Beruflich Dokumente
Kultur Dokumente
Madara Poison
Hochgeladen von
Millenium AyurvedaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Madara Poison
Hochgeladen von
Millenium AyurvedaCopyright:
Verfügbare Formate
742 www.japi.org JAPI VOL.
54 SEPTEMBER 2006
Case Report
Cleistanthus Collinus Poisoning
SPE Benjamin, M Edwin Fernando, J Jerene Jayanth, B Preetha
Abstract
Cleistanthus collinus is an extremely toxic plant poison. Cleistanthin A and B, the toxins of Cleistanthus collinus,
are diphyllin glycosides which produce cardiac arrhythmias, urinary potassium wasting, hypoxia, metabolic
acidosis and hypotension. We report ARDS, distal renal tubular acidosis and distributive shock secondary to
inappropriate vasodilatation in a case following ingestion of its leaves.
L and CK-MB 123 U/L. Ultrasonogram of abdomen and
echocardiogram were normal. ECG showed prominent
U waves. ABG (breathing room air): pH 7.290, pCO
2
34.0
mmHg, pO
2
89.8 mmHg and HCO
3
17.9 mmol/L.
Later, as he became hypoxic despite oxygen
supplementation, ventilator support was given. Peak
airway pressure was 48 cmsH
2
O. PaO
2
/FiO
2
ratio: 142.
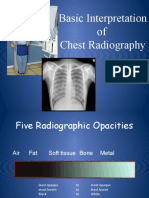
Central venous pressure (CVP) was low. A chest X-ray
showed bilateral peripheral alveolar infiltrates (Fig. 1).
ARDS was diagnosed and managed with PEEP and
prone ventilation.
There was increased urinary potassium loss (Table
1). This in combination with hyperchloremic metabolic
acidosis and normal serum anion gap suggested renal
tubular acidosis (RTA). Positive urinary anion gap
Departments of Medicine and Nephrology, CSI Kalyani
Multispeciality Hospital, Mylapore, Chennai.
Received : 31.3.2006; Revised : 10.8.2006; Accepted : 18.8.2006
INTRODUCTION
C
leistanthus collinus poisoning usually occurs
following intentional ingestion of the leaves with
mortality as high as 30%, usually occurs 3-7 days after
ingestion. Thomas K, et al,
1
identified hypokalemia due
to renal potassium wasting and cardiac dysrrhythmias.
Subrahmanyam DKS, et al,
2
identified other clinical
features of severe poisoning (Table 2). S Easwarappa, et
al,
3
have described neuromuscular weakness.
CASE REPORT
A 24 years male was referred from a rural hospital 2
days after ingestion of 40-50 leaves of oduvan with
history of abdominal pain, vomiting and breathlessness.
Gastric lavage had been done. Samples of the plant were
brought with him. It was identified as Cleistanthus collinus
at the Presidency College and Forensic Sciences
Department, Chennai.
On examination, he was conscious, oriented, afebrile
and dyspnoeic. Blood pressure was 110/70 mmHg,
pulse rate 128/min and respiratory rate 33/min. He had
epigastric tenderness. Fine crepitations were heard
bilaterally. Examination of the cardiovascular and
nervous system was unremarkable.
Total WBC count was 9800 cells/cumm with
predominant neutrophils. Serum potassium was 2.5
mEq/L, sodium 144 mEq/L, chloride 112 mEq/L,
bicarbonate 17 mEq/L, total calcium 6.7 mg/dL, urea 37
mg/dL, creatinine 1.4 mg/dL, total bilirubin 0.8 mg/
dL, direct bilirubin 0.4 mg/dL, SGOT 112 U/L, SGPT 90
U/L, SAP 1341 U/L, creatinine kinase (CK) total 883 U/
Fig. 1 : Chest X-ray of the patient showing ARDS. A right internal
jugular catheter and endotracheal tube are seen in position.
JAPI VOL. 54 SEPTEMBER 2006 www.japi.org 743
despite low serum bicarbonate confirmed RTA. Acidosis
was corrected using IV sodium bicarbonate followed by
Shohls solution and potassium citrate by Ryles tube.
