS OF CONTRACTOR (No., Street. County, State and ZIP COde)
Vendor Tn
DUNS:
9A. AMENDMENT OF SOLICITATION NO.
I
98. DATED (SEEITEM11)
(b)(6),(b)(7)(C)
CAGE:
lOA. MODIFiCATiON OF CONTRACT/ORDER NO.
X r )(6).(b)(7)(C)
I
109. DATED {SEEITEM13)
CODE FACILilY CODE
Sep 17, 2008
11. THIS ITEM ONLY APPLIES TO AMENDMENTS OF SOLICITATIONS
D The above numbered soDcilation is amended as set torth In Item 14. The hour arld dale specified lor receipt of Offers D is extended, D is not extended.
Offers must acknowledge receipt of this amendment prior to the hour and date specified in the solicitation or as amended, by one of the following methods:
(a} By completing Items B and 15. and returning copies oflhe amendment; (b) By ackno1lo1edging receipt ot thls amendment on each copy ol the olfer submitted; or (c) By separate letler
or telegram which includes a reference to the solicitation and amendment numbers. FAILURE OF YOUR ACKNOWLEDGMENT TO BE RECEIVED AT THE PLACE DESIGNATED FOR THE RECEIPT
OF OFFERS PRIOR TO THE HOUR AND DATE SPECIFIED MAY RESULT IN REJECTION OF YOUR OFFER. If by virtue of lhls amendment you desire to change an offer already submitted, such
change may be made by telegram or letler, provided each telegram or letter makes reference to the solicitation and this amendment. and io received prior to the opening hour and date specified.
12. ACCOUNTING AND APPROPRIATION DATA (if required)
2
l(b)(6),(b)(7)(C)
us -24,219. 98
13. THIS ITEM APPLIES ONLY TO MODIFICATIONS OF CONTRACTS/ORDERS.
IT MODIFIES THE CONTRACT/ORDER NO. AS DESCRIBED IN ITEM 14.
A. THIS CHANGE ORDER IS ISSUED PURSUANT TO : {Specify aulhority) THE CHANGES SET FORTH IN ITEM 14 ARE MADE IN THE CONTRACT ORDER NO. IN ITEM 10A.
X:
8. THE ABOVE NUMBER EO CONTRACT/ORDER IS MODIFIED TO REFLECT THE ADMINISTRATIVE CHANGES SET FORTH IN ITEM 14, PURSUANTTO THE AUTHORITY OF FAR 43.103 (b).
(such as changes in paying office, appropriation date. elc.)
C. THIS SUPPLEMENTAL AGREEMENT IS ENTERED INTO PURSUANT TO AUTHORITY OF:
0. OTHER (Specify type of modiRca/ion and aulhotii)'J
E. IMPORTANT: Contractor bLJ is not,
U is required to sign this document and return
copies to the issuing office.
14. DESCRif>TJON OF AMENDMENT/MODIFICATION (Organizeo oy UCF sec/ion headings, Including solicitation/contract subject matter where feasible.)
The purpose of this modification is to de-obligate the remaining balance of $24,219.98.
The contract is closed and no actditonal work/service is required.
Except as provided herein. all tem1s and conditioflS of the document refetenced in Item 9A or 10A. as heretofore changed, remains unchanged and in fuU force and etrect.
15A NAME AND TITLE OF SIGNER (Type or Print) 16A. NAME AND TITLE OF CONTRACTING OFFICER (Type or Prinl)
Crystal Thompson 202/326-2691
Contract Support
cthomoson@ftc. aov /7
159. CONTRACTOR/OFFEROR 15C. DATE SIGNED
tS/Qnature or oerscn authorized to $ign)
168. ST7S OF AMERICA ( - .
BY / -' --;:?Z; '//'U.n--.:n-
/,1' {Signature of Ccntroc/in(f(Jfficer)
'(, TE SIGNED
11il-f;o
l(b)(6),(b)(7)(C) I
PREVIOUS EDITIONS UNUSABLE
30-105 STANDARD FORM 30 (REV. 10.83)
Prescribed by GSA FAR (48 CFR) 5.1.243
SUPt'LIES OR SERVICES A!-10 E'R!CE:S/COSTS
ITE!1 NO.
0003
SUPPLIES OR SERVICES
COTR: Linda Henry
The purpose of t his modification to contract
numbed (b)(6),(b)(7)(C) I is to
deobligate remaining FY 2008 f unds and close.
r ){6),(b)(7XC)
Page - 2
QUANTITY UI
1 EA
UNIT PRICE AHOUNT
-24,219 .98
BUREAU OF CONSUMER PROTECTION CHECKLIST
Consent Authority
1. MA TIER NAME
Indoor Tanning Association
2. STAFF CONTACT and PHONE NUMBER 3. DIVISION/REGIONAL OFFICE
Janet Evans /202-326-2125 BCP/ Advertising Practices
Check if Matter involves:
r International r Internet r Small Business r Bankruptcy r Scofflaw r Privacy r CAN-SPAM r Hispanic Initiatives
r Expedited Treatment Requested I Reason
Date Commission action requested by:
r Routine matter (no significant legal or policy issues to be decided at the Bureau)
r Legal/Policy Issues
If there are legal or policy issues to be resolved at the Bureau, please describe briefly:
r Bureau Director briefed and has pre-approved matter
r Request that Bureau take a "quick look" at pleadings
r Pleadings checked against models in data base
Please note any unusual or important pleadings issues:
r BE consulted, if appropriate (economist:)
If BE has raised issues, please describe briefly:
r Copy to OCBE, if appropriate (Nat Wood- Mail Drop NJ-2267)
r Consumer Education/Outreach
Does this case provide an opportunity for consumer education, or media or other outreach efforts? If so, describe briefly:
FTC Form P-47 (03/05}
Federal Trade Commission
Matter Management System
MATTER UPDATE NOTICE
Use this form to add, update or delete information about new matters. See the FTC Information Handbook for instructions and information on codes. Please
use the following forms if you need more space: FTC Form 84 for respondents, FTC Form 83 for anything else. Please print.
1. MATTER NUMBER
1 os23Is9
2. CURRENT MATTEA NAME
!Indoor Tanning Association
3. UPDATE MATTER NAME (Complete only il you are changing the mauer name. Use Important descriptive words, up to 30 leiters and spaces in length.)
I
IDENTIFICATION CODES/TITLES (Complete if existing codes need to be updated}
4. MANAGER MIS NO. 5. ORGANIZATION CODE 6. PROGRAM CODE 7. MATTER SOURCE CODE
1 n4s 1 102 1
~
MATTER DESCRIPTION
8. IF THE DESCRIPTION OF THE MATTER HAS CHANGED, BRIEFLY DESCRIBE IT HERE.
EVENT
9. ACTION 10. EVENT DATE
11 . CODE AND NAME OF ORGANIZATION RESPONSIBLE FOR THE EVENT
A-ADD
U UPDATE
C CANCEL
PLANNED ADJUSTED
o6IOI !o9 1 L--1 ~
11145
jDivision of Advertising Practices
u
12. EVENT CODE
14. ACTUAL DATE
I I
17. LANDOC DOCUMENT
13. EVENT DESCRIPTION
15. MIS NO. AND NAME OF PERSON RESPONSIBLE FOR THE EVENT
I I I Janet Evans I
18. DOES THIS EVENT APPLY TO ALL RESPONDENTS?
(YIN)
LJ {If no. list applicable respondents in Item 20.)
19. EVENT COMMENT (Enter a brief description of the event.)
FTC Form 81 (rev 7/01)
16. EVENT SOURCE
u
EVENT RESPONDENTS/DEFENDANTS/PARTICIPANTS (EXTERNAL)
(Use for completed events only)
20. RESPONDENT/DEFENDANT NAME (60 fetters and spaces or less) 21. PARTY ID
CHECK IF NON
RESPONDENT
u
u
u
u
u
(Continue of FTC Form 84 if necessary)
22. ACTION
A-Add D-Delete
u
u
u
23. MIS NO.
FTC STAFF
24. PARTICIPANT NAME
MATTER STATUS
26. BRIEFLY DESCRIBE THE CURRENT STATUS OF THE ENTIRE MATTER.
As of
DATE
UPDATE CODES
27. ACTION TYPE OF CODE CODE
AAdd DDefete (e.g., violation, program)
u
u
u
u
28. ACTION
AAdd DDelete
UPDATE RESPONDENTS
RESPONDENT NAME
(60 letters and spaces or less)
CODE DESCRIPTION
25. TYPE
LJ
LJ
LJ
PARTYID
CHECK IF
PRIMARY
u
u
u
u
CHECK IF NON
RESPONDENT
U ~ ~ ~ ~ L J
u LJ
u LJ
Ul II ILJ
PREPARATION APPROVALS
PREPARED BY SIGNATURE OF APPROVING OFFICIAL SIGNATURE OF REVIEWING OFFICIAL
Clovia Hutchins
Send the completed and signed original form to your data entry staff. They will send the signers and the
manager a copy and forward the original form to the Office of the Secretary for filing.
FTC Form 81-Back (rev 7/01)
Federal Trade Commission
Matter Management System
MATTER UPDATE NOTICE
Use this form to add, update or delete infom1at1on about new matters. See the FTC Information Handbook for Instructions and Information on codes. Please
use the following forms if you need more space: FTC Form 84 for respondents, FTC Form 83 for anything else. Please print.
1. MATIER NUMBER 2. CURRENT MATIER NAME
1 os23ls9 I INDOOR TANNlNG ASSOCIATION
3. UPDATE MA TIER NAME (Cnmplele Mly H you aro changing the matterna:ne. Use importanl doscriplivo words. up In 3D leiters and "Pates in length.)
I
IDENTIFICATION CODES/TITLES (Complete if existing codes need to be updated)
4. MANAGER MIS NO. 5. ORGANIZATION CODE 6. PROGRAM CODE 7. MATTER SOURCE CODE
I I I
LJ
MATTER DESCRIPTION
8. IF THE DESCRIPTION OF THE MATIER HAS CHANGED, BRIEFLY DESCRIBE IT HERE.
EVENT
9. ACTION 10. EVENT DATE
11. CODE AND NAME OF ORGANIZATION RESPONSIBLE FOR THE EVENT
A-ADD
PLANNED
U- UPDATE
09/21109
I I C -CANCEL
u
12. EVENT CODE
14. ACTUAL DATE
I
09/21109
I
17. LANDOC DOCUMENT
ADJUSTED
.._ 11_14_5 _ __,IIADVERTISJNG PRACTICES
13. EVENT DESCRIPTION
15. MIS NO. AND NAME OF PERSON RESPONSIBLE FOR THE EVENT
l t t635 1 II JANET EVANS I
18. DOES THIS EVENT APPLY TO ALL RESPONDENTS?
(Y/N)
U (If no, lis/ respondenls in //em 20.)
16. EVENT SOURCE
u
19. EVENT COMMENT (Enter a brief description of the event.)
FTC Form B1 (rev 7/01)
EVENT RESPONDENTS/DEFENDANTS/PARTICIPANTS (EXTERNAL)
(Use for completed events only)
20. RESPONDENT/DEFENDANT NAME (60 letters and spaces or less) 21. PARTY ID
CHECK IF NON
RESPONDENT
u
u
u
u
u
(Continue of FTC Form 84 if necessary)
22. ACTION
A-Add D-Delete
u
u
u
23. MIS NO.
FTC STAFF
24. PARTICIPANT NAME
MATTER STATUS
26. BRIEFLY DESCRIBE THE CURRENT STATUS OF THE ENTIRE MA TIER.
As of
DATE
UPDATE CODES
27. ACTION TYPE OF CODE CODE
A-Add D-Delete (e.g., violation, program)
u
u
u
u
28. ACTION
A-Add 0-Delete
UPDATE RESPONDENTS
RESPONDENT NAME
(60 letters and spaces or less)
CODE DESCRIPTION
25. TYPE
LJ
LJ
LJ
PARTYID
CHECK IF
PRIMARY
u
u
u
u
CHECK IF NON
RESPONDENT
~ I JOliN OVERSTREET u
U ~ ~ ~ ~ L J
u u
u u
PREPARATION APPROVALS
PREPARED BY SIGNATURE OF REVIEWING OFFICIAL
Send the completed and signed original form to your data ntry staff. They will send the signers and the
manager a copy and forward the original form to the Office of the Secretary for filing.
FTC Form 81-Back (rev7/01)
BUREAU OF CONSUMER PROTECTION CHECKLIST
Recommendation to the Commission
1. MATIER NAME
INDOOR TANNING ASSOCIATION
2. STAFF CONTACT and PHONE NUMBER 3. DIVISION/REGIONAL OFFICE
JANET EVANS (202-326-2125) ADVERTISING PRACfiCES {1145)
Check if Matter involves:
G l nternationai15Z'Internet r Small Business r Bankruptcy r Scofflaw .r Privacy TJ CAN-SPAM I Hispanic Initiatives
r Expedited Treatment Requested I Reason
Date Commission action requested by:
r Routine matter (no significant legal or policy issues to be decided at the Bureau)
r Legal/Policy Issues
If there are legal or policy issues to be resolved at the Bureau, please describe briefly:
r Bureau Director briefed and has pre-approved matter
r Matter reviewed earlier by Bureau (Name of ATD:)
r consent authority r: other (specify):
Please describe any significant changes from earlier proposal:
I Pleadings checked against models in data base
Please note any unusual or important pleadings issues:
I GC consulted, if appropriate (attorney: )
---------------------------------------
lX BE consulted, if appropriate (economist: ) (
If GC or BE does not concur or has raised issues, please descflbe b 1ef/y.
I Copy to OCBE, if appropriate (Nat Wood - Mail Drop NJ-2267)
I Consumer Education/Outreach
Does this case provide an opportunity for consumer education, or media or other outreach efforts? If so, describe briefly:
FTr. Fnrm P- 4n
DOCUMENT CODING FORM (OSCAR)
Office of the Secretary
Federal Trade Commission
Please complete and submit this form with every document filed with, or submitted to, the Office of the Secretary.
1. NAME OF PERSON SUBM1IT1NG DOCUMENT
JANET EVANS
3. SOURCE ORGANIZATION (COMPANY NAME, LAW FIRM NAME OR FTC ORGANIZATION CODE)
1145
4. DOCUMENTTITLE
l(b)(5)
5. DOCUMENT DATE 6. NUMBER OF COPIES SUBMIITEO
09/21109
a. MATTEA NAME
INDOOR TANNING ASSOCIATION
9. BRIEF SUMMARY
2. TELEPHONE NUMBER (INClUDE AREA CODE)
202-326-2125
7. MAITEA NUMBER
0823159
TO BE COMPLETED BY FTC STAFF
tO. LEGAL RESEARCH SYSTEM INDEX TERMS (OPTIONAL)
FILE
11. DOCUMENTS SUBMITTED
RECOMMENDATIONS
c
HEADING
ACTION DOCUMENTS
12. HAS THIS MA TIER BEEN PREVIOUSLY SUBMIITED TO THE COMMISSION?
t NO C YES
TO BE COMPLETED BY THE OFFICE OF THE SECRETARY
SUBHEADING (IF ANY)
r
DOCUMENT TYPE CONFIDENTIALITY ENTRY INITIALS CHECK INITIALS DOCUMENT NUMBER DOCUMENT LOCATION
CODE
FTC Form 336 (rev9J02)
\
Federal Trade Commission
Matter Management System
MATTER UPDATE NOTICE
Use this form to add, update or delete information about new matters. See the FTC lnfonnation Handbook for instructions and infonnation on codes. Please
use the following forms if you need more space: FTC Form 84 for respondents, FTC Form 83 for anything else. Please print.
1. MATIER NUMBER
0823159
2. CURRENT MATIER NAME
!Indoor Tanning Association
3. UPDATE MA TIER NAME (Complete n y ~ you are d\allging lhe matter name Use IITipollal'll desctipttve wOtds, up to 30 leners and spaces on length.)
I
IDENTIFICATION CODES/TITLES (Complete if existing codes need to be updated)
4. MANAGER MIS NO.
116351
5. ORGANIZATION CODE 6. PROGRAM CODE 7. MATTER SOURCE CODE
1 1145
I I LJ
MATTER DESCRIPTION
8. IF THE DESCRIPTION OF THE MATTER HAS CHANGED. BRIEFLY DESCRIBE IT HERE.
EVENT
9. ACTION 10. EVENT DATE
11. CODE AND NAME OF ORGANIZATION RESPONSIBLE FOR THE EVENT
A-ADD
PLANNED
U- UPDATE
12/22/09
I I C- CANCEL
u
12. EVENT CODE
14. ACTUAL DATE
I I
17. LANDOC DOCUMENT
ADJUSTED
13. EVENT DESCRIPTION
15. MIS NO. AND NAME OF PERSON RESPONSIBLE FOR THE EVENT
l tl6351 II Janet M. Evans I
18. DOES THIS EVENT APPLY TO ALL RESPONDENTS?
(Y/N)
L.J (If no. list applcable respondents m Item 20)
19. EVENT COMMENT (Enter a brief description of the event. )
r ~
FTC Form 81 (rev 7/01)
16. EVENT SOURCE
u
EVENT RESPONDENTS/DEFENDANTS/PARTICIPANTS (EXTERNAL)
(Use for completed events only)
20. RESPONDENT/DEFENDANT NAME (60 letters and spaces or less) 21. PARTY ID
CHECK IF NON
RESPONDENT
u
u
u
u
u
(Continue of FTC Form 84 if necessary)
22. ACTION
A-Add D-Delete
u
u
u
23. MIS NO.
FTC STAFF
24. PARTICIPANT NAME
MATTER STATUS
26. BRIEFLY DESCRIBE THE CURRENT STATUS OF THE ENTIRE MATTER.
As of
DATE
27. ACTION TYPE OF CODE
A-Add D-Delete (e.g., violation, program)
u
u
u
u
UPDATE CODES
CODE CODE DESCRIPTION
25. TYPE
LJ
LJ
LJ
CHECK IF
PRIMARY
u
u
u
u
UPDATE RESPONDENTS
28. ACTION
A-Add D-Delete
l_QJ I John Overstreet
RESPONDENT NAME
(60 letters and soaces or less)
PARTY ID
CHECK IF NON
RESPONDENT
.____ ___ ____, u
U ~ ~ ~ ~ U
u u
u u
PREPARATION APPROVALS
PREPARED BY SIGNATURE OF REVIEWI NG OFFICIAL
Janet M. Evans
Send the completed and signed ongmal form to your data e send the s1gners and the
manager a copy and forward the origi nal form to the Office of the Secretary for filing.
FTC Form 81-Back (rev 7/01)
BUREAU OF CONSUMER PROTECTION CHECKLIST
Recommendation to the Commission
1. MATTER NAME
Indoor Tanning Association
2. STAFF CONTACT and PHONE NUMBER 3. DIVISION/REGIONAL OFFICE
Janet M. Evans 1145
Check if Matter involves:
J International I Internet I Small Business I Bankruptcy I Scofflaw I Privacy I CAN-SPAM r Hispanic Initiatives
I Expedited Treatment Requested I Reason
Date Commission action requested by:
I Routine matter (no significant legal or pol icy issues to be decided at the Bureau)
I Legal/Policy Issues
If there are legal or policy issues to be resolved at the Bureau, please describe briefly:
I Bureau Director briefed and has pre-approved matter
IX Matter reviewed earlier by Bureau (Name of ATD:) Mike Attleson
-----------------------------
r consent authority
r other (specify): --- - ---------------
Please describe any significant changes from earlier proposal:
r Pleadings checked against models in data base
Please note any unusual or imporlant pleadings issues:
IX GC consulted, if appropriate (attorney: )
Larry Wagman
fX BE consulted, if appropriate (economist: ) Dennis Murphy
----------------------
If GC or BE does not concur or has raised issues, please describe briefly:
I Copy to OCBE, if appropriate (Nat Wood - Mail Drop NJ-2267)
[x Consumer Education/Outreach
Does this case provide an opporlunity for consumer education, or media or other outreach efforls? If so. describe briefly:
DCBE is preparing a companion consumer ed piece.
FTC Form P-46 (03105)
FEDERAL
TRADE
COMMISSION
1. Circulation Type
r Walk-Around
COMMISSION CIRCULATION
r Adjudicative r Vote r Topping
r Agenda
IX Non-Adjudicative
r Limited
IX Information 2. Document Number 2a. Related Document
Number
IX Non-Agenda
r: Information- Pending
1
:::
1
!J
11
_
Motion : Ito J 545180
3. Matter Name
Indoor Tanning Association
6. Circulated By
Commissioner Pamela Jones Harbour
8. Document Title
9. Circulating Commissioner's Advisor
Tawana Davis
11. Previously Circulated: Commissioner
Harbour
Harbour
12. Action
0. Receiving Commissioner's Advisor
Date
12/10/200
11/3/2009
r xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
4. Matter Number 5. Circulation Date
082-3159 12/22/2009
7. To
(Adjudicative & Non-Adjudicative)
r Chairman Leibowitz
r Comm. Harbour
r Comm. Kovacic
r Comm. Rosch
C
JV'Minutes Section
r General Counsel
(Non-Adjudicative)
1gressional Relations
!Cutive Director
eau of Economics
eau of Consumer Protection
eau of Competition
lie Affairs
cy Planning
ional Offices
_m485
....,.,
1'-.)
,..,
=
C1
<::3 r-1
..,g
::::0
0 >
rrl
r-
('"')
-1
01
N
;u
(./) J>
N
Cl
(f)
m -o
n
C")
:X
0
--;
3::
"'
z
a :n
:;;:.:: c..>
:J"J
(l)
0
z
TO BE COMPLETED BY THE OFFICE OF THE SECRETARY STAFF
Majority Vote
!Voting Deadline
Notified Commissioners
Voting Deadline Tolled (Withdrawal of Vote) New Voting Deadline (Extended by Circulation)
Document Type Confidentiality Code Entry Initials Check Initials
FTC Form 213 Crev. 3/09)
FEDERAL
TRADE
COMMISSION
COMMISSION CIRCULATION.
1. Circulation Type
r Walk-Around
r Agenda
IX Non-Agenda
3. Matter Name
r Adjudicative
IX Non-Adjudicative
r Limited
Indoor Tanning Association
6. Circulated By
Commissioner Pamela Jones Harbour
PJH (Jffi
8. Document Title
r b)(S)
IX Vote
r Information
r
Information - Pending
Motion
I
9. Circulating Commissioner's Advisor ~ 0. Receiving Commissioner's Advisor
Tawana Davis
11. Previously Circulated: Commissioner Date Type
Harbour 11/3/09 NAINAIIPM
12. Action
l(b)(S)
r Topping
2. Document Number 2a. Related Document
Number
l%qa
545180
4. Matter Number 5. Circulation Date
082-3159 12/ 10/2009
7. To
(Adjudicative & Non-Adjudicative)
J Chairman Leibowitz
r Comm. Harbour
r Comm. Kovacic
r Comm. Rosch
r Secretary
~ Minutes Section
r General Counsel
(Non-Adjudicative)
r Congressional Relations
r Executive Director
r Bureau of Economics
r Bureau of Consumer Protection
r Bureau of Competition
r Public Affairs
r Policy Planning
r Regional Offices
r Room485
....,
3:
">
,.,
=
0
=
,...,
2:
-.&;)
:::0
c:
0 J>
,..,
r-
-;
('"')
Gl
-1
:::0
Ui
0
l>
(/)
0
rn
rr;
::b
"
("")
::;:
0
-1 ~
0
::::
z c...>
VJ
TO BE COMPLETED BY THE OFFICE OF THE SECRETARY STAFF
0
z
Majority Vote
'Voting Deadline
Notified Commissioners
Voting Deadline Tolled (Withdrawal of Vote) New Voting Deadline (Extended by Circulation) Effective Date of Action
Document Type I Confidentiality Code Entry Initials
~ h e c k Initials
Document Location
FTC Form 213 (rev. 3/09)
I'
FEDERAL
TRADE
COMMISSION
COMMISSION CIRCULATION
1. Circulation Type
r Walk-Around
r Agenda
IX Non-Agenda
3. Matter Name
r Adjudicative
IX Non-Adjudicative
r limited
Indoor Tanning Association
6. Ckoulaled By
Commissi oner Pamela Jones Harbour 1-
8. Document Title
\\
I
b)(S)
r Vote
r Information
IX
Information - Pending
Motion
I
9. Circulating Commissioner's Advisor r 0. Receiving Commissioner's Advisor
Tawana Davis
11. Previously Circulated: Commissioner Date Type
12. Action
r xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
r Topping
2. Document Number 2a. Related Document
Number
S+5Q05
545180
4. Matter Number 5. Circulation Date
082-3159 11/3/2009
?.To
(Adjudicative & Non-Adjudicative)
r Chairman Leibowitz
r Comm. Harbour
r Comm. Kovacic
r Comm. Rosch
r. Secretary
f/: Minutes Section
r General Counsel
(Non-Adjudicative)
I Congressional Relations
r Executive Director
I Bureau of Economics
I Bureau of Consumer Protection
r Bureau of Competition
r
Public Affairs
r Policy Planning
r Regional Offices
r Room485
"""
1'-.J 1..,
-,..
CC":)
0
_ .....
.:;;::,
1"'1
.L:J
:::0
c:
::;r:
>
(:::.;) r-
-
-:.::;
I< I
-t
I
::0
c.n
w
"J>
::1
(/)
r 1
rr1 ;::::.. (J
(") 0
.... -
__....,
0
(:.;
I)
TO BE COMPLETED BY THE OFFICE OF THE SECRETARY STAFF
....._
Majority Vote
'Voting Deadline
w
0
z
Notified Commissioners
Voting Deadline Toll ed (Withdrawal of Vote) New Voting Deadline (Extended by Circulation) Effective Date of Action
Document Type JConfidentiality Code Entry Initials
Initials
Document Location
FTC Form 213 (rev. 3/09\
f
FEDERAL
TRADE
COMMISSION
COMMISSION CIRCULATION
1. Circulation Type
O W.lt-Around
rJ Agenda
Non-Agenda
3. Matter Name
0 Adjudk:atfve
Non-AdjudicatiVe
C Umlted
Indoor Tanning Association
O Vote
0 Information
(!(j lntOnnatlon Pending
Motion
8. Cirallated By ,
Commissioner Pamela Jones Harbour .
8. Oocunent Trtle
(b){S)
I
9. Circulating Commlseioner'& Advlaor 0. Receiving Commissioner' Adveor
Tswana Davis
11. Previously Circulated: CommiAioner Dale Type
12. Action
0
QTopplng
Ooaunent Number
:1.1. Rellllld Oaclllnltlt
Ntm:a
; 8J-/f11..57(/
546349
4. Matter Number 5. Circ:ulttfan Date
082-31!S9 01/0812010
7.To
(A4udicatlve &
0 a.alrman LAibowltz
QCOmm. Harbour
O<:Gnwn.l<ov.dc
0Conn. Rosdt
{iSecretary
0Minwa Section
[JGen.r .. Counsel
(Non-Adjudlc:atlve)
0 Congr ... lonal Rellltlons
O EXecutive DINctor
O Banau of Ec:onomlca
O Bureau of Consumer Prvtedlon
D Bureau of Competition
D Public; Affairs
0 Polley Planning
0 Regional Ofllea.
0Room485
TO BE COMPLETED BY THE OFFICE OF THE SECRETARY STAFF
MajortyVca
Notified Commieeionel'll
Voting DHdllne Tolled (lMthchWal of Vote} New Voting Oeadlflle (Extended by Ckr:IIIBtlon} Effvctille Date of Action
Document Type !Confidentiality Code lnillals OccunJentlocation
FTC Fonn 213 (rev. 3109)
FEDERAL
TRADE
COMMISSION
COMMISSION CIRCULATION
1. Type
r Walk-Around
) Agenda
IK Non-Agenda
3. Matter Name
I Adjudicative
Non-Adjudicative
C Limlted
Indoor Tanning Association
G. Circulated By
Commissioner Pamela Jones Harbour
8. Document Title
IX Vote
r
Information
r , Information - Pending
Motion
Motion To Accept A Consent Agreement For Comment.
9. Circulating Commissioner's Advisor
Tawana Davis
0. Receiving Commissioner's Advisor
11. Previously Circulated: Commissioner
Commissioner Harbour
Date
01/08/10
I
12. Action I
IX I that recommendation, in which I c
Type
C Topping
2. Document Number 2a. Related Document
Number
5"46566
546349
4. Matter Number 5. Circulation Date
082-3159 01/21110
7.To
(Adjudicative & Non-Adjudicative)
) Chairman Leibowitz
) iComm. Harbour
f; Comm. Kovacic
C Comm. Rosch
rsecretary
Section
r General Counsel
(Non-Adjudicative)
C Congressional Relations
C: Executive Director
r Bureau of Economics
!";Bureau of Consumer Protection
) Bureau of Competition
C: Public Affairs
r Policy Planning
) Regional Offices
["; Room485
""
,....,
--
=>
-...
<::::)
,.,
,..,
CJ
,..,
*A Revised copyo1 the Analysis of Proposed""' C""" o-n-se-nt Order to Aid Public Comment is attached.
' ) Lf>
;;o
...
c:
<:_
;;;:..
:u.
.-
I .
<':l E:
1.1 0-
_ ...
.! : l..l
,. -:
r '"l l I
!.C
Majority Vote
TO BE COMPLETED BY THE OFFICE OF THE SECRETARY STAFF
r'll
(/)
(/)
f'71
("')
--
c
...._
Voting Deadline Tolled (Withdrawal of Vote) New Voting Deadline (Extended by Circulation) Effective Date of Action
Document Type Confidentiality Code Check Initials
FTC Form 213 (rev. 3/09)
::z
-1
N
;;o
>
(':J
,,...
-o ("')
::r .::>
(...,)
;;
.! ..
c.n
'l>
,,.,
w
S?
COMMISSIONER VOTING RECORD
,
Vote Leibowitz Harbour Kovacic Rosch
JD_{KV
0 .u )V1-te:fJ
() 17CJC!/4
;
Yes
Date \ /2\ /20\0 Date t / /0 Date t/at ltD
Date
-/()
Date
Time A : ?..Ol'"'Yv-1 Time Time ". D Time
/J'.
Time
.
No
-
Date Date Date
-
Date Date -
-
Time Time Time
'
Time Time
Abstain
Date Date Date Date Date
Time Time Time Time nme
NP
Absent
Date Date Date Date Date
Time Time Time Time Time
NP
Recused
Date Date Date Date Date
Time Time Time Time Time
--
NP
By Minutes
Date Date Date Date Date
Time Time Time Time Time
NP
Date Date Date Date Date
Time Time Time Time Time
Vote
Withdrawn
Date Date Date Date Date
Time Time Time Time Time
Vote
Leibowitz Harbour Kovacic Rosch
Reinstated
Yes
Date Date Date Date Date
Time Time Time Time Time
No
Date Date Date Date Date
Time nme Time Time Time
Abstain
Date Date Date Date Date
Time Time Time Time Time
NP
Date Date Date Date Date
Time Time Time Time Time
COMMENTS:
FTC Form 213-Back
Thursday, January 28, 201 Profile
Document Title
AGREEMENT CONTAINING CONSENT ORDER. COMPLAINT, AND
ANALYSIS OF PROPOSED CONSENT ORDER TO AID PUBLIC
COMMENT IN THE MATTER OF INDOOR TANNING ASSOCIATION
Document Date
11/22/2010
Page: 1
LANDOC Number
1248649
Oscar Number
I
INDOOR TANNING ASSOCIATION L5_4_66_7_2 __ __,
Matter Number I 0823159 . .
Do tT j::;; PART 2 CONSENT AGREEMENT DOCUMENTS WHEN
cumen ype .__ _ _ ___ ___, CONSENT AGREEMENT IS ACCEPTED FOR PUBLIC
Access I P Ll P_u_b_lic ______ ___J
CMS Ref Number
Format I ECOPY DESKTOP I ECOPY DESKTOP
Document Submitter 149891 l l r: C:-:-LA--:-::R""K=-. =D-=o""' N""" A-=- L=D--= s:-. - ---------------------,
Submitting Organization 1 0825 IILO_F_F_Ic _E_o_F_T_H_E_S_E_C_R _E_T_A_R_Y _ _____________ --'
Court Name
Judge Name
Comments
IVOTESo JL. PJH. WEK, AND JTRo ''YES"
Created By I ACORN ISH
Creation Date 11/28/2010 I
Typist_ld I ACORN ISH
Last Edit By 1 ACORN ISH
Last Edit Date 11/28/2010
0 Comments
0 Iris Exhbit
Iris Related Document I
Document Location I
In the Matter of Indoor Tanning Association
ANALYSIS OF PROPOSED CONSENT ORDER TO AID PUBLIC COMMENT
The Federal Trade Commission ("FTC" or "Commission") has accepted, subject to final
approval, an agreement containing a consent order from the Indoor Tanning Association
("respondent"). The proposed consent order has been placed on the public record for thirty (30)
days for receipt of comments by interested persons. Comments received during this period will
become part of the public record. After thirty (30) days, the Commission will again review the
agreement and the comments received, and will decide whether it should withdraw from the
agreement or make final the agreement's proposed order.
This matter involves the advertising and promotion of indoor tanning products and
facilities. According to the FTC complaint, respondent represented, in various advertisements,
that tanning, including indoor tanning, does not increase the risk of skin cancer. The complaint
alleges that this claim is false and unsubstantiated because tanning, including indoor tanning,
increases the risk of skin cancer, including squamous cell and melanoma skin cancers. Also,
according to the complaint, respondent represented that: tanning, including indoor tanning,
poses no danger; indoor tanning is approved by the government; and indoor tanning is safer than
tanning outdoors because, in indoor tanning facilities, the amount of ultraviolet light is
monitored and controlled. The FTC complaint alleges that these claims are false and
unsubstantiated.
The FTC complaint further charges that respondent represented that research shows that
vitamin D supplements may harm the body's ability to fight disease; and that a recent study in
the prestigious Proceedings of the National Academy of Sciences determined that the risks of not
getting enough ultraviolet light far outweigh the hypothetical risk of skin cancer, that getting a
healthy tan produces vitamin D, and that increased vitamin D has been linked to significantly
decreasing your risk of contracting internal cancers, such as lung, kidney, or liver cancer. The
complaint alleges that these claims are false and misleading. The FTC complaint also alleges
that respondent represented that tanning causes the skin to generate vitamin D and has health
benefits, but that respondent failed to disclose facts that would be material to consumers in their
purchase and use of indoor tanning services, specifically, that consumers can increase their
vitamin D levels through ultraviolet levels lower than the amount needed to get a tan, and that
ultraviolet radiation can injure the eyes and increases the risk of skin cancer. The complaint
alleges that respondent's failure to disclose these facts, in light of the representation made, is a
deceptive practice. Finally, the complaint alleges that respondent provided to others the means
and instrumentalities to engage in deceptive acts or practices.
The proposed consent order contains provisions designed to prevent respondent from
engaging in similar acts or practices in the future. The order covers representations made in
connection with the manufacturing, labeling, advertising, promotion, offering for sale, sale, or
distribution of any covered product or service, in or affecting commerce. It does not cover
representations made in non-commercial settings or contexts, such as communications to
legislative or executive bodies. The order defines a covered product or service as any ultraviolet
Page 1 of 3
lamp or sunlamp product, as defined in federal regulation 21 C.F.R. 1040.20, or any
commercial facility where consumers may use ultraviolet lamps or sunlamp products.
Part I of the order prohibits respondent from making the following representations:
tanning, including indoor tanning, does not increase the risk of skin cancer; tanning, including
indoor tanning, is safe or poses no danger; indoor tanning is approved by the government; and
indoor tanning is safer than tanning outdoors because in indoor tanning facilities, the amount of
ultraviolet light is monitored and controlled. The ban on representations that tanning, including
indoor tanning, is safe, is fencing-in relief. Part II of the order prohibits respondent from
misrepresenting (1) that research shows that vitamin D supplements may harm the body's ability
to fight disease and (2) that a study in the Proceedings of the National Academy of Sciences
determined: (a) that sun exposure does not cause skin cancer or melanoma, or that the risk of
such cancer is only hypothetical; (b) that getting a tan is healthy; (c) that the risks of not getting
enough ultraviolet light far outweigh the risk of skin cancer; or (d) that vitamin D has been
linked to significantly decreasing the risk of contracting lung, kidney, or liver cancer.
Part III prohibits respondent from making any representation about the safety, health-
related efficacy or performance, or health-related risks or benefits, of any covered product or
service; or about the sources, performance, efficacy, or health-related risks or benefits of vitamin
D; unless the representation is non-misleading, and, at the time it is made, respondent possesses
and relies upon competent and reliable scientific evidence that is sufficient in quality and
quantity based on standards generally accepted in the relevant scientific fields to substantiate that
the representation is true. For the purposes of the order, competent and reliable scientific
evidence is defined as tests, analyses, research, studies, or other evidence that have been
conducted and evaluated in an objective manner by qualified persons, that are generally accepted
in the profession to yield accurate and reliable results, and whose results are consistent with the
body of reliable scientific evidence relevant to the representation. Part IV of the order prohibits
respondent from misrepresenting the existence, contents, validity, results, conclusions, or
interpretations of any test, study, survey, or research.
Part V of the order is a disclosure provision. It prohibits respondent from making any
representation about the safety or health benefits of any covered product or service unless it
makes the following disclosure, clearly and conspicuously, and in close proximity to the
representation: "NOTICE: Exposure to ultraviolet radiation may increase the likelihood of
developing skin cancer and can cause serious eye injury." In the event, however, that respondent
represents that exposure to ultraviolet radiation produces vitamin Din the body, or otherwise
about the effectiveness or usefulness of such product for generation of vitamin D, the required
disclosure shall be as follows: "NOTICE: You do not need to become tan for your skin to
make vitamin D. Exposure to ultraviolet radiation may increase the likelihood of developing
skin cancer and can cause serious eye injury."
Part VI of the order prohibits respondent from providing to any other person or entity any
means or instrumentalities that contain any representation prohibited by the order. Part VII
requires respondent to send a notice about the FTC's law enforcement action to all of its
members, and all other entities to which it provided point-of-sale advertising on or after January
Page 2 of 3
1, 2008; the required notice is attached to the order as Attachment A.
Parts VIII, IX, X, and XI of the consent order require respondent to keep copies of
relevant advertisements and materials substantiating claims made in the advertisements; to
provide copies of the order to its personnel; to notify the Commission of changes in corporate
structure that might affect compliance obligations under the order; and to file compliance reports
with the Commission. Part XII provides that the order will terminate after twenty (20) years,
with certain exceptions.
The purpose of this analysis is to facilitate public comment on the proposed order, and it
is not intended to constitute an official interpretation of the agreement and proposed order or to
modify in any way their terms.
Page 3 of 3
Indoor Tanning Association. es FTC Charges That It About Ski ...
/ }t?/J;T fc;zJMS
'f//Jfo'11 &ff-1-e_
Federal Trade Commission
v Protecting America's Consumers
For Release: 01/26/2010
Page I of2
tJ /5 j7
Indoor Tanning Association Settles FTC Charges That It Deceived
Consumers About Skin Cancer Risks From Tanning
The Federal Trade Commission today charged the Indoor Tanning Association with making false health and safety claims
about indoor tanning. Contrary to claims in the association's advertising, indoor tanning increases the risk of squamous cell
and melanoma skin cancers, according to the FTC complaint. The association has agreed to a settlement that bars it from any
further deception.
"The messages promoted by the indoor tanning industry fly in the face of scientific evidence," said David C. Vladeck, Director
of the FTC's Bureau of Consumer Protection. "The industry needs to do a better job of communicating the risks of tanning to
consumers."
The Indoor Tanning Association represents tanning facilities and suppliers of tanning equipment. The FTC complaint alleges
that in March 2008, the association launched an advertising campaign designed to portray indoor tanning as safe and
beneficial. The campaign included two nati onal newspaper ads, television and video advertising, two Web sites, a
communicati ons guide, and point-of-sale materials that were provided to association members for distribution in local markets.
In addition to denying the skin cancer risks of tanning, the campaign allegedly also made these false claims:
- Indoor tanning is approved by the government;
- Indoor tanning is safer than tanning outdoors because the amount of ultraviolet light received when tanning indoors
is monitored and controlled;
- Research shows that vitamin D supplements may harm the body's ability to fight disease; and
- A National Academy of Sciences study determined that "the risks of not getting enough ultraviolet light far outweigh
the hypothetical risk of skin cancer.
The complaint also alleges that the association failed to disclose material facts in its advertising.
Under its settlement with the Commission, the association is prohibited from making the
misrepresentations challenged in the complaint, from misrepresenting any tests or studies, and from providing deceptive
advertisements to members. The settlement also requi res that future association ads that make safety or health benefits
claims for indoor tanning may not be misleading and must be substantiated. Further, the order requires that certain future
adverti sements from the associati on contain disclosures. Ads that make claims about the safety or health benefits of indoor
tanning are required to clearly and prominentl y make this disclosure:
"NOTICE: Exposure to ultraviolet radiation may increase the li kelihood of developing skin cancer and can cause serious eye
injury."
Ads that claim exposure to ultraviolet radiation produces vitamin Din the body, or make other claims about the effectiveness
or usefulness of indoor tanning products or services for the body's generation of vitamin D, must clearly and prominently make
this disclosure:
"NOTICE: You do not need to become tan for your skin to make vitamin D. Exposure to ultraviolet radiation may increase the
likelihood of developing skin cancer and can cause serious eye injury."
For more information about how indoor or outdoor tanning increases the risk of melanoma and other types of skin cancer, read
the FTC Consumer Alert Indoor Tanning at http://www.ftc.gov/bcp/edu/pubs/consumer/alerts/alt174.pdf
The Commission vote to approve the administrative complaint and proposed consent agreement was 4-0. The FTC will publish
an announcement regarding the agreement in the Federal Register shortly. The agreement will be subject to public comment
for 30 days, beginning today and continuing through February 26, 2010, after which the Commission will decide whether to
http://www.ftc.gov/opa/2010/01/tanning.shtm 2/ 1/2010
Indoor Tanning Association.tles FTC Charges That It Deceived C.mers About Ski ...
make it final. To fil e a public comment, please click on the following hyperlink:
https://public.commentworks.com/ftc/indoortanningassoc and follow the instructions at that site.
Copies of the complaint, the proposed consent agreement, and an analysis of the
Page 2 of2
agreement to aid in public comment are available from both the FTC's Web site at http://www.ftc.gov and the FTC's Consumer
Response Center, Room 130, 600 Pennsylvania Avenue, N.W. , Washington, DC 20580.
NOTE: The Commission files a complaint when it has "reason to believe" that the law has been or is being violated, and it
appears to the Commission that a proceeding is in the public interest. A consent agreement is for settl ement purposes only
and does not constitute an admission of a law violation. When the Commission issues a consent order on a final basis, it
carries the force of law with respect to future actions. Each violation of such an order may result in a civil penalty of up to
$16,000.
The Federal Trade Commission works for consumers to prevent fraudulent, deceptive, and unfai r business practices and to
provide information to help spot, stop, and avoid them. To fil e a complaint in English or Spanish, visit the FTC' s online
Complaint Assistant or call 1-877-FTC-HELP (1-877-382-4357). The FTC enters complaints into Consumer Sentinel, a secure,
online database available to more than 1,700 civil and criminal law enforcement agencies in the U.S. and abroad. The FTC's
Web site provides free information on a variety of consumer topics.
MEDIA CONTACT:
Betsy Lordan
Office of Public Affairs
202-326-3707
STAFF CONTACT:
Janet Evans
Bureau of Consumer Protection
202-326-2125
(FTC File No. 0823159)
(Indoor Tanning.wpd)
E-mai l thi s News Release
If you send this link to someone else, the FTC will not collect any personal information about you or the recipient.
Related Items :
I
In the Matter of Indoor Tanning Association, a corporation
FTC File No. 082 3159
Consumer Information:
Indoor Tanning
Last Modified: Tuesday, January 26, 201 0
http://www.ftc.gov/opa/201 0/01/tanning.shtm 2/1/2010
~ ~ ~
NOTICE OF EXPIRATION OF COMMENT PERIOD
TO
~ COMMISSION COUNSEL
D MINUTES BRANCH
OSCAR DOC. NUMBER
1 546672
TITLE
FROM
DOCUMENT PROCESSING
SECTION
RECORDS AND FILING OFFICE
DATE: [ o 2 / 2 6/ l o
FILE/DOCKET NO.
1 1 0823159
I PART 2 CONSENT AGREEMENT DOCUMENTS WHEN CONSENT AGREEMENT I S ACCEPTED FOR PUBLI C RECORD I
MATIERNAME
j Indoor Tanning Association
Agreement, complaint (if Part 2) and staff analysis of File noted above have been on the public record
for j_ 3 days .
Comments were received in the Document Processing Section. The file is being sent to you for
preparation of a response letter to each commentator and for submission to the Commission in
accordance with Operating Manual 6.13.3.2.
D
D
D
D
D
Agreement, complaint (if Part 2) and staff analysis of File noted above have been on the public record
for I _____ ] days.
No paper or electroni c Comments were received in the Document Processing Section. The file is
forwarded for Non-Agenda circulation for its final decision with the recommendation that the
Commission issue the complaint (if Part 2) and the decision and order.
Request to reopen the above noted File has been on the public record for 30 days from the date of
the Press Release. Comments were received and placed on the public record.
In accordance with OM Chapter 12.8.3.2., a reply to each letter must be prepared.
Request to reopen the above noted File has been on the public record for 30 days from the date the
Press Release issued.
No paper or electronic Comments have been received in the Document Processing Section.
Application to acquire/divest in the above noted File has been on the public record for 30 days from
the date of the Press Release. Comments were received and placed on the public record.
Application to acquire/divest in the above noted File has been on the public record for 30 days from
the date of the Press Release. No paper or electronic comments were received in the Document
Processing Section.
CC 0 Minutes Branch
:_] Commission Counsel
D Bureau Director
~ Assistant Director
FTC Form 140 (rev. 8/06)
Prepared by Berni t a Lofty
UNITED STATES OF AMERICA
FEDERAL TRADE COMMISSION
In the Matter of )
)
INDOOR TANNING ASSOCIATION, )
a corporation. )
File No. 082-3159
AGREEMENT CONTAINING
CONSENT ORDER
The Federal Trade Commission has conducted an investigation of certain acts and
practices of Indoor Tanning Association ("proposed respondent"). Proposed respondent, having
been represented by counsel, is willing to enter into an agreement containing a consent order
resolving the allegations contained in the attached draft complaint. Therefore,
IT IS HEREBY AGREED by and between Indoor Tanning Association and counsel for
the Federal Trade Commission that:
1. Proposed respondent Indoor Tanning Association is a Massachusetts corporation with its
principal office or place of business at 2025 M Street, N.W., Washington, D.C. 20036.
2. Proposed respondent admits all the jurisdictional facts set forth in the draft complaint.
3. Proposed respondent waives:
A. Any further procedural steps;
B. The requirement that the Commission's decision contain a statement of findings
of fact and conclusions of law; and
C. All rights to seek judicial review or otherwise to challenge or contest the validity
of the order entered pursuant to this agreement.
4. This agreement shall not become part of the public record of the proceeding unless and
until it is accepted by the Commission. If this agreement is accepted by the Commission, it,
together with the draft complaint, will be placed on the public record for a period of thirty (30)
days and information about it publicly released. The Commission thereafter may either
withdraw its acceptance of this agreement and so notify proposed respondent, in which event it
will take such action as it may consider appropriate, or issue and serve its complaint (in such
form as the circumstances may require) and decision in disposition of the proceeding.
5. This agreement is for settlement purposes only and does not constitute an admission by
proposed respondent that the law has been violated as alleged in the draft complaint, or that the
Page 1 of 9
facts as alleged in the draft complaint, other than the jurisdictional facts, are true.
6. This agreement contemplates that, if it is accepted by the Commission, and if such
acceptance is not subsequently withdrawn by the Commission pursuant to the provisions of
Section 2.34 of the Commission's Rules, the Commission may, without further notice to
proposed respondent, (1) issue its complaint corresponding in form and substance with the
attached draft complaint and its decision containing the following order in disposition of the
proceeding, and (2) make information about it public. When so entered, the order shall have the
same force and effect and may be altered, modified, or set aside in the same manner and within
the same time provided by statute for other orders. The order shall become final upon service.
Delivery of the complaint and the decision and order to proposed respondent's address as stated
in this agreement by any means specified in Section 4.4(a) of the Commission's Rules shall
constitute service. Proposed respondent waives any right it may have to any other manner of
service. The complaint may be used in construing the terms of the order, and no agreement,
understanding, representation, or interpretation not contained in the order or the agreement may
be used to vary or contradict the terms of the order .
7. Proposed respondent has read the draft complaint and consent order. It understands that
it may be liable for civil penalties in the amount provided by law and other appropriate relief for
each violation of the order after it becomes final.
ORDER
DEFINITIONS
For the purposes of this order, the following definitions shall apply:
1. Unless otherwise specified, "respondent" shall mean Indoor Tanning Association,
its successors and assigns, its officers when acting in active concert or
participation with Indoor Tanning Association, and its executive director .
2. "Covered product or service" shall mean any ultraviolet lamp or sunlamp product,
as defined in 21 C.F.R. 1040.20; and any commercial facility where consumers
may use ultraviolet lamps or sunlamp products.
3. "Clearly and conspicuously" means:
a. In print communications, the disclosure shall be presented in a manner
that stands out from the accompanying text, so that it is sufficiently prominent,
because of its type size, contrast, location, or other characteristics, for an ordinary
consumer to notice, read and comprehend it;
b. In communications made through an electronic medium (such as
television, video, radio, and interactive media such as the Internet, online
services, and software), the disclosure shall be presented simu1taneously in both
Page 2 of 9
the audio and visual portions of the communication. In any communication
presented solely through visual or audio means, the disclosure shall be made
through the same means through which the communication is presented. In any
communication disseminated by means of an interactive electronic medium such
as software, the Internet, or online services, the disclosure must be unavoidable.
Any audio disclosure shall be delivered in a volume and cadence sufficient for an
ordinary consumer to hear and comprehend it. Any visual disclosure shall be
presented in a manner that stands out in the context in which it is presented, so
that it is sufficiently prominent, due to its size and shade, contrast to the
background against which it appears, the length of time it appears on the screen,
and its location, for an ordinary consumer to notice, read and comprehend it; and
c. Regardless of the medium used to disseminate it, the disclosure shall be in
understandable language and syntax. Nothing contrary to, inconsistent with, or in
mitigation of the disclosure shall be used in any communication.
4. "Close proximity" means on the same print page, web page, online service page,
or other electronic page, and proximate to the triggering representation, and not
accessed or displayed through hyperlinks, pop-ups, interstitials, or other means.
5. "Commerce" shall mean as defined in Section 4 of the Federal Trade Commission
Act, 15 U.S.C. 44.
I.
IT IS HEREBY ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not represent, in any manner,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, that:
A. Tanning, including indoor tanning, does not increase the risk of skin cancer;
B. Tanning, including indoor tanning, is safe or poses no danger;
C. Indoor tanning is approved by the government; and
D. Indoor tanning is safer than tanning outdoors because in indoor tanning facilities,
the amount of ultraviolet light is monitored and controlled.
II.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
Page 3 of 9
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not misrepresent, in any manner,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, that:
A. Research shows that vitamin D supplements may harm the body's ability to fight
disease; and
B. A study in the Proceedings of the National Academy of Sciences determined: (a)
that sun exposure does not cause skin cancer or melanoma, or that the risk of such
cancer is only hypothetical; (b) that getting a tan is healthy; (c) that the risks of
not getting enough ultraviolet light far outweigh the risk of skin cancer; or (d) that
vitamin D has been linked to significantly decreasing the risk of contracting lung,
kidney, or liver cancer.
III.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not make any representation,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, about the safety, health-related efficacy or performance, or health-
related risks or benefits, of any covered product or service; or about the sources, performance,
efficacy, or health-related risks or benefits of vitamin D; unless the representation is non-
misleading, and, at the time it is made, respondent possesses and relies upon competent and
reliable scientific evidence that is sufficient in quality and quantity based on standards generally
accepted in the relevant scientific fields to substantiate that the representation is true. For the
purposes of this order, competent and reliable scientific evidence shall consist of tests, analyses,
research, studies, or other evidence that have been conducted and evaluated in an objective
manner by qualified persons, that are generally accepted in the profession to yield accurate and
reliable results, and whose results are consistent with the body of reliable scientific evidence
relevant to the representation.
IV.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not misrepresent, in any manner,
expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, the existence, contents, validity, results, conclusions, or interpretations
of any test, study, survey, or research.
Page 4 of 9
V.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not make any representation, in any
manner, expressly or by implication, including through the use of a product name, endorsement,
depiction, or illustration, about the safety or health benefits of any covered product or service
unless it discloses, clearly and conspicuously, and within close proximity to that representation:
NOTICE: Exposure to ultraviolet radiation may increase the likelihood of developing
skin cancer and can cause serious eye injury.
Provided that, in lieu of the above, in the event that advertising for any covered product or
service makes any representation, expressly or by implication, including through the use of a
product name, endorsement, depiction, or illustration, that exposure to ultraviolet radiation
produces vitamin D in the body, or otherwise about the effectiveness or usefulness of such
product for generation of vitamin D, the required disclosure shall be as follows :
NOTICE: You do not need to become tan for your skin to make vitamin D. Exposure
to ultraviolet radiation may increase the likelihood of developing skin cancer and can
cause serious eye injury.
VI.
IT IS FURTHER ORDERED that respondent, directly or through any corporation,
partnership, subsidiary, division, trade name, or other device, in connection with the
manufacturing, labeling, advertising, promotion, offering for sale, sale, or distribution of any
covered product or service, in or affecting commerce, shall not provide to any other person or
entity any means or instrumentalities that contain any representation or omission prohibited by
this order. For the purposes of this Part, "means or instrumentalities" shall mean any
information, including but not necessarily limited to any advertising, labeling, communications
guides, or other promotional material.
VII.
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall send as soon as practicable, but in no event later than thirty (30)
days after entry of this order, by first-class mail, postage prepaid and return receipt requested, an
exact copy of the notice attached hereto as Attachment A, showing the date of mailing, to all
Indoor Tanning Association members and all other entities to which Indoor Tanning Association
provided point-of-sale advertising on or after January 1, 2008. The notice required by this
paragraph shall not include any other document or enclosures and may be sent to the principal
place of business of each entity.
Page 5 of 9
vm.
IT IS FURTHER ORDERED that, for a period of five (5) years after the last date of
dissemination of any representation covered by this order, respondent Indoor Tanning
Association and its successors and assigns shall maintain and upon request make avai lable to the
Federal Trade Commission for inspection and copying:
A. All advertisements and promotional materials containing the representation;
B. All materials that were relied upon in disseminating the representation; and
C. All tests, reports, studies, demonstrations, or other evidence in its possession or
control that contradict, qualify, or call into question such representation, or the
basis relied upon for the representation, including complaints and other
communications with consumers or with governmental or consumer protection
organizations.
IX.
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall deliver a copy of this order to all current and future principals,
officers, directors, and other employees with managerial authority having responsibilities with
respect to the subject matter of this order, and shall secure from each such person a signed and
dated statement acknowledging receipt of the order. Respondent shall deliver this order to
current personnel within thirty (30) days after the date of service of this order, and to future
personnel within thirty (30) days after the person assumes such position or responsibilities.
X .
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall notify the Commission at least thirty (30) days prior to any change
in the corporation that may affect compliance obligations arising under this order, including but
not limited to a dissolution, assignment, sale, merger, or other action that would result in the
emergence of a successor corporation; the creation or dissolution of a subsidiary, parent, or
affiliate that engages in any acts or practices subject to this order; the proposed filing of a
bankruptcy petition; or a change in the corporate name or address. Provided, however, that, with
respect to any proposed change in the corporation about which respondent learns less than thirty
(30) days prior to the date such action is to take place, respondent shall notify the Commission as
soon as is practicable after obtaining such knowledge. All notices required by this Part shall be
sent by certified mail to the Associate Director, Division of Enforcement, Bureau of Consumer
Protection, Federal Trade Commission, Washington, D.C. 20580.
Page 6 of 9
XI.
IT IS FURTHER ORDERED that respondent Indoor Tanning Association and its
successors and assigns shall, within sixty ( 60) days after the date of service of this order file with
the Commission a true and accurate report, in writing, setting forth in detail the manner and form
in which respondent has complied with this order. Within ten ( 1 0) days of receipt of written
notice from a representative of the Commission, respondent shall submit additional true and
accurate written reports.
XII.
'
This order will terminate twenty (20) years from the date of its issuance, or twenty (20)
years from the most recent date that the United States or the Federal Trade Commission files a
complaint (with or without an accompanying consent decree) in federal court alleging any
violation of the order, whichever comes later; provided, however, that the filing of such a
complaint will not affect the duration of:
A. Any Paragraph in this order that terminates in less than twenty (20) years; and
B. This order's application to any respondent that is not named as a defendant in
such complaint; and
C. This order if such complaint is filed after the order has terminated pursuant to this
Paragraph.
Page 7 of 9
Provided, further, that if such complaint is dismissed or a federal court rules that the
respondent did not violate any provision of the order, and the dismissal or ruling is either not
appealed or upheld on appeal, then the order will terminate according to this Part as though the
complaint had never been filed, except that the order will not terminate between the date such
complaint is filed and the later of the deadline for appealing such dismissal or ruling and the date
such dismissal or ruling is upheld on appeal.
Signed this 'l \ day of (je_ C...
'2009.
---- ........
irector
Division of Advertising Practices
DAVID VLADECK
Director
Bureau of Consumer Protection
G ASSOCIATION
ON
Counsel for Respondent Indoor Tanning Association
Division of Advertising Practices
Page 8 of 9
ATIACHMENT A
[ON INDOOR TANNING ASSOCIATION LETTERHEAD]
IMPORTANT NOTICE ABOUT GOVERNMENT ACTION
[insert addressee name]
[insert addressee address]
Dear IT A Member or Affiliate:
In a recent lawsuit, the Federal Trade Commission (FTC) charged the Indoor Tanning
Association (ITA) with making misleading representations in its advertising and marketing for
indoor tanning. Among other things, the FTC alleged that IT A falsely claimed that indoor
tanning poses no risk to health, including no risk of skin cancer. In addition, the FTC alleged
than when ITA represented that indoor tanning caused the skin to generate vitamin D, IT A failed
to disclose material facts about the risks of indoor tanning. IT A has agreed to send this
notification to you as part of its settlement with the FTC.
IT A hereby requests that you immediately cease using all advertising and marketing
materials previously provided by to you by IT A. Among the materials you should no longer use
are all of the materials contained on the CD-ROM issued in 2008, including the following:
A. The "Melanoma Hype" print ad
B. The "Overdose of Hysteria" video
C. The "Communications: The Basics" guide and
D. The print ad with the tag line, "Time to rethink sun tanning?"
The FTC complaint alleges that these ads contain representations that are false and/or
misleading.
For further information about the FTC's complaint and order, go to www.ftc.gov and
search "Indoor Tanning Association."
Very truly yours,
John Overstreet
Executive Director
Page 9 of 9
UNITED STATES OF AMERICA
FEDERAL TRADE COMMISSION
COMMISSIONERS: Jon Leibowitz, Chairman
Pamela Jones Harbour
William E. Kovacic
J. Thomas Rosch
In the Matter of )
)
INDOOR TANNING ASSOCIATION, )
)
a corporation )
DOCKET NO. C-
COMPLAINT
082-3159
The Federal Trade Commission, having reason to believe that Indoor Tanning
Association, a corporation ("respondent"), has violated the Federal Trade Commission Act, and
it appearing to the Commission that .this proceeding is in the public interest, alleges:
1. Respondent Indoor Tanning Association ("ITA") is a Massachusetts corporation with its
principal place of business at 2025 M St., N.W., Washington, D.C. 20036. ITA is registered as a
nonprofit entity under Section 50l(c)(6) of the Internal Revenue Code. Its members include
indoor tanning manufacturers, distributors, facility owners, and representatives of other
supporting industries. ITA's purpose is to "advance the business growth and image of the indoor
tanning industry, and the welfare of its membership."
2. Respondent has advertised and promoted to the public the use of ultraviolet lamps and
sunlamp products, as defined in 21 C.F.R. 1040.20, and commercial indoor tanning facilities
where consumers may use ultraviolet lamps or sunlamp products. Ultraviolet lamps and
sunlamp products are "devices" within the meaning of Sections 12 and 15 of the Federal Trade
Commission Act.
3. The acts and practices of respondent, as alleged herein, have been in or affecting
commerce, as "commerce" is defined in Section 4 of the Federal Trade Commission Act.
4. As part of a coordinated campaign to promote ultraviolet lamps and sunlamp products
and indoor tanning, respondent created, prepared, disseminated, or caused to be disseminated
advertisements, including the attached Exhibits A through G. These advertisements contain the
following representations or statements, among others:
------------------------------------- ---- ---- ---- -----------------------------------
a. TANNING CAUSES MELANOMA HYPE
b.
Recent research indicates that the benefits of moderate exposure to sunlight
outweigh the hypothetical risks. Surprisingly, there is no compelling scientific
evidence that tanning causes melanoma. Scientists have proven, however, that
exposure to all forms of ultraviolet light - both indoors and out - stimulates the
natural production of vitamin D. And research has proven that vitamin D protects
against heart disease and many types of cancer, in addition to other important
health benefits.
It's time to rethink sunbathing.
Find out more at www.SunlightScam.com.
A message brought to you by the Indoor Tanning Association
- Exhibit A, newspaper advertisement and point-of-sale poster art
provided to IT A members
* * *
There are a lot of misconceptions about sunlight. After hearing relentless
campaigns telling us to lather on the sunscreen, many Americans have been led to
believe that ultra violet [sic] (UV) light - whether it comes from the sun or from a
tanning salon- is something to be feared, rather than cherished.
The reality is that UV light provides us with countless health benefits- both
physiological and psychological. And the rewards of "soaking up the sun" even
outweigh the risks of overexposure. Though there are various ways of getting the
recommended amount, such as mowing the lawn or lying by the pool, safe,
moderate tanning is the best way to maximize these benefits while minimizing any
risks.
*
* *
Melanoma Misinformation.
* * *
Getting a regular amount of sunlight is healthy, whether it's outdoors or in a sun
bed:--Moderate exposme to UV light benefits people with vitamin D deficiency
and makes people feel good. However, a great deal of misinformation has been
spread about the link between Melanoma and any amount [sic] UV exposure.
The truth may surprise you:
Sunburns, not sun tans are linked to melanoma
Melanoma is most common among those who work indoors, not
outside
Melanoma appears most commonly on body parts not regularly
exposed to sun
2
Safe, moderate exposure does not increase risk of melanoma skin cancer. And
tanning indoors is even safer because, unlike exposure to the sun, the environment
is controlled. In fact, the anti-cancer benefits of UV exposure highlighted be [sic]
recent studies far outweigh the risks associated with over-exposure.
- Exhibit B, website, http://www.trusttanning.com
c. Get the Facts About Tanning
* * *
SCAM: Getting a tan is dangerous
TRUTH: There is nothing dangerous about getting a tan. In fact, your body
needs ultraviolet light to live. And now, new research is unlocking the secrets of
vitamin D, which is naturally produced by skin when it is exposed to siJ.Il].ight or
indoor tanning lights. Earlier this year the London Telegraph reported:
Last week, a report in the prestigious US journal Proceedings of the
National Academy of Sciences revealed that people with higher levels [of
vitamin D] were more likely to survive colon, breast and lung cancer
The Proceedings of the National Academy of Sciences study determined that the
risks associated with not getting enough sun far outweighed any hypothetical
damage that might occur.
While a healthy tan poses no significant risks of damaging your skin, burning your
skin can be dangerous. For that reason, indoor tanning - where the amount ofUV
light you receive is monitored - is considered by many to be a safer alternative to
tanning outdoors.
* * *
SCAM: Every ray ofUV light from a tanning bed increases your risk of
contracting melanoma skin cancer
TRUTH:
* * *
A recent study in the prestigious Proceedings of the National Academy of Sciences
determined that the risks of not getting enough UV light far outweighed the
hypothetically minute risk of skin cancer. That's because getting a healthy tan
naturally produces vitamin D, which has been linked to significantly decreasing
your risk of contracting internal cancers like lung, kidney, or liver cancer.
While getting too much sun has been linked to some forms of cancer, indoor
tanning is a government-approved, controlled environment designed to give you a
tan without ever burning - which is the likely culprit in contracting cancer from
sun exposure.
* * *
3
e.
SCAM: Indoor tanning is more dangerous than tanning in the sun
TRUTH: Just the opposite is true. Unlike tanning outdoors, indoor tanning is
designed to match your skin type and desired tan in a well-regulated, controlled
environment. Consequently, the vast bulk of scientific research indicates that
indoor tanning is a safer alternative to tanning outdoors.
- Exhibit C, website, www.sunlightscam.com.
d. The fear of getting a tan has gone too far. Dermatologists with the sunscreen and
cosmetic industries are trying to scare us away from the sun. But tanning produces
vitamin D, and research shows vitamin D may fight heart disease, breast cancer,
stroke, and osteoporosis. So go get a tan, your body will thank you.
[on screen: Vitamin D Fights Heart Disease Breast Cancer Stroke Osteoporosis]
Bought to you by The Indoor Tanning Association .
- Exhibit D I, Transcript, television and website advertisement and
Exhibit E, DVD containing video of same
[on screen: www.SunLightScam.com]
The fear of getting a tan has gone too far. Dermatologists with the sunscreen and
cosmetic industries are trying to scare us away from the sun. But tanning produces
vitamin D, and research shows vitamin D may fight heart disease, breast cancer,
stroke, and osteoporosis. So go get a tan, your body will thank you.
[on screen: www.SunLightScam.com]
[on screen: Vitamin D Fights Heart Disease Breast Cancer Stroke Osteoporosis]
Bought to you by The Indoor Tanning Association.
* *
- Exhibit D2, Transcript, television and website advertisement and
Exhibit E, DVD containing video of same
*
By practicing what you find in this book, you will more effectively communicate
your message, build your image, and motivate desired behavior.
* * *
ARGUMENT 1- VITAMIN DIS GOOD (VITAMIN DIS THE "SUNSHINE
VITAMIN"):
* * *
It is impossible to get the requisite amount of vitamin D in cities north of
4
f.
*
37 degrees for as many as 6 months out of the year ...
Vitamin D isn't like other vitamins that you can easily ingest as part of
your diet. It is best absorbed through the skin from exposure to UV light.
New research indicates that supplement-based vitamin D, as opposed to
vitamin D naturally produced through exposure to UV light, may actually
harm the body's ability to fight disease.
* *
ARGUMENT 3- TANNING IN MODERATION IS BENEFICIAL:
*
*
*
- Indoor tanning in moderation is safer than exposure to the sun, because the
envirorunent is controlled.
- Unlike the sun, tanning is well regulated and approved by the goverrunent. When
used moderately and responsibly, tanning sessions are designed to prevent
burning.
- Exhibit F, IT A "Communications: the basics" guide provided to
ITA members
Enjoy the sun on doctor's orders
Solar rays can help protect against some cancers and heart disease, say scientists
- The Guardian, January 8, 2008
As Vitamins Go, D, You Are My Sunshine
Just 20 minutes of sun exposure without sunscreen enables the skin to produce
20, 000 IU of vitamin D
- The Washington Post, September 18, 2007
Sunshine prevents more deaths than it causes;
Sunshine has a protective effect overall because it helps to create vitamin D
- New Scientist, January 12, 2008
* * *
Time to rethink sun tanning?
For more information visit www. TrustTanning. com
Dermatologists and the sunscreen industry have spent millions on a deceptive
campaign to scare Americans away from the sun. Now the tide of research is
turning the other direction. The positive effects of getting vitamin D from sunlight
are clear. So soak up a little sunlight - indoors or out- a couple of times, each
week, and get your recommended dose of the "sunshine vitamin."
Paid for by the Indoor Tanning Association
-Exhibit G, newspaper advertisement and point-of-sale poster art
provided to IT A members
5
5. Through the means described in Paragraph 4, respondent has represented, expressly or by
implication, that:
A. Tanning, including indoor tanning, does not increase the risk of skin cancer;
B. Tanning, including indoor tanning, poses no danger;
C. Indoor tanning is approved by the government; and
D. Indoor tanning is safer than tanning outdoors because, in indoor tanning facilities,
the amount of ultraviolet light is monitored and controlled.
6. In truth and in fact:
A.
B.
C.
D.
Tanning, including indoor tanning, increases the risk of skin cancer, including
squamous cell and melanoma skin cancers;
Tanning, including indoor tanning, poses danger;
Indoor tanning is not approved by the government; and
Indoor tanning is not safer than tanning outdoors because the amount of
ultraviolet light received when tanning indoors is neither monitored nor
controlled sufficiently to prevent the health risks associated with ultraviolet
exposure.
Therefore, the representations set forth in paragraph 5 were, and are, false and misleading.
7. Through the means described in Paragraph 4, respondent has represented, expressly or by
implication, that it relied on a reasonable basis that substantiated the representations set forth in
Paragraph 5, at the time the representations were made.
8. In truth and in fact, respondent did not possess and rely upon a reasonable basis that
substantiated the representations set forth in Paragraph 5, at the time the representations were
made. Therefore, the representation set forth in paragraph 7 was, and is, false and misleading .
9. Through the means described in Paragraph 4, respondent has represented, express!y or by
implication, that:
A. Research shows that vitamin D supplements may harm the body's ability to fight
disease; and
B. A recent study in the prestigious Proceedings of the National Academy of
Sciences determined that the risks of not getting enough ultraviolet light far
outweigh the hypothetical risk of skin cancer, that getting a healthy tan produces
vitamin D, and that increased vitamin D has been linked to significantly
decreasing your risk of contracting internal cancers, such as lung, kidney, or liver
cancer.
6
10. In truth and in fact:
A. Research has not shown that vitamin D supplements may harm the body's ability
to fight disease; and
B. The study in the Proceedings of the National Academy of Sciences referenced by
respondent did not determine that the risk of getting skin cancer from ultraviolet
light is only hypothetical, that the risks of not getting enough ultraviolet light far
outweigh the risk of skin cancer, that getting a tan is healthy, or that increased
vitamin D has been linked to significantly decreasing the risk of contracting
internal cancers, such as lung, kidney, or liver cancer.
Therefore, the representations set forth in paragraph 9 were, and are, false and misleading.
11 . Through the means described in paragraph 4, respondent has represented that tanning
causes the skin to generate vitamin D and has health benefits. Respondent has failed to disclose
that consumers can increase their vitamin D levels through ultraviolet exposure levels lower than
the amount needed to get a tan, and that ultraviolet radiation can injure the eyes and increases the
risk of skin cancer. These facts would be material to consumers in their purchase or use of
indoor tanning services. The failure to disclose these facts, in light of the representation made,
was, and is, a deceptive practice.
12. Through the means described in Paragraph 4, respondent has provided to others the
means and instrumentalities to engage in deceptive acts or practices.
13. The acts and practices of respondent as alleged in this complaint constitute unfair or
deceptive acts or practices, and the making of false advertisements, in or affecting commerce in
violation of Section 5(a) and 12 of the Federal Trade Commission Act.
THEREFORE, the Federal Trade Commission this __ day of _ _ _ _ , has
issued this complaint against respondent.
By the Commission.
SEAL:
DonaldS. Clark
Secretary
7
e
e
Recent research indicates that the benefits of moderate exposure to sunlight outweigh
the hypothetical risks. Surprisingly, there is no compelling scientific evidence that
tanning causes melanoma. Scientists have proven. however, that exposure to all
forms of ultraviolet tight-both Indoors and out-stimulates the natural production of
vitamin D. And research has proven that vitamin D protects against heart disease and
many types of cancer, in addition to other important health benefits.
It's time to rethink sun bathing.
Find out more at
www.SunlightScam.com
A m ~ S a g ~ b,.,ught to you by tht Indoor 7iznning AJtot'iation
Exhibit A
.. , : '
. . .
. , i:;_ . .: . " ..... ' ..... i ..
; t.. .... =:: /: :' .. , . \ : ... . r .
, __ . _ _1,- ___ ,
.;
., . ;
Life on our planet needs sunlight to survive. And humans
are no exception. Unlike plants and animals that daily
struggle to stay in the light, we actively work to avoid
the sun.
There are a lot of misconceptions about sunlight. After
hearing relentless campaigns telling us to lather on the
sunscreen, many Americans have been led to believe
that ultra violet (UV) light-whether it comes from the
sun or from a tanning salon-is something to be feared,
rather than cherished. Until now, hope for a balanced
message in the public debate on this issue seemed to be
lost.
The reality is that UV light provides us with countless
health benefits-both physiological and psychological.
Page l of I
... .
And the rewards of "soaking up the sun" even outweigh t he risks of overexposure. Though there are various
methods of getting the recommend amount, such as mowing the lawn or lying by the pool, safe, moderate
tanning is the best way to maximize these benefits while minimizing any risks.
TrustTanning.com is devoted to answering the most frequently asked questions about tanning and
debunking some of the most pervasive myths .
http://www. trusttanning.cornl
Exhibit B, p. l :
- - - --- - - - - - - - -- - -
e
. -- --- -- - ~ .......... ""''. "'"""'!:>"''-""
-..
\ . f ..... i - ~ ..... _ .. ..., ~ .
:
1
I ! tJ .i ; ~ ' ! ". ~
. ,., . ...-.l . , #., ... t . . . . ; ; . . : . _ ~
"These data, together with those for Internal cancers
and the beneficial effects of an optimal vitamin D
status, indicate that increased sun exposure may
lead to improved cancer prognosis and, possibly,
give more positive than adverse health effects. "
-Proceedings from the National Academies of Science
2008
Getting a regular amount of sunlight is healt hy, whether
it 's outdoors or in a sun bed. Moderate exposure to UV
light benefits people with vitamin D deficiency and makes
people feel good. However , a great deal of misinformation
has been spread about the link between Melanoma and
any amount UV exposure.
The truth may surprise you :
Sunburns, not sun tans are linked to melanoma
Melanoma is most common among those who work
indoors, not outside
... _ .. _.
1
j
"':
.. . . -....
Melanoma appears most commonly on body parts not regularly exposed t o sun
Page 1 ot I
Safe, moderate exposure does not increase risk of melanoma skin cancer. And tanning indoors is even safer,
because unlike exposure to the sun, the environment is controlled. In fact, the anti -cancer benefits of UV
exposure highlighted be recent studies far outweigh t he risks associated wi th over -exposure.
Exhibit B, p. 2
hup:l/\vww.trusttanning.com/skinCancerMisinformation.htm
111312009
e
,.._. u '-'"""'e u ut 1.:> '.IVLI.:>- ..
Page 1 ot 2
;->c <1 ms. J<l!llli.ng
Blowback
1\bQ!!l.Us
Get the Facts about Tanning
The Sunscam Industry has spent millions of dollars scaring Americans out of the sun in an effort to sell
more sunscreen. But before you believe the sunscreen wmpanies. get the facts about UV light and
tanning.
Getting a tan is dangerous
Tanniog an .Q[
Every...rny of UV light from a tanning bed.increases your risk of .skill cancer
T.:uming beds are 15 times strlmger the S\_ln
is no such_ thing as a
You can get enough Yitamin D through supplements or drinking milk
gs<tt!D.g
lndQQ...I. tanning is more sun
... r, j\ "I
.
Gett ing a tan is dangerous
fRUfH:
There is nothing dangerous about getting a tan. In fact, your body needs ultraviolet li ght to live. And
now. new research is unlocking the secrets of vitamin D. which is naturally produced by skin when it is
exposed to sunlight or indoor tanning lights. Earlier this year the London Telegraph reported:
Last "veek. a report in the prestigious US journal Proceedings of the National Academy of
Sciences revealed that people with hi gher levels (of vitamin 01 were more likely to survive
colon. breast and lung cancer. This follows last year's University of San Diego review of 40
years of research, which revealed that a daily dose could halve the risk of breast and bowel
cancer.
Other claims are that it reduces the risk of heart disease (a study of 10,000 women in
Cali fornia lound that those who took supplements had a 31 per cent lower risk of dying
http:l/www. sunlightscam.com/scam l.html
Exhibit C, p. I
I l l .V::Wo9
Page Lot l.
from it), diabetes (in a Finnish study of 12.000 children, it cut their chance of developing
Type A diabetes by 80 pa even colds and flu (New Yorkers who took vitamin D had
11u 70 per cent less often).
The Proceedings of the Nat ional Academy of Sciences study determined that the risks associated with
not getting enough sun far outweighed any hypothetical damage that might occur.
White a healthy tan poses no signiticant risks of damaging your skin, burning your skin can be
dangerous. For that reason. indoor tanning- \vhere the amount of UV light you receive is monitored-is
considered by many to be a safer ahernati ve to tanning outdoors.
:W08 The Indoor Tanning Association
Exhibit C, p. 2
http:/ /www.sunlightscam.com/scam l.html
I I I
- .... .... .... -. -.;
t'age t ot !.
Fqrsid.:
:iW.1." ..
..l!l .. [qnni_tlg
131owback
.:1 tan i;; Jang ....rous
has quseJ an epidemic of cancer
Every ray of UV light from a tanning bed increases your risk of contracting melanoma skin
cancer
beds we 15 rimes stronger than the sun
i.::>_ !W <1 b tao.
Y Vit<uniJl D .. !h...rm.!gh .. Q..U.Iri.!!king mi.!.k
Joesn't protect ypu fron1 get_ting a pq_rn on
lnJQor ranning than tanning..ill tbJ!_;iun
Every ray of UV light from a tanning bed increases your risk of contracting melanoma ski n cancer
ftUJfH:
So careful sunbathing, with measmed exposure to the sun, may actually reduce rather than increase the
ri sk of mdanoma, reduce the overall risk of deat h from skin cancer, and improve survival for those who
develop melanoma.
- OG. )Q1Jf11al
The -c word is scary .. Nobody knows that more than the billion-dollar sunscreen industry. which has
:>ystematically attempted to link sun exposure to cancer in an effort to deceptively scare people into
buying their products. But despite their best efforts to link tanning to melanoma, no clear link exists. In
fact. more than 18 separate peer-reviewed scientific studies indicate that there is no link between tanni ng
indoors and melanoma.
That should put the debate about tanning and cancer to rest, but the sunscreen industry knows that the
fear of cancer is the Jriving force selling their product. As a resuJt. they have taken to quie1y fundi ng
front groups with deceptive names like the Skin Cancer Foundation and the Sun Safety Alliance to keep
the myth of tanning and cancer planted in the minds of the media and. ultimatel y. their consumers.
Ironically. (may require logi n) indicates that sunscreen does nothing tn protect
against contracting melanoma .. The industry is effectively selling a problem in search of a solution that
Exhibit C, p .. 3
hrtp://www.sunlightscam.com/scamJ.html
1/ 11/ 2009
-- ...... '"J v '-' ll uvu <1 lalllllllg, UC:U }'Ullf rtS.OntraCII11g mela .. .
1-'agel.otl
they don't even have.
In the meantime, the law of unintenued consequences reveals thnt the sunscreen industry's message of
UV abstinence may have back tired when it comes to preventing cancer.
A recent study in the prestigious Proceedings of the National Academy of Sciences cletermineu that the
risks of not getting enough UV li ght far outweighed the hypothetically minute risk of skin cancer. That's
because getting a healthy tan naturally produces vitamin D, which has been linked to significantly
decreasing your risk of contracting internal cancers like lung, kidney, or I i ver cancer.
While getting too much sun has been linked to some forms of cancer, indoor tanning is a government-
approved, controlled environment designed to give you a tan without ever burning-which is the likely
culprit in contracting cancer from sun exposure.
The bottom line is clear: the ri sks of not getting enough vitamin D outweighs the hypothetical risks of
UV light exposure .
2008 The [ndoor Tanning Association
Exhibit C, p. 4
http://www.sunlightscam.com/scam3.html
I r I J/200()
''- < , , ._ uuvvt t<llllllllt. l.C Udii):;O:IUU:S Llll:lll LUOOHl g 111 [Ot' SliO :).ghtSCaffi.COffi
Page I of I
r Prsitk:
Blowl:>ack
Uet! ing a tan is dangerous
Tai'Jning has an epidernic of sk_in.
.of l i\1.. bed <;oDJHL<;ti_ng
hqls arc_ ti_me? the_
Tllere is no such thing a;; a tan
'( 9V _enq_ugh Yitam in Jrink_i_ng
f
Indoor tanning is more dangerous than tanning in the sun
t" .. 'l '\\il
" , J , I
. 1 r. J,.;f
.. _ \ . .. .
Indoor tanning is more dangerous than tanning in the sun
'ffWfH:
Just the opposi te is true_ Unlike tanning outdoors, indoor tanning is designed to match your skin type
and desired tan in a well-regulated, controll ed environment Consequently, the vast bulk of scientific
research indicates that indoor tanning is a safer alternat ive to tanning outdoors .
,() 2008 The Indoor Tanning Association
Exhi bit C, p. 5
ht1p://www.sunli ght scam_com/scam8.html
I 1 I 312009
The fear of getting a tan has gone too far. Dennatologists with the sunscreen and
cosmetic industries are trying to scare us away from the sun. But tanning produces
vitamin D, and research shows vitamin D may fight heart disease, breast cancer, stroke,
and osteoporosis. So go get a tan, your body Will thank you.
[on screen: Vitamin D Fights Heart Disease Breast Cancer Stroke Osteop()rosis]
Bought to you by The Indoor Tanning Association.
-Exhibit D 1, Transcript, television and website advertisement
(on screen: www.SunLightScam.com]
The fear of getting a tan has gone too far. Dermatologists with the sunScreen and
cosmetic industries are trying to scare us away from the SWl. But tanning produces
vitamin D, and research shows vitamin D may fight heart disease, breast cancer, stroke,
and osteoporosis. So go get a tan, your body will thank you.
[on screen: www.SWlLightScam.com]
[on screen: Vitamin D Fights Heart Disease Breast Cancer Stroke Osteoporosis]
Bought to you by The Indoor Tanning Association.
-Exhibit D2, Transcript, television and website advertisement
'
I
,.
l .
1
~ ;
.
!
; .
(
Exhibit E
Exhibit F. P- I
AN EFFECTIVE COMMUNICAnONS STRATEGY IS ESSENnAL
FOR ANY BUSINESS OR O ~ R O F T ADVOCACY GROUP. In
a world where there is an inftnlte amoont of information com-
peting for the limited attention of consumers. lt Is Increasingly
Important to employ a messaging campaign that can cut
through the clutter and reach your Intended target.
It Is frequently assumed that to do this you need a multkniUion
dollar advertising budget. However, with solid research, new
or underreported facts. a creative or controversial advertising
campaign, and a coordinated media strategy, there are Inex-
pensive ways to ensure that the public hears and is lnftuenced
by your message.
By practicing what you find in this book, you will be able to
more effectively communicate your message, build your image,
and motivate desired behavior.
f
2
Exhibit F, p. 2
ARGUMENT 1-
VtTAMIN D IS GOOD (VITAMIN D IS THE .. SUNSHINE VITAMIN"):
Accordfng to a Harvard Uni\lersity study published In the New England
Journal of Medicine, 60% of Americans are vttamin 0 deficient.
Vitamin 0 deficiency is associated with an increased rtsk of colon,
prostate, and breast cancer and Is shown to ward off heart disease.
MS. and other chronic health problems.
Recent research shows that the beneflts associated with vitamin D
outweigh any potential risks associated with exposure to UV light.
Doctors estimate that there are 0\ler one billion people worldwide at,
risk of vitamin 0 deflclency, with 30-50% of children and adutts In the
' United States at high risk for this dangerous condition.
VItamin D Is also linked to many common wintertime complaints such
as fatigue, depression, and aches and pains
It ls impossible to get the requisite amount of vitamin D In cities north
of 37 degrees for as many as 6 months out of the year. That inctudes
cities like Richmond, VA, St. louis, MO. Sacramento. CA. ~ n those
further north.
Vitamin D isn't like other vi_tamlns that you can easily ingest as part
of your diet. It is best absorbed through the skin from exposure to UV
light. New research indicates that supplement-based vitamin D. as
opposed to vitamin D naturally produced through exposure to UV light,
may actually harm the body's ability to tight disease.
African Americans are particularly susceptible to vitamin 0 deficiency
because increased levels of skin pigment inhibit the body's natural
ability to produce vitamin D.
Exhibit F, p. 3
ARGUMENT 3-
TANNING IN MODERATION lS BENEACIAL:
: '-.
Tanning In moderatlon makes peopJe look and feel better.
Moderate exposure to UV light benefits people concerned about
vitamin D deficiency and has proven to boost Immunity to certain
diseases.
Indoor tanning in moderation Is safer than exposure to the sun,
because the environment Is controlled.
Unlike the sun, tanning Indoors is well regulated and approved by
the government. When used moderately and responsibly, tanning ses-
sions are designed to prevent burning.
Exhibit F, p. 4
Enjoy the sun on doctor's orders
Solar rays can help protect against some cancers and
heart disease, say scientists
-The Guardian, January 8, 2008
As Vitamins. Go, D, You Are My Sunsh.hie; ...
Just 20 minutes of sun exposure without sunscreen :
enables the skin to produce 20,000 IU of vitamin D. .
, -The Washington Post. Scpccmbci 18, 1007
' - - , ... .
Sunshine mor; than it causes;
Sunshine has a protective ejfect overall because
it helps to create vitamin D
. .... -- - -
-New Scientist. January 12,2003
. .. . .
The so-called vitamin is pois.ed to
become the nutrient of the decade
', .. -The '$ea. Fcbruaiy' l9, 2003
! i. -. .. ... . -- .
. .
Studies shed light on 'sunshine vitamin'
Americans typically get more than 90 percent of their vitamin D from
the source that nature intended-the sun ...
-The Oakland Tribune, January 22, 2008
Time to rethink sun tanning?
For more information visit www.TrustTanning.com
Dermatologists and the sunscreen industry have spent millions on a deceptive cam-
paign co scare Americans away from the sun. Now the tide of research is turning the
other direction. The positive effects of getting vitamin D from sunlight are clear. So
soak up a little sunlight- indoors or out-a couple of times each week, and get your
recommended dose of the "sunshine vitamin."
Exhibit G
L--- ---- ---------- ------ - ... - ------
--------
In the Matter of Indoor Tanning Association, File No. 0823159
ANALYSIS OF PROPOSED CONSENT ORDER TO AID PUBLIC COMMENT
The Federal Trade Commission ("FTC" or "Commission") has accepted, subject to final
approval, an agreement containing a consent order from the Indoor Tanning Association
("respondent"). The proposed consent order has been placed on the public record for thirty (30)
days for receipt of comments by interested persons. Comments received during this period will
become part of the public record. After thirty (30) days, the Commission will again review the
agreement and the comments received, and will decide whether it should withdraw from the
agreement or make final the agreement's proposed order.
This matter involves the advertising and promotion of indoor tanning products and
facilities. According to the FTC complaint, respondent represented, in various advertisements,
that tanning, including indoor tanning, does not increase the risk of skin cancer. The complaint
alleges that this claim is false and unsubstantiated because tanning, including indoor tanning,
increases the risk of skin cancer, including squamous cell and melanoma skin cancers. Also,
according to the complaint, respondent represented that: tanning, including indoor tanning,
poses no danger; indoor tanning is approved by the government; and indoor tanning is safer than
tanning outdoors because, in indoor tanning facilities, the amount of ultraviolet light is
monitored and controlled. The FTC complaint alleges that these claims are false and
unsubstantiated.
The FTC complaint further charges that respondent represented that research shows that
vitamin D supplements may harm the body's ability to fight disease; and that a recent study in
the prestigious Proceedings of the National Academy of Sciences determined that the risks of not
getting enough ultraviolet light far outweigh the hypothetical risk of skin cancer, that getting a
healthy tan produces vitamin D, and that increased vitamin D has been linked to significantly
decreasing your risk of contracting internal cancers, such as lung, kidney, or liver cancer. The
complaint alleges that these claims are false and misleading. The FTC complaint also alleges
that respondent represented that tanning causes the skin to generate vitamin D and has health
benefits, but that respondent failed to disclose facts that would be material to consumers in their
purchase and use of indoor tanning services, specifically, that consumers can increase their
vitamin D levels through ultraviolet levels lower than the amount needed to get a tan, and that
ultraviolet radiation can injure the eyes and increases the risk of skin cancer. The complaint
alleges that respondent's failure to disclose these facts, in light ofthe representation made, is a
deceptive practice. Finally, the complaint alleges that respondent provided to others the means
and instrumentalities to engage in deceptive acts or practices.
The proposed consent order contains provisions designed to prevent respondent from
engaging in similar acts or practices in the future. The order covers representations made in
connection with the manufacturing, labeling, advertising, promotion, offering for sale, sale, or
distribution of any covered product or service, in or affecting commerce. It does not cover
representations made in non-commercial settings or contexts, such as communications to
legislative or executive bodies. The order defines a covered product or service as any ultraviolet
Page 1 of 3
lamp or sunlamp product, as defined in federal regulation 21 C.P.R. 1040.20, or any
commercial facility where consumers may use ultraviolet lamps or sunlamp products.
Part I of the order prohibits respondent from making the following representations:
tanning, including indoor tanning, does not increase the risk of skin cancer; tanning, including
indoor tanning, is safe or poses no danger; indoor tanning is approved by the government; and
indoor tanning is safer than tanning outdoors because in indoor tanning facilities, the amount of
ultraviolet light is monitored and controlled. The ban on representations that tanning, including
indoor tanning, is safe, is fencing-in relief. Part II of the order prohibits respondent from
misrepresenting (1) that research shows that vitamin D supplements may harm the body's ability
to fight disease and (2) that a study in the Proceedings of the National Academy of Sciences
determined: (a) that sun exposure does not cause skin cancer or melanoma, or that the risk of
such cancer is only hypothetical; (b) that getting a tan is healthy; (c) that the risks of not getting
enough ultraviolet light far outweigh the risk of skin cancer; or (d) that vitamin D has been
linked to significantly decreasing the risk of contracting lung, kidney, or liver cancer .
Part III prohibits respondent from making any representation about the safety, health-
related efficacy or performance, or health-related risks or benefits, of any covered product or
service; or about the sources, performance, efficacy, or health-related risks or benefits of vitamin
D; unless the representation is non-misleading, and, at the time it is made, respondent possesses
and relies upon competent and reliable scientific evidence that is sufficient in quality and
quantity based on standards generally accepted in the relevant scientific fields to substantiate that
the representation is true. For the purposes of the order, competent and reliable scientific
evidence is defined as tests, analyses, research, studies, or other evidence that have been
conducted and evaluated in an objective manner by qualified persons, that are generally accepted
in the profession to yield accurate and reliable results, and whose results are consistent with the
body of reliable scientific evidence relevant to the representation. Part IV of the order prohibits
respondent from misrepresenting the existence, contents, validity, results, conclusions, or
interpretations of any test, study, survey, or research .
Part V of the order is a disclosure provision. It prohibits respondent from making any
representation about the safety or health benefits of any covered product or service unless it
makes the following disclosure, clearly and conspicuously, and in close proximity to the
representation: "NOTICE: Exposure to ultraviolet radiation may increase the likelihood of
developing skin cancer and can cause serious eye injury." In the event, however, that respondent
represents that exposure to ultraviolet radiation produces vitamin Din the body, or otherwise
about the effectiveness or usefulness of such product for generation of vitamin D, the required
disclosure shall be as follows: "NOTICE: You do not need to become tan for your skin to
make vitamin D. Exposure to ultraviolet radiation may increase the likelihood of developing
skin cancer and can cause serious eye injury."
Part VI of the order prohibits respondent from providing to any other person or entity any
means or instrumentalities that contain any representation prohibited by the order. Part VII
requires respondent to send a notice about the FTC's law enforcement action to all of its
Page 2 of 3
members, and all other entities to which it provided point-of-sale advertising on or after January
1, 2008; the required notice is attached to the order as Attachment A.
Parts VIII, IX, X, and XI of the consent order require respondent to keep copies of
relevant advertisements and materials substantiating claims made in the advertisements; to
provide copies of the order to its personnel; to notify the Commission of changes in corporate
structure that might affect compliance obligations under the order; and to file compliance reports
with the Commission. Part XII provides that the order will terminate after twenty (20) years,
with certain exceptions.
The purpose of this analysis is to facilitate public comment on the proposed order, and it
is not intended to constitute an official interpretation of the agreement and proposed order or to
modify in any way their terms .
Page 3 of 3
546631-00005 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00005
1/27/2010
Jamie Altman
PA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
As a dermatologist, I would like to thank you for taking a step towards protecting people from unwanted
skin cancer risk associated with tanning. This is particularly important for minors, who still,
unfortunately, have unregulated access to tanning booths in most states .
http://www.ftc.gov/os/comments/indoortanningassoc/546631-00005.htm
2/24/2010
546631-00057 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-0005 7
211112010
Andrews
CA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
I started using tanning booths when I was 16 years old. I believed the claims that it was safer to use a
tanning booth than to sunbathe outdoors. I believed it was good for me, and not harmful to me in any
way. I used indoor tanning salons quite regularly as a teenager and in my twenties. As I became older,
more mature, and less gullible At age 35, three months after the birth of my first child, I was diagnosed
with malignant melanoma, which could have taken my life and left my newborn baby without a mother.
The general public has been misled about the risks of indoor tanning beds. It is time for this to stop. The
public must be educated about the extreme risk, of malignant melanoma in particular, from the use of
indoor tanning salons. I believe it should be illegal for minors to use them, but at the very least, parental
consent must be required. Teenagers have not developed the rational thought process to consider long
term health risks for something that is so immediately gratifying to them. I wish laws like this had been
in place to protect me when I was young and making foolish decisions that would have a severely
adverse impact upon my health in future years. Thank you for considering this critical public health
lSSUe .
http://www .ftc.gov I os/ comments/indoortanningassoc/ 546631-0005 7 .htm 2/24/2010
54663l-00055.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00055
211 1/2010
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
I feel that tanning beds should be held accountable for luring customers in under false pretense (i.e. that
it is healthy and safe to tan). I feel this is especially unfair to young girls, who are more likely to fall for
these false forms of advertising. I have the scars of multiple biopsies to show what tanning does and the
health risk that you take everytirne you get into a tanning bed. I will see a dermatologist every 3 months
for the rest of my life as a result ofbeing a former tanner. Confidentiality requested .
http://www. ftc.gov I osl comments/indoortanningassoc/546631-0005 5 .htm
2/24/2010
546631-00036.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00036
1130/2010
Dessie Baker
FL
Federal Trade Commission
Page 1 ofl
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
I worked in a Tanning salons when I was 17 and they down play the risks tremendously. They can be
flat out deceiving or just ignorant to the risks. Girls as young as 15 go in and tan. What we as a society
don't realize is the risk we are putting ourselves in! Hollywood has glamorized this ritual of being
bronzed to be beautiful. As a young adult I felt this way for many years. A few Years later at 22 I was
diagnosed with Melanoma. Tanning is your skin cells showing damaging effects of the UVA rays. No
one is expecting tanning salons to disappear but lets be realistic and let people know the real risks.
Tanning before 35 really ups the risks so teens shouldn't tan at such a young age. "Melanoma Cancer
Counts for 4% of all skin cancers, It is responsible for approximately 74% of all deaths that arise from
skin cancers. Don't become a statistic. Early detection reduces the death rate"
http://www. ftc. gov/ os/ commentslindoortanningassoc/ 546631-0003 6 .htm 2/24/2010
546631-00051.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00051
2/10/2010
Lizabeth Bunte
IL
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
----- ------ -
Comments:
At one time I did use a tanning bed but noticed how dry my skin was becoming ... a stopped within a
year ... thankful that I did ... The use of the tanning bed is very harmfuL. the young people especially need
to be educated of its danger...cancer causing issues ..
http://www .ftc.gov/os!comments/indoortanningassoc/ 546631-00051.htm
2/24/2010
546631-00018.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00018
1/27/2010
Michelle Bush
MA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
Re: Indoor Tanning Association- Consent; FTC File No. 082 3159 Kudos for your efforts in this
important public health matter. I am a dermatologist who sees the devastating and costly effects of skin
cancer every day. The evidence is clear- exposure to ultraviolet radiation causes cancer, whether it be
from sunlight or from tanning beds. The tanning industry's claims that indoor tanning is safe and
beneficial are deceptive and dangerous. Thank you .
http://www .ftc.gov/os/comments/indoortanningassoc/546631-000 18.htm 2/24/2010
546631-00023 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00023
1/28/2010
Neil Capper
R Neil Capper MD
AL
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
----------------------
Comments:
I am so pleased to see that the FTC has addressed the misrepresentations of the Tanning Trade Industry
about the benefits of indoor tanning. It would be beneficial to require the organization to similarly
advertise corrections of their misrepresentations. This is a public health issue. A cease-and-desist order
alone, unfortunately, will not undo the public perception that resulted from the ad campaign. At the very
least, continued monitoring of advertising and press releases from the trade association would be in the
public interest. Unfortunately, the trade industry has a record of serving the financial interests of its
members, and not serving the public interest. We Dermatologists try to educate one patient at a time, and
have paid for public announcements, but studies to date of tanning bed use show that we have been
spitting into the wind. FTC monitoring and oversight with clear guidelines will help to overcome
misrepresentations .
http://www. ftc. gov I osl comments/indoortanningassoc/ 546631-00023 .htm 2/24/2010
546631-00040.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00040
2/1/2010
Make Tanning Inaccessible to Minors Meghan Cartwright
WA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
Melanoma is one of the fastest growing cancers in the U.S. as well as the leading cause of cancer deaths
in women ages 25-29. The World Health Organization has declared the UV light used in tanning beds to
be just as carcinogenic as asbestos and cigarettes. Exposure to UV radiation, especially at a young age,
is a well-known cause of melanoma. As a 20 year-old melanoma patient, I am painfully aware of the
serious consequences of tanning. As a teen I used tanning beds, naive to the huge amount of harm ofUV
exposure causes one's skin, like many of my friends. If young women are hearing the facts, they aren't
listening; the mantra "it won't happen to me" lives on-and because of this, young people are getting
cancer (and dying). UV exposure should be handled the way handle cigarettes-- illegal to sell to minors.
Instead, the federal health care bill has proposed a 10% tax on indoor tanning services. If the bill passes,
tanning won't be made illegal for minors because the U.S. government is unlikely to halt a new revenue
stream it has created. Let's get real-- a 10% tax won't stop minors from tanning. This tax is only going to
benefit the government.
http://www. ftc. gov I osl comments/indoortanningassoc/ 546631-00040 .htm 2/24/2010
546631-00024.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00024
1/28/2010
AmyCawvey
OH
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
1 started using tanning beds at age 14. This was 1984. There were no warnings about Melanoma. I did
not know how greatly using tanning beds would increase the chance of me developing Melanoma. I was
diagnosed at only age 33. Many young teens, children, and women in their 20's are not thinking about
how this might affect their lives later. It is only when you look into your children's eyes, knowing you
have a Melanoma diagnosis, which could have been prevented by not using tanning beds, do you realize
the danger. Tanning beds need to be banned from those under 18, just like cigarettes are banned.
Children under 18 do not realize the life long implications of using somehting like a tanning bed. A
parental waiver is not enough, as many parents do not do a good job in protecting their children .
http://www. ftc. gov I os/ comments/indoortanningassoc/ 546631-00024 .htm 2/24/2010
546631-00034.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00034
1/30/2010
Charles
IL
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
------------------- - ---
Comments:
I fully support the FTCs stance on the ludicrous claims made by the tanning industry in an effort to
promote unsafe exposure to carcinogenic ultraviolet light. Current science indeed is showing that some
amount of UV exposure is healthy for human function. But the amount ofUV needed for health
purposes if far below the amount needed to cause tanning and carcinogenesis. Myself and other
practicing dermatologist support the FTC in this decision .
http://www.ftc.gov/os/comments/indoortanningassoc/546631-00034.htm 2/24/2010
546631-00013 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00013
1/27/2010
Scatt Dale
NADC
AZ
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
---------------- --- ---------
I am heartened to know that the FTC respects scientific fact over fiction. As a dermatologist and Mobs
surgeon, I caution patients about sun exposure and tanning everyday because of their obvious
carcinogenic effects on human skin. Thank you FTC for standing up to IT A who has flagrantly lied to
the public about the 'benefits' of tanning. Good job!
http://www .ftc.gov/os/comments/indoortanningassoc/ 546631-000 13 .htm
2/24/2010
546631-00020.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
546631-00020
1/27/2010
F William Danby
NH
Federal Trade Commission
Page 1 of 1
Rule:
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
No Attachments
Comments:
Thank you for starting the ball rolling towards what we hope will be a complete ban on these
carcinogenic machines, run by liars and the easily led .
http://www. ftc.gov I os/ comments/indoortanningassoc/ 546631-00020 .htm
2/24/2010
546631-00009.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00009
1127/2010
Susan Dozier
TX
Federal Trade Commission
Page 1 ofl
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
--------------
Dear Sirs and Madames: I want to thank the FTC for censuring the indoor tanning industry for the
deceptive information they have promulgated regarding the supposed healthful benefits of indoor
tanning. As a dermatologic surgeon whose practice deals primarily with skin cancer, usually the result of
natural or artificial exposure to ultraviolet light, it was disheartening to me to have my efforts to educate
the public about the dangers of UV radiation contradicted. I hope having the true risks of indoor tanning
available to those who are considering it will dissuade at least some from exposing themselves to
additional carcinogens. I hope as a result the epidemic of skin cancers I am treating will be lessened.
Thank you for pursuing this important matter. Sincerely, Susan Dozier, M.D. Fellow, American College
of Mohs Surgery
http://www. ftc. gov/ os/ comments/indoortanningassoc/546631-00009 .htm 2/24/2010
546631 -00029 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
~
Comments:
546631-00029
1/28/2010
Thomas Ellis
VA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
I am an Engineer and a melanoma Patient. While I do not believe that all incidents of melanoma are
caused by sunlight, the empirical evidence strongly links a huge number of the melanoma occurrences to
the abuse of sunlight/tanning beds. Why is melanoma the leading cause of cancer deaths in young
females? It used to be considered an old folks disease. Why is lung cancer a major problem in smokers?
Something is definitely there as a catalyst to set off the mutations that result in cancer tumors. I have
urged my daughters not to use Tanning beds. The one that has, often gets a burn from them. There
definitely needs to be much tighter regulations and warnings about the dangers, especially restrictions on
teenage utilization.
http://www .ftc.gov/oslcomments/indoortanningassoc/ 546631-00029 .htm 2/24/2010
546631-00027 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00027
1128/2010
Jeffrey Evanson
St. Lukes Dermatology
MN
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
. ----------- ------
Comments:
Thank you for taking up and investigating this issue. Tanning customers and parents of teen customers
need to be informed about all the risks associated with unnecessary ultraviolet light exposure. Thank
you for following the trail of truth and not gratifying anecdotal hearsay and deception.
http://www .ftc.gov/os/comments/indoortanningassoc/546631-00027 .htrn
2/24/2010
546631-0003 8.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-0003 8
1/31/2010
Ellen Frankel
Ellen H. Frankel, M. D.
RI
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
As a practicing pediatric and adult dermatologist, who has witnessed first hand the rise in Melanoma, I
feel it behooves the government to provide stict and stringent guidelines prohibiting tanning. As we are
aware, the number 1 cause of death in women between the ages of 18 and 29 is melanoma, which is
directly related to tanning parlor/UV exposure.
http://www.ftc.gov/oslcornrnents/indoortanningassoc/546631-00038.htrn
2/24/2010
54663 I-00038.htm
Comment
Number:
Received:
Commentcr:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00038
1/31/2010
Ellen Frankel
Ellen H. Frankel, M. D.
RI
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
... --. ---------- ---
As a practicing pediatric and adult dermatologist, who has witnessed first hand the rise in Melanoma, I
feel it behooves the government to provide stict and stringent guidelines prohibiting tanning. As we are
aware, the number 1 cause of death in women between the ages of 18 and 29 is melanoma, which is
directly related to tanning parlor/UV exposure.
http://www. ftc. gov I osl cornmentslindoortanningassoc/ 546631-0003 8 .htm
2/24/2010
546631-00052.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00052
2/10/2010
Marie French
TX
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
My husband passed away 2/3/08 from stage IV melanoma. While his diagnosis was not from tanning
bed exposure, I am convinced this tyoe of exposure is detrimental. At one time, I, also, visited tanning
beds, but no more. I saw the ravages of this disease,was a caretaker, and over the course of three years
treatment at MD Anderson Cancer Center in Houston, Tx. I saw people of all ages. Many of them were
in their 20's and 30's, and you could spot the tanning bed users. This disease is no respecter of age. I
urge any restrictions, or banning of the use of tanning beds.
http://www.ftc.gov/os/cornments/indoortanningassoc/546631-00052.htrn
2/24/2010
546631-00033.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00033
1/29/2010
Andrea Garrett
St Louis dermatology and surgery center
MO
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
I am reminded of the false claims of the ITA frequently in my clinic with young people commonly
asking "is it really safe to tan?". Mu answer is always no. I support the FTC inquiry .
http://www. ftc.gov/ os/ comments/indoortanningassoc/ 546631-0003 3 .htrn
2/24/2010
546631-00028.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00028
1/28/2010
Victoria Hebb
VA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159 .
-----------
I am a 20 year old who was diagnosed with two spots of melanoma this past summer of2009. When I
went to the surgeons office he informed me that I more than likely got melanoma from the tanning beds.
After doing much research, I realized he was ri ght. I only visited the tanning beds a few times a week for
about 6 or 7 months in my entire life, and I developed melanoma. When I would sign up for a tanning
contract I would recieve emails, newsletters, and mail convincing me that tanning was healthy for me
and that I was actually doing my body good. I realized what I lie that was when I developed melanoma. I
wish everyday that I could go back in time and choose NOT to tan in the tanning beds, but I realize l
can't. It breaks my heart everyday when I see girl s and boys, men and women, being lied to about their
tanning habits. They are being told it's healthy because they are getting VitD, and it's lifting their mood,
and it's better than being in the sun. The REAL truth is that our bodies produce enough VitD from other
sources besides the sun or artificial light, their mood will change when they realize how much they have
increased their risk of skin cancer, and NO accessi ve amount od sun is good for you, inside or out - you
NEED to protect your skin with sunscreen and shade! I was decieved by the tanning industry and the
only way I figured it out was by getting cancer. I wish I would have been warned sooner and not lied to
by people who just want my money. I think that the tanning industry should be required to openly post
and admit the dangers of tanning just as cigarettes, since the FDA has now ranked tanning beds as just
as much of a danger. All of this to say that the tanning industry needs to be truthful and warn young
people about the dangers oftanning. I just don't see how a whole industry could be so money crazy that
they risk taking the lives ofbeautiful young girls, daughters, mothers, brothers, fathers, and everyone
else who tans.
http://www .ftc.gov/os/comments/indoortanningassoc/ 546631-00028.htm 2/24/2010
546631-00062.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00062
2/18/2010
Amanda Hom
WI
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
------ --------------
I started using indoor tanning beds at the age of 15. I would go a dozen or so times each spring to get a
good "base tan" for the summer. This was just over 10 years ago and at the time I was never presented
with any information regarding the risks of tanning leading to melanoma. I didn't even know young
people were at any sort of risk for melanoma. I tanned nearly every year until the age of 24. I initially
stopped tanning not because I was worried of the risk, I just didn't have the time or the money to spend
on it. Then I was diagnosed with Stage I Melanoma at the age of26. I have no family history of
melanoma and it is very difficult to wonder if I would have gotten melanoma if I had never stepped foot
into a tanning salon. I was so fortunate to catch it at Stage I, but many women aren't as lucky. Tanning
salons need to be prevented from being glamorized and they need to educate their customers of the risk
of tanning. They especially should not let anyone under the age of 18 into the salon. If tanning is going
to be grouped in the same carcinogenic category as smoking, then the age limit should also be the same.
These businesses need to get in trouble for allowing people under the age of 18 into the salon just as a
convenience store would be in trouble for selling cigarettes to someone under the age of 18. They should
also have to contribute money to the education and awareness of the tanning-melanoma link, just like
the large tobacco companies did with lung cancer. The IT A needs to come clean and stop getting away
with telling these lies .
http://www. ftc. gov/ os/ commentslindoortanningassoc/ 546631 -00062 .htm 2/24/2010
546631-00004.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attaclunents
Page 1 of 1
546631-00004
l/27/2010
James
PA
Federal Trade Commission
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
--- - - ---------------- ----
------ ----
Comments:
I agree wholeheartedly with your decision regarding indoor tanning. It is detrimental to the health of our
fellow citizens and the tanning industry is promoting thier product in a manner similar to cigarettes,
preying on our young people. Further action to limit or ban indoor tanning is justified .
http://www.ftc.gov/ os/comments/indoortanningassoc/ 546631-00004.htm
2/24/2010
546631-00017.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-0001 7
1/27/2010
Kay Johnston
Bel-Ami Dermatology
TX
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
----- -- ~ . . ----- ----------------- ----- ... _____ _
Comments:
I am pleased to see that the FTC has charged the Indoor Tanning Association (ITA) with making false
and deceptive health and safety claims regarding indoor tanning_ As a dermatologist, I have seen patient
as young as 17 years old with a Clark's Levellll Malignant Melanoma who admits to using a tanning
bed. I have also seen other patients in their teens and twenties who were diagnosed with melanoma and
also admitted to using tanning beds. In addition,! have also encountered patients who state that they
have stopped using sunscreen because of the fear that this would prevent them from obtaining adequate
amounts of Vitamin D! I applaude the FTC in doing their due diligence in investigating these claims in
order to help the patient. Sincerely,
http://www. ftc. gov/ os/ commentslindoortanningassoc/ 546631-00017 .htm
2/24/2010
546631-00008.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attaclunents
546631 -00008
1/27/2010
Kroeger
Outside the United States
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
------------ --
Comments:
BRAVO! This is the first time in a long time my academy has done something for which I am truly
proud. The AMA has woefully let me/us down. I am proud our academy has made our voices heard on
this dangerous industry_
http://www .ftc. gov I os/ comments/indoortanningassoc/ 546631-00008 .htm
2/24/2010
546631-00059.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00059
2/ 15/2010
Malcher
CT
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
-------------------------
Tanning beds should be regulated and persons under the age of 18 should need parental consent to use.
Skin cancer rates continue to increase and it known that increased UV exposure is a risk factor. By
regulating the use of tanning beds this would be a healthy and important first step to drive the onset of
skin cancer down. For this industry to stand by and state that they offer a "safe product" is irresponsible
to the consumer and general public .
http://www .ftc.gov/os/comments/indoortanningassoc/546631-00059 .htm
2/24/2010
546631-00035.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00035
1130/2010
Mark McCune, M.D.
Kansas City Dermatology, P.A.
KS
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
---------- - --------------- --
I am in full support of the FTC's position against the false advertising that has been ongoing for years by
the tanning industry. The American public has been misled and misinformed by this industry for
monetary gain and has placed' our citizens at increased health risk for the development of precancerous
and malignant skin conditions. When I enetered private practice in dermatology in 1981, the lifetime
risk of developing a melanoma in a child born that year was 1 in 250. Recent data suggests that that the
lifetime risk of developing melanoma in an American bom now is 1 in 50. This astronomical increase in
the risk of melanoma development is etiologically tied to ultraviolet exposure from both the sun as well
as from artificial tanning exposure. I have personally taken melanomas off of 18 to 25 year olds, all of
whom have had a history of tanning bed exposure from their mid-teens. As a former member of the
Kansas State Board of Healing Arts, I commend you for your action against false and misleading
advertising. I encourage the appropriate govemmental agencies to take the next logical step, which is to
aggressively regulate this industry which increases the cancer risk of our citizens as much as smoking
increases the risk of lung cancer (as reported by the World Health Organization in 2009). Federal
regulations will spare state legislatures, medical boards, and other responsible agencies from having to
regulate the tanning bed industry with the likelihood of inconsistent and incoherent results .
http://www.ftc. gov/os/comments/indoortanningassoc/546631 -00035.htm 2/24/2010
546631-0004 7 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-0004 7
2/ 10/2010
Kristin McJunkins
CT
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
~ ~ ~ ------------- --- ------- -- -------------------------
Comments:
People should know any dangers associated w/ tanning beds before making the choice to use them.
Melanoma is an aggressive cancer and anything that can be done to prevent it should be done .
http://www. ftc. gov/ os/ comments/indoortanningassoc/ 546631-0004 7 .htm
2/24/2010
546631-0004I.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00041
2/8/2010
Laura Mikkelson
fL
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association; FTC File
No. 082 3159
. ------ -------------- ---------- ---- -----------
Comments:
I was born in 1972 in Fort Myers, Florida. Back then my mom always bad a fascination with the beach which
why my parents moved to Florida. In the '70's and '80's I really don't recall much warning about sunblock and
skin cancer. If it was out there it definitely was not as widely advertised as it is today. I can honestly say that in
the mid '80's when I would lie out for 4 -5 hours with baby oil and iodine mixture I honestly did not know that I
was doing myself any hann ... except I did know that I was prematurely aging my skin ... but when you are in your
early to mid teens that is the last thing you worry about....after all... we are invincible .... or so we thought back
then. So I would tan as much and as frequently as I possibly could ... whether it be catching a ride with the parents,
friends, or even take the bus to Siesta Key. Plus I always had the old backyard as my back-up for catching some
rays on a beautiful Florida day (which we have plenty of those here). So the early '90's come and a girlfriend of
mine introduces me to tanning beds. At this point I have heard a little bit about melanoma and how the severe
bums I had suffered in my teens could come back to haunt me ... but again there really wasn't a lot of information
out there ... or at least I again chose not to pay particularly close attention. As I recall I remember hearing more
about AIDS and SID awareness than skin cancer. The tanning salons back then were even advertising
themselves as the safe alternative to sun. That the rays the beds put out were the good rays. I look back on that
know and realize what a joke that was. So I would hit a tanning salon with my girlfriends on the way to Siesta
Key, we would spend anywhere from 3 - 5 hours at the beach, and then hit a different tanning salon on the way
home. The salons did enforce the one tanning session a day but there was no way for them to track whether I had
been to a different location earlier in the day let alone even ask me if I had already spent time at the beach ... which
was something they obviously could tell but for them they just wanted my business. So over my lifetime l had
had way too many blistering sunburns to count on both of my hands, I was always as tan as I possibly could get,
my hair was always as bleached blonde as the sun could get it, and if! ever got to what I felt was a pale look I
would just step up my tanning ritual for a week or two and get back to the point that my skin would not get any
darker. In the late '90's I did finally start going to a dermatologist because at this point I had heard that I was high
risk for developing skin cancer. I am a natural blonde, blue eyes, fair skin, had the blistering bums when I was
growing up, and cancer is very rampant in my family. The doctor would do a few biopsies here and there mainly
to get rid of some ofthe moles that were raised & bothersome to me. They always came back negative so I
eventually quite going once all of the bothersome moles were gone and all had come back negative. I figured I
managed to get through that point in my life unscathed. But did I learn a lesson? Absolutely not!! I still would go
and tan but not to that extreme anymore. I would come home from work usually around 2pm and lay out in my
back yard or even go to Siesta Key for a couple of hours EVERYDAY. So I no longer would hit the tanning beds
or if I did it would be just one and no beach visit that day. In 2001 I fmally noticed a mole that just didn't look
right but did not follow the ABCDE's of melanoma. Lucky for me I had a very caring and nagging boyfriend who
ipsisted I get it looked at or he was going to break up w/ me. Even though I was annoyed with him I went to the
dermatologist and had it biopsied; good thing because it came back positive for melanoma and I had swollen
lymph nodes in the area as well. I am one of the fortunate ones who were able to have the cancer removed w/out
any further treatment. Not everyone is as lucky.
http://www.ftc.gov/os/ commentslindoortanningassoc/546631-00041.htm 2/24/2010
546631-00014.htrn
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attaclunents
Comments:
546631-00014
1127/2010
Christopher Moeller
Moeller Dermatology
KS
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
As practicing physician specializing in dermatology for the past 25 years, I have seen many patients
suffer and die from skin cancer caused by tanning beds. I and many other health professionals view the
tanning industry the same way we view the tabacco industry. I would urge the FTC to support a tax on
tanning bed use to help offset the costs associated with care of the patients with disease caused by
tanning .
http://www. ftc.gov/ os/ comments/indoortanningassoc/ 546631-00014 .htm
2/24/2010
546631-00058.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00058
2/12/2010
Sharon Noble
Outside the United States
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
---- - ----------------- _______________ .. ____ - -- -------------------
Comments:
tanning beds need to be regulated better or outlawed altogether. I know many people who have
melanoma now which is directly related to using tanning beds. They need to be shut down especially to
youing people under 18 yrs. old
http://www.ftc.gov/os/comments/indoortanningassoc/546631-00058.htm
2/24/2010
546631-00026.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00026
1/28/2010
Lisa Pawelski
Dermatologic Care, Inc.
PA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
- ------- ----------------
Comments:
The Department of Health and Human Services named ultraviolet light a "known human carcinogen"
years ago, in the same category as benzene, radon, and cigarette smoke. The current decree is welcome,
but the federal government must go further. Ban tanning by minors. Require consent for adults who
choose to tan. Ensure that consent forms list in everyday language what medical conditions and
medications further increase the danger of tanning, in addition to baseline risks of accelerated skin
damage, burning, and cancer. Require prominent posting of signs that say "YOU SHOULD NOT TAN
if you have lots of moles, a personal or close family history of skin cancer ... " etc. Make the consent
like the iPiedge consent: require initials after every sentence, not just one signature at the end. Make
tanners re-consent monthly. Most importnantly, tax tanning booth owners and manufacturers, so that
whatever it costs to inform and try to protect uninformed citizens comes out of the tanning industry's
pockets, not our tax dollars .
http://www .ftc. gov/ os/ comments/indoortanningassoc/ 546631 -00026 .htm 2/24/2010
546631-00054.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00054
2111/2010
Misty Peebles
IL
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
-- - .. - -- ---------- ------------- -- ------
---------
Comments:
Indoor tanning salons should be highly monitored if not banned by the government. 1 wish I had know
the effects of indoor tanning before I had used them. I am currently battling Stage 3 Melanoma, that I
most definitely acquired in the indoor tanning beds. It's too late for me, but it's not too late for others,
especially all the new high school girls getting ready for prom this year. Please do something for them,
for their lives .
http://www .ftc.gov I os/ comments/indoortanningassoc/546631-00054 .htm
2/24/2010
546631-000 ll.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
546631-00011
1/27/2010
Peterson Pierre
CA
Federal Trade Commission
Page 1 of 1
RuJe:
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
No Attachments
--------------- ------------------------- ---------------- ---
Comments:
Thank you very much for taking action on this very important topic .
http://www.ftc.gov/os/comments/indoortanningassoc/546631-000ll.htm
2/24/2010
----------------- ----
546631-00030.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00030
1128/2010
Kelly Ransdell
KY
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
---- ---------- - ---- -----
I am a stage IIIC Melanoma survivor who got melanoma from the ta1ming bed (it was on my left
buttocks) I wasnt aware of the risks oftanning beds and I ended up getting Melanoma from them. I was
diagnosed with this at age 30, started using tanning beds when I was 19 years old. The Melanoma went
into my left groin and all my lymph nodes had to be removed in that area and I went thru 6 months of
IL2 and OTIC. After a year im cancer free but I have to go for checkups every 6 months and I have a
35% chance of going thru this again. The tanning bed companies do not want to stand up and say they
cause Melanoma and they should. I had no idea what Melanoma was most people think skin cancer is
something you can cut off but it can invade your entire body and kill you. Please try to regulate tanning
beds for teenagers and adults, the tanning industry needs to state on the beds that it increases your
chance of Melanoma. Dont want anyone to have to go thru what I did. Thanks Kelly Ransdell
http://www. ftc.gov/os/comments/indoortanningassoc/546631-00030.htm 2/24/2010
546631-00045.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00045
2/ 10/2010
Daniel Read
CA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
..
Comments:
I support the FTCs proposed settlement with the indoor tanning industry .
http://www.ftc.gov/os/ commentslindoortanningassoc/546631-00045.htm
2/24/2010
546631 -0001 O.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
RuJe:
No Attachments
Comments:
546631-0001 0
1127/2010
Kelley Redbord
AAD
DC
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
----- ---------
As a dermatologist, I have seen first hand the harmful effects of tanning. I support the consent order and
appreciate the FDA's efforts in protecting patient's from harm .
http:/ /www.ftc.gov/os/comments/indoortanningassoc/ 546631-000 1 O.htm
2/24/2010
546631-00003.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00003
1126/2010
Lyvonn Reese
Reese Group, inc
TN
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
----- -----------
I have two comments: 1. Use some common sense. Did God create the sunshine (UV light) which gives
the earth solar energy and makes all things grow. Then create humans which every single cell in our
body has a vitamin D receptor, then expect us to go crawl under a rock and hide from it. I dont think so.
FTC is supposedly designed to keep unfair and untrue claims made. Yet, the pharmaceutical companies
can make up any kind of report they choose and run it all over the tv and print because they spend so
much advertising dollars. any one who has done any research on cancer will state the importance ofVit
D levels and the best way to obtain high levels is with moderate UV light exposure. 2. Yes, a sunburn is
damaging to the skin. you can certainly obtain a large dose of Vit. D without over exposure. A moderate
tan does protect you from sunburn That is the facts God created us this way. Stop allowing money to
dictate what is fair and unfair. Being exposed to outdoor UV light is best. However, what happens when
the the body is not in an area where they can obtain sunshine year round. The vit D levels drop below
healthy levels. 3. the problem is we over do everything from the way we report the truth, that is backed
up with who pads the pockets the best And 50% of the people dont know what moderation is Whether it
be sunshine, eating or excercise. If the public would tan in moderation whether in or out doors to keep a
light base tan, they would not be as many sunburns and everyone would be healthier, which would cut
down on medical costs Oh I am sorry, that would be a bad thing for the medical and pharmacy industry.
Please use common sense .
http://www .ftc. gov I osl comments/indoortanningassoc/546631-00003 .htm 2/24/2010
546631-00056.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00056
2/ 11/2010
Robert Reeves
CA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
----------------
--------- -----
Comments:
Melanoma is a serious and easily fatal disease with little therapy once it is in the advanced stages. The
Tanning Association has ignored its responsibility to its customers as it promotes its product and should
be reminded quite clearly that its needs to be completely truthful about the risks it is asking customers to
assume .
http://www.ftc.gov/os/comrnentslindoortanningassoc/546631-00056.htm
2/24/2010
)466J l-UUU56.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631 -00056
2/11/2010
Robert Reeves
CA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
- - ----- - ----------- -.. -----------
Comments:
Melanoma is a serious and easily fatal disease with little therapy once it is in the advanced stages. The
Tanning Association has ignored its responsibility to its customers as it promotes its product and should
be reminded quite clearly that its needs to be completely truthful about the risks it is asking customers to
assume .
http://www. ftc. gov I os/ commentslindoortanningassoc/ 546631 -00056.htm 2/24/2010
)466::5 l-UUU4Y .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00049
2/10/2010
Donna Regen
TX
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
My daughter Jaime was an avid tanning bed user when she was in high school, going to visit the tanning
salons daily during her lunch breaks. She was told by the tanning bed operators that because her skin
was very pale, she should get a "base tan" to protect her from the sun's burning rays. When Jaime was 20
years old, she was diagnosed with melanoma and her oncologist told her that her tanning bed days were
over because it had probably contributed to her developing this disease. Jaime had just signed a year's
contract with a tanning salon. When she called to cancel her contract, she was told that she could not
even though her doctor had advised it. They did tell her that they felt bad that she had skin cancer and
offered her a free month of tanning to make her feel better. She hung up on them. My daughter is not
commenting on this herself because 3 years ago she died from that melanoma. She was 29 year old .
http://www.ftc.gov/os/comments/indoortanningassoc/546631-00049.htm 2/24/2010
.)4boJ
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631 -00048
2110/2010
Peg Renery
CA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
--- ---------
------------------------------
Comments:
As a mother, I would really like the practice of tanning salons with their advertizing stopped. Skin
Cancer can result and we should do everthing possible to deter young woman among others from
thinking they are safe .
http://www.ftc.gov/os/commentslindoortanningassoc/546631-00048.htm
2/24/2010
546631-0003 7 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00037
1/30/2010
Todd Roach
IL
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
I believe the FTC is wrong in their remarks and actions concerning the IT A. First if there is a true
medical or scientific study performed by professionals in the field, then why can't the IT A or any
industry use those findings in advertising, there is evidence on both sides regarding the benefits of
tanning indoors. Also those companies and the cosmetic industry that sells Sun-Block use studies to
promote their products, I do not see the FTC taking action against any of these organizations, and why is
that ? The FTC should. not decided which studies are correct and which are not, since the FTC is not in
the science or medical fields the commission does not have the expertise to decide which studies are
correct on the issue. The one undisputed fact is that indoor tanning is no more dangerous than tanning
outside, or working outside, walking outside, sitting outside, and enjoying the outdoors, the effects of
the NATRUAL Sun, have the same effects as Indoor Tanning .
http://www .ftc.gov/os/comments/indoortanningassoc/546631-0003 7 .htm 2/24/2010
546631 -0006l.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
Attachments:
Comments:
546631-00061
2/17/2010
rachael robertson
TX
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
Qo}vnload __ Regder
----- -- -------- - -- -- --
i strongly believe that minors should not be allowed to tan at all underage tanning should be banned.
Also i think tanning salons should post warnings and posters of what to look for in moles that may be
cancerous. I tanned from the age of 16 until this past year when i was diagnosed with melanoma at the
age of23. I was rarely in the sun for long periods oftime due to the texas heat so i went to tanning beds
to get that glow. I disagree that tanning beds are safe, just like cigarettes not everyone will get cancer
from them but there are a hand full that wilL The people at the tanning salon would tell me tanning is
good for you its safer than the sun. I would see old women come into the salons that would have saggy
rough that was so brown and damaged and all they did was tan. It is so obviously dangerous just open
your eyes and see how many more cases of skin cancer is reported and how younger the the people are
getting. IT IS DANGEROUS and DEADLY!!!!!!! bellow is only one of my moles that was removed
that was from one summers growth of no mole to that and then what it looked like after they removed it.
That year was the first year that i went to the tanning salon everyday for 3 months until i noticed my
mole doubling tripling than i stopped thats three months grow!!!! you cannot prove me other wise that
tanning beds are bad
http://www. ftc. gov I osl comments/ indoortanningassoc/ 546631 -00061 .htm 2/24/2010
e
e
:,4o631 -UU05U.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00050
2/10/2010
Sally Robertson
CA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3 159
- --------- . - ----------------
I urge you to ban Indoor tanning machines! The public is not aware of the risks, nor has the the
manufacturers disclosed the risk of melanoma, and other skin cancers.
http://www .ftc.gov/oslcomments/indoortanningassoc/546631-00050.htm
2/24/2010
546631-00021.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00021
1/27/2010
Anna Ryan
AAD
NH
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
.. - ~ ........ .. ~ ~
Comments:
I am a dermatologist in private practice in NH. I'm writing to show my support for the consent order and
express my appreciation for the agency's efforts to protect the public from the deceptive practices of the
ITA. I was involved with some successful legislation in NH a few years back to limit access of minors
to tanning booths. Anything we can do to help disseminate accurate information will work towards true
"informed consent." thank you!
http://www .ftc.gov/os/comrnents!indoortanningassoc/546631-00021.htm
2/24/2010
)4bbJ l-UUU6U.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
RuJe:
No Attachments
546631-00060
2/15/2010
Jeannie Thornberry
MO
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
~ ~ . . . ~ ~ ~ ~ . ~ - --------
Comments:
I fully support the Fair Trade Commission's proposed settlement with the Indoor Tanning Associationt t
http://www. ftc. gov I os/ cornments/indoortanningassoc/546631-00060 .htm
2/24/2010
.J'tuuJ 1-uuu 1 LllLJU
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00012
l /27/201 0
Calvin Treger
American Academy of Dermatology
WA
Federal Trade Commission
Page 1 ot 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No .. 082 3159
-- - ~ - -- ---- . . ~ . -- ----.. ---------- - - --------P ~ -- 0 - .. ----- --------"-- -
Comments:
Thank you for your attention and action in this matter.. Demonstrates how gvernment is supposed to
work!!
http://www .. ftc .. gov I os/ comments/indoortanningassoc/546631-000 12 ..htm
2/24/2010
J'+UU.) 1 -vvv 1 o .nun
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631 -00016
1/27/ 2010
Robert Walther
Columbia University
NY
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
---- ------
Comments:
I support this consent agreement and suggest that it be carried to the individual tanning parlors
http://www .ftc.gov/os/commentslindoortanningassoc/546631-00016.htm
2/24/2010
J'"tVV.J 1-VVVVL.Illlll
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00002
1/26/2010
Christopher Whitley
CA
Federal Trade Commission
.Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
- - . ----- - ------- - -------- - -
Comments:
In regards to the FTC's settlement with the Indoor Tanning Association, I would like to explain my
disappointment in the FTC's position, it's remedies, and it's Consumer Alert. It's unfortunate that the
FTC has decided to confuse the difference between overexposure, i.e. burning, and mere exposure in a
non-burning fashion, which may or may not lead to a cosmetic tan. By doing so, the FTC, has joined in
with the pharmaceutical industry, some dermatologists, and special interests group, in confusing the
public about healthy exposure to UV. The notions that UV exposure in a non-burning fashion, getting a
cosmetic tan in a non-burning fashion, and that tanning increases your risk to skin cancer, are all
misleading in themselves. In the history of science there has never been a study to question whether
mere exposure to UV in a non-burning fashion leads to any adverse affects. Additionally, by using the
2009 report by the IARC, the FTC has overlooked a very important fact that the IARC itself makes
plainly clear: the elevation of indoor tanning units to category 1 does not specify quanity of exposure.
Just like all the other category 1 items, sunlight, alcohol, mineral oil, salted fish, arsenic, etc. quantity of
exposure is never explained. This is the problem with relying on the IARC. I suppose we should stop
drinking a glass of red wine for heart health and stop using most cosmetics, including SPF, which
contain mineral oil or derivatives, petroleum jelly, petrolatum, etc. Furthermore, suggesting 10-15
minutes of outdoor exposure to face and hands is a bold claim to be made by the FTC since thi s measure
is not scientifically proven and is currently debated amongst scientists. Food sources listed in the
consumer alert do not give sufficient amounts and do not give the proper type of vitamin D (vitamin D2
vs vitmain D3 made from UV exposure). Blood serum levels and proper amounts ofvitmain Dare
currently being debated by the scientific community. So claiming very minimum exposure to hands and
feet from outdoors and poor food sources is an overtly inappropriate claim to be made by the FTC. In
conclusion, I would like to say that relying on the Cancer Society and Dermatological Society alone is
not doing due diligence especially considering the growing number of scientists, medical doctors, and
yes, dermatologists, who are fmding that vitamin 0 levels are too important to completely avoid UV
exposure. Even the ACS has admonished the dermatologists for their staunch stance against UV
exposure. Getting moderate UV exposure from an indoor UV device from an indoor tanning salon for a
cosmetic tan in a non-burning fashion, for cosmetic skin conditions like psoriasis, eczema, and acne, for
chronic pain like fibromyalgia and back pain, for seasonal affectiveness disorder, and for many other
reasons should by an individual's choice. Please do not allow the FTC to take a stance on something that
the scientific community has not agreed upon and as science is currently evolving.
http://www. ftc. gov/ os/ comments/indoortanningassoc/ 546631-00002 .htrn 2/24/2010
546631-00039.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00039
211/2010
Caresse Schweitzer
AZ
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
~ ---- -----
Comments:
I am submitting my comment to fully support the FTC action. At only 22 I was diagnosed with
squamous cell skin cancer on my nose. Because of this daignosis I underwent Moh's surgery and lost a
very large portion of my nose. Following the removal of the cancer, 1 had extensive reconstructive
surgery to repair my nose. After I went to the doctor they informed me that using the tanning beds was
most likely the cause of the cancer because I rarely sat in the sun. For the rest of my lite I will have a
daily reminder of this painful experience all to have a nice tan. For years, almost daily I used the tanning
beds. Each day I went, there was a large sign telling me how beneficial and healthy it was to use the
beds. Never once was a sign posted informing me that the bed could increase chances or cause cancer.
Very little knowledge is spread about skin cancer causes, dangers, etc. Therefore I was completely
unaware that I was endangering myself with each trip or what serious effects it could have. Because of
this cancer and surgery, I lost income because of the surgery and recovery, must return to the doctor
every six months for check-ups, suffer emotionally at a very young age because of my appearance and
scars, and constantly monitor my health closely for the rest of my life. Had they posted warnings and
possible dangers I would have been better able to make a healthy decision for myself to not use the beds,
better protect myself, and at least be aware of the risk I was taking. I only hope that information can be
provided for young people so they may not suffer like I did .
http://www .ftc.gov/os/comments/indoortanningassoc/546631-00039 .htm 2/24/2010
e
e
e
)466 j 1-00015 .htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00015
1/27/2010
Keeter Sechrist
IN
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
-------------------- ---
Comments:
I am a Dermatologist in private practice. I have been in practice for 25 years. The indoor tanning
industry has been very aggressive in marketing themselves to the public assuring that tanning beds can
provide a nsafe tann. They would often provide free tanning to cheer leaders in the local high schools to
further entice tanning within that peer group. They continued this type of publicity and enticement
despite the many studies proving quite the opposite. I complement the FTC for their actions in forcing
the Indoor Tanning Association to tell the truth about their product and its enormous health hazards .
http: //www.ftc.gov/os/comments/indoortanningassoc/546631-00015.htm
2/24/2010
546631-00006.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00006
1/27/2010
Cindy Smith
American Academy of Dermatology
MN
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
-- . -------------
Comments:
To whom it may concern, The evidence is indisputable. UV exposure increases skin cancer risk. Every
year the data to support this increases. The WH 0 supports this position. Yet the ITA continues to
expound on UV health benefits and characterize dermatologists as "Scare Doctors." A dermatologist has
NO financial incentive to keep a patient out of a tanning booth, in fact the opposite is true. More skin
cancers mean more business. Contrarily the IT A and its members has tremendous incentive to do
anything in its power, no matter the legal, moral or ethical considerations to keep people tanning; indeed
it is their livelihood. In a recent lecture I wrote on skin cancers I scoured the available research for data
to support that tanning booths increased skin Vitamin D production and more importantly, serum
vitamin D levels. I could not find it. Depending on the wavelength emmitted, a tanning booth may have
no effect at all on vitamin D production. Vitamin D health benefit claims are in flux and in may
instances, based on anectode rather than sound data. Even if we assume that every health benefit
suggested is true the data that using a tanning booth will achieve them does not exist. Tanning booth use
increases skin cancer risk, including melanoma. That data exists in spades. I strongly support that the
FTC demand the IT A cease and desist propogating false claims and nonexistent data and warn people
that the very activity that they want people to pursue (tanning) has an extremely high likelihood of
contributing to the development of skin cancer, and in fact, could lead to their deaths. Respectfully,
Cindy Firkins Smith, MD Dermatologist, Affiliated Community Medical Centers. Adjunct Professor,
Department of Dermatology, University of Minnesota
http://www. ftc. gov/ osl comments/indoortanningassoc/ 546631-00006.htm 2/24/2010
e
546631-00053.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00053
2/ 10/2010
Sally Soffa
PA
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
I have malignant melanoma. Please help prevent others from getting it.
http://www.ftc.gov/os/comments/indoortanningassoc/ 546631-00053.htm
2/24/2010
54663 1-UU022.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
Comments:
546631-00022
1/27/2010
Stone
MO
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
-- ------------ ------------------------
Hooray!! Finally there is recognition from authoritative bodies and will be made public knowledge what
dermatologists have known for years that UV radiation (the sun) from tanning booths causes skin
cancer!! Our country is in a health care crisis. If we want to cut down health care spending, we need to
reduce the #1 cancer in humans: skin cancer. This is a victory first step in doing so. I appreciate the
FTC's efforts in helping to stop the tanning parlors from false advertising and claims (get a "healthy"
tan, get all your vitamin D with tanning, etc, etc.). Public safetly should be #1 priority; as we know
tanning causes skin cancer, including melanoma the most deadly type of skin cancer, advanced
wrinkling and leathery skin, eventually closing all such tanning parlors should be the next goal! Thank
you .
http://www.ftc.gov/oslcomments/indoortanningassoc/546631-00022.htm 2/24/2010
54663 l-OOUJ2.htm
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00032
1/29/2010
Trevor Thompson
HI
Federal Trade Commission
Page 1 of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
~ -------------- -~ -- ~ ~ .. ~ ~ ----- ___________________________ .. -
Comments:
Given the significant long term damage to the skin along with the increased risks of skin cancers and
melanoma including death, we should strongly declare these risks with strongly worded claims. We
have to long let our population especially those under 18 be exposed to radiation without proper
education, consent, supervision. Additionally, the lack of sanitary cleaning of the equipment exposes
them to further risks of infection .
http://www. ftc.gov/os/comments/indoortanningassoc/ 546631-00032.htm
2/24/2010
..!'"tVVJ! -VVV'"tL..IIUU
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00042
2110/2010
Elizabeth Wigginton
TX
Federal Trade Commission
Page I of 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
--------- - ----
------- -------- -- -- - - ---
Comments:
I agree completely that indoor tanning ads are deceptive and unhealthy! They have taken scientific data
regarding the benefits of vitamin D out of context and misled the public .
http://www.ftc.gov/os/comments/indoortanningassoc/546631-00042.htm
2/24/2010
J '"1"VVJ J - VVVL.J.Hllll
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00025
1128/2010
Wish
TX
Federal Trade Commission
!'age 1 ot 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
- - - - - - - - - - - - - - - - ~ - - - - - - - - - - - -w--------------
------------- ---------- --
Comments:
There are TONS of tanning businesses that advertise crazy things in my area!
http :I l www. ftc. gov I os/ comments/indoortanningassoc/ 546631-00025 .htm
2/24/2010
_, 1VV..JJ.-VVV1./.1.lUU
Comment
Number:
Received:
Commenter:
Organization:
State:
Agency:
Rule:
No Attachments
546631-00019
1/27/2010
Robert Wright
Denver Dermatology Consultants, PC
co
Federal Trade Commission
Page I ot 1
Proposed Consent Agreement In the Matter of the Indoor Tanning Association;
FTC File No. 082 3159
----- --- - ------------
Comments:
Over the years I have seen many patients with severe ultraviolet damage from the use of tanning
facilities. It is the people most at risk for skin cancer (light skinned individuals) who tend to use these
facilities under the mistaken impression that the tanning facility will decrease their risk of skin cancer. I
applaud the recent ruling requiring notification to the public about the risk involved with using these
facilities .
http://www.ftc.gov/os/comments/indoortanningassoc/54663 1-000 19 .htrn
2/24/2010
0[[1
AUGUSTA
DERMATOLOGY
ASSOCIATES, P.C.
Avis Brown Yount, M.D.
D IPLOMATE
American Board of
Dermatology
FELLOW
American Col lege of MOHS
Micrograph<c Surgery and
Cutaneous Oncology
PeterS. Yount, M.D.
DiPLOMATE
American Board of
Dermatology
Marshall A. Guill, M.D.
DIPLOMATE
American Board of
Dermatology
Karen C. Parviainen, M.D.
DIPLOMATE
American Board of
Dermatology
820 St. Sebastian Way
Su ite 6-C
Augusta Georgia
3090 1
Fax (706) 722-4298
Phone (706i 722-4280
465 North Belair Rd.
Suite 3-F
Evans Georgia
30809
Fax (706) 868-1749
Phone (706) 722-4280
February 2, 2010
Federal Trade Commission
Office of Secretary, Room H/135 (Annex D)
600 Pennsylvania Avenue, N. W.
Washington, D.C. 20580
Re: Indoor Tanning Association- Consent: FTC File#. 0823159
Dear Sir:
Thank you so much for your support for the consent order barring the
tanning association from continuing to make false and deceptive claims
about the health and safety benefits of indoor tanning. Hopefully, this will
help initiate a behavior change with respect to UV A radiation exposure
particularly in our young population and prevent skin cancers in the future.
Thank you for your efforts .
Sincerely,
ti2 ifwu- 11--P
A vis B. Yount, Mn.
ABY, MD/ld
Case# 4921 (10/24/08)
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Advertising Agency: Undisclosed
Challenger: National Advertising Division
-- Health and safety claims must be substantiated by competent and reliable
scientific evidence.
-- It is well-established that claims that are literally true may, depending upon the context
in which they appear, convey a message that is misleading to consumers.
Basis of Inquiry: As part of its routine monitoring program, NAD requested substantiation for
certain health and safety claims made by the Indoor Tanning Association for its print and website
advertising concerning the safety of tanning. The advertiser, in a full-page newspaper
advertisement, made the following express claims:
"TAJ\TNING CAUSES MELANOMA. HYPE."
"Recent research indicates that the benefits of moderate exposure to sunlight outweigh
the hypothetical risks. Surprisingly, there is no compelling scientific evidence that
tanning causes melanoma. Scientists have proven, however, that the exposure to all
forms of ultraviolet light - both indoors and out - stimulates the natural production of
Vitamin D. And research has shown that vitamin D protects against many types of
cancer, in addition to providing other important health benefits. "
"It's time to rethink sunbathing. "
NAD also requested substantiation for the following implied claims:
There is no evidence linking sunbathing (tanning) to the development of cancer.
Exposure to ultraviolet light provides health benefits and poses no health risks.
Advertiser's Position:
The advertiser is the Indoor Tanning Association, a professional association of tanning bed
owners. In response to NAD's request for substantiation, the advertiser submitted three articles
from the Proceedings of the National Academy of Science of the United States of America, the
National Health Institutes and the New England Journal of Medicine, all on the benefits of
Vitamin D on human health.
1
Vitamin D is a fat-soluble vitamin that is naturally present in very
few foods, added to others, available as a dietary supplement and produced endogenously when
ultraviolet rays from sunlight strike the skin.
1
After the initial submission, all follow-up requests for clarification and more infom1ation by NAD were repeatedly
ignored by the advertiser.
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page2
According to the advertiser, support for the statement "recent research indicates that the benefits
of moderate exposure to sunlight outweigh the hypothetical risks" comes from an article in the
Proceedings of the National Academy of Science of the United States of America (National
Academy Article), which determined that the risks of not getting enough vitamin D through sun
exposure outweighed the potentially negative health effects. The advertiser specifically pointed
to a passage in the abstract:
These data, together with those for internal cancers and the beneficial effects of an
optimal vitamin D status, indicate that increased sun exposure may lead to improved
cancer prognosis and, possibly, give more positive than adverse health effects.
So far, epidemiological data for cancer argue for an overall positive role of sun-induced
vitamin D. There may be more beneficial than adverse effects of moderately increased
sun exposure, even for total cancer mortality.
2
The advertiser also cited to a" 1999 study, British Medical Journal "
3
"There is evidence that the potential benefits of exposure to sunlight may outweigh the
widely publicised adverse effects on the incidence of skin cancer" and "for many people
the small absolute increase in risk of melanoma could easily be outweighed by the effect
of reduced sunlight on mood. "
4
The advertiser also maintained that the fact that numerous epidemiological studies have failed to
demonstrate any correlation between tanning and melanoma supported its claim that
"surprisingly, there is no compelling scientific evidence that tanning causes melanoma." The
advertiser claimed that in 2007, Dr. A. Bernard Ackennan, who was awarded the distinction of
Master Dermatologist by the American Academy of Dermatology in 2004, wrote in "Sun and the
Epidemic ofMelanoma:"
Data in opposition to the claim that tanning bed/sun lamps are responsible for inducing
melanoma are convincing sufficiently that we are forced to infer that such an association
has yet to be proved. In short, use of tanning beds has not in itself been demonstrated
2
Moan, Johan, et al, Addressing the health benefits and risks, involving vitamin D or skin cancer, of increased sun
exposure, 10 PNAS 668 (2008)(published in 2008 by the National Academy of Sciences of the USA).
3
The advertiser did not respond to requests for a copy of the study or even the name of the study, however, NAD
believes that it is, Ness, Andrew R, et at, Are We Really Dying For a Tan, 319 BMJ 114 (1999). This article also
goes on to state that any advice to increase sun exposure is premature.
4
The advertiser also cited an undated newspaper atticle in the "Daily Telegraph" about the 1999 British Medical
Journal study "The Bristol team of epidemiologists says that avoiding the sun will do little to decrease an
individual ' s risk of malignant melanoma, the most deadly of the three types of skin cancer, though it might improve
the national statistics for the disease."
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page3
compellingly to result in melanoma. The examples hyped as being representative are all
anecdotal.
5
The advertiser referred to the National Institutes of Health to support its assertion that "scientists
have proven, however, that exposure to all forms of ultraviolet light- both indoors and out-
stimulates the natural production of vitamin D:"
Sun exposure is perhaps the most important source of vitamin D because exposure to
sunlight provides most humans with their vitamin D requirement. UV rays from the sun
trigger vitamin D synthesis in skin. Season, geographic latitude, time of day, cloud
cover, smog, and sunscreen affect UV ray exposure and vitamin D synthesis. For
example, sunlight exposure from November through February in Boston is insufficient to
produce significant vitamin D synthesis in the skin.
6
With regard to the claim "and research has proven that vitamin D protects against heart disease
and many types of cancer, in addition to providing other important health benefits," the
advertiser maintained that the article in the National Academy Article outlined the role vitamin D
plays in fighting many cancers, thus their conclusion. Additionally, Dr. Michael Holick wrote in
a seminal review published in the New England Journal oflvfedicine:
Of great interest is the role it [vitamin D] can play in decreasing the risk of many chronic
illnesses, including common cancers, autoimmune diseases, infectious diseases, and
cardiovascular disease.
The advertiser denied that its advertisement reasonably conveys the implied message that "there
is no scientific evidence linking sunbathing (tanning) to the development of skin cancer" or
"exposure to ultraviolet light provides health bent;fits and poses no health risks." The advertiser
maintained that it very plainly addressed melanoma, never mentioning the term "skin cancer." In
the advertiser's view, neither the text nor image of the advertisement allude to the generic term
"skin cancer," which would include the most common and least threatening forms of skin cancer
in addition to deadly melanoma. Furthermore, the advertiser argued that the advertisement does
not claim that there are "no health risks" associated with tanning and that "unfounded, absolute
statements are the very problem the ad speaks out against." Finally, the advertiser asserted that
"if there is an 'implied claim' to the ad, it is that the health risks of tanning widely reported in the
media are overstated and the benefits are largely ignored."
Decision
When a matter is before NAD as a part of its routine monitoring program there is no challenger
to counter the advertiser's evidence or interpretation of the evidence. Therefore it is incumbent
upon NAD to critically review the record and take notice of relevant uncontroverted facts that
exist in the public sphere to place the advettiser's arguments into the proper context.
5
Requests for a copy of this publication were not answered.
6
See http://ods.od.nih.gov/factsheets/vitamind.asp.
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page4
Although there is evidence that some skin cancers are inherited, according to the American
Cancer Society and the American Academy of Dermatology, sun exposure is the leading cause
of skin cancers.
7
The American Cancer Society states that "many of the more than 1 million skin
cancers diagnosed each year could be prevented with protection from the sun's rays,"
8
which is
comprised of UV A and UVB rays.
Three types of skin cancer account for nearly 100% of all diagnosed skin cancer cases. Basal
cell carcinoma (BCC), the most common cancer, develops in the cells located in the lowest layer
of the epidermis.
9
Most BCCs appear on skin with a history of exposure to the sun, such as the
face, ears, scalp, and upper trunk. While these tumors very rarely metastasize, dermatologists
encourage early diagnosis and treatment to prevent extensive damage to surrounding tissue.
Squamous cell carcinoma (SCC) accounts for approximately 16% of diagnosed skin cancers and
requires early treatment to prevent metastasis.
Cutaneous malignant melanoma (CMM), accounting for about 4% of all diagnosed skin cancers,
begins in the melanocytes cells within the epidermis that give skin its color. Melanoma has been
coined "the most lethal form of skin cancer" because it can rapidly spread to the lymph system
and internal organs. In the United States alone, approximately one person dies from melanoma
every hour. With early detection and r o p r treatment, the cure rate for melanoma is about 95%.
Once it spreads, the prognosis is poor.
0
More than 1 million nonmelanoma skin cancers are diagnosed each year. If current trends
continue, l in 5 Americans will develop skin cancer during their lifetime. Melanoma continues
to rise at an alarming rate. In 1930, 1 in 5,000 Americans was likely to develop melanoma
during their lifetime.
11
By 2004, this ratio jumped to 1 in 65. Today, melanoma is the second
most common cancer in women aged 20 to 29.
12
It is well established that sun protection will significantly decrease a person's risk of developing
skin cancer, including applying a broad-spectrum sunscreen that offers UV A and UVB
protection with a sun protection factor (SPF) of 15 or higher year-round to all exposed skin, and
wearing a protective clothing, such as a wide-brimmed hat and sunglasses when outdoors.
13
Tanning beds also deliver UV A and UVB rays, although the overall health consequences of
tanning beds is not as well documented as that of exposure to natural solar radiation. However,
an article in the International Journal of Cancer systemically reviewed and synthesized the
corpus of studies through March 2006 on the available evidence of the association between
7
http://www.skincarephysicians.com/skincancemet/whatis.html (between 5% and 10% of melanomas develop in
people with a family histoty of melanoma).
8
Id.
9
Td.
10
All other skin cancers combined account for less than I % of diagnosed cases. These are classified as
nonmelanoma skin cancers and include Merkel cell carcinoma, dermatofibromasarcoma protuberans, Paget's disease
and cutaneous T-celllymphoma.
I I Td.
12 Td.
13 Id.
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
PageS
sunbed use, CMM and other skin cancers.
14
Only epidemiogical and biological studies case-
controlled, cohort or cross-sectional studies were selected.
15
Studies used for the meta-analysis
included a total of 7,355 cases in 19 studies, published mostly in Scandinavian countries and the
United States.
16
The systematic review of the published studies revealed an association of age at first use of less
than 35 years of age with melanoma risk. This is also in agreement with the finding that UV
exposure in childhood is an important contributing factor for melanoma risk in adulthood. In the
Norwegian Scandinavian studies, the highest risk for melanoma was found in women who used
indoor tanning equipment at least once per month between the ages of 20-29 years of age. The
article concluded that on balance, the evidence pertaining to the association of the use of indoor
tanning equipment before the age of 35 supports a causal relationship melanoma risk and that
more studies are required to allow for more definitive conclusions.
I. The Advertiser's Science
Vitamin D, which om skin synthesizes when exposed to ultraviolet light, unquestionably plays
an important role in human health. The advertiser's argument is that sunbathing or tanning is
necessary to achieve a healthy vitamin D status. It is well settled that health and safety claims
must be substantiated by competent and reliable scientific evidence.
17
As the advertiser bears the
burden of establishing a reasonable basis for its claims, NAD thoroughly reviewed the articles
submitted by the advertiser.
A. National Institutes of Health Article
The NIH Article is a primer on the role that vitamin D -- a fat-soluble vitamin that is natw-ally
present in very few foods, added to others, available as a dietary supplement and is produced
endogenously when ultraviolet rays from sunlight strike the skin -- plays in human health.
18
Vitamin D is essential for promoting calcium absorption, bone growth and remodeling and
enabling normal mineralization of bones. Without sufficient vitamin D, bones can become thin,
brittle, or misshapen. Vitamin D sufficiency prevents rickets in children and osteomalacia in
adults and, together with calcium, helps protect older adults from osteoporosis.
19
14
international Agency for research on Cancer Working Group, The association of use of sun beds with cutaneous
melanoma and other skin cancers: A systemic review, 120 Int'l J. Cancer 1116 (2006).
15
1d. at 1116.
16
ld. at 1118.
17
Selmedical Healthcare, LLC (Zeta-Cap The Gastric by-Pass Pill), Repott #4477, NADICARU Case Reports (April
2006).
18
Vitamin D obtained from sun exposure, food, and supplements is biologically inert and must undergo two
hydroxy1ations in the body for activation. The first occurs in the liver and converts vitamin D to 25-hydroxyvitamin
D [25(0H)D], also known as calcidiol. The second occurs primarily in the kidney and forms the physiologically
active 1 ,25-dihydroxyvitamin D [ 1 ,25(0H)
2
D], also known as calcitriol.
19
Vitamin D has other rol es in hwnan health, including modulation of neuromuscular and immune function and
reduction of inflammation. Many genes encoding proteins that regulate cell proliferati on, differentiation, and
apoptosis are modulated in part by vitamin D. Many laboratory-cultured human cells have vitamin D receptors and
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page6
According to the NIH article, season, geographic latitude, time of day, cloud cover, smog, skin
melanin content, and sunscreen are among the factors that affect UV radiation exposure and
vitamin D synthesis. The UV energy above 42 degrees north latitude (a line approximately
between the northern border of California and Boston) is insufficient for cutaneous vitamin D
synthesis from November through February; in far northern latitudes, this reduced intensity lasts
for up to 6 months. Latitudes below 34 degrees north (a line between Los Angeles and
Columbia, South Carolina) allow for cutaneous production of vitamin D throughout the year.
Sunscreens with a sun protection factor of 8 or more appear to block vitamin D-producing UV
rays. However, the NIH article pointed out that in practice people generally do not apply
sufficient amounts, cover all sun-exposed skin, or reapply sunscreen regularly. As typically
applied, skin likely synthesizes some vitamin D even when it is protected by sunscreen.
The factors that affect UV radiation exposure and research to date on the amount of sun exposure
needed to maintain adequate vitamin D levels make it difficult to provide general guidelines. It
has been suggested, for example, that approximately 5-30 minutes of sun exposure between 10
a.m. and 3 p.m. at least twice a week to the face, arms, legs, or back without sunscreen usually
lead to sufficient vitamin D synthesis and that the moderate use of commercial tanning beds that
emit 2-6% UVB radiation is also effective. Individuals with limited sun exposure need to include
good sources of vitamin Din their diet or take a supplement.
Despite the importance of the sun to vitamin D synthesis, the NIH article warned against the
dangers of tanning. It noted that UV radiation is a carcinogen responsible for most of the
estimated 1.5 million skin cancers and the 8,000 deaths due to metastatic melanoma that occur
annually in the United States and that lifetime cumulative UV skin damage is also responsible
for some age-associated dryness and other cosmetic changes. Currently, it is not known whether
a desirable level of regular sun exposure exists that imposes no (or minimal) risk of skin cancer
over time.
B. The New England Journal of Medicine Article
Like the NIH Article, the NEJM Article expounds upon on the role of vitamin D in human
health. Vitamin D from the skin and diet is metabolized in the liver to 25-hydroxyvitamin D,
which is used to determine a patient's vitamin D status. According to the article, although there
is no consensus on optimal levels of 25-hydroxyvitamin D, vitamin D deficiency is defined by
most experts as a 25-hydroxyvitamin D level of less than 20 ng per milliliter. A level of 25-
hydroxyvitamin D of 21 to 29 ng per milliliter can be considered to indicate a relative
insufficiency of vitamin D, and a level of 30 ng per milliliter or greater can be considered to
indicate sufficient vitamin D.
The NEJM article reported on several studies regarding possible vitamin D deficiency in
European and U.S. populations. One study claimed that 40 to 100% of U.S. and European
elderly men and women still living in the community (i.e. , not in nursing homes) are deficient in
vitamin D. More than 50% of postmenopausal women taking medication for osteoporosis had
some convert 25(0H)D to 1 ,25(0H)
2
D. It remains to be determined whether cells with vitamin D receptors in the
intact human carry out this conversion.
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page7
suboptimal levels of 25-hydroxyvitamin D - below 30 ng per milliliter. Children and young
adults are also potentially at high risk for vitamin D deficiency. For example, 52% of Hispanic
and black adolescents in a Boston study and 48% of white preadolescent girls in a study in
Maine had 25-hydroxyvitamin D levels below 20 ng per milliliter. In anther study, at the end of
the winter, 42% of 15- to 49-year-old African American girls and women throughout the United
States had 25-hydroxyvitamin D levels below 20 ng per milliliter.
20
The article states that there are many causes of vitamin D deficiency, including reduced skin
synthesis and absorption of vitamin D and acquired and heritable disorders of vitamin D
metabolism and responsiveness. Recommendations from the Institute of Medicine for adequate
daily intake of vitamin D are 200 IU for children and adults up to 50 years of age, 400 IU for
adults 51 to 70 years of age, and 600 TU for adults 71 years of age or older. Most experts agree
that without adequate sun exposure, children and adults require approximately 800 to 1000 IU of
vitamin D supplements per day. Sensible sun exposure can provide an adequate amount of
vitamin D3, which is stored in body fat and released during the winter, when vitamin D3 cannot
be produced. Exposure of arms and legs for 5 to 30 minutes, depending on time of day, season,
latitude, and skin pigmentation, between the hours of 10 a.m. and 3 p.m. twice a week is often
adequate.
C. National Academy Article
The purpose of the National Academy Article was to address the health benefits and risks of
vitamin D production and increased sun exposure. Accordingly, the authors weigh-in on the
positive causal connection between sun exposure and cutaneous malignant melanoma (CMM):
[I]n our opinion, a significant fraction of CMMs is related to sun exposure. The
main arguments for this relationship are: (i) the north- south gradients in CM-M
incidence between Scandinavia and Australia, (ii) before the advent of the "top-
less" fashion, few women developed CMM on the breast area (13, 16), and (iii) in
some animals (Sinclair swine, Monodelphis domestica, the fish Xiphophorus,
white horses, angora goats, transgenic mice, etc.) UV exposure leads to CMM.
20
As similarly expressed in the NlH Article, the authors here briefly explain the benefits of Vitamin D: Without
vitamin D, only 10 to 15% of dietary calcium and about 60% of phosphorus is absorbed. 1n one study, serum levels
of 25-hydroxyvitamin D were directly related to bone mineral density in white, black, and Mexican-American men
and women. Without an adequate calcium-phosphorus product (the value for calciwn times the value for serum
phosphorus), mineralization of the collagen matrix is diminished, leading to classic signs of rickets in children and
osteomalacia in adults. Vitamin D deficiency also causes skeletal muscle weakness.
Vitamin D also plays an important role in nonsketal health. Brain, prostate, breast, and colon tissues, among others,
as well as immune cells have a vitamin D receptor and respond to 1,25-dihydroxyvitamin D, the active form of
vitamin D. Tn addition, some of these tissues and cells express the enzyme 25-hydroxyvitamin D-1 a-hydroxylase.
Directly or indirectly, I ,25-dihydroxyvitamin D controls more than 200 genes, including genes responsible for the
regulation of cellular proliferation, differentiation, apoptosis, and angiogenesis. Tt decreases cellular proliferation of
both nom1al cells and cancer cells and induces their terminal differentiation.
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
PageS
The reason that CMM incidence rates decrease with decreasing latitude in Europe
is likely because of differences in skin color from region to region?
1
The article explained that sun exposure is a main source of vitamin D but also that "solar
radiation is the main cause of skin cancers. "
22
According to the article, for years, emphasis has
been placed on the increasing time trends of incidence and mortality rates of cutaneous
malignant melanoma (CMM) and, in contrast, on the protective role of vitamin D regarding
many types of internal cancer and other diseases. The observation that the incidence and
mortality of several types of internal cancers decreases with decreasing latitude in the United
States and other countries initiated the research on vitamin D-cancer relationships in the 1980s
and 1990s. However, in some cases, there is an inverse gradient of the rates of internal cancer
with latitude ( l ), with the rates being higher in regions with high annual UV tluences (New
Zealand and Australia) than in countries with low annual UV fluences (Northern Europe,
Scandinavia, and the U.K.), despite the fact that the populations of these regions are closely
related genetically or, at least, have similar skin types, which is important for the photosynthesis
ofvitamin D.
The article took the position that "these issues have health consequences far beyond those of
cancer because a number of diseases are associated with inadequate vitamin D levels or low sun
exposure: neurological, cardiovascular, metabolic, immune, and bone diseases." The authors
concluded that in view of the supposedly long latency times for cancer manifestation, decades
are needed for fmal evaluation of the impacts of the anti sun campaigns with respect to melanoma
incidence, cancer prognosis, and other possible positive or adverse health effects and that
"authorities should pay attention not only to skin cancer research, but also to research on vitamin
D-sun- health relationships occurring worldwide. "
23
T. Express Claims
As a preliminary matter, NAD determined that the advertiser incorrectly conflates the terms
"sunbathing" and "tanning" with "sun exposure."
24
Tanning and sunbathing, undertaken to
cause a browning of the skin, require prolonged exposure to ultraviolet radiation. Sun exposure,
on the other hand, can include very limited amounts of time. On this record it appears that there
is no hard consensus about how much time in the sun is recommended to meet vitamin D
requirements - from 0 minutes intentional exposure because, as typically applied, skin likely
synthesizes some vitamin D even when it is protected by sunscreen, to 5-30 minutes exposure of
the rums and legs twice a week - but certainly sunbathing/tanning or prolonged exposure was not
considered by any article to be healthful. Nor is prolonged exposure to the sun necessary to
produce an adequate amount if Vitamin D. Indeed, the advertiser's best evidence, the National
Academy Article, is a call to explore the sun-cancer-vitamin D relationships and in no way
21
Moan, Johan, et al , Addressing the health benefits and risks, involving vitamin D or skin cancer, of increased sun
exposure, 10 PNAS 668, 688 (2008)(published in 2008 by the National Academy of Sciences ofthe USA).
22 /d.
23
!d. at 673.
24
Merriam Webster Dictionary at www.m-w.com.
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page9
recommends tanning or sunbathing. Furthermore, all articles recognize that vitamin D
deficiencies may also be addressed by supplements.
Most importantly, however, each and every article submitted by the advertiser acknowledged
that UV radiation is a carcinogen responsible for skin cancers, including a significant portion of
CMMs. For example, the NIH Article cautions that
Despite the importance of the sun to vitamin D synthesis, it is prudent to limit
exposure of skin to sunlight. UV radiation is a carcinogen responsible for most of
the estimated 1.5 million skin cancers and the 8,000 deaths due to metastatic
melanoma that occur annually in the United States.
The NEJM Article states that
Excessive exposure to sunlight, especially sunlight that causes sunburn, will increase the
risk of skin cancer. Thus, sensible sun exposure (or ultraviolet B irradiation) and the use
of supplements are needed to fulfill the body's vitamin D requirement.
The National Academy Article states emphatically that "in our opinion, a significant fraction of
CMMs is related to sun exposure." Indeed, the ultimate conclusion of the National Academy
Article was that policy makers should be cognizant of the risks of skin cancer and also that more
research needs to be conducted on vitamin D over the next several decades. Finally, there is
competent and reliable emerging evidence in the International Journal of Cancer that indoor
tanning and the use of sunbeds is associated with melanoma risks when used by people under the
age of35.
As all of the advertiser's evidence unanimously refers positively to the causal link between
sunbathing/tanning and melanoma, NAD find that the advertiser's evidence is insufficient to
substantiate its claims that the link between them are "hype," "hypothetical" and that there is a
lack of "compelling scientific evidence" linking sun tanning to the development of melanoma.
Given the absence of competent and reliable scientific evidence supporting the advertiser's
claims,
25
NAD recommended that the advertiser discontinue the claims that "TANNING
CAUSES MELANOMA. HYPE," "recent research indicates that the benefits of moderate
exposure to sunlight outweigh the hypothetical risks," "surprisingly, there is no compelling
scient(fic evidence that tanning causes melanoma," and "it's time to rethink sunbathing," NAD
recommended that these claims be discontinued.
II. Implied Claims
The advertiser did not contest the fact that UV rays are a cause of basal and squamous cell
cancers. Instead, its argument is that neither the text nor image of the advertisement alludes to
the generic term "skin cancer." The advertiser failed to submit evidence on this point and
25
Selmedical Healthcare, LLC (Zeta-Cap The Gastric by-Pass Pill), Report #4477, NAD/CARU Case Reports (April
2006).
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page 10
therefore NAD used its own expertise to determine the reasonable take away from the challenged
claims.
It is well-established that claims that are literally true may, depending upon the context .in which
they appear, convey a message that is misleading to consumers and that advertisers are
responsible for all reasonable interpretations of their claims?
6
For example, an advertisement
making an accurate claim that a product contains no CFCs may nevertheless misleading if the
product contains other volatile chemicals?
7
Similarly, here, the advertiser highlights the fact that
sun light is an excellent source of vitamin D, while deriding the notion that sunlight is the main
carcinogen responsible for skin cancers. Further, NAD detennined that consumers are unlikely
to appreciate the difference between basal, squamous cell cancers and CMMs because they are
medical, rather than common pace, terms. Therefore, a reasonable take away message from the
claim that there is no evidence that tanning causes melanoma is that there is no proven link
between sunbathing and skin cancers. Moreover, the advertiser's own evidence suggests a link
between UV exposure and melanoma.
The advertiser further argued that it does not claim that there are "no health risks" associated
with tanning and that "unfounded, absolute statements are the very problem the ad speaks out
against." However, the advertisement very clearly states that risks associated with tanning are
"hypothetical" and that there is no compelling scientific evidence that links tanning to skin
cancer, which, again, are unfounded and unsupported statements. NAD determined that the
claims that "scientists have proven, however, that the exposure of all forms of ultraviolet light -
both indoors and out - stimulates the natural production of Vitamin D," and "research has
shown that vitamin D protects against many types of cancer, in addition to providing other
important health benefits, " while literally true, are confusing in the context of this advertisement
in that they reasonably convey the message that there is no evidence linking sunbathing (tanning)
to the development of cancer and exposure to ultraviolet light provides health benefits and poses
no health risks.
NAD is appreciative of the challenges facing advertisers in communicating what is often
complex scientific information in relatively brief advertising messages. NAD also recognized
that there is an honest scientific debate emerging in the public eye regarding vitamin D
deficiency and sun exposure which is clearly an important health topic of material interest to
consumers. However, the challenged advertisement overstates the benefits of Vitamin D
obtained through sun exposure and dismisses as hype the well-established causal relationship
between UV exposure and the development of skin cancer..
The claims that "scientists have proven, however, that the exposure of all forms of ultraviolet
light - both indoors and out - stimulates the natural production of Vitamin D," and "research
has shown that vitamin D protects against many types of cancer, in addition to providing other
important health benf!fits, " while literally true, are confusing in the context of this advertisement
in that they convey the false message that unlimited sun exposure is healthy and poses no risks
and, as such, NAD recommended that these claims be discontinued.
26
See Earth, Tnc., (Earth Brand Footwear), Report # 4896, NADICARU Case Reports (August 2008).
27
Nuclear Energy Institute (Nuclear Energy), Report # 3508, NAD!CARU Case Reports (November 1998).
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page 11
Conclusion: NAD found that the evidence in the record does not support the advertiser's
claims: "TANNING CAUSES MELANOMA. HYPE.," "Recent research indicates that the
benefits of moderate exposure to sunlight outweigh the hypothetical risks. Surprisingly, there is
no compelling scientific evidence that tanning causes melanoma" " and "It's time to rethink
sunbathing, " and recommended that they be discontinued.
NAD also found that the challenged advertisement conveyed an unsupported message that there
is no evidence linking sunbathing (tanning) to the development of cancer and exposure to
ultraviolet light provides health benefits and poses no health risks, and recommend that the
claims "scientists have proven, however, that the exposure of all forms of ultraviolet light - both
indoors and out - stimulates the natural production of Vitamin D. And research has shown that
vitamin D protects against many types of cancer, in addition to providing other important health
benefits" be discontinued. (closed 10/23/08 KAD).
Advertiser's Statement:
The Indoor Tanning Association (ITA) engaged in a public policy campaign to address an
ongoing important scientific debate about the health benefits and questionable risks of exposure
to one of our greatest natmal resources- sunlight. This debate about how sunlight helps our
bodies produce Vitamin D- which has unquestioned health benefits- has been widely covered
in the press. ITA exercised its right to engage in constitutionally protected free speech by
providing its opinions and truthful and substantiated information to policy makers, the public and
the press. NAD's opinion, in an area in which it has no jmisdiction or particular expertise,
serves no purpose other than to censor this scientific debate and suppress free speech.
NAD investigates "national advertising," which is a "paid commercial message" with the
purpose of "inducing a sale or other commercial transaction or persuading the audience of the
value or usefulness of a company product or service." IT A is not a commercial enterprise - it
sells no products or services. It is a non-profit trade association chartered to advocate, through
education and research, for responsible sun tanning via natural or artificial light. NAD's inquiry
into ITA's campaign, therefore, exceeds the boundaries ofNAD's mission: ITA did not engage
in commercial, national advertising, because it does not induce a sale nor does it promote
products or services. N AD should not interfere with IT A's efforts to educate policy makers, the
public and the press about the benefits of vitamin D and sunlight. Moreover, ITA's opinions and
statements are truthful and supported by increasing numbers of highly reputable and extensive
scientific studies, which have proven that vitamin D has significant health benefits; that people
benefit from UV exposure because it produces vitamin D in the body; and question whether there
is any link between moderate exposure to sunlight and the development of melanoma, a
particular form of skin cancer. Despite the conventional wisdom about the dangers of sunlight,
there is a countervailing health issue presented by the large number of the population that suffer
from vitamin D deficiency and therefore associated health risks and problems. Exposure to
sunlight can be an important remedy for Vitamin D deficiency.
