Beruflich Dokumente
Kultur Dokumente
Free Radical Mechanism
Hochgeladen von
pussipitaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Free Radical Mechanism
Hochgeladen von
pussipitaCopyright:
Verfügbare Formate
Pharmac. Ther. Vol. 47, pp. 219-231, 1990 0163-7258/90 $0.00 + 0.
50
Printed in Great Britain. All rights reserved 1990 Pergamon Press plc
Associate Editor: D. SHUGAR
DOXORUBI CI N ( ADRI AMYCI N) : A CRI TI CAL REVIEW OF
FREE RADICAL- DEPENDENT MECHANISMS OF
CYTOTOXICITY
H. G. KEIZER, *~ H. M. PINEDO, t G. J. SCHUURHUISt a n d H. JOENJE*
*Institute of Human Genetics and tDepartment of Oncology, Free University, P.O. Box 7161, 1007 MC
Amsterdam, The Netherlands
Abstract--The antineoplastic drug doxorubicin is capable of generating a variety of free radical species
in subcellular systems and this capacity has been considered critical for its antitumor action. However,
for most tumor cell lines this mechanism of cytotoxicity does not appear to play a major role. Free
radical-independent cytotoxicity mechanisms, taking place in the nuclear compartment of the cell, may
more likely be involved in the antitumor effect of doxorubicin.
CONTENTS
1. Introduction 219
2. Free Radical-Dependent Toxicity Mechanisms of Doxorubicin 220
2.1. Mechanism of free radical production due to redox-cycling 220
2.2. DNA damage due to redox-cycling 220
2.3. Lipid peroxidation induced by redox-cycling 221
2.4. Mechanism of free radical formation by the doxorubicin-iron complex 222
2.5. Doxorubicin-iron complex-mediated DNA damage 222
2.6. Doxorubicin-iron complex-mediated lipid peroxidation 223
3. The Relative Importance of Free Radicals in the Mechanism of Cytotoxicity of Doxorubicin 223
3.1. Free radicals generated by redox-cycling 223
3.2. Free radicals generated by the doxorubicin-iron complex 224
3.3. Doxorubicin-dependent hydroxyl radical formation by intact tumor cells 224
3.4. Effects of radical scavengers on the cytotoxicity of doxorubicin 225
3.5. Role of free radicals in doxorubicin-induced cardiotoxicity 226
3.5.1. Free radical chemistry of doxorubicin in cardiac tissue 226
3.5.2. Free radical damage in cardiac tissue 226
4. Free Radical-Independent Mechanisms of Cytotoxicity 227
5. Summary and Conclusions 228
Acknowledgements 228
References 228
1. I NTR ODUCTI ON
The ant hr acycl i ne ant i bi ot i c doxor ubi ci n ( Adr i -
amyci n) , or i gi nal l y i sol at ed f r om t he fungus
St rept omyces peucet i us ( Ar c a mone et al., 1972), is a
c he mot he r a pe ut i c agent wi t h s t r ong act i vi t y agai nst a
wi de r ange of huma n mal i gnant neopl as ms i ncl udi ng
acut e l eukemi a, n o n - Ho d g k i n l ymphomas , breast
cancer, Hodgki n' s di sease and sar comas ( Young
et al., 1981). Apa r t f r om side-effects t hat ar e c o mmo n
t o ma ny cancer chemot her apeut i cs , i.e. hemat opoi et i c
suppr essi on, nausea and vomi t i ng, and al opeci a, t he
clinical useful ness of doxor ubi ci n is l i mi t ed l argel y
++Present address: Department of Toxicology, Duphar
B.V., P.O. Box 900, 1380 DA Weesp, The Netherlands.
To whom correspondence should be addressed.
by a cumul at i ve dose- r el at ed c a r di omyopa t hy t hat
mani f est s i t sel f as congest i ve hear t fai l ure ( Young
et al., 1981).
Much effort has been devot ed t o unr avel i ng t he
mechani s m of a nt i t umor act i on of doxor ubi ci n.
Cur r ent l y t he bel i ef is wi despr ead t hat free radi cal
f or mat i on is cri t i cal l y i nvol ved in t he mechani s m
of cyt ot oxi ci t y o f doxor ubi ci n agai nst t umor cells.
However , mos t o f t he evi dence f avor i ng a free
r adi cal - dependent model has been obt ai ned by st udy-
i ng subcel l ul ar f r act i ons, of t en in c ombi na t i on wi t h
ext r emel y hi gh concent r at i ons of doxor ubi ci n t hat
ar e not encount er ed in cl i ni cal pract i ce.
Bel ow we revi ew t he mechani s m of free r adi cal
f or mat i on f r om doxor ubi ci n and di scuss t he likeli-
hood of t hese r adi cal s pl ayi ng a rol e in its a nt i t umor
effect. We concl ude t hat , in general , this rol e must be
219
220 H. G. KEIZER et al.
a mi nor one, even though doxorubicin-induced car-
diotoxicity may well be mediated by free radical
formation. Finally, an attractive alternative mecha-
nism, based on the interference of doxorubicin with
topoisomerase II, is discussed.
2. FREE RADICAL- DEPENDENT TOXICITY
MECHANISMS OF DOXORUBICIN
The chemical structure of doxorubicin is depicted
in Fig. 1. Fr om a 'free radical' poi nt of view both
rings B and C are of special interest. One-electron-
reduction of ring C leads to the format i on of a
semi qui none free radical (Fig. 2). This radical is
relatively stable under anoxic conditions, but under
oxic conditions its unpai red electron is donat ed to
oxygen (02) forming superoxide radicals (Doroshow,
1983a, b; Bachur e t al . , 1982; Svingen and Powis,
1981). Suitable flavoproteins catalyze the format i on
of r e d u c e d s e m i q u i n o n e r a d i c a l s by accepting electrons
from NADH or NADPH and donat i ng them to
doxorubicin. By reducing oxygen to superoxide the
parent al doxorubi ci n molecule is regenerated. This
sequence of reactions, known as ' redox-cycling' , is
potentially harmful to cells since relatively little
doxorubi ci n would suffice to catalyze the format i on
of numer ous superoxide radicals. For mat i on of an
o x i d i z e d s e m i q u i n o n e in ring B of doxorubi ci n is
o OH o
1 ~t2 11 to 13
] 4 I ] = I * ' %, _ . "
H3CO O OH O
| . ; ~ c . ,
Y'
2 ,'N'~ Rg 3
Ant hr acydi ne R 1 R 2 R 3 R 4 R 5
Adci amyci n CH2OH NH 2 OH H H
Oaun~ubicin CH 3 NH 2 OH H H
FIG. I. The chemical structure of doxorubicin. Chemically
doxorubicin (adriamycin) consists of a water-insoluble te-
tracycline aglycone (structures ABCD) and a water-soluble
reducing daunosamine sugar. Several parts of the molecule
can be involved in the metabolism of doxorubicin. Ring C
is a quinone group which can be activated into a
semiquinone radical after one-electron-reduction. Ring B is
a hydroquinone which can al so be activated into a
semiquinone radical after one-electron-oxidation. The C9
side chain is probably important in the iron-catalyzed
autoxidation of the molecule. Differences in the C9 side
chain form the only difference between doxorubicin and its
analog daunorubicin. The iron-chelation site is probably
formed by the oxygen atoms of CI1 and C12. Iron at this
site can be reduced by the doxorubicin molecule either by
oxidation of the hydroquinone or by oxidation of the C9
side chain. The sugar group is important for the water
solubility of doxorubicin; during anaerobic metabolic reduc-
tion of doxorubicin it is split off and the C7-deoxyaglycone
is formed. From Gianni et al. (1988). (Reproduced with
permission of the authors.)