Normal bicarbonate excretion following this and urinary
pH of 6.5 established distal (Type 1) renal tubular
acidosis (dRTA). Hypokalemia was corrected using IV
KCl and potassium citrate enterally (Table 1) following
which ECG normalised.
About 48 hrs after hospitalisation, he became
hypotensive with tachycardia, low CVP, oliguria and
increased urinary osmolality suggestive of toxin induced
vasodilatation. Blood pressure and urinary output were
corrected promptly when adequate fluids were given.
We used N-acetyl cysteine 150 mg/Kg over 1 hr
followed by 50 mg/Kg over 4 hrs and 100mg/Kg over
the next 16 hrs as glutathione depletion
4
and benefit
from SH containing compounds
5
has been reported in
animal studies. Cardiac and liver enzymes normalised
in a week. Distal RTA improved over 2 weeks. He was
off the ventilator on the 10th day and lung shadows
Table 1 : Estimated urinary potassium loss and serum potassium
Day 1 Day 1 Day 2 Day 2 Day 3 Day 5 Day 8
(Noon) (9 p. m.) (7 a. m.) (6 p. m.)
Urinary K
+
Loss (mEq/day) 210 170 335 611 120
Serum K
+
(mEq/L) 2. 6 2. 4 2. 5 3. 6 3. 6 4. 4 3. 9
Table 2 : Summary of previous observations and our investigations that lead to the diagnosis in this case and formulation
of the pathogenesis
Clinical and laboratory Published in the study by Further investigations done in Indicated a diagnosis of
features pertaining to Subrahmanyam DK, et al, as this patient
statistically significant risk
factors for death in Cleistanthus
collinus poisoning
Electrolyte and acid-base 1. ST depression, 1. Urinary potassium excretion, Distal renal tubular
disturbances 2. Potassium <3.1 mEq/L, 2. Normal Sr. Anion gap, acidosis.
3. Mean pH 7.28, 3. Urine anion gap,
4. Mean HCO
3
-
13.64, 4. Urine pH 6.5,
5. pH <7.3. 5. Normal urine HCO
3
-
excretion (after correction
of acidosis).
Shock 1. Clouding/blurring of vision, 1. Low central venous Distributive shock due to
2. Giddiness, pressure (CVP), inappropriate vasodilatation.
3. Pulse >120/min, 2. Normal LV function in
4. Hypotension. Echocardiography,
3. Oliguria and response to fluids.
Respiratory failure 1. Dyspnoea after 24 Hrs, 1. Infiltrates in chest X-ray, Non-cardiogenic pulmonary
2. Respiratory rate >30/min. 2. Low central venous pressure, oedema (ARDS).
3. Normal LV function in
Echocardiography,
4. PaO
2
/FiO
2
Ratio: 142.
disappeared after 3 weeks.
DISCUSSION
Hypokalemic metabolic acidosis, hypotension and
hypoxia have been described in this poisoning. We
evaluated further and identified dRTA, distributive
shock and ARDS respectively in this patient (Table 2).
Specific interventions against these entities were
initiated.
Hypokalemia was corrected by estimating urinary
losses and compensating for it. ARDS, dRTA and
distributive shock were also meticulously corrected.
Arrhythmias were either offset by these measures or
probably occur at higher blood levels of the toxin with a
permissive role for hypokalemia similar to digitoxicity.
Though we cannot categorically attribute this patients
survival to any of these measures or to N-acetyl cysteine,
these deserve evaluation in further trials.
Though the pathogenesis of Cleistanthus collinus
poisoning is well established, progress in our
744 www.japi.org JAPI VOL. 54 SEPTEMBER 2006
understanding of the pathophysiology could have
therapeutic and prognostic implications.
Acknowledgement
Our sincere thanks to Dr. S. Amerjothy. Ph. D., Reader
in Botany, Presidency College, Chennai, for her help in
identifying the plant.