INDOOR TANNING ASSOCIATION
Indoor/Outdoor Tanning
Page 12
For these reasons, ITA objects to NAD's attempted intrusion into this scientific debate and,
while it has no plans to run the "Tanning Causes Melanoma: Hype" piece that is the particular
focus of the NAD in any national publication in the future, it shall continue to engage in this
important debate. (#4921 KAD, closed 10/24/2008)
2008. Council of Better Business Bureaus, Inc.
NAD News
For Immediate Release
NAD EXAMINES ADVERTISING FROM
INDOOR TANNING ASSOCIATION
Contact: Linda Bean
212-705-0129
Recommends Trade Group Discontinue Claims Related to Health Benefits of Tanning
New York, NY - Nov. 3, 2008 - The National Advertising Division of the Council of Better Business
Bureaus has recommended that the Indoor Tanning Association discontinue advertising that
suggests tanning or sunbathing is necessary to achieve natural production of Vitamin D or conveys
the unsupported message that that there is no evidence linking tanning to the development of
cancer.
NAD, the advertising industry's self-regulatory forum, requested substantiation for certain health
and safety claims made by the Indoor Tanning Association in print and Website advertising. The
advertiser, in a full-page newspaper advertisement, made the following express claims:
"TANNING CAUSES MELANOMA: HYPE."
"Recent research indicates that the benefits of moderate exposure to sunlight outweigh the
hypothetical risks. Surprisingly, there is no compelling scientific evidence that tanning causes
melanoma. Scientists have proven, however, that the exposure to all forms of ultraviolet
light - both indoors and out - stimulates the natural production of Vitamin D. And research
has shown that vitamin D protects against many types of cancer, in addition to providing
other important health benefits."
"It's time to rethink sunbathing."
In response to NAD's request for substantiation, the association submitted three articles from the
Proceedings of the National Academy of Science of the United States of America, the National Health
Institutes and the New England Journal of Medicine, that address the benefits of vitamin D on human
health.
NAD noted that each of the articles, while addressing the importance of vitamin D and role of
sunlight in the production of vitamin D, warned against the role of UV radiation in producing certain
cancers.
NAD noted that it is "appreciative of the challenges facing advertisers in communicating what is
often complex scientific information in relatively brief advertising messages" and "recognized that
there is an honest scientific debate ... regarding vitamin D deficiency and sun exposure."
However, NAD stated, the challenged advertising overstates the benefits of vitamin D obtained
through sun exposure and dismisses as hype the well-established causal relationship between
ultraviolet light exposure and the development of skin cancer.
NAD found that the advertiser's evidence was insufficient to substantiate its claims that the link
between sunbathing and skin cancer is "hype," or "hypothetical" or the claim that there is a lack of
"compelling scientific evidence" linking sun tanning to the development of melanoma.
Given the absence of competent and reliable scientific evidence supporting the advertiser's claims,
NAD recommended that the advertiser discontinue the express and implied claims at issue.
In its advertiser's statement, the Indoor Tanning Association noted that it "objects to NAD's
attempted intrusion into this scientific debate and, while it has no plans to run the ' Tanning Causes
Melanoma: Hype' piece that is the particular focus of the NAD in any national publication in the
future, it shall continue to engage in this important debate."
NAD's inquiry was conducted under NAD/CARU/NARB Procedures for the Voluntary Self-Regulation of
National Advertising. Details of the initial inquiry, NAD's decision, and the advertiser's response will be
included in the next NAD/CARU Case Report.
###
About Advertising Industry Self-Regulation: The National Advertising Review Counci l (NARC) was formed i n 1971 by the
Association of National Advertisers, Inc. (ANA), the American Associat ion of Advertising Agencies, Inc. (AAAA), the American
Advertising Federation, I nc. (AAF), and the Council of Better Business Bureaus, Inc. (CBBB). Its purpose is to foster truth and
accuracy in national advertising t hrough voluntary self-regulation. NARC is the body t hat establ ishes the policies and
procedures for t he CBBB's National Advertising Division {NAD) and Chi ldren's Advertising Review Unit (CARU), as well as for
the National Advertising Review Board (NARB) and the Electronic Retailing Self-Regulation Program (ERSP).
NAD and CARU are the investigative arms of the advertisi ng industry's voluntary self-regulation program. Their casework
results from competitive challenges from other advertisers, and also from self-monitoring traditional and new media. The
National Advertisi ng Review Board (NARB), the appeals body, is a peer group from which ad-hoc panels are selected to
adjudicate those cases that are not resolved at the NAD/CARU level. This unique, self-regulatory system is funded entirely by
the business community; CARU is financed by the children's advertising industry, while NAD/NARC/NARB's sole source of
funding is derived f rom membershi p fees paid to the CBBB. ERSP's f unding is derived from membershi p in the Elect ronic
Retail ing Association. For more information about advertising self regulation, please visit www.narcpartners.org.
From: Colbert, Lynne J.
Sent: Thursday, April1 0, 2008 3:07PM
Evans, Janet M. To:
Subiect: RE: Website reoistration info
(b)(5)
-----Original Message-----
From: Evans, Janet M.
Sent: Thursday, April 10, 2008 12:00 PM
To: Colbert, Lynne J.
Subject: RE: Website registration info
www .theita.com
Janet M. Evans
Attorney, Division of Advertising Practices
Federal Trade Commission
NJ-3213
600 Pennsylvania Avenue, N.W.
Washington, D.C. 20580
(202) 326-2125 phone
(202) 326-3259 fax
jevans@ftc.gov
-----Original Message-----
From: Colbert, Lynne J.
Se nt: Thursday, AprillO, 2008 11:32 AM
To: Evans, Janet M.
Subject: RE: Website registration info
Send me the URL
-----Original Message-----
From: Evans, Janet M.
Sent : Thursday, April 10, 2008 11:30 AM
To: Colbert, Lynne J.
Subject: Websit e registration info
Is there any site now that is likely to give me useful info on the owner of a website? I looked
in whois and betterwhois and got next to nada.
Janet M. Evans
Attorney, Division of Advertising Practices
Federal Trade Commission
NJ-3213
600 Pennsylvania Avenue, N.W.
Washington, D.C. 20580
(202) 326-2125 phone
(202) 326-3259 fax
jevans@ftc.gov
Compli ance with federal and state legislati on by indoor tanning facilities in San Diego Page 1 of 1
More periodicals:
FIND A PERIODICAL
GO TO PRODUCT CATALOG
Regi ster or Login: Password: :::::J Auto-Login [Reminder]
Search This Periodical for
Advanced Search - MEDLINE - My Recent Searches - My Saved Searches - Search Tips
Vol ume 44, Issue 1, Pages 53-60 (January 2001)
Compliance with federal and state legislation by
indoor tanning facilities in San Diego
Carla A. Culley, MPH
8
, Joni A. Mayer, Ph0
8
, Laura Eckhardt, MPH
8
, April
J. Busic, MPH
8
, Lawrence F. Eichenfield, MOb, James F. Sallis, PhDb,
P.J.E. Quintana, Ph0
8
, Susan I. Woodruff, Ph0
8
Accepted 13 July 2000.
Abstract
Background: The prevalence rates of both skin cancers and indoor
tanning among the US population are high and have increased
substantially in recent years. Low compliance by indoor tanning facili ties
with safety regulations may place consumers at greater risk of skin and
ocular damage. Objective: Thi s study quantified the level of
compliance by indoor tanning facilities with selected federal and state
regulations and recommendations. Methods: Tanning faci li ties (N =54)
in San Diego County, California, were visited by a confederate posing as
a prospective customer. Compl iance with 13
regulations/recommendations were assessed by either direct query or
observation of the presence/absence of signs and warning labels.
Operators' responses to 5 risk-based questions also were noted.
Results: No facility complied with all 13 regulations/recommendations.
Compliance with 3 protective eyewear regulations was high (89%-
100%). In contrast, compliance with maximum tanning frequency
recommendations (approximately 6%) and parental consent regulations
(approximately 43%) was disturbingly low. Conclusion: The
investigators recommend instituting mandatory, comprehensive training
for operators, as well as systematic compl iance monitoring with
enforcement of penalties for noncompliance. (JAm Acad Dermatol
2001 ;44:53-60.)
San Diego, California
.. ABSTRACT
FULL TEXT
FULL-TEXT PDF (97 KB)
CITATION ALERT
CITED BY
RELATED ARTI CLES
EXPORT CITATION
EMAIL TO A COLLEAGUE
VIEW GENETIC INFO
RIGHTS/PERMISSIONS
NEED REPRINTS?
BOOKMARK ARTICLE
FULL TEXT ELSEWHERE
From the Graduate School of Public Health" and the Department of Psychology," San Diego State University, and the
Division of Pediatric Dermatology, University of California, San Diego School of Medicine and Children's Hospital and
Health Center, San Diegob
Reprint requests: Joni A. Mayer, PhD, Graduate School of Public Health, Hardy Tower #119,
San Diego State University, San Diego, CA 92182-4162.
JAm Acad Dermatol 2001 ;44:53-60.
Pll: S0190-9622(01 )92739-2
doi:10.1067/mjd.2001.11 0063
2001 American Academy of Dermatology, Inc. Published by Elsevier Inc. All rights reserved.
Copyright 2009 Elsevier, Inc. All rights reserved 1 Privacy Policy 1 Terms & Conditions 1 Feedback 1 About Us 1 Help 1 Contact Us 1
The content on this site is intended for health professionals.
http://www .eblue.org/article/SO 190-9622(0 1 )92739-2/abstract 9/22/2009
Access to commercial indoor tanning facilities by adults wit... : European Journal of Cane... Page 1 of 1
Europeanj ournal of Cancer Prevention:
October 2006 -Volume 15 - Issue 5 - pp 424-430
Research papers: Skin Cancer
Access to commercial indoor tanning facilities by
adults with highly sensitive skin and by under-age
youth: compliance tests at solarium centres in
Melbourne, Australia
Dobbinson, Suzanne; Wakefield, Melanie; Sam bell, Natalie
r-
. .
. .
i El l
Abstract
The study aimed to establish solarium operators' compliance with a newly revised voluntary
code for the industry in 2002. The revisions incorporate guidelines to ensure customers are
adequately informed of the risks associated with solarium use and that access by high-risk
groups, such as customers with fair skin that does not tan (skin type 1) or those less than 18
years of age, is limited or barred. Compliance tests with the industry standard were
conducted at 30 solarium centres in Melbourne, Australia. Compliance was tested by
surveys and in-person visits from three research assistants, each presenting as potential
customers but with different eligibility to attend a sunbed session: young adults eligible to
attend a solarium, young adults with skin type 1 and under-age (16 year old) customers. This
is the first study to assess solarium compliance using confederates with customer profiles
that correspond to the required restrictions on sunbed access. Results showed poor
l. compliance with specific aspects of the voluntary code. Fifty-two per cent of centres gave the ~
!::. underage teenagers access to sunbeds without written parental consent. Ninety per cent of ~ : :
centres provided sun bed access to clients with poor tanning ability and 75% of centres tried
I_ ~ ~ ~ ~ ~ ~ ~ ~ ~
2006 Lippincott Williams & Wilkins, Inc.
You currently do not have access to this article.
You may need to:
Register an account.
Login if you are a registered subscriber.
Subscribe to thisJ ournal , or
Purchase access to this article if you are not a current subscriber .
View this article in Ovid if your institution subscribes to this journal.
Note: If your society membership provides for full-access to this article, you may need to login
on your society's web site first.
http://journals.l ww .com/eurjcancerprev/ Abstract/2006/ 10000/ Access_to_commercial_indo... 9/22/2009
Compliance with restrictions on sale of indoor tanning sessions to youth in Minnesota and... Page 1 of 2
More periodicals:
FIND A PERIODICAL
GO TO PRODUCT CATALOG
Register or Login: Password: :::::J Auto-Login [Reminder]
Search This Periodical for
Advanced Search - MEDLINE - My Recent Searches - My Saved Searches - Search Tips
Volume 55, Issue 6, Pages 962-967 (December 2006)
Compliance with restrictions on sale of indoor tanning
sessions to youth in Minnesota and Massachusetts
Jean L. Forster, P h D a ~ DeAnn Lazovich, PhDa, Andrea Hickle, MPHb,
Glorian Sorensen, PhDc, Marie-France Demierre, MOd
Accepted 4 June 2006. published online 14 August 2006.
Background
Minnesota and Massachusetts requi re parental permission, for persons
younger than 16 or 18 years of age, respectively, for indoor tanning.
Objectives
This report examines business practices and characteristics associated
with sales of indoor tanning to underage girls.
Methods
Fifteen-year-old girls tried to purchase an ultraviolet tanning session in
200 indoor tanning businesses in the Minneapol is-St Paul and Boston
areas without parental consent. Business characteristics were recorded.
Later, businesses were intervi ewed by telephone about their facilities
and practices.
Results
Eighty-one percent of businesses sold a session to an underaged buyer
on at least one of two tries. Illegal purchases did not differ by state.
Businesses least likely to sell were larger, dedicated to indoor tanning,
required employee certification, and had a minimum age of sale for their
business. However, businesses in each of these categori es sti ll sold
tanning sessions to underaged adolescents at 44% to 62% of the visits.
Employees who requested parental consent or age identification almost
never sold a session.
Limitations
Businesses i n Minnesota and Massachusetts only were included.
Conclusion
Minnesota and Massachusetts laws specifying a minimum age of sale
for indoor tanning are ineffective.
Minneapolis, Minnesota, and Boston, Massachusetts
a From the Division of Epidemiology & Community Health
b Center for Public Health Education & Outreach, University of Minnesota, Mi nneapolis
.. ABSTRACT
FULL TEXT
FULL-TEXT PDF (105 KB)
CITATION ALERT
CITED BY
RELATED ARTICLES
EXPORT CITATION
EMAIL TO A COLLEAGUE
VIEW GENETIC INFO
RIGHTS/PERMISSIONS
NEED REPRINTS?
BOOKMARK ARTICLE
FULL TEXT ELSEWHERE
http://www .eblue.org/article/SO 190-9622(06)0 1840-8/abstract 9/22/2009
Compliance with restrictions on sale of indoor tanning sessions to youth in Minnesota and... Page 2 of 2
c Department of Society, Human Development, and Health, School of Public Health, Harvard University, Boston
d Department of Dermatology, Boston University School of Medicine
@ Reprint requests: Jean L. Forster, PhD, University of Minnesota, Division of Epidemiology & Community Health,
1300 S Second St, Suite 300, Minneapolis, MN 55454.
Supported by grant R01 CA079593 from the National Institutes of Health.
Conflicts of interest: None identified.
Pll : S0190-9622(06)01840-8
doi:1 0.1 016/j.jaad.2006.06.036
2006 American Academy of Dermatology, Inc. Published by Elsevier Inc All rights reserved.
Copyright 2009 Elsevier, Inc. All rights reserved I Privacy Policy I Terms & Conditions I Feedback I About Us I Help I Contact Us I
The content on this site is intended for health professionals.
http://www .eblue.org/article/SO 190-9622(06)0 1840-8/abstract 9/22/2009
Compliance With Youth Access Regulations
for Indoor UV Tanning
Eric]. Hester, MD; Lauren F. Heilig, BA; Renee D'Ambrosia, MD; Amanda L Drake, BS;
Lisa M. Schilling, MD; Robert P. Dellavalle, MD, PhD, MSPH
Obiectives: To describe youth access to indoor UV tan-
ning and youth discount pricing incentives in 4 states with
different age restrictions: Colorado (no age restric-
tions), Texas (age l3 years), Illinois (age 14 years), and
Wisconsin (age 16 years).
Design: Cross-sectional telephone survey conducted
in October 2003 using a standardized script to assess
the practices of randomly selected UV tanning opera-
tors.
Results: For a 12-year-old potential patron, 62% offacili-
ties in states with minimum age restrictions prohibiting 12-
year-olds had an operator report that they would not per-
mit indoor tanning (Texas, 23%; Illinois, 7 4%; and Wiscon-
sin, 89%) compared with 18% in Colorado, a state without
youth access regulations. For a 15-year-old patron, most
facilities in vVisconsin, the only state with a minimum age
restriction for 15-year -olds, prohibited access (77%). Over-
all, 15% of operators offered youth discounts: Texas, 23%;
Illinois, 14%; Wisconsin, 11 %; and Colorado, 11%.
Participants: Randomly selected licensed indoor UV tan-
ning facility operators in Colorado, Texas, Illinois, and
Wisconsin.
Main Outcome Measures: Number of facilities (l)
complying with indoor UV tanning minimum age
regulations for a 12-year-old potential patron and a
15-year-old potential patron and (2) offering youth
discounts.
Conclusions: Tanning facilities in 4 states o(fered price
incentives directed at youths. State youth access regula-
tions were associated with decreased youth access to in-
door tanning. High compliance levels in states with long-
standing youth access regulations (lllinois and Wisconsin)
demonstrate the potential for successful tanning indus-
try youth access regulation.
Arch Den-nato!. 2005;141:959-962
Author Affiliations:
Departments of Dermatology
(Drs Hester and Dellavalle and
Mss Heilig and Drake) ,
Medicine (Dr Schilling) , and
Preventive Medicine and
Biometrics (Ms Heilig and
Dr Schilling), University of
Colorado at Denver and Health
Sciences Center; Louisiana State
University School of Medicine,
New Orleans (Dr D'Ambrosia);
and Department of Veterans
Affairs Medi.cal Center, Denver
(Dr Dellavalle). Dr Hester is
now with the Department of
Dermatology. Oregon Health
and Science University,
Portland.
Financial Disclosure: None.
M
ULTIPLE STUDIES
1
2
CON-
firm widespread in-
door UV tanning use
by US adolescents. Al-
though youths may
seek indoor tanning owing to the por-
rrayal of tanned skin as healthy and at-
tractive, UV is classified as a carcinogen
and is associated with numerous short- and
long-term effects, including skin can-
cer.H The use of tanning devices is asso-
ciated with squamous and basal cell car-
cinomas8 and has been implicated in
increased melanoma risk
9
-
12
Because ado-
lescence represents a critical period dur-
ing which UV radiation increases skin can-
cer risk,
13
14
altering the tanning behavior
of minors is a target for skin cancer pre-
vention efforts.
8
.11.1s
In 2003, only 3 states had set age lim-
its for indoortanni ng patrons: Texas at age
13 years (instituted in 2002), Illinois at age
14 years (1992), and Wisconsin at age 16
years (1992) .
16
further youth access re-
quirements in these states include guard-
ian accompaniment for 13- to 15-year-
olds in Texas, guardian consent for 16- to
17-year-olds in Texas, and guardian con-
sent for 14- to 17 -year-olds in Illinois
(Table). Most states, including Colo-
rado, do not set age limits on access to in-
door tanning. Two previous studies ex-
amining compliance with youth access
laws for indoor tanning described poor
See also pages 963 and 1028
operator compliance: 43% of indoor tan-
ning facilities were compliant with paren-
tal consent regulations in San Diego,
Calif,
18
and 13% of North Carolina facili-
ties complied with a required guardian
consent fonn for youths.
19
Another issue in adolescent use of tan-
ning facilities is the marketing directed to-
ward teens. Although price incentives for
the general public have encouraged fre-
quent tanning,
20
discounts specifically
available to adolescents have not been well
described.
(REPRI NTED) ARCH DERMATOVVOL 141, AUG 2005
959
W\VVI!.A RCHDERtvlA TOL.COM
Downloaded from www.archdermatol.com at Federal Trade Commission, on September 22, 2009
2005 American Medical Association. All rights r eserved.
Table. Youth Access Regulation and Practices of Indoor UV Tanning Facilities in Texas, Illinois, Wisconsin, and Colorado
Texas Illinois Wisconsin Colorado
Variable (n = 100) (n = 100) (n = 100) (n = 100)
Regulations 1. No indoor tanning under 1. No indoor tanning under No indoor tanning under No youth access
age 13 y without age 14 y. age 16 y. regulations.
parental/legal guardian 2. Parental/legal guardian (last revised: 1992)
supervision and consent for ages 14-17 y.
physician's written (Last revised: 1992)
permission.
2. Parental/legal guardian
accompaniment for ages
13-15 y.
3. Parental/legal guardian
consent for ages 16-17 y.
(last revised: 2002)
Penalties First 3 youth access Warning letter issued for the Youth access violations Not applicable.
violations result in first violation. For a result in $50-$250
warning without fines. second violation, the fines.
Further violations may permittee may be fined
result in fines and permit $250. A third violation
revocation. may result in a minimum
fine of $500 and possible
permit revocation.
Enforcement 30 Randomly selected All licensed facilities are Licensed facilities with Not applicable
facilities and facilities audited yearly. complaints audited
with complaints are Approximately 10% of regarding the
audited yearly by patron records are complaint only.
examining records. examined. Patron age is
ascertained by recorded
date of birth.
Offered discounts for children, %t
Yes 23 14 11 11
No 77 74 86 80
Don't know/no answer 0 12 3 9
Practices regarding access by 12-year-olds
to indoor tanning. %t
Access allowed without restrictions 2 1 1 2
Cannot tan 2311 74 89 18
Parent/legal guardian consent 47 16 3 62
Parent/legal guardian accompaniment 8 0 0 8
Adult accompaniment or consent 13 6 0 1
Don't know 7 3 7 9
Practices regarding access by 15-year-olds
to indoor tanning, 'l'ot
Access allowed without restrictions 2 3 1 4
Cannot tan 5 4 77 10
Parent/legal guardian consent 64 74 16 70
Parent/legal guardian accompaniment 6 2 0 6
Adult accompaniment or consent 17 17 0 1
Don't know 6 0 6 9
*Sources: Youth access law penalties (http:l/www.uchsc.edu/dehsr/MapData.htm); Texas Department of Health, oral communication, January 21, 2004; Illinois
Department of Public Health, oral communication. January 21. 2004: Radiati on Protection Section. Wisconsin Division of Public Health, oral communication.
January 21, 2004; and Francis et al.
17
tP= .11.
tP< .01 .
Noncompliance with state laws.
II Nine facility operators stated that physician consent was required.
METHODS
Comprehensive lists of licensed tanning facility contact infor-
mation were obtained from state health departments (Febru-
ary to May 2003): Texas, 2332 facilities; ltlinois, 1905 facili-
ties; Wisconsin, 1447 facilities; and, Colorado, 580 facilities.
Colorado was chosen as the fourth state in this study for sev-
eral reasons: (1) in 2003, Colorado was 1 of 36 states without
any age or guardian requirements for UV tanning services; (2)
( REPRI NTED) ARCH DERMATOVVOL 141 , AUG 2005
960
surveying Colorado tanning facilities was most relevant for our
public health professional endeavors; and (3) of all states with-
out regulations, telecommunications charges for surveying Colo-
rado were the most economical.
One hundred facilities from each state were randomly se-
lected using a random number generator (http://www.random
.org) and were surveyed by telephone (October 2003). 1f a fa-
cility representative was unavailable after 3 calls, or if the
telephone number was disconnected, another facility from the
same state was randomly selected from the remaining facili-
W\VVI!.A RCHDERtvlA TOL .COM
Downloaded from www.archdermatol.com at Federal Trade Commission, on September 22, 2009
2005 American Medical Association. All rights r eserved.
ties. The survey consisted of a standardized script asking whet her
potential patrons aged 12 and 15 years would be allowed tore-
ceive indoor UV tanning treatments. If patronage was al-
lowed, the tanning facility operator was asked whether guard-
ian (including parent or legal guardian) or adult accompaniment
was required, whether guardian or adult consent was re-
quired, and whether any price discounts for youth were avail-
able. To maximize response rates, minimize social acceptabil-
ity response bias, and avoid deviation from information currently
given to potential customers, facility representatives were not
informed that they were participating in a study. This study re-
ceived Colorado institutional review board approval.
Health departments for each state were contacted by tele-
phone ro assess youth access to indoor tanning regulations, en-
forcement policies, penalties for noncompliance, and fre-
quency of imposing sanctions on violating facilities (November
2003 to January 2004). Survey data were entered into a data-
base management program (Microsoft Access; Microsoft Corp,
Redmond, Wash) by l investigator (R.D.) and were verified by
another investigator (L.F.H.). Using a statistical software pro-
gram (SAS 8.0; SAS Institute Inc, Cary, NC), a comparison of
compliance with minimum age restrictions for indoor UV tan-
ning by state was performed using the Fisher exact test.
RESULTS
Six hundred twenty-eight facilities were contacted by
telephone to obtain 400 licensed indoor tanning facility
survey responses (100 facilities in each state: Colorado,
Illinois, Texas, and Wisconsin). Two hundred twenty-
eight facilities were either unavailable after 3 calls or the
telephone number was disconnected (78 in Texas, 29 in
Illinois, 57 in Wisconsin, and 64 in Colorado). The Table
summarizes the survey responses. Overall, 15% of the tan-
ning facility operators reported that discounts were avail-
able for youths. For a 12-year-old potential patron, 62%
of facilities in states with age restrictions had operators
report that they would not permit indoor tanning (Texas,
23%; Illinois, 74%; and Wisconsin, 89%) compared with
18% in Colorado. The percentage of facilities prohibit-
ing a 12-year-old from tanning among facilities offering
and not offering youth discounts was similar ( 67% vs 58%;
P= .32) . For a 15-year-old potential patron, rates of ac-
cess without guardian accompaniment in noncompli-
ance with respective state statutes were as follows: 83%
of operators in Texas would allow access without guard-
ian accompanimem, 20% in Illinois would allow access,
and 17% in Wisconsin would allow access. Noncompli-
ance for 15-year-olds was higher for facilities offering
youth discounts compared with faci li ties not offering
youth discounts (60% vs 46%; P= .08). Youth access regu-
lations, penalties, and enforcement varied by state (Table).
Skin cancer prevention strategies may include decreas-
ing UV exposure by further educating our youth, in-
creasing sun protection behaviors, taxing indoor tan-
ning for youths,
21
and adopting regulations limiting youth
access to indoor tanning. Given the prevalence of in-
door UV tanning, especially by adolescent girls,
1
2
and the
known risks of indoor tanning, public health efforts need
to be directed at this underrecognized carcinogen expo-
( REPRI NTED) ARCH DERMATOVVOL 141 , AUG 2005
961
sure. Although the efficacy of youth access regulations
for decreasing tobacco use has been debated,
22
analo-
gous regulations may be effective for limiting indoor tan-
ning and merit consideration.
16
In this 4-state comparison, compliance with regula-
tions for youth access to indoor tanning varied greatly
by state, and many facilities encouraged young patrons
by offering price discounts. Facilities in lllinois and Wis-
consin reported closer adherence to regulations than those
in Texas. Adolescents in Texas were largely required to
have guardian consent but were frequently not compli-
am with minimum age regulations or guardian accom-
paniment regulations for 12- and 15-year-old potential
patrons, respectively.
Differing rates of compliance with youth access laws
may be due to differences in state enforcement, penal-
ties for noncompliance, and the length of time a statute
has been in place. Our results do not support a differ-
ence due to enforcement Wisconsin showed the high-
est compliance for a 12-year-old potential patron but lacks
rigorous enforcement compared \vith Texas, which has
lower compliance and more systematic regulation en-
forcement. Texas state department officials described more
lenient penalties than those in Illinois and Wisconsin.
In addition, Texas youth access regulations were more
recently enacted (2002) than those in Illinois and Wis-
COI1Sin (1992), which may partly explain compliance rates.
Lower compliance in Texas might also be a result of Texas
having the lowest age limit among the states with an age
restriction. Better dissemination of current regulations
in Texas may improve compliance. A recent electronic
surveyn of tanning facility operators reports support for
youth access regulations, suggesting that better educa-
tion of facility operators with youth access regulations
will result in improved compliance.
ln addition to regulations for youth access, this study
assessed the prevalence of tanning price incentives for
youths. The tobacco industry previously promoted smok-
ing in the United States by providing free cigarette samples
that were often available to children despite voluntary
codes prohibiting such access.
2
.
1
Given that youth dis-
coums may encourage teen tanning and promote youth
access regulation violations, state health departments
should consider promoting bans on youth discounts.
This smdy has several limitations: (l) The survey was
conducted via telephone, assessing practices regarding
potential adolescent patrons. Observed compliance may
have differed if a youth approached the facility in per-
son. (2) The telephone survey, although anonymous, was
subject to social acceptability and self-reporting biases.
(3) Information was not obtained on how or how often
tanni ng operators verify the age of potential patrons. ( 4)
Facility operators were not questioned regarding the range
of ages for which youth discounts would be available. (5)
The home use of privately owned indoor tanning de-
vices was not assessed by the study. (6) Findings from
Colorado, the only state surveyed that did not have youth
access restrictions, may not be generalizable to other states
without restrictions.
Despite high noncompliance with youth access laws
in Texas, higher compliance levels in states \vith long-
standing youth access regulations (Illinois and Wiscon-
W\VVI!.A RCHDERtvlA TOL.COM
Downloaded from www.archderrnatol.com at Federal Trade Commission, on September 22, 2009
2005 American Medical Association. All rights r eserved.
sin) suggest the potential for successful tanning indus-
try youth access regulation.
Accepted for Publication: April 9, 2005.
Correspondence: Robert P. Dellavalle, MD, PhD, MSPH,
Department of Veterans Affairs Medical Center, 1055
Clermont St, Mail Stop 165, Denver, CO 80220 (robert
. dellavalle@uchsc.edu).
Funding/Support: This study was supported by grant T32
AR07 411 from the National Institutes of Health, Bethesda,
Md (Dr Hester); grantS D14HP00153 from the Health Ser-
vices Research Award Faculty Development in Primary
Care (Dr Schilling); grant K-07 CA92550 from the Na-
tional Cancer Institute, Bethesda (Dr Dellavalle); and a seed
grant from the University of Colorado Cancer Center.
Previous Presentation: This study was presented at the
4th Combined European Dermatoepidemiology and
International Dermatoepidemiology Association Con-
gress; October 10, 2004; Venice, Italy.
Acknowledgment: We thank Brittany Wilson for help-
ing us conduct this study.
1. Demko CA, Borawski EA. Debanne SM, et al. Use of indoor UV tanning facilities
by white adolescents in the United States. Arch Pediatr Adolesc Med. 2003;
157:854860
2. Geller AC, Colditz G, Oliveria S, et al. Use of sunscreen, sunburning rates, and
tanning bed use among more than 10,000 US children and adolescents. Pediatrics.
2002; 109:1 0091 014.
3. National Toxicology Program. Available at: http://www.epa.gov/fedrgstr/EPA TOX
/1998/March/Day-19/17183.htm. Accessed January 5, 2004.
4. Spencer JM, Amonette RA. Indoor tanning: risks, benefits, and future trends.
JAm Acad Derma to!. 1995;33:288298.
5. Committee on Environmental Health. Ultraviolet light: a hazard to children.
Pediatrics. 1999;104:328333.
6. 11th Annual Report on Carcinogens from the Environmental Health Information
Service, a joint service of the NIH-National Institute of Environmental Health
Services and the US Department of Health and Human Services National Toxi-
cology Program. Available at: http://ehis.niehs.nih.gov/roc. Accessed January 5,
2004.
7. Centers for Disease Control and Prevention. Injuries associated with ultraviolet
tanning devices- Wisconsin. MMWR Morb Mortal Wk/y Rep. 1989;38:333
335.
8. Karagas MR, Stannard VA, Mott LA, Slattery MJ, Spencer SK, Weinstock MA.
Use of tanning devices and risk of basal cell and squamous cell skin cancers.
J Naif Cancer Jnst. 2002;94:224226.
9. Veierod MB, Weiderpass E. Thorn M, et al. A prospective study of pigmentation,
sun exposure, and risk of cutaneous malignant melanoma in women. J Naif Can-
cer/nsf. 2003;95:1530-1538 .
10. Wang SO, Setlow R, Berwick M, et al. Ultraviolet A and melanoma: a review.
JAm Acad Dermatol. 2001 ;44:837-846.
11. Swerdlow AJ, English JS. MacKie RM, et al. Fluorescent lights, ultraviolet lamps,
and risk of cutaneous melanoma. BMJ. 1988;297:647-650.
12. Dilley BL. A quantitative estimate of melanoma mortality from ultraviolet A sun-
bed use in the U.K. Br J Dermatol. 2003;149:578581.
13. Stern RS, Weinstein MC, Baker SG. Risk reduction for nonmelanoma skin can-
cer with childhood sunscreen use. Arch Dermatol. 1986;122:537545.
14. Khlat M, Vail A, Parkin M, et al. Mortality from melanoma in migrants to Austra-
lia: variation by age at arrival and duration of stay. Am J Epidemiol. 1992;135:
1103-1113.
15. Lim HW, Cooper K. The health impact of solar radiation and prevention strate-
gies: report of the Environment Council, American Academy of Dermatology.
JAm Acad Dermatol. 1999;41 :81 99.
16. Dellavalle RP, Parker ER, Cersonsky N. et al. Youth access laws: in the dark at
the tanning parlor? Arch Dermatol. 2003;139:443-448.
17. Francis SO, Burkhardt DL, Dellavalle RP. 2005: A banner year for new US youth
access tanning restrictions. Arch Dermatol. 2005;141:524-525.
18. Culley CA, Mayer JA, Eckhardt L, et al. Compliance with federal and state legis
lation by indoor tanning facilities in San Diego. JAm Acad Dermatol. 2001;
44:5360
19. Fleischer AB Jr, Lee WJ, Adams DP, etal. Tanning facility compliance with state
and federal regulations in North Carolina: a poor performance. JAm Acad Dermatol
1993;28:212-217.
20. Kwon HT, Mayer JA, Walker KK, et al. Promotion of frequent tanning sessions
by indoor tanning facilities: two studies. JAm Acad Dermatol. 2002;46:700-
705.
21. Dellavalle RP, Schilling LM, Chen AK, et al. Teenagers in the uv tanning booth?
tax the tan. Arch Pediatr Ado/esc Med. 2003;157:845-846.
22. Fichtenberg CM, Glantz SA. Youth access interventions do not affect youth smoking.
Pediatrics. 2002;109:10881092.
23. Hester EJ, Johnson KR, Crane l , et al. Attitudes and practices of indoor UV tan-
ning facility operators: an electronic survey. JAm Acad Dermatol. 2004;51:
814816.
24. Davis RM, Jason LA. The distribution of free cigarette samples to minors. Am J
Prev Med. 1988;4:21-26.
AJtJIOiliiCt'IIICIIt
Visit www.archdermatol.com. As an individual sub-
scriber to Archives of Dennatology, you have full-text on-
line access to the journal from 1998 forward. In addi-
tion, you can find abstracts to the journal as far back as
1965.
(REPRI NTED) ARCH DERMATOVVOL 141, AUG 2005 WWVv.ARCHDERtvlATOL.COM
962
Downloaded from www.archdermatol.com at Federal Trade Commission, on September 22, 2009
2005 American Medical Association. All rights r eserved.
Comparing two methods of measuring legislation compli ance among indoor tanning facili.. Page 1 of 2
More periodicals:
FIND A PERIODICAL
GO TO PRODUCT CATALOG
Register or Login: Password: :::::J Auto-Login [Reminder]
Search This Periodical for
Advanced Search - MEDLINE - My Recent Searches - My Saved Searches - Search Tips
Volume 54, Issue 3, Pages 433-439 (March 2006)
Comparing two methods of measuring legislation
compliance among indoor tanning facilities
Ami L. Hurd, MPHa, Joni A. Mayer, P h D a ~ Susan I. Woodruff, PhDa,
George E. Belch, PhDb, Minai R. Patel, MPHa
Accepted 21 November 2005. published online 3 1 January 2006.
Background
Accurate measurement of compliance by tanning faci lities to indoor
tanning legislation is important.
Objective
This study compared a telephone-based measurement procedure with a
face-to-face visit.
Methods
Indoor tanning faci lities (N = 115) in San Diego County, California, were
contacted by two adolescents posing as prospective customers using
each method. Two compliance variables were assessed: number of
times one can tan during 1 week and written parental consent for
minors.
Results
Facility compliance with the frequency variable by face-to-face and
telephone was 25.5% and 17.5%, respectively. These rates for the
parental consent variable were 73.3% and 80.8%, respectively. Percent
agreement between data collection methods was 71.3% for compliance
with the frequency recommendation and 76.3% for parental consent
regulation. Although traditional statistical tests indicated poor
concordance, an alternative test indicated good concordance.
Limitations
Levels of concordance for the confederates differed.
Conclusion
Telephone assessment of compliance is fairly comparable with the more
labor-intensive, face-to-face assessment.
San Diego, California
a From the Graduate School of Public Health
b Department of Marketing, San Diego State University
.. ABSTRACT
FULL TEXT
FULL-TEXT PDF (223 KB)
CITATION ALERT
CITED BY
RELATED ARTICLES
EXPORT CITATION
EMAIL TO A COLLEAGUE
VIEW GENETIC INFO
RIGHTS/PERMISSIONS
NEED REPRINTS?
BOOKMARK ARTICLE
FULL TEXT ELSEWHERE
http://www .eblue.org/article/SO 190-9622(05)04621-9/abstract 9/22/2009
Comparing two methods of measuring legislation compli ance among indoor tanning facili.. Page 2 of 2
requests: Joni A. Mayer, PhD. Graduate School of Public Health, San Diego State University, 5500
Campanile Dr, Hardy Tower No. 119, San Diego, CA 92182-4162.
Supported by grants from the National Institutes of Health, National Cancer Institute:
RO 1 CA93532 and KOSCA 1 0051 .
Conflicts of interest: None identified.
Pll : S0190-9622(05)04621 -9
doi:l 0. 1 016/j.jaad.2005.1 1.1 078
2006 American Academy of Dermatology, Inc. Published by Elsevier Inc All rights reserved.
Copyright 2009 Elsevier. Inc. All rights reserved I Privacy Policy I Terms & Conditions I Feedback 1 About Us 1 Help I Contact Us 1
The content on this site is intended for health professionals.
http://www .eblue.org/article/SO 190-9622(05)04621-9/abstract 9/22/2009
Promotion of frequent tanning sessions by indoor tanning facilities: Two studies Page 1 of 1
More periodicals:
FIND A PERIODICAL
GO TO PRODUCT CATALOG
Register or Login: Password: :::::J Auto-Login [Reminder]
Search This Periodical for
Advanced Search - MEDLINE - My Recent Searches - My Saved Searches - Search Tips
Vol ume 46, Issue 5, Pages 700-705 (May 2002)
Promotion of frequent tanning sessions by indoor
tanning facilities: Two studies
Harry T. Kwon, MPH, CHES
8
, Joni A. Mayer, PhD
8
, Kristina K. Walker,
MPHa, Henry Yu, MPHa, Elizabeth C. Lewis, MPHa, George E. Belch, PhDb
Accepted 31 May 2001.
Abstract
Background: Indoor tanning may increase the risk of melanoma and
other health problems. Frequent users of indoor tanning faci li ties may
be at particularly high risk. Objective: In study 1 our purpose was to
assess the prevalence and nature of indoor tanning advertisements; in
study 2 we aimed to assess tanning facil ity compliance to
recommended exposure schedules. Methods: In study 1, tanning
facility advertisements over a 4-month period from 24 San Diego
County newspapers were monitored. In study 2, we assessed
compliance with recommended exposure schedules via a telephone
interview of 60 San Diego County tanning faci lities. Results:
Approximately 75% of the indoor tanning advertisements promoted
unlimited tanning. Only 5% of faci lities were in compliance with
recommended tanning schedules, and 100% offered "unlimi ted" tanning
packages. Conclusions: These findings suggest that the indoor tanning
industry, through pricing incentives that allow frequent sessions, may be
promoting overexposure to UVR. Stronger legislation is needed to
address this issue. (JAm Acad Dermatol2002;46:700-5.)
San Diego, California
.. ABSTRACT
FULL TEXT
FULL-TEXT PDF (88 KB)
CITATION ALERT
CITED BY
RELATED ARTI CLES
EXPORT CITATION
EMAIL TO A COLLEAGUE
VIEW GENETIC INFO
RIGHTS/PERMISSIONS
NEED REPRINTS?
BOOKMARK ARTICLE
FULL TEXT ELSEWHERE
From the Graduate School of Public Health
8
and the Department of Marketing,b San Diego State University
Funding: None.
Conflict of interest: None.
Reprint requests: Joni A. Mayer, PhD, Graduate School of Public Health-Hardy Tower 119,
San Diego State University, San Diego, CA 92182-4162. E-mail : jmayer@mail.sdsu.edu.
Pll: S0190-9622(02)76726-1
doi:10.1067/mjd.2002.119560
2002 American Academy of Dermatology, Inc. Published by Elsevier Inc. All rights reserved.
Copyright 2009 Elsevier, Inc. All rights reserved I Privacy Policy I Terms & Conditions I Feedback I About Us I Help I Contact Us I
The content on this site is intended for health professionals.
http://www .eblue.org/article/SO 190-9622(02)76726-1/abstract 9/22/2009
ConsumerReports.org - CONSUMER REPORTS lNVESTIGATES THE UNEXPECTE .. . Page 1 of2
ExlHifl ln4 otmdll()t N ,
sumerReports
CONSUMER REPORTS INVESTIGATES THE UNEXPECTED
DANGERS OF INDOOR TANNING
--Nationwide survey finds widespread failures to inform customers of possible risks--
x Close
YONKERS, NY - Nearly 30 million Americans, including a growing number of teenage
girls, are expected to visit a tanning salon this year. Consumer Reports' nationwide survey
found evidence of a public health threat that goes beyond the familiar warnings that tanning
may increase the risk of developing wrinkles and skin cancer.
When CR called 296 tanning facilities in 12 cities, many not only denied or downplayed the
possible risks but also endorsed unsafe practices. Here are the highl ights of the CR
investigation:
Seventy-five percent of the surveyed employees said customers can come every day or as
often as they like, even if they are beginners.
February 2005 Issue Nearly 35 percent denied that indoor tanning can cause skin cancer, claimed it doesn't
prematurely age the skin, or said both.
About 6 percent said they permit the dangerous practice of tanning without protective eyewear.
More than 20 percent said minors, who may face the greatest long-term risks from such exposure to ultraviolet
rays, could come without adult consent.
About two-thirds of the employees said that an extremely pale-skinned person who burns but never tans
outdoors could come in for tanning or evaluation. But even the National Tanning Training Institute, an industry
group, omits people with such vulnerable skin from its chart on skin types in its current training manual.
About half of states in the U.S. have no tanning parlor regulations, and the existing rules are sometimes
minimal and frequently flouted by parlor employees.
Overall, the employees gave an average of three to four answers considered false, questionable, or
inadequate. Only 1 percent answered all questions appropriately. If those findings translate into actual practice,
many indoor tanners are being exposed to particularly high risk.
In addition, incorrect or questionable ideas about indoor tanning persist, including the
claim that lotions can reduce the aging effects of indoor tanning. Preliminary research
suggests that topical lotions containing antioxidant vitamins might possibly reduce skin
damage if applied before tanning. But any such protection woul d be quite minimal.
Another questionable claim is that indoor tanning may help prevent disease. It's true that
UVB, one of the main types of ultraviolet radiation, stimulates the skin to synthesize
vitamin D, which some research suggests may help ward off several diseases. But there
are safer ways to get enough D.
Consumers Union, the nonprofit publisher of Consumer Reports, believes the Food and
Drug Administration should promptly implement and publicize its 1999 proposal to reduce
UV exposure limits and require additional consumer warnings. Meanwhile, all states
should regulate tanning parlors, and county and state health officials should inspect the
facilities regularly to ensure compl iance with regulations. Consumer Reports does not
recommend indoor tanning for anyone. However, if you or your children can't resist sun
beds, CR recommends the following:
Be sure to get no more than the minimum tanning exposure for your skin type. New tanning bulbs emit
considerably more radiation than older bulbs, which should be taken into account. Raise the questions CR
asked, and be wary of any facility that provides improper answers.
http://www.consumerreports.org/cro/cu-press-room/pressroom/archive/2005/02/eng0502ta... 9/22/2009
ConsumerReports.org - CONSUMER REPORTS lNVESTIGATES THE UNEXPECTE.. . Page 2 of 2
Some people must avoid UV tanning entirely: those who have certain diseases, such as eczema or lupus, or
take certain drugs, such as some antibiotics, thiazide diuretics, or oral contraceptives. Check with your
physician or pharmacist before tanning.
People who've already tanned frequently should be especially cautious about further UV exposure. They
should wear sunscreen, sun protective clothing, or both outdoors, and both they and a dermatologist should
periodically check their skin for suspicious moles or other lesions.
To get bronzed without the potential risks of UV rays, consider spray-on tanning. Consumer Reports' informal
evaluation found that the spray could produce color resembling a real tan, but the results were variable. When
undergoing the procedure, ask for eye goggles and foam nose and ear plugs, or bring your own. And hold your
breath as much as possible during the spraying. The FDA has approved DHA (dihydroxyacetone) , the active
ingredient, only for external use.
The February 2005 issue of Consumer Reports goes on sale January 5 wherever
magazines are sold. To subscribe, call 1-800-765-1845.
FEBRUARY 2005
@Consumers Union 2005. The material above is intended for legitimate news entities only; it may not be used for commercial or promotional
purposes. Consumer Reports is published by Consumers Union, an expert, independent nonprofit organization whose mission is to work for
a fair. just, and safe marketplace for all consumers and to empower consumers to protect themselves. To achieve this mission. we test, inform,
and protect. To maintain our independence and impartiality, CU accepts no outside advertising, no free test samples, and has no agenda other
than the interests of consumers. CU supports itself througf1 the sale of our information products and services, individual contributions, and a
few noncommercial grants.
Copyright 2004-2009 Consumers Union of U.S., Inc. No reproduction, in whole or in part, without written permission.
http://www.consumerreports.org/cro/cu-press-room/pressroom/archive/2005/02/eng0502ta... 9/22/2009
ACS :: Skin Cancer Facts
t
American
Cancer
Society
-.. Prevention and
Early Detection
Prevention
Early Detection
Stories of Hope
Tobacco and
Cancer
Great American
Smokeout
Food and Fitness
Great American
Health Check
Great American Eat
Right Challenge
Environmental
Carcinogens
Glossary
I Want to Help
You can help in the
fight against cancer.
Donate and volunteer.
more
Home I Community I Get Involved I Donate I Contact Us I Site Index I Search
Skin Cancer Facts
Most of the more than 1 million cases of non-melanoma skin cancer
diagnosed yearly in the United States are considered to be sun-related.
Melanoma, the most serious type of skin cancer, will account for about
68,720 cases of skin cancer in 2009 and most (about 8,650) of the 11 ,590
deaths due to skin cancer each year.
Melanoma in the United States - 2009 Estimates
New Cases
Deaths Per Year
5-Year Locali zed Survival Rate*
5-Year Overall Survival Rate*
68,720
8,650
99%
91%
The 5-year survival rates represent persons who are living 5 years after diagnosis,
whether disease-free, in remission, or under treatment. They do not imply that 5-year
survivors have been permanently cured of cancer. Localized cancer represents cancer
that, at the time of diagnosis, had not spread to additional sites within the body. Typically
the earlier a cancer is detected and diagnosed, the more successful the treatment, thus
enhancing the survival rate.
For localized melanoma, the 5-year survival rate is 99%; survival rates for
regional and distant stage diseases are 65% and 16%, respectively. About
80% of melanomas are diagnosed at a localized stage.
Frequently Asked Questions
What is the skin? The skin is the largest organ of the body. It covers the
internal organs and protects them from injury; serves as a barrier between
germs, such as bacteria, and internal organs; and prevents the loss of too
much water and other fluids. The skin regulates body temperature and
helps the body get rid of excess water and salts. Certain cells in the skin
communicate with the brain and allow for temperature, touch, and pain
sensations.
What is non-melanoma (basal or squamous cell) skin cancer? Most
skin cancers are classified as non-melanoma, usually starting in either
basal cells or squamous cells. These cells are located at the base of the
outer layer of the skin or cover the internal and external surfaces of the
body.
Most non-melanoma skin cancers develop on sun-exposed areas of the
body, like the face, ear, neck, lips, and the backs of the hands. Depending
on the type, they can be fast or slow growing, but they rarely spread to
other parts of the body.
ISZI Emai l this Page
Also in this area
Skin Cancer
Prevention and
Early Detection
Skin Cancer
Prevention and
Early Detection
Skin Cancer Facts
' Take the Sun
Safety Quiz
Why You Should
Know About
Melanoma
Sun Safety
Resources
Related Tools &
Topics
,. Statistics
Not registered yet?
Register now or see
reasons to register.
http://www .cancer.org/docroot/PED/content/ped_7 _1_ What_ You_Need_To_Know _About_Skin_ Cancer.asp?sitearea=PED[ 12/112009 8:33:19 PM]
ACS :: Skin Cancer Facts
What is melanoma skin cancer? Melanoma is a cancer that begins in
the melanocytes -- the cells that produce the skin coloring or pigment
known as melanin. Melanin helps protect the deeper layers of the skin
from the harmful effects of the sun.
Melanoma is almost always curable when it is detected in its early stages.
Although melanoma accounts for only a small percentage of skin cancer, it
is far more dangerous than other skin cancers and causes most skin
cancer deaths.
How many people are affected by skin cancer? Skin cancer is the most
common of all cancers. It accounts for nearly half of all cancers in the
United States. More than 1 million cases of non-melanoma skin cancer are
found in this country each year. The American Cancer Society estimates
that about 68,720 new melanomas will be diagnosed in the United States
during 2009.
Who survives skin cancer? For basal cell or squamous cell cancers, a
cure is highly likely if detected and treated early. Melanoma, even though it
can spread to other body parts quickly, is also highly curable if detected
early and treated properly. The 5-year relative survival rate for patients
with melanoma is 91%. For localized melanoma, the 5-year survival rate
is 99%; survival rates for regional and distant stage diseases are 65% and
16% respectively. About 80% of melanomas are diagnosed at a localized
stage.
How many people will die from skin cancer? The American Cancer
Society estimates there will be about 11 ,590 deaths from skin cancer in
2009: 8,650 from melanoma and 2,940 from other skin cancers.
What are the risk factors for skin cancer? Risk factors for non-
melanoma and melanoma skin cancers include:
unprotected and/or excessive exposure to ultraviolet (UV) radiation
fair complexion
occupational exposures to coal tar, pitch, creosote, arsenic
compounds, or radium
family history
multiple or atypical moles
severe sunburns as a child
What are the signs and symptoms of skin cancer? Skin cancer can be
found early, and both doctors and patients play important roles in finding
skin cancer. If you have any of the following symptoms, tell your doctor.
any change on the skin, especially in the size or color of a mole or
other darkly pigmented growth or spot, or a new growth
scaliness, oozing, bleeding, or change in the appearance of a bump
or nodule
the spread of pigmentation beyond its border such as dark coloring
that spreads past the edge of a mole or mark
a change in sensation, itchiness, tenderness, or pain
Can skin cancer be prevented? The best ways to lower the risk of non-
melanoma skin cancer are to avoid intense sunlight for long periods of
time and to practice sun safety. You can continue to exercise and enjoy
the outdoors while practicing sun safety at the same time. Here are some
ways you can do this:
Avoid the sun between 10 a.m. and 4 p.m.
Seek shade: Look for shade, especially in the middle of the day
when the sun's rays are strongest. Practice the shadow rule and
http://www .cancer.org/docroot/PED/content/ped_7 _1_ What_ You_Need_To_Know _About_Skin_ Cancer.asp?sitearea=PED[ 12/112009 8:33:19 PM]
ACS :: Skin Cancer Facts
teach it to children. If your shadow is shorter than you, the sun's
rays are at their strongest.
Slip on a shirt: Cover up with protective clothing to guard as much
skin as possible when you are out in the sun. Choose comfortable
clothes made of tightly woven fabrics that you cannot see through
when held up to a light.
Slop on sunscreen: Use sunscreen and lip balm with a sun
protection factor (SPF) of 15 or higher. Apply a generous amount of
sunscreen (about a palmful) and reapply after swimming, toweling
dry, or perspiring. Use sunscreen even on hazy or overcast days.
Slap on a hat: Cover your head with a wide-brimmed hat, shading
your face, ears, and neck. If you choose a baseball cap, remember
to protect your ears and neck with sunscreen.
Wrap on sunglasses: Wear sunglasses with 99% to 100% UV
absorption to provide optimal protection for the eyes and the
surrounding skin.
Follow these practices to protect your skin even on cloudy or
overcast days. UV rays travel through clouds.
Avoid other sources of UV light. Tanning beds and sun lamps are
dangerous because they can damage your skin.
What Is the American Cancer Society Doing About Skin
Cancer?
Education: The Society delivers health information to the public, so
that individuals can make informed personal decisions. Examples
include: Printed materials, media coverage, community-based
outreach programs, and free, nationwide services such as
www.cancer.org and 1-800-227-2345. The American Cancer
Society also began its Sun Safe Community initiative in December
2000 to help prevent skin cancer. This community-based, multi-
component effort consists of prevention programs at schools,
childcare centers, primary care offices, and beach and recreation
areas.
Advocacy: With the help of grassroots volunteers in communities
across the country, the Society advocates with lawmakers at both
the state and federal levels to ensure responsible health policies
are enacted and to increase funding for research and testing and
treatment coverage.
Service: The Society works to improve quality of life for people
living with cancer through a variety of support services and
programs helping patients and families cope with the disease.
The Society also has collaborations with many nationwide
organizations to promote skin cancer prevention, education, and
sun-safe policies.
Last Medical Review: 07/06/2009
Last Revised: 07/06/2009
!::!sW;l l About ACS 1 Employment & Volunteer Opportunities I Legal & Privacy Information 1 Press Room
Copyright 2009 American Cancer Society, Inc.
All content and works posted on this website are owned and
copyrighted by the American Cancer Society, Inc. All rights reserved.
http://www .cancer.org/docroot/PED/content/ped_7 _1_ What_ You_Need_To_Know _About_Skin_ Cancer.asp?sitearea=PED[ 12/112009 8:33:19 PM]
ACS :: Skin Cancer Prevention and Early Detection
t
American
Cancer
Society
-.. Prevention and
Early Detection
Prevention
Early Detection
Stories of Hope
Tobacco and
Cancer
Great American
Smokeout
Food and Fitness
Great American
Health Check
Great American Eat
Right Challenge
Environmental
Carcinogens
Glossary
I Want to Help
You can help in the
fight against cancer.
Donate and volunteer.
more
Home I Community I Get Involved I Donate I Contact Us I Site Index I Search
Skin Cancer Prevention and Early
Detection
Skin cancer is the most common of all
cancer types. More than 1 million skin
cancers are diagnosed each year in
the United States. That's more than
cancers of the prostate, breast, lung,
colon, uterus, ovaries, and pancreas
combined. The number of skin cancer
cases has been on the rise for the
past few decades.
The good news is that there is a lot
you can do to protect yourself and your
family from skin cancer, or to catch it
early enough so that it can be treated
effectively. Most skin cancers are
caused by too much exposure to
ultraviolet (UV) rays. Much of this
exposure comes from the sun, but
some may come from manmade
sources, such as tanning beds.
This document discusses how skin
On this page:
What is skin cancer?
What is ultraviolet (UV)
radiation?
Are some people more
prone to sun damage?
How do I protect myself from
UV rays?
What about tanning pills and
other tanning products?
Examining your skin
What should I look for?
What if I find something
suspicious?
Additional Resources
cancer develops and some simple References
steps you can take to help protect
yourself from getting it. It also
describes how to look for signs of skin cancer on your body. Finding
possible skin cancers doesn't require any x-rays or blood tests -- just your
eyes and a mirror. If skin cancer does develop, finding it early is the best
way to ensure it can be treated effectively.
What is skin cancer?
Skin cancers are divided into 2 main types: keratinocyte cancers (basal
and squamous cell skin cancers) and melanomas.
Basal and squamous cell skin cancers are the most common cancers of
the skin. They develop from cells called keratinocytes, the most common
cells in the skin.
Melanomas are cancers that develop from melanocytes, the cells that
make the brown pigment that gives skin its color. Melanocytes can also
form benign growths called moles.
ISZI Email this Page
Also in this area
Skin Cancer
Prevention and
Early Detection
Skin Cancer
Prevention and
Early Detection
Skin Cancer Facts
' Take the Sun
Safety Quiz
Why You Should
Know About
Melanoma
Sun Safety
Resources
Related Tools &
Topics
,. Statistics
Not registered yet?
Register now or see
reasons to register.
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
There are several other types of skin cancers as well , but these are much
less common.
It is important for doctors to tell these types of skin cancer apart, because
they are treated differently. It is also important for you to know what
melanomas and basal and squamous cell skin cancers look like. That way,
you can find them at the earliest possible stage, when they are cured most
easily.
Basal and squamous cell cancers (keratinocyte cancers)
Basal cell cancers and squamous cell cancers are the most common
cancers of the skin. They develop from skin cells called keratinocytes.
Both basal cell and squamous cell cancers are found mainly on parts of
the body exposed to the sun, such as the head and neck, and their
occurrence is related to the amount of sun exposure over a person's
lifetime.
These cancers (especial ly basal cell cancers) rarely spread elsewhere in
the body and are less likely than melanomas to be fatal. Still, they are
important to recognize. If left untreated, they can grow quite large and
invade into nearby tissues, causing scarring, disfigurement, or even loss of
function in some parts of the body.
Keratinocyte cancers are discussed in more detail in a separate American
Cancer Society document, Skin Cancer: Basal and Squamous Cell.
Melanomas
Melanomas can occur anywhere on the body, but are more likely to
develop in certain locations. The trunk is the most common site in men. In
women, the legs are the most common site. Some experts think that
melanomas develop more often in these spots because these areas are
exposed to sun off and on and are more likely to get sunburned. Rarely,
melanomas can also develop in other parts of the body, such as the eyes.
Melanoma occurs much less often than basal cell and squamous cell skin
cancers, but it can be far more serious. Like basal cell and squamous cell
cancers, melanoma is almost always curable in its early stages. But if left
alone, melanoma is much more likely than basal or squamous cell cancer
to spread to other parts of the body, where it can be very hard to treat.
Melanomas are discussed in more detail in a separate American Cancer
Society document, Melanoma Skin Cancer.
What is ultraviolet (uv) radiation?
Ultraviolet (UV) rays are a form of invisible energy given off by the sun.
Ultraviolet radiation is divided into 3 wavelength ranges:
UV A rays cause skin cells to age and can cause some damage to
cells' DNA (the substance in each cell that controls its growth,
division, and function). UVA rays are mainly linked to long-term skin
damage such as wrinkles, but are also thought to play a role in
some skin cancers.
UVB rays are mainly responsible for direct damage to the DNA, and
are the rays that cause sunburns. They are also thought to cause
most skin cancers.
UVC rays don't penetrate our atmosphere and therefore are not
present in sunlight. They are not normally a risk factor for skin
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
cancer.
Although UVA and UVB rays make up only a very small portion of the
sun's wavelengths, they are mainly responsible for the harmful effects of
the sun on the skin. UVB radiation can damage the DNA of skin cells. If
this damage affects the DNA of genes that control skin cell growth, skin
cancer may be the result. Recent research has found that UVA also
contributes to skin cancer formation. Scientists now believe that both UVA
and UVB rays damage skin and cause skin cancer. There are no safe UV
rays.
Skin cancers are one result of getting too much sun, but there are others
as well. The short-term results of unprotected exposure to UV rays are
sunburn and tanning, which are forms of skin damage. Long-term
exposure causes prematurely aged skin, wrinkles, loss of skin elasticity,
dark patches (lentigos, sometimes called "age spots" or "liver spots"), and
pre-cancerous skin changes (such as dry, scaly, rough patches called
actinic keratoses).
The sun's UV rays also increase a person's risk of cataracts and certain
other eye problems and can suppress their immune system. Although
dark-skinned people are generally less likely to get skin cancer than light-
skinned people, they can still get cataracts and immune system
suppression.
The UV Index
The amount of UV light reaching the ground in any given place depends
on a number of factors, including the time of day, time of year, elevation,
and cloud cover. To help people better understand the intensity of UV light
in their area on a given day, the Environmental Protection Agency (EPA)
and the National Weather Service have developed the UV Index. The UV
Index number, on a scale from 1 to 11 +, is a measure of the amount of
UV radiation reaching the earth's surface during an hour around noon. The
higher the number, the greater the exposure to UV radiation.
The UV Index is given daily for regions throughout the country. Many
newspaper and television weather forecasts now include the projected UV
Index for the following day. Further information about the UV Index, as
well as your local UV Index forecast , is available on the EPA's web site at
www.epa oov/sunwjse/uvjndex html . As with any forecast, local changes in
cloud cover and other factors may change the actual UV levels
experienced, but the UV Index reminds the public to take precautions
against too much exposure.
Are some people more prone to sun damage?
Everyone's skin and eyes can be affected by the sun and other forms of
UV rays. Although people with light skin are much more likely to have sun
damage, darker-skinned people, including African Americans and Hispanic
Americans, also can be affected.
People with darker skin tan more easily than others. But tanning is still a
form of skin damage. Tanning occurs when UV radiation is absorbed by
the skin, causing an increase in the activity and number of melanocytes,
the cells that make the pigment melanin. Melanin helps to block out
damaging rays up to a point, which is why darker-skinned people burn
less easily.
People with lighter skin are more likely to burn. Sunburns are thought to
increase your risk of skin cancer, especially melanoma. But UV exposure
can raise skin cancer risk even without causing sunburn.
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
Aside from skin tone, other factors can also affect your risk of damage
from UV light. You need to be especially careful in the sun if you:
have lots of moles, irregular moles, or large moles
have freckles and burn before tanning
have fair skin or blond, red, or light brown hair
were previously treated for skin cancer
have a family history of skin cancer, especially melanoma
live or vacation at high altitudes (UV radiation increases 4% to 5%
for every 1 ,000 feet above sea level)
live or vacation in tropical or subtropical climates
work indoors all week and then get intense sun exposure on
weekends
spend a lot of time outdoors
have certain autoimmune diseases, such as systemic lupus
erythematosus (SLE, or "lupus")
have had an organ transplant
take medicines that lower your immunity
take oral contraceptives (birth control pills)
take tetracycline, sulfa drugs, or certain other antibiotics
take naproxen sodium or certain other non-steroidal anti-
inflammatory drugs (NSAIDs)
take phenothiazines (major tranquilizers and anti-nausea drugs)
take tricyclic antidepressants
take thiazide diuretics (medicines used for high blood pressure and
some heart conditions)
take sulfonylureas (a form of oral anti-diabetic medication)
Ask your doctor, nurse, or pharmacist about the risk of any medicines you
may be taking that could increase your sensitivity to sunlight.
How do I protect myself from UV rays?
It isn't possible or practical to completely avoid sunlight, and it would be
unwise to reduce your level of activity to avoid the outdoors. Time in
sunlight also helps your body make vitamin D, which can be important for
good health. But too much sunlight can be harmful. There are some steps
you can take to limit your amount of exposure to UV rays.
Some people think about sun protection only when they spend a day at
the lake, beach, or pool. But sun exposure adds up day after day, and it
happens every time you are in the sun. "Slip! Slop! Slap! ... and Wrap" is
a catch phrase that reminds people of the 4 key methods they can use to
protect themselves from UV radiation. Slip on a shirt, slop on sunscreen,
slap on a hat, and wrap on sunglasses to protect the eyes and sensitive
skin around them from ultraviolet light.
Following these practical steps can help protect you from the effects of the
sun. These steps complement each other -- they provide the best
protection when used together.
Cover up
When you are out in the sun, wear clothing to protect as much skin as
possible. Clothes provide different levels of protection, depending on many
factors. Long-sleeved shirts, long pants, or long skirts cover the most skin
and are the most protective. Dark colors generally provide more protection
than light colors. A tightly woven fabric protects better than loosely woven
clothing. Dry fabric is generally more protective than wet fabric.
If you can see light through a fabric, UV rays can get through too. Be
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
aware that covering up doesn't block out all UV rays. A typical light T -shirt
worn in the summer usually protects you less than sunscreen with a sun
protection factor (SPF) of 15 or higher.
The ideal sun-protective fabrics are lightweight, comfortable, and protect
against exposure even when wet. A few companies in the United States
now make sun-protective clothing. They tend to be more tightly woven,
and some have special coatings to help absorb UV rays. Some sun-
protective clothes have a label listing the ultraviolet protection factor (UPF)
value -- the level of protection the garment provides from the sun's UV
rays (on a scale from 15 to 50+) . The higher the UPF, the higher the
protection from UV rays.
Children's swimsuits made from sun-protective fabric and designed to
cover the child from the neck to the knees are popular in Australia. They
are now available in some areas of the United States.
Newer products are now available to increase the UPF value of clothes
you already own. Used like laundry detergents, they add a layer of UV
protection to your clothes without changing the color or texture.
Use a sunscreen with a sun protection factor (SPF) of 15 or higher
A sunscreen is a product that you apply to your skin for some protection
against the sun's UV rays, although it does not provide total protection.
Sunscreens are available in many forms -- lotions, creams, ointments,
gels, wipes, and lip balms, to name a few.
Some cosmetics, such as lipsticks and foundations, also are considered
sunscreen products if they contain sunscreen. Some makeup contains
sunscreen, but only the label can tell you. Makeup, including lipstick,
without sunscreen does not provide sun protection. Check the labels to
find out.
Read the labels: When selecting a sunscreen product, be sure to read
the label before you buy. Experts recommend products with a sun
protection factor (SPF) of at least 15. The SPF number represents the
level of protection against UVB rays provided by the sunscreen -- a higher
number means more protection.
It is important to remember that sunscreen does not give you total
protection. When using an SPF 15 and applying it correctly, you get the
equivalent of 1 minute of UVB rays for each 15 minutes you spend in the
sun. So, 1 hour in the sun wearing SPF 15 sunscreen is the same as
spending 4 minutes totally unprotected.
Sunscreens labeled with SPFs as high as 100 are now available. Higher
numbers do mean more protection, but many people mistakenly think that
the SPF scale is linear -- for example, that a sunscreen with an SPF 45
rating would give 3 times as much protection as one with an SPF of 15.
This is not true. SPF 15 sunscreens filter out about 93% of UVB rays,
while SPF 30 sunscreens fitler out about 97%, SPF 50 sunscreens about
98%, and SPF 1 00 about 99%. The higher you go, the smaller the
difference becomes. No sunscreen provides complete protection.
Regardless of the SPF, sunscreen should be reapplied about every 2
hours.
The SPF number indicates protection against UVB rays only. Sunscreen
products labeled "broad-spectrum" protect against UVA and UVB radiation,
but at this time there is no standard system for measuring protection from
UVA rays. Products with an SPF of 15 or higher that also contain
avobenzone (Parsol 1789), ecamsule, zinc oxide, or titanium dioxide are
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
likely to be effective against UVB and most UV A rays.
The Food and Drug Administration (FDA), which regulates sunscreens in
the United States, has proposed a new set of rules for sunscreen labels.
Part of this includes a rating system for UVA protection. Under the new
system, sunscreens would be rated from 1 to 4 stars, with 1 star being a
low level of UVA protection and 4 stars being the highest. It is not yet
clear when this new rule might go into effect.
Check for an expiration date on the sunscreen container to be sure it is
still effective. Most sunscreen products are no longer as effective after 2 to
3 years.
Some sunscreen products can irritate skin. Many products claim to be
"hypoallergenic" or "dermatologist tested," but the only way to know for
sure whether a product will irritate your skin is to apply a small amount for
3 days. If your skin does not turn red or become tender and itchy, the
product should be okay for you.
Be sure to apply the sunscreen properly. Always follow the label
directions. Most recommend applying sunscreen generously to dry skin 20
to 30 minutes before going outside so your skin has time to absorb the
chemicals. When applying it, pay close attention to your face, ears, hands,
and arms, and generously coat the skin that is not covered by clothing. If
you're going to wear insect repellent or makeup, apply the sunscreen first.
For high-glare situations, a higher SPF sunscreen or zinc oxide may be
used on your nose and lips.
Be generous. About 1 ounce of sunscreen (a "palmful") should be used to
cover the arms, legs, neck, and face of the average adult. For best results,
most sunscreens must be reapplied at least every 2 hours and even more
often if you are swimming or sweating. Products labeled "waterproof" may
provide protection for at least 80 minutes even when you are swimming or
sweating. Products that are "water resistant" may provide protection for
only 40 minutes. Remember that sunscreen usually rubs off when you
towel yourself dry, so you will need to reapply.
Sunless tanning products, such as bronzers and extenders (described
below) , give skin a golden color. But unlike sunscreens, these products
provide very little protection from UV damage.
Wear a hat
A hat with at least a 2- to 3-inch brim all around is ideal because it
protects areas often exposed to the sun, such as the neck, ears, eyes,
forehead, nose, and scalp. A shade cap (which looks like a baseball cap
with about 7 inches of fabric draping down the sides and back) also is
good. These are often sold in sports and outdoor supply stores.
A baseball cap can protect the front and top of the head but not the back
of the neck or the ears, where skin cancers commonly develop. Straw
hats are not recommended unless they are tightly woven.
Wear sunglasses that block UV rays
Research has shown that long hours in the sun without protecting your
eyes increase your chances of developing eye disease. UV -blocking
sunglasses can help protect your eyes from sun damage.
The ideal sunglasses do not have to be expensive, but they should block
99% to 100% of UVA and UVB radiation. Check the label to be sure they
do. Some labels may say, "UV absorption up to 400 nm." This is the same
as 100% UV absorption. Also, labels that say "Meets ANSI UV
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
Requirements" mean the glasses block at least 99% of UV rays. Those
labeled "cosmetic" block about 70% of the UV rays. If there is no label ,
don't assume the sunglasses provide any protection.
Darker glasses are not necessarily better because UV protection comes
from an invisible chemical applied to the lenses, not from the color or
darkness of the lenses. Look for an ANSI label.
Large-framed and wraparound sunglasses are more likely to protect your
eyes from light coming in from different angles. Children need smaller
versions of real, protective adult sunglasses -- not toy sunglasses.
Ideally, all types of eyewear, including prescription glasses and contact
lenses, should absorb the entire UV spectrum. Some contact lenses are
now made to block most UV rays. But because they don't cover the whole
eye and surrounding areas, they are not recommended for eye protection
use alone.
Limit direct sun exposure during midday
Another way to limit exposure to UV light is to avoid being outdoors in
sunlight too long. UV rays are most intense during the middle of the day,
usually between the hours of 10 am and 4 pm. If you are unsure about the
sun's intensity, take the shadow test: If your shadow is shorter than you,
the sun's rays are the strongest. Plan activities out of the sun during these
times. If you must be outdoors, protect your skin.
UV rays reach the ground throughout the year, even on cloudy days. UV
rays can also pass through water, so don't think you're safe if you're in the
water and feeling cool. Be especially careful on the beach and in the snow
because sand and snow reflect sunlight, increasing the amount of UV
radiation you receive.
Some UV rays can also pass through windows. Typical car, home, and
office windows block most of the UVB rays but a smaller portion of UVA
rays, so even if you don't feel you're getting burned your skin may still get
some long-term damage. Tinted windows help block more UVA rays,
although this depends on the type of tinting. UV radiation that comes
through windows probably doesn't pose a great risk to most people unless
they spend extended periods of time close to a window that receives direct
sunlight.
If you plan to be outdoors, you may want to check the UV Index for your
area. The UV Index usually can be found in the local newspaper or on TV
and radio news broadcasts. It is also available on the EPA's web site at
www .epa.gov/sunwise/uvindex. html.
Avoid tanning beds and sunlamps
Many people believe the UV rays of tanning beds are harmless. This is
not true. Tanning lamps give out UVA and frequently UVB rays as well.
Both UVA and UVB rays can cause serious long-term skin damage, and
both contribute to skin cancer. Because of these dangers, many health
experts advise people to avoid sunlamps and tanning beds.
Protect children from the sun
Children require special attention, since they tend to spend more time
outdoors and can burn more easily. Parents and other caregivers should
protect children from excess sun exposure by using the measures
described above. Older children need to be cautioned about sun exposure
as they become more independent. It is important, particularly in parts of
the world where it is sunnier, to cover your children as fully as is
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
reasonable. You should develop the habit of using sunscreen on exposed
skin for yourself and your children whenever you go outdoors and may be
exposed to large amounts of sunlight. If you or your child burns easily, be
extra careful to cover up, limit exposure, and apply sunscreen.
Babies younger than 6 months should be kept out of direct sunlight and
protected from the sun using hats and protective clothing.
What about tanning pills and other tanning products?
Several products claim to give a tan without UV radiation.
Tanning pills and accelerators
Tanning pills contain color additives similar to beta-carotene, the
substance that gives carrots their orange color. The additives are
distributed throughout the body, especially the skin, turning it an orange-
like color. Although the Food and Drug Administration (FDA) has approved
some of these additives for coloring food, they are not approved for use in
tanning agents. They may be harmful at the high levels that are consumed
in tanning pills. The main ingredient in sunless tanning pills,
canthaxanthin, can show up in your eyes as yellow crystals, which may
cause injury and impaired vision. There have also been reports of liver and
skin problems, as well as one reported case of a woman who died from
aplastic anemia, which her doctor attributed to her use of tanning pills.
Tanning accelerators, such as lotions or pills that contain the amino acid
tyrosine or its derivatives, are not effective and may be dangerous.
Marketers promote these products as substances that stimulate the body's
own tanning process, although most evidence suggests they don't work.
The FDA considers them unapproved new drugs that have not been
shown to be safe and effective.
No tanning pills have been approved by the FDA.
Bronzers and extenders
Two other sunless tanning products, bronzers and extenders, are
considered cosmetics for external use and are not thought to be harmful
when used properly.
Bronzers, made from color additives approved by the FDA for cosmetic
use, stain the skin for a short time when applied and can be washed off
with soap and water.
Extenders (also known as sunless tanners or self-tanners) are applied to
the skin as lotions or creams, where they interact with protein on the
surface of the skin to produce color. Like a tan, the color tends to wear off
after a few days. The only FDA-approved color additive for extenders is
dihydroxyacetone (DHA). Because application of these products can
sometimes lead to uneven coloring, some tanning salons have begun to
offer whole body sprays in tanning booths. A concern here is that DHA is
approved for external use only and should not be sprayed in or on the
mouth, eyes, or nose. People who choose to get a DHA spray should
make sure to protect these areas.
Although they can give skin a darker color, these products do not protect
you from the damaging effects of UV radiation.
Examining your skin
Get your skin checked by your doctor
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
As part of a routine cancer-related checkup, your doctor should check
your skin carefully. He or she should be will ing to discuss any concerns
you might have about this exam.
How to check your own skin
It's important to check your own skin, preferably once a month. A self-
exam is best done in a well -lit room in front of a full - length mirror. You
can use a hand-held mirror for areas that are hard to see. A spouse or
close friend or family member may be able to help you with these exams,
especially for those hard-to-see areas like the lower back or the back of
your thighs.
The first time you inspect your skin, spend a fair amount of time carefully
going over the entire surface of your skin. Learn the pattern of moles,
blemishes, freckles, and other marks on your skin so that you'll notice any
changes next time. Any trouble spots should be seen by a doctor. Follow
these step-by-step instructions to examine your skin:
Face the mirror:
Check the underarm areas, both
sides of your arms, the tops and
bottoms of your hands, in between
your fingers, and fingernail beds.
Check your face, ears, neck, chest,
and belly. Women will need to lift
breasts to check the skin
underneath.
Sit Down:
Check the front of your thighs, shins,
tops of your feet, in between your
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
You will need a hand mirror for
your thighs, back, and scalp.
Now look at the bottoms of your feet,
your calves, and the backs of your
thighs, first checking one leg and
then the other.
toes, and toenail beds.
Use the hand mirror to check the
buttocks, genital area, lower back,
upper back, and the back of the
neck.
Or it may be easier to look at your
back in the wall mirror using a hand
mirror.
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
Use a comb or hair dryer to part your
hair so that you can check your
scalp.
What should I look for?
Basal and squamous cell cancers
Basal cell cancers and squamous cell cancers are most often found in
areas that get exposed to a lot of sun, such as the head, neck, and arms,
but they can occur elsewhere. Look for new growths, spots, bumps,
patches, or sores that don't heal after 2 to 3 months.
Basal cell carcinomas often look like flat, firm, pale areas or small, raised,
pink or red, translucent, shiny, waxy areas that may bleed after a minor
injury. They may have one or more abnormal blood vessels, a lower area
in their center, and/or blue, brown, or black areas. Large basal cell
carcinomas may have oozing or crusted areas.
Squamous cell carcinomas may look like growing lumps, often with a
rough, scaly, or crusted surface. They may also look like flat reddish
patches in the skin that grow slowly.
Both of these types of skin cancer may develop as a flat area showing
only slight changes from normal skin.
Actinic keratosis, also known as solar keratosis, is a skin condition that is
sometimes pre-cancerous and is caused by too much sun exposure.
Actinic keratoses are usually small (less than V4 inch) , rough spots that
may be pink-red or flesh-colored. Usually they develop on the face, ears,
back of the hands, and arms of middle-aged or older people with fair skin,
although they can arise in younger people or on other sun-exposed areas
of the skin. People with one actinic keratosis usually develop many more.
Some can grow into squamous cell cancers, but others may stay the same
or even go away on their own. Because they can turn cancerous, such
areas should be looked at regularly by a doctor. Your doctor can then
decide whether these areas should be removed.
Melanomas
The "ABCD rule" is an easy guide to the usual signs of melanoma. Be on
the lookout and tell your doctor about any spots that match the following
description:
A is for ASYMMETRY: One half of a mole or birthmark does not
match the other.
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
B is for BORDER: The edges are irregular, ragged, notched, or
blurred.
C is for COLOR: The color is not the same all over and may
include shades of brown or black, or sometimes with patches of
pink, red, white, or blue.
D is for DIAMETER: The spot is larger than 6 millimeters across
(about 1J4 inch -- the size of a pencil eraser), although melanomas
can sometimes be smaller than this.
Another very important sign of possible melanoma is a change in the size,
shape, or color of a mole or the appearance of a new spot. Some
melanomas do not fit the ABCD rule described above, so it is very
important to tell your doctor about any changes in skin markings or new
spots on your skin.
Other warning signs are:
a sore that does not heal
spread of pigment from the border of a spot to surrounding skin
redness or a new swelling beyond the border
change in sensation -- itchiness, tenderness, or pain
change in the surface of a mole -- scaliness, oozing, bleeding, or
the appearance of a bump or nodule
a mole that looks very different from your other moles
What if I find something suspicious?
It's important to know the difference between melanoma and a harmless
mole. A normal mole is most often an evenly colored brown, tan, or black
spot on the skin. It can be either flat or raised. It can be round or oval.
Moles are usually less than 1/4 inch across, or about the width of a pencil
eraser. Moles can be present at birth or they can appear later. Several
moles can appear at the same time.
Once a mole has developed, it will usually stay the same size, shape, and
color for many years. Moles may fade away in older people.
Most people have moles, and almost all moles are harmless. But it is
important to recognize changes in a mole -- such as its size, shape, or
color -- that suggest a melanoma may be developing.
Be sure to show your doctor any area that concerns you. A qualified
doctor should be able to identify any suspicious areas you may have. If
your doctor suspects you might have skin cancer, he or she will use one
or more of the following methods to find out.
History and physical exam
Usually the first step is to take your medical history (ask questions about
symptoms and risk factors). The doctor probably will ask your age, when
the mark on the skin first appeared, and if it has changed in size or
appearance. You may also be asked about past exposures to known
causes of skin cancer and if you or anyone in your family has had skin
cancer.
During your physical exam, your doctor will note the size, shape, color,
and texture of the area in question, and if there is bleeding or scaling. The
rest of your body may be checked for spots and moles that may be related
to skin cancer.
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
The doctor may also feel the lymph nodes (bean-sized collections of
immune system cells) under the skin near the suspicious area. Some skin
cancers may spread to lymph nodes. Affected lymph nodes may become
larger and firmer than usual.
If you are being seen by your primary doctor and skin cancer is
suspected, you may be referred to a dermatologist (a doctor who
specializes in skin diseases), who will look at the area more closely.
Along with a standard physical exam, many dermatologists use
dermoscopy (also known as epiluminescence microscopy (ELM) , surface
microscopy, or dermatoscopy) to help determine if a spot might be a
melanoma or other type of skin cancer. This involves the use of a
dermatoscope, which is a special magnifying lens and light source held
near the skin. Sometimes the doctor will use a thin layer of oil with this
instrument. A digital or photographic image of the spot may be taken. The
use of these tests by experienced dermatologists can improve accuracy in
finding skin cancers early. It can also often reassure you that a lesion is
benign (non-cancerous) without the need for a biopsy.
Skin biopsy
If the doctor thinks that an area of skin might be cancerous, he or she will
take a sample of skin from that area to look at under a microscope. This is
called a skin biopsy. Different methods can be used for a skin biopsy. The
choice of method depends on the possible type of skin cancer, where it is
on the body, and the size of the affected area. For more detailed
information on biopsies, see our documents, Melanoma Skin Cancer and
Skin Cancer: Basal and Squamous Cell.
If a spot is found to be cancerous or pre-cancerous, your doctor may
recommend further tests or treatment. If the spot is small and localized, a
more extensive biopsy or some type of surgery may be needed. For
cancers that might be more extensive (especially melanomas) , imaging
tests might be done, and treatment might include chemotherapy or
radiation. Again, for more detailed information, see our skin cancer
documents.
Additional resources
More information from your American Cancer Society
The following information may also be helpful to you. These materials may
be ordered through our toll-free number, 1 -800-ACS-2345.
Melanoma Skin Cancer (also available in Spanish)
Skin Cancer: Basal and Squamous Cell (also available in Spanish)
Sun Basics: Skin Protection Made Simple (brochure for children
aged 8 to 14)
Why You Should Know About Melanoma (also available in Spanish)
National organizations and Web sites*
In addition to the American Cancer Society, other sources of information
and support include:
American Academy of Dermatology
Toll -free number: 1-888-462-3376 (1-888-462-DERM)
Web site: www. aad.org
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
ACS :: Skin Cancer Prevention and Early Detection
National Cancer Institute
Toll -free number: 1-800-422-6237 (1-800-4-cancer); TYY: 1-800-332-
8615
Web site: www.cancer.goy
Skin Cancer Foundation
Toll-free number: 1-800-754-6490 (1-800-SKIN-490)
Web site: www.skincancer.org
*Inclusion on this list does not imply endorsement by the American Cancer
Society.
No matter who you are, we can help. Contact us anytime, day or night, for
information and support. Call us at 1-800-ACS-2345 or visit
www.cancer.org.
References
American Cancer Society. Cancer Facts and Figures 2009. Atlanta, Ga:
American Cancer Society; 2009.
Carucci JA, Rigel OS, Friedman RJ. Basal cell and squamous cell
carcinomas of the skin. In: Lenhard RE Jr, Osteen RT, Gansler T, eds.
Clinical Oncology. Atlanta, Ga: American Cancer Society; 2000:563-576.
Food and Drug Administration. FDA Proposes New Rule for Sunscreen
Products. 2007. Available at:
www.fda.gov/bbs/topics/ NEWS/2007/NEW01687.html. Accessed April 2,
2008.
Food and Drug Administration. Sunless Tanners and Bronzers. 2006.
Avai lable at: www.cfsan.fda.gov/-dms/cos-tan4.html. Accessed April 2,
2008.
Levy SB. Sunscreens and Photoprotection. eMedicine. 2006. Available at:
www.emedicine.com/derm/topic510.htm. Accessed April 2, 2008.
Meadows M. Don't Be in the Dark About Tanning. FDA Consumer.
2003;37:16-17. Available at: www.fda.gov/fdac/features/2003/603_tan.html.
Accessed April 2, 2008.
Naylor MF, Rigel OS. Current concepts in sunscreens and usage. In: Rigel
OS, Friedman RJ, Dzubow LM, Reintgen OS, Bystryn JC, Marks R, eds.
Cancer of the Skin. Philadelphia, Pa: Elsevier Saunders; 2005:71 -83.
Last Medical Review: 06/11/08
Last Revised: 05/21/09
I About ACS I Employment & Volunteer Opportunities I Legal & Privacy Information I Press Room
Copyright 2009 American Cancer Society, Inc.
All content and works posted on this website are owned and
copyrighted by the American Cancer Society, Inc. All rights reserved.
http://www .cancer.org/docroot/PED/content/ped_7 _l_Skin_ Cancer_Detection_ What_ You_ Can_Do.asp?sitearea=&level=[ 12/1/2009 8:37:06 PMl
190
Origi nal Article
Indoor Tanning Use Among
Adolescents In the US, 1998 to 2004
Vi lma Cokkinides, PhD
1
, Marti n Weinstock, MD, PhD
2
5
, DeAnn Lazovich, PhD
6
, Eli zabeth Ward, PhD
1
,
and Michael Thun, MD, MS
1
BACKGROUND: A recent meta-analysis found that indoor tanning use before the age of 35 years increases
t he risk of melanoma. supporting policies to restrict indoor tanning use among adolescents. The objectives
of the current study were to provide a national assessment of prevalence and trends of indoor tanning use
among US adolescents, to examine changes in the prevalence of indoor tanning use from 1998 to 2004 in
relation to state pol icies on minors' access, and to assess the prevalence of burns, rashes, and infections
among users. METHODS: Two cross-sectional population-based surveys of US yout hs ages 11 to 18 years
and t heir parent s/guardians conducted in 1998 (N = 1196) and 2004 (N = 1613) used identical questions to
assess use of indoor tanni ng and correlates of this behavior. RESULTS: The prevalence of indoor tanning
use by adolescents wit hi n the past year changed lit t le from 1998 to 2004 (10% to 11%). In states with poli-
cies regarding minors' access to indoor tanning, the prevalence stayed the same or decreased from 1998 to
2004, whereas it increased in states wit hout such poli cies. Neither t rend was found to be stat istical ly signif-
icant. Youth tanning atti tudes, parental indoor tanning use. and parents' permission were st rongly associ-
ated with yout h use of indoor t anning. Fifty-eight percent of users reported burns from indoor tanni ng.
CONCLUSIONS: The presence of state legislation restricting mi nors' access to indoor tanning appears to
have limited effectiveness, perhaps because most states' policies permit use with parental consent . Multi-
pronged approaches are needed to reduce indoor tanning use in yout hs. Cancer 2009;115:190-8. Published
2008 by the American Cancer Society!
KEY WORDS: nonsolar ultraviolet radiation. skin cancer prevent ion, adolescents. indoor t anning.
Artificial (indoor) tanning can be a common source of ultraviolet radiation (UVR) . Exposure of the
skin to UVR in tanning booths has several adverse health consequences, including skin and eye burns,
alterations of immune system function, photo-aging, photo-induced medication reactions, and increased
risk of skin cancers.
1
Recently, a large meta-analysis concluded char first exposure ro sunbeds before 35
years of age was significantly associated wi th an increased risk of melanoma, based on 7 informative studies
(swnmary relative risk, 1.75; 95% confidence interval [95% CI], 1.35-2.26)_2
Corresponding author: Vilma Cokkinides, PhD, Department of Epidemiology and Surveillance Research, American Cancer Society, 250 Williams
Street, NW, Atlant a, GA 30303-1002; Fax: (404) 327-6450; vcokkini@cancer,org
'Department of Epidemiology and Surveillance Research, American Cancer Society, Atlanta, Georgia;
2
DermatoEpidemiology Unit, Providence Veter-
ans Affai rs Medical Cent er, Providence, Rhode Island;
3
Department of Dermat ology, Brown University, Providence, Rhode Island;
4
Department of
Community Health, Brown University, Providence, Rhode Island;
5
American Cancer Society Skin Cancer Advisory Group, American Cancer Society,
Atlanta, Georgia;
6
Division of Epidemiology and Community Heal th, Universi ty of Minnesota, Minneapolis, Minnesota
*This article Is a U.S. Government work and, as such, is in the public domain in the United States of America.
Received: May 21, 2008; Revised: August 4, 2008; Accepted: August 6, 2008
Published online: December 10, 2008, Published 2008 by the American Cancer
001: 10.1 002/cncr.2401 0, www.int erscience.wi ley.com
Cancer January 1, 2009
Previous studies conducted in adolescents have shown
that the prevalence of indoor tanning use varies by sex
(ranging from 2% to 11% in boys and from 12% to 37%
in girls); this behavior is more prevalem in older adoles-
cent girls, in those who intentionally ran outdoors or have
positive attitudes toward a tan, and in those less likely to
use sunscreens.
3
"
6
Some studies have found that social
influences, such as having friends or parents who use
indoor tanning or having parental permission to use
indoor tanning, are correlated with indoor canning use by
adolescenrs.
3
7
Because of the known health risks associ-
ated with indoor tanning, many health-related organiza-
tions recommend limiting minors' access to indoor
. 'I' . th h I . I
2
'
8
tannmg ac1 mes roug regu anon. '
In the US, some states have passed legislation to
limit minors' access to indoor tanning. Statutory require-
mems vary by state. Nearly all states permit minors' access
with parental consent and/or accompaniment, and only a
few prohibit access based on minors' age.
9
"
11
Studies sug-
gest that compliance with minors' access restrictions varies
by state.
9
12
"
14
In 1 study in which compliance with laws
regarding access to customers aged < 15 years was assessed
by telephone, the percentage of establishments adhering
ro the state's requirement was 11% in Texas, 77% in Wis-
consin, and 80% in Illinois.
9
No prior study has assessed
whether indoor tanning use among adolescents differs in
states with youth access legislation versus states with no
such state laws.
Our objective was ro analyze data from 2 national
population-based surveys (1998 and 2004, respectively)
that collected information regarding the recent use of
indoor tanning in adolescents aged 11 to 18 years. In the
current study, we assessed the change in past-year use of
indoor tanning among adolescents between 1998 and
2004; in addition, we examined whether state legislation
restricting minors' access ro indoor tanning is associated
with youths' use of indoor tanning after controlling for
significant correlates and assessed short-term adverse
effects from recem use of indoor tanning (eg, burns).
MATERIALS AND METHODS
In 1998, and again in 2004, the American Cancer Soci-
ery conducted 2 national, population-based, cross-sec-
tional telephone surveys of behaviors related to skin
cancer risk among youths ages ll to 18 years and their
Cancer January 1. 2009
Indoor Tanning by US Ad olescents I Cokkinides et al
primary caregivers in the continental US. The surveys
were conducted from August to November of the re-
spective years. The surveys consisted of a youth imer-
view (requiring permission and consem from a parent
or caregiver) and a nearly identical parem module that
asked questions regarding solar and nonsolar exposure
and sun protection behaviors. The 1998 survey had a
sample of 1196 youth-caregiver pairs; the 2004 subse-
quent survey had a sample of 1613 such pairs. Both sur-
veys used a similar telephone-based sampling
methodology (dual list-assisted random digit dialing
methodology), field operations (training and monitoring
of interviewers), and data collection surveys. According
to standard formulas to estimate responses of telephone-
based surveys, the overall response rate was 58% in
1998 and 44% in 2004. Despite lower response rates,
there were no significant demographic differences noted
among sampled adolescents by time periods. In a prior
published study of trends in sun exposure and sun pro-
tection behaviors,
15
we tested for any significant differ-
ences in the demographic profile of youths between the
2 surveys and determined that the samples were compa-
rable. The adolescents surveyed were mostly white
(77%), with a mean age of 14 years and a sex ratio of
nearly 1:1.
15
Additional information regarding survey
methodology and statistical comparabiliry of the 2 sam-
ples can be found elsewhere.
15
Both surveys asked iden-
tical questions regarding the use of indoor tanning
booths or sunlamps, frequency within rhe past year,
demographics, individual susceptibility to UV exposure,
and attitudes toward tanning. The 2004 survey also
asked about burns or skin rashes incurred from indoor
tanning use.
Measures
Use of Indoor Tanning and Adverse
Reactions From Indoor Tanning
Participants were asked whether in the past year they
had used an indoor tanning booth or sunlamp and the
number of times (frequency of use) during the past year.
The 2004 survey asked users a question regarding burns
from indoor canning ("got red or burned at any time in
the past when you used tanning booth or a sunlamp") and
another question concerning skin infection or rash ("ever
got an infection or skin rash from a tanning booth").
191
Original Article
Demographics and Skin Type
Each survey asked participants' age, sex, and race, and
4 questions relating to phenotypic skin characteristics (ie,
tendency of the skin to burn, ability to tan, natural skin
color, and hair color). From these, we derived a composite
measure of sun sensitivity based on a validated measure.
16
Attitudinal Correlates and Social Factors
Tanning attitudes were assessed using 2 items ("I feel
healthy when I have a nice tan" and "I look betrer when I
have a tan") anchored on a 5-point Likert format from
strongly agree to strongly disagree (Cronbach r:1. of .69). In
the 2004 survey, a new attitudinal item was added ("even
though it may not be good for me, I still like to get a tan"),
with a similar Likert format. This was combined with the
other 2 attitudinal items to derive a composite tanning atti-
tudinal factor (Cronbach \1. of .77) and used in the multi-
variate logistic analysis ro assess correlates of indoor
tanning use. In addition, in the 2004 survey, we assessed
parental permission by asking youths about their level of
agreement with the following statement: "My parents/
guardian would allow me to use indoor sunlamps or
booths." Recent evidence suggests that this particular factor
is a strong determinant of youth indoor tanning use? '
7
Sunscreen Use
The frequency of using sunscreen in the most recenr
summer was assessed by asking "how often was sunscreen
applied when going outside during the summer?" and
"how often was sunscreen with SPF (skin protection fac-
tor) 15+ used when at the beach or at the pool?"
Responses to these questions were provided on a 5-point
scale ranging from always ro never.
Parental Factors
Similar questions from the parenr/caregiver survey
were used to collect information regarding their use of
indoor tanning booths or sunlamps in the past year as well
as their demographic and educational status.
Legislation Restricting Minors' Access
to Indoor Tanning
We reviewed policy-based reports regarding if and
when states had passed regulations restricting minors'
access ro indoor tanning.
10
'
18
This information was linked
tO the state of residence of respondents and used to derive
192
Table 1. Listing of Stat es With Legislation on Minors'
Access Rest rict ions to Indoor Tanni ng
Policy Dates
Prior to 1998 and up to 2004, n = 8
From 1998 and up to 2004, n = 11
State, Date of Statute
California, 1997
Georgia, 1996
Louisiana, 1992
Maine, 1996
Massachusetts, 1996
Minnesota, 1995
Missi ssippi, 1989
Tennessee, 1996
Florida, 1998
Illinois, 2001
Indiana, 1999
Michigan, 2001
North Carolina, 2001
Ohio, 2001
Oregon, 2000
Rhode Island, 1998
South Carolina, 2001
Texas, 2001
Wisconsin, 1999
Polley reports used in reference to state legislation: Mclaughlin et allO and
Francis et al.
18
a state-policy indicator to be used for analysis. The catego-
ries of this state-policy indicator variable were developed
using a coding of state level policies that took into account
when legislation was implememed and the possibili ty of
repeal by 2004.
10
'
18
Hence, state poli cies were categorized
into 3 levels: 1) states that passed legislation before 1998
and retained the policy through 2004 (8 states); 2) states
that passed legislation between 1998 and 2004 (11 states);
and 3) states that had no legislation on this issue during
the 1998 to 2004 period of interest. (See Table 1 for addi-
tional information regarding listing of states that had laws
passed during the study period.)
Statistical Analysis
For both surveys, sampling weights took into account
unequal probabilities of selection because of sampling
design, nonresponse, and poststratiflcation. Data manage-
ment was conducted using SAS statistical software (ver-
sion 9.1; SAS Institute Inc, Cary, NC).
19
All descriprive
and multivariate analysis were conducted using SUDAAN
statistical software (version 9.0; Research Triangle Insti-
tute, Research Triangle Park, NC).
20
This software takes
into account the complex survey sampling design and
san1pli ng weights to derive appropriate standard errors
used for statistical testing and derivation of 95% Cis for
the weighted analysis.
Cancer Januar y 1, 2009
Assessment of Change in Indoor
Tanning Use
Weighted srarisrics were used ro describe the prevalence
estimates of indoor tanning and number of times of
indoor tanning use within the past year (because of the
skewed distribution of the latter variable, the median
rather than the mean was used). To examine differences
between 1998 and 2004, we subtracted the corresponding
weighted percentages (of past-year use of indoor tanning
and median number of times indoor tanning was used
within the past year) and calculated 95% Cis around these
differences. By using general linear contrasts, we rested
the statistical significance of trends.
Predictors of Indoor Tanning Use
Among Adolescents
A set of predictor variables, which included age, sex, skin
sun sensitivity, attitudes toward having a tan, and parental
factors, was selected based on previous research
3
'
4
; the key
predictor of inrerest was state policy on minor's access to
indoor tanning. By performing (unadjusted) univariate
analysis, we examined the unadjusted correlation between
these predictors and indoor tam1ing use within the past
year. From these analyses, all factors significant at P = .05
were considered for the weighted multivariate logistic
regression that examined the independent association
between stare minors' access restrictions and youth indoor
tanning use. Multivariate logistic regression modeling was
used to test for differences in the likelihood of adolescents'
indoor tanning use in stares with policies relative to states
without such policies after controlling for important cova-
riates (see previously described measures).
Predictors of Burns From Indoor Tanning
Using data from the 2004 survey, we estimated the preva-
lence of burns and skin rash from indoor tanning in ado-
lescenr users of sunlamps or ranning boorhs within the
past year. Weighted bivariate analysis were conducted to
assess individual characteristics (age, sex, skin sun sensitiv-
ity) associated with self-reported adverse effects from
indoor tanning. These individual factors were used as con-
trol factors in the assessment of the independent relation
bervveen experience of burns from indoor tanning and
frequency of use among youths reporting use of indoor
Cancer January 1. 2009
Indoor Tanning by US Adolescents I Cokkinides et al
tanning within the past year. Because a small number of
skin rashes were reported, we were unable to conduct
multivariate analysis of this characteristic.
RESULTS
Trends in Indoor Tanning
Nationally, the prevalence of indoor tanning use among
adolescents changed litrle from 1998 ro 2004 (a 1 o/o
increase; 95% CI, -1.5%-3.5%) (Table 2). Although not
statistically significant, increases in the prevalence of past-
year use of indoor tanning were observed among: girls
(from 15.6% to 17.7%), youths ages 14 to 15 years (from
7.1 o/o to 1 0.5%), those with medium sun sensitivity (from
10% ro 13.5%), and those with positive attitudinal prefer-
ences for a tan (from 18.8% to 25%). A significant
increase was noted in those who reported applying
sunscreen often or always while outdoors on sunny days
(3.7% increase; P = .02), although this group had a lower
prevalence of indoor tanning use. In contrast, among
youths whose parents used indoor tanning, there was a
slight decrease in use of indoor tanning between 1998 and
2004 (from 29.5% to 27.2%). We found a nonsignificant
declining trend in the prevalence of indoor tanning use
over the time period (1998-2004) in states with legislation
that restricted access to indoor tanning by minors com-
pared with those without such legislation.
Between 1998 and 2004, the median number of
times indoor tanning was used during the past year was
stable (Table 2). Characteristics predictive of indoor tan-
ning use 26 rimes within the past year included older
adolescence, female sex, mediwn Slm sensitivity, and
positive attitudes toward tanning.
Predictors of Indoor Tanning
Multivariate analysis identified 5 factors significantly
associated with indoor tanning use (Table 3): older age (in
those ages 16-18 years; adjusted prevalence odds ratio
[aPOR] of 4.26 [95% CI, 1.91-9.47]), female sex (aPOR
of 10.60; 95% CI, 5.74-19.59), positive attitudes toward
a ran (aPOR of 8.65; 95% CI, 3.49-21.40), having a par-
ent/guardian who used indoor tanning within the previ-
ous year (aPOR of 4.18; 95% CI, 2.20-7.90), and
parental permission ro use indoor tanning as reported by
193
Original Article
Table 2. Prevalence and Change i n Past Year Use of Indoor Tanni ng in Youths Between 1998 and 2004 and Among Past
Year Users: Median Change in the Frequency of Use of Indoor Tanning Between 1998 and 2004
Indoor Tanning Use Within
the Past Year, Prevalence
1998 2004 Change,
% (95% Cl)
No. % No. %
Overall 1196 10.1 1589 11.1 1.0 (- 1.53.5)
Sex
Male 602 4.8 808 4.8 0.0 (-2.6-2.6)
Female 594 15.6 781 17.7 2.1 (-2.1 -6.3)
Age, y
11-13 506 3.8 533 2.7 - 1.1 (-3.9-1.7)
14-15 289 7.1 437 10.5 3.4 (-0.7-7.6}
16-18 400 19.5 609 19.7 0.3 (-5.1 -5.6)
Race
White 1019 11.0 1372 12.8 1.8 (-1.1-4.6}
Nonwhite 166 7.0 207 5.1 - 1.9 (-7.3-3.5)
Skin sun sensitivity index*
Low 318 11.8 417 11.0 - 0.8 (-5.5-4.0}
Medium 591 10.0 768 13.5 3.5 (-0.3-7.3)
High 287 8.3 400 6.6 - 1.7 (-6.3-2.9)
Attitudes toward a tan
High 196 18.8 213 25.0 6.2 (-2.4-14.6)
Medium 425 10.7 630 14.3 3.6 (-1.08.1)
Low 444 6.8 729 5.4 - 1.4 (-4.5-1.7}
Used sunscreen on sunny days
Always or often 391 6.0 668 9.7 3.7 (0.2-7. 1)t
Sometimes 354 12.6 516 11.2 - 1.4 (-6.13.2)
Rarely or never 450 11.6 404 12.6 1.0 (-3.8-5. 7)
Used sunscreen with SPF 15+ at beach/pool
Always or often 583 7.0 951 8.4 1.4 (-1.5-4.2)
Sometimes 224 11.9 336 15.2 3.3 (-3.09.6}
Rarely or never 178 15.5 288 14.2 - 1.3 (- 10.3-3.8)
Parent/guardi an used indoor tanning in the past year
Yes 103 29.5 188 27.2 - 2.3 (-13.8-9.3)
No 1093 8.5 1401 9.0 0.5 (-2.0-3.0)
State has legisl ati on restricti ng youth indoor tanning
Policies+ present before 1997 247 8.4 311 8.0 - 0.4 (-5.1-4.3)
Policies present after 1997 (up to 2004) 411 12.5 570 10.0 - 2.5 (-6.8-2.0}
No policiesll throughout 1998-2004 538 9.4 708 12.9 3.5 (-0.3-7.3)
95% Cl indicates 95% confidence interval; SPF, sun protection factor.
Skin sun sensitivity index based on ability to tan, ability to burn, and natural hair and color of the skin.
t P < .05.
t Eight states had legislation restricting minors' access to indoor tanning before 1997 and through 2004.
Eleven states had not passed legislation after 1997 and through 2004.
II Remaining states with no such legislation passed in both 1998 and 2004.
Frequency of Use
Among Users
1998 2004 Change,
(n= 123), (n = 204), % (95% Cl)
median median
6.4 6.0 - 0.4 (- 4.0- 3.3)
3.7 4.1 0.4 (-3.24.1)
6.9 8.5 1.6 (-1.9-5.1)
2.6 4.1 1.5 (-1.84.8)
7.1 4.0 - 3.1 (-10.0-3.7)
7.8 8.9 1.1 (-3.35.5)
7.9 6.1 - 1.8 (-5.3-1.7}
2.1 5.3 3.2 (-6.4 12.7)
6. 1 11.3 5.2 (-3.0-13.4)
9.0 5.1 - 3.9 (-8.7-1.0)
3.3 4.0 0.7 (-3.1-4.4)
8.5 9.7 1.2 (-5.5-7.9)
6.5 5.6 - 0.9 (-6.5 4.7)
5.3 4.3 -1.0 (-4.2-2.2)
7.0 4.9 - 2.1 (-5.7-1.6)
5.0 8.7 3.7 (-2.4-9.8)
6.3 6.4 0.1 (-7.47.6}
5.6 5.7 0.1 (- 3.6-3.9)
5.2 5.0 - 0.2 (-6.6-6.3}
11.0 8.4 - 2.6 (- 11.8-6.6)
6.6 9.0 2.4 (-6.6-11.4)
6.4 5.4 -1.0 (-4.6-2.2)
6.8 3.0 - 3.8 (-8.9-1.4)
5.4 8.7 3.3 (-0.7-7.3)
7.8 5.0 - 2.8 (-7.5-1.8)
rhe adolescent (aPOR of 15.42; 95% CI, 8.94-26.60) .
State legislation restricting access to indoor tanning was
nor found ro be significantly associated with indoor can-
ning use in either unadjusted or adjusted analyses (aPOR
of0.77; 95% cr. 0.49-1.21).
Adverse Effects From Indoor Tanning Use
194
Among 204 adolescents who used indoor tanning booths/
sunlamps within the past year, the self-reported occur-
rence of burns from indoor tanning was 57.5% (Table 4).
The occurrence of burns from indoor tanning was found
Cancer January 1, 2009
Indo or Tanning by US Adolescents I Cokki n ides et al
Table 3. Predictors of Youth Indoor Tanni ng (Booths/Sunlamps) Use in the Past Year
Age, y
11-13
14-15
16-18
Sex
Female
Male
Skin sun sensitivity indext
Low (bottom tertile score)
Medium
High (top t ertile score)
Attitudes toward tanning preferences
High (top tertile score)
Medium (medium tertile score)
Low (bottom tertile score)
Unadjusted
POR* (95% Cl)
1.00
3.89 (1.87-8. 12)
8.04 (4.02-1 6.08)
4.74 (3.18-7.07)
1.00
1.00
1.23 (0.84-1.82)
0.55 (0.34-0.90)
10.72 (5.34-21.53)
3.57 (1.65-7.75)
1.00
State has legislat ion restricting minors' access to indoor tanning:
Policies present before 199711 0.64 (0.40-1.00)
Policies passed after 19g7 (up to 2004)'[ 0.75 (0.52-1 .0g)
No policies# duri ng 1gg8 and 2004 1.00
Parental factors: parent/ guardian used indoor tanning booth in t he past year
Yes 4.61 (3.04-6.97)
~ ~
My parents/guardian would allow me to tan indoors using a sunlamp or a tanning booth
Agree 20.3 (13.2-31.40)
Di sagree 1.00
Parent education
~ h i g h school
Some college
College graduate
POR indicates prevalence odds ratio; 95% Cl, 95% confidence interval.
Unadjusted POR and corresponding 95% Cis enclosed in parenthesis.
t Adjusted POR and corresponding 95% Cis enclosed in parenthesis.
1.53 (0.99-2.36)
1.39 (O.g9-2.05)
1.00
t Skin sun sensitivity index based on ability to tan, ability to burn, and natural hair and natural color of the skin.
Attitudes toward tanning preferences (based on 3 attitudinal items; refer to measure specification in text).
II Eight states had legislation restricting minors' access to indoor tanning before 1997 and through 2004.
'jJ Eleven states had not passed legislation after 1997 and through 2004.
#Remaining states with no such legislation passed in both 1998 and 2004.
DISCUSSION
Adjusted
POR (95% Cl)t
1.00
2.00 (0.85-4.60)
4.26 (1.91-9.50)
10.60 (5.73-19.60)
1.00
1.00
1.55 (0.88-2.71)
0. 71 (0.35-1.43)
8.84 (3.57-21.86)
3.36 {1.24-9.1 0)
1.00
0.77 (0.43-1.39)
0. 76 (0.45-1.29)
1.00
4.21 (2.23-7.98)
1.00
15.55 (9.02-26.80)
1.00
1.01 {0.55-1.85)
1.20 (0.72-2.00)
1.00
to be significantly associated with the frequent use of
indoor tanning (26 sessions within the past year; odds ra-
tio [OR] of3.23 (95% CI, 1.63-6.39]), but was not found
to be related tO sex, age, or sun sensitivity.
Among 204 adolescents who used indoor tanning
boorhs/sunlamps, 7 reported ever getting an infection or a
skin rash (estimated prevalence of 3%) from indoor tan-
ning. These 7 were all aged 2 15 years, were mostly girls
(n = 6), and had high levels of skin sun sensitivity (n = 5)
(data not shown) .
The principal findings from these 2 population-based sur-
veys of adolescents was that nationally the prevalence of
past-year use of indoor tanning did not change from 1998
to 2004 (10% to 11 %), despite an increasing number of
states restricting such use by minors. The prevalence of
indoor tanning use increased nonsignificandy among
youths who resided in states that lacked policies to control
minors' access ro indoor tanning and decreased nonsigni-
ficantly in states that enacted policies. States that had
Cancer January 1, 2009 195
Original Article
Table 4. Prevalence and Correlates of Erythema From Indoor Tanning Use Among Adolescent s Who Used
Indoor Tanning Booths/Sunlamps
Erythema Univariate Multivariate
or Burns,*% OR (95% Cl) Logistic Model for
Erythema/Burns,
AOR (95% Cl)
Total 204 57.5
Sex
Female 161 61. 1 1.96 (0.91-4.20) 1.96 (0.89-4.33)t
Male 43 44.6 1.0 1.0
Age, y
11-15 14 50.8 1.0 1.0
16-18 137 61.0 1.50 (0.76-2.95) 1.46 (0. 73-2.92)t
Skin sun sensitivity index
Low 58 55. 1 1.0 1.0
Medium 112 57.2 1.10 (0.53-2.23) 1.17 (0.56-2.44)
High 34 64.0 1.45 (0.57-3.69) 1.46 (0.56-3.93)
No. of times used i ndoor tanning within the past year
;::6 107 72.1 3.41 (1 . 78-6.54) II 3.23 (1.63-6.39)11.1
1-5 97 42.5 1.0 1.0
OR indicates odds ratio; 95% Cl. 95% confidence interval; AOR, adjusted odds ratio.
Adverse event assessed as 'Have you gotten red or burned at any time in the past when you used a tanning booth or a sunlamp?'
t AOR adjusted for sex.
t AOR adjusted for age.
AOR adjusted for sex and age.
IIP<.o001.
'll AOR adjusted for age, sex, and skin sun sensitivity.
minors access resmctwn policies had lower odds of
indoor tanning use among adolescents (unadjusted OR of
0.64; 95% CI, 0.40-1.00) compared with states that
lacked such policies. However, after controlling for
strongly associated (more proximate) determinants of
indoor tanning use in youths, state policies were not sig-
nificantly associated with indoor tanning (adjusted OR of
0.77; 95% CI, 0.43-1.39) .
Strengths of the current study include the use of
standardized methods and questions ro assess trends in
indoor tanning use over rime, the inclusion of nationally
representative samples of adolescents, and the abil ity to
examine and control for multiple factors associated with
indoor tanning use. Limitations of the study include reli-
ance on self-reports of both youths and primary care givers
and a sample size that was limited for certain analyses.
Our study's sample was limited to reliably estimate preva-
lence of less common evenrs from indoor tanning use (ie,
rash or skin infections) and to assess state-to-state varia-
tions in minors' indoor access restrictions and indoor tan-
ning use.
196
Power limitations may have contributed to the lack
of a significant association between state minors' access
laws and prevalence of indoor tanning use. It is also likely
that inadequate compliance and poor enforcement mech-
anisms reduce the effectiveness of such legislation.
1
12
-
14
For example, Forster er al
14
studied 2 srates (Minnesota
and Massachusetts) with established policies requiring pa-
rental written permission before rhe usage of indoor tan-
ning devices by an underage minor (aged < 16 years) and
found that 81 o/o of indoor tanning businesses sold a ses-
sion to an underaged minor on ar leasr 1 of 2 anempts,
and that the adolescents' age was not assessed in 40% of
attempts.
In keeping with other reports?'
21
we noted that
youths' report of parental permission to use indoor tan-
ning was strongly correlated with higher indoor tanning
used among adolescents. Thus, in stares that allow indoor
tanning use wirh parental consent or accompaniment,
greater efforts to inform parents about the hazards of
indoor tanning and/or more restrictive legislation may be
required to reduce adolescents' exposure to indoor
Cancer January 1, 2009
tanning.
22
Health professionals and the medical commu-
nity could play a greater role in educating parents about
the short-term and long-term skin cancer risks associated
with the use of indoor tanning and the role they can play
in assuring that their children do not use indoor tanning
establishments.
23
24
The approach of adopting more re-
strictive legislation (based on minors' age) is supported by
the World Health Organization and the International
Commission on Non-Ionizing Radiation Protection.
Both organizations recommend that use of these devices
nor be allowed by those aged < 18 years.
2
8
Of particular concern with respect to the prevention of
health effects related to indoor tanning exposure, no measura-
ble decreases in indoor tanning were observed among the sub-
groups of adolescents who typically exhibit a higher
prevalence of indoor tanning use, sud1 as older youths, girls,
those with medium skin sun sensitivity, those with high levels
of positive tanning attitudes, d10se who are less consistent
users of sunscreen, and those whose parent also used indoor
tanning. As expected, many of these previously associated fac-
tors were confirmed as strong independent predictors of
indoor tanning use in youths, and d1ese findings are consist-
em with previous findings.
4
25
It is concerning that older ad-
olescent girls continue to demonstrate higher use of indoor
tanning. In the US, most adolescents are aware of the deleteri-
ous effects ofUVR,
15
yet many continue this unsafe practice.
One principal factor driving tanning behavior is the sociocul-
tural belief that equates tanned skin with healthiness and
attracriveness.L
3
.4 In addition, the lack of improvements in
indoor tanning among teenage girls may be related to envi-
ronmental factors; there is evidence to suggest that tanning
facilities are more concentrated in geographic areas with
higher proportions of teenagers and females ages 15 to 24
years
26
Because of the ongoing growth and popularity of the
indoor tanning industry,
1
these findings w1derscore the need
for significant education at both the individual and commu-
nity level to change social norms pertaining to having a tan
and to educate community members regarding the serious
risks of indoor tanning.
1
2
Previous studies have also reported that indoor tan-
ning causes burns (erythema) in 18% to 55% of users.
27
-
29 Consistent with these findings, we found that 57.5% of
adolescent users of indoor tanning reported getting red or
burned from using these devices. The strongest factor
associated with eiythema from indoor tanning after con-
trolling for possible confounders (sex, age, and skin sun
Cancer J anuary 1. 2009
Indoor Tanning by US Ad olescents I Cokkinides et al
sensitivity) was higher frequency of use (2:6 times). This
apparent relation between burns from these devices and
higher-frequency use may be the result of inconsistent
usage of appropriate safety measures (ie, time-limited ses-
sions) to reduce risks.
30
Half of adolescent indoor tanners
in the US used indoor tanning 2:6 times during the past
year. It is important to bear in mind that a burn from UV
equipment likely increases the risk for skin cancers as is
the case for sunburns from excessive sunlight exposure,
especially at younger ages.
31
Such high levels of erythema
associated with indoor tanning may ultimately result in an
increasing burden of melanoma
2
and keratinocyte carci-
. 'ddl
32
noma 1n mt . e age.
Conclusions
In conclusion, the prevalence of indoor tanning use in
youths did not markedly change between 1998 and 2004,
despite increasing numbers of states with legislation
restricting youth access to indoor tanning. This suggests
the need to develop multipronged approaches that could
enhance changes in this behavior among underage
minors. Given the known health risks associated with this
. I 2.8 . c d . d I
pracuce, ' strategtes ror re uctng a o escent exposure to
indoor tanning include more stringent legislative mea-
sures, such as prohibiting the use of indoor tanning facili-
ties by those aged < 18 years, along with appropriate
enforcement mechanisms, as well as efforts to educate
adolescents and their parents regarding the hazards of
indoor tanning. It is important ro continue to monitor
the prevalence of indoor tanning use among adolescents
and to evaluate strategies for reducing such exposure.
Conflict of Interest Disclosures
The American Cancer Society sponsored data collection for both
surveys. Funding supporr for data collection of the second survey
was provided by the American Cancer Society and Neurrogena,
Inc. Ocher than financial supporr, rhe latter organization had no
involvemem in the analysis and imerpretation of the data, or in
rhe preparation, review, or approval of the article.
References
1. Levine JA, Sorace M, Spencer J, Siegel DM. The indoor
UV tanning industry: a review of skin cancer risk, health
benefit claims, and regulation. I Am Acad Dermatol.
2005;53: 1038-1044.
197
Original Article
2. International Agency for Research on Cancer Working
Group on Anificial Ultraviolet (UV) Light and Skin Can-
cer. The association of use of s1mbeds with cur.aneous ma-
lignant melanoma and other skin cancers: a systematic
review. lnt J Cancer. 2007;120: 11 16-1122.
3. Lawvich D, Forster J. Indoor tanning by adolescents:
prevalence, practices and policies. Eur J Cancer. 2005;41:
20-27.
4. Cokkinides VE, WeinstOck MA, O' Connell MC, Thun
MJ. Use of indoor tanning sunlamps by US youth, ages
11- 18 years, and by their parent or guardian caregivers:
prevalence and correlates. Pediatrics. 2002; I 09: 1124- I 130.
5. Demko CA, Borawski EA, Debanne SM, Cooper KD,
Stange KC. Use of indoor tanning facilities by white ado-
lescents in the United States. Arch Peditltr Adolesc Med.
2003; 157:854-860.
6. Geller AC, Coldirz G, Oliveria S, et al. Use of sunscreen,
sunburning rates, and tanning bed use among more than
10 000 US children and adolescents. Pediatrics.
2002; 109:1009-1014.
7. Stryker JE, Lazovich D, Forster JL, Emmons KM, Sorensen
G, Demierre MF. Maternal/female caregiver influences on
adolescent indoor tanning. j Ado/esc Hetdth. 2004;35:
528.e1-e9.
8. Sinclair C. Artificial tanning sunbeds: risk and guidance.
Geneva: World Health Organization; 2003. Available at:
www.who.int/uv/imersunprogramme/activities/uvartsunbeds/
en/index.hnnl Accessed April 29, 2008.
9. Hester EJ, Heilig LF, D'Ambrosia R, Drake AL, Schilling
LM, Dellavalle RP. Compliance with youth access regula-
tions for indoor UV tanning. Arch Dmnatol. 2005; 14 1:
959-962.
10. McLaughlin JA, Francis SO, Burkhardt DL, De.llavalle RP.
Indoor UV tanning youth access laws: update 2007. Arch
Derma to!. 2007; 143:529-532.
11. Dellavalle RP, Parker ER, Cersonsky N, et al. Youth access
laws: in d1e dark at d1e tanning parlor? Arch Dermatol.
2003; 139:443-448.
12. Culley CA, Mayer JA, Eckhardt L, et al. Compliance with
federal and state legislation by indoor tanning facilities in
San Diego. JAm Acad Dermatol. 200 I ;44:53-60.
13. Fleischer AB Jr, Lee WJ, Adams DP, Zanoll i MD. Tanning
facility compliance with state and federal regulations in
North Carolina: a poor performance. J Am Acad Dermacol.
1993;28(2 pt 1):212-217.
14. Forster JL, Lazovich D, Hickle A, Sorensen G, Demierre
MF. Compliance with restrictions on sale of indoor tanning
sessions to youd1 in Minnesota and Massachusetts. j Am
Acad Dermatol. 2006;55:962-967.
15. Cokkinides V, Weinstock M, Glanz K, Albano J, WardE,
Thun M. Trends in sunburns, sun protection practices, and
arcirudes toward sun exposure protection and tanning
among US adolescents, 1998-2004. Pediatrics. 2006; 118:
853-864.
198
16. Weinstock MA. Assessment of sun sensitivity by question-
naire: validity of items and formulation of a prediction
rule. J Clin Epidemiol. 1992;45:547-552.
17. Hoerster KD, Mayer JA, Woodruff Sl, Malcarne V, Roesch
SC, Clapp E. The influence of parents and peers on adoles-
cent indoor tanning behavior: findings from a multi-city
sample. JAm Acad Dermatol. 2007;57:900-907.
18. Francis SO, Burkhardt DL, Dellavalle RP. 2005: A banner
year for new US youth access tanning restrictions. Arch
Dermatol. 2005; 141 :524-525.
19. SAS Institute Inc. SAS/STAT User's Guide, version 9.1.
Cary, NC: SAS Institute Inc; 2000.
20. SUDAAN User's Manual, release 9.0. Research Triangle
Park, NC: Research Triangle Institute; 2006.
2l. Woodruff Sl, Pichon LC, Hoerster KD, Forster JL, Gilmer
T, Mayer JA. Measuring the stringency of states' indoor
tanning regulations: instrument development and outcomes.
jAm Acad Dermatol. 2007;56:774-780.
22. Balk SJ, Geller AC. Teenagers and artificial tanning. Pedia-
trics. 2008; 121: 1 040-1042.
23. Abdulla FR, Feldman SR, Williford PM, Krowchuk D,
Kaur M. Tanning and skin cancer. Pediatr Dermatol.
2005;22:501-512.
24. Johnson KR, Heilig LF, Hester EJ, Francis SO, Deakyne
SJ, Dellaval le RP. Indoor tanning attitudes and practices of
US dermatOlogists compared with ocher medical specialises.
Arch Derma to!. 2006; 142:465-470.
25. Lazovich D, Forster J, Sorensen G, et al. Characteristics asso-
ciated with use or intention to use indoor tanning among
adolescents. Arch Pediatr Adolesc Med. 2004; 158:918-924.
26. Patel MR, MayerJ, Slymen DJ, WeeksJR, HurdAL. Correlates
of tanning facility prevalence within San Diego County, Cali-
fornia Census T races.} Community Health. 2007;32:391-400.
27. Boldeman C, Beitner H, Jansson B, Nilsson B, Ullen H.
Sunbed use in relation to phenotype, erythema, sunscreen
use and skin diseases. A questionnaire survey among Swed-
ish adolescentS. Br} Dermatol. 1996; 135:7 12-716.
28. Rhainds M, De Guire L, Claveau J. A population-based sur-
vey on the use of artificial tanning devices in the Province of
Quebec, Canada.} Am A cad Dermatol. 1999;40:572-576.
29. Boldeman C, Branstrom R, Dal H, et al . Tanning habits
and sunburn in a Swedish population age 13-50 years. Eur
J Cancer. 2001;37:2441-2448.
30. Heilig LF, D'Ambrosia R, Drake AL, Dellavalle RP, Hester
EJ. A case for informed consent? Indoor UV tanning facil-
ity operaror's provision of health risks information (United
States). Cancer Causes Corum!. 2005; 16:557-560.
3 1. Whiteman DC, Whiteman CA, Green AC. Chil dhood sun
exposure as a risk factOr for melanoma: a systematic review of
epidemiologic studies. Cancer Gtuses Control. 2001; 12:69-82.
32. Karagas MR, Stannard VA, Mott LA, Slattery MJ, Spencer
SK, Weinstock MA. Use of tanning devices and risk of ba-
sal cell and squamous cell skin cancers. J Natl Cancer lnst.
2002;94:224-226.
Cancer January 1, 2009
Youth Access to Artificial UV Radiation Exposure
Practices of 364 7 US Indoor Tanning Facilities
La trice C. Pichon, PhD, MPH; ]oni A. Mayer, PhD; Katherine D. Hoerster, MS; Susan I. Woodruff, PhD;
Donald]. Slymen, PhD; George E. Belch, PhD; Elizabeth]. Clapp, MPH; Ami L. Hurd, MPH;
jean L. Forster, PhD, MPH; Martin A. Weinstoch, MD, PI1D
Obiective: To assess indoor tanning facility practices in
a sample of facilities in 116 cities representing all 50 states.
5% said they would not allow the confederate to tan ow-
ing to her age, and 7l% would allow tanning every day
the first week of indoor tanning. In Wisconsin, which
bans indoor tanning among those younger than 16 years,
70% of facilities would not allow the confederate to tan.
Multivariate analyses indicated that facilities in states with
a youth access law were significantly more likely to re-
quire parental consent (P<.OOl) and parental accom-
paniment (P <.001) than those in states without a youth
access law. Law was not significantly related to allow-
able tanning frequency (P= .81).
Design: Cross-sectional study.
SeHing: United States.
Participants: Employees of 364 7 indoor tanning facili-
ties were contacted by telephone. Data collectors (ie, con-
federates) posed as prospective, fair-skinned, 15-year-
old female customers who had never tanned before.
Main Outcome Measures: Confederates asked re-
spondents about their facility's practices related to pa-
rental consent, parental accompaniment, and allowable
tanning session frequency.
Conclusion: We recommend that additional states
pass youth access legislation, preferably in the form of
bans.
Results: Approximately 87% of the facilities required pa-
rental consent, 14% required parental accompaniment, Arch Dermatol. 2009;145(9):997-1002
Author Affiliations: San Diego
State University/University o[
California, San Diego,joim
Doctoral Program in Public
Health, San Diego (Dr Pichon);
joint Doctoral Program in
Clinical Psychology
(Ms Hoerster), Graduate School
of Public Health (Drs Mayer
and Slymen and Mss Clapp and
Hurd), School of Social Work
(Dr Woodruff). Department of
Marketing (Dr Belch), and
School of Public Health
(Dr Forster), University of
Minnesota, Minneapolis;
Dermatoepidemiology Unit,
Veterans Affairs Medical Center,
and the Departments of
Dermatology and Community
Health, Brown University,
Providence, Rhode Island
(Dr Weinstock).
E
XPOSURE TO UV RADIATION
(UVR) from indoor tanning
lamps has been linked with
both melanoma and squa-
mous cell cancer, and first ex-
posure before age 35 years may increase
melanoma risk by as much as 75%.
1
In the
United States, indoor tanning is especially
See also pages 989,
1051, and 1059
popular among adolescent girls,
2
4
and this
may help explain the recently reported rise
in melanoma incidence among US young
adult women (ages 15-39 years).
5
As of
2005, 28 states had an indoor tanning law
regulating tanning facility practices, with 21
of these having some sort of youth access
restriction.
6
The US Food and Drug Admin-
istration (FDA) recommends, but does not
require or enforce, an exposure schedule not
exceeding a 0. 75 minimal erythemal dose
3 times during the first week of tanning.
7
Several recent studies
8
13
have character-
ized the practices of indoor tanning facili-
ties with emphasis on youth access and ex-
posure levels. However, to our knowledge,
no study has included facilities in a large
number of cities representing all geographic
regions. Thus, our goal for this study, which
was part of the Correlates of! ndoor Tanning
in Youth (CITYlOO) Project, was to assess
facility practices in a large sample of facili-
ties representing 116large cities in all 50 US
states. We focused on practices (when in-
teracting with a 15-year-old girl) related to
requirements for parental consent, paren-
tal accompaniment, forbidding her to tan at
all because of her age (ie, ban), and tanning
session frequency allowed.
METHODS
SELECTION OF CITIES
AND TANNING FACILITIES
Our sample consisted of indoor tanning facili-
ties in 116 US cities: the 100 most populous
cities, which represented 34 states and the Dis-
trict of Columbia, plus the most populous city
in each of the 16 remaining st.ates.
14
Because residents living within the formal
boundaries of an incorporated city likely travel
(REPRINTED) ARCH DERMATOUVOL 145 (NO. 9), SEP 2009
997
\VWVv. ARCHDERMATOL.COM
2009 American Medical Association. All rights r eserved.
beyond those boundaries, we defined the city boundary as a 3-miJe
buffer zone surroundi ng the formal boundary. Using a mul-
tistep process with Geographic Infonnation Systems data de-
scribed in detail elsewhere,
15
we created these boundaries and
identified indoor tanning facilities within them. Our inclusion
criteria fora facility were that it must offer indoor UVR tanning,
be open to the public, and not require membership. With the
tem1 "tanning salons" as the key word, in March 2006 we iden-
tified all facilities within each city using ReferenceUSA.com as
the primary source and Superpages.com as the secondary source.
Tf an indoor tanning facility was shared by more than 1 city plus
a 3-mile buffer area, we assigned the main city affiliation to the
city whose center was closest to the facility.
ASSESSMENT OF OUTCOMES
AND POTENTIAL CORRELATES
We hired and trai ned 5 young-sounding female college stu-
dents (ie, confederates) to pose as 15-year-old potential cli-
ents, telephone the facilities, and follow a script for ascertain-
ing facility practices. During the confederate interview process,
we evaluated whether applicants sounded like teens by using
blinded telephone screening, as well as Sona-Speech II voice
software (version 2.7.0; KayPENTAX, Lincoln Park, New Jer-
sey) to assess the fundamental voice frequency (ie, pitch). All
5 confederates' voice frequencies fell within the acceptable ranges
for a 15-year-old girl (179-310 Hz).
16
Confederates telephoned all potential ly eligible faci li ties in
June through September of 2006; respondents were tanning fa-
cility staff who answered this telephone call. Up to 10 at-
tempts were made to reach each tanning business. At the be-
ginning of each 5-minute telephone contact, the confederate
stated that she was planning to visit the facility that day and
described herself as being 15 years old, having fair skin, and
having never used indoor tanning. She then asked several
scripted questions to assess the practices and characteristics of
indoor tanning facili ties and recorded all responses verbatim
on a data collection fom1. In a previous study, we had found
that data coll ected in person vs by telephone. had acceptable
concordance. u The ke>' questions were: (l) "Does my mom need
to sign anything sol can tan?", (2) "Does my mom need to be
there while I tan?", and (3) "How many times can I tan the first
week7" . The practice of banni ng owing to the customer's age
was not asked about directly but was coded when the respon-
dent replied that the confederate could not tan owing to age
when asked question 1, and a separate variable for banning (yes/
no) was then created.
We measured potential correlates of practices, includ-
ing facility type, number of tanning beds, respondent sex,
whether the state had any tanning law, and whether the state
had any law restricting youth access. Facili ty type, coded dur-
ing the facility identification process, consisted of tanning sa-
lon (ie, sole or mai n service was indoor UV tanning), beauty
salon or day spa (ie, provided UV tanning as a service) , and
"other" (ie, provided UV tanning but did not fit into the first 2
categori es). Toward the end of the telephone call , the confed-
erate asked "How many tanning beds or booths do you have 7"
(recorded and used in analyses as a continuous variable). Once
data were collected, we recoded the various responses to con-
federa tes' queries using a priori protocols. For law data, we sys-
tematically reviewed 2 legal databases and analyzed the con-
tent of existing indoor tanning laws.
6
To assess interrater reliability, the confederates' supervi-
sors (L.C.P. and K.D.H.) listened to a random 20% of the calls
on a second telephone line and recorded the respondent's com-
ments. All study procedures were approved by the San Diego
State University institutional review board.
STATISTICAL ANALYSIS
Data were analyzed with SPSS (version 15.0 for Windows; SPSS
Inc, Chicago, Illinois) and SAS (version 9.1.3; SAS Inc, Ca1y,
Nort h Carolina) statistical software. Facility was the unit of
analysis. We examined the data using 2 perspectives: (l) prac-
tices of all facilities, irrespective of whether the state had an
indoor tanning law, and (2) compliance of facilities under the
jurisdiction of specific state laws (ie, a card").
Descriptive statistics were computed for each facility prac-
tice (ie, parental consent , parental accompaniment, tanning ban
for a 15-year-old, and frequency that an individual was allowed
to tan); number of UV indoor tanning beds or booths; type of
facility; and respondent sex. We tested the bivariate relation-
ship between each facility practice and each potential correlate
using generalized estimating equations (GEEs)
17
18
that ad-
justed for city clustering. Potential correlates were number of beds,
facility type, respondent sex, presence of any state indoor tan-
ning law, and presence of state youth access resu"iction law. Mul-
tivariate analyses using GEEs- 1 for each practice- were con-
ducted to test the relationship between each facility practice and
multiple potential predictors simultaneously, adjusting for city
clustering and confederate. The "any state law" variable was ex-
cluded, and "youth access law" was included as a predictor in
the multivariate models because the latter was more relevant (and
was nested within the former). Respondent sex also was ex-
cluded from multivariate tests because it was consistently unre-
lated to outcomes in the bivariate analyses. A significance level
of P =.05 was used for all analyses.
For the report card, we assessed the percentage of facilities
in (1) the 20 relevant states that. complied with their parental
consent laws, (2) the 2 relevant states that complied with their
parental accompaniment laws, and (3) the 1 relevant state that
complied with its ban for those younger than 16 years. Using
x
2
tests, we compared these percentages \vith the percentages
of facili ties in states without these specific regulations.
\Ve evaluated interrater agreement on select variables for a
subset of the data using the K value for the categorical vari-
ables and intraclass correlation coefficients (lCCs) for the con-
tinuous variables.
RESULTS
CHARACTERISTICS OF THE SAMPLE
A total of 4561 indoor tanning facilities were initially iden-
ti fi ed. For the curren t analysis, 79 facili ties were ex-
cl uded because the telephone number and business name
resembled other businesses and our research team did
not want to raise any suspicion when calling. An addi-
tional 835 facilities were excluded owing to discon-
nected telephone lines (n=408) , no answer after 10 call-
ing auempts (n= 104), an answering machine picked up
(n= 27), the facility no longer provided UV tanning
(n = 180), the telephone number was wrong (n =67) , and
o ther reasons, including hang-up, the facility was out of
business, and the number used turned out to be a fax num-
ber ( n = 40). This resulted in 364 7 facili ties with usable
data.
Approximately 80% of the tanning facili ties were tan-
ning salons ( n = 2895), 17% were beauty salons or day
spas ( n =616) , and 3% were "other" (n = 106); in analy-
ses, the latter 2 categories were combined. Thirty of the
facilities had missing data for facility type. The mean (SO)
number of tanning beds was 9.94 (6.81) ( range, 1-50 tan-
(REPRINTED) ARCH DERMATOUVOL 145 ( NO. 9), SEP 2009
998
\VWVv. ARCHDERMATOL.COM
2009 American Medical Association . All rights r eserved.
Table 1. Facility Practices Regarding Parental Consent, Parental Accompaniment, Tanning Ban, and Tanning Session Frequency
Practice
Required parental consent
Yes
No
Required parental accompaniment
Yes
No
Would not allow confederate to tan, owing to age (15 y)e
Yes
No
Allowed only 3 or fewer sessions first week9
Yes
No
Abbreviation: NA, not applicable.
All Facilities a
3008 (86.9)
455(13.1)
495 (14.3)
2967 (85.7)
182 (5.0)
3463 (95.0)
320 (10.8)
2642 (89.2)
No.(%)
Facil ities in States
With This
Legislative Requirement
n=20 Statesb
1966 (92.8)
152 (7.2)
n=2 Statesd
203 (43.4)
265 (56.6)
n= 1 State
1
56 (70.0)
24 (30.0)
NAh
Facilities in States
Without This
Legislative Requirement
n=30 States
1042 (77.5)
303 (22.5)
n=48 States
292 (9.8)
2702 (90.2)
n=49 States
126 (3.5)
3439 (96.5)
NAh
xi
169.86C
373.41 c
728.65c
a Missing data were 184 for parental consent. 185 for parental accompaniment, 2 tor confederate not allowed to tan, and 685 tor session frequency. Session
frequency missing data primarily were missing due to respondent saying they needed to see confederate's skin and skip pattern (when they told confederate she
could not tan owing to age).
b Arizona, California, Florida. Georgia, Illinois, Indiana, Louisiana, Maine. Massachusetts, Michigan, Minnesota, Mississippi, New Hampshire, North Carolina,
Ohio, Oregon, Rhode Island, South Carolina, Tennessee, Texas.
cp< .001.
d Indiana and Texas.
erhe confederate did not ask this directly; respondent stated this when being asked about parental consent.
1
Wisconsin.
g Recommended by US Food and Drug Administration.
h None of the state laws explicitly regulated tanning session frequency.
ning beds). The facility respondents were primarily fe-
male (84.3%).
INTERRA TER RELIABILITY
The K values [or parental consent and parental accom-
paniment were 0.98 and 0.95, respectively. The ICCs for
number of sessions allowed and number of tanning beds
were 0.99 and 0.97, respectively.
F ACIUTY PRACTICES
As shown in Table 1, approximately 87% of facilities
required our confederates to get parental consent, about
14% required parental accompaniment, and 5% did not
allow tanning at all owing to the confederates' stated age.
Only around ll% followed the FDA recommendations
of3 or fewer sessions the first week. The mean (SD) num-
ber of sessions allowed the first week was 6.02 (1.61).
About 71% of respondents said they would allow a teen
to tan 7 days a week.
In bivariate analyses (Table 2 ) , there were no sig-
nificant associations between the respondent's sex and
any of the outcome variables. State law and youth ac-
cess law each were significantly related to parental con-
sent and parental accompaniment, with facilities in states
with a law more likely to require these than facilities in
states without such a law. Neither type of law was asso-
ciated with the 2 other practices. The number of tan-
ning beds was significantly associated with each out-
come variable, with the exception of tanning ban. More
specifically, facilities with more beds were significantly
more likely to require parental consent and parental ac-
companiment, and significantly less likely to follow the
FDA tanning session frequency recommendations. Tan-
ning facility type was significantly related only to tan-
ning session frequency allowed, with tanning salons less
likely to follow FDA frequency recommendations than
other facility types. (See Table 2 for P values.)
Multivariate analysis results indicated that for paren-
tal consent, youth access law, and number of beds were
significant predictors (see Table 3 for odds ratios, 95%
confidence intervals, and significance levels). Facilities in
states without a youth access law had only around one-
third the odds of requiring consent than facilities in states
with a law. For each 5-bed increase, facilities were 14%
more likely to require parental consent. For parental ac-
companiment, the following variables were significant pre-
dictors: facility type, youth access law, and number of beds.
Nonsalons were 53% more likely to require parental ac-
companiment than salons. Facilities in states without a
youth access law were 58% less likely to require accom-
paniment than facilities in states with a law. Facilities were
19% more likely to require parental accompaniment with
each 5-bed increase. For frequency that an individual was
allowed to tan, number of beds was the only significant
predictor; facilities were 29% less likely to follow the FDA
frequency recommendations for each 5-bed increase. Simi-
lar to the bivariate results, none of the variables tested sig-
nificantly predicted age-related banning.
COMPLIANCE OF SELECT FACILITIES
WITH SPECIFIC LAW CONTENT
We also assessed compliance of select facilities with their
specific state laws. Table l shows comparisons between fa-
(REPRINTED) ARCH DERMATOUVOL 145 (NO. 9), SEP 2009
999
\V'WVoJ. ARCHDERMATOL.COM
2009 American Medical Association. All rights r eserved.
Table 2. Bivariate Associations Between Facility Practices and Predictors, Adjusted for City Clustering
Using Generalized Estimating Equations
Required Requi red Confederate Not Allowed Allowed Only 3
Parental Consent Parental Accompaniment to Tan Owing to Age, 15 y or Fewer Sessions
(n=3463) (n=3462) (n=3645) (n=2962)
Predictors %Complying
xt
%Complying
xf
%Complying
xt
%Complying
x!
Facility type 3.65 3.17 0.03 20.07
3
Tanning salons 87.8 14.2 4.9 9.7
Other 843 15.0 5 7 15 4
Respondent's sex 0.16 0.09 0.61 0.16
Female 86.9 14.1 5.1 10.6
Male 86.8 15.4 4.4 11.8
Any state law 14.44
3
8.88b 085 0.11
Yes 88.8 15.8 5.3 11.1
No 79.7 8.9 3.9 9.7
Youth access law 38.94
3
16.97
3
0.61 0.72
Yes 92.3 17.3 5.6 9.7
No 78.0 9.4 4.1 12.5
No. of tanning beds 12.60
3
10.69b 0.40 32.83
3
3
P< .001 .
b p < .01.
Table 3. Multivariate Analyses Between Facility Practices and Predictors, Adjusted for City Clustering
Using Generalized Estimating Equationsa
Parental
Predictors Consent
Facility type
Tanning salons 1 [Reference]
Other 0.91 (0.67-1.22)
Youth access law
Yes 1 [Reference]
No 0 35 (0.25-0.49)b
No. of tanning beds: per 5-bed increase 1.1 4 (1.05-1.24)C
Abbreviations: Cl, confi dence interval; OR, odds ratio.
a All models are adjusted for confederate.
bp < .001.
cp < .01.
cilities in states with vs those without specific laws on prac-
tices related to parental consent, parental accompani-
ment, and banning underage youth. As indicated, although
compliance varied across the 3 practices, facilities in states
with a specific law were significantly more likely to imple-
ment the practice compared with facilities in states with-
out the specific law (P< .001) . Of the 20 parental consem
law states, facilities in 4 states (Louisiana, Maine, New
Hampshire, South Carolina) had perfect compliance, and
facilities in Georgia had the lowest level of compliance
(72.5%) . Using data we had collected previously on in-
spections conducted in states with tanning laws,
19
we found
that facilities in parental-consent states with annual (or more
frequent) inspections were significantly more likely tore-
quire parental consent than those in parental-consent states
with less-than-annual inspections (95% vs 91 %; x1= 12.19;
P< .001). Rates of requiri ng parental accompaniment in
Indiana and Texas were 45.3% and 42.8%, respectively. Wis-
con.o;in was the only state with a ban on tanning for indi-
viduals younger than 16 years.
OR (95%CI)
Parental Tanning Tanning
Accompaniment Ban Frequency
1 l Reference] 1 [Reference J 1 [Reference]
1.53 (1.20-1.95)b 0.95 (0.65-1.39) 1.27 (0.95-1.70)
1 [Reference] 1 (Reference] 1 (Reference]
0.42 (0.28-0.63)b 0.85 (0.36-2.01) 1.05 (0.71-1.54)
1.19 (1.1 1-1.27)b 0.98 (0.801.11) 0. 71 (0.630.81 )b
- - - - - ~ - 1 1 1 ' - ------
To our knowledge, this study is the largest study to date as-
sessing indoor tanning facility practices regarding youth ac-
cess. Our data on the proportion of facilities requiring pa-
rental consent-approximately 87% of all facilities-were
encouraging. Two previous studies
11
20
also found relatively
high rates of facilities requiri ng parental consent. In both
of those studies, as in ours, the confederates' ages were ex-
plicitly provided at the beginning of the interaction. In con-
trast, studies
9
10
using face-to-face methods have found more
lenient parental consent practices. The different patterns
in findings between these telephone vs in-person data col-
lection methods may be due to facilities' tendency to be stricter
during the telephone call (when a "sale" is more abstract) .
Results from our multivariate analysis suggested that
being in a state with any type of youtl1 access law made
it s ignificantly more likely that a facility would require
written consent (P<.OOl ). Also, the more tanning beds
(REPRINTED) ARCH DERMATOUVOL 145 (NO. 9), SEP 2009
1000
\VW\1-J. ARCHDERMATOL.COM
2009 American Medical Association. All rights r eserved.
a facility had, the more likely the facility was to require
consent. This latter finding may be due to the associa-
tion between facility type and number of beds, with sole-
purpose tanning salons having more beds than other types
of facilities. It is these salons that are most likely to be
part of a well-organized tanning industry network, in
which facility owners are encouraged to comply, at least
on the surface, with existing laws.
10
21
Although banning a 15-year-old prospective cus-
tomer was infrequent among all facilities in our sample,
the Wisconsin facilities had a moderately high rate of com-
pliance with this aspect of their law. Our rate of 70% for
banning a 15-year-old in Wisconsin was comparable with
the 77% rate in Wisconsin found by Hester et al .
11
More-
over, Hester et alu reported that for a prospective 12-
year-old client, 89% of Wisconsin facilities claimed they
would implement a ban. Banning by facilities was sub-
stantially less conunon than requiring parental consent.
Unlike a parental consent policy, which still provides the
possibility of a sale as long as the parent agrees,
22
impos-
ing an absolute ban on adolescents, who may constitute
a considerable proportion of a facility's profits, would be
"bad for business."
Compliance with FDA-recommended session-per-
first-week frequency was less than 11% in the present
study, with 71% of facility staff allowing the confeder-
ate to tan every day, and these findings are similar tore-
sults from several previous studies.
8
12
13
.2 These data high-
light the deficiencies in having recommendations vs
enforceabl e requirements. Not only do facilities allow fre-
quent tanning, but they promote it using "unlimited tan-
ning" discount price packages; these packages are ubiq-
uitous in the US tanning industry.U Unfortunately,
frequent use of indoor tanning is likely to increase the
risk for melanoma of individual customers by promot-
ing greater cumulative UVR exposure.
23
24
Our study had several methodological limitations. First,
we were not able to send confederates in person to assess
practices. However, when we attempted to validate our tele-
phone method against in-person visits in a pilot study, con-
cordance was acceptable.
12
A second limitation is that our
confederates were older than 15 years, and even though their
voices were relatively high-pitched and youthful sounding,
they may have produced different reactions from facility staff
than actual teens. Third, we conducted only l contact, with
only l respondent, per facility. Therefore, it is possible that
our data may not represent the '' typical" practices of all per-
sonnel at a given facility. Fourth, our results may not gen-
eralize to facilities in smaller cities or rural areas. Fifth, there
may be potential confounders (that we neglected to mea-
sure) of the associations we found in the analyses. Finally,
the cross-sectional design precludes making definitive con-
clusions about causal relationships between correlates and
the facilities' practices. Methodological strengths of our study
included a wide geographic area and large numbers of cit-
ies and facilities, assessment of several key practices that
could influence exposure to artificial UVR by youth, inclu-
sion of current legislative data as a potential correlate, and
highly reliable data.
These data have important implications related to the
safety of adolescent indoor tanners. Most facility person-
nel stated that a teen could tan every day the first week.
This finding highlights the high level of UV exposure teens
may be getting from indoor tanning. Nonregulated in-
door tanning frequency schedules potentially could re-
sult in overexposure and burning. Therefore, regulation
and enforcement of tanning schedules are warranted.
Are youth access laws, in general, and parental in-
volvement laws, in particular, effective? Should more states
pass these types of legislation? Our data indicated that
having any youth access law was associated with signifi-
cantly higher rates of requiring parental consent and pa-
rental accompaniment, and facilities in states with laws
specific to these practices had considerably higher rates
than facilities in states without comparable law content.
Thus, at one level, if one defines success as facility com-
pliance, our data could mean that the laws are having an
impact. However, given the relatively high rates of in-
door tanning by adolescent girls, as well as the poten-
tially important gatekeeping function of parents,
22
25
ap-
parently many parents are allowing their teens to tan and
are providing written consent or accompaniment.
Therefore, we encourage more states to adopt indoor
tanning bans for minors. In fact, the World Health Or-
ganization has recommended banning those younger than
18 years from commercial indoor tanning.
26
To date, 3
Australian states and France have banned those younger
than 18 years.
27
.
32
In the United States, as of]une 2008,
a law pending in Ohio would ban those younger than 18
yearsn Bans such as these may both reduce youth ac-
cess in a direct way and more forcefully educate parents
about the real dangers of indoor tanning.
Accepted for Publication: October 28, 2008.
Correspondence: joni A. Mayer, PhD, Graduate School
of Public Health, 9245 Sky Park Ct, Ste 220, San Diego,
CA 92123 (jmayer@mail.sdsu.edu).
Author Contributions: Dr Mayer had full access to all
of the data in the study and takes responsibility for the
integrity of the data and the accuracy of the data analy-
sis. Study concept and design: Mayer, Woodruff, Slymen,
Belch, Forster, and Weinstock. Acquisition of data: Pi-
chon, Hoerster, Woodruff, Clapp, and Hurd. Analysis and
interpretation of data: Pichon, Mayer, Hoerster, and Sly-
men. Drafting of the manuscript: Pichon and Mayer. Criti-
cal revision of the manuscript.for important intellectual con-
tent: Pichon, Mayer, Hoerster, Woodruff, Slymen, Belch,
Clapp, Hurd, Forster, and Weinstock. Statistical analy-
sis: Slymen. Obtained funding: Mayer. Administrative,
technical, and material support: Pichon, Mayer, Hoer-
ster, Woodruff, Slymen, Belch, Clapp, Hurd, Forster, and
Weinstock. Study supervision: Pichon, Mayer, Hoerster,
and Clapp.
Financial Disclosure: None reported.
Funding/Support: This study was supported by the Na-
tional Cancer institute, grant numbers ROl CA093532,
R01 CA093532S1, and K05 CA10005l. Dr Pichon was
supported by NCI grant No. 5 ROl CA093532Sl (mi-
nority supplement) ; Dr Mayer, by NCI grant numbers
5 ROl CA093532 and K05 CA10005l.
Role of the Sponsors: The sponsors had no role in the
design and conduct of the study; in the collection, analy-
sis, and interpretation of data; or in the preparation, re-
view, or approval of the manuscript.
(REPRINTED) ARCH DERMATOUVOL 145 (NO. 9), SEP 2009
1001
\VWVv. ARCHDERMATOL.COM
2009 American Medical Association. All rights r eserved.
Additional Contributions: Our 5 confederates were Lau-
rel Butcher, BA, Ashley Bickmore, MPH, Muriel Eclavea,
BA, Erin Greene, BA, and jennifer Nicol, MPH. James
Sallis, PhD, john Weeks, PhD, and Todd Gilmer, PhD,
helped design the study. Debra Rubio, BA, assisLed wilh
manuscript preparation.
1. The International Agency for Research on Cancer Working Group on Artificial
Ultraviolet Light and Skin Cancer. The association of use ot sunbeds with cuta
neous malignant melanoma and other skin cancers: a systematic review. lnt J
Cancer. 2007;120(5):11161 122.
2. Cokkinides VE, Weinstock MA, O'Connell MC, Thun MJ. Use of indoor tanning
sunlamps by US youth, ages 11-18 years, and by their parent or guardian care
givers: prevalence and correlates. Pediatrics. 2002;1 09(6):11241130.
3. Demko CA, Borawski EA, Debanne SM. Cooper KD, Stange KC. Use of indoor
tanning facilities by white adolescents in the United States. Arch Pediatr Ado
lese Med. 2003;157(9):854860.
4. Geller AC, Colditz G, Oliveria S, et al. Use of sunscreen, sunburning rates, and
tanning bed use among more than 10 000 US children and adolescents. Pediatrics.
2002; 109(6):10091014.
5. Purdue MP, Freeman LE, Anderson WF, Tucker MA. Recent trends in incidence
of cutaneous melanoma among US Caucasian young adults (published online
July 10. 2008). J Invest Oermatol. 2008;128(12):29052908. doi:1 0.1038/jid
.2008159
6. Woodruff Sl, Pichon LC, Hoerster KD, Forster JL, Gilmer T, Mayer JA. Measur
ing the stringency of states' indoor tanning regulations: instrument develop-
ment and outcomes. JAm Acad Oermatof. 2007;56(5):774780.
7. Department of Health and Human Services Food and Drug Administration. Qual
ity Control Guide for Sunlamp Products. Rockville. MD: Public Health Service:
1988. DHHS Publication No. (FDA) 8888234.
8. Culley CA, Mayer JA, Eckhardt L, et at. Compliance with federal and state legis
lation by indoor tanning facilities in San Diego. JAm Acad Dermatol. 2001;
44(1):5360.
9. Dobbinson S, Wakefield M, Sam bell N. Access to commercial indoor tanning fa
cilities by adults with highly sensitive skin and by under-age youth: compliance
tests at solarium centres in Melbourne, Australia. Eur J Cancer Prev. 2006;
15(5):424430.
10. Forster JL, Lazovich D, Hickle A, Sorensen G, Demierre MF. Compliance with
restrictions on sale of indoor tanning sessions to youth in Minnesota and
Massachusetts. JAm Acad Dermatol. 2006;55(6):962967.
11. Hester EJ, Heilig LF, D'Ambrosia R, Drake Al, Schilling LM, Dellavalle RP. Com
pliance with youth access regulations for indoor UV tanning. Arch Derma/of. 2005;
141(8):959962.
12. Hurd AL, Mayer JA, Woodruff Sl, Belch GE, Patel MR. Comparing two methods
of measuring legislation compliance among indoor tanning facilities. JAm Acad
Derma/of. 2006;54(3):433439.
13. Kwon HT. Mayer JA, Walker KK, YuH, Lewis EC, Belch GE. Promotion of tre
quent tanning sessions by indoor tanning facili ties: two studies. JAm Acad
Derma/of. 2002;46(5):700-705.
14. Census 2000 PHCT-5. Ranking tables tor incorporated places of 100.000or more:
1990 and 2000 Table 2: incorporated places of 100,000 or more, ranked by popu
lation: 2000. http://www.census.gov/population/www/cen2000/briefs/phct5
/tables/tab02.pdf. Accessed July 22, 2008.
15. Hoerster K. Garrow R, Mayer J, et al. Density of indoor tanning facilities in 11 6
large U.S. cities. Am J Prev Med. 2009;(3):243246.
16. lseli M, Shue YL, Alwan A. Age, sex. and vowel dependencies of acoustic mea
sures related to the voice source. J Acoust Soc Am. 2007;121(4):22832295.
17. Liang KY. Zeger SL. Longitudinal data analysis using generalized li near models.
Biometrika. 1986;73(1):1322.
18. Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous
outcomes. Biometrics. 1986;42(1):121-1 30.
19. Mayer JA, Hoerster KD, Pichon LC, Rubio DA, Woodruff Sl, Forster JL. Enforce
ment of state indoor tanning laws in the United States. Prev Chronic Dis. 2008;
5(4):A125.
20. Indoor tanning: unexpected dangers. Consum Rep. 2005;70(2):3033.
21. Bizzozero J. Looking Fit: Tanning Fact Book: A Guide for Today's Successful Sa
/on Owners 20062007. Phoenix, AI.: Virgo Publishing; 2006.
22. Hoerster KD, Mayer JA. Woodruff Sf, Malcarne V, Roesch SC, Clapp E. The in
fluence of parents and peers on adolescent indoor tanning behavior: findings from
a multi-city sample. JAm Acad Oermatof. 2007;57(6):990-997.
23. Autier P, Donl JF, Lejeune F, et al; EORTC Melanoma Cooperative Group. Cuta-
neous malignant melanoma and exposure to sunlamps or sunbeds: an EORTC
multicenter case-control study in Belgium, France and Germany. /nt J Cancer.
1994;58(6):809813.
24 Westerdahl J. Olsson H, ~ s b a c k A, et a!. Use of sunbeds or sunlamps and rna
lignant melanoma in southern Sweden. Am J Epidemiof. 1994;140(8):691
699.
25. Stryker JE, Lazovich D, Forster JL, et al. Maternal/female caregiver influences
on adolescent indoor tanning. J Ado/esc Health. 2004;35(528):e521529.
26. World Health Organization. Artificial tanning sunbeds risks and guidance: 1-14.
http://www.who.int/uv/publications/sunbedpubVen/. Accessed July 22, 2008.
27. Cesarini JP. The French regulations tor ultraviolet radiation sunbeds. Radial Pro-
tection Dosimetry. 2000;91 (13):205207.
28. Deere! no97617 du 30 mai 1997 relatif a Ia vente et a Ia mise a disposition du
public de certains appareils de bronzage utilisant des rayonnements ultravio-
lets, Article 4. http://www.legifrance.gouv. f r/affi ch Texte .do?cidTexte
=LEGITEXT000005623814&dateTexte=2008071 1. Accessed July 11 , 2008.
29. Dellavalle RP, Parker ER, Cersonsky N, et al. Youth access laws: in the dark at
the tanning parlor? Arch Dermatol. 2003:139(4):443448.
30. Government of South Australia Radiation Protection and Control (Cosmetic Tan
ning Units), Regulations 2008. http://legislation.sa.gov.au/LZIC/RIRADIATION
%20PROTECTI ON%20AND%20CONTROL%20(COSMETIC%20TANNING
o/o20UNITS)o/o20REGULA TIONS%202008.aspx. Accessed June 30, 2008.
31. Government of Western Australia Department of Health. Key Requirements of
the Australian Standard (AS/NZS 2635:2002) for Solaria Cosmetic Purposes. http:
//www. public.health. wa.gov .au/cproot/1487/2/Key _Requirements_of
_ASNZS26352002_Solaria_for_Cosmetic_Purposes.pdf. Accessed June 30, 2008.
32. Solaria Regulation: new regulations tor Victoria, January 4, 2008. State Govern
ment of Victoria Australia Department of Human Services Web site. http://www
.health.vic.gov.au/environment/radiation/solarium.htm. Accessed June 30, 2008.
33. 127th General Assembly Regular Session, 20072008: HB 230: a bill to amend
section 4713.08 and to enact section 4713.50 ofthe Revised Code regarding use
of tanning services by individuals under 18 years of age. State of Ohio legisla
l ure Web site. http://www.legislature.state.oh.uslbills.cfm?ID=127 _HB_230. Ac
cessed June 30, 2008.
(REPRINTED) ARCH DERMATOUVOL 145 (NO. 9), SEP 2009
1002
\VWVv. ARCHDERMATOL.COM
2009 American Medical Association. All rights r eserved.
This report is based on research conducted by the Tufts Evidence-based Practice Center (EPC)
under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD
(Contract No. HHSA 290-2007-10055-1). The findings and conclusions in this document are
those of the author(s), who are responsible for its content, and do not necessarily represent the
views of AHRQ. No statement in this report should be construed as an official position of AHRQ
or of the U.S. Department of Health and Human Services.
The information in this report is intended to help clinicians, employers, policymakers, and others
make informed decisions about the provision of health care services. This report is intended as a
reference and not as a substitute for clinical judgment.
This report may be used, in whole or in part, as the basis for the development of clinical practice
guidelines and other quality enhancement tools, or as a basis for reimbursement and coverage
policies. AHRQ or U.S. Department of Health and Human Services endorsement of such
derivative products may not be stated or implied.
Evidence Report/Technology Assessment
Number 183
Vitamin D and Calcium: A Systematic Review of
Health Outcomes
Prepared for:
Agency for 1-Iealthcare Research and Quality
U.S. Department of Health and Human Services
540 Gaither Road
Rockville, MD 20850
www.ahrg.gov
Contract No. HHSA 290-2007-10055-1
Task Order No. 4
Prepared by:
Tufts Evidence-based Practice Center, Boston, MA
Investigators:
Mei Chung, M.P.H.
Ethan M Balk, M.D., M.P.H.
Michael Brendel, B.A.
Stanley Ip, M.D.
Joseph Lau, M.D.
Jounghee Lee, Ph.D.
Alice Lichtenstein, D.Sc.
Kamal Patel, M.B.A., M.P.H.
Gowri Raman, M.D.
Athina Tatsioni, M.D., Ph.D.
Teruhiko Terasawa, M.D.
Thomas A Trikalinos, M.D., Ph.D.
AHRQ Publication No. 09-E015
August 2009
II
This document is in the public domain and may be used and reprinted without permission except
those copyrighted materials noted for which further reproduction is prohibited without the
specific permission of copyright holders.
Suggested Citation:
Chung M, Balk EM, Brendel M, Ip S, Lau J, Lee J, Lichtenstein A, Patel K, Raman G, Tatsioni
A, Terasawa T, Trikalinos TA. Vitamin D and Calcium: A Systematic Review of Health
Outcomes. Evidence Report No. 183. (Prepared by the Tufts Evidence-based Practice Center
under Contract No. HHSA 290-2007-10055-I.) AHRQ Publication No. 09-E015. Rockville, MD:
Agency for Healthcare Research and Quality. August, 2009.
No investigators have any affiliations or financial involvement (e.g.,
employment, consultancies, honoraria, stock options, expert testimony,
or patents received or or royalties) that conflict with
111
Preface
The Agency for Healthcare Research and Quality (AHRQ), through its Evidence-based
Practice Centers (EPCs), sponsors the development of evidence reports and technology
assessments to assist public- and private-sector organizations in their efforts to improve the
quality ofhealth care in the United States. The Office of Dietary Supplements/National Institutes
of Health, the Public Health Agency of Canada, Health Canada, and Food and Drug
Administration requested and provided funding for this report. The reports and assessments
provide organizations with comprehensive, science-based information on common, costly
medical conditions and new health care technologies. The EPCs systematically review the
relevant scientific literature on topics assigned to them by AHRQ and conduct additional
analyses when appropriate prior to developing their reports and assessments.
To bring the broadest range of experts into the development of evidence reports and health
technology assessments, AHRQ encourages the EPCs to fonn partnerships and enter into
collaborations with other medical and research organizations. The EPCs work with these partner
organizations to ensure that the evidence reports and technology assessments they produce will
become building blocks for health care quality improvement projects throughout the Nation. The
reports undergo peer review prior to their release.
AHRQ expects that the EPC evidence reports and technology assessments will inform
individual health plans, providers, and purchasers as well as the health care system as a whole by
providing important information to help improve health care quality.
We welcome comments on this evidence report. They may be sent by mail to the Task Order
Officer named below at: Agency for Healthcare Research and Quality, 540 Gaither Road,
Rockville, MD 20850, or by email to epc@ahrq.gov.
Carolyn M. Clancy, M.D.
Director
Agency for Healthcare Research and Quality
Beth A. Collins Sharp, R.N., Ph.D.
Director, EPC Program
Agency for Healthcare Research and Quality
Paul M. Coates, Ph.D.
Director, Office of Dietary Supplements
National Institutes ofHealth
IV
Jean Slutsky, P.A., M.S.P.H.
Director, Center for Outcomes and Evidence
Agency for Healthcare Research and Quality
Stephanie Chang, M.D., M.P.H.
EPC Program Task Order Officer
Agency for Healthcare Research and Quality
Elizabeth A. Y etley, Ph.D.
Senior Nutrition Research Scientist, Retired
Office ofDietary Supplements
National Institutes of Health
Mary Frances Picciano, Ph.D.
Senior Nutrition Research Scientist
Office of Dietary Supplements
National Institutes ofHealth
Margaret de Groh, Ph.D.
Manager, Risk Factors Unit
Centre for Chronic Disease Prevention and Control
Health Canada
Linda Greene-Finestone, Ph.D., R.D.
Nutrition Advisor
Centre for Chronic Disease Prevention and Control
Public Health Agency of Canada
v
Kimberly D. Elmslie, M.Sc.
Director General
Centre for Chronic Disease Prevention and
Control
Public Health Agency of Canada
Hasan Hutchinson, Ph.D., N.D.
Director General
Office ofNutrition Policy and Promotion
Public Health Agency of Canada
Paula R. Trumbo, Ph.D.
Supervisor, Nutrition Science Evaluation
Office ofNutrition, Labeling and Dietary
Supplements
Center for Food Safety and Applied
Nutrition
Food and Drug Administration
Acknowledgments
We would like to acknowledge with appreciation the following members of the Technical
Expert Panel for their advice and consultation to the Tufts Evidence-based Practice Center
during the preparation for this report:
Steven Abrams, M.D.
Professor of Pediatrics
Baylor College of Medicine
Section ofNeonatology
Texas Children's Hospital
Houston, Texas
Stephanie Atkinson, Ph.D.
Professor and Associate Chair
Department of Pediatrics
Biochemistry and Biomedical Sciences
Health Sciences
McMaster University
Hamilton, Canada
Patsy M. Brannon, Ph.D.
Professor
Division ofNutritional Sciences
Cornell University
Ithaca, New York
Rebecca D. Jackson, M.D.
Associate Professor
Department oflntemal Medicine
Division of Endocrinology, Diabetes, and
Metabolism
The Ohio State University
Columbus, Ohio
Vl
Glenville Jones, Ph.D.
Professor and Head
Department of Biochemistry
Queen's University
Ontario, Canada
Susan Taylor Mayne, Ph.D., F.A.C.E.
Professor
Division of Chronic Disease Epidemiology
Yale School of Public Health
New Haven, Connecticut
Clifford J. Rosen, M.D.
Senior Scientist
Maine Medical Center Research Institute
Scarborough, Maine
Structured Abstract
Background: Since the 1997 Dietary Reference Intake (DRI) values for vitamin D and calcium
were established new data have become available on their relationship, both individually and
combined, to a wide range of health outcomes. The Institute of Medicine/Food and Nutrition
Board has constituted a DRI committee to undertake a review of the evidence and potential
revision of the current DRI values for these nutrients. To support this review, several US and
Canadian federal government agencies commissioned a systematic review of the scientific
literature for use during the deliberations by the committee. The intent of providing a systematic
review to the committee is to support transparency of the literature review process and provide a
foundation for subsequent reviews of the nutrients.
Purpose: To systematically summarize the evidence on the relationship between vitamin D,
calcium, and a combination of both nutrients on a wide range of health outcomes as identified by
the IOM, AHRQ and technical expert panel convened to support the project.
Data sources: MEDLINE; Cochrane Central; Cochrane Database of Systematic Reviews; and
the Health Technology Assessments; search limited to English-language articles in humans.
Study selection: Primary interventional or observational studies that reported outcomes of
interest in human subjects in relation to vitamin D and/or calcium, as well as systematic reviews
that met the inclusion and exclusion criteria. Cross sectional and retrospective case-control
studies were excluded.
Data extraction: A standardized protocol with predefined criteria was used to extract details on
study design, interventions, outcomes, and study quality.
Data synthesis: We summarized 165 primary articles and 11 systematic reviews that
incorporated over 200 additional primary articles. Available evidence focused mainly on bone
health, cardiovascular diseases or cancer outcomes. For many outcomes, it was difficult to draw
firm conclusions on the basis of the available literature concerning the association of either
serum 25(0H)D concentration or calcium intake, or the combination of both nutrients. Findings
were inconsistent across studies for colorectal and prostate cancer, and pregnancy-related
outcomes including preeclampsia. There were few studies for pancreatic cancer and immune
function. Among trials of hypertensive adults, calcium supplementation lowered systolic, but not
diastolic, blood pressure by 2-4 mm Hg. For body weight, the trials were consistent in finding no
significant effect of increased calcium intake on weight. For growth rates, a meta-analysis did
not find a significant effect on weight or height gain attributable to calcium supplement in
children. For bone health, one systematic review found that vitamin D plus calcium
supplementation resulted in small increases in BMD of the spine and other areas in
postmenopausal women. For breast cancer, calcium intakes in premenopausal women were
associated with a decreased risk. For prostate cancer, some studies reported that high calcium
intakes were associated with an increased risk.
Limitations: Studies on vitamin D and calcium were not specifically targeted at life stages
(except for pregnant and postmenopausal women) specified for the determination ofDRI. There
vii
is large variation on the methodological quality of studies examined. Use of existing systematic
reviews limits analyses that could be performed on this source of infonnation.
Conclusions: The majority of the findings concerning vitamin D, calcium, or a combination of
both nutrients on the different health outcomes were inconsistent. Synthesizing a dose-response
relation between intake of either vitamin D, calcium, or both nutrients and health outcomes in
this heterogeneous body of literature prove challenging.
viii
Contents
Executive Summary
Evidence Report .......................................................................................................................... 15
Chapter 1. Introduction
Background
Sources, metabolism and functions of vitamin D
Sources, metabolism and functions of calcium
Challenges for the DRI committees
Key Questions addressed in this report
Chapter 2. Methods
Overview
Sponsoring Federal agencies
AHRQ Task Order Officer (TOO)
Technical Expert Panel (TEP)
EPC methodologists
Development of the analytic framework and refinement of key questions
Definitions
Vitamin D and calcium exposures
Clinical outcomes
Indicators of exposure (nutrient intake)
Surrogate outcomes
Intermediate outcomes
Life stages
Key questions
Literature search strategy
Study selection
Abstract screening
Full text article eligibility criteria
Primary studies
Systematic reviews
Other specific eligibility criteria
Data extraction
Data analysis
Meta-analysis
Grading of studies analyzed in this evidence report
Critical appraisal and grading of primary studies
Additional considerations of methodological quality of primary studies for the
purpose of DRI decision making
Critical appraisal of systematic reviews
Reporting of the evidence
Evidence tables
Summary tables
IX
Graphical presentation of dose-response relationship
Grand summary tables (evidence map)
Units of measurement
Assay method
Sunlight exposure
Primary and secondary outcomes
Study quality
Organization of the Results Section
Chapter 3. Results
Literature search results
Vitamin D and health outcomes
Vitamin D and growth
Vitamin D and cardiovascular disease
Vitamin D and body weight
Vitamin D and cancer
Cancer from all causes and total cancer mortality
Prostate cancer
Colorectal cancer
Colorectal adenoma
Breast cancer
Pancreatic cancer
Vitamin 0 and immunologic outcomes
Vitamin 0 and pregnancy-related outcomes
Preeclampsia
Other outcomes
Vitamin 0 and clinical outcomes ofbone health
Rickets
Fractures, falls, or performance measures
Vitamin D and all-cause mortality
Vitamin D and hypertension and blood pressure
Hypertension
Vitamin D and blood pressure
Vitamin D and bone mineral density or bone mineral content
Calcium and health outcomes
Calcium and growth
Calcium and cardiovascular disease
Calcium and body weight
Calcium and cancer
Cancer from all cause and total cancer mortality
Prostate cancer
Colorectal cancer
Colorectal adenoma
Breast cancer incidence
Breast Mammographic Density
Pancreatic cancer
X
Calcium and pregnancy-related outcomes
Preeclampsia
High blood pressure with or without proteinuria during pregnancy
Preterm birth
Small for gestational age infant
Calcium and all-cause mortality
Calcium and hypertension and blood pressure
Calcium and hypertension
Calcium and blood pressure
Combined vitamin D and calcium and health outcomes
Combined vitamin D calcium and growth
Combined vitamin D and calcium and cardiovascular disease
Combined vitamin D and calcium and body weight
Combined vitamin D and calcium and cancer
Cancer from all causes and total cancer mortality
Colorectal cancer
Colorectal adenoma
Breast cancer
Combined vitamin D and calcium and pregnancy-related outcomes
Preeclampsia
Other pregnancy-related outcomes
Combined vitamin D and calcium and clinical outcomes of bone health
Rickets, fractures, falls, or performance measures
Combined vitamin D and calcium and all-cause mortality
Combined vitamin D and calcium and hypertension and blood pressure
Combined vitamin D and calcium and hypertension
Combined vitamin D and calcium and blood pressure
Combined vitamin D and calcium and bone mineral density or bone mineral content
How does dietary intake of vitamin D from fortified foods and vitamin D
supplementation affect serum 25(0H)D concentrations (arrow 4)?