known to occur in the presence of iron (Gi anni e t al . ,
1985; Zweier, 1985) when no reducing system is
present. When the oxidized doxorubicin semi-
qui none- i r on complex reacts with oxygen, this will
ultimately lead to the format i on of a fully oxidized
form of doxorubicin, with format i on of oxygen
radicals. Both radical-producing systems are dis-
cussed below.
2.1. MECHANISM OF FREE RADICAL PRODUCTION DUE
TO REDOX-CYCLING
Reductive redox-cycling of doxorubicin was
described by Goodman and Hochstein (1977), who
observed that cytochrome P-450 reductase causes
NADPH- dependent oxygen consumpt i on in the
presence of doxorubicin, in excess of the amount of
drug present. Later studies indicated that not only
NADPH cytochrome P-450 reductase (Pan e t al . ,
1981), but also NADH dehydrogenase (Doroshow,
1983b; Davies e t al . , 1983a, b) and xant hi ne oxidase
(Doroshow, 1983a; Pan and Bachur, 1980), catalyze
the one-electron-reduction of doxorubicin. As a con-
sequence, redox-cycling of doxorubicin can occur in
cytoplasm, mitochondria, endoplasmic reticulum
(Doroshow, 1983a), and nucleus (Bachur e t al . , 1982).
The nucleus-catalyzed redox-cycling led Bachur e t al .
(1978) to postulate the concept of site-specific free
radical format i on in the nucleus: doxorubicin binds
selectively to nuclear DNA and can be metabolically
activated in the nucleus to produce free radical-
mediated damage to DNA.
The possible importance of redox-cycling is
stressed by the observation that not only isolated
enzymes, but also intact cells, can support one-
electron-reduction of doxorubicin and subsequent
doxorubi ci n-i nduced oxygen consumpt i on (Sato
e t al . , 1977). Furt hermore, one-electron-reduction of
doxorubicin might also occur in the clinical situation,
since an i mport ant metabolite found in patients is
the C7-deoxy-aglycone form of doxorubicin (Mross
e t al . , 1988), which is a metabolite known to be
formed from doxorubicin semiquinone radicals under
anoxic conditions (Guti6rrez e t al . , 1983; Pan e t al . ,
1981). In short, doxorubicin may be involved in a
' redox-cycling' process, which is potentially impor-
t ant for its cytotoxicity.
2.2. DNA DAMAGE DUE TO REDOx-CYCLING
Redox-cycling is rapid in the presence of oxygen
and slow under hypoxic conditions. Thus, in the
presence of oxygen, large amount s of superoxide may
be formed, whereas in its absence the semiquinone
radical will accumulate. As indicated below, different
toxicity mechanisms might be operative, depending
on the amount of oxygen present.
An o x y g e n - d e p e n d e n t mechanism of DNA damage
has been described by Berlin and Haseltine (1981),
who observed extensive DNA strand scission in a
system cont ai ni ng NADPH, NADPH cytochrome
P-450 reductase and DNA, and by Gutteridge and
Toeg (1982), who found deoxyribose breakdown in a
system cont ai ni ng deoxyribose, doxorubicin semi-
qui none radicals and iron. The aut hors proposed that
Doxorubicin (Adriamycin) 221
_ 9" 9" o . on
Orug-macromolecule DNA,RNA ~ * ~ ~ C O R t ~ ; r J ~ * , ~ C O R
complexes ' Proteins C H ~ " O H 4 ~ ~ , ~ " O H
so o- o. c' s0 6 0H
(CT-Ouinone methide) T (C 7-Deoxyaglycone )
/
DNA- nicking
0 OH DNA /
/ ~ C O R
f
, j r " o ,
\ f \ / - ' ~
y F~I( % 0 o o . 6-s,or ~ ( - - / ~L,p,~,
J qo.
. , o, . J \, y \ .,o,00.,o,,o.,,o.
~
"OH ~ "~- 02
CH30 O" OH C)-sugor
(Semiquinone)
Oruo-mocromolecule DNA,RNA ~ j ~ z ~ , , ~ C OR
complexes * ~ L ~ ~ OH
Proteins
CHso 0 OH
CT-Free rodicol
FIG. 2. Free radical and alkylating intermediates in the metabolism of doxorubicin. Doxorubicin can be
reduced by cellular flavoproteins to form its one-electron reduced semiquinone form. In the presence of
oxygen the semiquinone free radical is oxidized back into the parental quinone form under formation of
superoxide radicals. In the absence of oxygen the semiquinone is unstable; it loses its sugar moiety and
an intermediate C7 free radical can be formed. This radical can bind covalently to cellular macromolecules
or become again reduced forming a relatively stable product, the C7-deoxyaglycone, which is in fact a
doubly reduced doxorubicin molecule that has lost its sugar moiety. A tautomer of C7-deoxyaglycone is
the C7-quinone-methide, which is a potent DNA alkylating species and potentially toxic for tumor cells.
From Sinha et al. (1984). Reproduced with permission of the authors and the copyright holder, Cancer
Research, Inc., Philadelphia.
the DNA damagi ng species is the hydroxyl radical
formed from the following sequence of reactions:
202- + 2H+ ~H202 + 02
02 + Fe 3 + ~ O: + Fe 2+
H202 + Fe 2+ --*'OH + OH- + Fe 3+.
The sum of the latter two reactions
H202 + O~- ~ ' OH + OH- + 02
is known as the iron-catalyzed Haber-Wei ss reaction.
That superoxide-generating systems can indeed
damage DNA by this series of reactions was shown
by Rowley and Halliwell (1983), who were able to
inhibit DNA damage in a superoxide-producing
system with superoxide dismutase, catalase, iron
chelators and hydroxyl radical scavengers.
I n t h e a b s e n c e o f o x y g e n the semiquinone is
converted to its C7-deoxyaglycone metabolite, which
in itself is not pharmacologically active (Averbuch
e t al . , 1985). However, its tautomer, the C7-qui none
methide is a DNA-al kyl at i ng species (Moore, 1977).