REFERENCES
1. Thomas K, Dayal AK, Narasimhan, Alka G, Seshadri MS,
Cherian AM, Kanakasabapathi, Molly B. Metabolic and
Cardiac effects of Cleistanthus Collinus poisoning. J Assoc
Physicians India 1991;39:3124.
2. Subrahmanyam DK, Mooney T, Raveendran R, Zachariah B.
A clinical and laboratory profile of Cleistanthus collinus
poisoning. J Assoc Physicians India 2003;51:1052-4.
3. Eswarappa S, Chakraborty AR, Palatty BU, Vasnik M.
Cleistanthus Collinus Poisoning: Case Reports and Review of
the Literature. Clinical Toxicology 2000;41:369-72.
4. Sarathchandra G, Balakrishnamoorthy P. Acute toxicity of
Cleistanthus collinus, an indigenous poisonous plant in Cavia
procellus. Journal of Environmental Biology 1998:145-8.
5. Annapoorani KS, Damodaran C, Chandrasekharan P. A
promising antidote to Cleistanthus collinus poisoning. J Sci Soc
Ind 1986;2:3-6.
Announcement
28th CME in Internal Medicine conducted by Medical Education and Research Trust, Bangalore will be
held from 7th to 12th October 2006.
Morning - Guest Lectures, Work Shops and Afternoon - Bedside clinics.
Registration Fees - Rs. 600/- only
Pay by draft to Convener CME in Internal Medicine, Bangalore.
For further details contact : Dr. KR Raveendra, Convenor, CME Internal Medicine, Medical Education and
Research Trust, API Bhavan, No. 16/F, Millers Tank Bed Area, Vasanthnagar, Bangalore 560052.
Das könnte Ihnen auch gefallen
- Hepatitis C and Its Homeopathic Self Treatment Scheme - Bashir Mahmud ElliasDokument4 SeitenHepatitis C and Its Homeopathic Self Treatment Scheme - Bashir Mahmud ElliasBashir Mahmud Ellias100% (1)
- The History of Psychological TreatmentDokument16 SeitenThe History of Psychological TreatmentNeann Medina De JesusNoch keine Bewertungen
- Alchemical Gold PDFDokument34 SeitenAlchemical Gold PDFMillenium AyurvedaNoch keine Bewertungen
- Choose The Correct Answer For Questions (1 - 90)Dokument12 SeitenChoose The Correct Answer For Questions (1 - 90)حمزة الفنيني100% (3)
- ACUTE AND CHRONIC PANCREATITIS-undoneDokument6 SeitenACUTE AND CHRONIC PANCREATITIS-undonecory kurdapyaNoch keine Bewertungen
- Acid-Base and Electrolyte Handbook for Veterinary TechniciansVon EverandAcid-Base and Electrolyte Handbook for Veterinary TechniciansAngela Randels-ThorpNoch keine Bewertungen
- CholilithiasisDokument94 SeitenCholilithiasisdr.hendraNoch keine Bewertungen
- 1.case Study in Canine Intestinal LymphangiectasiaDokument5 Seiten1.case Study in Canine Intestinal LymphangiectasiaIhda AdilaNoch keine Bewertungen
- Autism9 Parenting Stress IndexDokument9 SeitenAutism9 Parenting Stress IndexPatty SiaNoch keine Bewertungen
- Basic Gastroenterology: Including Diseases of the LiverVon EverandBasic Gastroenterology: Including Diseases of the LiverNoch keine Bewertungen
- 3rd Year Syllabus PDFDokument24 Seiten3rd Year Syllabus PDFMillenium Ayurveda100% (1)
- Bedside Techniques Methods of Clinical Xamination Muhammad InayatullahDokument6 SeitenBedside Techniques Methods of Clinical Xamination Muhammad InayatullahAli HusnainNoch keine Bewertungen