RCTs on dietary intakes of vitamin D from fortified foods and serwn 25(0H)D
concentrations
RCTs on vitamin D supplementation and serum 25(0H)D concentrations
Outcomes for Tolerable Upper Intake Levels
Renal outcomes
Adverse events reported in RCTs
Chapter 4. Discussion
Strengths of this report
DRI and the literature on vitamin D and calcium
Limitations of our methodological approach
Comments on the observational studies
Sources of heterogeneity and potential biases
Vitamin D intake and response in serum 25(0H)D concentration
Considerations for future DRI committees
XI
Abbreviations
Latitudes of selected cities
XII
Tables
Table 1. Number of primary studies on vitamin D intake or concentration and specific
health outcomes that could be applicable to certain life stages
Table 2. Number of primary studies on calcium intake and specific health outcomes that
could be applicable to certain life stages
Table 3. Number of primary studies on combined vitamin D and calcium intake and
specific health outcomes that are relevant to certain life stages
Table 4. Vitamin Don growth outcome: Characteristics ofinterventional studies
Table 5. Vitamin D and growth outcomes: Characteristics of cohort studies
Table 6. Vitamin D and growth outcomes: Results ofRCTs
Table 7. Vitamin D and growth outcomes: Results of cohort studies
Table 8. Vitamin D and cardiovascular outcomes: Characteristics ofRCTs
Table 9. Vitamin D and cardiovascular outcomes: Results ofRCTs
Table 10. Vitamin D and cardiovascular outcomes: Characteristics of cohort studies
Table 11. Vitamin D and cardiovascular outcomes: Results of cohort studies
Table 12. Vitamin D and weight: Characteristics ofRCTs
Table 13. Vitamin D and weight: Results of RCTs
Table 14. Vitamin D and total cancer: Characteristics ofRCTs
Table 15. Vitamin D and total cancer: Characteristics of cohort studies
Table 16. Vitamin D and total cancer: Results ofRCTs
Table 17. Vitamin D and total cancer: Results of cohort studies
Table 18. Vitamin D and prostate cancer: Characteristics of nested case-control studies
Table 19. Vitamin D and prostate cancer: Results of nested case-control studies
Table 20. Vitamin D and colorectal cancer: Characteristics ofRCTs
Table 21. Vitamin D and colorectal cancer: Results of RCTs
Table 22. Vitamin D and colorectal cancer: Characteristics of observational studiesA
Table 23. Vitamin D and colorectal cancer: Results of observational studies
Table 24. Vitamin D and colorectal adenoma: Characteristics of observational studies
Table 25. Vitamin D and colorectal adenoma: Results of observational studies
Table 26. Vitamin D and breast cancer: Characteristics of observational studies
Table 27. Vitamin D and breast cancer: Results of observational studies
Table 28. Vitamin D and pancreatic cancer: Characteristics of observational studies
Table 29. Vitamin D and pancreatic cancer: Results of observational studies
Table 30. Vitamin D (mother) and immunologic outcomes (offspring): Characteristics of
cohort studies
Table 31. Vitamin D (mother) and immunologic outcomes (offspring): Results of cohort
studies
Table 32. Vitamin D and preeclampsia: Characteristics of nested case-control studies
Table 33. Vitamin D and preeclampsia: Results of nested case-control studies
Table 34. Summary of systematic review of the effect of vitamin D on bone health
Table 35. Vitamin D and bone health: Characteristics of RCTs published after the Ottawa
EPC report
Table 36. Vitamin D and bone health: Results of RCTs published after the Ottawa EPC
report
Xlll
Table 37. Summary of systematic review on vitamin D supplementation and all-cause
mortality
Table 38. Vitamin D and all-cause mortality: Characteristics of cohort studies
Table 39. Vitamin D and all-cause mortality: Results of cohort studies
Table 40. Vitamin D and hypertension: Characteristics of cohort studies
Table 41. Vitamin D and hypertension: Results of cohort and nested case control studies
Table 42. Vitamin D and blood pressure: Characteristics ofRCTs
Table 43. Vitamin D and blood pressure: Results ofRCTs
Table 44. Vitamin D and bone mineral density: Characteristics ofRCTs published after
the Ottawa EPC report
Table 45. Vitamin D and bone mineral density or bone mineral contents: Results ofRCTs
published after the Ottawa EPC report
Table 46. Summary of systematic review of calcium on growth in children
Table 47. Calcium and growth: Characteristics of primary studies
Table 48. Calcium and growth: Results of primary studies
Table 49. Calcium and cardiovascular outcomes: Characteristi.cs of cohort studies
8
Table 50. Calcium and cardiovascular outcomes: Results of cohort studies
Table 51. Systematic reviews of calcium supplementation and weight
Table 52. Calcium and weight: Characteristics ofRCTs
Table 53. Calcium and weight: Results ofRCTs
Table 54. Calcium and total cancer mortality: Characteristics ofRCTs
Table 55. Calcium and total cancer incidence or mortality: Characteristics of cohort
studies
Table 56. Calcium and total cancer mortality: Results ofRCTs
Table 57. Calcium and total cancer incidence or mortality: Results of cohort studies
50-71, males
Table 58. Calcium and prostate cancer: Characteristics of observational studies
Table 59. Calcium and prostate cancer: Results of observational studies
Table 60. Systematic review of calcium supplementation and colorectal cancer incidence
or adenoma recurrence
Table 61. Calcium and colorectal cancer: Characteristics of observational studies
Table 62. Calcium and colorectal cancer: Results of cohort studies
Table 63. Calcium and colorectal cancer: Results of nested case-control studies
Table 64. Calcium and colorectal adenoma: Characteristics of interventional studies
Table 65. Calcium and colorectal adenoma: Characteristics of cohort studies
Table 66. Calcium and colorectal adenoma recurrence: Results ofRCTs
Table 67. Calcium and colo rectal adenoma recurrence: Results of nonrandomized
comparative study
Table 68. Calcium and colorectal adenoma: Results of cohort studies
Table 69. Calcium and breast cancer: Characteristics of cohort studies
Table 70. Calcium and breast cancer: Results of cohort studies
Table 71. Calcium and breast mammography density: Characteristics of cohort studies
Table 72. Calcium and breast cancer: Results of cohort studies
Table 73. Calcium and pancreatic cancer: Characteristics of cohort studies
Table 74. Calcium and pancreatic cancer: Results of cohort studies
XIV
Table 75. Summary table of systematic review on calcium supplementation and
preeclampsia, small for gestational age, preterm birth
Table 76. Calcium and preeclampsia and other pregnancy outcomes: Characteristics of
cohort studies
Table 77. Calcium and preeclampsia and other pregnancy outcomes: Results of cohort
studies
Table 78. Calcium intake and all-cause mortality: Characteristics of cohort studies
Table 79. Calcium intake and all-cause mortality: Results of cohort studies
Table 80. Calcium and hypertension incidence: Characteristics of cohort studies
Table 81. Calcium and hypertension incidence: Results of cohort studies
Table 82. Summary of systematic reviews of calcium and blood pressure
Table 83. Calcium and blood pressure: Characteristics ofRCTs
Table 84. Calcium and blood pressure: Results ofRCTs
Table 85. Combined vitamin D and calcium and cardiovascular outcomes:
Characteristics of RCTs
Table 86. Combined vitamin D and calcium and cardiovascular outcomes: Results of
RCTs
Table 87. Combined vitamin D and calcium and weight: Characteristics ofRCTs
Table 88. Combined vitamin D and calcium and weight: Results of RCTs
Table 89. Combined vitamin D and calcium and total cancer incidence: Characteristics of
RCTs
Table 90. Combined vitamin D and calcium and total cancer incidence: Results of RCTs
Table 91. Combined vitamin D with calcium and colorectal cancer: Characteristics of
RCTs
Table 92. Combined vitamin D with calcium and colorectal cancer: Results ofRCTs
Table 93. Combined vitamin D and calcium and breast cancer outcomes: Characteristics
ofRCTs
Table 94. Combined vitamin D and calcium and breast cancer outcomes: Results of
RCTs
Table 95. Combined vitamin D and calcium and preeclampsia: Characteristics ofRCTs
Table 96. Combined vitamin D and calcium and preeclampsia: Results ofRCTs
Table 97. Combined vitamin D and calcium and bone health: Characteristics ofRCTs
published after the Ottawa EPC report
Table 98. Combined vitamin D and calcium and bone health: Results of RCTs published
after the Ottawa EPC report (stress fracture)
Table 99. Combined vitamin D and calcium and bone health: Results ofRCTs published
after the Ottawa EPC report (performance measures)
Table 100. Combined vitamin D and calcium and incident hypertension: Characteristics
ofRCTs
Table 101. Combined vitamin D and calcium and incident hypertension: Results of
RCTs
Table 102. Combined vitamin D and calcium and blood pressure: Characteristics of
RCTs
Table 103. Combined vitamin D and calcium and blood pressure: Results ofRCTs
Table 104. Combined vitamin D and calcium and bone mineral density/content:
Characteristics of RCTs published after the Ottawa EPC report
XV
Table 105. Combined vitamin D and calcium and bone mineral density/content: Results
ofRCTs published after the Ottawa EPC report
Table 106. The relationship between vitamin D3 daily doses and changes in 25(0H)D
concentrations in RCTs
Table 107. Adverse events reported in RCTs
Figures
Figure 1. Summary of the vitamin D endocrine system
Figure 2. Generic analytic framework to assist formulation of key questions for the
development of DRis
Figure 3. Analytic framework for vitamin D and/or calcium EARs
Figure 4. Analytic framework for vitamin D and/or calcium ULs
Figure 5. Literature flow in this report
Figure 6. Cardiovascular outcomes risk stratified by vitamin D concentration
Figure 7. Prostate cancer risk stratified by vitamin D concentration
Figure 8. Colorectal cancer risk stratified by vitamin D concentration
Figure 9. Colon cancer risk stratified by vitamin D concentration
Figure I 0. Rectal cancer risk stratified by vitamin D concentration
Figure 11. Cardiovascular outcomes risk stratified by calcium intake
Figure 12. Stroke risk stratified by calcium intake
Figure 13. Prostate cancer risk stratified by calcium intake
Figure 14 Colorectal cancer risk in both sexes stratified by calcium intake
Figure 15 Colorectal cancer risk in men stratified by calcium intake
Figure 16 Colorectal cancer risk in women stratified by calcium intake
Figure 17 Colon cancer risk stratified by calcium intake
Figure 18. Rectal cancer risk stratified by calcium intake
Figure 19. Colorectal adenomatous polyp risk stratified by calcium intake
Figure 20. Breast cancer risk stratified by calcium intake
Figure 21. Hypertension risk stratified by calcium intake
Figure 22. Forest plot of trials of combined vitamin D and calcium supplementation and
effects on all-cause mortality
Figure 23. Relationship between doses of Vitamin D3 supplementation and net changes
in serum 25(0H)D concentrations in RCTs
Figure 24. Relationship between doses of Vitamin D
3
supplementation and net changes in
serum 25(0H)D concentrations in RCTs by baseline vitamin D status among adults
Figure 25. Relationship between doses of Vitamin D
3
supplementation and net changes in
serum 25(0H)D concentrations in RCTs by duration of supplementation among
adults
Appendixes
Appendix A. Search Strategy for Primary Studies
Appendix B. Search Strategy for Systematic Reviews
Appendix C. Evidence Tables
Appendix D. Existing Systematic Reviews
XVI
Appendix E. Blank Data Extraction Form and Qua lity Assessment Checklists
Appendix F. Excluded Studies With Reasons
Appendixes and Evidence Tables for this report are provided electronically at
http://www.ahrq.gov/downloads/pub/evidence/pdf/vitadcaVvitadcal.pdf.
XVII
Evidence Report
15
16
Chapter 1. Introduction
Background
The Food and Nutrition Board of the Institute of Medicine (IOM), with funding from
agencies and departments of the US and Canadian governments, recently completed their 1 0-
year development of nutrient reference values entitled Dietary Reference Intakes (DRI).
1
In
September, 2007, the IOM held a conference to examine the lessons learned and future
challenges from the process used to develop the DRI values.
2
One improvement identified at that
meeting for DRI updating was the use of systematic reviews to enhance the transparency and
rigor of the literature review process that is a necessary component in the deliberations ofDRI
committees. To assess the feasibility of implementing this approach in the DRI updating process,
the Office ofDietary Supplements (ODS) of the National Institutes ofHealth (NIH) through the
Agency for Healthcare Research and Quality (AHRQ) requested the Tufts Medical Center
Evidence-based Practice Center (Tufts-EPC) perform an exercise to identify the issues and
challenges of conducing systematic reviews as a component of the process used to support the
development and updating ofDRI values. The Tufts-EPC assembled a group of nutrition experts
from academic institutions and federal government agencies, led participants in teleconferences
and meetings, and conducted exercises in formulating questions that would be amenable to a
systematic review of the scientific literature and abstract screening.
3
One of the intents of this
exercise was to identify limitations, challenges, and unanticipated issues that IOM committees
may face prior to actually initiating the use systematic reviews as a routine part of the DRI
process.
Following these activities, a working group of US and Canadian government scientists
convened to determine whether the scientific literature was sufficient to justify a new review of
the vitamin D DRI. To address this issue in May and September of2007, two conferences were
held on the topic of vitamin D and health.
4
As a result of these conferences in March of2008 the
IOM convened a working group of US and Canadian government scientists to detennine whether
significant new and relevant scientific evidence had become available since the 1997 IOM
publication of vitamin D DRI to justify initiating a formal review and potential revision of the
values.
5
The working group reviewed the proceedings of the two conferences and the results
from a systematic review commissioned by the ODS on the effectiveness and safety of vitamin D
in relation to bone health conducted by the University of Ottawa EPC (Ottawa-EPC).
6
They
concluded that there was sufficient new data on bone health for several of the lifestage groups,
on potential adverse effects, and on dose-response relationships between intakes and circulating
25-hydroxyvitarnin D [25(0H)D] concentrations, and between 25(0H)D concentrations and
several health outcomes to warrant a formal review and potential revision of the values.
5
As a
result, the NIH/ODS, Public Health Agency of Canada, Health Canada and FDA commissioned
the Tufts-EPC to update the Ottawa-EPC report, and systematically review the data related to
vitamin D and calcium with respect to a broader spectrum of health outcomes.
Sources, Metabolism and Functions of Vitamin D
Vitamin D was classified as a vitamin in the early 20
1
h century and in the second half of the
20th century as a prohormone ("conditional" vitamin).
7
'
8
There are two forms of vitamin D,
vitamin D
3
(cholecalciferol), which is produced from the conversion of7-dehydrocholesterol in
17
the epidetmis and dermis in humans, and vitamin D
2
(ergocalciferol) which is produced in
mushrooms and yeast. The chemical difference between vitamin D
2
and D
3
is in the side chain;
in contrast to vitamin D3, vitamin D2 has a double bond between carbons 22 and 23 and a methyl
group on carbon 24.
The major source of vitamin D for humans is exposure to sunlight. The efficiency of the
conversion of7-dehydrocholesterol to vitamin D
3
is dependent on time of day, season of the
year, latitude, skin color and age. There is little vitamin D that occurs naturally in the food
supply. The major naturally occurring food sources include fatty fish, beefliver and egg yolk. fn
the U.S. and Canada, the major dietary source of dietary vitamin D is fortified foods, including
cow' s milk and, depending on country, other fortified foods and dietary supplements. These
sources cannot be relied on in countries other than the U.S. and Canada. Dietary vitamin Dis
absorbed from the intestine and circulates in plasma bound to a vitamin D binding protein.
In its native form vitamin Dis not biologically active, the active form is 1,25(0H)2D. The
conversion of vitamin D to 1,25(0H)
2
D requires two hydroxylation in tandem. Vitamin Dis
first hydroxylated by the liver to form 25(0H)D, which is then hydroxylated by the kidney to
form 1 ,25(0H)
2
D. 25(0H)D has low biological activity, but it is the major form of vitamin D
that circulates in the blood stream. Serum 25(0H)D concentrations are generally thought to
reflect nutritional status.
7
'
8
When adequate amounts of vitamin Dare available, the kidney, the
major site of 1,25(0H)2D production converts some of the 25(0H)D to alternate hydroxylated
metabolites, which have low biological activity (e.g., 24,25(0HhD or 1 ,24,25(0H)3D). Renal
synthesis of 1 ,25(0H)
2
D is tightly regulated by plasma parathyroid hormone, together with
serum calcium and phosphorus concentrations. Additional tissues that express the enzyme that
catalyses the conversion of25(0H)D to 1,25(0H)2D, 25-hydroxyvitamin D3-1-a-hydroxylase,
include colon, prostate, mammary gland, macrophages, antigen-presenting cells, osteoblasts and
keratinocytes.
9
Vitamin D has both genomic and nongenomic functions. For the genomic functions,
1 ,25(0H)
2
D interacts with nuclear vitamin D receptors to influence gene transcription. Nuclear
receptors for 1 ,25(0H)
2
D have been identified in over 30 cell types, including bone, intestine,
kidney, lung, muscle and skin. For the nongenomic functions, 1,25(0H)2D acts like a steroid
hormone, working through activation of signal transduction pathways linked to vitamin D
receptors on cell membranes. Major sites of action include .intestine, bone, parathyroid, liver and
pancreatic beta cells. Biological actions include increases in intestinal calcium absorption,
transcellular calcium flux and opening gated calcium channels allowing calcium uptake into cells
such as osteoblasts and skeletal muscle.
One of the major biological functions of vitamin Dis to maintain calcium homeostasis which
impacts on cellular metabolic processes and neuromuscular functions. Vitamin D affects
intestinal calcium absorption by increasing the expression of the epithelial calcium channel
protein, which in tum enhances the transport of calcium through the cytosol and across the
basolateral membrane of the enterocyte. Vitamin D also facilitates the absorption of intestinal
phosphate. 1 ,25(0H)
2
D indirectly affects bone mineralization by maintaining plasma calcium
and phosphorus concentrations, and subsequently extracellular calcium and phosphorus
concentrations at the supersaturating range necessary for mineralization. 1,25(0H)2D, in concert
with parathyroid hormone, also causes demineralization of bone when calcium concentrations
fall to maintain plasma concentrations within a narrow range. It has yet to be determined whether
1 ,25(0H)
2
D directly influences bone mineralization.
18
In addition to intestine and bone, a wide range of other tissues and cells that are influenced
by vitamin D. Five biological systems have vitamin D receptors and are responsive to
1,25(0H)
2
D, as summarized in Figure 1.
10
These systems include immune, pancreas,
cardiovascular, muscle and brain; and control of cell cycle. The biological effects of 1 ,25(0H)
2
D
are diverse. For example, as recently noted, 1,25(0H)
2
D inhibits PTH secretion and promotes
insulin secretion, inhibits adaptive immunity and promotes innate immunity, and inhibits cell
proliferation and stimulates their differentiation.
11
A number of recent reviews have appeared on
these topics.
10
"
17
Figure 1. Summary of the vitami n D endocrine system
VITAMIN D ENDOCRINE SYSTEM
SELECTED BIOLOGICAL RESPONSES
I A.WN20C8 I
ZIU!i!Otii,O. R<:PTORS
QtOHMOCVI"!
FAACTURf HEAlJNG CAI.LU$ .
REASSOIIPnOH 01' Ca'" 6 PI ~
A850APnONOfi Ca'" ------+-!
!oiOIIILl.lATION I ACCRE110H 0# Ca'" & P, ---+-1
From Norman AW. A vitamin 0 nutritional cornucopia: new insights concerning the serum 25-
hydroxyvitamin 0 status of the US population.
10
Sources, Metabolism, and Functions of Calcium
The major source of dietary calcium in the North American diet, but not necessarily other
counties, is dairy products (about 70 percent). Additional sources include commercial white
bread made with calcium sulfate, foods made with milk products, leafy greens, canned fish and
calcium fortified foods. Oxalic acid impedes the absorption of calcium from many plant foods.
Intestinal calcium absorption is regulated by two processes. One route of intestinal calcium
19
absorption is dependent on 1,25(0H)
2
D. This process occurs primarily in the duodenum and
proximal jejunum, is saturable, is energy dependent, and involves a calcium binding protein. The
1 ,25(0H)
2
D-dependent absorption of calcium is stimulated by low dietary calcium intakes. The
other route of intestinal calcium absorption is independent of 1 ,25(0H)
2
D and is termed
paracellular. This process is passive (does not depend on carrier proteins or energy) and occurs
primarily in the jejunum and ileum. Calcium is absorbed between cells, rather than through cells,
and down the concentration gradient. Calcium can be transported in blood bound to albumin and
prealbumin, complexed with sulfate, phosphate or citrate, or in a free (ionized) state.
Calcium is transported in blood bound to proteins ( 4 0 percent), primarily albumin and
prealbumin, complexed with sulfate, phosphate or citrate ( 10 percent), and in the ionized form
~ 5 0 percent). Blood calcium concentrations are controlled extracellularly by parathyroid
hormone, calcitriol and calcitonin. Intracellular calcium concentrations are maintained at
relatively low levels. Increased intracellular calcium concentrations occur in response to second
messengers by stimulating release from intracellular sites (endoplasmic reticulum, mitochondria)
and hormones by facilitating influx from extracellular sites by transmembrane diffusion or
channels.
Calcium balance measures provide information on calcium absorption relative to calcium
loss in urine, sweat and endogenous intestinal secretions. During periods of growth, positive
calcium balance implies bone mineralization but does not provide an indication of whether the
rate of bone mineralization is optimal. During adulthood negative calcium balance implies
calcium lost from bone but does not provide an indication of which site(s). Calcium balances
measures provide an indication of current but not prior calcium balance. An alternate approach to
assessing bone mineralization is by measuring bone mineral density.
Approximately 99 percent of the calcium in the human body is in bone and teeth. fn addition
to structural roles, calcium has other critical functions. These include serving as a second
messenger (e.g., cytosolic calcium, calcium-dependent trigger proteins, removal of calcium
stimulus) and protein activator (e.g. phospholipase A
2
, calpains [calcium dependent proteins that
contain calmodulin-like domains], blood clotting enzymes, annexins [calcium and phospholipid
binding proteins]). 1,25(0H)2D plays a critical role in regulating plasma calcium concentrations
through its role in intestinal calcium absorption, bone resorption and renal calcium resorption.
These functions of calcium are frequently classified into the following general categories; bone
development and maintenance, blood clotting, transmission of nerve impulses to target cells,
muscle contraction and cell metabolism. In addition, calcium may play a role in colon cancer,
kidney stones, blood pressure, body weight and lead absorption.
Challenges for the DRI Committees
The following generic challenges must be addressed, preferably in a standardized way,
before additional systematic reviews are conducted for use by upcoming DRI committees to
ensure the resulting product will yield a maximally useful document.
3
Because the potential
volume of peer reviewed literature on the biological effects of most essential nutrients is large
and continues to grow, rational and well defined eligibility criteria will need to be identified by
the committee to manage the workload. Appropriate questions must be formulated so that the
answers to those questions can be used to inform the DRI development process, ensure
transparency and reproducibility, and serve as the foundation for future updates as new data
emerge. Experience has shown that in the absence of unlimited resources, only a limited set of
20
questions can be addressed. Hence, it is critical that the committee prioritize the topics and refine
the questions in a way that will address critical issues for development and revision ofDRI
values.
Age specific intermediate or surrogate outcomes will need to be identified by the committee
when few or no studies directly link specific nutrient intakes with clinical outcomes. Preferably,
these would include only validated surrogates of the clinical outcome, that is outcomes that are
strongly correlated with the clinical outcome (e.g., bone mineral density as a surrogate for
fractures in postmenopausal women), and changes in their status reflect corresponding changes
in the risk of the clinical outcome (e.g., changes in bone mineral density reflect changes in
fracture risk in postmenopausal women).
18
In the absence of validated surrogate outcomes,
intermediate outcomes must be identified and considered (e.g., absence of anemia as an
intermediate outcome for the absence of disease or serum osteocalcin [bone turnover index] as an
intermediate marker for fractures). When a nonvalidated intermediate outcome must be
considered, the implicit assumption is that they would have the properties of a validated
surrogate outcome. Not only should this assumption be made explicit, but the uncertainties
involved in applying thi s assumption should be identified, documented, and discussed by the
committee.
Reliable indicators of exposure (or biomarkers) need to be identified by the panel. A reliable
biomarker should accurately reflect the degree of biological exposure to the nutrient of interest
and fulfill the classic risk assessment model (e.g., exhibit a dose-response relationship). To that
extent, the measurement of biological exposure should be independent and free from any
interaction with the self-estin1ated intake of the nutrient of interest. It is important for the DRI
committee to recognize that use of a biomarker to evaluate the strength of downstream
associations requires that the biomarker concentrations be back translated into levels of nutrient
intake and that if an association is found between a given biomarker concentration and risk of a
clinical outcome, an estimate of the nutrient intake that corresponds to the clinical outcome will
likewise be necessary.
Additional challenges for the DRI committees with respect to the conduct of systematic
review include defining relevance of studied populations with respect to nutrient distributions
and health risks to those for which reference values are being established, generalizability of
well-controlled experiments with few subjects, generalizability of studies of subjects having
narrow eligibility criteria, applicability for findings of animal studies to humans when data in
humans are nonexistent, generalizability of early studies that used methodologies not considered
state of the art or directly comparable with contemporary methods (e.g., change in analytical
techniques or standardization), appropriate approaches to evaluating, interpreting and integrating
data from observational studies with interventional data, and approaches to factor contemporary
issues into the process, such as the role of genomics and nutrient fortification into the systematic
review.
21
Key Questions Addressed in this Report
The aim of this report is to answer specific questions formulated to support the review and
updating ofDRI values by the DRI committee. The primary purpose of this report is to
summarize all existing literature of vitamin D and calcium, and clinical outcomes in a way that
will facilitate the deliberations of the IOM committee commissioned to review and potentially
revise the DRI values for these nutrients. Specific clinical, surrogate and intermediate outcomes
that are relating to vitamin D or calcium functions were selected by a technical expert panel.
Detailed methods and analytic frameworks are described in Chapter 2. The intent of this report is
not to make recommendations on specific outcomes nor specific values for DRI to be based
upon, the intent of this report is to provide information for use during the deliberations of the
10M committee. The federal agencies of the US and Canadian governments involved in the DRI
process formulated the key questions listed below based on the generic analytic framework as
recently described (Figure 2).
3
The key questions are:
What is the effect of exposures on functional or clinical outcomes? (Arrow 1)
What is the effect of exposures on indicators of functional or clinical outcomes? (Arrow 2)
What is the effect of indicators of exposure or body stores on functional or clinical
outcomes? (Arrow 3)
What is the effect of exposures on indicators of exposure? (Arrow 4)
What is the effect of indicators of exposure or body stores and intermediate indicators of
outcomes? (Arrow 5)
What is the effect of intermediate indicators of outcomes and functional or clinical
outcomes? (Arrow 6)
For each of these questions, the mandate was to also address factors that affect these
relationships.
22
Figure 2. Generi c analytic framework to assist formulation of key questions for the development
of ORis.
Arrow 4
Arrow 1
Arrow 2
Indicators
of
,
(Valid) Surrogate
Outcomes
(Predictors of
clinical outcomes)
Arrow 3
Exposure \ . ,
, ........... \
' lntermed1'ate
1
',, Arrow 2 ;
1 1
l/
i: Outcomes 1
l
1
i (Possible predictors of
1
1
.
\ ___
Arrow 1 : Association of exposure with clinical outcomes of interest
Clinical
Outcomes
Arrow 2: Association of exposure with surrogate or intermediate outcomes (with good or possible
evidence for linkage with clinical outcomes).
Arrow 3: Association of indicators of exposure to clinical outcomes.
Arrow 4: Association between exposure and indicators of exposure.
Arrow 5: Association of indicators of exposure to surrogate or intermediate outcomes (with good or
possible evidence for linkage with clinical outcomes).
Arrow 6: Association between surrogate outcomes (with good or possible evidence for linkage) and
clinical outcomes.
The focus oftbis evidence report is on the relationship of vitamin D only, calcium only, and
combinations of vitamin D and calcium to relevant health outcomes. Serum 25(0H)D
concentration was used as an indicator of vitamin D status and calcium intake (dietary and
supplement) as an indicator of calcium status. Evidence was sought for the life stages as defined
in the DRI process. For the above questions, information relevant to benefit (efficacy) and safety
(adverse effects) were considered. The questions were refined with input from a committee of
vitamin D and calcium experts, discussed in the Methods chapter.
23
Chapter 2. Methods
Overview
This report is based on a systematic review of key questions on the relationships between
vitamin D [either 25(0H)D concentrati ons or supplements] or dietary calcium intake, and health
outcomes. The methodologies employed in this evidence report generally follow the methods
outlined in the AHRQ Methods Reference Guide for Effectiveness and Comparative
Effectiveness Reviews
(bttp://effectivehealthcare.ahrg.gov/repFiles/2007 I ODraftMethodsGuide.pdf) . The initial
questions identified by the federal sponsors of this report were refined with input from a
Technical Expert Panel (TEP). This report does not make clinical or policy recommendations.
The report is being provided to an TOM committee charged with updating vitamin D and calcium
DRis.
A description of roles and responsibilities of sponsoring federal agencies, AHRQ, the TEP
and the EPC is included to clarify the relationships that support the process and ensure
transparency and that the approach adhered to the highest standards of scientific integrity.
Because of the large number of abbreviations for unfamiliar terms are used, their
explanations have been repeated whenever deemed necessary. A table of Abbreviations can be
found after the references in page 316. We also provide a table with the latitudes of several major
cities in Central and North America, right after the Abbreviations table, on page 320.
Sponsoring Federal agencies.
The sponsoring agencies were responsible for specifying the topic-specific task order
requirements. They participated in a Kick-Off meeting with the EPC and the Task Order Officer
(TOO) to facilitate a common understanding of the topic-specific work requirements, and
responded to inquiries from the TOO if modifications to the work order were requested by the
EPC. Any communication between the sponsoring agencies and the EPC occurred with oversight
from the TOO.
Review by Federal sponsors was limited to comments on factual errors, requests for
clarification, and consistency with the original contract task order. Comments on the scientific
content of the report were not provided. In all cases, reviewer comments are advisory only and
are not binding on the scientific authors of the final report.
AHRQ Task Order Officer (TOO).
The TOO was responsible for overseeing all aspects of this Task Order. The TOO served as
the point person for all communication required between the sponsoring agencies, the EPC, and
other AHRQ officials. The purpose of this communication was to facilitate a common
understanding of the task order requirements among the sponsors, the TOO, and the EPC,
resolve ambiguities and to allow the EPC to focus on the scientific issues and activities.
Technical Expert Panel (TEP).
The TEP is comprised of qualified experts including, but not limited to, individuals with
knowledge ofDRI decision making processes, vitamin D and calcium nutrition and biology
across the life cycle, health outcomes of interest, and the methodology of conducting systematic
reviews. The EPC worked closely with the TEP in the formative stages of the project on question
25
refinement and throughout the evidence review process to address questions that occurred. The
EPC conducted the actual systematic review of the questions independent of the TEP and other
stakeholders. It was specified, a priori, that a TEP member who served as a peer reviewer for the
final report could not also serve as a member of the subsequent calciwn and vitamin D DRI
Committee.
Those serving on the TEP provided input on such factors as reviewing search terms to ensure
they were adequately inclusive, assessing search strategies to ensure they comprehensively
covered the questions of interest, and answering questions about technical details (e.g., nuances
of laboratory methods of performing an assay). Members of the TEP did not participate in EPC
research meetings or in reviewing and synthesizing evidence. Their function was limited to
providing domain-specific knowledge and advising the proper context that is relevant to the
process of evaluating DRI. They did not have any decision making role and did not participate in
writing any part of the evidence report.
EPC methodologists.
This evidence report was carried out under the AHRQ EPC program, which has a 12-year
history of producing over 175 evidence reports and numerous technology assessments for
various users including many federal agencies. EPCs are staffed by experienced methodologists
who continually refine approaches to conducting evidence reviews and develop new methods on
the basis of accumulated experience encompassing a wide range of topics. The Tufts EPC has
produced many evidence reports on nutrition topics
19
-
24
(http://www.ahrq.gov/clinic/epcix.htm).
We have also conducted methodological research to identify the issues and challenges of
including evidence-based methods as a component of the process used to develop nutrient
reference values, such as the DRI, using vitamin A as an example.
3
Development of the Analytic Framework and Refinement of
Key Questions
The focus of this report is on the relationship of vitamin D only, calcium only, and
combinations of vitamin D and calciwn with specific health outcomes. Key questions and
analytic frameworks were developed by defining each box in the generic analytic framework
described in Chapter 1 with specific reference to vitamin D and calcium.
A one-day meeting of the federal sponsors, TEP and Tufts EPC staff was held in Boston on
September 20, 2008. At this meeting, the analytic framework was discussed, the key questions
refined, and study eligibility criteria established. Two analytic frameworks were developed: one
for vitamin D and/ or calcium Estimated Average Requirements (EARs) and one for Tolerable
Upper Intake Levels (ULs) (Figures 3 & 4). We used the PI(E)CO method to establish study
eligibility criteria. This method defines the Population, Intervention (or Exposure in the case of
observational studies), Comparator, and Outcomes of interest. Details are described in the
sections that follow.
26
Figure 3. Analytic framework for vitamin D and/or calcium EARs
,/ ..
\
Foods &
supplements
Arrow 4
Arrow 1
Arrow 2
25(0H)D;
1,25(0H)D
r
balance
Hypertension
(
BMD, BMC
'---../ \ Arrow 5 _..
......
\ ..
., Cancer markers [/Arrow 6
Arrow 2 ' , --------------"-.
.............................................. .,:;; Blood Pressure !
!:
circulating levels
Arrow 1: Association of exposure with clinical outcomes of interest.
Function
Immune
Arrow 2: Association of exposure with surrogate or intermediate outcomes (that have good or possible
evidence for linkage with cli nical outcomes, respectively). (Surrogate outcomes are depicted in boxes
with a solid outline, and intermediate outcomes are depicted in boxes with dashed outline.)
Arrow 3: Association of indicators of exposure to clinical outcomes.
Arrow 4: Association between exposure and indicators of exposure.
Arrow 5: Association of indicators of exposure to surrogate or intermediate outcomes.
Arrow 6: Association between surrogate or intermediate outcomes and cli nical outcomes.
27
Figure 4. Analytic framework for vitamin D and/or calcium Uls
Arrow 1
25(0H)D;
1,25(0H)D
Arrow 3
Arrow 1: Association of exposure with clinical outcomes of interest.
Arrow 3: Association of indicators of exposure to clinical outcomes.
Arrow 4: Association between exposure and indicators of exposure.
Definitions
Vitamin D and Calcium Exposures
Outcomes
Psoriasis
Soft tissue
calcification
Cancer
All cause
mortality
Vitamin D exposure included intake of vitamin D2 or vitamin D3 from foods and
supplements, including human milk and commercial infant formulas. Because the primary source
of vitamin D in the human body is produced in skin exposed to sunlight, background information
on ultraviolet B (UVB) exposure was captured to the extent possible. However, we did not
include studies that evaluated the effect of or association between exposure to sunlight (or UVB)
and clinical outcomes or serum 25(0H)D concentrations. In other words, we did not investigate
sunlight exposure as a proxy for or a source of vitamin D intake. Sunlight exposure was
considered only as a potential confounder or effect modifier of associations between vitamin D
or calcium and clinical outcomes.
Calcium exposure included intake of calcium from foods and supplements, including
calcium-containing antacids, mineral-supplemented water, human milk and commercial infant
formulas.
Combined vitamin D and calcium exposure included any relevant combinations of the above.
Clinical Outcomes
Clinical outcomes are measures of how a person (e.g., a study participant) feels, functions or
survives, or a clinical measurement ofthe incidence or severity of a disease (e.g., diagnosis of
disease or change from one disease state to another). Examples of clinical outcomes used in this
report are incidence of cancer, vascular events, and preeclampsia. The clinical outcomes of
interest in this report are described in the "Specific Outcomes of Interest" section.
28
Indicators of Exposure (Nutrient Intake)
Indicators of exposure are measures that correlate with dietary intake of a nutrient, such as
nutrient biomarkers, nutritional status, or markers of nutritional status.
Indicators of vitamin D exposure (i.e., vitamin D intake and sun exposure) included serum
25(0H)D and 1,25(0H)2D concentrations.
Indicators of dietary calcium intakes included calcium balance (i.e., calcium accretion,
retention, and loss).
Surrogate Outcomes
Surrogate outcomes are biomarkers or physical measures that are generally accepted as
substitutes for or predictors of specific clinical outcomes.
18
Changes induced by the exposure or
intervention on a surrogate outcome marker are expected to reflect changes in a clinical outcome.
Examples of surrogate outcomes used in this report are bone mineral density (as a surrogate
marker of fracture risk) and breast mammographic density (as a surrogate marker of breast
cancer risk). The surrogate outcomes of interest in this report are described in "Specific
Outcomes of Interest" section.
Intermediate Outcomes
Intennediate outcomes are possible predictors of clinical outcomes that are not generally
accepted to fulfill the criteria for a surrogate outcome. However, in the absence of data for surrogate
outcomes, intermediate markers are often used. Examples of intermediate markers used in this
report are prostate cancer antigen (as a marker of prostate cancer risk) and blood pressure (as a
marker of stroke risk). All intermediate markers of interest in this report are described in
"Specific Outcomes of Interest" section.
Life Stages
In consultation with the TEP, the 22 life stages defined by the FNB/IOM for the development
of DRI were consolidated to 9 categories to facilitate the reporting of results. Within each life
stages, men and women (or boys and girls) were considered separately when possible. There are
also some inevitable overlaps between these categories. For example, most women in 51-70
years life stage are postmenopausal women. The 9 categories created for this report are:
o 0 - 6 months
o 7 months - 2 years
o 3-8 years
o 9 - 18 years
o 19 - 50 years
o 51 - 70 years
o 2:71 years
o Pregnant and lactating women
o Postmenopausal women
In summarizing studies for each given outcome, we used our best judgment to describe the
study results for each applicable life stage.
29
Key Questions
In agreement with the TEP, the following key questions were addressed in this evidence
report. It was decided that arrow 6 in the analytic framework (What is the relationships between
intermediate or surrogate outcomes and clinical outcomes?) is outside the scope of the DRI
literature review in this report. All outcomes of interest in this report are described in "Eligibility
Criteria" section.
Key Question 1. What is the effect of vitamin D, calcium, or combined vitamin D and calcium
intakes on clinical outcomes, including growth, cardiovascular diseases, weight outcomes,
cancer, immune function, pregnancy or birth outcomes, mortality, fracture, renal outcomes, and
soft tissue calcification? (Arrow 1)
Key Question 2. What is the effect of vitamin D, calcium or combined vitamin D and calcium
intakes on surrogate or intermediate outcomes, such as hypertension, blood pressure, and bone
mineral density? (Arrow 2)
Key Question 3. What is the association between serum 25(0H)D concentrations or calcium
balance and clinical outcomes? (Arrow 3)
Key Question 4. What is the effect of vitamin D or combined vitamin D and calcium intakes on
serum 25(0H)D concentrations? (Arrow 4)
Key Question 5. What is the association between serum 25(0H)D concentrations and surrogate
or intermediate outcomes? (Arrow 5)
Literature Search Strategy
We conducted a comprehensive literature search to address the key questions. For primary
studies, the EPC used the Ovid search engine to conduct searches in the MEDLINE and
Cochrane Central database. A wide variety of search terms were used to capture the many
potential sources of information related to the various outcomes (see Appendix A). Search terms
that were used to identify outcomes of interest, for both EARs and ULs, can be categorized into
the following groups: 1) body weight or body mass index; 2) growth (height and weight); 3)
fracture or bone mineral density; 4) falls or muscle strength; 5) cardiovascular diseases; 6)
hypertension or blood pressure; 7) cancer or neoplasms, including adenomas, colon polyps, and
mammography; 8) autoimmune diseases (e.g., type 1 diabetes, psoriasis, rheumatoid arthritis,
multiple sclerosis, inflammatory bowel disease, ulcerative colitis, and Crohn's disease); 9)
preeclampsia, eclampsia and pregnancy-related hypertension; 1 0) preterm or low birth weight;
11) breast milk or lactation; 12) death; 13) infectious diseases; 14) soft tissue calcification (for
ULs only); and 15) kidney disease or hypercalcemia (for ULs only). The different outcomes
were crossed with terms to identify vitamin D and calcium exposure: "vitamin D", "plasma
vitamin D", "25-hydroxyvitamin D" and its abbreviations, "25-hydroxycholecalciferol", "25-
hydroxyergocalciferol", "calcidiol ", "calcifediol", "ergocalciferol", "cholecalciferol",
"calciferol", "calcium", "calcium carbonate", "calcium citrate", "calcium phosphates" and
30
"calcium malate". Literature searches of the outcomes alone without references to vitamin D or
calcium were not conducted.
The searches were limited to human studies, English language publications, and citations
from 1969 to September 2008 for all but bone outcomes. For outcomes related to bone health
(i.e., bone mineral density, fracture, fall or muscle strength), we relied on a recent comprehensive
systematic review performed by the Ottawa EPC.
6
The Ottawa EPC report was updated from
January 2006 to September 2008. The electronic search was supplemented by bibliographies of
relevant review articles. Unpublished data, including abstracts and conference proceedings, were
not included. An updated literature search was performed in April2009 for all the topics to
include relevant primary studies published since September 2008 for the final report.
For potentially relevant systematic reviews, we also searched MEDLINE, the Cochrane
Database of Systemic Reviews, and the Health Technology Assessments database up to
December 2008. We searched for systematic reviews of the relationships between vitamin D or
calcium and the prespecified outcomes. In this search, terms for identifying vitamin D or calcium
exposures were crossed with terms for identifying systematic reviews, such as "systematic,"
"evidence," "evidence-based," "meta-analysis," or "pooled analysis"; specific terms for the
outcomes were not included (Appendix B).
Study Selection
Abstract Screening
All abstracts identified through the literature search were screened. Eligible studies included
all English language primary interventional or observational studies that reported any outcome of
interest in human subjects in relation to vitamin D and/or calcium.
Full Text Article Eligibility Criteria
Articles that potentially met eligibility criteria at the abstract screening stage were retrieved
and the full text articles were reviewed for eligibility. Rejected full text articles were examined
only once, unless the articles were equivocal for inclusion or exclusion. In that event, the article
in question was examined again by a different reviewer and a consensus was reached after
discussion with the first reviewer. We recorded the reason for rejection of all full text articles.
Primary studies.
Because the outcomes of interest ranged from very broad topics with common occurrences
(e.g., cardiovascular disease) to narrowly focused topics with relatively few occurrences (e.g.,
preeclampsia), the number and types of studies available for each outcome varied widely in the
distribution of study designs and sample sizes. It was neither possible nor desirable to use a
uniform, strict set of inclusion and exclusion criteria applicable to all outcomes. Therefore,
additional eligibility criteria germane to the specific outcome were applied to all accepted full
text articles. Details are described in the "Eligibility criteria" section.
General eligibility criteria for the full text articles were:
Population of interest:
Primary population of interest is generally healthy people with no known disorders
31
Studies that include a broad population that might have included some people with
diseases. For example, some hypertensive and diabetic patients were included.
People with prior cancers (or cancer survivors), prior fractures, and precancer conditions
(e.g., colon polyps) were included
Studies that enrolled more than 20 percent subjects with any diseases at baseline were
excluded. An exception was made for older adults (mean age 2:65 years old) due to high
prevalence of diseases in this population. For studies of older adults, only studies that
exclusively enrolled subjects with particular disease (e.g., 100 percent type 2 diabetes)
were excluded. In addition, for studies of blood pressure, studies of people exclusively
with hypertension were included.
For UL outcomes, we included any adverse effects of high intake in any population.
Intervention/exposure of interest.
For observational studies:
o Serum 25(0H)D or 1,25(0H)2D concentration
o Dietary intake level of vitamin D were not included due to inadequacy of nutrient
composition tables for vitamin D?
5
o Dietary intake level of calcium from food and/or supplements
o Calcium balance (i.e., calcium accretion, retention, and loss)
For interventional studies:
o Vitamin D supplements (but not analogues) with known doses
o Calcium supplements with known doses
o The only combination of dietary supplements of interest was the combination of
vitamin D and calcium. Any other combinations of supplements and/or drug
treatments were excluded unless the independent effects of vitamin D and/or
calcium can be separated. Thus studies of multivitamins were excluded.
o Trials in which participants in both study groups took the same calcium (or
vitamin D) supplement were evaluated as vitamin D (or calcium) versus control
trials. In other words, the intervention common to both study groups was ignored
(though it was noted).
o Food based interventions were included if the doses of vitamin D and/or calcium
were quantified and there were differences in the doses between the comparison
groups. For example, a trial of dairy supplementation (with 500 mg/d calcium)
versus no supplementation was qualified to be included. However, a trial of
calcium fortified orange juice (with 1200 mg/d calcium) versus milk (with 1200
mg/d calcium) was not qualified to be included because there are no differences in
the calcium doses.
o Non-oral routes of nutrient delivery were excluded
Specific outcomes of interest.
Growth outcomes
o In infants and premenarchal children: weight and height gain
Cardiovascular disease clinical outcomes
o Cardiac events or symptoms (e.g., myocardial infarction, angina)
o Cerebrovascular events (stroke, transient ischemic attacks)
o Peripheral vascular events or symptoms (diagnosis, claudication)
32
o Cardiovascular death
o Study-specific combinations of cardiovascular events
CVD intermediate outcomes
o Diagnosis of hypertension
o Blood pressure
Weight outcomes
o In adults only: incident overweight or obesity, body mass index, or weight (kg)
Cancer (incident or mortality)
o Cancer from alI cause (or total cancer)
o Prostate
o Colorectal cancer
o Breast cancer
o Pancreatic cancer
o Cancer-specific mortality
Cancer intermediate outcomes
o Colorectal adenoma
o Aberrant cryptic
o Breast mammographic density (quantitative whole breast density)
Immune function clinical outcomes
o Infectious diseases
o Autoimmune diseases
o Infectious disease-specific mortality
Pregnancy-related outcomes
o Preeclampsia
o High blood pressure with or without proteinuria
o Preterm birth or low birth weight
o Infant mortality
Mortality, all cause
Bone health clinical outcomes
o Rickets
o Fracture
o Fall or muscle strength
Bone health intermediate outcomes
o Bone mineral density or bone mineral content
Dose-response relationship between intake levels and indicators of exposure (arrow 4 of
Figures 2 and 3)
o Serum 25(0H)D concentration
o Breast milk or circulating concentrations of 25(0H)D in infants
Outcomes of tolerable upper intake levels (ULs)
o All-cause mortality
o Cancer and cancer-specific mortality
o Renal outcomes
o Soft tissue calcification
o Adverse events from vitamin D and/or calcium supplements
33
Study design.
Randomized controlled trials (RCTs)
Nonrandomized, prospective comparative studies of interventions
Prospective, longitudinal, observational studies (where the measure of exposure occurred
before the outcome)
Prospective nested case-control studies (case-control study nested in a cohort so the
measure of exposure occurred before the outcome)
We excluded cross-sectional studies and traditional, retrospective case-control studies
(where the measure of exposure occuned after or concunent with the outcome)
Systematic reviews.
We included relevant systematic reviews that addressed the key questions. Systematic review
is defined as a study that has at a minimum the following three components: a statement of the
research questions (aims or objectives); a description of the literature search; and a listing of the
study eligibility criteria. We did not attempt to contact authors for clarifications of outstanding
questions. In addition, the following types of reviews were excluded: reviews of foods or diets
that did not quantify vitamin D or calcium intake; reviews that included non-oral routes of
nutrient delivery; reviews that did not evaluate the association between vitamin D or calcium
intake to health outcomes; reviews of nonhuman data; and pooled analyses of primary databases
(i.e., secondary database analyses of multiple cohorts) that did not include a systematic review
(except possibly as a replacement for data from the original cohorts).
To determine the relevance of a systematic review to this report, the following inclusion
criteria were applied:
Address key question(s) of interest (i .e., similar Pl(E)CO criteria used):
a. Systematic review must include only healthy population at baseline or have
separate analyses for population with diseases and without diseases.
b. Systematic reviews of interventional studies had to include only vitamin D or
calcium interventions. Cointerventions with other nutrients had to be disallowed
or separate analyses were needed for studies of vitamin D or calcium
interventions alone.
c. Systematic review of observational studies had to report the baseline
concentrations of serum 25(0H)D and the assay methods used or the dietary
assessment methods used to measure dietary calcium intake (e.g. food frequency
questionnaire, 24 hour recall).
d. Exposure levels (e.g., level of25(0H)D or calcium intake) or doses of
interventions had to be reported
e. Outcome definitions had to be reported
f. Designs of primary studies had to be reported. If cross-sectional or case-control
studies were included, the systematic review must provide sufficient information
or separate analyses to separate them from RCTs or cohort studies.
We include only the most recent update if there were multiple systematic reviews from
the same group of investigators using the same review process.
Where there were several systematic reviews on the same topic with similar conclusions
and the same set of primary studies, we selected the systematic review with either the
latest cutoff date for the end of the literature search or the most included primary studies.
34
Other Specific Eligibility Criteria
Growth outcomes (weight and height gain)
o Only infants (<1 year old) and children (age <18 years old) were included
o For infants, we include all eligible study designs. The vitamin D and/ or calcium
intervention or exposure can be administered to the mothers or to the infants in
the study.
o For infants, premenarchal girls, and boys of similar age, only RCTs that reported
weight as a primary or secondary outcome were included. RCTs of weight loss
were excluded.
Cardiovascular disease clinical outcomes
o Only adults (aged 2:18 years old) were included.
Blood pressure and body weight
o Only adults (aged 2:18 years old) were included.
o Only RCTs of calcium or vitamin D interventions were included. We did not
include observational studies of associations between calcium or vitamin D intake
or serum vitamin D concentrations and blood pressure or weight measurements
(as continuous outcomes). This decision was made in agreement with the TEP in
part because it was agreed that any conclusions based on observational studies
(e.g., associations between baseline calcium intake and change in systolic blood
pressure) would be weak and difficult to interpret.
Bone health clinical outcomes
o The Ottawa EPC report
6
was updated with literature published between January
2006 and September 2008. Only RCTs qualified for inclusion.
o Studies of calcium and bone health clinical outcomes were excluded.
Bone health intermediate outcomes
o The Ottawa EPC report
6
was updated with literature published between January
2006 and September 2008. For adults, we included only BMD indices. For
children, we included only BMC indices. Only RCTs with duration of more than
1 year were qualified for inclusion.
o Studies of calcium and bone health clinical outcomes were excluded.
Dose-response relationship between intake levels and indicators of exposure (arrow 4 of
Figures 2 and 3)
o Studies for this question were identified in our literature search that crossed
vitamin D terms with various outcomes terms. Some studies that addressed this
question but do not report any of the outcomes of interest would not have been
identified in this manner. Because the availability of serum 25(0H)D
concentration is unlikely to be adequately indexed in the Medline citation, it
would be difficult to comprehensively search the literature for this question. To
do so would require retrieving all full text articles mentioning vitamin D
supplements (in excess of 1 0,000) to look for data on serum 25(0H)D
concentration.
35
o Only RCTs were included for this question. However, RCTs of different regimens
but with the same dose of vitamin D supplementation were excluded (e.g.,
comparison of daily, weekly versus monthly dose).
Data Extraction
For outcomes that had not been subjected to a prior systematic review, we extracted and
summarized the relevant data from the primary studies. Where previous systematic reviews were
available, we summarized their results into our report. In addition, we updated the previous
systematic reviews (with our eligibility criteria) and extracted and summarized the additional
primary studies.
Data extraction forms (evidence tables) were developed separately for extraction of
systematic reviews and primary studies. For pri mary studies, the items extracted were: study
characteristics, baseline population characteristics, background diet data, dietary assessment
methods for calcium intake, 25(0H)D assay methods, interventions (for interventional studies
only), confounders and effect modifiers that were adjusted for in statistical analysis, results, and
quality assessments. Whenever the type of vitamin D supplement (D
2
or D
3
) was clearly
reported, we extracted and reported this information. Otherwise, we used the general term
"vitamin D". Evidence tables for all eligible studies are available in Appendix C. For systematic
reviews, items extracted were: design, population, intervention (exposure) and comparator,
results, and AMST AR
26
checklist criteria (a measurement tool created to assess the
methodological quality of systematic reviews). A table with a list of all systematic reviews with
the evaluation of their relevance to this report, and evidence tables of the qualified systematic
reviews are available in Appendix D.
Data Analysis
We explored the dose-response relationship between the level of intake of vitamin D (with or
without calcium) and serum 25(0H)D concentrations graphically, using a scatter ("bubble") plot.
We plotted the observed net changes in 25(0H)D concentration, against the doses of vitamin D
supplementation. In these plots studies were represented by empty circles (bubbles) with area
proportional to the inverse ofthe within-study variances. Typically, the larger the bubble, the
larger the sample size and the smaller the standard error of the changes in 25(0H)D.
Studies were included only if they reported sufficient data to estimate both mean net change
and SE of the net change. We required data on both the mean net change in outcome level and
the SE of the change. However, many studies provided only the SEs for the baseline and final
outcome levels. In order to include these studies in the analyses we bad to make several
assumptions to estimate the SE of the change. To do this we used the equation:
SE12 = (SE1
2
+ SEl - 2pSE1SE2)
where SE
1
, SE
2
, and SE
1
2 are theSEs for baseline, final and change, respectively, and pis the
correlation between the baseline and final measurements?
7
We arbitrarily chose the correlation,
p, to be 0.50, the midpoint value. In our experience, using different values for p generally does
not greatly affect the meta-analysis results of quantitative analyses or conclusions.
For each RCT, theSE of the net change was then calculated using the standard calculation
for determining the SE of2 independent cohorts. Namely, in the above equation where the
correlation factor p becomes 0, and thus the final term drops out. Where studies reported either
within-cohort SEs or net change SEs, these numbers were used. Some RCTs may have more than
36
two arms (e.g., two different doses ofvitamin D supplement compared to the placebo), and in
this case, the same control am1 was used to calculate the net change and the SE of the net change
as for two independent comparisons.
Meta-analysis
Overall, we did not perform new meta-analyses in this report because of large degree of
clinical and methodological heterogeneity across studies. However, we reanalyzed an existing
meta-analysis using available data in the all-cause mortality section. We performed random
effects model meta-analyses of risk ratios using the DerSimonian and Laird model.
28
The random
effects model assigns a weight to each study that is based both on the individual study variance
and the between-study heterogeneity. Compared with the fixed effect model, the random effects
model is more conservative in that it results in broader confidence intervals when between-study
heterogeneity is present. We tested for using Cochran's Q (considered significant
for P <0.1 0) and quantified its extent with rZ
2
30
. 1
2
ranges between 0 and 100 percent and
quantifies the proportion of between-study variability that is attributed to heterogeneity rather
than chance.
lntercooled Stata SE version 9.2 and Meta-Analyst version 3.2 (developed by Tufts EPC)
were used for analyses. All P values are two tailed and considered significant when less than
0.05, unless otherwise indicated.
Grading of Studies Analyzed in This Evidence Report
Studies included as part of accepted in this report have been designed, conducted, analyzed,
and reported with various degrees of methodological rigor and completeness. Deficiencies in any
of these items may lead to biased reporting or interpretation of the results. While it is desirable to
have a simple evidence grading system using a single quantity, the quality of evidence is
multidimensional. A single metric cannot adequately capture information needed to interpret a
study. Not withstanding these limitations, providing an indication of study quality adds an
important dimension to the summary of published data.
Critical Appraisal and Grading of Primary Studies
Critical appraisal of the evidence is an important aspect of conducting a systematic review.
For the assessment of interventional studies, the criteria were based on the CONSORT
31
statement for reporting RCTs (a checklist with specifications for reporting important aspects of a
trial). We primarily considered the methods used for randomization, allocation concealment, and
blinding as well as the use of intention-to-treat analysis, the report of well-described valid
primary outcomes, and the dropout rate.
For interventional studies with nonrandomized design, we used the report of eligibility
criteria and assessed the adequacy of controlling for differences between compared groups in
terms of baseline characteristics and prognostic factors. We also considered the reporting of
intention-to-treat analyses and crossovers when so designed, as well as important differential loss
to followup between the compared groups or overall high loss to followup. The validity and the
adequate description of outcomes and results were also assessed.
37
For the assessment of prospective cohorts and nested case-control studies (cross-sectional
and retrospective case-control studies were excluded from this review), we developed a rating
checklist specifically designed for nutritional epidemiology study based on some of the reporting
items for cohort study in STROBE (STrengthening the Reporting of OBservational studies in
Epidemiology) checklise
2
and the nutrition-specific items in our previous publication.
33
Items
assessed include: eligibility criteria and sampling of study population, blinding of exposure and
outcome assessors, dietary assessment methodology (when applicable), assay methodology of
biomarkers of intake (when applicable), clear reporting of comparisons in the study, statistical
analyses, adequacy of controlling for baseline characteristics and prognostic factors (including
confounders), clear reporting of outcome defmitions, and prospective study design with
preplanned hypotheses.
The quality assessment checklists for intervention or observational studies can be found in
Appendix E. Additional considerations that were not included in the checklists are described
later in this section.
In this report we adapted a three-category grading system of the AHRQ Methods Reference
Guide for Effectiveness and Comparative Effectiveness Reviews. This system defines a generic
grading system that is applicable to each type of study design including interventional and
observational studies:
A
B
c
Studies have the least bias and results are considered valid. These studies adhere mostly to
the commonly held concepts of high quality including the following: a formal study design;
clear description of the population, setting, interventions, and comparison groups;
appropriate measurement of outcomes; appropriate statistical and analytic methods and
reporting; no reporting errors; less than 20 percent dropout; clear reporting of dropouts; and
no obvious bias. Sh1dies must provide valid estimation of nutrient exposure, from dietary
assessments and/or biomarkers with reasonable ranges of measurement errors, and
justifications for approaches to control for confounding in their design and analyses.
Studies are susceptible to some bias, but not sufficient to invalidate t he results. They do not
meet all the criteria in category "A", they have some deficiencies but none likely to cause
major bias. The study may be missing information, making it difficult to assess limitations
and potential problems.
Studies have significant bias that may invalidate the results. These studies have serious errors
in design, analysis, or reporting; there are large amounts of missing information, or
discrepancies in reporting.
If the initial assigned grade was equivocal, then the study received a second round of review
by an independent reviewer, and the final grade was reached via consensus. Lastly, it should be
noted that the quality grading system evaluates and grades the studies within their own design
strata (i.e., RCTs, cohorts, nested case-control). It does not attempt to assess the comparative
validity of studies across different design strata. Thus, it is important to be cognizant of the study
design when interpreting the methodological quality grade of a study.
38
Additional Considerations of Methodological Quality of Primary
Studies for the Purpose of DRI Decision Making
Randomized controlled trials of all outcomes.
The Tufts EPC debated about the quality assessment ofRCTs. A consensus was reached to
include additional considerations for RCTs to receive grade A. The general quality assessment of
interventional studies as described earlier has been widely adopted for the purpose of grading
high quality effectiveness trials (in contrast with a more standardized efficacy trial) which are
most relevant to the actual use of supplements. Thus the crossover of interventions (i.e.,
contamination between supplementation and placebo groups) affects the applicability more than
the methodological quality. However, it was the consensus among the Tufts EPC methodologists
that the RCTs with contamination between supplementation and placebo groups cannot receive
grade A because this issue affects the actual differences in the doses given to the subjects.
Therefore it is particularly important when the trial results are used to guide decisions about DRl,
as opposed to decisions about whether to actively recommend supplementation for an individual.
Observational studies of cancer outcomes.
When cancer cases were identified based on cancer registries or questionnaire-based data, we
perused whether the investigators verify the diagnoses independently (e.g., by medical records or
pathological reports). An observational study of cancer outcomes cannot receive grade A if the
cancer diagnoses were not verify independently. We also examined if the study adequately
control for other risk factors for specific cancer. We used the suggested risk factors by National
Cancer Institute (www.cancer.org). An observational study of cancer outcomes cannot receive
grade A if important risk factors for the specific cancer were not fully controlled for in their
analyses.
Critical Appraisal of Systematic Reviews
We also critically appraised systematic reviews utilized in this report. However, a summary
quality grade for systematic review is difficult to interpret. While it may be straightforward to
assign a high quality grade to a rigorously carried out systematic review of high quality primary
studies, a rigorously conducted systematic review finding only poor quality primary studies to
summarize has uncertain value. Similarly, a poorly conducted systematic review of high quality
studies may also result in be misleading conclusions. Therefore, to appreciate its validity, the
various dimensions and nuances of the systematic review must be understood.
To help readers appreciate the methodological quality of a systematic review, we applied the
AMST AR checklist/
6
a tool that was created for this purpose. This tool does not assign a
composite grade. Instead, the items evaluated are made explicit for the reader. Another
challenge in evaluating systematic reviews is that none of the existing systematic reviews were
specifically conducted to be used for DRI development; therefore their "quality'', for the purpose
ofDRl development, is impossible to reliably define.
In addition to using AMSTAR, we made comments on special considerations, issues or
limitations concerning design, conduct and analyses of the systematic review, and interpretability
of the results for the purpose of DRI development.
39
Reporting of the Evidence
Evidence tables.
Evidence tables offer a detailed description of the primary studies we identified that address
each of the key questions. These tables provide detailed infmmation about the study design,
patient characteristics, background diet, inclusion and exclusion criteria, interventions (or
exposures), comparators used, and outcomes assessed in the study. A study, regardless of how
many interventions (or exposures) or outcomes were reported, appears once in the evidence
tables. Evidence tables are ordered alphabetically by the first author's last name to allow for easy
searching within the tables. Evidence tables are available electronically in Appendix C.
Summary tables.
Summary tables were created to assist (qualitative) synthesis of primary studies ofthe same
outcomes and life stage. If feasible, data were also grouped by sex. Typically, in each outcome
section, we presented one summary table for the study characteristics of all included studies,
followed by another summary table for study findings.
We created different summary tables for different exposures (i.e., vitamin D or calcium) and
for different study designs (i.e., interventional or observational studies). Key study
characteristics, such as population characteristics (i.e., health status, age and sex), vitamin D
assay method and season in which blood was drawn, dietary assessment methods and whether
the instrument was internally validated, patient or participant adherence, and study comparisons,
were presented in the summary table for study characteristics. We reported daily vitamin D doses
(IU/d) and/or elemental calcium doses (mg/d) in all summary tables.
For observational studies, we also list the confounders adjusted in either design (e.g.,
matching factors) or analyses. If any confounders or effect modifiers in each prespecified
category (i.e., nutrients, demographics, anthropometry, medical conditions, ultraviolet exposure,
and life styles) were controlled for, we marked "X" in the category. Otherwise, the category was
left blank.
Graphical presentation of dose-response relationship.
We present graphically the results of studies associating outcomes with categorical
exposures (e.g., percentiles or other arbitrary categories of 25(0H)D concentration or of total
calcium intake). The graphs complement the information mentioned in the tables and allow the
reader to appreciate the direction of the estimated effects, even when the choice of the reference
category is inconsistent across studies. The graphs do not readily convey the slope (strength) of
the dose-response relationship between exposure and outcome, because the exposure categories
are simply ranked and their spacing does not necessarily correspond to the actual values that they
represent within study or across studies.
Grand summary tables (evidence map).
In the beginning of the Results section, we created a grand overview table. The table details
how many studies reported an outcome of interest (either as a primary or non-primary outcome)
and also listed the total number of Lmique studies (including systematic reviews) as each study
may have provided data on more than one outcome. The number of primary studies included in
each existing systematic review is also reported.
40
Units of measurement.
In this report, we converted serum 25(0H)D concentrations as reported by various studies as
different units (i.e., ng/mL, ~ t g / d L ~ g / L and ng/dL) to nrnol/L. The conversion formula is 1
ng/ mL = 2.5 nmol/L. To limit the variation in the reporting of vitamin D unit (e.g., nmol, IU, ~ g
and mg), IU was chosen as the standard unit and all other units were converted using a standard
formula. The conversion formula for micrograms is 1 ~ g = 40 IU.
Assay method.
For 25(0H)D measurements, we present information on the assay used in our evidence
tables, and summary tables describing individual studies. When reported, we also recorded
details on the methodology or kit used (e.g., RIA-radioimmunoassay, RIA "DiaSorin") used.
Often, additional information was lacking. We did not perform any subgroup analyses based on
the type of 25(0H)D assay used.
Sunlight exposure.
We report information on country where the study took place and its latitude (when this was
meaningful), and when available, the season when serum 25(0H)D concentrations were
measured. A substantial amount of vitamin D is formed in the skin in humans. The amount of
vitamin D synthesized in the skin depends on a person's exposure to UV irradiation. Therefore,
information on country's latitude (and season of serum 25(0H)D measurements) informs on
whether different populations are likely to have similar or different amount of endogenous
vitamin D production. Latitudes were extracted directly from the published reports, or
extrapolated from the city or country where the study took place (by searching Google for
"<county/city> latitude"). For national or international studies that spanned a wide range of
latitudes (e.g., NHANES), the latitude information was summarized simply as "various." To
facilitate the reader, we also provide a Table with the latitudes of major cities in Central and
North America (this table is found right after the Abbreviations table on page 316.
Primary and secondary outcomes.
For intervention studies, we distinguished primary from secondary (or nonspecified)
outcomes. Outcomes were considered primary only when they were clearly reported as such or
when the outcome was used in an ad hoc sample size calculation. For observational studies we
did not separate primary from secondary outcomes. For example, many observational studies are
analyses of the same well known cohorts for several different outcomes. Each of these studies
may have a different "primary" outcome.
Study quality.
We summarize methodological and reporting quality of individual studies and meta-analyses.
More details on the reporting characteristics of individual studies and systematic reviews are
found in the evidence tables (Appendix C).
41
Organization of the results section.
The Results section is organized in the following way:
Nutrient (vitamin D I calcium I combined calcium and vitamin D)
o Outcome (e.g., growth, cardiovascular diseases)
Synopsis
Detailed presentation (depending on availability of data)
Findings per calcium intake level I vitamin D concentration
Findings per age and sex
Findings by life stage
42
43
Chapter 3. Results
Literature Search Results
The original MEDLINE and Cochrane Central database search for primary studies yielded
15,621 citations ofEAR outcomes and 194 citations ofUL outcomes. The update search for
primary studies published between September, 2008 and April, 2009 yielded 918 citations We
identified 654 of these as potentially relevant and retrieved the full-text articles for further
evaluation. Of these, 478 did not meet eligibility criteria (Appendix E); thus, a total of 165
primary study articles met the inclusion criteria and were included in this report (Figure 5). Of
the 165 primary study articles, 60 were randomized controlled trials (RCTs), 3 were
nonrandornized comparative studies, and 102 were observational studies (either cohort or nested
case-control studies). The publication dates of the 165 primary study articles ranged from 1980
to 2009.
The MEDLINE, Cochrane Database of Systemic Reviews, and the Health Technology
Assessments database search for systematic reviews yielded 1746 citations. We identified 68 of
these as potentially relevant and retrieved the full-text articles for further evaluation. Of these, 46
did not meet eligibility criteria. After examining the 22 qualifying systematic reviews, 11 were
excluded for various reasons (Appendix D; Figure 5).
The grand overview tables (Tables 1, 2, and 3) detailed how many studies reported an
outcome (either as a primary or secondary outcome) that is of interest and also listed the total
number of unique studies (including those from systematic reviews) as each study may have
provided data for more than one outcome.
35
Figure 5. Literature flow in thi s report
Citations identified in MEDLINE and Cochrane
Central database search for primary studies,
published between 1969 and Arpil 2009
(n=16,733)
Citations identified in MEDLINE, Cochrane
Database of Systemic Reviews, and the Health
Technology Assessments database search for
systematic review articles published before
December, 2008 (n=1 ,746)
..
Abstracts fai led to meet
...
criteria (n=17,825)
Primary study articles retreived for full-text review
(n=584)
Systematic review articles retreived for full-text
review (n=68)
..
Articles failed to meet
...
criteria (n= 476)
Primary study articles reviewed (n=165)
- 60 randomized, controlled trials
- 3 nonrandomized comparative studies
- 1 02 observational studies (either cohort or
nested case-control studies)
Systematic reviews included (n=11)
36
Tabl e 1. Number of primary studies on vitamin D intake or concentration and specific health outcomes that could be applicable to
certain life stages
1/)
Ql
1/)
E Ql
E
0
E
(.)
.?;-
0
5
1/) Ql (.)
'iii
5
0
Ql
E
s:::
0 >
E
0
Ql (.) 0 (.)
'0
iii
s:::
(.)
0 (.) (.) CIS
5
:c
:5
s:::
0
.?;-
CIS
Ol
E
c.
(j l!!
iii 'iii
3
... CIS ...
c.
(.)
s:::
Ql 0 c,
Ql
s:::
:5
'0 ...
(.) s:::
(.)
.S! oiS
iii
Ql
Ql
Ql
s::: Ql
0
s:::
t:: (j
'0
...
(.) ...
E (j CIS CIS '0 Ql
CIS
0
s::: :I
iii .E
... s:::
(.) CIS (.)
E
(.)
s::: 'iii
E
=
0 1/)
Ql CIS
(.) Ol (.) s:::
.2 .2
c.
Ql
'iii
1/)
(.)
iii iii
CIS
iii
Ql
'i:
a; s::: CIS
E iii
E
Ql s:::
s:::
CIS
Ql (j (j (.)
Ql 1/) Ql .E
Q.
.s:::
(j
3: (.)
iii Ql Ql
c;; c;;
Ql s:::
CIS
:I .s:::
c;;
...
0
...
:I
(j
CIS '0
>
iii
(.) Ql Ql Ql
0 '0
0 CIS CIS
E
Ql
f.
s::: s::: c.
0
0
0
0
0 0
Ql
l!!
s:::
0
&
> 0 ... ... CIS
.5
C(
0 0 >
ii:i 0 m .... D.. 0 0 m m D.. D.. m m J:
0 - 6 mo 8
7 mo - 2 y
18
38y
9 - 18 y 2 2
19 - 50 y 2
51 -70 y 3 2 10 6 2 2 8
y 2 8 3 2
Pregnant & lactating women 7
18
2
Total unique studies per outcome 9 5 3 3 12 9 3 0 2 2 8 3 3
2c
3
(Total number of ACTs per outcome] [6] (1) (3A) [2] [0] (1 1 [0] [0] (0) [0] [0] [8] [3] (3A) [0] (3A)
Systematic reviews (unique studies) per outcome 0 0 0 0 0 0 0 0 0 0 0 0 0 0
Shaded cells indicate that either the eligibility criteria excluded outcomes in those life stages or the outcomes are not applicable to those life stages. Blank unshaded cells indicate no
primary studies were identified in this report in those life stages.
A
Only RCTs were eligible for this outcome
8
Relationship between maternal 25{0H)D concentration and atopic eczema in infants
c
1 study was a combined analysis of Nurses Health Study and Health Professionals Follow-up Study
37
Table 2. Number of studies on calcium intake and health outcomes that could be to certain life stages
VI
Q)
VI
E Q)
E
0
'E
(.J
::-
0
'5
VI Q)
(.J
u;
'5
0
Q)
E
r::
0
>.
E
0
Q) (.J 0 (.J
"C
iii r::
(.J
....
(.J (.J nl
'5 0
:c
c:
r::
0
::-
Cl
nl
c..
u
Q)
iii u;
3
.... E
Qj Q.
(.J
r::
"C
Q) 0
Cl
r::
iii
c: Q)
Qj
(.J r::
(.J
.2 oil Q)
0 r:: "C
(.J
r:: Q)
....
E nl
0
nl
t::
u
....
nl "C Q) 0 iii
r:: :::1
iii E
....
r:: (.J nl (.J
E
0
r:: u;
=
0 VI
Q)
nl E
....
r::
.2
c..
Q)
"iii
VI
(.J Cl (.J (.J
s s
nl
iii
Q)
:E
.ii> r::
nl
E iii
E
Q) r::
r:: ....
.!
(.J Q) VI Q)
e s:: 3:
nl (.J (.J
nl
Q) c..
u
(.J
nl
Q) Q)
iii iii
Q)
r:: :::1 s::
t::
i >.
iii iii
.... ....
:::1 u nl Q) Q) Q)
"C
c
0 0 nl nl
E
Q)
0
0
"C
0
0
0 0 l!!
Q) r::
l!!
r:: r:: c..
0
....
> 0
Q:
.... <
. <(
0 0 >.
iii C)
0 al 1- 0 0 al al D. D. al al :t:
0-6 mo
7 mo -2 y
3-8 y
18
9- 18 y 3
19-50 y 2 3 3 5 3
51 - 70 y 9 5 12 17 6 5 2 4 2
2:71 y
18
2
Pregnant & lactating women 14
4 4 2
Total unique studies per outcome 3 11 8 3 12 21 6 6
2c 50
5
(SA]
0 14
(Total number of ACTs per outcome] [1] [0] [2] [0] [0] (1] [0] [0] [0] [0]
3 1 6
Systematic reviews (unique studies) per outcome 0 0 0 0 0 0 0 0 0
(17)
(2) (2) (12)
{64l
Shaded cells indicate that either the eligibility criteria excluded outcomes in those life stages or the outcomes are not applicable to those life stages. Blank unshaded cells indicate no
primary studies were identified in this report in those life stages.
A
Only RCTs were eligible for this outcome
c
Association between total calcium intake in childhood and colo rectal cancer after 65 years of followup
1 study was a combined analysis of Nurses Health Study and Health Professionals Follow-up Study
D
6 analyses, including 2 separate analyses of NHANES I
38
Tabl e 3. Number of primary studies on combined vitamin D and calcium intake and specific health outcomes t hat are relevant to certain
life sta es
Ill
41
II)
E
41
E
0
'E
u
0
'5
II)
41
u
'iii
'5
0
41
'E
s:::
0 >
E
0
41 u 0 u
'0 "iij s::: u
...
u u Ill
'5 0
:i:
:E
s:::
0
Ill
01
E
c.
u
"iij
'iii
'3
... Ill
Qj c.
u
s:::
'0 ...
41 0 c,
Q
s:::
"iij
:E
41
u s:::
.2
o!l
41
s::: 41 ...
0 s:::
t::
u
'0
u
Ill '0 41 E Ill
ti
Ill
0 "iij s::: ::I
E
... s::: u
'iii "iij 41
u Ill u
E
s:::
E
... 0 Ill
Ill
s:::
.!::! .a
c. 41 'iii
II)
u 01 u u "iij "iij Ill
"iij 41
c:
a; s::: Ill
E n; E
41 s:::
s:::
Ill
41
ti ti
u 41 II) 41 .E 41 Q.
.:::
u
u n; 41
-
u;
41 s:::
Ill
::I .:::
t::
i
Ill
...
u Ill '0
> "iij u;
0
u
::I
41 41 41
0
0 '0
0 Ill Ill
s::: E
41
J.
s::: s::: c.
0
0
0
0 0
41
41 0
(;
> 0 ... ... Ill
.E
...
<
0 0 >
iii (.) Ill 1- D.. (.) (.) Ill Ill D.. D.. Ill Ill J:
0 - 6 mo 1
7 mo - 2 y
3 - 8y
9 - 18 y 1
19 - 50 y 1 1 1
51 -70 y 1 1 1 3 1 1
y 1 8
Pregnant & lactating women 1
-
I 2 ] 8 3
Total unique studies per outcome
18 28 28
0
18 28 18 118C 28
4
18 28
[2Aj
0 0 0
[4Aj [2Aj [Total number of ACTs per outcome] [1] [2] [1] [1) [1) [11) [2) [1)
Systematic reviews (unique studies) per outcome 0 0 0 0 0 0 0 0 0 0 0 0 0 0
Shaded cells indicate that either the eligibility criteria excluded outcomes in those life stages or the outcomes are not applicable to those life stages. Blank unshaded cells indicate no
primary studies were identified in this report in those life stages.
A Only ACTs were eligible for this outcome
8
Including the Women's Health Initiative (WHI) trial
c A de novo reanalysis of the 10 ACTs in a previous systematic review and one newly added trial
39
Vitamin D and Health Outcomes
Vitamin D and Growth
We reviewed primary studies that evaluated relationships between vitamin D and growth
parameters in infants and children.
Synopsis.
Seven intervention studies and two observational studies evaluated intake of or exposure to
vitamin D and growth parameters in infants and children. Two intervention studies from the
same center found a significant association of maternal vitamin D intakes with infant birth
weights. Study methodologies were incompletely reported in these two studies. The rest of the
studies did not find a significant association between either maternal or offspring vitamin D
intake and offspring's weight or height. No overall conclusions could be drawn as the studies
reviewed had diverse populations and methodological approaches.
Detailed presentation (Tables 4, 5, 6 & 7).
Six RCTs
34
-
40
and one nonrandomized comparative studl' in eight publications reported on
the effect of vitamin D supplementation on growth parameters in infants and children. Two
cohort studies reported on the association between maternal serum 25(0H)D concentration and
her offspring' s growth parameters.
42
43
The number of subjects in the RCTs ranged from 19 to
200. The two cohort studies had 374 and 466 subjects, respectively. The latitudes of the studies
ranged from 38 to 51. Four studies administered vitamin D exclusively to expectant mothers
during the third trimester of pregnancy. One study administered vitamin D to both the lactating
mothers and her offspring. Two studies administered vitamin D only to the infants or children.
Followup ranged from delivery Lmtil 9 years. Methodological quality of two studies were rated B
and seven studies were rated C. The studies were limited by such factors as incomplete reporting
and small sample sizes.
Infant 0 - 6 months; 7 months - 2 years; pregnant or lactating women.
One RCT from UK administered vitamin D 1000 IU/d or placebo to 126 expectant mothers
(first generation Asian immigrants) during the third trimester and found no significant difference
between the infants' birth weights or birth lengths and those of the control population.
34
38
There
were twice as many low birth weight infants ( <2500 g) in the control group compared to the
supplemented group (21. 7 percent vs. 11.9 percent); however, this difference was not significant.
A study from US supplemented 10 lactating mothers with vitamin D 400 IU/d and their infants
with 300 IU/d for 6 months. Compared to the group where nine mothers received 6400 IU/d and
their infants none, there was no significant difference in the infants' weight or length at 1 month,
4 months, and 7 months of age.
39
A study from China randomly assigned 255 newborn infants to
100, 200, or 400 IU/d of vitamin D for 6 months and reported no significant difference in weight
or length among the three groups at 6 months of age.
36
One study from India randomly selected
100 expectant mothers to receive a total of 1.2 million IU of vitamin D (600,000 IU of vitamin
D
2
in ih and grh month) during the third trimester. The newborns' birth weight was significantlf
increased compared to those from 100 unsupplemented expectant mothers (difference 190 g).
3
Important elements of the study methodology like randomization technique and any blinding of
outcome assessors were not reported. An earlier nonrandomized comparison from the same study
center involving smaller samples reported similar findings.
41
The estimated baseline mean
40
dietary vitamin D intake in the expectant mothers from these two studies was less than 30 to 35
IU/d (the validity of these measures is unclear). An RCT from France supplemented 48 expectant
mothers with either vitamin D 1000 IU/d in the third trimester or 200,000 IU one time dose at 7
month pregnancy and found no significant difference in the infants' birth weights between the
two methods.
40
A cohort study from Australia analyzed the maternal serum 25(0H)D
concentration in 374 women at 28-32 week gestation (geometric mean in winter 48 nmoVL;
summer 69 nmoVL) and found no association with infant birth weight or length.
43
One cohort
study from UK analyzed the serum 25(0H)D concentration in 466 white women in late
pregnancy ~ 3 3 wk) and found the concentrations (from <30 to >75 nmol/L) were not related to
their offspring' s weight or height at birth, 9 months, and 9 years.
42
9 - 18 years.
One RCT of vitamin D3 (placebo, 200, or 2000 IU/d for 1 year) on girls in Lebanon aged 10-
17 years found no significant difference at 1 year followup in weight or height among the 34
girls who were premenarchal at time of enrollment.
35
Findings by life stage.
0- 6 mo One RCT found that supplementing expectant mothers with vitamin D
1000 fU/d during the 3rd trimester has no effect on infant birth weight or length. Another
RCT found that supplementing expectant mothers with a total of 1.2 million IU of
vitamin D during the 3rd trimester effected a significant increase in birth weight(+ 190 g).
Background diet is low in vitamin Din this study. A study compared supplementing
lactating mothers with vitamin D 400 IU/d and their infants 300 IU/d for 6 months with
mothers supplemented with 6400 IU/d and their infants none, there was no significant
difference in the infants' weight or length at 1 month, 4 months, and 7 mouths of age.
Another study compared supplementing newborn infants with 100, 200, or 400 IU/d of
vitamin D for 6 months and reported no significant difference in weight or length at 6
months of age. An RCT supplemented expectant mothers with either vitamin D 1000
IU/d during the third trimester or 200,000 IU one time dose at 7 mouth pregnancy and
found no significant difference in the infants' birth weights between the two methods. A
cohort study analyzed the maternal serum 25(0H)D concentration at 28-32 week
gestation (geometric mean in winter 48 nmol/L; summer 69 nmol/L) and found no
association with infant birth weight or length. Another cohort study found that serum
25(0H)D concentration (ranged from <30 to >75 nmoVL) in late pregnancy ~ 3 3 wk)
was not related to the newborn's weight or height at birth, 9 months, and 9 years.
7 mo- 2 y A cohort study found that serum 25(0H)D concentration (ranged from
<30 to >75 mnol/L) in late pregnancy ~ 3 3 wk) was not related to the newborn' s weight
or height at birth, 9 months, and 9 years.
3-8 y No study covered this life stage.
9 - 18 y A cohort study found that serum 25(0H)D concentration (ranged from
<30 to >75 nmol/L) in late pregnancy ~ 3 3 wk) was not related to the newborn's weight
or height at birth, 9 months, and 9 years. One RCT of vitamin D
3
(placebo, 200, or 2000
IU/d for 1 year) on girls 10-17 years old found no significant difference at 1 year
followup in weight or height among the girls who were premenarchal at time of
enrollment.
19 -50 y Not reviewed
51 - 70 y Not reviewed
41
:::::71 y Not reviewed
Postmenopause Not reviewed
Pregnant & lactating women One RCT found that supplementing expectant mothers
with vitamin D 1000 IU/d during the 3rd trimester has no effect on infant birth weight or
length. Another RCT found that supplementing expectant mothers with a total of 1.2
million IU of vitamin D during the 3rd trimester effected a significant increase in birth
weight ( + 190 g). Background diet is low in vitamin D in this study. A study compared
supplementing lactating mothers with vitamin D 400 IU/d and their infants 300 IU/d for 6
months with mothers supplemented with 6400 IU/d and their infants none, there was no
significant difference in the infants' weight or length at 1 month, 4 months, and 7 months
of age. An RCT supplemented expectant mothers with either vitamin D 1000 IU/d during
the third trimester or 200,000 IU one time dose at 7 month pregnancy and found no
significant difference in the infants' birth weights between the two methods.
42
Table 4. Vitamin D on growth outcome: Characteri stics of interventional studies
Author Year
Study Name Background
Location Population Calcium Intake & Comparisons Compli ance Comments
(l atitude) Vitamin D Data
[PMID]
RCTs
Health pregnancy 25(0H)O at 28-32 Vit 0 1000 nd First generation
status wk: 20.1 nmoi/L IU/d 3'd Asian
Mean age nd trimester only immigrants only
(range/SO), y
Male(%) 0
Feliciano Health healthy term 86% infant breastfed Vit 0 100 IU/d nd
1994
36
status unti l 5-6 mo vs. 200 IU/ d
China (22
2
N
Mean age newborn vs. 400 IU/d
to 47
2
N) (range/SO), y
[8078115]
Male(%) nd
EI-Hajj 2006
35
Health healthy 25(0H)O 35 nmoi/L; Vii 0
3
200 98% in placebo; 7.4 h sun
Lebanon status dietary Ca 677 mg/d IU/d vs. 2000 98% in low dose; exposure/wk
(33
2
N)
Mean age 13.2 (10-17) IU/d vs. 97% in high dose
(16278262] (range/SO), y placebo x 1 y
Male(%) 0
Wagner Health Fully lactating; Lactating mother's Mother Vit 03 in mothers; 78%white;
2006
39
status <1 mo dietary Vit 0 273 400 IU/ d + as low as 61% for 11% black;
Charleston, postpartum IU/d; dietary calcium infant 300 infants 11% Hispanic
US (32
2
N) Mean age 29 intake: 1125 mg/d; IU/d vs.
(17661565] (range/SO), y mother 6400
Male(%) 0 IU/d + infant 0
IU/d
Marya 1988 Health no pregnancy- Expectant mother's Mother Vii 0 nd
India status related dietary Vit 0 35 IU/d; 1.2miiiU
(28
2
N) complications calcium 429 mg/d (total ; 600,000
[3243609) Mean age 24 IU vit 02 in ih
(range/SO), y & 8
1
h mo) vs.
Male(%) 0 no
Mallet 1986
40
Health pregnancy Ca intake 550 to Vit 0 1000 nd
France (48
2
status 1000 mg/ d in 55% of IU/d vs.
N)
Mean age newborn the subjects 200,000 IU 1 X
[3755517] (range/SO), y dose
Male(%) nd
Nonrandomized comparative study
Marya 1981
4
Health no pregnancy- Expectant mother's Vit 0 1200 nd
India status related daily milk intake IU/d + Ca 375
(28
2
N) complications <500 ml; dietary Vit mg/ d (3'd
[7239350] Mean age nd 0 <30 IU/d trimester) or
(range/SO), y VitO 1.2mil
Male(%) 0 IU (total ;
600,000 IU in
ih & 8
1
h mo)
or no
sueelement
43
Table 5. Vitamin D and growth outcomes: Characteristi cs of cohort studies
Confounders/Effect Modifiers
Author Year
Adjusted
C/)
Study Name Q) E
Vitamin D .s:
:;
Q)
Location Population
Concentration
Comparisons Q. E
C/)
IU
C/)
E
(Latitude)
E
... Q.
iii
0
Q)
en 0
Q.
~
0
[PMID]
~
0 .. () )( (.)
E
.s:
'6
Q) C/)
:; Q) E
Q)
>
.2!
z c <
==
:::::> :J
a r i e ~ Health singleton Assay RIA Length and X X X X 99%
2006
4
status pregnancy; method weight in white;
Australia no disease offspring excluded
(38QS)
Mean age 29 stratified by dark skin
[16352684] (range/SO), mother's or women
y 25(0H)O with
Male (%) 0 Season winter & concealing
blood summer clothing
drawn
Gale 2008 Health singleton Assay RIA Length and X X White only
PAHSG status pregnancy method weight in
UK (502N) <17wk offspring
[1 731 1 057] Mean age 26.3 stratified by
(range/SO), mother's
y 25(0H)O
Male(%) 0 Season nd
blood
drawn
44
Tabl e 6. Vitamin D and growth outcomes: Results of ACTs
Author Year
Mean Interventions, No. Change Change Net Net Diff Study
Study Name Life St age Outcome 1/2 Unit Baseline PBtw
l PMID]
Follow up Daily Dose Analyzed {SO) 95% CI Diff 95% CI Quali ty
Maxwell Pregnant Infant
20
until
Vit D 1000 IU 59 NA
Final Diff
NS
1981
38
women & birth delivery
g
3157 3037 3277 +123 -50, 296c
.................................." .
Brooke infant 0-6 mo weight Control 67 NA 3034 2909,3159
B
1980
34
(Asians) infant
20
until Final Diff
[6793058) birth delivery
Vii D 1000 IU 59 em NA
49.7 49.6, 49.8 +0.2 0.1, 0.3
NS
---------
[6989438) length Control 67 NA 49.5 49.4, 49.6
Feliciano 0-6 mo Weight
10
6mo Vit D 400 IU 12 g nd 3745 2613, 4877 -463 -1852, 926(;
1994
36
gain born
Vit D 200 IU 13 nd 5296 4718,5874 1088 96,2080 NS
[8078115] in spring,
Vii D 100 IU 17 nd
N. ChinaA
4208 3402, 5013
Length
10
6 mo Vii D 400 IU 12 nd 18.8 17.4, 20.2 -0.5 -2.7, 1.7c NS
c
em
gain born Vii D 200 IU 13 nd 19.0 18. 1 19.9 -0.3 -2.2, 1.6c
in spring,
Vit D 100 IU 15 nd 19.3 17.6, 21.0
N. China
9 18 y Height
20
1 y Vit D3 2000 IU
nd,S34
% nd 5.6% -4.8, 6.4 -1.8% -0.6, 3.0
2006 female,
Vit 200 !U_ ..
total
nd 5.0% -4.2, 5.8 -1.2%
0.07
[16278262] premenarche Placebo nd 3.8% -0.9, 6.7
c
Weight
20
1 y Vii D3 2000 IU % nd 18.4% - 14.7 22.1c -3.5% - -1.3, 8.3c
_'!it D3 200 !!!__
nd,S34
nd 15.3% - 12.5, 18.1 -0.4
" c-
0.25
total
__ :_3.1.,_!?._ .
Placebo nd 14.9% - 11.8, 18.0
Wagner Lactating Infant 10
7 mo Mother (400)
10 NA
Final Diff
0.30
2006
39
mothers & weight
8
+infant {300}
g
7600 7100, 8100 -800 -2300, 700c
[17661565) infant Mother (6400)
9 NA 8400 7700, 9100
0-6 mo; 7 +infant 0
mo- 2 y Infant
10
7 mo Mother (400) Final Diff
c
length +infant (300}
10 em NA
65.5 64.4, 66.6 -3.8 -7.8, 0.2c
0.06
---------
Mother (6400)
9 NA 69.3 67.4, 71.2
+infant 0
Marya Pregnant Birth
12
Delivery Vii D 1.2 mil
100 NA
Final Diff
<0.001
1988
37
women & weight IU total
g
2990 2920,3060 +190 90,290
---------
India infant 06 mo No
100 NA 2800 2730, 2870
[3243609) su Iemen!
c
Bi rth
22 Vit D 1.2 mil Final Diff
length IU total
100 em NA
50.06 49.7 50.4 +1 .6 1.1 2.1
<0.001
No
100 NA 48.45 48. 1, 48.8
su Iemen!
Marya Pregnant Birth 22 Delivery Vit D 1.2 mil
20 NA
Final Diff
0.001
1981
41
women & weight _ IU total
g
3140 2940 3340 +41 0 166 654c
[723935Q)E infant 0-6 mo Vit D 1200 IU
---------
Final Diff
+ 375 mg Ca 25 g NA
2890 2760, 3020 +160 0, 320
0.05 c
(3'd
---------
No
75 NA 2730 2650,2810
su lement
Continued
45
Author Year
Study Name
~ M I ]
Life Stage
Pregnant
women &
infant 0-6 mo
Outcome
Birth
weight
1/2
Mean
Follow up
20
delivery
Interventions,
Daily Dose
No.
Analyzed
46
Uni t Baseline
Change
{SO)
Change
95% CI
Net
Diff
Diff
+160
Net Diff
PBtw
Study
95% CI Quality
NS c
"NO-NM .. MO __ ,,MOM-"0
Table 7. Vitamin D and growth outcomes: Results of cohort studies
Author Year
Study Name
PMID
2006
4
Australia
[16352684]
Gale 2008
PAHSG, UK
[1 7311 057]
A Nonadjusted
Life Stage
Pregnant
women;
infant 0-6 mo
Pregnant
women;
infant 0-6 mo
Pregnant
women;
infant 0-6 mo
Outcome
(n/N; Incidence)
Birth weight
(N=374)
Birth length
(N=374)
Birth weight
(N=466)
Weight at 9 mo
(N=440}
Weight at 9 y
(N=178)
Birth length (N=466)
Length at 9 mo
(N=440)
Height at 9 y
(N=178}
Followup
Duration
Delivery
Delivery
Delivery
9mo
9y
Delivery
9 mo
9y
Maternal 25(0H)D concentration,
nmoi/L
<28 at 28-32 wk
No. in
Category
Final
value
27 3397 g
............................................................... ................................................
at 28-32 wk 347 3555
<28 at 28-32 wk 27 49.8 em
at 28-32 wk 347 50.4
<30 (Quartile) nd 3.38 kg
I49 :
50-75 nd 3.49
> 75 ;;;:r.. 3:43 ................
<30 nd 15.9
Final
so
57
52
2.7
2.4
0.46
0.56
1.57
0.51
1.14
j$..?. : 1.26
50-75 nd 16.1 1.34
>75 ;;d........................... .................1 ..i5:'9... 1.09
<30 nd 27.4 kg 1.19
?$..4. : 1.21
50-75 nd 30 1.20
> 75 ;;d........................... ................29.:':3" 1 .1 9
<30 nd 50 em
------:::370--= 570_____ nd 50 .
50-75 ;;CI........................... .................so:s
------='::'=''------ ............................................................... ................................................
>75 nd 50.1
<30 nd 71 .2 em
-----....,3=-= o,...,-5=-=o =------ nCi 71:4
_____
>75 nd 71.1
<30 nd 129.6 em
1.83
2.29
2.25
2.09
2.85
2.60
2.89
2.67
5.88
------:::3-=- o--= 5-=- o----- nCi i3T5 . 6.66
-----""' 5"=o-='=7"" 5 _____ 5.o9
>75 nd 130.6 6.45
47
p
value
NS
NS
0.58
0.10
0. 15
0.86
0. 19
Study
Quality
B
c
Vitamin D and Cardiovascular Disease
Synopsis.
No qualified systematic reviews have evaluated the association between vitamin D intake or
serum 25(0H)D concentrations and incidence of hypertension. One RCT of almost 2700 elderly
British who received either vitamin D
3
100,000 IU every 4 months or placebo for 5 years found
no statistically significant difference in event rates for various cardiovascular outcomes,
including total events and cardiovascular deaths. No effects were also found in subgroup
analyses of men and women. Three cohort and one nested case-control studies have analyzed the
association between serum 25(0H)D concentrations and cardiovascular outcomes
(cardiovascular events, nonfatal myocardial infarction or fatal coronary heart disease,
cardiovascular death, myocardial infarction, and stroke). Significant associations were found
between progressively lower 25(0H)D concentration and progressively increased risk of
cardiovascular events in two studies of people approximately 40 to 75 years old. No significant
associations were found between serum 25(0H)D concentrations and cardiovascular death,
myocardial infarction, or stroke in one study each.
Detailed presentation (Tables 8, 9, I 0 & 11; Figure 6).
Total cardiovascular events.
Total cardiovascular events were evaluated by an RCT,
44
the Framingham Offspring Study
(FOS),
45
and a nested case-control study derived from the Health Professionals Follow-up Study
(HPFS).
46
The RCT found no significant effect of vitamin D; both cohort studies found
significant associations between lower serum 25(0H)D concentrations and increased rates of
outcomes.
The RCT randomized almost 2700 elderly participants (65-85 years) from the general
population in Ipswich, UK (52 N) to vitamin D
3
100,000 IU every 4 months or placebo.
44
After
5 years, 36 percent of the participants had a cardiac or cerebrovascular event, but there was no
statistically significant difference between those taking vitamin D or placebo. Similar results
were found in subgroups of men and women. The RCT was rated quality B primarily due to
inadequate verification of outcomes.
The FOS cohort evaluated 1739 men and women with no history of cardiovascular disease
and a mean age of 59 years (based on the standard deviation, with an approximate rage of 41 to
77 years).
45
After 5.4 years, 6.9 percent had a cardiovascular event (including myocardial
infarction, coronary insufficiency, angina, stroke, transient ischemic attack, claudication, and
heart failure). Overall, the methodological quality of the study was A; though their secondary
analysis of three categories of serum 25(0H)D concentrations (as opposed to two categories)
was rated C due to incomplete reporting and lack of adjustment for important variables including
season of blood draw. In their primary analysis, people with serum 25(0H)D concentrations less
than 37.5 nmol!L were 70 percent more likely (P=0.02) to have a cardiovascular event. In their
secondary analysis, those with 25(0H)D concentrations between 25 and 37.5 nmol/L were about
50 percent more likely (P=O.Ol) to have an event than those with higher concentrations.
Furthermore, a rnultivariable analysis of continuous 25(0H)D concentrations suggested
increased likelihoods of cardiovascular events in those with 25(0H)D concentrations below
approximately 50 to 55 nmol/L.
48
In a nested case-control study of the HPFS, 454 men 40 to 75 years old with no
cardiovascular history who had a nonfatal myocardial infarction or coronary heart disease death
over a 10 year period were matched with 1354 controls.
46
The methodological quality of the
analysis was A, although due to limitations on analyzable serum, the investigators had to use a
case-control analysis instead of a complete analysis of all eligible men in the HPFS. Across four
categories of men based on their serum 25(0H)D concentrations, lower concentrations were
significantly associated with increased cardiovascular events (trend across categories P=0.02).
Compared with men who had 25(0H)D concentrations above 75 nmol/L, those with 25(0H)D
concentrations 56 to 75 nmol/L had an adjusted relative risk (RR) of 1.6 (95 percent CI 1.1, 2.3),
those with 25(0H)D 37.5 to 56 nmol/L had an RR of 1.4 (95 percent CI 0.96, 2.1), and those
with 25(0H)D below 37.5 nmol/L had an RR of2.1 (95 percent CI 1.2, 3.5).
Cardiovascular death.
The British RCT ofvitamin D3l OO,OOO IU every 4 months versus placebo analyzed
cardiovascular death as a primary outcome; 8 percent of the participants had cardiovascular
deaths within 5 years.
44
Fewer people taking vitamin D
3
supplements had cardiovascular deaths
(RR = 0.84), but this finding was not statistically significant (95 percent CI 0.65, 1.10). Similar
results were found in subgroups of men and women.
An analysis ofNHANES III (methodological quality C) evaluated cardiovascular death (due
to hypertensive disease, ischemic heart disease, arrhythmia, heart failure, cerebrovascular
disease, atherosclerosis or other disease of the arteries) in over 13,000 men and women
regardless of baseline medical history.
47
During almost 9 years of followup, 5.8 percent bad a
cardiovascular death. The analysis compared four categories of serum 25(0H)D concentrations
ranging from less than 44.5 nmoi/L to more than 80 nmol/L. No significant association was
found between serum 25(0H)D concentration and cardiovascular death.
Ischemic heart disease.
The RCT evaluated total ischemic heart disease.
44
In this elderly British population, 17
percent had an ischemic heart disease event; no effect of vitamin D
3
supplementation was found.
Similar results were found in subgroups of men and women.
Ischemic heart disease death.
The RCT evaluated total ischemic heart disease death as a primary outcome.
44
In the trial, 3.4
percent had an ischemic heart disease event; no effect of vitamin D3 supplementation was found
(RR = 0.84 [95 percent CI 0.56, 1.27]). Similar results were found in subgroups of men and
women.
Myocardial infarction.
In one small analysis, 755 elderly (age 65 to 99 years) Finnish men and women, regardless of
cardiovascular history, were evaluated on the basis of myocardial infarction (methodological
quality C due to lack of reporting of relevant data including information on the serum 25(0H)D
or 1,25(0H)2D concentrations within the tertiles).
48
During 10 years of followup, 17 percent of the participants had a myocardial infarction. Both
analyses of serum 25(0H)D and 1 ,25(0H)
2
D concentrations found no significant association
with risk of myocardial infarction.
49
Stroke.
The RCT evaluated total cerebrovascular disease.
44
In this elderly British population, 7.7
percent had a cerebrovascular event; no effect of vitamin D3 supplementation was found. Similar
results were found in subgroups of men and women.
Stroke was evaluated in the same small Finnish study. During 10 years offollowup, 9.3
percent of the participants had a stroke. Both analyses of serum 25(0H)D and 1 ,25(0H)
2
D
concentrations found no significant association with risk of stroke.
Cerebrovascular death.
The RCT evaluated cerebrovascular disease death as a primary outcome.
44
In the trial, 2.0
percent had a fatal stroke; no effect of vitamin D
3
supplementation was found. Similar results
were found in subgroups of men and women.
Findings per vitamin D concentration.
The RCT compared vitamin D
3
supplementation 100,000 IU every 4 months with placebo,
but found no effect on cardiovascular outcomes. Two cohort studies found a significant
association between higher serum 25(0H)D concentrations and lower risk of combined
cardiovascular events. Both found that those people in the highest 25(0H)D category analyzed
within each study had the lowest risk. The FOS used a maximum threshold of37.5 nmol/L; the
HPFS used a maximum threshold of75 nmol/L. The FOS provided a graphic representation of a
multivariable regression of continuous 25(0H)D concentrations (Figure 2 in the study).
45
The
risk of cardiovascular events rose below 37 to 50 nmoi/L serum 25(0H)D concentration. The
Finnish cohort did not report the range of serum 25(0H)D and 1,25(0H)2D concentrations.
48
Findings per age and sex.
The single RCT included elderly people from the general population. No effects on various
cardiovascular events were found. Subgroup analyses of men and women yielded similar
fmdings. The four cohort studies included adults across the full age range. Three of the cohorts
included about half men and women; one included only men. None evaluated potential
differences in associations based on age or sex, but no differences were evident across studies.
Findings by life stage.
0-6 mo Not reviewed
7 mo- 2 y Not reviewed
3-8 y Not reviewed
9-18 y Not reviewed
19-50 y For cardiovascular events, only a minority of evaluated participants were
within this life stage (almost all above 40 years). The NHANES III study, which found
no association between serum 25(0H)D concentration and cardiovascular death, included
largely people within this life stage.
51 - 70 y The majority of people investigated for the association between serum
25(0H)D concentration and cardiovascular events were within this life stage. Significant
associations were found between lower serum 25(0H)D concentrations and increased
rates of cardiovascular events, across a range of 25(0H)D concentrations. The NHANES
III study likely included many people within this life stage; no association was found
with cardiovascular death.
~ 7 y The majority of participants in the British RCT included men and women
within this age group. Vitamin D supplementation was not found to have an effect on
50
Postmenopause Only the RCT provided data on a subgroup that included only
postmenopausal women. No effect of vitamin D3 supplementation was found.
Pregnant & lactating women Not reviewed
Table 8. Vitamin D and cardiovascular outcomes: Characteristics of ACTs
Author Year
Study Name
Location
(Latitude)
[PMID]
Trivedi 200
Ipswich, UK
(52N)
[12609940)
Population
Health
status
Mean
age
(range), y
Male (%)
General
population
75 (65-85)
76%
Background
Calcium Intake &
Vitamin D Data
742 mg/ day (at 4
years, no difference
by treatment
allocation}
51
Comparisons
Vi! 03 100,000 IU
vs placebo every 4
months
Compliance
76% with at least 80%
compliance; 66% at last
dose (80% if excluding
deaths}
Comments
Tabl e 9. Vitamin D and cardiovascular outcomes: Results of RCTs
Author Year
Age
Outcome
Study Name
Range,
Outcome 1/2
Mean Interventions, n N
Metric Resul t 95%CI
p
Study
[ PMID]
Sex Follow up Daily Dose Event Tot al
(Compari son)
Btw Quality
(Subgp)
Trivedi 200
44
65-85 y, CVO, total
20
5y Vit 03100,000 IU
477 1345
Age adj RR
0.90A 0.77, 1.06 0.22
[12609940) Both ~ m o
......................................
(Vit 0/Piacebo)
Placebo 503 1341
IHO, total
20
Vit 03 224 1345
Age adj RR
0.94A 0.77, 1.15 0.57
......................................
(Vit 0/Piacebo)
--
Placebo 233 1341
------]
CeVO,
20
Vit 0
3 105 1345
Age adj RR
1.02A 0.77, 1.36 0.87
total
......................................
(Vit 0/Piacebo)
Placebo 101 1341
B
CVO death
10
Vit 03 101 1345
Age adj RR
0.84A 0.65, 1.10 0.20
......................................
(Vit 0/Piacebo)
......................................
Placebo 117 1341
IHO death
10
Vit 03 42 1345
Age adj RR
0.84A 0.56, 1.27 0.41
......................................
(Vit 0/Piacebo)
- - -------.
Placebo 49 1341
CeVO
10
Vit 03 28 1345
Age adj RR
1.04A 0.61' 1.20 0.89
death
......................................
(Vit 0/Piacebo)
Placebo 26 1341
-----r
A
Similar results for subgroups of men and women
52
Table 10. Vitamin D and cardiovascular outcomes: Characteristics of cohort studies
Confounders/Effect Modifiers
Author Year
Adjusted
Study Name
Q)
Specific
.t::
:5
Location Population Vitami n D Concentration Comparisons
c..
CVD
Ill
f!
"'
(Latitude) 'E
c..
iii
0
Q)
Outcomes
Cl 0 c.. >.
[PMID]
~
0
... u )(
u;
E
.t::
'5
Q)
'S Q) 'E Q)
>
.!
z Q
ct :: ~ ::i
Wang 2008
45
Health No Assay RIA Outcome
xA
X X X
xA
X CVD event
Framingham status CVD method (DiaSorin) stratified by 2
Offspring
Mean 59 (9) or 3
Framingham, age categories
MA (mostly)
(SD), y
(42N)
Male 45 Season All
[18180395]
{%) blood drawn
Giovannucci Health No Dietary RIA (Holl is Outcome X X X X X X Nonfatal
2008
46
status CVD assessment 1993) stratified ~ 4 Ml or fatal
HPFS
Mean 64 method categories CHD
us age (40-75)
(various) (range),
[18541825) y
Male 100 Internal All
(%) validation?
In
Melamed Health Any Assay RIA Outcome X X X X X X CVD death
2008
47
status method (DiaSorin) stratified by 4
NHANES Ill
Mean 45 categories
us age (2:20)
(various) (range),
[18695076] y
Male 46 Season All (even
(%) blood drawn distribution)
Marniemi Health Any Assay RIA Outcome X X Ml
2005
48
status method (lncstar) stratified by Stroke
Turku,
Mean 79 terti les
Finland age (65-99)
(60N) (range),
[15955467) y
Male 48 Season All
(%) blood drawn
A
Not in 3-category analysis
B
Case-control study
53
Tabl e 11. Vitamin D and cardiovascular outcomes: Results of cohort studies
Author Year Age
Followup
Study Name Range,
Outcome Duration Vit D Concentration, No. of No. in Adjusted
95% CI
P for Study
[ PMID] Sex
(n/N; Incidence) (Time to Measure nmoi/L Cases Category OR Trend Quality
Dx)
CVD Events
Both Sexes
Wang 2008 Mean
Framingham (SO) CVD event (120/ 1739;
5.4 y 25(0H)D <37.5 50 481 1.70 1.08, 2.67* Q.Q2A A
Offspring 59 (9), 0.069)
[18180395) Both
-----------
~ 3 7 5 70 1258 1 Reference
<25 nd nd
----------
1.80 1.05, 3.08* 0.01 c
25-37.5 nd
------------------
nd 1.53 1.00, 2.36*
~ 3 7 5 70 1258 1 Reference
Men
Giovannucci
Nonfatal Ml or fatal
2008
46
4075 y,
CHD (454 cases; 10 y 25(0 H)D S37.5 63 150 2.09 1.24, 3.54 0.02
6
C A
HPFS Men
[1 8541825]
1354 controls)
37.5-56.25 156 463 1.43 0.96, 2.13
56.25-75
---1s---
464 1.60 1. !Q. 2.32
>75 70 277 1 Reference
CVD Death
Both Sexes
Melamed
2008
47
~ 2 0 y, CVD death
8.7 y 25(0H)D <44.5 nd nd 1.20 0.87, 1.64 nd c
NHANES Il l Both (777/13,331; 0.058)
[18695076)
-----------
44.560.75 nd nd 0.88 0.69, 1.14
60.75-80.25 nd nd 0.83 0.65 1.07
>80.25 nd nd 1 Reference
Myocardial
Infarction
Both Sexes
Marniemi
65-99 y, Ml
2005
48
10 y 25(0 H)D nd nd -252 Reference nd c
[15955467)
Both (13on55; o.172)
------------
nd nd
-------------------
-252 0.99 0.64, 1.53
nd nd -252 0.77 0.47, 1.27
1,25(0H)2D nd nd -252 1 Rete renee nd
nd
, ____ .!]_Q _____ -252 1.05 0.68, 1.62
nd nd -252 0.82 0.52, 1.30
Continued
54
Author Year Age
Followup
Study Name Range,
Outcome Duration Vit D Concentration, No. of No. in Adjusted
95%CI
P for
[PMID] Sex
(n/N; Incidence) (Time to Measure nmoi/L Cases Category OR Trend
Dx)
Stroke
Both Sexes
Marniemi
65-99 y, Stroke
2005
48
10 y 25(0H)D nd nd -252 Reference nd
[15955467]
Both (70/755; 0.093)
..----------
nd
-----QQ----
- 252 1.13 0.62, 2.05
nd nd -252 1.00 0.51 ' 1.94
1,25(0H)2D nd nd -252 1 Reference nd
nd nd -252 0.63 0.37 ,J..,QL_
nd nd -252 0.41 0.22, 0.77"
Statistically significant (P<0.05)
A Multivariable Cox regression with continuous 25(0H)D and regression splines with nonlinear relationships suggests an increased hazard of CVD events at serum 25(0H)D
concentrations below approximately 50-55 nmoi/L. See Figure 2 on page 508 of article.
Study
Quality
c
6
Adjusted regression analyses found 0R=0.98 (0.96, 0.998) per 2.5 nmoi/L increase in 25(0H)D and risk reduction of -2.1% (-0.2%, -4.0%) per 2.5 nmoi/L increase in serum
25(0H)D concentration.
c In a subgroup analysis of participants on no cholesterol lowering drugs at baseline, comparing the highest serum 25(0H)D concentration category (>75 nmoi/L) to the lowest (s37.5
nmoi/L), adjusted RR=2.30 (1.33, 3.97).
55
Figure 6. Cardiovascular outcomes risk stratified by vitamin D concentration
2S(OH)D
p
concentration for
Study Category (nmol!ll trend Quality
CVO Events, Both Sexes
1
Framingham Offspring 2008 Cat 1&2 <37 0.02 A
(n=1739) Cat 3 (ref) >37
-
Cat 1 <25 O.ol c
Cat 2 25-37
Cat 3 (ref) >37
CVO Events, Men
HPFS 2008 Cat 1 <37 0.02 A
(n=4S4 cases, 1354 cont rols) Cat2 37 - 56
Cat 3 56 - 75
Cat 4 (ref) >75
CVD Death, Both Sexes
-
NHANES 111 2008 Cat 1 <45 nd c
(n=13,331) Cat 2 45-61
Cat 3 61 - 80
Cat 4 (ref) >80
-
Myocardial Infarction, Both Sexes
Marniemi (Finland) 2005 Tl (ref ) nd nd c
(n=755) T2 nd
T3 nd
-
Stroke, Both Sexes
Marniemi (Finland) 2005 T1 (ref ) nd nd c
(n=755) T2 nd
T3 nd
I I I
0.5 2 4
Decreased risk Increased risk
56
Vitamin D and Body Weight
We searched for systematic reviews and primary studies that evaluated associations between
vitamin D intake or body stores and incidence of overweight or obesity; no such studies were
found. For the outcome weight change (in kilograms or body mass index units), we included
only randomized controlled trials. The EPC and the TEP agreed that the limited resources would
not be expended on reviewing observational studies for the surrogate outcome body weight
(where overweight or obesity are considered to be the clinical outcomes). We included only
studies of adults. Studies of weight gain in children are included in the "Growth" section.
Synopsis.
No qualified systematic reviews have evaluated the association between vitamin D intake or
serum 25(0H)D concentrations and body weight in adults. Three RCTs from Finland, Norway,
and India compared different doses of vitamin D (300 IU daily, 20,000 or 40,000 IU weekly, or
120,000 IU every 2 weeks) to placebo, with or without supplemental calcium in both groups. The
study participants also varied: they were postmenopausal women, obese men and women, or
only obese men. In the Finnish and Norwegian studies, the participants on average, gained
weight in all groups over 1 or 3 years; in the Indian study weight remained mostly stable over 6
weeks. All studies found no difference in weight change with or without vitamin D
supplementation.
Detailed presentation (Tables 12 & 13 ).
Three RCTs ofvitamin D reported body weight (or body mass index [BMI]) as an outcome.
The Kuopio (Finland) Osteoporosis Risk Factor and Prevention Study (Kuopio ORFPS) included
postmenopausal women in a four-arm study.
49
Two of the study arms included hormone
replacement treatment and are not further discussed here. The remaining two arms compared
vitamin D
3
300 IU (83 women) versus placebo (95 women), where all women were taking low
dose calcium lactate 500 mg/d (equivalent to 93 mg Ca++/d). Women on cholesterol-lowering
medication at any point during the trial were excluded. The primary outcome of the trial was the
serum lipid profile. The women ranged in age from 47 to 56 years. After 3 years, women, on
average, gained weight in both study arms (about 1-2 kg). Those in the placebo arm gained an
absolute 1.5 percent more weight than those in the vitamin D arm, but the difference was not
statistically significant. The study had a methodological quality of C due to an uneven
distribution ofbody weights between study arms at baseline (means 71.5 and 67.6 kg) and an
overall withdrawal rate of over 30 percent.
The second trial was conducted in Norway among healthy overweight and obese women and
men. 5 The participants' mean baseline serum 25(0H)D concentration was 53 nmol/L. The trial
compared vitamin 0
2
40,000 IU weekly (116 participants completed), 20,000 IU weekly ( 106
participants), and placebo (112 participants). All study participants also took calcium carbonate
500 mg daily. Almost all participants complied with the vitamin D (or placebo). Changes in
weight and BMI were primary outcomes. The participants ranged in age from 21 to 70 years.
After 1 year, changes in weight were small (increases of 0.1-0.5 kg) in each trial group.
Compared to the placebo group, those taking the larger dose of vitamin D had less weight gain
than those taking the smaller dose, but none of the differences among study groups were
statistically significant. The study was rated methodological quality B, primarily due to the high
dropout rate (25 percent), which was not explained.
57
The third trial was conducted in New Delhi, India among healthy obese men. 5
1
The
participants' mean baseline serum 25(0H)D concentration was about 33 nmol/L. The trial
compared vitamin D3 120,000 given under supervised conditions every 2 weeks and placebo in
100 men, of whom 71 were analyzed; most dropouts occurred because of refusals for subsequent
blood draws (to assess the primary outcome). After 6 weeks, weight in kg and BMI were
essentially stable, with no difference in weight change between the interventions. The study was
rated methodological quality B because of the high dropout rate; for weight (in kg), the study
was of quality C because baseline weights were not reported.
Findings per vitamin D dose.
There was a lack of effect found across a range of doses from 300 IU to 8570 IU (prorated)
daily.
Findings per age and sex.
There was a lack of effect found in studies both of men mostly in their 40s, somewhat older
people of both sexes, and postmenopausal women.
Findings by life stage.
0- 6 mo Not reviewed
7 mo- 2 y Not reviewed
3-Sy
9-18 y
19-50 y
weeks.
Not reviewed
Not reviewed
No effect was found in one trial of men mostly within this life stage after 6
51 - 70 y The majority of people in the trials were within this life stage. No
significant effect was found on weight from vitamin D supplementation for 1 or 3 years.
~ 7 y No data
Postmenopause All the women in the Finnish trial were postmenopausal.
Pregnant & lactating women Not reviewed
58
Table 12. Vitamin D and weight : Characteristics of RCTs
Author Year
Background
Study Name
Calcium Intake
Location Population
& Vitamin D
Comparisons Compliance Comments
(Latitude)
Data
[PMID]
Heikkinen Health All, post- nd Vit 0
3
& Ca nd
1997
49
status menopause lactate vs
Kuopio
Mean 53 (47-56) Placebo & Ca
ORFPS age lactate
Kuopio, (range),
Finland
y
(63N)
Male 0
[9405029)
%
Sneve Health Healthy 25(0H)D Vit D3 40,000 IU The compliance rate for
2008
50
status overweight 53. 116.9 per week vs cholecalciferol/placebo
Troms0, and obese nmoi/L Vit 03 20,000 IU capsules were 95% in all 3
Norway Mean 48 (21 -70) Ca intake per week vs groups, and for the calcium
(70N) age 940398 mg/d Placebo tablets 81-85% across all 3
[19056900) (range), AII:Ca groups.
y carbonate 500
Male 36 mg/d
%
Nag pal
Health Healthy, 25(0H)D: 36.5 Vit 03 120,000 100% (implied); supervised Excluded
2009
51 status obese nmoi/L IU every 2 home visits subjects who
New Delhi,
Mean 44 (8) (treatment weeks vs refused
India
age group), 30.0 Placebo subsequent
(28SN)
(SD), y nmoi/L (control blood draws
[19125756)
Male 100% group)
(%)
59
Table 13. Vitamin D and weight: Results of ACTs
Author Year
Age
Interventions, Daily No. Net Net Diff 95%
p
Study Range, Mean
Unit Baseline Change Change 95% Cl
Quality
Study Name Outcome
10/20
Analyzed Diff Cl Btw Sex Follow up Dose
[PMID]
(Sub )
lsocaloric
Diet
Vit 0
3
300 IU + Ca
83 kg 71.5 +1 .84% +0.43%, +3.25% -1.5% 3.6%, +0.6o/oA NSB
47-56 y, . ___________
c Women
Weight
20
3y
Ca lactate 93 mg 95 67.6 +3.32% +1.73%,4.91%
Vit 0
3
40,000 IU weekly+
116 kg 101.0 +0.1 -0.6, +0.8 -0.4 -1.3, +0.5A NS
Ca carbonate 500 mg
Weight
10
1 y Vit Ds 20,000 IU weekly +
106 98.6 +0.3 -0.3, +0.9 -0.2 -1 .1 , +0.7A NS
Sneve
____ ............__ _ ____
100.6
--+0.5
-0.2, +1 .2
21-70 y,
Ca carbonate 500 mg 112
B 2008
50
Both
Vit 0
3
40,000 IU weekly +
116 BMI 35.0 0.0 -0.2, +0.2 -0.2 -0.6, +0.2A NS [ 19056900]
Ca carbonate 500 mg
BMI
10
1 y Vit Ds 20,000 IU weekly +
106 34.4 +0.1 -0. 1, +0.3 -0. 1 -0.4, +0.2A NS
__ .. ?.9.9. !!.lg _____
35. 1 +0.2
----
Ca carbonate 500 mg 112
Vii 0
3
120,000 IU every
35 kg nd +0.03 -0.6, +0.6 +0.42 -0.4, +1 .2 NS
c
Nagpal
Weight
20
6wk
---------------------
I
"j
2009
51
44 (8,
Placebo 36 nd -0.38
New Delhi, SO)
Vii 0
3
120,000 IU every
35 BMI 26.7 -0.02 -0. 2, +0.2 +0.02 -0.3, +0.3 NS
B
India Men
BMI
20
6wk 2wk
1
[ 19125756)
--J3Tace'bo---------------
36 26.0 -0.04 -0.3, +0.2
A
Estimated from reported data
B
Per estimated 95% confidence interval, P=0. 17
60
Vitamin D and Cancer
Cancer from all causes and total cancer mortality.
Synopsis.
No qualified systematic reviews have evaluated relationships between vitamin D and total
cancer incidence or mortality. One RCT showed no effect of combined vitamin D
3
(1000 IU/d)
and calcium (- 1500 mg/d) supplementation versus calcium supplementation (- 1500 mg/d) alone
on the risk of total cancer in healthy postmenopausal women (>55 years old) living in Nebraska
(latitude 41 N). Another RCT also found no difference in total cancer mortality or incidence
between supplemental vitamin D
3
(100,000 IU every 4 months) and placebo in elderly (71 +
years old) men and women living in the United Kingdom (latitude 52 N). Both RCTs were rated
B quality.
Analyses using NHANES III data (general adult populations living in the US) showed no
significant association between baseline 25(0H)D concentrations and total cancer mortality.
Detailed presentation (Tables 14, 15, 16 & 17).
A 4-year population-based RCT,
52
sampled from a 9 county, largely rural area in eastern
Nebraska (latitude 41 N), aimed to determine the efficacy of vitamin D
3
( 1000 IU/d) plus
calcium (either calcium citrate 1400 mg/d or calcium carbonate 1500 mg/d) or calcium alone
(either calcium citrate 1400 mg/d or calcium carbonate 1500 mg/d) compared to placebo in
reducing fracture incident. Only the comparison between the combined vitamin D and calciwn
versus the calcium alone groups is discussed here. The other comparisons are described in the
calcium and combined vitamin D and calcium sections. This study was rated methodological
quality B. Incidence of cancer was a secondary outcome of this trial. A total of 1179
postmenopausal women, aged more than 55 years old, were randomized. The mean 25(0H)D
concentration at baseline was 72 nmol/L. The relative risk of developing cancer at the end of
study was 0.76 (95 percent CI: 0.38, 1.55). On the hypothesis that cancers diagnosed early in the
study would have been present, although unrecognized on entry, the analyses were restricted to
women who were free of cancer at 1 year intervention. The relative risk of developing cancer at
the end of study for the vitamin D
3
plus calcium group changed to 0.55 (95 percentCI 0.24,
1.28).
Another 5-year RCT compared the effects of supplemental vitamin D3 (100,000 IU every 4
months) with placebo on total cancer mortality and incidence in 2686 elderly participants with a
mean age of75 years in the United Kingdom (latitude 52 N).
44
Total cancer mortality and
incidence were evaluated as two of multiple secondary endpoints. The primary endpoint was the
prevention of fracture. At 5 years vitamin D
3
supplementation had no significant effect on the
prevention of total cancer mortality (HR 0.86; 95 percent CI 0.61 , 1.20) or incidence (HR 1.09;
95 percent CI 0. 86, 1.36). This trial was rated B because it did not report in sufficient detail the
randomization method, and the outcome ascertainment was based on death certificates or self-
reported data, not verified with another objective documents (e.g., medical records or pathology
reports).
Reported in two publications (one was rated B and one was rated C), there was no
association between baseline 25(0H)D concentrations and total cancer mortality in the total
NHANES III study population
47
'
53
or in subgroup analyses by either season or latitude after a
median 9 years offollowup.
53
61
Findings by age, sex and/or ethnicity.
There were no differences in the total cancer mortality and incidence between men and
women, reported in a 5-year RCT compared the effects of supplemental vitamin D3 (1 00,000 IU
every 4 months) with placebo. In the NHANES III analysis, there was a suggestion of increased
risk of total cancer mortality in men whose baseline 25(0H)D were in the two highest categories
(80 to <100 nmoVL; 2: 100 nmol!L) compared to the reference category (<50 nmoVL) [80 to <100
nmoVL: RR = 1.21, 95 percent CI 0.83 to 1.78; 2: 100 nmol/L: RR = 1.35; 95 percent CI 0.78 to
2.31; P for trend=0.08]. However, this relationship was not seen in women (P for trend=0.12).
53
When racial/ethnic groups were considered separately, there was also no association between
baseline 25(0H)D concentrations and total cancer mortality in non-Hispanic whites (P for
trend=0.80), non-Hispanic blacks (P for trend=O.l4), or Mexican Americans (P for trend=0.37).
Findings by l ~ f stage.
0- 6 mo No data
7 mo- 2 y No data
3-8 y No data
9- 18 y No data
19- 50 y Analyses using NAHANES III data showed no significant association
between baseline 25(0H)D concentrations and total cancer mortality. NHANES III
included participants mostly wit hin this life stage.
51 - 70 y A proportion of participants in NHANES III were in this life stage, but no
unique conclusions are possible for this life stage separate from those for people 19 to 50
years.
2:71 y One RCT included elderly men and women mostly in this life stage. The
trial found no difference in total cancer mortality or incidence between supplemental
vitamin D3 (100,000 IU every 4 months) and placebo.
Postmenopause One RCT with healthy postmenopausal women showed no effect
of vitamin D
3
supplementation (1 000 IU/d) on the risk of total cancer.
Pregnant & lactating women No Data
62
Tabl e 14. Vitamin D and total cancer: Characteristics of RCTs
Author Year
Study Name Background
Location Population Cal cium Intake & Comparisons Compl iance Comments
(Latitude) Vitamin D Data
[PMI D]
Lappe o Health Mentally and 25(0H)O: 71.8 Vit 03 1000 IU/d + Ca nd
2007
52
status physically fit; nmoi/L (citrate 1400 mg/d or
Nebraska, US post- carbonate 1500 mg/d)
(41
2
N) menopause vs. Ca (citrate 1400
[17556697) o Mean 67 (7.3) mg/d or carbonate 1 500
age (SO), mg/d) vs. placebo
y
o Male 0
Trivedi 2003
44
(%)
o Health General 25(0H)O: 53.4 Vit 03 100,000 IU VS Participants Previous CVD:
Oxford, UK status population nmoi/L placebo every 4 months taking ;::80% of 28%, previous
(52"N) o Mean 75 (65-85) study cancer: 6%,
[12609940) age Calcium intake= medication: steroids user:
(range), y 742 mg/d (at 4 76"// 5%, and HRT
o Male 76% years, no taker: 7%
(%}
difference by
treatment
A
allocation}
No difference between the vitamin 0 and the placebo arm.
Tabl e 15. Vitamin D and t otal cancer : Characteri stics of cohort studies
Confounders/Effect Modifiers
Author Year
Adj usted
Study Name
Gl
Vitamin D
.r:
...
Location Popul ati on Comparisons
Q. :I
Comments
Concent ration
Ul
~
Ul
(Latitude) c
Q.
iii
0 Gl
Cl 0
Q.
>.
[ PMID]
~
0 ... CJ )(
u;
E
.r:
:g
Gl
'5 Gl c >
.!
z c
"'
:E ;:) ::::i
Cohort
Freedman o Health Any o Assay RIA Cancer X X X X X X Final model
2007
53
status method (DiaSorin) mortality includes sex,
NHANES Il l o Mean 44 stratified by race/ethnicity,
us age (;::17) prespecified and smoking
(various) (range), baseline pattern. Other
[1 6481636)
y
25(0H)O cut potential
o Male 45 o Season All
points confounders
(%) blood
were
drawn
examined but
not chosen.
Melamed o Health OM o Assay RIA Cancer X X X X X X
2008
47
status 7.4%, method (OiaSorin) mortality
NHANES Il l history stratified by
us of baseline
(various) CVD 25(0H}D
[18695076) 7.9%, quartiles
HTN
25%
o Mean 45
age ~ 2 0 )
(range},
y
o Male 46 o Season All
(%) blood
drawn
63
Table 16. Vitamin D and total cancer: Results of ACTs
Follow up, Interventions, Daily N
Outcome
p
Study
Life Stage Outcome
10/20
n
Metric Result 95%CI
y Dose Event Total
(Comparison)
Btw Quality
Lappe Post- Incident cancer (all
20
4 Vii 03 1000 IU + Ca 13 446 RR (Vii O+Ca 0.76 0.38, NS
2007
52
menopausal causes) (citrate 1400 mg or vs Ca) 1.55
women carbonate 1500 mg)
B
Nebraska, US Ca (citrate 1400 mg 17 445
(41
2
N) or carbonate 1 500
[17556697) m
Post- Incident cancer
20
4 Vit 0
3
1000 IU + Ca 8 403 RR (Vii O+Ca 0.55 0.24,1 28 NS
menopausal (restricted to subjects (citrate 1400 mg or vs Ca)
women who were free of carbonate 1500 mg)
B
cancer at 1 y Ca (citrate 1400 mg 15 416
intervention) or carbonate 1 500
mg)
Trivedi 2003
44
65-85 y. Both Incident cancer (all
20
5 Vit 03100,000 IU 188 1345 HR (Vit 0 vs 1.09 0.86, NS
[ 12609940) sexes causes) every 4 mo (-833 placebo) 1.36
B
IU/d)
Placebo 173 1341
Total cancer mortality
20
5 Vit 03100,000 IU 63 1345 HR (Vit 0 vs 0.86 0.61 , 1.2 NS
every 4 mo (-833 placebo)
IU/d)
Placebo 72 1341
64
Table 17. Vitamin D and total cancer: Results of cohort studies
Author Year
Study Name
[PMID]
Freedman 2007
53
NHANES Ill
us
[16481636]
Melamed 2008
NHANES Ill
us
(various)
[1 8695076)
Life Stage
Adults,
both sexes
Adults,
males
Adults,
females
Adults,
both sexes
Statistically significant (P<0.05)
Outcome
(n/N; Incidence)
Cancer mortality
(536/ 16818; 0.032)
Cancer mortality
(318n632; o.042)
Cancer mortality
(218/9163; 0.024)
Cancer mortality
(N=13331)
Follow up
Duration
(Time to Dx)
105 mo
105 mo
105 mo
Median 8.7 (lOR
7.1 10.2) y
25(0H)D,
nmoi/L
<50
No. of
Cases
175
No. in
Category
5744
Adjusted
HR
95% CI
Reference
50 to <62.5 103 3143 1.22 0.91, 1.64
_
1:02
8o to <1oo 8o 4218 (total, i :oo
- -------------
__ 41_ _ _____ 0.92 0.58, 1.46
2: 120 20 1:49
<50 88 1993 Reference
__ .. ........
2333 (total,
80 to <1 00 58 __ - 1::1
>1 00 44 1.35 0.78, 2.31
<50 87 3751 Reference
- - ---:-::-::-::--......................................................... .. .. .. .. .. .. .. .. .. .. ...
50 to <62.5 46 1682 1.40 0.94, 2.08
1:02 a:s2; i-:6:; -
8o to <1 oo
22
_ _
2: 100 17 0.78 0.40, 1.53
>80 nd nd Reference
65
P for
Trend
0.65
0.08
0. 12
nd
Study
Quality
B
c
Prostate cancer.
Synopsis.
No qualified systematic reviews have evaluated the association between serum vitamin D
concentrations and incidence of prostate cancer. Eight nested case-control studies (2B, 6C) found
no association between baseline serum 25(0H)D concentrations and the risk of prostate cancer.
One study rated C found a significant association between lower baseline serum 25(0H)D
concentrations (<30 compared to >55 nmol/L) and higher risk of prostate cancer (adjusted OR
1.8, lowest compared to highest quartile). The same study found that the prostate cancer risk was
increased in subjects less than 52 years at study entry and who had serum 25(0H)D
concentration less than 40 nmol/L (adjusted OR 3.5). However, there was no difference in risk
between low and high serum 25(0H)D concentration for those older than 51 years at study entry.
A C study suggested an U-shaped association between baseline serum 25(0H)D concentrations
and the risk of prostate cancer.
Detailed presentation (Tables 18 & 19; Figure 7).
A total of 12 nested case-control studies in 14 publications reported on the association
between baseline serum 25(0H)D concentrations and the risk of prostate cancer.
53
"
66
The number
of cases ranged from 61 to 749. The latitudes of the studies ranged from 21 N to 60 N. The
mean age of the subjects ranged from 44 to 68 years. Baseline serum concentrations of 25(0H)D
in these studies ranged from 12.8 to 194 nmol/L. The time between blood drawn and the
diagnosis of prostate cancer varied from 2 to 16 years. The methodological quality of three
studies was rated B and nine studies were rated C.
19-50 years.
Two studies grovided data on younger subjects. Ahonen et al. analyzed subjects from 40 to
57 years of age.
5
The study found that the prostate cancer risk was increased in subjects less
than 52 years at study entry and had low serum 25(0H)D concentration (:S40 nmol/L) (adjusted
OR 3.5, 95% CI 1.7, 7.0). The corresponding adjusted OR for those older than 51 years at study
entry was 1.2 and was not significant. This study adjusted for factors related to insulin resistance
syndrome but not those potentially related to prostate cancer.
Freedman et al. analyzed data from NHANES III and reported on subjects with a mean age
of 44 years and found that the adjusted relative risk of mortality from prostate cancer was 0.91
(95% CI 0.39, 2.14) in the group with baseline serum 25(0H)D concentration of at least 62.5
nmol/L compared to the group with less than 62.5 nmol/L.
53
51-70 years.
Ten studies reported data on subjects with a mean age ranged from 51 to 68 years. Eight
studies did not find an association by trend analysis between baseline serum 25(0H)D
concentrations and the risk of prostate cancer.
54
56
.
63
66
One study found no association between
baseline serum 25(0H)D concentrations and mortality from prostate cancer. 5
8
One study found
an association between lower baseline serum 25(0H)D concentrations ( <30 compared to >55
nmol/L) and the risk of prostate cancer (P for trend = 0.01).
55
The adjusted OR of the lowest
compared to highest quartile was 1.8. The study also found that the prostate cancer risk was
increased in subjects less than 52 years at study entry and had low serum 25(0H)D concentration
(:S40 nmol/L) (adjusted OR 3.5, 95 percent CI 1.7, 7.0). However, there was no difference in risk
(adjusted OR 1.2, P=NS) between low (:S40 nmol/L) and high (>40 nmol!L) serum 25(0H)D
66
concentration for those older than 51 years at study entry. This study did not adjust for factors
potentially relevant to prostate cancer. One study reported an U-shaped association between
baseline serum 25(0H)D concentrations and the risk of prostate cancer: the odds ratio in the
group with 25(0H)D concentration of at least 80 nmol/L was 1.7 (95 percent CI 1.1, 2.4)
compared to the group with a 25(0H)D concentration of 40-49 nmol/L; the odds ratio in the
group with 25(0H)D concentration of no more than 19 nmol/L was 1.5 (95 percent CI 0.8, 2.7)
compared to the group with a 25(0H)D concentration of 40 to 49 nmol/L.
64
Even though this
study used a conditional logistic regression in its analysis to maintain matching status, it was
unclear if additional factors potentially relevant to prostate cancer were also entered into the
regression analysis.
1,25(0H)2D.
Five studies reported on the association between 1,25(0H)
2
D serum concentrations and the
risk of prostate cancer. Four studies did not find an association.
59
62
63
66
One study found that the
risk of prostate cancer decreased with higher serum concentrations of 1 ,25(0H)
2
D in men with
low serum concentrations of25(0H)D (unadjusted OR 0.15, comparing 4th quartile of
1,25(0H)2D (104-211 pmol/L) to 1
51
quartile (13-68 pmol!L) in men with serum 25(0H)D
concentrations that ranged from 7.5-45 nmol/L).
58
When stratified by age and race, this
association was only found in men above the median age of 57 years at time of blood drawn but
not in younger men; the association was similar in black and white men.
Findings by life stage.
0 - 6 mo not applicable
7 mo - 2 y not applicable
3 - 8 y not applicable
9 - 18 y not reviewed
19- 50 y One study found that the prostate cancer risk was highest in subjects less
than 52 years at study entry and had low serum 25(0H)D concentration ~ 0 nmol/L)
(adjusted OR 3.5, 95 percent CI 1.7, 7.0). Another study analyzed data from NHANES III
and reported on subjects with a mean age of 44 years and found that the adjusted relative
risk of mortality from prostate cancer was 0.91 (95 percent Cl 0.39, 2.14) in the group
with baseline serum 25(0H)D concentration of at least 62.5 nmol/L compared to the
group with less than 62.5 nmol!L.
51 - 70 y Eight studies did not find an association by P for trend analysis between
baseline serum 25(0H)D concentrations and the risk of prostate cancer. One study found
an inverse association ofbaseline serum 25(0H)D concentrations (<30 compared to >55
nmol/L) and the risk of prostate cancer (adjusted OR 1.8, lowest compared to highest
quartile, P for trend = 0.01). This study found that the prostate cancer risk was increased
in subjects less than 52 years at study enhy and had low serum 25(0H)D concentration
~ 4 0 nmol/L) (adjusted OR 3.5, 95 percent CI 1.7, 7.0). However, there was no
difference in risk (adjusted OR 1.2, P=NS) between low (S40 nmol/L) and high (>40
nmol/L) serum 25(0H)D concentration for those older than 51 years at study entry. One
study reported an U-shaped association between baseline serum 25(0H)D concenhations
and the risk of prostate cancer: the odds ratio in the group with 25(0H)D concentration of
at least 80 nmol/L was 1.7 (95 percent CI 1.1, 2.4) compared to the group with a
25(0H)D concentration of 40-49 nmol/L; the odds ratio in the group with 25(0H)D
67
concentration of no more than 19 nmoVL was 1.5 (95 percent CI 0.8, 2. 7) compared to
the group with a 25(0H)D concentration of 40 to 49 nmoVL.
~ 7 y No study specifically targeted men older than 70 years.
Postmenopause Not applicable
Pregnant & lactating women Not applicable
68
Table 18. Vitamin D and cancer: Characteri stics of nested case-control studies
Confounders/Effect Modifiers
Adjusted
Author Year
Study Name .!::!
I!?
.r:.
Location Population 25(0H)D Comparisons c.
::::J U) Comments
U)
f!
U)
Ql
(Latitude)
'E
c.
(;j
0
Cl 0 c.
[PMID]
0
... ()
>< U)
E
.r:.
:0
Ql
'5 Ql 'E Ql
>
.S!
z c
"'
::E :::::> :.::i
Ahn Health 8% current Assay RIA Prostate X X X X
2008
54
status smoker (Heartland) cancer risk
PLCO Mean age 67.8 (5.3) stratified by
us (range/SO), baseline
(21
2
N to y 25(0H)O
44
2
N) Male(%) 100 Season nd quintiles
[18505967) blood
drawn
Platz 2004
63
Health Smoked Assay RIA Prostate X X X X X X 6%
Mikhak status 18%; OM cancer risk nonwhite
2007
61
3.6% stratified by
HPFS Mean age 66 (7) baseline
us (range/SO), 25(0H)O
(multiple y quartiles
latitudes) Male (%) 100 Season nd
[15090720) blood
[1 7440943] drawn
Freedman Health 28% Assay RIA Prostate X X X X X X 71% white;
2007
53
status current cancer 14% black;
NHANES Ill smoker mortality 6%
US (multiple Mean age 44 stratified by 2 Hispanics
latitudes) (range/SO), baseline
[17971526) y 25(0H) O
Male(%) 100 Season South: Nov categories
blood to Mar;
drawn North: Apr
to Oct
Tuohimaa Health Gemfibrozil Assay RIA Prostate X X
2004
64
status vs. placebo (l ncstar) cancer risk
Helsinki subjects stratified by 5
Heart Mean age <40 to >60 baseline
Vasterbotten; (range/SO), 25(0H) O
Janus y categories
Project ; Male(%) 100 Season nd
Finland blood
(60N) drawn
[14618623]
Li 2007
60
Health on ASA, 13- Assay RIA (Bruce Prostate X X 94%white
Gann 1996
66
status carotene, Hollis) cancer risk
PHS placebo stratified by
us trial; 9% baseline
(multiple current 25(0H)O
latitudes) smoker quartiles
[17388667) Mean age 58.9 (8.3)
[8850273) (range/SO),
y
Male (%) 100 Season 24% spring
blood or winter
drawn
Corder Health nd Assay Competitive Prostate X X 50% black;
1993
58
status protein- cancer risk 50% white
San Mean age 57 (38-81) binding compared by
Francisco (range/SO), (Haddad, baseline
us 1971l 25(0Hl0
-------
69
Confounders/Effect Modifiers
Adjusted
Author Year
Study Name
(,)
Q)
:c
...
Location Population 25(0H)D Comparisons 0.
:I U) Comments
U) co
U)
Q)
(Latitude)
c
... 0.
(;j
0
Cl 0 0.
[PMID]
0
... (,) )(
U)
E
.r.
'5
Q)
:; Q) c
Q)
>
.S!
z c
"'
::E
::;) :.::i
(372N)
Male (%) 100 Season nd
[8220092]
blood
drawn
continued
Ahonen Health Gemfibrozil Assay RIA Prostate X X X X X
2000
55
status vs. placebo (lncstar) cancer risk
Helsinki subjects stratified by
Heart Mean age 40-57 baseline
Finland (range/SO), 25(0H)O
(6oN) y quartiles
(11075874) Male (%) 100 Season Jan-Feb;
blood Mar-May;
drawn Se
Nomura Health 64% Assay Protein- Prostate X X X 100%
1998
62
status smoked binding cancer risk Japanese
Honolulu Mean age 58 (49-70) stratified by Americans
Heart (range/SO), baseline
us y 25(0H)O
(21
2
N) Male(%) 100 Season nd quartiles
(9794175] blood
drawn
Tuohimaa Health Gemfibrozil Assay RIA Prostate X X X
2007
65
status vs. placebo (lncstar) cancer risk
Helsinki subjects stratified by 3
Heart Mean age 51 (3.7) baseline
Finland (range/SO), 25(0H)O
(6oN) y categories
17301263 Male (%) 100 Season Most in
blood winter
drawn
Jacobs Health Selenium Assay RIA Prostate X X X X X
2004
59
status vs. placebo cancer risk
NPC subjectsA stratified by
Eastern US Mean age 68 (nd) baseline
(25
2
46'N to (range/SO), 25(0H)O
41
2
N) y tertiles
[15225833) Male(%) 100 Season nd
blood
drawn
Braun Health nd Assay RIA (Bruce Prostate X 100%
1995
57
status Hollis, cancer risk white
WCC, MD Mean age <45-75+ 1993) stratified by
us (range/SO), baseline
(39N) y 25(0H)O
[7612803] Male(%) 100 Season Aug quintiles
blood through
drawn Nov
Baron Health had >1 Assay Competitive Prostate X X X 5% black
2005
56
status colon protein- cancer risk
CPP adenoma binding stratified by
us removal (Quest) baseline
(multiple Mean age 62 (8.7) 25(0H)O
latitudes) (range/SO), tertiles
[15767334]
8
y
Male(%) 100 Season nd
blood
drawn
continued
70
Author Year
Study Name
Location Population
(Latitude)
[PMID]
Braun Health
1995
57
status
WCC, MO Mean age
us (range/SO),
(39N) y
[7612803] Male(%)
Baron Health
2005
56
status
CPP
us
(multiple Mean age
latitudes) (range/SO),
[15767334]
6
y
Male(%)
25(0 H)D
nd Assay RIA (Bruce
Hollis,
<45-75+ 1993)
100 Season Aug
blood through
drawn Nov
had >1 Assay Competitive
colon protein-
adenoma binding
removal (Quest)
62 (8.7)
100 Season nd
blood
drawn
A
For prevention of recurrence of non-melanoma skin cancer
6
This is a cohort study, not a nested case-control study.
71
Comparisons
Prostate
cancer risk
stratified by
baseline
25(0H)O
quintiles
Prostate
cancer risk
stratified by
baseline
25(0H)O
terti les
Confounders/Effect Modifiers
Adjusted
(,)
:c
0.
:I
Ill
0
0.
)(
Q)
111 Comments
X
Cl
0
E
Q)
c
X
X
>
::;)
X
Q)
Ill
.S!
:.::i
100%
white
5% black
Table 19. Vitamin D and prostate cancer: Results of nested case-control studies
Author Year
Study Name
PMID
Ahn 2008
54
PLCO
[8505967]
Platz 2004
Mikhak 2007
6
'
HPFS
[15090720)
[ 17440943)
Freedman
2007
53
NHANES Il l
[17971526)
Tuohimaa 2004
64
Helsinki Heart
[14618623)
Li 2007
PHS
[17388667)
Gann 1996
PHS
[8850273)
continued
Life
Stage
(male), y
51 -70
51-70
19-50
19-50
51 -70
19-50
51 -70
19-50
51 -70
Outcome (no. of
cases; no. of
control)
Prostate cancer
(741 ; 781)
Prostate cancer
(460; 460)
Mortality prostate
cancer
Prostate cancer
(622; 1451)
Prostate cancer
(492; 664)
Prostate cancer
(232; 414)
Prostate cancer;
age :>61 y
Prostate cancer;
age >61 y
Time to
diagnosis, y
2-8
2.2 (mean)
nd
s;9 -> 14 (range)
11 (median)
6 (mean)
25(0H)D concentration,
nmoi/ L
12.8-42.5
42.5-51.
51.4-60.5
...............................................
60.6-71.7
...............................................
71.8-129.5
Quartile 1A
Ouar:tiie2
Ouar:ti ie 3
...............................................
Quartile 4
<62.5
:2:62.5
No. of
cases
No. of
control
119 157
Adjusted
OR
____ ............................................................................
1t) _________ _______ _
......:..: 19:-:0:-----.1 .. ......................... ..................... .
......:..: 1 6"-;7,.---..J.5..t> ............................1 .. _______ ,_
148 155 1.18
109 114
---:- 11:-:5:--- _______ _
-----------------------
.....:::..94-'-=--- _1?..Q _________ ()]?. .............. .
142 113 1.19
22 nd
____ ............................................................. ..
25 nd 0.91
19 nd 1.5
20:39 ...............................................................................................,.. 1 6:-:9:----r;c:r----------1""3--
.................................
.....:2 =::2'=-9--.!1<:1. ........... J .................... .
...... _ __!1.<:1.................... .1:?. ________ _
:2:80 67 nd 1.7
15.7-53.3 nd nd 1.00
53.4-70.9 nd
..............................................
71 -93.5 nd
........................................
93.6-194 nd
95% CI
Reference
0.78, 1.56
1.10, 2.13*
0.95, 1.86
0.83, 1.68
Reference
0.67, 1.49
0.51' 1.15
0.79, 1.79
Reference
0.39, 2.14
0.8, 2.7
0.98, 1.6
Reference
0.9, 1.5
1. 1' 2.4*
0.71' 1.44
0.89, 1.80
0.71, 1.41
Reference
nd
nd
nd
0.56, 1.50
15.7-53.3 nd nd 1.00 nd
53.4-70.9
..............................................
71 -93.5
........................................
93.6-194
15.7-53.3
53.4-70.9
...............................................
71-93.5
........................................
93.6-194
nd
nd
nd
nd nd 1.00
____ ....................................................................... ..
nd ---'-"=--- nd ___J,Q() _______ _
nd ---'-"=--- .f1<.:1 ___________ _____ _
nd nd 0.76
72
nd
nd
0.73, 2.98
nd
nd
nd
0.39, 1.47
P for
t rend
0.20
0.59
0.95
0.91
0.82
nd
nd
Study
Quality
B
B
B
c
c
c
Author Year
Study Name
PMID
Corder
1993
58
[8220092)
Ahonen 2000
Helsinki Heart
[ 11075874)
Nomura
1998
62
Honolulu Heart
[9794175]
Tuohimaa 2007
Helsinki Heart
[1 7301263)
Jacobs
2004
59
NPe
[ 15225833)
Braun 1995
wee
[7612803)
Baron
2005
56
ePP
[ 15767334(
Life
Stage
(male), y
19 50
51 70
19-50
51-70
19-50
51 -70
19-50
51 -70
51 -70
19-50
51 -70
19-50
51 -70
*Statistically significant (P<0.05)
Outcome (no. of
cases; no. of
control)
Prostate cancer
(181; 181)
Mortality prostate
cancer
Prostate cancer
(1 49; 566)
Prostate cancer in
those <52 years
old at entry
Prostate cancer in
those >51 years
old at entry
Prostate cancer
(136; 136)
Prostate cancer
(132; 456)
Prostate cancer
(83; 166)
Prostate cancer
(61; 122)
Prostate cancer
(70 cases in a total
of 672}F
Time to
diagnosis, y
>5 (mode}
8-14 (mode)
16 (mean)
10.8 (mean)
5. 1 (mean)
14 (mean)
<4 (34%}
25(0H)D concentration,
nmoi/L
60.0 (case) vs. 50.5
(control) (est.)
nd
No. of
cases
181
51
48
No. of
control
181
nd
131
Adjusted
OR
1.8
95% CI
1.0, 3.2*
31=45.. 41 -143----------r.-4-------- o .8, 2.4
4r s4 o.5, 1.5
>55
34 144 Reference
:S40 nd nd 3.5 1.7, 7.0*
>40
-..,...-----------------------------
nd nd
S40 nd nd 1.2 0.7, 2.1
;46 ...............................................................................................-nd-:-----;:;c:r-------------------
<85 38 34 Reference
?.?.:1..9.1 ......::.;35,____ .................... _Q,_?. _________ 0.4, 1.8
....... ...1 .. 30 0. 8 0. 4' 1 . 7
33 34 0.8 0.4, 1.8
<40 1.88 1.15, 3.08*
------------------------------
...... ........................................................................................ _____ ,_,_,_,_,_,_,_,_,_,_,_, __ !_ ________ ,, Reference
1.25 0.64, 2.43
20-63.3
63.4-81.9
...............................................
82-149
<60.1
60.1 -73.8
...............................................
73.9-88.5
..............................................
..
>103
<62.9
62.9-84.9
..............................................
85
73
7 24
==1
......:,: 1 6,__ __ .... ....................................... ..3...... --------
4 25 0.6
.................................. ______ _
nd NA
---------------------- - - - - - -
......:.:;nd=--- _r::J!.\ .................. _:1:.?..? _______ _
nd NA 0.32
Reference
0.68, 4.34
0.29, 1.91
Reference
0.7, 7.8
0.7, 7.7
0.1 , 2.5
0.8, 8.2
Reference
0.66, 2.26
0.72, 2.43
P for
trend
0.01
0.68
0.51
0.60
0.70
Study
Quality
c
c
e
e
e
e
e
A Cut points separated by analytical run; season, distributions among control (see Table 3 in original study)
8
Cut points based on control standardized by season of collection
c Cut points based on total original cohort
Cut points based on control frequency
e Unadjusted
F This is a cohort study, not a nested case-control study
74
Figure 7. Prostate cancer risk stratified by vitamin D concentration
25(0H)D
p
concent ration for
Study Category (nmoi!L) trend Quali ty
-
Ahn 2008 Ql (ref) 13 - 43
0.20 B
(n=1 530) Q2 43 - 51
Q3 51 -61
Q4 61 -72
Q_ S _ 72 - l ll.._
--
Platz 2004 Q1 (ref) nd
0.59 B
(n=920) Q2
nd
Q3 nd
:-
Q4 nd
L
--
Tuohimaa 2004 Cat l <19 nd c
(n=2073) Cat2 20-39
Cat3 (ref) 40 - 49
Cat 4 50 - 79
CatS >80
Li 2007 Ql nd
=f
0.91 c
(n=11 56) Q2 nd
Q3 nd
Q4 (ref) nd
-
Ahonen 2000 Ql <30
--F
0,01 c
(n=715) Q2 31 - 40
Q3 41-54
Q4 ir_ef) >55
-
Nomura 1998 Ql (ref) <85
0.68 c
(n=272} Q2 85 - 101
Q3 102 - 119
Q4 >120
Tuohimaa 2007
r
--
Cat 1 <40 0.51 c
(n=S88} Cat 2 (ref) 40 - 59
Cat 3 >60
Jacobs 2004--
--
Tl (ref) 20 - 63
. l
nd c
(n=249) T2 63 - 82
T3 82- 149
Braun 1995 Ql (ref) <60. 0.60 c
(n=1 83) Q2 60 - 74
Q3 74 - 89
Q4 89- 103
QS >103
I I I I I I
0.1 0.2 0.5 2 s 10
Decreased ris k Increased risk
75
Colorectal cancer.
Synopsis.
No qualified systematic reviews have evaluated the association between 25(0H)D
concentrations and colorectal cancer mortality or incidence. One B quality RCT of elderly
population reported no significant difference in colorectal cancer mortality or incidence between
supplemental vitamin D
3
and no supplements. One B quality cohort study found an inverse
association between higher 25(0H)D concentrations and the risk of colorectal cancer mortality
(HR 0.28, highest compared to lowest tertile). Two B quality nested case-control studies of
women found a trend between higher 25(0H)D serum concentrations and lower risk of
colorectal cancer incidence (trend analysis). Another two B quality nested case-control studies of
men, and one B quality and t\vo C quality nested case-control studies of both sexes reported no
significant association between 25(0H)D concentrations and risk of colorectal cancer or colon
cancer.
Detailed presentation of supplemental vitamin D and colo rectal caner (Tables 20 & 21 ).
An RCT compared supplemental vitamin D3 (100,000 IU every 4 months) with placebo in
2686 elderly participants with a mean age of75 years in the United Kingdom (latitude 52 N).
44
Colorectal cancer mortality and incidence were evaluated as two of multiple secondary
endpoints. The primary endpoint was the prevention of fracture. At 5 years vitamin D
3
supplementation had no significant effect on the prevention of colorectal cancer mortality
(P=0.33) or incidence (P=0.94). This trial was rated B because it did not report in sufficient
detail the randomization method, and the outcome ascertainment was based on death certificates
or self-reported data, not verified with another objective documents (e.g. , medical records or
pathology reports).
Findings per age and sex.
The same British trial reported no significant difference in colorectal cancer mortality or
incidence between the vitamin D supplements group and the placebo at 5 years in men (P=0.96
and 0.59, respectively). In women, the trial also found no significant difference in colorectal
cancer incidence between the two groups (P=0.32), whereas the risk of colorectal cancer
mortality in the supplements group was significantly decreased compared to the placebo (0/326
deaths vs. 4/323 deaths; HR, not reported; P=0.04).
Findings per special populations.
No subgroup data were available regarding special populations (e.g. , obese participants,
smokers, ethnic groups, or users of contraceptives).
76
Table 20. Vitamin D and colorectal cancer: Characteristics of ACTs
Author Year
Study Name
Location
(Latitude)
[PMID]
Trivedi
2003
44
Oxford, UK
{52N)
[12609940]
Population
Health General
status population
Mean 75 (6585)
age
(range), y
Male 76%
'%l
Background Calcium
Intake & Vitamin D
Data
25(0H)D: 53.4 nmoi/L
Calcium intake= 742
mg/day (at 4 years, no
difference by
treatment allocation)
CVD =cardiovascular disease; HRT =hormone replacement therapy.
A No difference between the vitamin D and the placebo arm.
77
Comparisons
Vii 0
3
100,000 IU vs
placebo every 4
months
Compliance Comments
Participants Previous CVD: 28%,
taking <::80% previous cancer: 6%,
of study steroids user: 5%,
medication: and HRT taker: 7%
76%A
Tabl e 21. Vitamin D and colorectal cancer: Results of ACTs
Author Year
Age
Outcome
Study Name
Range,
Outcome
10/20
Mean Interventions, n N
Metric Resul t 95%CI
p
Study
[PMID]
Sex Followup Dally Dose Event Total
(Compari son)
Btw Quality
(Subgp)
Trivedi 2003
44
65-85 y, CRC,
20
5y Vit 0
3
100,000 IU
7 1345
Age adj HR
0.62 0.24, 1.60 0.33
B
(12609940) Both sexes mortality every 4 mo (Vii 0/Piacebo)
...................................... .................................._
Placebo 11 1341
CRC,
20
Vii 03 28 1345
Age adj HR
1.02 0.60, 1.74 0.94
incidence
......................................
(Vit 0/Piacebo)
Placebo 27 1341
r
65-85 y, CRC,
20
5y
Vit 03 7 1019
Age adj HR
0.97 0.34, 2.78 0.96
Men mortality
......................................
(Vii 0/Piacebo)
Placebo 7 1018
CRC,
20
Vit 03 25 1019
Age adj HR
1.18 0.65, 2.12 0.59
incidence
......................................
(Vii 0/Piacebo)
Placebo 21 1018
----- ,
65-85 y, CRC,
20
5y
Vit 0
3 0 326
Age adj HR
NA NA 0.04
Women mortality
......................................
(Vit 0/Piacebo)
......................................
Placebo 4 323
------y
CRC,
20
Vii 03 3 326
Age adj HR 0.49 0.12, 1.98 0.32
incidence
......................................
(Vii 0/Piacebo)
......................................
Placebo 6 323
78
Detailed presentation of25(0H)D concentrations and colorectal cancer (Tables 22 & 23;
Figures 8, 9, & 10).
A total of seven nested case-control studies evaluated the associations between 25(0H)D
concentrations and risk of colo rectal cancer
67
-
71
or colon cancer.
72
'
73
The number of pairs of cases
and controls in these studies ranged from 101 to 588. Another cohort study comprising 16,818
adult community volunteers from the NHANES III
53
assessed the association between 25(0H)D
concentrations and colorectal cancer mortality. The mean age of the subjects ranged from 44 to
66 years. Locations of the studies ranged from 20 N to 60 N. Baseline 25(0H)D concentrations
ranged from 10 nmol/L to 227.5 nmol!L. No studies reported followup 25(0H)D concentrations.
Time between blood drawn and the diagnosis of colorectal cancer incidence or mortality ranged
from less than 1 year to 17 years. None of the studies reported power calculations.
Methodological quality of five nested case-control studies
67
-
71
were rated B and two were rated
C.
72
'
73
Common reasons for downgrading the quality ratings included exclusion of participants
without available blood samples, no verification of cancer diagnosis, and lack of adequate
statistical adjustments. The cohort study
53
was rated B because it was unclear whether cases were
verified and there was no statistical adjustment for family history.
Findings per age and sex.
The NHANES III
53
analyzed data for both sexes combined. An adjusted analysis found an
inverse association between 25(0H)D concentrations and the risk of colorectal cancer mortality
(HR: 0.28, highest [2:80 nmol/L] compared to lowest tertile [<50 nmol/L]; P for trend= 0.02).
Two studies from WCC reported colon cancer incidence for both sexes combined.
72
'
73
One study
reported a significantly lower 25(0H)D concentrations in colon cancer cases than controls (58.9
nmol/ L vs. 86.6 nmol/L; P<0.001).
73
Both studies reported no significant association between
25(0H)D concentrations and colon cancer risk by trend analysis.
Three studies, from the Japan PHC, HPFS, and A TBC respectively, provided data on adult
men.
67
-
69
None of the studies found an association between 25(0H)D concentrations and
colorectal cancer risk. Although all three studies provided data on colon cancer and rectal cancer
as subgroup analysis, only HPFS reported a significant trend between higher 25(0H)D
concentrations and lower risk of colon cancer (OR 0.46, highest [median 97.0 nmol/L] compared
to lowest quartile [median 48.3 nmol/L]; P for trend= 0.005).
69
The HPFS also reported a
subgroup analysis on men aged 65 years or older.
69
No significant association was reported
between 25(0H)D concentrations and colorectal cancer risk by trend analysis.
The Japan PHC and HPFS compared 25(0H)D concentrations between colorectal cancer
cases and controls.
68
'
69
Neither reported a significant difference. One study explored subgroup
analyses. Only the rectal cancer cases had significantly lower 25(0H)D concentrations compared
to the controls (55 nmol/L for cases vs. 110 nmol/L for controls; P = 0.005).
68
Two nested case-control studies from the NHS and Japan PHC provided data on adult
women.
68
'
70
The NHS reported a trend between higher 25(0H)D concentrations and lower
colorectal cancer risk (OR 0.53, highest [median 99.1 nmol/L] compared to lowest quintile
[median 40.2 nmol/L]; P for trend= 0.02).
70
This trend remained significant in a subgroup
analysis of women age 60 years or older (OR 0.35 between the highest quintiles [median 99.1
nmol!L] and lowest [median 40.2 nmol!L]; P for trend= 0.006) or in rectal cancer alone (OR
0.31, highest [median 92.4 nmol/L] compared to lowest tertile [median 44.4 nmol/L]; P for trend
= 0.03).
70
The WHI focused on postmenopausal women.
71
A significant trend was reported
79
between higher 25(0H)D concentrations and lower colorectal cancer risk (OR 2.53, between
highest [2:58.4 nmol!L] and lowest quintiles (<31.0 nmol/L]; P for Trend= 0.02).
The Japan PHC compared 25(0H)D concentrations between cases and controls; no
significant difference was reported.
68
Findings per special populations.
No subgroup data were available regarding the association between 25(0H)D concentrations
and colorectal cancer risk in obese persons. One study exclusively included male smokers aged
between 50 and 69 years,
67
and reported no significant association between 25(0H)D
concentrations and colorectal cancer risk by trend analysis. Another study that exclusively
included white population also found no association.
72
In addition, another study that focused on
women who were taking hormone replacement therapy reported no significant association
between 25(0H)D and colorectal cancer.
70
Findings excluding early cases.
Three studies performed sensitivity analyses on the association between 25(0H)D
concentrations and colorectal cancer risk by excluding cases diagnosed within the first 1 to 2
years after blood draw.
67
69
70
One study found a significant association between higher 25(0H)D
concentrations and lower colon cancer risk (OR 0.3, between highest [>48.2 nmoVL] and lowest
quartiles [:S 24.5 nmol/L]; P for Trend= 0.04), which was not significant in main analysis.
67
Otherwise, the results were not materially different from the main analysis.
Findings on 1,25-Dihydroxyvitamin D.
A total of three studies evaluated the associations between 1,25(0H)
2
D concentrations and
colorectal cancer risk
67
'
70
or colon cancer.
73
None of the studies found a significant association
by trend analysis. One study reported no significant association between 1,25(0H)2D
concentrations and rectal cancer risk.
67
Findings by life stage.
0 - 6 mo Not reviewed
7 mo - 2 y Not reviewed
3 - 8 y Not reviewed
9-18 y Not reviewed
19- 50 y The analysis of the NHANES III with a mean age of 44 years included
participants mostly within this life stage. The study found an inverse association between
25(0H)D and colorectal cancer mortality.
51 - 70 y The seven nested case-control studies included people with a mean age
ranged from 55 to 66 years. A trend between higher 25(0H)D concentrations and lower
colo rectal cancer risk was found in two studies of women. Out of five studies that
separately assessed the tisk of colon cancer and rectal cancer, only one study of men and
another study of women found trends between higher 25(0H)D concentrations and lower
ri sks of colon cancer and rectal cancer, respectively. Otherwise, no association was found
between 25(0H)D concentrations and cancer risk.
2:71 y One RCT with a mean age of75 included participants mostly within this
life stage. The trial found no difference in colorectal cancer mortality or incidence
between supplemental vitamin D and no supplements.
80
Postmenopause One study and a subgroup analysis in another study focused on
postmenopausal women. A trend between higher 25(0H)D concentrations and lower
colorectal cancer risk was found in these two studies.
Pregnant & lactating women Not reviewed
81
Table 22. Vitamin D and colorectal cancer: Characteri stics of observational studiesA
Confounders/Effect Modifiers
Adjusted
Author Year VI
Study Name
Ql E
Vitamin D
.1:.
...
Ql
Location Population Comparisons
c.
:I
E
Concentration
VI
f!
VI
(Latitude) E
c.
(ij
0 Ql
E
Cl 0 c.
0
[PMID]
0 ... u ><
(.J
E
.1:.
'6
Ql VI
'S Ql E Ql
>
z Q
""'
:::E ;:) :::;
Cohort
Freedman Health Any Assay RIA Colorectal X X X X X X White:71%;
2007
53
status method (OiaSorin) cancer Black: 14%;
NHANES Il l
Mean
44 (:<:17) mortality Hispanic:
us age stratified by 6%; Others:
(various) (range), prespecified 9%
[16481636] y baseline
Male 45 Season Ali
25(0H)D cut
(%) blood
points
drawn
Nested
case-
control
Braun Health Any Assay RIA 25(0H)D X X
1995
73
status method (Harris levels
wee Mean 55 (nd) 1993) between
Maryland,
age cases and
US (38N)
(range), controls
[329893] y Colon cancer
Male Nd Season Fall risk stratified
(%) blood by baseline
drawn 25(0H)D
uintiles
Feskanich Health Any Assay RIA Colorectal X X X X X X Aspirin user
2004
70
status method (Harris cancer risk (>10 y):
NHS
Mean 60 {43-70) 1997) stratified by 10%;
us age
baseline Hormone
(various)
(range),
25(0H)D replacement
[15342452] y quintiles therapy:
Male 0 Season All 34%
(%) blood
drawn
Garland Health Any Assay HPLA 25(0 H)D X X White:
1989
72
status method (Clemens levels 100%
wee
Mean 63 (nd) 1982) between
Maryland,
age cases and
us (range), controls
(38N) y Colon cancer
[2572900)
Male 50 Season Fall risk stratified
(%) blood by baseline
drawn 25(0 H)D
guintiles
Otani 2007
68
Health Any Assay CPBA 25(0H)D X X X X X X
Japan PHC status method (Haddad levels
Japan
Mean Men: 57 1971) between
(various) age (40-69); cases and
[17622244)
(range), Women: 56 controls
y (40-69) Colorectal
Male Season Ali cancer risk
(%) blood stratified by
drawn baseline
25(0H)D
uartiles
continued
82
Confounders/Effect Modifiers
Adjusted
Author Year Vl
Study Name
Q) E
Vitamin D
.c
.. Q)
Location Population Comparisons
c.
::J
E
Concentration
Vl 111
Vl
(Latitude) E
.. c.
i;
0
Q)
E
Cl 0
c. >. 0
[PMID]
Q)
0
.. (.) )(
iii
(.J ;::
E
.c
:0
Q)
5 Q) E
Q)
>
z Q
:::E ;:) ::;
i angrea
Health Smoker
9
Assay RIA Colorectai X "'"X' X X
1997
67
status
method (Horris cancer risk
ATBC
Mean 60 (50-69)
1993) stratified by
Finland
age
baseline
(-60N)
(range),
25(0H)D
[9242478)
y
quartiles
Male 100 Season All
(%) blood
drawn
Wactawski- Health Post- Assay RIA Colo rectal X X X X White:83%;
Wende status menopausal method (DiaSorin) cancer risk Black: 9%;
2006
71
womenc stratified by Hispanic:
WHI Mean Nd (50-79) baseline 4% Others:
us age 25(0H)D 4%
(various) (range), quartiles
[16481636) y
Male 0 Season All
(%) blood
drawn
Wu 2007
6
" Health Smoker 5% Assay RIA 25(0H)D X X X X X X Aspirin user
HPFS status method (Horris levels in 1994:
us Mean 66 (nd) 1997) between 40%;
(various)
age cases and Current
[17623801)
(range), controls smoker: 5%
y Colorectal
Male 100 Season All cancer risk
(%) blood stratified by
drawn baseline
25(0H)D
A
guintiles
This table is ordered alphabetically by study author.
B
Participants of a lung cancer prevention 2 by 2 RCT of alpha-tocopherol and beta-carotene.
c
Participants of a hip fracture prevention RCT of vitamin 03 and calcium
83
Table 23. Vitamin D and colorectal cancer: Results of observational studies
Author Year Life Stage Outcome Followup 25(0H)D No. of No. in Adjusted 95% CI P for Study
Study Name (n/N; Incidence) Duration Concentration, Cases Category OR Trend Quality
[PMID] (Time to nmoi/L
Ox)
Cohort stud
Colorectal cancer mortality
Women
Freedman 2007
53
19-5QA Colorectal Cancer nd <50 28 -5606 Reference 0.02 B
[ 17971526] 51 -70 Mortality
2:71 (66/ 16818; 0.004)
------------
50-80 24 -5606 0.44 0.20, 0.95.
----------
....................................................,
2:80 14 -5606 0.28 0.1 1, 0.68.
Nested case-control study
Colorectal cancer
Men
Otani 2007 19-50 Colorectal cancer 1-13 <57.2 43 74 Reference 0. 39 B
Japan PHC 51 -7QA (N=196 cases; 392
[1 7622244] controls)
---"'"'-'"''"'""'"""""'""'"''' '
40 85 0.76 0.42, 1.4
----------- --
69.0-80.2 36 85 0.76 0.39, 1.5
2:80.2 44 80 0.73 0.35, 1.5
Wu 2007 19-50 Colorectal cancer 1-9 46, median 45 71 1 Reference 0.24 B
HPFS 51 -7QA (179 cases; 356
(17623801 ] 2:71 controls)
---------------
....................................................,
62.5 44 71 0.97 0.55, 1.70
-------------
.....................................................
72.8 30 68 0.66
------------
83.3 23 74 0.51
.......9..:.?..?.... .....
98.5 37 72 0.83 0.45, 1.52
19-50 Colorectal cancer, 48.2, median 25 34 1 Reference 0.13
51 -7QA age <65
---------------
....................................................,
66.8 15 28 1.03 0.36, 2.91
----------- -
80.0 9 30 0.38
........ ..?.., .... ...:.? ........