Furthermore, an intermediate in the formation of
C7-deoxyaglycone from the doxorubicin semi-
qui none is the C7 free radical, which can also bi nd
covalently to DNA (Sinha and Chignell, 1979; Sinha
and Lewis Gregory, 1981; Sinha e t al . , 1984). The
structures of these reactive species are depicted in
Fig. 2.
Anot her DNA- damagi ng mechanism that may
operate at l o w p a r t i a l p r e s s u r e o f o x y g e n has been
described by Wi nt er bour n and collaborators. They
showed that in the absence of oxygen the semi-
qui none of doxorubicin reacts with H202 causing
breakdown of deoxyribose (Bates and Wi nt erbourn,
1982). This reaction was catalyzed by very low con-
centrations of iron: submi cromol ar concent rat i ons
are sufficient for a maximal effect (Wi nt erbourn e t al . ,
1985). Both the low i ron requirement of the reaction
and the optimal reaction rate at an oxygen tension of
approximately 4 mm Hg, may mimic the situation in
a t umor cell, since almost all intracellular iron is
believed to be in a complexed form, while oxygen
tensions of 3-6 mm Hg are considered to be common
(Wi nt erbourn e t al . , 1985). These data underscore the
potential importance of this reaction.
2.3. LIPID PEROXIDATION INDUCED BY
REDOX-CYCLING
Unsat urat ed fatty acids are peroxidized when
exposed to hydroxyl radicals in the presence of a
metal catalyst (Gutteridge, 1982). This process might
damage cellular membranes and eventually kill cells.
Doxorubicin can cause lipid peroxidation after
metabolic activation by heart, liver or kidney micro-
somes (Glazer e t al . , 1982; Mi mnaugh e t al . , 1982;
Bachur e t al . , 1977, 1978), mi t ochondri a (Mi mnaugh
222 H. G. KEIZER e t al.
e t a l . , 1985b), or nuclei ( Mi mnaugh e t a l . , 1985a).
In the presence of oxygen, doxor ubi ci n- dependent
lipid per oxi dat i on is general l y i nhi bi t ed by superoxi de
di smut ase, cat al ase, gl ut at hi one, i ron chel at ors
and hydroxyl radi cal scavengers ( Mi mnaugh e t a l . ,
1985a, b, 1983), suggesting t hat OH radi cal s gener-
at ed by the i r on- cat al yzed Haber - Wei s s react i on are
involved. The rat e of l i pi d per oxi dat i on in the pres-
ence of i ron and superoxi de, pr oduced by reduced
ant hracycl i nes, was much higher for deri vat i ves of
doxor ubi ci n t hat bi nd to mi crosomes t han for non-
bi ndi ng deri vat i ves (St errenberg e t a l . , 1985).
Anal ogous to DNA damage, membr ane l i pi d per-
oxi dat i on can also be i nduced in the absence of
oxygen with H202 present ( Wi nt er bour n e t a l . , 1985).
Wi t hout H:O2 very low concent r at i ons of oxygen are
requi red for opt i mal l i pi d per oxi dat i on, pr obabl y to
provi de H202 from the di smut at i on of superoxi de,
which is f or med by the react i on of 02 with doxor u-
bicin semi qui none radicals. Li pi d per oxi dat i on
occurred wi t hout added i ron, but i ncreased when i ron
was added in the 0. 1- 1pM range. OH radi cal
scavengers di d not i nhi bi t l i pi d per oxi dat i on in this
system. This is pr obabl y due to bi ndi ng of doxor u-
bicin to the l i posomes used in this test, since the
react i vi t y of "OH is so high t hat , when generat ed in
a ' site-specific' way, compet i t i on by scavengers is very
inefficient ( Wi nt er bour n e t a l . , 1985).
In concl usi on, under bot h hypoxi c and normoxi c
condi t i ons, l i pi d per oxi dat i on can be i nduced by the
reduced doxor ubi ci n semi qui none radi cal , which in
bot h cases is pr obabl y medi at ed by the OH radi cal .
2. 4. MECHANISM OF FREE RADICAL FORMATION BY
THE DOXORUBICIN-IRON COMPLEX
The doxor ubi ci n- i r on compl ex can suppor t the
f or mat i on of free radi cal s by two di st i nct mecha-
nisms, one dependent on the presence of a reduci ng
system, and anot her formi ng radi cal s f r om the
doxor ubi ci n- i r on compl ex itself, in the absence of a
reduci ng system. Bot h mechani sms are schemat i cal l y
depi ct ed in Fig. 3.
The upper par t of Fig. 3 i l l ust rat es free radi cal
f or mat i on i n t h e p r e s e n c e of a reduci ng system.
Doxor ubi ci n- Fe 3 is reduced to doxor ubi ci n- Fe 2+
either enzymat i cal l y by NADH cyt ochr ome P-450
reduct ase (Sugi oka and Nakano, 1982) or by thiols
like gl ut at hi one ( GSH) or cysteine (Zweier, 1985).
Doxor ubi ci n- Fe 2 can react with oxygen to form
superoxi de radi cal s ( O; - ) which di smut at e to form
hydrogen peroxi de (H202). Hydr ogen peroxi de can
also react with doxor ubi ci n- Fe 2 and form hydroxyl
radi cal s (Eliot e t a L , 1984; Myers e t al . , 1982). Thi s
GSH- dr i ven hydroxyl radi cal f or mat i on is a cyclic
process compar abl e to redox-cycl i ng in t hat no
doxor ubi ci n met abol i t es are being f or med (Zweier,
1985; Myers e t a L , 1982) and, in the presence of
sufficient GSH, the cycling process can proceed in-
definitely.
I n t h e a b s e n c e of a reduci ng system, doxor u-
bi ci n- Fe 3+ can reduce its chel at ed i ron by an i nt ra-
mol ecul ar redox react i on, ei t her by oxi dat i on of the
side chai n on C9 (Zweier e t a L , 1986; Gi anni e t a l . ,
1988; see also Fig. l ) or the hydr oqui none moi et y at
ring B (Zweier, 1983; Gi anni e t a l . , 1985), formi ng a
N A D P~ - . ~ 1 . , - DOX- Fe ~* , , ~ . . . , - . ~ GS S G
NADPH - ' / ~ ' - DOX. Fe ~+ GSH
a+
I:~X-Fe
Dol l , g"
O H ~," ~
oox . ~=g
[
9 - C OOH - D OX
FIG. 3. Free radical production from the doxorubicin iron
complex. The doxorubicin-iron II complex (DOX-Fe 2+)
can react with molecular oxygen (O2) or hydrogen peroxide
(H202) leading to the formation of superoxide ( O~) or
hydroxyl radicals ('OH), respectively, while the complex is
oxidized to doxorubicin-iron III (DOX-Fe3+). DOX-Fe 3+
can be reduced enzymatically by cytochrome P-450 reduc-
tase (Fp) or nonenzymatically via reaction with reduced
glutathione (GSH), forming back DOX Fe 2+, which can
again react with 02 or H202. In the presence of a reducing
system no metabolites are formed and radical production
can proceed indefinitely. In the absence of a reducing
system, DOX-Fe 3+ can reduce its iron intramolecularly by
oxidizing its hydroquinone moiety leading to the formation
of an oxidized doxorubicin semiquinone radical or by
oxidizing its C9 side chain. This intramolecular reduction of
iron is probably catalyzed by DNA. Electrons from the C9
chain of doxorubicin can keep the iron of the complex
reduced and thus support free radical production until the
side chain is fully oxidized. The end product of such
oxidation is 9-COOH-doxorubicin.