- 3.4 Paralytic Ileus Due To Potassium Depletion. Dr. S. GieveDokument3 Seiten3.4 Paralytic Ileus Due To Potassium Depletion. Dr. S. GieveDaru KristiyonoNoch keine Bewertungen
- Case Report: Surgical Removal of A Canine Aortic Thromboembolism Secondary To PancreatitisDokument8 SeitenCase Report: Surgical Removal of A Canine Aortic Thromboembolism Secondary To PancreatitisIvan RisnaNoch keine Bewertungen
- A Case of Mushroom Poisoning With Russula Subnigricans: Development of Rhabdomyolysis, Acute Kidney Injury, Cardiogenic Shock, and DeathDokument4 SeitenA Case of Mushroom Poisoning With Russula Subnigricans: Development of Rhabdomyolysis, Acute Kidney Injury, Cardiogenic Shock, and DeathsuserNoch keine Bewertungen
- Paralisis de M.inferioresDokument2 SeitenParalisis de M.inferioresHector Garcia LermaNoch keine Bewertungen
- Case 1 CKDokument4 SeitenCase 1 CKmcpaulfreemanNoch keine Bewertungen
- Accidental Plant Poisoning With Colchicum Autumnale: Report of Two CasesDokument3 SeitenAccidental Plant Poisoning With Colchicum Autumnale: Report of Two CasesDiana IrimescuNoch keine Bewertungen
- Glucocorticoid-Induced Central Diabetes Insipidus in A Case of Malignant LymphomaDokument10 SeitenGlucocorticoid-Induced Central Diabetes Insipidus in A Case of Malignant LymphomaoliviaNoch keine Bewertungen
- 13no2 3Dokument5 Seiten13no2 3Wisnu WardanaNoch keine Bewertungen
- Asidosis Laktat 2Dokument10 SeitenAsidosis Laktat 2MizanMaulanaNoch keine Bewertungen
- AcuteKidneyInjury 000Dokument48 SeitenAcuteKidneyInjury 000Judith HallNoch keine Bewertungen
- Acute Kidney InjuryDokument48 SeitenAcute Kidney InjuryAnggioppleNoch keine Bewertungen
- Ascites With Right Heart Failure in A Dog: Diagnosis and ManagementDokument5 SeitenAscites With Right Heart Failure in A Dog: Diagnosis and ManagementairaNoch keine Bewertungen
- Hypokalemic NephropathyDokument7 SeitenHypokalemic NephropathyGoris HariyadiNoch keine Bewertungen
- HPTH Și Acidoza MetabolicaDokument6 SeitenHPTH Și Acidoza MetabolicaDana GoșmanNoch keine Bewertungen
- Case ReportDokument5 SeitenCase ReportkevserNoch keine Bewertungen
- Case Report: Rapport de CasDokument6 SeitenCase Report: Rapport de CasWidya KartikaNoch keine Bewertungen
- Lectura Recomendada HiperkalemiaDokument7 SeitenLectura Recomendada HiperkalemianeomaosNoch keine Bewertungen
- Long QT Pada CSWSDokument6 SeitenLong QT Pada CSWSSofie HanafiahNoch keine Bewertungen
- ECG of The Month: Journal of The American Veterinary Medical Association March 2016Dokument5 SeitenECG of The Month: Journal of The American Veterinary Medical Association March 2016Dewa Aix61Noch keine Bewertungen
- Weakness Following Diarrhea: 1/4: 1. What Can Be The Cause of Her Condition?Dokument4 SeitenWeakness Following Diarrhea: 1/4: 1. What Can Be The Cause of Her Condition?ZauzaNoch keine Bewertungen
- Elevated Liver Enzymes and Renal Failure, With A Surprising Outcome. Two Similar CasesDokument4 SeitenElevated Liver Enzymes and Renal Failure, With A Surprising Outcome. Two Similar CasescastrelinaNoch keine Bewertungen