-----------
97.0 14 36 0.45 0. 15, 1.40
51 -70 Colorectal cancer, 48.2, median 34 55 1 Reference 0.34
2:71 age <::65
------------
.....................................................
66.8 36 61 0.97 0.50, 1.87
------------
....................................................,
80.0 19 58 0.56 0.27, 1.15
97.0 27 54 0.83
""'""6':'39:"'1":'75"""
Tangrea 1997 19-50 Colorectal cancer 1-8 :524.5 46 72 1 Reference 0.13 B
ATBC 51 -7QA (146 cases; 292
[9242478) controls)
....................................................,
24.5-34.7 35 73 0.7 0.4, 1.3
---------- ---
....................................................,
36 73 0.8 0.4, 1.3
>48.2 29 72 0.6 0.3, 1.1
continued
Author Year Life Stage Outcome Followup 25(0H)D No. of No. in Adjusted 95%CI P for Study
Study Name (n/N; Incidence) Duration Concentration, Cases Category OR Trend Quality
[PMID] (Time to nmol/l
Ox)
Women
Wactawski-Wende 2006 Post- Colorectal cancer 1-1 2 <31.0 88 67 2.53 1.49, 4.32 0.02 B
WHI menopausal (306 cases; 306
[1 6481636) women controls}
------------
.....................................................
31.0-42.3 80 73 1.96 1.18, 3.24*
-------42.4-58 .3
78 73 1.95
.,________ _____
60 93 1 Reference
Feskanich 2004 19-50 Colorectal cancer 1-11 40.2, median 53 77 1 Reference 0.02 B
NHS 51 -7QA (192 cases; 384
[15342452] controls)
....................................................,
55.1 47 79 0.93 Q,:3,1:>:3 .
-----------
66.7 35 75 0.79 0.44, 1.40
------------ -
77.5 29 77 0.58 0.31' 1.07
--------------- -
99. 1 29 75 0.53 0.27, 1.04
Otani 2007 19-50 Colorectal cancer 1-13 <57.2 41 77 1 Reference 0.74 B
Japan PHC 51-?QA (179 cases; 358
[17622244) controls)
....................................................,
57.2-69 0 34
------------------
73 1.0 0.55, 1.9
69.0-80.2 44
---------
71 1.2 0.65, 2.3
41 76 1.1 0.50, 2.3
Colon cancer
Both sexes
Braun 1995 19-50 Colon cancer (57 1-17 <43 nd nd Reference 0.57 c
wee 51 7QA cases; 114
[329893) controls)
------------- --
.....................................................
43.0-51.5 nd nd 0.3 0.1' 1.0
-------51.5-61 .8
nd nd 0.5
"""""""i5':2:"'1":'5""""'"'
-----------------
....................................................,
61.8-75.3 nd nd 0.7 0.2, 2.0
------------------ -
nd nd 0.4 0.1, 1.4
Garland 1989 19-50 Colon cancer (34 1-9 10 to <50 9 8 1 Reference 0.41 c
wee 51-?QA cases; 67 controls)
[2572900)
....................................................,
50.0-67.5 7 13 0.48 0.13, 1.80
----------------
.....................................................
67.5-82.5 5
------------
18 0.25 0.06, 0.98*
82.5-105 4
----------- .
17 0.21 0.05, 0.89*
105-227.5 9 11 0.73 0.20, 2.66
Men
Otani 2007 19-50 Colon cancer (141 1-13 <57. 2 25 54 Reference 0.70 B
Japan PHC 51 7QA cases;282
(17622244) controls)
....................................................,
57.2-69.0 27 55 0.98
.......... .....?..:.9............
.. ____ 29 66 1.0
38 62 1.2 0.51, 2.7
continued
85
Author Year Life Stage Outcome Followup 25(0H)D No. of No. in Adjusted 95%CI P for Study
Study Name (n/N; Incidence) Duration Concentration, Cases Category OR Trend Quality
[PMID] (Time to nmol/l
Ox)
Wu 2007 19-50 Colon cancer (139 1-9 48.3, median 49 66 Reference 0.005 B
HPFS 51 -70A cases;276
[ 17623801] 2:71 controls)
---------------
....................................................,
66.8 44 68 0.74 0.42, 1.33
-----------
.....................................................
80.0 17 68 0.29
.......9..:.. .. 1., .. ......
-----------
97.0 29 74 0.46 o.24, o 89.
Tangrea 1997 19-50 Colon cancer (91 1-8 :524.5 30 47 1 Reference 0.69 B
ATBC 51 70A cases;182
[9242478] controls}
------------
....................................................,
24.5-34.7 18
--------------
47 0.6 0.3, 1.2
34.7-48.2 22
------------
45 0.8 0.4, 1.6
>48.2 21 42 0.8 0.4, 1.6
Women
Feskanich 2004 19-50 Colon cancer (148 1-11 41.2, median 41.2 75 Reference 0.17 B
NHS 51-70A cases;296
[15342452] controls)
59.7 59.7 71 1.03 0.56, 1.89
73.3 73.3 77 0.54 0.28, 1.03
98. 1 98.1 72 0.70 0.35, 1.38
Otani 2007 19-50 Colon cancer (115 1-13 <57.2 21 53 1 Reference 0.12 B
Japan PHC 51-70A cases;230
[1 7622244] controls)
"'-"'''""" ' '"""""""""""""'"'"' '
--57 27 48 1.7 0.78, 3.6
---------------
69.0-80.2 27
-----------------
41 2.1 0.90, 4.7
2:80.2 31 53 2.1 0.78, 5.6
Rectal cancer
Men
Otani 2007 19-50 Rectal cancer (55 1-13 <57.2 18 20 Reference 0.06 B
Japan PHC 51-70A cases; 110
[1 7622244] controls}
---------------
.....................................................
57.2-69.0 13 30 0.17 0.02, 1.2
--------------
:.: ....IQ$.; ...f:I ...... :
69.0-80.2 7 19 0.25
<::80.2 6 18 0.075 0.005, 0.99
Tangrea 1997 19-50 Rectal cancer (55 1-8 :524.5 16 25 Reference 0.06 B
ATBC 51 70A cases; 110
[9242478) controls)
24.5-34.7 17 26 0.9 0.4, 2.4
-------34. 7-48.2
14 28 0.8 ::::::::::::::Q.;II:i?.::::::
--------; 48:2-------
8 30 0.4 0.1' 1.1
continued
86
Author Year Life Stage Outcome Followup
Study Name (n/N; Incidence) Duration
[PMID] (Time to
Ox)
Wu 2007 19-50 Rectal cancer (40 1-9
HPFS 51 -70A cases; 80 controls)
[ 17623801 ] 2:71
Women
Otani 2007 19-50 Rectal cancer (64 1-13
Japan PHC 51 70A cases; 128
[1 7622244] controls)
Feskanich 2004 19-50 Rectal cancer (44 1-11
NHS 51 70A cases; 88 controls}
[ 15342452]
* Statistically significant (P<0.05)
A Most representative life stage.
25(0H)D
Concentration,
nmol/l
53.0, median
73.3
------------
93.5
<57.2
-----------------
57.2-69.0
----------------
69.0-80.2
--------------
<::80.2
44.4, median
-------------
66.2
92.4
No. of
Cases
11
15
14
20
7
17
10
24
10
10
No. in Adjusted
Category OR
30
28 1.74
22 3.32
24
25 0.26
30 0.46
23 0.33
31
26 0.52
31 0.31
95% CI
Reference
....................................................,
0.61' 5.00
....................................................,
0.87, 12 69
Reference
....................................................,
0.07, 1.0
(),J,J 4.
0.08, 1.3
Reference
....................................................,
........ 9 : ~ ..1.1 .... ... ~ ~ ........
0.08, 1.31
P for
Trend
0.08
0.17
0.03
Study
Quality
B
B
B
8
P for trend = 0.31 when cases diagnosed within 2 years of blood collection were excluded.
c Results were not notably changed when cases diagnosed within the first year after blood collection were excluded (P for trend not reported). Subgroup analyses per age were also
reported as follows: Age 2: 60, OR = 0.35 (95% Cl 0.14, 0.87} between the lowest and highest quintiles; P for trend = 0.006. Age < 60, OR = 1.36 (95% Cl 0.48, 3.92} between the
lowest and highest quintiles; P for trend= 0.70.
0
P for trend = 0.008 when cases diagnosed within 2 years of blood collection were excluded.
E P for trend = 0.58 when cases diagnosed within 2 years of blood collection were excluded.
P for trend = 0.04 when cases diagnosed within 2 years of blood collection were excluded.
87
Figure 8. Colorectal cancer risk stratified by vitamin D concentration
25(0H)D
p
concentrat ion for
Study Category (nmoi/ U trend Quality
-
Men
Japan PHC 2007 Q1 (ref) <57 0.39 B
(n=588) Q2 57 - 69
Q3 69-80
Q4 >80
--
HPFS 2007 Ql (ref) 46 0.24 B
(n=535) Q2 63
Q3 73
Q4 83
Q5 99
ATBC 1997 Q1 (ref) <25 0.13 B
(n=438) Q2 25-35
Q3 35 - 48
Q4 >48
Women
WHI 2006 Q1 <31 0.02 B
(n=61 2) Q2 31 - 42
Q3 42-58
Q4 (ref) >58
--
NHS2004 Q1 (ref) 40 0.02 B
(n=576) Q2 55
Q3 67
Q4 78
Q5 99
-
Japan PHC 2007 Ql (ref) <57 0.74 B
(n=537) Q2 57 - 69
Q3 69 - 80
Q4 >80
I I I I
0.2 0.5 2 5
Decreased risk Increased risk
Figure 9. Colon cancer risk stratified by vitamin 0 concentration
25(0H)D
p
concent rat ion for
Study Category (nmoi/L) t rend Quality
-- -
Bot h sexes
wee 1995 Q1 (ref ) <43 0.57 c
(n=171) Q2 43-52
Q3 52-62
Q4 62 - 75
- --
Q5 >75
wee 1989 Q1 (ref) <50 0.41 c
(n=1 01 ) Q2 50- 68
Q3 68 - 83
Q4 83 - 105
Q5 105 - 228
Men
I
Japan PHC 2007 Q1 (ref ) <57 0.70 B
(n=423) Q2 57 - 69
Q3 69- 80
Q4 >80
--
if
HPFS 2007 Q1 (ref ) 48 0.005 B
(n=415) Q2 67
Q3 80
--
Q4 97
--
ATBC 1997 Ql (ref) <25
j
0.69 B
(n=273) Q2 25 - 35
Q3 35 - 48
Q4 >48
Women
J
NHS 2004 Ql (ref) 41 0.17 B
(n=444) Q2 60
Q3 73
Q4 98
- -
olTref )
---- --
Japan PHC 2007 <57 0.12 B
(n=345) Q2 57-69
Q3 69 - 80
Q4 >80
I I I I I I I
O.Q2 0.1 0.2 0.5 1 2 5 1 0
Decreased risk Increased risk
89
Figure 1 0. Rectal cancer risk stratified by vitamin D concentration
25(0H)D
p
concentration for
Study Category (nmolll) trend Quality
-
Men
Japan PHC 2007 Q1 (ref) <57 0.06 B
(n=165) Q2 57- 69
Q3 69-80
Q4 >80.2
ATBC 1997 Q1 (ref) <25
:1
0.06 B
(n=165) Q2 25-35
03 35 - 48
Q4 >48
:-
E
HPFS 2007 Q1 (ref) 53 0.08 B
(n=120) Q2 73
Q3 94
Women
Japan PHC 2007 Q1 (ref) <57 0.17 B
(n=192) Q2 57 - 69
Q3 69-80
Q4 >80
NHS 2004 Q1 (ref) 44 0.03 B
(n=132) Q2 66
Q3 92
I I I I I I I I
0.005 0.02 0.2 0.5 1 2 5 10 50
Decreased risk Increased risk
Colorectal adenoma.
Synopsis.
No systematic reviews have evaluated the association between 25(0H)D concentrations and
the risk of colorectal adenoma. One B quality nested case-control study in women found no
significant association between 25(0H)D concentrations and the risk of colorectal adenoma.
Detailed presentation (Tables 24 & 25 ).
One nested case-control study within the NHS evaluated the relationship between 25(0H)D
concentrations and the risk of colorectal adenoma in women.
74
At 5 years, an adjusted analysis
found no significant association between 25(0H)D concentrations and the incidence of
colorectal adenoma by trend analysis. Subgroup analyses also found no significant association
between 25(0H)D concentrations and the incidence of colon or rectal adenoma. No subgroup
data were available regarding age or other special populations (e.g., obese, smokers, ethnic
groups, or users of contraceptives). This study was rated B because it excluded more than 50
percent of participants of the original cohort because their blood samples were not available.
Findings by life stage.
0 - 6 mo Not reviewed
7 mo - 2 y Not reviewed
3 - 8 y Not reviewed
9 - 18 y Not reviewed
19- 50 y A proportion of participants in the NHS was in this life stage. No unique
conclusions are possible for this life stage separate from those for people 51 to 70 years.
51 - 70 y The analysis of the NHS included female participants mostly within this
life stage. The study found no association between 25(0H)D and the incidence of
colorectal adenoma.
?71 y A proportion of participants in the NHS was in this life stage. No unique
conclusions are possible for this life stage separate from those for people 51 to 70 years.
Postmenopause The analysis ofNHS partially included postmenopausal women.
However, no unique conclusions are possible for this life stage separate from those for
people 51 to 70 years.
Pregnant & lactating women Not reviewed
91
Table 24. Vitamin D and colorectal adenoma: Characteristics of observational studies
Confounders/Effect Modifiers
Adjusted
Author Year
"'
Study Name !!!
c
Vitamin D
.1:. Ill
Location Population Comparisons
c.
:I
E
Concentration
"'
f!
Ill
(Latitude) c
c.
(ij
0 Ill
E
Cl 0 c.
0
[PMID]
!
0
... u ><
()
E
.1:.
:0
Ill Ill
'S Ill c Ill
>
.1!!
z
Q
cs: :::1 ::;
Nested case-
control
Platz 2000 Health Any Assay RIA Colorectal X X X X X X Aspirin user:
NHS status method (Horris adenoma risk 26%;
us Mean 59 1993) stratified by Hormone
(various)
age (7) baseline replacement
[1 1045788) (SO), y 25(0H)D therapy: 36%
Male 0 Season All quartiles
(%) blood
drawn
92
Table 25. Vitamin D and colorectal adenoma: Results of observational studies
Author Year Life Outcome Follow up 25(0H)D No. of No. in Adjusted 95% CI P for Study
Study Name Stage (n/N; Incidence) Duration Concentration, Cases Category OR Trend Quality
[PMID] (Time to Ox) nmoi/L
Nested case-control study
Colorectal
adenoma
Women
Platz 2000 19-50 Colorectal adenoma 5 16.3, median 103 82 Reference 1.0 B
NHS 51-70A (326 cases; 326
[1 1045788) :2:71 controls)
------------------------
22.6 62 80 0.64 0.41 , 1.00
-------------------------
().36-;-6-:9-5 ' 28.3 61 82 0.58
-----
38.0 100 82 1.04 0.66, 1.66
Colon adenoma
Women
Platz 2000 19-50 Colon adenoma (261 5 16.3, median 79 64 Reference 1.0 B
NHS 51 70A cases; 261 controls)
[1 1045788) <::71
------------------------
22.6 55
------------------------------------------
64 0.71 0.43, 1.18
28.3 51 69 0.60 0.35, 1.02
--------- 3s :o __________
76
--64 ___
1.02 o--:-60, 1.73 .
Rectal adenoma
Women
Platz 2000
14
19-50 Rectal adenoma (65 5 16.3, median 24 18 Reference 0.9 B
NHS 51-70 A cases; 65 controls)
[1 1045788) <::71
------------------------
22.6 7 16 0.38 0. 12, 0.19
-----------------------------------------
- o:08. 1.42-
28.3 10 13 0.34
---------------------
38.0 24 18 1.59 0.50, 5.03
Statistically significant (P<0.05)
A
Most representative life stage
Breast cancer.
Synopsis.
No qualified systematic reviews evaluated the association between vitamin D and calcium
intake or serum 25(0H)D concentration and risk of breast cancer. One cohort study compared
serum 25(0H)D concentrations and the risk of breast cancer-specific mortality ,5
3
and two nested
case-control studies compared 25(0H)D concentrations and the risk of breast cancer.
75
76
The
cohort study utilizing NHANES III data found significant decrease in breast cancer-specific
mortality during 9 years offollowup in those with serum concentration of25(0H)D greater than
62 nmol/L. The Nurses' Health Study and Prostate, Lung, Colorectal, and Ovarian (PLCO)
Cancer Screening Trial, however, found no significant relationship between serum concentration
of25(0H) D and risk of breast cancer diagnosis in either pre- or postmenopausal women during
7 to 12 years offollowup.
75
'
76
All three studies were rated B quallty.
Detailed presentation (Tables 26 & 27).
The NHANES III study followed 16,818 adults with a mean age of 44 years with a
background calcium intake on average of about 812 mg/day (from diet and supplements).
53
The
study included 71 percent non-Hispanic white, 14 percent non-Hispanic black, 6 percent
Mexican American, and 9 percent from other races. During 9 years of followup, women with
serum concentration of 25(0H) D greater than 62 nmol/L had a hazard ratio of 0.28 for breast
cancer-specific mortality compared to those with 62 nmol/L or lower (95 percent CI 0.08-0.93).
The breast cancer-specific mortality was one of many cancer-specific mortality outcomes
reported in this study.
Two nested case-control studies of women with a mean age of 57 years and 67 years,
respectively, found no relationship between serum 25(0H)D concentrations and risk of breast
cancer.
75
76
However, in the second study, when compared with the lowest quintile, quintiles 3 to
5 were associated with nonsignificantly elevated risks. In multivariable adjusted analyses, the
risk associated with 25(0H)D levels below 15 ng/mL compared with higher levels was 0.81 (95
percent CI 0.59, 1.12).
76
Findings by age and sex.
In the one nested case-control study (methodological quality B) including both
premenopausal and postmenopausal women, no relationship was found between vitamin D levels
and risk of breast cancer. However, in this study, there was a statistically significant trend
towards decreased risk ofbreast cancer among women older than 60 years of age with serum
concentration of 25(0H)D greater than 62 nmol/L.
Findings by ~ f stage.
0 - 6 mo Not applicable
7 mo- 2 y Not applicable
3 - 8 y Not applicable
9 - 18 y Not applicable
19-50 y A followup study ofNHANES III including women with a mean age of 44
years found a decreased mortality (hazard ratio 0.28) due to breast cancer among those
with serum concentration of 25(0H)D greater than 62 nrnol/L.
51 - 70 y Two nested case-control studies of women with a mean age of 57 years
and 67 years, respectively, found no relationship between vitamin D levels and risk of
breast cancer. However, in one of these studies, there was a statistically significant trend
towards decreased risk of breast cancer among women older than 60 years of age with
serum concentration of 25(0H)D greater than 62 nmol/L.
~ 7 y Not reviewed
Postmenopause Not reviewed
Pregnant & lactating women Not reviewed
Table 26. Vitamin D and breast cancer: Characteristics of observational studies
Confounders/Effect Modifiers
Author Year
Adjusted
Study Name
Vitamin D
.::::
~
Location Population Comparisons
Q.
:I
Comments
Concentration
1/1 (1J 1/1
(Latitude) 'E
... Q.
"iii
0 Gl
Ol 0 Q.
~
[PMID]
Gl 0 ... (,)
><
;:
E
.::::
'6
Gl 1/1
'S Gl 'E Gl
>
2
z c <( :::iE ::J :J
Cohort
Freedman Health Non- Assay RIA Breast cancer X X X X X
2007
53
status institutionalized method risks: Ouintile
NHANES Ill
Mean age 44 (NO) 1 vs. Ouintile
us (range/SO), 2
(38
2
N) y
[17971526)
Season All
blood year
drawn
Nested
Case-
Control
Bertone- Health No Cancer Assay RIA Breast cancer X X X X X
Johnson status method risks: Quintile
2005
75
Mean age 57 (7.0) 1 vs. Quintile
NHS (range/SO), 2, 3, 4, 5
us y
{38
9
N)
Season All
[16103450]
blood year
drawn
Freedman Health No Cancer Assay RIA Breast cancer X X X X X
2008
76
status method risks: Quintile
PLCO Trial
Mean age 67 (NO) 1 vs. Ouintile
us (range/SO),
2,3,4,5
(38
2
N) y
[18381472]
Season Dec-
blood Sep
drawn
95
Tabl e 27. Vitamin D and breast cancer: Results of observational studies
Author Year Life Stage Outcome Follow up Vit D Concentration, No. of No. in Adjusted 95% CI P for Study
Study Name (n/N; Durati on Measure nmoi/L Cases Category RR Trend Quality
[ PMID] Incidence) (Time to
Dx)
Cohort
Freedman 2007
53
All Adults Breast cancer 105 mo 25(0H)D <63 20 ND Reference NS B
NHANES Ill mortality
[17971526] (28/NDt
-------------
2:63 8 ND HR 0.28
Nested Case-
Control
Bertone-Joh nson Pre- and Post- Breast cancer <1 -82 mo 25(0H)D s50 (1"
1
batch) 159 297 Reference nd B
2005
75
menopausal (701/ 1425) S70 (2nd batch)
NHS s45 (3'd batch)
[16103450]
------------- -------------
51 - 70 149 278 0.95 0.66, 1.36
72-85
47 to 60
72- 82 125
----266----
0.74
--o:sT;--1.-os
87 - 97
62 - 72
------------- - ----------- ..
85-97 144 296 0.80 0.58, 1.11
100- 117
75-90
------------- --------------
2:100 124 265 0.73 0.49, 1.07
2:1 20
2:92
Breast cancer 97 191 Reference NS
<60 y
(701/ 1425)
------------- --------------
84 170 0.96 0.62, 1.49
77
rs4
0.80
-------------
90 192 0.85 0.55, 1.32
--------------
--a:s=;-:--1:4a-
70 146 0.92
Breast cancer 62 109 Reference 0.03
2:60 y
(701/ 1425)
65 114 1.07
---o:so:-1-:92-
------------
48 105 0.64
-------------
54 99 0.68 0.38, 1.24
--------------
---o.-31:--1-:()4-
54 125 0.57
continued
Author Year Life Stage Outcome Follow up Vit D Concentration, No. of No. in Adjusted 95% CI P for Study
Study Name (n/N; Duration Measure nmoi/L Cases Category RR Trend Quality
[PMID] Incidence) (Time to
Dx)
Freedman Pre- and Post- Breast cancer 12 y 25(0H)D <46 172 2010 Reference NS B
2008
76
menopausal (1 005/201 O)
PLCO Cancer
Screening Trial
[1 8381472]
------------ -------------
46-58 188 ----?..QJ_Q _________ 1.02 _ ...Q2.,J..,1.L-.
59-71 244 2010 1.36 ____
-------------
72-83 205 2010 1.13 0.82, 1.55
-------- -----
2:84 196 2010 1.04
Statistically significant (P<0.05)
A Total number of women not reported
97
Pancreatic cancer.
Synopsis.
No qualified systematic reviews evaluated associations between serum vitamin D
concentrations and the incidence of pancreatic cancer. Two nested case-control studies, rated A
in methodological quality, evaluated the association between serum 25(0H) concentration and
the risk of developing pancreatic cancer in two different populations. One study found that older
adult male smokers living in Finland with higher baseline serum 25(0H)D concentration had an
increased risk of exocrine pancreatic cancer compared with those with lower concentration
(>65.5 vs. <32 nmol/L; OR=2.92; P for trend=O.OOl). The other study found that baseline
25(0H)D concentrations were not associated with the risk of overall pancreatic cancer (>82.3 vs.
<45.9 nmoVL; OR=l.45; P for trend=0.49) among older adults living in the United States.
However, there was an increased risk of pancreatic cancer among the study participants with
higher compared to lower 25(0H)D concentrations (>78.4 vs. <49.3 nmol/L; OR=4.03) only in
those living in low residential UVB exposure areas but not among those living in moderate or
high residential UVB exposure areas.
Detailedpresentation (Tables 28 & 29).
51 - 74 years.
One nested case-control study based on the Alpha-Tocopherol, Beta-Carotene Cancer
Prevention Study (A TBC) in older adult male smokers aged 54 to 62 years in Finland identified
200 cases of incident exocrine pancreatic cancer.
77
These cases were matched to 400 controls.
Baseline semm 25(0H)D concentration was stratified into quintiles. The odds ratio for exocrine
pancreatic cancer was 2.92 (95 percent CI 1.56, 5.48) comparing 5
111
quintile (>65.5 nmoi/L) to
1
51
quintile (<32 nmol/L). The result was adjusted for age, month of blood drawn, years smoked,
number of cigarettes smoked per day, reporting to have quit smoking more than three
consecutive visits(> 1 y) during the trial (1985-1993), occupational physical activity, education,
and serum retinol. The study authors excluded islet cell carcinomas from analysis because the
etiology for their pathogenesis might be different from that of exocrine tumors.
Another nested case-control study based on the Prostate, Lung, Colorectal, and Ovarian
Screening (PLCO) trial in older men and women ~ e d 55 to 74 years in the United States
identified 184 cases of incident pancreatic cancer.
7
These cases were matched to 368 controls.
Baseline serum 25(0H)D concentration was stratified into quintiles. The odds ratio for exocrine
pancreatic cancer was 1.45 (95 percent CI 0.66, 3 .15) comparing 5th quintile (>82.3 nmol/L) to
1st quintile (<45.9 nmol/L). The result was adjusted for age, race, sex, date of blood draw based
on 2-month blocks, BMI and smoking. The association was not significantly modified by season
ofblood collection (P for interaction> 0.14); but estimated residential annual solar UVB
exposure significantly modified the 25(0H)D concentration and pancreatic cancer association (P
for interaction = 0.015). In the joint effects models, among subjects with low estimated annual
UVB residential exposure, higher compared with lower 25(0H)D concentrations were associated
with increased risk of pancreatic cancer (compared with the lowest quartile, the ORs for each
respective quartile were 2.52, 2.33, and 4.03; 95 percent CI 1.38, 11.79), whereas among
subjects with moderate to high residential UVB exposure, 25(0H)D concentrations were not
associated with pancreatic cancer. There was no significant interaction of25(0H)D
concentration and pancreatic cancer by smoker status, sex, physical activity, or total vitamin A
intake.
Findings by life stage.
0 - 6 mo not reviewed
7 mo - 2 y not reviewed
3 - 8 y not reviewed
9 - 18 y not reviewed
19- 50 y No study specifically targeted this age group.
51 - 70 y One nested case-control study found that male smokers living in Finland
with higher baseline serum 25(0H)D concentration had an increased risk of pancreatic
cancer compared with those with lower concentration (5th vs. 1st quintile, >65.5 vs. <32
nmoi/L: OR 2.92, 95 percent CI 1.56, 5.48, P for trend= 0.001). Another study found
that baseline 25(0H)D concentrations were not associated with overall risk of pancreatic
cancer among older adults living in the United States (5
111
vs. 1st quintile, >82.3 vs. <45.9
nmol/L: OR 1.45, 95 percent Cl 0.66, 3.15; P for trend=0.49). However, there was an
increased risk of pancreatic cancer among the study participants living in low residential
UVB exposure areas (4
111
vs. 1
51
quartile >78.4 vs. <49.3 nmol/L: OR=4.03; 95 percent CI
1.38, 11.79).
~ 7 y No study specifically targeted this age group.
Postmenopause not reviewed
Pregnant & lactating women not reviewed
99
Table 28. Vitamin D and pancreati c cancer: Characteristics of observational studies
Confounders/Effect Modifiers
Author Year
Adjusted
Trial/Cohort
0
Country 25(0 H)D
Gl
Population Comparisons :.c
...
(Latitude)
Q.
:I
"'
"'
!!!
Ill
"'
Gl E
[PMID]
c,
Q.
(ij
0
Gl
c
0
Q.
0
... 0 )(
"'
E
E
.t:
'6
Q)
E
'S Q) E
Q)
> 0
z c :E ;:) :::; (.)
Stolzenberg- Health All Assay RIA Exocrine X X X X
Solomon status smokers (OiaSorin) pancreatic risk
2006
77
Mean age 58
stratified by
ATBC
(range/SO),
baseline
Finland
y
25(0H)O
(6oN)
Male(%) 100 Season nd; but
quintiles
[1 7047087]
blood result
drawn adjusted
for this
variable
Stolzenberg- Health OM: Assay RIA Pancreatic risk X X X X
Solomon status 10.5% (Heartland stratified by
2009
78
Mean age 66 (55-
Assays baseline
PLCO
(range), y 74)
lab) 25(0 H)O
us
Male(%) 65.2 Season All
quintiles
(various)
blood seasons
[19208842]
drawn
Pancreatic risk
stratified by
residential sun
exposure
levels and
baseline
25(0H)O
guartil es
100
Table 29. Vitamin D and pancreatic cancer: Results of observational studies
Author Year
Study Name
PMID
Stolzenberg-Solomon
2006
77
ATBC
Finland
(60N)
[17047087)
Stolzenberg-Solomon
2009
78
PLCO
us
(various)
[19208842]
Life
Stage, y
51 -70,
male
only
51 -70,
both
sexes
Statistically significant (P<0.05)
Outcome (no. of
cases; no. of
control)
Exocrine
pancreatic cancer
(200; 400)
Pancreatic cancer
(184; 368)
Pancreatic
cancer: Low
residential sun
exposure area
(91; 167)
Pancreatic
cancer: Moderate
residential sun
exposure area
(91; 167)
Time to
diagnosis, y
11.8 (median)
5.4 (median),
up to 11 y
nd
nd
25(0H)D
concentration,
nmolll
<32
No. of
cases
27
No. of
control
80
Adjusted
OR
95% CI
Reference
32-41.1 ___ 1.30 0.70, 2.40
"""4.'L'EI3 ........................................... 47 8o ......2:1"2 ................................. _..,.. 1.
7
15 =--=3"'= .9"=' o_ _
51.1-65.5 35 81 1.50 0.81, 2::.:..7 c..:: 6 __
>65.5 57 79 2.92 1.56, 5.48*
S45.9
>60.310
>69.5 to
.................................................................
>82.3
<49.3
44 74 Reference
__:.:40::....__ ___:7...:. 4___ _9.:.1? 1.98
27 73 0.86 0.40, 1.84
___ o:a4
42 73 1.45 0.66, 3.15
22 44 Reference
-=22=--__ ...:.4=.2___ 2.52 0.92, 6.90
>65.2 to <78.4 ___ ...... .................................
......;.7if4 ........................................................ 26 38 4.03 1.38, 11.79
<49.3 33 48 1.97 0.80, 4.82
--;49.:3 ..io .. .......................--:-15=----=5-=-o -----a:ss .................................--:::- o-= .2:-:: 2-. 2=-.-=- o1-:---
... ---7 18=-----=49:::...._ __ 0.91 0.31, 2.71
>78.4 24 54 1.45 0.53, 3.96
P for trend
0.001
0.49
P for
interaction
between low
and
moderate/high
residential
sun exposure
= 0.015
Study
Quality
A
A
Vitamin D and Immunologic Outcomes
We reviewed primary studies that evaluated relationships between vitamin D and any
immune function related outcomes.
Synopsis.
Analyses using NHANES III data (general adult populations living in the US) showed no
significant association between baseline 25(0H)D concentrations and infectious disease
mortality.
One cohort study from UK suggested a relationship between maternal 25(0H)D
concentration and the risk of eczema in their children, but the analysis did not control for
important potential confounders, and the 25(0H)D concentrations in children were not
measured.
Detailed presentation (Tables 30 & 31 ).
One study analyzed NHANES III data and showed no association between baseline 25(0H)D
concentrations and infectious disease.
47
NHANES III cohort represents general adult populations
living in the United States. This study was rated quality C.
One cohort study from UK analyzed the serum 25(0H)D concentration in 440 white women
in late pregnancy (- 33 wk) and found their infants' risk of eczema at age 9 months was higher in
those mothers in the top quartile ofthe distribution of serum 25(0H)D (>50 nmol/L) compared
with those at the bottom quartile (<30 nmol/L), although the results were not statistically
significant.
42
However, this analysis did not control for important potential confounders, and the
25(0H)D concentrations in children were not measured. This study was rated quality C.
Findings by life stage.
0 - 6 mo No data
7 mo - 2 y No data
3 - 8 y No data
9 - 18 y No data
19 - 50 y NHANES III data include people in this life stage. Analyses using
NHANES III data (general adult populations living in the US) showed no significant
association between baseline 25(0H)D concentrations and infectious disease mortality.
51 - 70 y NHANES III data also include people in this life stage.
~ 7 y NHANES III data also include people in this life stage
Postmenopause No data
Pregnant & lactating women One cohort study from UK analyzed the serum
25(0H)D concentration in white women in late pregnancy (- 33 wk) and showed a
relationship between maternal 25(0H)D concentration and the risk of eczema in their
children. However, this analysis did not control for important confounders, and the
25(0H)D concentrations in children were not measured.
Table 30. Vitamin D (mother) and immunologic outcomes (offspring): Characteristics of cohort
studies
Confounders/Effect Modifiers
Author Yea
Adjusted
r
Study Nam
Vitamin D Comparison
Cl)
Comment
e Population
.r:.
:;
0.
Concentration s Ul ftl
Ul
s
Location
c
.... 0.
iii
0
Cl)
Ol 0 0.
(Latitude)
Cl)
0 .... 0 )(
;::
E
.r:.
'6
Cl) Ul
[PMID]
'S Cl) c
Cl)
>
z 0 ct :z ::I :J
Melamed Health OM 7.4%, Assay RIA Infectious X X X X X X
2008
47
status history of method (OiaSorin disease
NHANES Ill CVO ) mortality
us 7.9%, stratified by
(various) HTN 25% baseline
[18695076] Mean age 45 {2:20) 25(0H)O
(range), y quarti les
Male (%) 46 Seaso Ail
n blood
drawn
Gale 2008 Health singleton Assay RIA Length and X X White only
PAHSG status pregnane method weight in
UK (50
2
N) y <17 wk offspring
[1 731 1 057) Mean age 26.3 stratified by
(range/SO), mother's
y 25(0H)O
Male (%) 0 Seaso nd
n blood
drawn
103
Table 31. Vitamin D and immunologic outcomes Results of cohort studies
Author Year Life Stage Outcome Follow up Vit D Measure Concentration, No. of No. in Adjusted 95% CI P for Study
Study Name (n/N; Duration nmoi/L Cases Category OR Trend Quality
lPMID] Incidence) (Time to Dxl
Melamed 2008
41
Adults, Infectious Median 8.7 25(0H)D <44 nd 13331 0.84 0.38, 1.86 nd c
NHANES Ill both disease (IRQ7. 1- (Total)
us sexes mortality 10.2) y
(various) (N=13,331)
[1 8695076)
---------
44-60 nd
-----------
nd 0.87 0.43, 1.74
61 -80 nd nd 1.01 0.53, 1.93
>80 nd nd 1 Reference
Gale 2008 Pregnant Atopic eczema 9mo Maternal <30 (Quartile) 9 440 (total) Reference nd c
PAHSG women; at 9 mo 25(0H)D at
UK infant at 9 (48/ 440; 0.11) late pregnancy
(54N) mo
(1731 1 057]
30-50 10 1.11 A 0.43, 2.84
---- - ----
1.75"- 50-75 15 0.73, 4.17
>75 14 1.62 0.67, 3.89
Crude OR
Vitamin D and Pregnancy-related Outcomes
Preeclampsia.
Synopsis.
A single nested case-control study found an association between low 25(0H)D concentration
( <3 7.5 nmol/L) early in pregnancy and preeclampsia. The study was rated B for methodological
quality.
Detailed presentation (Tables 32 & 33).
A nested case-control study evaluated the association between 25(0H)D concentration and
risk of preeclampsia.
79
The study found an association between 25(0H)D concentrations less
than 37.5 nmol/L (measured approximately 30 wk before outcome assessment) and increased
risk of preeclampsia. The study was rated B for methodological quality.
Findings by ~ f e stage.
0- 6 mo No data
7 mo- 2 y Not applicable
3 - 8 y Not applicable
9 - 18 y Not applicable
19 - 50 y See pregnant and lactating women.
51 - 70 y Not applicable
~ 7 y Not applicable
Postmenopause Not applicable
Pregnant & lactating women A single nested case-control study found an
association between low 25(0H)D concentration (<37.5 nmol/L) early in pregnancy and
preeclampsia.
Other outcomes.
Synopsis.
We did not identify any eligible studies on the relationship of vitamin D with or without
calcium and high blood pressure, pretenn birth, or small infant for gestational age.
105
Table 32. Vitamin D and preeclampsia: Characteristics of nested case-control studies
Author Year
Study Name
Location
(Latitude)
[PMID]
Bodnar2007
PEPPSA
us
(41 N)
[17535985]
Population
Health Healthy
status
Age 2029
range, y
Male (%) 0
Vitamin D
Concentration
Assay ELISA
method
Season NO
blood
drawn
A Pregnancy Exposures and Preeclampsia Prevention Study
106
Confounders/Effect Modifiers
Adjusted
Cll
.s:
...
Q.
;:,
Ill Cll
Ill
i:
... Q.
iij
0
1:1)
0
Q.
Cll 0 ... 0 )(
;:::
E
.s:
'6
Cll
'S Cll 'E Cll
>
z 0 <( :!: ::J
Comparisons
Comparison of X X
mean 25(0H)D
levels in cases
and controls
Cll
Ill
.S!
:.:i
Table 33. Vitamin D and preeclampsia: Results of nested case-control studies
Author Year Life Stage Outcome Followup Vit D Concentration,
Study Name (n/N; Duration Measure nmoi/L
Location Incidence) (Time to Ox)
(Latitude)
[PMID]
Bodnar 2007
1
YA
PEPPS
8
us
(41 N)
17535985
Pregnancy
This is a nested case-control study
Preeclampsia
(55/ 11 98; 4%) c
ND 25(0H)D
0
9
Pregnancy Exposures and Preeclampsia Prevention Study
c Incidence obtained from the "parent'" cohort study in which this case control study is nested.
0
Early in pregnancy, approximately 30 wk before outcome assessment
107
<37.5 (vs. >37.5)
No. of No. in
Cases Category
49 265
Adjusted
OR
5.0
95%CI
1.7, 14.1
Study
Quality
8
Vitamin D and Clinical Outcomes of Bone Health
For bone health outcomes (e.g. , bone mineral density, fracture, fall or muscle strength), we
relied on a recent comprehensive systematic review (Effectiveness and Safety of Vitamin D in
Relation to Bone Health) performed by the Ottawa EPC (Table 28).
6
Because the Ottawa's EPC
report did not report separate analyses for the effect of vitamin D supplementation alone, the
results for the effect of vitamin D alone or in combination with calcium supplementation were
presented in the "Combined Vitamin D and Calcium" section. The Ottawa EPC report also did
not report separate analyses by study designs (i.e., RCTs, prospective cohorts, before and after
study, and case-control studies), although the report primarily included RCTs.
The Ottawa EPC report was updated with literature published between January 2006 and
September 2008, selected according to our eligibility criteria. Only RCTs qualified for inclusion.
Rickets.
Synopsis.
The Ottawa EPC report concluded that there is fair evidence for an association between low
serum 25(0H)D concentrations and confirmed rickets, regardless of the types of assay measures
of 25(0H)D concentrations (RIA, CPBA, HPLC). According to the report, there is inconsistent
evidence to determine whether there is a threshold concentration of serum 25(0H)D above
which rickets do not occur.
Our updated search did not identify new RCTs examining the effect of vitamin D
supplementation on rickets.
Detailed presentation (Table 34).
Ottawa EPC Report: Rickets- infants (0 through 12 months) and young children (I through 5
years).
Overall, there is fair evidence for an association between low serum 25(0H)D concentrations
and confirmed rickets, regardless of the types of assay measures of 25(0H)D concentrations
(RIA, CPBA, HPLC). There is inconsistent evidence to determine whether there is a threshold
concentration of serum 25(0H)D above which rickets do not occur.
Six studies (one RCT, three before-after and two case-control studies) reported mean or
median serum 25(0H)D concentrations < 30 nmol/L in children with rickets whereas the other
studies reports the mean or median 25(0H)D concentrations were above 30 nmol/L (and up to 50
nmol/L). In seven of eight case-control studies, serum 25(0H)D concentrations were lower in the
children with rickets compared with controls.
Findings by ~ f stage.
0 - 6 mo The Ottawa EPC report included infants and young children and
concluded that there is fair evidence for an association bet\veen low serum 25(0H)D
concentrations and confirmed rickets, regardless of the types of assay measures of
25(0H)D concentrations (RIA, CPBA, HPLC). There were no new data since the Ottawa
EPC report.
7 mo- 2 y The Ottawa EPC report included infants and young children. There were
no new data since the Ottawa EPC report.
108
3 - 8 y The Ottawa EPC report included young children. There were no new data
since the Ottawa EPC report.
9-18 y Not reviewed
19-50 y Not reviewed
51-70 y Not reviewed
2:71 y Not reviewed
Postmenopause Not reviewed
Pregnant & lactating women Not reviewed
Table 34. Summary of systematic review of the effect of vitamin D on bone health
Author Year [PMID] Cranney 2007\i [18088161)
Design Systematic review of RCTs and observational studies
Population Include all ages
Intervention (Exposure) and
Comparator
Exclude secondary causes of osteoporosis (e.g., glucocorticoid-induced, renal or liver
disease)
Exclude studies on the treatment of vitamin D-dependent rickets (to minimize clinical
heterogeneity as treatments is often nondietary sources of vitamin D)
Intervention (Exposure):
Include vitamin 0
2
or 0
3
with or without calcium.
Exclude vitamin D preparations, calcitriol, a-calcidol (because they are not nutritional
supplements, and have different safety profile)
Comparator:
No vitamin D or lower doses/levels of vitamin D
Results See text for summary results for the following outcomes in both vitamin D and combined vitamin
D and calcium sections of the report:
Rickets
Fractures, falls, or performance measures
Bone mineral density or bone mineral contents
How does dietary intake of vitamin D from fortified foods and vitamin D
supplementation affect serum 25(0H)D Concentrations
Adverse events
Comments Case-control studies were included but always summarized separately from cohort studies and
RCTs. Meta-analyses were performed to pool results from RCTs only.
A priori design?
Two independent reviewers?
Comprehensive literature search?
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
Yes
Yes
Yes
No
Yes
Yes
AMSTAR
Study quality assessment performed?
Study quality appropriately used in analysis?
Appropriate statistical synthesis?
Publication bias assessed?
Conflicts of interest stated?
Fractures, falls, or performance measures.
Synopsis.
Yes
Yes
Yes
No
Yes
Overall, the Ottawa EPC report concluded that the associations between serum 25(0H)D
concentrations and the risk of fractures, falls, and performance measmes among postmenopausal
women or elderly men are inconsistent.
6
Findings from three additional RCTs (published after the Ottawa EPC report)
80
"
82
also did not
show significant effects of either vitamin 0
2
or D
3
supplementation (daily doses ranged from 400
IU to 822 IU) in reducing the risk of total fractures or falls in elderly populations (?:.71 years old).
109
Detailed presentation (Tables 35 & 36).
Ottawa EPC Report: Fractures - Postmenopausal women or elderly men.
Overall, there is inconsistent evidence for an association between serum 25(0H)D
concentrations and the risk of fractures. Fifteen studies (three prospective cohorts and twelve
case-controls) reported on the association between serum 25(0H)D concentrations and fracture
rates. One of three cohorts reported an inverse association between serum 25(0H)D
concentrations and fracture rates, and nine of twelve case-control studies found significantly
lower 25(0H)D concentrations in cases versus controls. Differences in results may be attributed
to whether all relevant confounders were controlled for and differences in baseline serum
25(0H)D concentrations. Other factors may also contribute to the heterogeneity, such as
diagnosis of fractures.
Ottawa EPC Report: Falls - Postmenopausal women or elderly men.
Overall, there is fair evidence of an association between lower serum 25(0H)D
concentrations and an increased risk of falls in institutionalized elderly. One study suggested a
serum 25(0H)D concentration below 39 nmol!L was associated with an increased risk of falls.
Five studies (one RCT, three cohorts and one case-control) evaluated the association between
serum 25(0H)D concentrations and risk of falls. One RCT, two of the three cohorts and one
case-control study reported an inverse association between serum 25(0H)D concentrations and a
risk of falls. In one cohort with a low percentage of vitamin D deficient participants, the
association did not persist after adjustment for age and illness severity. In another cohort with an
undetermined proportion of vitamin D deficient participants no significant association between
serum 25(0H)D concentrations and risk of falls was observed. One case-control study reported
no significant association between serum 25(0H)D concentrations and risk of falls after
adjusting for serum PTH.
Ottawa EPC Report: Performance measures - Postmenopausal women or elderly men.
Overall, there is inconsistent evidence for an association of serum 25(0H)D concentrations
with performance measures. In studies that reported an association, specific concentrations
below which, declines in performance measures were increased, ranged from 50 to 87 nmol/L.
Seven studies (three RCTs and four cohorts) assessed the relation between 25(0H)D
concentrations and performance related measures. Two of the three RCTs and two of the four
cohorts reported an association between 25(0H)D concentrations and performance measures.
The other studies did not fmd an association between 25(0H)D concentrations and perfonnance
measures.
Additional RCTs published after the Ottawa EPC report.
We identified three additional RCTs (published after the Ottawa EPC report)
80
-
82
that
examined the effect of either vitamin D
2
or D
3
supplementation on total fractures, falls, or
performance in elderly populations (?.71 years old). All three RCTs were rated C. In two of the
three RCTs
80
'
81
calcium supplementation (800 or 1200 mg/d) was given to all participants.
Baseline serum 25(0H)D concentrations were less than 40 nmoVL. The other RCT did not
provide any information on background calcium intake or baseline serum 25(0H)D
concentrations.
82
All three RCTs reported no significant reduction in the risk of total fracture or
falls in elderly populations at daily vitamin D doses ranging from 400 IU to 822 IU.
80
-
82
Only
one of the three new RCTs among elderly reported data on performance measures. Vitamin D
supplementation (400 IU/d) improved gait speed and body sway in healthy elderly subjects.
80
110
Findings by life stage.
0-6 mo Not reviewed
7 mo- 2 y Not reviewed
3-8 y Not reviewed
9-18 y Not reviewed
19-SOy Nodata
51 - 70 y The Ottawa EPC report concluded that the associations between serum
25(0H)D concentrations and risk of fractures, falls, and performance measures are
inconsistent. There were no new data since the Ottawa report
~ 7 y Findings from three new RCTs did not show significant effects of either
vitamin D2 or D3 supplementation (daily doses ranged from 400 IU to 822 IU) in
reducing the risk of total fractures or falls among men and women in this life stage.
Postmenopause The Ottawa EPC rep01t concluded that the associations between
serum 25(0H)D concentrations and risk of fractures, falls, and performance measures are
inconsistent. There were no new data since the Ottawa report
Pregnant & lactating women Not reviewed
111
Table 35. Vitamin D and bone health: Characteri stics of RCTs published after the Ottawa EPC
re ort
Author Year Background
Study Name Calcium
Location Population Intake & Comparisons Compliance Comments
(l atitude) Vitamin D
[PMID] Data
Lyons 2007 Health Living in care nd Vit 02 100,000 IU 80% (percentage of
South Wales, status facilities including 4-monthly vs. occasions observed
UK some elderly with placebo to take tablets)
(52N) mobility, cognitive,
[17473911] visual, hearing or
communication
impairments
Mean 84 (62-107)
age
(range),
y
Male 23.7
(%}
Burleigh 2007
81
Health Inpatient with high 25(0H)D: 22.0 Vit D3 800 IU/ d + Ca group=87%, Vit
Scotland status levels of comorbidity, nmoi/L Ca carbonate D+Ca group=89%
(5557'N) mortality and 1200 mg/d vs. Ca (total study drug
[17656420) polypharmacy carbonate 1200 taken/ total study
Mean 83 (7.6) mg drug prescribed, as
age recorded in drug
(SO), y prescription charts)
Male 40
(%}
Bunout 2006su Health Healthy 25(0H)D: ~ 4 Ca 800 mg/d vs. 92% (tablet
Chile status nmoi/L Ca 800 mg/d + Vit counting)
(32S)
Mean 76 (4) D 400 IU/d (with
[16797903]
age
and without
(SD), y exercise training)
Male 11.6
1%!
112
Table 36. Vitamin D and bone health: Results of RCTs after the Ottawa EPC
Author Year
Life Interventions, Daily n N
Outcome
p
Study
Study Name Outcome 10/20 Mean Followup Metric Result 95% CI
l PMID]
Stage Dose Event Total
(ComEarisonl
Btw Quality
Lyons <!:71
First
10
Vii 0
2
-822 IUA 205 1670 HRVit 0.95 0.79,1 .15 NS c
2007
82
both
fracture D/ t:!lacebo
[ 17473911) sexes
Placebo 218 1673
"'"'"'"'"'"' "[
Burlei9h <!:71
Fall
10
Vit 0 3 800 IU + Ca 36 100 RR (Vit 0.82 0.59,1.16 NS c
2007
8
both
carbonate 1200 mg D+Ca)/Ca
[ 17656420) sexes
Ca carbonate 1200 45 103
I
m
Fracture
10
Median 1 (IQR Vii 0
3
800 IU + Ca 100 nd nd NS
15- 71 d} carbonate 1200 mg
Ca carbonate 1200 3 103
I m
Bun out <!:71 Fall
20
9 mo Ca800 mg 13 24 Fall free nd NS c
2006
80
both survival curve
[ 16797903) sexes Ca 800 mg + 6 22
exercise training
Vii D 400 IU + Ca
96
24
800 mg
Vit D 400 IU + Ca
8s
22
800 mg + Exercise
_
A Daily dose was calculated from the intermittent doses that were used in the study (i. e. , 100,000 IU tablets every 4 months}
8
Estimated from figure
113
Vitamin D and all-cause Mortality
Synopsis.
This synopsis is based on our reanalysis of a systematic review ofRCTs on vitamin D
supplementation for mortality. i In addition, it summarizes four observational studies on the
association of vitamin D and all-cause mortality.
Three RCTs from the previous systematic review and an additional Crated RCT were
included in our reanalysis. Three used daily doses that ranged between 400 and 880 IU, and one
used 100,000 IU every 3 months. Our meta-analysis of the 4 RCTs (13,833 participants) shows
absence of significant effects of vitamin D supplementation on all-cause mortality (RR = 0.97,
95 percent Cl: 0.92, 1.02; random effects model). There is little evidence for between-study
heterogeneity in these analyses.
One cohort study (rated B for methodological quality) found a significant trend for lower
odds for death with increasing 25(0H)D concentrations. Three other cohort studies did not find a
significant association between 25(0H)D concentrations and all-cause mortality. These three
studies were rated C for their methodological quality.
The above are applicable to older (50-70 y) and elderly (?..71 y) men and women (mean age
was >70 yin the included studies).
Detailed presentation (Tables 37, 38 & 39).
As mentioned in the Methods section, we updated and reanalyzed published meta-analyses of
mortality outcomes. We drew our own conclusions based on our analyses. We also comment on
the concordance of our conclusions with those of the published meta-analyses.
Relevant published systematic reviews of RCTs (with meta-analyses).
We identified two systematic reviews (with meta-analyses) ofRCTs that summarized the
effect of vitamin D supplementation with or without calcium on mortality.
83
84
One systematic
review (Avenell 2008) examined only trials on fall prevention, and briefly described results on
mortality.
84
The second meta-analysis (Autier 2007) focused specifically on mortality.
83
It
included all RCTs identified in the first, as well as additional trials (which were not eligible for
the primary analysis of the Avenell 2008 systematic review, namely prevention of falls).
83
Therefore, the Autier 2007 meta-analysis was used as the basis for our reanalysis.
Table 37 summarizes the findings ofthe Autier 2007 systematic review.
; Numerical data were extracted from previous systematic reviews -no additional studies were identified. For this reason, we did not
appraise studies for their methodological quality.
114
Table 37. Summary of systematic review on vitamin D supplementation and all-cause mortality
Author Year [PMID] Autier 2007
89
[17846391)
Design (Search Years) Randomized controlled trials (1992-2006}
Population Community dwelling or institutionalized adults
Intervention (Exposure) Supplementary vitamin D (at least 1000 mg/d) without calcium vs. placebo or no treatment
and Comparator
Results
Comments
A priori design?
18 trials of combined vitamin D and vitamin D + calcium
RR: 0.93 (95% Cl 0.87, 0.99); favoring vitamin D (calcium) supplementation
Statistically homogeneous
In our reanalysis we and excluded 3 of 18 trials and separated studies with vitamin D only from
those with vitamin D and calcium combination.
For details and results of our reanalysis, see text.
See text in vitamin D and vitamin D + calcium sections for reanalyses of the separated trials.
Study participants, vitamin D assays, and vitamin D status are not described in detail.
AMST AR Criteria
Yes Study quality assessment performed? No
Two independent reviewers?
Comprehensive literature search?
No Study quality appropriately used in analysis? NA
Yes Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
Yes Publication bias assessed? No
No Conflicts of interest stated? Yes
Yes The meta-analysis did not perform quality assessment
(neither using individual quality items nor using qual ity
scores)
Additional identified RCTs (not included in published systematic reviews).
Lyons 2007 (n=3343, 24 percent males) used monthly supplementation with 100,000 IU of
vitamin D
2
, orally for 3 years.
82
The trial took place in South Wales (latitude 5 2 N and
included older people (mean age 84 y) Jiving in sheltered accommodation. The primary outcome
was prevention of fractures. The Lyons 2007 RCT received grade "C" for the all-cause mortality
outcome, because of inconsistencies in the reported data. This RCT is included in the reanalysis
described below.
Reanalysis.
We excluded 5 of 18 trials in the Autier 2007 meta-analysis: One trial was on patients with
congestive heart failure,
85
one was published only in abstract form,
86
in one trial the controls also
received supplementation with vitamin D, albeit with a smaller dose,
87
and two trials used
vitamin D injections.
88
89
One additional eligible RCT (Lyons 2007)
82
was identified and
included in our meta-analysis.
Overall, four trials (13,899 patients) used only vitamin D supplementation without calcium.
Among the four trials, sample sizes ranged from 2578 to 5292 participants. Followup periods
ranged from 36 to 60 months. Vitamin D doses in most trials ranged between 400 and 830 IU per
day.
Overall, there were no significant effects of vitamin D supplementation on mortality. The RR
was 0.97 (95 percent CI 0.92, 1.02), with no evidence for between-study heterogeneity (P=0.39,
l =O percent).
Cohort studies.
We identified four prospective cohort studies described in 5 publications.
47
90
-
93
The
characteristics of the four cohorts are shown in Table 38. One was rated "B"
90
for
methodological quality and the remaining were rated "C".
Table 39 summarizes the findings of the four studies. Briefly, only Jia 2007
90
found a
statistically significant trend between increasing 25(0H)D concentrations and lower odds for all-
cause mortality (P=0.03). However, none of the odds ratios of the different 25(0H)D categories
was significant, and if anything, they suggest an U shaped relationship between 25(0H)D and
115
mortality. All other cohorts did not find significant associations. Melamed 2008
47
performed
analyses in subgroups of men and women, and <65 or ;?:65 years of age, and found no significant
associations (Table 33).
Findings by l ~ f e stage.
0- 6 mo No data
7 mo - 2 y No data
3 - 8 y No data
9 - 18 y No data
19 - 50 y A subgroup analysis of people younger than 65 years in NHANES III
(Melamed 2008) found no significant associations between 25(0H)D concentrations and
all cause mortality.
51 -70 y Overall, there were no significant effects of vitamin D supplementation on
mortality.
o In a random effects model meta-analysis of five RCTs (n=13,899) the summary
RR was 0.97 (95 percent CI 0.92, 1.02), with no evidence for between-study
heterogeneity (p=0.39, /
2
=0 percent). The mean participant age was more than 70
years in these RCTs.
o Overall, data from four cohorts suggest no association between baseline 25(0H)D
measurements and all-cause mortality (one coh01t found a statistically significant
trend for). A subgroup analysis of people aged 65 years or older in NHANES III
(Melamed 2008) found no significant associations between 25(0H)D
concentrations and all cause mortality.
~ 7 y The above (51- 70 y) are applicable.
Postmenopause No data
Pregnant & lactating women No data
116
Table 38. Vitamin D and all-cause mortalitx: Characteri stics of cohort studies
Confounders/Effect Modifiers
Author Year
Adjusted
Study Name
Vitamin D
.s::.
Location Population Comparisons
c.
:I
Concentration
Ill ftl
Ill
(Latitude) c c,
c.
'iij
0
Q)
0
c.
[PMID]
Q)
0 ... u ><
1:
E
.s::.
:0
Q) Ill
5 Q) c Q)
>
z
Q
cs: :::E ::1 ::::i
Jia 2007 Health Not Assay RIA Comparison of X X X X
status terminally ill method various 25(0H)D
UK or concentration
(57N) demented categories
[17442130) Age >75
range, y
Male 52 Season ND
(%) blood
drawn
Shambrook Health Not Assay RIA (Dia- Association with X X
2004 & 2006
91
'
92
status bedridden method sorin) log 25(0H)D
FREEA
Age >65
Australia range, y
(33S) Male 22 Season ND
[15531500 & (%) blood
16598375] drawn
Visser 2006
93
Health General Assay Competitive Comparison of X X X
Longitudinal status population
8
method protein various 25(0H)D
Aging Study
Age >65 binding concentration
Netherlands
range, y
categories
(52N)
Male 51 Season ND
[16960177) (%) blood
drawn
Melamed 2008
41
Health General Assay RIA (Dia- Comparison of X X X X X X
NHANES Ill status population method sorin) various 25(0H)D
us Age 45 (>=20} concentration
(various)
mean
categories
[18695076)
(range), y
Male 46 Season ND
(%) blood
drawn
A Fracture Risk Epidemiology in the Elderly
8
- 40% with CVD and -60% arthritis
117
Tabl e 39. Vitamin D and all-cause mortality: Results of cohort studies
Author Year Age Outcome Followup Vit D Concentration, No. of No. in Adjusted 95%CI P for Study
Study Name range, Duration Measure nmoi/ L Cases Category OR trend Quality
Location sex (Time t o
(Lati t ude) Dx)
[ PMID]
Jia 2007
96
>75, both Mortality 69 25(0H)D 6.0-23.0 (M)/ 41 75 1.74 0.91 ' 3.34 0.03 B
UK sexes 7.0-19.0 (F)
(57N)
[17442130)
2:ff3i:i':'o ...(M)7
"----M ....M ..OMMO_O_O_OO
34 86 1.40
...............................................
- --------------
30.1 -37.0 (M)/ 21 80 0.90 0.45, 1.79
...............................................
37.1 -47.0 (M)/ 17 78 0.80 0.39, 1.62
.............. 3.9.:.3..:3..l:l.:.Q.{ E.l ..........._
47.1 82.0 (M)/
16- """"""""""79'""""""'""
1.00 Reference
Shambrook 2004 & 200691.
92
39.1 -82.0 (F)
0.87
8
>65, both Mortality 27 25(0H)D NA 559 1112 0.75, 1.01 nd c
FREEA sexes
Australia
(33S)
[ 15531500 & 16598375)
Visser 2006
93
>65, both Mortality 72 25(0H)D <25 66 127 1.28 0.85, 1.92 0.19 c
Longitudinal Aging Study sexes
Netherlands
(52N)
[16960177]
...............................................
- -------------
25-49.9 42 462 1.00 0.72, 1.40
..........................so:7;r9 ........................
..............................................
- o-:-65.1:26 ...
30 440 0.91
...............................................
--Reiereilc_e .....
<:75 29 231 1.00
Melamed 2008 >20, both Mortality 104 25(0H)D <17.8 nd nd 1.26 1.08, 1.46 nd c
NHANES Ill sexes
us
(various)
[18695076)
- - -------------
17.824.3 nd nd 1.06
.......... ... ......... ............................................................... ...............................................
24.432.1 nd nd 0.93
........9 .. ..... . .............................................................
-
>32.1 nd nd 1.00 Reference
Melamed 2008 >20, men Mortality 104 25(0H)D <17.8 nd nd 1.04 0.83, 1.30 nd c
NHANES Ill only
us
(various)
[ 18695076)
- - -------------.
17.8-24.3 nd nd 0.94 ___ 9. 7,J.J..g_ __
...................... .....................
nd
""""""""""iid"'"'""""""'
0.82 ...... ..!..:Q9 ...._
-
>32.1 nd nd 1.00 Reference
continued
118
Author Year Age Outcome Followup Vit D Concentration, No. of No. in Adjusted 95% CI P for Study
Study Name range, Duration Measure nmoi/L Cases Category OR trend Quality
Location sex (Time to
(Latitude) Dx)
[PMID]
Melamed 2008
41
>20, Mortality 104 25(0H)D <17.8 nd nd 1.55 1.15, 1.98 nd c
NHANES Ill women
us only
(various)
[18695076]
fra:2;i":3 ;:;a ------------.......
nd 1.27 __ ____
-
24.4-32.1 nd nd 1.16 __ Q:.?., __ ____
............................................................. . ..............................................
>32.1 nd nd 1.00 Reference
Melamed 2008 20-65, Mortality 104 25(0H)D <17.8 nd nd 1.28 0.93, 1.76 nd c
NHANES Ill both
us sexes
(various)
[1 8695076)
- ------ --------
17.8-24.3 nd nd 1.13 ___9_:.!,..!.: ?.!3___
............................................................... . ..............................................
24.4-32.1 nd nd 0.81 0.58, 1.14
.............................................................
-
--'Reterenc_e __
>32.1 nd nd 1.00
Melamed 2008 both Mortality 104 25(0H)D <17.8 nd nd 1.26 1.03, 1.54 nd c
NHANES Ill sexes
us
(various)
[1 8695076)
...............................................
.......................1":ra:24:3 ....................
nd nd 0.99
...............................................
24.4-32.1 nd nd 0.97 0.79, 0.82
.............................................................
-
--Refer-ence_,
>32.1 nd nd 1.00
Fracture Risk Epidemiology in the Elderly
6
Per unit change in the log-transformed concentration.
119
Vitamin D and Hypertension and Blood Pressure
We searched for systematic reviews and primary studies that evaluated associations between
vitamin D supplementation or serum concentrations and incidence of hypertension and change in
blood pressure. For the outcome incidence of hypertension, we reviewed RCTs and other
longitudinal studies. For the outcome change in blood pressure, we reviewed only RCTs. The
EPC and the TEP agreed that due to the large volume of literature, the limited resources would
not be expended on reviewing observational studies for the surrogate outcome blood pressure.
We included only studies of adults. Studies of pregnancy-related hypertension and blood
pressure control are included in the "Pregnancy-related outcomes" section.
Hypertension.
Synopsis.
No systematic reviews evaluated the association between vitamin D intake or serum
25(0H)D concentrations and incidence of hypertension. A combined analysis of a small subset
of the Health Professionals Follow-up (HPFS) and Nurses Health Studies (NHS) evaluated the
association with serum 25(0H)D concentrations. The analysis found higher incidence of
hypertension at 4 and 8 years in men with baseline 25(0H)D concentration less than 37.5 nmol!L
(OR- 3-6). In women, serum 25(0H)D concentrations less than 37.5 nrnol!L also had a
significantly higher incidence of hypertension at 4 years (OR- 3), but not at 8 years (OR- 1.5).
Detailed presentation (Tables 40 & 41 ).
One analysis (methodological quality B) evaluated the incidence of hypertension in a
combined set of 613 men from the HPFS and 1198 women from the NHS who had serum
25(0H)D concentrations measured.
94
The men were on average 65 years old and the women 57
years old. Among the men at 4 years, those with serum 25(0H)D concentrations less than 37.5
nmol/ L were significantly more likely to have new onset hypertension than either men with
25(0H)D concentrations above 75 nmol/L (OR=6.1) or above 37.5 nrnol!L (OR=5.7). The
association remained significant at 8 years, although with a smaller effect size (OR=3.5 and 3.0,
respectively). In women, a similar, though weaker, effect was seen at 4 years, such that those
with 25(0H)D concentrations less than 37.5 nmol/L were significantly more likely to have new
onset hypertension than either women with 25(0H)D concentrations above 75 nmol/L (OR=2.7)
or above 37.5 nrnol/L (OR=3.0). However, this effect was smaller and nonsignificant at 8 years
(OR=1.7 and 1.4, respectively). The study was limited primarily by its inclusion of only a
relatively small subset of participants and its reliance on self-reported hypertension without
assessment of blood pressure measurements.
In the second analysis by the same investigators, the NHS 2 study was analyzed for the
association between serum 25(0H)D concentration and hypertension as a nested case-control
study.
95
These women were on average 43 years old. Cases and controls (per the 2005 biennial
questionnaire) were chosen from among those women without hypertension, cardiovascular
disease, diabetes, obesity, or cancer at baseline (blood samples drawn from 1997 to 1999). After
approximately 7 years, a statistically significant trend was found such that women in the three
quartiles with serum 25(0H)D concentrations of 80.5 nmol/L or less were about 50 to 60 percent
more likely to develop hypertension than those women with higher serum concentrations of
25(0H)D (adjusted OR = 1.52 to 1.66, each of which was statistically significant compared to
120
the highest quartile). The study was graded methodological quality B for similar reasons as the
analysis of the HPFS and NHS studies.
Findings per vitamin D concentration.
The HPFS and NHS studies were analyzed with 25(0H)D cutpoints of37.5 and 75 nmol/L.
Significant associations were found for those with serum concentrations below 37.5 nmol/L. The
NHS 2 study was analyzed with 25(0H)D quartiles, such that significant associations were found
for those with serum concentrations of 80.5 nmol/L or less.
Findings per age and sex.
See above Detailed presentation of the HPFS and NHS for the separate analyses by sex. No
subgroup analyses were reported by life stage. The participants in the studies were approximately
40 to 80 years old.
Findings by ~ f e stage.
0 - 6 mo Not reviewed
7 mo - 2 y Not reviewed
3 - 8 y Not reviewed
9-18 y Not reviewed
19 - 50 y The NHS 2 included all women within the life stage. After approximately
7 years, those with serum 25(0H)D concentrations of 80.5 runol/L or less were about 50
to 60 percent more likely to develop hypertension.
51 - 70 y HPFS and NHS included participants mostly within this life stage. In men
and women, the study found higher incidence of hypertension at 4 years followup in
those with serum 25(0H)D concentrations less than 37.5 nmol/L; at 8 years, the
association was significant only for men.
~ 7 y A minority of the men and few of the women appear to have been in this
life stage. No unique conclusions are possible for this life stage separate from those for
people 51 to 70 years.
Postmenopause The majority of the women in NHS were postmenopausal. A
significant association between serum 25(0H)D concentrations less than 37.5 nmol/L and
increased hypertension was found at 4 years, but not 8 years followup.
Pregnant & lactating women Not reviewed
121
Table 40. Vitamin D and Characteristics of cohort studies
Confounders/Effect Modifiers
Author Year
AdJusted
Study Name
Vitamin D
.s::.
Location Population Comparisons
Q. :I
Comments
Concentration
Ill
Ill
(Latitude) E
Q.
(ij
0 Cll
0)
0
Q.
[PMID]
Cll
0 ... u ><
;:
E
.s::.
:0
Cll Ill
'5 Cll E Cll
>
z 0 <1: :: ::1 :::i
Forman Health Any Assay RIA Hypertension X X X
2007
94
status method incidence
HPFS, NHS
Mean Men 65 (8) stratifi ed by
us age (SO), Women 57 25(0H)O
(various)
y (7) categories (2
[17372031 )
Male 34 Season All
and 3
(%) blood
categories)
drawn
Health No HTN, Assay EIA Hypertension X X X X
status CVO, OM, method incidence
Forman obesity, stratified by
2008
95
cancer 25(0H)O
NHS2 Mean 43 (40-46) categories (2
us age (SO), and 3
(various) y categories)
[18838623)
Male 0 Season All
(%) blood
drawn
122
Table 41. Vitamin D and hypertension: Results of cohort and nested case control studies
Author Year
Study Name
[PMID]
Men
Forman 2007
94
HPFS
[17372031]
Women
Forman 2008
95
NHS2
[18838623)
Forman 2007
NHS
[17372031]
Mean (SO) Outcome
Age, Sex (n/N; Incidence)
65 (8),
Men
43 (40-46,
range) ,
Women
57 (7),
Women
Hypertension
(61/613; 0.100)
Hypertension
{131/613; 0.214)
Hypertension
(742 cases; 742
controls)
Nested case
control
Hypertension
(129/ 1198; 0.108)
Hypertension
(274/613; 0.229)
Followup
Duration
4y
8y
-7 y
4y
8y
Vit D
Measure
25(0H)D
25(0H)D
25(0H)D
25(0H)D
25(0H)D
Concentration,
nmoi/L
<37.5
__ --'<. 37.57."- 5 __
__ _
<37.5
37.5-75
<37.5
41.75 (15.5-52.5)
59.5 (52.75-66.25)
73.0 (66.5-80.5)
94.75 (80.75-224)
<37.5
37.5-75
<37.5
<37.5
37.5-75
___ <37_.5 ___ _
Statistically significant (P<0.05)
A Due to formatting error in study table, no data on numbers of women in each category.
123
No. of
Cases
6
33
22
6
55
9
nd
nd
9
124
208
188
195
151
11
60
58
11
118
20
nd
nd
20
254
No. in
Category
Adjusted
OR
33 6.13
95%CI
1.00, 37.8*
--------------,:-c:::-
--2..4.?. ............__ 1 .12__ (),!)1,?:4.?.
233 1 Reference
.... 1.01, 32.3*
580 1 Reference
33 3.53 1.02, 12.3*
-------- 247 ----------nd-:--- nd
---------------- .................................
233 1 Reference
371
370
374
369
1.66
1.55
1.52
1
ndA 2.67
1.11 , 2.48
1.07, 2.23
1.06, 2.18
Reference
1.05, 6.79*
..... f.l<:l ____ __ 0._85__
nd 1 Reference
ndA 1.70 0.92, 3.16
................... f.l<:1................._ ___.: 1.;_ . 4:..:: 2___.:_ ?:?.>
nd 1 Reference
P for
Trend
nd
<0.05
nd
NS
0.01
nd
<0.05
nd
NS
Study
Quality
B
B
B
Vitamin D and blood pressure.
Synopsis.
No qualified systematic reviews have evaluated the association between vitamin D intake or
serum 25(0H)D concentrations and changes in blood pressure. Three trials from Germany, UK,
and India compared different doses ofvitamin D (800 IU daily, a single dose of 100,000 IU, or
120,000 IU every 2 weeks) with placebo, with or without supplemental calcium in both groups.
The study participants also varied: either older men, older men and women, or men mostly in
their 40s. Both recruited older adults (over 63 or 70 years). All trials reported no significant
effect on diastolic blood pressure. The A quality British study of a single dose of vitamin D
100,000 IU found no difference in systolic blood pressure after 5 weeks. The B quality German
study found a significant net reduction of 7 mm Hg after 8 weeks in older women taking vitamin
D 800 IU daily. The B quality Indian study of obese men mostly in their 40s, found a nearly
significant net increase of 4 mm Hg after 6 weeks of vitamin D 120,000 IU every 2 weeks. No
long term data were available.
Detailed presentation (Tables 42 & 43 ).
The A quality trial of single-dose vitamin D, performed in Cambridge, UK, recruited older
adults (63 to 76 years, mean 70 years) who were not taking antihypertensive medications.
96
During the winter, they were given either a one-time dose of vitamin D
3
(100,000 IU (2.5 mg])
or placebo, and blood pressure was rechecked at 5 weeks. In both study arms, systolic and
diastolic blood pressures fell by equal amounts, resulting in no net difference between vitamin D
supplemented and placebo groups. No subgroup analyses were reported.
The German B quality trial of supplementation with combined vitamin D and calcium versus
calcium alone recruited older women (70 to 86 years) without severe hypertension.
97
For 8
weeks, the women took either vitamin D
3
800 IU and calcium carbonate 1200 mg or calcium
carbonate 1200 mg alone daily. Systolic blood pressure decreased by 13 mm Hg in those
supplemented with vitamin D and calcium compared with a 6 mm Hg decrease in those taking
calcium alone (P=0.02). Diastolic blood pressure declined by 7 mm Hg in both groups. No
subgroup analyses were reported. The study was limited by inadequate reporting of its study
methods and lack of blinding.
The Indian B quality study compared every other week vitamin D3 supplementation 120,000
IU with placebo for 3 weeks in generally healthy but obese men without hypertension. 5
1
The men
who received the vitamin D supplements had a net increase in systolic blood pressure of 4 mm
Hg, which was close to statistically significant (P=0.06), but no significant difference in diastolic
blood pressure. The study was limited by a high dropout rate (26 percent).
Findings per intake level.
No conclusions can be reached about an intake level threshold. In individual trials, a single
dose of 100,000 IU of cholecalciferol had no significant effect on systolic and diastolic blood
pressure after 5 weeks, a daily dose of vitamin D
3
800 IU together with calcium significantly
lowered systolic blood pressure more than calcium alone, but every other week vitamin D
3
120,000 IU resulted in a nearly statistically significant increase in systolic blood pressure.
Findings per age and sex.
No conclusions can be reached about differences in effect based on age or sex. The study of
older women found a significant decrease in systolic blood pressure with relatively low dose
124
Findings by life stage.
0 - 6 mo Not reviewed
7 mo- 2 y Not reviewed
3-8 y Not reviewed
9 - 18 y Not reviewed
19 - 50 y A single study of men in this life stage found a near significant increase in
systolic blood pressure with vitamin D and no effect on diastolic blood pressure.
51 - 70 y One trial included people with an average age of 70 years, implying that
about half were within this life stage. No significant effect on blood pressure was found
of a single large dose of vitamin D.
~ 7 y Both trials included people within this life stage. The trial of people with
an average age of 70 years found no significant effect of a single large dose of vitamin D.
The single trial of women over age 70 years found a significant benefit for systolic blood
pressure for vitamin D3 800 IU and calcium carbonate 1200 mg compared with calcium
carbonate I 200 mg alone.
Postmenopause The women in both trials were postmenopausal. See the ~ 7 y life
stage.
Pregnant & lactating women Not reviewed
125
Table 42. Vitamin D and blood pressure: Characteristics of RCTs
Author Year
Study Name Background
Location Population Calcium Intake & Comparisons Compl iance Comments
(Latitude) Vitamin D Data
[PMID]
Scragg 1995
96
Health NoHTN 25(0H)D: 34.5 Vit 03 100,000 nd Complete trial
Cambridge, UK status nmoi!L (treatment IU (2.5mg) performed in
(52N)
Mean 70 (63- group), 32.25 nmoi!L one-time dose winter
[7498100]
age 76) (control group) vs. Placebo
(range) , y
Male 46%
(%}
Pfeifer 2001
97
Health Healthy, 25(0H)D <50 Vit 03 + Ca 951 2% for the Ca
Lower Saxony, status lowVit D nmoi!L supplement vs. tablets and 961 0%
Germany
Mean 75 (70- Ca supplement for the Vit 0
3
+ Ca
{52N)
age 86) tablets (pill counting)
[1 1297596]
(range), y
Male 0
%
Health Healthy, 25(0H)D: 36.5 Vit 03 120,000 100% (implied); Excluded
Nagpal 2009
51 status obese nmoi!L (treatment IU every 2 supervised home subjects who
New Delhi, India
Mean 44 (8) group), 30.0 nmoi/L weeks vs. visits refused
(28.SON)
age (SD), (control group) Placebo subsequent blood
[19125756]
y draws
Male 100%
(%)
126
Table 43. Vitamin D and blood Results of ACTs
Author Year Age
Mean Interventions, No. Change Net Net Diff
p
Study
Study Name Range, Outcome
10/20
Follow up Daily Dose Analyzed
Unit Baseline Change
95% CI Diff 95% CI Btw Quality
l PMID] Sex
SYSTOLIC BLOOD PRESSURE
63-76 y, SBP
10
5wk Vii 03 100,000 A
1995 Both IU (2.5 mg), 1 95
mm
149 -5 -14.4, 4.4A 0 -4.2, 4. 2A 0.81
UK dose
Hg
[7498100] Placebo 94 147 -5 -17.9, 7.9"
Pfeifer
70-86 y, SBP
10
8wk Vii 03 800 IU B
Women +Ca carbonate 73
mm
144.1 -13.1 nd -7.4 -13.6, -1.2A 0.02
2001
97
Hg
Germany
1200 mg
[1 1297596]
Ca carbonate
72 140.6 -5.7 nd
1200 m
44 (8, SBP
20
6wk Vit 03 120,000
35
mm
124 +0.6 -2.7, 3.9 +4.0 -0.02, 8.0 0.06
8
SO) IU 2 wk Hg
Men
Placebo 36 124 -3.4
10
5wk Vii 03 1 00,000
mm
A
IU (2.5 mg) , 1 95
Hg
82 -1 -6.8, 4.8A 0 -2.8, 2.8A 0.92
dose
-
Placebo 94 82 -1 -6.8, 4.8
Pfeifer
70-86 y, SBP
10
8wk Vii 03 800 IU 8
Women +Ca carbonate 73
mm
84.7 -7.2 nd -0.3 -0.7, -0.1A 0.10
2001
97
Hg
Germany
1200 mg
---------
[ 11297596]
Ca carbonate
72 82.6 6.9 nd
1200 m
Nagpal 44 (8, SBP
20
6wk Vit 03 120,000
35
mm
78 +0.4 -2.1, 3.0 +1.7 -1.5, 4.9 0.31
8
2009
51
SO) IU every 2 wk Hg
New Delhi, Men
------------ ---------
r
India Placebo 36 77 -1.3 -3.2, 0.7
k19125756j
Estimated from available data
127
Vitamin D and Bone Mineral Density or Bone Mineral Content
For bone health outcomes (e.g., bone mineral density, fracture, fall or muscle strength), we
relied on a recent comprehensive systematic review performed by the Ottawa EPC (Table 28).
6
Because the Ottawa's EPC report did not have separate analyses on the effect of vitamin D
supplementation alone, the results for the effect of vitamin D alone or in combination with
caJcium supplementation are presented in "Combined vitamin D and Calcium" section.
The Ottawa EPC report was updated with literature published between January 2006 and
September 2008, selected according to our eligibility criteria. For adults, we included only bone
mineral density (BMD) indices. For children, we included only bone mineral content (BMC)
indices. Only RCTs with duration more than 1 year qualified for inclusion.
Synopsis.
The Ottawa EPC report concluded that observational studies suggested a correlation between
higher serum 25(0H)D concentrations and larger values ofBMC indices for older children and
adolescents (6 months through 18 years old). Furthem1ore, Based on results of the observational
studies, there is fair evidence to support an association between serum 25(0H)D and BMD or
changes in BMD at the femoral neck in postmenopausal women and elderly men. However, there
was discordance between the results from RCTs and the majority of observational studies.
6
Three
new RCTs identify from our updated search all showed no significant effects of vitamin D
supplementation on BMC or BMD in children or adults, respectively.
Our updated search did not identify any new RCTs examining the effect of vitamin D on
BMD and related outcomes in pregnant or lactating women.
Detailed presentation (Tables 44 & 45 ).
Ottawa EPC Report: Bone mineral content- Infants (0 through 12 months).
Overall, there is inconsistent evidence for an association between a specific serum 25(0H)D
concentration and the bone health outcome BMC in infants. Of the two RCTs examining BMC,
one demonstrated no significant benefit of higher serum 25(0H)D concentrations on radial bone
mass while the other showed a transient increase ofBMC compared to the unsupplemented
group at 12 weeks but not 26 weeks. Of the three case-control studies, greater whole body BMC,
was related to higher serum 25(0H)D concentrations.
Ottawa EPC Report: Bone mineral content or density- Older children (6 months through before
puberty) and adolescents (the onset of puberty through 18 years).
Overall, there was fair evidence of an association between 25(0H)D concentrations and
baseline BMD and change in BMD or BMC indices from the studies in older children and
adolescents. However, the results from two RCTs of vitamin D supplementation have not
confirmed a consistent benefit on BMD or BMC across sites and age groups.
There were seven studies in older children and adolescents (two RCTs, three cohorts, one
case-control and one before-after study) that evaluated the relationship between serum 25(0H)D
concentrations and BMC or BMD. 1n older children, there was one RCT, one prospective cohort
and one before-after study. One RCT did not find an association between serum 25(0H)D
concentrations and distal radial BMC. Two of three studies found an association between lower
baseline serum 25(0H)D concentrations and lower BMC or BMD. The effect of bone size and
muscle mass on these outcomes in relation to baseline serum 25(0H)D concentrations was not
reported. One RCT demonstrated a significant relation between baseline serum 25(0H)D
128
concentrations and baseline BMD of the lumbar spine, femoral neck and radius. However, only
high dose supplementation with 14,000 IU/wk ofvitamin D
3
increased BMC of the total hip.
Ottawa EPC Report: Bone mineral density- Postmenopausal women and elderly men.
Overall, there was discordance between the results from RCTs and the majority of
observational studies that may be due to the limitations of observational studies to control for all
relevant confounders. Five RCTs, and three cohort studies did not find an association between
serum 25(0H)D concentrations and BMD or bone loss. Four cohort studies found a significant
association between 25(0H)D concentrations and bone loss, which was most evident at the hip
sites but the evidence for an association between 25(0H)D concentrations and lumbar spine
BMD was weak. Six case-control studies suggested an association between 25(0H)D
concentrations and BMD and the association was most consistent at the femoral neck BMD.
Based on the results from the observational studies, there is fair evidence to support an
association between serum 25(0H)D and BMD or changes in BMD at the femoral neck. Specific
circulating concentrations of25(0H)D below which bone loss at the hip was increased ranged
from 30-80 nmol/L.
Ottawa EPC Report: Bone mineral density- pregnant or lactating women.
One coh01t study did not find an association between serum 25(0H)D concentrations and
change in BMD that occurred during lactation. Limitations in the study design and sources of
bias highlight the need for additional research on vitamin D status in pregnancy and lactation,
and the association with bone health outcomes.
Additional studies published after the Ottawa EPC report.
One A quality RCT compared the effect of vitamin D
2
supplementation on hip BMC in 256
elderly women between 70 and 90 years of age.
98
All elderly women in this trial had normal
physical functioning. They were randomly assigned to receive either vitamin D
2
(1000 IU/d) plus
calcium (1200 mg/d) supplement or calcium (1200 mg/d) supplement alone for one year. The
mean baseline dietary calcium intake was I 097 mg/d and mean 25(0H)D concentration was 44.3
nmol/L. Total hip BMD increased significantly in both groups, with no difference between the
vitamin D
2
plus calcium and calcium alone groups (hip BMD change: vitamin D, +0.5 percent;
control , +0.2 percent).
One B quality RCT analyzed 89 and 83 healthy adult women and men separately.
99
The
participants were Pakistani immigrants living in the Copenhagen area of Denmark (latitude 55
N). Women and men were randomly assigned to receive either daily dose of 400 IU or 800 IU
vitamin D
3
, or placebo for one year. For women, the mean baseline dietary calcium intake was
495 mg/d and mean 25(0H)D concentration was 12 nmol/L. For men, the mean baseline dietary
calcium intake was 548 mg/d and mean 25(0H)D concentration was 21 nmol/L. At the end of
study, in both women and men, there were no significant differences in lumbar spine BMD
changes between the two doses of vitamin D
3
( 400 Wi d or 800 IU/d) and the placebo groups.
Two RCTs, both rated C, compared the effect of vitamin D supplementation on BMC in
healthy girls, aged between 10 and 17 years old.
35
99
First RCT analyzed 26 healthy girls, who
were Pakistani immigrants primarily living in the Copenhagen area Denmark (latitude 55 N).
99
Girls were randomly assigned to receive either daily dose 400 IU or 800 ru vitamin D
3
, or
placebo for one year. The mean baseline dietary calcium intake was 510 mg/d and mean
25(0H)D concentration was 11 nmol/L. At the end of study, there were no significant
differences in whole body BMC changes between the two doses of vitamin D3 (400 IU/d or 800
ill/d) and the placebo groups. Second RCT analyzed 168 healthy girls, living in the Greater
129
Findings by life stage.
0 - 6 mo The Ottawa EPC report concluded that there is inconsistent evidence for
an association between a specific serum 25(0H)D concentration and the bone health
outcome BMC in infants. There were no new data since the Ottawa report.
7 mo - 2 y The Ottawa EPC report concluded that there was fair evidence of an
association between 25(0H)D concentrations and baseline BMD and change in BMD or
BMC indices from the studies in older children and adolescents. There were no new data
since the Ottawa report.
3 - 8 y The Ottawa EPC report concluded that there was fair evidence of an
association between 25(0H)D concentrations and baseline BMD and change in BMD or
BMC indices from the studies in older children and adolescents. There were no new data
since the Ottawa report.
9 - 18 y The Ottawa EPC report concluded that there was fair evidence of an
association between 25(0H)D concentrations and baseline BMD and change in BMD or
BMC indices from the studies in older children and adolescents. Two new RCTs enrolled
only girls in this life stage. The results showed no significant differences in whole body
BMC changes between either lower doses of vitamin D (200 or 400 IU/d) or higher dose
of vitamin D (800 or 2000 IU/d) and the placebo groups.
19 - 50 y The Ottawa EPC report concluded that there was discordance between the
results from RCTs and the majority of observational studies in postmenopausal women
and elderly men. Based on results of the observational studies, there is fair evidence to
support an association between serum 25(0H)D and BMD or changes in BMD at the
femoral neck. One new RCT enrolled primarily men and women in this life stage. The
results showed that there were no significant differences in lumbar spine BMD changes
between the two doses of vitamin D
3
( 400 JU/d or 800 IU/d) and the placebo groups.
51 - 70 y The Ottawa EPC report concluded that there was discordance between the
results from RCTs and the majority of observational studies in postmenopausal women
and elderly men. Based on results of the observational studies, there is fair evidence to
support an association between serum 25(0H)D and BMD or changes in BMD at the
femoral neck. One new RCT enrolled some men in this life stage. The results showed that
there were no significant differences in lumbar spine BMD changes between the two
doses of vitamin D3 ( 400 IU/d or 800 IU/d) and the placebo groups.
~ 7 y The Ottawa EPC report concluded that there was discordance between the
results from RCTs and the majority of observational studies in postmenopausal women
and elderly men. Based on results of the observational studies, there is fair evidence to
130
support an association between serum 25(0H)D and BMD or changes in BMD at the
femoral neck. One new RCT enrolled only elderly women in this life stage. The results
showed that vitamin D2 supplementation (1000 IU/d) had no additional effect on hip
BMD compared to calcium supplementation alone.
Postmenopause There were no new data since the Ottawa report.
Pregnant & lactating women There were no new data since the Ottawa report.
131
Table 44. Vitamin D and bone mineral density: Characteristics of ACTs published after the Ottawa
EPC r ~ o r t
Author Year Background
Study Name Calcium
Location Population Intake & Compari sons Compliance Comments
(Latitude) Vitamin D
[PMID] Data
Zhu 2008gg
Health nd (based on the inclusion and 25(0H)D: Vii 02 1000 86.7%and
Perth, Australia status exclusion criteria, assume subjects 44.3 nmoi/L IU/d + Ca 86.8% in the
(32 S) were not very healthy but normal citrate 1200 vitamin D
[1 8410225) physical functioning) Ca: 1097 mg/d vs. Ca and the
Mean 77 (4.5) mg/d citrate 1200 control
age mg/d groups
(SD), y (tablet
Male 0 counting)
%
Andersen Health Healthy 25(0H)D: Vit D3 400 The median Pakistani,
2008
99
status Adolescent IU/d, or Vii D3 compliance living in
Copenhagen,
Mean Adolescent girls: 12.2 (10. 1-14.7) girls: 11 800 IU/d VS. was 85 Denmark.
Denmark (55 age Women: 36.2 (18.1-52.7) nmoi/L placebo (range 43- Compliance
W) (range), Men: 38.3 (17.9-63.5) Women: 12 100), 92 was lower
[18208636) y nmoi/L (42 11 5) for girls.
Male 42
Men: 21 and 93 (33-
(%)
nmoi/L 105)% for
girls,
Ca: women, and
Adolescent men,
girls: 510 respectively
mg/d (pill
Women: 495 counting)
mg/d
Men: 548
mg/d
EI-Hajj 2006
35
Health Healthy 25(0H)D: Weekly oral Placebo -
Beirut, Lebanon status 34.9 nmoi/L Vit D doses of 98%, Low
(3353'N) Mean 13.2 (10-17) 1400 IU (=Vit dose group -
[16278262) age Ca: 677 D 200 IU/d) 98%, High
(range), mg/d or 14,000 IU ( dose group -
y Vit D 2000 97%(pill
Male 0
IU/d) vs. counting)
(%l
placebo
132
Table 45. Vitamin D and bone mineral density or bone mineral contents: Results of RCTs published after the Ottawa EPC report
Author Year
Study Name
Location
(Latitude)
[PMID]
Zhu 2008M
Perth,
Australia
(32 sJ
[18410225)
Andersen
2008
99
Copenhagen,
Denmark (55
N)
[18208636)
Andersen
2008
99
Copenhagen,
Denmark (55
N")
[1 8208636)
Andersen
2008
99
Copenhagen,
Denmark (55
N)
[18208636)
EI-Hajj 2006
35
Beirut,
Lebanon
(33N)
[16278262)
Life Stage
71+. Women
only
18-53, Women
only
18-64, Men
only
10-15 y girls
10-17 y girls
Subgroup-
Premenarcheal
girls, mean
age 10 y
Outcome
Hip BMD
Lumbar
spine
BMD
Lumbar
spine
BMD
BMC
BMC
BMC
1/2
10
1
1
1
10
Mean
Followup,
mo
12
12
12
12
12
12
Interventions,
Daily Dose
Vit D2 1000 IU
+ Ca citrate
No.
Analyzed
123
Unit Baseline
mg/cm
2
851
Change
0.5%
Change
95% CI
-0.09,
1.09
Net
Diff
0.3%
Net Diff
95% CI
nd
p
Btw
NS
Ca citrate 133 826 0.2% -0.19,
1200 mg 0.59
Vit Da 40"'- 0 __ ___!: 3Q/21A
. _ __,0<.!.: % _ _ __ -,., 1-" %"-------"n""- d
___ 3;::..; 0'"" /2=-1'---------------------- 0.98 1% nd r% nd
Placebo 29/ 18 0.99 1% nd I
NS
Vit D'l.,., 4"" 00,_ __ _:2:::: 5""' / 1'=" 9'- A- _ _.!. 1 '-'= "0""- 3 __ -=2,., Yoc_ _ __,n_, d'----=- O !.::! Yoc_ _ __,n_, d'--- .NS
Vit Da'-' 8:..: 0c::. 0 ___ .._ .._ .._ .._ .._ .._ .._ .._ ..._ ___::. 0:..:: .9.= 2 __
Placebo 27/ 19 1.03 2% nd
Vit D3 400 917A ... _._ _,_1_,_, .3'----'2,_ 2!.::! Yoc_ _ ____,_,_ nd"'---_ __ ____,_,_ nd"'- NS
Vit 0
3
80"'- 0-----" 9/7 1.5 10% nd -5% nd
........................... __ .....
Placebo 8/7 1.7 15% nd
---'- V"- it ..:,; 1 U"---__ 1 . 2 6. 2% 4. 7, 7. 7 0.1% -1 .1 , 2.0c NS
---"- V:..:.. it ..::: D...;: 2:..:: 0..::. 0...:.. 1U =--___ 5 ::..: 8:;___ ........................... _ ___:.; 4c.:: 6,_ , 3=.2=e==N=S=
Placebo 55 1.1 5.0% 3.8, 6.2
Vii D 2000 IU 14 kg 0.8 11 .6%
9.4,
4.2% 0.7, 7.7c NS
13.8
Vit D 200 IU 12 0.7 11.4%
9. 1,
4.0%
13.7
0.5, 7.5c NS
"MMMMMMMMMMMMM .. MMMM
Placebo 8 0.8 7.4%
4.7,
10. 1
A Baseline/final sample size
9
Downgraded to C because very small sample size (insufficient power) and no adjustments for confounders
c Estimated from available data
133
Study
Quality
A
8
8
c
Calcium and Health Outcomes
Calcium and Growth
We reviewed systematic reviews and primary studies that evaluated relationships
between calcium intake and growth parameters in infants and children.
Synopsis.
One systematic review and three primary studies evaluated supplemental intake of
calcium and growth parameters in infants and children. The systematic review with a
meta-analysis of 17 RCTs did not find an effect on weight and height gain attributable to
calcium supplement in children ranging from 3 to 18 years of age. Three additional
primary studies reported similar findings. Overall, the studies reviewed did not find a
relationship between supplemental calcium intake and growth parameters.
Detailed presentation (Tables 46, 47 & 48).
0 - 6 months; 3 - 8 years; 9 - 18 years; pregnant women.
One systematic review ofRCTs of supplemental calcium on bone related outcomes in
children (age 3-18 y) also examined changes in height and weight at followup.
100
The
systematic review (comprised of studies in Australia, China, Gambia, Israel, Switzerland,
and US) conducted a meta-analysis of 17 RCTs with a total of2088 subjects and found
no significant difference in weight (weighted mean difference +0.14 kg (favors
contro1)(95 percent CI -0.28, +0.57 kg)) and height gain (weighted mean difference +0.22
em (favors control)(95 percent CI -0.30, +0.74 em)) between those who were and those
who were not supplemented. There was no significant statistical heterogeneity in the
included studies. The calcium intake ranged from 300 to 1200 mg/d lasting from 0.7 to 4
years. The majority of the supplement used was calcium carbonate. This systematic
review met seven of I 1 AMSTARi quality checklist items.
Two primary studies rated B in methodological quality and one primary study rated C
provided additional information. One RCT from Denmark randomly assigned 110 girls
(mean age 13 years) with either low (<713 mg/d) or medium (1000 to 1304 mg/d)
habitual calcium intake to a supplement of calcium 500 mg/d (calcium carbonate) or
placebo for 1 year.
101
There was no significant difference in height or weight gain among
the groups at followup. One post hoc analysis of an RCT in Nebraska on bone mass
analyzed 59 girls (mean age 9.5 years) who were randomly assigned to either a calcium
enriched diet, supplying at least 1500 mg of calcium per day ( - 1656 mg/d), or usual diet
(961 mg/d).
102
There was no significant difference in weight gain at 2 years followup. A
cohort study in Washington DC analyzed dietary intake data from 322 pregnant African
American women (mean age 21.6 years; 39 percent 16-19 years) and found that "none of
the food energy and nutrient intakes [mean calcium intake 933 mg 52 (SE)] was
significantly correlated with any of the pregnancy outcome measures". No specific
quantitative relationship between calcium intake and infant birth weight or length was
reported.
103
; A measurement tool to assess the methodological quality of systematic reviews
134
Findings by life stage.
0- 6 mo A cohort study of dietary intake in 322 pregnant African American
women found that calcium intake was not significantly correlated with any
pregnancy outcome measures, including infant birth weight or length.
7 mo- 2 y No study covered this life stage.
3-8 y One meta-analysis of 17 RCTs in children (age 3-18 y) found no
significant difference in weight and height gain between those who were and
those who were not supplemented at followup. The calcium intake ranged from
300 to 1200 mg/d lasting from 0.7 to 4 years.
9- 18 y In addition to the findings from the above meta-analysis, two
primary studies provided additional information. One RCT of calcium 500 mg/d
(calcium carbonate) versus placebo for 1 year found no significant difference in
height or weight gain among the 110 girls (mean age 13 years) at followup. A
post hoc analysis of an RCT of calcium enriched 1656 mg/d) versus usual
diet (- 961 mg/d) on bone mass found no significant difference in weight gain at 2
years followup in 59 girls (mean age 9.5 years).
19 - 50 y Not reviewed
51 - 70 y Not reviewed
y Not reviewed
Postmenopause Not reviewed
Pregnant & lactating women See 0 - 6 month results.
135
Table 46. Summary of systematic revi ew of calcium on growt h in children
Author Year [PMID] Winzenberg 2007
166
(17636098]
Desi gn (Search Years) Randomized controlled trials (1966-2005)
Population Children <18 y
Interventi on (Exposure) Supplemental and dietary calcium 300-1200 mg/d vs. placebo
and Comparator
Results
Comments
17 trials (2088 participants)
Weighted mean difference: +0.14 (95% Cl -0.28, +0.57} kg; favors control
Weighted mean difference: +0.22 (95% Cl -0.30, +0.74} em; favors control
No significant statistical heterogeneity
Post hoc analysis performed on trials identified for a meta-analysis of randomized
controlled trials of calcium on bone outcomes
AMSTAR
A priori desi gn? Yes
Yes
Yes
No
Study quality assessment performed? Yes
Two independent reviewers?
Comprehensi ve l iterature search?
All publication types and l anguages
included?
Included and excluded studies listed?
Study characteristics provided?
No
Yes
Study qual ity appropriately used in anal ysis? No
Appropriate statistical synthesi s? Yes
Publ ication bi as assessed? Yes
Conflicts of interest stated? No
Unclear if all languages included; study quality assessed
but not factored into the M-A
Table 47. Calcium and growth: Characteri stics of r i m r ~ studies
Confounders/Effect Modifiers
Adj usted
Author Year Background Ul
Study Name Calcium Q) E
.::::
... Q)
Locati on Population Intake & Compari sons c.
:I
E
!l ~
Ul
E
(Latitude) Vitamin D c.
iii
0
Q)
c C)
0 c.
~
0
(PMID) Data
~
0
... u )( (.)
E
.::::
'ii
Q) Ul
:; Q) E
Q)
>
~
z 0 ~ ::::!: ::I ::i
Lorenzen Health no specific 88-item FFQ Ca C03 (Ca X X X RCT;
2006
101
status health issue (no internal 500 mg/d) X 1 Danish
Denmark reported validation); y vs. placebo surnames
(55
2
N) Mean age 13 dietary only
(16400044) (range/SO), calcium: 957
y mg/d;
Male(%) 0 25(0H)D:
34.5 nmoi/L
Lappe Health healthy 3-d food Calcium rich X X X X Post hoc
2004Hl2
status record (no diet (-1 656 ofRCT
Omaha, NE
Mean age 9.5 internal mg/d) vs. on bone
us (range/SO), validation); usual diet mass;
(41 0N)
y dietary (- 961 mg/d); 95%
[15354150]
Male(%) 0
intake wt & ht white, 5%
calcium: 819 change at 2 y black
mg/d; dietary
vit D 180
IU/d (4.5
fd
Johnson Health pregnant; no FFQ (no Relationship Cohort
1994
103
status OM, sickle, internal between study; all
Washington thalassemia, validation); maternal African
DC, US HbC calcium calcium intake American;
(38gN) disease 933.4 mg/d and birth Total Ca
[8201444) Mean age 22 (39% 16- weight, height (from
(range/SO), 19) food)
y
Male(%) 0
136
Table 48. Calcium and growth: Results of studies
Author Year
Life
Mean
Interventions, No. Change Net Net Diff
p
Study
Study Name Outcome 10/20 Followup, Unit Baseline Change
PMID
Stage
y
Ca daily Dose Anal yzed 95% CI Diff 95%CI Btw Quality
RCT
Lorenzen 9-1 8 wtin 30 kg 51.8 5.1 _LZ.,__1:!_.5 0.2 -4.4_,_4.9 8
2006
101
female medium
(55
2
N) Ca intake
[1 6400044) group
1 Q
Placebo 30 kg 50.7 4.9 1.8, 8.0A
(1000-
1304
mg/d)
wt in low 500 mg/d x 1 y_ 30
kg ___ 52.2 4.1 -3.6, 5.8A NS
Ca intake
group
p
Placebo 30 kg 49.5 3.0 -0.2, 6.2A
(<713
m /d
ht in 30 em 162.5 3.7 -0.3 -3.3,_?.8
medium
Ca intake
group
1 Q
Placebo 30 161 .9 4.0 1.7,6.3A
(1000-
em
1304
mg/d)
ht in low _500_J!!9/d X 1 y_ 30 em 159.6 3.6 1_,_!, 6.t 0.5 -3.3, 4.3A NS
Ca intake
group
p
Placebo 30 160.1 3.1 0.3, 5.9A
(<713
em
m /d)
Post hoc anal:tsis of an RCT on bone outcomes
Lappe 9-18
27 kg 32.2 10.7 8.2, 13.2A -0.2 -4.1 , 3.7A NS
8
2004
102
female
(41 QN)
WI
20
2 -------------
(15354150)
32 kg 33.2 10.9 7.9, 13.9A
27 em 137 14
11 .5}.,
-2, 4A NS
hi
22
2
16.5
32 em 138 13 11 , 15A
Cohort
Johnson 9-18 322 African American women with a mean dietary calcium intake of 933 mg/d; c
1994
103
female; birth wt &
1 Q
until "None of the food energy and nutrient intakes was significantly correlated with any of the pregnancy
(38QN) infant 0- length delivery outcome measures". No specific quantitative relationship between calcium intake and infant birth weight or
6 mo lenji!th was
Estimated from reported data
137
Calcium and Cardiovascular Disease
Synopsis.
No qualified systematic reviews evaluated the association between calcium intake and
incidence of cardiovascular disease. No calcium intervention trials evaluated cardiovascular
outcomes. Ten longitudinal cohort studies and one nested case-control study analyzed
associations with various specific cardiovascular events. In all studies, baseline calcium intake,
assessed by food frequency questionnaires, were analyzed as predictors of long-term
cardiovascular outcomes. We point out where there were "suggestions" of associations in cases
where P values were about 0.10 and/or there were consistent, though not statistically significant
differences in risk compared to the lowest risk category of at least 20 percent.
Notably, the implied ranges of calcium intake within studied populations varied widely
across studies. At one extreme, men and women in the Japan CC study had mean calcium intakes
in the lowest quintile of 250 or 266 mg/day and in the highest quintile of 665 and 667 mg/day.
The Japan PHC study and the Taiwanese CVD-FACTS study had similarly low calcium intake.
The study with the highest calcium intake was the A TBC study of men in Finland. Median
calcium intakes in the lowest and highest quintiles were 876 and 1916 mg/day, respectively; the
overall median intake was 1379 mg/day.
Cardiovascular death was analyzed in two large studies analyzed, separately in men and
women. Neither found a significant association between calcium intake and cardiovascular death
after 9 or 28 years in either men or women.
Combined fatal and nonfatal cardiac events were analyzed in two large and one relatively
small studies, in either both sexes together or just men. None found a significant association
between calcium intake and cardiac events after 10 to 13 years.
Cardiac death was analyzed in three large and one relatively small studies, separately in men
and women. Overall, no consistent significant association between calcium intake and cardiac
death after 8, 9, 12, or 28 years of followup was found in the various studies, in either men or
women. One study (the Iowa WHS) found a significant association between calcium intake of
less than 696 mg/day and higher risk of ischemic heart disease death in white women aged 55 to
69 years.
Nonfatal myocardial infarction was analyzed by one large study of men. No significant
association was found with calcium intake after 12 years of followup.
Total strokes were analyzed in five large and one relatively small studies, in both sexes
combined, and separately for men and women. The studies had disparate findings. A Japanese
and a Taiwanese study of men and women (40-59 y and 4 y, respectively) found progressively
lower risks for stroke in people in higher quintiles of calcium intake after 13 and 11 years,
respectively, in the setting of overall relatively low dietary calcium intake. A small Finnish study
of both men and women (65-99 y) found no significant association after 10 years. The two
studies of men ( 40 to 75 years old) found suggestions of associations (not statistically
significant), though with trends in opposite directions; one suggested the highest risk for stroke
in men with calcium intake below approximately 750 mg/day after 8 years; one suggested the
highest risk for cerebral infarctions in men with calcium intake above about 1000 mg/day after
14 years. The study of women (32-57 y) found a nonsignificant trend after 14 years, but
significantly higher stroke risk in those with calcium intake less than about 500 mg/day
compared with women in the next two higher quintiles of calcium intake.
138
Fatal strokes were analyzed in one large cohort study and a nested case-control study,
separately in men and women. None found a significant association between calcium intake and
cardiac events after 10 to 13 years of followup.
Detailed presentation (Tables 49 & 50, Figures 11 & 12).
Cardiovascular death.
Two longitudinal cohort studies analyzed risk of cardiovascular death (death from cardiac or
cerebrovascular events), separately in men and women, according to quintiles.
In the Japan Collaborative Cohort (Japan CC),
104
about 23,000 men aged 40 to 79 years
without a history of cardiovascular disease were followed for 8.9 years; 3 percent died of a
cardiovascular event. Men within the calcium quintiles had mean calcium intakes that ranged
from 250 to 665 mg/day. No significant association was found between calcium quintile and
cardiovascular death risk. In a study of Dutch civil servants (and spouses),
105
1340 men aged 40
to 65 years (regardless of cardiovascular history) were followed for 28 years. About 27 percent
(age-adjusted) had a cardiovascular death. The calcium intake quintiles ranged from less than
585 mg/day to more than 1245 mg/day. No significant associations were found between calcium
intake and risk of cardiovascular death; however, men in the lowest quintile ~ 5 8 5 mg/day) had
an adjusted odds ratio of cardiovascular death of 1.3 (95 percent CI 0.8, 1.9) compared to those
in the highest quintile. Both studies had methodological quality B. The Japanese study did not
define cardiovascular mortality and the Dutch study did not report a complete analysis of the
calcium intake quintiles.
In the Japan CC, about 35,600 women aged 40 to 79 years without a history of
cardiovascular disease were followed for 8.9 years; 1.8 percent died of a cardiovascular event.
Women within the calcium quintiles had mean calcium intakes that ranged from 266 to 667
mg/day. No significant trend across quintiles or associations among quintiles was found for risk
of cardiovascular death. However, women in the lowest quintile had about 25 to 30 percent
lower risks of cardiovascular death than women in the next two higher quintiles. In the Dutch
civil servants study, 1265 women were followed for 28 years. About 14 percent had a
cardiovascular death. The calcium intake quintiles ranged from less than 445 mg/day to more
than 850 mg/day. No significant associations were found between calcium intake and risk of
cardiovascular death.
Cardiac events, total.
Three longitudinal cohort studies analyzed combined fatal and nonfatal cardiac events,
including coronary heart disease, acute myocardial infarction, and ischemic heart disease; two
combined both sexes, one included only men.
In the Japan Public Health Center (Japan PHC) study (methodological quality A),
106
about
41,500 people aged 40 to 59 years, without cardiovascular disease, were followed for 13 years;
0.8 percent had cardiac events. People within the calcium intake quintiles had median calcium
intakes that ranged from 233 to 753 mg/day. No association was found between calcium intake
and risk of coronary heart disease events. In a small Finnish longitudinal study,
48
755 people
aged 65 to 99 years, regardless of cardiovascular history were followed for 10 years; 17 percent
had a cardiac event. No significant association was found between tertiles of calcium intake and
all acute myocardial infarctions. This methodological quality C study did not report relevant data
including information on the calcium intake within the tertiles.
In the Health Professionals Follow-up Study (HPFS),
107
about 39,000 men with a mean age
of 54 years, without cardiovascular disease were followed for 12 years; 3.7 percent had an
139
ischemic heart disease event. The study was of methodological quality A. Men within the
calcium quintiles had mean calcium intakes that ranged from 523 to 1377 mg/day. No significant
association was found between calcium intake and risk of cardiac events.
Cardiac death.
Four longitudinal cohort studies analyzed death from cardiac events, separately in men (3
studies) and women (3 studies).
In the three studies of men, all found no significant association between calcium intake and
cardiac death. All three studies are described above. In HPFS 1.1 percent of men died of a
cardiac event during 12 years offollowup.
107
In the Japan CC study 0.6 percent of men died of a
cardiac event during 9 years of followup (methodological quality A for thi s outcome).
104
In the
Dutch civil servants study about 15 percent (age-adjusted) died of a cardiac event during 28
years of followup. LOS
Three studies analyzed cardiac death in women. In two studies, both described above, there
was no signi ficant association between calcium intake and cardiac death. In the Japan CC study
0.3 percent of women died of a cardiac event during 9 years of followup.
104
In the Dutch civil
servants study about 6 percent (age-adjusted) died of a cardiac event during 28 years of
followup.
105
The Iowa Women's Health Study (Iowa WHS) analyzed about 34,500 white
women, aged 55 to 69 years, without ischemic heart disease. During 8 years of followup, 1.1
percent died of a cardiac event. However, the study was of methodological quality B for this
outcome because the outcome was not fully ascertained. The calcium intake quartiles ranged
from less than 696 mg/day to more than 1425 mg/day. There was a suggestion of an association
between lower calcium intake and higher risk of cardiac death, with a P value of 0.09 for the
trend across quartiles and statistically significant adjusted relative risks of cardiac death for
women with calcium intakes above 696 mg/day of0.62 to 0.75 (compared to the lowest quartile).
Cardiac events, nonfatal.
Only the HPFS, described above, analyzed nonfatal cardiac events (methodological quality
A).
107
During 12 years offollowup 2.6 percent of almost 40,000 men had nonfatal myocardial
infarctions. No significant association was found between calcium intake and nonfatal cardiac
events.
Stroke, total.
Six longitudinal cohort studies analyzed combined fatal and nonfatal strokes, in either both
sexes combined, or men and women separately.
In the Japan PHC study, described above (cardiac events, total), 3 percent of people suffered
strokes during 13 years of followup (methodological quality A).
10
The study found a significant
association between baseline calcium intake and risk of stroke. The risk of stroke was
progressively lower in progressively higher quintiles of calcium intake. People with a median
calcium intake of 439 mg/day (middle quintile) had a statistically significant adjusted hazard
ratio (HR) of0.79 compared to those with a median calcium intake of233 mg/day. Those in
higher quintiles had lower HRs; across quintiles, the trend had a P value of0.02. As is evident
from the median calcium intake levels within the quintiles, the middle-aged Japanese in this
study had considerably lower average calcium intake than in most other studies (particularly
those performed in the US). Compared to similar studies evaluated here, the calcium intake was
approximately half of that in the HPFS or Iowa WHS. The CVD-FACTS study, perfom1ed in
men and women at least 40 years old in Taiwan, evaluated ischemic strokes.
108
After a mean
followup of 10.6 years, 7.4 percent of the cohort had an ischemic stroke. The B quality study
140
divided the cohort into tertiles. Similar to the Japanese study, the typical calcium intake was
relatively low by Western standards (the average dietary calcium intake was approximately 520
mg/day). Those in the lower t\vo tertiles had about a 50 percent increased risk of ischemic stroke
than those in the highest tertile (>591 mg/day). While the adjusted OR for each tertile were not
quite statistically significant (1.52 [95 percent CI 0.98-2.35] for lowest tertile; 1.49 [95 percent
CI 0.99-2.24] for middle tertile; compared to highest tertile), the trend across tertiles had a P
value of 0.03. The third study of combined men and women, of older Finns (described above
under Cardiac events, total), found no significant association with stroke m o n ~ 755 people
followed for 10 years (stroke incidence 9.3 percent; methodological quality C).
8
Both studies of men alone suggest trends across quintiles of calcium intake and stroke risk;
however, the associations were in opposite directions. The HPFS, described above (cardiac
events, total; methodological quality A) had a stroke incidence of 0.75 percent during 8 years of
followup. Men in higher quintiles of calcium intake had generally lower adjusted relative risks
(RR) of stroke compared to the lowest quintile (median calcium intake 500 mg/day); though
none of the RRs was statistically significant and the P value for the trend across quintiles was
0.10. Notably, the RR of stroke for men in the middle quintile (median calcium intake 800
mg/day) was 0.72 (95 percent CI 0.50, 1.03); though the RRs for men in higher quintiles were
closer to 1 with wider 95 percent confidence intervals. In the Alpha-Tocopherol, Beta-Carotene
Cancer Prevention (ATBC) Study, performed in southern Finland, about 26,500 men aged 50 to
69 years without a history of stroke were followed for almost 14 years; 10 percent suffered a
stroke. The study was of methodological quality C because there was large misclassification of
stroke outcomes in a sample of subjects (5-21 percent). Men in the lowest quintile of calcium
intake (median 876 mg/day) had the lowest adjusted RR for cerebral infarction. Men in all higher
quintiles (medians ranging from 1178 to 1916 mg/day) all had RR of about 1.10 that were near
statistical significance (e.g., 95 percent CI for highest quartile was 0.98, 1.26). The P value of the
trend of association across quintiles was 0.09.
One study evaluated total strokes in women alone. The Nurses Health Study (NHS) evaluated
about 86,000 women aged 32 to 57 years with no history of cardiovascular disease. The study
was rated methodological quality A. During 14 years of followup 0.8 percent of women suffered
a stroke. The women in the four quintiles above the lowest quintile (who had a median calcium
intake of395 mg/day) all had similar adjusted RR of stroke (0.71-0.87); the RRs ofthose women
in the second and third quintiles were statistically significant. However, the trend of associations
across quintiles was not statistically significant.
Stroke death.
One longitudinal cohort study (with subanalyses in men and women separately) and one
nested case-control study (in men) evaluated fatal strokes.
Both studies of men found no significant association benveen calcium intake and risk of
stroke death. In the Japan CC study (described above, methodological quality A for this
outcome) 1.4 percent ofmen died of stroke during 9 years offollowup. The second study was a
nested case-control study performed in China. In a prospective cohort of about 18,000 men aged
45 to 64 years, regardless of cardiovascular history, 245 died of stroke (1.3 percent) during 12
years of followup. These cases were matched with 1225 controls. The remaining 17,000 men
were omitted from the analysis. The study also did not report data on the calcium intake within
the tertiles. The methodological quality was C.
In the Japan CC study, 0.9 percent of women died of stroke. The study also found no
consistent association benveen calcium intake and stroke death.
141
Findings per calcium intake level.
Among the outcomes for which studies had either statistically significant associations or
suggestions of associations between calcium intake and cardiovascular events, the following
findings of calcium intake level were reported.
Regarding the risk of overall cardiovascular mortality, one of two studies in women (Japan
CC) found a suggestion that higher calcium intake may be associated with increased risk of
cardiovascular death. The association can be seen for quintiles 2 to 4, where women in the lowest
quintile had a median calcium intake of 266 mg/day and those in the second quintile had a
median calcium intake of 379 mg/day.
Regarding the risk of cardiac mortality, one of three studies in women (Iowa WHS) found
that women in the lowest quartile of calcium intake, below 696 mg/day, had the highest risk of
cardiac mortality.
Regarding the risk of stroke, among studies of both sexes combined, two (Japan PHC and the
Taiwanese CVD-FACTS) ofthree studies found a statistically significant association between
lower calcium intake and higher risk of stroke. In Japan PHC, those in the third to fifth quintiles,
with median calcium intakes of 439 mg/day or higher, had lower risks than those in the lowest
quintile. Those in the second quintile had a median calcium intake of 344 mg/day and those in
the lowest quintile 233 mg/day. In CVD-F ACTS, those in the two tertiles with calcium intake
below 591 mg/day had about a 50 percent increased risk of stroke compared to those with higher
calcium intake. The two studies restricted to men had opposite findings. The HPFS found lower
risks of stroke among men in the third to fifth quintiles of calcium intake (median 800 mg/day or
higher) compared to the lowest quintile (median 500 mg/day). Those in the second quintile had a
median calcium intake of 700 mg/day. In contrast, the ATBC study in Finland found somewhat
higher risks of stroke R R ~ 1. I) in all quintiles above the lowest quintile. The median calcium
intakes in the first and second quintiles were 876 and 1178 mg/day, respectively. The one study
of women (NHS) had lower risks of stroke in all quintiles above the lowest quintile. The median
calcium intakes in the first and second quintiles were 395 and 645 mg/day, respectively.
Findings per age and sex.
The majority of studies (and the large majority of individuals) included mostly people
between the ages of about 40 and 70 years. The youngest individuals included were 32 year old
women in the NHS. Apparently very few individuals were over the age of 70 years. Only a small
Finnish study (Mamiemi 2005
48
) restricted the study cohort to only older adults (65 years and
older). This study found no significant associations between calcium intake and cardiovascular
events. No study reported a subgroup analysis based on age. The reported data do not allow
further conclusions based on age.
Almost all studies or analyses separately evaluated men and women. The fmdings that could
be interpreted as an association between calcium intake and cardiovascular risk were mostly
found in women (low calcium intake being associated with increased risk of cardiac death (in
one of three studies) and stroke (in a single study), but with lowered risk of overall
cardiovascular death (in one of two studies). The only potential associations between calcium
intake and cardiovascular events in men were found for stroke; however, the two studies had
opposite findings about the direction of the association.
Findings by life stage.
0 - 6 mo Not reviewed
7 mo- 2 y Not reviewed
142
3 - 8 y Not reviewed
9- 18 y Not reviewed
19-50 y Overall, the studies included relatively few people in this life stage. All
were at least 32 years old, and most were at least 40 to 45 years old. However, the one
study of stroke in women was conducted in women who were mostly in this life stage.
Those in the lowest quintile of the NHS appear to have had higher risks of stroke than
those women with greater calcium intake.
51 - 70 y The majority of evidence regards people in this life stage. Overall, the
majority of analyses found no significant association between calcium intake and most
cardiovascular events. Only for stroke did at least two studies find significant
associations between calcium intake and the outcome. In two Asian studies, where the
average dietary calcium intake was about half that in the US and which also included
people in the younger life stage, stroke risk was progressively higher in lower quantiles
(maximum quantiles were median of753 mg/day and >59 1 mg/day). For studies of
people within this life stage, other significant associations were found in one of three
studies of cardiac death in women (calcium intake below 696 mg/day was associated with
increased risk) and in one of two studies of cardiovascular death in women (calcium
intake above about 300 mg/day may be associated with increased risk).
~ 7 y Few studies included people in this life stage. The one study of people in
this life stage found no association between calcium intake and cardiac events or stroke in
a relatively small, quality C study.
Postmenopause Only the Iowa WHS included primarily postmenopausal women.
In their analysis, calcium intake below 696 mg/day was associated with increased risk of
ischemic heart disease death.
Pregnant & lactating women Not reviewed
143
Table 49. Calcium and cardi ovascular outcomes: Characteristics of cohort studies
8
Confounders/Effect Modifiers
Author Year
Adjusted
Study Name
Q)
Dietary Calcium
.t::
:s Specific CVD
Location Population Comparisons
Q.
intake
Ill
!!
Ill
Outcomes
(Latitude) 'E
Q.
iii
0
Q)
Ol 0
Q. >.
[PMID]
0
... u )(
iii
E
.t::
:s
Q)
'S Q) 'E
Q)
>
z c
<
:: ::I :::;
AI-Delaimy Health No Dietary FFQ Outcome X X X X X IHD
2003
107
status CVD assessment stratified by Ml
HPFS
Mean 54 (9) met hod total Ca intake Cardiac death
us age
quintiles
(various)
(SD), y
Total Ca
[1 2663277]
Male 100 Internal Yes
(both)
(%) validation?
In
Ascherio Health No Dietary FFQ Outcome X X X X X Stroke
1998
109
status CVD assessment strati fied by
HPFS
Mean nd method total Ca intake Total Ca
us age (40-75) quintiles {both)
(various)
(range),
[9743511) y
Male 100 Internal Yes
(%) validation?
In
Bost ick Health No IHD Dietary FFQ Outcome X X X X X Cardiac death
1999
110
status assessment stratified by
Iowa WHS
Mean 61 method total Ca intake Total Ca
Iowa age (55-69) quartiles (both)
(42) (range),
[9921960) y
Male 0 Internal Yes
(%) validation?
In
lso 1999 Health No Dietary FFQ Outcome X X Stroke
NHS status CVD assessment stratified by
us Mean 46 method total Ca intake Total Ca
(various) age (32-57) quintiles (food)
[ 10471422) (range),
y
Male 0 Internal No
(%) validation?
In
Larsson Health No Dietary FFQ Outcome X X X X X Stroke
2008
11 2
status stroke assessment strati fied by (cerebral
ATBC
Mean 57 method total Ca intake infarct)
SW Fi nland
age (50-69) quintiles
(-60"N) (range), Total Ca
[ 18332289) y (food)
Male 100 Internal No
(%) validation?
In
Marniemi Health Any Dietary Interview Outcome X X X Ml
2005
48
status assessment strati fied by Stroke
Turku
Mean 79 method total Ca intake
Finland
age (65-99) tertiles Total Ca
(60N)
(range), {both)
[15955467) y
Male 48% Internal No
(%) validation?
In
continued
144
Confounders/Effect Modifiers
Author Year
Adjusted
Study Name
Cll
Dietary Calcium
s:; ..
Specific CVD
Location Population Comparisons
Q.
J
intake
Ul t\1
Ul
Outcomes
(Latitude) 'E
... Q.
iU
0
Q)
Cl
0
Q. >.
[PMID]
Cll
0 .. 0 )(
iii ;::
E
s:;
:.0
Q)
:; Q) 'E
Q)
>
.!
z c
<
:: ::I ::;
Ross
Health Cases Dietary FFd Outcome -x- X -x- x Fatal stroke
1997
11
3A
status &
assessment stratified by
Shanghai
controls method total Ca intake Total Ca
China
Mean nd
tertiles (food)
(31 "N)
age (45-64)
[9236416)
(range),
y
Male 100 Internal nd
(%) validation?
In
Umesawa Health No Dietary FFQ Outcome X X X X X Cardiac death
2006
104
status CVD assessment stratified by Stroke death
Japan CC
Mean 56 method total Ca intake CVD death
Japan age (40-79) quintiles
(various)
(range),
Total Ca
[16339476] y
(food)
Male 39 Internal No
(%) validation?
In
Umesawa Health No Dietary FFQ Outcome X X X X X CHD
2008
106
status CVD assessment stratified by Stroke
Japan PHC
Mean 49 method total Ca intake
Japan age (40-59) quintiles Total Ca
(various)
(range),
{food)
[ 18635855)
y
Male 48 Internal Yes
(%) validation?
In
van der Health Any Dietary FFQ Outcome X X X Cardiac death
Vijver status assessment stratified by CVD death
1992
105
Mean 52 method total Ca intake
Dutch civil age (40-65) quintiles Total Ca
servants (range) , {food)
Amsterdam
y
Netherlands
Male 51 Internal No
(52")
(%) validation?
[1 544755)
In
W e n ~ Health No Dietary FFQ Outcome X X X X Ischemic
2008
8
status stroke, assessment stratified by stroke
CVD- cancer method total Ca intake
FACTS
Mean 57
quartiles (top Total Ca
Taiwan
age (;::40)
2 quartiles {both)
(22"-25)
(range),
combined)
[ 18988909)
y
Male 44 Internal No
(%) validation?
~ n l
A Nested case-control study
8
This table is ordered alphabetically by study author
145
Tabl e 50. Calcium and cardi ovascular outcomes: Results of cohort studies
Author Year Age Outcome (n/N; Follow up Total Ca No. of No. in Adj usted 95% CI P for Study
Study Name Range, Sex Incidence) Duration Intake, mg/day Cases Category OR Trend Quality
PMID
CVD Death
Men
Umesawa 2006 4079 y, CVD death 8.9 y 250, mean 140 4623 Reference 0.95 B
Japan CC Men (685/23, 117; 0.030}
[1 6339476)
-------------
363 141 4624 0.98 0.75, 1.30
449 135 4623 0.93 0.67 1.29
536 135 4624 0.92 0.64 1.32
665 134 4623 0.97 0.64, 1.48
van der Vijver 40-65 y, CVD death 28 y S585 31.9%, 271 1.3 0.8, 1.9 nd B
1992'
05
Men (nd/1340; -0.27, age-
Dutch civil age-adjusted) adjusted
servants
[1 544755]
585-1245 26. 7% 798
------------
1.1 0.8, 1.5
>1245 24.9% 271 1 Reference
Women
Umesawa 2006 40-79 y, CVD death 8.9 y 266, mean 153 7121 Reference 0.14 B
Japan CC Women (644/35,609; 0.018}
[1 6339476)
379 156 7122 1.29 0.99, 1.67
462 136 7122 1.24 0.90, 1.69
545 98
___ ][21_ ____
0.92 0.64 1.34
667 101 7122 1.14 0.74, 1.74
van der Vijver 40-65 y, CVD death 28 y S445 14.6%, 258 1.1 0.6, 2.0 nd B
1992
105
Women (nd/1265; -0.1 4, age-
Dutch civil age-adjusted) adjusted
servants
[1 544755)
----------
445-850 14.4% 750 1. 1 0.7, 1.7
>850 12.6% 257 1 Reference
Cardiac Events,
Total
Both Sexes
Umesawa 2008 40-59 y, CHD 13 y 233, median 72 - 8305 Reference NS A
Japan PHC Both (322/41,526; 0.0078)
[18635855]
344 72 -8305 1.18 0.83, 1.68
---
439 56 ____ : ..:m_ ___ 0.91 0.60 1.37
603 58 - 8305 1.08 0.71 1.65
753 64 - 8305 0.93 0.58, 1.50
continued
Author Year Age Outcome (n/N; Follow up Total Ca No. of No. in Adjusted 95% CI P for Study
Study Name Range, Sex Incidence) Duration Intake, mg/ day Cases Category OR Trend Quality
PMID
Marniemi 2005 6599 y, AMI 10 y nd nd -252 Reference nd c
(Finland) Both (130/755; 0.172)
[1 5955467)
nd nd -252
-------------
0.87 0.57, 1.37
nd nd -252 1.14 0.70, 1.84
Men
AI-Delaimy 2003
101
Mean (SO) IHD, total 12 y 523, mean 300 7960 Reference 0.43 A
HPFS 54 (9) y, (1458/39,800; 0.037)
[1 2663277) Men
670 296 7960 1.03 0.88, 1.22
803 267 7960 0.92 0.78, 1.09
995 299
796_6_
1.01 0.85, 1.19
137 7 296 7960 0.94 0.79, 1.11
Cardiac Death
Men
AI-Delai my 2003
101
Mean (SO) IHD death 12 y 523, mean 88 7960 Reference 0.72 A
HPFS 54 (9) y, (428/39,800; 0.01 1)
(1 2663277) Men
-----------
670 90 7960
--------- ----
1.17 0.87, 1.50
803 70 7960
------------
0.93 0.67, 1.29
995 79 7960 1.06 0.77, 1.47
1377 101 7960 1. 10 0.79, 1.51
Umesawa 2006 40-79 y, CHD death 8.9 y 250, mean 37 4623 1 Reference 0.43 A
Japan CC Men (148/ 23, 117; 0.0064)
[1 6339476)
363 26 4624 0.84 0.47, 1.50
449 33 4623 1.20 0.62, 2.30
536 32
1.27 0.60 2.68
665 20 4623 0.92 0.37, 2.29
van der Vijver 40-65 y, CHD death 28 y S585 16.6%, 271 0.9 0.6, 1.6 nd B
1992
105
Men (nd/1340; -0. 15, age-
Dutch civil age-adjusted) adjusted
servants
1544755
585 1245 15.1% 798 1.0 0.6, 1.5
>1245 14.5% 271 1 Reference
Women
Umesawa 2006
104
40-79 y, CHD death 8.9 y 266, mean 38 7121 Reference 0.50 A
Japan CC Women (116/35,609; 0.0033)
[1 6339476)
-------------
379 21 7122
------------
0.88 0.48, 1.62
462 25 7122 1.28 0.62, 2.61
545 17 7122 0.84 0.35, 2.02
667 15 7122 0.87 0.31 ' 2.45
continued
147
Author Year Age Outcome (n/N; Follow up Total Ca No. of No. in Adjusted 95% CI P for Study
Study Name Range, Sex Incidence) Duration Intake, mg/ day Cases Category OR Trend Quality
PMID
Bostick 1999 55-69 y, IHD death 8y <696 127 - 8621 Reference 0.09 B
Iowa WHS Women (387/34,486; 0.01 1)
[9921960)
696-1051 84 - 8621
-------------
0.62 0.45, 0.85*
1052-1425 94 - 8621
-------- ---
0. 75 0.55, 1.03
>1425 82 -8621 0. 67 0.47, 0.94.
van der Vij ver 40-65 y, CHD death 28 y !>445 6.2%, 258 1.1 0.5, 2.5 nd B
1992
105
Women (nd/1265; - 0.06, age-
Dutch civil age-adjusted) adjusted
servants
[1 544755]
445-850 6.3%
---
750 1.2 0.6, 2.3
>850 4.4% 257 1 Reference
Cardiac Event,
Nonfatal
Men
AI-Delaimy 2003
107
Mean (SD) Nonfatal Ml 12 y 523, mean 212 7960 Reference 0.43 A
HPFS 54 (9) y, (1 030/39,800; 0.026)
[12663277] Men
670 206 7960
----------
1.01 0.83, 1.23
803 197 7960
-------------
0.96 0.78, 1.17
995 220 7960 1.04 0.85, 1.28
1377 195 7960 0.92 0.74, 1.14
Stroke
Both Sexes
Umesawa 2008
106
40-59 y, Stroke, Total 13 y 233, median 31 4 - 8305 Reference 0.02 A
Japan PHC Both (1321/41 ,526; 0.032)
[1 8635855]
257 - 8305 0.94 0.79 1.13
252 - 8305
-----------
0.79 0.65, 0.97*
247 - 8305
-------------
0.78 0.63, 0.96*
251 - 8305 0. 71 0.56, 0.89*
Weng 2008 ?:40 y Stroke, Ischemic 10.6 y <451 nd 443 1.52 0.98, 2.35 0. 03 B
CVD- FACTS Both (132/1772; 0.074)
[18988909]
451-591 nd 443 1.49 0.99, 2.24
>591 nd 886 1 Reference
Marniemi 2005 65-99 y, Stroke, Total 10 y nd nd -252 1 Reference nd c
(Finland) Both (70/755; 0.093)
[1 5955467]
-------------
nd nd -252
----------
0.981 0.53, 1.81
nd nd -252 1.34 0.70, 2.55
Men
continued
148
Author Year Age Outcome (n/N; Follow up Total Ca No. of No. in Adjusted 95% CI P for Study
Study Name Range, Sex Incidence) Duration Intake, mg/ day Cases Category OR Trend Quality
PMID
Ascherio 1998
1
0 40-75 y, Stroke, Total By 500, median 75 - 8748 Reference 0.10 A
HPFS Men (328/43,738; 0.0075)
[9743511]
700 69 - 8748
-------------
0.95 0.68, 1.32
800 51 - 8748
-----------
0. 72 0.50, 1.03
1000 63 -8748 0.84 0.60, 1.19
1400 70 - 8748 0.88 0.63, 1.23
Larsson 2008 50-69 y, Cerebral infarction 136 y 876, median 518 -531 1 Reference 0.09 c
ATBC Men (2702/26,556; 0. 1 02)
[1 8332289]
1178 541 -5311 1.08 0.95, 1.22
137 9 542 -5311 1.09 0.96, 1.23
1581 546 - 5311 1.11 0.98 1.26
1916 555 - 531 1 1.10 0.98, 1.26
Women
lso 1999 32-57 y, Stroke, Total 14 y 395, median 165 -17153 Reference NS A
NHS Women (690/85, 764; 0.0080)
(10471422] ______ M___
645 132 - 17153 0.79 0.63, 1.00*
675 117 -17153 0.71 0.56, 0.90*
837 142 -17153 0.87 0.70, 1.09
--1-145
134 -17153 0.83 0.66, 1.04
Stroke, Fatal
Men
Umesawa 2006 40-79 y, Stroke death 8.9 y 250, mean 61 4623 Reference 0.95 A
Japan CC Men (322/23,117; 0.01 4)
(1 6339476]
__ 363 76 ~ ~ 4 _ ____ 1.14 0.76 1.70
449 69 4623 0.90 0.56, 1.45
536 59 4624 0.69 0.40, 1.18
665 57 4623 0.68 0.37, 1.26
Ross 1997 45-64 y, Stroke death 12 y nd 103 460 controls 1 Reference NS c
(China) Men (245/ 18,244;0.013)
[9236416) [245 cases vs. 1225
controls]
nd 68 369 controls 0.8 0.6, 1.6
nd 74 396 controls 1.0 0.8, 1.4
Women
Umesawa 2006 40-79 y, Stroke death 8.9 y 266, mean 70 7121 Reference 0.50 A
Japan CC Women (322/35,609; 0.0090)
[1 6339476]
-------------
379 82 7122 1.38 0.95, 2.01
462 73 7122 1.24 0.79 1.95
545 42 7122 0.69 0.40 1.18
667 55 7122 0.94 0.51' 1.72
149
Statistically significant (P<0.05)
A Case-control study from prospective, longitudinal cohort.
150
Figure 11. Cardiovascular outcomes risk stratified by calcium intake
Ca
Study Category Intake (mg/ d)
CVD Death, Men
Japan CC 2006 01 (ref) 250
(n-=23,117) 02 363
03 449
04 536
Q5 665
Dutch cfv11 servants 1992 <lt <585
(n-=1340) Q2&4 585 - 1245
05 (ref) >1245
CVD Death, Women
Japan cc 2006 01 (ref) 266
(n-=35,609) Q2 379
03 462
g ~
545
s MZ
Dutch ciVIl servants 1992 Q1 <445
(ns1265) 02&4 445 .850
QS(ref) >850
Cardiac Events, Both Sexes
Japan PHC 2008 Q1 (ref) 233
(n-=41 ,526) Q2 344
03 439
Q4 603
QS 753
Mam iernl (Finfaii"d) 2005 T1 (ref)
(n=755) T2
T3
- c ardlaCEvent5;"Men-
HPFS 2003 0 1 (ref) 523
(n-39,800) Q2 670
Q3 803
04 995
05 1377
Cardiac Death, Men
HPFS 2003 Q1 (ref) 523
(n=39,800) 02 670
03 803
Q4 995
f-Jap.liiLL 1006
QS 1377
01 {ref)
363 (11=23,117) Q2
Q3 449
04 $36
Q5 665
D utch ciVIl servants 1992 Q1 <585
(n-=1340) Q2&4 585- 1245
OS (ref) >1245
Cardiac Death, WOmen
Japan CC 2006 Q1 (ref) 266
(n=35,609) Q2 379
03 462
04 545
--
05 667
Iowa WHS 1999 01 (ref) <696
(n-34,486) 02 696- 105 1
Q3 1052 - 1425
Q4 >1425
Dutch civil servants 1992 01 <445
(n=1265) 02&4
Q5 (ref)
445-850
>850
Cardiac events, No nfatai;"'Men
HPFS 2003 0 1 (ref) 523
(11=39,800) Q2 670
03 803
04 995
05 1377
~
:
;
I
o.s
. t
r
. t ..
f
~
=
.I
. f
~ t
t
r
Decreased risk
I
2
Increased rlsk
p
for
trend Quality
0.95 B
--
nd B
-
-
0.14 B
nd B
-
NS A
nd--c -
-
0.43 A
-
0.72 A
lrf3
"
nd B
-
0.50 A
-
0.09 B
nd
B
-
--
0.43 A
I
3
Figure 12. Stroke risk stratified by calcium intake
Study
Stroke, Both Sexes
Japan PHC 2008
(11=41,526)
CVD-f ACTS 2008
(0=1772}
Mamiemi1t.mnd)200s-
(n=755)
Stroke, Men
K'FS 1998
(n=43,738)
AJBC20M
(0=26,556)
Stroke, W<li'"N.'n
NHS 1999
(n=85,764)
Stroke ~ a t h Men
.lapanCC2006
(n: 23,1 17)
Ross (Shanghai) 1997
(n .. 145 cases; I ll5 ClXltrof.s)
Stroke a t h Women
.lapanCC2006
(0=15,609)
Category
Ql (ref)
Q2
Q3
Q4
QS
Tl
T2
T3{refl
Tl frefr-
T.2
T3
Q1 (ref)
Q2
Q3
Q4
QS
Q11tef)
Q2
Q3
Q4
QS
Ql (ref)
Q2
Q3
Q4
QS
Q1 (ref)
Q2
Q3
Q4
Q5
T1 (ref)
T2
T3
Q1 (18)
Q2
Q3
Q4
Q5
{a
intake
{mgt d)
233
344
439
W3
733
<451
451 - 591
>591
500
700
roo
1000
1400
876
1178
1379
1581
1916
395
645
675
837
1145
250
363
449
536
: : 665
166
379
462
545
667
05
152
1
f
- ~
r+-
~
t
f
'
'
2 3
p
ror
ln!nd Quality
O.ll2 A
OJB
c---=1
nd c
0.10 A
1Ul9 C
NS A
0.95 8
NS c
0.50 A
Calcium and Body Weight
We searched for systematic reviews and primary studies that evaluated associations between
calcium intake or body stores and incidence of overweight or obesity; no such studies were
found. For the outcome weight change (in kilograms or body mass index units), we included
only randomized controlled trials. The EPC and the TEP agreed that the limited resources would
not be expended on reviewing observational studies for the surrogate outcome body weight
(where overweight or obesity are considered to be the clinical outcomes). We included only
studies of adults. Studies of weight gain in children are included in the "Growth" section.
Synopsis.
No studies evaluated the association of calcium intake and incidence of overweight or
obesity. We identified three systematic reviews that evaluated RCTs of calciwn intake and
changes in body weight. Eight additional trials not identified by these systematic reviews met
eligibility criteria for this report and are summarized together with the systematic reviews.
Altogether, 49 trials have been identified by the previous and current systematic reviews.
Because the systematic reviews all used somewhat different eligibility criteria, they included
overlapping groups of trials. No one or two systematic reviews captured most of the relevant
trials; therefore, all systematic reviews are included here.
The three systematic reviews performed separate analyses for calcium supplementation and
dairy product intake. Only one of the systematic reviews separately analyzed studies of people
on isocaloric diets (where weight loss was not a goal) and studies of people on energy-restricted
diets. Overall, 24 included trials investigated calcium supplementation and 15 investigated dairy
product intake; 29 trials had isocaloric background diets and 13 evaluated calcium
supplementation in the setting of an energy-restricted (weight loss) diets. Although there was not
complete agreement among the systematic reviews, overall, the trials in the systematic review do
not support an effect of calcium (or dairy) supplementation on body weight. No systematic
review analyzed effects of calcium supplementation based on life stage or calcium dose.
Seven of the eight additional trials investigated calcium supplements in the setting of
isocaloric diets; two of the trials investigated calcium supplements in overweight people on
energy-restricted diets. All these trials found no significant effect of calcium supplementation on
body weight.
Detailed presentation (Tables 51, 52, & 53).
The three systematic reviews explicitly or implicitly used generally different eligibility
criteria, resulting in large overlaps in the trials included among the reports.
114
-
116
Overall, the
systematic reviews included 42 trials. All systematic reviews separately analyzed calcium
supplementation and dairy product intake. The largest, most recent systematic review
114
included
trials up to 2007, separated isocaloric from energy-restricted trials, but did not perform meta-
analysis. The next largest systematic review
115
included trials through 2004. The last systematic
review/
16
through 2001, also did not perform meta-analyses. All the dairy product trials in this
review were also included in the most recent systematic review and are thus not discussed further
here. Seven more recent calcium supplementation trials not included in any of the systematic
reviews were found.
117
-
123
153
lsocaloric trials.
The systematic review by Lanou et al. (2008)
114
evaluated 19 isocaloric trials of increased
calcium intake in adults. Nine trials compared calcium supplements to placebo; 10 trials
compared high calcium dairy intake to lower calcium nondairy intake. The systematic review did
not provide details of every included trial, nor was meta-analysis performed. In summary, 16
trials (8 calcium supplement, 8 dairy product) of the 19 trials reported no significant effect of
increased calcium intake on body weight, 1 calcium trial found significantly greater weight loss
in those receiving calcium supplements, and 2 dairy trials found significantly greater weight gain
in those in the dairy product group. This latter finding was theorized to be due to the extra
calories from the dairy products.
Seven additional isocaloric trials were not included in the systematic reviews.
117
-
122
124
Four
ofthese trials were conducted in postmenopausal women, two in young women (age early 20s),
and one in men and women aged 30 to 34 years. The trials used a variety of calcium compounds
with doses ranging from 800 to 2000 mg; one compared dairy (- 1250 mg calcium) to nondairy
(- 375 mg calcium) intakes.
120
The studies ranged in duration from 1 month to almost 3 years.
Among the studies, one was of methodological quality A, three B, and three C. Methodological
limitations included inadequate reporting of methodology or outcomes, statistical issues, high
dropout rates, and large difference in baseline weights between groups. The participants' weights
were generally stable, on average changing less than 1 kg during 6 weeks to 3 years of followup.
The net weight changes (calcium group minus control group) ranged from -0.8 to +0.5 kg. No
trial found a significant effect of calcium.
Findings per calcium intake level.
Overall, there was no evidence of different effects related to calcium intake level. No study
directly compared a range of calcium intake levels.
Findings per age and sex
The systematic review did not address the question of different effects based on age or sex.
Among the additional trials reviewed here, no significant difference was found across trials of
different populations. Most were conducted in postmenopausal women.
Energy-restricted diets.
The systematic review by Lanou et al. (2008)
114
evaluated 11 trials that compared dairy
intake (6 trials) or calcium supplements (5 trials) in the setting of energy-restricted diets with the
goal of weight loss. Of the six dairy product trials, three were conducted by the same
investigators. These three trials all reported significantly more weight loss in participants with
high dairy product intake than those with low or no dairy product intake (1137 vs. 430 mg Ca;
1100 vs. 500 mg; 3 vs. <1 servings). The systematic review authors note that due to incomplete
reporting in the trials, it was impossible to determine whether the difference in weight loss may
have been due to differences in calcium (or dairy) intake or differential compliance with the
calorie restriction protocol. One of the five calcium supplement trials, which was part of one of
the posit ive dairy trials by the same researchers, found greater weight loss with calcium
supplementation; the others found no significant effect.
The two additional trials not included in the systematic reviews reported no significant
effects of calcium supplementation on body weight loss.
119
'
123
Both trials were conducted in
overweight women, one trial with a mean age of 49 years and one trial of postmenopausal
women. One trial compared two different formulations of 500 mg calcium with placebo in the
154
setting of a low calcium intake (350 mg/day); the other compared higher (1200 mg) to lower
( 400 mg) doses of calcium citrate. Over 3 or 6 weeks, women in all trial groups lost between 3.3
and 4.3 kg, with no significant differences between those with higher than lower calcium intake.
Findings per calcium intake level.
Overall, there was no evidence of different effects related to calcium intake level. No study
directly compared a range of calcium intake levels.
Findings per age and sex.
The systematic review did not address the question of different effects based on age or sex.
The two additional trials did not add any information regarding age or sex subgroups.
Combined isocaloric and energy-restricted diets.
Two of the systematic reviews did not separately analyze studies based on background diet
(regarding weight). The systematic review by Trowman et al. (2006)
115
performed meta-analyses
of 13 trials, separately for calcium supplement and dairy product trials. This systematic review
found a significant effect of calcium supplements (weighted mean difference= -1.79 [95 percent
CI -3.04, -0.55]) suggesting greater weight loss (or smaller weight gain) in adults taking calcium
supplements. However, the investigators noted that the difference in effect of calcium
supplement trials may be due to significant differences (in aggregate) in the baseline weights of
the two arms. Across studies, the calcium supplement group participants had significantly lower
body weights at baseline. The meta-analysis of dairy trials found no si?,nificant effect of dairy
products on body weight. The systematic review by Barret al. (2003)
1 6
reviewed both calcium
supplement and dairy trials; however, the dairy trials were all included in the later systematic
review by Lanou et al. (2008)
1 14
and are thus not repeated here. Among the eight trials of
calcium supplementation, all but one found no significant effect on body weight. Between the
two systematic reviews, over two-thirds of the trials were conducted in post- or perimenopausal
women; the mean age of participants (among trials with data reported in the systematic reviews)
ranged from 36 to 72 years. Only four of the trials were conducted in men. The range of calcium
supplement doses was 700 to 1600 mg/day, with most studies using 1000 mg. The range of
calcium intake among the dairy trials was 610 to 2400 mg/day. In the Trowman et al. (2006)
systematic review,'
15
the range offollowup durations of the trials was 12 weeks to 3 years. The
Barret al. (2003) systematic review
116
included longer duration trials, ranging from 6 months to
4 years.
Findings per calcium intake level.
The systematic reviews did not find evidence of differential effects based on calcium intake
level (supplement dose or dairy calcium).
Findings per age and sex.
The large majority of trials reviewed in the systematic reviews were conducted in
postmenopausal women. The systematic reviews did not find evidence of differential effects
based on age or sex.
Findings by life stage.
0 - 6 mo Not reviewed
7mo-2y
3-Sy
9-18 y
Not reviewed
Not reviewed
Not reviewed
155
19 -50 y Many of the trials are applicable to people within this life stage; though
relatively few trials included men. For both people on energy-restrictive diets and on
isocaloric diets, overall, the evidence suggests no significant effect on body weight with
increased calcium intake, either as supplements or from dairy product intake.
51 - 70 y The majority of studies are applicable to women within this life stage; few
trials included men. The conclusions are the same as for those in the 19-50 y life stage.
2::71 y The evidence is scant for this life stage. Few of the studies appear to have
included people over age 70 years.
Postmenopause The majority of studies are appl icable to postmenopausal women.
The conclusions are the same as for those in the 19-50 y life stage.
Pregnant & lactating women Not reviewed
Table 51. Systematic reviews of calcium supplementation and weight
Author Year [PMID] Lanou 2008
114
(18454813)
Design (Search Years) Randomized controlled trials {19662007)
Population All, generally healthy (adults and children, only studies of adults included here)
Intervention and Comparator Calcium supplements or dairy intake versus no supplement or low calcium intake
Results 29 trialsA
Comments
A priori design?
No energy restriction
Calcium supplement: 8/9 trials no significant effect. 1 found significantly more weight loss
on calcium supplement.
Dairy supplementation: 8/ 10 trials no significant effect. 2 found significantly more weight
gain among those on dairy
Energy restriction
Calcium supplement: 4/5 trials no significant effect. 1 found significantly more weight loss
with calcium.
Dairy supplementation: 3/6 trials significantly more weight loss on high calcium intake
All 4 trials with significant differences were by same study investigators
AMSTAR
Study quality assessment performed? No
Two independent reviewers?
Comprehensive literature search?
Yes
nd
Yes
No
No
Study quality appropriately used in analysis? NA
Appropriate statistical synthesis? None
All publication types and languages included?
Included and excluded studies listed?
Publication bias assessed? No
Conflicts of interest stated? No
Study characteristics provided? Only published trials. Excluded studies not enumerated or listed.
Author Year [PMID]
Design (Search Years}
Population
Intervention and Comparator
Results
Comments
A priori design?
Trowman 2006 [16768823)
Randomized controlled trials (1800
8
/2002-2004}
Nonpregnant, nonlactating, ~ 8 y
Calcium supplements or dairy intake versus no supplement or low calcium intake
13 trials
Calci um supplement WMD = 1.79 (3.04, 0.55)c, statistically homogeneous
Dairy supplementation WMD = +0.85 (4.39, +6.08), statistically heterogeneous
ANCOVA, adjusting for baseline weight:
Calcium Effect= -0.41 ( 1.07, +0.25} kg
Dairy Effect= +0.23 (2.88, +3.34) kg
Apparent difference in effect of calcium supplement trials may be due to significant differences (in
aggregate} in baseline weights of two arms across studies (intervention arm participants were
significantly lighter at baseline).
AMSTAR
Yes Study quality assessment performed? No
Two independent reviewers?
Comprehensive literature search?
nd
Yes
Study quality appropriately used in analysis?
Appropriate statistical synthesis?
Publication bias assessed?
NA
Debatable
Yes All publication types and languages included?
Included and excluded studies listed?
Study characteri stics provided?
continued
Yes
(implied)
No
Yes
Conflicts of interest stated? Yes
Excluded studies not enumerated or listed. Used WMD instead of
net difference, then needed to perform an ANCOVA to adjust for
baseline differences.
156
Author Year [PMID]
Design (Search Years)
Population
Intervention and Comparator
Results
Barr 2003 [12514301 I
Randomized controlled trials (19662001)
All , generally healthy (adults and children, only studies of adults included here)
Calcium supplement or dietary calcium versus no supplement or usual calcium intake (see
Comment
8 trials
Calcium supplement 7/8 trials found no significant effect
Comments 6 dairy supplementation trials reviewed. Not included here. These represent a subset of the dairy
trials reviewed by Lanou 2008
114
A priori design?
Two independent reviewers?
Comprehensive literature search?
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
Yes
nd
Yes
No
No
Yes
AMSTAR
Study quality assessment performed?
Study quality appropriately used in analysis?
Appropriate statistical synthesis?
Publication bias assessed?
Conflicts of interest stated?
Studies publ ished in English only. Excluded studies not
enumerated or listed.
WMD, weighted mean difference
A The systematic review included the Women's Health Initiative (WHI) trial of vitamin D +calcium supplementation. This trial is
omitted here and is discussed separately in the vitamin D + calcium and body weight section.
6
Cochrane Library Database of Controlled Trials
c Numbers in parentheses are 95% confidence intervals
157
No
NA
None
No
No
Table 52. Calcium and weight: Characteristics of RCTs
Author Year Background
Study Name Calcium
Location Population Intake & Comparisons Compliance Comments
(Latitude) Vitamin D
[PMID] Data
Yamamoto Health Healthy Ca 970 mgfd Ca carbonate vs Eligibility for
1995
117
status placebo randomization required
TOHP
Mean age 43 (30-54) consumption of at least
us (range), y two-thirds of 6 wks of
(various)
Male(%) 69
supplement placebo
[7795837] dosing. During the study,
pill counts averaged 95%
(with three-fourths taking
at least 95% of their
su lements .
van Health Healthy nd Ca carbonate vs nd
Beresteyn status placebo
1986
11 8
Mean age 21 (20-23)
Netherlands (range/SO),
(52N) y
[3788835)
Male(%) 0
Health Overweight, nd Ca supplement nd Factorial design
status post vs placebo with weight loss
menopause and
Mean age 61 (52-75) maintenance
(range), y diets
Male(%) 0
Ghadirian Health Healthy, Ca 776 mgfd Dairy vs dairy Non-compliant and those
1995
120
status post free intake who provided incomplete
Montreal, menopause data were excluded.
Canada Mean age -80 (-<!:50)
(46N) (range), y
[7493659)
Male(%) 0
Aloia 1995 Health Healthy, nd Ca supplement nd
Mineola, NY status post- vs placebo (Vit D
(41 N) menopause in both groups)
[7892882) Mean age 53 (0.6)
(SO), y
Male(%) 0
Thomsen Health Healthy, nd Combination Ca nd
1987
122
status post lactate
Copenhagen, menopause gluconate & Ca
Denmark Mean age nd carbonate vs
(55N) (range/SO), placebo
[3307307) y
Male(%) 0
Bortolotti Health Healthy Ca 586 (137 Ca phosphate vs Measured but not Crossover
2008
124
status SE) mg/d, all placebo reported study (5 wk with
Lausanne, o Mean age 22 (1.2) <800 mgld 10wk
Switzerland
(SE), y
washout), 1 o
(4?0N)
Male(%) 30
outcomes were
[1 8842771) metabolic
Kabrnova- o Health Overweight, nd Ca carbonate vs nd (a dietitian checked Energy
Hlavata status healthy "lactoval" vs that subjects took restriction
2008
123
Mean age 49 (12)
placebo tablets)
Lausanne,
(SO), y
Czech Rep
o Male(%} 0
(50N)
[1 7552880) Male(%) 0
158
Table 53. Calcium and weight: Results of RCTs
Author Year
Age Range, Mean Interventions, No. Change Net Net Diff
p
Study
Study Name Outcome 1/2 Unit Baseline Change
l PMID]
Sex Follow up Daily Dose Analyzed 95% CI Diff 95% CI Btw Quality
lsocalori c
Yamamoto Ca carbonate
217 Kg/m
2
27.4 +0.07 -0.05, 0.19 -Q.Q5A -0.23, 0.13
6
NS
1995117
30-54 y,
BMI
20
6 mo
1000 mg
A
TOHP Both
Placebo 218 27.0 +0. 12 -0.02, 0.26
779583
van Ca carbonate
29 Kg 61.8 -0.3 -2. 7, 2.1
8
-0.8 -4.3, 2.7
8
NS
Beresteyn Weight
20 6wk 1500 mg B
1986
118 20-23 y,
Placebo 29 62.5 +0.5 -2.0, 3. 0
13
Netherlands
Women
Ca 29 Kg/m 20.8 -0.1 -0.8, 0.6 -0.2 1 2, _0.8 NS
[3788835]
BMI
20
Placebo 29 21.0 +0.1 0.6, 0.8B
Cifuentes Ca citrate
10 Kg 70.9 0 -3.3, 3.3
8
-0.4c -5.5, 4.7
8
NS
2004
119
52-75 y,
Weight jO 6wk
1200 mg
B
New Jersey Women Ca citrate 400
15 68.0 +0.4 -3.4, 4.2
6
[1 5213038) m
Ghadirian
Dairy intake
81 Kg 59.84 +0. 10 -2.4, 2.6
8
+0.5 -3.7, 4.7
8
NS
1995
120
->=50 y,
(1242 mg Ca)
Canada Women
Weight
20
1 mo Nondairy c
[7493659)
intake (377 77 59.65 -0.40 -3.8, 3.0
8
m
Aloia 1995 Mean (SO) Ca 1700 mg
36 Kg/y 65.8 +0.1 nd 0 nd NS
New York 53 {0.6) y, Weight
20
2.9 y + Vit D 400 IU c
[7892882) Women Vit D 400 IU 28 65.6 +0.1 nd [
~
Thomsen
Ca lactate-
198i
22 Early post- gluconate &
14 Kg 60.6 +0.4 -2.4, 3.2
6
-0.2 -8.0, 7.6
8
NS
Denmark
menopause, Weight
20
1 y carbonate c
[3307307)
Women 200Q!_T1g
Placebo 14 66.4 +0.6 -6.7, 7.9
13
[
Bortolotti
Mean (SE) Ca phosphate Final
Diff
2008
124
Kg Final -5.7, +6.5 NS
Switzerland
22 (1.2) y, Weight
20
5wk 800 mg 10E
78. 1 80.0
+0.4
B
Both -----------
[1 8842771) Placebo 79.6
......................................................__ !
Energy
Restricted
continued
Author Year
Study Name
[PMID]
Kabrnova-
Hlavata
2008
123
Czech Rep
(17552880)
Cifuentes
2004
119
New Jersey
[1 5213038)
Age Range,
Sex
49 (SD) y,
Women
52-75 y,
Women
Outcome
Weight
Weight
Mean
1/2
Follow up
20
3wk
6wk
Interventions,
Daily Dose
Ca carbonate
500 mg + 350
mg Ca in diet
(4.5 MJ/d)
Lactoval (Ca
phosphate,
citrate, &
lactate) 500
mg + 350 mg
Ca in diet (4.5
MJ/d)
Placebo + 350
mg Cain diet
4.5 MJ/d
Ca citrate
1200 mg
(>=2.5% w1
loss _goal)
Ca citrate 400
mg (>=2.5% w1
loss goal)
No.
Analyzed
Unit Baseline Change
21 Kg 85.37 -4.34
25 84.95 -3.34
21 83.43 -3.87
16 Kg 71.5 -3.6
16 74.5 -3.3
Change
95% CI
-4.9, -3.8
-4.0, -2.6
-4.6, -3.2
-6.4, -0.8
8
6.8, 0.2B
Net
Diff
-0.47
+0.53
A Subgroup data available for black and white men and women (4 groups). No substantive differences among groups. All statistically nonsignificant.
8
Estimated from reported data
c Adjusted for multiple factors, including baseline weight.
0
No data on calci um type
e Crossover study
F Adjusted for multiple factors, including baseline weight
160
Net Diff
95%CI
1.4, 0.4
8
P Study
Btw Quality
NS
---------------
B
0.5, 1.5
8
NS
-4.8, 4.2 NS
B
Calcium and Cancer
Cancer from all cause and total cancer mortality.
Synopsis.
No qualified systematic review evaluated associations between calcium intake and incidence
of all cancer and total cancer mortality. One RCT showed a borderline nonsignificant reduction
of the risk of total cancer among healthy postmenopausal women (>55 years old) living in
Nebraska (latitude 41 N) who received calcium supplementation (either calcium citrate 1400
mg/d or calcium carbonate 1500 mg/d) . However, one cohort study analyzed US AARP cohort
(men and women 50-71 y) showed that that total calcium intake was not associated with the risk
of total cancer incident.
There is insufficient data to draw a conclusion regarding association between dietary calcium
intakes and total cancer mortality.
Detailed presentation (Tables 54, 55, 56 & 57).
A 4-year population-based RCT,
52
sampled from a 9-county, largely rural area in eastern
Nebraska (latitude 41 N), aimed to compare the efficacy of vitamin D
3
( 1000 ill/d) plus calcium
(either calcium citrate 1400 mg/d or calcium carbonate 1500 mg/d) or calcium alone (either
calcium citrate 1400 mg/d or calcium carbonate 1500 mg/d) to placebo in reducing fracture
incidence. Incidence of cancer was a secondary outcome of this trial. A total of743
postmenopausal women over 55 years old were analyzed for the effect of calcium
supplementation alone. The mean serum 25(0H)D concentration at baseline was 72 nmol/L.
At the end of study the relative risk of developing cancer was 0.53 (95 percent CI 0.27, 1.03;
P=0.06) comparing calcium supplementation (either calcium citrate 1400 mg/d or calcium
carbonate 1500 mg/d) to the placebo. This study was rated B.
A cohort study analyzed data from AARP (the American Association of Retired Persons)
members, aged 50 to 71 years old, living in six specific states in the US.
125
During 3,383,377
person-years offollowup (over 7 years), a total of36,965 cancer cases in men and 16,605 cancer
cases in women were identified. The results showed that that total calcium intake was not
associated with the risk of total cancer after controlling for potential risk factors pertinent to
individual cancers. Methodological quality of this study was rated B.
Findings by age, sex and/or ethnicity.
A cohort study analyzing a total of 1553 men and 1397 women, aged between 40 and 65
years, living in Amsterdam (52N) showed that there was no significant association between
dietary calcium from foods and total cancer mortality in either men or in women after 28 years of
followup.
126
This study was rated C because the food frequency questionnaire was not internally
validated and could not estimate usual intake through 1-week food frequency recall.
Findings by life stage.
0- 6 mo No data
7 mo - 2 y No data
3- 8 y No data
9- 18 y No data
19 - 50 y A cohort study in Amsterdam included some men and women in this life
stage. However, this study provided insufficient data regarding association between
dietary calcium intakes and total cancer mortality.
51 - 70 y The cohort study in Amsterdam also included some men and women in
this life stage. However, this study provided insufficient data regarding association
between dietary calcium intakes and total cancer mortality. One study analyzed US
AARP cohort with men and women in this life stage showed that that total calcium intake
was not associated with the risk of total cancer incident
~ 7 y No data
Postmenopause One RCT with healthy postmenopausal women showed a
borderline nonsignificant reduction of risk of total cancer by calcium supplementation
(either calcium citrate 1400 mg/d or calcium carbonate 1500 mg/d).
Pregnant & lactating women No data
162
Table 54. Calcium and total cancer mortality: Characteristics of ACTs
Author Year
Study Name
Location
(Latitude)
[PMID]
Lappe
2007
52
Nebraska, US
41 2 N
[17556697]
Population
Health
status
Mean age
(range/SO}, y
Male(%)
Mentally
and
physically
fit
67 (7.3)
0
Background
Calcium Intake
& Vitamin D
Data
25(0H)D: 71.8
nmoVL
Comparisons
Vit 03 1000 IU/d + Ca (citrate
1400 mg/d or carbonate 1500
mg/ d} vs. Ca (citrate 1400
mg/ d or carbonate 1500 mg/d)
vs. placebo
Compliance Comments
Table 55. Calcium and total cancer incidence or mortality: Characteristics of cohort studies
Confounders/Effect Modifiers
Adjusted
Author Year
!1
Study Name ~
c
.1:. Q)
Location Population Dietary Calcium intake Comparisons
c.
:I
E
en ca
en
(Latitude) E c,
c.
(ij
0
Q)
E
0 c.
~
0
[PMID]
Q)
0
.. t)
><
0 ;:
E
.1:.
:0
Q) en
'S Q) 'E
Q)
>
~
z 0 <( ::1: ::::l ::i
Cohort
Park 2009 Health No Dietary FFQ Total cancer X X X X X Total
NIH-AARP status cancer assessment (NCI- risk stratified by calcium
us Mean 50-71 method DHQ} quintile of total intake from
38
2
N age USDA calcium intake diet and
[19237724] (range/}, Nutrient supplement
y Database
Male 60 Internal y
(%) validation?
In
Slob 1993 Health nd Dietary FFQ Cancer X X
Amsterdam status assessment mortality
52N Mean 53 method stratified by
[8478144]
age (40- dietary calcium
(range}, 65} intake quintiles
y (from foods
Male 51 Internal no only)
(%) validation?
~ ~ n
163
Tabl e 56. Calcium and total cancer mort ality: Results of RCTs
Author Year
Followup, Interventions, n N
Outcome
Study
Study Name Life Stage Outcome
10/20
Metric Result 95%CI PBtw
[ PMID]
y Daily Dose Event Tot al
Quality
Lappe Post- Incident cancer (all
20
4 Ca (citrate 1400 17 445 RR 0.53 0.27, 1.03 0.06 B
2007
52
menopausal causes) mg or carbonate Ca/placebo
nd women 1500 mg)
[17556697) Placebo 20 288
Post- Incident cancer
20
4 Ca (citrate 1400 15 416 RR 0.59 0.29, 1.21 0.147
menopausal (restrict to subjects mg or carbonate Ca/placebo
women who were free of 1500 mg)
cancer at 1 y Placebo 18 266
164
Table 57. Calcium and total cancer incidence or mortality: Results of cohort studies
Author Year
Study Name
[PMID]
Park 2009
NIHAARP
125
[19237724]
Life
Stage
50-71,
males
5071 ,
females
Outcome (n/N;
Incidence)
Total cancer
(36,965/3,383,377
person-years)
Total cancer
(16,605/3,383,377
person-years)
Followup
Duration
(Time to
Ox)
7y
7y
Total Ca
Intake,
mg/day
526
No. of
Cases
No. in Category
3,383,377 person
36
965
years (total, both
__ _
Adjusted
OR
1 (HR)
....................... ...................... ...........................................________ (),9.9.
857 0.99
494
16
605
3,383,377 person- 1 (HR)
years (total, both
(total) males and females)
....................................................................................................
95%CI
Reference
0.96, 1.03
0.96, 1.03
0.96, 1.03
0.95, 1.03
Reference
717 --------................9:.9..?. ................. 0.93,1.03
....................... ...................... ..........................................: 0.89, 0.99* 000
.....................1 ..?..9..E>................... ........................................... (),9.?. 0.88, 0.98*
1881 0.96 0.91, 1.02
P for
Trend
0.74
0.23
Slob 1993
nd
[8478144]
4065 y,
males
Cancer mortality
(232/ 1553; 0.15)
28 y nd nd 1.0 0.6, 1.6 nd
4065 y,
females
Cancer mortality
(127/ 1397; 0.09)
28 y
-----,-----
........!5.?!5J() ... 11<:1 ------'n.:.::d=----- 1:() _Qjl_,J_,L_
........?..?!51() ... .........................11.<:1................. nd 1 :Cl 0. 6, 1 . 5
935 to nd nd 0.8 0.5, 1.3
-----,-----..................................................--=-:----
..................;:'i245"'"'"'"'' ..................nd................ nd 1 .0 Reference
nd nd 1.1 0.6, 2.1
44510 nd ----n-d:-----
0.8 0.4, 1.5
-----:----- 000000000000000000000000000000000000 --:-:::-::--::---
........4.9 ..'!9 .. ............ ...............: nd .................J ...&..... 0.9, 2.8
11<:1 .------'n.:.:: d=-----....................1 ...:.": ................... __ 0. 7, 2.5 __
>850 nd nd 1.0 Reference
Not a reasonable number based on the reported confidence interval; probably a typographical error in the article.
165
nd
Study
Quality
B
c
Prostate cancer.
We reviewed primary studies that evaluated associations between calcium intake and
incidence and mortality of prostate cancer.
Synopsis.
No trials of calcium interventions evaluated prostate cancer. Four cohort studies rated A in
methodological quality reported on the association between total calcium intake and the risk of
prostate cancer. Three studies found significant associations between higher calcium intake and
increased risk of prostate cancer. One study found the risk was higher in the group that took
more than 1500 mg/d of calcium compared to those that took less than 700 mg/d (adjusted RR
1.3). A second study found only the group that took more than 2000 mg/d of calcium had higher
risk of prostate cancer compared to those that took 500 to 749 mg/d of calcium (adjusted RR
1.26). A third study also found that male smokers who took more than 2000 mg/d of calcium
had higher risk compared to those who took less than 1000 mg/d (adjusted RR 1.63). The fourth
study found no relation between calcium intake ( <500 to 2:2000 mg/d) and the risk of prostate
cancer in men aged 50-70 years.
Detailed presentation (Tables 58 & 59; Figure 13 ).
A total of 12 cohort studies in 13 publications reported on the association between calcium
intake and the risk of prostate cancer.
56
'
127
-
138
One of the studies also provided a post hoc analysis
of an RCT on calcium supplement.
56
The incidence of prostate cancer in these studies ranged
from 0.008 to 0.10. Most of the studies were conducted in Europe or North America, one study
was conducted in Japan. Mean age of the subjects ranged from 53 to 67 years. Total calcium
intake ranged from less than 500 mg/d to at least 2000 mg/d. Time between dietary assessment
and the diagnosis of prostate cancer varied from 1 to 17 years. Methodological quality of four
studies was rated A, seven studies were rated B, and one study was rated C.
19-50 years.
No study specifically targeted men between 19 to 50 years old.
51-70 years.
Twelve studies reported data on subjects with a mean age ranged from 53 to 67 years. Seven
studies did not find an association between calcium intake and the risk of prostate
cancer.
56
,
130
,
131
,
133
134
'
136
,
137
Five studies found that the risk was higher in the groups that took
more calcium compared to the groups that took lower amount (adjusted OR 1.2-
2.2).127'129' 132' 135'138 The higher amount ranged from 921 to at least 2000 mg/d of calcium; the
lower amount ranged from 455 to 1000 mg/d. Three studies also reported on the association
between calcium intake and mortality from prostate cancer. Two studies found no
association
130
'
134
and one study found an increased risk comparing the group that took at least
2000 mg/d of calcium with the group that took 500 to 749 mg/d (adjusted RR 2.02, 95 percent CI
1.14, 3.58).
129
One study was a post hoc analysis of an RCT of high calcium supplement (1200
mg/d) to prevent colorectal adenoma.
56
This study did not find an increased risk of prostate
cancer in those supplemented with calcium compared to those who were not (unadjusted RR
0.83, 95 percent CI 0.52, 1.32). This study did not adjust for factors potentially relevant to
prostate cancer.
166
Findings by life stage.
0- 6 mo Not applicable
7 mo- 2 y Not applicable
3 - 8 y Not applicable
9- 18 y Not reviewed
19- 50 y No study specifically targeted men 19 to 50 years old.
51 - 70 y Seven studies did not find an association between calcium intake and the
risk of prostate cancer. Five studies found that the risk was higher in the groups that took
more calcium compared to the groups that took lower amount (adjusted OR 1.2-2.2). The
higher amount ranged from 921 to at least 2000 mg/d; the lower amount ranged from 455
to 1000 mg/d.
?:71 y No study specifically targeted men older than 70 years.
Postmenopause Not applicable
Pregnant & lactating women Not applicable
167
Table 58. Calcium and cancer: Characteri stics of observati onal studies
Confounders/Effect Modifiers
Author,
Adjusted
Year
Trial/Cohort
Name Population Dietary calcium intake Comparisons (.)
Country :c
Cl)
..
c.
::J U)
U)
(Latitude) U)
E
U)
Cl)
'E
'E
c.
iii
0
Cl)
[PMID]
Cl
0
c.
0 .. (.)
>< U) E
E
.r.
'5
Cl)
E
5 Cl) 'E
Cl)
> 0
z 0 ct :::E ::;) ::i (.)