doxor ubi ci n free radi cal chelate with Fe 2+ (Gi anni
e t al . , 1985; Zweier e t al . , 1986; Zweier, 1985). The
f or mat i on of this doxor ubi ci n- Fe 2+ compl ex is
pr obabl y cat al yzed by DNA (Mui ndi e t a l . , 1985). In
the presence of oxygen this compl ex is oxidized, with
f or mat i on of superoxi de radi cal s ( Gi anni e t al . , 1985),
while it can also react with H202 via f or mat i on of
hydroxyl radi cal s (Zweier, 1985; Mui ndi e t a l . , 1984,
1985). Fur t her oxi dat i on of the side chai n will
ul t i mat el y l ead to the f or mat i on of the oxi di zed met a-
bol i t e of doxor ubi ci n 9-dehydroxyacet yl -9-carboxyl
doxor ubi ci n ( 9- COOH- doxor ubi ci n) (Gi anni e t al . ,
1988) (see Fig. 3).
2. 5. DOXORUBICIN--IRON COMPLEX-MEDIATED DNA
DAMAGE
Doxor ubi ci n- i r on compl exes bi nd t i ght l y to DNA
(El i ot e t a L , 1984). However, cont r ar y to i nt ercal at ed
doxor ubi ci n ( Mi mnaugh e t a l . , 1985b; Si nha and
Chignell, 1979; Sat o e t al . , 1977; Berlin and Haseltine,
1981; Rowley and Halliwell, 1983), the doxor u-
bi ci n- i r on compl ex preserves its abi l i t y to cat al yze the
f or mat i on of oxygen free radi cal s in the presence of
Doxorubicin (Adriamycin)
223
double-stranded DNA (Eliot e t a L , 1984). Thus, the
doxorubi ci n-i ron complex-driven hydroxyl radical
format i on can proceed in close proximity to DNA
and has therefore the potential to damage DNA
efficiently, especially since DNA seems t o catalyze
hydroxyl radical format i on by this complex (Muindi
e t a l . , 1984, 1985). Hydroxyl radicals are probabl y
involved in damagi ng of DNA since the generation of
hydroxyl radicals by the Dox- Fe 3 complex corre-
lates with its ability to cleave DNA (Muindi e t a l . ,
1984) and also since catalase, iron chelators and
hydroxyl radical scavengers are protective in this
system (Eliot e t a l . , 1984). Relatively high concentra-
tions of hydroxyl radical scavengers were required for
protection, indicating t hat these radicals were indeed
generated in a site-specific way.
2.6. DOXORUBICIN-IRON COMPLEX-MEDIATED LIPID
PEROXIDATION
In the presence of GSH, doxorubicin efficiently
damages erythrocyte ghost membranes (Myers e t a l . ,
1982). This reaction was inhibited by superoxide
dismutase, catalase and hydroxyl radical scavengers,
indicating the involvement of the hydroxyl radical.
Even in the absence of reducing agents, doxoru-
bicin-iron complexes appear to have the potential to
damage biomembranes, since such complexes pro-
voke lipid peroxidation (Sugioka and Nakano, 1982;
Gutteridge, 1982, 1983, 1984; Gianni e t a l . , 1988).
In this case, however, superoxide dismutase, catalase
or hydroxyl radical scavengers did not protect
(Sugioka and Nakano, 1982; Gutteridge, 1983;
Gianni e t a l . , 1988). The reduction of iron by the
side chain of doxorubicin was probabl y involved in
this type of membrane damage, since daunorubicin,
a structural analog of doxorubicin, lacking a readily
oxidizable side chain, was much less efficient (Gianni
e t a l . , 1988). Thus, bot h in the absence and presence
of reducing agents, the doxorubi ci n-i ron complex
can damage membranes, probabl y due to a hydroxyl
radical-dependent mechanism.
3. THE RELATIVE IMPORTANCE OF FREE
RADICALS IN THE MECHANISM OF
CYTOTOXICITY OF DOXORUBI CI N
As summarized in the previous section, roughly
two mechanisms of doxorubicin-mediated free radi-
cal format i on can be distinguished, one dependent on
the format i on of semiquinone radicals generated
during flavoprotein-mediated redox-cycling, and the
other dependent on the doxorubi ci n-i ron complex.
Below we discuss the likelihood of such mechanisms
playing a role in the tumoricidal and cardiotoxic
effects of doxorubicin.
3.1. FREE RADICALS GENERATED BY REDOX-CYCLING
With respect to redox-cycling, Bachur e t a l . (1978,
1982) have suggested that free radical format i on can
occur site-specifically in the nucleus, since isolated
nuclei bind doxorubicin and can also support
semiquinone format i on from doxorubicin (Bachur
e t a l . , 1982). However, the situation in intact cells
might be different, as in some cell types more t han
99.8% of the doxorubicin is present in a DNA- bound
form (Gigli e t a l . , 1988), whereas binding t o double
stranded DNA is known to preclude chemical (Sinha
and Chignell, 1979), enzymatic (Berlin and Haseltine,
1981; Rowley and Halliwell, 1983), and microsomal
(Sato e t a l . , 1977) one-electron-reduction of doxoru-
bicin. As a consequence of this, redox-cycling-depen-
dent DNA strand scission (Berlin and Haseltine,
1981), lipid peroxidation (Mi mnaugh e t a l . , 1985a)
and generation of superoxide from doxorubicin by
microsomes (Kal yanaraman e t a l . , 1980) is largely
prevented in the presence of double-stranded DNA.
That Bachur e t a l . (1982) nevertheless found redox
activity of doxorubicin in intact nuclei may be due to
the extremely high concentrations of doxorubicin
( > 500 11 M) used.
Even t hough radical format i on by redox-cycling
may not take place in the nucleus, semiquinone or
oxygen radicals may well be formed at some cytoplas-
mic site, e.g. the endoplasmic reticulum (Bachur
e t a l . , 1978), and reach the nucleus by diffusion.