- A Detail of The Molecular AnatomyDokument5 SeitenA Detail of The Molecular AnatomyMihaela Simona IsacNoch keine Bewertungen
- Nefrologia 30 Dias Electrolitos3Dokument31 SeitenNefrologia 30 Dias Electrolitos3JUAN ANDRES GUARDIAS GARZONNoch keine Bewertungen
- Jha2 2 118Dokument3 SeitenJha2 2 118Renato DantasNoch keine Bewertungen
- Hypokalaemia Periodic Paralysis: Liam J StapletonDokument4 SeitenHypokalaemia Periodic Paralysis: Liam J StapletonJL DeomampoNoch keine Bewertungen
- Case Study Internal MedDokument3 SeitenCase Study Internal MedChibueze AfugbuomNoch keine Bewertungen
- Renal InsufficiencyDokument12 SeitenRenal Insufficiencyluluburke.lbNoch keine Bewertungen
- Aproach UroanalysisDokument8 SeitenAproach UroanalysisJuaan AvilaNoch keine Bewertungen
- Renal ReviewDokument10 SeitenRenal ReviewZen Lenin CaroNoch keine Bewertungen
- Adynamic Osteopathy: About A Case With Review of The LiteratureDokument6 SeitenAdynamic Osteopathy: About A Case With Review of The LiteratureIJAR JOURNALNoch keine Bewertungen
- Ajmcr 10 9 10Dokument4 SeitenAjmcr 10 9 10saNoch keine Bewertungen
- Module 2 Fluid Electrolyte Disorders Acid Base NotesDokument9 SeitenModule 2 Fluid Electrolyte Disorders Acid Base NotesSara FNoch keine Bewertungen
- QT Prolongation Due To Organophosphate Poisoning: AYC Siu, LCH Tsoi, WCB Lo, CCH ChungDokument2 SeitenQT Prolongation Due To Organophosphate Poisoning: AYC Siu, LCH Tsoi, WCB Lo, CCH ChunghlNoch keine Bewertungen
- When Past Is Prologue: Clinical Problem-SolvingDokument7 SeitenWhen Past Is Prologue: Clinical Problem-SolvingJoni WitziNoch keine Bewertungen
- AscitesDokument1 SeiteAsciteseditorveterinaryworldNoch keine Bewertungen
- RLEFandECS Garlitos RoanneDokument4 SeitenRLEFandECS Garlitos RoannePaul JacksonNoch keine Bewertungen
- Ischemic Hepatitis Induced by Severe Anemia: Miry Blich, Shimon Edelstein, Roy Mansano and Yeouda EdouteDokument2 SeitenIschemic Hepatitis Induced by Severe Anemia: Miry Blich, Shimon Edelstein, Roy Mansano and Yeouda EdouteAthan KurniawanNoch keine Bewertungen
- Irreversible ShockDokument50 SeitenIrreversible ShockAnonymous YWmEwCNoch keine Bewertungen
- Hypokalemic Periodic Paralysis A Case ReportDokument2 SeitenHypokalemic Periodic Paralysis A Case ReportEditor IJTSRDNoch keine Bewertungen
- Kasus 1 (Asphyxiated Newborn)Dokument3 SeitenKasus 1 (Asphyxiated Newborn)D'Via Bintarra WNoch keine Bewertungen
- Case Report: Acute Warfarin Toxicity As Initial Manifestation of Metastatic Liver DiseaseDokument7 SeitenCase Report: Acute Warfarin Toxicity As Initial Manifestation of Metastatic Liver DiseaseAndrexixNoch keine Bewertungen
- Nephrorounds3 2015final 150907110921 Lva1 App6892 PDFDokument133 SeitenNephrorounds3 2015final 150907110921 Lva1 App6892 PDFTabada NickyNoch keine Bewertungen
- Two Cases of BRASH Syndrome: A Diagnostic Challenge: European Journal Internal MedicineDokument4 SeitenTwo Cases of BRASH Syndrome: A Diagnostic Challenge: European Journal Internal MedicineDesi MeliaNoch keine Bewertungen
- Ascites of Cardiac Origin in A Dog - A Case StudyDokument3 SeitenAscites of Cardiac Origin in A Dog - A Case StudyFaisal MohommadNoch keine Bewertungen