Park Health 12% Dietary 124-item Prostate X X X X X 92% white;
2007
134
status current assessment FFQ cancer risk Total Ca
NIH-AARP smoker method stratified by (both)
Diet& Mean age 50- different
Health (range/SO), 71 (est.) intakes of
us y calcium
(multiple Male(%) 100 Internal y (dietary and
latitudes) validation? supplement
[ 18000020)
(:ti n}
combined)
Rodriguez Health 9.5% Dietary 68-item FFQ Prostate X X X X Total Ca
2003
1 5
status current assessment (modified cancer risk (both)
CPS II smoker method Block) stratified by
Nutrition Mean age 64 different
Cohort (range/SO), intakes of
us y calcium
(multiple Male(%) 100 Internal y (dietary and
latitudes) validation? supplement
[12869397) (y/n) combined &
dietary
calcium
alone
Giovannucci Health -10% Dietary Semi- Prostate X X X X X >91%
2006128
status current assessment quantitative cancer risk white;
2007
129
smoker method FFQ stratified by Total Ca
HPFS Mean age 40-75 different (both)
us (range/SO), intakes of
(multiple y calcium
latitudes) Male(%) 100 Internal y
(dietary and
[1 6492906) validation? supplement
[ 17450530)
combined)
Mitrou Health all Dietary 276-item Prostate X X X X X 100%
2007
132
status smokers assessment FFO cancer risk white;
ATBC Mean age 57 (est.) method stratified by Total Ca
Finland (range/SO), different (food)
(60N) y intakes of
[1 7106437) Male(%) 100 Internal y calcium
validati on? (dietary and
(y/n) supplement
combined
Park Health -17% Dietary self- Prostate X X X X -equal%
2007
133
status current assessment administered cancer risk of African
MCS, HI, smoker method FFQ stratified by Americans,
CA Mean age 45-75 different native
us (range/SO), intakes of Hawaiians,
(multiple y dietary Japanese
latitudes) Male(%) 100 Internal y calcium Americans,
[ 17925283) validation? Hispanics,
(y/n) whites;
Total Ca
both
continued
168
Confounders/Effect Modifiers
Author,
Adjusted
Year
Trial/Cohort
Name Population Dietary calcium intake Comparisons (.)
Country :c
Cl)
..
c.
::J U)
U)
(Latitude) U)
E
U)
Cl)
'E
'E
c.
iii
0
~
Cl)
[PMID]
Cl
0
c.
~
0 .. (.)
>< U) E
E
.r.
'5
Cl)
~
E
5 Cl) 'E 41
> 0
z c c(
~
::::> ::; (.)
Chan
Health on ASA,
D1etary short self- Prostate ' ---r- X x Total Ca
2001
127
status ~
assessment administered cancer risk (dairy)
PHS
carotene,
method questionnaire stratified by
us
placebo
different
(multiple
trial;
intakes of
latitudes)
-1 1%
dietary
(11566656)
current
calcium
smoker
Mean age 53
(range/SO),
y
Male(%) 100 Internal n
validation?
In
Koh Health 7.5% Dietary 23-item FFQ Prostate X X X X Total Ca
2006
130
status smoker assessment (Willett 1985, cancer risk (dairy)
HAH Mean age 67 method 1987) stratified by
us (range/SO), different
(multiple y intakes of
latitudes) Male(%) 100 Internal n
dietary
[17106437)
validation?
calcium
In
Schurrman Health nd Dietary 150-item Prostate X X Total Ca
1999
137
status assessment semi- cancer risk (food)
Netherlands Mean age 61 method quantitative stratified by
Cohort (range/SO), FFQ quinti le of
(52N) y dietary
(10362125) Male(%) 100 Internal n calcium
validation? intakes
In
Kurahashi Health -44% Dietary FFQ Prostate X X X Total Ca
2008
13 1
status current assessment cancer risk (food)
Japan PHC smoker method stratified by
(multiple Mean age 45-74 quartiles of
latitudes) (range/SO), dietary
(1 8398033) y calcium
Male(%) 100 Internal y intakes
validation?
In
Rohrmann Health 17% Dietary 60-item FFQ Prostate X X X 99%white;
2007
136
status current assessment (Block) cancer risk Total Ca
WCC,MD smoker method stratified by (both)
us Mean age 54 tertiles of
(39
2
N) (range/SO), calcium
(1 7315319) y intakes
Male(%) 100 Internal n (dietary and
validation? supplement
In
combined)
continued
169
Confounders/Effect Modifiers
Author,
Adj usted
Year
Trial/Cohor t
Name Population Dietary calcium intake Comparisons (.)
Country :c
Cl)
..
c.
::J
Ul
Ul
(Latitude) Ul
E
Ul
Cl)
'E
'E
c.
iii
0
>.
Cl)
[PMID]
Cl
0
c.
0 .. (.)
><
....
E
Ul
E
.r.
'5
Cl)
.!!
E
5 Cl) 'E 41
> 0
z c c(
::::>
:::; (.)
Health nd
D1etary i 6S-1tem Prostate
X , ---y-
X x 88% white;
2005
38
status
assessment FFQ cancer risk 11% black;
NHEFS
Mean age 58(14.6)
method stratified by Total Ca
us
(range/SO),
tertiles of (both)
(multiple
y
calcium
latitudes)
Male(%) 100 Internal n
intakes
(1 5883441]
validation?
(dietary and
(y/n)
supplement
combined)
Baron Health had >1 Dietary FFQ (Block, Prostate X X 5% black;
2005
56
status colon assessment 1986) cancer risk Total Ca
CPP adenoma method stratified by (suppl)
us removal tertiles of
(multiple
Mean age 62 (8.7)
dietary
latitudes)
(range/SO),
calcium
(15767334]
y
intakes
Male(%) 100 Internal N
validation?
170
Tabl e 59. Calcium and prostate cancer: Results of observational studies
Author Year Life
Out come Follow up
Total Ca
No. of Total no. i n Adjusted P for Study
Study Name Stage i ntake in 95% CI
[ PMID] (male), y
(n/N; Incidence) Duration
mg/d
Cases Category RR Trend Quality
Park Prostate cancer
2007
134
51 -70 (1 0, 180/293,888; 8y <500 767 nd 1.01 0.93, 1.10
NIH-AARP Diet & Health 0.035)
................................,_
[1 8000020) 500-<750 2927 nd 1 Reference
. --------
750-<1000 2808 nd 0.99 __
0.41
1000-
<1500
2572 nd 0.99 0.93, 1.05
1000-
2572 nd 0.99 0.93, 1.05
<1500
-------------
<?:2000 309 nd 0.97 0.85, 1.10 A
Mortality
<500 11 nd 0.76 0.38, 1.53
Prostate cancer
500-<750
----43---
nd 1 Reference ..
750-<1000 56 nd 1.50
...
1000-
50 nd 1.42 0.86, 2.35
0.99
<1500
1500-
18 nd 1.05 0.54, 2.05
-------------
<?:2000 0 nd
Rodriguez
51 -70
Prostate cancer
S7 y <700 1323 23,653 Reference
2003
1 5
(3811 /65,321; 0.058)
-------------
CPS II 700-999 1293 nd 1.0 0.9, 1.1
0.02 A
[1 2869397] 1000-1 499 835 nd 1.0 ___ ......
1500- 1999 265 nd 1.3 1 .. ! .!:_.:.. __
<?:2000 95 1330 1.2 1.0, 1.6*
Giovannucci 2006 19-50 Prostate cancer
S16 y <500 183 nd 0.98 0.84, 1.15
HPFS 51 -70 (3544/47,750; 0.074)
[1 6492906) [17450530) 750-999 1099 nd 1.07 __
500-749
---
1072 nd 1 Refe!_e.!l4i!_ 0. 10
1500-1999 207 nd 1.06
__ ....
1000- 1499 898 nd 1.03
J ..:.!4. ....
<::2000 85 nd 1.28 1.02, 1.60*
A
Mortality
<500 21 nd 1.05 0.65, 1.69
Prostate cancer .....-........, .., __ ,_, __,_,_
750-999 81 nd 0.95
O}Q,_L?..?. ......
500-749 94 nd 1 Reference 0.01
------
1500-1999 26 nd 1.56
1000-1 499
------76
nd 1.04 ...... <uz, __1.42
<?:2000 14 nd 2.02 1.14, 3 58*
Continued
171
Author Year Life
Outcome Follow up
Total Ca
No. of Total no. in Adjusted P for Study
Study Name Stage
(n/N; Incidence) Duration
intake in
Cases Category RR
95% CI
Trend Quality
(male), y mg/d
1trou
51-70
Prostate cancer
S17 y <1000A 151 nd Reference
2007
132
(1267/27,028; 0.047)
ATBC
1000-1499 61 1
_11L_ 1.07, 1.54.*
<0.0001 A
[1 7106437)
1500-1999 402 nd 1.38
.......L1.4..t.1.,6.!*. ..
<!:2000 103 nd 1.63 1.27, 2.10*
Park 19-50 Prostate cancer
8y <470 706 nd Reference
2007
133
51 -70 (4404/82,483; 0.053)
MCS 470-692 925 __ n_d 1.03 1_,1"5
0.69 B
[1 7925283)
692935 949 nd 1.04
935-1300 936 nd 1.05 __
<!: 1301 888 nd 1.04 0.91, 1.20
Chan
51 -70
Prostate cancer
S11 y 0 150A 155 nd Reference
2001
127
(1 012/20,885; 0.048)
PHS 151-300 206 nd 1.21 J.3 0.05 B
[1 1566656) 301-600 377 nd 1.35
. ..
>600 274 nd 1.29 1.04, 1.62*
Koh
51 -70
Prostate cancer
S10 y 0 199A 209 nd Reference
2006
130
(815/ 10,011 ; 0.081)
HAH 200-449 167 nd 0.81
....... Q,64.,J,.Q? ..
0.64
[1 7106437) 450-599 238 nd 0.91
__ .Q,Z?.,J.J.1.
>600 201 nd 0.91 0.70, 1.18
B
Mortality
0-199 30 nd 1.00 Reference
Prostate cancer
200-449 21 nd 0.57
() ,?.?., ...
0.52
450-599 23 nd 0.60 0.29, 1.22
<!:600 25 nd 0.81
Schuurman
51 -70
Prostate cancer
S6.3 y
602A,B
120 nd Reference
1999
137
(704/58,279; 0.012)
Netherlands Cohort 780 126 nd 1.10
QJ30,J1.
0.34 B
[1 0362125)
911 127 nd 1.04 0.76, 1.42
1064 140 nd 1.21 a:a9:1-:ss
1329 129 nd 1.09 o:79, i.5o
Kurahashi 19-50 Prostate cancer
S7.5 y 283A.B 56 nd Reference
2008
131
51 -70 (329/43,435; 0.008)
Japan PHC 404 68 nd 1.03 0.70, 1.51 0.1 6 B
[1 8398033)
522 98 nd 1.32
--o:92;T9o
725 107
--nd
1.24 o.as; 1.81
Rohrmann
51 -70
Prostate cancer
S15 y <686 58 nd Reference
2007
136
(199/ 3892; 0.051)
0.99 B
wee 686-958 65 nd 0.98 __ .Q,Z?,J.,.4.?. .
[1 7315319)
>958 76 nd 0.99 0.70, 1.41
Continued
172
Author Year Life
Outcome Follow up
Total Ca
No. of Total no. in Adjusted P for Study
intake in 95% CI Study Name Stage
(n/N; Incidence) Duration Cases Category RR Trend Quality
:l matd
51-70
Prostate cancer
7.7 y 455
8
28 nd Reference
2005
8
(131/ 3779; 0.035)
0.001 8
NHEFS
642 37
1.0 0.6, 1.7
[1 5883441)
921 66 nd 2.2 1.4, 3.5*
Baron
51 -70
Prostate cancer
S12 y
<675A,B
nd nd 1 Reference
2005
56
(70/672; 0.1 0)
......
0.51 c
CPP 675-991 nd nd 1.48
(15767334) >991 nd nd 1.20 0.64, 2.23
* Statistically significant (P<0.05)
A Dietary calcium
8
median of tertile, quartile or quintile
c Adjusted hazard ratio
173
Figure 13. Prostate cancer risk stratified by calcium intake
Ca Pfor
Study Category intake (mg/d) trend Quality
Park 2007 Catl <500
-
0.41 A
(n=293,888) Cat 2 (ref) 500 - 750
Cat3 750-1000 oo4io
Cat4 1000-1500
Cat 5 1500 - 2000
.::
Cat6 >2000
2003 - cat1VetT <700
b
0.02
A-
(n=65,321) Cat2 700-999
Cat3 1000 - 1499
Cat4 1500-1999
Cat 5 >2000
Glovannuccl 2006 & 2007 Catl <500
L
0.10 A
(n=47,750) Cat 2 (ref) 500 - 749
Cat3 750-999
Cat4 1000-1499
CatS 1500 - 1999
Cat6 >2000
-
Park 2007 Cat 1 (ref ) <470
I
0.69 B
(n=82,483) Cat2 470 - 692
Cat3 692-935
Cat4 935-1300
Cat 5
- Mitrou2007 Cat 1 (ref) <1000
1
<0.0001 B
(n=27,028) Cat2 1000-1499
Cat3 1500-1999
:C han 2001
Cat4 >2000
- Cat 1 (ref) 0-150
f:=:=_
0.05 B
(n=20,885) Cat2 151 -300
Cat3 301 - 600
Cat4 >600
-
:- Koh 2006 Cat 1 (ref) o7 199
-3:_
0.64 B
(n=10,011 ) Cat2 200-449
Cat 3 450 - 599
Cat4 >600
Scnuurman 1999 0 1 (ref ) 602
E
0.34 B -
(n=58,279) 02 780
03 911
Q4 1064
05 1329
J<U"rafmtti2oo8 Of(ref) 283
f
o.i6 B
(n=43,435) 02 404
03 522
:- Rohrmann 2007 -
Q4 725
- Ti(retr--<6ar-
!
0.99 B
(n=3892) T2 686-958
]
T3 >958
""1Se'i)g 2005 Tl (ref) 455 0.001
B-
(n=3779) T2 642
T3 921
Ba'ron 20o5 T1 (ref) <675 Qs1 c
--
(n=672) T2 675 - 991
T3 >991
I I I
05 2 4
Decreased risk Increased risk
174
Colorectal cancer.
Synopsis.
This synopsis is based on one systematic review, 19 cohort studies in 20 publications, and
one nested case-control study. The systematic review of two RCTs that evaluated high risk
population found no difference in colorectal cancer incidence between those participants who
received supplemental calcium and those who did not. Among five cohort studies and one nested
case-control study with methodological quality B, two cohort studies showed a significant
inverse association between total calcium intake and colorectal cancer. Among 14 cohort studies
with methodological quality C, five studies showed a significant inverse association between
total calcium intake and colorectal cancer, one found an inverse association between total
calcium intake and colon cancer, and two showed an inverse association between calcium and
rectal cancer. All the studies that found a significant association recruited men or women who
were followed for a period that ranged between 1.4 and 11.3 years. None of these studies
included participants younger than 45 years.
Detailed presentation (Tables 60, 61,62 & 63; Figures 14, 15, 16, 17 & 18)
One systematic review of two RCTs of supplemental calcium on prevention of recurrent
colorectal adenoma comprising 1346 adults (mean age 59 to 61 years) examined colorectal
cancer incidence.
139
A fixed-effects model meta-analysis found no significant difference in
colorectal cancer incidence between supplemental calcium and no supplements. This meta-
analysis is considered inconclusive because only 5 colorectal cancer cases were diagnosed during
the study period.
Nineteen cohort studies in 20 publications
125
'
140
"
158
and one nested case-control study
159
evaluated the association between calcium intake and colorectal, colon, or rectal cancer. Sample
sizes ranged from 1954 to 492,810. Half of the studies were conducted in the US (latitude ranged
from 21 oN to 54o N),I25, 140,I42,144,145,147,1 50-1 52,154,155,1 58 one study was conducted in China
(latitude 31 N),
149
and the rest were conducted in Europe including France (latitude 46 N),
141
the Netherlands (latitude 52 N),
159
the United Kingdom (latitude ranged between 54 Nand 55
N),
156
and Scandinavia (latitude ranged between 59 Nand 69 N).
143
146
148
153
157
For colorectal
cancer, the incidence ranged from 0.003 to 0.025 for cohorts, while in the nested case-control
study, the colorectal cancer incidence was 0.142; for colon cancer, the incidence ranged from
0.003 to 0.024; and for rectal cancer, the incidence ranged from 0.003 to 0.004. The participants'
mean age ranged from 7.6 to 61.9 years. Average followup ranged from 1.4 to 19.6 years. Only
one study reported that exposure assessors were blinded to outcome.
154
No studies mentioned
that outcome assessors were blinded to exposure. None of the studies reported power
calculations. The majority of the studies evaluated the potential effect of various factors besides
calcium on colorectal cancer. All performed analyses adjusted at least for age. Except for four
studies
151
156
-
158
that used dietary history, all other studies used a food frequency questionnaire to
assess dietary intake. More than half of the studies did not confirm all or part of cancer cases
with pathology reports. Six studies
125
140
-
143
159
were rated B, and 15 publications
144
-
158
were rated
C for methodological quality.
175
Findings by age, sex and/or ethnicity.
One cohort study analyzed a total of 4374 children (IQR 4-11 years old) living in the United
Kingdom. It found no significant association between total calcium intake and colorectal cancer
in these children after 65 years of followup.
156
One cohort study analyzed a total of 127,749 adults aged between 50 and 74 years old living
in US. It found an inverse association between total calcium intake and colorectal cancer.
145
However, another cohort study and one nested case-control study did not find such an
association.
157
159
The only cohort study that analyzed subjects older than 15 years did not find a
significant association between total calcium intake and colon cancer as well as rectal cancer in
subgroup analyses.
157
Out of seven cohort studies
125
'
140
143
-
145
'
148
154
that analyzed male adults
older than 40 years living in US, or Scandinavia, five
125
'
143
-
145
'
148
found an inverse association
between total calcium intake and colorectal cancer. Out of eleven cohort studies
125
140
-
142
144
-
147' 149' 154' 155 that analyzed women, four
125
144
'
146
'
147
found an inverse association between total
calcium intake and colorectal cancer.
Out of four cohort studies
145
'
148
'
151
'
153
that analyzed men, one
145
found an inverse association
between total calcium intake and colon cancer in a subgroup analysis. Out of four cohort
studies
146
147
150
153
that analyzed women, none found an association between total calcium intake
and colon cancer. For rectal cancer, one
148
oftwo
145
'
148
studies that analyzed men and one
152
of
three
146
147
152
studies that analyzed women found an inverse association between total calcium
intake and rectal cancer.
148
'
152
One cohort study in the US found an inverse association between total calcium intake and
colorectal cancer in a subgroup analysis of Japanese Americans aged 45 to 75 years, and a
borderline inverse association in Caucasians of the same age range; however, the same cohort
study did not find any significant association in subgroup analyses of African Americans, Native
Hawaiians, and Latinos.
144
Another cohort study in the US that recruited only Japanese
American men living in Hawaii did not find an association between total calcium intake and
colon cancer.
151
One cohort study did not find any association in Chinese women (aged 40 to 70
years) living in Shanghai,
149
Findings by life stage.
0- 6 mo No data
7mo-2y Nodata
3 - 8 y One study that followed up children with an interquartile range of age of 4
to 11 years for 65 years found no significant association between total calcium intake at
baseline and the risk of colorectal cancer.
9 - 18 y Three studies included some children and/or adolescents in this life stage,
but no studies adequately evaluated this life stage.
19-50 y Four studies included people with a mean or median age ranging from 39
to 50 years. No significant association was found between total calcium intake and
colorectal cancer risk. Ten additional studies may have included participants in this life
stage; however in these studies, no conclusions are possible for the subgroup in this life
stage.
51-70 y One inconclusive meta-analysis of2 RCTs in adults with previous
adenomatous polyps (mean age 59-61 years) found no significant difference in colorectal
cancer incidence between those who were and those who were not supplemented at
followup. Ten studies included people with a mean or median age ranged from 53 to 69
176
years. An association between higher total calcium intake and lower colorectal cancer
risk was found in three studies in men and two studies in women. Another study of
women found an association between higher total calcium intake and lower rectal cancer
risk. Ten additional studies may also have included participants in this life stage An
association between higher total calcium intake and lower colorectal cancer risk was
found in two studies in men and two studies in women. However in these studies, the
results are inconclusive for the subgroup in this life stage.
71 + One study that specifically included people in the retirement community
found no association between total calcium intake and colorectal cancer risk. Nine
additional studies may have also recruited participants in this life stage; however in these
studies, no conclusions are possible for the subgroup in this life stage.
Postmenopause One study focused on postmenopausal women. This study found
an association between higher calcium intake and lower rectal cancer risk. However, it
did not find any association for colon cancer risk.
Pregnant & lactating women No data
177
Table 60. Systematic review of calcium supplementation and colorectal cancer incidence or
adenoma recurrence
Author Year [PMID]
Design
Population
Intervention (Exposure) and
Com arator
Results
Comments
A priori design?
Weingarten, 2008
139
(18254022]
Randomized controlled trials: Cochrane Library Issue 2, 2007, the Cochrane Colorectal Cancer
Group (CCCG) specialized register, MEDLINE {1966 to July 2007 ), Cancerlit {1963 to April
2002), Embase (1980 to July 2007)
Healthy adults and studies of adults at higher risk of colon cancer due to family history, previous
adenomatous polyps, or inflammatory bowel disease
Calcium (> 1200 mg/d) vs. placebo
Calcium vs. placebo
Colorectal cancer incidence: OR 0.34, Cl 0.05-2.15, P=0.20 (1
2
=0%)
Colorectal adenoma recurrence: OR 0.74; 95%CI 0.58, 0.95, P=0.02 (1
2
=0%)
At least one adverse event requiring discontinuation: OR 0.93; 95% Cl 0.42, 2.05, P=0.80
Based only on two RCTs {1346 participants). Heterogeneity due to different dose of
supplementation (one RCT supplemented with 1200 mg/d and the other RCT with 2000 mg/d).
Analysis based on fixed effects model ; however, considering there are only two studies, random
effects model might have been more appropriate. The result of no significant difference in
colorectal cancer incidence is inconclusive since there were only 5 colorectal cancer cases
during the study period. Analy,sis on adverse events is based only on reported data of one out of
the two RCTs (Barron 1999).
60
Only participants with high risk due to previous adenomas were
recruited in these two RCTs; therefore, applicability of the results can only be considered for
high risk population. Insufficient evidence to recommend the general use of calcium
supplements to prevent colorectal adenoma or colorectal cancer
AMSTAR
Study quality assessment performed?
Two independent reviewers?
Comprehensive literature search?
X
X
X
Study quality appropriately used in analysis?
Appropriate statistical synthesis?
Publication bias assessed?
X
X
X
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
X
X
Conflicts of interest stated? X
178
Table 61. Calcium and colorectal cancer: Characteristics of observational studies
Confounders/Effect
Author, Year
Modifiers Adjusted
Trial/Cohort
CJ
Name
Population Dietary Calcium intake Comparisons
:.c
Comments
Country
c. U)
U)
<II U)
CD
... ...
c.
~ (Latitude)
c: Cl 0
iii c:
~
0 ... CJ 0
U)
[Pubmed ID]
E
.c
'6
U)
'5 i:
<II
.2!
CD CD
CD
z c <( ~ en
::;
Cohort
Park, 2009 Health Generally Dietary Semi- CRC across 5 X X X X X White
NIH-AARP status healthy assessment quantitati categories of Male -92%;
Diet & Health men and method ve FFO total calcium Female
(various) women (NCI- intake -89%; Total
us Mean age 50-71 DHQ) Ca (both)
[19237724) range, yr
Male(%) 60 Internal y
validation?
(y/n)
Wu, 2002
140
Health HPFS: Dietary HPFS: For HPFS, X X X X X Total Ca
HPFS status generally assessment 131-item NHS (both)
NHS healthy method semi- separately:
(various) male health quantitati CRC across 7
us professional ve FFQ categories of
[11904316) s (by cumulative
NHS: Willet) average
generally calcium intake
healthy NHS:61-
female item
nurses semi-
Mean age HPFS: 54.4 quantitati
(range/SO), NHS: 46.6 ve FFQ
yr (by
Willet)
Male(%) HPFS: 100 Internal y
NHS:O validation?
(y/n)
Kesse, Health Generally Dietary FFO CRC across X X X X Total Ca
2005
141
status healthy assessment total calcium (food)
Etude women method intake
Epidemiologi Mean age 52.7 quartiles
que aupres (range/SO),
de femmes yr
de Male(%) 0 Internal y
!'Education validation?
Nationale
France
(y/n)
(46N)
[1588053?{
Lin, 2005
14
Health Generally Dietary 131-item CRC across X X X X X Total Ca
WHS status healthy assessment FFQ total calcium (both)
us women method intake
(various) Mean age nd quintiles
[15800268) (range/SO),
yr
Male(%) 0 Internal y
validation?
In
continued
179
Confounders/Effect
Author, Year
Modifiers Adjusted
Trial/Cohort
CJ
Name
Population Dietary Calcium intake Comparisons
:.c
Comments
Country
c.. U)
U)
<II U)
CD
... .... c..
~ (Latitude)
c: Cl 0
iii c:
- ~
0 .... CJ 0
U)
[Pubmed ID]
E
.c:
'6
U)
'5 i:
<II
.2!
CD CD
CD
z c <( ~ en
::;
Pietinen,
Health Generally Dietary 276-item CRC across X x X x Total Ca
1999
143
status healthy assessment FFQ total calcium {food)
ATBC men; method intake
Finland smokers quartiles
(-64N)
Mean age Median,
[10530608)
(range/SO), cases: 60.1;
yr non cases:
57.1
Male(%) 100 Internal y
validation?
~ n )
Park, 2007'
44
Health Generally Dietary FFQ CRC per X X X X X Total Ca
The status healthy assessment gender across (both)
Multiethnic men and method total calcium
Cohort Study women intake
us Mean age nd quintiles
(various) (range/SO),
[17215380) yr
Male(%) 45 Internal y
validation?
(y/n)
McCullough, Health Generally Dietary 68-item CRC across X X X X X Total Ca
2003
145
status healthy assessment semi- total calcium (both)
CPS II men and method quantitati intake
us women ve FFQ quintiles
(various) Mean age nd (modifica
[12708719) (range/SO), tion of Subgroup
yr the brief analyses per
Health gender
Habits
and For men,
History subgroup
Question analyses per
naire site (colon,
(HHHQ) rectal)
by Block)
Male(%) 48 Internal y
validation?
~ n )
Shin, 2006
149
Health Generally Dietary 77-item CRC across X X X X Chinese;
Shanghai status healthy assessment FFQ total calcium Total Ca
Women' s women method used in intake (food)
Health Study Mean age Cases: 59 Shanghai quintiles
China (range/SO), {8.5); non- Women's
(31N) yr cases: 52 Health Subgroup
[17019716) (9.1 ) Study analyses per
site (colon,
Male(%) 0 Internal y rectal)
validation?
In
continued
180
Confounders/Effect
Author, Year
Modifiers Adjusted
Trial/Cohort
CJ
Name
Population Dietary Calcium intake Comparisons
:.c
Comments
Country
c.. U)
U)
<II U)
CD
... .... c..
~ (Latitude)
c: Cl 0
iii c:
~
0 .... CJ 0
U)
[Pubmed ID]
E
.c:
'6
U)
'5 i:
<II
.2!
CD CD
CD
z c <( ~ en
::;
Terry,
Health Generally Dietary s ell- CRC across X x X x Total Ca
2002
146
status healthy assessment administ total calcium (food)
Swedish
women method ered 67- intake
Mammograp
Mean age nd
item FFQ quartiles
hy Screening
(range/SO).
Cohort
yr
Subgroup
Sweden
Male(%) 0 Internal y
analyses per
(59N)
validation?
site (colon,
[1 2467133)
(y/n)
rectal)
Subgroup
analyses per
age(< 55 vs.
~ 5 5 years
old) and site
(colon, rectal)
Gaard,1996 Health Generally Dietary semi Colon cancer X X X Total Ca
3
status healthy assessment quantitati per gender {food)
nd men and method ve FFQ across total
Norway women (Oslo calcium intake
(6o-69N) Mean age 43 Universit quartiles
[9061 275) (range/SO). y)
yr
Male(%) 49 Internal y
validation?
In
Flood, Health Generally Dietary 62-item CRC cancer X X X X X Total Ca
2005
147
status healthy assessment semi across total (both)
The Breast women method quantitati calcium intake
Cancer Mean age 61.9 ve FFQ quintiles
Detection (range/SO), (by
Demonstratio yr Block) Subgroup
n Project
Male(%) 0 Internal y analyses per
(BCDDP) validation? site (colon,
us
(various)
(y/n)
rectal)
[1 5668485)
Larsson, Health Generally Dietary 96-item CRC across X X X X X Total Ca
2006
148
status healthy assessment semi- total calcium (both)
The Cohort men method quantitati intake
of Swedish Mean age 60.3 ve FFQ quartil es
Men (range/SO),
Sweden yr Subgroup
(59N)
Male(%) 100 Internal y analyses per
[16522915) validation? site (colon,
In
rectal)
Bostick, Health Generally Dietary 127-item Colon cancer X X X Same cohort
1993
150
status healthy assessment semi- across total as Zheng
Iowa post- method quantitati calcium intake 1998; Total
Women's menopausa ve FFQ quintiles Ca (both)
Health Study I women (by
us Mean age 61.5 Willet)
(40N ) (range/SO),
[8333412) yr
Male(%) 0 Internal y
validation?
( In
continued
181
Confounders/Effect
Author, Year
Modifiers Adjusted
Trial/Cohort
CJ
Name
Population Dietary Calcium intake Comparisons
:.c
Comments
Country
c.. U)
U)
<II U)
CD
... .... c..
~ (Latitude)
c: Cl 0
iii c:
~
0 .... CJ 0
U)
[Pubmed ID]
E
.c:
'6
U)
'5 i:
<II
.2!
CD CD
CD
z c <( ~ en
::;
Zhen&, Health Generally Dietary 127-item Rectal cancer X x X x x Same cohort
1998
2
status healthy assessment semi - across total as Bostick
Iowa post- method quantitati calcium intake 1993; Total
Women's menopausa ve FFQ tertiles Ca (both)
Health Study I women (by
us
Mean age 61.5 Willet)
(40N)
(range/SO),
[9521437]
yr
Male(%) 0 Internal y
validation?
Kato, 1997'
55
(y/n)
Health Generally Dietary 70-item CRC across X X Total Ca
New York status healthy assessment semi- total calcium (food)
University women method quantitati intake
Women's Mean age nd ve FFQ quartiles
Health Study (range/SO), (slightly
us yr modified
(various) from
[9343837) Block' s)
Male(%) 0 Internal y
validation?
(y/n)
Wu, 1987'
54
Health Generally Dietary 56-item CRC per X Total Ca
status healthy assessment FFQ gender across (dairy)
us men and method total calcium
(21N) women intake tertiles
[3620314) Mean age nd
(range/SO),
yr
Male(%) 33 Internal n
validation?
In
Jarvinen, Health Generally Dietary Diet CRC across X X X X Total Ca
2001
157
status healthy assessment history total calcium (food)
nd men and method intake
Finland women quartiles
(64N) Mean age 39.1
[11641750) (range/SO), Subgroup
yr analyses per
Male(%) nd Internal y site (colon,
validation? rectal)
(y/n)
Stem merman Health Generally Dietary 24-hour Colon cancer X Japanese;
n, 1990
151
status healthy assessment diet across total Total Ca
Japan Hawaii men method recall calcium intake (food)
Cancer Study Mean age nd interview tertiles
us (range/SO),
(21 N) yr
[2311461)
Male(%) 100 Internal y
validation?
In
continued
182
Confounders/Effect
Author, Year
Modifiers Adjusted
Trial/Cohor t
CJ
Name
Population Dietary Calcium intake Comparisons
:.c
Comments
Countr y
c.. U)
U)
<II U)
CD
... .... c..
~ (Latitude)
c: Cl 0
iii c:
~
0 .... CJ 0
U)
[ Pubmed ID]
E
.c:
'6
U)
'5 i:
<II
.2!
CD CD
CD
z c <( ~ en
::;
van der Pols,
Health Generally Dietary 7-day CRC between X x X x Total Ca
2007
156
status healthy assessment house hoi lowest and (food)
The Boyd Orr children method d highest total
Cohort
Mean age 7.6 inventory calcium intake
UK
(range/SO),
method groups
(54 55N)
yr
[8333412]
Male(%) 49.5 Internal n
validation?
In
Garland, Health Generally Dietary 28-day CRC across X X X X Total Ca
1985
158
status healthy assessment diet total calci um (food)
Western men method histories intake
Electric Mean age 48.7 (4.4) quartiles
Health Study (range/SO),
us yr
(41N)
Male (%) 100 Internal n
[2857364] validation?
In
Nested case-control
Kampman, Health Generally Dietary 150-item CRC across X X X X Total Ca
1994
159
status healthy assessment semi- total calcium (food)
The men and method quantitati intake
Netherlands women ve FFQ quintiles
Cohort Study Mean age nd
Netherlands (range/SO),
(52N) yr
[8205538] Male(%) nd Internal y
validation?
('t/n)
183
Table 62. Calcium and colorectal cancer: Results of cohort studies
Author Year
Study Name
Location
(Lati t ude)
PMID
Park, 2009
NIH-AARP Diet & Health
us
{various)
(19237724]
Wu 2002
140
HPFS: Health Professionals
Follow-up Study
NHS: Nurses' Health Study
us
(various)
(11904316]
continued
Life Stage
Male adult
(50-71 y)
Female adult
(50-71 y)
Male adult
(40-75 y)
Female adult
(3055 y)
Outcome (n/N, Total Ca
Incidence) Intake,
mg/ day
CRC (nd) 526
_____
.........................4.98
---
______ ____ 857
______ .Q_f'!Q.JiJ.gL ____ 1073
-----
CRC (nd) 1530
CRC (nd) 494
--------------------
............................................................
______ <::_BQJJ!gL ____ 717
............................................................
______ <::fl _QJiJ.qL ____ 969
............................................................
CRC (nd) 1296
--------------------
............................................................
CRC (nd) 1881
CRC (nd) !> 500
--------------------- ---
...................._ C ...()_1_:?00
______ Q.f3_<::_lf!.gL ____ _ __ f3.()1:?90
______ <::B.<:: Jf!9L ____ ?.91: ?.99
______ _ _ ?.91 : ! 9()_()
______ QB.Q_{f!QL____ 1Q()1 :.t?.O
CRC (nd) >1250
CRC (nd) s 500
------------ -----------
______ <::B.<::J f!Ql_____ ?.91 :.99.
______ Q:l.Q_(n.qL ____ _ __ 13.()1_:?.99
______ QB9JiJ.. qL ____ ?91:.?.90
______ Qf3_Q_lf!.t:!L____ ?.Q1 : ! Q.9()
______ 9_FlQ f n_9L ____
CRC (nd) >1250
184
No. of
Cases
nd
nd
nd
nd
nd
nd
nd
nd
nd
nd
47
48
58
51
81
84
60
70
79
83
90
130
106
68
No. in Follow up Adjusted 95%CI P for Study
Category Duration RR Trend Quality
(Time to
Ox)
nd 84mo 1.0 Reference 0.001 B
nd 84mo 0.89
O":aa:a:9a
...................................................
nd 84mo 0.83 0.75, 0.93*
nd 84mo 0.87 0.78, 0.97*
nd 84mo 0.79 0.70, 0.89*
nd 84mo 1.0 Reference 0.001
.................................................. ---------- ...
nd 84mo 0.87 0.75, 1.01
- ....... ------------
nd 84mo 0.83 0.71 , 0.97*
........................................ ......................................... ---------- ...
nd 84mo 0.71 0.60, 0.84*
.................................................. ---------- ...
nd 84mo 0.72 0.61 , 0.86*
nd nd 1.0 Reference 0. 17 B
..................................................
nd nd 0.69
..... .....! .. .......
nd nd 0.69 0.47, 1.01
nd nd 0.60 0.40, 0.90*
nd nd 0.67 0.47, 0.97*
nd nd 0.62 0.42, 0.92*
nd nd 0.64 0.43, 0.95'
nd nd 1.0 Reference 0.35
..................................................
nd nd 1.19 0.86, 1.64
nd nd 1.07 0.77, 1.47
nd nd 1.18 .
nd nd 1.04 0.77, 1.40
...................................................
nd nd 1.05 0.77, 1.44
nd nd 0.94 0.66, 1.33
Author Year
Study Name
Location
(Latitude)
PMID
Kesse 2005
Etude Epidemiologique aupres
de femmes de !'Education
Nationale
France
(46N)
(15880532)
Lin 2005
142
The Women's Health Study
us
(various)
[15800268)
Pietinen
1999
143
ATBC
Finland
(-64N)
[10530608)
continued
Life Stage
Female adult
(4065 y)
Female adult
(?: 45 y)
Male adult
(5069 y)
Outcome (n/N,
Incidence)
Total Ca
Intake,
mg/day
No. of
Cases
No. in
Category
Follow up Adjusted 95% Cl P for
Duration RR Trend
(Time to
Ox)
CRC (nd) <766.22 163 nd 82.8 mo 1.0 Reference 0.08
CRC (nd) 766.22 154 nd 82.8 mo
----::-::-:----...................................................
0.94 0.63, 1.41
-------------------- ................. ---,----...................................................
CRC (nd) 962.63- 150 nd 82.8 mo 0.78 0.51 , 1. 19
1201.81
- CRC(nd) ---; - 12o1"" .s:..,. 1 ___ 1.,., 3,... 1 ____ n_d,-----,8..,. 2'"" .s,_m_o ___ .,.. o.-= 7.,.. 2- o:47; 1:16
CRC (41/7691 ; <614 41 7691 120 mo 1.0 Reference 0.21
0.01 )
---,---
0.74 0.46, 1.18
1.19 0.78, 1.81
-........::3:,:1_ _ _ --==' nd=-=--__ ......:.: 12:=::- 0 mo
52 7690 120 mo
0.92 0.58, 1.44
1.20 0.79,1.85
_ _ _ = nd=-=--__ ......:.: 120 mo
58 7690 120 mo
CRC (nd) Median 01, 60 nd 96mo 1.0 Referenc.e 0.04
856
CRC (nd) Median 02, 41 nd 96mo
---=-=--
0.7 0.5, 1.0
1241
-------------------- ---- -
CRC (nd) Median 03, 45 nd 96 mo
0.7 0.5,1 .1
1484
-----c "Rc -(n-ci)----MeCiian :o -:=...,.. 4 -, --..,.. 39,....----n...., d ____ 9.,... 6:-m- o __ _
i:i':6:a:9;
0.6
1789
185
Study
Quality
B
B
B
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95% CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/ day (Time to
(Latitude) Ox)
PMID
Park 2007
144
Male adult CRC (nd) < 288 /1000 342 nd 87.6 mo 1.0 Reference 0.006 c
The Multiethnic Cohort Study (45-75 y) kcal
us
{various)
(17215380)
--eFie {ndJ
................. 28'8-369
a-:-i3s;r22
271 nd 87.6 mo 1.02
/1000 kcal
-------------------- --------
...................................................
CRC (nd) 369-457 258 nd 87.6 mo 1.08 0.89, 1.31
/1000 kcal
--------------------------------
...................................................
CRC (nd) 457-61 1 177 nd 87.6 mo 0.85 0.68, 1.07
/1000 kcal
90 nd
87. 6;;:;;;--
0.70
o-:s2; a-:!33'
kcal
Female adult CRC (nd) < 288 /1000 172 nd 87.6 mo 1.0 Reference 0.003
(45-75 y)
---------------------
kcal
...................................................
CRC (nd) 288-369 175 nd 87.6 mo 0.77 0.60, 0.97'
/1000 kcal
---------------------- ----
...................................................
CRC (nd) 369457 194 nd 87.6 mo 0.76 0.60, 0.97'
/1000 kcal
-------------------- ----
...................................................
CRC (nd) 457-611 197 nd 87.6 mo 0.74 0.57, 0.94*
/1000 kcal
...................................................
.............. CRC (nd)
000 234 nd 87.6 mo 0.64 0.50, 0.83.
kcal
McCullough Adult CRC (nd) <561 156 nd nd 1.0 Reference 0.02 c
2003
145
(50-74 y)
CPS II
us
(various)
(12708719)
-------------------- ---
...................................................
______ QB.9.Jr:!9L ____ 165 nd nd 1.05 0.84, 1.31
______ 9_139 .. (n.Q.L_____ .... 137 nd nd 0.88 0.70, 1.12
............. .9_13..(DQ) __ , ............ . .?55
108 nd nd 0.72
.....Q.:.?..t:>., .. .....
CRC (nd) >1255 11 7 nd nd 0.87 0.67, 1.12
Male adult CRC {nd) <561 89 nd nd 1.0 Reference 0.04
(50-74 y)
--------------------------
...................................................
______ QB9 ..Jr:! ..ci.L____ ..! 106 nd nd 1.01 0.76, 1.34
----- CRC (n_q)_ ____ . ............... .J.?..?.-925
98 nd nd 0.93
.......9.:.?.9 ..... .1..:.?..?........
______ g_f39. 1r:!<:l.L ____ 926-1255 70
---
nd nd 0.71 0.52, 0.98'
CRC (nd) >1255 58 nd nd 0.82 0.58, 1.16
continued
186
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95%CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/ day (Time to
(Latitude) Ox)
PMID
__ gg_12f1 __ <561 64 nd nd 1.0 Reference 0.02
-----
...................................................
___ 561 -731 82
---------
nd nd 1.08 0.77, 1.50*
__g()j()_ll __ 732-925 67
-- --
nd nd 0.89 0.63, 1.27*
Colon cancer (nd) 926-1255 51 nd nd 0.72 0.49, 1.05'
Colon cancer (nd) >1255 38 nd nd 0.74 0.49, 1.12.
Rectal cancer <561 23 nd nd 1.0 Reference 0.71
________ JJ1d.j_ _______
--------
...................................................
Rectal cancer 561 -731 22 nd nd 0.78 0.43, 1.41
________ fr1_c!L ______
---------
...................................................
Rectal cancer 732-925 29 nd nd 1.02 0.58, 1.79
_________ (f1_(j)__ _______
---------
...................................................
Rectal cancer 926-1255 16 nd nd 0.60 0.31, 1.16
_________ (!!c_!L _______
-----------
...................................................
Rectal cancer >1255 19 nd nd 1.01 0.53, 1.93
(nd
Female adult CRC (nd) <561 67 nd nd 1.0 Reference 0.31
(50-74 y)
--------------------
...................................................
______ ____ 561 -731 59 nd
-
nd 1.16 0.82, 1.66
______ <;;B.9J.n..c!L ____ 732-925 39 nd
-------
nd 0.80 0.54, 1.21
___ g_f!C (nd) 926-1255 38 nd nd 0.78 0.51, 1.18
0":6s;r:s9
CRC (nd) >1255 59 nd nd 0.94
Shin 2006
149
Female adult CRC (nd) s 291.9 nd nd Median, 1.0 Reference 0.48 c
Shanghai Women's Health Study {40-70) 68.9 mo
China
(31 N)
[17019716)
...................................................
CRC (nd)
-
nd nd Median, 1.0 0.7, 1.4
68.9 mo
-------------------- -----------
...................................................
CRC (nd) $488.2 nd nd Median, 1.0 0.7, 1.4
68.9 mo
-------------------- ---------
...................................................
CRC (nd) $610.8 nd nd Median, 0.9 0.6, 1.3
68.9 mo
---------------------- ------
...................................................
CRC (nd) > 610.8 nd nd Median, 0.9 0.6, 1.3
68.9 mo
continued
187
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95%CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/ day (Time to
(Latitude) Ox)
PMID
Terry 2002 Female adult CRC (nd) Mean (SO) 156 nd 135.6 mo 1.0 Reference 0.02 c
Swedish Mammography (S 76 y) 01, 486 (79)
Screening Cohort
Sweden
(59N)
[124671 33)
-------------------- ----
...................................................
CRC (nd) Mean (SD) 149 nd 135.6 mo 0.97 0.77, 1.21
--------------------
9?. . !??.lJ3..4.) ...................................................
CRC (nd) Mean (SD) 145 nd 135.6 mo 0.95 0.75, 1.20
--------------------
...................................................
CRC (nd) Mean (SD) 122 nd 135.6 mo 0.72 0.56, 0.93*
04, 914 136
Colon cancer (nd) Mean (SO) 100 nd 135.6 mo 1.0 Reference 0.06
--------------------
...................................................
Colon cancer (nd) Mean (SD) 97 nd 135.6 mo 0.97 0.74, 1.30
.......s;g ...
34
-c-oion""cancer (nd)
Mean (SD) 92 nd 135.6 mo 0.93
a::;;o;r24 .......
-----------------------
9?., ?.4.?( 3.Z) ...................................................
Colon cancer (nd) Mean (SD) 82 nd 135.6 mo 0.74 0.54, 1.01
04, 914 136
Rectal cancer Mean (SO) 55 nd 135.6 mo 1.0 Reference 0. 12
_________ (Q(jj ________
..................................................
Rectal cancer Mean (SD) 48 nd 135.6 mo 0.89 0.60, 1.32
_______ ..i!:!<:lL ______
...................................................
Rectal cancer Mean (SD) 49 nd 135.6 mo 0.94 0.63, 1.39
_________ Jf19L ______
93.,?4?(3.ZL ...................................................
Rectal cancer Mean (SD) 39 nd 135.6 mo 0.70 0.45, 1.09
(nd} 04, 914 (136}
Female adult CRC (nd) 176-568 nd nd 135.6 mo 1.0 Reference 0.77
(<55 y)
-------------------- --
...................................................
______ _ nd nd 135.6 mo 1.06 0.68, 1.66
__ f _Rf _Jn._q) __ ............ .. nd nd 135.6 mo 1.1 1
,,.... .. , ....
CRC (nd) 816 1300 nd nd 135.6-mo 0.91 0.56, 1.48
Female adult CRC (nd) 176-568 nd nd 135.6 mo 1.0 Reference 0.008
(<::55 y)
-------------------- ---------
...................................................
______ QBQJr!<:lL ____ nd nd 135.6 mo 0.93 0.71 , 1.21
.............. ..................?..?.816
nd nd 135.6 mo 0.89 0.68,1 .17
CRC (nd) 816 1300 nd nd 135.6 mo 0.66
Female adult Colon cancer (nd) 176-568 nd nd 135.6 mo 1.0 Reference 0.92
(<55 y)
-------------------- ---
...................................................
__ 568-688 nd nd 135.6 mo 1.32 0.75 2.30
--------
...................................................
_ g.2.).Q.!)_ancer (!J..<:!L ....._ .._ .... 6 nd nd 135.6 mo 1.02
........9&2 .....!..:.?..2 .......
Colon cancer (nd) 8161300 nd nd 135.6 mo 1.1 1 0.60, 2.05
continued
188
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95%CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/day (Time to
(Latitude) Ox)
PMID
Female adult Colon cancer (nd) 176-568 nd nd 135.6 mo 1.0 Reference 0.02
(<:55 y)
- ---- - - - - - - - - --------
...................................................
.... 568688 nd nd
-
135.6 mo 0.89 0.64, 1.23
___ ................?..?..:.1 6
nd nd 135.6 mo 0.91
.......Q. ....J..:.?.. .......
Colon cancer (nd) 816-1300 nd nd 135.6 mo- 0.64 0.44, 0.92'
Female adult Rectal cancer 176-568 nd nd 135.6 mo 1.0 Reference 0.75
(< 55 y) _______ Jr::td. l_ _______
--------
...................................................
Rectal cancer 568-688 nd nd 135.6 mo 0.33 0.34, 1.59
________ Jr::t ..<!.L ______
---------
...................................................
Rectal cancer 688-816 nd nd 135.6 mo 1.30 0.66, 2.56
_______ j_r.1_cj)__ _______
---------
...................................................
Rectal cancer 816-1300 nd nd 135.6 mo 0.70 0.31, 1.62
nd
Female adult Rectal cancer 176-568 nd nd 135.6 mo 1.0 Reference 0.15
(<:55 y)
--.{!)9.) __ ..............................
a:6f;r52 .......
Rectal cancer 568-688 nd nd 135.6 mo 0.96
________ illd.L _______
--------
...................................................
Rectal cancer 688-816 nd nd 135.6 mo 0.79 0.48, 1.29
_______ j_n_gL_ _______ m__ ..
. ..................................................
Rectal cancer 816-1300 nd nd 135.6 mo 0.70 0.42, 1.19
Gaard 1996
153
Male adult
(nd)
Colon cancer (nd) <758 22 nd 134.4 mo 1.0 Referenc.e 0.15 c
(20-53 y)
Norway
(60-69N)
[9061275]
.. 24 nd 134.4 mo 1.02
a:5:;;ra3 .......
__
24 nd 134.4 mo 1.04 0.58, 1.86
...................................................
Colon cancer (nd) >1067 13 nd 134.4 mo 0.57 0.29, 1. 13
Female adult Colon cancer (nd) <527 15 nd 134.4 mo 1.0 Reference 0.94
(20-53 y)
..
.................528-628
20 nd 134.4 mo 1.25
a:53;2:45 .......
...................................................
__ gg_I2!:J .... 629-743 7 nd 134.4 mo 0.46 0.19, 1.12
-
...................................................
Colon cancer (nd) >744 18 nd 134.4 mo 1.20 0.60, 2.39
continued
189
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95%CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/ day (Time to
(Latitude) Ox)
PMID
Flood 2005 Female adult CRC (nd) <472 102 nd 17 mo 1.0 Reference 0.02 c
The Breast Cancer Detection (nd)
Demonstration Project (BCDDP)
us
(various)
[1 5668485)
-------------------- ----
...................................................
______ Qfl_Q_in_<& _____ 472-635 110 nd 17 mo 1.03 0.79, 1.35
---------
...................................................
______ ____ 636-844 86
---------
nd 17 mo 0.80 0.60, 1.06
______ QB.QJ!l_<!L ____ 845-1270 106
---------
nd 17 mo 0.96 0.73, 1.26
CRC (nd) >1270 80 nd 17 mo 0.74 0.55, 0.99*
___
<472 nd nd 17mo 1.0 Ref erence 0.10
---------
...................................................
__ QQIQ!l __ 472-635 nd
-----
nd 17 mo 0.84 0.59, 1.18
__ __
636-844 nd
----
nd 17 mo 0.66 0.46, 0.96*
__ 845-1270 nd
-----
nd 17 mo 0.78 0.55, 1.11
Colon cancer (nd) >1270 nd nd 17 mo 0.69 0.48, 0.99*
Rectal cancer <472 nd nd 17 mo 1.0 Reference 0.30
(nd)
Rectal cancer 472-635 nd nd 17 mo 1. 19 0.57, 2.48
(nd)
Rectal cancer 636-844 nd nd 17 mo 1.10 0.52, 2.32
(nd)
Rectal cancer 845-1270 nd nd 17 mo 1.23 0.60, 2.53
(nd)
Rectal cancer >1270 nd nd 17 mo 0.93 0.43, 2.01
Larsson 2006
148
(nd)
Male adult CRC <956 127 11,348 80.4 mo 1.0 Reference O.Q1 c
The Cohort of Swedish Men (45-79 y) (1 11/ 11,341 ;
Sweden 0.011)
(59N)
[16522915)
-------------------- --------
...................................................
CRC ( 107/ 11295; 956-1179 111 11 ,341 80.4 mo 0.80 0.61, 1.04
---------0.01 0)_ ___ ..............................
CRC 1180-1444 107 11 ,295 80.4 mo 0.73
a:ss;a:9iv ...
(1 04/ 11 ,322;
--- ___ Q.,QQ!:lL ____
--
...................................................
CRC (67/ 11 ,322; >1445 104 11,322 80.4 mo 0.68 0.51 ' 0.91 *
0.009
Colon cancer <956 67 11 ,322 80.4 mo 0.72 0.50, 1.04 0.15
(77/ 11 ,348;
_______ _Q"QQP.L_________ -- --
...................................................
Colon cancer 956-1179 77 11,348 80.4 mo 1.0 Reference
(70/ 11 ,295;
0.007)
continued
190
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95% CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/ day (Time to
(Latitude) Ox)
PMID
Colon cancer 1180-1444 70 11 ,295 80.4 mo 0.80 0.57, 1.12
(67/ 11 ,322;
_______ 9,Q9.2L ______
...................................................
Colon cancer >1 445 67 11,322 80.4 mo 0.72 0.50, 1.04
(50/ 11 ,348;
0.006
Rectal cancer <956 50 11 ,348 80.4 mo 1.0 Reference 0.02
(49/ 11 ,341;
________ __________
----
...................................................
Rectal cancer 956-1179 49 11,341 80.4 mo 0.91 0.61' 1.37
(37/ 11 ,295;
_______ ______
---------
...................................................
Rectal cancer 1180-1444 37 11 ,295 80.4 mo 0.63 0.40, 0.98*
(37/ 11 ,322;
_______ _____
----
...................................................
Rectal cancer >1 445 37 11 ,322 80.4 mo 0.61 0.38, 0.98*
(37/ 11 ,322;
Bostick 1993
150
Female adult
0.003)
Colon cancer (nd) <629 54 nd nd 1.0 Reference 0.22
Iowa Women' s Health Study (55-69 y)
us
(40N)
[833341 2)
----------------------
...................................................
__ gg_12f1 __ 629-896 44
--
nd nd 0.89 0.59, 1.33
___ 897-1188 42 nd nd 0.88 0.58, 1.33
---------
...................................................
__g_()j()_ll __ 1189-1547 44
-----
nd nd 0.97 0.63, 1.50
Colon cancer (nd) >1548 28 nd nd 0.68 0.41 , 1.11
Zheng 1998
152
Female adult, Rectal cancer <800.8 56 nd 108mo 1.0 Reference 0.02 c
Iowa Women's Health Study (55-69 y) (nd)
us
(40N)
[9521437)
...................................................
, ___ FieC:Ialcanc-e-r---- ......so'O:a-1278. 7
52 nd
108 mo--
0.90 0.61 ' 1.33
_________ (ll.QL _______
-----------
...................................................
Rectal cancer 36 nd 108 mo 0.59 0.37, 0.94*
nd
continued
191
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95%CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/day (Time to
(Latitude) Ox)
PMID
Kato 1997 Female adult CRC (nd) Lowest, Q1 nd nd 85.2 mo 1.0 Reference 0.18 c
New York University Women's (3465 y) (nd)
Health Study
us
(various)
[9343837]
-------------------- --
...................................................
______ Qfl_Q_i n_<& _____ _Q?._(n.sJJ nd nd 85.2 mo 1.15 0.67, 1.95
...................................................
______ ____
nd nd 85.2 mo 0.90 0.52, 1.57
CRC (nd) Highest 04 nd nd 85.2 mo 0.71 0.39, 1.28
Wu 1987'
54
Male adult CRC (nd)
(nd)
Low tertile nd nd nd 1.0 Reference ns c
(nd) (nd)
us
(21 N)
[3620314]
-------------------- --
...................................................
CRC (nd) Medium nd nd nd 1.19 0.6, 2.2
--------------------
...................................................
CRC (nd) High tertile nd nd nd 0.86 0.4, 1.7
nd
Female adult CRC (nd) Low terti le nd nd nd 1.0 Reference ns
(nd)
---.(f.llfl.
CRC (nd) Medium nd nd nd 0.9
a:s:-l':s
--------------------
...................................................
CRC (nd) High terti le nd nd nd 0.89 0.5, 1.6
Jarvinen 2001
151
Adolescent CRC (nd)
(nd)
Male: 20 nd 235.2 mo 1.0 Reference 0.97 c
and adult <1178.2
Finland (> 15 y) Female:
(64N) <862.5
[1 1641750]
-------------------- ---------
...................................................
CRC (nd) Male: 1178.2- 19 nd 235.2 mo 1.17 0.60, 2.27
1557.1
Female:
862.51 110.7
---------------------- ------
...................................................
CRC (nd) Male: 1557.2- 18 nd 235.2 mo 1.37 0.67, 2.81
1953.2
Female:
11 10.8-
1416.6
--c-R<S (nd)---"MaTe: >
15 nd 235.2 mo 1.43
6:s-r:i39-
1953.3
Female:>
1416.7
continued
192
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95%CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/day (Time to
(Latitude) Ox)
PMID
Colon cancer (nd) Male: 10 nd 235.2 mo 1.0 Reference 0.17
<1178.2
Female:
<862.5
--------------------- ----
...................................................
Colon cancer (nd) Male: 1178.2- 14 nd 235.2 mo 1.44 0.61, 3.39
1557.1
Female:
862.5 1110.7
-------------------- ---
...................................................
Colon cancer (nd) Male: 1557.2 9 nd 235.2 mo 1.04 0.38, 2.83
1953.2
Female:
1110.8-
1416.6
--------------------
...................................................
Colon cancer (nd) Maie:;
5 nd 235.2 mo 0.63 0.17, 2.35
1953.3
Female:>
1416.7
Rectal cancer Male: 10 nd 235.2 mo 1.0 Reference 0.19
(nd} <1178.2
Female:
<862.5
----------------------- ----- -
...................................................
Rectal cancer Male: 1178.2- 5 nd 235.2 mo 0.77 0.25, 2.37
(nd) 1557.1
Female:
862.5 1110.7
-------------------- --------
..................................................
Rectal cancer Male: 1557.2- 9 nd 235.2 mo 1.88 0.67, 5.30
(nd) 1953.2
Female:
1110.8
1416.6
------ --------------
...................................................
Rectal cancer
Maie:; -
10 nd 235.2 mo 3.01 0.93, 9 73
(nd) 1953.3
Female:>
1416.7
continued
193
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95%CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/day (Time to
(Latitude) Ox)
PMID
Stemmermann Male adult Colon cancer Low (nd) 74 2466 nd 1.3 0.9, 1.8 0.16 c
1990
151
(nd) (74/2466; 0.02)
Japan Hawaii Cancer Study
us
(21 N)
[2311461 ]
-------------------- --
...................................................
Colon cancer Medium (nd) 57 2456 nd 1.0 0.7, 1.4
___
--------
...................................................
Colon cancer High (nd) 58 2461 nd 1.0 Reference
(58/2461 ; 0.03)
van der Pols 2007 Children CRC (nd) Lowest 01 , nd nd nd 1.0 Reference 0. 18 c
The Boyd Orr Cohort (IQR 4-1 1 y) (nd)
UK
(5455N)
[8333412)
-------------------- --------
...................................................
CRC (nd) HighestQ4, nd nd nd 1.91 0.84, 4.32
(nd
Garland 1985 Male adult CRC (1 9/488; 102-241 19 488 nd nd nd nd c
Western Electric Health Study (40-55 y) 0.04} 11000 kcal
us
(41 N)
[2857364)
-------------------- --------
...................................................
CRC (12/ 489; 242-306 12 489 nd nd nd
________ 9-'-Q?L ______ / 1000kcal
...................................................
---
CRC (12/489; 307-383 12 489 nd nd nd
________ Q_,9.?L ______ /1000 kcal
...................................................
--------
CRC (6/ 458; 384-906 6 458 nd nd nd
0.01 ) /1000 kcal
194
Table 63. Calcium and colorectal cancer: Results of nested case-control studies
Author Year Life Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95% CI P for Study
Study Name Stage Incidence) Intake, mg/day Cases Category Duration RR Trend Quality
Location (Time to Ox)
(Latitude)
PMID
Kampman 1994
159
Adult (55 CRC (443/31 11, Median 0 1, 98 623 39.6 mo 1.0 Reference 0.89 B
The Netherlands Cohort 69 y) 0.14) 596
Study
Netherlands
(52N)
[8205538)
-------------*
Median 02, 89 619 39.6 mo 0.83
o:sa; 1:22
768
---------------
................................................,
Median 03, 87 622 39.6 mo 0.96 0.67, 1.39
893
--------------
................................................,
Median 0 4, 81 627 39.6 mo 0.93 0.64, 1.36
1032
--------------
................................................,
Median 05, 88 620 39.6 mo 092 0.64, 1.34
1288
195
Figure 14 Colorectal cancer risk in both sexes stratified by calcium intake
Study Category Ca Intake (mg/d)
Children
van der Pols 2007 Ql (ref) nd
Q2 nd
Both sexes
Kampman 1994 Ql (ref) S96
(n = 31 11) Q2 768
Q3 893
Q4 1032
as 1288
-
CPS 112003 Ql (ref) <561
(n = 127,749) Q2 561-731
Q3 732- 925
Q4 926-1255
as >12SS
-
Jarvinen 2001 Q1 (ref) M: < 1178, f ; <863
(n =99S9) Q2 M: 1178-1557, F: 6 ~ 1 1 1 1
Q3 M: 1557-1953, F: 1111- 1417
Q4 M:> 1953, F: >1417
196
I
0.2
-
....
......,_
......
I
0.5
Decreased risk
I
2
Increased risk
p
for
trend Quality
0. 18 c
0.89 B
--
0.02 c
--
0.97 c
I
5
Figure 15 Colorectal cancer risk in men stratified by calcium intake
Study Category
Men
Park2009 01 (ref)
(n = 293,907) 02
03
Q4
05
HPFS 2002 01 (ref)
(n =47,344) 02
03
Q4
05
Q6
07
ATBC 1999 01 (ref)
(n = 27,11 1) 02
03
Q4
Park2007 01 (ref)
(n =85,903) 02
03
Q4
05
-
CPS 112003 01 (ref)
(n=60,866) 02
03
Q4
Q ~
Larsson 2006 01 (ref)
(n =45,306) 02
03
Q4
-
Wu 1987 01 (ref)
(nd) 02
03
Ca intake (mg/ d)
526
498
857
1073
1530
~ ~
<501
501-600
601- 700
701 - 800
801- 1000
1001 - 1250
>1250
856
1241
1484
1789
<288 (/1 000 kcal)
288- 369 (/1000 kcao
369-457 (/1000 kcal)
457-611 (/1000 kcaO
>61 1 J11 ooo kcal)
<561
561 - 731
732- 925
926- 1255
>1255
<956
956- 1179
1180- 1444
>1445
nd
nd
nd
1
1
3
I I I
0.2 0.5
Decreased ri sk
2
Increased risk
197
I
5
p
for
trend Quality
0.001 B
0.17 B
0.04 B
--
0.006 c
----
0.04 c
0.01 c
--
nd c
Figure 16 Colorectal cancer risk in women stratified by calcium intake
p
for
Study Category Ca intake (m9ld) trend Quality
Women
~
Park 2009 Ql (ref) 494 0.001 8
(n s I 98,903) Q2 717
03 969
Q4 1296
QS 1881
NHS 2002 Ql (ref) <SOl 0.35
_8 ___
(n = 87,998) 02 501-600
Q3 601 - 700
Q4 701-800
Q5 801- 1000
Q6 1001-1250
07 >1250
Kesse 2005 Ql (ref) <766
4
0.08
--B
(n = 67,484) Q2 766-963
Q3 963- 1202
Q4 > 1202
W H 5 ~ Qi(;ef) <6 14
~
0.21 B
(n = 36,976) 02 614-785
Q3 785-10 16
Q4 1016-1357
Q5 > 1357
Park 2007 Ql (ref) <288 (/ 1000kcal)
if
0.003--
c
(n = 105,108) 02 288-369 (/ 1000 kcal)
Q3 369-457 (/1000 kcal}
Q4 457-611 (/1000 kcal)
as >611 (/ 1000 kcal)
Shin 2006 Q1 (ref) - <"292
:l
0.48 c
{0 = 73,314) 02 292- 390
Q3 390- 488
Q4 488- 6 11
05 >611
CPSII2003 Q1 (ref) <561
~
0.31 c
(n = 66,883} Q2 561- 731
03 732-925
Q4 926-1255
05 >1255
Terry2007 Ql (ref) 486
_:f
0.02 c
(n = 61,463) 02 631
03 747
Q4 914
Flood 2005 01 (ref) <472
~
0.02 c
(n = 45,354) 02 472- 635
03 636-844
Q4 845- 1270
05 ___
>1270
Kato 1997 01 (ref) nd
~
0.18 c
(n = 14727) Q2 nd
Q3 nd
Q4 nd
Wu 1987 Q1 (ref) nd
1
nd c
(nd) 02 nd
03 nd
0.2 05 2 5
Decreased risk Increased risk
198
Figure 17 Colon cancer risk stratified by calcium intake
p
for
Study Category Ca intake (mg/d) trend Quality
Both sexes
Jarvinen 2001 Q1 (ref) M: <1178, F: <863 0.17 c
(n = 9959) 02 M: 1178-1557, F: 863- 1111
Q3 M:1557- 1953,F:1111- 1417
Q4 M: >1953, F: >1417
Men
J
-
CPS 112003 Q1 (ref) <561 0.02 c
(n = 60,866) 02 561-731
Q3 732- 925
04 926-1255
05 >1255
-
Larsson 2006 01 (ref) <956
:;4
0.15 c
(n = 45,306) Q2 956- 1179
Q3 11 80-1444
Q4 >1445
- Gaard 199r;- Qll'fet)--;(758-
~
o.f5 c
(n = 25,638) Q2 759- 912
Q3 913-1066
Q4 >1067
Slemmermani11990 Q 1
---no-
f
0.16 c
(n = 7,383) Q2 nd
Q3 (ref) nd
- women
-
1
-
Terry 2007 Q1 (ref) 486 0.06 c
(n = 61,463) 02 631
Q3 747
~
04 914
Flood 2005 Q1 (ref) <472
~
0.10 c
(n = 45,354) Q2 472-635
Q3 636- 844
04 845-1 270
- Bost1c1< 1993
Q5 >1270
~ l (ref)
<629
~
0.22 c
(n = 35,216) 02 629-896
Q3 897-1188
Q4 1189-1547
Q5 >1548
llaarcfl996 Ul tret) <!>2/ 0.94 l
(n = 24,897) Q2 528- 628
Q3 629-743
Q4 >744
I I I I I
0.1 0.2 0.5 2 5
Decreased risk Increased risk
199
Figure 18. Rectal cancer risk stratified by calcium intake
p
for
Study Category Ca intake (mg/d) trend Quality
Both sexes
Jarvi nen 2001Q1 (ref) M: <11 78, F: <863 0.19 c
(n = 9959) Q2 M: 1178-1557, F: 863-1 1
Q3 M: 1557-1 953, F:1111-1417
Q4 M: >1953, F: >1417
Men
--
CPS II 2003 Q1 (ref) <561 0.71 c
(n = 60,866) Q2 561-731
Q3 732-925
Q4 926-1255
Q5 >1255
Larsson 2006Q1 (ref) <956 0.01 c
-
(n = 45,306) Q2 956-1179 ......
-
Q3 1180-1444
Q4 >1445
Women
Terry 2007 Q1 (ref) 486 0.12 c
(n = 61,463) Q2 631
.....
-
Q3 747
~
-
__Q_4
214
c ~
Flood 2005 Q1 (ref) <472
~
0.30
(n = 45,354) Q2 472-635
Q3 636-844
Q4 845-1270
Q5 >1270
Zheng 1 9 ~ 1 (Tef) <801 0.02 c
(n = 34702) Q2 801-1279
......
-
Q3 >1279
I I I I I
0.2 0.5 1 2 5 10
Decreased ri sk Increased ri sk
200
Colorectal adenoma.
Synopsis.
This synopsis is based on one systematic review, two comparative trials (one post hoc followup
study of an RCT and one nonrandomized trial), and four cohort studies. The systematic review
that included two RCTs which evaluated high risk population for the prevention of colorectal
adenoma recurrence showed a reduction in the risk of colorectal adenoma with calcium
supplementation (OR 0.74, 95 percent CI 0.58, 0.95; P=0.02). The B quality long-term
followup study of an RCT of calcium supplementation (I 200 mg/d) versus placebo in healthy
adults showed no significant difference in the risk of recurrence of colorectal adenoma. The
nonrandomized comparative trial (methodological quality C) also found a significant reduction
in adenoma recurrence risk among healthy adults who received calcium supplementation.
Among four cohort studies (methodological quality B), two found an inverse association
between total calcium intake and the risk of colorectal adenoma, while the others found no
significant association.
Detailed presentation (Tables 64, 65, 66, 67 & 68; Figure 19).
One systematic review included two RCTs that recruited high risk population for colorectal
adenoma due to previous adenomatous polyps.
139
A total of 1346 participants were analyzed for
the effect of calcium supplementation (1200 to 2000 mg elemental calcium daily). The odds ratio
of colorectal adenoma recurrence was 0.74 (95 percent CI 0.58, 0.95; P=0.02), comparing
calcium supplementation to the placebo. A B quality post hoc followup analysis
161
of one of the
two RCTs that were included in the meta-analysis examined the long-term effect of calcium
supplementation to prevent colorectal adenoma recurrence. The trial recruited participants with
previous colorectal adenoma, and compared the preventative efficacy of calcium
supplementation (1200 mg/d) to placebo. Adenoma recurrence at 4 years was the original
primary outcome. During the followup period after the trial treatment, about 50 percent of
participants in both groups took some calcium supplements. In 347 participants who underwent
colonoscopy during the first 5 years after the intervention period, the relative risk of adenoma
recw-rence was 0.63 (95 percent CI 0.46, 0.87; P=0.005) comparing calcium supplementation to
placebo, whereas no difference was found in 424 participants who underwent colonoscopy in the
subsequent 5 to 10 years after the trial treatment.
A nonrandomized comparative study
162
presented the percentage of adenoma recurrence in a
group of men and women who underwent polypectomy, and received calcium supplementation
(2000 mg/d) as chemoprevention. The same study also presented the percentage of adenoma
recurrence in a group of men and women who underwent polypectomy but were not
supplemented with calcium. The intervention group included 175 participants while the
nonsupplemented group included nine patients. The two groups were followed for an average of
3. 1 years. The trial was rated C for methodological quality. In this study,
162
the percentage of
participants with adenoma recurrence was lower in the intervention group compared to the
nonsupplemented participants (13 percent versus 55 percent); however, no further statistical
analysis was provided.
Four cohort studies evaluated the association between calcium intake and colorectal
adenoma.
141
'
163
-
165
Three studies were conducted in the US (latitude range between 33N and
38N), and one in France (latitude 46N). Sample sizes ranged from 1304 to 48,115. Two
studies recruited participants with a history of colorectal adenoma, and the other two recruited
201
healthy subjects without a history of adenoma. The incidence rate of colorectal adenomas ranged
between 0.003 and 0.025. The participants' mean age ranged from 52.7 to 61.1 years. Average
followup ranged from 36.8 to 44.4 months. Three ofthe four studies did not report infonnation
on assessor blinding.
141
'
164
165
All studies assessed dietary intake with food frequency
questionnaires and confirmed cases with pathology reports. The quality of all four studies was
rated B.
Findings by age and sex.
One cohort study
165
that analyzed men and women (aged 40-80 y) with a history of colorectal
adenoma found an inverse association between total calcium intake and colorectal adenoma
recurrence after an average of 3.1 years of followup (RR 0.62, highest[> 1279 mg/d] compared
with lowest intake [ <778 mg/d]; P for trend= 0.005). The study did not test statistically whether
the strength of the association differed between men and women. Another study ofboth men and
women with previous adenomatous polyps found no significant association between total
calcium intake and colorectal adenoma recurrence.
One cohort study that analyzed exclusively women (aged 40-65 y) without a history of
colorectal adenoma found an inverse association between total calcium intake and colorectal
adenoma (RR 0.80, highest[> 1226 mg/d] compared with lowest intake [ <786 mg/d); P for trend
= 0.04).
141
Another study of women without previous adenomatous polyps found no significant
association.
163
Findings by life stage.
0-6 mo No data
7 mo - 2 y No data
3- 8 y No data
9 - 18 y No data
19-50 y One cohort study of women age 30 to 55 years found no association
between total calcium intakes and colorectal adenoma. Three additional studies included
some men or women in this life stage. Two of these studies reported a significant inverse
association between total calcium intake and colorectal adenoma. However, their results
are inconclusive for adults in this life stage.
51-70 y One meta-analysis of2 RCTs in adults with previous adenomatous polyps
(mean age 59 to 61 years) found a significant decrease in colorectal adenoma recurrence
in supplemental calcium (1200 to 2000 mg elemental calcium daily) compared to no
supplements (odds ratio, 0.74 [95 percent CI 0.58, 0.95]; P=0.02). A long-term followup
study of one of the two trials found no difference in recurrence after 5 to l 0 years after
the intervention. One nonrandomized comparative trial also found a significant reduction
in adenoma recurrence risk among healthy adults with a mean age 55 years who received
calcium supplementation compared to no supplements (13 percent vs. 55 percent; P value
not reported). Two cohort studies evaluated participants with a mean age 53 and 61 years
respectively. One additional study recruited adults in this life stage. Two of the three
studies, one including adults with a history of adenoma and another including women
without adenoma history, found an inverse association between total calcium intake and
colorectal adenoma.
71 + No studies specifically focused on this life stage. Two studies also
included some men and women with a history of adenoma corresponding to this life
202
stage. One found an inverse association between total calcium intake and colorectal
adenoma, while the other did not find such an association.
Postmenopause No data
Pregnant & lactating women No data
203
Table 64. Calcium and colorectal adenoma: Characteristics of interventional studies
Author, Year
Trial/Cohort
Name
Country
(Latitude)
[Pubmed ID]
RCTs
Grau, 2007
Calcium Polyp
Prevention
Studl
us
(3444N)
[17227996)
Non randomized
comparative
study
Duris, 1996
162
nd
Slovakia
(48N)
[8682453)
Population
Health
status
Mean age
(range/SO), y
Male(%)
Health
status
Mean age
(range/SO), y
Male(%)
Generally healthy
men and women
with a recent
colorectal adenoma
60.6
71 .7
Generally healthy
men and women;
history of
adenomatous
polyps after
polypectomy
54.7
62
Vit D & Ca
Background
Diets
Calcium,
mean: 876
mg/d
8
nd
Interventions Compliance
Elemental
calcium, 1200
mg/d
Calcium
carbonicum (2
g/d)
nd
Comments
Duplicated with
Wallace; results
during the
observational post-
intervention phase
(5-1 0 years)
No statistical
comparison
between groups
A A post hoc followup study (Calcium Follow-up Study) of a RCT (Calcium Polyp Prevention Study).
8
Two percent of the participants in the both groups took calcium supplements during the intervention period. Forty-seven percent in
the placebo group and 49 percent in the supplement arm took any calcium supplements during the followup period after the
intervention. The dosage was not reported (based on the self-reported data in the earlier report).
1
6()
204
Table 65. Calcium and colorectal adenoma: Characteristics of cohort studies
Confounders/Effect Modifiers
Author, Year
Adjusted
VI
Trial/Cohort
u E
Name :.c
Q)
Country
Population Dietary Calcium intake Comparisons Q, VI E
VI IV
VI
Q)
E
E
.. Q,
>.
(Latitude) Ol 0
iii c 0
- ~
0 .. u 0
Ui
(.)
[Pubmed ID]
E
.c:
'5
VI
5 E
IV
.2! Q) Q)
Q)
z c ~ :::!: C/) ::;
Cohort
Oh, 2007 Health Generally Dietary 61-item semi- Colorectal X X X X X Total
The Nurses status healthy assessment quantitative adenoma Ca
Health Study women method FFQ (by across total (both)
us Mean age 30-55 Willet) calcium intake
(38N) (range/SO), quintiles
[17379616) y
Male(%) 0 Internal y
validati on?
(y/n)
Kesse, 2005 Health Generally Dietary FFQ Colorectal X X X X Total
Etude status healthy assessment adenomas Ca
Epidemiologique women method across total (both)
aupres de Mean age 52.7 calcium intake
femmes de (range/SO), quartiles
I' Education y
Nationale
Male(%) 0 Internal y
France validation?
(46N) (y/n)
15880532
Hartman, Health Generally Dietary FFO Adenoma X X X X Total
2005
164
status healthy assessment recurrence Ca
The Polyp men and method across total (both)
Prevention Trial women; calcium intake
us history of at quintiles
(38N) least one
[15671222) colorectal
adenoma;
90%
Caucasian
Mean age 61. 1 (9.9)
(range/SO},
y
Male(%) 64 Internal y
validation?
In
Martinez, Health Generally Dietary 113-item Adenoma X X X Total
2002
165
status healthy assessment Arizona Food recurrence Ca
Wheat Bran men and method Frequency across total (food)
Fiber (WBF) trial women; Questionnaire calcium intake
us history of (AFFQ} quartiles
(33N}
colorectal
[1 2020102)
adenoma(s) Subgroup
Mean age nd analyses per
(range/SO), gender
y
Male(%) 57. 1 Internal y
validation?
( ~ I n
205
Table 66. Calcium and colorectal adenoma recurrence: Results of ACTs
Life Outcome
10/20
Mean Interventions, n N Outcome Result 95%CI
p
Stage Followup, mo Daily Dose Event Total Metric Btw
(Comparison)
Grau Adult All
10
92.4 Calcium carbonate 82 208 RR 1.09 0.85, 1.39 0.51
2007
161
adenomas _____ _{!_?QO._I!lg!g_L_ ___
Calcium Polyp Placebo 82 216
Prevention Study
us
(various)
[17227996)
Table 67. Calcium and colorectal adenoma recurrence: Results of nonrandomized comparative study
Author Life Outcome 1/2 Mean Interventions, Daily n N Outcome Result 95% P
Year Stage Followup, mo Dose Event Total Metric Cl Btw
Study Name (Comparison)
[PMID]
Duris 1996
162
Adult (30- Adenoma nd 37.2 Calcium carbonicum, 12 175 RR nd nd nd
Slovakia 75 y) recurrence 2g/d
(48N) No chemoprevention 5 9
[8682453)
206
Study
Quality
B
Study
Quality
c
Table 68. Calcium and colorectal adenoma: Results of cohort studies
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95% CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/day (Time to
(Latitude) Ox)
[PMID]
Oh 2007
163
Female Adenoma (nd) Median 01, nd nd nd 1.0 Reference 0.06 8
The Nurses Health Study adult (3055 584
us y)
(38N)
(17379616]
Adenoma (nd) Median 02,
----r;,r---
nd nd 1.05 0.93, 1.20
779
-------"--
Adenoma (nd) Median 03, nd nd nd 0.96 0.84, 1.11
949
....-------
Adenoma (nd) Median 04, nd nd nd 0.96 0.82, 1.12
1139
Adenoma (nd) Median 05,
---r;;:r--
nd nd 0.88 0.74, 1.04
1451
Kesse 2005 Female Adenoma (nd) <785.62 154 nd 44.4 mo 1.0 Reference 0.04 B
Etude Epidemiologique aupres adult (40-65
de femmes de !'Education y)
Nationale
France
(46N)
[1 5880532]
------
Adenoma (nd) 785.62- 150 nd 44.4 mo 0.97 0.76, 1.22
1226.16
>MO_O_O_O_ON .... O_O_O_O
Adenoma (nd) 981.67- 131 nd 44.4 mo 0.83 0.65, 1.07
1226.16
----------
Adenoma (nd) >1226.16 156 nd 44.4 mo 0.80 0.62, 1.03
Hartman 2005
164
Adult (2: 35 Adenoma < 666 156 nd nd 1.0 Reference 0.20 8
The Polyp Prevention Trial y) recurrence ( nd)
us
(38N)
(1 5671222]
Adenoma 666814 163 nd nd 1.12 0.83, 1.51
recurrence (nd
Adenoma 815-969 154 nd nd 1.02 0.76, 1.38
__ recurrence (nd)
Adenoma 970-1226 150 nd nd 1.00 0.74, 1.36
recurrence
Adenoma >1226 131 nd nd 0.86 0.62, 1.18
recurrence (nd)
continued
207
Author Year Life Stage Outcome (n/N, Total Ca No. of No. in Follow up Adjusted 95% CI P for Study
Study Name Incidence) Intake, Cases Category Duration RR Trend Quality
Location mg/day (Time to
(Latitude) Ox)
[PMID]
Martinez 2002
165
Adult (4080 Adenoma < 778 178 326 36.8 mo 1.0 Reference 0.005 8
Wheat Bran Fiber (WBF) trial y) recurrence
us (178/326; 0.55)
(38" N)
[12020102)
Adenoma 778-996
----:;75 ___
326 36.8 mo 0.94 0.66, 1.32
recurrence
(175/326; 0.54
-----------
Adenoma 997-1279 148 326 36.8 mo 0.68 0.48, 0.97*
recurrence
Adenoma >1279 138 326
--36.8mo
0.62 o."9o-
Male adult Adenoma < 778 nd nd 36.8 mo 1.0 Reference nd
(40-80 y) recurrence ( n.)
Adenoma 778-996 nd nd 36.8 mo 1.01 0.68, 1.51
recurrence (nd)
Adenoma 997-1279 nd nd 36.8 mo 0.83 0.54, 1.26
recurrence (nd)
----------
Adenoma >1279 nd nd 36.8 mo 0.67 0.40, 1.10
recurrence (nd)
Female Adenoma < 778 nd nd 36.8 mo 1.0 Reference nd
adult (40-80 recurrence (nd}
y)
------..---
Adenoma 778-996 nd nd 36.8 mo 0.81 0.40, 1.64
Adenoma 997-1279 nd nd 36.8 mo 0.42 0.21, 1.87
recurrence
Adenoma >1279 nd nd 36.8 mo 0.52 0.28, 0.98*
recurrence nd
208
Figure 19. Colorectal adenomatous polyp risk stratified by calcium intake
p
for
Study Category Ca intake (mg/d) trend Quality
-
Women (primary)
NHS 2007 Q1 (ref) 584 0.06 B
(n = 48, 115) Q2 779
....
Q3 949 -4
..
Q4 1139 ---4
-
QS 1451 .....
-
Kesse 2005 Q1 (ref) <786 0.04 B
(n = 5320) Q2 786-982
-
Q3 982-1226
Q4 >1226
Botfi sexes (recurrence)
Hartman 2005 Q1 (ref) <666 0.20 B
(n = 1905) Q2 666-814
Q3 815-969
Q4 970-1226
Q5 >1226
Martinez iooi Q1 (ref}
-- -
B <778 0.005
(n = 1304) Q2 778-996
Q3 997-1 279
Q4 >1279
[Men {recurrence}
Martinez 2002 Ql (ref) <778 nd B
(n = 874) Q2 778- 996
Q3 997- 1279
Q4 >1279
Women (recurrence)
Martinez 2002 Q1 (ref) <778 nd B
(n = 430) Q2 778- 996
Q3 997-1279
Q4 >1279
I I I
0.2 0.5 2
Decreased risk Increased risk
209
Breast cancer incidence.
Synopsis.
No qualified systematic reviews evaluated the association between dietary and supplemental
calcium intake and the risk of breast cancer. No RCTs were identified. Six cohort studies
compared calcium intake and the risk of breast cancer. In four studies, premenopausal women
with calcium intakes in the range of 780-1750 mg/d had a decreased risk of incident breast
cancer.
125
.1
66
"
170
Only one study reported decreased risk of breast cancer in both premenopausal
and postmenopausal women for calcium intake ranged from 1250 to 17 50 mg/d compared with
the lowest quintile of intake of less than 500 mg/d.
168
In two of six studies, there was no
association between calcium intake and breast cancer (both overall and by menopausal
status).
125
'
17
Five studies were rated Band one study rated C.
Detailed presentation (Tables 69 & 70; Figure 20).
Six studies recruited a total of 452,398 (ranged from 3600 to 198,903) pre-and
postmenopausal women and followed them for a period of 7 to 16 years. The participants had an
average age ranged from 47 to 63 years. Four studies conducted in the US and one study
conducted in Sweden used validated food frequency questionnaire to quantify calcium intake
levels. One study conducted in France used computerized questionnaire to quantify calcium
intake levels. The incidence of breast cancer in these studies ranged from 2.5 to 4.8 percent. In
four of the six cohort studies, premenopausal women with calcium intakes in the range of 780 to
1750 mg/d had a decreased risk of incident breast cancer compared to those with lowest quintile
intake levels in each study. There was no association between calcium intake and breast cancer
in the two of six studies.
125
'
170
Findings by age and sex.
In subgroup analysis of four cohort studies, premenopausal women had a consistently
decreased risk of breast cancer. No association was found for postmenopausal women.
Findings by life stage.
0 - 6 mo Not applicable
7 mo- 2 y Not applicable
3 - 8 y Not applicable
9 - 18 y Not applicable
19-50 y A cohort study ofNurses' Health Study including women with an average
age of 47 years had a decrease risk (RR 0.75, 95 percent CI 0.55, 0.99) in breast cancer
among those with calcium intake levels of 1000-1250 mg/d compared to those with
intake levels lesser than 500 mg/d.
51 - 70 y Three of the five cohort studies of women with an average age between
51- 63 years, found a decreased risk ofbreast cancer among those with calcium intakes in
the range of 780- 1750 mg/d compared to those with lowest quinti1e intake levels in each
study.
~ 7 y Not reviewed
Postmenopause Cohort studies did not find an association between breast cancer
risk and calcium intake levels among postmenopausal women.
Pregnant & lactating women Not reviewed
210
Table 69. Calcium and breast cancer: Characteri stics of cohort studies
Confounders/Effect Modifiers
Adjusted
Author Year
"'
Study Name f
E
s::; Q)
Location Population Dietary Calcium intake Comparisons
Q.
;::)
E
"'
CQ
"'
(Latitude) E c,
Q.
"iij
0
Q)
E
0
Q.
~
0
[PMID]
Q)
0 .. (J )(
0 ;::
E
s::;
'6
Q)
"'
5 E
Q)
Q) Q)
>
- z 0 <( ::: ::J ::i
Cohort
Park 2009 Health No Dietary FFQ (NCI Quintile 1 vs. X X X X X Total
NIH-AARP status cancer assessment DHQ) Quintile 2, 3, calcium
us method USDA 4, 5 intake from
38
2
N Nutrient diet and
[19237724) Database supplement
Mean age 50-71
(range/SO),
y
Internal y
validation?
Shin 2002
169
~ ~ n ~
Health No Dietary 61 item FFQ 500 mg vs. X X X X X X Total
NHS status cancer assessment USDA 500-600, 600- calcium
us
Mean age 47 method Nutrient 700, 700-800, intake from
38N (range/ SO), (ND) Database 800-1000, diet and
[ 12208895) y 1000-1250, supplement
Internal y >1250
validation?
I n
McCullough Health No Dietary Modified FFQ 500 mg vs. X X X X X X Total
2005
168
stat us cancer assessment of Block et al. 500-750, 750- calcium
CPS II Mean age 63 method 1000, 1000- intake from
Nutrition (range/SO), (NO) 1250, 1250- diet and
Cohort y 1500, 1500- supplement
us
Internal y 1750, >1750
38N validation?
[ 16365007)
In
Larsson Health No Dietary FFQ <727 vs. X X X X X Total
2009
170
status cancer assessment Swedish 727-862, 863 calcium
Swedish method National Food 980, 980 intake from
Mammography Administ ration 1125, >1125 diet and
Cohort Database supplement
Sweden Mean age 53.7
62N (range/ SO), (9.7)
[1 9056569) y
Internal y
validation?
~ n }
Lin J 2007'
61
Health No Dietary Willet method Quintile 1 vs. X X X X X Total
WHS status cancer assessment USDA Quintile 2, 3, calcium
us or method Nut rient 4, 5 intake from
38
2
N CVD Database diet and
[1 7533208) Mean age 55 supplement
(range/ SO), (55-
y 56)
Internal y
validation?
In
continued
211
Author Year
Study Name
Location
(Latitude)
[PMID]
Resse-Guyot
2007
166
SU.VI.MAX
France
46N
[1 7536191)
Population
Health No
status cancer
Mean age 51
(range/SO), (6.3)
y
Dietary Calcium intake Comparisons
Dietary Computenzed d wnt1ie 1 vs.
assessment questionnaires Quintile 2, 3,
method 4
Internal ND
validation?
(y/n}
212
Confounders/Effect Modifiers
Adjusted
"'
l!!
E
.s;; (I)
c.
E
"'
Cll
"'
E
.. c.
iii
0
(I)
E
01 0 c. >. 0
(I)
0 .. 0 )(
u; (.) ;:
E
.s;;
:0
(I)
:; (I) E
(I)
>
.!
z c
<
:::E ::I ::i
X X X
'x
X D1etary
calcium
intake
Tabl e 70. Calcium and breast cancer: Results of cohort st udies
Author Year
Follow up
Total Ca
Study Name Life Stage
Out come (n/N; Duration
Intake,
No. of No. in Adjust ed
95% CI
P f or Study
[ PMID]
Incidence) (Time to
mg/day
Cases Category RR Trend Quality
Ox)
Park 2009 Pre and Post-
Breast cancer
NIH-AARP menopausal
(5856/198,903; 2.9%)
7y 0 1 494 5856 HR 1 Reference NS B
[19237724] women
02 717 5856 0.96 0.88-1.04
M
0 3 969 5856 0.95 0.87-1.03
..................................................
04 1296 5856 0.94 0.86-1.02
M
05 1881 5856 0.98 0.90-1.07
Shin 2002
Pre-menopausal Breast cancer
NHS 16 y $500 142 NO Ref erence 0.05 B
[1 2208895]
women (3172/88,381 ; 3.6%)
500-600 106 NO 0.88 0.68, 1.1 3
600-700 133 NO 0.97 .........
700-800 119 NO 0.95 0.74, 1.22
M
800-1000 161 NO 0.82 0.64, 1.05
1000-1250 104 NO 0.75 o:s?;o:99;
>1250 62 NO 0.80 0.58, 1.12
Post-menopausal
women
s 500 240 NO Reference NS
500-600 216 NO 0.86 0.72, 1.04
M
600-700 293 NO 0.94
700-800 292 NO 0.92
--.. _ . .9 ..n ..... 1 ..: ..1 ..9 ....
800-1 000 518 NO 0.93
1000-1250 433 NO 0.90
>1250 353 NO 0.93 0.77, 1.1 2
McCullough
Pre- and Post
2005
168
Breast cancer
CPS II Nutrition Cohort
menopausal
(2855/68,567; 4.1 %)
By :>500 457 10,620 Reference 0.07 B
[16365007]
women
500-750 729 17,880 0.91 0.81 , 1.02
750-1000 581 14,023 0.92
1000-1250 407 9120 0.97 0.85, 1.1 1
1250-1500 248 6296 0.84
....... 0':72;-a:9a--
M
1500-1750 144 3983 0.76 0.63, 0.92.
1750 289 6645 0.91 c:?9; i:o6
continued
213
Author Year
Follow up
Total Ca
Study Name Lif e Stage
Outcome (n/N; Duration
Intake,
No. of No. i n Adjusted
95% CI
P for Study
[PMID]
Incidence) (Time to
mg/day
Cases Category RR Trend Quality
Ox)
Larsson 2009
Pre and Post- Invasive Breast
Swedish Mammography
menopausal cancer 9y <727 595 2952 Reference NS B
Cohort
[1 9056569)
women (2952/61 ,433; 4.8%)
727-862 595 2952 0.97
----
................................................
863-980 592 2952 0.95 0.84-1.06
..................................................
980-1125 571 2952 0.93 0.83-1.04
M
>1125 599 2952 0.97 0.87-1.09
Lin J 2007
Pre-menopausal
Invasive breast
WHS cancer (878/31 ,487; 10 y <617 70 10,578 HR1 Reference .04 B
[17533208)
women
2.8%)
617-789 65 10,578 0.84
........o:s9: ...i ..:i"9 .......
789-1026 44 10,578 0.60 Q.41.;9.f3.?.*.
1026-1366 59 10,578 0.79 0.55, 1.14
38 10,578 0.61 o:4o:o:92;
Post-menopausal
<617 104 20,909 HR1 Reference NS
women
617-789 116 20,909 1.21 0.95, 1.54
789-1026 112 20,909 1.09
1026-1366 119 20,909 1.21
9:9.!5, 1:!>!>
<!: 1366 151 20,909 1.17 0.92, 1.50
Kesse-Guyot 2007
Pre- and Post- Breast cancer
SU.VLMAX trial
menopausal (92/3627; 2.5%)
8y <807 32 3627 Reference 0.04 c
(17536191 )
807-960 24 3627 0.73 0.42, 1.25
961-1144 20 3627 0.65 0.37, 1.14
>1144 16 3627 0.50 0.27, 0.91.
Post-menopausal <807 14 nd Reference 0.64
807-960 13 nd 0.71 0.33, 1.54
M
961-1144 10 nd 067 0.30, 1.53
----M---MMMMMMM"""""'"'"'' >
>11 44 11 nd 0.76 0.34, 1.70
continued
214
Author Year
Follow up
Total Ca
Study Name Life Stage
Outcome (n/N; Duration
Intake,
No. of No. in Adjusted
95% CI
P for Study
[PMID]
Incidence) (Time to
mg/day
Cases Category RR Trend Quality
Ox)
Pre-menopausal <807 18 nd Reference 0.01
807-960 11 nd 0.77 0.36, 1.66
961-1144 10 nd 0.63 0. 29, 1.38
>11 44 5 nd 0.26 o:1a:o:71;
HR: hazard ratio
*Statistically significant (P<0.05)
215
Figure 20. Breast cancer risk stratified by calcium intake
p
Ca for
Study Cat egory intake (mg/ d) trend Quality
Premenopause
WHS 2007 Q1 (ref) <617 0.04 8
(n=1 0,578) Q2 617-789
Q3 789-1026
Q4 1026-1366
Q5 >1366
Shin 2002 0 1 (ref) <500 0.05 8
(n = 827) 02 500- 600 -+
03 600- 700
Q4 700- 800
Q5 800- 1000 -+-
Q6 1000-1250 --+-
IIZE
07
---
>1250
esse- Guyot 2007 Q1 (ref) <807 0.01 c
(n = 1480} Q2 807-960
03 961- 1144
Q4 >1144
Postmenopause
WHS 2007 Q1 (ref) <617 0.35 8
(n = 20909} Q2 617-789
r+-
Q3 789-1026
-
Q4 1026-1366 r+-
Q5 >1366 f+-
;srun 2002 Q1 (ret) <500 nd 8
-
(n = 2345) Q2 500- 600
....
03 600- 700 ....
Q4 700- 800
Q5 800- 1000 -41-
Q6 1000- 1250 ...
Q7 >1250
Kesse- GuyoC2007 0.64 L
(n=2147} Q2 807-960
Q3 961-1144
Q4 >1144
I I I I
0.1 0.2 0.5 2
Decreased ri sklncreased ri sk
216
Breast Mammographic Density.
Synopsis.
No systematic reviews evaluated the association between dietary and supplemental calcium
intake and breast mammographic density. No RCTs of calcium intake evaluated breast
mammography density. One prospective cohort study evaluated the association of calcium intake
and breast mammographic density.
171
Both premenopausal and postmenopausal women with
calcium intakes in the range of 523 mg/d to greater than 1021 mg/d were followed for almost 40
years, and there was no association between calcium intake and breast mammographic density.
The methodological quality of this study was rated B.
Detailed presentation (Tables 71 & 72).
One prospective cohort study followed from birth of a British national representative sample
of2547 women and followed them for a period of 53 years.
171
Women had an average age of
51.5 years. Dietary calcium intake was evaluated using 5-day food records. The breast density in
women was assessed through mammography at the ages 36, 43, and 53 years. Since the
measurement at the age of 53 years was cross-sectional, this has been excluded from our
analyses. There was no linear association between dietary calcium intakes in the range of 523
mg/d to greater than 1021 mg/d and breast mammographic density.
Findings by age and sex.
In subgroup analysis by age categories, there was no linear association between calcium
intake and breast mammography density.
Findings by life stage.
0 - 6 mo Not applicable
7 mo - 2 y Not applicable
3 - 8 y Not applicable
9 - 18 y Not applicable
19-50 y There was no linear association between calcium intake in the range of
523 mg/d to greater than 1021 mg/d and breast mammographic density
51 - 70 y No data
~ 7 y No data
Postmenopause No data
Pregnant & lactating women Not reviewed
217
Table 71. Calcium and breast mammography density: Characteristics of cohort studies
Author Year
Study Name
Location
(Latitude)
[PMID]
Cohort
Mishra 2008
Medical MRC
NSHD
UK
54
2
N
[ 18827811)
Population
Health status No breast
cancer
Mean age 52
(range/ SO), y
Dietary Calcium intake
Dietary 5day food diaries
assessment McCance and
method Widdowson's food
table
Internal ND
validation? (y/n)
Comparisons
At age 36 y:
<523, 524-648,
652-784, 785-940,
>941
At age 43 y:
<611 , 612-735,
736-859, 860-
1020,>1021
Confounders/Effect Modifiers Adjusted
X
Ill
E
Cll
.:
'S
z
X
J:.
c.
Cl
0
E
Cll
0
X
c.
0
..
J:.
E
<(
X
1!!
:I
Ill
0
c.
><
Cll
>
::::l
X
Table 72. Calcium and breast cancer: Results of cohort studies
Author Year
Study Name
[PMID]
Mishra 2008
171
Medical MRC NSHD
[ 18827811
Life Stage
Premenopausal
women
Outcome (n/N;
Incidence)
Breast cancer
density
(nd; median
21.9%)
Follow up
Duration
(Time to Dx)
-32 y
-32 y
-32 y
-32 y
-32 y
-39 y
-39 y
-39 y
-39 y
-39 y
Total Ca
Intake,
mg/day
S523
No. of
Cases
133
524-648 143
652-784 156
No. in
Category
766
766
766
Adjusted
RR
13 coefficient
1
-0.11
-0.05
95% CI
Reference
-0.33,
0. 10
-0.27,
785 - 940 .................i"6'0""""""'"-----:7:-: 6::-: 6--................... -
174
S611 145
612-735 - ................Tiii'6 ............
736-859 145
860-1 020 1 56
153
218
0. 19
766
- ----===---...__ 0_.1_7_ ,
755 13 coefficient
1
Reference
755
----:a:-i-3---..----o-=-.::-: 3s ;:- .-
-----::=-=-=---.......................................................__ o_._o9 __
755 -0.06 -0.29,
755 -0.11
755 -0.16
0. 17
-0.34,
0. 12
-0.42,
0.09
Ill
E
Cll
E
E
0
()
Total calcium
intake from diet
and supplement
P for
Trend
NS
NS
Study
Quality
B
Pancreatic cancer.
We reviewed primary studies that evaluated associations between calcium intake and
incidence of pancreatic cancer.
Synopsis.
Two studies analyzed three US cohorts and found that total daily calcium intake was not
associated with the risk of pancreatic cancer in men and women. No RCTs of calcium intake or
supplement have evaluated this outcome.
Detailed presentation (Tables 73 & 74).
One study analyzed data from Nurses' Health Study (NHS) and the Health Professionals
Follow-up Study (HPFS).
172
The study identified a total of 365 cases of pancreatic cancer
(178/75,427 women aged 38 to 65 years from NHS; 178/46,771 men aged 40 to 75 years from
HPFS). Comparing the group with at least 1000 mg/d of calcium intake to the group with less
than 500 mg/d, there was no significant difference in the relative risk of pancreatic cancer (RR
0.94; 95 percent CI 0.62, 1.41 for overall; 0.75; 95 percent CI 0.43, 1.30 for NHS; 1.23; 95
percent CI 0.67, 2.25 for HPFS). The result was adjusted for age, categories of total vitamin D
intake, smoking, diabetes, BMI, height, region of residence, use of multivitamin, and parity (for
women). The pancreatic cancer was not stratified into endocrine versus exocrine tumors.
Methodological quality of this study was rated A.
Another study analyzed data from AARP (the American Association of Retired Persons)
members, aged 50 to 71 years old, living in six specific states in the US.
125
The study identified a
total of 717 and 3 84 cases of pancreatic cancer in men and women over 7 years of followup
period, respectively. Pancreatic cancer was one of many other cancer outcomes evaluated in this
study. The results showed that that total calcium intake was not associated with the risk of
pancreatic cancer after controlling for potential risk factors pertinent to individual cancers. The
methodological quality of this study was rated B.
Findings by life stage.
0-6 mo Not reviewed
7 mo - 2 y Not reviewed
3 - 8 y Not reviewed
9 - 18 y Not reviewed
19-50 y One study analyzed two US cohorts (NHS [women 38- 65 y] and HPFS
[men 40 -75 y]) and found that total daily calcium intake was not associated with the risk
of pancreatic cancer.
51-70 y One study analyzed two US cohorts (NHS [women 38- 65 y] and HPFS
[men 40 -75 y]) and found that total daily calcium intake was not associated with the risk
of pancreatic cancer. Another study analyzed US AARP cohort with men and women in
this life stage found similar result.
::::71 y One study that analyzed HPFS included males up to 75 years old and
found that total daily calcium intake was not associated with the risk of pancreatic cancer.
Postmenopause No data
Pregnant & lactating women Not reviewed
219
Table 73. Calcium and cancer: Characteri sti cs of cohort studies
Confounders/Effect Modifiers
Author,
Adjusted
Year
Study Name
Population Diet ary calcium intake Comparisons
.2 41
Comments
Location
s:
...
Q.
:I
"' (Latitude)
"'
"'
Ql
'E
Q.
i;j
0
[PMID]
C)
0
Q.
0 ... 0
>< VI
E
s:
:s
41
'5 41 'E
Ql
>
z 0
<
:::!!: ::> ::::i
Skinner Health OM: Dietary 131 -item Pancreatic X X X X X X current
2006
172
status NHS assessment FFQ cancer risk smoker
NHS, HPFS 3%; method (Willet, stratified by -23%
us HPFS 1990) different
(multiple 1% intakes of
latitudes)
Mean age NHS
calcium
[1 6985031)
(range/SO), 51;
(dietary and
y HPFS
supplement
55
combined)
Male(%) NHS O; Internal y
HPFS validation?
100 (x:Jn)
Park 2009
125
Health No Dietary FFQ Pancreatic X X X X X Total
NIH-AARP status cancer assessment (NCI- cancer risk calcium
us
Mean age 50-71
method DHQ) stratified by intake from
38
2
N
(range/), y
USDA quintile of diet and
[ 19237724) Nutrient total calcium supplement
Database intake
Male (%) 60 Internal y
validation?
-------
Table 74. Calcium and pancreatic cancer: Results of cohort studies
Author Year
Life Outcome Followup
Total Ca
No. of Total no. in Adjusted P for Study
Study Name intake in 95%CI
[PMID]
Stage, y (n/N; Incidence) Duration, y
mg/d
Cases Category RR Trend Quality
Skinner 2006
19-50 Pancreatic cancer <500 41 nd Reference A
NHS, HPFS
51 -70 (365/ 122, 198; 0.003) 14.5
500-999 228 nd
0.83, 1.66
0.29
us
overall
nd
----------------
(multiple latitudes)
<:1000 96 0.94 0.62, 1.41
[ 16985031)
19-50 Pancreatic cancer <500 24 nd 1 Reference
51 -70 ( 178/75,427; 0. 002)
-------------
15.4 500-999 109 nd 1.09 0.69, 1.73 0.09
---------------
women NHS <:1000 45 nd 0.75 0.43, 1.30
19-50 Pancreatic cancer 13.1 <500 17 nd 1 Reference 0.86
---------------
51 -70 (187/46,771; 0.004) 500-999 119 nd
................................................................................................................
1.28 0.76, 2.18
220
Author Year
Life Outcome Followup
Total Ca
No. of Total no. in Adj usted P for Study
Study Name intake in 95% CI
[PMID]
Stage, y (n/N; Incidence) Duration, y
mg/d
Cases Category RR Trend Quality
men HPFS 51 nd 1.23 0. 67, 2.25
526 717 293,907
1 (HR) Reference
Park 2009
(total) (total)
---------------
NIH-AARP
125 50-71, Pancreatic cancer
7
498 0.93 0.74, 1.16
0.39 B
(717/293,907; 0.002)
-------------
[1 9237724)
men 857 0.9 0.72,1.14
--------- ------
1073 0.98 0.78, 1.23
1530
0.68, 1.11
526 384 198,903
1 (HR) Reference
(total) (total)
---------------
50-71, Pancreatic cancer
7
498 1.03 0.75, 1.40
0.40
(384/ 198,903; 0.002)
------ -------
women 857 0.93 0.67, 1.28
......................._M__ .....................
1073 0.97
------ ----------
0.71 , 1.34
1530 0.88 0.63, 1.24
221
Calcium and pregnancy-related outcomes
Preeclampsia.
Synopsis.
This summary is primarily based on a systematic review of 12 RCTs (n=15,528
women) of calcium supplementation (?:: 1000 mg/d) during pregnancy versus placebo for
preventing preeclampsia. In addition, it includes findings from two cohort studies (one of
which is a reanalysis of one of the 12 RCTs mentioned above).
Overall, the random effects meta-analysis of the 12 RCTs favored calcium
supplementation (RR=0.48, 95 percent CI 0.33, 0.69), albeit with substantial between-
study heterogeneity. More than 80 percent of the total number of randomized women
(n= 12,914) came fi"om two large trials that found no significant effect of calcium
supplementation for preventing preeclampsia (RR=0.95, 95 percent CI 0.89, 1.05). Based
on their confidence interval, the two large studies excluded large effects of calcium for
preeclampsia prevention. There is no obvious explanation for the observed between-study
heterogeneity in the aforementioned meta-analysis. The heterogeneity sterns from
differences in the effects between smaller trials (claiming protective effects) and large
trials (showing no effect).
The two cohort studies did not detect associations between calcium intake during the
first or second trimester of pregnancy with preeclampsia. Both cohorts were rated B for
methodological and reporting quality.
Based on the above, there is not a clear answer to whether calcium supplementation is
effective for preeclampsia prevention.
Detailed presentation (Tables 75, 76 & 77).
Relevant published systematic reviews of RCTs (with meta-analyses).
We identified five systematic reviews
173
-
177
(with meta-analyses) ofRCTs on calcium
supplementation in the first or second trimester versus placebo for the prevention of
preeclampsia (Appendix D). We selected a 2006 Cochrane review as eligible for this
section.
176
All other systematic reviews were covered by the Cochrane review. We did
not identify any RCTs published after the Cochrane review was conducted.
Eligible were RCTs comparing at least 1000 mg/d of calcium versus placebo in
pregnant women. Studies were performed in several countries (both developed and
developing). The review defined preeclampsia as high gestational blood pressure
(diastolic blood pressure >90 mrnHg, or increase more than 15 mm Hg in diastolic or
more than 30 mm Hg in systolic blood pressure) with significant proteinuria (at least 300
mg/d or at least 500 mg). i
Table 75 summarizes the findings of the Cochrane review. A random effects meta-
analysis of all studies suggests that calcium supplementation reduces the risk for
preeclampsia (RR=0.48, 95 percent CI 0.33, 0.69). However, there is substantial
heterogeneity among the included studies (P<O.OOl).
i Note that a strict definition of preeclampsia requires confirmation of no hypertension or proteinuria outside of pregnancy.
222
In subgroup analyses, the effects of calcium appear larger in women at high risk for
hypertension versus women at low risk for hypertension. The same is observed when
trials are grouped according to whether women had adequate average calcium intake
versus low average calcium intake.
More than 80 percent of the total number of randomized women in this meta-analysis
(n=12,914) came from two large trials that reported no significant effects of calcium
supplementation for preeclampsia (RR=0.95, 95 percent CI 0.89, 1.05; by fixed effects
synthesis). Based on their combined confidence interval, these two studies exclude
modest and large effects of calcium for preeclampsia prevention. The remaining (smaller)
trials show a protective effect. One of the large RCTs was performed in populations with
low background calcium diets
178
and the other in populations with adequate background
calcium diets.
179
Allowing for the above, there is no clear explanation for the observed discrepant
findings across the trials in the systematic review. The recurrent pattern is that large trials
showed no effect for calcium supplementation, whereas smaller trials showed large
effects. Calcium supplementation for preeclampsia prevention is a well known example
where large trials and smaller trials show systematically different effects. Past
methodological explorations (before the publication of the WHO trial
178
) have
hypothesized that effects may be observed mostly among women with low calcium in
their background diet.
180
However, as mentioned above, this is not supported by the
subgroup analyses.
223
Table 75. Summary table of systematic review on calcium supplementation and
preeclampsia, small for gestational age, preterm birth
Author Year [PMID] Hofmeyr 2006
116
(16855957)
Desi gn (Search Years) Randomized controlled trials (19882006)
Population Pregnant women less than 35 weeks of gestation regardless of their risk of hypertensive of
pregnancy or their previous calcium intake
Intervention (Exposure)
and Comparator
Results
Comments
A priori design?
Calcium supplement (at least 1000 mg/d) vs. placebo
12 trials (n=15,528t
Preeclampsia (mother):
All 12 trials (n=15,528): RR=0.48 (0.33, 0.69)
6
; statistically heterogeneous
Among 4 trials (n=5022) with adequate Ca in diet: RR=0.62 (0.32, 1.20); statistically
heterogeneous
Among 7 trials (n=10,1 54) with low Cain diet: RR=0.36 (0. 18, 0.70); statistically
heterogeneous
Among 5 trials (n=587) at high risk for hypertension: RR=0.22 (0.12, 0.42); statistically
homogeneous
Among 6 trials (n=14,619) at low risk for hypertension: RR=0.68 (0.49, 0.94);
statistically heterogeneous
High blood pressure with or without proteinuria (mother):
Among 11 trials (n=1 4,946): RR= 0.70 (95% Cl 0.57, 0.86); statistically heterogeneous
Among 4 trials (n=5022) with adequate Cain diet: RR=0.90 (0.81, 0.99); statistically
homogeneous
Among 6 trials (n=9684) with low Ca in diet: RR=0.47 (0.29, 0.76) ; statistically
heterogeneous
Among 4 trials (n=327) at high risk for hypertension: RR=0.47 (0.22, 0.97); statistically
heterogeneous
Among 7 trials (n=14,619) at low risk for hypertension: RR=0.78 (0.64, 0.95);
statistically heterogeneous
Preterm birth:
Among 10 trials (n=14,751 ): RR = 0.81 {0.64, 1.03); statistically heterogeneous
Among 4 trials (n=5033) with adequate Ca in diet: RR=0.59 {0.26, 1.33); statistically
heterogeneous
Among 6 trials (n=9684) with low Ca in diet: RR=0.90 (0.80, 1.02); statistically
homogeneous
Among 4 trials (n=478) at high risk for hypertension: RR=0.45 (0.24, 0.83); statistically
homogeneous
Among 7 trials (n=14,183) at low risk for hypertension: RR=0.91 (0.74, 1.12);
statistically heterogeneous
Small for gestational age (infant):
Among 3 trials (n=13,091; fixed effects): RR = 1.10 (0.88, 1.37); statistically
homogeneous
About 80% of participants are from two well designed and well conducted RCTs
1 78
119
The
two large ACTs show no effects for all four outcomes.
AMST AR Criteria
Yes Study quality assessment performed?
Two independent reviewers?
Comprehensive literature search?
All publication types and languages
included?
Yes Study quality appropriately used in analysis?
Yes Appropriate statistical synthesis?
Yes Publication bias assessed?
Yes
Yes
Yes
No
Included and excluded studies listed?
Study characteristics provided?
A RR <1 .0 favors calcium supplementation
6
95% confidence interval
Yes
Yes
Conflicts of interest stated? Yes
224
Cohort studies.
We identified two eligible prospective cohort studies (Table 76).
181
'
182
Both were
rated B for methodological and reporting quality. The first was a reanalysis of a large
RCT and reported no associations of dietary calcium intakes during the first and second
trimester with preeclampsia.
181
The second study was a prospective cohort that again
reported no association between dietary calcium intake in the first trimester and risk of
preeclampsia.
182
(See Table 77)
Findings by life stage.
0 - 6 mo Not appli cable
7 mo - 2 y Not applicable
3 - 8 y Not applicable
9- 18 y Not applicable
19- 50 y Not applicable
51 - 70 y Not applicable
2:71 y Not applicable
Postmenopause Not applicable
Pregnant & lactating women Based on a Cochrane review that
synthesized data from 12 RCTs on 15,528 pregnant women, calcium
supplementation significantly lowered the risk for preeclampsia during
pregnancy. However, this meta-analysis was heterogeneous; significant effects
were observed only among small studies, and not in the two largest RCTs that
comprised more than 80 percent of the women in the meta-analysis. ln addition,
two coh01t studies found no association between calcium intake and
preeclampsia. Overall, the effects of calcium supplementation on preeclampsia
are unclear.
225
Table 76. Calcium and preeclampsia and other pregnancy outcomes: Characteristics of
cohort studiesA.
8
Author Year
Study Name
Location
(Latitude)
[PMID]
Morris
2007
181
CPEP
reanalysisc
us
(various)
(11262466)
Oken
2007'
82
Project Viva
us
(42N)
[17521921)
Population
Health
status
Mean
age
(SO), y
Male
(%)
Health
status
Mean
age
(SO), y
Male
(%)
Healthy
NO
0
Healthy
[most 30
to <40)
0
Dietary Calcium
intake
Dietary FFQ
assessment
method
Internal No
validati on?
In
Dietary FFQ
assessment
method
No Internal
validation?
(y/n)
A Both table entries are treated as cohort studies.
Comparisons
Outcome
stratified by
total Ca intake
quintiles
Outcome as a
function of Ca
intake
Confounders/Effect Modifiers
Adjusted
.J:.
::s Q.
VI Rl
VI
E 0,
Q.
iii
0
Q)
0
Q.
>.
Q)
0
... (,)
><
Ui ;:
E
.J:.
'5
Q)
; Q) 'E Q)
>
z c <( :: ::I
::::;
X X X
X X
"0
C: VI
m-
VI C:
Q) Q)
E E
o E
(,) 0
; u
0
Total
Ca
{both)
Total
Ca
(both)
6
In contrast with most other summary tables of study characteristics, this table is ordered alphabetically by study author.
c Reanalysis of the CPEP trial (calcium versus placebo) for preeclampsia preventi on focusing on calcium content in diet
(and including the intervention dose in the analyses)
226
Table 77. Calcium and preeclampsia and other pregnancy outcomes: Results of cohort studies
Age Outcome (n/N; Followup Total Ca No. of No. in Adjusted 95%CI P for Study
Range, Incidence) Duration Intake, Cases Category OR Trend Quality
Sex mg/d
Preeclampsia
Morris 2007'
81
30-40 y, Preeclampsia ND 579 NO ND 1.00 (ref) ND B
CPEP reanalysis Women (326/431 4; 7.6%)
us
(various)
[1 1262466)
.......................................................
580-845 ND ND
.......................................................
0.90 0.61, 1.30
846-1131 ND ND 0.95 0.65, 1.39
1132-1 560 NO
.......................N'D ....................
0.97 0.65, 1.45
.......................................................
1561 NO NO 0.78 0.49, 1.24
Oken 2007 Preeclampsia -1300 59
(59/ 1599; 3.7%)A
1599 1.03 0.84, 1.27 NS B
High blood pressure with
or without
Morris 2007
81
30-40 y, High blood pressure with ND 579 ND ND 1.00 (ref) ND B
CPEP reanalysis Women or without proteinuria
us (747/4314; 17.3%)
(various)
[1 1262466)
.......................................................
580-845 ND ND
.......................................................
1.09 0.84, 1.42
846-1131 ND ND uo 0.83, 1.44
1132-1560 NO
.......................N'D .....................
1.14 0.85, 1.53
.......................................................
1561 NO NO 1.35 0.98, 1.86
Oken 2007 Pregnancy-induced NO -1300 119 1659 0.99 0.85, 1.15 NS B
hypertension
(1 19/ 1659)c
Excludes 119 women with pregnancy-induced hypertension - comparison versus normotensive women
6
Per 300 mg of Ca intake (from supplement or diet)
c Excludes 59 women with preeclampsia- comparison versus normotensive women
227
High blood pressure with or without proteinuria during pregnancy.
Synopsis.
The synopsis of this outcome is based on the same systematic review described under
preeclampsia. Overall , the meta-analysis of 11 RCTs favored calcium supplementation
RR = 0.70 (95 percent CI 0.57, 0.86) for the treatment of hypertension during pregnancy,
with or without proteinuria. However, there was substantial between-study heterogeneity.
(Included in this meta-analysis are the two large trials mentioned in the preeclampsia
section, which found no significant effect of calcium supplementation on blood pressure.)
The systematic review did not offer a clear explanation for the observed heterogeneity.
Based on the above, there is no clear answer to whether calcium supplementation is
effective for preventing high blood pressure (with or without proteinuria) in pregnancy.
Detailed presentation (Tables 75, 76 & 77).
Relevant published systematic reviews (with meta-analyses).
The Cochrane review that was selected for preeclampsia was applicable for
hypertension during pregnancyi as well.
176
Table 75 summarizes the findings ofthe
Cochrane review.
A meta-analysis of 11 trials (14,946 pregnant women) suggested that calcium
supplementation reduces the risk for hypertension during pregnancy (RR=0.70, 95
percent CI 0.57, 0.86). However, there is substantial heterogeneity among the included
studies (p<O.OOl). As described in Table 75, the heterogeneity was not explained by
whether the trials included women with low versus adequate background dietary calcium
intake.
In subgroup analyses, the effects of calcium appear larger in women at high risk for
hypertension versus women at low risk for hypertension. The same is observed when
trials are grouped according to whether women had adequate average dietary calcium
intake versus low average calcium intake (see Table 75).
Cohort studies.
A single prospective cohort study
182
(Table 68) reported no association between
calcium intake levels and risk for preeclampsia.
182
(See Table 69.)
Findings by life stage.
0 - 6 mo Not applicable
7 mo - 2 y Not applicable
3 - 8 y Not applicable
9- 18 y Not applicable
19- 50 y Not applicable
51 - 70 y Not applicable
~ 7 y Not applicable
Postmenopause Not applicable
i The Cochrane review doc.s not clarify whether the women were confi rmed normotensive outside pregnancy. This is why we do not
usc the term pregnancy- induced hypertension for this outcome.
228
Pregnant & lactating women Based on a Cochrane review that
synthesized data from 11 RCTs on 14,946 pregnant women, calcium
supplementation significantly lowered the risk for hypertension with or without
proteinuria during pregnancy. However, this meta-analysis was very
heterogeneous; significant effects were observed only among small studies, and
not in the two largest RCTs that comprised more than 80 percent of the women in
the meta-analysis. In addition, a cohort study found no association between
calcium intake and hypertension during pregnancy. Therefore, the effects of
calcium supplementation on hypertension with or without proteinuria during
pregnancy are unclear.
Preterm birth.
Synopsis.
The synopsis of this outcome is based on the same systematic review described under
preeclampsia. Among 10 RCTs (n=14,751), calcium supplementation has no significant
effect on preterm births RR 0.81 (95 percent CI 0.64, 1.03). (Included in this meta-
analysis are the two large trials mentioned in the preeclampsia section, which found no
significant effects.)
Based on the above, there is no evidence for an effect of calcium supplementation on
preterm births.
Detailed presentation (Table 75).
Relevant published systematic reviews (with meta-analyses).
The Cochrane review that was selected for preeclampsia was applicable for preterm
birth as well.
176
Table 67 summarizes the findings of the Cochrane review.
A meta-analysis of 10 trials suggests that calcium supplementation had no significant
effect on preterm births. There is evidence for between-study heterogeneity in this meta-
analysis.
In subgroup analyses, the effects of calcium appear larger in women at high risk for
hypertension versus women at low risk for hypertension. The same is observed when
trials are grouped according to whether women had low average dietary calcium intake
versus adequate average dietary calcium intake.
Findings by life stage.
0-6 mo Based on a Cochrane review that synthesized data from ten RCTs
on 14,751 pregnant women, calcium supplementation had no significant effect on
whether infants were born prematurely or not.
7 mo- 2 y Not applicable
3 - 8 y Not applicable
9 - 18 y Not applicable
19- 50 y Not applicable
51 - 70 y Not applicable
~ 7 y Not applicable
Postmenopause Not applicable
Pregnant & lactating women Not applicable
229
Small for gestational age infant.
Synopsis.
The synopsis of this outcome is based on the same systematic review described under
preeclampsia. The overall effects of calcium supplementation were not significant
(among three RCTs in 13,091 randomized women RR = 1.10, 95 percent CI 0.88, 1.37).
(Included in this meta-analysis are the two large trials mentioned in the preeclampsia
section, which found no significant effects.)
Based on the above, there is no evidence for an effect of calcium supplementation on
preterm births.
Detailed presentation (Table 75 ).
Relevant published systematic reviews (with meta-analyses).
The Cochrane review that was selected for preeclampsia was applicable for this
outcome as well.
176
Table 75 shows that among three trials with pertinent information
there was no significant effect of calcium supplementation on the proportion of infants
who were small for gestational age.
178
,
179
Findings by life stage.
0 - 6 mo Based on a Cochrane review that synthesized data from three
RCTs on 13,091 pregnant women, calcium supplementation has no significant
effect on whether born infants were small for gestational age or not.
7 mo - 2 y Not appli cable
3 - 8 y Not applicable
9 - 18 y Not applicable
19 - 50 y Not applicable
51 - 70 y Not applicable
~ 7 y Not applicable
Postmenopause Not applicable
Pregnant & lactating women Not applicable
230
Calcium and all-cause Mortality
Synopsis.
One cohort study (rated B for methodological and reporting quality) reported no
significant associations between calcium intakes and all-cause mortality in men or
women aged between 40-65 years. No RCTs of calcium intake evaluated all-cause
mortality.
Detailed presentation (Tables 78 & 79).
One cohort study from Amsterdam, Netherlands (52N), reported in two
publications
105
126
evaluated associations between calcium intake and all-cause mortality.
The cohort was based on a general population health survey and enrolled civil servants or
their spouses (aged 40-65 years). The reports received grade "B" for methodological and
reporting quality (Table 70).
The publications reported no association between calcium intake and all-cause
mortality among men or women. Table 71 shows the results of the various analyses
conducted in the two publications.
105
126
Findings by life stage.
0 - 6 mo No data
7mo - 2y Nodata
3 - 8 y No data
9- 18 y No data
19 - 50 y One cohort study found no associations between calcium intakes
and all-cause mortality in men or women aged between 40-65 y.
51- 70 y The above (19-50 y) may be applicable here as well, based on the
age range of cohort participants.
~ 7 y No data
Postmenopause No data
Pregnant & lactating women No data
231
Table 78. Calcium intake and all-cause mortalit y: Characterist ics of cohort studi es
Author Year
Study Name
Location
(Latitude)
[PMID]
Vander
Vijver
1992
105
&
Slob 1993
1
:re
Netherlands
(52N)
[1544755 &
8478144)
Population
Health General
status population
Age 40-65y
range, y
Male 51
(%)
Calcium intake Comparisons
Dietary FFQ Outcome
assessment stratified by
method total Ca intake
quintiles
Internal No
validation?
(y/n)
232
Confounders/Effect Modifiers
Adjust ed
!!!
.s::.
c.
:I
VI ftl
VI
E c,
c.
iij
0
(I)
0 c.
(I)
0 ... u ><
'0::
E
.s::.
:0
(I) VI
'S (I) E
(I)
>
.1!!
z
Q
<1: :::E ::1 ::;
X X X X
VI
E
(I)
E
E
0
(.)
Total
Ca
(food)
Table 79. Calcium intake and all-cause mortality: Results of cohort studies
Author Year Age Outcome (n/N; Followup Total Ca No. of No. in Adjusted 95% CI P for Study
Study Name Range, Incidence) Duration Intake, Cases Category OR Trend Quality
Location Sex mg/d
(Latitude)
[PMID]
Van der Vijver 1992
105
& Slob 40-65 y, All cause 336 mo (28 S585 nd nd 1.1 0.7, 1.6 nd B
1993
126
men mortality y)
Netherlands (nd)
(52N)
[1 544755 & 8478144]
----------
585 - 725 nd
--------
nd 1.1 0.7, 1.6
725 - 935
___ 1]_9____
nd 0.8 0.5 1.2
935 - 1245 nd nd 0.9 0.6, 1.3
>1245 nd nd 1.0 Reference
Van der Vijver 1992 & Slob 40-65 y, All cause 336 mo (28 S445 nd nd 1.2 0.8, 1.9 nd B
1993
126
women mortality y)
Netherlands (nd)
(52N)
[1 544755 & 8478144]
----------
445 - 540 nd nd 1.1 0.7, 1.7
540 - 640 nd nd 1.3 0.9, 2.0
640 - 850 !,19,__ nd 1.1 0.7 1.7
>850 nd nd 1.0 Reference
233
Calcium and Hypertension and Blood Pressure
We searched for systematic reviews and primary studies that evaluated associations between
calcium intake or body stores and incidence of hypertension and change in blood pressure. For
the outcome incidence of hypertension, we reviewed randomized controlled trials and other
longitudinal studies. For the outcome change in blood pressure, we reviewed only randomized
controlled trials. The EPC and the TEP agreed that due to the large volume of literature, the
limited resources would not be expended on reviewing observational studies for the surrogate
outcome blood pressure. We included only studies of adults. Studies of pregnancy-related
hypertension and blood pressure control are included in the pregnancy section.
Calcium and hypertension.
Synopsis.
No systematic reviews evaluated the association between calcium intake and incidence of
hypertension. The association has been analyzed in five large studies (6 articles/analyses). No
RCTs of calcium intake evaluated hypertension incidence. In analyses of men and women
together and of men alone, there was no evidence of an association between calcium intake and
risk of hypertension. In the Women's Health Study (WHS), a highly significant trend was found
across quintiles of calcium intake and risk of hypertension, with significantly lower rates of
hypertension found among women consuming at least 679 mg calcium per day compared to less
than 558 mg calcium per day. The two articles that reported subgroup analyses based on age
found associations between lower calcium intake and hypertension among younger adults (below
40 or 50 years of age), but no significant associations in older adults.
Detailed presentation (Tables 80 & 81 and Figure 21 ).
The six articles, reporting investigations of five studies, included two analyses of combined
men and women in the NHANES I study and Navarra, Spain (both methodological quality
C),
183
,
184
two analyses of men alone in the Health Professionals Follow-up Study (HPFS) and
NHANES I (of methodological quality Band C, respectively),
185
'
186
and three analyses of
women alone in the WHS, the Nurses Health Study (NHS), and NHANES I (of methodological
quality A, B, and C, respectively).
186
-
188
All studies included only people without hypertension at
baseline. Only the A quality analysis, WHS, included elevated blood pressure in their outcome
definition ofhypertension; all other analyses used self-reported hypertension (generally based on
a physician's diagnosis or treatment). The mean ages of the participants varied widely across
studies (36-54 years) among those that reported mean data; the range of ages within studies
varied from broad (20-90 years) to narrow (30-55 years) among those that reported ranges. All
studies reported adjusted analyses; though each adjusted for different factors. Most of the studies
were limited by such factors as reliance on self-reported hypertension (without assessment of
blood pressure), exclusion of numerous participants due to lack of data, inadequate reporting of
results data, and lack of reporting of definitions (ranges or averages of calcium quintiles ).
Two studies reported analyses for combined men and women. These are discussed here. The
remaining analyses of men or women separately are discussed below. In analyses of combined
men and women (each with almost 7000 participants), neither study reported a significant
association. No significant trend or individual analyses of quintiles was found in the short
duration (2 years) Spanish cohort study. A poorly reported analysis from NHANES I concluded
that there was progressively higher incidence of hypertension in lower quartiles of calcium
234
intake after 10 years, but no statistical analysis was performed and the definitions of the quartiles
were not provided.
Findings per calcium intake level.
Among the studies that provided definitions of the compared categories of calcium intake,
consistent significant associations were found for calcium intakes below 500 mg/day in men
under age 50 years (compared to over 1100 mg/day) and below 558 mg/day in women
(compared to over 678 mg/day).
Findings per age and sex.
Men alone were analyzed from the PHFS (about 31,000 men) and NHANES I (about 2000
men, split by race). Neither analysis found a significant trend or any significant differences
among different calcium intake categories at 4 and 10 years, respectively for the two studies.
Women alone were analyzed from three studies. The studies had heterogeneous findings. The
A quality analysis of the WHS (about 29,000 women) found a highly significant trend across
quintiles (P<0.0001) at 10 years with a significantly higher rate of hypertension in women in the
lowest calcium intake quintile (189-557 mg/day) compared to all quintiles with intakes above
679 mg/day. However, the B quality analysis of the NHS (about 41,500 women) found no
significant association by calcium intake at 14 years and the C quality analysis of NHANES I
(about 3500 women, split by race) found no consistent association at 10 years.
One C quality analysis ofNHANES I assessed subgroups of combined men and women by
age (divided at 40 years old). Among people under age 40 years, those in the lowest quartile of
calcium intake had significantly higher rates of being treated for hypertension after 1 0 years;
however, the article fai led to define the calcium intake quartiles. No significant association was
found among older participants. In the HPFS, in men under age 50 years, a higher rate of
hypertension at 4 years was found in those with calcium intake less than 500 mg/d compared to
over 1100 mg/d; but no association was found in older men.
Findings by life stage.
0-6 mo Not reviewed
7 mo- 2 y Not reviewed
3-8 y Not reviewed
9-18 y Not reviewed
19-50 y Five of the six studies included mostly people within this life stage.
183
-
186' 188 Overall, there was no evidence of a significant association between calcium intake
and risk of hypertension. However, as described in detail in the Findings per age and sex
section above, in two subgroup analyses, significant associations were found between the
lowest category of calcium intake and increased risk of hypertension in younger people
(under age 40 - calcium intake range not reported, or age 50 years - less than 500 mg/d
compared to over 1100 mg/d.
51 -70 y Four of the six studies included people largely within this life
stage.
184
185
187
188
The studies mostly found no significant associations between calcium
intake and risk of hypertension, including within the 2 subgroups of adults above 40 or 50
years of age. However, the WHS, which included women mostly within this life stage,
found a highly significant trend across quintiles (P<O.OOOl) at l 0 years with a
significantly higher rate of hypertension in women in the lowest calcium intake quintile
(189-557 mg/d) compared to all quintiles with intakes above 679 mg/d.
235
:::::71 y Few of the people in the studies appear to have been in this life stage. No
unique conclusions are possible for this life stage separate from those for people 51 to 70
years.
Postmenopause Only the WHS appeared to have included (or analyzed) primarily
postmenopausal women. The study found a highly significant trend across quintiles
(P<O.OOOl) at 10 years with a significantly higher rate of hypertension in women in the
lowest calcium intake quintile ( 189-557 mg/d) compared to all quintiles with intakes
above 679 mg/d.
Pregnant & lactating women Not reviewed
236
Table 80. Calcium and incidence: Characteristics of cohort studies
Confounders/Effect Modifiers
Adjusted
Author Year
1/)
'E
Study Name Dietary Calcium
.J:. Q)
Population Comparisons
Q. ::s
E
Location intake
Ul ftl
Ul
'E 0,
Q.
(ij
0
Q)
E
[PMID]
0
Q.
>. 0
0 ... u ><
c;; 0
E
.J:.
:0
Q)
'S Q) 'E
Q)
>
z c <1: ::I ::J
Alonso 2005 Health Norma- Dietary FFQ Hypertension X X X X X Total
U Navarra status tensive assessment incidence Ca
Follow-up
Mean 36 method stratified by (both)
Navarra Spain age (20-90) total Ca intake
(43N) (range), y
quintiles
[16280427)
Male 39 Internal No
(%) validation?
Dwyer 1996
184
A
(:i/n)
Health Normo- Dietary 24 hr Hypertension X X X X Total
NHANESI status tensive assessment recall incidence Ca
us
Mean 46 (25- method stratified by (both)
(various) age 74) total Ca intake
[8890661] (range) , y quartiles
Male 63 Internal nd
(%) validation?
(:t/n)
Ascherio 1992
185
Health Normo- Dietary FFQ Hypertension X X X Total
HPFS status tensive assessment incidence Ca
us Median 50 (40- method stratified by (both}
(various) age 75) total Ca intake
[1330360) (range), y categories
Male 100 Internal Yes
(%) validation?
/n)
Ford 1991 Health Norma- Dietary nd Hypertension X X Total
NHANESI status tensive assessment incidence Ca
us Mean nd method stratified by (both}
(various)
age total Ca intake
[1937662] (range), y quartiles
Male 35 Internal nd
(%) validation?
Wang 2008
181
Health Norma- Dietary FFQ Hypertension X X X X X Total
WHS status tensive assessment incidence Ca
us Mean 54 (6.5; method stratified by (both}
(various)
age (SD, total Ca intake
[18259007]
range), y
quintiles
Male 0 Internal No
(%) validation?
(:i/n)
Ascherio 1996
188
Health Normo- Dietary FFO Hypertension X X X Total
NHS status tensive assessment incidence Ca
us
Mean nd (30- method stratified by (both)
(various) age 55) total Ca intake
[8621198) (range), y categories
Male 0 Internal Yes
(%) validation?
(:t/n}
A Overall and age subgroup analyses from NHANES I reported in this study. However, different samples selected; 63% male.
8
Sex and race subgroup analyses from NHANES I reported in this study. However, different samples selected; 35% male.
237
Table 81. Calcium and hypertension incidence: Results of cohort studies
Author Year Age Range, Outcome (n/N, Followup Total Ca No. of
Cases
No. in
Category
Adjusted 95% Cl P for
Study Name Sex Incidence) Duration Intake, OR Trend
[PMID] (Time to Ox) mg/day
Both Sexes
Alonso 2005
U Navarra Follow-up
[16280427]
Dwyer 1996
184
A
NHANESI
[8890661)
Men
Ascherio 1992
HPFS
[1330360)
continued
20-90 y,
Both
25-74 y, Both
$40 y
>40 y
40-75 y,
Men
:550 y
>50 y
Hypertension
(180/6686, 0.027)
Hypertension, treated
(1704/6634, 0.257)
Hypertension, treated
(nd/nd)
Hypertension, treated
(nd/nd)
Hypertension
(1248/30,681 , 0.041)
Hypertension
(nd/14,354)
Hypertension
(nd/ 16,31 4)
2y
10 y
10 y
10 y
4y
4y
4y
Mean (SD)
900 (200)
39 - 1337 Reference 0.67
1000 (200) 39 - 1337 0.98 0.62, 1.54
1200 {200) 35 - 1337 0.82 0.511':36-
1400 (300) """'"'"' 3 0 '"'"'"'" - 1337 0.73
...........37 ...... 1.54
nd nd - 1658 29.8% nd
nd nd
__ _,n-"' d,__ ___ .. n,d .
nd nd
nd nd
nd nd
__ _,n-"' d,__ ___ ........
nd nd
nd nd
nd nd
__ _,n-"' d,__ ___ .. n,d .
nd nd
<500 85
500-700 297
- --7-:: 7070'-'-9""0':" 0:--- .... 3.3.3. ..
900-1100 195
338
<500 nd
500-1100
<500
5001100
238
nd
nd
nd
n,d
nd
--_..,.. 16 ""5::-:: 8c----_...., 2:-:: 7:-:- %,...--------------
- 1658 -25%
- 1658 21.3%
nd 1 Reference
__ ....;. n;.;:; d ___ _____ Q;_51,_
___ __
nd 0.89 0 81 , 0.97
nd
nd 1 Reference
__ ____
__ ,_, nd,_ __ _ _,0.89J.1:..HL.
nd
nd 1.04 0.84, 1.28
1677 1.1 7 0.91 ' 1.50 0.53
--77:::-: 50o-: 4'----=' o.
7
9=- 1 - .
76., 1.04
5038 0.91 0. 76,1.09 -
7890 1 - Re ference
nd 1 .52 nd* nd
nd 0.86 nd
nd 1 Reference
nd 0.98 nd
nd 0.91 --n d--
Reference
Study
Quality
c
c
B
Author Year Age Range, Outcome (n/N, Followup Total Ca No. of No. in Adjusted 95% CI P for Study
Study Name Sex Incidence) Duration Intake, Cases Category OR Trend Quality
[PMID] (Time to Dx) mg/day
Ford 1991
1968
y, Hypertension 10 y <344 47 -215 Reference nd c
NHANESI Men (White) (360/1707, 0. 211)
[937662)
344-591 78 -382 0.91 0.60, 1.38
591-954 104 -448 1.09 0.73, 1.63
. ... ... .......... ..........
0. 64,1.45'- >954 131 -662 0.96
y, Hypertension 10 y <344 20 -34 1 Reference nd
Men (Black) (64/ 183, 0.350}
...........................................
344-591 17 - 45 0.68 0.28, 1.65_
591-954 18 -56 0.54 0.22, 1.33
>954 9 -34 0.35 0.11, 1.13
Women
Wang 2008 y, Hypertension 10 y 189-557 1860 5777 Reference <0.0001 A
WHS Women (8529/28,886, 0.295)
[8259007)
558-678 1778 5777 0.96 0.90, 1.03
679-801 .. j626 .. 5777 0.89
-- c-
0.83, 0.95
..... - ....----c-
802-999
.......... ............
5777 0.89 0.83, 0.95
1000-2559 1631 5777 0.87
e .
0.81, 0.93
Ascherio 1996 30-55 y, Hypertension 14 y <400 87 5581 1 Reference 0.76 B
NHS Women (2526/41 ,541 , 0.061) person-y
[621198)
...............6oi3'
400-600 36 605 1.07
600-800 712 42,544 1.05
800-1000 407
..................................
24,240 1.03
:2: 1000 712 41,325 1.04
Ford 1991 y, Hypertension 10 y <344 186 -865 1 nd c
NHANESI Women (White) (645/3065, 0. 210)
[937662)
344-591 183 -806 1.11
o .8.?..J..:.4.L . ... ... ............ _., ... ...
591-954 172 -775 1.17 0.90, 1.51
>954 104 -619 1.01
0.74.1.38- .
y, Hypertension 10 y <344 94 -225 1 Reference nd
Women (Black) (171/456, 0.375)
------.
344-591 35 -120 0.61
591-954 31 -74 1.11 0.62, 2.01
>954 11 -37 0.77 0.33, 1.81
Statistically significant (P<0.05)
A Overall and age subgroup analyses from NHANES I reported in this study. However, different samples selected; 63% male.
9
Sex and race subgroup analyses from NHANES I reported in this study. However, different samples selected; 35% male.
c Estimated from available data
239
Figure 21. Hypertension risk stratified by calcium intake
Ca P for
St udy Category intake (mg/d) trend Quality
:
Both sexes
U Navarra Fo llowup Q1 (ref) 900 0.67 c
St udy 2005 Q2 1000
(n=6686) 03 1200
0 4 1400
05 1700
Men
t
HPFS 1992 01 <500 0.53 B
(n=30,681 ) 02 500.700
03 700 - 900
0 4 900 - 1100
.95 (ref) >1.)00
-
NHANES 9 ~ l l (White) Q1 (ref) <344
~
nd c
(n=1707) Q2 344 - 591
Q3 591 954
04 >954
NHANES 11991 (Blacl() o1lre'fl <344
f
nd c
(n=183) 02 344-591
03 591 - 954
0 4 >954
-
Women
WHS 2008 01 (ref) 189557 <0.0001 A
(n=28,886) 02 558.678
Q3 679-801
0 4 802 - 999
05 1000,:.2559
-
NHS 1996 Cat 1 (ref) <400 0.76 B
(n=41,541) Cat 2 400 - 600
Cat 3 600 - 800
Cat 4 800-1000
CatS >1000
NHANES 11991 (White) 01 (ref) <344
~
nd c
(n=3065) 02 344 - 591
03 591 - 954
0 4 >954
-
NHANES 11991 (Black) 01 (ref) <344 nd c
(n=456) Q2 344- 591
Q3 591 -954
04 >954
I I I I
0.1 0.2 0.5 2
De<reased risk Increased risk
240
Calcium and blood pressure.
Synopsis.
We identified six systematic reviews that evaluated RCTs of calcium intake and changes in
blood pressure. Five additional trials not identified by these systematic reviews met eligibility
criteria for this report and are summarized together with the systematic reviews. Altogether, 69
trials have been identified. The range of intervention calcium doses were approximately 400 to
2000 mg/d, with most studies using 1000 to 1500 mg/d. The systematic reviews followed the
patterns of the primary studies in that they were divided among those that focused on studies of
people without hypertension, people with hypertension, and general populations (with or without
hypertension, without subgroup analyses). Because the systematic reviews all used somewhat
different eligibility criteria, they included overlapping groups of trials. No one or two systematic
reviews captured most of the relevant trials; therefore, all systematic reviews are included here.
Two overlapping systematic reviews evaluated trials of normotensive individuals. Both
found no significant effect of calcium supplementation and blood pressure. The two additional,
more recent primary studies of normotensive participants were consistent with this finding.
Four overlapping systematic reviews of the effect of calcium on blood pressure in
hypertensive individuals mostly found significant effects on systolic blood pressure (ranging
from about -2 to -4 mm Hg). An older, highly selective systematic review found no significant
effect. The systematic review that found the largest effect of calcium on systolic blood pressure
also found a significant effect on diastolic blood pressure ( -1.5 mm Hg), but the other systematic
reviews found no significant effect. None of the more recent primary studies were in people
exclusively with hypertension.
Four of the systematic reviews performed meta-analyses of all people regardless of
hypertension diagnosis. Except for the oldest, highly selective systematic review, they found
significant effects on systolic blood pressure (ranging from -1.9 to - 0.9 mm Hg). The summary
estimates of the effect on diastolic blood pressure ranged from -1.0 to +0.03 mm Hg, which were
mostly nonsignificant. The individual, recent primary studies of mixed populations (in terms of
hypertension) found larger, though statistically nonsignificant, effects.
The systematic reviews that evaluated factors including age, sex, calcium dose, background
dietary calcium, supplement versus dietary source, and other factors found no significant
associations (or differences). The five additional primary studies did not provide further insights
into these subgroup analyses.
Detailed presentation (Tables 82, 83, & 84).
The six systematic reviews explicitly or implicitll used generally different eligibility criteria,
resulting in large overlaps in the trials included.
169
18
"
193
The systematic reviews included a total
of 64 trials. The largest systematic review
189
included trials up to 1997 and was an update of a
previous review
191
that reported more analyses. The next largest systematic review
190
was one of
the more recent systematic reviews (including trials through 2003). The most recent systematic
review
169
was restricted to trials of people with hypertension. Five more recent trials, not
included in any ofthe systematic reviews were found.
120
194
-
197
Two of the trials were restricted
to normotensive individuals; none included only people with hypertension.
241
Normotensive individuals.
The systematic reviews by Bucher et al. (1996)
191
and Allender et al. (1996)
192
evaluated
trials of normotensive individuals. The range of intervention calcium doses were approximately
400 to 2000 mg/d, with most studies using 1000 to 1500 mg/d. Both found no significant effect
of calcium supplementation on blood pressure (net effect on systolic blood pressure of -0.27 and
-0.53 mm Hg, respectively, and on diastolic blood pressure of -0.33 and -0.28 mm Hg,
respectively). The two additional, more recent primary studies of normotensive participants were
consistent with this finding. The TOHP trial compared calcium supplement to placebo in people
without hypertension but high normal diastolic blood pressure (80-89 mm Hg) and found a
nonsignificant net change in blood pressure of approximately -0.5/+0.35 nun Hg
(systolic/diastolic) after 18 months.
195
Lijnen 1995 also compared calcium supplement to
placebo, but in men who had been put on a low calcium run-in diet, and found a nonsignificant
net change in blood pressure of approximately -2/-1 mm Hg after 4 months.
197
Both trials had
methodological quality C due to inadequate reporting of this outcome or of the background
calcium intakes of the participants. Bucher et al. (1996) reported a wide range of study quality;
Allender et al. (1996) did not evaluate study quality.
Findings per calcium intake level.
Neither systematic review performed subgroup analyses of the normotensive individuals to
evaluate a dose (calcium intake) effect. Qualitative examination of the data provided in the
systematic review tables and the two additional trials did not indicate any dose effect.
Findings per age and sex.
Neither systematic review performed subgroup analyses of the nonnotensive individuals to
evaluate age or sex. The trials in the Allender et al. ( 1996) systematic review and the two
additional trials represented a wide range of ages, though apparently all participants were under
age 70 years. Studies were of all men, all women, and both sexes. There were no apparent
differences based on age or sex.
Hypertensive indi vicluals.
Four systematic reviews evaluated trials of hypertensive individuals (Bucher et al. 1996
191
,
Allender et al. 1996
192
, Cappuccio et al. 1989
193
, and Dickinson 2006
198
). Dickinson et al. (2006)
included only studies of people with hypertension. The range of supplemental calcium was
approximately 400 to 2000 mg/d in most systematic reviews, with most studies using 1000 to
1500 mg/d. The systematic reviews generally found significant effects on systolic blood pressure
of about -2 to -4 mm Hg, but no (or small) effects on diastolic blood pressure. The one
systematic review that found no effect of calcium supplementation on systolic blood pressure
(Cappuccio et al. 1989) was the oldest systematic review (including trials up to only 1988). In
addition, the reviewers were highly selective in their eligibility criteria, having excluded trials
that did not report various types of baseline data. The one systematic review that found a
significant effect of calcium supplementation on diastolic blood pressure (Bucher et al. 1996)
meta-analyzed only 6 trial subgroups of people with hypertension, compared to 10 to 16 trials in
the other systematic reviews. None of the more recent trials provided analyses in only people
with hypertension.
242
Findings per calcium intake level.
Only Dickinson et al. (2006), the systematic review of only trials of people with
hypertension, evaluated calcium intake (or dose) as a predictor of effect. They found essentially
the same overall effects on systolic and diastolic blood pressures in studies that used less than
1200 mg/d or 1200 to 2000 mg/d of calcium. Qualitative examination of the data provided in the
tables of the remaining systematic reviews did not indicate any dose effect.
Findings per age and sex.
No systematic review evaluated the association between age or sex and treatment effect in
trials of people with hypertension. Overall, the range of ages of participants was about 20 to 75
years. Studies were of all men, all women, and both sexes. There were no apparent differences
based on age or sex.
All trials (combined normotensive and hypertensive individuals).
Five systematic reviews (including one which is an update of a second) combined trials of
hypertensive, normotensive, or mixed groups of o ~ l (Griffith et al. 1999
189
, van Mierlo et al.
2006
190
, Bucher et al. 1996
191
, Allender et al. 1996
19
, and Cappuccio et al. 1989
193
) . The range
of calcium supplementation was approximately 400 to 2000 mg/d in most systematic reviews,
with most studies using 1000 to 1500 mg/d. The systematic reviews generally found a significant
effect of calcium supplementation on systolic blood pressure of -0.9 to -1.9 mm Hg (excluding
the earliest, highly selective systematic review by Cappuccio et al. ( 1989)
193
, as discussed
above). The two systematic reviews that included the most studies (Griffith et al. 1999
189
and van
Mierlo et al. 2006
190
) found a significant effect on diastolic blood pressure (-0.8 and -1.0 mm Hg,
respectively). The smaller, older systematic reviews found no significant effect (Allender et al.
1996
192
and Cappuccio et al. 1989
193
) . The reason for the difference in conclusions of the
systematic reviews may relate to greater statistical power in the more recent meta-analyses or
differences in study eligibility criteria. The systematic reviews that reported on study
heterogeneity found significant heterogeneity. Three of the systematic reviews reported data on
subgroup or regression analyses to explain the heterogeneity. The only factor that explained a
significant amount of the heterogeneity was the difference in effect between studies of people
with or without hypertension. (The age, sex, and calcium dose analyses are described below.)
Two recent randomized trials included postmenopausal women (over 50 or 55 years)
regardless of their blood pressure;
120
194
a third trial enrolled pregnant women and evaluated
long-term postpartum blood pressures.
196
The trials each compared different interventions:
calcium citrate 1000 mg versus placebo; dairy product intake (with a mean of 1242 mg/d
calcium) versus nondairy product intake (377 mg/d calcium); and calcium carbonate 2000 mg/d
versus placebo in women all taking prenatal vitamins that included 400 IU/d vitamin D
2
The
calcium citrate trial was of methodological quality B; the other two trials C. The recent trials
found broadly similar conclusions to that of the systematic reviews, with women with greater
calcium intake having lower systolic blood pressme (-2.2 to -5.4 mm Hg) and smaller decreases
in diastolic blood pressure (-0.7 to -2.2 mm Hg); though none of the effects was statistically
significant.
Findings per calcium intake.
Three systematic reviews
190
-
192
evaluated calcium dose (or intake) as a source of
heterogeneity. None found a significant association. Specifically, van Mierlo et al. (2006) found
similar (though smaller) effects in studies of over 1000 mg/d of calcium (SBP/DBP -1 .75/-0.56)
compared to studies of 1000 mg/d of calcium or less ( -2.17/-1.41 ).
243
Findings per age and sex.
Age and sex were evaluated as potential explanations of heterogeneity in two systematic
reviews.
190
,
192
Neither found that age or sex were significantly associated with the effect of
calcium on blood pressure. However, these analyses are subject to ecological fallacy, as they
used the mean ages and the percent of study participants who were male as proxies for the effects
of calcium intake in people of a particular age or sex. Most studies included participants under
age 70 years. Studies were of all men, all women, and both sexes.
Findings by ~ f stage.
0-6 mo Not reviewed
7 mo- 2 y Not reviewed
3 - 8 y Not reviewed
9-18 y Not reviewed
19- 50 y The majority of studies are applicable to people within this life stage;
though people under approximately 40 years are less well represented. The evidence
suggests no significant effect of calciwn supplementation on blood pressure in
normotensive individuals. In people with hypertension, the evidence suggests that
calcium supplementation lowers systolic blood pressure by about -2 to -4 mm Hg, but
does not change diastolic blood pressure. The effect appears to be consistent across
calcium supplement doses (specifically above or below 1200 mg/d).
51 - 70 y The majority of studies are applicable to people within this life stage. The
conclusions are the same as for those in the 19-50 years life stage.
?:71 y The evidence is scant for this life stage. Few of the studies appear to have
included people over age 70 years.
Postmenopause Our review of the evidence does not allow for a definitive
conclusion for this life stage. None of the systematic reviews evaluated menopausal
status as an explanatory variable for heterogeneity.
Pregnant & lactating women Not reviewed
244
Table 82. Summary of systematic reviews of calcium and blood pressure
Author Year [PMID] Griffith 1999
1
BY [10075392)
Design (Search Years) Randomized controlled trials (1966-1997)
Population Both hypertensive and normotensive partici pants
Intervention and Comparator Dietary and nondietary calcium supplementation versus placebo (no supplement)
Dose range 600-2000 mg (36% 1000 mg; 26% 1500-1 600 mg; 12% 2000 mg)
Results 42 trials
SBP: -1.44 (2.20, 0.68t; statistically heterogeneous
DBP: -0.84 ( 1.44, -0.24); statistically heterogeneous
Subgroup analyses did not find that heterogeneity could be explained by age, sex, baseline
calcium, dietary versus nondietary calcium, or quality.
Subgroups with hypertensive versus normotensive people were significantly different (no
further details).
Conclusions similar to previous systematic review (Bucher 1996
191
)
Comments Update of Bucher 1996
191
(see below).
AMSTAR
A priori design? Study quality assessment performed? Yes
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
Yes
Yes
Yes
Study quality appropriately used in analysis? No
Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Publication bias assessed? No
Conflicts of interest stated? No
Study characteristics provided?
Author Year [PMID]
Design (Search Years)
Population
Intervention and Comparator
Results
Comments
A priori design?
Study quality not discussed in conclusions. Funding
source reported, but not conflict of interest.
van Mierlo 2006
100
(16673011)
Randomized controlled trials (1966-2003)
Both hypertensive and normotensive participants
Calcium supplementation versus placebo (no supplement)
Dose range 355-2000 mg (40% 1000 mg; 32%1500-1600 mg; 6%2000 mg)
40 trials
SBP: -1.86 (95% Cl -2.91, -0.81 ); statistically heterogeneous
DBP: -0.99 (95% Cl -1.61, -0.37); statistically heterogeneous
In multivariable analysis including age, sex, initi al calcium intake, calcium dose, and initial
blood pressure:
SBP DBP
Age <45 y -1.45 (-2.99, +0.09) -1.26 (-2.20, -0.33)
2:45 y -2.33 (-3.69, -0.96) -0.80 (-1.62, +0.02)
Male S50% -2.20 ( -3.68, -0. 72) -1.12 ( -1 .98, -0.26)
>50% -1.77 (-3.13, -0.42) -0.84 (-1 .65, -0.04)
Initial BP <140/90 mm Hg -2.04 (-3.40, -0.68) -1.04 (-1.86, -0.22)
2:140/90 mm Hg -1.85 (-3.45, -0.32) -0.89 (-1.79, +0.01)
Ca dose S1000 mg -2.17 (-3.59, -0.75) -1.41 (-2.24, -0.59)
>1000 mg -1.75 (-3.20, -0.31) -0.56 ( 1.40, +0.29)
Blood pressures not statistically signifi cantly different between any strata.
AMSTAR
Study quality assessment performed? Yes
Two Independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
Unclear
Partial
Yes
Study quality appropriately used In analysis? No
Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
245
Publication bias assessed? Yes
Conflicts of interest stated? Yes
No data on inclusion of unpublished data. Excluded
studies available from authors
Table 82. continued
Author Year [PMID]
Design (Search Years)
Population
Intervention and Comparator
Results
Comments
A priori design?
Bucher1996 [8596234]
Randomized controlled trials (1966 1994)
Both hypertensive and normotensive participants
Dietary and nondietary calcium supplementation vs. placebo (no supplement)
Dose range 4062000 mg (41% 1000 mg; 31% 15001 600 mg; 8%2000 mg)
33trials
[Overall summary results were updated in Griffith 1999
189
, above]
Studies with specifi ed subgroups of hypertensive and normotensive participants (6trials}:
Hypertensives SBP 4.30 (6.47, 2. 13) DBP 1.50 (2.77, 0.23)
Normotensives SBP -0.27 (1.80, + 1.27) DBP -0.33 (1 .56, +0.90)
Regression analyses:
BP (continuous scale) SBP OR= 0.99 (0.96, 1.01} DBP OR= 0.99 (0.96, 1.03)
Dose of calcium, duration of supplementation, dietary vs. nondietary calcium supplementation,
methodological quality did not demonstrate a relationship with the magnitude of treatment effect.
Updated in Griffith 1999
189
(see above)
AMSTAR
Study quality assessment performed?
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
Yes
Yes
Yes
Study quality appropriately used in analysis?
Appropriate statistical synthesis?
Publication bias assessed?
Yes
Yes
Yes
No
No
All publication types and languages included?
Included and excluded studies listed? Conflicts of interest stated?
Study characteristics provided?
Author Year [PMID]
Design (Search Years)
Population
Intervention and Comparator
Results
Comments
A priori design?
Funding source reported, but not conflict of interest.
Allender 1996
192
[861 0952]
Randomized controlled trials (1982 1993)
Both hypertensive and normotensive participants
Dietary and nondietary calcium supplementation vs. placebo (no supplement)
Dose range 4002160 mg (35% 1000 mg; 29% 15001600 mg; 10% 2000 mg}
26 trials (22 trials included in meta-analyses}
SBP: 0.89 ( 1.74, 0.05)
DBP: 0. 18 (0.75, +0.40)
Hypertensives SBP 1.68 (3.18, 0. 18) DBP +0.02 (0.96, +1.00}
Normotensives SBP 0.53 (1.56, +0.49) DBP 0.28 (0.99, +0.42)
By weighted linear regression analyses, age, sex, calcium dose, trial duration were not
associated with treatment effect (P>0.1 0}
AMSTAR
Study quality assessment performed? No
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
Yes
No
Yes
Study quality appropriately used in analysis? No
Appropriate statistical synthesis? No
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
Author Year [PMID] Cappuccio 1989 [2697729]
Publication bias assessed? No
Conflicts of interest stated? No
Excluded studies not enumerated or listed. Fixed effects
models used.
Design (Search Years) Randomized controlled trials (1983 1988)
Population
Intervention and Comparator
Results
Comments
A priori design?
Both hypertensive and normotensive participants
Nondietary calcium supplementation versus placebo (no supplement) or low calcium intake
Dose range 800 1600 mg (60% 1 000 mg; 27% 15001600 mg)
15 trials
SBP (supine}: 0. 13 ( 0.46, +0.19)
DBP (supine): +0.03 (0.17, +0.22)
Hypertensives SBP +0.06 (0.59, +0.72} DBP +0.03 ( 0.21, +0.27}
AMSTAR
Study quality assessment performed? No
Two independent reviewers?
Comprehensive literature search?
Yes
nd
Yes
nd
No
Yes
Study quality appropriately used in analysis? NA
Appropriate statistical synthesis? No
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
246
Publication bias assessed? No
Conflicts of interest stated? No
Excluded studies not enumerated or listed. Fixed effects
models used.
Table 82. continued
Author Year [PMID]
Design (Search Years)
Population
Intervention and Comparator
Results
Comments
Dickinson 20061 [16625609)B
Randomized controlled trials (1982-2003/ 2005c)
Hypertensive participants
Dietary and nondietary calcium supplementation versus placebo (no supplement)
Dose range 400-2000 mg (50% 1000 mg; 25% 1500-1600 mg; 6% 2000 mg)
13 trials
SBP: -2.53 (4.45, -0.60); statistically heterogeneous
DBP: 0.81 (2.07, +0.44) ; statistically heterogeneous
Ca dose <1200 mg SBP 2.67 (5.15, -0.18)
Ca dose 1200-2000 mg SBP -2.69 (-5.86, +0.47)
Not statistically significantly different by calcium dose
AMSTAR
DBP -0.75 (2.13, +0.63)
DBP -0.78 (-3.82, +2.25)
A priori design? Yes Study quality assessment performed? Yes
Two independent reviewers? Yes Study quality appropriately used in analysis? Yes
Comprehensive literature search? Yes Appropriate statistical synthesis? Yes
All publication types and languages included? Yes Publication bias assessed? Yes
Included and excluded studies listed? Yes Conflicts of interest stated? Yes
Study characteristics provided? Yes
A Numbers in parentheses are 95% confidence intervals
8
A technical update, with no further studies added was published in the Cochrane database in 2008.
c Different dates for different databases.
247
Table 83. Calcium and blood ~ r e s s u r e Characteristics of ACTs
Author Year Background
Study Name Calcium
Location Population Intake & Comparisons Compliance Comments
(Latitude) Vitamin D
[PMI D] Data
Whelton 1997 Health No HTN (DBP nd Calcium nd
TOHP status 80-89 mm Hg) supplement vs.
us
Mean age 43 (30-54) Placebo
(various) (range), y
[9022561]
Male(%) 68
Lijnen 1995 Health Normotensive "Low calcium Calcium nd With low
Leuven, Belgium status diet" run-in supplement vs. dairy intake
(5FN)
Mean age 24 (20-44) Placebo
[8557965]
(range), y
Male(%) 100
Reid 2005 Health Healthy Ca 857 mg/ day Calcium Calcium group:
Auckland, New status supplement vs. 55%, Placebo
Zealand Mean age 75 (2:55) Placebo group: 58%
(36.5S) (range), y
[15827103]
Male(%) 0
Ghadirian 1995
120
Health Healthy Ca 776 mg/ day Dairy vs. Dairy-free Non-compliant and
Montreal, Canada status intake those who
(46N)
Mean age -80 (2:50) provided
[7493659] (range), y incomplete data
Male(%) 0
were excluded.
Hatton 2003 Health Pregnant nd Calcium nd (but all had to Oregon site
CPEP status during trial supplement vs. meet a compliance only. Post-
Portland, Oregon
Mean age nd
Placebo (both on test prior to pregnancy
(45.SON)
(range/SO),
prenatal vitamins randomization) followup
[1 4553957]
y
including Vit 0
2
Male(%) 0
400 IU)
248
Table 84. Calcium and blood Results of RCTs
Author Year
Age
Mean
Study Name
Range,
Outcome
10/20
Followup,
Interventions, No.
Unit Baseline Change
Change
Net Diff
Net Diff
p
Study
[PMID]
Sex;
unit
Daily Dose Analyzed 95%CI 95%CI Btw Quality
Po ulation
SYSTOLIC BLOOD PRESSURE
Normotensive
Whelton
30-54 y, Ca carbonate
221
mm
126.0 nd nd - -Q.5A --2, -1 NS
199i
95 Both; 1000 mg __ljg __
------------- -----------
TOHP
No HTN SBP
10
18 mo c
[9022561)
(DBP 80- Placebo 224 125.4 nd nd
89mmH
Lijnen 1995
197
Ca gluconate
mm
-4A 20-44 y,
SBP,
2000 mg (low 16
Hg
114 nd - -2 nd NS
Belgium Men
supine
20
4 mo dairy intake)
-------------------------
c
[8557965) No HTN Placebo (low
16 114 --2 nd
dair intake)
All women
Reid 2005 <::55 y, Ca citrate
732
mm
134.9 0.0 -0.1 , 0.1 -2.4 -0.8, 5.6 0.14
New Zealand Women; SBP
20
30 mo 1000 mg _ljg __ B
[1 5827103] AIIBP Placebo 739 133.9 +2.4
Ghadirian
<::50 y, 81
mm
140.34 2.69 -7.3, 2.0* -5.4 -12.3, 1.4c NS
1995
120
Women; SBP
20
1 mo
.. H.g_-
c
Canada
All BP 77 131.71 +2.75 -2.3, 7.8*
[7493659)
Ca carbonate
mm Final Difference
Hatton 2003
196
Pregnant,
2 y post-
2000 mg (+Vit 37
Hg
nd
101 .9 -2.2 -7.8, 3.4c
NS
CPEP Women
8
; SBP
20
D2 400 IU) c
[14553957) All BP
partum
Placebo (+Vit
D2 400 IU
25 nd 104.1
DIASTOLIC BLOOD PRESSURE
Normotensive
Whelton
30-54 y, Ca carbonate
221
mm
84.1 nd nd - +0.35A
- -1' 1 NS
1997
195 Both; 1000 mg Hg.
------------
TOHP
No HTN DBP
10
18 mo c
[9022561]
(DBP 80 Placebo 224 83.9 nd nd
89mmH
Lij nen 1995
197
Ca gluconate
mm
- -1A 20-44 y,
DBP,
2000 mg (low 16
Hg
74 nd - - 1 nd NS
Belgium Men
supine
20
4mo dair:t intake)
------------
c
[8557965] No HTN Placebo {low
16 72 -o nd
dair intake
All women
Reid 2005 C::55 y, Ca citrate
732
mm
70.1 -0. 2 -0.2, -0.2 -1 .0 -2.3, 0.3 0.13
New Zealand Women; DBP
20
30 mo 1000 mg
.. H.g_-
B
[ 15827103] All BP Placebo 739 69.6 +0.8 0.8, 0.8
continued
249
Author Year
Study Name
[PMID]
Ghad1nan
1995
120
Canada
[7493659)
Hatton 2003
196
CPEP
[1 4553957)
Age
Range,
Sex;
Population
y,
Women;
AIIBP
Pregnant,
Women
8
;
AIIBP
Outcome
10/20
DBP
20
DBP
20
A From figure
8
Blood pressure outcomes are 1 year post-partum
c Estimated from available data
Mean
Followup,
unit
1 mo
2 y post-
partum
Interventions,
Daily Dose
No.
Analyzed
Unit
81 mm
Ca carbonate
2000 mg ( + Vit
D2 400 IU)
Placebo (+Vit
D2 400 IU)
77
37
25
250
mm
Hg
Baseline Change
81.17 -7.78
Change
95% CI
-1 0.0, -5.5*
Net Diff
-2.2
Net Diff
95%CI
-5.4, 1.0c
p
Btw
NS
79.09 -5.59 -7.9, -3.3.
nd
Final Difference
67.1 -0.7 -4.8, 3.4
NS
nd
Study
Quality
c
c
Combined Vitamin D and Calcium and Health Outcomes
Women 's Health Initiative (WHI) trial.
The WHI trial provided data for numerous health outcomes of interest. For this reason and
because of some methodological issues unique to this trial, the study is discussed here. The trial
compared combined vitamin D3 400 IU and calcium carbonate 1000 mg daily versus placebo in a
7 year trial in 36,282 postmenopausal women (age 50-79 y). The Tufts EPC, members of the
Technical Expert Panel, and reviewers of the draft report debated about the quality of this trial. It
was generally agreed that the overall methodological rigor and analyses were of good quality for
most outcomes. However, there was not complete consensus on how to regard the fact that the
women in both groups of this 7 year trial were allowed to take additional vitamin D supplements
up to 600 IU and later I 000 IU per day and calcium supplements up to I 000 mg per day. At
baseline, about one-third of women in both supplement and placebo groups were taking vitamin
D supplements of at least 400 IU/d and 29 percent were taking at least 500 mg/d of supplemental
calcium; by the end of the trial 69 percent of women were taking any additional supplemental
calcium. During the 7 years, only about 60 percent of women (in any given year) were taking at
least 80 percent of the study pills; at the end of the trial, only 76 percent were still taking any
study medications. Regarding the overall quality of the study, arguments were put forward that
this was a high quality effectiveness trial (in contrast with a more standardized efficacy trial) and
thus had increased relevance to the actual use of supplements, that the crossover of interventions
affects the applicability more than the methodological quality, and that the trial should not be
downgraded because data reporting was more complete than for most trials. However, it was the
consensus among the Tufts EPC that overall, the methodological quality of the trial was B,
particularly when the trial is being used to guide decisions about DRI, as opposed to decisions
about whether to actively recommend supplementation for an individual woman.
Combined Vitamin D Calcium and Growth
We reviewed primary studies that evaluated relationships between vitamin D and growth
parameters in infants and children.
Synopsis.
One C-rated nonrandomized study compared combined vitamin D (1200 IU/d) and calcium
(375 mg/d) to no supplementation in women in their third trimester of pregnancy. Infants of
women who received supplementation were significantly heavier at birth.
Detailed presentation (Tables 4 & 6).
Infant 0 - 6 months; 7 months - 2 years; pregnant or lactating women.
We identified a study from India that included a nonrandomized comparison between
combined vitamin D (1200 IU/d) and calcium (375 mg/d) for the expectant mothers versus no
supplementation. The outcome was infant birth weight.
41
This study has already been described
in the "Vitamin D and growth" section, as it also included a vitamin D only intervention arm.
The study included expectant mothers with daily milk intake less than 500 mL and estimated
daily vitamin D intake less than 30 IU. It was rated C for methodological quality, because of the
lack of randomization and incomplete reporting of analyses. According to the reported analysis,
251
infants of women who received supplementation were significantly heavier at birth by 160 g on
average (95 percent CI 0, 320).
Findings by life stage
0 - 6 mo One C-rated nonrandomized study from India compared combined vitamin
D (1200 IU/d) and calcium (375 mg/d) to no supplementation in women in their third
trimester of pregnancy. Infants of women who received supplementation were
significantly heavier at birth by 160 g on average (95 percent CI 0, 320). (See also the
Pregnant & lactating women.)
7 mo- 2 y No identified study covered this life stage.
3 - 8 y No identified study covered this life stage.
9- 18 y No identified study covered this life stage.
19 -50 y Not reviewed
51 - 70 y Not reviewed
~ 7 y Not reviewed
Postmenopause Not reviewed
Pregnant & lactating women One C-rated nonrandomized study from India
compared combined vitamin D (1200 IU/d) and calcium (375 mg/d) to no
supplementation in women in their third trimester of pregnancy. Infants of women who
received supplementation were significantly heavier at birth by 160 g on average (95
percent CI 0, 320). (See also the 0-6 mo category.)
252
Combined Vitamin D and Calcium and Cardiovascular Disease
Synopsis.
No qualified systematic reviews evaluated the association between combined vitamin D and
calcium, body stores, or serum concentrations, and cardiovascular events. A variety of
cardiovascular events after 7 years were evaluated in the Women's Health Initiative (WHI) trial
of combined daily vitamin D3 400 IU and calcium carbonate 1000 mg versus placebo in 50 to 79
year old women. No statistically significant effect was found with combined vitamin D and
calcium supplementation on any cardiovascular outcome. However, near significant associations
were found for three outcomes, suggesting increased risk with supplementation for a composite
cardiac outcome that included invasive cardiac interventions, invasive cardiac interventions, and
transient ischemic attacks. No significant associations were found for cardiovascular death, a
composite cardiac outcome (myocardial infarction or cardiac death), coronary heart disease
death, myocardial infarction, hospitalization for heart failure, angina, combined stroke or
transient ischemic attack, stroke alone, or cerebrovascular death.
Detailedpresentation (Tables 85 & 86).
In the WHI trial, discussed above, the evaluated cardiovascular outcomes were all
prespecified secondary outcomes.
199
'
200
On average, the women had normal blood pressure.
There were no significant effects of the supplementation on any of the outcomes, though three of
the outcomes did approach statistical significance suggesting increased events with
supplementation: composite cardiac events (HR = 1.08 [95 percent CI 0.99, 1.19]), coronary
artery bypass grafting or percutaneous coronary interventions (HR=l.09 [95 percent CI 0.98,
1.22]), and transient ischemic attacks (HR=l.l6 [95 percent CI 0.95, 1.42]). The authors,
however, concluded that calcium and vitamin D supplementation neither increased nor decreased
coronary or cerebrovascular risk in generally healthy postmenopausal women. The outcomes
cardiac death and stroke were evaluated by age decade. No interaction was found with age (no
significant difference across age groups). A similar analysis based on total calcium intake
(dietary plus supplemental) also found no interaction.
Findings per intake level.
No conclusions are possible about a dose effect from this single study, especially since the
women were allowed to take additional concurrent calcium and vitamin D supplements.
However, no interaction was found with total reported calcium intake.
Findings by age and sex.
The study investigated postmenopausal women 50 to 79 years old. No interaction of effects
with decade of age was found.
Findings by l ~ f stage.
0 - 6 mo Not reviewed
7mo - 2y Not reviewed
3 - Sy Not reviewed
9-18 y Not reviewed
19 - 50 y No data available
253
51 - 70 y One large trial that included women mostly within this life stage (WHI)
found no significant effect of combined vitamin D3 ( 400 IU) and calcium carbonate
(I 000 mg) on cardiovascular outcomes after 7 years.