However, the semiquinone radical is relatively un-
stable, with an estimated diffusion radius of 0.6 #m
under anaerobic and 0.1 # m under aerobic conditions
(Svingen and Powis, 1981), while an average cell has
a diameter in the range of 5-20/~m. This suggests that
only a minor fraction of the semiquinone radicals
produced in the cytoplasm may be able to reach
the nucleus. Theoretically, the probability for
semiquinone radicals to reach the nucleus is six-fold
higher under anoxic t han under aerobic conditions.
Yet, the sensitivity of cells to doxorubicin is essen-
tially similar under bot h anoxic and aerobic condi-
tions (Kennedy e t a l . , 1983), which seems to argue
against involvement of semiquinone format i on in the
cytotoxicity of doxorubicin.
Alternatively, superoxide and hydrogen peroxide
formed in the cytoplasm by redox-cycling might
diffuse into the nucleus and damage the DNA.
However, such a mechanism seems unlikely, since
increasing the concentration of intracellular SOD and
catalase, either artificially (Cervantes e t a l . , 1988) or
by selection for resistance to hyperoxia (Keizer e t a l . ,
1988), has been shown not to protect against the
cytotoxicity of doxorubicin. Furthermore, a recent
spin-trapping study failed to provide evidence for an
involvement of ESR-observable oxygen-derived radi-
cals in the ant i t umor activity of doxorubicin (Alegria
e t a l . , 1989).
In addition to DNA damage, free radical damage
to cellular membranes by lipid peroxidation may also
be involved in the ant i t umor effect of doxorubicin. In
fact, doxorubicin-induced lipid peroxidaton has been
observed in hepatocytes (Meredith and Reed, 1983;
Babson e t a l . , 1981) and cardiocytes (Julicher e t a l . ,
1985). However, to observe this effect, relatively high
concentrations of doxorubicin (100pM) were re-
quired; in addition, the experiments were done with
glutathione-depleted cells under an atmosphere of
pure oxygen, conditions known to accelerate the
process of lipid peroxidation. Bearing in mind that
hepatocytes and cardiocytes are probabl y better
suited to support redox-cycling of doxorubicin, com-
pared to t umor cells, such dat a can not be taken to
indicate that lipid peroxidation is involved in the
224 H. G. KEIZER e t a l .
ant i t umor effect of doxorubi ci n, especially since lipid
per oxi dat i on has not been report ed for t umor
cells t reat ed with clinically rel evant concent r at i ons of
doxorubi ci n.
To investigate the role of f l avopr ot ei n- medi at ed
redox-cycl i ng of doxor ubi ci n in its cyt ot oxi ci t y
agai nst SW-1573 human lung t umor cells, Kei zer
e t a l . (1989a) made use of a set of i nhi bi t ors of
f l avopr ot ei n- medi at ed reduct i on of doxor ubi ci n and
observed t hat none of these agents pr ot ect ed agai nst
the cyt ot oxi ci t y of doxorubi ci n, al t hough the cyt o-
toxicity of mi t omyci n C, which is known to depend
on ft avoprot ei n activity, was st rongl y i nhi bi t ed.
Fr om the evidence present ed above we must con-
clude t hat the si t uat i on inside the i nt act t umor cell is
not f avor abl e for redox-cycling, and t hat the involve-
ment of redox-cycl i ng in the cyt ot oxi ci t y of doxor u-
bicin in t umor cells has not been proven.
In the next section we discuss the pr obabi l i t y t hat
doxor ubi ci n- i r on compl ex- dependent free radi cal
f or mat i on is involved in the mechani sm of cyt ot oxi c-
ity of doxorubi ci n.
3.2. FREE RADICALS GENERATED BY THE
DOXORUBICIN-IRON COMPLEX
T h i o l - i n d e p e n d e n t free radi cal f or mat i on is very
unl i kel y to occur in i nt act cells, since i nt racel l ul ar
thiols are known to be abundant l y present, which is
expected to prevent aut oxi dat i on of doxor ubi ci n
(Zweier, 1985). In addi t i on the 9- COOH- doxor ubi ci n
met abol i t e is not det ect ed in pat i ent s t reat ed with
doxorubi ci n, Al t hough t umor cells i n v i v o were not
prot ect ed by ext racel l ul arl y added thiols ( Fr eeman e t
a l . , 1980; Dor oshow e t a l . , 1981; Yoda e t a l . , 1986),
it cannot be excluded t hat this mechani sm of free
radi cal f or mat i on occurs in ext racel l ul ar fluids, where
gl ut at hi one levels are relatively low.
T h i o l - d e p e n d e n t free radi cal f or mat i on from
doxor ubi ci n- i r on compl exes is a mor e at t ract i ve
model for hydroxyl r adi cal - medi at ed DNA damage,
since doxor obuci n- i r on compl exes bi nd efficiently to
DNA, where they can still be reduced by thiols and
pr oduce hydroxyl radi cal s in a site-specific way at
target. However, t hi ol depl et i on does not pr ot ect
t umor cells agai nst the cyt ot oxi ci t y of doxor ubi ci n
( Ramu e t a l . , 1984; Hami l t on e t a l . , 1985), nor does
an increased thiol cont ent pot ent i at e its cyt ot oxi ci t y
( Dor oshow e t a l . , 1981). The onl y system descri bed
thus far, in which thiols increase doxorubi ci n-
medi at ed damage, is the mi cr osomal fract i on
from ki dney, in which thiols pot ent i at e l i pi d peroxi -
dat i on ( Mi mnaugh, 1986). Thus ki dney damage due
to doxor ubi ci n may be par t i al l y caused by t hi ol -
dependent free radi cal f or mat i on (Mi mnaugh, 1986;
Mi mnaugh e t a l . , 1986). For t umor cell killing,
however, the occurrence of this mechani sm remai ns
to be proven.
In concl usi on, of all free radi cal -dependent mecha-
nisms, t hi ol -dependent free radi cal f or mat i on from
the doxor ubi ci n- i r on compl ex seems to be the most
at t ract i ve model for t umor cell killing by doxor u-
bicin, even t hough it is far from cert ai n whet her such
a mechani sm act ual l y t akes pl ace in the i nt act t umor
cell, since doxor ubi ci n- i r on compl exes have not been
demonst r at ed in i nt act cells, and may not even exist
in i nt act cells under clinically relevant condi t i ons
(Gel van and Samuni, 1988).
3.3. DOXORUBICIN-DEPENDENT HYDROXYL RADICAL
FORMATION BY INTACT TUMOR CELLS
As appear s from the dat a summari zed in Section
2.1, in all model s for doxor ubi ci n- i nduced free radi cal
damage, the ul t i mat e damagi ng species is presumed
to be the hydroxyl radi cal . Therefore several groups
of i nvest i gat ors have at t empt ed to detect ' OH
f or mat i on in i nt act t umor cells aft er t r eat ment with
doxorubi ci n.