- Larussa 2017Dokument25 SeitenLarussa 2017alan.rangel.puenteNoch keine Bewertungen
- Homicidal Arsenic Poisoning: Andrew Duncan, Andrew Taylor, Elizabeth Leese, Sam Allen, Jackie Morton and Julie McadamDokument6 SeitenHomicidal Arsenic Poisoning: Andrew Duncan, Andrew Taylor, Elizabeth Leese, Sam Allen, Jackie Morton and Julie McadamFachryNoch keine Bewertungen
- Hipokalemia, Hipovolemia y Repercusión Electrocardiográfica Secundarias A Ingesta Prolongada de Furosemida. Caso ClínicoDokument7 SeitenHipokalemia, Hipovolemia y Repercusión Electrocardiográfica Secundarias A Ingesta Prolongada de Furosemida. Caso ClínicoIvan TapiaNoch keine Bewertungen
- Hepatology - 2012 - Fede - Adrenocortical Dysfunction in Liver Disease A Systematic ReviewDokument10 SeitenHepatology - 2012 - Fede - Adrenocortical Dysfunction in Liver Disease A Systematic ReviewJelena PaunovicNoch keine Bewertungen
- Primary Hyperaldosteronism Started by Hypokalemic Coma - Case ReportDokument8 SeitenPrimary Hyperaldosteronism Started by Hypokalemic Coma - Case ReportbreadfanNoch keine Bewertungen
- Jcem 2160Dokument8 SeitenJcem 2160vegagbNoch keine Bewertungen
- 001 ICU Case CoyocaDokument9 Seiten001 ICU Case CoyocaMiguel Kelly CataneNoch keine Bewertungen
- Renal CaseDokument3 SeitenRenal CaseAndy BiersackNoch keine Bewertungen
- ALF 418RLE Group1Dokument22 SeitenALF 418RLE Group1PAOLA LUZ CRUZNoch keine Bewertungen
- Effect of Curcumin On Inhibiting Atherogenesis by Down-Regulating Lipocalin-2 Expression in Apolipoprotein E Knockout MiceDokument11 SeitenEffect of Curcumin On Inhibiting Atherogenesis by Down-Regulating Lipocalin-2 Expression in Apolipoprotein E Knockout MicemaulanaardhiNoch keine Bewertungen
- Metabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentVon EverandMetabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentCarole IchaiNoch keine Bewertungen
- WHO Concept Paper PDFDokument13 SeitenWHO Concept Paper PDFMillenium AyurvedaNoch keine Bewertungen
- 4thBAMS Syllabus PDFDokument29 Seiten4thBAMS Syllabus PDFRajeev B PillaiNoch keine Bewertungen
- WHO Concept Paper PDFDokument13 SeitenWHO Concept Paper PDFMillenium AyurvedaNoch keine Bewertungen
- Homeopathy & Ayurvedic Medicine: A Study On The Plants Used As ChopachiniDokument4 SeitenHomeopathy & Ayurvedic Medicine: A Study On The Plants Used As ChopachiniMillenium AyurvedaNoch keine Bewertungen
- Ancient Ceylon PDFDokument320 SeitenAncient Ceylon PDFMillenium Ayurveda100% (1)
- Sinhalese Rituals PDFDokument567 SeitenSinhalese Rituals PDFMillenium AyurvedaNoch keine Bewertungen
- Avalokitsvara PDFDokument44 SeitenAvalokitsvara PDFMillenium AyurvedaNoch keine Bewertungen
- Historical Journl I PDFDokument62 SeitenHistorical Journl I PDFMillenium AyurvedaNoch keine Bewertungen
- Garbhaguhya Tantra PDFDokument47 SeitenGarbhaguhya Tantra PDFMillenium Ayurveda100% (1)
- Deities Buddhist PDFDokument22 SeitenDeities Buddhist PDFMillenium AyurvedaNoch keine Bewertungen
- Citadel of Anuradhapura PDFDokument119 SeitenCitadel of Anuradhapura PDFMillenium AyurvedaNoch keine Bewertungen