:::::71 y Inadequate available data.
Postmenopause All women in the WHI trial were postmenopausal. See 51-71 y life
stage.
Pregnant & lactating women Not reviewed
Table 85. Combined vitamin D and calcium and cardiovascular outcomes: Characteristics of
RCTs
Author Year
Study Name
Location
(Latitude)
[PMID]
Hsia 2007
199
LaCroix 2009
200
WHI
us
(various)
[ 17309935
19221190]
Population
Health Any
status
Mean age 62
(range), y (50-79)
Male (%) 0
Background Calcium
Intake & Vitami n D Data
Ca: 1148 (654) mg/d in
treatment group; 1154 (658)
in placebo group
Low Ca intake (<800
mg/ day): 34%
254
Comparisons Compliance Comments
Combined Vit D & Ca See page
supplement vs. 242
Placebo
Table 86. Combined vi tamin D and calcium and cardiovascular outcomes: Results of RCTs
Author Year
Life Mean Interventions, Daily n N Outcome Metric
p
Study
Study Name Outcome 1/2 Result 95% CI
[PMID]
Stage Followup, y Dose Event Total (Comparison) Btw Quality
Hsia 2007
1
50-79 y,
Cardiovascular
7
Vit D + Ca 226 18,176
HR
0.92* 0.77, 1.10 NS
B
LaCroix 2009
200
Women
2
_
WHI
death
Placebo 244 18,106
[17309935 Cardiac composite Vit 03 400 IU + Ca
920 18,176 HR 1.08 0.99, 1.19 0.10
19221190] (MI, CHD death,
20
1QQ() 1119
CABG, or PCI) Placebo 841 18,106
------!
Cardiac composite
20
.....Y.it.Q .... .. ..............................-i99 __ 7f}
HR 1.04 0.92, 1.18 0.50
(MI or CHD death) Placebo 475 18,106
CHD death
20
Vit D + Ca 130 18,1 76 HR 1.01* 0.79, 1.29 0.92
F>iacebo
................................................................. ....................................
------1
128 18,106
Ml
20
Vit D + Ca 411 18,176 HR 1.05 0.91, 1.20 0.52
......F>.iace'b'o ....................................................
. ....................................................................... ...................................
390 18,106
CABG or PCI 2
Vit D + Ca 674 18,176 HR 1.09 0.98, 1.22 0.12
F>iace'bo
.....----------------
607 18,106
Hospitalized for
20
Vit D + Ca 394 18,176 HR 0.95 0.83, 1.10 0.50
..................................................
----------------
. .................................
heart failure Placebo 407 18,106
Angina
20
Vii D + Ca 404 18,176 HR 1.08 0.94, 1.24 0.30
F>iacebo
- ...
.................................
377 18,106
Cerebrovascular Vit D + Ca 563 18,176 HR 1.02 0.91, 1.15 0.75
composite
20
..................................................
. ....-----------------
...................................
------, (Stroke or TIA)
Placebo 547 18,106
Stroke
20
Vit D + Ca 362 18 176 HR 0.95 0.82 1.10 0.51
..... f'Iacei:lo ........................................
377 18,106
TIA 2
Vit D + Ca 213 18,176 HR 1.16 0.95, 1.42 0.13
..................................................
---------------
.. ................................
--------]
Placebo 182 18,106
Cerebrovascular
20
Vii D + Ca 213 18,176 HR 0.89* 0.62, 1.29 NS
death
......p;a:c;e;i:lo ....................................................
......................................................................... ....................................
182 18,106
255
Combined Vitamin D and Calcium and Body Weight
We searched for systematic reviews and primary studies that evaluated associations between
combined vitamin D and calcium and incidence of overweight or obesity; no such studies were
found. For the outcome weight change (in kilograms or body mass index units), we included
only randomized controlled trials. The EPC and the TEP agreed that the limited resources would
not be expended on reviewing observational studies for the surrogate outcome body weight
(where overweight or obesity are considered to be the clinical outcomes). We included only
studies of adults. Studies of weight gain in children are included in the "Growth" section.
Synopsis.
No qualified systematic reviews evaluated the association between combined vitamin D and
calcium, body stores, or serum concentrations, and body weight in adults. One RCT each tested
the effect of combined vitamin D and calcium in the setting of either an isocaloric diet or an
energy restricted diet. Both used vitamin D
2
400 IU/d and calcium carbonate (one 1000 mg/d,
one 1200 mg/d) and were restricted to women. In the WHI trial of postmenopausal women on an
isocaloric diet after 7 years, there was a statistically significant 0.1 kg smaller weight gain in
those assigned to the supplement. The effect was statistically similar across age groups. In a
Quebec study of 63 overweight premenopausal women, the apparent effect of supplementation in
the setting of an energy restricted diet was greater than the WHI trial (net change -1.0 kg), but
this was not a significant difference between the supplement and placebo groups.
Detailed presentation (Tables 87 & 88).
lsocaloric diet.
The WID trial was analyzed for the effect of daily combined vitamin D2 400 IU and calcium
carbonate 1000 mg on weight.
201
The trial included about 36,000 postmenopausal women aged
50 to 79 years. The methodological quality of the study was B. At 7 year followup, the net
change in body weight (supplemented minus control) was -0.13 kg (95 percent CI -0.21, -0.05;
less weight gained in supplement group). This was of questionable clinical significance, but was
statistically significant. The investigators performed numerous subgroup analyses including
those based on age. There were no substantive or statistically significant differences among the
evaluated age subgroups.
Energy restricted diet.
A trial performed in Quebec City analyzed 63 premenopausal overweight or obese women
(mean age 43) comparing daily vitamin D
2
400 IU and calcium carbonate 1200 mg versus
placebo.
202
Women in both study groups were placed on a weight-loss intervention which
consisted of a 700 Kcal!day decrease in energy intake for 15 weeks; the women met biweekly
with a nutritionist. The trial was rated methodological quality C due to a high drop out rate (25
percent) and poor description of the methodology. Women in both study groups on average lost
weight, with those in the supplement group losing 1.0 kg more ( 4 vs. 3 kg). However, this effect
was not statistically significant (P=0.19).
Findings per vitamin D and calcium dose.
No conclusion could be reached about a possible effect of vitamin D and calcium dose.
256
Findings per age and sex.
The trials included only women. The effect of supplementation on postmenopausal women
not on an energy restricted diet was of questionable clinical significance after 7 years. The effect
of supplementation for 15 weeks on overweight and obese premenopausal women (in an
approximate age range of32 to 54 years) on an energy restricted diet was relatively large (-4 vs.
-3 kg), but this difference between the supplemented and control groups was not statistically
significant.
Findings by ~ f e stage.
0-6 mo Not reviewed
7 mo - 2 y Not reviewed
3 - 8 y Not reviewed
9 - 18 y Not reviewed
19 - 50 y A single trial of women on an energy restricted diet found a nonsignificant
difference in weight loss between that those assigned to vitamin D 300 IU and calcium
1200 mg supplementation for 15 weeks.
51 - 70 y The WHI trial found no clinically significant effect on weight of vitamin
D 300 lU and calcium 1000 mg after 7 years.
~ 7 y The subgroup of women in the WHI trial in this life stage had a similar net
weight change as all the study participants as a whole, but the effect was not statistically
significant.
Postmenopause All the women in the WHI trial were postmenopausal.
Pregnant & lactating women Not reviewed
Table 87. Combined vitamin D and calcium and weight: Characteri stics of RCTs
Author Year
Study Name
Location
(Lati tude)
[ PMID]
Caan 2007
261
WHI
us
(various)
[17502530)
Major 2007
202
Quebec City,
Canada
(4JON)
[17209177)
Populati on
Health All, post
status menopause
Mean age 62 (50-79)
(range), y
Male(%) 0
Health Overweight,
status healthy, pre-
menopause
Mean age 43 (5.5)
(range/SO). y
Male(%) 0
Background
Calcium Intake & Comparisons Compliance
Vitamin D Data
Ca: 1148 (654) mg/d Vit 0 & Ca See page
in treatment group; carbonate vs. 242
1154 (658) in placebo Placebo
group
Ca 704 mg/d Vii 0 + Ca nd
carbonate vs.
Placebo
257
Comments
Factorial
design with HT
vs. Placebo
Energy
restriction
Table 88. Combined vitamin D and calcium and weight: Results of ACTs
Author Year
Age
Study Name
Range,
Outcome 1/2
Mean Interventions, No.
Unit Baseline Change
Change Net Net Diff
PBtw
Study
Sex Follow up Daily Dose Analyzed 95% CI Diff 95% CI Quality
[PMID]
(Sub )
lsocaloric
Diet
Caan 2007
201
50-79 y,
Vit D2 400 IU +
Ca carbonate 18,129 kg 76.0 nd nd -0.13 -0.21' -0.05 .001A
WHI
Women
Weight 2 7y
_j OOO mg
B
(1 7502530)
Placebo 18,055 75.9 nd nd
(50-54 y)
Vit 0
3
+ Ca 2592 kg nd nd <0.05
Placebo 2561 nd nd
(55-59 y)
Vit 03 + Ca 4134 kg nd nd -0.24, +0.09 NS
Placebo 4135 nd nd
(60-69 y)
Vit 03 + Ca 8276 kg nd nd
Placebo 8243 ----rid nd
(70-79 y)
_ Vit 0
3
+Ca 3174 kg nd nd -0.27, +0.09 NS
Placebo 2561 nd nd
(White)
Vit 03 + Ca 15,047 kg nd nd -0.22, -0.04 <0.05
Placebo 15,106 nd nd
(Black)
Vit 0
3
+ Ca 1682 kg nd nd -0.59 -0.06
Placebo 1635 nd nd
(Hispanic)
Vit 03 + Ca 789 kg nd nd -0.08 -0.48, ;t-0.32 NS
Placebo 718 nd nd
J
-
'
(Asian I Vit 03 + Ca 369 kg nd nd +0. 19
Pacific
Placebo 353 nd nd
r
Islander
Energy
Restricted
Di et
Major 2007 Vit 02 400 IU +
Quebec City,
43 (SO)
Weight
20
15 wk
Ca carbonate 30 kg 81.5 -4.0 +-9.0 -1.0 -2.31. +0.31 0.19
c
Canada ____goo mg
(1 7209177) Placebo 33 83.6 -3.0 +-1 1.7
A In addition, subgroup analyses by baselinEi"'BMMand baseline dietary calcium intake are r p o r t ~
8
No statistically significant interaction with age.
c No statistically significant interaction with ethnicity.
258
Combined Vitamin D and Calcium and Cancer
Cancer from all causes and total cancer mortality.
Synopsis.
No qualified systematic reviews evaluated the association between combined vitamin D and
calcium, body stores, or serum concentrations, and total cancer incidence or mortality. Two
RCTs reported different effects of combined vitamin D3 and calcium supplementation on the risk
oftotal cancer. The WHI showed no effects,
71
while the trial conducted in Nebraska (latitude
41 N) reported significant reduction of risk of total cancer. 5
2
However, both vitamin D doses and
baseline vitamin D status were substantially different between these two RCTs. Therefore, the
effects from these two RCTs were not comparable.
Detailed presentation (Tables 89 & 90).
The 7-year WHI trial that enrolled 36,282 postmenopausal women across the US compared a
daily supplement of vitamin D
3
( 400 IU) and elemental calcium ( 1000 mg) with placebo and
evaluated incidence of total cancer and total cancer mortality as part of multiple secondary
analyses.
71
The median serum 25(0H)D level of the study population was 42 nmol/L. The trial
did not find significant effect of combined vitamin D
3
and calcium supplementation on either the
risk of total cancer (adjusted HR: 0.98, 95 percent CI 0.91, 1.05) or total cancer mortality
(adjusted HR: 0.89, 95 percent CI 0.77, 1.03). The methodological quality of this study was rated
B.
A 4-year population based RCT,
52
sampled from a 9-county, largely rural area in eastern
Nebraska (latitude 41 N), aimed to determine the efficacy of vitamin D
3
(1000 IU/d) plus
calcium (either calcium citrate 1400 mg/d or calcium carbonate 1500 mg/d), or calcium alone
(either calcium citrate 1400 mg/d or calcium carbonate 1500 mg/d), compared to placebo in
reducing the incidence of fracture. Incidence of cancer was a secondary outcome in this trial. A
total of 734 postmenopausal women, aged more than 55 years old, were analyzed for the effect
of vitamin D3 (1000 IU/d) plus calcium (either calcium citrate 1400 mg/d or calcium carbonate
1500 mg/d). The mean 25(0H)D concentration at baseline was 72 nmol!L. Compared to the
placebo group, the relative risk of developing cancer at the end of study was 0.40 (95 percent CI
0.20, 0.82; P=0.013) for the vitamin D
3
plus calcium group. On the hypothesis that cancers
diagnosed early in the study would have been present, although unrecognized at entry, the
analyses were restricted to women who were free of cancer at 1 year intervention. The relative
risk of developing cancer at the end of study for the vitamin D
3
plus calcium group changed to
0.23 (95 percent CI 0.09, 0.60; P= 0.005). The methodological quality of this study was rated B.
Findings by life stage.
0 - 6 mo No data
7 mo- 2 y No data
3 - 8 y No data
9-18 y No data
19-50 y No data
51-70 y No data
~ 7 y No data
259
Postmenopause The WHI trial using vitamin D
3
400 IU/d plus calcium carbonate
1000 mg/d showed no effects, while the trial in Nebraska using vitamin D3 1000 IU/d
plus calcium citrate or carbonate 1500 mg/d showed significant reduction of risk of total
cancer.
Pregnant & lactating women No Data
Table 89. Combined vitamin D and calcium and total cancer incidence: Characteristics of ACTs
Author Year
Background
Study Name
Calcium Intake
Location Population
& Vitamin 0
Comparisons Compliance Comments
(Latitude)
Data
[PMID]
Wactawski-Wende Health Post- Ca intake Vit 03 400 IU/d + See page
2006
71
status menopausal (mg/d) : Ca 1000 mg/ d 242
WHI women <800, 34%; vs.
us Mean age nd (50-79) 800-200, 26%; Placebo
(various) (range/SO), y ~ 1 2 0 0 40%
[16481636)
Median
25(0H) O: 42
nmoi/ L
Lappe Health Mentally and 25(0H) O: 71.8 Vit 0 3 1000 IU/d + Ca nd
2007
52
status physically fi t; nmoVL (citrate 1400 mg/d or
Nebraska, US (41 2 post- carbonate 1500 mg/d)
N) menopause vs. Ca (citrate 1400
[17556697) Mean age 67 (7.3) mg/d or carbonate 1 500
(range/SO), y mg/d) vs. placebo
260
Table 90. Combined vi tamin D and calcium and total cancer incidence: Results of ACTs
Author Year
Follow up, Interventions, N
Outcome
Study
Study Name Life Stage Outcome 1/2
n
Metric Result 95%CI P Btw
[PMID]
year Daily Dose Event Total
Quality
Wactawski -Wende
Post-
Vii 03 400 IU + 1634 18176 Adjusted HR 0.98 0.91 , 1.05 0.53
2006
71
menopausal
Incident cancer
20
7
Ca carbonate (Vii
8
WHI (all causes) 1000 mg O+Ca)/placebo
women - -------
[ 16481636) Placebo 1655 18106
Post-
Vit 03 400 IU + 344 18176 Adjusted HR 0.89 0.77, 1.03 0.12
menopausal
Total cancer
20
7
Ca carbonate (Vii
mortality 1000 mg O+Ca)/placebo
women
Placebo 382 18106
Vit 03 1000 IU + 0.40 0.20, -0.82 0.01
Lappe Post-
Incident cancer
Ca (citrate 1400
13 446
RR (Vit
2007
52
menopausal
(all causes)
20
4 mg or carbonate O+Ca)/placebo 8
[17556697] women 1500 mg)
.................................
Placebo 20 288
Incident cancer Vii 03 1000 IU + 0.23 0.09, -0.60 <0.005
Post-
(restrict to Ca (citrate 1400
8 403
RR (Vit
menopausal
subj ects who
20
4
mg or carbonate O+Ca)/placebo
women
were free of 1500 mg)
.................................
cancer at 1 y
Placebo 20 288
261
Colorectal cancer.
Synopsis.
No qualified systematic reviews evaluated the association between combined vitamin D and
calcium, body stores, or serum concentrations, and colorectal cancer mortality or incidence. One
B quality RCT of postmenopausal women reported no significant association between
supplemental vitamin D
3
and calcium and, colorectal cancer mortality or incidence.
Detailed presentation (Table 91 & 92).
The WHI compared daily supplemental vitamin D
3
(400 IU) and elemental calcium (1000
mg) with placebo in 36,282 postmenopausal women. Colorectal cancer was evaluated as a
secondary endpoint.
71
The primary endpoint was the prevention of hip fracture. At 7 years
vitamin D3 and calcium supplementation had no significant effect on colorectal cancer mortality
(P=0.39) or incidence (P=0.51 ). In a subgroup analysis, risks of colon cancer and rectal cancer
were also not significantly different between the supplemented and unsupplemented groups
(P=0.99 and P=0.11, respectively). This trial was rated B because it did not restrict the
participants from taking calcium or vitamin D supplements; they had mean daily total calcium
intake of 1151 mg and vitamin D intake of 367 TU at enrollment.
Findings per special populations.
The WHI performed 18 subgroup analyses based on baseline participant characteristics
including ethnic groups, body mass index, smoking status, and geographic regions according to
solar irradiance.
71
No significant interactions were found with these baseline characteristics. The
same RCT with multifactorial design reported an interaction between estrogen alone or
combined estrogen and progestin therapy, and combined vitamin D and calcium supplementation
for colorectal cancer risk in a post hoc analysis?
03
Among women concurrently assigned to
hormone replacement therapies, colorectal cancer incidence was increased in the combined
supplemental vitamin D and calcium ann compared to placebo (HR 1.50, 95 percent Cl 0.96,
2.33), whereas among those concurrently assigned to placebo in the estrogen trials, colorecta1
cancer risk was reduced in the vitamin D plus calcium arm compared to placebo (HR 0.71, 95
percent CI 0.46, 1.09) (P for interaction = 0.02).
Findings by ~ f stage.
0 - 6 mo Not reviewed
7 mo- 2 y Not reviewed
3 - 8 y Not reviewed
9 - 18 y Not reviewed
19- 50 y No data
51 - 70 y One trial that included women mostly within this life stage (WHI) found
no significant association between combined vitamin D
3
( 400 ill) and calcium carbonate
(1000 mg) and colorectal cancer mortality or incidence.
71 + The WHI included some people within this life stage, but no study
adequately evaluated this life stage.
262
Postmenopause The WHI exclusively focused on postmenopausal women. The
study found no association between vitamin D and calcium intake and colorectal cancer
mortality or incidence.
Pregnant & lactating women Not reviewed
Table 91. Combined vitamin D with calcium and colorectal cancer: Characteristics of RCTs
Author Year
Study Name
Location
(Latitude)
[PMID]
Wactawski-Wende
2006
71
WHI
us
(various)
[16481636]
Population
Health
status
Mean
age
(range),
y
Male
(%)
Post-
menopausal
women
nd (50-79)
0
Background
Calcium Intake
& Vitamin D
Data
Total Ca intake
(mg/d)
(Mean for both
groups: 1151)
Ca + Vit D
arm: 1148
<800: 34%
800-<1200: 26%
2:1200:39%
Placebo arm:
1154
<800: 33%
800-<1200: 26%
2:1200:40%
Total Vit D intake
(IU/d)
(Mean for both
groups: 367)
Ca + Vit D
arm: nd
<200: 38%
200-<400: 19%
400-<600: 23%
600: 19%
Placebo arm:
nd
<200: 37%
200-<400: 19%
400-<600: 24%
600: 19%
263
Comparisons Compliance
Ca 1000 mg/d
+ Vit 03 400
IU/d vs.
Placebo
See page
242
Comments
The outcomes were based
on self-reported
questionnaires. Only
colorectal cancers were
verifi ed centrally.
Colorectal cancer
screening was not
mandated in the protocol.
Lost to followup:
Ca + Vit D arm: 0.8%
Placebo arm: 0.8%
Withdrawn:
Ca + Vit D arm: 1.9%
Placebo arm: 1.8%
Table 92. Combined vitamin D with calcium and colorectal cancer: Results of RCTs
Author Year Mean
Interventions, N Outcome Metric
p
Study
Study Name Life Stage Outcome 1/2 Followup,
n
Result 95% CI
Daily Dose Event Total (Comparison) Btw Quality
lPMID]
~
Wactawski-Wende
Post- Colorectal
Vit 03 400 IU +
HR
2006
71
Ca carbonate 34 18,176 0.82 0.52, 1.29 0.39
WHI
menopausal cancer
20
7
1000 mg
(Suppi/Piacebo) B
women mortality
.............................................
[16481636] Placebo 41 18,106
Colorectal
20
Vit D + Ca 168 18,1 76 HR 1.08 0.86, 1.34
..................................................
cancer Placebo 154 18,106
Colon
20
Vii D+ Ca 128 18 176 HR 1.00 0.78 1.28 0.99
cancer Placebo 126 18,106
Rectal
20
Vii D + Ca 44 18,176 HR 1.46 Q ~ ? ? : g
-----
cancer Placebo 30 18,106
264
Colorectal adenoma. Synopsis.
No qualified systematic reviews evaluated the association between combined vitamin D and
calcium, body stores, or serum concentrations, and incidence of intestinal adenoma. One B
quality RCT of postmenopausal women found no significant effect of combined vitamin D
3
and
calcium supplements on the incidence of colorectal adenoma. Another B quality post hoc
subgroup analysis of a secondary prevention trial of adenomatous adenoma reported that calcium
supplemented patients with higher baseline 25(0H)D concentrations had significantly lower risk
of relapse compared to placebo (interaction P = 0.01 between subgroups). In contrast, no
significant difference in relapse rates was found in calcium supplemented patients with lower
baseline 25(0H)D concentrations compared to placebo.
Detailed presentation (Table 91 & 92).
The WHI compared a daily supplement of vitamin D
3
(400 IU) and elemental calcium (1000
mg) with placebo and evaluated incidence of self-reported colo rectal adenoma as part of multiple
secondary analyses.
71
At 7 years, the incidence of adenoma was not significantly different
between the supplement and placebo groups (p=0.71). All the adenoma cases were based on self-
reported data, not verified by medical record review or histopathology report.
A post hoc subgroup analysis of the CPP trial of secondary adenoma prevention on the basis
of calcium supplementation (1200 mg of elemental calcium) evaluated the risk of colorectal
adenoma stratified by baseline 25(0H)D concentrations?
04
The primary endpoint of the original
trial was the risk of recurrent adenoma. After 4 years, in the subgroup with 25(0H)D
concentrations greater than 72.6 nmoVL at baseline, subjects who received supplemental calcium
had a significantly lower incidence of recurrent adenoma compared to placebo (HR=0.71 [95
percent CI 0.57,0.89] versus HR=l.05 [95 percent CI 0.85, 1.29]; interaction P=O.Ol). In the
subgroup with 25(0H)D concentrations lower than 72.6 nmol/L, the risk of recurrence was not
significantly different between supplemental calcium and placebo. No subgroup data were
available regarding sex, separate life stages, or other special populations (e.g., obese, smokers,
ethnic groups, or users of contraceptives).
Findings by ~ f stage.
0 - 6 mo Not reviewed
7 mo- 2 y Not reviewed
3 - 8 y Not reviewed
9 - 18 y Not reviewed
19 - 50 y The CPP included some people within this life stage, but no study
adequately evaluated this life stage.
51 - 70 y The analysis of the CPP with a mean age of 61 years included participants
mostly within this life stage. The study found a significant association between
supplemental calcium and reduced risk of colorectal adenoma in a subgroup with
25(0H)D concentrations higher than 72.6 nmoi/L.
71 + The CPP included some people within this life stage, but no study adequately
evaluated this life stage.
Postmenopause The WHI found no association between combined vitamin D
3
and
calcium supplements and the incidence of colorectal adenoma.
Pregnant & lactating women Not reviewed
265
Breast cancer
Synopsis
No qualified systematic reviews evaluated the association between vitamin D and calcium
intake, body stores, or serum concentrations, and breast cancer. Breast cancer incidence and
breast cancer related mortality after 7 years were evaluated in the Women's Health Initiative
(WHI) trial of combined daily vitamin D
3
400 IU and calcium carbonate 1000 mg versus placebo
in 50 to 79 year old women without a prior history of breast cancer.
205
No statistically significant
effect was found with combined vitamin D and calcium supplementation on incident breast
cancer outcome. No significant associations were found for breast cancer related mortality.
Detailed presentation (Tables 93 & 94)
In the WHI trial, the evaluated breast cancer incidence and breast cancer related mortality
outcomes were secondary outcomes.
205
There were no significant effects of combined vitamin D
and calcium supplementation on both outcomes. The authors concluded that invasive breast
cancer incidence was similar in the two groups of healthy postmenopausal women: calcium and
vitamin D supplementation and placebo groups. The relationship of 25(0H)D serum
concentrations and the risk of breast cancer was examined in a nested case-control design. The
study found no relationship between total vitamin D intake and 25(0H)D serum concentrations
with the risk of breast cancer.
Findings per intake level
No conclusions are possible regarding a dose effect from this single study, especially since
the women in the intervention and placebo groups were allowed to take additional concurrent
calcium and vitamin D supplements.
Findings by age and sex
The study investigated postmenopausal women 50 to 79 years old.
Findings by life stage
0 - 6 mo Not reviewed
7 mo - 2 y Not reviewed
3-8 y Not reviewed
9- 18 y Not reviewed
19- 50 y No data available
51 - 70 y The WHI trial that included women mostly within this life stage found no
significant effect of combined vitamin D
3
( 400 IU) and calcium carbonate ( 1000 mg) on
incident breast cancer and mortality from breast cancer after 7 years.
2':71 y Inadequate available data.
Postmenopause All women in the WHI trial were postmenopausal.
Pregnant & lactating women Not reviewed
266
Table 93. Combined vitamin D and calcium and breast cancer outcomes: Characteristics of RCTs
Author Year
Study Name
Location
(Latitude)
[PMID]
Chebowski
2008
205
WHI
us
(various)
[1 9001601)
Population
Health No
status breast
cancer
Mean 50-79
age
(range), y
Male 0
(%)
Background
Calcium Intake &
Vitamin D Data
Baseline Ca
supplementation:
Vit D & Ca arm
<800: 34.3%
800-<1200: 26.5%
~ 1 2 : 39.3%
Placebo arm
<800: 33.8%
800-<1200: 26.2%
:2:1200: 40.0%
Baseline Vit D
supplementation:
Vit D & Caarm
Yes: 47.1%
No: 52.9%
Placebo arm
Yes 47.6%
No 52.4%
267
Comparisons Compliance
Combined Vit D & See page
Ca supplement 242
vs. Placebo
Comments
Intervention and placebo
groups were allowed to
take additional
concurrent calcium and
vitamin D supplements.
Table 94. Combined vi tamin D and calcium and breast cancer outcomes: Results of ACTs
Life Outcome 1/2 Mean Interventions, Daily n N Outcome Metric Result 95%CI
p
Study
Stage Followup, y Dose Event Total (Comparison) Btw Quality
Chebowski 50-79 y, Breast cancer incidence 2 7 Vit 0
3
400 IU + Ca 668 18176 HR 0.96 0.86, 1.07 NS B
2008
205
Women _sa[Qonate 1 000 mg
.. ..
WHI Placebo 693 18106
......,, ..., ..,, ..,, ..,, ..., ..,, ..,, ..,, ..,,..
[19001601) Death from breast
20
7 Vit 03 400 IU + Ca 23 18176 HR 0.99 0.55, 1.76 NS
cancer carbonate 1000 mg
--
Placebo 23 18106
Invasive breast cancer
20
7 Vit 0
3
400 IU + Ca 86 195 AdjOR 0.89 0.58, 1.36 NS
- subgroup >67.6 1000 mg
--
baseline 25(0H)D Placebo 76 185
Invasive breast cancer
20
7 Vit D3+ Ca 95 171 AdjOR 1.25 0.83, 1.90 NS
-subgroup 55.4-<67.6
--
baseline 25(0H)D Placebo 86 171
Invasive breast cancer
20
7 Vit 0
3
+ Ca 102 176 AdjOR 1.07 0.70, 1.62 NS
- subgroup 43.9- <55.4
baseline 25(0H)D Placebo 92 195
..............................................--,
Invasive breast cancer
20
7 Vit 03+ Ca 71 185 Adj OR 0.69 0.45, 1.06 NS
- subgroup 32.4-<43.9
......................................................................... ...............................................--
baseline 25(0H)D Placebo 102 171
Invasive breast cancer
20
7 Vit D3+ Ca 94 171
........................
0.91 0.60, 1.39 NS
P lacebo
--
- subgroup <32.4 91 176
baseline 25!0HlD
268
Combined Vitamin D and Calcium and Pregnancy-related Outcomes
Preeclampsia.
Synopsis.
Based on data from a single RCT, there is no significant effect of combined vitamin D and
calcium supplementation on the prevention of preeclampsia.
Detailed presentation (Tables 95 & 96.)
One RCT from India used a combination of vitamin D (1200 IU/ d) and calcium (375 mg/d)
for the prevention of preeclampsia.
206
Table 85 desctibes the characteristics of the trial. The trial
found no significant difference between the compared arms (Table 86). Note that this RCT was
excluded from the meta-analysis of trials for preeclampsia in the calcium section.
Findings by l ~ f stage.
0 - 6 mo No data
7 mo - 2 y Not applicable
3 - 8 y Not applicable
9-18 y Not applicable
19-50 y [see pregnant and lactating women]
51 -70 y Not applicable
71 + Not applicable
Postmenopause Not applicable
Pregnant & lactating women Based on data from a single RCT, there is no
significant effect of combined vitamin D (1200 IU/d) and calcium (375 mg/d)
supplementation on the prevention of preeclampsia.
Other pregnancy-related outcomes.
Synopsis.
We did not identify any eligible studies on the relationship of vitamin D with or without
calcium and high blood pressure, preterm birth, or small for gestational age infant.
Table 95. Combined vitamin D and calcium and preeclampsia: Characteristics of RCTs
Author Year
Study Name
Location
(Latitude)
[PMID]
Marya 1987
206
India
(29N)
[3623260)
Population
Health Any
status
Age 20-35
range, y
Background Calcium Intake
& Vitamin D Data
Ca: 500 mg/ d in in diet;
Vit D: - 40 IU/ d (unclear how it
was quantified)
269
Comparisons
Combined Vit D (1200
IU/ d) & Ca (375 mg/ d)
supplement vs. no
supplement
Compliance
nd
Comments
Table 96. Combined vitamin D and calcium and preeclampsia: Results of RCTs
Mean
Outcome
Life Stage Outcome 1/2 Followup,
Interventions, Daily n N Metric
Result 95% CI
p
Study
Dose Event Total (Com pari- Btw Quality
y
son)
Marya Vii D (1200 IU) &
12 200 RR 0.67 0.33, 1.35
1987
206
Toxemia
calcium (375 mg)
---------- (combined ---------------.
India Pregnancy
(preeclampsia)
10 NO
Vit D & Ca
0.26 c
(29N) No supplement 18 200
vs. nothing)
~ 3 6 2 3 2 6 ]
270
Combined Vitamin D and Calcium and Clinical Outcomes of Bone
Health
Rickets, fractures, falls, or performance measures.
For bone health outcomes (e.g., bone mineral density, fracture, fall or muscle strength), we
relied on a recent comprehensive systematic review perfonned by the Ottawa EPC (Table 34).
6
Because the Ottawa's EPC report did not have separate analyses for the effect of vitamin D
supplementation alone, the results for the effect of vitamin D alone or in combination with
calcium supplementation are presented in this section.
The Ottawa EPC report was updated with literature published between January 2006 and
April 2009, selected according to our eligibility criteria. Only RCTs qualified for inclusion.
Synopsis.
The Ottawa EPC report concluded that supplementation with vitamin D (most studies used
D
3
) plus calcium is effective in reducing fractures in institutionalized populations, but there is
inconsistent evidence that supplemental vitamin D reduces falls in postmenopausal women and
older men. Our update search did not identify new RCT examining the combined effect of
vitamin D plus calcium supplementation on rickets, fractures, or falls in postmenopausal women
and older men.
One study published after the Ottawa EPC report analyzed the performance measure
outcomes in a small sample of postmenopausal women from WHI trial showed generally no
differences in performance measures between vitamin D (400 IU/d) plus calcium (1000 mg/d)
supplementation or placebo groups after 5 years offollowup.
207
One RCT of premenopausal
women, aged 17 to 35 years old, showed that 800 IU/d ofvitamin Din combination with 2000
mg/d of calcium supplementation can reduce the risk of stress fracture from military training
compared to placebo.
208
Detailed presentation (Table 34, 97, 98 & 99).
One RCT of female Navy recruits, aged 17 to 35 years, aimed to determine whether
supplementation with vitamin D (800 IU/d) plus calcium (2000 mg/d) can reduce the risk of
stress fractures from military training near the Great Lakes ( 41 N)?
08
The median dairy intake
was <1 serving/day, which provided less than 300 mg of calcium. The combined
supplementation significantly reduced the risk of stress fractures by 20 percent compared to
placebo. The methodological quality of this study was rated B.
One study analyzed the performance measure outcomes in a sample of 2928 postmenopausal
women from the WHI trial who had objective physical function measures.
207
The results showed
that physical function, measured by grip strength, chair stands, and walking time, had generally
declined in postmenopausal women who were assigned to either vitamin D ( 400 IU/d) plus
calcium (1000 mg/d) supplementation or placebo group. However, women who had received
vitamin D plus calcium supplementation showed less declines in walking time than those who
had received placebo. The methodological quality ofthis study was rated C because only a small
proportion of women from the WHI trial were in the analyses and their baseline characteristics
were unclear.
271
From the Ottawa EPC Report: Fractures - Postmenopausal women and older men.
Fifteen RCTs examined the effect of either vitamin D
2
or D
3
alone or in combination with
calcium on total, non vertebral and hip fractures in postmenopausal women or older men. Few
trials evaluated vertebral fractures. Most trials used vitamin D
3
. There were no trials identified in
premenopausal women.
Meta-analysis results from 13 RCTs of vitamin D
2
or D3 with or without calcium showed a
nonsignificant reduction in the risk of total fractures that persisted when only trials of higher
quality were combined. Most trials used vitamin D3. When combining seven RCTs of vitamin D3
( 400-800 IU) plus calcium, there was a reduction in the risk of total and hip fractures. However,
in a subgroup analysis (800 IU vitamin D3 ), this benefit was only evident in trials of
institutionalized elderly subjects. One possible explanation for the discrepancy is that the mean
serum 25(0H)D concentration achieved in trials of institutionalized participants was higher than
in the trials on community dwellers. The combined estimate from trials with higher end-of-study
serum 25(0H)D concentrations (>74 nmol/L) was consistent with a significant reduction in the
risk of fractures.
In Ottawa EPC report: Falls- Postmenopausal women and older men.
Meta-analysis results from 12 RCTs demonstrated a small reduction in the risk of falls with
supplemental vitamin D2 or D3 (oral or injectable) with or without calcium (OR 0.89, 95 percent
CI 0.80, 0.99). The individual treatment effects ranged from OR 0.28 (95 percent CI 0.12, 0.67)
to 1.16 (95 percent CI 0.70, 1.92). In the two cluster RCTs, one demonstrated a significant
reduction in the risk of falls in postmenopausal women taking vitamin D3 plus calcium (RR 0.88,
95 percent CI 0.79, 0.98), whereas the other trial did not show a significant reduction in the risk
of falls in elderly individuals taking vitamin D2 (RR 1.09, 95 percent CI 0.95, 1.25). Meta-
analysis of eight RCTs of oral vitamin D2/D3 supplementation with calcium showed a reduction
in the risk of falls, whereas four RCTs of oral vitamin D3 alone did not. Subgroup analyses
showed a significant reduction in the risk of falls when only trials of postmenopausal women
were combined. Sensitivity analyses showed a significant reduction in the risk of falls when
combining (1) RCTs that explicitly defined falls and the method of fall ascertainment and (2)
those in which the allocation concealment was unclear. However, combining trials by degree of
compliance and loss to followup did not.
Findings by life stage.
0 - 6 mo Not reviewed
7 mo - 2 y Not reviewed
3 - 8 y Not reviewed
9 - 18 y Not reviewed
19 - 50 y The Ottawa EPC report concluded that supplementation with vitamin D
(most studies used D
3
) plus calcium is effective in reducing the risk of fractures in
institutionalized populations, but there is inconsistent evidence that supplemental vitamin
D reduces the risk of falls in postmenopausal women and older men. One RCT of female
Navy recruit, aged 17 to 35 years old, showed that vitamin D (800 IU/d) in combination
of calcium (2000 mg/d) supplementation can reduce the risk of stress fractures from
military training compared to placebo.
51 - 70 y No new data since the Ottawa report
71+ No new data since the Ottawa report
272
Postmenopause One study analyzed the performance measure outcomes in a small
sample of postmenopausal women from the WHI trial showed generally no differences in
performance measures between vitamin D ( 400 fU/d) plus calcium (I 000 mg/d)
supplementation and placebo groups after 5 years of followup.
Pregnant & lactating women No data
Table 97. Combined vitamin D and calcium and bone health: Characteristics of RCTs published
after the Ottawa EPC report
Author Year
Background
Study Name
Calcium Intake
Location Population
& Vitamin D
Comparisons Compliance Comments
(Latitude)
Data
[PMID]
Lappe Health Assumed Mean dairy Vit D 800 IU/d + Monitor pill taking: project
2008
208
status healthy servings/wk = 6 Ca 2000 mg/d staff observed the galley
Great Lakes, (Navy (ranged 126) vs. Placebo food lines, visited recruits
IL, US recruits) in thei r quarters, and
(41 N) Mean 19 (17-35) conducted an exit
[18433305) age interview.
(range) , y
Male 0
(%)
Brunner Health nd (for the nd Vit D 400 IU/d + nd (however, adherence A sub sample
2008
207
status sub sample Ca 1000 mg/d was assessed at least from WHI trial.
WHI from WHI vs. Placebo annually from the weight Post hoc
us trial) of remaining pills along analyses of a
(various) Mean 50-79 with a structured interview RCT.
[1 8755319) age in WHI trial)
(range) , y
Male 0
(%)
273
Table 98. Combined vitamin D and calcium and bone health: Results of RCTs published after the Ottawa EPC report (stress fracture)
Author Year Life Mean Interventions, n N Outcome Metric Result Cl P Study
Study Name Stage Outcome
1
12
Followup, Daily Dose Event Total (Comparison) " Btw Quality
[PMID] mo
Lappe
2008
208
[1 8433305)
17-35 y
women
Stress fracture from
Navy training (ITI)
Stress fracture from
Navy training (per
protocol)
1 2
2
Vit D 800 IU + Ca 139 2626 RR (Vit 0.8 0.64, 0.99 0.026
200 mg
Placebo 170 2575 r-""'"' """"'-
Vii D 800 IU + Ca 126 1852 Adjusted OR (Vit 0.79 0.62, 1 01 0.059
200 mg __________ _________
Placebo 160 1848
Table 99. Combined vitamin D and calcium and bone health: Results of RCTs published after the Ottawa EPC report (performance
measures)
Author Year Mean
Interventions, No. Change Net Net Diff
p
Study Name Life Stage Outcome 1/2 Followup,
Daily Dose Analyzed
Unit Baseline Change
so Diff 95% CI Btw
PMID mo
Brunner Grip Vii D 400 IU + 1185 22.81 -2.49 5.81 0.15 0.24 0.52
2008
207
Post- strength
20
60
Ca carbonate kg
[1 8755319) menopause 1000 mg
Placebo 1162 22. 96 2.64 5.69
Vit D 400 IU + 1065 0.38 1.81 0.04 0.08 0.603
Chair
2 60
Ca carbonate counts 6.52
stands __lQQO_!!lg
Placebo 1053 6.63 -0.43 1.81
Vit D 400 IU + 1160 seconds +0. 26 6.28 0.26 0.030
Walking
2 60
Ca carbonate 0.54
time 1000 mg
Placebo 1141 +0.81 6.43
274
B
Study
Quality
c
Combined Vitamin D and Calcium and all-cause Mortality
Synopsis.
This synopsis is based on a meta-analysis ofRCTs of combined vitamin D and
calcium supplementation evaluating mortality. Numerical data were extracted from
previous systematic reviews. Most trials used daily regimens; in these trials, vitamin D
doses ranged between 300 and 880 IU per day. Most trials combined vitamin D and
calcium supplementation; when used, calcium doses ranged between 500 and I 200 mg
per day.
Our meta-analysis of 11 RCTs (44,688 participants) suggests no significant
relationship between combined supplementation of vitamin D and calcium all-cause
mortality (RR=0.93, 95 percent CJ 0.86, 1.01; random effects model). There is little
evidence for between-study heterogeneity in these analyses. Among 8 RCTs on 44,281
postmenopausal women, the summary random effects RR was 0.93 (95 percent CI 0.86,
1.00), again with little evidence for between-study heterogeneity.
Although the meta-analyses suggest decreased risk for all-cause mortality with
combined vitamin D and calcium supplementation, the relationship is not statistically
significant in the performed analyses.
Detailed presentation (Table 37; Figure 22).
As mentioned in the Methods section, we updated and reanalyzed published meta-
analyses of mortality outcomes. We drew our own conclusions based on our analyses.
We also comment on the concordance of our conclusions with those of the published
meta-analyses.
Relevant published systematic reviews ofRCTs (with meta-analyses).
As described in the vitamin D and all-cause mortality section, we identified two
potentia11y eligible systematic reviews,
83
'
84
and selected one as the basis for our
reanalysis (Autier 2007).
83
Table 37 in the "Vitamin D" section summarizes the findings
of the Autier 2007 systematic review.
As detailed below, we identified one additional trial of combined vitamin D and
calcium supplementation reporting all-cause mortality.Z
09
Eligible studies published after the systematic reviews.
The literature searches in Autier 2007 extended up to November 2006. We identified
two additional RCT reports published after November 2006.
71
'
209
One publication
71
reported on the same trial as another publication
210
in the Autier 2007 meta-analysis, and
was therefore excluded from our reanalysis. The other RCT (Bjorkman 2008
209
) was
included in our meta-analysis.
One three-arm RCT (Bjorkman 2008
209
, n=218) compared no supplementation versus
daily supplementation with 400 IU and 1200 IU of vitamin D
3
and 500 mg of calcium.
Mortality was assessed at 6 months. It included people older than 65 years, with
chronically impaired mobility and stable general condition. The Bjorkman 2008 RCT was
assigned grade "A" for overall reporting quality.
275
Reanalysis.
We excluded 5 of 18 trials in the Autier 2007 meta-analysis: One trial was on patients
with congestive heart failure,
85
one was published only in abstract form,
86
and in the last
trial the controls also received supplementation with vitamin D, albeit with a smaller
dose,
87
and two used injections of vitamin D.
88
'
89
Altogether, 11 RCTs were included in
the reanalysis of combined vitamin D and calcium supplementation and all-cause
mortality (i.e., 10 out of 18 in the Autier 2007 meta-analysis, and a subsequently
published one
209
).
Among the 12 trials, sample sizes ranged from 55 to 36,282 participants, with 7
studies including more than 500 participants. Followup periods ranged from 6 to 84
months (median 24 months). Vitamin D doses in most trials ranged between 300 and 880
IU per day. One trial used 100,000 IU orally every 4 months. Calcium supplementation
doses ranged between 500 to 1200 mg per day.
Overall, a meta-analysis of the 11 RCTs ( 44,688 participants; Figure 22) found no
statistically significant relationship between vitamin D and aU-cause mortality (RR=0.93,
95 percent CI 0.86, 1.01 ). There is little evidence for between-study heterogeneity in
these analyses (P=0.58, 1
2
=0 percent). Among 8 RCTs on 44,281 postmenopausal
women, the summary random effects RR was 0.93 (95 percent CI 0.86, 1.00), again with
little evidence for between-study heterogeneity (P=0.46, l =O percent). There are no
RCTs with mean participant age below 50 years. It is unclear whether these findings are
directly applicable to other life stages. In addition, in a subgroup analysis among 8 RCTs
(n=81 09) where the mean participant age was above 70 years, the summary random
effects RR=0.98 (95 percent Cl 0.84, 1.15), with little evidence for between study
heterogeneity (P=0.33, /
2
=13 percent).
Findings by life stage.
0-6 mo No data
7 mo - 2 y No data
3 - 8 y No data
9 - 18 y No data
19 -50 y No data
51-70 y Our meta-analysis of 12 RCTs (44,838 participants) suggests no
significant relationship between combined supplementation of vitamin D and
calcium all-cause mortality (RR=0.94, 95 percent CI 0.87, 1.01; random effects
model). There is little evidence for between-study heterogeneity in these analyses.
71+ The above are likely applicable here. In addition, in a subgroup
analysis among 8 RCTs (n=81 09) where the mean participant age was above 70
years, the summary random effects RR=0.98 (95 percent CI 0.84, 1.15), with little
evidence for between study heterogeneity.
Postmenopause Among 8 RCTs on 44,281 postmenopausal women, the
summary random effects RR was 0.93 (95 percent CI 0.86, 1.00), again with little
evidence for between-study heterogeneity.
Pregnant & lactating women No data
276
Figure 22. Forest plot of trials of combined vitamin D and calcium supplementation and
effects on all-cause mortality.
Risk Ratio 95% Confidence Interval
Study Name N Counts Confidence Interval
CMpuy (1992) 3270 25811634 vs. 27411630 0.943 (0.807. 1 101)
Baeksgaard (1998) 160 OIWvs 1/80 0.333 (0.01 4, 8.062)
Komutainen (1999) 232 0111ovs 1/116 0.333 (0.01 4, 8 099)
Kneg (1999) 248 21/124 vs. 261124 0.808 (0 481, 1 356)
Chapuy (2002) 583 711393 vs 451190 0 763 (0.648 1 062)
Avenell (2004) 134 4170 vs 3J64 I 219 (0 284. 5239)
Mete! (2004) 55 0130 vs lfl6 0 280 (0 012. 6 576)
Porthoun (2006) 3314 671l321 vs. 68/1993 1 265 (0.896, 1 786)
Brazier (2005) 192 3195 vs 1197
Jackson (2006) 30282 74411 !f176 vs 807118106 0.918 (0.833, 1 012)
BJorkman (2008) 218 27/150 vs. 9168 1.360 (0.677. 2.733)
Overall 0.932 (0.803. 1.006)
0.1 10
277
Combined Vitamin D and Calcium and Hypertension and Blood
Pressure.
We reviewed systematic reviews and primary studies that evaluated associations between
combined vitamin D and calcium intake and incidence of hypertension or change in blood
pressure. For the outcome incidence of hypertension, we included RCTs and other longitudinal
studies. For the outcome change in blood pressure, we included only RCTs. We included only
studies of adults. Studies of pregnancy-related hypertension and blood pressure control are
included in the "Pregnancy-related outcomes" section.
Combined vitamin D and calcium and hypertension.
Synopsis.
No qualified systematic reviews evaluated the association between combined vitamin D and
calcium intake, body stores, or serum concentrations and incidence of hypertension. The WHI
trial reported an analysis of the risk of developing hypertension among the subset of women
without hypertension at baseline. Over 7 years, combined vitamin 0 and calcium
supplementation had no effect on the risk of hypertension.
Detailed presentation (Tables 100 & 101).
The WHI trial of a combined vitamin D3 400 IU and calcium carbonate 1000 mg supplement
daily versus placebo had methodological quality B for the blood pressure outcome. The 36,282
women were postmenopausal (age 50-79 y) with a background calcium intake on average of
about 1150 mg/day (from diet and supplements)?
11
The women were allowed to take additional
concurrent calcium and vitamin D supplements. The analysis of incident hypertension was
reported briefly in a larger analysis ofthe blood pressure outcome (see Combined vitamin D and
calcium and blood pressure, below). Among 17,122 initially nonhypertensive women, 39
percent either were prescribed medication for hypertension or developed blood pressure above
140/90 mm Hg. The adjusted HR of developing hypertension over 7 years was 1.01 (95 percent
CI 0.96, 1.06). Among 377 women with available data, there was a statistically significant trend
across subgroups based on serum 25(0H)D concentration such that combined vitamin D and
calcium supplementation increased the risk of developing hypertension more in those women
with progressively lower baseline 25(0H)D (P<O.Ol for trend). Other subgroup analyses based
on age, race or ethnicity, weight, or baseline total calcium intake did not find any interactions
with the effect of the supplement intervention.
Findings per intake level.
This single trial did not analyze different actual intake levels.
Findings by age and sex.
This trial found no difference in (lack of) effect by age among postmenopausal women.
Findings by life stage.
0-6 mo Not reviewed
7 mo-2y
3-Sy
9-18 y
19-50 y
Not reviewed
Not reviewed
Not reviewed
No data.
278
51 - 70 y One large trial that included women mostly within this life stage found no
significant effect of combined vitamin D and calcium supplementation.
~ 7 y The WHI trial included some women within the life stage, but no study
adequately evaluated this life stage.
Postmenopause All women in the WHI trial were postmenopausal. See 51-71 y life
stage.
Pregnant & lactating women Not reviewed
Table 100. Combined vitamin D and calcium and incident hypertension: Characteristics of RCTs
Author Year
Study Name
Location
(Latitude)
[PMID]
Margolis
2008
211
WHI
us
(various)
[18824662)
Population
Health
status
Mean
age
(range), y
Male
(%)
No
HTN
62
(50-79)
0
Background
Calcium Intake &
Vitamin D Data
Ca: 1148 (654) mg/d
in treatment group;
1154 (658) in
placebo group
52% used Ca
supplements
40% had intake
<:1200 mg/d
(based on all
subjects, including
those with
hypertension)
Comparisons Compliance
Combined Vit D + See page
Ca supplement vs. 242
Placebo
279
Comments
Mean dose of open label
supplemental Ca increased
by <1 00 mg/d from 325
mg/d at enroll ment ; similar
in both groups
(based on all subjects,
including those with
hypertension)
Table 101. Combined vitamin D and calcium and incident hypertension: Results of ACTs
Author Year
Life Stage Mean Interventions, Daily n N Outcome Metric
p
Study
Study Name Outcome 1/2 Result 95% CI
[PMID]
[Subgp] Followup, y Dose Event Total (Comparison) Btw Quality
Margolis Vii 0
3
400 IU + Ca
3377 -8578
HR
1.01 0.96, 1.06 0.69
2008
211
50-79 y,
HTN
20
7
carbonate 1000 mg
B
WHI Women
Placebo - 8544
[1 8824662)
[25(0H)D Vit D+ Ca 1.52 0.89, 2.59 NS
<34.4 nmoi/ L) Placebo
[25(0H)D Vii D + Ca 1.48
34.4-47.6
Placebo
nmoi/L
[25(0H)D Vii D + Ca 1.15
47.7-64.6
Placebo 45
nmoi/L
[25(0H)D Vit D+ Ca 48 0.79
:<:64.7 nmoi/L] Placebo 61
280
Combined vitamin D and calcium and blood pressure.
Synopsis.
No qualified systematic reviews evaluated the association between vitamin D and calcium
intake, body stores, or serum concentrations, and changes in blood pressure. Two RCTs
compared combined vitamin D and calcium supplementation with placebo. Both the small trial
of a combined vitamin D
3
400 IU and calcium carbonate 1200 mg supplement daily and the WHI
trial found no significant effect of supplementation on blood pressure after 15 weeks or 6.1
years, respectively. The WH1 trial analyzed blood pressure changes in a variety of subgroups,
including by age, ethnicity, baseline total calcium intake, and baseline diagnosis of hypertension,
but found no significant differences in effect across any subgroup.
Detailed presentation (Tables 102 & 103).
The WHI trial of a combined vitamin 0
3
400 IU and calcium carbonate l 000 mg supplement
daily versus placebo had methodological quality B for the blood pressure outcome. The 36,282
women were postmenopausal (age 50-79 y) with a background calcium intake on average of
about 1150 mg/day (from diet and supplements).
211
On average, the women had nonnal blood
pressure and were allowed to take additional concurrent calcium and vitamin D supplements. At
74 months, the women's mean systolic blood pressure had risen and diastolic blood pressure had
fallen in both trial arms (by less than about 2 mm Hg each at 2 years
199
). The absolute changes
were not significantly different in the women assigned to the supplement than placebo (net
difference 0.2 mm Hg systolic and 0.1 mm Hg diastolic). In subgroup analyses there was no
differences in results by age, ethnicity, baseline total calcium intake, baseline diagnosis of
hypertension, or a variety of other factors.
The C quality trial of combined vitamin D and calcium, performed in Quebec City, recruited
premenopausal women (mean age 43 y) with low calcium intake (800 mg calcium per day) who
did not have severe hypertension (blood pressure over 160/95 mm Hg).
202
The mean baseline
calcium intake was 704 mg/day. On average, the 63 women had nonnal blood pressure. They
were given either combined vitamin D
3
400 TU and calcium carbonate 1200 mg daily or placebo.
All women were on an energy restriction diet with a 700 kcal/day deficit. At 15 weeks, systolic
and diastolic blood pressures were reduced in both study groups; systolic blood pressure was
reduced by 2.5 mm Hg more in women on vitamin D and calciun1 than placebo, but this
difference was not statistically significant. Diastolic blood pressure was reduced by the same
amount in both groups. No subgroup analyses were reported. The study was limited by a 25
percent dropout rate due to lack of compliance with the diet and exercise portion of the trial,
without performing an intention to treat analysis, an adequate description of the study methods,
or a complete statistical analysis.
Findings per intake level.
Both trials used similar doses, vitamin D
3
400 IU and calcium carbonate 1000 or 1200 mg
daily. The background calcium intake was lower in the study of premenopausal women (800
mg/day) than the WHI trial (1150 mg/day). The WHI trial found no significant difference in
(lack of) effect in subgroups with different baseline total calcium intake.
281
Findings by age and sex.
Both the one small, short tem1, C quality trial of premenopausal women and the 6 year WHI
trial of postmenopausal women found no effect. The WHI trial also found no difference in effect
in subgroups of women based on age. No trials of men were found.
Findings by life stage.
0- 6 mo Not reviewed
7 mo - 2 y Not reviewed
3 - 8 y Not reviewed
9- 18 y Not reviewed
19 - 50 y One small trial that included women mostly within this life stage found no
significant effect of combined vitamin D and calcium supplementation.
51 - 70 y One large trial that included women mostly within this life stage found no
significant effect of combined vitamin D and calcium supplementation.
~ 7 y The WH1 trial included some women within the life stage, but no study
adequately evaluated this life stage.
Postmenopause All women in the WHI trial were postmenopausal. See 51-71 y life
stage.
Pregnant & lactating women Not reviewed
282
Table 102. Combined vitamin D and calcium and blood pressure: Characteristics of ACTs
Author Year
Study Name Background
Location Population Calcium Intake & Comparisons Compliance Comments
(Latitude) Vitamin D Data
[PMID]
Margolis Health Any Ca: 1148 (654) Combined Vit D + See page Mean dose of open label
2008
211
status mg/d in treatment Ca supplement 242 supplemental Ca
WHI
Mean 62 (50-79) group; 1154 (658} vs. Placebo increased by <1 00 mg/d
us
age
in placebo group from 325 mg/d at
(various)
(range}, y
52% used Ca enroll ment; simi lar in
[1 8824662)
Male 0
supplements both groups
{%)
40% had intake
~ 1 2 0 0 mg/d
Major 2007w
2
Health Healthy, Ca: -704 mg/d; all Combined Vit D + nd
Quebec City, status Overweight, <800 mg/d Ca supplement
Canada low Ca intake vs. Placebo
(47N) Mean 43 (5.5)
[1 7209177) age (SD},
y
Male 0
~ )
283
Table 103. Combined vitamin D and calcium and blood Results of ACTs
Author Year Age
Mean Interventions, No. Change Net Net Diff
p
Study
Study Name Range, Outcome 10/20
Followup Daily Dose Analyzed
Unit Baseline Change
95% CI Diff 95% CI Btw Quality
lPMID] Sex
SYSTOLIC BLOOD PRESSURE
Margolis Vit 03 400 IU +
mm
2008
211
50-79,
SBP
20
6.1 y
Ca carbonate 18,176
Hg
127A +1.1%A 0.9, 1.3 +0.22 -0.05, +0.49 0.11
B
WHI Women 1000 mg
-------------
[1 8824662) Placebo 18,106 +0.7%)( 0.5, 0.9
Vii 03 400 IU +
Ca carbonate
Major 1200 mg 30
mm
112.4 -4.1 -6.5, -1.7 -2.5 -6.2, 1.2 0.18
2007202
43 (5.5), (energy
Hg
Quebec City Women
SBP
20
15wk
restriction diet)
c
------------
[1 7209177) Placebo
(energy 33 109.5 -1.6 -4.2, 1.0
restriction diet
DIASTOLIC BLOOD PRESSURE
Margolis Vit 03 400 IU +
mm -0.4, -
2008
211
50-79, Ca carbonate 18,1 76
76A 0.2%A +0.11 -0.04, +0.27 0.14
WHI Women
OBP
20
6.1 y
1000 mg
Hg 0.02 B
---------- ---
76/( -0.6%)1 [1 8824662) Placebo 18, 106 -0.8, -0.4
Vit 03 400 IU +
Ca carbonate
mm
Major 1200 mg 30 74.9 -3.0 -4.8, -1.2 0 -2.7, 2.7* 1.0
2007
202
43 (5.5), (energy
Hg
Quebec City Women
OBP
20
15 wk
diet)
c
[1 7209177) Placebo
(energy 33 75.2 -3.0 -5.0, -1.0
A Hsia 20071YY [17309935]
restriction diet)
284
Combined Vitamin D and Calcium and Bone Mineral Density or Bone
Mineral Content.
For bone health outcomes (e.g., bone mineral density, fracture, fall or muscle strength), we
relied on a recent comprehensive systematic review performed by the Ottawa EPC (Table 34).
6
Because the Ottawa's EPC report did not have separate analyses on the effect of vitamin D
supplementation alone, the results for the effect of vitamin D alone or in combination with
calcium supplementation were presented in this section.
The Ottawa EPC report was updated with literature published between January 2006 and
April2009, selected according to our eligibility criteria. For adults, we included only BMD
indices. For chi ldren, we included only BMC indices. Only RCTs with duration more than I year
qualified for inclusion.
Synopsis
One RCT found that, compared to placebo, there was no significant effect of
supplementation with vitamin 0 3 (200 IU/d) plus calcium (1000 mg/d) on BMC changes in
healthy girls, between 10 and 12 years.
Overall, findings from the Ottawa EPC report showed that vitamin D
3
(:S 800 IU/d) plus
calcium ( - 500 mg/d) supplementation resulted in small increases in BMD of the spine, total
body, femoral neck and total hip in predominantly populations oflate menopausal women.
6
Two
of the three new RCTs showed consistent findings in postmenopausal women, comparing
vitamin D
3
or D
2
(300 or 1000 IU/d, respectively) plus calcium (1200 mg/d) to placebo.
Detailed presentation (Table 34, 104 & 105).
One RCT compared the effect of vitamin D3 (200 IU/d) plus calcium (l 000 mg/d)
supplementation to placebo on bone indices in healthy girls, aged 10 and 12 years.
212
The mean
background dietary calcium intake was 670 mg/d. The intention-to-treat analyses showed that
after 2 years of supplementation, there was no significant difference in the BMC changes
between girls who received vitamin D plus calcium supplement or placebo. The methodological
quality of this study was rated C, due to underpower and low compliance rate.
Three RCTs (two were rated Band one was rated C) examined the effect of vitamin D plus
calcium supplementation on BMD changes. All three trials were conducted in postmenopausal
women. However, the doses of vitamin D and calcium combinations varied. One RCT used daily
dose of 400 ru vitamin D
3
plus 100 mg elemental calcium for 2 years
213
The second RCT used
daily dose of 1000 IU vitamin D
2
plus 1200 mg calcium citrate for 5 years.
214
The third RCT
used a daily dose of vitamin D3 300 ru plus calcium citrate 1200 mg from calcium supplemented
low-fat dairy products for 1 year.
215
The latter two RCTs resulted in a significant increase in hip
or total BMD comparing vitamin D plus calcium supplementation to placebo.
214
'
215
The one RCT
that did not show significant change in femoral neck BMD comparing vitamin D plus calcium
supplementation to placebo used a substantially lower dose of calcium (100 mg/d) than the other
two RCTs.
In Ottawa EPC report- Bone Mineral Density and women of reproductive age, postmenopausal
women, and older men.
Overall, there is good evidence that vitamin D3 plus calcium supplementation resulted in
small increases in BMD of the spine, total body, femoral neck and total hip. Based on included
285
trials, it was less certain whether vitamin D3 supplementation alone has a significant effect on
BMD.
Seventeen RCTs evaluated the effect of supplemental vitamin D2 or D3 on BMD,
predominantly in populations of late menopausal women. Only one small RCT included
premenopausal women, and two trials included older men(> 60 years). Most trials were two to
three years in duration and used vitamin D doses of::::; 800 IU daily. Most trials used vitamin D3
and also included calcium 500 mg as a cointervention.
Meta-analysis results of 17 RCTs of vitamin D3 plus calcium versus placebo were consistent
with a small effect on lumbar spine, femoral neck, and total body BMD. The WHI trial found a
significant benefit of 400 IU vitamin D3 plus 1000 mg calcium supplementation on total hip
BMD. However, when the effect of vitamin D3 plus calcium versus calcium alone
supplementation is assessed, no significant increase in BMD was observed with either
intervention, suggesting vitamin D3 may be of less benefit in calcium replete postmenopausal
women. Vitamin D3 alone versus placebo did not result in a significant increase in BMD in
postmenopausal women, except in one trial that noted an increase in femoral neck BMD. Only a
few trials reported the impact of baseline serum 25(0H)D concentrations on BMD and in all of
these trials, baseline 25(0H)D concentration was not associated with increased BMD.
Findings by life stage.
0-6 mo No data
7 mo - 2 y No data
3-8 y No data
9 - 18 y One RCT showed that, compared to placebo, there was no significant
effect of vitamin D3 (200 IU/d) plus calcium (1000 mg/d) on BMC changes in healthy
girls, aged between 10 and 12 years old.
19- 50 y No data
51-70 y No new data since the Ottawa EPC report
2::71 y No new data since the Ottawa EPC report
Postmenopause Findings from the Ottawa EPC report showed that vitamin D
3
(::S
800 IU/d) plus calcium ( 5 mg/d) supplementation resulted in small increases in BMD
of the spine, total body, femoral neck, and total hip in predominantly populations of late
menopausal women. Two of the three new RCTs showed a significant increase in hip or
total BMD in postmenopausal women, comparing D
3
or D
2
(300 or l 000 IU/d,
respectively) plus calcium (1200 mg/d) to placebo.
Pregnant & lactating women No new data since the Ottawa EPC report
286
Table 104. Combined vitamin D and calcium and bone mineral density/content : Characteristics of
ACTs after the Ottawa EPC
Author Year Background
Study Name Calcium
Location Population Intake & Comparisons Compliance Comments
(Latitude) Vitamin D
[PMID] Data
Health Healthy Diet Vii D: Vit 03 200 65%
2005
2 2
status 100 IU/d IU/d + Ca completed
Jyvaskyla, Mean 11.2(10-12) carbonate intervention
Finland age Ca: 670 1000 mg/d vs. with >50%
(6224'N) (range), mg/d placebo compliance
[16280447) y
Male 0
%)
Bolton-Smith Health Healthy (assumed 25(0H)D: Vit 03 400 Good Noncompliant
2007
21 3
status postmenopausal) 59.4 nmoi/L IU/d + supplement women were
(UK 542N)
Mean 68 (2!:60) Elemental Ca adherence excluded.
[1 7243866)
age
Ca: 1548 100 mg/ d vs. based on pill
(range), mg/d placebo count
y (median, 99;
Male 0
IQE 97.3-
(%)
99.8%).
Zhu 2008
214
Health nd (assumed postmenopausal) 25(0H)D: Vit D2 1000 No
CIFOS status 68.0 nmoi/L IU/d + Ca differences
Western
Mean 74.8 (2.6) citrate 1200 in
Australia
age
Ca: 1010 mg/d vs. adherence
[ 18089701)
(SO), y mg/d placebo among
Male 0 groups (81 -
(%)
89%by
tablet
countin
Moschonis Health Postmenopausal DietVit 0: Vit 03 300 Dairy group Control group
2006
215
status 23.6 IU/d IU/ d + Ca 93% had no
Greece Mean 61 (55-65) 1200 mg/d (assessed intervention (
(31QN)
age Ca 680 mg/ d (from low fat via or usual diet )
[17181890) (range), dairy information so
y products) vs. obtained at compliance
Male 0
control (usual the biweekly issue not
diet) sessions applicable
287
Table 105. Combined vitamin D and calcium and bone mineral Results of ACTs after the Ottawa EPC
Author Year Mean
Interventions, No. Change 95% Net Net Diff
p
Study
Study Name Life Stage Outcome
10(20
Follow up,
Daily Dose Analyzed
Unit Baseline Change
Cl Diff 95% CI Btw Quality
PMID mo
Chen:!i'
Vi! 0 200 IU +
2005
2
1 0-12 y girls BMC
10
24
Ca carbonate 46 kg 1.3 34.7% 34.3%, 35.1% 0.3% 0.8, 0.? NS
c
[1 6280447)
1000 m
Placebo 39 1.3 35.0% 34.6%, 35.4% [ 1
Bolton-Smith Femoral
Vi! 03400 IU
2007
213 Postmenopausal
neck nd 24
+Elemental 50 mgfcm
2
nd +1.9 -6.5, 10.3 +1. 2 12.6, 15.0A NS
8
[1 7243866)
women
BMD
Ca 100m
Placebo 56 nd +0.7 -1 0.2, 11.6
Zhu 2008 Vit 02 1000 IU
Australia Postmenopausal
HipBMD
10
60
+ Ca citrate 39/33
8
mg/cm
2
783 nd +2.2% 1.9, 2.5 0.05
8
CIFOS women 1200 mg
[1 8089701) Placebo 41 /36
8
828 nd
f
Vit 03 300 IU
+ Ca 1200 mg
mg/cm
2
1.3, 3.1A Moschonis
Postmenopausal
Total (from low fat 39 1.13 1.5% 0.9%, 2.2% +2.2% <0.05
2006
21 5
body F 12 dairy c
[1 7181890)
women
BMO
Control (usual
...
l
diet)
36 1.12 0.7% 1.4%, 0.1%
A Estimated from reported data.
8
Baseline/follow-up number of subjects analyzed
288
How does dietary intake of vitamin D from fortified foods
and vitamin D supplementation affect serum 25(0H)D
concentrations (arrow 4)?
The evidence for this question comes from studies identified in our literature search
that crossed vitamin D terms with various outcomes terms. Studies that addressed this
question but do not report any of the outcomes of interest would not have been identified
in this manner. Because the availability of serum 25(0H)D concentration is unlikely to be
adequately indexed in the Medline citation, it would be difficult to comprehensively
search the literature for this question. To do so would require retrieving all vitamin D
supplements full text articles (in excess of 10,000) to look for serum 25(0H)D
concentration data. Given that there is no plausible reason for a systematic bias of studies
of a specific outcome choosing to report serum 25(0H)D concentration, we believe that
the evidence found, while not comprehensive, is a small but representative random
sample. Only RCTs were included for this question. RCTs of different regimens but with
the same dose of vitamin D supplementation were excluded (e.g., comparison of daily,
weekly versus monthly dose).
This question was also addressed in the Ottawa EPC report.
6
When appropriate, we
extracted relevant data from the Ottawa EPC report to be incorporated into our analyses.
RCTs on Dietary Intakes of Vitamin D From Fortified Foods and
Serum 25(0H)D Concentrations.
Synopsis.
Our updated search did not identify new RCT evaluating the effect of food
fortification on serum 25(0H)D concentrations since the Ottawa EPC report.
6
The
Ottawa EPC report concluded that there is "good" evidence that dietary intake of vitamin
D increases serum 25(0H)D concentrations among adults.
Detailed presentation.
Ottawa EPC report -Adults.
There were eleven RCTs (n=1281) of which seven (n=668) pennitted a quantitative
analysis. Ten of eleven trials found a significant effect of dietary intake from foods
fortified with vitamin D on serum 25(0H)D concentrations. There was significant
heterogeneity of the treatment effect. Potential sources of heterogeneity are the different
25(0H)D assays used (two studies each used HPLC, RIA or CPBA, and one study did
not report the assay), the dietary vehicles used, and study populations. The increase in
serum vitamin D concentration in the seven trials ranged from 15 (95 percent CI I 1, 18)
to 40 (95 percent CI 25, 55) nmol/L (fortification consisting of 100- 1000 IU of vitamin
D).
There can be a potential confounding of the data by the food source, the assay used to
measure 25(0H)D and potential differences in the bioavailability and/or metabolism of
vitamin D2 versus vitamin D3. Most studies in this review used dairy products as the
289
source of fortified food. It is important to note that there is potential for study
contamination through altered intake of other nutrients such as calcium, phosphate and
acid load that can affect the study outcomes.
RCTs on Vitamin D Supplementation and Serum 25(0H)D
Concentrations.
Synopsis.
Because the avai lability of serum 25(0H)D concentration is unlikely to be adequately
indexed in the Medline citation, it would be difficult to comprehensively search the
literature for this question. We believe that studies summarized here is a small but
representative random sample of all available data.
We plot the net changes in serum 25(0H)D concentration against the doses of
vitamin D supplementation using data from 26 RCTs with 28 comparisons in adults. Only
RCTs of daily vitamin D3 supplementation (doses ranged from 200 to 5000 IU/d) alone
or in combination with calcium supplementation (doses ranged from 500 to 1550 mg/d)
that provided sufficient data for the calculations were included in the plot. It is important
to note that the studies had varied compliance rates in the vitamin D intake; limited or no
adjustment for skin pigmentations, calcium intake, or background sun exposure; different
vitamin D assay methodologies and measurement (both intra- and interassay) variabil ity.
All these factors increase the heterogeneity and limit the usefulness of an overall
summary estimate for an intake dose response in serum 25(0H)D concentration.
Nonetheless, the relationship between increasing doses of vitamin D3 with increasing net
change in 25(0H)D concentration was evident in both adults and chi ldren (Figure 23). It
was also apparent that the dose-response relationships differ depending on study
participants' serum 25(0H)D status (:540 vs. >40 nmol/L) at baseline (Figure 24), and
depending on duration of supplementation (:53 vs. >3 months) (Figure 25).
Vitamin D
2
supplementation was more commonly used in RCTs of infants and
pregnant or lactating women, than vitamin D
3
supplementation. Results showed that
supplementation of vitamin D
2
significantly increased 25(0H)D concentrations in infants,
lactating mothers and in cord blood.
Detailed presentation (Table 106; Figures 23, 24 & 25).
The results from 26 RCTs with 28 comparisons in adults and two RCTs with three
comparisons in children evaluating the effect of vitamin D
3
supplementation alone or in
combination with calcium supplementation on serum 25(0H)D concentrations were
shown in Table 106. Most of the data were extracted directly from the Ottawa EPC
report. In adults, the doses of vitamin D
3
ranged from 200 to 5000 IU/d, and the doses of
calcium supplementation ranged from 500 to 1550 mg/d across the 25 comparisons. In
children, the doses of vitamin D
3
ranged from 200 to 2000 IU/d across the three
comparisons. Duration of supplementation ranged from 0.5 to 60 months. Study
populations and baseline vitamin D concentrations varied across these comparisons.
Ottawa EPC report- Infants.
Seven RCTs included infants and few trials used vitamin D
3
supplementation. One
RCT concluded that 200 IU of vitamin D
2
may not be enough to prevent vitamin D
deficiency in those infants residing at northern latitudes. A dose-response relationship
290
was noted in this trial (100, 200, 400 IU/day). Consistent responses to vitamin D
supplementation were noted across the seven trials, and some trials suggested that infants
who are vitamin D deficient may respond differently and require higher doses of vitamin
D to achieve serum 25(0H)D concentrations within the normal range.
Ottawa EPC report- Pregnant or lactating women.
There were six small RCTs of vitamin D supplementation in pregnant or lactating
women. No randomized trials studied the effect of 400 IU vitamin D
3
/d. Three trials used
1000 IU vitamin D
2
/d and one trial used 1000 IU/d of vitamin D
3
. Supplementation of
vitamin D
2
1000-3600 IU/d and vitamin D3 1000 IU/d resulted in significant increases in
serum 25(0H)D concentrations in lactating mothers and in cord blood. One trial found
that supplementation of lactating mothers with 1000 IU vitamin D
2
/d during winter
months did not significantly increase serum 25(0H)D concentrations in the infants.
Ottawa EPC report - Children and adolescents.
There were four trials that examined the effect of vitamin Don serum 25(0H)D
concentrations in children or adolescents with doses ranging from 200 to 2000 IU of
vitamin D
3
per day and 400 IU of vitamin D
2
. There were consistent increases in serum
25(0H)D concentrations ranging from 8 nmol/L (200 IU/d), 16.5 (with 600 IU D
3
/d) to
60 nmol/L (2000 IU of vitamin D3/d).
Ottawa EPC report - Premenopausal women and younger men.
Ten small trials included premenopausal women and younger males. Three trials
compared vitamin D2 to vitamin D3 in healthy young adults. Two of the three trials used
RIA, and one used HPLC to measure serum 25(0H)D concentrations The doses of
vitamin D3 ranged from 600 to 10,000 IU/day and vitamin D2 ( 4000 IU/d or 50,000 to
100,000 for single dose).
Three trials found that supplementation with vitamin D2 and D3 in healthy adults may
have different effects on serum 25(0H)D concentrations. One trial compared I 00,000 IU
vitamin D2 given orally versus injection and found a greater variability in response with
the intramuscular preparation. There appeared to be dose-response effect in those trials
that used multiple doses of vitamin D3, although there were insufficient data to perform a
meta-analysis.
Ottawa EPC report - Postmenopausal women and older men.
Forty-four trials were conducted exclusively in postmenopausal women and older
men, with 14 of these in elderly populations living in long-term care or nursing homes.
One trial enrolled only women in early menopause (n=l29). Doses of vitamin DHanged
from 100 to 4000 IU/day and vitamin D
2
was 9000 IU/day. One trial was conducted in
African American women.
One trial found that wintertime declines in serum 25(0H)D concentrations were
prevented with 500 IU vitamin D3 per day. A dose response with increasing doses of
vitamin D3 was noted for serum 25(0H)D concentrations. There was variability in
response to similar doses across trials that may have been due to differences in serum
25(0H)D assays or baseline 25(0H)D concentrations. Similarly, although some trials
reported a greater response to vitamin D in populations that were vitamin D deficient at
baseline compared to those who were not, there were insufficient data. on which to base a
definitive conclusion on this point.
291
Figure 23. Relationship between doses of Vitamin 03 supplementation and net changes in
serum 25(0H)D concentrations in RCTs
..J
-- 0
c
E
0
I
Q
l.{)
N
c
<1>
0>
c
<U
.c
(.)
-<1>
z
..J
--
0
c
E
0
I
Q
l.{)
N
c
<1>
Ol
c
<U
.c
(.)
Q)
z
100 Adults
0
0
80
60
40
20
0
0 ~ . . . . .
0 1000
100
80
60
40
20
0
0 0
0 1000
2000 3000
Vit 03 daily dose(IU)
Children
0
2000 3000
Vit 03 daily dose(IU)
4000 5000
4000 5000
Legends: Each empty circle represents one study. The area of the circle is proportional to the inverse of the within-study
variances. Typically, the larger the bubble, the larger the sample size and the smaller the standard error of the changes in
25(0H)D.
292
Figure 24. Relationship between doses of Vitamin 0
3
supplementation and net changes in
serum 25(0H)D concentrations in RCTs by baseline vitamin D status among adults
100 Adults with low 25(0H)O concentrations
_J
80
-- 0
0
c
E
0
I 60
0
Q
o
0
c0
l.{)
N
c
<1>
40
0>
c
@
<U
.c
(.)
-<1>
z
20
(9
0
0 1000 2000 3000 4000 5000
Vit 03 daily dose(IU)
100 Adults with normal/high 25(0H)O concentrations
0
0
_J
--
80
0
c
E
0
I
60
Q
l.{)
N
c
Qo
<1>
40
0
Ol
c
<U
.c
Q ) ~
(.)
Q)
0
z
20
0
0 1000 2000 3000 4000 5000
Vit 03 daily dose(IU)
Legends: Each empty circle represents one study. The area of the circle is proportional to the inverse of the within-study
variances. Typically, the larger the bubble, the larger the sample size and the smaller the standard error of the changes in
25(0H)D.
293
Figure 25. Relationship between doses of Vitamin 0
3
supplementation and net changes in
serum 25(0H)D concentrations in RCTs by durati on of supplementation among adults
.....1
:::::,
0
c
E
0
-
I
Q_
1.0
N
c
<1>
0>
c
(lj
.c.
(,)
-<1>
z
.....1
-- 0
c
E
6
:C
0
10
N
c
<1>
0>
c
(lj
.c.
(,)
-<1>
z
100 Duration of supplementation <=3 mo
80
60
0
0
40
0
20
~
0
0
0
0 1000 2000 3000 4000 5000
Vit D3 daily dose(IU)
100 Duration of supplementation >3 mo
0
0
80
60
40
20
0 ~ - - - - - - - - - - - - - - - - - - . - - - - - - - - - - . - - - - - - - - - - . - - - - - - - - - ~
0 1000 2000 3000
Vit D3 daily dose(IU)
4000 5000
Legends: Each empty circle represents one study. The area of the circle is proportional to the inverse of the within-study
variances. Typically, the larger the bubble, the larger the sample size and the smaller the standard error of the changes in
25(0H)D.
294
Table 106. The relationship between vitamin 0
3
daily doses and changes in 25(0H}D concentrations in RCTs
Author
Bjorkman
Bjorkman
Blum
Bunout
Chapuy
Chel
Deroisy
Himmelstein
Kenny
Krieg
Pfeifer
Pfeifer
Sorva
Zhu
Barnes
Bolton-Smith
Dawson-
Hughes
Harris
Heaney
Heaney
Heikkinen
Honkanen
Jensen
Nelson
Orwell
Patel
Riis
continued
Year
20082()
9
2006
80
1992
217
2002
219
1990 22()
2003
221
1999
222
2000
223
2001
97
1991
224
2008
214
2006
225
2007
213
1997
226
2002
227
2003
228
2003
228
1998
229
2002
231
2009
232
1988
233
2001
234
1984
235
Life stage
71 +
71+
71+
71+
71+
71+
71 +
71+
71 +
71+
71 +
71+
71 +
71+
adults
adults
adults
adults
adults
adults
adults
adults
adults
adults
adults
adults
adults
Base 25(0H)D,
nmoi/L
23
23
73
40
36
23
28
45
62
29
25
25
11
68
52
60
74
55
71
71
26
31
41
62
58
72
41
Vit 03 dose
(IU/d)
400
1200
700
400
800
600
200
2000
1000
880
880
800
1000
1000
600
400
700
800
1000
5000
300
1800
400
800
1000
800
2000
Ca dose
(mg/d)
0
0
1200
0
0
500
1200
1000
100
500
0
0
0
1550
1450
0
1000
0
500
295
Duration
(mo)
6
6
12
9
18
4
3
1.5
6
24
2
2
10
60
2
24
36
2
5
5
12
2.75
36
12
12
12
12
n
60
63
132
46
73
46
50
15
29
34
74
73
5
29
12
50
145
27
16
17
18
55
33
55
46
35
8
Vit 03 Ca Group
Mean
change
from
baseline
26.5
49.1
48.5
33.4
65.0
46.9
14.7
39.7
22.3
36.5
40.5
39.2
44.6
36.2
38.6
12.0
35.2
22.3
12.0
91.9
9.4
39.5
34.6
35.3
25.0
8.4
87.5
so
11.8
19.5
35.3
14.3
16.5
15.4
10.0
15.7
10.1
14.0
27.0
22.4
28.9
27.5
15.1
15.1
32.6
14.0
16.0
37.6
10.9
12.1
23.2
23.2
19.1
13.1
14.1
Placebo or Ca Group
n
59
59
125
46
69
45
50
15
31
38
74
72
10
34
15
56
167
23
16
16
18
60
33
31
46
35
7
Mean
change
from
baseline
1.9
1.9
9.3
3.5
-4.5
0.3
4.5
-2.7
-2.5
-15.0
18.3
19.7
-1.4
-2.9
-7.2
-8.2
-2.1
-4.6
-11.4
-11.4
-3.3
-13.1
16.5
10.9
3.0
-9.2
-5.0
so
10.2
10.2
21 .5
10.0
13.5
12.2
10.0
13.4
11.4
11.1
20.9
23.8
2.3
27.4
11.3
14.3
22.7
6.3
17.6
17.6
6.4
9.2
28.2
16.9
19.1
12.8
23.8
Vit D3 Ca Group Placebo or Ca Group
Author Year life stage
Base 25(0H)D, Vit 03 dose Ca dose Duration
Mean Mean
nmoi/L (IU/d) (mg/d) (mo)
change change
n
from
so n
from
so
baseline baseline
Trang 1998
236
adults 42 4000 0 0.5 24 23.3 17.5 24 3.0 19.8
Chan 1982
237
children 43 400 0 6 30 22.5 6.6 30 2.5 6.6
EI-Hajj
2006
35
(Fuleihan) children 35 200 0 12 58 7.5 19.8 55 5.0 18.8
EI-Hajj
2006
35
(Fuleihan) children 35 2000 0 12 55 59.9 67.1 55 5.0 18.8
A Calcium supplement was given to all pati ents
The format of t his table has been slightly modifies to fit each RCT in one line.
296
Outcomes for Tolerable Upper Intake Levels
We included only clinical outcomes oftolerable upper intake levels, such as all-cause
mortality, cancer (incidence and mortality), soft tissue calcification, renal outcomes, and
adverse events reported in RCTs.
Results of all-cause mortality and cancer have been described in previous sections. In
brief, we did not find vitamin D and/or calcium associated with an increased risk of
mortality. For cancer risk, there were some observational studies reporting high calcium
intake may be associated with an increased risk of prostate cancer (see "Prostate cancer"
in "Calcium and cancer" section). We did not identify any studies on soft tissue
calcification and tolerable upper intake levels.
Renal Outcomes
The WHI trial on women aged 50 to 79 years, examined the effect of vitamin D3 400
IU (the Recommended Dietary Allowance for women aged 50 to 70 years and below the
600 IU recommended intake for women > 70 years) in combination with 1000 mg
calcium carbonate versus placebo and found an increase in the risk of renal stones
(Hazard Ratio 1.17 95 percent CI 1.02, 1.34), corresponding to 5.7 events per 10,000
person years of exposure.
71
It should be noted that women in both groups were allowed to
take additional vitamin D supplements up to 600 IU and later 1000 IU per day and
calcium supplements up to 1000 mg per day. The baseline total calcium intakes (from
foods and supplements) were high: 34 percent consumed less than 800 mg/d, 26 percent
consumed 800 to 1200 mg/d, and 40 percent consumed more than 1200 mg/d. A prior
publication from WHI trial provided the same data on the risk of renal stones was also
included in the Ottawa EPC report.
No studies were identified that evaluated the effect of vitamin D, calcium, or
combined vitamin D and calcium on other renal outcomes.
Adverse Events Reported in RCTs.
The reporting of adverse events in RCTs was generally inadequate, and most trials
were not adequately powered to detect adverse events. Among the 63 RCTs included in
this report, 47 did not report infonnation on adverse events.
Five RCTs (in 6 publications) that enrolled a total of 444 subjects reported no adverse
events during the trial periods.
35
51
227
238
239
Of these, one RCT administered combination
of vitamin D
2
(1600 or 3600 IU/d) and vitamin D
3
(400 IU/d) supplements for 3 months,
two RCTs administered vitamin D supplements (type of vitamin D not reported) with
doses ranging from 200 to 2000 IU/d for 3 weeks or 1 year, one RCT used high-dose
intermittent vitamin D
3
supplement ('120,000 ru sachets given 3 times, every 2 weeks, for
6 weeks), and one RCT administered 1200 IU/d vitamin D
2
supplement for 5 years.
Eleven RCTs reported at least one adverse event (Table 1 07). Excessive gas, bloating,
and gastrointestinal discomforts were reported to be associated with calcium
supplementation (doses ranged from 600 to 1000 mg/d). Other RCTs of vitamin D (doses
ranged from 400 to 5714 IU/d vitamin D
3
or ranged from 5000 to 10,000 vitamin D
2
)
and/or calcium supplementations (doses ranged from 200 to 1500 mg/d) reported few
297
cases of gastrointestinal disruption such as constipation, diarrhea, upset stomach,
musculoskeletal soreness, primary hyperparathyroidism, hypercalcemia, renal calculi and
craniotabes. One RCT reported some adverse events that required hospital admission,
including retrosternal pain, a non-ST elevation myocardial infarction and a transient
ischemic attack (all 3 cases in vitamin D 400 IU/d plus exercise training group) and one
case of acute cholecystitis (in calcium, vitamin D plus exercise training group).
80
Another
RCT reported that "there were no significant differences between the vitamin D and the
control groups in the rate of incident cancer and vascular disease (ischemic heart disease
and stroke)" (actual data not provided), and one participant died during the study.
98
However, these adverse events may or may not be associated with vitamin D and/or
calcium supplementation in this study. Also described earlier in the "Renal outcomes"
section, the WHI trial examined the effect of vitamin D3 400 fU in combination with
1000 mg calcium carbonate versus placebo and found an increase in the risk of renal
stones (Hazard Ratio 1. 17 95 percent CI 1.02, 1.34), corresponding to 5.7 events per
10,000 person years of exposure.
71
Ottawa EPC report:
A total of22 trials reported data on toxicity-related outcomes, 21 of which used doses
above 400 IU/d. Toxicity results from trials with intakes of vitamin D above current
reference intakes varied and this may have been related to different doses, baseline
characteristics of populations or exposure times. Most trials excluded subjects with renal
insufficiency or hypercalcemia, were of small sample sizes and had short durations of
exposure to vitamin D. Event rates were low across trials in both the treatment and
placebo arms.
298
Table 107. Adverse events reported in RCTs
Author Year N enrolled Vit D dose (IU/d) Ca dose (mg/d) Duration Adverse Event data (n=case#)
Yamamoto 1995
117
471 0 1000 6mo Comparing calcium group to the placebo group, excessive gas and bloating
were more frequently reported by white women at 3 months and by whites,
in general, at 6 months, and white men reported more loose stools at 6
months.
Moschonis 2006
215
112 300 0 3 600 or 1200 12 mo Bloating, constipation and intestinal discomfort apparently related to the
calcium su lement
Bunout 2006 so 96 400 800 9mo Adverse events that required hospital admission:
Vit 0 plus exercise training group (n=3): retrosternal pain, a non-ST
elevation myocardial infarction and a transient ischemic attack.
Calcium, Vit 0 plus exercise training group (n=1 ): acute cholecystitis
Wactawski-Wende 36282 400 1000 7y The WHI trial found an increase in the risk of renal stones (Hazard Ratio
2006
71
1.17 95% Cl 1.02, 1.34), corresponding to 5.7 events per 10,000 person
ears of ex osure.
Burleigh 2007
51
205 800 0 3 1200 Median 1 Hypercalcemia (n=2)
mo
Lappe 2008
2011
5201 800 200 8wks Gl disruption such as constipation, diarrhea, upset stomach (4%), and
musculoskeletal soreness (0.9%)
Brooke 1980
34
126 1000 0
3rd
Vit 0 group (craniotabes, n=2), placebo group (hypocalcemia, n=5;
trimester craniotabes, n=6)
on I
Lappe 2007
52
1180 1000 03 1400-1500 4y Renal calculi in placebo (n=1), renal calculi in calcium only (n=3), renal
calculi in calcium plus vit 0 (n=1)
Mastaglia 2006
240
65 5000 or 10,000 0 2 500 3 mo Hypercalciuria (n=1) in control group
Zhu2008
98
256 1000 02 1200 12 mo There were no significant differences between the vitamin 0 and the control
groups in the rate of incident cancer and vascular disease (ischemic heart
disease and stroke).
There were 8 and 5 adverse events in vitamin 0 and the control groups,
respectively. One participant in the vitamin 0 group had mild asymptomatic
hypercalcemia one occasion. No case of renal calculus was reported.
1 participant was deceased during the study.
Sneve 2008
50
445 Group 1: 2 capsules of 500 12 mo Primary hyperparathyroidism (n=2), increase in serum calcium to 2.62
vitamin 0
3
each mmoi/L (n=1 ), transient increases in serum calcium > 2.59 mmoi/L (n=4).
20,000 IU taken twice
a week (Monday and
317 other adverse events were recorded, most of them related to Gl
Thursday): - 571 4 IU/d
discomfort. There were no significant differences between the treatment
Group 2: 1 capsules of
groups regarding adverse events.
vitamin 0
3
each
20,000 IU taken twice
a week (Monday and
Thursda : -2857 1U/d
299
300
Chapter 4. Discussion
This evidence report on vitamin D and calcium in relation to health outcomes was prepared
for consideration by the Committee on Dietary Reference Intakes for Vitamin D and Calcium at
the request of AHRQ on behalf of the various sponsors. This report does not make nor was it
intended to make recommendations for DRI values concerning vitamin D or calcium.
Responsibility for setting DRI values lies with the Committee. Evidence from systematic reviews
is one of several types of information available to the Committee for use in its deliberations to
establish DRI values. This is the first time that an independent systematic review is being
commissioned to support the DRl process. Thus, it is important for users of this report to fully
appreciate the nuances of the methodologies employed, as well as the strengths and limitations of
this approach. In particular, it should be noted that total vitamin D exposure was not evaluated in
this report because there is no valid method to quantify the contribution of endogenous vitamin
D synthesis resulting from sun exposure and it is also the TEP's consensus that vitamin D intake,
as estimated by current food frequency questionnaires, is too inaccurate to be of value.
For this report, we identified 165 primary articles that met the eligibility criteria established
by the TEP. In addition, we included 11 published systematic reviews that incorporated over 200
additional primary articles. Despite the relatively large number of studies included, with the
following few exceptions, it is difficult to make any substantive and concise statements on the
basis of the available evidence concerning the association of serum 25(0H)D concentration,
supplemental vitamin D, dietary calcium intake, or the combination of both nutrients with the
various health outcomes. It proved challenging because many of the studies contained substantial
heterogeneity and their findings were inconsistent for the health outcomes examined.
In general, among RCTs ofhypertensive adults, calcium supplementation (400 to 2000 mg/d)
lowered systolic, but not diastolic, blood pressure by a small but statistically significant amount
(2 to 4 mm Hg).
For body weight, despite a wide range of calcium intakes (from supplements or from dairy
and nondairy sources) across the calcium trials, the RCTs were fairly consistent in finding no
significant effect of increased calcium intake on body weight.
For growth, a meta-analysis of 17 RCTs did not find a significant effect on weight and height
gain attributable to calcium supplement in children ranged from 3 to 18 years of age.
For bone health, one well-conducted systematic review ofRCTs found that vitamin D
3
(up to
800 IU/d) plus calcium ( - 500 mg/d) supplementation resulted in small increases in BMD of the
spine, total body, femoral neck, and total hip in populations consisting predominantly of women
in late menopause.
For breast cancer, subgroup analyses in four cohort studies consistently found that calcium
intake in the range of780 to 1750 mg/d in premenopausal women was associated with a
decreased risk for breast cancer. However, no RCTs of calcium supplementation to prevent
breast cancer in premenopausal women have been published. In contrast, cohort studies of
postmenopausal women are consistent in showing no association of calcium intake with the risk
of breast cancer.
For prostate cancer, three of four cohort studies found significant associations between
higher calcium intake(> 1500 or >2000 mg/day) and increased risk of prostate cancer, compared
to men consuming lower amount of calcium (500-1 000 mg/day).
For cardiovascular events, a cohort study and a nested case-control study found associations
between lower serum 25(0H)D concentrations (less than either about 50 or 75 nmol/L) and
311
increased risk of total cardiovascular events; however an RCT found no effect of
supplementation and studies of specific cardiovascular events were too sparse to reach
conclusions. Taken together, six cohort studies of calcium intake suggest that in populations at
relatively increased risk of stroke and with relatively low dietary calcium intake (i.e., in East
Asia), lower levels of calcium intake under about 700 mg/day are associated with higher risk of
stroke. This association, however, was not replicated in Europe or the US, and one Finnish study
found a possible association of increased risk of stroke in men with calcium intakes above 1000
mg.
Studies on the association between either serum 25(0H)D concentration or calcium intake
and other forms of cancer ( colorectum, pancreas, prostate, all-cause); incidence of hypertension
or specific cardiovascular disease events; immunologic disorders; and pregnancy-related
outcomes including preeclampsia were either few in number or reported inconsistent findings.
Too few studies of combined vitamin D and calcium supplementation have been conducted to
allow adequate conclusions about its possible effects on health. The WHI trial was commonly
the only evidence available for a given outcome.
Strengths of This Report
The strengths of this report lie in the wide range of topics covered, critical appraisal, detailed
documentation, transparent methods to assess the scientific literature, and an unbiased selection
of studies. A team of evidence-based methodologists not previously directly involved in research
related to vitamin D and calcium worked with nutrient experts to refine the key questions
(initially defined by AHRQ with input from various sponsors), analytic framework, and review
criteria for the systematic review. After defining the questions and eligibility criteria with input
from content experts and the sponsoring agencies, the Tufts EPC reviewed the published
evidence on the topic. The intent was to perform a thorough and unbiased systematic review of
the literature base on available evidence as defined by prespecified criteria. Once the review
process began, input from experts in the field was sought to clarify technical questions during the
literature review process. These individuals did not participate in study selection or detailed data
extraction from the included studies nor were any members serving on the IOM committee on
vitamin D and calcium involved in the review of this document. A quality rating as detailed in
Chapter 2 (Methods section) was assigned for each primary study and systematic review, and
incorporated into the data summaries section of the report. On the basis of this work, a sound
foundation has been created which will facilitate rapid and efficient future updates as needed.
Details concerning the process of question formulation, selection of health outcomes of
interest, justification for study selection criteria, methods used for critical appraisals of studies
and quality rating, and summary of results are described fully in the Methods chapter. This
approach is critical to the establishment of a transparent and reproducible process. Furthermore,
important variables that affect vitamin D status such as life stages, latitude of the study locale,
background diet and skin pigmentation are documented in this review.
This evidence report was carried out under the AHRQ EPC program, which has a 12-year
history of producing over 175 evidence reports and numerous technology assessments for
various users including many federal agencies. EPCs are staffed by experienced methodologists
who continuously refine approaches to conducting systematic reviews and develop new methods
on the basis of accumulated experience encompassing a wide range of topics. In addition, the
Tufts EPC has conducted a number of nutrition-related evidence reports
19
-
22
241
, as well as
312
conducted the mock exercise on vitamin A panel.
3
This report drew on these experiences, the
expertise of the TEP, and the support of federal agencies.
DRI and the Literature on Vitamin D and Calcium
It should be emphasized that none of the studies reviewed were designed to address issues
specifically relevant for establishing DRI values (i.e., to ascertain the optimal dose in a particular
life stage to promote growth and tissue maintenance, and prevent chronic disease throughout the
lifecycle). In general, the studies did not enroll subjects with ages that could be easily mapped to
specific life stages as defined within the DRI framework (with the exception of postmenopausal
women and pregnant or lactating women) and did not evaluate health outcomes on the basis of
what doses will lower risk for a particular disease in prespecified life stages. Therefore, data will
need to be extrapolated from these studies to craft a set of DRI values for vitamin D and calcium.
This extrapolation may prove challenging.
Certain issues concerning the studies of vitamin D must be noted. As mentioned previously,
it is difficult to evaluate nutritional adequacy because there are no methods currently available to
quantify the contribution of endogenous vitamin D synthesis resulting from sun exposure on an
individual or group level. In addition, it is generally accepted that estimating intake by dietary
assessments is not a valid indicator of vitamin D status, because there are limitations in the
completeness of nutrient databases for both food and dietary supplements vitamin D content and
the rapidly changing landscape of vitamin D food fortification has not yet been captured in either
instruments used to assess intake and the databases used to analyze the data. For example,
vitamin D values are available for only about 600 out of 1400 foods in the USDA National
Nutrient Database for Standard Reference (http://www.ars.usda.gov/nutrientdata) and notably
missing are foods recently fortified with vitamin D?
5
Given the recent trend towards increased
nutrient fortification of the North American food supply, the lag in updating food composition
tables, and the inability to distinguish between fortified and unfortified foods when using most
dietary assessment tools, it is difficult to accurately estimate dietary intakes of vitamin D,
especially for a given year. Shifts in methodological approaches to measure serum 25(0H)D
concentrations, the heterogeneous nature of the data available with respect to study locations
(i.e., latitude) and times during the year (i.e., season) hamper our ability to succinctly sununarize
dose-response relationships. We did not perform a dose-response meta-analysis of the
relationship between serum 25(0H)D concentrations and health outcomes because limited and
inconsistent data would result in a meta-analysis that is difficult to interpret and results that may
be misleading. Furthermore, many of the large cohorts analyzed for associations of vitamin D
with health outcomes enrolled mostly white participants aged approximately 40 to 70 years old
and much of the data on intake dose-response and serum 25(0H)D concentration were derived
from studies designed to measure bone health in postmenopausal women. These factors limit the
applicability of the findings to other life stages and other racial groups.
Unlike serum 25(0H)D concentrations for vitamin D, there is no equivalent serum biomarker
to indicate calcium status. Relying on dietary assessment to gauge calcium intake is limited by
the confounding effect of vitamin D status on the efficiency of calcium absorption and
uncertainties in the calcium content of many foods due to the recent trend in nutrient fortification
of food, limited ability of current dietary assessment tools to distinguish among fortified and
unfortified foods and the lag in updating nutrient databases with current nutrient information.
313
Limitations of our Methodological Approach
The number of potentially relevant (English language articles on humans and not reviews)
vitamin D studies indexed in MEDLINE is very large and the number of calcium
studies is even larger ( 11 0,000). Without unlimited time and resources, the systematic review
conducted in this report had to focus on selected key questions predefined by our federal
sponsors with input from the TOM, and capitalize on systematic reviews. Using previous
systematic reviews risks propagating deficiencies and errors
42
introduced in those reviews (e.g.,
errors in data abstraction, flawed assumptions in quantitative synthesis). Although we have
assessed the quality of these systematic reviews using AMSTAR
26
checklist, we cannot reliably
know the validity of the reported summary data without knowing the details of the primary
studies. It should also be stressed that a well-performed systematic review does not necessarily
imply that the body of evidence for a particular outcome of interest is of high quality. While
some systematic reviews assessed the quality of the individual studies, the methods used varied.
Any systematic review is limited by the quality of the primary studies included in the review.
Unless the methods used to assess the quality of the primary studies is transparent and the details
made available for examination, it would be difficult to reliably determine the validity of the
conclusions. Also, relying on existing systematic reviews alone could have potentially precluded
us from identifying all relevant studies because those systematic reviews might have addressed
somewhat different questions and had a different scope from this review. For example, for
growth outcome in children, we principally relied on the findings from a meta-analysis of RCTs
of calcium originally designed to evaluate bone density outcomes. If there were RCTs of calcium
intake specifically designed to measure growth outcomes such as weight and height gain, but not
bone density, then those studies would not have been identified. In addition, as per the task order
from AHRQ, we relied on the Ottawa report for bone health outcomes and we did not examine
specific studies included in that report. As a consequence, if those studies had reported other
(than bone health) outcomes that were of interest, those studies would not have been included in
this review.
As there is no consensus on how to assess the quality of the nutrition observational studies,
we created a quality checklist based on a newly published reporting standard for observational
studies
32
and nutrition reporting items that we believe should be considered in qual ity
assessment. This checklist, however, has not been calibrated and the intra- and interrater
variability have not been assessed. We should also remind the readers that impeccable study
reporting does not equate study validity. However, transparent, comprehensive, and accurate
reporting does help in evaluating a study' s validity.
Also, studies on vitamin D and calcium were not specifically targeted at life stages (except
for children, pregnant, and postmenopausal women) specified for the determination ofDRI. We,
therefore, were unable to structure our report strictly according to prespecified life stages. When
a study enrolled populations that spanned across multiple life stages, we provided our best
estimates as to which life stage(s) the study's findings would be of most relevance.
Comments on the Observational Studies
All the included observational studies were designed to generate hypotheses of potential
associations of multiple factors with vitamin D or calcium. Therefore, a finding of a significant
association in these studies, after exploratory analyses, should not be considered equivalent to
314
the result of studies that were designed to confirm this relationship. Many of the nested case-
control studies typically excluded a substantial portion of participants (some as high as 60 to 70
percent) in the original cohorts because blood samples, or completed dietary questionnaires were
not available. How this selection bias would affect the reported association is unclear. In
addition, several of the studies might have suffered from outcome rnisclassification; for example,
when cancer cases were identified from registries without histopathology verification. The effect
of outcome misclassification is unpredictable. Furthermore, many of the studies did not report a
power calculation. Even though many of the studies included cohorts with relatively large
numbers of subjects (tens of thousands), it is plausible that, in fact, the included studies may
have been underpowered to detect the true effect sizes. If that were the case, the significant effect
reported may, in fact, be spurious. Furthermore, many ofthe reported effect sizes were small to
moderate (with OR ranged from 1.03 to 2.0). When the effect size is small, the possibility of
residual confounding by unmeasured variables must be considered.
Sources of Heterogeneity and Potential Biases
As have been mentioned previously, most of the findings reported in this review were
inconsistent for each of the outcomes of interest. Many studies showed substantial heterogeneity.
Some studies adjusted the serum 25(0H)D concentration by season of serum collection, some
did not. While the majority of the studies used some forms ofRIA to measure the serum
25(0H)D concentration, a minority used competitive protein-binding assay. Some studies
reported a substantial proportion of the frozen serums were accidentally thawed and limited the
analyses that could be performed. It is unclear how this would alter the overall results. Many
studies suffered from potentially inadequate outcome ascertainment (e.g., reliance on self-
reported calcium intake and hypertension diagnosis). Time between measurement of serum
25(0H)D concentration and the diagnosis of interest varied. For prostate and colorectal cancer, it
ranged from 1 to more than 16 years. Factors potentially relevant to the outcomes of interest like
family history (in colorectal cancer) were not consistently reported and accounted for in the
studies. Also, the blinding of case assessors to the risk factor of interest (e.g., serum 25(0H)D
concentrations) as well as that of investigators who measured the risk factor per se to outcomes
were rarely reported.
For studies on calcium supplementation, intake compliance, information on the
bioavailability of the calcium source, the role of background sun exposure, and associated
vitamin D effects were not consistently available across all studies. Thus, it is difficult to
interpret those fmdings on an absolute level and among studies.
Finally, all systematic reviews, including this report, may suffer from potential publication
and reporting biases since currently there is no reliable way to detect and correct these biases.
However, there is an underlying suspicion of publication bias against studies having either null
or negative outcomes and reporting bias toward "significant" outcomes in the literature.
243
'
244
Thus, it is important to consider these biases when reviewing the overall findings of any
systematic review.
Vitamin D Intake and Response in Serum 25(0H)D Concentration
The findings of this review on the association between vitamin D intake dose and change in
serum 25(0H)D concentration was primarily derived from RCTs reviewed in a systematic
review of bone health in postmenopausal women. This limits the applicability of the findings to
315
other life stages. Though, we did not find any reason to consider these trials to be biased, they
are nonetheless an arbitrary sample of all studies that have reported the association between
vitamin D intake dose and change in serum 25(0H)D concentration. We did not perform a
quantitative synthesis (e.g., meta-regression) to examine the relationship between vitamin D
intake dose and serum 25(0H)D concentration due to the heterogeneity across studies. Studies
had varied compliance rates in the vitamin D intake; limited or no adjustment for skin
pigmentations, calcium intake, or background sun exposure; different vitamin D assay
methodologies and measurement (both intra- and interassay) variability. All these factors
increase the heterogeneity and limit the usefulness of an overall summary estimate for an intake
dose response in serum 25(0H)D concentration. Nonetheless, overall, there appeared to be a
trend for higher vitamin D supplementation dose resulting in higher net change in serum
25(0H)D concentration.
Considerations for Future DRI Committees
Formulating the appropriate key questions is the most important aspect of conducting a
systematic review to ensure the final product will meet the intended purpose. Ideally, this should
be an iterative process involving the sponsors, EPC, TEP and targeted end-users. The questions
should be reviewed and potentially refined once the "state" of the literature has been
systematically appraised, with the understanding that any modifications to the key questions after
the review process has started will likely extend the literature review and synthesis processes. In
addition, developing relevant study selection criteria for the systematic review is critical to
fmding pertinent data to answer the key questions; the TEP should be engaged early in this
process. Crafting a framework of the entire review process depicting the explicit roles of the
sponsors, TEP, and targeted end-users could also be helpful for future reviews.
While the process of conducting the actual systematic review of a nutrient or group of
nutrients on an agreed upon set of key questions concerning specific health outcomes is carefully
laid out and could be replicated without undue difficulty, the process of selecting which health
outcomes would be important for inclusion in a systematic review could not be easily replicated.
The health outcomes selected were decided after much deliberation by the TEP with input from
the various partners. As the nature of the deliberation hinged much on the expertise reflected by
the particular composition of the TEP, it is conceivable that a different TEP composed of
members with different expertise may have recommended a different set of health outcomes for
inclusion. To minimize this variability, an a priori designed set of instructions to weigh each
outcome (taking into account such factors like population attributable risk, morbidity, and others)
for possible inclusion would be valuable.
316
Reference
( 1) Dietary reference intakes : the essential guide to nutrient requirements. Institute of
Medicine (IOM). The National Academy Press. ; 2006.
(2) The development of DR!s 1994-2004: lessons learned and new challenges: workshop
summary. Institute of Medicine (IOM). The National Academies Press.; 2007.
(3) Russell R, Chung M, Balk EM et al. Opportunities and challenges in conducting
systematic reviews to support the development of nutrient reference values: vitamin
A as an example. Am J Clin Nutr. 2009;89:728-733.
( 4) Vitamin D and Health in the 21st Century: an Update. Proceedings of a conference held
September 2007 in Bethesda, Maryland, USA. Am J Clin Nutr. 2008;88:483S-592S.
(5) Yetley EA, Brule D, Cheney MC et al. Dietary Reference Intakes for vitamin D:
justification for a review of the I 997 values. Am J Clin Nutr. 2009;89:7 19-727.
(6) Cranney A, Horsley T, O'Donnell Setal. Effectiveness and safety of vitamin Din
relation to bone health. Evidence Report/Technology Assessment. 2007;158: 1-235.
(7) Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-281.
(8) DeLuca HF. Overview of general physiologic features and functions of vitamin D. Am J
Clin Nutr. 2004;80:1689S-1696S.
(9) Townsend K, Evans KN, Campbell MJ, Colston KW, Adams JS, Hewison M. Biological
actions of extra-renal 25-hydroxyvitamin D-1 alpha-hydroxylase and implications for
chemoprevention and treatment. J Steroid Biochem Mol Bioi. 2005;97: 103-109.
( l 0) Norman A W. A vitamin D nutritional cornucopia: new insights concerning the serum
25-hydroxyvitamin D status of the US population. Am J Clin Nutr. 2008;88: 1455-
1456.
(1 1) Bikle D. Nonclassic actions of vitamin D. J Clin Endocrinol Metab. 2009;94:26-34.
(12) White JH. Vitamin D signaling, infectious diseases, and regulation of innate immunity.
Infect lmmun. 2008;76:3837-3843.
(13) Mohr SB. A brief history of vitamin d and cancer prevention. Ann Epidemiol.
2009; 19:79-83.
(14) Dawson-Hughes B. Serum 25-hydroxyvitamin D and functional outcomes in the elderly.
Am J Clin Nutr. 2008;88:537S-540S.
(15) Buell JS, wson-Hughes B. Vitamin D and neurocognitive dysfunction: preventing
"D"ecline? Mol Aspects Med. 2008;29:4 1 5-422.
317
(16) Quarles LD. Endocrine functions of bone in mineral metabolism regulation. J Clin
Invest. 2008;118:3820-3828.
(17) Hewison M. Vitamin D and innate immunity. Curr Opin lnvestig Drugs. 2008;9:485-
490.
(18) Bucher HC, Guyatt GH, Cook DJ, Holbrook A, McAlister FA. Users' guides to the
medical literature: XIX. Applying clinical trial results. A. How to use an article
measuring the effect of an intervention on surrogate end points. Evidence-Based
Medicine Working Group. lAMA. 1999;282:771-778.
(19) BalkE, Chung M, Chew P, IpS, Raman G, Kupelnick B, Tatsioni A, SunY, Wolk B,
DeVine D, and Lau J. Effects of Soy on Health Outcomes. Evidence
Report/Technology Assessment No. 26 (Prepared by Tufts-New England Medical
Center Evidence-based Practice Center under Contract No. 290-02-0022). AHRQ
Publication No 05-E024-l. 2005. Rockville, MD, Agency for Healthcare Research
and Quality.
RefType: Report
(20) Balk, E, Chung, M, Raman, G, Tatsioni, A, Chew, P, Ip, S, DeVine, D, and Lau, J. B
Vitamins and Berries and Age-Related Neurodegenerative Disorders. Evidence
Report/Technology Assessment No. 134 (Prepared by Tufts-New England Medical
Center Evidence-based Practice Center under Contract No. 290-02-0022). AHRQ
Publication No 05-E008. 2006. Rockville, MD, Agency for Healthcare Research and
Quality.
RefType: Report
(21) Balk E, Chung M, Lichtenstein A et al. Effects of omega-3 fatty acids on cardiovascular
risk factors and intermediate markers of cardiovascular disease. Evidence
Report/Technology Assessment No. 93 (Prepared by Tufts-New England Medical
Center Evidence-based Practice Center under Contract No. 290-02-0022). AHRQ
Publication No. 04-EOJ0-2. Rockville, MD: Agency for Healthcare Research and
Quality. 2004.
(22) Ip, S., Chung, M., Raman, G. , Chew, P., Magula, N., DeVine, D. , Trikalinos, T., and
Lau, J. Breastfeeding and Maternal and Infant Health Outcomes in Developed
Countries. Evidence Report/Technology Assessment No. 153 (Prepared by Tufts-
New England Medical Center Evidence-based Practice Center under Contract No.
290-02-0022). AHRQ Publication No 07-E007. 4-20-2007. Rockville, MD, Agency
for Healthcare Research and Quality.
RefType: Report
(23) Jordan H, Matthan N, Chung Metal. Effects of omega-3 fatty acids on arrhythmogenic
mechanisms in animal and isolated organ/cell culture studies. Evidence
Report/Technology Assessment No. 92 (Prepared by Tufts-New England Medical
Center Evidence-based Practice Center under Contract No. 290-02-0022). AHRQ
318
Publication No. 04-EO 11-2. Rockville, MD: Agency for Healthcare Research and
Quality. 2004.
(24) Wang C, Chung M, Lichtenstein A et al. Effects of omega-3 fatty acids on
cardiovascular disease. Evidence Report/Technology Assessment No. 94 (Prepared
by Tufts-New England Medical Center Evidence-based Practice Center under
Contract No. 290-02-0022). AHRQ Publication No. 04-E009-2. Rockville, MD:
Agency for Healthcare Research and Quality. 2004.
(25) Holden JM, Lemar LE. Assessing vitamin D contents in foods and supplements:
challenges and needs. Am J Clin Nutr. 2008;88:551 S-553S.
(26) Shea BJ, Grimshaw JM, Wells GA et al. Development of AMSTAR: a measurement
tool to assess the methodological quality of systematic reviews. BMC Med Res
Methodol. 2007;7:10.
(27) Ballantyne JC, Carr DB, deFerranti Setal. The comparative effects of postoperative
analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized,
controlled trials. Anesth Analg. 1998;86:598-612.
(28) DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials.
1986;7:177-188.
(29) Higgins JP, Whitehead A, Turner RM, Omar RZ, Thompson SG. Meta-analysis of
continuous outcome data from individual patients. Stat Med. 2001;20:2219-2241.
(30) Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-
analyses. BMJ. 2003;327:557-560.
(31) Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations
for improving the quality of reports of parallel-group randomised trials. Clin Oral
lnvestig. 2003;7:2-7.
(32) von EE, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)
statement: guidelines for reporting observational studies. Lancet. 2007;370: 1453-
1457.
(33) Chung M, Balk EM, Ip S et al. Reporting of systematic reviews of micronutrients and
health: a critical appraisal. Am J Clin Nutr. 2009;89: 1099-1113.
(34) Brooke OG, Brown IR, Bone CD et al. Vitamin 0 supplements in pregnant Asian
women: effects on calcium status and fetal growth. BMJ. 1980;280:751-754.
(35) El-Hajj FG, Nabulsi M, Tamim H et al. Effect of vitamin D replacement on
musculoskeletal parameters in school children: a randomized controlled trial. J Clin
Endocrinol Metab. 2006;91 :405-412.
319
(36) Feliciano ES, Ho ML, Specker BL et al. Seasonal and geographical variations in the
growth rate of infants in China receiving increasing dosages of vitamin D
supplements. J Trop Pediatr. 1994;40:162-165.
(37) Marya RK, Rathee S, Dua V, Sangwan K. Effect of vitamin D supplementation during
pregnancy on foetal growth. Indian J Med Res. 1988;88:488-492.
(38) Maxwell JD, Ang L, Brooke OG, Brown IR. Vitamin D supplements enhance weight
gain and nutritional status in pregnant Asians. BJOG. 1981 ;88:987 -991.
(39) Wagner CL, Hulsey TC, Fanning D, Ebeling M, Hollis BW. High-dose vitamin D3
supplementation in a cohort of breastfeeding mothers and their infants: a 6-month
follow-up pilot study. Breastfeed Med. 2006; 1:59-70.
(40) Mallet E, Gugi B, Brunelle P, Henocq A, Basuyau JP, Lemeur H. Vitamin D
supplementation in pregnancy: a controlled trial of two methods. Obstet Gynecol.
1986;68:300-304.
(41) Marya RK, Rathee S, Lata V, Mudgil S. Effects of vitamin D supplementation in
pregnancy. Gynecol Obstet Invest. 1981;12:155-161.
(42) Gale CR, Robinson SM, Harvey NC et al. Maternal vitamin D status during pregnancy
and child outcomes. Euro J Clin Nutr. 2008;62:68-77.
( 43) Morley R, Carlin JB, Pasco JA, Wark JD. Matemal25-hydroxyvitamin D and
parathyroid hormone concentrations and offspring birth size. J Clin Endocrinol
Metab. 2006;91 :906-912.
(44) Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol)
supplementation on fractures and mortality in men and women living in the
community: randomised double blind controlled trial. BMJ. 2003;326:469.
(45) Wang TJ, Pencina MJ, Booth SL et al. Vitamin D deficiency and risk of cardiovascular
disease. Circulation. 2008; 117:503-511.
(46) Giovann.ucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of
myocardial infarction in men: a prospective study. Arch lnt Med. 2008; 168:1174-
1180.
(47) Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of
mortality in the general population. Arch Int Med. 2008;168:1629-1637.
( 48) Marniemi J, Alan en E, Jmpivaara 0 et al. Dietary and serum vitamins and minerals as
predictors of myocardial infarction and stroke in elderly subjects. Nutr Metab
Cardiovasc Dis. 2005;15:188-197.
( 49) Heikkinen AM, Tuppurainen MT, Niskanen L, Komulainen M, Penttila I, Saarikoski S.
Long-term vitamin D3 supplementation may have adverse effects on serum lipids
320
during postmenopausal hormone replacement therapy. Eur J Endocrinol.
1997;137:495-502.
(50) Sneve M, Figenschau Y, Jorde R. Supplementation with cholecalciferol does not result
in weight reduction in overweight and obese subjects. Euro J Endocrinol.
2008;159:675-684.
(51) Nagpal J, Pande JN, Bhartia A. A double-blind, randomized, placebo-controlled trial of
the short-term effect of vitamin D3 supplementation on insulin sensitivity in
apparently healthy, middle-aged, centrally obese men. Diabet Med. 2009;26: 19-27.
(52) Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP. Vitamin D and
calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin
Nutr. 2007;85: 1586-1591.
(53) Freedman DM, Looker AC, Chang SC, Graubard BI. Prospective study of serum
vitamin D and cancer mortality in the United States. J Nat! Cancer Inst.
2007;99: 1594-1602.
(54) Ahn J, Peters U, Albanes D et al. Serum vitamin D concentration and prostate cancer
risk: a nested case-control study. J Natl Cancer lnst. 2008; 100:796-804.
(55) Ahonen MH, Tenkanen L, Teppo L, Hakama M, Tuohimaa P. Prostate cancer risk and
prediagnostic serum 25-hydroxyvitamin D levels (Finland). Cancer Causes Control.
2000;11 :847-852.
(56) Baron JA, Beach M, Wallace Ketal. Risk of prostate cancer in a randomized clinical
trial of calcium supplementation. Cancer Epidemiol Biomarkers Prev. 2005;14:586-
589.
(57) Braun MM, Helzlsouer KJ, Hollis BW, Comstock GW. Prostate cancer and
prediagnostic levels of serum vitamin D metabolites (Maryland, United States).
Cancer Causes Control. 1995;6:235-239.
(58) Corder EH, Guess HA, Hulka BS et al. Vitamin D and prostate cancer: a prediagnostic
study with stored sera. Cancer Epidemiol Biomarkers Prev. 1993;2:467-472.
(59) Jacobs ET, Giuliano AR, Martinez ME, Hollis BW, Reid ME, Marshall JR. Plasma
levels of 25-hydroxyvitamin D, 1 ,25-dihydroxyvitamin D and the risk of prostate
cancer. J Steroid Biochem Mol Biol. 2004;89-90:533-537.
(60) Li H, Stampfer MJ, Hollis JB et al. A prospective study of plasma vitamin D
metabolites, vitamin D receptor polymorphisms, and prostate cancer. PLoS Medicine
I Public i b r a ~ y ofScience. 2007;4:e103.
(61) Mikhak B, Hunter DJ, Spiegelman D, Platz EA, Hollis BW, Giovannucci E. Vitamin D
receptor (VDR) gene polymorphisms and haplotypes, interactions with plasma 25-
321
hydroxyvitamin D and 1,25-dihydroxyvitamin D, and prostate cancer risk. Prostate.
2007;67:911-923.
(62) Nomura AM, Stemmermann GN, Lee J et al. Serum vitamin D metabolite levels and the
subsequent development of prostate cancer (Hawaii, United States). Cancer Causes
Control. 1998;9:425-432.
(63) Platz EA, Leitzmann MF, Hollis BW, Willett WC, Giovannucci E. Plasma 1,25-
dihydroxy- and 25-hydroxyvitamin D and subsequent risk of prostate cancer. Cancer
Causes Control. 2004;15:255-265.
(64) Tuohimaa P, Tenkanen L, Ahonen Metal. Both high and low levels of blood vitamin D
are associated with a higher prostate cancer risk: a longitudinal, nested case-control
study in the Nordic countries. /nt J Cancer. 2004;108:104-108.
(65) TuohimaaP, Tenkanen L, Syvala H et at. Interaction offactors related to the metabolic
syndrome and vitamin D on risk of prostate cancer. Cancer Epidemiol Biomarkers
Prev. 2007;16:302-307.
(66) Gann PH, Ma J, Hennekens CH, Hollis BW, Haddad JG, Stampfer MJ. Circulating
vitamin D metabolites in relation to subsequent development of prostate cancer.
Cancer Epidemiol Biomarkers Prev. 1996;5:121-126.
(67) Tangrea J, Helzlsouer K, Pietinen Petal. Serum levels of vitamin D metabolites and the
subsequent risk of colon and rectal cancer in Finnish men. Cancer Causes Control.
1997;8:615-625.
(68) Otani T, Iwasaki M, Sasazuki S, Inoue M, Tsugane S, Japan Public Health Center-Based
Prospective Study Group. Plasma vitamin D and risk of colorectal cancer: the Japan
Public Health Center-Based Prospective Study. Br J Cancer. 2007 ;97 :446-451.
(69) Wu K, Feskanich D, Fuchs CS, Willett WC, Hollis BW, Giovannucci EL. A nested case
control study of plasma 25-hydroxyvitamin D concentrations and risk of colorectal
cancer. J Natl Cancer Jnst. 2007;99: 1120-1129.
(70) Feskanich D, Ma J, Fuchs CS et al. Plasma vitamin D metabolites and risk of colorectal
cancer in women. Cancer Epidemiol Biomarkers Prev. 2004; 13:1502-1508.
(71) Wactawski-Wende J, Kotchen JM, Anderson GL et al. Calcium plus vitamin D
supplementation and the risk of colorectal cancer. N Engl J Med. 2006;354:684-696.
(72) Garland CF, Comstock GW, Garland FC, Helsing KJ, Shaw EK, Gorham ED. Serum
25-hydroxyvitamin D and colon cancer: eight-year prospective study. Lancet.
1989;2: 1176-1178.
(73) Braun MM, Helzlsouer KJ, Hollis BW, Comstock GW. Colon cancer and serum vitamin
D metabolite levels 10-17 years prior to diagnosis. Am J Epidemiol. 1995; 142:608-
611.
322
(74) Platz EA, Hankinson SE, Hollis BW et al. Plasma 1,25-dihydroxy- and 25-
hydroxyvitamin D and adenomatous polyps of the distal colorectum. Cancer
Epidemiol Biomarkers Prev. 2000;9:1059-1065.
(75) Bertone-Johnson ER, Chen WY, Holick MF et al. Plasma 25-hydroxyvitamin D and
1,25-dihydroxyvitamin D and risk of breast cancer. Cancer Epidemiol Biomarkers
Prev. 2005;14:1991-1997.
(76) Freedman DM, Chang SC, Falk RT et al. Serum levels of vitamin D metabolites and
breast cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial.
Cancer Epidemiol Biomarkers Prev. 2008; 17:889-894.
(77) Stolzenberg-Solomon RZ, Vieth R, Azad A et al. A prospective nested case-control
study of vitamin D status and pancreatic cancer risk in male smokers. Cancer Res.
2006;66: 10213-10219.
(78) Stolzenberg-Solomon RZ, Hayes RB, Horst RL, Anderson KE, Hollis BW, Silverman
DT. Serum vitamin D and risk of pancreatic cancer in the prostate, lung, colorectal,
and ovarian screening trial. Cancer Res. 2009;69:1439-1447.
(79) Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM. Maternal
vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Me tab.
2007;92:3517-3522.
(80) Bunout D, Barrera G, Leiva Let al. Effects of vitamin D supplementation and exercise
training on physical performance in Chilean vitamin D deficient elderly subjects. Exp
Gerontal. 2006;41:746-752.
(81) Burleigh E, McColl J, Potter J. Does vitamin D stop inpatients falling? A randomised
controlled trial. Age Ageing. 2007;36:507-513.
(82) Lyons RA, Johansen A, Brophy S et al. Preventing fractures among older people living
in institutional care: a pragmatic randomised double blind placebo controlled trial of
vitamin D supplementation. Osteoporos Int. 2007;18:811-818.
(83) Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of
randomized controlled trials. Arch Intern Med. 2007; 167: 1730-1737.
(84) Avenell A, Gillespie WJ, Gillespie LD, O'Connell DL. Vitamin D and vitamin D
analogues for preventing fractures associated with involutional and post-menopausal
osteoporosis. Cochrane Database Syst Rev. 2008.
(85) Schleithoff SS, Zittermann A, Tenderich G, Berthold HK, Stehle P, Koerfer R. Vitamin
D supplementation improves cytokine profiles in patients with congestive heart
failure: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr.
2006;83:754-759.
323
(86) Flicker L, Macinnis R, Stein M, et al. Should all older people in residential care receive
Vitamin D to prevent falls? Results of a randomized trial. J Bone Miner Res.
2004;19:S99.
(87) Meyer HE, Smedshaug GB, Kvaavik E, Falch JA, Tverdal A, Pedersen n. Can vitamin
D supplementation reduce the risk of fracture in the elderly? A randomized controlled
trial. J Bone Miner Res. 2002; 17:709-715.
(88) Harwood RH, Sahota 0 , Gaynor K, Masud T, Hosking DJ. A randomised, controlled
comparison of different calcium and vitamin D supplementation regimens in elderly
women after hip fracture: The Nottingham Neck of Femur (NONOF) Study. Age
Ageing. 2004;33 :45-51.
(89) Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID. A
randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail
older people: the Frailty Interventions Trial in Elderly Subjects (FITNESS). JAm
Geriatr Soc. 2003;5 1 :291-299.
(90) Jia X, Aucott LS, McNeill G. Nutritional status and subsequent all-cause mortality in
men and women aged 75 years or over living in the community. Br J Nutr.
2007;98:593-599.
(91) Sambrook PN, Chen JS, March LM et al. Serum parathyroid hormone is associated with
increased mortality independent of25-hydroxy vitamin d status, bone mass, and renal
function in the frail and very old: a cohort study. J Clin Endocrinol Metab.
2004;89:5477-5481.
(92) Sambrook PN, Chen CJ, March Let al. High bone turnover is an independent predictor
ofmortality in the frail elderly. J Bone Miner Res. 2006;21:549-555.
(93) Visser M, Deeg DJ, Puts MT, Seidell JC, Lips P. Low serum concentrations of25-
hydroxyvitamin D in older persons and the risk of nursing home admission. Am J
Clin Nutr. 2006;84:616-622.
(94) Forman JP, Giovannucci E, Holmes MD et al. Plasma 25-hydroxyvitamin D levels and
risk of incident hypertension. Hypertension. 2007;49: 1063-1069.
(95) Forman JP, Curhan GC, Taylor EN. Plasma 25-hydroxyvitamin D levels and risk of
incident hypertension among young women. Hypertension. 2008;52:828-832.
(96) Scragg R, Khaw KT, MurphyS. Effect of winter oral vitamin D3 supplementation on
cardiovascular risk factors in elderly adults. Euro J Clin Nutr. 1995;49:640-646.
(97) Pfeifer M, Begerow B, Minne HW, Nachtigall D, Hansen C. Effects of a short-term
vitamin D(3) and calcium supplementation on blood pressure and parathyroid
hormone levels in elderly women. J Clin Endocrinol Me tab. 2001 ;86: 1633-1637.
324
(98) Zhu K, Bruce D, Austin N, Devine A, Ebeling PR, Prince RL. Randomized controlled
trial of the effects of calcium with or without vitamin D on bone structure and bone-
related chemistry in elderly women with vitamin D insufficiency. J Bone Miner Res.
2008;23: 1343-1348.
(99) Andersen R, Molgaard C, Skovgaard LT et al. Effect of vitamin D supplementation on
bone and vitamin D status among Pakistani immigrants in Denmark: a randomised
double-blinded placebo-controlled intervention study. Br J Nutr. 2008;100:197-207.
(100) Winzenberg T, Shaw K, Fryer J, Jones G. Calcium supplements in healthy children
do not affect weight gain, height, or body composition. Obesity. 2007; 15:1789-1798.
( 10 1) Lorenzen JK, Molgaard C, Michaelsen KF, Astrup A. Calcium supplementation for 1
y does not reduce body weight or fat mass in young girls. Am J Clin Nutr.
2006;83:18-23.
(102) Lappe JM, Rafferty KA, Davies KM, Lypaczewski G. Girls on a high-calcium diet
gain weight at the same rate as girls on a normal diet: a pilot study. JAm Diet Assoc.
2004; 104:1361-1367.
(103) Johnson AA, Knight EM, Edwards CH et al. Dietary intakes, anthropometric
measurements and pregnancy outcomes. J Nutr. 1994;124:936S-942S.
(104) Umesawa M, Iso H, Date C et al. Dietary intake of calcium in relation to mortality
from cardiovascular disease: the JACC Study. Stroke. 2006;37:20-26.
(105) van der Vijver, van der Waal MA, Weterings KG, Dekker JM, Schouten EG, Kok FJ.
Calcium intake and 28-year cardiovascular and coronary heart disease mortality in
Dutch civil servants. lnt J Epidemiol. 1992;21:36-39.
(106) Umesawa M, lso H, Ishihara Jet al. Dietary calcium intake and risks of stroke, its
subtypes, and coronary heart disease in Japanese: the JPHC Study Cohort I. Stroke.
2008;39:2449-2456.
(107) Al-Delaimy WK, Rimm E, Willett WC, Stampfer MJ, Hu FB. A prospective study of
calcium intake from diet and supplements and risk of ischemic heart disease among
men. Am J Clin Nutr. 2003;77:814-818.
( 1 08) Weng LC, Y eh WT, Bai CH et al. Is ischemic stroke risk related to folate status or
other nutrients correlated with folate intake? Stroke. 2008;39:3152-3158.
(109) Ascherio A, Rimm EB, Hernan MA et al. Intake of potassium, magnesium, calcium,
and fiber and risk of stroke among US men. Circulation. 1998;98: 1198-1204.
(110) Bostick RM, Kushi LH, Wu Y, Meyer KA, Sellers TA, Folsom AR. Relation of
calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among
postmenopausal women.AmJ Epidemiol. 1999;149:151-161.
325
(111) Iso H, Stampfer MJ, Manson JE et al. Prospective study of calcium, potassium, and
magnesium intake and risk of stroke in women. Stroke. 1999;30: 1772-1779.
(112) Larsson SC, Virtanen MJ, Mars Metal. Magnesium, calcium, potassium, and sodium
intakes and risk of stroke in male smokers. Arch lnt Med. 2008; 168:459-465.
(113) Ross RK, Yuan JM, Henderson BE, Park J, Gao YT, Yu MC. Prospective evaluation
of dietary and other predictors of fatal stroke in Shanghai, China. Circulation.
1997;96:50-55.
(114) Lanou A.T, Barnard ND. Dairy and weight loss hypothesis: an evaluation of the
clinical trials. Nutr Rev. 2008;66:272-279.
(1 15) Trowman R, Dumville JC, Hahn S, Torgerson DJ. A systematic review ofthe effects
of calcium supplementation on body weight. Br J Nutr. 2006;95: 1033-1038.
(1 16) Barr ST. Increased dairy product or calcium intake: is body weight or composition
affected in humans? J Nutr. 2003; 133:245S-248S.
(117) Yamamoto ME, Applegate WB, Klag MJ et al. Lack of blood pressure effect with
calcium and magnesium supplementation in adults with high-nonnal blood pressure.
Results from Phase I of the Trials ofHypertension Prevention (TOHP). Trials of
Hypertension Prevention (TOHP) Collaborative Research Group. Ann Epidemiol.
1995;5:96- 1 07 0
(118) van Beresteyn EC, Schaafsma G, de WH. Oral calcium and blood pressure: a
controlled intervention trial. Am J Clin Nutr. 1986;44:883-888.
(1 19) Cifuentes M, Riedt CS, Brolin RE, Field MP, Sherrell RM, Shapses SA. Weight loss
and calcium intake influence calcium absorption in overweight postmenopausal
women. Am J Clin Nutr. 2004;80:123-130.
(120) Ghadirian P, Shatenstein B, Verdy M, Hamet P. The influence of dairy products on
plasma uric acid in women. Euro J Epidemiol. 1995;1 1:275-281.
(121) Aloia JF, Vaswani A, Russo L, Sheehan M, Flaster E. The influence of menopause
and hormonal replacement therapy on body cell mass and body fat mass. Am J Obstet
Gynecol. 1995; 172:896-900.
(122) Thomsen K, Nilas L, Christiansen C. Dietary calcium intake and blood pressure in
normotensive subjects. Acta Med Scand. 1987;222:51-56.
(123) Kabrnova-Hlavata K, Hainer V, Gojova Met al. Calcium intake and the outcome of
short-term weight management. Physiol Res. 2008;57:237-245.
(124) Bertolotti M, Rudelle S, Schneiter Petal. Dairy calcium supplementation in
overweight or obese persons: its effect on markers of fat metabolism. Am J Clin Nutr.
2008;88:877-885.
326
(125) Park Y, Leitzmann MF, Subar AF, Hollenbeck A, Schatzkin A. Dairy food, calcium,
and risk of cancer in the NIH-AARP Diet and Health Study. Arch Int Med.
2009;169:391-401.
(126) Slob JC, Lambregts JL, Schuit AJ, Kok FJ. Calcium intake and 28-year gastro-
intestinal cancer mortality in Dutch civil servants. Int J Cancer. 1993;54:20-25.
(127) Chan JM, Stampfer MJ, Ma J, Gann PH, Gaziano JM, Giovannucci EL. Dairy
products, calcium, and prostate cancer risk in the Physicians' Health Study. Am J Clin
Nutr. 2001 ;74:549-554.
(128) Giovannucci E, Liu Y, Stampfer MJ, Willett WC. A prospective study of calcium
intake and incident and fatal prostate cancer. Cancer Epidemiol Biomarkers Prev.
2006; 15:203-210.
(129) Giovannucci E, Liu Y, Platz EA, Stampfer MJ, Willett WC. Risk factors for prostate
cancer incidence and progression in the health professionals follow-up study. Int J
Cancer. 2007; 121:1571-1578.
(130) Koh KA, Sesso HD, Paffenbarger RS, Jr., Lee IM. Dairy products, calcium and
prostate cancer risk.[see comment]. Br J Cancer. 2006;95:1582-1585.
(131) Kurahashi N, Inoue M, Iwasaki M, Sasazuki S, Tsugane AS, Japan Public Health
Center-Based Prospective Study Group. Dairy product, saturated fatty acid, and
calcium intake and prostate cancer in a prospective cohort of Japanese men. Cancer
Epidemiol Biomarkers Prev. 2008; 17:930-93 7.
(132) Mitrou PN, Albanes D, Weinstein SJ et al. A prospective study of dietary calcium,
dairy products and prostate cancer risk (Finland). lnt J Cancer. 2007;120:2466-2473.
(133) Park SY, Murphy SP, Wilkens LR, Stram DO, Henderson BE, Kolonel LN. Calcium,
vitamin D, and dairy product intake and prostate cancer risk: the Multiethnic Cohort
Study. Am J Epidemiol. 2007; 166:1259-1269.
(134) Park Y, Mitrou PN, Kipnis V, Hollenbeck A, Schatzkin A, Leitzmann MF. Calcium,
dairy foods, and risk of incident and fatal prostate cancer: the NIH-AARP Diet and
Health Study. Am J Epidemiol. 2007;166:1270-1279.
(135) Rodriguez C, McCullough ML, Mondul AM et al. Calcium, dairy products, and risk
of prostate cancer in a prospective cohort of United States men. Cancer Epidemiol
Biomarkers Prev. 2003;12:597-603.
(136) Rohrmann S, Platz EA, Kavanaugh CJ, Thuita L, Hoffman SC, Helzlsouer KJ. Meat
and dairy consumption and subsequent risk of prostate cancer in a US cohort study.
Cancer Causes Control. 2007;18:41-50.
327
(137) Schuurman AG, van den Brandt PA, Dorant E, Goldbohm RA. Animal products,
calcium and protein and prostate cancer risk in The Netherlands Cohort Study. Br J
Cancer. 1999;80: 1107-1113.
(138) Tseng M, Breslow RA, Graubard BI, Ziegler RG. Dairy, calcium, and vitamin D
intakes and prostate cancer risk in the National Health and Nutrition Examination
Epidemiologic Follow-up Study cohort. Am J Clin Nutr. 2005;81:1147- 1154.
(139) Weingarten MA, Zalmanovici A, Yaphe J. Dietary calcium supplementation for
preventing colorectal cancer and adenomatous polyps. Cochrane Database Syst Rev.
2008;CD003548.
(140) Wu K, Willett WC, Fuchs CS, Colditz GA, Giovannucci EL. Calcium intake and risk
of colon cancer in women and men. J Natl Cancer Inst. 2002;94:437-446.
(141) Kesse E, Boutron-Ruault MC, Norat T, Riboli E, Clavei-Chapelon F, Group N.
Dietary calcium, phosphorus, vitamin D, dairy products and the risk of colorectal
adenoma and cancer among French women of the E3N-EPIC prospective study. lnt J
Cancer. 2005;117:137-144.
(142) Lin J, Zhang SM, Cook NR, Manson JE, Lee IM, Buring JE. Intakes of calcium and
vitamin D and risk of colorectal cancer in women. Am J Epidemiol. 2005;161 :755-
764.
(143) Pietinen P, Malila N, Virtanen Metal. Diet and risk of colorectal cancer in a cohort
of Finnish men. Cancer Causes Control. 1999; I 0:387-396.
(144) Park SY, Murphy SP, Wilkens LR, Nomura AM, Henderson BE, Kolonel LN.
Calcium and vitamin D intake and risk of colorectal cancer: the Multiethnic Cohort
Study. Am J Epidemiol. 2007;165:784-793.
(145) McCullough ML, Robertson AS, Rodriguez C et al. Calcium, vitamin D, dairy
products, and risk of colorectal cancer in the Cancer Prevention Study II Nutrition
Cohort (United States). Cancer Causes Control. 2003;14:1-12.
(146) Terry P, Baron JA, Bergkvist L, Holmberg L, Wolk A. Dietary calcium and vitamin
D intake and risk of colorectal cancer: a prospective cohort study in women. Nutr
Cancer. 2002;43:39-46.
(147) Flood A, Peters U, Chatterjee N, Lacey JV, Jr., Schairer C, Schatzkin A. Calcium
from diet and supplements is associated with reduced risk of colorectal cancer in a
prospective cohort of women. Cancer Epidemiol Biomarkers Prev. 2005; 14: 126-132.
(148) Larsson SC, Bergkvist L, Rutegard J, Giovannucci E, Wolk A. Calcium and dairy
food intakes are inversely associated with colorectal cancer risk in the Cohort of
Swedish Men. Am J Clin Nutr. 2006;83:667-673.
328
( 149) Shin A, Li H, Shu XO, Yang G, Gao YT, Zheng W. Dietary intake of calcium, fiber
and other micronutrients in relation to colorectal cancer risk: Results from the
Shanghai Women's Health Study. lnt J Cancer. 2006;119:2938-2942.
(150) Bostick RM, Potter JD, Sellers TA, McKenzie DR, Kushi LH, Folsom AR. Relation
of calcium, vitamin D, and dairy food intake to incidence of colon cancer among
older women. The Iowa Women's Health Study. Am J Epidemiol. 1993;137: 1302-
1317.
(151) Stemmermann GN, Nomura A, Chyou PH. The influence of dairy and nondairy
calcium on subsite large-bowel cancer risk. Dis Colon Rectum. 1990;33: 190-194.
( 152) Zheng W, Anderson K.E, Kushi LH et al. A prospective cohort study of intake of
calcium, vitamin D, and other micronutrients in relation to incidence of rectal cancer
among postmenopausal women. Cancer Epidemiol Biomarkers P rev. 1998; 7:221-
225.
(153) Gaard M, Tretli S, Loken EB. Dietary factors and risk of colon cancer: a prospective
study of 50,535 young Norwegian men and women. Eur J Cancer Prev. 1996;5:445-
454.
(154) Wu AH, Paganini-Hill A, Ross RK, Henderson BE. Alcohol, physical activity and
other risk factors for colorectal cancer: a prospective study. Br J Cancer.
1987;55:687-694.
(155) Kato I, Akhmedkhanov A, Koenig K, Toniolo PG, Shore RE, Riboli E. Prospective
study of diet and female colo rectal cancer: the New York University Women's Health
Study. Nutr Cancer. 1997;28:276-281.
(156) van der Pols JC, Bain C, Gunnell D, Smith GD, Frobisher C, Martin RM. Childhood
dairy intake and adult cancer risk: 65-y follow-up of the Boyd Orr cohort. Am J Clin
Nutr. 2007;86: 1722-1729.
(157) Jarvinen R, Knekt P, Hakulinen T, Aromaa A. Prospective study on milk products,
calcium and cancers of the colon and rectum. Eur J Clin Nutr. 200 I ;55: 1000-1007.
(158) Garland C, Shekelle RB, Barrett-Connor E, Criqui MH, Rossof AH, Paul 0. Dietary
vitamin D and calcium and risk of colorectal cancer: a 19-year prospective study in
men. Lancet. 1985;1 :307-309.
(159) Kampman E, Goldbohm RA, van den Brandt PA, van', V. Fermented dairy products,
calcium, and colorectal cancer in The Netherlands Cohort Study. Cancer Res.
1994;54:3186-3190.
(160) Baron JA, Beach M, Mandel JS et al. Calcium supplements for the prevention of
colorectal adenomas. Calcium Polyp Prevention Study Group. N Engl J Med.
1999;340: 101-107.
329
(161) Grau MV, Baron JA, Sandler RS et al. Prolonged effect of calcium supplementation
on risk of colorectal adenomas in a randomized trial. J Natl Cancer Inst.
2007;99: 129-136.
(162) Duris I, Hruby D, Pekarkova B et al. Calcium chemoprevention in colorectal cancer.
Hepato-gastroenterology. 1996;43: 152-154.
(163) Oh K, Willett WC, Wu K, Fuchs CS, Giovannucci EL. Calcium and vitamin D
intakes in relation to risk of distal colorectal adenoma in women. Am J Epidemiol.
2007;165:1178-1186.
(164) Hartman TJ, Albert PS, Snyder Ketal. The association of calcium and vitamin D
with risk of colorectal adenomas. J Nutr. 2005; 135:252-259.
(165) Martinez ME, Marshall JR, Sampliner R, Wilkinson J, Alberts DS. Calcium, vitamin
D, and risk of adenoma recurrence (United States). Cancer Causes Control.
2002; 13:213-220.
(166) Kesse-Guyot E, Bertrais S, Duperray Bet al. Dairy products, calcium and the risk of
breast cancer: results of the French SU.Vl.MAX prospective study. Ann Nutr Metab.
2007;51 :139-145.
(167) Lin J, Manson JE, Lee IM, Cook NR, Buring JE, Zhang SM. Intakes of calcium and
vitamin D and breast cancer risk in women. Arch Intern Med. 2007;167:1050-1059.
(168) McCullough ML, Rodriguez C, Diver WR et al. Dairy, calcium, and vitamin D intake
and postmenopausal breast cancer risk in the Cancer Prevention Study II Nutrition
Cohort. Cancer Epidemiol Biomarkers Prev. 2005; 14:2898-2904.
(169) Shin MH, Holmes MD, Hankinson SE, Wu K, Colditz GA, Willett WC. Intake of
dairy products, calcium, and vitamin d and risk of breast cancer. J Natl Cancer lnst.
2002;94:1301-0311.
( 170) Larsson SC, Bergkvist L, Wolk A. Long-term dietary calcium intake and breast
cancer risk in a prospective cohort of women. Am J Clin Nutr. 2009;89:277-282.
(171) Mishra G, McCormack V, Kuh D, Hardy R, Stephen A, dos SS, I. Dietary calcium
and vitamin D intakes in childhood and throughout adulthood and mammographic
density in a British birth cohort. Br J Cancer. 2008;99:1539-1543.
(172) Skinner HG, Michaud DS, Giovannucci E, Willett WC, Colditz GA, Fuchs CS.
Vitamin D intake and the risk for pancreatic cancer in two cohort studies. Cancer
Epidemiol Biomarkers Prev. 2006; 15: 1688-1695.
(173) Bucher HC, Guyatt GH, Cook RJ et al. Effect of calcium supplementation on
pregnancy-induced hypertension and preeclampsia: a meta-analysis of randomized
controlled trials. lAMA. 1996;275:1113-1117.
330
(174) Carroli G, Duley L, Belizan JM, Villar J. Calcium supplementation during pregnancy:
a systematic review ofrandomised controlled trials. BJOG. 1994;101:753-758.
(175) Hofmeyr GJ, Roodt A, Atallah AN, Duley L. Calcium supplementation to prevent
pre-eclampsia--a systematic review. S A.fr Med J. 2003;93:224-228.
(176) Hofmeyr GJ, Atallah AN, Duley L. Calcium supplementation during pregnancy for
preventing hypertensive disorders and related problems. Cochrane Database Syst
Rev. 2006;3:CD001059.
(177) Hofmeyr GJ, Duley L, Atallah A. Dietary calcium supplementation for prevention of
pre-eclampsia and related problems: a systematic review and commentary. BJOG.
2007;114:933-943.
(178) Villar J, bdel-Aleem H, Merialdi Metal. World Health Organization randomized trial
of calcium supplementation among low calcium intake pregnant women. Am J Obstet
Gynecol. 2006; 194:639-649.
(179) Levine RJ, Hauth JC, Curet LB et al. Trial of calcium to prevent preeclampsia. N
Engl J Med. 1997;337:69-76.
(180) DerSimonian R, Levine RJ. Resolving discrepancies between a meta-analysis and a
subsequent large controlled trial. lAMA. 1999;282:664-670.
(181) Morris CD, Jacobson SL, Anand Ret al. Nutrient intake and hypertensive disorders
of pregnancy: Evidence from a large prospective cohort. Am J Obstet Gynecol.
2001 ;184:643-651.
(182) Oken E, Ning Y, Rifas-Shiman SL, Rich-Edwards JW, Olsen SF, Gillman MW. Diet
during pregnancy and risk of preeclampsia or gestational hypertension. Ann
Epidemiol. 2007; 17:663-668.
(183) Alonso A, Beunza JJ, gada-Rodriguez M, Martinez JA, Martinez-Gonzalez MA.
Low-fat dairy consumption and reduced risk of hypertension: the Seguimiento
Universidad de Navarra (SUN) cohort. Am J Clin Nutr. 2005;82:972-979.
(184) Dwyer JH, Li L, Dwyer KM, Curtin LR, Feinleib M. Dietary calcium, alcohol, and
incidence of treated hypertension in the NHANES I epidemiologic follow-up study.
Am J Epidemiol. 1996; 144:828-838.
(185) Ascherio A, Rimm EB, Giovannucci EL et al. A prospective study of nutritional
factors and hypertension among US men. Circulation. 1992;86:1475-1484.
(186) Ford ES, Cooper RS. Risk factors for hypertension in a national cohort study.
Hypertension. 1991; 18:598-606.
331
(187) Wang L, Manson JE, Buring JE, Lee IM, Sesso HD. Dietary intake of dairy products,
calcium, and vitamin D and the risk of hypertension in middle-aged and older
women. Hypertension. 2008;51: 1073-1079.
(188) Ascherio A, Hennekens C, Willett WC et at. Prospective study of nutritional factors,
blood pressure, and hypertension among US women. Hypertension. 1996;27:1065-
1072.
(189) Griffith LE, Guyatt GH, Cook RJ, Bucher HC, Cook DJ. The influence of dietary and
nondietary calcium supplementation on blood pressure: an updated metaanalysis of
randomized controlled trials.[ see comment]
1927. Am J Hypertens. 1999;12:84-92.
(190) van Mierlo LA, Arends LR, Streppel MT et al. Blood pressure response to calcium
supplementation: a meta-analysis of randomized controlled trials. J Hum Hypertens.
2006;20:571-580.
(191) Bucher HC, Cook RJ, Guyatt GH et al. Effects of dietary calcium supplementation on
blood pressure. A meta-analysis of randomized controlled trials. lAMA.
1996;275: 1016-1022.
(192) Allender PS, Cutler JA, Follmann D, Cappuccio FP, Pryer J, Elliott P. Dietary
calcium and blood pressure: a meta-analysis of randomized clinical trials. Ann Intern
Med. 1996;124:825-831.
(193) Cappuccio FP, Siani A, Strazzullo P. Oral calcium supplementation and blood
pressure: an overview ofrandomized controlled trials. 1 Hypertens. 1989;7:941-946.
(194) Reid IR, Home A, Mason B, Ames R, Bava U, Gamble GD. Effects of calcium
supplementation on body weight and blood pressure in normal older women: a
randomized controlled trial. J Clin Endocrinol Metab. 2005;90:3824-3829.
(195) Whelton PK, Kumanyika SK, Cook NR et al. Efficacy ofnonpharmacologic
interventions in adults with high-normal blood pressure: results from phase 1 of the
Trials ofHypertension Prevention. Trials ofHypertension Prevention Collaborative
Research Group. Am J Clin Nutr. 1997;65:652S-660S.
(196) Hatton DC, Harrison-Hohner J, Coste S, Reller M, McCarron D. Gestational calcium
supplementation and blood pressure in the offspring. Am J Hypertens. 2003;16:801-
805.
(197) Lijnen P, Petrov V. Dietary calcium, blood pressure and cell membrane cation
transport systems in males. J Hypertens. 1995;13:875-882.
(198) Dickinson HO, Nicolson D, Cook Net al. Calcium supplementation for the
management of primary hypertension in adults. Cochrane Database of Systematic
Reviews. 2006.
332
(199) Hsia J, Heiss G, Ren H et al. Calcium/vitamin D supplementation and cardiovascular
events. Circulation. 2007;115:846-854.
(200) Lacroix AZ, Kotchen J, Anderson Get al. Calcium plus vitamin D supplementation
and mortality in postmenopausal women: the Women's Health Initiative calcium-
vitamin D randomized controlled trial. J Gerontal A Biol Sci Med Sci. 2009;64:559-
567.
(201) Caan B, Neubouser M, Aragaki A et al. Calcium plus vitamin D supplementation and
the risk of postmenopausal weight gain. Arch Intern Med. 2007;167:893-902.
(202) Major GC, Alarie F, Dore J, Phouttama S, Tremblay A. Supplementation with
calcium + vitamin D enhances the beneficial effect of weight loss on plasma lipid and
lipoprotein concentrations. Am J Clin Nutr. 2007;85:54-59.
(203) Ding EL, Mehta S, Fawzi WW, Giovannucci EL. Interaction of estrogen therapy with
calcium and vitamin D supplementation on colorectal cancer risk: reanalysis of
Women's Health Initiative randomized trial. lnt J Cancer. 2008;122:1690-1694.
(204) Grau MY, Baron JA, Sandler RS et al. Vitamin D, calcium supplementation, and
colorectal adenomas: results of a randomized trial. J Nat/ Cancer lnst. 2003;95: 1765-
1771.
(205) Chlebowski RT, Johnson KC, Kooperberg C et al. Calcium plus vitamin D
supplementation and the risk of breast cancer. J Natl Cancer lnst. 2008; 100:1581-
1591.
(206) Marya RK, Rathee S, Manrow M. Effect of calcium and vitamin D supplementation
on toxaemia of pregnancy. Gynecol Obstet Invest. 1987;24:38-42.
(207) Brunner RL, Cochrane B, Jackson RD et al. Calcium, vitamin D supplementation,
and physical function in the Women's Health Initiative. JAm Diet Assoc.
2008;108: 1472-1479.
(208) Lappe J, Cullen D, Haynatzki G, Recker R, AhlfR, Thompson K. Calcium and
vitamin d supplementation decreases incidence of stress fractures in female navy
recruits. J Bone Miner Res. 2008;23:741-749.
(209) Bjorkman M, Sorva A, Risteli J, Til vis R. Vitamin D supplementation has minor
effects on parathyroid honnone and bone turnover markers in vitamin D-de:ficient
bedridden older patients. Age Ageing. 2008;37:25-31 .
(21 0) Jackson RD, Lacroix AZ, Gass Metal. Calcium plus vitamin D supplementation and
the risk of fractures. N Engl J Med. 2006;354:669-683.
(211) Margolis KL, Ray RM, Van HL et al. Effect of calcium and vitamin D
supplementation on blood pressure: the Women's Health Initiative Randomized Trial.
Hypertension. 2008;52:847-855.
333
(212) Cheng S, Lyytikainen A, Kroger H et al. Effects of calcium, dairy product, and
vitamin D supplementation on bone mass accmal and body composition in 10-12-y-
old girls: a 2-y randomized trial. Am J Clin Nutr. 2005;82: 1115-1126.
(213) Bolton-Smith C, McMurdo ME, Paterson CR et al. Two-year randomized controlled
trial of vitamin K1 (phylloquinone) and vitamin D3 plus calcium on the bone health
of older women. J Bone Miner Res. 2007;22:509-519.
(214) Zhu K, Devine A, Dick IM, Wilson SG, Prince RL. Effects of calcium and vitamin D
supplementation on hip bone mineral density and calcium-related analytes in elderly
ambulatory Australian women: a five-year randomized controlled trial. J Clin
Endocrinol Metab. 2008;93:743-749.
(215) Moschonis G, Manios Y. Skeletal site-dependent response ofbone mineral density
and quantitative ultrasound parameters following a 12-month dietary intervention
using dairy products fortified with calcium and vitamin D: the Postmenopausal
Health Study. Br J Nutr. 2006;96:1140-1148.
(216) Blum M, Dallal GE, wson-Hughes B. Body size and semm 25 hydroxy vitamin D
response to oral supplements in healthy older adults. JAm Coil Nutr. 2008;27:274-
279.
(217) Chapuy MC, Arlot ME, Duboeuf F et al. Vitamin D3 and calcium to prevent hip
fractures in the elderly women. N Engl J Med. 1992;327: 1637-1642.
(218) Chel V, Wijnhoven HA, Smit JH, Ooms M, Lips P. Efficacy of different doses and
time intervals of oral vitamin D supplementation with or without calcium in elderly
nursing home residents. Osteoporos Int. 2008; 19:663-671.
(219) Deroisy R, Collette J, Albert A, Jupsin I, Reginster JY. Administration of a
supplement containing both calcium and vitamin D is more effective than calcium
alone to reduce secondary hyperparathyroidism in postmenopausal women with low
25(0H)vitamin D circulating levels. Aging Clin Exp Res. 2002;14:13-17.
(220) Himmelstein S, Clemens TL, Rubin A, Lindsay R. Vitamin D supplementation in
elderly nursing home residents increases 25(0H)D but not 1,25(0H)2D. Am J Clin
Nutr. 1990;52:701-706.
(221) Kenny AM, Biskup B, Robbins B, Marcella G, Burleson JA. Effects of vitamin D
supplementation on strength, physical function, and health perception in older,
community-dwelling men. JAm Geriatr Soc. 2003;51: 1762- 1767.
(222) Krieg MA, Jacquet AF, Bremgmtner M, Cuttelod S, Thiebaud D, Burckhardt P.
Effect of supplementation with vitamin D3 and calcium on quantitative ultrasound of
bone in elderly institutionalized women: a longitudinal study. Osteoporos Int.
1999;9:483-488.
334
(223) Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C. Effects of a
short-term vitamin D and calcium supplementation on body sway and secondary
hyperparathyroidism in elderly women. J Bone Miner Res. 2000; 15:1113-1118.
(224) Sorva A, Risteli J, Risteli L, Valimaki M, Ti lvis R. Effects of vitamin D and calcium
on markers of bone metabolism in geriatric patients with low serum 25-
hydroxyvitarnin D levels. CalcifTissue Int. 1991;49 Suppl:S88-S89.
(225) Barnes MS, Robson PJ, Bonham MP, Strain JJ, Wallace JM. Effect of vitamin D
supplementation on vitamin D status and bone turnover markers in young adults. Eur
J Clin Nutr. 2006;60:727-733.
(226) Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D
supplementation on bone density in men and women 65 years of age or older. N Engl
J Med. 1997;337:670-676.
(227) Harris SS, wson-Hughes B. Plasma vitamin D and 250HD responses of young and
old men to supplementation with vitamin D3. JAm Coil Nutr. 2002;21:357-362.
(228) Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. Human serum 25-
hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J
Clin Nutr. 2003;77:204-210.
(229) Heikkinen A, Parviainen MT, Tuppurainen MT, Niskanen L, Komulainen MH,
Saarikoski S. Effects of postmenopausal hormone replacement therapy with and
without vitamin D3 on circulating levels of 25-hydroxyvitamin D and 1 ,25-
dihydroxyvitamin D. CalcifTissue Int. 1998;62:26-30.
(230) Honkanen R, Alhava E, Parviainen M, Talasniemi S, Monkkonen R. The necessity
and safety of calcium and vitamin Din the elderly. JAm Geriatr Soc. 1990;38:862-
866.
(231) Jensen C, Holloway L, Block G et al. Long-term effects of nutlient intervention on
markers of bone remodeling and calciotropic hormones in late-postmenopausal
women. Am J Clin Nutr. 2002;75:1114-1120.
(232) Nelson ML, Blum JM, Hollis BW, Rosen C, Sullivan SS. Supplements of20
microg/d cholecalciferol optimized serum 25-hydroxyvitamin D concentrations in
80% of premenopausal women in winter. J Nutr. 2009; 139:540-546.
(233) Orwoll ES, Weigel RM, Oviatt SK, McClung MR, Deftos LJ. Calcium and
cholecalciferol: effects of small supplements in normal men. Am J Clin Nutr.
1988;48: 127-130.
(234) Patel R, Collins D, BullockS, Swaminathan R, Blake GM, Fogelman I. The effect of
season and vitamin D supplementation on bone mineral density in healthy women: a
double-masked crossover study. Osteoporos Int. 2001; 12:319-325.
335
(235) Riis B, Christiansen C, Rodbro P. The effect of different vitamin D treatments on
semm vitamin D levels in early postmenopausal women. Acta Vitaminol Enzymol.
1984;6:77 -82.
(236) Trang HM, Cole DE, Rubin LA, Pierratos A, Siu S, Vieth R. Evidence that vitamin
D3 increases semm 25-hydroxyvitamin D more efficiently than does vitamin D2. Am
J Clin Nutr. 1998;68:854-858.
(237) Chan GM, Roberts CC, Folland D, Jackson R. Growth and bone mineralization of
normal breast-fed infants and the effects of lactation on maternal bone mineral status.
Am J Clin Nutr. 1982;36:438-443.
(238) Basile LA, Taylor SN, Wagner CL, Horst RL, Hollis BW. The effect of high-dose
vitamin D supplementation on semm vitamin D levels and milk calcium
concentration in lactating women and their infants. Med. 2006; 1:27-35.
(239) Hollis BW, Wagner CL. Vitamin D requirements during lactation: high-dose maternal
supplementation as therapy to prevent hypovitaminosis D for both the mother and the
nursing infant. Am J Clin Nutr. 2004;80: 1752S-1758S.
(240) Mastaglia SR, Mautalen CA, Parisi MS, Oliveri B. Vitamin D2 dose required to
rapidly increase 250HD levels in osteoporotic women. Eur J Clin Nutr. 2006;60:681-
687.
(241) Bonis PA, Chung M, Tatsioni A et al. Effects of omega-3 fatty acids on organ
transplantation. Evidence Report/Technology Assessment No. 115 (Prepared by
Tufts-New England Medical Center Evidence-based Practice Center under Contract
No. 290-02-0022). AHRQ Publication No. 05-012-2. Rockville, MD: Agency for
Healthcare Research and Quality. 2005.
(242) Whitlock EP, Lin JS, Chou R, Shekelle P, Robinson KA. Using existing systematic
reviews in complex systematic reviews. Ann lnt Med. 2008;148:776-782.
(243) Dickersin K, Rennie D. Registering clinical trials. lAMA. 2003;290:516-523.
(244) Rising K, Bacchetti P, Bero L. Reporting bias in drug trials submitted to the Food and
Drug Administration: review of publication and presentation. PLoS Med.
2008;5:e217.
336
Abbreviations
25(0H)D
AHRQ
AMSTAR
Anthrop
ASA
ATBC
BCDDP
BMC
BMD
BMI
Ca
CABG
CeVD
CHD
CHD
Cl
CIFOS
CONSORT
CPBA
CPEP
CPP
CPS
CRC
CYD
DBP
Demograph
OM
DRJ
Ox
EAR
EPC
25-hydroxyvitamin D
Agency for Healthcare Research and Quality
Assessment of multiple systematic reviews
Anthropometric measures
Acetyl-salicylic acid (aspirin)
Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study
Breast Cancer Detection Demonstration Project
Bone mineral content
Bone mineral density
Body Mass Index
Calcium
Coronary artery bypass graft
Cerebrovascular disease
Coronary heart disease
Coronary Heart Disease
Confidence Interval
Calcium Intake Fracture Outcome Study
Consolidated Standards of Reporting Trials
Competitive protein binding assay
Calcium for Prevention of Preeclampsia Trial
Calcium Polyp Prevention Study
Cancer Prevention Study
Colorectal cancer
Cardiovascular disease
Diastolic blood pressure
Demographics
Diabetes Mellitus
Dietary Reference Intake
Diagnosis
Estimated average requirement
Evidence-based Practice Center
337
FFQ
FNB
FOS
FREE
HAH
HbC
HPFS
HPLC
HR
ht
HT
HTN
IHD
IOM
Iowa WHS
IQR
IU
Japan CC
Japan PHC
Food frequency questionnaire
Food and Nutrition Board
Framingham Offspring Study
Fracture Risk Epidemiology in the Elderly
Harvard Alumni Health Study
Hemoglobin C disease
Health Professionals Follow-up Study
High pressure liquid chromatography
Hazard ratio
Height
Honnone (replacement) therapy
Hypertension
Ischemic heart disease
Institute of Medicine
Iowa Women's Health Study
Interquartile range
International unit
Japan Collaborative Cohort
Japan Public Health Center study
Kupio ORFPS Kupio Osteoporosis Risk Factor and Prevention Study
MCS Multietbnic Cohort Study, Hawaii, Cali fornia
MI Myocardial infarction
mil Million
mo
N
n
NA
nd
NHANES
NHEFS
NHS
Months(s)
Number of subjects
Number of subjects had event(s)
Not applicable
No data
National Health and Nutrition Examination Survey
NHANES I Epidemiologic Follow-up Study
Nurses' Health Study
338
NIH
NIH-AARP
NPC
NS
ODS
OR
PAHSG
PCI
PHS
PI(E)CO
PLCO
PMID
PSA
PTH
RCT
RDA
RIA
RR
SBP
SD
SE
STROBE
Subgp
Suppl
TEP
TIA
TOHP
TOO
UK
UL
us
USDA
National Institutes of Health
National Institutes of Health- American Association of Retired Persons
Nutrition Prevention of Cancer trial
Not significant
Office of Dietary Supplements
Odds Ratio
Princess Anne Hospital Study Group, UK
Percutaneous coronary intervention
Physicians' Health Study
Population, Intervention (or Exposure), Comparison and Outcome
Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial
PubMed (unique) identifier
Prostate specific antigen
Parathyroid hormone
Randomized-controlled trial
Recommended Dietary Allowance
Radioinununoassay
Relative risk
Systolic blood pressure
Standard deviation
Standard error
STrengthening the Reporting of OBservational studies in Epidemiology
Subgroup
Supplement(s)
Technical Expert Panel
Transient ischemic attach
Trials of Hypertension Prevention
Task order officer
United Kingdom
Tolerable upper intake levels
United States
United States Department of Agriculture
339
uv Ultraviolet rays
Yit Vitamin
wee Washington County Cohort
WHI Women's Health Initiative
WHS Women' s Health Study
wk week(s)
WMD Weighted mean difference
wt Weight
y Year(s)
340
Latitudes of Selected Cities
Latitude
64 N
60-61 N
56 N
52 N
51 N
49 N
48 N
4rN
34 N
33 N
30 N
29 N
26 N
22 N
21 N
19 N
15 N
10N
4 N
1 N
12 s
23 s
26 s
34 s
35 s
37 s
38 s
41 s
Western Hemisphere
Reykjavik, Iceland
Nome, Alaska
Anchorage, Alaska
Calgary, Alberta
Vancouver, British Columbia
Seattle, Washington
Quebec City, Quebec
Bismarck, North Dakota
Ottawa, Ontario
Minneapolis, Minnesota
Toronto, Ontario
Portland, Maine
Boston, Massachusetts
Chicago, Illinois
New York, New York
Salt Lake City, Utah
Philadelphia, Pennsylvania
Columbus, Ohio
Washington, DC
St Louis, Missouri
Sacramento, California
Louisville, Kentucky
Wichita, Kansas
San Francisco, California
Raleigh, North Carolina
Las Vegas, Nevada
Columbia, South Carolina
Los Angeles, California
Dallas, Texas
New Orleans, Louisiana
San Antonio, Texas
Miami , Florida
Honolulu, Hawaii
Mexico City, Mexico
Guatemala City, Guatemala
Caracas, Venezuela
Bogota, Columbia
Lima, Peru
Rio de Janeiro, Brazil
Buenos Aires, Argentina
341
Eastern Hemisphere
Oslo, Norway
Copenhagen, Denmark
Berlin, Germany
Amsterdam, Netherlands
London, England
Paris, France
Munich, Germany
Zurich, Switzerland
Milan, Italy
Rome, Italy
Barcelona, Spain
Madrid, Spain
Beijing, China
Athens, Greece
Tokyo, Japan
Fez, Morocco
Cairo, Egypt
New Delhi , India
Hong Kong, China
Mumbai (Bombay), India
Manila, Philippines
Singapore
Johannesburg, South Africa
Sydney, Australia
Cape Town, South Africa
Auckland, New Zealand
Melbourne, Australia
Wellington, New Zealand
342
Appendix A. Search strategy for primary studies
a. Overall Search Strategy for Outcomes of Estimated Average
Requirements
Database: Ovid MEDLINE(R), CCTR (1969 to April 2009)
1. exp Vitamin D/
2. (25-hydroxy vit D or plasma vit D or 250HD or 25-0HD).mp. [mp=title, original title,
abstract, name of substance word, subject heading word]
3. (250HD3 or "25(0H)D3" or 25-0HD3 or "25-(0H)D3").tw.
4. ("25(0H)D" or "25-(0H)D" or "25-0H-D").tw.
5. 25-hydroxycholecalciferol.tw.
6. 25-hydroxyergocalciferol.tw.
7. calcidiol. tw.
8. Calcifediol/
9. (vit adj (d or d2 or d3)).mp.
10. Ergocalciferols/
11. Ergocalciferol$.tw.
12. Cholecalciferol/
13. Cholecalciferol$.tw.
14. calciferol.tw.
15. or/1-14
16. exp Calcium/
17. exp Calcium Carbonate/ or exp Calcium Citrate/ or exp Calcium Phosphates/ or exp Calcium
Malate/
18. exp Calcium, Dietary/
19. calcium.tw.
20. or/ 16-19
21. (ANIMALS not HUMAN).sh.
22. *Dialysis/ or *hemodialysis/ or *peritoneal dialysis/
23. 15 or 20
24. 23 not 21
25. 24 not 22
26. limit 25 to (addresses or bibliography or biography or comment or congresses or consensus
development conference or consensus development conference, nih or dictionary or directory or
duplicate publication or editorial or in vitro or interview or lectures or letter or news or
newspaper article or "review")
27. 25 not 26
28. limit 27 to english language
29. randomized controlled trial.pt.
30. controlled clinical trial.pt.
31. randomized controlled trials/
32. Random Allocation/
33. Double-blind Method/
34. Single-Blind Method/
3 5. clinical trial. pt.
36. Clinical Trials.mp. or exp Clinical Trials/
37. (clinic$ adj25 trial$).tw.
38. ((singl$ or doubl$ or trebl$ or tripl$) adj (mask$ or blind$)).tw.
39. Placebos/
40. placebo$.tw.
41. random$.tw.
42. trial$.tw.
43. (latin adj square).tw.
44. Comparative Study.tw.
45. exp Evaluation studies/
46. Follow-Up Studies/
47. Prospective Studies/
48. (control$ or prospectiv$ or volunteer$).tw.
49. Cross-Over Studies/
50. or/29-49
51. 50 and 28
52. 28 not 51
53. limit 51 to yr=" 1969-2008"
54. limit 52 to yr=" 1969-2008"
55. 53 not ("200810$" or "200811$" or "200812$").ed.
56. 54 not ("200810$" or "200811$" or "200812$").ed.
57. 55 or 56
58. exp Vitamin D/
59. (25-hydroxy vit D or plasma vit D or 250HD or 25-0HD).mp. [mp=title, original tit le,
abstract, name of substance word, subject heading word]
60. (250HD3 or "25(0H)D3" or 25-0HD3 or "25-(0H)D3").tw.
61. ("25(0H)D" or "25-(0H)D" or "25-0H-D").tw.
62. 25-hydroxycho lecalciferol. tw.
63. 25-hydroxyergocalciferol.tw.
64. calcidiol.tw.
65. Calcifediol/
66. (vit adj (d or d2 or d3)).mp.
67. Ergocalciferols/
68. Ergocalciferol$.tw.
69. Cholecalciferol/
70. Cholecalciferol$.tw.
71. calciferol. tw.
72. or/58-71
73. exp Calcium/
74. exp Calcium Carbonate/ or exp Calcium Citrate/ or exp Calcium Phosphates/ or exp Calcium
Malate/
75. exp Calcium, Dietary/
76. calcium.tw.
77. or/73-76
78. (ANIMALS not HUMAN).sh.
79. (ANIMALS not HUMAN).sh.