Usi ng spi n-t rappi ng, Sinha e t a l . (1987a, b) de-
tected hydroxyl radi cal f or mat i on in MCF7 human
br east cancer cells; however, the doxor ubi ci n concen-
t r at i ons used were t hree orders of magni t ude higher
t han t hat needed to cause 50% i nhi bi t i on of
growt h (IC50). Fur t her mor e, in a doxorubi ci n-
resi st ant vari ant , hydroxyl radi cal f or mat i on was still
undet ect abl e, even at concent r at i ons t hat were 100-
fold higher t han the IC50 value for this vari ant . This
i ndi cat es t hat hydroxyl radi cal s measured under such
experi ment al condi t i ons are not necessarily involved
in the cyt ot oxi c effect of doxorubi ci n. The observa-
t i ons t hat ext racel l ul arl y added NADPH st rongl y
st i mul at ed hydroxyl radi cal format i on, whereas bot h
superoxi de di smut ase and cat al ase were i nhi bi t ory,
suggest t hat at least par t of the hydroxyl radi cal s were
generat ed out si de the cells (Sinha e t a l . , 1987a, b; cf.
Al egri a e t a l . , 1989). It follows t hat enzymes at the
out er cell surface mi ght reduce doxorubi ci n, thus
l eadi ng to the f or mat i on of superoxi de radi cal s and
hydr ogen peroxi de t hr ough redox-cycling. Since i ron
scavengers i nhi bi t ed hydroxyl radi cal f or mat i on
(Sinha e t a l . , 1987a, b) an i r on- cat al yzed Haber
Wei ss react i on mi ght thus be responsi bl e for hydroxyl
radi cal f or mat i on in this system; al t ernat i vel y extra-
cellular reduct i on of doxor ubi ci n- i r on complexes
mi ght pr oduce these radicals.
Usi ng met hane f or mat i on from DMSO as an assay
for hydroxyl radi cal format i on, Dor oshow (1986b)
obt ai ned essentially similar dat a for intact Ehrlich
ascites t umor cells. However, since cat al ase com-
pletely i nhi bi t ed hydroxyl radi cal format i on,
Dor oshow' s results i ndi cat e t hat the hydroxyl radi -
cals det ect ed were generat ed out si de the cells.
Hydr oxyl radi cal s generat ed at the out er surface of
cells mi ght pl ay a role in the mechani sm of t umor cell
killing by i mmobi l i zed doxorubi ci n. In this case
doxor ubi ci n is compl exed to a synthetic carri er, so
t hat the dr ug cannot ent er the cells; nevertheless such
a compl ex is highly cyt ot oxi c (Tri t t on and Yee, 1982;
Rogers and T6k~s, 1984; Panneersel vam e t a l . , 1987;
Rogers e t a l . , 1983). At sites where the cells make
cont act with the i mmobi l i zed doxorubi ci n, the local
doxor ubi ci n concent rat i ons may be high enough to
suppor t hydroxyl radi cal f or mat i on aft er reduct i on of
doxor ubi ci n by cell surface-bound reducing enzymes.
That redox activity out si de the cells, as well as
hydroxyl radi cal format i on, is necessary for the cyt o-
toxicity of i mmobi l i zed doxorubi ci n, is suggested by
the observat i ons t hat hydroxyl radi cal scavengers
t oget her with superoxi de di smut ase and cat al ase
i nhi bi t ed cyt ot oxi ci t y (Panneersel vam e t a l . , 1987).
Fur t her mor e, i mmobi l i zed i mi nodaunor ubi ci n, a
Doxorubicin
derivative of doxorubicin that is less readily reduced
metabolically, was much less cytotoxic t han i mmobi -
lized doxorubicin (Panneerselvam e t a l . , 1987). Such
data underline the possibility that under certain
conditions hydroxyl radicals formed outside the cells
can kill t umor cells. However, this mechanism of
cytotoxicity may be quite distinct from the usual
toxicity mechanism operating against t umor cells,
as is further suggested by the observation that a
pharmacologically inactive analog, 4-demethoxy-7,9-
di-epi-daunorubicin, after coupling to a macromolec-
ular carrier, acquired significant cytostatic activity to
both doxorubicin-resistant and -sensitive L1210 cells
(Rodgers and T6k6s, 1984).
Al t hough OH radical formation has only been
detected at relatively high doxorubicin concentra-
tions at the outer cell surface, we cannot entirely
rule out the possibility that OH radicals are also
formed inside the cells at clinically achievable concen-
trations of doxorubicin, since OH radicals formed
inside the cell might react with cellular constituents
too rapidly to be detected by the relatively insensitive
competitive detection methods that are based on
spin-trapping and reaction with DMSO. To investi-
gate the role of OH radical formation in the cyto-
toxicity of doxorubi ci n at clinically achievable
concentrations, the effect of several free radical scav-
engers on the cytotoxicity of doxorubicin has been
studied. The findings from these studies are reviewed
in the next section.
3.4. EFFECTS OF RADICAL SCAVENGERS ON THE
CYTOTOXICITY OF DOXORUBICIN
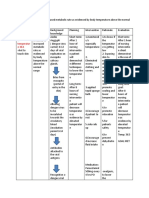
As indicated in Table 1, extracellularly added
superoxide dismutase or catalase protected MCF7
(Sinha e t a l . , 1987b; Doroshow, 1986a) and Ehrlich
ascites t umor (Doroshow, 1986b) cells against the
cytotoxicity of doxorubicin. However, no protection
by superoxide dismutase and catalase was observed in
A2780 and A2780 AD cells (Cervantes e t a l . , 1988).
Apparently, since superoxide dismutase and catalase
are presumed not to enter cells, MCF7 and Ehrlich
ascites cells are killed to some extent by activated
oxygen species generated outside the cells by a mech-
anism that is probabl y dependent upon iron, since
iron chelators were also protective, (Ooroshow,
1986a, b; see also Alegria e t a l . , 1989). That A2780
cells are not killed by a similar mechanism, as sug-
gested from the lack of effect of superoxide dismutase
and catalase, indicates that this may not be a univer-
(Adriamycin) 225
sal mechanism of cytotoxicity. Furthermore, murine
S180 cells were not protected against doxorubicin by
the iron chelating drug ICRF 187 (Wadler e t a l . ,
1986). An i mport ant question now is which cell
model is representative for the most common mecha-
nism of t umor cell killing by doxorubicin.