- GayadasaDokument5 SeitenGayadasaMillenium AyurvedaNoch keine Bewertungen
- Alchemy PDFDokument24 SeitenAlchemy PDFMillenium AyurvedaNoch keine Bewertungen
- CBC ArticleDokument22 SeitenCBC ArticleSubbie OutlierNoch keine Bewertungen
- Buddhadatta Buddhagosa PDFDokument7 SeitenBuddhadatta Buddhagosa PDFMillenium Ayurveda100% (2)
- Wachemo University Department of Obstetrics and Gynecology Clinical Year One Group I ScheduleDokument2 SeitenWachemo University Department of Obstetrics and Gynecology Clinical Year One Group I ScheduleDira DitaNoch keine Bewertungen
- DDB Board Reg No. 7, S. 2019Dokument72 SeitenDDB Board Reg No. 7, S. 2019keith tanueco100% (1)
- Ÿ Sex-Biased AutoimmunityDokument31 SeitenŸ Sex-Biased AutoimmunityJessy NingNoch keine Bewertungen
- Miyagawa Et Al-2015-Human Genome VariationDokument4 SeitenMiyagawa Et Al-2015-Human Genome Variationece142Noch keine Bewertungen
- COVID-19 Prevention PlanDokument12 SeitenCOVID-19 Prevention PlanZubair KhanNoch keine Bewertungen
- Bloodstream Infection MBDokument47 SeitenBloodstream Infection MBDarshan Koirala100% (1)
- Fourth Quarter Examination in Arts 7Dokument3 SeitenFourth Quarter Examination in Arts 7Jennifer Dapilmoto MandalNoch keine Bewertungen
- Whole Spine MriDokument2 SeitenWhole Spine MriImg UsmleNoch keine Bewertungen
- Nama Obat Jumlah Harga Beli Pabrik Syrup: GuardianDokument6 SeitenNama Obat Jumlah Harga Beli Pabrik Syrup: GuardianFitria Amalia SukmaNoch keine Bewertungen
- Self Instructional Module On Adolescent AnemiaDokument7 SeitenSelf Instructional Module On Adolescent AnemiaSagiraju SrinuNoch keine Bewertungen
- NCP ShockDokument5 SeitenNCP ShockJanina Patricia BuddleNoch keine Bewertungen
- ECT - Patient LeafletDokument4 SeitenECT - Patient LeafletSarah GrixtiNoch keine Bewertungen
- CASE STUDY Unstable Angina - 3Dokument25 SeitenCASE STUDY Unstable Angina - 3Renee RoSeNoch keine Bewertungen
- Pharmacokinetic in Pediatrics: and Implications For Drug TherapyDokument35 SeitenPharmacokinetic in Pediatrics: and Implications For Drug TherapyW MegaNoch keine Bewertungen
- CDE Course 2019Dokument19 SeitenCDE Course 2019Ellen HungNoch keine Bewertungen
- M3 Health HomeworkDokument1 SeiteM3 Health HomeworkKarlyNoch keine Bewertungen
- Nclex (1301) (1) (1315)Dokument43 SeitenNclex (1301) (1) (1315)Elizabeth SharmaNoch keine Bewertungen
- Basic Interpretation of CXRDokument84 SeitenBasic Interpretation of CXRAbdiqani Mohamed AdanNoch keine Bewertungen
- LabReportNew - 2023-06-23T171149.608Dokument1 SeiteLabReportNew - 2023-06-23T171149.608B AZAD SIMHANoch keine Bewertungen
- Katelynn Owens - 1.2.1 Autopsy Report GuideDokument3 SeitenKatelynn Owens - 1.2.1 Autopsy Report GuideKATELYNN OWENSNoch keine Bewertungen
- Lequesne Knee ScoreDokument3 SeitenLequesne Knee ScoreBagus PutraNoch keine Bewertungen
- PM - NaceDokument3 SeitenPM - Nacemohammad tahirNoch keine Bewertungen
- Coordinators BibleDokument60 SeitenCoordinators BibleSava SánchezNoch keine Bewertungen
- Anti EmesisDokument63 SeitenAnti EmesisOtilia SerescuNoch keine Bewertungen