80. 72 or 77
81. 80 not 78
82. 81 not 79
83. limit 82 to (addresses or bibliography or biography or comment or congresses or consensus
development conference or consensus development conference, nih or dictionary or directory or
duplicate publication or editorial or in vitro or interview or lectures or letter or news or
newspaper article or "review")
84. 82 not 83
85. limit 84 to english language
86. randomized controlled trial. pt.
87. controlled clinical trial. pt.
88. randomized controlled trials/
89. Random Allocation/
90. Double-blind Method/
91. Single-Blind Method/
92. clinical trial. pt.
93. Clinical Trials.mp. or exp Clinical Trials/
94. (clinic$ adj25 trial$).tw.
95. ((singl$ or doubl$ or trebl$ or tlipl$) adj (mask$ or blind$)).tw.
96. Placebos/
97. placebo$.tw.
98. random$.tw.
99. trial$.tw.
100. (latin adj square).tw.
101. Comparative Study.tw.
102. exp Evaluation studies/
103. Follow-Up Studies/
104. Prospective Studies/
105. (control$ or prospectiv$ or volunteer$).tw.
106. Cross-Over Studies/
1 07. or/ 86- 1 06
108. 107 and 85
1 09. 85 not 108
ll 0. limit 108 to yr=" 1969-2008"
111. limit 109 to yr=" 1969-2008"
112. 110 not ("200810$" or "200811$" or "200812$").ed.
113. 111 not ("200810$" or "200811$" or "200812$").ed.
114.112or113
115. verapamil.mp. or 52-53-9.m.
116. nifedipine.mp. or 21829-25-4.m.
117. diltiazem.mp. or42399-41-7.m.
118. Azelnidipine.mp. or 123524-52-7 .rn.
119. nicardipine.mp. or 55985-32-5.m.
120. felodipine.mp. or 72509-76-3.rn.
121. mepirodipine.mp. or 104713-75-9.rn.
122. Amlodipine.mp. or 88150-42-9.rn.
123. isradipine.mp. or 75695-93- l.m.
124. bepridil.mp. or 64706-54-3.rn.
125. gallopamil.mp. or 16662-47-8.m.
126. aranidipine.mp. or 86780-90-7.m.
127. nitrendipine.mp. or 39562-70-4.m.
128. Bamidipine.mp.
129. benidipine.mp. or 105979-17-7.m.
130. Cilnidipine.mp. or 132203-70-4.m.
131. clevidipine.mp.
132. efonidipine.mp. or 111011-53-l.rn.
133. Lacidipine.mp. or 1 03890-78-4.m.
134. Lercanidipine.mp. or 100427-26-7 .m.
135. Manidipine.mp. or 89226-50-6.m.
136. Nilvadipine.mp. or 75530-68-6.m.
137. Nimodipine.mp. or 66085-59-4.m.
138. Nisoldipine.mp. or 63675-72-9.rn.
139. Pranidipine.mp. or 99522-79-9.m.
A-4
140. ((calcium orCa) adj3 channel$).mp.
141. ((calcium orCa) adj3 agonist$).mp.
142. (intracellular adj2 (calcium or Ca)).mp.
143. or/ 115- 142
144. weight loss.mp. or exp Weight Loss/
145. body mass index.mp. or exp Body Mass Index/ or exp Body Mass/ or body mass.mp. or exp
body weight/ or body weight.mp.
146. 144 or 145
147. obesity.mp. or exp OBESITY/pc, di, ep, et
148. or/ 144-147
149. limit 148 to ("all infant (birth to 23 months)" or "newborn infant (birth to 1 month)" or
"infant (1 to 23 months)" or "preschool child (2 to 5 years)")
150. limit 149 to ("all adult (19 plus years)" or "child (6 to 12 years)" or "adolescent (13 to 18
years)" or "adult (19 to 44 years)" or "middle age (45 to 64 years)" or "middle aged (45 plus
years)" or "all aged (65 and over)" or "aged (80 and over)'')
151. 149 not 150
152. 148 not 151
153. exp Body Height/
154. exp body size/
155. growth velocity.af.
156. growth retardation.af.
157. growth delay .af.
15 8. growth restriction.af.
159. (height adj6 restrict$).af.
160. linear velocity .af.
161. (height adj6 delay).af.
162. length delay.af.
163. (length adj6 retardation).af.
164. or/ 153-163
165. limit 164 to ("all infant (birth to 23 months)" or "all child (0 to 18 years)" or "newborn
infant (birth to 1 month)" or "infant (1 to 23 months)" or "preschool child (2 to 5 years)" or
"child (6 to 12 years)" or "adolescent (13 to 18 years)")
166. 164 not 165
167. limit 166 to ("all adult (19 plus years)" or "adult (19 to 44 years)" or "middle age (45 to 64
years)" or "middle aged (45 plus years)" or "all aged (65 and over)" or "aged (80 and over)")
168. 164 not 167
169. Bone Density/
170. exp Osteoporosis/
171. ((bone$ or plate$) adj3 mineral$).tw.
172. (bone adj2 (loss or turnover or densi$)).tw.
173. (Skelet$ adj2 (mineral$ or development$)).tw.
174. mineralization defect$.tw.
175. Mineral$ content$.tw.
176. BMC.tw.
177. Osteoporo$.tw.
178. Osteomalac$.tw.
179. Osteopath$.tw.
180. Bone Development/
18 I . Osteogenesis/
182. fracture$.tw.
183. Accidental Falls/
184. fall s.tw.
185. exp "Bone and Bones"/
186. or/ 169-185
187. Rickets/
188. rachitis.tw.
189. rickets.tw.
190. or/187-189
191. tooth loss.mp. or exp Tooth Loss/
192. 190 or 186 or 191
193. limit 192 to yr-"2006-2008"
194. exp Cardiovascular Diseases/pc, di, ep, et
195. Cardi$.mp.
196. 195
197. Coronary.mp.
198. heart disease$.mp.
199. Myocardial infarct$.mp.
200. exp Cerebrovascular Accident/
201. stroke.tw.
202. Transient Ischemic Attack.tw.
203. exp Ischemia/
204. cardioprotect$.mp.
205. Pulmonary Embo1$.tw.
206. Heart failure$.tw.
207. (embol$ or thromb$).tw.
208. exp Peripheral Vascular Diseases/ or peripheral artery disease.mp.
209. arterial occlusive diseases/
210. or/ 194-209
A-6
211. limit 210 to "all adult (19 plus years)"
212. exp hypertension/pc, di, ep, et
213. exp hypertension, renal/
214. hypertens$.af.
215. high blood pressure.af.
216. (eleva$ adj2 blood pressure).tw.
217. systolic blood pressure/
218. diastolic blood pressure/
219. mean arterial pressure/
220. or/212-219
221. limit 220 to "all adult (19 plus years)"
222. exp Neoplasms/db, pc, et, di, ep [Diet Therapy, Prevention & Control, Etiology, Diagnosis,
Epidemiology]
223. ("cancer risk" or "melanoma risk" or "lymphoma risk" or "leukemia risk" or "myeloma risk"
or "sarcoma risk").tw.
224. (("risk of' or "occurrence of') and (cancer$ or neoplasm$ or malignan$ or adenocarcinom$
or carcinom$ or melanom$ or lymphom$ or leuk?emi$ or myelodysplas$ or myelom$ or
sarcom$)).tw.
225. 222 or 224 or 223
226. colon polyps.mp. or exp adenomatous polyps/ or exp colonic polyps/
227. (colon$ or rectum or rectal or colorectum or colorectal).ti,ab.
228. (adenoma$ or polyps or polyp).ti,ab.
229. 228 and 227
230. 229 or 226
231. mammography.mp. or exp mammography/
232. mammog$.ti,ab.
233. 231 or 232
234. dens$.ti,ab.
235. 233 and 234
236. prostate specific antigen.mp. or exp prostate-specific antigen/
237. (aberrant crypt$ foe$ or ACF).ti,ab.
238. (prostat$ and (intraepitheli$ or intra-epitheli$ or intra epitheli$) and Neoplas$).ab,ti.
239. 236 or 238 or 235 or 237 or 230
240. type 1 diabetes mellitus.mp. or exp Diabetes Mellitus, Type 11
241. psoriasis.mp. or exp Psoriasis/
242. rheumatoid arthritis.mp. or exp Arthritis, Rheumatoid/
243. multiple sclerosis.mp. or exp Multiple Sclerosis/
244. inflammatory bowel disease.mp. or exp Inflammatory Bowel Diseases/
245. ulcerative colitis.mp. or exp Colitis, Ulcerative/
246. Crohn's disease.mp. or exp Crohn Disease/
247. 240 or 241 or 242 or 243 or 244 or 245 or 246
248. tuberculosis.mp. or exp Tuberculosis/
249. influenza.mp. or exp Influenza, Human/
250. 248 or 249
251. exp "Activities of Daily Living"/
252. muscle strength.mp. or exp Muscle Strength/
253. exp Musculoskeletal Equilibrium! or exp Walking/
254. ("balance test" or "timed walk" or "physical performance" or "hand-grip strength").tw.
255. exp Hand Strength/
256. exp Muscles/
257. ("walking time" or "muscle strength").tw.
258. or/251-257
259. limit 258 to ("all adult (19 plus years)" or "all aged (65 and over)" or "aged (80 and over)' ')
260. exp Pre-eclampsia/
261. (pre-eclampsia or preeclampsia).mp.
262. pregnancy complication$.mp. or exp Pregnancy Complications/
263. or/260-262
264. limit 263 to male
265. limit 263 to female
266. 264 not 265
267. 263 not 266
268. limit 267 to animal
269. limit 267 to human
270. 268 not 269
271. 267 not 270
272. limit 271 to english language
273. exp infant,low birth weight/
274. low birth weight.af.
275. exp infant, premature/
276. ("small for gestational age" or sga).af.
277. ((preterm or prematur$) adj6 (infant or newborn)).af.
278. or/273-277
279. exp Milk, Human/
280. human rnilk.mp.
281. (human adj2 milk).tw.
282. breast rnilk.mp.
283. breastmilk.mp.
284. breast feeding.mp.
285. breastfeed$.mp.
286. breast fed.mp.
287. breastfed.mp.
288. (breast adj2 fed).tw.
289. exp lactation/
290. (lactating or lactation).mp.
291. or/279-290
292. Mortality.mp. or exp Mortality/
293. Fatal Outcome.mp. or exp Fatal Outcome/
294. exp Death/ or exp "Cause of Death"/ or death.mp.
295. Survival Rate.mp. or exp Survival Rate/
296. 295 or 292 or 294 or 293
297. heterotopic ossification.mp. or exp Ossification, Heterotopic/
298. myositis ossificans.mp. or exp Myositis Ossificans/
299. calcinosis.mp. or exp Calcinosis/
300. extraosseous calcification.mp.
301. metaplastic calcification.mp.
302. myo-osteosis.mp.
303. neurogenic osteoma.mp.
304. osseous heteroplasia.mp.
305. ossifying fibromyopathy.mp.
306. para-articular calci'fication.mp.
307. heterotopic calcification.mp.
308. pathological bone.mp.
309. pathological calcification.mp.
310. periarticular calcification.mp.
311. synostosis.mp.
312. ectopic bone.mp.
313. heterotopic bone.mp.
314. dystrophic ossification.mp.
315. ectopic ossification.mp.
316. metaplastic ossification.mp.
317. para-articular ossification.mp.
318. periarticular ossification.mp.
319. pathological ossification.mp.
320. ectopic calcification.mp.
321. soft tissue calcification.mp.
A-9
322. (vascular adj3 calcification).mp.
323. (aort$ adj3 calcification).mp.
324. (valv$ adj3 calcification).mp.
325. or/297-324
326. limit 325 to animal
327. limit 325 to human
328. 326 not 327
329. 325 not 328
330. limit 329 to english language
3 3 1. exp kidney disease/
332. exp kidney/
333. kidney.mp.
334. renal.af.
335. nephro$.af.
336. exp renal replacement therapy/
337. exp kidney, artificial/
338. (hemodialy$ or haemodialy$ or dialy$).af.
339. exp Kidney Glomemlus/
340. exp Kidney Function Tests/
341. ur?emia.tw.
342. exp Kidney Calculi/
343. (kidney stone$ or renal stone$ or renal calcul$ or kidney calcul$ or nephrolith$).af.
344. 343 not 342
345. exp nephrolithiasis/
346. or/331-345
347. allerg$.mp. or exp Hypersensitivity/
b. Overall Search Strategy for Outcomes of Upper Limits
Database: Ovid MEDLINE(R), CCTR (from 1966 to December 2008)
1. exp Vitamin D/
2. (25-hydroxy vit D or plasma vit D or 250HD or 25-0HD).mp. [mp=title, original title,
abstract, name of substance word, subject heading word]
3. (250HD3 or "25(0H)D3" or 25-0HD3 or "25-(0H)D3").tw.
4. ("25(0H)D" or "25-(0H)D" or "25-0H-D").tw.
5. 25-hydroxycholecalciferol.tw.
6. 25-hydroxyergocalciferol. tw.
7. calcidiol. tw.
8. Calcifediol/
A- 10
9. (vit adj (d or d2 or d3)).mp.
10. Ergocalciferols/
11. Ergocalciferol$.tw.
12. Cholecalciferol/
13. Cholecalciferol$.tw.
14. calciferol. tw.
15. exp Calcium Carbonate/ or exp Calcium Citrate/ or exp Calcium Phosphates/ or exp Calcium
Malate/
16. or/ 1- 15
17. supplement$.tw.
18. exp Dietary Supplements/to, ae, po, ut [Toxicity, Adverse Effects, Poisoning, Utilization]
19. No-Observed-Adverse-Effect Level/
20. upper limit$.tw.
21. UL.tw.
22. (excess$ or toxic$).tw.
23. vit d intox$.tw.
24. (noael or noel).tw.
25. (no observed adj2 effect$).tw.
26. or/ 17-25
27. 26 and 16
28. (ANIMALS not HUMAN).sh.
29. *Dialysis/ or *hemodialysis/ or *peritoneal dialysis/
30. 27 not 28
31. 30 not 29
32. limit 31 to (addresses or bibliography or biography or comment or dictionary or directory or
duplicate publication or editorial or in vitro or interview or lectures or letter or news or "review")
33. 31 not 32
34. limit 33 to english language
35. exp kidney disease/
36. exp kidney, artificial/
37. exp Kidney Function Tests/
38. ur?emia.tw.
39. (kidney stone$ or renal stone$ or renal calcul$ or kidney calcul$ or nephrolith$).af.
40. exp nephrolithiasis/
41 . heterotopic ossification.mp. or exp Ossification, Heterotopic/
42. myositis ossificans.mp. or exp Myositis Ossificans/
43. calcinosis.mp. or exp Calcinosis/
44. extraosseous calcification.mp.
45. metaplastic calcification.mp.
A- l l
46. myo-osteosis.mp.
47. neurogenic osteoma.mp.
48. osseous heteroplasia.mp.
49. ossifying fibromyopathy.mp.
50. para-articular calcification.mp.
51. heterotopic calcification.mp.
52. pathological bone.mp.
53. pathological calcification.mp.
54. periarticular calcification.mp.
55. synostosis.mp.
56. ectopic bone.mp.
57. heterotopic bone.mp.
58. dystrophic ossification.mp.
59. ectopic ossification.mp.
60. metaplastic ossification.mp.
61. para-articular ossification.mp.
62. periarticular ossification.mp.
63. pathological ossification.mp.
64. ectopic calcification.mp.
65. soft tissue calcification.mp.
66. (vascular adj3 calcification).mp.
67. (aort$ adj3 calcification).mp.
68. (valv$ adj3 calcification).mp.
69. or/41-68
70. Calcitication, Physiologic/de [Drug Effects]
71. Hypercalcemia/
72. Kidney Calculi/
73. Nephrocalcinosis/
74. Urinary Calculi/
75. Bladder Calculi/
76. Ureteral Calculi!
77. Calcinosis/
78. Hypercalcemi$.tw.
79. (Burnett$ adj2 syndrome$).tw.
80. Hypercalciuri$.tw.
81. or/70-80
82. psoriasis.mp. or exp Psoriasis/
83. 81 or 69 or 82
A- 12
84. 34 and 83
85. limit 84 to case reports
86. 84 not 85
A- 13
Appendix B. Search strategy for systematic reviews
Databases: MEDLINE(R), the Cochrane Database of Systemic Reviews, and the
Health Technology Assessments (up to December 2008)
1. (meta-analys$ or metaanalys$).mp. [mp=title, abstract, full text, keywords, caption text]
2. (systematic review$ or systematic literature or evidence-based or evidence review$).mp.
[mp=title, abstract, full text, keywords, caption text]
3. (EBM or EBR or EBRs).mp. [mp=title, abstract, full text, keywords, caption text]
4. or/ 1-3
5. (vitamin D or cholecalciferol or ergocalciferol or hydroxy vitamin D or calcitriol).mp.
[mp=title, abstract, full text, keywords, caption text]
6. Calcium.mp. [mp=title, abstract, full text, keywords, caption text]
7. 5 or 6
8. 4 and 7
Appendix D. Evaluation of existing systematic reviews
and evidence tables of the qualified systematic
reviews
Evaluation of existing reviews
Author Year Intervention Outcome Study Healthy Only included Clear reporting Clear reporting Clear reporting Comments*
or exposure design populati on Ca +- Vit D of comparison of outcome of study
Journal included at interventions? and control definitions? designs (need
/ Source baseline?* group? separate
Reported reporting if
baseline two or more
dietary Ca different
intake with designs are
dietary included)?
assessment
methods?***
Autier 2007 Vitamin D [+/ - All cause RCTs Yes Yes Yes Yes Yes One
Arch Intern Med Calcium) mortality additional
[17846391f found
Avenell2008 Vitamin D [+/ - All cause RCTs Yes Yes Yes Yes Yes All relevant
Cochrane Calcium] mortality studies
Database of included in
Systematic Autier 2007
Reviews
[16034849f Conclusions
are same as
Autier 2007.
Allender 1996 Ca Blood RCT Yes Yes Yes Yes Yes 26 of 64
Ann Intern Med supplement pressure (subgroup potential
anal sis RCTs
Cappuccio 1995 Ca intake Blood Observat Unclear No NA Yes No REJECT
AJE pressure ional, (regressions) Includes XS
including
cross
sectional
Dickinson 2008 Ca Blood RCT No Yes Yes Yes Yes Revision of
Cochrane supplement pressure All with HTN 2006 SR
15/64
potential
RCTs
1
We excluded a study on patients with congestive heart failure in our reanalysis of data from this systematic review
2
Author Year Intervent ion Outcome Study Healt hy Only incl uded Clear reporting Clear reporting Clear reporting Comments*
or exposure design population Ca +- Vit 0 of comparison of outcome of study
Journal included at interventions? and cont rol definitions? desi gns (need
/ Source baseline?* group? separate
Reported reporting if
baseli ne two or more
dietary Ca different
intake with designs are
dietary included)?
assessment
methods?***
Griffith 1999 Ca Blood RCT Yes & No Yes Yes Yes Yes Update of
AJH supplement pressure HTN & NTN Bucher
combined 1996 (2263)
See Subgp
comment analysis
HTN vs
NTN in
Bucher only
42/64
potential
RCTs
van Mierlo 2006 Ca Blood RCT Yes Yes Yes Yes Yes 40/64
J Hum Hypert supplement pressure Subgroup of potential
HTN & NTN RCTs
Trumbo 2007 Ca Blood All Yes Yes (interv) No No No REJECT
Nutr Rev supplement pressure, Subgroup of No (observ) Qualitative
HTN, HTN & NTN only
Pregnancy- Count of sig
induced HTN studies only
Unclear if
SR.
Bergsma-Kadijk Ca intake cancer and Cohort nd (probably nd on dietary nd on Ca intake nd nd on the Reject
1996 polyp and healthy assessment (only RR!OR definition of
Case- population) method between lowest case-control
Epidemiology control and highest study
categories
re orted
Weigarten 2008 Ca cancer and RCT yes (pts with yes yes yes yes Accept
supplement polyp prior
Cochrane (> 1200 mg/ d) adenoma)
Database of
Systematic
Reviews
3
Author Year Intervention Outcome Study Healthy Only included Clear reporting Clear reporting Clear reporting Comments*
or exposure design population Ca +- Vit 0 of comparison of outcome of study
Journal included at interventions? and control definitions? designs (need
/ Source baseline?* group? separate
Reported reporting if
baseli ne two or more
dietary Ca different
intake with designs are
dietary included)?
assessment
methods?***
Davies 2006 Nutritional Cancer, RCT No (both pts nd no no yes Part of a
RCTs, recurrence of with cancer larger SR of
J Natl Cancer including Ca preinvasive and both diet
lnst supplement lesions preinvasive and physical
lesions) activity on
outcome
among
patients with
cancer or
preinvasive
lesions
Berge! maternal offspring BP RCTs& y (RCT) no yes yes no Data from 2
2007 calcium intake cohort yes RCTs may
be useful.
BMC Pediatrics Reect
Carroli 1994 Ca Preeclampsia RCT Yes Yes Yes Yes Yes Covered by
Brit J Obstet supplement latest
Gynecol Cochrane
SR
Hofmeyer 2003 Ca Preeclampsia RCT Yes Yes Yes Yes Yes Covered by
S African J Supplement latest
Cochrane
SR
Hofmeyer 2007 Ca Preeclampsia RCT Yes Yes Yes Yes Yes Covered by
S African J Supplement (and latest
summary of Cochrane
the outcomes SR
mentioned
above
4
Author Year Intervention Outcome Study Healthy Only included Clear reporting Clear reporting Clear reporting Comments*
or exposure design population Ca +- Vit 0 of comparison of outcome of study
Journal included at interventions? and control definitions? designs (need
/ Source baseline?* group? separate
Reported reporting if
baseli ne two or more
dietary Ca different
intake with designs are
dietary included)?
assessment
methods?***
Hoffmeyr 2006 Ca Preeclampsia, RCT Yes Yes Yes Yes Yes Eligible
Cochrane supplement pregnancy review
Database of induced
Systematic hypertension
Reviews with and
without
proteinuria,
maternal
death or
serious
morbidity,
other
maternal
outcomes,
stillbirth,
neonatal
mortality
or morbidity,
preterm birth,
small
gestational
age, and
other
outcomes for
the child
Bucher1996 Ca Preeclampsia, RCT Yes Yes Yes Yes Yes Covered by
JAMA supplement pregnancy- latest
induced Cochrane
h ertension SR
Gao calcium intake prostate prospecti yes yes yes yes yes
2005 or dairy cancer ve cohort (assumed
product from study
NCI desi n
Shaukat 2005 Ca recurrent RCT yes (pts with no (1/3 included yes yes? yes? "RCT" Reject
supplement polyp prior Ca+Vit "recurrence of
AmJ adenoma) AIC/E+selenium adenoma"
Gastroenterol )
5
Author Year Intervention Outcome Study Healthy Only included Clear reporting Clear reporting Clear reporting Comments*
or exposure design population Ca +- Vit 0 of comparison of outcome of study
Journal included at interventions? and control definitions? designs (need
/ Source baseline?* group? separate
Reported reporting if
baseli ne two or more
dietary Ca different
intake with designs are
dietary included)?
assessment
methods?***
Barr 2003 Increased Weight RCTs Yes Yes (separate yes yes yes No meta-
J Nutr dairy product "healthy" studies of analysis.
or calcium increased dairy Included
intake (from product and children and
supplements) those of calcium adults
su lements)
Trowman 2006 Calcium Weight RCTs Yes Yes (Separate yes yes yes May need to
Br J Nutr supplements (excluded meta-analyses redo the
or increased populations for calcium meta-
provision of with severe supplement and analyses to
dairy products co- increased separate out
morbidities, provision of energy
such as dai ry products) restriction
renal diet studies.
problems or This SR
cancer) included
adults onl
Wi nzenberg calcium weight RCTs yes yes yes yes yes 2
2
analysis
2007 supplementati of RCTof
on food or calcium on
Obesity chemical bone
density
outcome
Lanou 2008 Calcium or Weight, body RCTs nd yes no yes yes Included
Nutr Rev dairy fat both dairy
supplementati and calcium
on with or supplement
without ation RCTs.
energy No
restriction individual
study
characteristi
cs re orted
*Either included only healthy population at baseli ne or SR had separate analyses for population with diseases and without diseases
**For SR of interventional studies
***For SR of observational studies
****Please comment on issues such as update of previous SRs or specific reasons for using or not using the SR, other than not fulfill ing the screening criteria.
6
Evidence table of systematic review of the effect of vitamin D on bone health
Author Year [PMID] Cranney 2007 [18088161]
Design Systematic review of RCTs and observational studies
Population Include all ages
Intervention (Exposure) and
Comparator
Exclude secondary causes of osteoporosis (e.g. , glucocorticoid-induced, renal or liver
disease)
Exclude studies on the treatment of vitamin Ddependent rickets (to minimize clinical
heterogeneity as treatments is often non-dietary sources of vitamin D)
Intervention (Exposure):
Include vitamin 02 or 0
3
with or without calcium.
Exclude vitamin D preparations, calcitriol, alphacalcidol (because they are not nutritional
supplements, and have different safety profile)
Comparator:
No vitamin D or lower doses/levels of vitamin D
Results See text for summary results for the following outcomes in both vitamin D and combined vitamin
D and calcium sections of the report:
Rickets
Fractures, falls, or performance measures
Bone mineral density or bone mineral contents
How does dietary intake of vitamin D from fortified foods and vitamin D
supplementation affect serum 25(0H)D Concentrations
Adverse events
Comments Case-control studies were included but always summarized separately from cohort studies and
RCTs. Meta-analyses were performed to pool results from RCTs only.
AMSTAR
A priori design? Study quality assessment performed?
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
No
Yes
Yes
Study quality appropriately used in analysis?
Appropriate statistical synthesis?
Publication bias assessed? All publication types and languages included?
Included and excluded studies listed? Conflicts of interest stated?
Study characteristics provided?
Evidence table of systematic review on vitamin D supplementation and all-cause mortality
Author Year [PMID]
Design (Search Years)
Population
Intervention (Exposure)
and Comparator
Results
Comments
Autier 2007 [17846391]
Randomized controlled trials (1992-2006)
Community dwelling or institutionalized adults
Supplementary vitamin D (at least 1000 mg/ d) without calcium vs. placebo or no treatment
18 trial s of combined vitamin D and vitamin D + calcium
RR: 0.93 (95% Cl 0.87, 0.99); favoring vitamin D (calcium) supplementation
Statistically homogeneous
In our reanalysis we and excluded 3 of 18trials and separated studies with vitamin D only from
those with vitamin D and calcium combination.
For details and results of our reanalysis, see text.
See text in vitamin D and vitamin D + calcium sections for reanalyses of the separated trials.
Study participants, vitamin D assays, and vitamin D status are not described in detail.
AMST AR Criteria
Yes
Yes
Yes
No
Yes
A priori design? Yes Study quality assessment performed? No
Two independent reviewers?
Comprehensive literature search?
No Study quality appropriately used in analysis? NA
Yes Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Yes Publication bias assessed? No
No Conflicts of interest stated? Yes
Study characteristics provided? Yes The meta-analysis did not perform quality assessment
(neither using individual quality items nor using quality
scores
Evidence table of systematic review of calcium on growth in children
Author Year [PMID]
Design (Search Years)
Population
Intervention (Exposure) and
Com arator
Results
Winzenberg 2007 [17636098]
Randomized controlled trials (1966-2005)
Children <18 y
Supplemental and dietary calcium 300 1200 mg/d vs. placebo
17 trials (2088 participants)
Weighted mean difference: +0.14 (95% Cl -0. 28, +0.57) Kg; favors control
Weighted mean difference: +0.22 (95% Cl -0.30, +0.74) em; favors control
No significant statistical heterogeneity
7
Comments
A priori design?
Post hoc analysis performed on trials identified for a metaanalysis of randomized controlled trials
of calcium on bone outcomes
AMSTAR
Study quality assessment performed? Yes
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
No
No
Yes
Study quality appropriately used in analysis? No
Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Publication bias assessed? Yes
Conflicts of interest stated? No
Study characteristics provided? Unclear if all languages included; study quality assessed but not
factored into the M-A
Evidence table of systematic review s of calcium and blood pressure
Author Year [PMID] Griffith 1999 (1 0075392)
Design (Search Years) Randomized controlled trials (1966-1997)
Population Both hypertensive and normotensive participants
Intervention and Comparator Dietary and nondietary calci um supplementation versus placebo (no supplement)
Dose range 600-2000 mg (36% 1000 mg; 26% 1500-1600 mg; 12%2000 mg)
Results 42 trials
SBP: -1.44 (-2.20, -0.68)
2
; statistically heterogeneous
DBP: -0.84 (-1.44, -0.24); statistically heterogeneous
Subgroup analyses did not find that heterogeneity could be explained by age, sex, baseline
calcium, dietary versus nondietary calcium, or quality.
Subgroups with hypertensive versus normotensive people were significantly different (no
further details).
Conclusions similar to previous systematic review (Bucher 1996{2263 /id})
Comments Update of Bucher 1996{2263 /id) (see below).
AMSTAR
A priori design? Study quality assessment performed? Yes
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
Yes
Yes
Yes
Study quality appropriately used in analysis? No
Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Publication bias assessed? No
Conflicts of interest stated? No
Study characteristics provided?
Author Year [PMID]
Design (Search Years)
Population
Intervention and Comparator
Results
Comments
A priori design?
Study qual ity not discussed in conclusions. Funding
source reported, but not conflict of interest.
van Mierlo 2006 [166730 11)
Randomized controlled trials (1966-2003)
Both hypertensive and normotensive partici pants
Calcium supplementation versus placebo (no supplement)
Dose range 355-2000 mg (40% 1000 mg; 32% 1500-1 600 mg; 6% 2000 mg)
40 trials
SBP: 1.86 (95% Cl -2.91, -0.81 ); statistically heterogeneous
DBP: -0.99 (95% Cl -1.61, -0.37); statistically heterogeneous
In multivariable analysis including age, sex, initi al calci um intake, calci um dose, and initial
blood pressure:
SBP DBP
Age <45 y -1.45 (-2.99, +0.09) -1.26 (-2.20, -0.33)
~ 4 5 y -2.33 (-3.69, -0.96) -0.80 (-1.62, +0.02)
Male S50% -2.20 ( -3.68, -0. 72) -1.12 ( -1 .98, -0.26)
>50% -1.77 (-3.13, -0.42) -0.84 (-1.65, -0.04)
Initial BP <140/90 mm Hg -2.04 (-3.40, -0.68) -1.04 (-1.86, -0.22)
~ 1 4 0 9 0 mm Hg -1.85 (-3.45, -0.32) -0.89 (-1 .79, +0.01)
Cadose S1000 mg -2.17 (-3.59, -0.75) -1.41 (-2.24, -0.59)
>1000mg -1.75(-3.20,-0.31) -0.56(-1.40,+0.29)
Blood pressures not statistically significantly different between any strata.
AMSTAR
Study quality assessment performed? Yes
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
Unclear
Partial
Yes
Study quality appropriately used in analysis? No
Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
2
Nwnbers in parentheses are 95% confidence intervals
8
Publication bias assessed? Yes
Conflicts of interest stated? Yes
No data on inclusion of unpublished data. Excluded
studies available from authors
Evidence table of systematic review s of calcium and blood pressure. continued
Author Year [PMID] Bucher 1996 [8596234]
Design (Search Years) Randomized controlled trials (1966-1994)
Population Both hypertensive and normotensive participants
Intervention and Comparator Dietary and nondietary calcium supplementation versus placebo (no supplement)
Dose range 406-2000 mg (41% 1000 mg; 31% 1500-1600 mg; 8%2000 mg)
Results 33 trials
[Overall summary results were updated in Griffith 1999{1 927 /id), above]
Studies with specified subgroups of hypertensive and normotensive participants (6 trials):
Hypertensives SBP -4.30 (-6.47, -2.13) DBP -1.50 (-2.77, -0.23)
Normotensives SBP -0.27 (-1.80, +1.27) DBP -0.33 (-1.56, +0.90)
Regression analyses:
BP (continuous scale) SBP OR = 0.99 (0.96, 1.01) DBP OR = 0.99 (0.96, 1.03)
Dose of calcium, duration of supplementation, dietary vs nondietary calcium supplementation,
methodological quality did not demonstrate a relationship with the magnitude of treatment effect.
Comments Updated in Griffith 1999(1927 /id) (see above)
AMSTAR
A priori design? Study quality assessment performed?
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
Yes
Yes
Yes
Study quality appropriately used In analysis?
Appropriate statistical synthesis?
Publication bias assessed? All publication types and languages included?
Included and excluded studies listed? Conflicts of interest stated?
Study characteristics provided?
Author Year [PMID]
Design (Search Years)
Population
Intervention and Comparator
Results
Comments
Fundi ng source reported, but not conflict of interest.
Allender 1996 [861 0952]
Randomized controlled trials ( 1982-1993)
Both hypertensive and normotensive participants
Dietary and nondietary calcium supplementation versus placebo (no supplement)
Dose range 400-2160 mg (35% 1000 mg; 29%1500-1600 mg; 10%2000 mg)
26 trials (22 trials included in metaanalyses)
SBP: 0.89 (1.74, 0.05)
DBP: -0.18 (-0.75, +0.40)
Hypertensives SBP -1.68 (-3.18, -0.18) DBP +0.02 (-0.96, +1.00)
Normotensives SBP -0.53 (-1.56, +0.49) DBP -0.28 (-0.99, +0.42)
By weighted linear regression analyses, age, sex, calcium dose, trial duration were not
associated with treatment effect (P>0.1 O)
AMSTAR
Yes
Yes
Yes
No
No
A priori design? Yes
Yes
Yes
Yes
No
Yes
Study quality assessment performed? No
Two independent reviewers?
Comprehensive literature search?
All publication types and languages Included?
Included and excluded studies listed?
Study characteristics provided?
Author Year [PMID] Cappuccio 1989 [2697729)
Study quality appropriately used in analysis? No
Appropriate statistical synthesis? No
Publication bias assessed? No
Conflicts of interest stated? No
Excluded studies not enumerated or listed. Fixed effects
models used.
Design (Search Years) Randomized controlled trials ( 1983-1988)
Population
Intervention and Comparator
Results
Comments
A priori desi gn?
Both hypertensive and normotensive participants
Nondietary calcium supplementation versus placebo (no supplement) or low calcium intake
Dose range 800-1600 mg (60% 1000 mg; 27% 1500-1600 mg)
15 trials
SBP (supine): -0.13 (0.46, +0. 19)
DBP (supine): +0.03 (-0.17, +0.22)
Hypertensives SSP +0.06 (-0.59, +0.72) DBP +0.03 (-0.21, +0.27)
AMSTAR
Study quality assessment performed? No
Two independent reviewers?
Comprehensive literature search?
Yes
nd
Yes
nd
No
Yes
Study quality appropriately used in analysis? NA
Appropriate statistical synthesis? No
All publication types and languages included?
Included and excluded studies listed?
Study characteristi cs provided?
9
Publication bias assessed? No
Conflicts of interest stated? No
Excluded studies not enumerated or listed. Fixed effects
models used.
Evidence table of systematic review s of calcium and blood pressure. continued
Author Year [PMID] Dickinson 2006 [16625609)
3
Design (Search Years) Randomized controlled trials (1982-2003/2005
4
)
Population Hypertensive participants
Intervention and Comparator Dietary and nondietary calcium supplementation versus placebo (no supplement)
Dose range 400-2000 mg (50% 1000 mg; 25% 1500-1600 mg; 6% 2000 mg)
Results 13 trials
Comments
A priori design?
SBP: -2.53 (4.45, -0.60); statistically heterogeneous
DBP: -0.81 {2.07, +0.44); statistically heterogeneous
Ca dose <1200 mg SBP -2.67 (-5.15, -0. 18) DBP -0.75 (-2.13, +0.63)
Ca dose 1200-2000 mg SBP -2.69 (-5.86, +0.47) DBP -0.78 (-3.82, +2.25)
Not statistically significantly different by calcium dose
AMSTAR
Study quality assessment performed? Yes
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
Yes
Yes
Yes
Study quality appropriately used in analysis? Yes
Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
Publication bias assessed? Yes
Conflicts of interest stated? Yes
Evidence table of systematic review of calcium on growth in children
Author Year [PMID] Winzenberg 2007 [17636098]
Design (Search Years) Randomized controlled trials (1966-2005)
Population Children <18 y
Intervention (Exposure) and Supplemental and dietary calcium 300-1200 mg/d vs. placebo
Com arator
Results
Comments
A priori design?
17 trials (2088 participants)
Weighted mean difference: +0. 14 (95% Cl -0.28, +0.57) Kg; favors control
Weighted mean difference: +0.22 (95% Cl -0.30, +0.74) em; favors control
No significant statistical heterogeneity
Post hoc analysis performed on trials identified for a metaanalysis of randomized controlled trials
of calcium on bone outcomes
AMSTAR
Study quality assessment performed? Yes
Two independent reviewers?
Comprehensive literature search?
Yes
Yes
Yes
No
No
Yes
Study quality appropriately used in analysis? No
Appropriate statistical synthesis? Yes
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
Publication bias assessed? Yes
Conflicts of interest stated? No
Unclear if all languages included; study quality assessed but not
factored into the M-A
3
A technical update, with no further studies added was published in the Cochrane database in 2008.
4
Different dates for different databases.
10
Evidence table of systematic review on calcium intake and adenoma recurrence
Author Year [UI] Weingarten, 2008 [18254022)
Design Randomized controlled trials: Cochrane Library Issue 2, 2007, the Cochrane Colorectal Cancer
Group (CCCG) specialized register, MEDLINE {1966 to July 2007 ), Cancerlit {1963 to April
2002), Embase (1980 to July 2007)
Population
Intervention (Exposure) and
Com arator
Results
Comments
A priori design?
Healthy adults and studies of adults at higher risk of colon cancer due to family history, previous
adenomatous polyps, or inflammatory bowel disease
Calcium (> 1200 mg/d) vs. placebo
Calcium vs. placebo
colorectal adenoma recurrence: OR 0.74, Cl 0.58-0.95, P=0.02
CRC: OR 0.34, Cl 0.05-2.15, P=0.20
at least one adverse event requiring discontinuation: OR 0.93, Cl 0.42-2.05, P=0.80
Based only on two RCTs (1346 participants). Heterogeneity due to different dose of
supplementation (one RCT supplemented with 1200 mg/d and the other RCT with 2000 mg/d).
Analysis based on fixed effects model; however, considering there are only two studies, random
effects model might have been more appropriate. Analysis on adverse events is based only on
reported data of one out of the two RCTs (Barron 1999). Only participants with high risk due to
previous adenomas were recruited in these two RCTs; therefore, applicability of the results can
only be considered for high risk population. Insufficient evidence to recommend the general use
of calcium supplements to prevent colorectal adenoma or colorectal cancer
AMSTAR
Study quality assessment performed?
Two independent reviewers?
Comprehensive literature search?
X
X
X
Study quality appropriately used in analysis?
Appropriate statistical synthesis?
Publication bias assessed?
X
X
X
All publication types and languages included?
Included and excluded studies listed?
Study characteristics provided?
X
X
Conflicts of interest stated? X
11
Appendix E. Blank Data Extraction Form and Quality
Assessment Checklists
ELIGIBILITY CRITERIA AND OTHER CHARACTERISTICS
Ul Author Study Design*
Inclusion Exclusion Enrollment Years Trial or Cohort Name Funding Source Extractor
Year
RCT
RCT-post hoc ..
Other intervention study
Cohort study
Case-cohort study
.
Leave appropnate cho1ce of study des1gn and delete all others
**Post hoc analyses of an existing RCT for outcomes that were not planned in the original RCT
POPULATION (BASELINE)'*
Location
Mean Age Anthropometry data
Specific Nutrition
Author Study (e.g., City and N N Male, Race / Health Status Data (e.g.,
Ul
Year Design Country, enrolled*** analyzed
(SO) Range I
% Ethnicity
(e.g., BMI, weight, or
Status malnourish, low Vit D
latitude)
Age, yr IQR %body fat ... etc)
orCa intake ... etc.)
' Please copy from above
**Report baseline data for all subjects: preferred data for subj ects actually analyzed than for subjects that enrolled in the study.
***For ACT, N enrolled is the number of subjects randomized. For cohort study, N enrolled is the total number of subjects fulfilled study inclusion criteria. For case-cohort study, please
report as detailed information as possible on subjects selection. For example, original cohort sample size, number of subjects provided exposure data (eg. blood sample or dietary
assessment), number of subj ects had outcome data .. . etc.
B k do ac tgroun 1et
Internal Calibration
Analytical
Season/Date
Dietary Food (or Validity) of
Validity of Time between
when the Background
Author Biomarker Biomarker Data Biomarker
Ul
Year
Exposure Assessment Composition Dietary
Assay**** Reported? (y/n) Sampling and
biomarker exposure
Method** Database*** Assessment? (y/n)
If Yes, Provide Analysis
samples were data
If Yes, Provide Data
Data
drawn
25(0H)D
and/or
1,25(0HhD
Dietary
calcium
intake
Wnte "nd" 1f t here was no data reported. Please do not leave blank
**Please refer to common dietary assessment method table. If other method was used, please describe the detail. Otherwise, please simply use the brief name described in the table
. .. USDA Nutrient Database, Minnesota Food and Nutrient Database (NDSR), Food product manufacturer, McCance and Widdowson's food table, Country-specific food tables, Other
nutrient analysis (please specify)
... *ONLY biomarker of interest for calcium is calcium balance
INTERVENTION(S), SKIP IF OBSERVATIONAL STUDY
Ul
Author
lntervention(s)
Source (e.g., brand name, foods, or Vit D and/or Ca Total Interventi on Intervention Frequency (e.g. capsules were
Year formulation) Daily Dose Duration taken 2 times a day)
Co-intervention(s) *:
Compliance/ Adherence:
Duplicate one row per 1ntervent1on, mclud1ng control mtervent1 on.
*Report the non-vit D orCa intervention(s) (e.g., other drug interventi on, or background low-fat diet). We are interested in only independent effect of vitamin D and/or calcium.
Therefore, describe how effects of co-intervention(s) were controlled for in the analyses or study design.
LIST OF ALL OUTCOMES
Ul
Author
Primary I Secondary Outcome** Outcome Definition
Year
Duplicate one row per outcome of 1nterest. Only need to list outcomes that were included in the result section.
'*Must have been explicitly stated in the original paper. Otherwise, please enter ''nd''
-----Confounders: Please report all confounders controlled in the analyses reported in the following result section
(adjusted results}
Ul Author
Confounder Groups
Please Li st Name of Confounder (including Specific comments for
Year matching factors) confounders
Other nutrients or dietary factors (e.g., certain food consumption), including
supplement use and total energy intake
Demographics (e.g., age, gender, race, education)? Yes/no*
Anthropometries (e.g., BMI, body weight,% body fat)? Yes/no*
Medical conditions
Medication
Sunlight exposure and its proxy variables (e.g., seasonal variation of 25(0H)D, UV
exposure, location)
Smoking and other life styles variables (e.g., physical activity, occupation, alcohol Yes/no*
consumption)
Other
' Please choose "yes" 1f any one of the confounders m th1s group was controlled 1n the analys1s
FOLLOWING IS RESULT SECTION. PLEASE CHOOSE APPROPRIATE TYPE OF DATA COLLECTION TABLE FOR
ALL OUTCOMES OF INTEREST
-----Main Analyses (For analyses that adjusted for confounders, choose the " best" model)
2 ARMS/GROUPS: DICHOTOMOUS OUTCOMES (e.Q. OR, RR. %death)
Author Exposure I
Mean
N N Outcome Metric (e.g. OR, RR, HR, %)
Unadjusted
Ul
Year
Outcome
Intervention
Follow-up,
Event Total and direction of comparison* Result
95%
mo Cl
.................................
*Example: OR Ca/placebo
2 ARMS/GROUPS: CONTINOUS OUTCOMES (e.Q BMD, BP)
Author Exposure I
Mean
No. Baseline Cl Final or
Final or
Net
Ul
Year
Outcome Unit
Intervention
Follow-up,
Analyzed
Baseline
I SE / SO* Delta**
Delta Cl /
difference
mo SE I SD*
--
------- --
------M"
..............___ , ...........
Basell ne=basellne value; Fmal=flnal value; Delta=change value from baseline, wh1ch IS Fmai-Basell ne value; Net d1fference=d1fferences m deltas
*Enter outcome metric reported in the unadjusted or adjusted result section
**Delta value is preferred than the Final value. Please report the direction for the change by using "+" or "-" sign: e.g. +2.8 or -2.8
~ ARMS/GROUPS: DICHOTOMOUS OUTCOMES (e.Q. OR, RR, %death)
Exposure
Mean Mean
Author
Categories( e.g.,
Vit D Ca
Ul
Year
Outcome Tertiles) I
level / level 1
Intervention
dose dose
Groups
Duplicate one row per exposure category or mtervent1on group.
' Number of subjects with outcome
'*Please choose one and delete the others
No. of
Cases
(Event)*
... Specify the comparison. For example group 1 vs. 3 = -6; group 1 vs. 2 = -8
No. of
Non-
cases I
Total
N ..
****P value for testing the linear trend of the OR/RR across different categories or doses
Outcome
Mean Crude or Metric
Follow-up, Adjusted (e.g. OR,
mo analysis? RR, HR,
%)
Outcome
effect
size
Adjusted
p
Result
95%
p
btw Cl btw
Net difference
p
Cl I SE I SD* between
Cll
SE
p
P for
I between
trend* .. '
so groups***
..
<:::2 ARMS/GROUPS: CONTINOUS OUTCOMES (e.q BMD, BP)
Crude or Final
Exposure Adjusted
Mean Baseline Final
or
Author Category I analysis? No. Delta
Ul
Year
Outcome Unit
Intervention
Follow-up
Analyzed
Baseline Cl/ SE I or
Cl/
Group
(months) SO* Delta**
SE /
SO*
Duplicate one row per exposure category or 1ntervenlion group. Please wnte "nd" 1f there was no data reported. DO NOT LEAVE BLANK.
*Please choose one and delete the others
**Delta value is preferred than the Final value. Please report the direction for the change by using"+" or "-" sign: e.g. +2.8 or -2.8
specify the comparison. For example group 1 vs. 3 = -6; group 1 vs. 2 = -8
Net
Net difference
difference* ** Cl/ SE I
SO*
MEAN DATA. THIS SHOULD ONLY APPLY TO CASE-COHORT STUDIES THAT COMPARE BASELINE VIT D I CA LEVELS BETWEEN CASES {WITH DISEASE) AND
CONTROLS (WITHOUT DISEASE)
Time between
Crude or Mean
Vit 0
Mean Ca CaCI
p
Ul
Author Outcome Baseline Exposure
Adjusted
No.
25(0H)O
leveiCI
intake or / SE / between
Year Group and Outcome Analyzed / SE I
Assessments
analysis? Level
SO*
Ca balance SO* groups
Cases:
Control :
Duplicate one table per outcome
OTHER RESULTS ONLY USE THE FOLLOWING BOX WHEN THE TYPE OF RESULT DATA DO NOT FIT THE TABLES PROVIDED ABOVE
Ul
Ul
Author
Year
Author
Year
Outcome Results
Comments for Results
-----Subgroup Analyses
Please copy the appropriate table above for all subgroup analyses of interest.
P between
groups***
QUALITY of INTERVENTI ONAL STUDIES
Appropriate
Appropriate
Blinded Intention Appropriate Assessment
Clear
Author Randomization
Allocation Washout Dropout
Outcome to Treat Statistical for
Reporting
OVERALL
Ul
Year
Design
Technique
Conceal ment Period Rate
Assessment Analysis Anal ysis* Confounding
with No
Grade
(y/n/nd/NA)
(y/n/nd/NA) (y/n/ nd/NA) <20%
(y/n/nd) (y/n/nd) (y/n) (y/n/nd/NA)
Discrepancies
(y/n)
Adverse Event(s): ** I
Explanation for Overall Quality Grade (if not Grade A):
I
NA:not applicable
*Please do not copy the 4 categories of study designs from above sections. Specify the exact study design: RCT - Parallel , RCT - Cross-over, RCT - Cluster, quasi-RCT,
Non-randomized, but controlled trial, before-and-after trial , other interventional design (please explai n in detail)
**Please do not leave blank. Type nd if there was no data on adverse events.
QUALITY of COHORT OR NESTED CASE-CONTROL STUDIES
Ul
Author
Population Exposure (All)
Dietary
Biomarkers
Year assessment*
a) Exposure
a) One of the
a) Eligibility assessor a) Method
prespecified
methods* ..
criteria clear? blinded to reported?
was used?
(y/n) outcome info? (y/n)
(y/n)
(y/n)
...........................................................
-
b) Outcome
b) Food Time from
b) Sampling
assessor
composition sample
of population
blinded to
database or collection to
random or suppl sample
consecutive?
exposure
composition analysis
measurement?
(y/n)
(y/n)
reported? reported?
(vinl
----
...................................
---
c) Internal
calibration of
method
perform (if
FFQ)?
(y/n/NA)
OVERALL Grade (AlB/C):
Explanation for Overall Quality Grade (If not Grade A):
*Check " NA" and sk1p all questions 1f study d1d not use dietary assessment or biomarkers
.. We will judge in the end if the set of confounders is adequate
... Prespecified methods: HPLC, RIA kits, LC-MS/MS; EIA/Chemiluminescence
Comparator
Statistical
Outcome Design
Anal ysis
a) Clear
a) Level of the
definition of
a) Prospective
outcome,
exposure in
a) Adjusted or including time of
coll ection of
comparative
matched for ascertainment?
data? (y/n)
categories (eg
ANY (y/n)
quartiles) is
confounders
given
(ranges)? (y/n)
(other than b) Analysis
applicable for
age and b) Loss to was planned
categorical
sex)?** (y/n) follow-up <20%? when cohort
(y/n) was formed?
analyses only
(y/n)
- --- --
b)
c) Justification
Justification
of fi nal
c) Do the of sample size
adjusted
authors specify (includes
model
a primary sample size
selection?
outcome? (y/n) calculations)?
(y/n)
(y/n)
Appendix F. Excluded Studies
Excluded Study
Aalberts JS, Weegels PL, van der HL et al. Calcium supplementation:
effect on blood pressure and urinary mineral excretion in normotensive
male lactoovovegetarians and onmivores. American Journal of Clinical
Nutrition 48 ( 1 ): 131-8, 1988.
Abbasi AA, Chemplavil JK, Farah S, Muller BF, Arnstein AR.
Hypercalcemia in active pulmonary tuberculosis. Annals of Internal
Medicine 90 (3):324-8, 1979.
Abrams SA, Griffin IJ, Hawthorne KM, Ellis KJ. Effect ofprebiotic
supplementation and calcium intake on body mass index. Journal of
Pediatrics 2007; 151 (3):293-298.
Adams JS, Lee G. Gains in bone mineral density with resolution of
Vitamin D intoxication. Annals oflnternal Medicine 127 (3):203-6,
1997.
Akcakus M, Koklu E, Budak N, Kula M, Kurtoglu S, Koklu S. The
relationship between birthweight, 25-hydroxyVitamin D concentrations
and bone mineral status in neonates. Annals ofTropical Paediatrics
2006; 26(4):267-275.
Ala-Houhala M, Koskinen T, Terho A, Koivula T, Visakorpi J. Maternal
compared with infant Vitamin D supplementation. Archives of Disease
in Childhood 61 (12): 1159-63, 1986.
A1a-Houhala M. 25-HydroxyVitamin D levels during breast-feeding
with or without maternal or infantile supplementation of Vitamin D.
Journal of Pediatric Gastroenterology & Nutrition 4(2):220-6, 1985.
Ahnendingen K, Hofstad B, Vatn MH. Dietary habits and growth and
recurrence of colorectal adenomas: results from a three-year endoscopic
follow-up study. Nutrition & Cancer 49 (2): 131-8, 2004.
Almendingen K, Hofstad B, Vatu MH. Lifestyle-related factors and
colorectal polyps: preliminary results from a Norwegian follow-up and
intervention study. European Journal of Cancer Prevention 11(2): 153-8,
2002.
Almendingen K, Trygg K, Hofstad B, Veierod MB, Vatu MH. Results
from two repeated 5 day dietary records with a l y interval among
patients with colo rectal polyps. European Journal of Clinical Nutrition
55 (5):374-9, 2001.
Al-oanzi ZH, Tuck SP, Raj Net al. Assessment of Vitamin D status in
male osteoporosis. Clinical Chemistry 52 (2):248-54, 2006.
Aloia JF, Talwar SA, Pollack S, Feuerman M, Yeh JK. Optimal Vitamin
D status and serum parathyroid hormone concentrations in African
American women. American Journal of Clinical Nutrition 84 (3):602-9,
2006.
Anonymous. Calcium supplementation during pregnancy reduces the
risk of developing preeclampsia in nulliparous women. Canadian Family
Physician 45:614, 618-20, 1999.
1
Reason
No outcomes of interest
No UL outcomes
Not a calcium intervention trial
Case report
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Not RCT arrow 4 study
In Ottawa EPC report
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No outcomes of interest
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No outcomes of interest
Editorial-like brief review
Excluded Study
Anonymous. Vitamin D supplementation for northern native
communities. Indian and Inuit Health Committee, Canadian Paediatric
Society. CMAJ Canadian Medical Association Journal 138 (3):229-30,
1988.
Armitage NC, Rooney PS, Gifford KA, Clarke PA, Hardcastle JD. The
effect of calcium supplements on rectal mucosal proliferation. British
Journal of Cancer 71 (1):186-90, 1995.
Armstrong AL, Oborne J, Coupland CA, Macpherson MB, Bassey EJ,
Wallace WA. Effects of hormone replacement therapy on muscle
petformance and balance in post-menopausal women. Clinical Science
91 (6):685-90, 1996.
Arunabh S, Pollack S, Yeh J, Aloia JF. Body fat content and 25-
hydroxyVitamin D levels in healthy women. Joumal of Clinical
Endocrinology & Metabolism 88 (!): 157-61, 2003.
August P, Helseth G, Cook EF, Sison C. A prediction model for
superimposed preeclampsia in women with chronic hypertension during
pregnancy. American Joumal of Obstetrics & Gynecology. 191(5):1666-
72, 2004 Nov.
August P, Marcaccio B, Gertner JM, Druzin ML, Resnick LM, Laragh
JH. Abnonnal I ,25-dihydroxyVitamin D metabolism in preeclampsia.
American Journal of Obstetrics & Gynecology 166 (4): 1295-9, 1992.
Back 0, Blomquist HK, Hernell 0, Stenberg B. Does vitamin D intake
during infancy promote the development of atopic allergy? Acta
Dermato -Venereologica 89 (1):28 -32,2009.
Bailey BW, Sullivan DK, Kirk EP, HallS, Donnelly JE. The influence
of calcium consumption on weight and fat following 9 months of
exercise in men and women. Journal of the American College of
Nutrition 2007; 26(4):350-355.
Bakker R, Rifas-Shiman SL, Kleinman KP, Lipshultz SE, Gillman MW.
Maternal calcium intake during pregnancy and blood pressure in the
offspring at age 3 years: a follow-up analysis of the Project Viva cohort.
American Journal of Epidemiology 168 ( 12 ): 1374 -80 , 2008.
Baron .TA, Beach M, Mandel JS et al. Calcium supplements and
colorectal adenomas. Polyp Prevention Study Group. Annals of the New
York Academy of Sciences 889:138-45, 1999.
Baron .TA, Beach M, Mandel .TS et al. Calcium supplements for the
prevention of colorectal adenomas. Calcium Polyp Prevention Study
Group .. New England Journal ofMedicine 340 (2):101 -7, 1999.
Baron .TA, Tosteson TD, Wargovich MJ et al. Calcium suppl ementation
and rectal mucosal proliferation: a randomized controlled tri al. . Joumal
of the National Cancer Institute 87 (17):1303-7, 1995.
Barr SI. Calcium and body fat in petipubertal girls: cross-sectional and
longitudinal observations. Obesity 2007; 15(5):1302-1310.
Barsoum GH, Hendrickse C, Winslet MC et al. Reduction of mucosal
crypt cell proliferation in patients with colorectal adenomatous polyps by
dietary calcium supplementation. British Journal of Surgery 79 (6):581-
3, 1992.
2
Reason
Review paper
No outcomes of interest
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
>=20% subjects with diseases
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
combination of vit D/Ca and other
treatment w/o analysis of independent
effect
No outcomes of interest
age <18 (BP outcome)
Duplicate publication (see Baron 1999
NEJM)
In Weigarten 2008 systematic review
No outcomes of interest
Not RCT growth study
No outcomes of interest
Excluded Study
Basile LA, Taylor SN, Wagner CL, Horst RL, Hollis BW. The effect of
high-dose Vitamin D supplementation on serum Vitamin D levels and
milk calcium concentration in lactating women and their infants.
Breastfeeding Medicine: The Official Journal of the Academy of
Breastfeeding Medicine 2006; I (I ):27-35.
Belizan JM, Villar J, Berge! E eta!. Long-term effect of calcium
supplementation during pregnancy on the blood pressure of offspring:
follow up of a randomi sed controlled trial.. BMJ 315 (71 03):281 -5,
1997.
Belizan JM, Villar J, Gonzalez L, Campodonico L, Berge! E. Calcium
supplementation to prevent hypertensive disorders of pregnancy .. New
England Journal of Medicine 325 (20): 1399 -405, 1991.
Belizan JM, Villar J, Pineda 0 et al. Reduction of blood pressure with
calcium supplementation in young adults. JAMA 249 (9): 1161 -5, 1983.
Belizan JM, Villar J, Zalazar A, Roj as L, ChanD, Bryce GF.
Preliminary evidence of the effect of calcium supplementation on blood
pressure in normal pregnant women. American Journal of Obstetrics &
Gynecology 146 (2): 175 -80, 1983.
Bell NH, Epstein S, Greene A, Shary J, Oexmann MJ, Shaw S. Evidence
for alteration of the Vitamin D-endocrine system in obese subjects.
Journal of Clinical Investigation 76 (1):370-3, 1985.
Bell NH, Epstein S, Shary J, Greene V, Oexmann MJ, Shaw S. Evidence
of a probable role for 25-hydroxyVitamin Din the regulation of human
calcium metabolism. Journal of Bone & Mineral Research 3(5):489-95,
1988.
Bell NH, Godsen RN, Henry DP, Shary J, Epstein S. The effects of
muscle-building exercise on Vitamin D and mineral metabolism. Journal
of Bone & Mineral Research 3(4):369-73, 1988.
Bell NH. Hypercalcemic and hypocalcemic disorders: diagnosis and
treatment. Nephron 23(2-3):147-51, 1979.
Berggren M, Stenvall M, Olofsson B, Gustafson Y. Evaluation of a fall-
prevention program in older people after femoral neck fracture: a one-
year follow-up. Osteoporosis International1919;801 -9.
Berkey CS, Rockett HR, Willett WC, Colditz GA. Milk, dairy fat,
dietary calcium, and weight gain: a longitudinal study of adolescents ..
Archives of Pediatrics & Adolescent Medicine 159 (6):543 -50, 2005.
Berube S, Diorio C, Masse B eta!. Vitamin D and calcium intakes from
food or supplements and mammographic breast density. Cancer
Epidemiology, Biomarkers & Prevention 14(7): 1653-9, 2005.
Bierenbaum ML, Fleischman AI, Raichelson RI. Long tenn human
studies on the lipid effects of oral calcium. Lipids 7 (3):202-6, 1972.
Bierenbaum ML, WolfE, Bisgeier G, Maginnis WP. Dietary calcium. A
method of lowering blood pressure. American Journal of Hypertension
1(3 Pt 3):149S -152S, 1988.
3
Reason
ln Ottawa EPC report
In Hofmeyer 2007 systematic review
In Hofrneyer 2007 systematic review
In systematic review
In Hofmeyer 2007 systematic review
Not RCT arrow 4 study
Not RCT arrow 4 study
No outcomes of interest
Review paper
I 00% patients with femoral neck
fracture who admitted to the hospital
Not RCT growth study
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No outcomes of interest
In systematic review
Excluded Study
Bischoff HA, Stahelin HB, Dick Wet al. Effects of Vitamin D and
calcium supplementation on falls: a randomized controlled trial.. Journal
of Bone & Mineral Research 18 (2):343-51, 2003.
Bischoff-Fenari HA, Conzelmann M, Stahelin HB et al. Is fall
prevention by Vitamin D mediated by a change in postural or dynamic
balance? Osteoporosis International 2006; 17(5):656-663.
Bischoff-FeJTari HA, Orav EJ, wson-Hughes B. Effect of cholecalciferol
plus calcium on falling in ambulatory older men and women: a 3-year
randomized controlled trial. Archives oflntemal Medicine 166 (4):424-
30, 2006.
Blum M, Kirsten M, Worth MH, Jr. Reversible hypertension. Caused by
the hypercalcemia of hyperparathyroidism, Vitamin D toxicity, and
calcium infusion. JAMA 237 (3):262 -3, 1977.
Boggess KA, Samuel L, Schmucker BC, Waters J, Easterling TR. A
randomized controlled trial of the effect of third-trimester calcium
supplementation on maternal hemodynamic function. Obstetrics &
Gynecology 90 (2):157-61, 1997.
Bonithon-Kopp C, Kronborg 0, Giacosa A, Rath U, Faivre J. Calcium
and fibre supplementation in prevention of colorect:al adenoma
recurrence: a randomised intervention trial. European Cancer Prevention
Organisation Study Group .. Lancet 356 (9238): 1300-6, 2000.
Bonithon-Kopp C, Piard F, Fenger C et al. Colorectal adenoma
characteristics as predictors of recurrence. Diseases of the Colon &
Rectum 47 (3):323-33, 2004.
Boon N, Koppes LL, Saris WH, Van MW. The relation between calcium
intake and body composition in a Dutch population: The Amsterdam
Growth and Health Longitudinal Study. American Journal of
Epidemiology 162 (1):27-32, 2005.
Bostick RM, Fosdick L, Grandits GA, Grambsch P, Gross M, Louis TA.
Effect of calcium supplementation on serum cholesterol and blood
pressure. A randomized, double-blind, placebo-controlled, clinical trial.
Archives of Family Medicine 9( I ):31-8 2000.
Bostick RM, Fosdick L, Wood JR et al. Calcium and colorectal
epithelial cell proliferation in sporadic adenoma patients: a randomized,
double-blinded, placebo-controlled clinical trial .. Journal of the National
Cancer Institute 87 (17): 1307-15, 1995.
Bostick RM, Potter JD, Fosdick Let al. Calcium and colorectal
epithelial cell proliferation: a preliminary randomized, double-blinded,
placebo-controlled clinical trial. Journal of the National Cancer Institute.
85(2): 132-41, 1993 Jan 20.
Boutron MC, Faivre J, Marteau P, Couillault C, Senesse P, Quipourt V.
Calcium, phosphorus, Vitamin D, dairy products and colorectal
carcinogenesis: a French case--control study .. British Joumal of Cancer
74 (1 ):145-51, 1996.
4
Reason
ln Ottawa EPC report
Secondary analysis of an original RCT
by Bischoff-Ferrari 2003, which is
already in Ottawa's repott
In Ottawa EPC report
No 25(0H)D or dietary Ca
In Hofmeyer 2007 systematic review
In Weigarten 2008 systematic review
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No outcomes of interest
>=20% subjects with diseases
No outcomes of interest
No outcomes of interest
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Excluded Study
Bowen J, Noakes M, Clifton PM. Effect of calcium and dairy foods in
high protein, energy-restricted diets on weight loss and metabolic
parameters in overweight adults. Intemational Journal of Obesity 29
(8):957-65, 2005.
Braverman AS. Evidence that high calcium and Vitamin D intake
decrease the risk of breast cancer in premenopausal women: implications
for breast cancer prevention and screening. Southern Medical Journal
100 (11):1061-2, 2007.
Brekke HK, Ludvigsson J. Vitamin D supplementation and diabetes-
related autoimmunity in the ABTS study. Pediatric Diabetes 2007;
8(1):1 1- 14.
Broe KE, Chen TC, Weinberg J, Bischoff-Ferrari HA, Holick MF, Kiel
DP. A higher dose of Vitamin d reduces the risk of falls in nursing home
residents: a randomized, multiple-dose study. Journal of the American
Geriatrics Society 2007; 55(2):234-239.
Brooke OG, Butters F, Wood C. Intrautetine Vitamin D nutrit.ion and
postnatal growth in Asian infants. British Medical Joumal Clinical
Research Ed 283 ( 6298): 1024, 1981.
Brooke OG. Supplementary Vitamin D in infancy and childhood.
Archives of Disease in Childhood 1983; 58(8):573-574.
Brunvand L, Quigstad E, Urdal P, HaugE. Vitamin D deficiency and
fetal growth. Early Human Development 45 (1-2):27-33, 1996.
Brunvand L, Shah SS, Bergstrom S, HaugE. Vitamin D deficiency in
pregnancy is not associated with obstructed labor. A study among
Pakistani women in Karachi. Acta Obstetricia et Gynecologica
Scandinavica 77 (3):303-6, 1998.
Campbell CG, Chew BP, Luedecke LO, Shultz TD. Yogurt consumption
does not enhance immune function in healthy premenopausal women.
Nutrition & Cancer 37 (1):27-35, 2000.
Cancela L, Le BN, Miravet L. Relationship between the Vitamin D
content of matemal milk and the Vitamin D status of nursing women and
breast-fed infants. Journal ofEndocrinology 110 ( 1):43-50, 1986.
Canto-Costa MH, Kunii I, Hauache OM. Body fat and cholecalciferol
supplementation in elderly homebound individuals. Brazilian Journal of
Medical & Biological Research 39 (I ):9 1-8, 2006.
Caplan RH, Miller CD, Si lva PD. Severe hypercalcemia in a lactating
woman in association with moderate calcium carbonate
supplementation: a case report. Journal of Reproductive Medicine 49
(3):214-7, 2004.
Cappuccio FP, Elliott P, Allender PS, Pryer J, Follman DA, Cutler JA.
Epidemiologic association between dietary calcium intake and blood
pressure: a meta-analysis of published data .. American Journal of
Epidemiology 142 (9):935-45, 1995.
Carlon GC, Howland WS, Goldiner PL, Kalm RC, Bertoni G, Tumbull
AD. Adverse effects of calcium administration. Report of two cases.
Archives of Surgery 113 (7):882-5, 1978.
5
Reason
ln systematic review
Review paper
No 25(0H)D or dietary Ca
In Ottawa EPC report
No 25(0H)D or dietary Ca
Review paper
Cross-sectional or retrospective
assessment of djet after djsease
diagnosis
No outcomes of interest
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Not RCT arrow 4 study
Not RCT anow 4 study
Case report
Meta-analysis
Case report
Excluded Study
Carlson LA, Derblom H, Lanner A. Effect of different doses of Vitamin
D on serum cholesterol and triglyceride levels in healthy men.
Atherosclerosis 12 (2):313-7, 1970.
Camso JB, Patel RM, Julka K, Parish DC. Health-behavior induced
disease: return of the. milk-alkali syndrome. Journal of General Internal
Medicine 2007; 22(7): I 053-1055.
Cats A, Kleibeuker JH, van der MR et al. Randomized, double-blinded,
placebo-controlled intervention study with supplemental calcium in
fami lies with hereditary nonpolyposis colorectal cancer. Journal of the
National Cancer Institute 87 (8):598-603, 1995.
Cervellin G, Bonino P, Palummeri E, Passeri M. Calcium phosphate and
blood pressure: their relationships in a geriatric population. American
Journal of Nephrology 6 Suppl 1: 16-8, 1986.
Chan GM, Roberts CC, Folland D, Jackson R. Growth and bone
mineralization of nonnal breast-fed infants and the effects of lactation on
maternal bone mineral status. Ametican Journal of Clinical Nutrition 36
(3):438-43, 1982.
Chan GM. Growth and bone mineral status of discharged very low birth
weight infants fed different formulas or human milk. Journal of
Pediatrics 123 (3):439-43, 1993.
Chan JM, Pietinen P, Virtanen Metal. Diet and prostate cancer risk in a
cohort of smokers, with a specific focus on calcium and phosphorus
(Finland). Cancer Causes & Control11(9):859-67, 2000.
Chen W, Dawsey SM, Qiao YL eta!. Prospective study of serum
25(0H)-Vitamin D concentration and risk of oesophageal and gastric
cancers. British Journal ofCancer2007; 97(1):123-128.
Chyou PH, Nomura AM, Stemmermann GN. Diet, alcohol, smoking and
cancer of the upper aerodigestive tract: a prospective study among
Hawaii Japanese men. International Journal of Cancer 60 (5):616-21,
1995.
Cleghorn GJ, Tudehope Dl. Neonatal intestinal obstruction associated
with oral calcium supplementation. Australian Paediatric Journal
17( 4):298-9, 1981.
Cockburn F, Belton NR, Purvis RJ et al. Maternal Vitamin D intake and
mineral metabolism in mothers and their newborn infants. British
Medical Joumal 281 (6232): 11 -4, 1980.
Cohen GR, Curet LB, Levine RJ et al. Ethnicity, nut1ition, and birth
outcomes in nulliparous women. American Journal of Obstetrics &
Gynecology 200 I; 185(3 ):660-667.
Colditz GA, Manson JE, Stampfer MJ. Rosner B, Willett WC, Speizer
FE. Diet and risk of clinical diabetes in women. American Journal of
Clinical Nutrition 55 (5):1018 -23, 1992.
Combs GF, Jr., Hassan N, Dellagana Net al. Apparent efficacy of food-
based calcium supplementation in preventing rickets in Bangladesh.
Biological Trace Element Research 121 (3):193 -204,2008.
6
Reason
Multiple antioxidant trials analyses
Case report
No outcomes of interest
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
In Ottawa EPC report
>=20% subjects with diseases
Superseded by Mitrou 2007
No outcomes of interest
No outcomes of interest
Case repo11
Not RCT anow 4 study
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No outcomes of interest
>=20% subjects with diseases
Excluded Study
Cong K, ChiS, Liu G. Calcium supplementation during pregnancy for
reducing pregnancy induced hypertension. Chinese Medical Journal l 08
(1):57-9, 1995.
Corless D, Dawson E, Fraser Fetal. Do Vitamin D supplements
improve the physical capabilities of elderly hospital patients? Age &
Ageing 14(2):76-84, 1985.
Cosman F, Nieves J, Shen V, Lindsay R. Oral 1 ,25-dihydroxyVitamin D
administration in osteoporotic women: effects of estrogen therapy.
Journal of Bone & Mineral Research 10(4):594-600, 1995.
Costenbader KH, Feskanich D, Holmes M, Karlson EW, ito-Garcia E.
Vitamin D intake and risks of systemic lupus erythematosus and
rheumatoid arthritis in women. Annals of the Rheumatic Diseases 67
(4):530-5, 2008.
Crowther CA, Hiller JE, P1idmore B et al. Calcium supplementation in
nulliparous women for the prevention of pregnancy-induced
hypertension, preeclampsia and preterm birth: an Australian randomized
trial. FRACOG and the ACT Study Group. Australian & New Zealand
Journal of Obstetrics & Gynaecology 39 (1): 12-8, 1999.
Dahifar H, Faraji A, Yassobi S, Ghorbani A. Asymptomatic rickets in
adolescent girls. Indian Journal of Pediatrics 2007; 74( 6):571-575.
Dattani JT, Exton-Smith AN, Stephen JM. Vitamin D status of the
elderly in relation to age and exposure to sunlight. Human Nutrition -
Clinical Nutrition 38 (2): 131-7, 1984.
Dauchet L, Kesse-Guyot E, Czernichow S et al. Dietary patterns and
blood pressure change over 5-y follow-up in the SU.VI.MAX cohort.
American Journal of Clinical Nutrition 2007; 85(6): 1650-1656.
Davie MW, Abraham RR, Hewins B, Wynn V. Changes in bone and
muscle constituents during dieting for obesity. Clinical Science 70
(3):285-93, 1986.
Davies KM, Heaney RP, Recker RR et al. Calcium intake and body
weight. Journal of Clinical Endocrinology & Metabolism 85 (12):4635-
8, 2000.
Deheeger M, Bell isle F, Rolland-Cachera MF. The French longitudinal
study of growth and nutrition: data in adolescent males and females.
Joumal of Human Nutrition & Dietetics 15 (6):429-38, 2002.
DeJongh ED, Binkley TL, Specker BL. Fat mass gain is lower in
calcium-supplemented than in unsupplemented preschool children with
low dietary calcium intakes. American Joumal of Clinical Nutrition 84
(5):1123-7, 2006.
Dent CE, Gupta MM. Plasma 25-hydroxyVitamin-D-levels during
pregnancy in Caucasians and in vegetarian and non-vegetmian Asians.
Lancet 2(7944): 1057-60, 1975.
DeSantiago S, Alonso L, Halhali A, Larrea F, lsoard F, Bourges H.
Negative calcium balance during lactation in rural Mexican women.
American Journal of Clinical Nutrition 76 (4):845-51, 2002.
7
Reason
ln Hofrneyer 2007 systematic review
In Ottawa EPC report
Not RCT arrow 4 study
Observational study estimated Vitamin
D supplement doses
In Hofmeyer 2007 systematic review
Not RCT arrow 4 study
Not RCT arrow 4 study
No 25(0H)D or dietary Ca
No outcomes of interest
Meta-analysis; five clinical studies
Analysis did not relate exposure to
outcome
<9y (a study on BMI)
No outcomes of interest
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Excluded Study
Devereux G, Litonjua AA, Turner SW eta!. Maternal Vitamin D intake
during pregnancy and early childhood wheezing. American Journal of
Clinical Nutrition 2007; 85(3):853-859.
Dewey KG, Lonnerdal B. Milk and nutrient intake of breast-fed infants
from 1 to 6 months: relation to growth and fatness. Journal of Pediatric
Gastroenterology & Nutrition 2(3):497 -506, 1983.
Dhesi JK, Bearne LM, Moniz C et a!. Neuromuscular and psychomotor
function in elderly subjects who fall and the relationship with Vitamin D
status. Journal of Bone & Mineral Research 17(5):891 -7, 2002.
Dhesi JK, Jackson SH, Bearne LM et al. Vitamin D supplementation
improves neuromuscular function in older people who fall. Age &
Ageing 33 (6):589-95, 2004.
Dijkslra SH, van BA, Janssen JW, de Vleeschouwer LH, Huysman WA,
van den Akker EL. High prevalence of Vitamin D deficiency in newborn
infants of high-risk mothers.[enatum appears in Arch Dis Child. 2007
Nov;92(11):1049]. Archives of Disease in Childhood 2007; 92(9):750-
753.
Dixon LB, Pellizzon MA, Jawad AF, Tershakovec AM. Calcium and
dairy intake and measures of obesity in hyper- and
normocholesterolemic children. Obesity Research 13(1 0): 1727-38, 2005.
Dobnig H, Pilz S, Schamagl H et al. Independent association of low
serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with
all-cause and cardiovascular mortality. Archives of Internal Medicine
168 (12 ):1340 -9 ' 2008.
Doege C, Bauer J. Effect of high volume intake of mother's milk with an
individualized supplementation of minerals and protein on early growth
of preterm infants <28 weeks of gestation. Clinical Nutrition 26 (5):581-
8, 2007.
Domrongkitchaipom S, Ongphiphadhanakul B, Stitchantrakul W et a!.
Risk of calcium oxalate nephrolithiasis after calcium or combined
calcium and calcitriol supplementation in postmenopausal women.
Osteoporosis International II (6):486-92, 2000.
Drinka PJ, Nolten WE. Hazards of treating osteoporosis and
hypertension concurrently with calcium, Vitamin D, and distal diuretics.
Joumal of the American Geriatrics Society 32 (5):405-7, 1984.
Drouillet P, Balkau B, Charles MA et at. Calcium consumption and
insulin resistance syndrome parameters. Data from the Epidemiological
Study on the Insulin Resistance Syndrome (DESIR). Nutrition
Metabolism & Cardiovascular Diseases 2007; 17(7):486-492.
Ehrenberg A. Non-medical prevention of pre-eclampsia. Acta
Obstetricia et Gynecologica Scandinavica- Supplement 164: I 08-IO,
1997.
Epstein S, Bell NH, Shary J, Shaw S, Greene A, Oexmann MJ. Evidence
that obesity does not influence the Vitamin D-endocrine system in
blacks. Journal ofBone & Mineral Research 1(2):181-4, 1986.
8
Reason
No 25(0H)D or dietary Ca
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Intramuscular injection of high dose
ergocalciferol
Relationship betweem mother's
25(0H)D and infant's 25(0H)D levels
Outcome is BW but participants age is
from 4 to lOy (mostly <9y)
>=20% subjects with diseases
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No outcomes of interest, no UL
outcomes
Case report
No outcomes of interest
Review paper
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Excluded Study
Epstein S, Stern PH, Bell NH, Dowdeswelll, Turner RT. Evidence for
abnormal regulation of circulating I alpha, 25-dihydroxyVitamin D in
patients with pulmonary tuberculosis and normal calcium metabolism.
Calcified Tissue International36 (5):541-4, 1984.
Ertbeg P, Norgaard P, Bang L, Nyholm H, Rudnicki M. Ionized
magnesium in gestational diabetes. Magnesium Research 17(1 ):35-8,
2004.
Faivre J, Couillault C, Kronborg 0 et al. Cbemoprevention of
metachronous adenomas of the large bowel: design and interim results of
a randomized trial of calcium and fibre. ECP Colon Group. European
Journal of Cancer Prevention 6(2):132-8, 1997.
Farrerons J, Barnadas M, Rodriguez Jet al. Clinically prescribed
sunscreen (sun protection factor 15) does not decrease serum Vitamin D
concentration sufficiently either to induce changes in parathyroid
function or in metabolic markers. British Journal of Dennatology 139
(3):422-7, 1998.
Faulkner KA, Cauley JA, Zmuda JM et al. Higher 1,25-
dihydroxyVitamin D3 concentrations associated with lower fall rates in
older community-dwelling women. Osteoporosis International 2006;
17(9): 1318-1328.
Feeley RM, Eitenmiller RR, Jones JB, Jr., Barnhart H. Calcium,
phosphorus, and magnesium contents of human milk during early
lactation. Journal of Pediatric Gastroenterology & Nutrition 2(2):262-7,
1983.
Felson DT, Niu J, Clancy Metal. Low levels of Vitamin D and
worsening of knee osteoarthritis: results of two longitudinal studies.
Arthritis & Rheumatism 2007; 56(1):129-136.
Fleischman AR, Rosen JF, Cole J, Smith CM, DeLuca HF. Maternal and
fetal serum 1,25-dihydroxyVitamin D levels at term. Journal of
Pediatrics 1980; 97( 4):640-642.
Fleischman AR, Rosen JF, Nathenson G. 25-hydroxyVitamin D. Serum
levels and oral administration of calcifediol in neonates. Archives of
Internal Medicine 138 Spec No: 869-73, 1978.
Forman JP, Bischoff-Ferrari HA, Willett WC, Stampfer MJ, Curhan GC.
Vitamin D intake and risk of incident hypertension: results from three
large prospective cohort studies. Hypertension 46 (4):676-82, 2005.
Franco A, Sikalidis AK, Solis Herruzo .TA. Colorectal cancer: influence
of diet and lifestyle factors. Revista Espanola de Enfennedades
Digestivas 97 (6):432-48, 2005.
Freedman DM, Tangrea JA, Virtamo J, Albanes D. The effect of beta-
carotene supplementation on serum Vitamin D metabolite
concentrations. Cancer Epidemiology, Biomarkers & Prevention 8
(12):1115-6, 1999.
Fronczak CM, Baron AE, Chase HP et al. In utero dietary exposures and
risk of islet autoimmunity in children. Diabetes Care 26 (12):3237 -42,
2003.
9
Reason
Not RCT arrow 4 study
No 25(0H)D or dietary Ca
Design and interim results article
No outcomes of interest
In Ottawa EPC report
No outcomes of interest
No outcomes of interest
No outcomes of interest
Premature infants
No 25(0H)D or dietary Ca
Review paper
No outcomes of interest
Observational study estimated Vitamin
D supplement doses
Excluded Study
Galloe AM, Graudal N, Moller J, Bro H, Jorgensen M, Christensen HR.
Effect of oral calcium supplementation on blood pressure in patients
with previously untreated hypertension: a randomised, double-blind,
placebo-controlled, crossover study. Journal of Human Hypertension 7
(I ):43-5, 1993.
Gambacciani M, Ciaponi M, Cappagli Bet al. Body weight, body fat
distribution, and hormonal replacement therapy in early postmenopausal
women.[ erratum appears in J Clin Endocrinol Metab 1997
Dec;82(12):4074]. Journal of Clinical Endocrinology & Metabolism 82
(2):414-7, 1997.
Garland CF, Garland FC. Do sunlight and Vitamin D reduce the
likelihood of colon cancer? [reprint in Int J Epidemiol. 2006
Apr;35(2):217-20; PMID: 16303809]. International Journal of
Epidemiology 9 (3):227-31, 1980.
Garland CF, Mohr SB, Gorham ED, Grant WB, Garland FC. Role of
ultraviolet B irradiance and Vitamin D in prevention of ovarian cancer.
American Journal ofPreventive Medicine 2006; 31(6):512-514.
Genkinger JM, Hunter DJ, Spiegelman D eta!. Dairy products and
ovarian cancer: a pooled analysis of 12 cohort studies. Cancer
Epidemiology, Biomarkers & Prevention 15 (2):364-72, 2006.
Gertner JM, Domenech M. 25-HydroxyVitamin D levels in patients
treated with high-dosage ergo- and cholecalciferol. Journal of Clinical
Pathology 30(2): 144-50, 1977.
Gillies DR, Hay A, Sheltawy MJ, Congdon PJ. Effect of phototherapy
on plasma 25(0H)-Yitamin Din neonates. Biology of the Neonate 1984;
45(5):225-227.
Gillman MW, Oliveria SA, Moore LL, Ellison RC.lnverse association
of dietary calcium with systolic blood pressure in young children. JAMA
267 (17):2340-3, 1992.
Gillman MW, Rifas-Shiman SL, Kleinman KP, Rich-Edwards JW,
Lipshultz SE. Maternal calcium intake and offspring blood pressure.
Circulation ll 0 ( 14): 1990-5, 2004.
Giovannucci E, Liu Y, Rimm EB et al. Prospective study of predictors
of Vitamin D status and cancer incidence and mortality in men .. Journal
of the National Cancer Institute 98 (7):451-9, 2006.
Giovannucci E, Rimm EB, Wolk A et al. Calcium and fructose intake in
relation to risk of prostate cancer. Cancer Research 58 (3):442-7, 1998.
Giovannucci E, Stampfer MJ, Colditz GA et al. MultiVitamin use,
folate, and colon cancer in women in the Nurses' Health Study .. Annals
oflnternal Medicine 129 (7):517 -24, 1998.
Gonzalez AJ, White E, Krista! A, Littman AJ. Calcium intake and I 0-
year weight change in middle-aged adults. Journal of the American
Dietetic Association 106 (7): 1066-73 2006.
10
Reason
ln systematic review
No outcomes of interest
Ecological study
No 25(0H)D or dietary Ca
Pooled analysis
>=20% subjects with diseases
Not RCT arrow 4 study
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Relationship behveen matemal intake
and offspring blood pressure
Superseded by Giovannucci 2007
Predictive model was used to predict
25(0H)D levels of whole cohort
No 25(0H)D or dietary Ca
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Excluded Study
Goswami R, Gupta N, Ray D, Singh N, TomarN. Pattern of25-hydroxy
vitamjn D response at short (2 month) and long (1 year) interval after 8
weeks of oral supplementation with chole.calciferol in Asian Indians
with chronic hypovitaminosis D. British Journal ofNutrition 100 (3):526
-9' 2008.
Grady D, Halloran B, Cummings Set at. I ,25-DihydroxyVitamin 03
and muscle strength in the elderly: a randomized controlled trial. Journal
of Clinical Endocrinology & Metabolism 73 (5): 1111 -7, 1991.
Grant WB. The likely role of Vitamin D from solar ultravi olet-B
irradiance in increasing cancer survival. Anticancer Research 26 (4A
):2605- 14, 2006.
Grau MV, Baron JA, Barry EL et al. Interaction of calcium
supplementation and nonsteroidal anti-inflammatory drugs and the risk
of colorectal adenomas. Cancer Epidemiology, Biomarkers &
Prevention 14(10):2353-8, 2005.
Greene MF. Trial of calcium to prevent preeclampsia. Journal of
Women's Health 6(4):485-6, 1997.
Greer FR, HoM, Dodson D, Tsang RC. Lack of25-hydroxyVitarnin D
and 1,25-dihydroxyVitamin Din human milk. Journal of Pediatrics 99
(2):233-5, 1981.
Greer FR, Hollis BW, Cripps DJ, Tsang RC. Effects of maternal
ultraviolet B irradiation on Vitamin D content of human milk. Journal of
Pediatrics 105 (3):431-3, 1984.
Greer FR, Marshall S. Bone mineral content, serum Vitamin D
metabolite concentrations, and ultraviolet B light exposure in infants fed
human milk with and without Vitamin D2 supplements. Journal of
Pediatrics 114 (2):204-12, 1989.
Greer FR, Searcy JE, Levin RS, Steichen JJ, Asch PS, Tsang RC. Bone
mineral content and serum 25-hydroxyVitamin D concentration in
breast-fed infants with and without supplemental Vita1nin D. Journal of
Pediatrics 98 (5):696-701, 1981.
Gmson M, Cancela L, Denne MA, Miravet L. Relationship between
bone GLA-protein (BGP) and calcidiol (25-hydroxycalciferol) in serum
of breast-fed infants. Endocrinologia Experimentalis. 20(2-3):329-34,
1986 Aug.
Gunther CW, Legowski PA, Lyle RM et al. Dairy products do not lead
to alterations in body weight or fat mass in young women in a 1-y
intervention. American Journal of Clinical Nutrition 81 (4):751 -6, 2005.
Gunther CW, Legowski PA, Lyle RM et al. Parathyroid hormone is
associated with decreased fat mass in young healthy women.
International Journal of Obesity 30 (1):94-9, 2006.
Haddad JG, Jr. , Rojanasathit S. Acute administration of25-
hydroxychol ecalciferol in man. Journal of Clinical Endocrinology &
Metabolism 42 (2):284 -90, 1976.
Hakala P, Karvetti RL. Weight reduction on lactovegetarian and mixed
diets. Changes in weight, nutrient intake, skinfold thicknesses and blood
pressure. European Journal of Clinical Nutrition 43 (6):421-30, 1989.
11
Reason
not RCT curve 4 study
I ,25(0H)2D supplement
Ecological study
In Weigarten 2008 systematic revi ew
Commentary
No 25(0H)D or dietary Ca
No 25(0H)D or dietary Ca
In Ottawa EPC report
In Ottawa EPC report
25(0H)D supplement
In systematic review
Ca intake and BW measured but not
assessed ==> no relevant results
reported
Not RCT arrow 4 study
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Excluded Study
Halhali A, Villa AR, Madrazo E eta!. Longitudinal changes in maternal
serum 1,25-dihydroxyVitamin D and insulin like growth factor I levels
in pregnant women who developed preeclampsia: comparison with
normotensive pregnant women. Journal of Steroid Biochemistry &
Molecular Biology 89 -90 ( 1-5):553-6, 2004.
Hamet P, Mongeau E, Lambert Jet al. Interactions among calcium,
sodium, and alcohol intake as determinants of blood pressure.
Hypertension 17(1 Suppl):JI50-4, 1991.
Hamid Z, Riggs A, Spencer T, Redman C, Bodenner D. Vitamin D
deficiency in residents of academic long-term care facilities despite
having been prescribed Vitamin D .. Journal of the American Medical
Directors Association 2007; 8(2):71-75.
Hansen KE, Jones AN, Lindstrom MJ, Davis LA, Engelke JA, Shafer
MM. Vitamin D insufficiency: disease or no disease? Journal of Bone &
Mineral Research 23(7): 1052-60, 2008.
Haub MD, Simons TR, Cook CM, Remig VM, Al-Tamimi EK,
Holcomb CA. Calcium-fortified beverage supplementation on body
composition in postmenopausal women. Nutrition Joumal4:21, 2005.
Heilbrun LK, Hankin JH, Nomura AM, Stemmermann GN. Colon
cancer and dietary fat, phosphorus, and calcium in Hawaiian-Japanese
men. American Journal of Clinical Nutrition 43 (2):306-9, 1986.
Heilbrun LK, Nomura A, Hankin JH, Stemmermann GN. Dietary
Vitamin D and calcium and risk of colorectal cancer. Lancet 1985;
1(8434):925.
Herrera JA, revalo-Herrera M, Herrera S. Prevention of preeclampsia by
linoleic acid and calcium supplementation: a randomized controlled trial.
Obstetrics & Gynecology 91 ( 4):585 -90, 1998.
Herrmann U, Schwille PO, Schmied! A, Fan J, Manoharan M. Acute
effects of calcium sodium citrate supplementation of a test meal on
mineral homeostasis, oxalate, and calcium oxalate crystallization in the
urine of healthy humans--preliminary results in patients with idiopathic
calcium urolithiasis. Biomedicine & Pharmacotherapy 53 (5-6):264-73,
1999.
Hill KM, Braun M, Kern Metal. Predictors of calcium retention in
adolescent boys. Journal of Clinical Endocrinology & Metabolism 93
(12 ):4743 -8 '2008.
Hiller JE, Crowther CA, Moore VA, Willson K, Robinson JS. Calcium
supplementation in pregnancy and its impact on blood pressure in
children and women: follow up of a randomised controlled trial.
Australian & New Zealand Journal of Obstetrics & Gynaecology 2007;
47(2):115-121.
Hillman LS, Haddad JG. Perinatal Vitamin D metabolism. II. Serial 25-
hydroxyVitamin D concentrations in sera oftem1 and premature infants.
Journal of Pediatrics 1975; 86(6):928-935.
12
Reason
No outcomes of interest
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Not RCT arrow 4 study
In systematic review
Letter to the editor
Superceded by Stemmermann, 1990
ReflD 1691
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No UL outcomes: CaOx crystallization;
saturation of CaOx
no outcomes of interest
No outcomes of interest
No clear Vitamin D dose for term
infants
Excluded Study
Hillman LS, Johnson LS, Lee DZ, Vieira NE, Yergey AL. Measurement
of true absorption, endogenous fecal excretion, urinary excretion, and
retention of calcium in term infants by using a dual-tracer, stable-isotope
method. Journal of Pediatrics 1993; 123(3):444-456.
Hintzpeter B, Mensiuk GB, Thierfelder W, Muller MJ, Scheidt-Nave C.
Vitamin D status and health correlates among German adults. European
Journal of Clinical Nutrition 62 (9 ): I 079 -89 , 2008.
Hofmeyr GJ, Mlokoti Z, Nikodem VC et al. Calcium supplementation
during pregnancy for preventing hypertensive disorders is not associated
with changes in platelet count, urate, and urinary protein: a randomized
control trial. Hypertension in Pregnancy 27 (3):299 -304, 2008.
Hofstad B, Almendingen K, Vatn Metal. Growth and recurrence of
colorectal polyps: a double-blind 3-year intervention with calcium and
antioxidants. Digestion 59 (2): 148-56, 1998.
Hofstad B, Vatn MH, Andersen SN, Owen RW, Larsen S, Osnes M. The
relationship between faecal bile acid profile with or without
supplementation with calcium and antioxidants on recurrence and
growth of colorectal polyps. European Joumal of Cancer Prevention 7
(4):287-94, 1998.
Hollis BW, Wagner CL. Vitamin D requirements during lactation: high-
dose maternal supplementation as therapy to prevent hypoVitaminosis D
for both the mother and the nursing infant. Am J Clin Nutr 2004; 80(6
Suppl): 1752S-1758S.
Hollis JH, Mattes RD. Effe.ct of increased dairy consumption on
appetitive ratings and food intake. [erratum appears in Obesity (Silver
Spring). 2007 Oct;15(10):2520]. Obesity 2007; 15(6):1520-1526.
Holt PR, Atillasoy EO, Gilman J et al. Modulation of abnormal colonic
epithelial cell proliferation and differentiation by low-fat dairy foods: a
randomized controlled trial.. JAMA 280 (12):1074-9, 1998.
Holt PR, Bresalier RS, Ma CK et al. Calcium plus Vitamin D alters
preneoplastic feah1res of colorectal adenomas and rectal mucosa. Cancer
I 06 (2):287 -96, 2006.
Holt PR, Wolper C, Moss SF, Yang K, Lipkin M. Comparison of
calcium supplementation or low-fat dairy foods on epithelial cell
proliferation and differentiation. Nutrition & Cancer 41 (1-2): 150-5,
2001.
Hunt CD, Johnson LK. Calcium requirements: new estimations for men
and women by cross-sectional statistical analyses of calcium balance
data from metabolic studies. American Jol1111al of Clinical Nutrition
2007; 86(4):1054-1063.
Hvarfner A, Ljunghall S, Morlin C, Wide L. Calcium metabolism and
arterial blood pressure in a healthy population sample and in
hypertensive men. American Journal of Nephrology 6 Suppl 1:14-5,
1986.
Hyman J, Baron JA, Dain BJ et al. Dietary and supplemental calcium
and the recurrence of colorectal adenomas. Cancer Epidemiology,
Biomarkers & Prevention 7 (4):291-5, 1998.
13
Reason
All neonates included weighed < 1500
gm
cross-sectional or retrospective
assessment of diet after disease
diagnosis
ancillary study (small sample) of WHO
trial. The preeclampsia data of WHO
trial was already included in the
previous SR (Hofmeyer2007).
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No independent Ca effect
In Ottawa EPC report
No outcomes of interest
No outcomes of interest
No outcomes of interest
No outcomes of interest
Arrow 4: calcium balance
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Multiple antioxidant trials analyses
Excluded Study
Hypponen E, Hartikainen AL, Sovio U, Jarvelin MR, Pouta A. Does
Vitamin D supplementation in infancy reduce the risk of pre-eclampsia?
European Journal of Clinical Nutrition 2007; 61(9): 1136-1139.
Hypponen E, Laara E, Reunanen A, Jarvelin MR, Virtanen SM. Intake
of Vitamin D and risk of type 1 diabetes: a bi.Jth-cohort shtdy .. Lancet
358 (9292):1500-3, 2001.
Hypponen E, Sovio U, Wjst Metal. Infant Vitamin d supplementation
and allergic conditions in adulthood: northern Finland birth cohott 1966.
Annals of the New York Academy of Sciences 1037:84-95, 2004.
Tlich-Ernst JZ, McKenna AA, Badenhop NE et al. Iron status, menarche,
and calcium supplementation in adolescent girls.[ erratum appears in Am
J Clin Nutr 1999 Mar;69(3):577]. American Journal of Clinical Nutrition
68 (4):880-7, 1998.
Ish-Shalom S, Segal E, Salganik T, Raz B, Bromberg IL, Vieth R.
Compatison of daily, weekly, and monthly vitamin 03 in ethanol dosing
protocols for two months in elderly hip fracture patients. Journal of
Clinical Endocrinology & Metabolism 93 (9 ):3430 -5, 2008.
Ito M, Koyama H, Ohshige A, Maeda T, Yoshimura T, Okamura H.
Prevention of preeclampsia with calcium supplementation and Vitamin
03 in an antenatal protocol. International Journal of Gynaecology &
Obstetrics47(2):115-20, 1994.
Jackson RD, Donepudi S, Mysiw WJ. Epidemiology of fracture risk in
the Women's Health Initiative. Current Osteoporosis Reports 6 (4): 155-
61 '2008.
Jackson RD, Lacroix AZ, Cauley JA, McGowan J. The Women's Health
Initiative calcium-Vitamin D trial: overview and baseline characteristics
of participants. Annals of Epidemiology 13(9 Suppl):S98-106, 2003.
Jackson RD, Lacroix AZ, Gass Met a!. Calcium plus Vitamin D
supplementation and the risk of fractures.[ erratum appears in N Engl J
Med. 2006 Mar 9;354(10): 1102]. New England Journal of Medicine 354
(7):669-83, 2006.
Jacobs D. Calcium and myocardial infarction. South African Medical
Journal Suid -Afrikaanse TydskrifVir Geneeskunde 48 (13):523-7,
1974.
Jacobs ET, Alberts DS, Benuzillo J, Hollis BW, Thompson PA,
Martinez ME. Serum 25(0H)D levels, dietary intake of Vitamin D, and
colorectal adenoma recurrence. Journal of Steroid Biochemistry &
Molecular Biology 2007; 1 03(3-5):752-756.
Jacques PF, Felson DT, Tucker KL et al. Plasma 25-hydroxyVitamin D
and its detenninants in an elderly population sample. American Journal
of Clinical Nutrition 66 (4):929-36, 1997.
Joffe GM, Esterlitz JR, Levine RJ et al. The relationship between
abnormal glucose tolerance and hypertensive disorders of pregnancy in
healthy nulliparous women. Calcium for Preeclampsia Preventjon
(CPEP) Study Group .. American Journal of Obstetrics & Gynecology
179 (4): 1032-7, 1998.
14
Reason
Observational study estimated Vitamin
D supplement doses
Observational shtdy estimated Vitamin
D supplement doses
Observational study estimated Vitamin
D supplement doses
Ca intake, BMI, LBM and BW
measured, but the analyses on the
relationship among these were not
performed.
arrow 4 RCT but daily doses were the
same in the comparison groups
(comparison of daily, weekly versus
monthly dose)
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
review paper
Overview of trial participants
Same as Wactawski-Wende 2006 ReflD
1967 in which longer f/up data reported
No 25(0H)D or dietary Ca
Analyses include 25(0H)D
measurements taken after outcome
( colorectal polyps) occurred.
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No 25(0H)D or dietary Ca
Excluded Study
John EM, Dreon DM, Koo J, Schwartz GG. Residential sunlight
exposure is associated with a decreased risk of prostate cancer. . Journal
of Steroid Biochemistry & Molecular Biology 89 -90 (1-5):549 -52,
2004.
John WG, Noonan K, Mannan N, Boucher BJ. HypoVitaminosis Dis
associated with reductions in semm apol ipoprotein A-I but not with
fasting lipids in British Bangladeshis. American Journal of Clinical
Nutrition 82 (3):517-22, 2005.
Johnson MA, Fischer JG, Park S. Vitamin D deficiency and
insufficiency in the Georgia Older Americans Nutrition Program.
Journal ofNutrition for the Elderly 27 (1-2):29 -46 , 2008.
Johnson NE, Smith EL, Freudenheim JL. Effects on blood pressure of
calcium supplementation of women. American Journal of Clinical
Nutrition 42 (1):12-7, 1985.
Jones G, Scott F. Low bone mass in premenopausal parous women:
identification and the effect of an information and bone density feedback
program .. Journal of Clinical Densitometry 2(2): 109-15, 1999.
Jorde R, Bonaa KH. Calcium from dairy products, Vitamin D intake,
and blood pressure: the Tromso Study .. American Journal of Clinical
Nutrition 71 (6): 1530-5, 2000.
Kampman E, Giovatmucci E, van', Vet a!. Calcium, Vitamin D, dairy
foods, and the occurrence of colorectal adenomas among men and
women in two prospective studies. Am J Epidemio11994; 139(1):16-29.
Karanja N, Morris CD, Illingworth DR, McCarron DA. Plasma lipids
and hypertension: response to calcium supplementation. American
Journal of Clinical Nutrition 45 (1):60-5, 1987.
Karanja N, Morris CD, Rufolo P, Snyder G, Illingworth DR, McCarron
DA. Impact of increasing calcium in the diet on nutrient consumption,
plasma lipids, and lipoproteins in humans .. American Journal of
Clinical Nutrition 59 (4):900-7, 1994.
Kawano Y. Role of blood pressure monitoring in non-pharmacological
management of hypertension. Blood Pressure Monitoring 7 (1):51 -4,
2002.
Kearney J, Giovannucci E, Rimm EB eta!. Calcium, Vitamin D, and
dairy foods and the occurrence of colon cancer in men. American
Journal ofEpidemiology 143 (9):907-17, 1996.
Kemi VE, Karkkainen MU, Karp HJ, Laitinen KA, Lamberg-Allardt CJ.
Increased calcium intake does not completely counteract the effects of
increased phosphorus intake on bone: an acute dose-response study in
healthy females. British Journal ofNutiition 99 (4):832-9, 2008.
Kenny AM, Bellantonio S, Gruman CA, Acosta RD, Prestwood KM.
Effects of transdermal testosterone on cognitive function and health
perception in older men with low bioavailable testosterone levels.
Journals of Gerontology Series A-Biological Sciences & Medical
Sciences 57 (5):M321-5, 2002.
15
Reason
No 25(0H)D or dietary Ca
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
combination of vit D/Ca and other
treatment w/o analysis of independent
effect
In systematic review
No outcomes of interest
No outcomes of interest
Same cohorts as Wu 2002 ReflD 529
(HPFS & NHS) and same exposure-
outcome relationship but shorter follow-
up
No outcomes of interest
No outcomes of interest
Review paper
Longer followup data were published in
Wu 2002
No outcomes of interest
No 25(0H)D or dietary Ca
Excluded Study
Kenny AM, Biskup B, Robbins B, Marcella G, Burleson JA. Effects of
Vitamin D supplementation on strength, physical function, and health
perception in older, community-dwelling men. Journal of the American
Geriatrics Society 51 (12):1762-7, 2003.
Kesteloot H, Geboers J. Calcium and blood pressure. Lancet
1 (8276):813 -5, 1982.
Khaw KT, Barrett-Connor E. Dietary potassium and stroke-associated
mortality. A 12-year prospective population study. New England Journal
ofMedicine 316 (5):235-40, 1987.
Kigutha HN, van Staveren W A, Wijnhoven TM, Hautvast JG. Maternal
nutritional status may be stressed by seasonal fluctuations in food
availability: evidence from rural women in Kenya. International Journal
of Food Sciences & Nutrition 46 (3):247-55, 1995.
Knekt P, Laaksonen M, Mattila C et al. Serum Vitamin D and
subsequent occunence of type 2 diabetes. Epidemiology. 19( 5) :666-71,
2008 Sep.
Knight KB, Keith RE. Calcium supplementation on normotensive and
hypertensive pregnant women. American Journal of Clinical Nutrition
55 (4):891-5, 1992.
Knox EG. lschaemic-heart-disease mortality and dietary intake of
calcium. Lancet 1(7818):1465-7, 1973.
Kobayashi E, Okubo Y, Suwazono Yet al. Association between urinary
calcium excretion level and mortality in inhabitants of the Jinzu River
basin area of Japan. Biological Trace Element Research 89(2):145-53,
2002.
Koh-Banerjee PK, Ferreira MP, Greenwood Metal. Effects of calcium
pyruvate supplementation during training on body composition, exercise
capacity, and metabolic responses to exercise. Nutrition 21(3):312-9,
2005.
Kokot F, Pietrek J, Srokowska Setal. 25-hydroxyVitamin Din patients
with essential hypertension. Clinical Nephrology 16 (4):188-92, 1981.
Koralek DO, Bertone-Johnson ER, Leitzmann MF et al. Relationship
between calcium, lactose, Vitamin D, and dairy products and ovarian
cancer. Nutrition & Cancer 2006; 56(1 ):22-30.
Krista! AR, Chi C, Tangen CM, Goodman PJ, Etzioni R, Thompson JM.
Associations of demographic and lifestyle characteristics with prostate-
specific antigen (PSA) concentration and rate ofPSA increase. Cancer
I 06 (2):320-8, 2006.
Kromhout D, Bosschieter EB, Coulander CD. Potassium, calcium,
alcohol intake and blood pressure: the Zutphen Study. American Journal
ofClinical Nutrition 41 (6):1299-304, 1985.
Kulier R, de OM, Gulmezoglu AM, Villar J. Nutritional interventions
for the prevention of maternal morbidity. International Journal of
Gynaecology & Obstetrics 63 (3):231-46, 1998.
16
Reason
ln Ottawa EPC report
No 25(0H)D or dietary Ca
Continuous Ca intake analysis only
Ca intake, BMJ and BW measured, but
analysis did not relate Ca intake to
BMI/BW.
No outcomes of interest
No outcomes of interest
Analysis @ region level, not individual
level
No 25(0H)D or dietary Ca
No 25(0H)D or dietary Ca
On drug Rx for hypertension
No outcomes of interest
No outcomes of interest
No outcomes of interest
SR of prevention of maternal morbidity
Excluded Study
Kumar R, Cohen WR, Silva P, Epstein FH. Elevated 1,25-
dihydroxyVitamin D plasma levels in normal hwnan pregnancy and
lactation. Journal of Clinical Investigation 63 (2):342-4, 1979.
Kuroda T, Shi.raki M, Tanaka S, Ohta H. Contributions of25-
hydroxyvitami.n D, co-morbidities and bone mass to mortality in
Japanese postmenopausal women. Bone 44 (1):168 -72,2009.
Kynast-Gales SA, Massey LK. Effects of dietary calcium from dairy
products on ambulatory blood pressure in hypertensive men .. Journal of
the American Dietetic Association 92 (12):1497-501 , 1992.
Laaksi I, Ruohola JP, Tuohimaa Petal. An association of serum
Vitamin D concentrations < 40 nmol/L with acute respiratory tract
infection in young Finnish men. American Journal of Clinical Nutrition
86 (3):714-7, 2007.
Lakdawala DR, Widdowson EM. Vitamin-D in human milk. Lancet
1(8004):167-8, 1977.
Lamberg-Allardt C, Larjosto M, Schultz E. 25-HydroxyVitamin D
concentrations in maternal and cord blood at delivery and in maternal
blood during lactation in Finland. Human Nutrition - Clinical Nutrition
38 (4):261-8, 1984.
Lancia B, Tedesco M, Sergio G, Tenna M. Anthropometric and
nutritional assessment in Italian elderly subjects. Journal of Nutrition,
Health&Aging 1(3):174-80, 1997.
Lappe JM, Davies KM, Travers-Gustafson D, Heaney RP. Vitamin D
status in a rural postmenopausal female population. Journal of the
American College of Nutrition 2006; 25(5):395-402.
Laraia BA, Bodnar LM, Siega-Riz AM. Pregravid body mass index is
negatively associated with diet quality during pregnancy. Public Health
Nutrition 2007; I 0(9):920-926.
Lasco A, Gaudio A, Morini E eta!. Effect of long-term treatment with
raloxifene on mammary density in postmenopausal women. Menopause
2006; 13(5):787-792.
Latham NK, Anderson CS, Lee A et al. A randomized, controlled trial of
quadriceps resistance exercise and Vitamin D in frail older people: the
Frailty Interventions Trial in Elderly Subjects (FITNESS) . . Journal of
the American Geriatrics Society 51 (3):291 -9, 2003.
Le BN, Cancela L, Miravet L. Calcidiol in human milk. The effect of
prohormone on Vitamin D status of breast fed unsupplemented infants.
Endocrinologia Experimentalis. 20(2-3):325-8, 1986.
Lee DC, Lee GY. The use of pamidronate for hypercalcemia secondary
to acute Vitamin D intoxication. Journal ofToxicology- Clinical
Toxicology 36 (7):719-21, 1998.
Lee WT, Leung SS, Wang SH et al. Double-blind, controlled calcium
supplementation and bone mineral accretion in children accustomed to a
low-calcium diet.. American Journal of Clinical Nutrition 60 (5):744-
50, 1994.
17
Reason
No outcomes of interest
>=20% subjects with diseases
In systematic review
No outcomes of interest
No outcomes of interest
Not RCT arrow 4 study
Cross-sectional or retrospective
assessment of djet after djsease
djagnosis
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
In Ottawa EPC report
Correlation b/tw breastrnilk 25(0H)D
with infant's serum 25(0H)D
Case report
In Winzenberg 2007 systematic review,
no outcomes of interest
Excluded Study
Levine AJ, Harper JM, Ervin CM et al. Serum 25-hydroxyVitamin D,
dietary calcium intake, and distal colorectal adenoma risk. Nutrition &
Cancer 2001; 39(1):35-41.
Levine RJ, Esterlitz JR, Raymond EG et al. Trial of Calcium for
Preeclampsia Prevention (CPEP): rationale, design, and methods.
Controlled Clinical Trials 17(5):442-69, 1996.
Levine RJ, Hauth JC, Curet LB et al. Trial of calcium to prevent
preeclampsia .. New England Journal ofMedicine 337 (2):69-76, 1997.
Lewandowski S, Rodgers AL. Renal response to lithogenic and anti -
lithogenic supplement challenges in a stone-free population group.
Journal ofRenal Nutrition 14(3):170-9, 2004.
Liebman M, Chopin LF, Carter E et al. Factors related to blood pressure
in a biracial adolescent female population. Hypertension 8(1 0):843-50,
1986.
Lin PH, Appel LJ, Funk Ketal. The PREMIER intervention helps
participants follow the Dietary Approaches to Stop Hypertension dietary
pattern and the current Dietary Reference Intakes recommendations.
Journal of the American Dietetic Association 2007; 107(9): 1541-1551.
Lin YC, Lyle RM, McCabe LD, McCabe GP, Weaver CM, Teegarden
D. Dairy calcium is related to changes in body composition during a
two-year exercise intervention in young women. Journal of the
American College ofNuttition. 19(6):754-60, 2000 Nov-Dec.
Lind L, Lithell H, Skarfors E, Wide L, Ljunghall S. Reduction of blood
pressure by treatment with alphacalcidol. A double-blind, placebo-
controlled study in subjects with impaired glucose tolerance. Acta
Medica Scandinavica 223 (3):211-7, 1988.
Lipkin M, Friedman E, Winawer SJ, Newmark H. Colonic epithelial cell
proliferation in responders and nonresponders to supplemental dietary
calcium. Cancer Research 49 (1):248 -54, 1989.
Lipkin M, Newmark H. Effect of added dietary calcium on colonic
epithelial-cell proliferation in subjects at high risk for familial colonic
cancer. New England Journal of Medicine 313 (22):1381-4, 1985.
Liu LS. Epidemiology of hypertension and cardiovascular disease--
China experience. Clinical & Experimental Hypertension - Part A,
Theory & Practice 12 (5):831 -44, 1990.
Reason
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Methods for trial
In Hofmeyer 2007 systematic review
No UL outcomes: saturation of CaOx
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No outcomes of interest
>=20% subjects with diseases
>=20% subjects with diseases
No outcomes of interest
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Liu S, Choi HK, Ford E et al. A prospective study of dairy intake and the No 25(0H)D or dietary Ca
risk of type 2 diabetes in women. Diabetes Care 29 (7): 1579-84, 2006.
Ljunghall S, Lind L, Lithell H et al. Treatment with one-alpha-
hydroxycholecalciferol in middle-aged men with impaired glucose
tolerance--a prospective randomized double-blind study. Acta Medica
Scandinavica222 (4) :361-7, 1987.
Lanzer MD, hruie R, Rogers D, Worley D, Licata A, Secic M. Effects of
heredity, age, weight, puberty, actiVitaminy, and calcium intake on bone
mineral density in children. Clinical Pediatrics 35 (4):185-9, 1996.
18
>=20% subjects with diseases
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Excluded Study
Lopez-Jaramillo P, Delgado F, Jacome P, Teran E, Ruano C, Rivera J.
Calcium supplementation and the risk of preeclampsia in Ecuadorian
pregnant teenagers. Obstetrics & Gynecology 90 (2): 162-7, 1997.
Lopez-Jararnillo P, Narvaez M, Weigel RM, Yepez R. Calcium
supplementation reduces the risk of pregnancy-induced hypertension in
an Andes population. British Journal of Obstetrics & Gynaecology 96
(6):648 -55, 1989.
Luft FC, AronoffGR, Sloan RS, Fineberg NS, Weinberger MH. Short-
tenn augmented calcium intake has no effect on sodium homeostasis.
Clinical Pharmacology & Tilerapeutics 39 ( 4):414-9, 1986.
Lutter CK, Rodriguez A, Fuenmayor G, Avila L, Sempertegui F,
Escobar J. Growth and micronutrient status in children receiving a
fortified complementary food. Journal ofNutrition 138 (2):379-88,
2008.
Lyle RM. Does baseline serum total calcium level int1uence the blood
pressure response to calcium supplementation? A double-blind study.
Netherlands Journal of Medicine 41 (1 -2):48-55, 1992.
Lynch MF, Griffin IJ, Hawthorne KM, Chen Z, Hamzo M, Abrams SA.
Calcium balance in 1-4-y-old children. American Journal of Clinical
Nutrition 2007; 85(3):750-754.
Ma J, Stampfer MJ, Gann PH et al. Vitamin D receptor polymorphisms,
circulating Vitamin D metabolites, and risk of prostate cancer in United
States physicians. Cancer Epidemiology, Biomarkers & Prevention 7
(5):385-90, 1998.
Macdonald HM, New SA, Campbell MK, Reid DM. Longitudinal
changes in weight in perimenopausal and early postmenopausal women:
effects of dietary energy intake, energy expenditure, dietary calcium
intake and hormone replacement therapy. International Journal of
Obesity & Related Metabolic Disorders: Journal of the International
Association for the Study of Obesity 27 (6):669-76, 2003.
Madore F, Stampfer MJ, Rirnm EB, Cmhan GC. Nephrolithiasis and risk
ofhypertension. American Journal ofHypertension 11(1 Pt 1):46-53,
1998.
Mali1a N, Virtanen M, Pietinen Petal. A comparison of prospective and
retrospective assessments of diet in a study of colorectal cancer.
Nutrition & Cancer 32 (3):146 -53, 1998.
Mandic-Puljek M, Mandie ML, Perl A, Kenjeric D. Calcium intake,
food sources and seasonal variations in eastern Croatia. Collegium
Antropologicum 29 (2):503-7, 2005.
Manios Y, Moschonis G, Grammatikaki E, Katsaroli I, Kanelou P,
Tanagra S. Nutrition education in postmenopausal women: changes in
dietary and cardiovascular indices. Maturitas 2006; 55(4):338-347.
Marangella M, Vitamina1e C, Petrarulo M, Rovera L, Dutto F. Effects of
mineral composition of drinking water on tisk for stone formation and
bone metabolism in idiopathic calcium nephrolithiasis. Clinical Science
91 (3):313-8, 1996.
19
Reason
ln Hofrneyer 2007 systematic review
In Hofrneyer 2007 systematic review
No outcomes of interest
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
In systematic review
Arrow 4: calcium balance
Main results had been previous
published (Gann 1996, RefiD 3783), and
no additional usable data
No outcomes of interest
No outcomes of interest
Superseded by Pietinen 1999
No outcomes of interest
Nutrition education intervention study
No UL outcomes: saturation of CaOx
Excluded Study
Markestad T, Kolmannskog S, Arntzen E, Toftegaard L, Haneberg B,
Aksnes L. Serum concentrations of Vitamin D metabolites in exclusively
breast-fed infants at 70 degrees north. Acta Paediatrica Scandinavica 73
(1):29-32, 1984.
Markestad T. Effect of season and Vitamin D supplementation on
plasma concentrations of25-hydroxyVitamin Din Norwegian infants.
Acta Paediatrica Scandinavica 72 (6):817-21, 1983.
Markestad T. Plasma concentrations of Vitamin D metabolites in
unsupplemented breast-fed infants. European Journal of Pediatrics 141
(2):77-80, 1983.
Marniemi J, Jarvisalo J, Toikka T, Raiha T, Ahotupa M, Sourander L.
Blood Vitamins, mineral elements and inflammation markers as risk
factors of vascular and non-vascular disease mortality in an elderly
population. International Journal of Epidemiology 27 (5):799-807, 1998.
Martinez ME, Giovannucci EL, Colditz GA et al. Calcium, Vitamin D,
and the occunence of colo rectal cancer among women. Journal of the
National Cancer Institute 88 (19):1375-82, 1996.
Marx SJ, Swart EG, Jr., Hamstra AJ, DeLuca HF. Nonnal intraute1ine
development of the fetus of a woman receiving extraordinarily high
doses of 1,25-dihydroxyVitamin D3. Journal of Clinical Endocrinology
& Metabolism 51 (5):1138 -42, 1980.
Masse PG, Tranchant CC, Jougleux JL, Coburn SP, Cole DE.
Cardiovascular disease-risk factors in middle-aged osteopaenic women
treated with calcium alone or combined to three nutrients essential to
artery and bone collagen. Journal of Human Nutrition & Dietetics
21 (2): 117-28, 2008.
Matheson NA. Letter: Multiple sclerosis and diet. Lancet 2 (7884 ):831,
1974.
Matsumoto T, Kubodera N. ED-71, a new active Vitamin D3, increases
bone mineral density regardless of serum 25(0H)D levels in
osteoporotic subjects. Journal of Steroid Biochemistry & Molecular
Biology 2007; I 03(3-5):584-586.
Mawer EB, Berry JL, Sommer-Tsilenis E, Beykirch W, Kuhlwein A,
Rohde BT. Ultraviolet iJTadiation increases serum 1,25-
dihydroxyVitamin Din Vitamin-D-replete adults. Mineral & Electrolyte
Metabolism 10(2):117-21, 1984.
Mazess RB, Peppler WW, Chesnut CH, ITT, Nelp WB, Cohn SH, Zanzi
T. Total body bone mineral and lean body mass by dual-photon
absorptiometry. II. Comparison with total body calcium by neutron
activation analysis. Calcified Tissue International33 (4):361-3, 1981.
Mazess RB, Peppler WW, Harrison JE, McNeill KG. Total body bone
mineral and lean body mass by dual-photon absorptiometry. Ill.
Comparison with trunk calcium by neutron activation analysis. Calcified
Tissue International 33 (4):365-8, 1981.
20
Reason
No relation with 25(0H)D to growth
outcome
Not RCT arrow 4 study
No outcomes of interest
No 25(0H)D or dietary Ca
Longer followup data were published in
Wu2002
Case report
No outcomes of interest
Letter to the editor
Vitamin D analog
Not RCT arrow 4 study
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No 25(0H)D or dietary Ca
Excluded Study
McCarron DA, Morris CD. Blood pressure response to oral calcium in
persons with mild to moderate hypettension. A randomized, double-
blind, placebo-controlled, crossover trial. Annals of Internal Medicine
103 (6 (Pt 1)):825 -31, 1985.
Merlino LA, Curtis J, Mikuls TR et al. Vitamin D intake is inversely
associated with rheumatoid arthritis: results from the Iowa Women's
Health Study .. Arthritis & Rheumatism 50(1 ):72-7, 2004.
Methy N, Binquet C, Boutron-Ruault MC, Paillot B, Faivre J, Bonithon-
Kopp C. Dietary fatty acids and recurrence of colorectal adenomas in a
European intervention trial. Nutrition & Cancer 60 (5):560 -7,2008.
Michaud DS, Spiegelman D, Clinton SK, Rimm EB, Willett WC,
Giovannucci E. Prospective study of dietary supplements,
macronutrients, micronutrients, and risk of bladder cancer in US men.
American Journal of Epidemiology 152 ( 12): 1145-53, 2000.
Misselwitz J, Hesse V, Markestad T. Nephrocalcinosis, hypercalciuria
and elevated serum levels of 1,25-dihydroxyVitamin D in children.
Possible link to Vitamin D toxicity. Acta Paediatrica Scandinavica 79
(6-7):637-43, 1990.
Moerman CJ, Smeets FW, Kromhout D. Dietary risk factors for
clinically diagnosed gallstones in middle-aged men. A 25-year follow-up
study (the Zutphen Study). Annals of Epidemiology 4(3):248-54, 1994.
Mohr SB, Garland CF, Gorham ED, Garland FC. The association
between ultraviolet B irradiance, vitamin D status and incidence rates of
type 1 diabetes in 51 regions worldwide. Diabetologia 51 (8 ):1391-8,
2008.
Moller VK, Ramlau-Hansen CH, Rejnmark L, Heickendorff L,
Henriksen TB, Mosekilde L. Postpartum Vitamin D insufficiency and
secondary hyperparathyroidism in healthy Danish women. European
Journal of Clinical Nutrition 2006; 60(10):1214-1221.
Morley R, Carlin JB, Dwyer T. Maternal calcium supplementation and
cardiovascular risk factors in twin offspring .. International Journal of
Epidemiology 33 (6): 1304-9, 2004.
Morosetti M, Jankovic L, Palombo G et al. High-dose calcitriol therapy
and progression of cardiac vascular calcifications. Journal of
Nephrology 21(4):603 -8 , 2008;-Aug.
Morris CD, McCarron DA. Effect of calcium supplementation in an
older population with mildly increased blood pressure. American Journal
ofHypertension 5(4 Pt 1):230-7, 1992.
Munger KL, Levin LT, Hollis BW, Howard NS, Ascherio A. Serum 25-
hydroxyVitamin D levels and risk of multiple sclerosis. JAMA.
296(23):2832-8, 2006 Dec 20.
Muray S, Marco MP, Craver L, Rue M, Valdivielso JM, Fernandez E.
Influence of mineral metabolism parameters on pulse pressure in healthy
subjects .. Clinical Nephrology 2006; 66(6):411-417.
21
Reason
ln systematic review
Observational study estimated Vitamin
D supplement doses
no 25(0H)D or dietary Ca
No outcomes of interest
Case report
No outcomes of interest
ecological study
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No 25(0H)D or dietary Ca
i.v. calcitriol
No outcomes of interest
No outcomes of interest
No 25(0H)D or dietary Ca
Excluded Study
Nakamura K, Nishiwaki T, Ueno K, Yamamoto M. Age-related decrease
in serum 25-hydroxyVitamin D concentrations in the frail elderly: a
longitudinal study. Journal of Bone & Mineral Metabolism 2007;
25( 4):232-236.
Nakamura R, Saruta T. Effect of calcium supplementation on blood
pressure in essential hypertensive subjects. Japanese Journal of Medicine
26 (2):203-6, 1987.
Nako Y, Fukushima N, Tomomasa T, Nagashima K, Kuroume T.
HyperVitaminosis D after prolonged feeding with a premature formula.
Pediatrics 1993; 92(6):862-864.
Narang NK, Gupta RC, Jain MK. Role of Vitamin D in pulmonary
tuberculosis. Joumal of the Association of Physicians of India 32
(2):185-8,1984.
Nayir A, Kadioglu A, Sirin A, Entre S, Tongue E, Bilge I. Causes of
increased renal medullary echogenicity in Turkish children. Pediatric
Nephrology 9 (6):729 -33, 1995.
Need AG, O'Loughlin PD, Horowitz M, Nordin BE. Relationship
between fasting serum glucose, age, body mass index and serum 25
hydroxyVitamin D in postmenopausal women. Clinical Endocrinology
62 (6):738-41, 2005.
Nieves JW, Barrett-Connor E, Siris ES, Zion M, Barlas S, Chen YT.
Calcium and vitamin D intake influence bone mass, but not short-tenn
fracture risk, in Caucasian postmenopausal women from the National
Osteoporosis Risk Assessment (NORA) study. Osteoporosis
lnternationall919;673-9.
Nilas L, Christiansen C. Treatment with Vitamin D or its analogues does
not change body weight or blood glucose level in postmenopausal
women.lntemational Joumal ofObesity 8(5):407-11, 1984.
Niromanesh S, Laghaii S, Mosavi-Jarrahi A. Supplementary calcium in
prevention of pre-eclampsia. International Journal of Gynaecology &
Obstetrics 74 (1):17-21, 2001.
Nishimura K, Shima M, Tsugawa N et al. Long-term hospitalization
during pregnancy is a risk factor for Vitamin D deficiency in
neonates.[erratum appears in J Bone Miner Metab. 2003;21 (4):253].
Joumal of Bone & Mineral Metabolism 21 (2): I 03-8, 2003.
Nishiyama T. Effects of calcium on muscular training . .Toumal of
Nutritional Science & Vitaminology 31 Suppl: S45-7, 1985.
Nowak A, Pachocka L, Targosz U, Klosiewicz-Latoszek L. Dietary
calcium and obesity in men. Roczniki Panstwowego Zakladu Higieny 58
(1):301-5, 2007.
Nowson C, Morgan T. Effect of calcium carbonate on blood pressure in
normotensive and hypertensive people. Hypertension 13(6 Pt 1):630-9,
1989.
Obarzanek E, Hunsberger SA, Van HL et al. Safety of a fat-reduced diet:
the Dietary Intervention Study in Children (DISC). Pediatrics 100
(1):51-9, 1997.
22
Reason
Effect of aging on 25(0H) D
No outcomes of interest
Case report
No outcomes of interest
Case report
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
not RCT bone study (postmenepausal
women)
Review paper
In Hofmeyer 2007 systematic review
No outcomes of interest
Calcium only and bone/muscle
outcomes
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
In systematic review
No outcomes of interest
Excluded Study
Ochner CN, Lowe MR. Self-reported changes in dietary calcium and
energy intake predict weight regain following a weight loss diet in obese
women. Journal ofNutrition 2007; 137(10):2324-2328.
Olafsdottir AS, Wagner KH, Thorsdotti.r I, Elmadfa I. Fat-soluble
Vitamins in the matemal diet, influence of cod liver oil supplementation
and impact of the maternal diet on human milk composition. Annals of
Nutrition & Metabolism 45 ( 6):265-72, 200 I.
Paganus A, Juntunen-Backman K, Savilahti E. Follow-up of nutritional
stahts and dietary survey in children with cow's milk allergy. Acta
Paediatrica 81 (6-7 ):518 -21 , 1992.
Palacios C, Benedetti P, Fonseca S. Impact of calcium intake on body
mass index in Venezuelan adolescents. Puerto Rico Health Sciences
Journal 26 (3): 199-204, 2007.
Park SB, Suh DH, Youn JI. A pilot study to assess the safety and
efficacy of topical calcipotriol treatment in childhood psoriasis. Pediatric
Dern1atology 16 (4):321-5, 1999.
Pasch A, Frey FJ, Eisenberger U, Mohaupt MG, Bonny 0. PTH and 1.25
vitamin D response to a low-calcium diet is associated with bone
mineral density in renal stone fmmers. Nephrology Dialysis
Transplantation 23(8 ):2563 -70 , 2008.
Pehlivan I, Hatun S, Aydogan M, Babaoglu K, Gokalp AS. Maternal
Vitamin D deficiency and Vitamin D supplementation in healthy infants.
Turkish Journal of Pediatrics 45 (4):315-20, 2003;-Dec.
Peters U, Hayes RB, Chatterjee Net al. Circulating Vitamin D
metabolites, polymorphism in Vitamin D receptor, and colorecta1
adenoma risk. Cancer Epidemiology, Biomarkers & Prevention 2004;
13(4):546-552.
Peters U, McGlynn KA, Chatterjee Net al. Vitamin D, calcium, and
Vitamin D receptor polymorphism in colorectal adenomas. Cancer
Epidemiology, Biomarkers & Prevention 2001; 10(12):1267-1274.
Pettifor JM, Bikle DD, Cavaleros M, Zachen D, Kamdar MC, Ross FP.
Serum levels of free 1,25-dihydroxyVitamin Din Vitamin D toxicity.
Annals oflnternal Medicine 122 (7):5 11-3, 1995.
Phillips SM, Bandini LG, Cyr H, Colclough-DouglasS, Naumova E,
Must A. Dairy food consumption and body weight and fatness studied
longitudinally over the adolescent period .. International Journal of
Obesity & Related Metabolic Disorders: Journal of the International
Association for the Study of Obesity 27 (9): II 06-1 3, 2003.
Pilz S, Dobnig H, Fischer JE et at. Low Vitamin d levels predict stroke
in patients referred to coronary angiography. Stroke 39 (9):2611-3, 2008.
Pilz S, Dobnig H, Winklhofer-Roob B et al. Low serum levels of25-
hydroxyVitamin D predict fatal cancer in patients referred to coronary
angiography. Cancer Epidemiology, Biomarkers & Prevention
17(5): 1228-33, 2008.
Pittard WB, III, Geddes KM, Hulsey TC, Hollis BW. How much
Vitamin D for neonates? American Journal of Diseases ofChi1dren 145
(10):1147-9, 1991.
23
Reason
No outcomes of interest
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
>=20% subjects with diseases
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No 25(0H)D or dietary Ca
no outcomes of interest
Cross-sectional or retrospective
assessment of djet after djsease
diagnosis
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Case repo11
Not RCT growth study
>=20% subjects with diseases
>=20% subjects with diseases
Not RCT arrow 4 study
Excluded Study
Pittard WB, l11, Geddes KM, Sutherland SE, Miller MC, Hollis BW.
Longitudinal changes in the bone mineral content of term and premature
infants .. American Journal of Diseases of Children 1990; 144( 1 ):36-40.
Pittas AG, Harris SS, Stark PC, wson-Hughes B. The effects of calcium
and Vitamin D supplementation on blood glucose and markers of
inflammation in nondiabetic adults .. Diabetes Care 2007; 30(4):980-986.
Porojnicu AC, Robsahm TE, Dahlback A et al. Seasonal and
geographical variations in lung cancer prognosis in Norway. Does
Vitamin D from the sun play a role? Lung Cancer 2007; 55(3):263-270.
Prentice A, Ginty F, Stear SJ, Jones SC, Laskey MA, Cole TJ. Calcium
supplementation increases stature and bone mineral mass of 16- to 18-
year-old boys. Journal of Clinical Endocrinology & Metabolism 90
(6):3153-61, 2005.
Prineas RJ, Folsom AR, Zhang ZM, Sellers TA, Potter J. Nutrition and
other risk factors for renal cell carcinoma in postmenopausal women.
Epidemiology 8 ( 1):31-6, 1997.
Purwar M, Kulkarni H, Motghare V, Dhole S. Calcium supplementation
and prevention of pregnancy induced hypertension. Journal ofObstetJics
& Gynaecology Research 22 (5):425-30, 1996.
Rajalakshmi R, Sail SS, Shah DG, Ambady SK. The effects of
supplements varying in carotene and calcium content on the physical,
biochemical and skeletal status of preschool children. British Journal of
Nutrition 30 (1):77-86, 1973.
Rajpathak SN, Rimm EB, Rosner B, Willett WC, Hu FB. Calcium and
dairy intakes in relation to long-term weight gain in US men. American
Journal of Clinical Nutrition 83 (3 ):559-66, 2006.
Rees GA, Doyle W, Srivastava A, Brooke ZM, Crawford MA, Costeloe
KL. The nutrient intakes of mothers of low birth weight babies - a
comparison of ethnic groups in East London, UK. Maternal & Child
Nutrition 1(2):91-9, 2005.
Repke JT, Villar J, Anderson C, Pareja G, Dubin N, Belizan JM.
Biochemjcal changes associated with blood pressure reduction induced
by calcium supplementation during pregnancy. American Journal of
Obstetrics & Gynecology 160 (3):684-90, 1989.
Repke JT, Villar J. Pregnancy-induced hypertension and low birth
weight: the role of calcium. American Journal of Clinical Nutrition
1991 ; 54(1 :Suppl): Suppl-241 S.
Resnick LM, Oparil S, Chait A et al. Factors affecting blood pressure
responses to diet: the Vanguard study. American Journal of
Hypertension 13(9):956-65, 2000.
Reunanen A, Knekt P, Marniemi J, Maki J, Maatela J, Aromaa A. Serum
calcium, magnesium, copper and zinc and risk of cardiovascular death.
European Journal of Clinical Nutrition 50 (7):431-7, 1996.
Rich GM, McCullough M, Olmedo A, Malarick C, Moore TJ. Blood
pressure and renal blood flow responses to dietary calcium and sodium
intake in humans. American Journal of Hypertension 4(11 ):642S-645S,
1991.
24
Reason
Changes in 25(0H)D status of term and
premature infants
No outcomes of interest
Ecological study
In Winzenberg 2007 systematic review
No outcomes of interest
In Hofmeyer 2007 systematic review
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No outcomes of interest
No outcomes of interest
In Hofmeyer 2007 systematic review
Review paper
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No 25(0H)D or dietary Ca
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Excluded Study
Roberts CC, Chan GM, Folland D, Rayburn C, Jackson R. Adequate
bone mineralization in breast-fed infants. Journal of Pediatrics 99
(2):192-6, 1981.
Robien K, Cutler GJ, Lazovich D. Vitamin D intake and breast cancer
risk in postmenopausal women: the Iowa Women's Health Study. Cancer
Causes & Control 2007; 18(7):775-782.
Rogers MS, Fung HY, Hung CY. Calcium and low-dose aspirin
prophylaxis in women at high risk of pregnancy-induced hypertension.
Hypertension in Pregnancy I 8 (2): 165-72, 1999.
Roongpisuthipong C, Kantawan R, Roongpi suthipong W. Reduction of
adipose tissue and body weight: effect of water soluble calcium
hydroxycitrate in Garcinia atroviridis on the short term treatment of
obese women in Thailand. Asia Pacific Journal of Clinical Nutrition
2007; 16(1):25-29.
Rosell M, Hakansson NN, Wolk A. Association between dairy food
consumption and weight change over 9 yin 19,352 perimenopausal
women. American Journal of Clinical Nutri tion 2006; 84(6):1481-1488.
Rothberg AD, Petti for JM, Cohen DF, Sonnendecker EW, Ross FP.
Maternal-infant Vitamin D relationships during breast-feeding. Journal
ofPediatrics 101 (4):500-3, 1982.
Rourke KM, Brehm BJ, Cassell C, Sethuraman G. Effect of weight
change on bone mass in female adolescents. Journal of the American
Dietetic Association 103 (3):369-72, 2003.
Rozen P, Fireman Z, Fine N, WaxY, Ron E. Oral calcium suppresses
increased rectal epithelial proliferation of persons at risk of colorectal
cancer. Gut 30(5):650-5, 1989.
Rozen P, Lubin F, Papo Net al. Calcium supplements interact
significantly with long-term diet while suppressing rectal epithelial
proliferation of adenoma patients. Cancer 91 ( 4):833-40, 2001.
Rum.iris D, Purwosunu Y, Wibowo N, Farina A, Sekizawa A. Lower rate
of preeclampsia after antioxidant supplementation in pregnant women
with low antioxidant status. Hypertension in Pregnancy 2006; 25(3):241-
253.
Rush D, Sloan NL, Leighton Jet al. The National WJC Evaluation:
evaluation of the Special Supplemental Food Program for Women,
Infants, and Children. V. Longitudinal study of pregnant women.
American Journal of Clinical Nutrition 48 (2 Suppl):439-83, 1988.
Saadi HF, Dawodu A, Afandi B et al. Effect of combined maternal and
infant vitamin D supplementation on vitamin D status of exclusively
breastfed infants. Maternal & Child Nutrition 5(1):25 -32 , 2009.
Sacks FM, Brown LE, AppelL, Borhani NO, Evans D, Whelton P.
Combinations of potassium, calcium, and magnesium supplements in
hypertension. Hype11ension 26 (6 Pt 1):950-6, 1995.
Sacks FM, Obarzanek E, Windhauser MM et al. Rationale and design of
the Dietary Approaches to Stop Hypertension trial (DASH). A
multicenter controlled-feeding study of dietary patterns to lower blood
pressure. Annals of Epidemiology 5(2): 108-18, 1995.
25
Reason
ln Ottawa EPC report
Observational study estimated Vitamin
D supplement doses
In Hofmeyer 2007 systematic review
No 25(0H)D or dietary Ca
Ca intake and BW measured but not
assessed ==> no relevant results
reported
In Ottawa EPC report
No 25(0H)D or dietary Ca
No outcomes of interest
No outcomes of interest
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No exposure of interest
arrow 4 RCT but daily doses were the
same in the comparison groups
(comparison of daily vs. monthly doses)
Combinations of minerals
No outcomes of interest
Excluded Study
Sacks FM, Willett WC, Smith A, Brown LE, Rosner B, Moore TJ.
Effect on blood pressure of potassium, calcium, and magnesium in
women with low habitual intake. Hypertension 31 (1):131-8, 1998.
Saito K, Sano H, Kawahara J, Yokoyama M. Calcium supplementation
attenuates an enhanced platelet function in salt-loaded mildly
hypertensive patients. Hypertension 26 (I): 156-63, 1995.
Sakhaee K, BakerS, Zerwekh J, Poindexter J, Garcia-Hernandez PA,
Pak CY. Limited risk of kidney stone formati on during long-te1m
calcium citrate supplementation in nonstone forming subjects. Journal of
Urology 152 (2 Pt I ):324-7, 1994.
Sakhaee K, Poindexter JR, Griffith CS, Pak CY. Stone forming risk of
calcium citrate supplementation in healthy postmenopausal women.
Journal of Urology 172 (3):958-61, 2004.
Salazar-Martinez E, Lazcano-Ponce E, Sanchez-Zamorano LM,
Gonzalez-Lira G, Escudero-DE Los RP, Hernandez-Avila M. Dietary
factors and endometrial cancer risk. Results of a case-control study in
Mexico. International Journal of Gynecological Cancer 15 (5):938-45 ,
2005.
Sampath V, Havel PJ, King JC. Calcium supplementation does not alter
lipid oxidation or lipolysis in overweight/obese women. Obesity 16
(11 ):2400 -4, 2008.
Sanchez-Ramos L, Adair CD, Kaunitz AM, Briones DK, Del Valle GO,
Oelke 1. Calcium supplementation in mild preeclampsia remote from
term: a randomized double-blind clinical trial. Obstetrics & Gynecology
85 (6):915-8, 1995.
Sanchez-Ramos L, Briones DK, Kaunitz AM, Delvalle GO, Gaudier FL,
Walker CD. Prevention of pregnancy-induced hypertension by calcium
supplementation in angiotensin 11-sensitive patients. Obstetrics &
Gynecology 84 (3):349-53, 1994.
Sanders T A, Purves R. An anthropometric and dietary assessment of the
nutritional status of vegan preschool children. Journal of Human
Nutrition 35 (5):349-57, 1981.
Sato K, Emoto N, Toraya Setal. Progressively increased serum I ,25-
dihydroxyVitamin 02 concentration in a hypoparathyroid patient with
protracted hypercalcemia due to Vitamin 02 intoxication. Endocrine
Journal 41 (4):329-37, 1994.
Satterfield S, Cutler JA, Langford HG et al. Trials of hypertension
prevention. Phase T design. Annals ofEpidemiology 1(5):455-71, 1991.
SchleithoffSS, Zittermann A, Tenderich G, Berthold HK, Stehle P,
Koerfer R. Vitamin D supplementation improves cytokine profiles in
patients with congestive heart failure: a double-blind, randomized,
placebo-controlled trial.[see comment]. American Joumal of Clinical
Nutrition 83 (4):754 -9 , 2006.
Schumann SA, Ewigman B. Double-dose Vitamin D lowers cancer risk
in women over 55. Joumal ofFamily Practice 2007; 56(11):907-910.
26
Reason
ln systematic review
Data too incomplete
No UL outcomes
No UL outcomes: saturation of CaOx
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
not RCT wt study
100% patients with already diagnosed
"mild" preeclampsia
ln Hofmeyer 2007 systematic review
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Case report
Shows research design, but no result
>=20% subjects with diseases
Editorial-like brief review
Excluded Study
Sellers T A, Bazyk AE, Bostick RM et a!. Diet and risk of colon cancer
in a large prospective study of older women: an analysis stratified on
family history (Iowa, United States). Cancer Causes & Control9(4):357-
67, 1998.
Shahar DR, Abel R, Elhayany A, Vardi H, Fraser D. Does dairy calcium
intake enhance weight loss among overweight diabetic patients?
Diabetes Care 2007; 30(3):485-489.
Shapses SA, Heshka S, Heymsfield SB. Effect of calcium
supplementation on weight and fat loss in women. Journal of Clinical
Endocrinology & Metabolism 89 (2):632-7, 2004.
Sharkey JR, Giuliani C, Haines PS, Branch LG, Busby-Whitehead J,
Zohoori N. Summary measure of dietary musculoskeletal nutrient
(calcium, Vitamin D, magnesium, and phosphorus) intakes is associated
with lower-extremity physical performance in homebound elderly men
and women. American Journal of Clinical Nutrition 77 (4):847-56, 2003.
Shaunak S, Ang L, Colston K, Patel S, Bland M, Maxwell JD. Muscle
strength in healthy white and Asian subjects: the relationship of
quadriceps maximum voluntary contraction to age, sex, body build and
Vitamin D. Clinical Science 73 (5):541-6, 1987.
Sibai BM, Ewell M, Levine RJ eta!. Risk factors associated with
preeclampsia in healthy nulliparous women. The Calcium for
Preeclampsia Prevention (CPEP) Study Group .. American Journal of
Obstetrics & Gynecology 177 (5): 1003-10, 1997.
Sieg J, Sieg A, Dreyhaupt J, Schmidt-Gayk H. tnsufficient Vitamin D
supply as a possible co-factor in colorectal carcinogenesis. Anticancer
Research 26 (4A):2729 -33, 2006.
Silverman SL, Delmas PD, Kulkarni PM, Stock JL, Wong M, Plouffe L,
Jr. Comparison of fracture, cardiovascular event, and breast cancer rates
at 3 years in postmenopausal women with osteoporosis. Journal of the
American Geriatrics Society 52 (9):1543-8, 2004.
Sita-Lumsden A, Lapthorn G, Swaminathan R, Milburn HJ. Reactivation
of tuberculosis and Vitamin D deficiency: the contribution of di et and
exposure to sunlight. Thorax 62 (11):1003-7, 2007.
Siwek RA, Burkinshaw L, Oxby CB, Robinson PA. Multi-element
analysis of the obese subject by in vivo neutron activation analysis.
Physics in Medicine & Biology 29 (6):687-701, 1984.
Skinner JD, Bounds W, Carruth BR, Ziegler P. Longitudinal calcium
intake is negatively related to children's body fat indexes .. Journal of the
American Dietetic Association 103 (12):1626-31, 2003.
Slemenda CW, Reister TK, Hui SL, Miller JZ, Christian JC, Johnston
CC, Jr. Influences on skeletal mineralization in children and adolescents:
evidence for varying effects of sexual maturation and physical
actiVitaminy. Journal of Pediatrics 125 (2):201-7, 1994.
Specker BL, Beck A, Ka1kwarf H, Ho M. Randomized trial of varying
mineral intake on total body bone mineral accretion dming the first year
of life. Pediatrics 99(6): E12, 1997.
27
Reason
Same cohort as Zheng 1998 (ReflD
2924) only difference is that taking into
consideration the family history of colon
cancer in the analysis
>=20% subjects with diseases
In systematic review
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No Cadose
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
Not relevant
Not RCT growth study
No 25(0H)D or dietary Ca
No independent Ca effect
Excluded Study
Specker BL, Tsang RC, HoM, Miller D. Effect of vegetarian diet on
serum 1,25-diliydroxyVitamin D concentrations during lactation.
Obstetrics & Gynecology 70 (6):870-4, 1987.
Specker BL, Valanis B, Hertzberg V, Edwards N, Tsang RC. Sunshine
exposure and serum 25-hydroxyVitamin D concentrations in exclusively
breast-fed infants. Journal of Pediatrics 107 (3):372-6, 1985.
Stamler J, Liu K, Ruth KJ, Pryer J, Greenland P. Eight-year blood
pressure change in middle-aged men: relationship to multiple nutrients.
Hypertension 39 (5): 1000-6, 2002.
Stern HS, Gregoire RC, Kashtan H, Stadler J, Bruce RW. Long-term
effects of dietary calcium on risk markers for colon cancer in patients
with familial polyposis. Surgery I 08 (3):528-33, 1990.
Sugden JA, Davies ll, Witham MD, Monis AD, Struthers AD. Vitamin
D improves endothelial function in patients with Type 2 diabetes
mellitus and low vitamin D levels. Diabetic Medicine 2008;25:320-5.
Swanenburg J, de Bruin ED, Stauffacher M, Mulder T, Uebelhart D.
Effects of exercise and nutrition on postural balance and risk of falling in
elderly people with decreased bone mineral density: randomized
controlled trial pilot study. Clinical Rehabilitation 2007; 21 (6):523-534.
Takeuchi A, Okano T, Tsugawa N et al. Effects of ergocalciferol
supplementation on the concentration of Vitamin D and its metabolites
in human milk. Journal of Nutrition 119 (11):1639-46, 1989.
Tanji JL, LewEY, Wong GY, TreguboffC, Ward JA, Amsterdam EA.
Dietary calcium supplementation as a treatment for mild hypertension ..
Journal of the American Board of Family Practice 4(3): 145-50, 1991.
Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of
incident kidney stones in men: new insights after 14 years of follow-up.
Journal of the American Society of Nephrology 15 (12):3225-32, 2004.
Teegarden D, White KM, Lyle RM et al. Calcium and dairy product
modulation of lipid utilization and energy expenditure. Obesity 16
(7): 1566-72, 2008.
Thompson IM, Coltman CA, Jr., Crowley J. Chemoprevention of
prostate cancer: the Prostate Cancer Prevention Trial. Prostate 33
(3):217-21 , 1997.
Thompson WG, Rostad HN, Janzow D.T, Slezak JM, Morris KL, Zemel
MB. Effect of energy-reduced diets high in dairy products and fiber on
weight loss in obese adults .. Obesity Research 13(8): 1344-53, 2005.
Thomson K, Morley R, Grover SR, Zacharin MR. Postnatal evaluation
of Vitamin D and bone health in women who were Vitamin D-deficient
in pregnancy, and in their infants.[erratum appears in Med J Aust. 2005
Jan 3; 182(1 ):48 Note: Thompson, Kathetine [corrected to Thomson,
Katherine]]. Medical .Toumal of Australia 181 (9):486-8, 2004.
Tomoda S, Kitanaka T, Ogita S, Hidaka A. Prevention of pregnancy-
induced hypertension by calcium dietary supplement: a preliminary
report. Journal of Obstetrics & Gynaecology 21 (3):281-8, 1995.
28
Reason
No 25(0H)D or dietary Ca
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No outcomes of interest
No outcomes of interest
>=20% subjects with diseases
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Not RCT arrow 4 study
In systematic review
No outcomes of interest
No outcomes of interest
Commentary
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
No analysis of association between
25(0H)D and outcomes
No outcomes of interest
Excluded Study
Tretli S, Hernes E, Berg JP, Hestvik UE, Robsahm TE. Association
between serum 25(0H)D and death from prostate cancer. British Journal
of Cancer 100 (3):450 -4,2009.
Tsang RC, Gigger M, Oh W, Brown DR. Studies in calcium metabolism
in infants with intrauterine growth retardation. Journal of Pediatrics 86
(6):936-41 ' 1975.
Tworoger SS, Lee IM, Buring JE, Rosner B, Hollis BW, Hankinson SE.
Plasma 25-hydroxyVitamin D and I ,25-dihydroxyVitamin D and risk of
incident ovarian cancer. Cancer Epidemiology, Biomarkers &
Prevention 2007; 16(4):783-788.
van Beresteijn EC, Riedstra M, van der W A, Schouten EG, Burema J,
Kok FJ. Habitual dietary calcium intake and blood pressure change
around the menopause: a longitudinal study. International Journal of
Epidemiology 21(4):683-9, 1992.
van Buul BJ, Steegers EA, Jongsma HW et al. Dietary sodium restriction
in the prophylaxis of hypertensive disorders of pregnancy: effects on the
intake of other nutrients. American Journal of Clinical Nutrition 62
(1):49-57, 1995.
Vatanparast H, Baxter-Jones A, Faulkner RA, Bailey DA, Whiting SJ.
Positive effects of vegetable and fruit consumption and calcium intake
on bone mineral accrual in boys during growth from childhood to
adolescence: the University of Saskatchewan Pediatric Bone Mineral
Accrual Study. American Journal of Clinical Nutrition 82 (3):700-6,
2005.
Vergnaud AC, Peneau S, Chat-Yung Setal. Dairy consumption and 6-y
changes in body weight and waist circumference in middle-aged French
adults. American Journal of Clinical Nutrition 88 (5): 1248 -55 , 2008.
Verhaar HJ, Samson MM, Jansen PA, de Vreede PL, Manten JW,
Duursma SA. Muscle strength, functional mobility and Vitamin Din
older women .. Aging-Clinical & Experimental Research 12 (6):455-60,
2000.
Verreault R, Semba RD, Volpato S, Ferrucci L, Fried LP, Guralnik JM.
Low serum Vitamin d does not predict new disability or loss of muscle
strength in older women .. Journal of the American Geriatrics Society 50
(5):912-7, 2002.
Verreault R, Semba RD, Volpato S, Ferrucci L, Fried LP, Guralnik JM.
Low serum Vitamin d does not predict new disability or loss of muscle
strength in older women .. Journal of the American Geriatrics Society
50(5):912-7, 2002.
Villar J, bdei-Aieem H, Merialdi Metal. World Health Organization
randomized trial of calcium supplementation among low calcium intake
pregnant women. American Journal of Obstetrics & Gynecology.
194(3):639-49, 2006 Mar.
Villar J, Gulmezoglu AM, de OM. Nutritional and antimicrobial
interventions to prevent preterm birth: an overview of randomized
controlled trials. Obstetrical & Gynecological Survey 53 (9):575-85 ,
1998 Sep.
29
Reason
>=20% subjects with diseases
No 25(0H)D or dietary Ca
No outcomes of interest
No outcomes of interest
Ca intake and BM (mothers and
neonates) measured but not assessed
==> no relevant results reported
No 25(01-I)D or dietary Ca
not RCT (weight outcome)
In Ottawa EPC report
In Ottawa EPC report
In Ottawa EPC report
In Hofmeyer 2007 systematic review,
systematic review
Not relevant systematic review
Excluded Study
Villar J, Repke JT. Calcium supplementation during pregnancy may
reduce preterm delivery in high-risk populations. American Journal of
Obstetrics & Gynecology 163 (4 Pt 1):1124 -31, 1990.
Visser M, Deeg DJ, Lips P, Longitudinal Aging SA. Low Vitamin D and
high parathyroid hormone levels as determinants of loss of muscle
strength and muscle mass (sarcopenia): the Longitudinal Aging Study
Amsterdam. Journal of Clinical Endocrinology & Metabolism 88
(12):5766-72, 2003.
von Hurst PR, Stonehouse W, Matthys C, Conlon C, Kruger MC, Coad
J. Study protocol--metabolic syndrome, vitamin D and bone status in
South Asian women living in Auckland, New Zealand: a randomi sed,
placebo-controlled, double-blind vitamin D intervention. BMC Public
Health 8 :267 , 2008.
Wallace K, Baron JA, Cole BF eta!. Effect of calcium supplementation
on the risk of large bowel polyps.[see comment]. Journal of the National
Cancer Institute 96 ( 12 ):921 -5, 2004.
Wallace K, Baron JA, Karagas MR eta!. The association of physical
actiVitaminy and body mass index with the risk of large bowel polyps.
Cancer Epidemiology, Biomarkers & Prevention 14(9):2082-6, 2005.
Waltman NL, Twiss JJ, Ott CD eta!. Testing an intervention for
preventing osteoporosis in postmenopausal breast cancer survivors.
Journal of Nursing Scholarship 35 (4):333-8, 2003.
Wanchu M, Malhotra S, Khullar M. Calcium supplementation in pre-
eclampsia. Journal of the Association of Physicians of India 49:795-8,
2001.
Wang LD, Qiu SL, Yang GR, Lipkin M, Newmark HL, Yang CS. A
randomized double-blind intervention study on the effect of calcium
supplementation on esophageal precancerous lesions in a high-risk
population in China. Cancer Epidemiology, Biomarkers & Prevention
2(1):71-8, 1993.
Wargovich MJ, Isbell G, Shabot Metal. Calcium supplementation
decreases rectal epithelial cell proliferation in subjects with sporadic
adenoma .. Gastroenterology 103 ( 1):92-7, 1992.
Webb AR, Pilbeam C, Hanafin N, Holick MF. An evaluation of the
relative contributions of exposure to sunlight and of diet to the
circulating concentrations of25-hydroxyVitamin Din an elderly nursing
home population in Boston. American Journal of Clinical Nutrition 51
(6): I 075-81, 1990.
Webber CE, Blake JM, Chambers LF, Roberts JG. Effects of2 years of
hormone replacement upon bone mass, serum lipids and lipoproteins.
Maturitas. 19(1):13-23, 1994 May.
Wei EK, Giovannucci E, Fuchs CS, Willett WC, Mantzoros CS. Low
plasma adiponectin levels and risk of colorectal cancer in men: a
prospective study. Journal of the National Cancer Institute 97 (22): 1688-
94,2005.
30
Reason
ln Hofrneyer 2007 systematic review
In Ottawa EPC report
RCT protocol only
In Weigarten 2008 SR
No outcomes of interest
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
In Hofmeyer 2007 systematic review
>=20% subjects with diseases
No outcomes of interest
Not RCT arrow 4 study
No 25(01-I)D or dietary Ca
No 25(01-I)D or dietary Ca
Excluded Study
Weinberger MH, Wagner UL, Fineberg NS. The blood pressure effects
of calcium supplementation in humans of known sodium responsiveness.
American Journal of Hypertension 6 (9):799-805, 1993.
Weisgerber UM, Boeing H, Owen RW, Waldberr R, Raedsch R,
Wahrendorf J. Effect of Jongterm placebo controlled calcium
supplementation on sigmoidal cell proliferation in patients with sporadic
adenomatous polyps. Gut 38 (3):396-402, 1996.
Weisman Y, Bawnik JC, Eisenberg Z, Spirer Z. Vitamin D metabolites
in human milk. Journal of Pediatrics 100 (5):745-8, 1982.
Weston TL, Aronson KJ, Siemiatycki J, Howe GR, Nadon L. Cancer
mortality among males in relation to exposures assessed through a job-
exposure matrix. International Journal of Occupational & Environmental
Health 6(3):194-202, 2000.
Widga AC, Lewis NM. Defined, in-home, prenatal nutrition intervention
for low-income women. Joumal of the American Dietetic Association
99(9): I 058-62, 1999.
Reason
ln systematic review
No outcomes of interest
Cross-sectional or retrospective
assessment of diet after disease
diagnosis
No 25(0H)D or dietary Ca
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Willett WC, Stampfer MJ, Colditz GA, Rosner BA, Speizer FE. Relation No 25(0H)D or dietary Ca
of meat, fat, and fiber intake to the risk of colon cancer in a prospective
study among women. N Eng! J Med 1990; 323(24): 1664-16 72.
Williams CP, Child DF, Hudson PR eta!. Why oral calcium
supplements may reduce renal stone disease: report of a clinical pilot
study. Journal of Clinical Pathology 54 ( 1):54-62, 2001.
Wimalawansa SJ. Antihypertensive effects of oral calcium
supplementation may be mediated through the potent vasodilator CGRP.
American Journal of Hypertension 6 (12):996-1002, 1993.
Witteman JC, WiHett WC, Stampfer MJ eta!. A prospective study of
nutritional factors and hypertension among US women. Circulation 80
(5):1320-7, 1989.
W01tsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased
bioavailability ofVitanlin Din obesity. [erratum appears in Am J Clio
Nutr. 2003 May;77(5):1342). American Journal of Clinical Nutrition 72
(3):690-3, 2000.
Wosje KS, KalkwarfHJ. Lactation, weaning, and calcium
supplementation: effects on body composition in postpartum women.
American Journal of Clinical Nutrition 80 (2):423-9, 2004.
Wyatt HR, Jo1tberg BT, Babbel C eta!. Weight loss in a community
initiative that promotes decreased energy intake and increased physical
actiVitaminy and dairy consumption: Calcium Weighs-In. Journal of
Physical ActiVitaminy & Health 5( I ):28-44, 2008.
Yang YX, Han JH, Shao XP eta!. Effect of micronutrient
supplementation on the growth of preschool children in China.
Biomedical & Environmental Sciences 15 (3): 196-202, 2002.
31
No UL outcomes
n=8, Ca to Rx HTN
Superceded by Ascherio (4022)
Not RCT arrow 4 study
No outcomes of interest
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Excluded Study
Yesudian PD, Berry JL, Wiles Setal. The effect of ultraviolet B-
induced Vitamin D levels on host resistance to Mycobacterium
tuberculosis: a pilot study in immigrant Asian adults living in the United
Kingdom. Photodermatology, Photoimmunology & Photomedicine 24
(2):97-8, 2008.
Zemel MB, Richards J, Milstead A, Campbell P. Effects of calcium and
dairy on body composition and weight loss in African-American adults.
Obesity Research 13(7):1218 -25, 2005.
Zemel MB, Thompson W, Milstead A, Morris K, Campbell P. Calcium
and dairy acceleration of weight and fat loss during energy restriction in
obese adults .. Obesity Research 12 ( 4 ):582-90, 2004.
Zhang Y, Kiel DP, Ellison RC et al. Bone mass and the risk of prostate
cancer: the Framingham Study. American Journal of Medicine 113
(9):734 -9, 2002.
Zhou C, Fan S, Zhou L, Ni Y, Huang T, Shi Y. Clinical observation of
treatment of hypertension with calcium. American Journal of
Hypertension 7 (4 Pt 1):363-7, 1994.
Zofkova I, Hill M. Long-term I ,25(0H)2 Vitamin D therapy increases
bone mineral density in osteopenic women. Comparison with the effect
of plain Vitamin D. Aging-Clinical & Experimental Research.
19(6):472-7, 2007 Dec.
Zorbas YG, Petrov KL, Kakurin VJ et al. Calcium supplementation
effect on calcium balance in endurance-trained athletes during prolonged
hypokinesia and ambulatory conditions. Biological Trace Element
Research 73 (3):231-50, 2000.
32
Reason
No outcomes of interest
rn systematic review
rn systematic review
No 25(0H)D or dietary Ca
rn systematic review
Combination of Vitamin D/Ca and other
treatment w/o analysis of independent
effect
Arrow 4: calcium balance
FTC Consumer Alert
Federal Trade Commission Bureau of Consumer Protection Di vision of Consumer & Business Education
Indoor Tanning
Ads for tanning salons, sun lamps and tanning beds promise a bronzed body year-round, but
experts agree that ultraviolet (UV) radiation from these devices damages the skin and poses serious
health risks. Sunburns and tans are signs of skin damage. Deliberate tanning, either indoors or out,
increases your risk of melanoma and nonmelanoma skin cancer.
The Federal Trade Commission (FTC), the nation's consumer protection agency, and the Food
and Drug Administration (FDA), enforce laws dealing with tanning devices. The FTC investigates
false, misleading, and deceptive advertising claims about the devices; the FDA enforces regulations
that deal with the labels on the devices.
Myths and Reality
Here are some claims commonly made about indoor tanning- and the facts.
"Get a beautiful tan indoors without increasing your risk of skin cancer. "
The lamps used in tanning booths and beds emit two forms of ultraviolet (UV) radiation - UV A
and UVB. UVB rays penetrate the top layers of your skin and are most responsible for burns. UVA
rays penetrate to the deeper layers of skin and often are associated with allergic reactions, like a rash.
Both UV A and UVB rays damage the skin and can lead to skin cancer. What's more, scientists say,
tanning can cause premature aging, immune suppression, and serious eye damage.
"Indoor tanning is safer than the sun because the environment is controlled. "
Sun lamps may be more dangerous than the sun because they can be used at the same high
intensity every day of the year. Radiation from the sun varies in intensity with the time of day, the
season, and cloud cover. Studies show that many people who tan indoors get burns.
"Indoor tanning is approved by the government. "
No U.S. government agency recommends the use of indoor tanning equipment. And the
International Agency for Research on Cancer (IARC), part of the World Health Organization, also has
concluded that tanning devices that emit UV radiation are more dangerous than previously thought.
IARC moved these devices into the highest cancer risk category.
"Indoor tanning is a safe way to increase vitamin D levels. "
Vitamin D has many roles in human health. For example, it is essential for promoting good bone
health. While UVB radiation helps your body produce vitamin D, you don't need a tan to get that
benefit. In fact, 10 to 15 minutes of unprotected natural sun exposure on your face and hands 2 to 3
times a week during the summer gives you with a healthy dose of vitamin D. You also can get vitamin
D from food: good sources include low-fat milk, salmon, tuna, and fortified orange juice.
For More Information
To learn more about the risks of tanning, visit:
The Food and Drug Administration
www .fda. gov /ForConsumers/ConsumerUpdates/ucm186687 .htm
The American Cancer Society
www.cancer.org
The American Academy of Dermatology
www .aad.org
The FTC works for the consumer to prevent fraudulent, deceptive and unfair business practices
in the marketplace and to provide information to help consumers spot, stop and avoid them. To file a
complaint or to get free information on consumer issues, visit ftc.gov or call toll-free,
1-877-FTC-HELP (1-877-382-4357); TTY: 1-866-653-4261. The FTC enters consumer complaints
into the Consumer Sentinel Network, a secure online database and investigative tool used by hundreds
of civil and criminal law enforcement agencies in the U.S. and abroad.
January 2010
BMJ
BMJ 2012;345:e5909 doi: 1 0.1136/bmj.e5909 (Published 2 October 2012) Page 1 of 9
RESEARCH
Indoor tanning and non-melanoma skin cancer:
systematic review and meta-analysis
S ~ OPEN ACCESS
Mackenzie R Wehner medical student
1
MPhil scholar in epidemiologl, Melissa L Shive medical
student
3
, Mary-Margaret Chren professor
4
, Jiali Han associate professor
56
, Abrar A Qureshi associate
professor
5
, Eleni Li nes assistant professor
4
'Stanford University School of Medicine, Stanford, CA, USA;
2
Department of Public Health and Primary Care, University of Cambridge, Cambridge,
UK;
3
University of California San Francisco (UCSF) School of Medicine, San Francisco, CA, USA; Department of Dermatology, University of
California San Francisco (UCSF). 2340 Sutter Street , San Francisco, CA, 94143-0808, USA;
5
Department of Dermatology, Channing Laboratory,
Department of Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA;
6
Department of Epidemiology, Harvard School
of Public Health, Boston, MA, USA
Abstract
Objective To synthesise the literature on indoor tanning and
non-melanoma skin cancer.
Design Systematic review and meta-analysis.
Data sources PubMed (1966 to present), Embase (1974 to present),
and Web of Science (1898 to present).
Study selection All articles that reported an original effect statistic for
indoor tanning and non-melanoma skin cancer were included. Articles
that presented no data, such as review articles and editorials, were
excluded, as were articles in languages other than English.
Data extraction Two investigators independently extracted data.
Random effects meta-analysis was used to summarise the relative risk
of ever use versus never use of indoor tanning. Dose-response effects
and exposure to indoor tanning during early life were also exami ned.
The population attributable risk fraction for the United States population
was calculated.
Results 12 studies with 9328 cases of non-melanoma skin cancer were
included. Among people who reported ever using indoor tanning
compared with those who never used indoor tanning, the summary
relative risk for squamous cell carcinoma was 1.67 (95% confidence
interval 1.29 to 2.17) and that for basal cell carcinoma was 1 .29 (1.08
to 1.53). No significant heterogeneity existed between studies. The
population attributable risk fraction for the United States was estimated
to be 8.2% for squamous cell carcinoma and 3.7% for basal cell
carcinoma. This corresponds to more than 170 000 cases of
non-melanoma skin cancer each year attributable to indoor tanning. On
the basis of data from three studies, use of indoor tanning before age
25 was more strongly associated with both squamous cell carcinoma
Correspondence to: E Linos linose@derm.ucsf.edu
(relative risk 2.02, 0.70 to 5.86) and basal cell carcinoma (1.40, 1.29 to
1.52).
Conclusions Indoor tanning is associated with a significantly increased
risk of both basal and squamous cell skin cancer. The risk is higher with
use in early life (<25 years). This modifiable risk factor may account for
hundreds of thousands of cases of non-melanoma skin cancer each
year in the United States alone and many more worldwide. These findings
contribute to the growing body of evidence on the harms of indoor tanning
and support public health campaigns and regulation to reduce exposure
to this carcinogen.
Introduction
The incidence of basal cell carcinoma and squamous cell
carcinoma of the skin, collectively termed non-melanoma skin
cancer (NMSC), has increased dramatically over previous
decades, in what some have termed an epidemic.'
2
NMSC is
by far the most common human malignancy, and nearly 30%
of white people living in areas of exposure to high ultraviolet
radiation will develop an NMSC in their lifetime.
3
Because of
its high prevalence, NMSC is a considerable financial burden
to healthcare systems:.,;
Although NMSC is the most common cancer, it is often
excluded from national cancer registries and cancer databases
because it typically does not affect survivaL NMSC is more
common in older men, but more tumours have recently been
documented in women and in younger people of both sexes.
7 8
Besides older age and male sex, major risk factors for
development of NMSC include light skin, family history,
residence at latitudes near the equatOr, and exposure to
ultraviolet radiation.
9 10
Extra material supplied by the author (see http://www.bmj.com/content/345/bmj .e5909?tab=related#webextra)
No commercial reuse: See rights and reprints http11www.bmJ.COm/perm,sstons Subscribe: http://www.bmj.comlsubscrl be
BMJ 2012;345:e5909 doi: 1 0.1 136/bmj.e5909 (Publi shed 2 October 2012)
Because it is potentially modifiable, indoor tanning is a
particularly important type of exposure to ultraviolet radiation.
Indoor tanning is a class I carcinogen, considered "carcinogenic
to humans" by the International Agency for Research on
Cancer. '' Indoor tanning is significantly associated with
increased ri sk of malignant melanoma and was shown to be a
potential risk factor for NMSC in a previous, smaller
meta-analysis.
12
u Several studies have examined the link
between NMSC and indoor tanning.
1
4-
29
However, the study
sizes and the percentage of participants reporting exposure have
been smal l, yielding varied results. Our aim in this study was
to synthesise the available data on indoor tanning and NMSC.
Methods
We carried out this review in accordance with the Preferred
Reporting Items for Systematic Reviews and Meta-Analyses
(PRISMA) guidelines.
30
Literature search
We defined NMSC as either basal cell carcinoma or squamous
cell carcinoma and indoor tanning as the use of an ultraviolet
emission device to produce a cosmetic tan. The terminology
used in the li terature is diverse. In this analysis, we considered
indoor tanning. sun bed, sunlamp. tanning bed, tanning booth,
solarium. artificial tanning, anificial ultraviolet tanning,
non-solar ultraviolet tanning, and variations of these to be
synonymous with indoor tanning.
We identified studies through searches of electronic databases
and by scanning reference li sts of articles. We searched PubMed
(1966 to present), Em base ( 1974 to present), and Web of Science
(1898 to present). Two authors (MRW and MLS) did the search,
and the last search was run on 16 March 2012. Additionally,
we reviewed identifi ed arti cles and reviews on the topics of
NMSC and ultraviolet exposure closely to locate additional
articl es. Specifics of the search strategy used in each database
are detailed in the supplementary materials.
All publi shed articles in English that reported an effect statistic
for indoor tanning and NMSC or that reported measuring or
adjusting for indoor tanning in a study including participants
with NMSC were eli gible for inclusion. Two authors (MRW
and MLS) assessed the eligibility of studies by using the title
and abstract for initial screening followed by review of the full
text. We excl uded anicles that presented no data, such as review
articles and editorials, and articles in languages other than
English. Inclusion criteria for quantitative meta-analysis were
studies reporting an effect estimate, such as an odds ratio or
hazard ratio, or reponing measurement of or adjustment for
indoor tanning that could be used to ca.lculate an effect estimate.
We used a data extraction sheet , which was developed on the
basis of the Cochrane Consumers and Communication Review
Group's data extraction template. We extracted the following
data items from each st udy: characteristics of study participants
(including age, sex, type of NMSC) and inclusion/exclusion
criteria, characteristics of study design (including design type,
presence of matching in case-control studies, matching
characteristics, and number of controls per case), outcomes
(including effect estimates of different doses of exposure to
indoor tanning), and stati sti cal methods (incl uding univariate
or multivariate analyses, logistic regressions, and variables
included).
No commercial reuse. See rights and reprints http www.blllJ.com OOfm ss ons
Page 2of 9
RESEARCH
Statistical methods
For the primary meta-analysis, we used the odds ratio or hazard
ratio for ever exposure to indoor tanning, which was the
exposure measure used by most of the studies. Ever exposure
(for example, pan icipants were asked: "Have you ever used an
indoor u.ltraviolet tanning device to produce a cosmetic tan?")
was avai lable for 10 studies. For two studies, the only available
measure was "regular" exposure (Bakos et al
17
) or greater than
five exposures per year (Walther et al
28
). We thus did the primary
analysis on the 10 studies reporting ever exposure and a
subsequent sensiti vity analysis that included all 12 studies. In
one instance, we calculated an unadj usted odds ratio and 95%
confidence interval from the raw data of a matched study. Data
comparing ever use versus never use of indoor tanning came
directly from the authors of one study that did not show this
comparison in the manuscript.
29
We also did a sensitivity
analysis excl uding four retrospective studies that did not fully
. . I bl ) t t9 21 21
adJUSt lor confounders (see supp ementary ta e .
We did additional analyses on studi es that reported effect
statistics for hi gh dose exposures and on studies that reported
effect stati sti cs for young age at exposure. High dose exposure
was assessed by four studies, which used exposure measures of
"regular use of tanning beds in lifetime,"'
7
6-26 years of regular
exposure,
20
exposure more than fi ve times per year,
28
and
exposure four times per year.