In this context it is i mport ant to note that both
Ehrlich ascites cells and MCF7 cells are exceptional
with respect to the level of their ant i oxi dant de-
fense capacity. Ehrlich ascites cells are known to be
catalase-deficient and to have very low levels of
glutathione-dependent free radical-detoxifying en-
zymes (Bozzi e t a l . , 1981), while MCF7 cells cont ai n
unusually high levels of doxorubicin-reducing en-
zymes (Sinha e t a l . , 1987b), along with a relatively
low glutathione-S-transferase activity (Broxterman e t
a l . , 1989), an i mport ant peroxide detoxification en-
zyme. That endogenous ant i oxi dant levels in MCF7
and Ehrlich ascites cells may indeed be limiting for
cellular tolerance to doxorubicin is suggested by the
fact that PZ51, an agent which can be taken up by
cells and function as an intracellular peroxidase in the
presence of glutathione, protects both MCF7 and
Ehrlich ascites cells against the cytotoxicity of dox-
orubicin (Doroshow, 1986a, b). The observation that
doxorubicin-resistant variants of MCF7 cells cont ai n
increased levels of glutathione-S-transferase and glu-
tathione peroxidase (Kramer e t a l . , 1988) further
supports this concept. In several other cell lines
(Ramu e t a l . , 1984; Meijer e t a l . , 1987; Ross e t a l . ,
1988; Keizer e t a l . , 1989b), the level of ant i oxi dant
defense does not increase duri ng selection for doxoru-
bicin resistance, which strongly suggests t hat in these
cell lines the ant i oxi dant defense does not limit
cellular tolerance to doxorubicin treatment. The same
was concluded for Chinese hamster ovary cells, since
an oxygen-resistant vari ant having increased levels of
superoxide dismutases, catalase, glutathione and glu-
tathione peroxidase was as sensitive to doxorubicin as
the parental CHO line (Keizer e t a l . , 1988).
In this respect an i mport ant observation was made
by Potmesil e t a l . (1984), who observed that doxoru-
bicin causes two types of DNA strand breaks in
L1210 cells, i.e. protein-associated single-strand
breaks and direct single-strand breaks. Up to a
doxorubicin concent rat i on of 2.8 pM, which kills
more t han 99.99% of the cells (Ross and Smith,
1982), only protein-associated strand breaks were
observed (Potmesil e t a l . , 1983). At higher concentra-
tions protein-associated strand breakage decreased,
whereas direct strand breakage increased (Potmesil
e t a l . , 1983). Interestingly, direct strand breakage
TABLE 1. E f f e c t o f F r e e R a d i c a l S c a v e n g e r s o n t h e C y t o t o x i c i t y o f D o x o r u b i c i n
Cell growth in the presence of doxorubicin (%)
Cell type Control + SOD + Catalase 'OH scavengers + PZ 51 Reference
Ehrlich acites 51 72 75 87-104 94 Dor os how (1986b)
MCF 7 49 93 87 100 74 Dor os how (1986a)
MCF 7 40 80 60 ND ND Sinha e t a l . (1987b)
A 2780 31 28 31 28 70 ND Cer vant es e t a l . (1988)
A 2780 AD 43-46 46 42 47-80 ND Cer vant es e t a l . (1988)
Effect of superoxide dismutase (SOD), catalase, several OH radical scavengers and a synthetic glutathione peroxidase
(PZ 51) on the cytotoxicity of doxorubicin, as reported in the literature. Cells were treated with doxorubicin concentrations
leading to a relative growth of 31-51% compared to untreated controls. The relative growth in the presence of antioxidant
is indicated. ND, not determined.
JPT 47/2--F
226 H. G. KEIZER e t al.
occurred onl y in the presence of oxygen (Potmesil
e t al . , 1983) and was i nhi bi t ed by ext racel l ul arl y
added superoxi de di smut ase or cat al ase (Potmesil
e t al . , 1984). These results clearly i ndi cat e t hat free
radi cal s generat ed at the cell surface have the pot ency
to damage the cel l ul ar DNA. However, since l et hal i t y
of L1210 cells was al most 100% wi t hout occurrence
of this t ype of DNA damage, at doxor ubi ci n concen-
t rat i ons which even exceed the clinically achi evabl e
concent r at i ons in pl asma (Potmesil e t a l . , 1984;
Er t t mann e t al . , 1988), a free r adi cal - dependent
mechani sm of t oxi ci t y is appar ent l y not very i mpor -
t ant in the killing of L1210 cells by doxorubi ci n.
Nevertheless, for cell lines with a relative l ack of
ant i oxi dant enzymes, like Ehrl i ch ascites and MCF7
cells, this t ype of damage mi ght pl ay a mor e i mpor -
t ant role in the cyt ot oxi ci t y of doxorubi ci n.
A r at her consi st ent finding is t hat scavengers of
hydroxyl radi cal s prot ect cells agai nst the cyt ot oxi ci t y
of doxor ubi ci n (Tabl e 1). However, pr ot ect i on is
t ypi cal l y found onl y at ext remel y high scavenger
concent rat i ons, oft en in the range between 100 and
250 mM ( Dor oshow, 1986a, b; Cervant es e t a l . , 1988).
Of course, onl y high "OH scavenger concent r at i ons
are expected to be abl e to pr ot ect agai nst hydroxyl
radi cal damage in view of the ext reme react i vi t y of
this radi cal . However, in the same concent r at i on
range, sodi um chl ori de also pr ot ect ed agai nst the
cyt ot oxi ci t y of doxor ubi ci n (Il i aki s and Lazar, 1987).
Therefore, there are serious doubt s about the specifi-
city of t he hydroxyl radi cal scavengers when used at
such high concent rat i ons. Thus, al t hough the effects
of hydroxyl radi cal scavengers are consi st ent with a
role for these radi cal s in the cyt ot oxi ci t y of doxor u-
bicin, the critical i nvol vement of hydroxyl radi cal s
remai ns unproven.
Not onl y i n v i t r o but also i n v i v o effects of radi cal
scavengers have been i nvest i gat ed on the t umor i ci dal
effect of doxorubi ci n. Ascor bat e ( Fuj i t a e t al . , 1982),
N-acet yl cyst ei ne ( Fr eeman e t a l . , 1980; Dor oshow e t
al . , 1981 ), cysteine ( Fr eeman e t al . , 1980), gl ut at hi one
( Yoda e t al . , 1986) and al pha- t ocopher ol (Myers
e t a l . , 1977) have been tested i n v i v o . None of these
t reat ment s reduced the t umor i ci dal effect of doxor u-
bicin agai nst L1210 ( Fuj i t a e t a l . , 1982; Yoda e t a l . ,
1986), P388 ( Fr eeman e t al . , 1980; Myers e t a l . , 1977)
or Ehrlich ascites cells ( Fr eeman e t al . , 1980), while
these t reat ment s di d reduce car di ot oxi ci t y in the
ani mal s under i nvest i gat i on. Since free radi cal
damage is likely to be responsi bl e for car di ot oxi ci t y
in mice (see below), these dat a suggest t hat this t ype
of damage is not responsi bl e for the i n v i v o ant i t umor
effect of doxorubi ci n.