29
Three studies reported young
age at first exposure. using 16 years of age or younger,
20
less
than 20 years of age,
25
and ''high schooUcollege," which is
typically 14-25 years of age.
29
Although these studies used
different doses of exposure for high dose exposure and different
cut-off ages for young age, these represent the only and thus
best available data.
We used Stata II statistical software to do random effects model
meta-analyses, yielding summary relative risks and 95%
confidence interval s. All stati stical tests were two sided. We
analysed data for basal cell carcinoma and squamous cell
carcinoma separately. To investi gate variability (heterogeneity)
in study outcomes, we used a x
2
test for heterogeneity and an 1
2
stati stic.
We used the STROBE statement guidelines to assess the quality
ofindividual studies.
1
' Of 16 studies identified, two did not state
when data was coll ected,
13 26
three case-control studies did not
match cases and controls,
19 21 28
and three case-control studies
used frequency rather than individual matching.
2025 27
Additionally, nine studies did not clearly repon participation
rates, u
17 18 19 21 23 20 2
29
and three did not state ages or sexes of
panicipants.
22 23 20
To assess potential small study effects and publication bias
across studies, we created funnel plots by plotti ng the effect
found by each study against the inverse of its standard error.
We reviewed the funnel plot visually and used Begg's rank
correlation test and Egger' s weighted linear regression test for
formal testing. This aimed to investigate the possibilities that
smaiJ studies showing no effects may not be published and that
small studies are more likely to be done with less methodological
rigor, leading to inaccurate effect estimates.
We calculated popul ation proportional attributable risk as
(prevalence of exposurex(RR-l))/(1 +prevalence of
exposurex( RR- 1 )), where RR is relative risk. We calculated
this for the United States, for which we had representative data
on both the incidence of NMSC (estimated at 3 507 693 new
cases in 2006
2
) and one year prevalence of indoor tanning
(estimated at 13.4% for 2005
32
).
Subscribe: t-up: www bmj.com subscnbe
BMJ 2012;345:e5909 doi: 1 0.1 136/bmj.e5909 (Published 2 October 2012)
Results
Figure 1 JJ. shows the study selection process. Database searches
yielded a total of 558 unique publications whose title and
abstract were screened. We discarded 536 because of no
relevance (n=416), no unique data presented (for example,
editorial article or review, n=110), or language other than
English (n=lO). We examined the remaining 22 articles in full
text. Sixteen studies met the inclusion criteria and are included
in table I JJ. . We included 12 studies in the quantitative
meta-analysis. Excluded from meta-analysis were one study
that reported only mean numbers of exposures (numbers of
indoor tanning visits),
18
one study that grouped patients with
basal cell carcinoma, squamous cell carcinoma, and melanoma,
24
and two studies that grouped basal cell carcinoma and squamous
cell carcinoma together.2.
26
These last two studies also used
patients admitted to hospital with solid organ cancer as controls,
which are unlikely to be representative of the population from
which the cases arose.
23 26
All four studies showed
non-significant associations, although one showed a statistically
significant positive association when sunbed exposure was
grouped with medical phototherapy?
The 12 studies included in the meta-analysis were published
between 1985 and 2012, used data collected between 1977 and
2010 in six different countries, and included 80 661 total
participants and 9328 cases of NMSC. All 12 studies reported
or provided raw data for effect estimates as odds ratios or hazard
ratios (table 2Jj. ). When available, we preferentially present
effect estimates reported using multivariate models.
Effect estimates for ever exposure to indoor tanning compared
with never exposure were available for I 0 out of 12 studies. A
meta-analysis of these studies yielded summary relative risks
of 1.29 (95% confidence interval 1.08 to 1.53) for basal cell
carcinoma and 1.67 (1.29 to 2. 17) for squamous cell carci noma
(fig 2Jj.). A X
2
test for heterogeneity was non-signifi cant for both
basal cell carcinoma (P=0.14) and squamous cell carcinoma
(P=0.09); 1
2
statistics were 36.8% (95% confidence interval 0%
to 72%) for basal cell carcinoma and 47.1% (0% to 79%) for
squamous cell carcinoma. To include all available studies, we
did a sensitivity analysis using the effect statistics from alll2
studies, including the two studies that reported only higher dose
exposure. ''
28
Both studies considered only basal cell carcinoma;
with these two studies included, the summary relative risk for
basal cell carcinoma was 1.25 (1.01 to 1.55). Funnel plots
assessing publication bias were symmetrical for both basal cell
carcinoma and squamous cell carci noma, and all Begg' s and
Egger's tests were not statistically significant, suggesting that
publication bias was unlikely. Our results did not change
appreciably in a sensitivity analysis excluding four retrospective
studies that did not fully adjust for confounders.
14 19 21 27
To assess the presence of a dose-response effect, we did a
sub-analysis on studies that included effect estimates for frequent
or multiple (high dose) exposures to indoor tanning (table 3Jj.,
top). High dose exposure was associated with a relative risk of
1.50 (0.81 to 2.77) for basal cell carcinoma. To assess the
potential effect of exposure to indoor tanning at a young age,
we did a sub-analysis on studies that included effect estimates
for early life exposure (table 3U, bottom). Indoor tanning
exposure before age 25 was associated with a relative risk of
1.40 (1.29 to 1.52) for basal cell carcinoma and 2.02 (0.70 to
5.86) for squamous cell carcinoma.
Population attributable risk
Applying our summary risk estimates to the prevalence of
exposure to indoor tanning in the United States, we calculated
No commercial reuse: See rights and reprinls htlp11www.bmt.com/perm,ssJons
Page3 of 9
RESEARCH
the population attributable risk fraction at 3.7% for basal cell
carcinoma and at 8.2% for squamous cell carcinoma. This
corresponds to 98 408 cases of basal cell carcinoma and 72 244
cases of squamous cell carcinoma, making 170 652 cases of
non-melanoma skin cancer each year attributable to indoor
tanning (see supplementary figure).
Discussion
In this systematic review and meta-analysis of more than 9300
cases of non-melanoma skin cancer from 12 studies, we found
a positive, statistically significant association between exposure
to indoor tanning and NMSC. Ever exposure to indoor tanning
was associated with a 67% higher risk for squamous cell
carcinoma and a 29% higher risk for basal cell carcinoma.
Exposure to indoor tanning at a young age was signifi cantly
associated with an increased risk for basal cell carcinoma and
showed a non-significant increased risk for squamous cell
carcinoma. High dose exposure to indoor tanning showed a
non-significant increased risk for basal cell carcinoma. This
suggests a critical period for exposure during early life and a
potential dose-response effect.
Possible explanations for findings
A causal link between indoor tanning and NMSC is one possible
explanation for our findings. This link is biologically plausible,
because both ultraviolet A and ultraviolet B radiations are
established carcinogens in animal models and human studies.'
1 33
Several population based studies have documented rapid rises
in skin cancer among young women, coinciding with the
adoption of indoor tanning and supporting this causal
relation.g
35
The dose-response effect noted in several studies
further supports this argument.
20 29
The temporal relation in
which indoor tanning at a young age is a stronger risk factor
not only supports a causal interpretation but also implies a
critical period of higher susceptibility during early life.
Alternative explanations for these findings include the possibility
that these observational and mostly retrospective smdies were
confounded by skin type or outdoor exposure to ultraviolet
radiation. For example, fair skinned people who are more
susceptible to NMSC might use indoor tanning more often, and
indoor tanners may also get more outdoor ultraviolet exposure.
35
Because most of the studies included in the primary
meta-analysis (8/10) controlled for skin type or sun sensitivity
and many (5/10) controlled for outdoor ultraviolet exposure,
we do not feel that this confounding alone could account for
the significant associations observed. Also, differential recall
of use of indoor tanning in people already diagnosed as having
skin cancer is a concern in case-control studies. However, given
that prospective cohort studies found similar effect sizes, and
are heavily weighted in this meta-analysis, we do not think that
recall bias significantly affects our conclusion. Although they
are always a concern in literature based meta-analyses,
publication bias and small study effects are unlikely to fully
explain these fmdings on the basis of our analyses.
Comparison with other studies
These findings are consistent with a previous meta-analysis of
indoor tanning and NMSC, '
3
which, using only five studies,
found a significant increase in risk for squamous cell carcinoma
(summary relative risk 2.25, 95% confidence interval 1.08 LO
4.70) and a non-significant effect for basal cell carcinoma
(summary relative risk 1.03, 0.56 to 1.90). Our analysis, using
substantially more studies, found a similarly significantly
increased risk for squamous cell carcinoma and, notably, found
Subscribe: http://www.bmj.comlsubscrlbe
BMJ 2012;345:e5909 doi: 1 0.1 136/bmj.e5909 (Published 2 October 2012)
a significantly increased risk for basal cell carcinoma. Our
findings add to the growing body of evidence on the banns of
indoor tanning. Indoor tanning is already considered a class I
carcinogen on the basis of its effect on malignant melanoma.
11 12
Although NMSC is generall y not a lethal cancer, it affects a
vast number of people worldwide and accounts for a
considerable disease burden.
1 2 6 36
Although the population
attributable risk fraction of indoor tanning on NMSC is modest,
when applied to the 3.5 million new cases of NMSC diagnosed
each year, indoor tanning may account for hundreds of thousands
of new cases each year in the United States alone. Yet this is a
global problem: recent studies from Australia, France, Derunark,
Germany and Sweden suggest that 10.6-35% of people have
used a tanning bed at least once in their lives, and 1.3-29.9%
have done so in the previous year.37 >s J9 o 41 42 43
Limitations of study
This study is limited by the fact that it included only
observational and mostly case-control studies. However, a
randomised trial of indoor tanning is not realistic, and most of
the included studies controlled for multiple potential
confounders, making this the best level of evidence possible.
Another potential limitation of this meta-analysis is the broad
time period spanned by the data. Included studies collected data
from the 1970s to the 201 Os, which is important because indoor
tanning devices have changed over time from high ultraviolet
B output to predominately ultraviolet A output.
44 45 46
However,
multiple studies have indicated that both ultraviolet B and
ultraviolet A seem to be capable of causing significant
mutagenic damage to skin."
33 47
<&
Conclusions
Indoor tanning, which is already an established risk factor for
malignant melanoma, is probably a risk factor for both squamous
cell carcinoma and basal cell carcinoma, which are the most
common human cancers. We hope that these findings can
support public health campaigns and motivate increased
regulation to reduce exposure to this carcinogen, especially
during early life.
We thank Stephen Bent of the University of California San Francisco
and Emanuele Di Angelantonio of the University of Cambridge for their
assistance.
Contributors: MRW, M-MC, and EL were involved in the conception and
design of the study. MRW, MLS, and EL did the data collection and
analysis. MRW, MLS, M-MC, and EL interpreted the data. MRW and
EL drafted the manuscript, and all authors critically revised it for
important intellectual content. All authors approved the final version to
be published. EL is the guarantor.
Funding: This project was supported by award number KL2RR024130
from the National Center for Research Resources of the National
Institutes of Health, and by award number K24 AR052667 from the
National Institute of Arthritis and Musculoskeletal and Skin Diseases of
the National Institutes of Health. The study sponsors were not involved
in the study design and the collection, analysis, and interpretation of
data, nor the writing of the article or the decision to submit it for
publication. The authors were independent from the study sponsors.
Competing interests: All authors have completed the Unified Competing
Interest form at www.icmje.org/coi_disclosure.pdf (available on request
from the corresponding author) and declare: no support from any
organisation for the submitted work; MMC does consultancy for
Genentech; no other relationships or activities that could appear to have
influenced the submitted work.
Ethical approval: Not needed.
No commercial reuse: See rights and reprints http11www.bmr .com/permrssons
Page 4 of 9
RESEARCH
Data sharing: No additional data available.
Lomas A. LeonardiBee J, BathHextall F. A systematic review ol worklwide incidence of
nonmelanoma skin cancer. Br J Dermato/2012;166:106980.
2 Rogers HW, Weinslock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, et al.
Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermato/
2010:1 46:2837.
3 Miller DL. Weinstock MA. Nonmelanoma skin cancer in the United States: incidence. J
Am Acad Dermato/1994:30:774-8.
4 Chen JG, Fleischer AB Jr. Smith ED. Kancler C. Goldman NO, Williford PM, et al. Cost
ot nonmelanoma skin cancer treatment in the United Slates. Dermatol Surg
2001:27: 1035-8.
5 Housman TS, Feldman SR, Willfford PM, Fleisctler AB Jr, Goldman NO, Acostamadiedo
JM, et al. Sl<in cancer is among the mosl costly of all cancers to treat lor the Medicare
population. JAm Acad Derma/o/2003;48:4259.
6 Mudigonda T, Pearce OJ, Yentzer BA, Williford P, Feldman SR. The economic impact of
non-melanoma skin cancer: a review. J Nat/ Comp Cane Netw 201 0;8:888-96.
7 RoewertHuber J, LangeAsschenfeldt B, Stockfleth E, Kerl H. Epidemiology and aetiology
of basal cell carcinoma. Br J Dermatot2007;t 57(suppl2):4751.
8 Chri stenson LJ. Incidence of basal cell and squamous cell carcinomas in a populalion
younger lhan 40 years. JAMA 2005:294:68190.
9 Armstrong BK, Kricl<er A. The epidemiology of UV induced skin cancer. J Photochem
Photobiol 82001:63:8-18.
10 Wei-Passanese EX. Han J, Lin W, U T, Laden F. Qureshi AA. Geographical variation in
residence and risk of multiple nonmelanoma skin cancers in US women and men.
Photochem Photobio/20
11 El Ghissassi F, Baan R, Straff K, Grosse Y, Secretan B. Bouvard V, et al. A review of
human carcinogens- part 0: radiation. Lancet Onco/2009;1 0:751 2.
12 Gallagher RP, Spinelli JJ, Lee TK. Tanning beds, sunlamps. and risk of cutaneous
malignant melanoma. Cancer Epidemiol Biomarkers Prev2005;1 4:56266.
13 fnlemational Agency for Research on Cancer Working Group on Artificial Unraviolat (UV)
Light And Skin Cancer. The association of use of sunbads with cutaneous malignant
melanoma and other skin cancers: a systematic review. tnt J Cancer 2007;120:111622.
14 Asgari MM, While E, Warton EM, HaraJah MK. Friedman GO, Chren MM. Associati on
of tea consumpti on and cutaneous squamous cell carcinoma. Nutr Cancer2011 ;63:3148.
15 Aubry F, MacGibbon B. Risk factors of squamous eell carcinoma of the sl<in: a ease-con1rol
study in the Montreal region. Cancer 1985;55:90711.
16 Bajdik CD. Gallagher RP, Astrakianakis G, Hill GB, Fincham S, McLean Of. Non-solar
ultraviolet radiation and the ri sk of basal and squamous eell skin caneer. Br J Cancer
1996;73:16124.
17 Bakos AM. Kriz M. MuhlstMt M. Kunte C, Ruzid<a T, Ber1<ing C. Risk factors for early-onset
basal cetl carcinoma in a German instituli on. Eur J Dermato/201 1;21 :7059.
18 Boyd AS. Shyr Y, King LE Jr. Basal cetl carcinoma in young women: an evaluation of the
association of tanning bed use and smoking. JAm Acad Dermato/2002;46:7069.
19 Corona R, Dogliotti E, O'Errico M. Sera F. l avarone I, Saliva G, et al. Ri sk factors for basal
cell carcinoma in a Mediterranean population: role of recreational sun exposure early in
lffe. Arch Dermato/2001;137:1 1628.
20 Fenvoci L.M, Cartmal B, Molinaro AM, Leffell OJ, Bale AE, Mayne ST.Indoor tanning and
ri sk of early-onset basal cell carcinoma. JAm Acad Dermatol 2011; published online 8
Dec.
21 Goo A, Minelli L. Risk factors for basal cell carcinoma in a southern Brazilian population:
a ease-control study. lnt J Dermato/ 201 1;50:128690.
22 Han J , Colditz GA, Hunter OJ. Risk factors for skin cancers: a nested ease-control study
within the Nurses' Health Sludy. lntJ Epidemio/2006;35:151421.
23 Herity 8, O"Loughlin G. Moriarty MJ, Conroy R. Risk factors for non-melanoma skin cancer.
lr MedJ 1989;82:1512.
24 Hogan OJ, To T, Wilson ER, Miller AB, Robson 0, Holfeld K. et al. A study of acne
treatments as risk factors for skin cancer of the head and neck. Br J Dermatol
1991 ;1 25:3438.
25 Karagas MR. Stannard VA. Mott LA, Slattery MJ. Spencer SK, Weinstock MA. Use of
tanning devices and risk of basal cell and squamous cell skin cancers. J Nat/ Cane lnst
2002;94:2246.
26 O"Loughlin C, Moriarty MJ, Herity B, Daly L. A reappraisal of risk factors for skin carcinoma
in Ireland: a case control sludy. lr J Mad Sci 1985; 154:615.
27 Rosso S, Joris F, ZaneHi R. Risk of basal and squamous cell carcinomas of the skin in
Sion, Switzerland: a case-control sludy. Tumori 1999;85:43542.
28 Wallher U, Kron M, Sander S, Sebastian G, Sander R, Peler AU, el al. Risk and protective
factors for sporadic basal cell carcinoma: results of a two-centre case-control study in
southern Germany. Clinical actinic elastosis may be a protective factor. Br J Derma to/
2004:151:170-8.
29 Zhang M. Qureshi AA, Geller AC. Frazier L, Hunter OJ. Han J. Use of tanning beds and
incidence of skin J CJin Onco/ 2012;30:158893.
30 Moher D. Uberati A, Tetzlaff J,Aitman OG. Preferred reporti ng items for systematic reviews
and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535.
31 Von Elm E. Altman OG. Egger M, Pocock SJ. G0tzsche PC. Vandenbroucke JP.
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)
statement: guidelines for reporting observational studies. BMJ 2007;335:8068.
32 Heckman CJ, Coups EJ, Manne SL. Prevalence and correlates of indoor tanning among
US adulls. JAm Acad Dermato/2008;58:76980.
33 Council on Scienlffic Affairs. Harmful effects of ultraviolet radiation. JAMA 1989;262:3804.
34 Hausauer AK, Swetter SM, Cockburn MG, Clarke CA Increases in melanoma among
adolescent girts and young women in California: trends by socioeconomic status and UV
radiation exposure. Arch Dermato/ 2011 ;147:7839.
35 Purdue MP, Freeman LEB, Anderson WF, Tucker MA. Recent 1rends in incidence of
cutaneous melanoma among US Caucasian young adults. J Invest Dermstol
2008:128:29058.
36 Guy GP, Ekwueme OU. Years of potential life lost and indirect costs of melanoma and
non-melanoma skin cancer: a systematic review of the literature. Pl>armacoeconomics
2011 ;29:86374.
37 Francis K, Oobbinson S, Wakefield M, Girgis A. Solarium use In Australia, recent trends
and context. Aust N Z J Public Health 2010;34:42730.
38 Lawter SP, Kvaskoff M, OiSipio T, Whiteman 0. Eakin E, Ai tken J, et al. Solaria use in
Queensland. Australia. Aust N Z J Public Health 2006;30:479-82.
Subscribe: http://www.bmj.comlsubscrl be
BMJ 2012;345:e5909 doi: 1 0.1 136/bmj.e5909 (Published 2 October 2012) Page 5of 9
RESEARCH
What Is already known on this topic
Non-melanoma ski n cancer (NMSC) is the most common human cancer
Indoor tanning is a known risk factor for malignant melanoma, but the data on NMSC are less clear because small individual studies
have resul ted in varied effect estimates
What this study adds
Indoor tanning is associated with NMSC, especially when exposure occurs early in life
This modifiable risk factor accounts for hundreds of thousands of new cancer cases in the United States each year
More countries, including the United States, should follow in the footsteps of Europe, Australia, and Canada and restrict tanning bed
use for minors
39 Ezz.edine K, Matvy 0, Mauger E, Nageotte 0 , Galan P, Hercberg s. et at. Artificial and
natural ultraviolet radiation exposure: beliefs and behaviour of 7200 French adults. J Eur
Acad Dermatol Venereo/2008;22:18694.
40 Kester B, Thorgaard C, Philip A, Clemmensen I. Sunbed use and campaign initiatives in
the Danish population, 20072009: a cross-sectional study. J Eur Acad Dermatol Venereol
2011: published online 9 Jan.
41 Bomer FU, SchOlZ H. Wiedemann P. A populationbased survey on tanning bed use in
Germany. BMC Dermalo/2009;9:6.
42 Bofdema.n C, Branstrom R. Oat H, Kristjansson S, Rodvall Y, Jansson B. et at. Tanning
habits and sunbum in a Swedish population age 13-50 years. Eur J Cancer
2001 ;37:24418.
43 BranstrOm R, U118n H, Brandberg Y. AHitudes, subjective norms and percepti on or
behavioural control as predJctors of sun-related behaviour in Swedish adults. Prev Med
2004;39:9929.
44 Dilley BL. Farr PM. TaMing with UVB or UVA: an appraisal of risks. J Pholochem Photobk>l
B 1991 ;8:219.
45 Gerber B, Mathys P. Moser M, Bressoud D. Braun-Fahrlancfer C. Ultraviolet emission
spectra of sunbeds. Photochem Photobiol 2002;76:6648.
No commercial reuse: See rights and reprints http:ilwww.bml .com/perm,sslons
46 Nilsen LTN, Hannevik M, Aalerud TN, Johnsen B, Friberg EG, Veier0c1 MB. Trends in UV
irraciance of tanning devi<:es in Nol\vay: 19832005. Pltotochem Photobio/2008:84:1100-8.
47 Wang SO, Setl ow R. Berwick M, Polsky 0, Marghoob AA. Kopf AW, et al. Ultraviolet A
and melanoma: a review. JAm Acad Dermato/ 200 1 ;44 :837-46.
48 Hocker T, Tsao H. Ultraviolet radiation and melanoma: a systematic review and analysis
of reported sequence variants. Hum Muta/2007;28:57886.
Accepted: 28 August 2012
Cite this as: BMJ2012;345:e5909
This is an open-access article distributed under the terms of the Creative Commons
Al1ribution Non-commercial License. which permits use, distfibution, and reproduction in
any medium, provided the original work is properly cited, the use is non commercial and
is otherwise in compliance with the license. See: http:/lcreativecommons.org/licenseS!by
nc/2.0/ and http:itcreativecommons.orglllcenseS!byncf2.0negalcode.
Subscribe: hl1p:/lwww.bmj.comlsubscrlbe
BMJ 2012;345:e5909 doi: 1 0.1 136/bmj.e5909 (Published 2 October 2012) Page 6of 9
RESEARCH
Tables
Table 11 Summary of studies
Data
Reference Country, year of publication collection Diagnosis* Total No No of cases Age (years) %male Exposuret
Studies included in meta-analysis
Asgari et al " United States, 2011 200405 sec 830 415 43 85 619 Ever/never
Aubry and Canada, 1985 1977-78 sec 266 92 Unknown 65.8 Ever/never
McGibbon''
Bajdik et al'
6
Canada. 1996 1983-84 sec; sec 812 226 BCC; 180 2579 100.0 Ever/never
sec
Bakos et al" Germany, 2011 200408 sec 50 25 1940 40.0 "Regular"
exposure
Corona et al '
9
Italy, 2001 1995-97 sec 324 166 47.8 Ever/never
Ferrucci et ar United States, 2011 2006 10 sec 766 376 <40 30.8 Ever/never
Gon and Minelli
21
Brazil, 2011 2006-07 sec 407 127 18-80 41.7 Ever/never
Hanetal" United States, 2006 1989-98 BCC;SCC 1362 283 BCC; 275 43-68 0.0 Ever/never
sec
Karagas et al
25
United States, 2002 1993-95 sec; sec 1436 603 sec 293 25-74 59.5 Ever/never
sec
Rosso et al
21
Switzerland, 1999 1994-96 sec; sec 290 120 BCC; 25 2075 52.4 Ever/never
sec
Walther et al., Germany, 2004 199799 BCC 624 213 19-92 48.1 >5 exposures per
year:t
Zhang et al
29
United States. 2012 1989-2009 sec; sec 73494 5506 BCC; 403 25-62 0.0 Ever/never
sec
Studies not included in meta-analysis
Boyd et al '
6
United States, Unknown sec 60 30 20-40 0.0 No of exposures
2002
Herity et al" Ireland, 1989 1984-85 NMSC 792 202 BCC; 194 Unknown Unknown Ever/never
sec
Hogan et al"' Canada, 1991 1989 Skin 4820 791 BCC; 41 1056 37.3 Ever/never
sec; 1s MM ..
O'Loughli n et al"' Ireland, 1985 Unknown NMSC 242 sa sec: 63 sec Unknown 71 .9 "Often" exposed
*BCC=basal cell carcinoma; SCC=squamous cell carcinoma of skin; NMSC=non-melanoma skin cancer (BCC and SCC grouped together in publication); skin
cancer (malignant melanoma, sec, sec all grouped together i n publication).
tEver/never: measurement of ever exposure to indoor tanning compared with never exposure; "regular exposure: defined i n publication as "regular" exposure to
indoor tanning, with no further specifics; "often" exposed: defined in publication as "often" exposed to indoor tanning, with no further specifics.
:1:>5 exposures to indoor tanning per year compared with $5 exposures per year.
Ever/never comparison obtained directly from authors.
'tjSkin cancer of head and neck .
.. MM=malignant melanoma.
No commercial reuse: See rights and reprints http11www.bmt .com/perm.ssons Subscribe: http://www.bmj.comlsubscrl be
BMJ 2012;345:e5909 doi : 1 0.1 136/bmj.e5909 (Published 2 October 2012)
Table 21 Outcome effect sizes for studies included in primary meta-analysis
Odds ratio (95% Cf)
Reference Basal cell carcinoma Squamous cell carcinoma
Studies comparing ever exposure with indoor tanning to never exposure
Asgari et ai" 1.41 (0.90 to 2.22)
Aubry and McGibbon" 13.42 (1.38 to 130.48)
Bajdik et al'' 1.2 (0.7 to 2.2) 1.4 (0. 7 to2. 7)
Corona et ai " 0.6 (0.3 to 1.2)
Ferrucci et af 1.69 (1 .15 to 2.48)
Gon and Minelli" 0.31 (0.07 to 1.35)
Han et al
22
1.32 (0.87 to 2.03) 1.44 (0.93 to 2.24)
Karagas et al
25
1.5 (1 .1 to 2.1) 2.5 ( 1.7 to 3.8)
Rosso et al" 1.24 (0.53 to 2.88)
Zhang et al" 1.29 (1.22 to 1.35)ll: 1 .50 ( 1.20 to 1. 78):j::j:
Studies measuring higher dose exposure: "regul ar" exposure" or >5 exposures per year''
Bakos et al " 25.0 (2.26 to 277.36)
Walther et al
20
o. 7 (0.3 to 1.5)
Page 7 of 9
RESEARCH
Adjustments
None (crude)
Age, sex, eye and hair colour, ski n type, ethnicity,
sun exposuret
Age, (sex:j:), hair col our, skin type , ethnicity, sun
exposuret
Age, sex, skin type, sun exposuret, family history
of skin cancer
Age, sex. body site, skin type, sun sensitivity, family
history of skin cancer, melanocortin 1 receptor gene
non-synonymous variants
Age, sex, eye colour, hair colour, skin type, family
history of skin cancer, presence of actinic keratosis
Age, (sex:j:), sun exposuret, sun sensitivity, history
of severe sunburns1J, geography ... family history of
skin cancer
Age, sex, sun sensitivi tytt
Age, sex
Age, (sex:j:), hair colour, sun exposuret, sun
sensitivity, history of severe sunburns1J,
geography .. , number of moles on legs, family history
of melanoma
Sunscreen use, parents' sunscreen use, smoking
None (crude)
"Skin type: complexion (Aubry and McGi bbon), skin colour (Bajdik et al, Ferrucci et al), pigmentary traits (Corona et al).
tSun exposure: non-occupational sun exposure (Aubry and McGibbon) , lifetime occupational sun exposure (Bajdik et al) , number of weeks spent at beach before
age 20 and outdoor work (Corona et af), cumulative sun exposure while wearing bathing suit (Han et al) , outdoor sun exposure (Zhang et al).
:j:Study not adjusted for sex because only included one sex.
Skin sensitivity to sun: skin response to fi rst exposure of season to 1 hour of summer sun and to prolonged exposure to sun (Ferrucci et al), constitutional
susceptibility score (Han et al) , sun sensitivity (Karagas et al), childhood tendency to sunburn (Zhang et al).
of severe sunburns: lifeti me sunburns which blistered (Han et al), number of severe sunburns between 15 and 20 (Zhang et al) .
.. Geography: geographic region at baseline (Han et al), ultraviolet index in area of residence at bi rth and 15 and 30 years of age (Zhang et al).
ttAdjusted for age and sex in basal cell carcinoma analysis because adjustment for sun sensitivity did not change results.
:j:Hazard ratio (95% Cl), obtained directly from authors.
No commercial reuse: See rights and reprints http11www.bmJ.COm/perm,ssons Subscribe: http://www.bmj.comlsubscrl be
BMJ 2012;345:e5909 doi: 1 0.1 136/bmj.e5909 (Published 2 October 2012) Page8of 9
RESEARCH
Table 31 Outcome effect sizes for studies included in subset analyses of high dose exposure and young age at exposure
Odds ratio (95% Cl)
Reference Exposure/age Basal cell carcinoma Squamous cell carcinoma
Studies assessing high dose exposure to indoor tanning
Bakos et al" "Regular use of tanning beds in lifetime" 25.0 (2.26 to 277.36)
Ferrucci et at 6-26 years of "regular"' exposure 2.16 (1.34 to 3.48)
Walther et al"" >5 exposures per year 0.7 (0.3 to 1.5)
Zhang et al" 4 exposures per year 1.15(1.11 to 1.19)' 1.15 (1 .01 to 1.31)*
Summary relative risk 1.50 (0.81 to 2.77)
Studies assessing young age at exposure to indoor tanning
Ferrucci et at> ~ 6 years of age 1.83 (1.12 to 2.97)
Karagas et al
25
<20 years of age 1.8 {1.0 to 3.0) 3.66 (1 .9 to 6.9)
Zhang et al
29
"High school/college 1.38 (1 .27 to 1.5)t 1.21 (0.85 to 1.71 Jt
Summary relative risk 1.40 (1 .29 to 1 .52) 2.02 (0.70 to 5.86)
Hazard ratio (95% Cl).
t Hazard ratio (95% Ct) obtained directly from authors.
No commercial reuse: See rights and reprints http11www.bmt .com/perm,sslons Subscribe: http://www.bmj.comlsubscrl be
BMJ 2012;345:e5909 doi: 1 0. 1136/bmj.e5909 (Published 2 October 2012)
Figures
Total records identified through database searches (n929):
PubMed (n303) Embase (n368) Web of Science (n258)
l
Records after duplicates removed (nSSO)
Additional records identified by hand search (n=8)
Records screened by title and abstract(nSS8)
Records excluded (nS36):
Not relevant (n416)
Reviews/ editorials (n110)
Language otherthan English (nlO)
Full text articles assessed for etigiblllty (n-22)
Records excluded (n6):
No effect statistic possible (1 ecological analysis, 1 study using only NMSC cases) (n2)
Incorrect exposure (1 grouped Indoor tanning with overall ultraviolet exposure,
1 assessed medical ultraviolet treatments) (n2)
Duplicate study population (n1)
Mathematical model (nl)
Studies included in qualitative synthesis (n-16)
Studies excluded (o4):
Compared mean numbers of exposures (nl)
Grouped sec, sec, and melanoma (n=1)
Grouped BCC and SCC (n2)
Studies included in quantitative synthesis (meta-analysis) (n12)
Page9 of 9
RESEARCH
Fig 1 PRISMA flow diagram of literature search and study selection for meta-analysis of indoor tanning and non-melanoma
skin cancer. BCC=basal cell carcinoma; NMSC=non-melanoma skin cancer; SCC=squamous cell carcinoma
No exposed/ No In group
Study Cases Controls Odds rati o or Odds ratio or
hazard ratio hazard ratio
Bas a I cell caret noma
(95%CI) (95%CI)
Bajdik 1996 23/226 33/ 404 1.20 (0.70 to 2.20)
Corona 2001 17/161 31/1 54 0.60 (0.30 to 1.20)
Ferrucci 2011 246/375 245/382 1.69 (1.1510 2.48)
Goo and Minelli 2011 3/127 25/280 0.31 (0.0710 1.35)
Han 2006 44/ 259 87/712 1.32 (0.8710 2.03)
Karagas 2002 127/601 75/539 t.so (1.10 to 2.1 o)
Rosso 1999 10/ 120 9/144 1.24 (0.53 to 2.88)
Zhang 2012 617/5494 1.29 (1.22 to 1.35)
Summary 1.29 (1.08 to 1.53)
Squamous cell carci noma
Asgari 2011 49/ 415 36/415 1.41 (0.90 to 2.22)
Aubrey and McGibbon 1985 4/ 92 l/174 13.42 (1.38 to 130.5)
Bajdik 1996 18/180 33/404 1.40 (0.70 to 2.70)
Han 2006 41/ 253 87/712 1.44 (0.9310 2.24)
Karagas 2002 63/292 75/539 2.50 (1.70 to 3.80)
Zhang 2012 36/402 1.50 (1.20 to 1.78)
Summary 1.67 (1.29 to 2.17)
0.04 0.1 0.33 1 3 10 25
Fi g 2 Relative risk of basal cell carcinoma and squamous cell carcinoma in participants ever exposed to indoor tanning
compared with participants never exposed to indoor tanning
No commercial reuse: See ri ghts and reprints http11www.bmt .com/perm,sslons Subscribe: http://www.bmj.comlsubscrl be
I
Compliance with restrictions on sale of indoor tanning
sessions to youth in Minnesota and Massachusetts
Jean L. Forster, PhD," DeAnn Lazovich, PhD," Andrea Hickle, MPH,b Glorian Sorensen, PhD,c
and Marie-France Demierre, MDd
Minneapolis, Minnesota, and Boston, Massachusetts
Background: Minnesota and Massachusetts require parental permission, for persons younger than 16 or
18 years of age, respectively, for indoor tanning.
Objectives: This report examines business practices and characteristics associated with sales of indoor
tanning to underage girls.
Methods: Fifteen-year-old girls tried to purchase an ultraviolet tanning session in 200 indoor tanning
businesses in the Minneapolis-St Paul and Boston areas without parental consent. Business characteristics
were recorded. Later, businesses were interviewed by telephone about their facilities and practices.
Resulls: Eighty-one percent of businesses sold a session to an underaged buyer on at least one of two tries.
Illegal purchases did not differ by state. Businesses least likely to sell were larger, dedicated to indoor
tanning, required employee certification, and had a minimum age of sale for their business. However,
businesses in each of these categories still sold tanning sessions to underaged adolescents at 44% to 62% of
the visits. Employees who requested parental consent or age identification almost never sold a session.
Limitations: Businesses in Minnesota and Massachusetts only were included.
Co11clrtsiot1: Minnesota and Massachusetts laws specifying a minimum age of sale for indoor tanning are
ineffective. (]Am Acad Dennatol 2006;55:962-7.)
R
ecent studies that encompass the modern
indoor tanning era provide evidence that
melanoma increases with regular use of
indoor tanning, especially among younger per-
sons.1.2 In light of these findings and other health
risks, national and inte rnational health organizations
From the Division of Epidemiology & Community Health" and the
Center for Public Health Education & Outreach, b University of
Minnesota, Minneapolis; t he Department of Society, Human
Development, and Health, School of Public Health, Harvard
University, Boston<; and the Department of Dermatology,
Boston University School of Medicined
Supported by grant R01 CA079593 from the National Institutes
of Health.
Conflicts of interest: None identified.
Accepted for publication June 4, 2006.
Reprint requests: Jean L. Forster, PhD, University of Minnesota,
Division of Epidemiology & Community Health, 1300 S Second
St, Suite 300, Minneapolis, MN 55454. E-mail: f orster@epi.umn.
edu.
Published onli ne August 14, 2006.
0190-9622/ $32.00
2006 by t he American Academy of Dermatology, Inc.
doi:l 0.1 016/j.jaad.2006.06.036
962
recommend avoiding all sources of ultraviolet radi-
ation. 3-5 However, the indoor tanning industry in the
United States is a multibillion dollar enterprise.
6
A
2002 statewide survey of Minnesota adults found that
45o/o of \vomen (76o/o of women 25-34 years of age)
and 30% of men had ever used an indoor tanning
device.
7
A recent review of indoor tanning use
among adolescents found that prevalence ranged
from 2% to llo/o among boys and from 12% to 37%
among girls between the ages of 11 and 18 years in
the United States.s Among 14- to 17-year-olds in the
Minneapolis-St Paul metropolitan area, 12% of boys
and 42% of girls reported tanning indoors
9
The Food and Drug Administration and the US
Federal Trade Commission regulate indoor tanning
business practices. The Food and Drug Administra-
tion regulations cover equipment specifications,
exposure schedules, use of eyewear, and warning
statements, whereas the Federal Trade Commission
prohibits deceptive advertising of health benefits
from indoor tanning
10
11
In addition, 21 states reg-
ulate access of minors to indoor tanning.
12
1.
3
All 21
states require written pare ntal consent to tan if the
) AM ACAD DRMATOL
VOLUME 55. NUMBER 6
person is younger than 16 or 17 years of age. Eight
of these states require that a parent also accompany
minors under the age of 14 ro 18 years. Six states impose
a minimum age at which adolescents are allowed to
use indoor tanning facilities (generally age 14).
Minnesota and Massachusetts both have state laws
that regulate indoor tanning businesses. Massachu-
setts state law requires that municipalities license
tanning businesses and that they inspect them twice
annually, and the law specifies penalties for viola-
tions.
14
Minnesota law includes no requirements for
licensure and provides no penalties or enforcement
mechanism or authority.
15
Both states require pa-
rental permission to tan. In both states a parent or
guardian must sign a required warning statement in
person, witnessed by an employee, before the
initial tanning session of the adolescent (age 16 years
in Minnesota, age 14-17 in Massachusetts). Those
younger than 14 years of age must be accompanied
by a parent each time by law in Massachusetts.
A limited number of studies in the past 10 years
have assessed tanning business compliance with
state restrictions on age of sale. A phone survey of
businesses in the San Diego, California area included
a question about whether a hypothetical IS-year-old
sister would be permitted to tan. More than 57% of
the businesses agreed without mentioning parental
permission, in violation of California state law.
16
Another study, also in San Diego, compared the
results of a telephone interview by a minor to visits to
the same tanning businesses by a minor. In this study
the minor told the employee (on the phone or in
person) that she was 15 years old and had never
tanned before and asked the employee if a parent
needed to sign something before she tanned.
Compliance with the California state law was higher,
with 64.3% (in person) and 69.5% (on the phone) of
businesses requiring parental permission compared
with the earlier San Diego study.
17
Another study
used telephone surveys of businesses in 4 states
(Texas, Illinois, and Wisconsin, which regulate age
of sale for indoor tanning, and Colorado, which has
no requirement). Tanning business employees were
asked if a 12-year-okl or a 15-year-old person would
be allowed to tan and if parental permission was
required. Businesses in the regulated states were
more restrictive than Colorado, with Wisconsin
businesses being the most restrictive, consistent
with their strong state regulation.
18
The methodolo-
gies for each of these studies included direct ques-
tions about age of sale and thus do not directly
measure business behavior when not prompted to
think about this issue. Therefore actual compliance
with the state law by the businesses may be
overestimated.
Forste1" et a! 963
In the Minnesota and Massachusetts Indoor
Tanning Study, adolescent girls aged 15 years, who
are required by law in each state to provide parental
consent to tan indoors, visited 200 indoor tanning
businesses in the Minneapolis-St Paul and Boston
metropolitan regions to attempt to purchase a tan-
ning session without parental consent and without
volunteering their age. These businesses were later
interviewed about their facilities and practices by
telephone. The purpose of our report is to examine
which business practices and characteristics were
associated with the likelihood of a successful pur-
chase attempt.
METHODS
Sample selection
Tanning businesses in the Minneapolis-St Paul
and Boston metropolitan areas were identified
through Yellow Pages, Dun & Bradstreet, and
American Business Disc as well as through environ-
mental health officials at local health departments.
Businesses in Minneapolis-St Paul were also found
through the Office of the Secretary of State. A total of
358 businesses in the Minneapolis-St Paul area and
138 in the Boston area were enumerated, and the list
for each area was randomly sorted before screening
for eligibility. Starting at the top of each list, one staff
person in each of the metropolitan areas called each
business to ask if the business was (1) open to the
public, (2) accepted walk-in customers, and (3) sold
single tanning sessions. If the business responded
"yes" to all 3 questions, they remained in the study
sample; otherwise, we replaced the business with
another eli gible business until 100 eligible busi-
nesses in each location were obtained.
Data collection
Each husiness was visited on two occasions,
approximately 2 weeks apart, by a 15-year old girl
posing as a customer (the buyer). Nine adolescents
conducted the assessments; no business was visited
twice by the same buyer. The buyers were all non-
Hispanic white. Buyers followed a script, were given
cash to purchase a tanning session, and carried state-
issued photo identification with correct date of birtl1.
They were instructed to answer honestly all ques-
tions posed by the employee. Tf sold a session, the
buyers paid cash for it, entered the tanning room to
observe signage, and after a few minutes, left the
business without tanning, usually offering that they
had received an urgent call on their cell phone
and had to leave. Upon returning to the car where
the adult driver waited, the buyers completed a sur-
vey that included questions about the success of the
purchase attempt, whether age eligibility was
964 Forster et at
assessed (ie, the employee asked age, asked for
date of birth, and/ or asked for age identification),
whether parental consent was requested, and char-
acteristics of the employee (gender, age). The buyers
also recorded business practices, such as whether
they were asked to sign a warning statement,
whether the employee inquired about propensity to
burn or medications, if the employee made recom-
mendations for length or frequency of tanning ses-
sions or how to use the bed, availability of goggles,
and evidence of signs (warnings, sanitation). These
business practices could be collected only if a session
had been purchased. The underaged buyers asked
no questions about non-ultraviolet tanning.
On the second business visit, the adult drivers
(n = 9) who had accompanied the buyers to the site
but had remained in the car during the buyers' visits
also entered the business as future customers. The
drivers proceeded to ask the employee questions
about knowledge of health risks and business prac-
tices. Health and safety questions included whether a
base tan protects against sunburn, whether tanning
devices are safe, and if indoor tanning could cause
sunburns or skin cancer. Responses could range
from an affirmative or qualified response (it de-
pends) to a negative or unknown response (em-
ployee did not know or driver did not ask). These
items were coded so that a high score indicated
correct knowledge of health and safety (range 1 to 4;
if unknown, the response for that item was set to
missing). We then created a health and safety knowl-
edge score by taking the mean across items for which
a response was provided. The drivers also recorded
employee responses to 5 recommended business
practices, including how often to tan, how to termi-
nate a session, whether the business or customer
cleaned the beds, and if the business required and/ or
provided goggles. For each response that was in
compliance with state regulations, a point was given
and summed to create a responsible business prac-
tices score. The proportion of correct responses in
relation to the number of questions actually asked by
the drivers was calculated (drivers did not always ask
every question). For these two summary measures,
businesses were grouped into high and low cate-
gories according to the median value for each
measure.
After completion of the business visits, we at-
tempted to interview the owner or manager for each
of the 200 businesses by telephone. Two businesses
no longer provided tanning services at the time of
the interview, 19.7% refused to participate, and, for
11 .6%, the manager was never reached, leaving 136
businesses with a completed telephone interview
(64 in Minnesota, 72 in Boston). We asked the
J AM ACAD 0 ERMATOL
DECEMBER 2006
responsible individual to provide us information on
the number of years they had been with that business
and how long the business had been in operation,
whether the business was part of a chain, the number
of tanning units, the number of employees and the
percentage under 18 years of age, and the percent-
age of their customers that come for tanning (as
opposed to other services, such as hairstyling cuts).
We also inquired about associations to which the
business belonged, requirements for employee train-
ing and the elements of the training, employee
certification, percentage of time that a manager is
on the premises, a sy::;tem of monitoring employee
compliance with business rules, knowledge of local
ordinances, and licensure to operate. Business pro-
motional practices were also obtained. We collected
those practices required by law including placement
of warning signs, provision of free goggles, equip-
ment maintenance and sanitation, rules for teen-
agers, and whether the businesses had ever been
inspected.
All data collection methods were reviewed and
approved by the Human Subjects' Committees of
the University of Minnesota and Harvard University
School of Public Health.
Statistical analysis
We compared the likelihood that the buyer's
purchase attempt was successful for businesses
with and without the characteristic of interest as
reported by the business, or observed by the buyer
or driver. Logistic regression was used to calculate
odds ratios and 95% confidence intervals, taking into
account the clustering of buyers and drivers within
each city and repeated visits to each business.
Characteristics associated with a successful purchase
attempt did not differ by city; therefore we adjusted
for city in all analyses, treating it as a fixed effect.
RESULTS
Among the 100 businesses in Massachusetts and
the 100 businesses in Minnesota visited twice by
adolescent buyers, 81% sold a tanning session to the
adolescent buyer on at least one visit, whereas 57%
sold a session to the buyers on both visits; 69% of
al l purchase attempts were successful (n = 400).
Businesses participating in the telephone interview
(n = 136) ::;old a tanning session more often than
those that did not (76% vs 65%; P = .07). Businesses
in Minnesota and Massachusetts were equally likely
to sell a tanning session to the adolescent buyers.
The average cost of a single tanning session in the
businesses where attempts were successful was
$6.00; sessions were slightly more expensive in
Massachusetts ($6.12) than in Minnesota ($5.91).
) AM ACAD DRMATOL
VOLUME 55. NUMBER 6
Table T presents the business characteristics as
reported by the business that are associated with the
likelihood of a successful purchase attempt. Larger
businesses and those dedicated to indoor tanning
were less likely to sell tanning sessions to underaged
adolescents than businesses with fewer beds or
those whose prima1y business was not indoor tan-
ning. Staff ce1tification of training to provide indoor
tanning services, particularly when both the man-
ager and employees had been certified, also led to
fewer s uccessful purchase attempts, as did industry
association membership. Among businesses that
reported having adolescent customers, those with a
mini mum age or a parental consent requirement
were much less likely than those without these
requirements to allow the adolescent buyer to pur-
chase a tanning session. Even so, the probability of a
successful purchase attempt ranged from 46.1% to
61.5% for businesses reporting these requirements.
Table TT reports the association between business
characteristics and practices observed by the buyers
and drivers and sales to underage buyers. Only 8
businesses asked the buyer for age identification on
one visit; only one business asked for identification
on both visits. Although the probability of a success-
ful purchase attempt was lowest among these busi-
nesses, just asking about age or date of birth also
greatly reduced the likelihood of a successful pur-
chase attempt relative to those businesses that did
not check age eligibility by any method (49.7% vs
98.3%). Empl oyees who told the adolescent that
parental consent was needed almost never sold a
session to the buyers ( < 1% of attempts successful)
compared with almost universal success among
businesses that did not mention the requirement
(95.8% successful). Employees perceived by the
buyer to be younger than 18 years of age or who
were male were more likely to sell sessions to the
buyers (all female) . Although employee compliance
with a higher percentage of responsible business
practices or greater employee knowledge of health
and safety for indoor tanning, as observed by the
driver, were associated with a lower likelihood
of a successful purchase attempt, neither measure
achieved statistical significance.
Limitations
Chief among the limitations of this study is the
possible bias introduced by activities of the tanning
industry associations. When the associations became
aware of our study, they sent letters to tanning
businesses recommending that they not participate
in the telephone interview. The 68% of business
representatives who agreed to the interview are
those who either did not get the letter before the
Forste1" et a! 965
Table I. The likelihood of a successful purchase
attempt according to business characteristics and
practices reported by 136 tanning business
managers who completed telephone survey
% Purchase
attempt
Characteristics No. ORt
No. of tanning
units
1-2 32 80.7 1.00
3-5 26 79.1 0.92
6-10 51 60.5 0.37
10+ 27 44.6 0.19
P trend < .0001
Percentage of
customers
who tan
< 50% 47 77.9 1.00
50%-99% 32 63.8 0.50
100% 48 53.4 0.33
P trend .0003
Staff certification*
Neither manager 54 74.2 1.00
nor employees
Manager or 26 57.8 0.48
employees,
not both
Both manager 31 52.9 0.39
and employees
P trend .OS
Belongs to an industry
association
No 87 73.7 1.00
Yes 45 51.2 0.37
Minimum age
requirement
No 80 69.5 1.00
Yes 19 46.1 0.37
Requires parental
consent
No 13 86.4 1.00
Yes 86 61.5 0.27
Cl. Confidence interval; OR, odds ratio.
*Represents number of individual businesses.
t Adjusted for city (Boston vs Minneapolis).
95%CJ
(0.32, 2.65)
(0.16, 0.87)
(0.07, 0.51 )
(0.22, 1.13)
(0.16, 0.68)
(0.21, 1.09)
(0.18, 0.86)
(0.20. 0.69)
(0.16, 0.88)
(0.07, 1.01)
*Asked only of businesses report ing t raining for employees.
Asked only of businesses that reported serving minors.
interview or who chose to disregard the industry
advice. In addition, the study includes only metro-
politan Boston and Mi nneapolis-Sl Paul tanning
businesses; therefore it is possible that a generaliza-
tion of the results outside these two areas of the
United States cannot be made. finally, adolescent
buyers were instructed not to lie about their age or in
any other way to act older or disguise their age,
strategies that might be used by teens intending to
tan. Despite those constraints, the buyers had no
966 Forster et at
Table n. Likelihood of a successful purchase
attempt according to business characteristics
and practices observed by adolescent buyer
and adult driver
Characteristics
Adolescent buyer
observation
Employee gender
Female
Male
Perceived
employee
age (y)
> 25
18-25
< 18
Age eligibility
Did not assess
Asked age, no
ID checked
ID checked
Told that parental
consent needed
No
Yes
Adult driver
observation
Responsible
business
practices*
Low
High
Knowledge of
health and
safety
Low
High
<yo
Purchase
attempt
No. successful ORt
317 66.5 1.00
95%Cl
83 78.3 1.80 (1.01, 3.23)
216 67.8 1.00
156 67.8 1.01 (0.64, 1.59)
27 83.9 2.51 (0.91, 6.92)
162 98.3 1.00
228 49.7 O.Ql (0.003, 0.05)
10 35.2 0.01 (0.001, 0.04)
267 95.8 1.00
123 0.9 0.004 (0.002, 0.009)
192 72.4 1.00
204 66.2 0.69 (0.39, 1.20)
214 72.9 1.00
182 63.7 0.64 (0.38, 1.08)
Cl, Confidence interval; OR, odds ratio.
*Represents number of buys, since the characteristic assessed
could differ from buy to buy within a business; however, analysis
was performed at the business level.
t Adjusted for city and individual confederates (buyer or driver
depending on source of information).
*Calculated as percentage of business-reported compliance for
those practices that the driver recorded (up to 5 practices total).
Calculated as the mean of the score across each of 4 knowledge
items.
trouble purchasing sessions, and our results likely
underestimate actual ease of purchase by minors.
DISCUSSION
The rate of sales of tanning sessions to 15-year-old
girls in this study was high (81%). Age was not
assessed in more than 40% of the attempts, and,
J AM ACAD 0 ERMATOL
DECEMBER 2006
when not. assessed, sale to underaged girls was
almost universal. It is important to emphasize that
even among businesses with characteristics associ-
ated with higher compliance relative to the other
categories, the sales rate was high in absolute terms.
The only practice that produced acceptable compli-
ance rates was asking for parental permission (99%
compliance).
We were surprised to find no differences in
sales to underaged buyers between Minnesota and
Massachusetts, despite the more restrictive regula-
tion of indoor tanning businesses in Massachusens.
Although the restrictions on youth access and other
requirements of the Ia ws are very similar in the two
states, Massachusetts state law requires licensure
and annual inspections and specifies penalt ies for
noncompliance, whereas Minnesota law does not
include enforcement provisions or penalties.
14
15
A previous rep01t showed that although environ-
mental health speciali sts repo1ted more regular in-
specti ons of tanning businesses in Massachusetts
compared with Mi nnesota, environmental health
specialists in both states reported less specific knowl-
edge of and attention to youth access provisions in
the state law compared with other areas covered by
the state laws.
19
The businesses in this study actually performed
worse than those in most previous studies where
compliance with youth access laws was assessed.
16
"
18
Differences in methods for assessing business
compliance may account for much of that difference,
since asking businesses about their practices by
telephone raises the issue directly and their results
may reflect social desirability. Indeed, 46% of the
businesses that told us on the phone that they had a
minimum age for tanning sold a session to underage
buyers, as did 62% of the businesses that in the
telephone interview stated that they required paren-
tal consent. Although our buyers did not lie about
their age and carried identification giving their
correct age, they did not bring the issue up either,
in contrast to the study by Hurd et al/
7
possibly
reflecting more closely the practices of underaged
teenagers seeking to tan. Undoubtedly, state differ-
ences do occur, as Hester et al
18
discovered when
comparing 4 states in which businesses were chal-
lenged with the same protocol.
Organizations representing the tanning industry
officially encourage in training materials that busi-
nesses require parental consent or parent presence
for adolescents to tan
6
20
Indeed, businesses in our
study that reported belonging to an industJy associ-
ation, pa1t icipating in a staff certification program, or
havi ng an established minimum age of sale were less
likely to sell to the study confederates. However,
) AM ACAD DRMATOL
VOLUME 55. N UMBER 6
purchase attempts were still successful about half the
time for businesses with these characteristics. This
may be due, in part, to the inherent conflict between
industry support for compliance and industry mar-
keting strategies that include targeting high school
students (offering free sessions to social role models,
employing teenagers, holding drawings for concert
tickets, making donations to high school sports
teams), and for maintaining young customers who
tan primarily before an event such as tbe prom.
21
-
24
The scenarios most likely to result in a sale to an
underaged buyer are strikingly similar to those
leading to sales of tobacco to minors. In both cases
male employees are more likely to sell than female
employees, younger employees are more likely ro
sell than older employees, and checking age identi-
fication rarely results in a sale to an underaged
buyer.
25
In fact, access of adolescents to indoor
tanning mirrors the situation of tobacco sales to
minors several years ago, with illegal sales almost
ubiquitous, and social norms not proscribing illegal
use
2 6
Tobacco sales to minors have declined dra-
matically over the past decade in many parts of the
country because of several factors, all of which are
more likely to lead to a request for age identification
by clerks.
25
27
Stronger state and local laws that
specify enforcement authority and penalties and
fund enforcement could motivate tanning businesses
to change their practices in a similar fashion.
To conclude, our data show that when the age of
adolescents is not assessed, illegal sale of indoor
tanning is al most universal. Significant work needs
to be done at the individual and communi ty levels
to change the social norms around having a tan, to
reduce opportunities ro ran indoors by changing
policies and business practices, and to educate
community members about the serious risks of
indoor tanning.
We rhank Ms Natania Rernba and the adolescents and
adults who assisted with the purchase attempts.
REFERENCES
1. Westerdahl J, lngvar C, Masback A, Jonsson N, Olsson H. Risk
of cutaneous malignant melanoma in relation to use of
sunbeds: further evidence for UV-A carcinogenicity. Br J
Cancer 2000;82:1 593-9.
2. Veierod MB, Weiderpass E, Thorn M, Hansson J, Lund E,
Armstrong B, et al. A prospective study of pigmentation, sun
exposure, and risk of cutaneous malignant melanoma in
women. J Nat l Cancer lnst 2003;95:1530-8.
3. Saraiya M, Glanz K, Briss P, Nichols P, White C, Das D.
Preventing skin cancer: findings of t he Task Force on Com-
munity Preventive Services On Reduci ng Exposure to Ultra-
violet Light. MMWR Recomm Rep 2003;52(RR- 15):1-1 2.
Forste1" eta! 967
4. Cancer prevention and early detection facts & figures. Atlanta:
American Cancer Society; 2004.
5. World Health Organization. Art ificial tanning sunbeds- risks
and guidance. Geneva: World Health Organization; 2003.
6. Indoor Tanning Association. ITA Estimates Industry Overview
2004. Available at : http://www.t heita.com/ pdf/estimates.pdf.
Accessed Feb 4, 2005.
7. Lazovich D, Sweeney C, Forster J. Prevalence of indoor tanning
use in Minnesota, 2002. Arch Dermatol 2005;141 :523-4.
8. Lazovich D, Forster J. Indoor t anning by adolescents: preva-
lence, practices and policies. Eur J Cancer 2005;41:20-7.
9. Lazovich D, Forster J, Sorensen G, Emmons K, Stryker J,
Demierre MF, et al. Characteristics associated with use or
intention t o use indoor tanning among adolescent s. Arch
Pediatr Adolesc Med 2004;1 58:918-24.
10. Federal Trade Commission. Policy Statement on Deception.
Available at: http://www.ftc.gov/bcp/policystmt/ad-decept.htm.
Accessed May 30, 2003.
11. Medications t hat increase sensitivity to light: a 1990 listing.
Washington (DC): US Department of Health and Human
Services; 1990. HHS Publication FDA 91 -8280.
12. Dellavalle RP, Parker ER, Cersonsky N, Hester RJ, Hemme B,
Burkhardt JD, et al. Yout h access laws? In t he dark at the
tanning salon? Arch Dermatol 2003;139:4438.
13. Francis SO, Burkhardt DL, Dellavalle RP. 2005: A banner year
for new US youth access tanning rest rict ions. Arch Dermatol
2005;141 :524-5.
14. Massachusetts statutes. Tanning facilities. 105SMRVol123; 1994.
1 5. Minnesota statutes. Regulat ion of tanning facilities. 325H;
1993.
16. Culley CA, Mayer JA, Eckhardt L, Busic AJ, Eichenfield LF, Sallis
JF, et al. Compliance with federal and state legislation by
indoor tanning facilities in San Diego. J Am Acad Dermatol
2001 ;44:53-60.
17. Hurd AL, Mayer JA, Woodruff 51, Belch GE, Pat el MR.
Comparing two methods of measuring legislation compli-
ance among indoor tanning facilities. J Am Acad Dermatol
2006;54:433-9.
18. Hester EJ, Heilig LF, D'Ambrosia R, Drake AL, Schill ing LM,
Dellavalle RP. Compliance with youth access regulations for
indoor UV tanning. Arch Dermatol 2005;141:95962.
19. Hickle A, Forst er J, Lazovich D, Allwood P, Remba N,
Grossmeier J, et al. Sanitarians' work wit h indoor-tanning
businesses: findings f rom interviews in two major metropol-
itan areas. J Environ Health 2005;67:306, 54.
20. International Smart Tan Network Manual. 5th ed. Jackson (MI):
International Smart Tan Network; 1998.
21. Barrett SA. Profitable spring. Looking Fit 2002;17:86-8.
22. Edvardsen L. Making advertising work for you. Tanning Trends
2003;18(3):91-6.
23. Barrett SA. Sell ing st rategies: holding on t o prom tanners.
Looking Fit 2003;18(4):64-8.
24. Freeman S, Francis S, Lundahl K. Bowland T, Dellavalle RP.
UV tanning advert isement s in high school newspapers. Arch
Dermatol 2006;142:460-2.
25. Forster JL, Wolf son M. Youth access to tobacco: policies and
polit ics. Annu Rev Public Health 1998;19:203-35.
26. Stryker JE, Lazovich 0, Forster JL, Emmons KM, Sorensen G,
Demierre MF. Maternal/ female caregiver influences on ado-
lescent indoor tanning. J Adolesc Health 2004;35:528.e 1-9.
27. DiFranza JR, Dussault GF. The federal initiative to halt t he sale
of tobacco to children-the Synar Amendment, 19922000:
lessons learned. Tob Control 2005;14(2):93-8.
Compliance With Youth Access Regulations
for Indoor UV Tanning
Eric]. Hester, MD; Lauren F. Heilig, BA; Renee D'Ambrosia, MD; Amanda L Drake, BS;
Lisa M. Schilling, MD; Robert P. Dellavalle, MD, PhD, MSPH
Obiectives: To describe youth access to indoor UV tan-
ning and youth discount pricing incentives in 4 states with
different age restrictions: Colorado (no age restric-
tions), Texas (age l3 years), Illinois (age 14 years), and
Wisconsin (age 16 years).
Design: Cross-sectional telephone survey conducted
in October 2003 using a standardized script to assess
the practices of randomly selected UV tanning opera-
tors.
Results: For a 12-year-old potential patron, 62% offacili-
ties in states with minimum age restrictions prohibiting 12-
year-olds had an operator report that they would not per-
mit indoor tanning (Texas, 23%; Illinois, 7 4%; and Wiscon-
sin, 89%) compared with 18% in Colorado, a state without
youth access regulations. For a 15-year-old patron, most
facilities in vVisconsin, the only state with a minimum age
restriction for 15-year -olds, prohibited access (77%). Over-
all, 15% of operators offered youth discounts: Texas, 23%;
Illinois, 14%; Wisconsin, 11 %; and Colorado, 11%.
Participants: Randomly selected licensed indoor UV tan-
ning facility operators in Colorado, Texas, Illinois, and
Wisconsin.
Main Outcome Measures: Number of facilities (l)
complying with indoor UV tanning minimum age
regulations for a 12-year-old potential patron and a
15-year-old potential patron and (2) offering youth
discounts.
Conclusions: Tanning facilities in 4 states o(fered price
incentives directed at youths. State youth access regula-
tions were associated with decreased youth access to in-
door tanning. High compliance levels in states with long-
standing youth access regulations (lllinois and Wisconsin)
demonstrate the potential for successful tanning indus-
try youth access regulation.
Arch Den-nato!. 2005;141:959-962
Author Affiliations:
Departments of Dermatology
(Drs Hester and Dellavalle and
Mss Heilig and Drake) ,
Medicine (Dr Schilling) , and
Preventive Medicine and
Biometrics (Ms Heilig and
Dr Schilling), University of
Colorado at Denver and Health
Sciences Center; Louisiana State
University School of Medicine,
New Orleans (Dr D'Ambrosia);
and Department of Veterans
Affairs Medi.cal Center, Denver
(Dr Dellavalle). Dr Hester is
now with the Department of
Dermatology. Oregon Health
and Science University,
Portland.
Financial Disclosure: None.
M
ULTIPLE STUDIES
1
2
CON-
firm widespread in-
door UV tanning use
by US adolescents. Al-
though youths may
seek indoor tanning owing to the por-
rrayal of tanned skin as healthy and at-
tractive, UV is classified as a carcinogen
and is associated with numerous short- and
long-term effects, including skin can-
cer.H The use of tanning devices is asso-
ciated with squamous and basal cell car-
cinomas8 and has been implicated in
increased melanoma risk
9
-
12
Because ado-
lescence represents a critical period dur-
ing which UV radiation increases skin can-
cer risk,
13
14
altering the tanning behavior
of minors is a target for skin cancer pre-
vention efforts.
8
.11.1s
In 2003, only 3 states had set age lim-
its for indoortanni ng patrons: Texas at age
13 years (instituted in 2002), Illinois at age
14 years (1992), and Wisconsin at age 16
years (1992) .
16
further youth access re-
quirements in these states include guard-
ian accompaniment for 13- to 15-year-
olds in Texas, guardian consent for 16- to
17-year-olds in Texas, and guardian con-
sent for 14- to 17 -year-olds in Illinois
(Table). Most states, including Colo-
rado, do not set age limits on access to in-
door tanning. Two previous studies ex-
amining compliance with youth access
laws for indoor tanning described poor
See also pages 963 and 1028
operator compliance: 43% of indoor tan-
ning facilities were compliant with paren-
tal consent regulations in San Diego,
Calif,
18
and 13% of North Carolina facili-
ties complied with a required guardian
consent fonn for youths.
19
Another issue in adolescent use of tan-
ning facilities is the marketing directed to-
ward teens. Although price incentives for
the general public have encouraged fre-
quent tanning,
20
discounts specifically
available to adolescents have not been well
described.
(REPRI NTED) ARCH DERMATOVVOL 141, AUG 2005
959
W\VVI!.A RCHDERtvlA TOL.COM
Downloaded from www.archderrnatol.com at Brown University, on August 28, 2009
2005 American Medical Association . All rights reserved.
Table. Youth Access Regulation and Practices of Indoor UV Tanning Facilities in Texas, Illinois, Wisconsin, and Colorado
Texas Illinois Wisconsin Colorado
Variable (n = 100) (n = 100) (n = 100) (n = 100)
Regulations 1. No indoor tanning under 1. No indoor tanning under No indoor tanning under No youth access
age 13 y without age 14 y. age 16 y. regulations.
parental/legal guardian 2. Parental/legal guardian (last revised: 1992)
supervision and consent for ages 14-17 y.
physician's written (Last revised: 1992)
permission.
2. Parental/legal guardian
accompaniment for ages
13-15 y.
3. Parental/legal guardian
consent for ages 16-17 y.
(last revised: 2002)
Penalties First 3 youth access Warning letter issued for the Youth access violations Not applicable.
violations result in first violation. For a result in $50-$250
warning without fines. second violation, the fines.
Further violations may permittee may be fined
result in fines and permit $250. A third violation
revocation. may result in a minimum
fine of $500 and possible
permit revocation.
Enforcement 30 Randomly selected All licensed facilities are Licensed facilities with Not applicable
facilities and facilities audited yearly. complaints audited
with complaints are Approximately 10% of regarding the
audited yearly by patron records are complaint only.
examining records. examined. Patron age is
ascertained by recorded
date of birth.
Offered discounts for children, %t
Yes 23 14 11 11
No 77 74 86 80
Don't know/no answer 0 12 3 9
Practices regarding access by 12-year-olds
to indoor tanning. %t
Access allowed without restrictions 2 1 1 2
Cannot tan 2311 74 89 18
Parent/legal guardian consent 47 16 3 62
Parent/legal guardian accompaniment 8 0 0 8
Adult accompaniment or consent 13 6 0 1
Don't know 7 3 7 9
Practices regarding access by 15-year-olds
to indoor tanning, 'l'ot
Access allowed without restrictions 2 3 1 4
Cannot tan 5 4 77 10
Parent/legal guardian consent 64 74 16 70
Parent/legal guardian accompaniment 6 2 0 6
Adult accompaniment or consent 17 17 0 1
Don't know 6 0 6 9
*Sources: Youth access law penalties (http:l/www.uchsc.edu/dehsr/MapData.htm); Texas Department of Health, oral communication, January 21, 2004; Illinois
Department of Public Health, oral communication. January 21. 2004: Radiati on Protection Section. Wisconsin Division of Public Health, oral communication.
January 21, 2004; and Francis et al.
17
tP= .11.
tP< .01 .
Noncompliance with state laws.
II Nine facility operators stated that physician consent was required.
METHODS
Comprehensive lists of licensed tanning facility contact infor-
mation were obtained from state health departments (Febru-
ary to May 2003): Texas, 2332 facilities; ltlinois, 1905 facili-
ties; Wisconsin, 1447 facilities; and, Colorado, 580 facilities.
Colorado was chosen as the fourth state in this study for sev-
eral reasons: (1) in 2003, Colorado was 1 of 36 states without
any age or guardian requirements for UV tanning services; (2)
( REPRI NTED) ARCH DERMATOVVOL 141 , AUG 2005
960
surveying Colorado tanning facilities was most relevant for our
public health professional endeavors; and (3) of all states with-
out regulations, telecommunications charges for surveying Colo-
rado were the most economical.
One hundred facilities from each state were randomly se-
lected using a random number generator (http://www.random
.org) and were surveyed by telephone (October 2003). 1f a fa-
cility representative was unavailable after 3 calls, or if the
telephone number was disconnected, another facility from the
same state was randomly selected from the remaining facili-
W\VVI!.A RCHDERtvlA TOL .COM
Downloaded from www.archderrnatol.com at Brown University, on August 28, 2009
2005 American Medical Association. All rights r eserved.
ties. The survey consisted of a standardized script asking whet her
potential patrons aged 12 and 15 years would be allowed tore-
ceive indoor UV tanning treatments. If patronage was al-
lowed, the tanning facility operator was asked whether guard-
ian (including parent or legal guardian) or adult accompaniment
was required, whether guardian or adult consent was re-
quired, and whether any price discounts for youth were avail-
able. To maximize response rates, minimize social acceptabil-
ity response bias, and avoid deviation from information currently
given to potential customers, facility representatives were not
informed that they were participating in a study. This study re-
ceived Colorado institutional review board approval.
Health departments for each state were contacted by tele-
phone ro assess youth access to indoor tanning regulations, en-
forcement policies, penalties for noncompliance, and fre-
quency of imposing sanctions on violating facilities (November
2003 to January 2004). Survey data were entered into a data-
base management program (Microsoft Access; Microsoft Corp,
Redmond, Wash) by l investigator (R.D.) and were verified by
another investigator (L.F.H.). Using a statistical software pro-
gram (SAS 8.0; SAS Institute Inc, Cary, NC), a comparison of
compliance with minimum age restrictions for indoor UV tan-
ning by state was performed using the Fisher exact test.
RESULTS
Six hundred twenty-eight facilities were contacted by
telephone to obtain 400 licensed indoor tanning facility
survey responses (100 facilities in each state: Colorado,
Illinois, Texas, and Wisconsin). Two hundred twenty-
eight facilities were either unavailable after 3 calls or the
telephone number was disconnected (78 in Texas, 29 in
Illinois, 57 in Wisconsin, and 64 in Colorado). The Table
summarizes the survey responses. Overall, 15% of the tan-
ning facility operators reported that discounts were avail-
able for youths. For a 12-year-old potential patron, 62%
of facilities in states with age restrictions had operators
report that they would not permit indoor tanning (Texas,
23%; Illinois, 74%; and Wisconsin, 89%) compared with
18% in Colorado. The percentage of facilities prohibit-
ing a 12-year-old from tanning among facilities offering
and not offering youth discounts was similar ( 67% vs 58%;
P= .32). For a 15-year-old potential patron, rates of ac-
cess without guardian accompaniment in noncompli-
ance with respective state statutes were as follows: 83%
of operators in Texas would allow access without guard-
ian accompanimem, 20% in Illinois would allow access,
and 17% in Wisconsin would allow access. Noncompli-
ance for 15-year-olds was higher for facilities offering
youth discounts compared with facilities not offering
youth discounts (60% vs 46%; P= .08). Youth access regu-
lations, penalties, and enforcement varied by state (Table).
Skin cancer prevention strategies may include decreas-
ing UV exposure by further educating our youth, in-
creasing sun protection behaviors, taxing indoor tan-
ning for youths,
21
and adopting regulations limiting youth
access to indoor tanning. Given the prevalence of in-
door UV tanning, especially by adolescent girls,
1
2
and the
known risks of indoor tanning, public health efforts need
to be directed at this underrecognized carcinogen expo-
( REPRI NTED) ARCH DERMATOVVOL 141 , AUG 2005
961
sure. Although the efficacy of youth access regulations
for decreasing tobacco use has been debated,
22
analo-
gous regulations may be effective for limiting indoor tan-
ning and merit consideration.
16
In this 4-state comparison, compliance with regula-
tions for youth access to indoor tanning varied greatly
by state, and many facilities encouraged young patrons
by offering price discounts. Facilities in lllinois and Wis-
consin reported closer adherence to regulations than those
in Texas. Adolescents in Texas were largely required to
have guardian consent but were frequently not compli-
am with minimum age regulations or guardian accom-
paniment regulations for 12- and 15-year-old potential
patrons, respectively.
Differing rates of compliance with youth access laws
may be due to differences in state enforcement, penal-
ties for noncompliance, and the length of time a statute
has been in place. Our results do not support a differ-
ence due to enforcement Wisconsin showed the high-
est compliance for a 12-year-old potential patron but lacks
rigorous enforcement compared \vith Texas, which has
lower compliance and more systematic regulation en-
forcement. Texas state department officials described more
lenient penalties than those in Illinois and Wisconsin.
In addition, Texas youth access regulations were more
recently enacted (2002) than those in Illinois and Wis-
COI1Sin (1992), which may partly explain compliance rates.
Lower compliance in Texas might also be a result of Texas
having the lowest age limit among the states with an age
restriction. Better dissemination of current regulations
in Texas may improve compliance. A recent electronic
surveyn of tanning facility operators reports support for
youth access regulations, suggesting that better educa-
tion of facility operators with youth access regulations
will result in improved compliance.
ln addition to regulations for youth access, this study
assessed the prevalence of tanning price incentives for
youths. The tobacco industry previously promoted smok-
ing in the United States by providing free cigarette samples
that were often available to children despite voluntary
codes prohibiting such access.
2
.
1
Given that youth dis-
coums may encourage teen tanning and promote youth
access regulation violations, state health departments
should consider promoting bans on youth discounts.
This smdy has several limitations: (l) The survey was
conducted via telephone, assessing practices regarding
potential adolescent patrons. Observed compliance may
have differed if a youth approached the facility in per-
son. (2) The telephone survey, although anonymous, was
subject to social acceptability and self-reporting biases.
(3) Information was not obtained on how or how often
tanning operators verify the age of potential patrons. ( 4)
Facility operators were not questioned regarding the range
of ages for which youth discounts would be available. (5)
The home use of privately owned indoor tanning de-
vices was not assessed by the study. (6) Findings from
Colorado, the only state surveyed that did not have youth
access restrictions, may not be generalizable to other states
without restrictions.
Despite high noncompliance with youth access laws
in Texas, higher compliance levels in states \vith long-
standing youth access regulations (Illinois and Wiscon-
W\VVI!.A RCHDERtvlA TOL.COM
Downloaded from www.archderrnatol.com at Brown University, on August 28, 2009
2005 American Medical Association . All rights r eserved.
sin) suggest the potential for successful tanning indus-
try youth access regulation.
Accepted for Publication: April 9, 2005.
Correspondence: Robert P. Dellavalle, MD, PhD, MSPH,
Department of Veterans Affairs Medical Center, 1055
Clermont St, Mail Stop 165, Denver, CO 80220 (robert
. dellavalle@uchsc.edu).
Funding/Support: This study was supported by grant T32
AR07 411 from the National Institutes of Health, Bethesda,
Md (Dr Hester); grantS D14HP00153 from the Health Ser-
vices Research Award Faculty Development in Primary
Care (Dr Schilling); grant K-07 CA92550 from the Na-
tional Cancer Institute, Bethesda (Dr Dellavalle); and a seed
grant from the University of Colorado Cancer Center.
Previous Presentation: This study was presented at the
4th Combined European Dermatoepidemiology and
International Dermatoepidemiology Association Con-
gress; October 10, 2004; Venice, Italy.
Acknowledgment: We thank Brittany Wilson for help-
ing us conduct this study.
1. Demko CA, Borawski EA. Debanne SM, et al. Use of indoor UV tanning facilities
by white adolescents in the United States. Arch Pediatr Adolesc Med. 2003;
157:854860
2. Geller AC, Colditz G, Oliveria S, et al. Use of sunscreen, sunburning rates, and
tanning bed use among more than 10,000 US children and adolescents. Pediatrics.
2002; 109:1 0091 014.
3. National Toxicology Program. Available at: http://www.epa.gov/fedrgstr/EPA TOX
/1998/March/Day-19/17183.htm. Accessed January 5, 2004.
4. Spencer JM, Amonette RA. Indoor tanning: risks, benefits, and future trends.
JAm Acad Derma to!. 1995;33:288298.
5. Committee on Environmental Health. Ultraviolet light: a hazard to children.
Pediatrics. 1999;104:328333.
6. 11th Annual Report on Carcinogens from the Environmental Health Information
Service, a joint service of the NIH-National Institute of Environmental Health
Services and the US Department of Health and Human Services National Toxi-
cology Program. Available at: http://ehis.niehs.nih.gov/roc. Accessed January 5,
2004.
7. Centers for Disease Control and Prevention. Injuries associated with ultraviolet
tanning devices- Wisconsin. MMWR Morb Mortal Wk/y Rep. 1989;38:333
335.
8. Karagas MR, Stannard VA, Mott LA, Slattery MJ, Spencer SK, Weinstock MA.
Use of tanning devices and risk of basal cell and squamous cell skin cancers.
J Naif Cancer Jnst. 2002;94:224226.
9. Veierod MB, Weiderpass E. Thorn M, et al. A prospective study of pigmentation,
sun exposure, and risk of cutaneous malignant melanoma in women. J Naif Can-
cer/nsf. 2003;95:1530-1538 .
10. Wang SO, Setlow R, Berwick M, et al. Ultraviolet A and melanoma: a review.
JAm Acad Dermatol. 2001 ;44:837-846.
11. Swerdlow AJ, English JS. MacKie RM, et al. Fluorescent lights, ultraviolet lamps,
and risk of cutaneous melanoma. BMJ. 1988;297:647-650.
12. Dilley BL. A quantitative estimate of melanoma mortality from ultraviolet A sun-
bed use in the U.K. Br J Dermatol. 2003;149:578581.
13. Stern RS, Weinstein MC, Baker SG. Risk reduction for nonmelanoma skin can-
cer with childhood sunscreen use. Arch Dermatol. 1986;122:537545.
14. Khlat M, Vail A, Parkin M, et al. Mortality from melanoma in migrants to Austra-
lia: variation by age at arrival and duration of stay. Am J Epidemiol. 1992;135:
1103-1113.
15. Lim HW, Cooper K. The health impact of solar radiation and prevention strate-
gies: report of the Environment Council, American Academy of Dermatology.
JAm Acad Dermatol. 1999;41 :81 99.
16. Dellavalle RP, Parker ER, Cersonsky N. et al. Youth access laws: in the dark at
the tanning parlor? Arch Dermatol. 2003;139:443-448.
17. Francis SO, Burkhardt DL, Dellavalle RP. 2005: A banner year for new US youth
access tanning restrictions. Arch Dermatol. 2005;141:524-525.
18. Culley CA, Mayer JA, Eckhardt L, et al. Compliance with federal and state legis
lation by indoor tanning facilities in San Diego. JAm Acad Dermatol. 2001;
44:5360
19. Fleischer AB Jr, Lee WJ, Adams DP, etal. Tanning facility compliance with state
and federal regulations in North Carolina: a poor performance. JAm Acad Dermatol
1993;28:212-217.
20. Kwon HT, Mayer JA, Walker KK, et al. Promotion of frequent tanning sessions
by indoor tanning facilities: two studies. JAm Acad Dermatol. 2002;46:700-
705.
21. Dellavalle RP, Schilling LM, Chen AK, et al. Teenagers in the uv tanning booth?
tax the tan. Arch Pediatr Ado/esc Med. 2003;157:845-846.
22. Fichtenberg CM, Glantz SA. Youth access interventions do not affect youth smoking.
Pediatrics. 2002;109:10881092.
23. Hester EJ, Johnson KR, Crane l , et al. Attitudes and practices of indoor UV tan-
ning facility operators: an electronic survey. JAm Acad Dermatol. 2004;51:
814816.
24. Davis RM, Jason LA. The distribution of free cigarette samples to minors. Am J
Prev Med. 1988;4:21-26.
AIIIIOiliiCCIIICilt
Visit www.archdermatol.com. As an individual sub-
scriber to Archives of Dennatology, you have full-text on-
line access to the journal from 1998 forward. In addi-
tion, you can find abstracts to the journal as far back as
1965.
(REPRI NTED) ARCH DERMATOVVOL 141, AUG 2005 WWVv.ARCHDERtvlATOL.COM
962
Downloaded from www.archderrnatol.com at Brown University, on August 28, 2009
2005 American Medical Association. All rights r eserved.
Cancer Causes and Control (2005) 16:557- 560
DOl I 0. 1007 /s I 0552-004-6572-x
Springer 2005
A case for informed consent? Indoor UV tanning facility operator's provision
of health risks information (United States)
Lauren F. Heilig
1
2
, Renee D'Ambrosia
4
, Amanda L. Drake
1
, Robert P. Dellavalle1,3, & Eric J. Hester'
1
Department o.f Dermatology;
2
Department o.f Preventive Medicine and Biometrics, University o.f Colorado Denver and
Health Sciences Center, Denver, CO, 80262, USA;
3
Department of Veterans Affairs A1edical Center, Denver, CO,
80220, USA;
4
Louisiana State University School of Medicine, New Orleans, LA, 70112, USA
Received 7 June 2004; accepted in revised form 22 November 2004.
Key words: informed consent, risk, tanning, ultraviolet rays.
Abstract
Objective: Indoor UV tanning is associated with skin cancer. This study desctibes consumer health risks
informat ion provided by indoor UV tanning facility operators in four states (Colorado, Illinois, Texas, and
Wisconsin) with varying operator training, regulations, enforcement and penalties.
Methocll-: Using a cross-sectional survey study design, 100 randomly selected licensed indoor UV tanning facilities
from each state were surveyed anonymously by telephone. Facility operators were questioned regarding the
provision of information on potential adverse effects of indoor UV exposure.
Results: Of 628 licensed indoor UV tanning facilities contacted, 400 facilities were surveyed. Most (87%) advised
patrons of the potential risk of sunburn from indoor tanning. Less than half of facility operators in Colorado, Texas
and Wisconsin informed patrons about the risk of skin cancer (42, 43 and 48%, respectively) compared with 81% of
Illinois operators. Likewise, more operators in Illinois reported the risk of premature aging (79%) compared with
other states (41% Colorado, 43% Texas and 51% Wisconsin).
Conclusions: Tanning facility operators frequently misinformed patrons of indoor UV exposure risks. The
provision of informed consent by indoor tanning facility operators needs improved adaptation by the tanning
industry as a standard for customer service.
Introduction
Despite the cutaneous health risks, the number of
Americans using indoor ultraviolet (UV) tanning has
increased more than three fold between 1986 and 1996,
from 2 to 6% of adults [1]. Use of indoor tanning is
associated with squamous and basal cell carcinomas
[2- 3], and may increase melanoma risk (4-8]. Chronic
exposure to UV light also leads to premature aging and
wrinkling of tl1e skin [9, I 0].
Federal and state statutes regulate licensed commer-
cial indoor UV tanning facilities . The Federal Drug
Administration (FDA) requires that warning statement
* Address for correspondence to: Robert P. Dellavalle, MD, PhD,
MSPH, Department of Dermatology. VA Medical Center, 1055
Clermont Street, # 165, CO 80220, Denver, USA. Ph.: + 303-399-
8020 x2475; Fax: + 303-399-4686; E-mai l: robert.dellavallc@uchsc.edu
labels accompany sunlamp products, stating risks that
include skin cancer and premature aging [II). Similarly,
various state regulations require additional provision of
information regarding health risks associated with
indoor UV exposure [12- 15].
Limited studies have examined the informati on given
to potential customers: ( I) J 9% of North Carolina
tanning facilities provided consumers with a statement
outlining the risks of UV tanning [16], and (2) 17% and
32% of operators stated that sunburn and skin cancer
was a tisk, respectively, in San Diego (17). The effect of
differing state tanning industry regulations, enforcement
and operator training has yet to be reported. This cross-
sectional study examined indoor tanning operator
knowledge of tanning facility regulations for risk
information in four states (Colorado, Illinois, Texas
and Wisconsin) with varying operator training, regula-
tion, enforcement and penalties.
558
Materials and methods
Lists of licensed tanning facilities were obtained from
the state health departments of Texas (n = 2332),
Illinois (n = 1905), Wisconsin (n = 1447) and Colorado
(n = 580) (February- May 2003). Using a random
number generator (www.random.org), 100 facilities
from each state were randomly selected and surveyed
by telephone (October- November 2003). The survey
consisted of a standardized script asking whether indoor
UV tanning increases one's risk of sunburn, skin cancer
or premature aging. These questions were part of a more
extensive survey assessing additional variables (Hester
2005, submitted). Interviewers posed as a potential
patron and operators were not informed that their
responses were being collected in order to maximize
response rates, minimize social acceptability response
bias and avoid deviation from information currently
given to potential customers. This study received Col-
orado Institutional Review Board approval (#03- 816).
The survey was conducted by two authors (LH,
RD'A) over a three-week period (October- November,
2003). If a facility's telephone number was out of service
or if no facility operators were available to answer
questions after three attempts, another facility from that
state was selected via randomization of remaining
facilities. Ambiguous responses were coded as ' Don't
know/ No answer'. Inter- and intra-rater reliability was
examined by surveying 30 facilities in two states by the
two different authors (Hester 2005, submitted).
Survey data were entered into a computer database
(Microsoft Access) by one author (RD' A) and verified
by another (LH) . Descriptive statistics and kappa
statistics were performed using SAS (SAS, Cary, NC,
1999).
L.F. Heilig et al.
Results
Six-hundred-twenty-eight licensed indoor UV tanning
facilities were telephoned (164 Colorado, 129 Illinois,
178 Texas and 157 Wisconsin) to obtain 100 survey
responses from each state. Inter- and intra-rater reli-
ability for one survey question was K = 0.4 and 0.3,
respectively (Hester 2005, submitted).
Eighty-seven percent of all operators reported sun-
burn as a potential risk of indoor UV tanning (Colorado
87, Illinois 93, Texas 76 and Wisconsin 92%). About
half of operators (54%) reported that skin cancer was a
potential health risk of indoor UV tanning (Colorado
42, Illinois 81, Texas 43 and Wisconsin 48/c)). Similarly,
54% reported that premature aging was a potential
health risk of indoor UV tanning (Colorado 41, Illinois
79, Texas 43 and Wisconsin 51%) (Table 1).
Discussion
Indoor UV tanning poses health risks to patrons.
A survey of physicians found that 42% of dermatolo-
gists and 29% of emergency room physicians had
treated a patient for burns incurred from a UV tanning
device [18]. Although regulations that protect indoor
UV tanning patrons exist, previous studies suggest
compliance varies and is suboptimal.
This is the first multi-state comparative study to
examine indoor UV tanning facility operator's provision
of health ri sks information to patrons. On average the
best health risk information was provided by operators
in Illinois, a state with long-standing regulations that
thoroughly audits indoor tanning operations and
imposes penalties for non-compliance [12] (Table 2).
Tahle /. Practices of indoor tanning facility operators in Colorado. Illinois, Texas and Wisconsin
Colorado Illinois Texas Wisconsin
(n = 100) (n = 100) (n = 100) (n = 100)
Informed patron of possible risk of sunburn
Yes 87 93 76 92
No 9 7 12 2
Don't knowf no answer 4 0 12 6
Informed patron of possible risk of skin cancer
Yes 42 81 43 48
No 31 13 28 23
Don' t koowjno answer 27 6 29 29
Informed patron of possible risk of premature aging
Yes 4 1 79 43 51
No 32 16 29 22
Don't know/ no answer 27 5 28 27
Indoor UV tanning facility operator knowledge to health risks 559
Table 2. Indoor UV tanning regulations, enforcement and penalties in Colorado, Illinois, Texas and Wisconsin
Colorado Illinois Texas Wisconsin
Regulations
Trained operator present
during operational hours
Signed warning statement
No regulation Required Required Required
None (required to give copy
of warning statement)
Required Required Required
Enforcement AJI facilities on a rotating
basis (every facilit y is
examined approximately
every three years)
All facilities audited
yearly
Random selection
of 30 facilities and
those with complaints
AU facilities with
complaints
Penalties None Warning letter for Warning for first three
violations and thereafter
possible fines and permit
revocation
$50 to $250 fine
and possible
permit revocation
first violation, a fine
up to $250 for second
violation, and a
minimum fine of $500
and possible permit
revocation for third
violation
Operators should advise patrons of potential adverse
effects of indoor tanning and direct patrons to addi-
tional informational resources. Although most opera-
tors advised patrons of cutaneous burning risk,
improved risk information provision is warranted:
46% of operators 'did not know' or misinformed the
interviewer of the risk of skin cancer. These results
suggest that operators are counseling with insufficient or
incorrect information.
Informed consent is 'a process of information ex-
change that may include, in addition to reading and
signing the informed consent document ... measures of
subject understanding' [19]. Obtaining informed consent
is standard for medical procedures and should be a
standard for the indoor tanning industry, as it is
unethical to permit indoor tanning if the patron is
unaware of potential risk. Wisconsin, Texas and Illinois
require signed consent forms (Colorado requires that a
copy of warning statements be provided to patrons)
(Table 2), however there are no regulations that assess
patron comprehension. The use of signed consent forms
is only one aspect of informed consent; provision of the
best available information and a demonstrated under-
standing ofinf01mation by the patron are also necessary.
Our study has several limitat ions: (1) the survey was
conducted via telephone and observed compliance may
have differed if a patron approached the facility in
person. For example, an operator might be unaware of
adverse health risks from "UV exposure but may
routinely provide consent forms specifying risks to
patrons; (2) since telephone calls were placed using
calling cards, we cannot rule out the remote possibility
that operators not recognizing an incoming phone
number with a familiar area code may have provided
different information than that usually provided (social
desirability bias); (3) the home use of privately owned
indoor UV tanning devices was not captured by the
study; (4) observed reliabi li ty was conducted with a
survey question not reported in this study and
additional questions were not included for fear that
further resurveying of the operators would have jeop-
ardized result validity by raising suspicion regarding the
confederate caller; and (5) the name of the operator
answering the phone was not asked, therefore we do not
know how often the repeat questions for reliability were
directed to the same operator.
Still the study clearly shows that tanning facilities are
fai ling to fully inform potential patrons and obtain
informed consent, an et hical necessity for patron deci-
sion-making and safety. Obtaining informed consent
relies on several factors: (!) supplying consumers with
the best available information on the benefits and risks
of a therapy; (2) improved operator knowledge by
enhancing operator training; and (3) continued enforce-
ment and penalties of current regulations. While the
existence of voluntary facility restrictions suggests tan-
ning industry support for the principle of informed
consent, formal regulations accompanied by enforce-
ment and penalties may be needed to protect patron
safety. The tanning industry should aspire to the highest
standards of patron service - obtaining informed
consent from its patrons.
Acknowledgements
We thank Brittany Wilson for her help conducting this
study. Dr. Hester was supported by National I nstitutes of
560
Health grant T32 AR074ll and Dr. Dellavalle was
supported by the National Cancer Institute (NCI) grant
K-07 CA92550. This project was supported in part by a
seed grant from the University of Colorado Cancer
Center. Internet addresses referenced in this article
have been preserved by the authors using FURL
(www.furl.net).
References
I. Robinson JK, Rigel DS, Amonette RA (1997) Trends in sun
exposure knowledge, attitudes, and behaviors: 1986-1996. J Am
Acad Dermato/37(2 Pt 1): 179- 186.
2. Karagas RK, Stannard VA, Mott LA, e1 a/. (2002) Use of tanning
devices and risk of basal cell and squamous cell skin cancers. J Nat!
Cancer l nst 94: 224- 226.
3. English DR, Armstrong BK, Kricker A. Fleming C (1997)
Sunlight and cancer. Cancer Causes ControlS: 271- 283.
4. Whiteman DC, Whiteman CA, Green AC (2001) Childhood sun
exposure as a risk factor for melanoma: a systematic review of
epidemiologic studies. Cancer a t ~ ~ e s Control 12: 69- 82.
5. Veierod MB. Weiderpass E. Thorn M. eta/. (2003) A prospective
study of pigmentation, sun exposure, and risk of cutaneous
mal ignant melanoma in women . .I Nat! Cancer Ins/ 95: 1530-
1538.
6. Wang SQ, Setlow R, Berwick M, et al. (2001) Ultraviolet A and
melanoma: a review. JAm Acad Dermato/ 44: 837- 846.
7. Swerdlow AJ, English JS, MacKie RM, et al. (1988) Fluorescent
lights, ultraviolet lamps, and risk of cutaneous melanoma. BM.!
297: 647- 650.
L.F. Heilig et al.
8. Diffey BL(2003) A quantitativeestimate of melanoma mortality from
ultraviolet A sun bed use in the U.K. Br J Derma to/ 149: 578-581.
9. Lavker RM, Gerberick GF, Veres D, Irwin CJ, Kaidbey KH
(1995) Cumulative effects from repeated exposures to suberythe-
mal doses of UVB and UVA in human skin. JAm A cad Derma to/
32: 53-62.
10. Lowe NJ, Meyers DP, Wieder JM, eta/. (1995) Low doses of
repetitive ultraviolet A induce morphologic changes in human
skin. J Invest Dermato/ 105: 739-743.
II. Department of Health and Human Services (US), Food and Drug
Administration (2003) Performance standards for light-emitting
products (21 CFR 1040). Fed Reg: Title 21 , Volume 8.
12. Illinois Department of Public Health (1992) Tanning facilities code
(77 Ill. Adm. Code 795). Rules of the Illinois Department of Public
Health.
13. 2001- 2002 Wisconsin Statutes & Annotations (2001) Chapter 255:
Chronic disease and injuries (s. 255.08).
14. Texas Department of Health (2002) Rules for licensure of tanning
facilities (25 Texas Administrative Code, 229.341- 229.357).
15. Colorado Department of Public Health and the Environment
( 1989) Artificial tanning device regulations (Section 25-5-1 06( 1 ).
(2)(a),(2)(b)).
16. Fleisher AB, Lee WJ. Adams DP, eta/. (1993) Tanning facility
compliance with state and federal regulations in North Carolina: a
poor performance. JAm Acad Dermato/28(2): 212- 217.
17. Culley CA, Mayer JA. Eckhardt L. et al. (2001) Compliance with
federal and state legislation by indoor tanning facilities in San
Diego. J Am A cad Dermato/ 44: 53-60.
18. Centers for Disease Control ( 1989) Injuries associated with
ultraviolet tanning devices - Wisconsin. lAMA 261: 3519- 3520.
19. Food and Drug Administration ( 1998) The consent process. In:
Guidance for Inst itutional Review Boards and Clinical Investiga-
tors. http:f/ www.fda.govjocfohrt/irbsfinformedconscnt.html#pro-
cess, accessed on June 4, 2004.
Dietary Supplement Fact Sheet: Vitamin D
OFFICT OF
DII:.IARY
SUPPLE tENTS
Dietary Supplement Fact Sheet
Table of Contents
Introduction
Reference Intakes
Sources of Vitamin D
Vitamin D Intakes and Status
Vitamin D Deficiency
Groups at Risk of Vitamin D Inadequacy
Vitamin D and Health
Health Risks from Excessive Vitamin D
Interactions with Medications
Vitamin D and Healthful Diets
References
Introduction
Vitamin D
Vitamin D is a fat-soluble vitamin that is naturally present in very few foods, added to others, and available as a dietary
supplement. It is also produced endogenously when ultraviolet rays from sunlight strike the skin and trigger vitamin D synthesis
[1,2]. Vitamin D obtained from sun exposure, food, and supplements is biologically inert and must undergo two hydroxylations in
the body for activation. The first occurs in the liver and converts vitamin D to 25-hydroxyvitamin D [25(0H)D], also known as
calcidiol. The second occurs primarily in the kidney and forms the physiologicall y active 1,25-dihydroxyvitamin D [1,25(0H}2D], also
known as calcitriol [3].
Vitamin D is essential for promoting calcium absorption in the gut and maintaining adequate serum calcium and phosphate
concentrations to enable normal mineralization of bone and prevent hypocalcemic tetany. It is also needed for bone growth and
bone remodeling by osteoblasts and osteoclasts [3,4,5] . Without sufficient vitamin D, bones can become thin, brittle, or misshapen.
Vitamin D sufficiency prevents rickets in children and osteomalacia in adults [2,6, 7] . Together with calcium, vitamin D also helps
protect older adults from osteoporosis.
Vitamin D has other roles in human health, including modulation of neuromuscular and immune function and reduction of
inflammation. Many genes encoding proteins that regulate cell proliferation, differentiation, and apoptosis are modulated in part by
vitamin D [3,5,8,9] . Many laboratory-cultured human cells have vitamin D receptors and some convert 25(0H)D to 1,25(0H}zD [10] .
It remains to be determined whether cells with vitamin D receptors in the intact human carry out this conversion.
Serum concentration of 25(0H)D is the best indicator of vitamin D status. It reflects vitamin D produced cutaneously and that
obtained from food and supplements [4] and has a fairly long circulating half-life of 15 days [11 ]. However, serum 25(0H)D levels do
not indicate the amount of vi tamin D stored in other body tissues. Circulating 1,25(0H}zD is generally not a good indicator of
vitamin D status because it has a short half -life of 15 hours and serum concentrations are closely regulated by parathyroid hormone,
calcium, and phosphate [ 11]. Levels of 1,25(0H}zD do not typically decrease until vitamin D deficiency is severe [ 5, 10].
There is considerable discussion of the serum concentrations of 25(0H)D associated with deficiency (e.g. , rickets), adequacy for
bone health, and optimal overall health (Table 1 ). A concentration of <15 nanograms per milliliter (ng/ml) (or <37 .5 nanomoles per
liter [nmoi/L]) is generally considered inadequate; concentrations >15 ng/ml (>37 . 5 nmoi/L) are recommended. Higher levels are
proposed by some (>30 ng/ml or >75 nmoi/L) as desirable for overall health and disease prevention [12], but insufficient data are
available to support them [ 13]. Serum concentrations of 25(0H)D consistently >200 ng/ml (>500 nmoi/L) are potentially toxic.
Ta bl d e 1: Serum 25-Hyc roxyvitamin D [25(0H}D] Concentrations an d I h* Heat
I ngtmL ** II nmoltL ** II
Health status
1<10-11 11<25-27.5
with vitamin D deficiency, leading to rickets in infants and children and osteomalacia in
adults [ 4, 13]
1<10-15 11<25-37. 5 !I Generally considered inadequate for bone and overall health in healthy individual s [4,13]
1=15 11 =37.5 !IGenerally considered adequate for bone and overall health in healthy individuals [4]
II II II
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
I
I
I
Dietary Supplement Fact Sheet: Vitamin D
Consistently Consistently Considered potentially toxic, leading to hypercalcemia and hyperphosphatemia, although human data
>200 >500 are limited. In an ani mal model, concentrations =400 ng/ml (=1,000 nmoi/L) demonstrated no toxicity
[11,14].
. . .
*Serum concentrations of 25(0H)D are reported m both nanograms per millil iter (ng/ml) and nanomoles per liter (nmoi/L) .
** 1 ng/ml = 2.5 nmoi/L
An additional compl ication in assessing vitamin D status is in the actual measurement of serum concentrations of 25(0H)D.
Considerable variability exists among the various assays available and among laboratories that conduct the analyses [15, 16, 17]. This
means that compared to the actual concentration of 25(0H)D in a sample of blood serum, a falsely low or falsely high value may be
obtained depending on the assay or laboratory used [18]. A standard reference material for 25(0H)D became avail abl e in july 2009
that will now permit standardization of values across laboratories [19].
Reference Intakes
Intake reference values for vi t amin D and other nutrients are provided in the Dietary Reference Intakes (ORis) developed by the
Food and Nutrition Board (FNB) at the Institute of Medicine of The National Academies (formerly National Academy of Sciences) [4].
DRI is the general term for a set of reference val ues used to plan and assess nutrient intakes of healthy people. These val ues, which
vary by age and gender [4], include:
Recommended Dietary Allowance (RDA): average daily level of intake sufficient to meet the nutrient requirements of nearly
all (97%-98%) healthy people.
Adequate Int ake (AI): establi shed when evidence is insufficient t o develop an RDA and is set at a level assumed to ensure
nutritional adequacy.
Tolerable Upper Intake Level (UL): maximum daily intake unlikely to cause adverse health effects [4].
The FNB established an AI for vitami n D that represents a dail y intake that is sufficient to maintain bone health and normal calcium
metabolism i n healthy people. Ais for vitami n D are listed in both micrograms (meg) and International Units (IUs); the biological
activity of 1 meg is equal to 40 IU (Table 2). The Ais for vitamin D are based on the assumption that the vitamin is not synthesized
by exposure to sunl ight [4].
bl d k Ta e 2: A equate Inta es (Als) or VItamin D [ 4]
I
Age IIChildrenll Men IIWomeniiPregnancyiiLactationl
meg
B1rth to 13 years (
200
IU)
ID O l II I
114-18 years
5 meg 5 meg ,,,5 meg
(200 IU) (200 IU) (200 IU)
(200 IU)
119-50 years
5 meg 5 meg
(200 IU) (200 IU) (200 IU) (200 IU)
151-70 years
10 meg 10 meg
I II I
(400 IU) (400 IU)
171+ years
15 meg 15 meg
I II I
(600 IU) (600 IU)
In 2008, the American Academy of Pediatrics (MP) issued recommended intakes for vitamin D that exceed those of FNB [20]. The
AAP recommendat ions are based on evidence from more recent cl inical trials and the history of safe use of 400 IU/day of vitamin D
in pediatric and adolescent populations. MP recommends that exclusively and partially breastfed infants receive supplements of
400 IU/day of vitamin D shortly after birth and continue to receive these supplements until they are weaned and consume =1 ,000
mllday of vitamin D-fortified formula or whole milk [20]. (All formulas sold in the Uni t ed States provide =400 IU vitamin 0
3
per
liter, and the majority of vitamin D-only and multivitamin liquid supplements provide 400 IU per serving.) Simil arly, all non-
breastfed infants i ngesting <1 ,000 mllday of vitamin D-fortified formula or milk should receive a vitamin D suppl ement of 400
IU/day. MP also recommends that older children and adolescents who do not obtain 400 IU/day through vitamin D-fortified milk
and foods should take a 400 IU vitamin D supplement dai ly [20].
The FNB established an expert committee in 2008 to review the ORis for vitamin D (and calcium). The current DR!s for this nutri ent
were established in 1997, and since t hat time substantial new research has been published to justify a reevaluation of adequate
vitamin D intakes for healthy populations. Determinations of ORis are based on i ndicators of adequacy or hazard; dose-response
curves; health outcomes; life-stage groups; and relations between intakes, biomarkers, and outcomes. For vitamin D, the FNB
committee will focus on (1) effects of circulating concentrations of 25(0H)D on health outcomes, (2) effects of vitamin D intakes on
circulating 25(0H)D and on health outcomes, and (3) levels of intake associated with adverse effects [21]. The FNB expects to issue
its report, updat ing as appropriate the ORis for vitamin D and calcium, by May 2010 [22].
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Dietary Supplement Fact Sheet: Vitamin D
Sources of Vitamin D
Food
Very few foods in nature contain vitamin D. The flesh of fish (such as salmon, tuna, and mackerel) and fish liver oils are among the
best sources [4]. Small amounts of vitamin Dare found in beef liver, cheese, and egg yolks. Vitamin Din these foods is primarily in
the form of vitamin D3 (cholecalciferol) and its metabolite 25(0H)D3 [23]. Some mushrooms provide vitamin D2 (ergocalciferol) in
variable amounts [24-26]. Mushrooms with enhanced l evels of vitamin D
2
from being exposed to ultraviolet light under controlled
conditions are also avail able.
Fortified foods provide most of the vitamin Din the American diet [4,26]. For example, almost all of the U.S. milk supply is fortified
with 100 IU/cup of vitamin D (25% of the Dai ly Value or 50% of the AI level for ages 14-50 years). In the 1930s, a mi l k fortification
program was implemented in the United States to combat rickets, then a major public health problem. This program virtually
eliminated the disorder at that time [4, 14]. Other dairy products made from milk, such as cheese and ice cream, are generally not
fortified. Ready-to-eat breakfast cereals often contain added vitamin D, as do some brands of orange juice, yogurt, and margarine.
In the United States, foods all owed to be fortified with vitamin D include cereal flours and related products, milk and products
made from milk, and calcium-fortified fruit juices and drinks [27]. Maximum levels of added vitamin Dare specified by law.
Several food sources of vitamin D are listed in Table 3.
Table 3 Selected Food Sources of Vitamin D [ 30) .
I
Food
IUs per
serving*
II Percent
DV**
lcod liver oil, 1 tablespoon 1,360 340
!salmon (sockeye), cooked, 3 ounces 794 199
Mushrooms that have been exposed to ultraviolet light to increase vitamin D, 3 ounces (not yet
400 100
commonly available)
!Mackerel, cooked, 3 ounces 388 97
!Tuna f ish, canned in water, drained, 3 ounces 154 39
IMilk, nonfat, reduced fat, and whole, vitamin D-fortified, 1 cup 115-124 29-31
Orange juice fortified with vitamin D, 1 cup (check product labels, as amount of added vitamin D
100 25
varies)
Yogurt, fortified with 20% of the DV for vitamin D, 6 ounces (more heavily fortified yogurts provide
80 20
more of the DV)
!Margarine, fortified, 1 tablespoon 60 15
!sardines, canned in oil, drained, 2 sardines 46 12
!Liver, beef, cooked, 3.5 ounces 46 12
Ready-to-eat cereal , fortified with 10% of the DV for vitamin D, 0.75-1 cup (more heavily fortified
40 10
cereals might provide more of the DV)
IEgg, 1 whole (vitamin D is found in yolk) 25 6
!cheese, Swiss, 1 ounce 6 2
*IUs = International Units.
**DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration to help consumers compare t he nutrient
contents of products within the context of a total diet. The DV for vitamin D is 400 IU for adults and chi ldren age 4 and older.
Food labels, however, are not required to list vitamin D content unless a food has been fortified with this nutrient. Foods
providing 20% or more of the DV are considered to be high sources of a nutrient.
The U.S. Department of Agriculture's Nutrient Database Web site, http://www.nal.usda.gov/fnic/foodcomp/search, lists the
nutrient content of many foods and provides a list of foods containing vitamin D:
http;//www.ars.usda.gov/SP2UserFiles/Piace/123545QO/Data/SR22/nutrlist/sr22a324,pdf . A growing number of foods are bei ng
analyzed for vitamin D content. Simpler and faster methods to measure vitamin D in foods are needed, as are food standard
reference materials with certified values for vitamin D to ensure accurate measurements [31 ].
Sun exposure
Most people meet their vitamin D needs through exposure to sunlight [5,31]. Ultraviolet (UV) B radiation with a wavelength of 290-
315 nanometers penetrates uncovered skin and converts cutaneous 7-dehydrocholesterol to previtamin D
3
, which in turn becomes
vitamin D
3
[9,32,33]. Season, geographic latitude, time of day, cloud cover, smog, skin melanin content, and sunscreen are among
the factors that affect UV radiation exposure and vitamin D synthesis [33]. The UV energy above 42 degrees north latitude (a l ine
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
I
I
I
I
I
I
I
I
I
I
I
I
I
I
Dietary Supplement Fact Sheet: Vitamin D
approximately between the northern border of California and Boston) is insufficient for cutaneous vitamin D synthesis from
November through February [5]; in far northern latitudes, this reduced intensity lasts for up to 6 months. In the United States,
latitudes below 34 degrees north (a line between Los Angeles and Columbia, South Carolina) allow for cutaneous production of
vitamin D throughout the year [27].
Complete cloud cover reduces UV energy by 50%; shade (including that produced by severe pollution) reduces it by 60% [34]. UVB
radiation does not penetrate glass, so exposure to sunshine indoors through a window does not produce vitamin D [35]. Sunscreens
with a sun protection factor of 8 or more appear to block vitamin D-producing UV rays, although in practice people generally do not
apply sufficient amounts, cover all sun-exposed skin, or reapply sunscreen regularly [36]. Skin likely synthesizes some vitamin D
even when it is protected by sunscreen as typically applied.
The factors that affect UV radiation exposure and research to date on the amount of sun exposure needed to maintain adequate
vitamin D levels make it difficult to provide general guidelines. It has been suggested by some vitamin D researchers, for example,
that approximately 5-30 minutes of sun exposure between 10 AM and 3 PM at least twice a week to the face, arms, legs, or back
without sunscreen usually lead to sufficient vitamin D synthesis and that the moderate use of commercial t anning beds that emit
2%-6% UVB radiation is also effective [10,33]. Individuals with limited sun exposure need to include good sources of vitamin Din
thei r diet or take a supplement.
Despite the importance of the sun to vitamin D synthesis, it is prudent to limit exposure of skin to sunlight [36] and UV radiation
from tanning beds [37]. UV radiation is a carcinogen responsible for most of the estimated 1.5 million skin cancers and the 8,000
deaths due to metastatic melanoma that occur annually in the United States [36]. Lifetime cumulative UV damage to skin is also
largely responsible for some age-associated dryness and other cosmetic changes. It is not known whether a desirable level of regular
sun exposure exists that imposes no (or minimal) risk of skin cancer over time. The American Academy of Dermatology advises that
photoprotective measures be taken, including the use of sunscreen, whenever one is exposed to the sun [38].
Dietary supplements
In supplements and fortified foods, vitamin D is available in two forms, 0
2
(ergocalciferol) and 0
3
(cholecalciferol). Vitamin 0
2
is
manufactured by the UV irradiation of ergosterol in yeast, and vitamin D3 is manufactured by the irradiation of 7-dehydrocholesterol
from lanolin and the chemical conversion of cholesterol [ 10]. The t wo forms have t raditionally been regarded as equivalent based
on their ability to cure rickets, but evidence has been offered that they are metabolized differently. Vitamin 0
3
could be more than
three times as effective as vitamin 0
2
in raising serum 25(0H)D concentrations and maintaining those levels for a longer time, and
its metabolites have superior affinity for vitamin D-binding proteins in plasma [5,39,40]. Because metabolite receptor affinity is not
a functional assessment, as the earlier results for the healing of rickets were, further research is needed on the comparative
physiological effects of both forms. Many supplements are being reformulated to contain vitamin 0
3
instead of vitamin 0
2
[40]. Both
forms (as well as vitamin D in foods and from cutaneous synthesis) effectively raise serum 25(0H)D levels [5].
Vitamin D Intakes and Status
In 1988-1994, as part of the thi rd National Health and Nutrition Examination Survey (NHANES III), the frequency of use of some
vitamin D-containing foods and supplements was examined in 1,546 non-Hispanic African American women and 1,426 non-Hispanic
white women of reproductive age (15-49 years) [41 ]. In both groups, 25(0H)D levels were higher in the fall (after a summer of sun
exposure) and when milk or fortified cereals were consumed more than three times per week. The prevalence of serum
concentrations of 25(0H)D =15 ng/ml (=37 .5 nmoi/L) was 10 times greater for the African American women (42.2%) than for the
white women (4.2%).
The 2000-2004 NHANES provides the most recent data on the vitamin D nutritional status of the U.S. population. Generally, younger
people had higher serum 25(0H)D levels t han older people, males had higher levels than females, and non- Hispanic whites had
higher levels than Mexican Americans, who in turn had higher level s than non-Hispanic blacks. Depending on the population group,
1%-9% had serum 25(0H)D levels <11 ng/ml (<27.5 nmoi/L), 8%-36% had levels <20 ng/ml (<50 nmoi/L), and t he majority (50%-78%)
had levels <30 ng/ml (<75 nmoi/L) [42].
In NHANES 2000-2004, age-adjusted mean serum 25(0H)D concentrations were 2-8 ng/ml (5-20 nmoi/L) lower compared to NHANES
III [ 43]. However, after adjustment for assay shifts, age-adjusted means in NHANES 2000-2004 remained significantly lower (by 2.0-
3.6 ng/ml (5-9 nmoi/L)) in most males, but not in most females. In a study subsample, adjustment for the confounding effects of
assay differences changed mean serum 25(0H)D concentrations by - 4 ng/ml (-10 nmoi/L), and adjustment for changes in the
factors likely related to real changes in vitamin D status (such as body mass index (BMI), milk intake, and sun protection) changed
mean serum 25(0H)D concentrations by 0.4-0.64 ng/ml (1.0-1.6 nmoi/L).
Subsequent to this report, another investigator [44] evaluated vitamin D levels measured in NHANES 2001-2004 compared to NHANES
III and reported a marked decline, leading some to suggest that the majority of children and adults in the United States (and almost
all African Americans and Mexican Americans) are vitamin D insufficient. However, this analysis exaggerates the temporal and
demographic trends in vitamin D status because it uses a higher than usual cutoff to characterize vitamin D insufficiency, does not
separate the independent effects of season and latitude in data and, most seriously, fails to compensate for a change in the
25(0H)D measurement assay used between both sets of NHANES surveys [45]. Over time, mean serum 25(0H)D concentrations in the
United States have declined, but only modestly, when compensating for the assay change [43]. The real decline (-2.0-3.6 ng/ml
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Dietary Supplement Fact Sheet: Vitamin D
(-S-9 nmoi/L)) is likely due to simultaneous increases in BMI, reduced milk intake, and greater use of sun protection in the U.S.
population.
According to NHANES data from 2005-2006, only 29% of adult men and 17% of adult women (ages 19 and older) had intakes of
vitamin D from food alone that exceeded their Ais. Overall in the U.S. population, only about one-third of individuals 1 year of age
and older had vitamin D intakes from food exceeding their respective Ais [46]. However, dietary supplements as well as foods
contribute vitamin D, so both sources must be included to obtain a true picture of total intakes. In 2005-2006, 37% of people in the
United States reported the use of a dietary supplement containing vitamin D. Total intake estimates of vitamin D from both food and
supplements are currently being tabulated by the Office of Dietary Supplements.
Vitamin D Deficiency
Nutrient deficiencies are usually the result of dietary inadequacy, impaired absorption and use, increased requirement, or increased
excretion. A vitamin D deficiency can occur when usual intake is lower than recommended levels over time, exposure to sunlight is
limited, the kidneys cannot convert vitamin D to its active form, or absorption of vitamin D from the digestive tract is inadequate.
Vitamin D-deficient diets are associated with milk allergy, lactose intolerance, and strict vegetarianism [47].
Rickets and osteomalacia are the classical vitamin D deficiency diseases. In children, vitamin D deficiency causes rickets, a disease
characterized by a failure of bone tissue to properly mineralize, resulting in soft bones and skeletal deformities [34]. Rickets was
first described in the mid-17th century by British researchers [34,48]. In the late 19th and early 20th centuries, German physicians
noted that consuming 1-3 teaspoons of cod liver oil per day could reverse rickets [48]. In the 1920s and prior to identification of
the structure of vitamin D and its metabolites, biochemist Harry Steenbock patented a process to impart antirachitic activity to
foods [27]. The process involved the addition of what turned out to be precursor forms of vitamin D followed by exposure to UV
radiation. The fortification of milk with vitamin D has made rickets a rare disease in the United States. However, rickets is still
reported periodically, particularly among African American infants and children [34,48]. A 2003 report from Memphis, for example,
described 21 cases of rickets among infants, 20 of whom were African American [48].
Prolonged exclusive breastfeeding without the AAP-recommended vitamin D supplementation is a significant cause of rickets,
particularly in dark-skinned infants breastfed by mothers who are not vitamin D replete [6]. Additional causes of rickets include
extensive use of sunscreens and placement of children in daycare programs, where they often have less outdoor activity and sun
exposure [34,48]. Rickets is also more prevalent among immigrants from Asia, Africa, and the Middle East, possibly because of
genetic differences in vitamin D metabolism and behavioral differences that lead to less sun exposure [34].
In adults, vitamin D deficiency can lead to osteomalacia, resulting i n weak muscles and bones [6, 7,11 ]. Symptoms of bone pain and
muscle weakness can indicate inadequate vitamin D levels, but such symptoms can be subtle and go undetected in the initial stages.
Groups at Risk of Vitamin D Inadequacy
Obtaining sufficient vitamin D from natural food sources alone can be difficult. For many people, consuming vitamin D-fortified
foods and being exposed to sunlight are essential for maintaining a healthy vitamin D status. In some groups, dietary supplements
might be required to meet the daily need for vitamin D.
Breastfed infants
Vitamin D requirements cannot be met by human mi lk alone [4,49], which provides only about 25 IU/L [SO]. A recent review of
reports of nutritional ricket s found that a majority of cases occurred among young, breastfed African Americans [51]. The sun is a
potential source of vi tamin D, but AAP advises keeping infants out of direct sunlight and having them wear protective clothing and
sunscreen [52]. As noted earlier, MP recommends that exclusively and partially breastfed infants be supplemented with 400 IU of
vitamin D per day [20].
Older adults
Americans aged SO and older are at increased risk of developing vitamin D insufficiency [33]. As people age, skin cannot synthesize
vitamin D as efficiently and the kidney is less able to convert vitamin D to its active hormone form [4,53]. As many as half of older
adults in the United States with hip fractures could have serum 2S(OH)D levels <12 ng/ml (<30 nmoi/L) [5] .
People with limited sun exposure
Homebound individuals, people living in northern latitudes (such as New England and Alaska), women who wear long robes and head
coverings for religious reasons, and people with occupations that prevent sun exposure are unlikely to obtain adequate vitamin D
from sunlight [54,55].
People with dark skin
Greater amounts of the pigment melanin result in darker skin and reduce the skin's ability to produce vitamin D from exposure to
sunlight. Some studies suggest that older adults, especially women, with darker skin are at high risk of developing vitamin D
insufficiency [41 ,56]. However, one group with dark skin, African Americans, general ly has lower levels of 25(0H)D yet develops
fewer osteoporotic fractures than Caucasians (see section below on osteoporosis).
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Dietary Supplement Fact Sheet: Vitamin D
People with fat malabsorption
As a fat-soluble vitamin, vitamin D requires some dietary fat in the gut for absorption. Individuals who have a reduced ability to
absorb dietary fat might require vitamin 0 supplements [57]. Fat malabsorption is associated with a variety of medical conditions
including some forms of liver disease, cystic fibrosis, and Crohn's disease [27].
People who are obese or who have undergone gastric bypass surgery
Individuals with a BMI =30 typically have a low plasma concentration of 25(0H)D [58]; this level decreases as obesity and body fat
increase [59]. Obesity does not affect skin's capacity to synthesize vitamin D, but greater amounts of subcutaneous fat sequester
more of the vitamin and alter its release into the circulation. Even with orally administered vitamin D, BMI is inversely correlated
with peak serum concentrations, probably because some vitamin 0 is sequestered in the larger pools of body fat [58]. Obese
individuals who have undergone gastric bypass surgery may become vitamin D deficient without a sufficient intake of this nutrient
from food or supplements, since part of the upper small intestine where vitamin Dis absorbed is bypassed [60,61].
Vitamin D and Health
Optimal serum concentrations of 25(0H)D for bone and general health throughout life have not been established [5, 1 0] and are
likely to vary at each stage of life, depending on the physiological measures selected. The three-fold range of cut points that have
been proposed by various experts, from 16 to 48 ng/ml (40 to 120 nmoi/L), reflect differences in the functional endpoints chosen
(e.g., serum concentrations of parathyroid hormone or bone fractures), as well as differences in the analytical methods used.
In March 2007, a group of vitamin D and nutrition researchers published a controversial and provocative editorial contending that
the desirable concentration of 25(0H)D is =30 ng/ml {=75 nmoi/L) [12]. They noted that supplemental intakes of 400 IU/day of
vitamin D increase 25(0H)D concentrations by only 2.8-4.8 ng/mL (7-12 nmoi/L) and that daily intakes of approximately 1,700 IU
are needed to raise these concentrations from 20 to 32 ng/ml (50 to 80 nmoi/L).
Osteoporosis
More than 25 million adults in the United States have or are at risk of developing osteoporosis, a disease characterized by fragile
bones that significantly increases the risk of bone fractures [62]. Osteoporosis is most often associated with inadequate calcium
intakes (generally <1 ,000-1,200 mg/day}, but insufficient vitamin D contributes to osteoporosis by reducing calcium absorption [63].
Although rickets and osteomalacia are extreme examples of the effects of vitamin D deficiency, osteoporosis is an example of a
long-term effect of calcium and vitamin 0 insufficiency [64]. Adequate storage levels of vitamin D maintain bone strength and might
help prevent osteoporosis in older adults, nonambulatory individuals who have difficulty exercising, postmenopausal women, and
individuals on chronic steroid therapy [65].
Normal bone is constantly being remodeled. During menopause, the balance between these processes changes, resulting in more
bone being resorbed than rebuilt. Hormone therapy with estrogen and progesterone might be able to delay the onset of
osteoporosis. However, some medical groups and professional societies recommend that postmenopausal women consider using
other agents to slow or stop bone resorption because of the potential adverse health effects of hormone therapy [66-68].
Most supplementation trials of t he effects of vitamin D on bone health also include calcium, so it is not possible to isolate the
effects of each nutrient. The authors of a recent evidence-based review of research concluded that supplements of both vitamin D3
(at 700-800 IU/day) and calcium (500-1 ,200 mg/day) decreased the risk of falls, fractures, and bone loss in elderly individuals aged
62-85 years [5]. The decreased risk of fractures occurred primarily in elderly women aged 85 years, on average, and living in a
nursing home. Women should consult their healthcare providers about their needs for vitamin D (and calcium) as part of an overall
plan to prevent or t reat osteoporosis.
African Americans have lower levels of 25(0H)D than Caucasians, yet they develop fewer osteoporotic fractures. This suggests that
factors other than vitamin D provi de protection [69]. African Americans have an advantage in bone density from early childhood, a
function of their more efficient calcium economy, and have a lower risk of fracture even when they have the same bone density as
Caucasians. They also have a higher prevalence of obesity, and the resulting higher estrogen levels in obese women might protect
t hem from bone loss [69]. Further reducing the risk of osteoporosis in African Americans are their lower levels of bone-turnover
markers, shorter hip-axis length, and superior renal calcium conservation. However, despite this advantage in bone density,
osteoporosis is a signifi cant health problem among African Americans as they age [69].
Cancer
Laboratory and animal evidence as well as epidemiologic data suggest that vitamin 0 status could affect cancer risk. Strong
biological and mechanistic bases indicate that vitamin D plays a role in the prevention of colon, prostate, and breast cancers.
Emerging epidemiologic data suggest that vitamin D has a protective effect against colon cancer, but the data are not as strong for
a protective effect against prostate and breast cancer, and are variable for cancers at other sites [70, 71 ]. Studies do not
consistently show a protective effect or no effect, however. One study of Finnish smokers, for example, found that subjects in t he
highest quintile of baseline vitamin D status have a three-fold higher risk of developing pancreatic cancer [72].
Vitamin D emerged as a protective factor in a prospective, cross-sectional study of 3,121 adults aged =50 years (96% men) who
underwent a colonoscopy. The study found that 10% had at least one advanced cancerous lesion. Those with the highest vitamin D
intakes {>645 IU/day) had a significantly lower risk of these lesions [73]. However, the Women's Health Initiative, in which 36,282
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Dietary Supplement Fact Sheet: Vitamin D
postmenopausal women of various races and ethnicities were randomly assigned to receive 400 IU vitamin D plus 1,000 mg calcium
daily or a placebo, found no significant differences between the groups in the incidence of colorectal cancers over 7 years [74].
More recently, a clinical trial focused on bone health i n 1,179 postmenopausal women residing in rural Nebraska found that subj ects
supplemented daily with calcium (1 ,400-1,500 mg) and vitamin 0
3
(1, 100 IU) had a significantly lower incidence of cancer over 4
years compared to women taking a placebo [64] . The small number of cancers reported (50) precludes generalizing about a
protective effect from either or both nutrients or for cancers at different sites. This caution is supported by an analysis of 16,618
participants in NHANES III, where total cancer mortality was found to be unrelated to baseline vitamin D status [76]. However,
colorectal cancer mortality was inversely related to serum 25(0H)D concentrations.
Further research is needed to determine whether vitamin D inadequacy in particular increases cancer risk, whether greater exposure
to the nutrient is protective, and whether some individuals could be at increased risk of cancer because of vitamin D exposure
[70, 77] .
Other conditions
A growing body of research suggests that vitamin D might play some rol e in the prevention and treatment of type 1 [78] and type 2
diabetes [79]. hypertension [80]. glucose i ntolerance [81]. multiple sclerosis [82], and other medical conditions [83,84]. However,
most evidence for these rol es comes from i n vitro, ani mal, and epidemiol ogical studies, not the randomized cl i ni cal trials
considered to be more definitive. Unti l such trials are conducted, the implications of the avai labl e evidence for public health and
patient care will be debated. A systematic review of health outcomes related to vitamin D and calcium i ntakes, both alone and in
combination, was published in August 2009 [85].
A recent meta-analysis found that use of vitamin D supplements was associated with a reduction in overall mortality from any cause
by a statistically signifi cant 7% [86,87]. The subj ects in these trials were pri mari ly healthy, middl e aged or elderly, and at high risk
of fractures; they took 300-2,000 IU/day of vitamin D supplements.
Health Risks from Excessive Vitamin D
Vitamin D toxicity can cause nonspecific symptoms such as nausea, vomiting, poor appetite, constipation, weakness, and weight loss
[88]. More seriously, it can also raise blood levels of calci um, causing mental status changes such as confusion and heart rhythm
abnormali ties [7]. The use of supplements of both calcium (1 ,000 mg/day) and vitamin D (400 IU/day) by postmenopausal women
was associated with a 17% increase in the risk of kidney stones over 7 years in the Women's Health Initiative [89] . Deposition of
calcium and phosphate in the kidneys and other soft tissues can also be caused by excessive vitamin D levels [47]. A serum 25(0H)D
concentration consistently >200 ng/ml (>500 nmoi/L) is considered to be pot entially toxic [11 ] . In an animal model, concentrations
=400 ng/ml (=1,000 nmoi/L) were not associated with harm [ 14].
Excessive sun exposure does not result in vitamin D toxi city because the sust ained heat on the skin is thought to photodegrade
previtamin 0
3
and vitamin 0
3
as it is formed [10,35]. High intakes of dietary vitami n Dare very unlikely to result in toxicity unless
large amounts of cod liver oil are consumed; toxicity is more likely to occur from high intakes of supplements.
Long-term int akes above the UL increase the risk of adverse health effects [4] (Table 4). Substantially larger doses administered for
a short time or periodically (e.g., 50,000 IU/week for 8 weeks) do not cause toxicity. Rather, the excess is stored and used as
needed to maintain normal serum 25(0H)D concentrations when vitamin D intakes or sun exposure are limited [ 11, 90].
T bl 4 T I bl U a e : o era e 1pper nta e eve s or 1tamm k l I (Uls) f v
. D [4]
I
Age II Childrenll Men II Women IIPregnancyiiLactation I
Birth to 12 months
25 meg
CJCJI II I
(1 ,000 IU)
11-13 years
ISO meg
. (2,000 IU)
CJCJI II I
114+ years meg meg meg
. (2,000 IU) (2,000 IU) (2,000 IU)
meg
(2,000 IU)
Several nutrition scientists recently challenged these Uls, first published in 1997 [90]. They point to newer clinical trials conducted
in healthy adults and conclude that t he data support aULas high as 10,000 IU/day. Although vitamin D supplements above
recommended levels given in clinical trials have not shown harm, most trials were not adequately designed to assess harm [5].
Evidence is not sufficient to determine the potential risks of excess vitamin D in infants, children, and women of reproductive age.
As noted earlier, the FNB is current ly reviewi ng data to determine whether updates to the ORis (incl uding the Uls) for vitamin Dare
appropriate [4].
Interactions with Medications
Vitamin D suppl ements have the potential to interact with several types of medications. A few examples are provided below.
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Dietary Supplement Fact Sheet: Vitamin D
Individuals taking these medications on a regular basis should discuss vitamin D intakes with their healthcare providers.
Steroids
Corticosteroid medications such as prednisone, often prescri bed to reduce inflammation, can reduce calcium absorption [ 91-93] and
impair vitamin D metaboli sm. These effects can further contribut e t o the loss of bone and the development of osteoporosis
associated with their long-term use [ 92, 93].
Other medications
Both the weight-loss drug orli stat (brand names Xenical and aiiPM) and the cholesterol-lowering drug cholestyramine (brand names
Questran, LoCholest, and Prevalite) can reduce the absorption of vitamin D and other fat-soluble vitamins [ 94,95]. Both
phenobarbital and phenytoin (brand name Dilantin), used to prevent and control epi l eptic seizures, increase the hepatic
metabolism of vitamin D t o inactive compounds and reduce calcium absorption [96].
Vitamin D and Healthful Diets
According to the 2005 Dietary Guidelines for Americans, "nutrient needs should be met primarily through consuming foods. Foods
provide an array of nut rient s and other compounds that may have beneficial effects on health. I n cert ain cases, fortified foods and
dietary supplements may be useful sources of one or more nutrients that otherwise might be consumed i n less than recommended
amounts. However, dietary supplements, while recommended in some cases, cannot replace a healthful diet. "
The Dietary Guidelines for Americans describes a healthy di et as one that
Emphasizes a variety of fruits, vegetables, whole grains, and fat-free or low-fat milk and milk products.
Mil k is fortified with vitamin D, as are many ready-to-eat cereals and a few brands of yogurt and orange j uice. Cheese
naturall y contains small amounts of vitamin D.
Incl udes lean meats, poultry, fish, beans, eggs, and nuts.
Fish such as salmon, tuna, and mackerel are very good sources of vitamin D. Small amounts of vitamin D are also found
in beef liver and egg yolks.
Is low in saturated fats, trans fats, cholesterol, salt (sodium}, and added sugars.
Vitamin D is added to some margarines.
Stays within your dail y calorie needs.
For more informat ion about building a healthful diet, refer to the Dietary Guidelines for Americans
(http:/ /www.health.gov/djetaryguidelines/dga2005/document/default.htm) and the U.S. Department of Agriculture's food guidance
system, My Pyramid (http:/ /www.mypyramid. gov).
References
1. Deluca HF, Zierold C. Mechanisms and functions of vitamin D. Nutr Rev 1998;56:54-10. [PubMed abstract]
2. Deluca HF. Overview of general physiologic features and functions of vitamin D. Am j Clin Nut r 2004;80:1689S-96S. [PubMed
abstract]
3. van den Berg H. Bioavailability of vitamin D. Eur j Clin Nutr 1997;51 :576-9. [PubMed abstract]
4. Institute of Medi cine, Food and Nutrition Board. Dietary Reference Intakes: Calcium, Phosphorus, Magnesium, Vitamin D, and
Fluoride. Washington, DC: National Academy Press, 1997.
5. Cranney C, Horsely T, O'Donnell S, Weil er H, Ooi D, Atkinson S, et al. Effectiveness and safety of vitamin D. Evidence
Report/Technology Assessment No. 158 prepared by the University of Ottawa Evidence-based Practice Center under Contract
No. 290-02.0021. AHRQ Publication No. 07-E013. Rockville, MD: Agency for Heal t hcare Research and Qual ity, 2007. [PubMed
abstract]
6. Goldring SR, Krane S, Avioli LV. Disorders of calcification: osteomalacia and rickets. In: DeGroot Lj, Besser M, Burger HG,
jameson j L, Loriaux DL, Marshall j C, et al., eds. Endocrinology. 3rd ed. Philadelphia: WB Saunders, 1995:1204-27.
7. Favus Mj, Christakos S. Pri mer on the Metabolic Bone Diseases and Disorders of Mineral Metaboli sm. 3rd ed. Phi ladelphia, PA:
Lippincott-Raven, 1996.
8. Holick MF. Evol ution and function of vitami n D. Recent results. Cancer Res 2003; 164:3-28. [PubMed abstract]
9. Hayes CE, Hashold FE, Spach KM, Pederson LB. The immunological functions of the vitamin D endocri ne system. Cell Mol Bioi
2003;49:277-300. [ PubMed abstract]
10. Holick MF. Vitamin D deficiency. N Englj Med 2007;357:266-81. [PubMed abstract]
11 . j ones G. Pharmacokinetics of vitamin D toxicity. Am j Clin Nutr 2008;88:582S-6S. [PubMed abstract]
12. Vieth R, Bischoff-Ferrari H, Boucher Bj, Dawson-Hughes B, Garland CF, Heaney RP, et al. The urgent need to recommend an
i ntake of vitamin D that is effective. Am j Clin Nutr 2007;85: 649-50. [PubMed abstract]
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Dietary Supplement Fact Sheet: Vitamin D
13. Scientific Advisory Committee on Nutrition. Update on Vitamin D. Position Statement by the Scientific Advisory Committee on
Nutrition. London: The Stationery Office, Limited, 2007.
14. Shepard RM, Deluca HF. Plasma concentrations of vitamin D3 and its metabolites in the rat as influenced by vitamin D3 or
245-hydroxyvitamin D3 intakes. Arch Biochem Biophys 1980;202:43-53. [PubMed abstract]
15. Carter GD. 25-hydroxyvitamin D assays: the quest for accuracy. Clio Chern 2009;55:1300-02.
16. Hollis BW. Editorial: the determination of circulating 25-hydroxyvitamin D: no easy task. j. Clio Endocrinol Metab
2004;89:3149-3151.
17. Lensmeyer GL, Wiebe DA, Binkley N, Drezner MK. HPLC method for 25-hydroxyvitamin D measurement: comparison with
contemporary assays. Clio Chern 2006;52:1120-26. [PubMed abstract]
18. Binkley N, Krueger D, Cowgill CS, Plum L, Lake E, Hansen KE, et al. Assay variation confounds the diagnosis of
hypovitaminosis D: a call for standardization. J Clio Endocrinol Metab 2004;89:3152-57. [PubMed abstract]
19. National Institute of Standards and Technology. NIST releases vitamin D standard reference material, 2009.
20. Wagner CL, Greer FR; American Academy of Pediatrics Section on Breastfeeding; American Academy of Pediatrics Committee
on Nutrition. Prevention of rickets and vitamin D deficiency in infants. children. and adolescents . Pediatrics 2008;122: 11 42-
1152. [PubMed abstract]
21. Yetley EA, Brule D, Cheney MC, Davis CD, Esslinger KA, Fischer PWF, et al. Dietary Reference Intakes for vitamin D:
justification for a review of the 1997 values. Am J Clio Nutr 2009;89:719-27. [PubMed abstract]
22. Institute of Medicine, Food and Nutrition Board. Pietary Reference Intakes for vitamin p and calcium.
23. Ovesen L, Brot (,Jakobsen J. Food contents and biological activity of 25-hydroxyvitamin D: a vitamin D metabolite to be
reckoned with? Ann Nutr Metab 2003;47:1 07-13. [PubMed abstract]
24. Mattila PH, Piironen VI, Uusi-Rauva EJ, Koivistoinen PE. Vitamin D contents in edible mushrooms. J Agric Food Chern
1994;42:2449-53.
25. Outila TA, Mattila PH, Piironen VI, Lamberg-AIIardt CJ E. Bioavailability of vitamin D from wild edible mushrooms
(Cantharellus tubaeformis) as measured with a human bioassay. Am j Clio Nutr 1999;69:95-8. [PubMed abstract]
26. Calvo MS, Whiting SJ, Barton CN. Vitamin D fortification in the United States and Canada: current status and data needs. Am
j Clio Nutr 2004;80:171 OS-6S. [PubMed abstract]
27. Holick MF. Vitamin D. In: Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ, eds. Modern Nutrition in Health and Disease,
10th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.
28. PenningtonjA, DouglassjS. Bowes and Church's Food Values of Portions Commonly Used. 18th ed. Philadelphia: Lippincott
Williams & Wilkins, 2004.
29. Nutrition Coordinating Center. Nutrition Data System for Research (NDS-R). Version 4.06/34. Minneapolis: University of
Minnesota, 2003.
30. U.S. Department of Agriculture, Agricultural Research Service. USDA Nutrient Database for Standard Reference. Release 22,
2009.
31. Byrdwell we, DeVriesj, Exler J , Harnly JM, Holden J M, Holick MF, et al. Analyzing vitamin Din foods and supplements:
methodologic challenges. Am J Cli o Nutr 2008;88:554S-7S. [PubMed abstract]
32. Holick MF. McCollum Award Lecture, 1994. Vitamin D: new horizons for the 21st century. Amj Clio Nutr 1994;60:619-30.
[PubMed abstract]
33. Holick MF. Vitamin D: the underappreciated D-lightful hormone that is important for skeletal and cellular health. Curr Opin
Endocrinol Diabetes 2002;9:87-98.
34. Wharton B, Bishop N. Rickets. Lancet 2003;362:1389-400. [PubMed abstract]
35. Holick MF. Photobiology of vitamin D. In: Feldman D, PikejW, Glorieux FH, eds. Vitamin D, Second Edition, Volume I.
Burlington, MA: Elsevier, 2005.
36. Wolpowitz D, Gilchrest BA. The vitamin D questions: how much do you need and how should you get it? J Am Acad Dermatol
2006;54:301 -1 7. [PubMed abstract]
37. International Agency for Research on Cancer Working Group on ultraviolet (UV) light and skin cancer. The association of use
of sunbeds with cutaneous malignant melanoma and other skin cancers: a systematic review. Intj Cancer 2006;120:1116-22.
[PubMed abstract]
38. American Academy of Dermatology. Position statement on vitamin D. November 1, 2008.
39. Armas LAG, Hollis BW, Heaney RP. Vitamin D2 is much less effective than vitamin D3 in humans. J Clio Endocrinol Metab
2004;89:5387-91. [ PubMed abstract]
40. Houghton LA, Vieth R. The case against ergocalciferol (vi tamin D2) as a vi tamin supplement. Am J Clio Nutr 2006;84:694-7.
[PubMed abstract]
41. Nesby-O' Dell S, Scanlon KS, Cogswell ME, Gillespie C, Hollis BW, Looker AC, et al. Hypovitaminosis D prevalence and
determinants among African-American and white women of reproductive age: thi rd National Health and Nutrition Examination
Survey, 1988-1994. Am j Clio Nutr 2002;76: 187-92. [PubMed abstract]
42. Yetley EA. Assessing the vitamin D status of the US population. Am J Clio Nutr 2008;88:558S-64S. [PubMed abstract]
43. Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US
population: 1988-1994 compared with 2000-2004. Am J Clio Nutr 2008;88:1519-27. [PubMed abstract]
44. Ginde AA, Liu MC, Camargo J r, CA. Demographic differences and trends of vitamin D insufficiency in the US population, 1988-
2004. Arch Intern Med 2009;169:626-32. [PubMed abstract]
45. National Center for Health Statistics. Analytical note for NHANES 2000-2006 and NHANES III 0988 -1994) 25-hydroxyyitamin D
analysis, 2009.
46. Moshfegh A, Goldman J, Ahuja J, Rhodes D, LaComb R. 2009. What We Eat in America, NHANES 2005-2006: Usual Nutrient
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Dietary Supplement Fact Sheet: Vitamin D
Intakes from Food and Water Compared to 1997 Dietary Reference Intakes for Vitamin D, Calcium, Phosphorus, and
Magnesium. U.S. Department of Agriculture, Agricultural Research Service. [http://www.ars.usda.gov/ba/bhnrc/fsrg]
47. Biser-Rohrbaugh A, Hadley-Miller N. Vitamin D deficiency in breast-fed toddlers.J Pediatr Orthop 2001;21:508-11. [PubMed
abstract]
48. Chesney R. Rickets: an old form for a new century. Pediatr Int 2003;45: 509-11. [PubMed abstract]
49. Picciano MF. Nutrient composition of human milk. Pediatr Clin North Am 2001 ;48:53-67. [PubMed abstract]
50. Gartner LM, Greer FR, American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D
deficiency: new guidelines for vitamin D intake. Pediatrics 2003:111 :908-10. [PubMed abstract]
51. Weisberg P, Scanlon KS, Li R, Cogswell ME. Nutritional r ickets among children in the United States: review of cases reported
between 1986 and 2003. Am J Clin Nutr 2004;80:16975-7055. [PubMed abstract]
52. American Academy of Pediatrics Committee on Environmental Health. Ultraviolet light: a hazard to chi ldren. Pediatrics
1999;104:328-33. [PubMed abstract]
53. Need AG, Morris HA, Horowitz M, Nordin C. Effects of skin thickness, age, body fat, and sunlight on serum 25-hydroxyvitamin
D. Am J Clin Nutr 1993;58:882-5. [PubMed abstract]
54. Webb AR, Kline L, Holick MF. I nfluence of season and latitude on the cutaneous synthesis of vitamin 03: Exposure to winter
sunlight in Boston and Edmonton will not promote vitamin 03 synthesis in human skin. J Clin Endocrinol Metab 1988;67:373-8.
[PubMed abstract]
55. Webb AR, Pilbeam C, Hanafin N, Holick MF. An evaluation of the relative contributions of exposure to sunlight and of diet to
the circulating concentrations of 25-hydroxyvitamin D in an elderly nursing home population in Boston. Am J Clin Nutr
1990;51 :1075-81. [PubMed abstract]
56. Harris 55, Soteriades E, Coolidge JAS, Mudgal S, Dawson-Hughes B. Vitamin D insufficiency and hyperparathyroidism in a low
income, multiracial, elderly population. J Clin Endocrinol Metab 2000;85:4125-30. [PubMed abstract]
57. Lo CW, Paris PW, Clemens TL, Nolan J, Holick MF. Vitamin D absorption in healthy subjects and in patients with intestinal
malabsorption syndromes. Am J Clin Nutr 1985;42:644-49. [PubMed abstract]
58. Wortsman J, Matsuoka LV, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr
2000;72:690-3. [PubMed abstract]
59. Vilarrasa N, MaravaiiJ, Estepa A, Sanchez R, Masdevall C, Navarro MA, et al. Low 25-hydroxyvitamin D concentrations in
obese women: their clinical significance and relationship with anthropometric and body composition variables. J Endocrinol
Invest 2007;30:653-8. [PubMed abstract]
60. Malone M. Recommended nutritional supplements for bariatric surgery patients. Ann Pharmacother 2008;42:1851-8. [PubMed
abstract]
61. Compher CW, Badellino KO, Boullatajl. Vitamin D and the bariatric surgical patient: a review. Obes Surg 2008;18:220-4.
[PubMed abstract]
62. Reid IR. The roles of calcium and vitamin Din the prevention of osteoporosis. Endocrinol Metab Clin North Am 1998;27: 389-
98. [PubMed abstract]
63. Heaney RP. Long-latency deficiency di sease: insights from calcium and vitamin D. AmJ Clin Nutr 2003;78:912-9. [PubMed
abstract]
64. Parfitt AM. Osteomalacia and related disorders. In: Avioli LV, Krane SM, eds. Metabolic bone disease and clinically related
disorders. 2nd ed. Philadelphia: WB Saunders, 1990:329-96.
65. LeBoff MS, Kohlmeier L, Hurwitz S, Franklin J, Wright J, Glowackij. Occult vitamin D deficiency in postmenopausal US
women with acute hip fracture. JAMA 1999;251 :1505-11. [PubMed abstract]
66. Kirschstein R. Menopausal hormone therapy: summary of a scientific workshop. Ann Intern Med 2003;138:361-4. [PubMed
abstract]
67. American College of Obstetricians and Gynecologists. Frequently Asked Questions About Hormone Therapy. Nm
Recommendations Based on ACOG's Task Force Report on Hormone Therapy.
68. North American Menopause Society. Role of progestrogen in hormone therapy for postmenopausal women: position statement
of The North American Menopause Society. Menopause 2003;10:113-32. [PubMed abstract]
69. Aloia JF. African Americans, 25-hydroxyvitamin D, and osteoporosis: a paradox. Am J Clin Nutr 2008;88:5455-505. [PubMed
abstract]
70. Davis CD. Vitamin D and cancer: current dilemmas and future research needs. Am J Clin Nutr 2008;88:5655-95. [PubMed
abstract]
71. Davis CD, Hartmuller V, Freedman M, Hartge P, Picciano MF, Swanson CA, Milner JA. Vitamin D and cancer: current dilemmas
and future needs. Nutr Rev 2007;65:S71 -S74. [PubMed abstract]
72. Stolzenberg-Solomon RZ, Vieth R, Azad A, Pietinen P, Taylor PR, Virtamo J, et al. A prospective nested case-control study of
vitamin D status and pancreatic cancer ri sk in male smokers. Cancer Res 2006;66:1 0213-9. [PubMed abstract]
73. Lieberman DA, Prindiville S, Weiss DG, Willett W. Risk factors for advanced colonic neoplasia and hyperplastic polyps in
asymptomatic individuals. JAMA 2003;290:2959-67. [PubMed abstract]
74. Wactawski-Wende J, Kotchen J M, Anderson GL, Assaf AR, Brunner RL, O'Sullivan MJ, et al. Calcium plus vitamin D
supplementation and the risk of colorectal cancer. N Eng I J Med 2006;354:684-96. [PubMed abstract]
75. LappeJM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP. Vitamin D and calcium supplementation reduces cancer
risk: results of a randomized trial. Am J Clin Nutr 2007;85:1586-91. [PubMed abstract]
76. Freedman OM, Looker AC, Chang S-C, Graubard Bl. Prospective study of serum vitamin D and cancer mortality in the United
States. J Natl Cancer I nst 2007;99:1594-602. [PubMed abstract]
77. Davis CD, Dwyer JT. The 'sunshine vitamin': benefits beyond bone? J Nat I Cancer Inst 2007;99:1563-5. [PubMed abstract]
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Dietary Supplement Fact Sheet: Vitamin D
78. Hypponen E, Uiara E, Reunanen A, jarvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort
study. Lancet 2001 ;358: 1500-3. [PubMed abstract]
79. Pittas AG, Dawson-Hughes B, Li T, Van Dam RM, Willett we, Manson J E, et al. Vitamin D and calcium intake in relation to
type 2 diabetes in women. Diabetes Care 2006;29:650-6. [PubMed abstract]
80. KrauseR, BUhring M, HopfenmUIIer W, Holick MF, Sharma AM. Ultraviolet Band blood pressure. Lancet 1998;352:709-10.
[PubMed abstract]
81. Chiu KC, ChuA, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin
Nutr 2004;79:820-5. [PubMed abstract]
82. Munger KL, Levi n LI, Hollis BW, Howard NS, Asche rio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA
2006;296:2832-8. [PubMed abstract]
83. Merlino LA, Curtis J, Mikuls TR, Cerhan J R, Criswell LA, Saag K. Vitamin D intake is inversely associated with rheumatoid
arthritis: results from the Iowa Women's Health Study. Arthritis Rheum 2004;50:72-7. [PubMed abstract]
84. Schleithoff SS, Zittermann A, Tenderich G, Berthold HK, Stehle P, Koerfer R. Vitamin D supplementation improves cytokine
profi les in patients with congestive heart failure: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr
2006;83:754-9. [PubMed abstract]
85. Chung M, Balk EM, Brendel M, IpS, Lauj, Leej, et al. Vitamin D and calcium: a systematic review of health outcomes.
Evidence Report/Technology Assessment No. 183 prepared by the Tufts Evidence-based Practice Center under Contract No.
290-2007-10055-I. AHRQ Publication No. 09-E015. Rockville, MD: Agency for Healthcare Research and Quality, 2009.
86. Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized control led t rials. Arch
Intern Med 2007;167:1730-7. [PubMed abstract]
87. Giovannucci E. Can vitamin D reduce total mortality? Arch Intern Med 2007;167:1709-10. [PubMed abstract]
88. Chesney RW. Vitamin D: can an upper limit be defined?J Nutr 1989;119 (12 Suppl):1825-8. [PubMed abstract]
89. jackson RD, LaCroix AZ, Gass M, Wallace RB, RobbinsJ, Lewis CE, et al. Calcium plus vitamin D supplementation and the risk
of fractures. N Engl J Med 2006;354:669-83. [PubMed abstract]
90. HathcockJN, Shao A, Vieth R, Heaney R. Risk assessment for vitamin D. AmJ Clin Nutr 2007;85:6-18. [PubMed abstract]
91. Buckley LM, Leib ES, Cartularo KS, Vacek PM, Cooper SM. Calcium and vitamin D3 supplementation prevents bone loss in the
spine secondary to low-dose corticosteroids in patients with rheumatoid arthritis. A randomized, double-blind, placebo-
controlled trial. Ann Intern Med 1996;125:961-8. [PubMed abstract]
92. Lukert BP, Raisz LG. Glucocorticoid- induced osteoporosis: pathogenesis and management. Ann Intern Med 1990;112:352-64.
[PubMed abstract]
93. de Sevaux RGL, Hoitsma AJ, Carstens FHM, Wetzels J FM. Treatment with vitamin D and calcium reduces bone loss after renal
transplantation: a randomized study. J Am Soc Nephrol 2002;13:1608-14. [PubMed abstract]
94. McDuffie J R, Calis KA, Booth SL, Uwaifo GI, Yanovski JA. Effects of orlistat on fat-soluble vitamins in obese adolescents.
Pharmacotherapy 2002;22:814-22. [PubMed abstract]
95. Compston J E, Horton LW. Oral 25-hydroxyvitamin D3 i n treatment of osteomalacia associated with ileal resection and
cholestyramine therapy. Gastroenterology 1978;74:900-2. [PubMed abstract]
96. Gough H, Goggin T, Bissessar A, Baker M, Crowley M, Callaghan N. A comparative study of the relative infl uence of different
anticonvulsant drugs, UV exposure and diet on vitamin D and calcium metabolism in outpatients with epilepsy. Q J Med
1986;59:569-77. [PubMed abstract]
Disclaimer
Reasonable care has been taken in preparing this document and the information provided herein is believed to be accurate.
However, this i nformation is not intended to constitute an "authoritative statement" under Food and Drug Administration rules
and regulations.
About ODS
The mission of the Office of Dietary Supplements (ODS) is to strengthen knowledge and understanding of dietary supplements by
evaluating scientific information, stimulating and supporting research, disseminating research results, and educating the public to
foster an enhanced quality of life and health for the U.S. population.
General Safety Advisory
Health professionals and consumers need credible i nformat ion t o make thoughtful decisions about eating a healthful diet and
using vitamin and mineral supplements. These Fact Sheets provide responsible information about the role of vitamins and
minerals in health and disease. Each Fact Sheet in this series received extensive review by recognized experts from the academic
and research communities.
The information is not intended to be a substitute for professional medical advice. It is important to seek the advice of a
physician about any medical condition or symptom. It is also important to seek t he advice of a physician, registered dietitian,
http://dietary-supplements.info.nih.gov/factsheets!VitaminD_pf.asp[l2/l/2009 8:09:29 PM]
Das könnte Ihnen auch gefallen
- NYT Amicus Brief For MeltwaterDokument36 SeitenNYT Amicus Brief For Meltwaterjeff_roberts881Noch keine Bewertungen
- The Public Availability of Warn Notices: Lack of Accessibility and Disclosure Calls For ReformDokument23 SeitenThe Public Availability of Warn Notices: Lack of Accessibility and Disclosure Calls For ReformProgressTXNoch keine Bewertungen
- Issa Letter 20110105Dokument3 SeitenIssa Letter 20110105loren_steffyNoch keine Bewertungen
- UANMDFAQDokument2 SeitenUANMDFAQUANoMoreDeathsNoch keine Bewertungen
- Research Paper On News MediaDokument8 SeitenResearch Paper On News Mediacapz4pp5100% (1)
- This Content Downloaded From FF:FFFF:FFFF:FFFF:FFFF:FFFF:FFFF:FFFF On Thu, 01 Jan 1976 12:34:56 UTCDokument33 SeitenThis Content Downloaded From FF:FFFF:FFFF:FFFF:FFFF:FFFF:FFFF:FFFF On Thu, 01 Jan 1976 12:34:56 UTCKuthu BhaiNoch keine Bewertungen
- Questions To Ask When Employees Are Disparaged by OutsidersDokument13 SeitenQuestions To Ask When Employees Are Disparaged by Outsidersdan_michalukNoch keine Bewertungen
- Reprint SamplesDokument3 SeitenReprint SamplesscribdsgayNoch keine Bewertungen
- ICW Bartlesville 9-22-13Dokument1 SeiteICW Bartlesville 9-22-13Price LangNoch keine Bewertungen
- Letter For The Record To Members of The House Committee On Energy and Commerce On Facebook, Transparency and Use of Consumer DataDokument4 SeitenLetter For The Record To Members of The House Committee On Energy and Commerce On Facebook, Transparency and Use of Consumer DataThe Committee for JusticeNoch keine Bewertungen
- The CorporationDokument4 SeitenThe CorporationGlory Mae OraaNoch keine Bewertungen
- Corporate Law II - ProjectDokument29 SeitenCorporate Law II - ProjectSumathy AsviniNoch keine Bewertungen
- Research Paper Over ObamacareDokument7 SeitenResearch Paper Over Obamacareafedetbma100% (1)
- Asbestos companies' ethical dilemmaDokument5 SeitenAsbestos companies' ethical dilemmaAster DemissieNoch keine Bewertungen
- ConsumeramicusDokument34 SeitenConsumeramicuslegalmattersNoch keine Bewertungen
- Elle Ourso Writing SamplesDokument6 SeitenElle Ourso Writing SampleselleoursoNoch keine Bewertungen
- Research Paper On Johnson JohnsonDokument5 SeitenResearch Paper On Johnson Johnsonafeaxbgqp100% (1)
- MR Saheed Organization and StrategyDokument4 SeitenMR Saheed Organization and StrategyMoshoodNoch keine Bewertungen
- IB311: Ethical Issues in International BusinessDokument69 SeitenIB311: Ethical Issues in International BusinessSiri SirisakdiwanNoch keine Bewertungen
- Capitol Hill BeaconDokument1 SeiteCapitol Hill BeaconPrice LangNoch keine Bewertungen
- House Hearing, 113TH Congress - The Health Insurance Fee: Impact On Small BusinessesDokument55 SeitenHouse Hearing, 113TH Congress - The Health Insurance Fee: Impact On Small BusinessesScribd Government DocsNoch keine Bewertungen
- Contemporary Vocabulary GuideDokument5 SeitenContemporary Vocabulary GuideSaskia LourensNoch keine Bewertungen
- ALA Brief Ct. App. May 24, 2010Dokument28 SeitenALA Brief Ct. App. May 24, 2010BK AinsworthNoch keine Bewertungen
- Senate Hearing, 111TH Congress - Deceptive Health Insurance Industry Practices: Are Consumers Getting What They Paid For? - Part IiDokument42 SeitenSenate Hearing, 111TH Congress - Deceptive Health Insurance Industry Practices: Are Consumers Getting What They Paid For? - Part IiScribd Government DocsNoch keine Bewertungen
- Proffesional EthicsDokument15 SeitenProffesional EthicsROSE THERASANoch keine Bewertungen
- Senate Hearing, 110TH Congress - Preparing For The Digital Television Transition: Will Seniors Be Left in The Dark?Dokument165 SeitenSenate Hearing, 110TH Congress - Preparing For The Digital Television Transition: Will Seniors Be Left in The Dark?Scribd Government DocsNoch keine Bewertungen
- 1Dokument68 Seiten1Kunwar Mahipal Singh KheecheeNoch keine Bewertungen
- Scott Neal E-Cigarette E-Mails (FOIA Request To King County Health Department)Dokument1.574 SeitenScott Neal E-Cigarette E-Mails (FOIA Request To King County Health Department)American Vaping AssociationNoch keine Bewertungen
- Corporate Law 2Dokument17 SeitenCorporate Law 2Sumathy AsviniNoch keine Bewertungen
- The Corporation Summary AnalysisDokument3 SeitenThe Corporation Summary AnalysisAlmira RoblesNoch keine Bewertungen
- Monday - Michael Winn StudyDokument3 SeitenMonday - Michael Winn StudyTom SnyderNoch keine Bewertungen
- Senate Hearing, 110TH Congress - Surgeons For Sale: Conflicts and Consultant Payment in The Medical Device IndustryDokument109 SeitenSenate Hearing, 110TH Congress - Surgeons For Sale: Conflicts and Consultant Payment in The Medical Device IndustryScribd Government DocsNoch keine Bewertungen
- Federal Anti-SLAPP Law Needed to Protect Free SpeechDokument13 SeitenFederal Anti-SLAPP Law Needed to Protect Free SpeechNitesh dhankhar100% (1)
- Jurnal CorporateDokument16 SeitenJurnal CorporateRatih Frayunita SariNoch keine Bewertungen
- HHRG 116 VR08 Wstate DevineT 20190625Dokument25 SeitenHHRG 116 VR08 Wstate DevineT 20190625mikekvolpeNoch keine Bewertungen
- Thesis Thomas EggarDokument5 SeitenThesis Thomas Eggarlupitavickreypasadena100% (1)
- Claremore ICW PrintDokument1 SeiteClaremore ICW PrintPrice LangNoch keine Bewertungen
- Affordable Healthcare: A Big Problem For Small BusinessesDokument60 SeitenAffordable Healthcare: A Big Problem For Small BusinessesScribd Government DocsNoch keine Bewertungen
- Thesis Statement For Human ServicesDokument5 SeitenThesis Statement For Human Servicesmariestarsnorthlasvegas100% (2)
- Spooky BusinessDokument54 SeitenSpooky Businesssuasponte2Noch keine Bewertungen
- Behavioral Advertising - The Offer You Cant Refuse PDFDokument25 SeitenBehavioral Advertising - The Offer You Cant Refuse PDFIgor PachecoNoch keine Bewertungen
- House Hearing, 110TH Congress - Full Committee Hearing On Expanding Small Business Health Insurance Coverage Using The Private Reinsurance MarketDokument67 SeitenHouse Hearing, 110TH Congress - Full Committee Hearing On Expanding Small Business Health Insurance Coverage Using The Private Reinsurance MarketScribd Government DocsNoch keine Bewertungen
- Faulty Lawyers HitDokument5 SeitenFaulty Lawyers HitMelody EstebanNoch keine Bewertungen
- Research Paper FullDokument6 SeitenResearch Paper Fullgz9avm26100% (1)
- Innovation in The Aging Network: The Future of Social Services For Older AmericansDokument413 SeitenInnovation in The Aging Network: The Future of Social Services For Older AmericansScribd Government DocsNoch keine Bewertungen
- Senate Hearing, 113TH Congress - Delivering Better Health Care Value To Consumers: The First Three Years of The Medical Loss RatioDokument73 SeitenSenate Hearing, 113TH Congress - Delivering Better Health Care Value To Consumers: The First Three Years of The Medical Loss RatioScribd Government DocsNoch keine Bewertungen
- House Hearing, 112TH Congress - Hearing On Reducing Federal Agency Overreach: Modernizing The Regulatory Flexibility ActDokument75 SeitenHouse Hearing, 112TH Congress - Hearing On Reducing Federal Agency Overreach: Modernizing The Regulatory Flexibility ActScribd Government DocsNoch keine Bewertungen
- Encouraging Internal WhistleblowingDokument8 SeitenEncouraging Internal WhistleblowingMissi Missi ANoch keine Bewertungen
- Research Paper Government ControlDokument5 SeitenResearch Paper Government Controlfvja66n5100% (1)
- Senate Hearing, 111TH Congress - Deceptive Health Insurance Industry Practices: Are Consumers Getting What They Paid For? - Part IDokument58 SeitenSenate Hearing, 111TH Congress - Deceptive Health Insurance Industry Practices: Are Consumers Getting What They Paid For? - Part IScribd Government DocsNoch keine Bewertungen
- Goris ATMAE WifiDokument12 SeitenGoris ATMAE Wifihamza laouajNoch keine Bewertungen
- The New Lawsuit Ecosystem: Trends, Targets and PlayersDokument164 SeitenThe New Lawsuit Ecosystem: Trends, Targets and PlayersU.S. Chamber of Commerce50% (2)
- The Center For Consumer Information and Insurance Oversight, and The Anniver-Sary of The Patient Protection and Affordable Care ActDokument87 SeitenThe Center For Consumer Information and Insurance Oversight, and The Anniver-Sary of The Patient Protection and Affordable Care ActScribd Government DocsNoch keine Bewertungen
- Voluntary Carbon Offsets: Getting What You Pay For: HearingDokument184 SeitenVoluntary Carbon Offsets: Getting What You Pay For: HearingScribd Government DocsNoch keine Bewertungen
- Credit Report Disputes Are A Shell Game - Admitted in Testimony To SubcommiteeDokument11 SeitenCredit Report Disputes Are A Shell Game - Admitted in Testimony To Subcommitee83jjmackNoch keine Bewertungen
- The California Privacy Rights Act (CPRA) – An implementation and compliance guideVon EverandThe California Privacy Rights Act (CPRA) – An implementation and compliance guideNoch keine Bewertungen
- The California Consumer Privacy Act (CCPA): An implementation guideVon EverandThe California Consumer Privacy Act (CCPA): An implementation guideBewertung: 4 von 5 Sternen4/5 (2)
- Managing Privacy: Information Technology and Corporate AmericaVon EverandManaging Privacy: Information Technology and Corporate AmericaNoch keine Bewertungen
- 2016 12 30 Responsive DocumentsDokument15 Seiten2016 12 30 Responsive DocumentsCREWNoch keine Bewertungen
- Via Electronic Mail OnlyDokument2 SeitenVia Electronic Mail OnlyCREWNoch keine Bewertungen
- 2017-01-06 Documents Produced 1Dokument365 Seiten2017-01-06 Documents Produced 1CREWNoch keine Bewertungen
- 2017-01-06 Final ResponseDokument2 Seiten2017-01-06 Final ResponseCREWNoch keine Bewertungen
- FBN Materials 422.15Dokument64 SeitenFBN Materials 422.15CREWNoch keine Bewertungen
- 2016 12 16 FOIA RequestDokument3 Seiten2016 12 16 FOIA RequestCREWNoch keine Bewertungen
- 2016 12 16 FOIA RequestDokument3 Seiten2016 12 16 FOIA RequestCREWNoch keine Bewertungen
- 2016 12 28 Final ResponseDokument2 Seiten2016 12 28 Final ResponseCREWNoch keine Bewertungen
- 2017-01-06 Documents Produced 2Dokument36 Seiten2017-01-06 Documents Produced 2CREWNoch keine Bewertungen
- 2016-12-21 FOIA Request (Documents To Congress)Dokument3 Seiten2016-12-21 FOIA Request (Documents To Congress)CREWNoch keine Bewertungen
- New York Office of The Attorney General (Trump Foundation Investigation) Request 9-14-16Dokument2 SeitenNew York Office of The Attorney General (Trump Foundation Investigation) Request 9-14-16CREWNoch keine Bewertungen
- FOIA Request - OGE (Trump Transition) 12-7-16Dokument3 SeitenFOIA Request - OGE (Trump Transition) 12-7-16CREWNoch keine Bewertungen
- 2016-12-21 FOIA Request (Communications With Trump and Congress)Dokument3 Seiten2016-12-21 FOIA Request (Communications With Trump and Congress)CREWNoch keine Bewertungen
- Florida Office of The Attorney General (Daily Schedules and Travel) Request 9-14-16Dokument5 SeitenFlorida Office of The Attorney General (Daily Schedules and Travel) Request 9-14-16CREWNoch keine Bewertungen
- 2016 12 16 FOIA RequestDokument3 Seiten2016 12 16 FOIA RequestCREWNoch keine Bewertungen
- Final Installment 10-17-2016Dokument47 SeitenFinal Installment 10-17-2016CREWNoch keine Bewertungen
- FBI Denial 12-1-2016Dokument2 SeitenFBI Denial 12-1-2016CREWNoch keine Bewertungen
- FOIA Request - OGE (Trump Tweets) 12-6-16Dokument3 SeitenFOIA Request - OGE (Trump Tweets) 12-6-16CREWNoch keine Bewertungen
- Final Response Letter 10-17-2016Dokument2 SeitenFinal Response Letter 10-17-2016CREWNoch keine Bewertungen
- FBI (Kallstrom Communications) 11-22-16Dokument3 SeitenFBI (Kallstrom Communications) 11-22-16CREWNoch keine Bewertungen
- FBI (Congress Communications Re Comey Letter) 11-22-16Dokument3 SeitenFBI (Congress Communications Re Comey Letter) 11-22-16CREWNoch keine Bewertungen
- FBI Denial 12-1-2016Dokument2 SeitenFBI Denial 12-1-2016CREWNoch keine Bewertungen
- FBI (Giuliani Communications) 11-22-16Dokument3 SeitenFBI (Giuliani Communications) 11-22-16CREWNoch keine Bewertungen
- FBI Denial 11-29-2016Dokument1 SeiteFBI Denial 11-29-2016CREWNoch keine Bewertungen
- Second Declaration of James L. MartinDokument9 SeitenSecond Declaration of James L. MartinCREWNoch keine Bewertungen
- Memorandum in Opposition To Plaintiffs' Motion For Temporary Injunction and Declaration of Amy Frederick With ExhibitsDokument19 SeitenMemorandum in Opposition To Plaintiffs' Motion For Temporary Injunction and Declaration of Amy Frederick With ExhibitsCREWNoch keine Bewertungen
- Plaintiffs' Memorandum in Support of Motion For Temporary InjunctionDokument6 SeitenPlaintiffs' Memorandum in Support of Motion For Temporary InjunctionCREWNoch keine Bewertungen
- Plaintiffs' Reply in Support of Motion For Preliminary InjunctionDokument2 SeitenPlaintiffs' Reply in Support of Motion For Preliminary InjunctionCREWNoch keine Bewertungen
- Amended Complaint For Declaratory Judgment, Temporary, and Permanent InjunctionDokument22 SeitenAmended Complaint For Declaratory Judgment, Temporary, and Permanent InjunctionCREWNoch keine Bewertungen
- Complaint For Declaratory Judgment, Temporary and Permanent InjunctionDokument8 SeitenComplaint For Declaratory Judgment, Temporary and Permanent InjunctionCREWNoch keine Bewertungen
- Event Management Guide for Planning Successful EventsDokument2 SeitenEvent Management Guide for Planning Successful Eventsrakeshgopinath4999Noch keine Bewertungen
- Russian Social Media Information OperationsDokument10 SeitenRussian Social Media Information OperationsThe American Security ProjectNoch keine Bewertungen
- Imc - VODAFONEDokument28 SeitenImc - VODAFONEPayal Homagni MondalNoch keine Bewertungen
- BbasDokument23 SeitenBbasYashien AbdulaNoch keine Bewertungen
- Individual Assignment 1Dokument5 SeitenIndividual Assignment 1Rajendrasinh M. Dodia50% (2)
- Marketing StrategiesDokument61 SeitenMarketing StrategiesKateNoch keine Bewertungen
- Jolidon in RomaniaDokument15 SeitenJolidon in RomaniaCorina Barbu100% (1)
- Recruitment Selection Process Methods and Steps 1207897252784197 9Dokument84 SeitenRecruitment Selection Process Methods and Steps 1207897252784197 9AdityaNoch keine Bewertungen
- Imc ProjectDokument3 SeitenImc ProjectNickTamNoch keine Bewertungen
- Additional Sample Career Objective 1Dokument3 SeitenAdditional Sample Career Objective 1Mehul DhananiNoch keine Bewertungen
- PFPI Report To FTC On Biomass Power GreenwashingDokument55 SeitenPFPI Report To FTC On Biomass Power Greenwashingpetersoe0Noch keine Bewertungen
- Teacher's Guide. Unit 4Dokument24 SeitenTeacher's Guide. Unit 4laurawhite100% (1)
- Vanish Magazine 8Dokument176 SeitenVanish Magazine 8MagicProject Sv100% (1)
- YouTube One-PagerDokument1 SeiteYouTube One-PagerClaribeth MuñozNoch keine Bewertungen
- Sales and Distribution of BisleriDokument28 SeitenSales and Distribution of Bislerimilanbais100% (2)
- October 2013Dokument120 SeitenOctober 2013Pumper MagazineNoch keine Bewertungen
- VP Sales Marketing B2B in Albany NY Resume Christopher WallaceDokument2 SeitenVP Sales Marketing B2B in Albany NY Resume Christopher WallaceChristopherWallaceNoch keine Bewertungen
- Chapter 2 Job Order CostingDokument72 SeitenChapter 2 Job Order CostingLORENZE VIRNUEL UCAB IBA�EZ0% (1)
- Strategic Managment in PTCL: Group MembersDokument18 SeitenStrategic Managment in PTCL: Group MembersHamid NasirNoch keine Bewertungen
- Womens Health Issue - Reducing Teen PregnancyDokument15 SeitenWomens Health Issue - Reducing Teen Pregnancyapi-482726932Noch keine Bewertungen
- Wholesale Product,: Literature & Promote! Price ListDokument12 SeitenWholesale Product,: Literature & Promote! Price ListHilman LimNoch keine Bewertungen
- TLE (Industrial Arts)Dokument8 SeitenTLE (Industrial Arts)Julius EstadorNoch keine Bewertungen
- Answer Key Language ArtsDokument80 SeitenAnswer Key Language Artsumm_aasiyaNoch keine Bewertungen
- Cadbury UnityDokument5 SeitenCadbury UnitymaxsoniiNoch keine Bewertungen
- Kelloggs IndiaDokument2 SeitenKelloggs Indiasiddmehta321Noch keine Bewertungen
- Digital vs Traditional Marketing: Which to UseDokument2 SeitenDigital vs Traditional Marketing: Which to UseLearner's LicenseNoch keine Bewertungen
- CCW332 - Digital Marketing - SyllabusDokument2 SeitenCCW332 - Digital Marketing - SyllabusV ArunachalamNoch keine Bewertungen
- Management of Technology Task: Skype Business CanvasDokument26 SeitenManagement of Technology Task: Skype Business Canvassittialvina0% (1)
- Club Med & Social MediaDokument15 SeitenClub Med & Social MediaMaerten Caroline100% (1)
- Starbucks Entry into the Indian Coffee MarketDokument33 SeitenStarbucks Entry into the Indian Coffee MarketMehervaan KohliNoch keine Bewertungen