Al t oget her these results suggest t hat in the clinical
si t uat i on onl y t hose cells coul d be damaged by a free
r adi cal - dependent mechani sm t hat are well oxy-
genat ed and exposed to relatively high concent r at i ons
of doxor ubi ci n or have a relative l ack of ant i oxi dant
defense capaci t y. Pr obabl y this will include onl y a
mi nor fract i on of the t umor cells. However, in heart
tissue such condi t i ons are met duri ng t r eat ment with
a single high dose of doxorubi ci n, and, in fact, acut e
car di ot oxi ci t y is frequently observed. The possi bl e
par t i ci pat i on of free radi cal s in the devel opment
of doxor ubi ci n- i nduced cardi ot oxi ci t y is discussed
below.
3.5. ROLE OF FREE RADICALS IN
DOXORUBICIN-INDUCED CARDIOTOXICITY
Fr ee radi cal pr oduct i on in car di ac cells due to
one-el ect ron-reduct i on of doxor ubi ci n mi ght occur at
the nuclear envelope (Bachur et al . , 1982), in mi t o-
chondr i a ( NADH dehydrogenase), cyt osol (xant hi ne
oxidase) or sarcopl asmi c ret i cul um ( NADPH cyt o-
chrome P-450 reduct ase) ( Dor oshow, 1983a). In this
respect car di ac cells are not except i onal . Nevert he-
less, the occurrence of car di ot oxi ci t y is an i mpor t ant
dose-l i mi t i ng fact or in doxor ubi ci n t r eat ment of
cancer pat i ent s (Green e t al . , 1984). The selective
t oxi ci t y of doxor ubi ci n to heart cells mi ght simply
reflect an unusual l y high level of drug accumul at i on
in these ceils, as report ed by several aut hors
( Lampi di s e t al . , 1981; Johnson e t al . , 1986). In
addi t i on, as discussed below, free radi cal damage
mi ght be i mpor t ant for the devel opment of
cardi ot oxi ci t y.
3.5.1. F r e e R a d i c a l C h e m & t r y o f D o x o r u b i c i n i n
C a r d i a c T i s s u e
Hear t muscle cells are ext remel y rich in mi t ochon-
dri a, which mi ght render t hem par t i cul ar l y vul nerabl e
to free radi cal s generat ed at these organelles. In
addi t i on, unlike liver mi crosomes, where doxor ubi ci n
semi qui none radi cal s react preferent i al l y with molec-
ul ar oxygen to form relatively harml ess superoxi de
radi cal s, semi qui nones formed in heart mi t ochondr i a
appear to react r at her with hydrogen peroxi de with
f or mat i on of the highly reactive hydroxyl radi cal
(Nohl and Jor dan, 1983). Compar ed to liver micro-
somes, sarcosomes from heart tissue are relatively
inefficient in reduci ng doxor ubi ci n to its semi qui none
form (Nohl and Jor dan, 1983), pr obabl y due to a
relative lack of NADPH cyt ochrome P-450 reduc-
tase. However, semi qui nones generat ed at this site
also tend to react preferent i al l y with hydrogen per-
oxide, even in the presence of oxygen (Thornal l ey and
Dodd, 1985), while in t umor cells this react i on t akes
pl ace onl y in the absence of oxygen (Bates and
Wi nt er bour n, 1982).
Al t hough i nt racel l ul ar hydroxyl radi cal forma-
t i on in cardi ac tissue coul d not be demonst r at ed
( Raj agopal an e t al . , 1988), the fact t hat mi croscopi -
cally visible cardi ac damage st art s to occur at the
endopl asmi c reticulum and mi t ochondr i a (Olson and
Capen, 1977) suggests t hat free radi cal f or mat i on
may be involved in the cardi ot oxi ci t y of doxorubi ci n.
3.5.2. F r e e R a d i c a l D a m a g e i n C a r d i a c T i s s u e
In mice, bot h with acut e (Myers e t al . , 1977) and
chroni c (Lazzari no e t al . , 1987) doxor ubi ci n- i nduced
cardi ot oxi ci t y, l i pi d per oxi dat i on of heart tissue has
been observed, even t hough this process coul d not be
demonst r at ed in t umor cells (Myers e t a l . , 1977) or
liver tissue (Lazzari no e t a l . , 1987) of the same mice.
This suggests t hat cardi ac tissue is specifically dam-
aged by a free radi cal -dependent mechani sm causing
lipid peroxi dat i on. This is pr obabl y not onl y the
result of the relative abundance of mi t ochondr i a, and
efficient hydroxyl radi cal f or mat i on in cardi ac tissue
as discussed above, but also of a relatively poor
Doxorubicin (Adriamycin)
227
ant i oxi dant defense, since the heart has r at her low
levels of superoxi de di smut ase and cat al ase
( Dor oshow e t al . , 1980) and a relatively low rat e of
gl ut at hi one t urnover when compar ed t o e.g. liver
tissue (Griffith and Meister, 1979). Fur t her mor e,
duri ng doxor ubi ci n t reat ment , gl ut at hi one peroxi -
dase t ends to become depl et ed ( Dor oshow e t al . ,
1980).
That a relative l ack of ant i oxi dant defense is indeed
involved in the devel opment of cardi ot oxi ci t y in mice
is suggested by experi ment s showing t hat i nhi bi t i on
of gl ut at hi one peroxi dase ( Dor oshow e t a L, 1980) or
decreasing gl ut at hi one levels in car di ac cells (Olson
e t al . , 1980) increased the severity of doxorubi ci n-
i nduced cardi ot oxi ci t y, while agents t hat prot ect cells
agai nst free radi cal damage, i ncl udi ng N-acet yl cys-
teine ( Dor oshow e t al . , 1981; Ol son e t a L, 1980),
cysteine (Olson e t al . , 1980), reduced gl ut at hi one
( Yoda e t al . , 1986) and al pha- t ocopher ol (Myers
e t al . , 1977), pr ot ect ed agai nst doxorubi ci n-i nduced
lipid per oxi dat i on and cardi ot oxi ci t y.
In rats, the si t uat i on differs from t hat in mice, since
rat cardi ac tissue appear s to be unusual l y resi st ant to
i nduct i on of lipid per oxi dat i on ( Mi mnaugh e t al . ,
1981; Julicher e t al . , 1985). As a consequence, l i pi d
per oxi dat i on of rat heart tissue is barel y det ect abl e
( Por t a e t al . , 1983; Mul i awan e t al . , 1980) and, in
cases where it was det ect ed, di d not paral l el the
devel opment of cardi ot oxi ci t y ( Por t a e t al . , 1983).
Fur t her mor e, neither N-acet yl cyst ei ne nor al pha-
t ocopherol prot ect ed rat myocar di al cell cultures
in v i t r o agai nst t he cyt ot oxi ci t y of doxor ubi ci n
(Newman e t al . , 1981). Therefore, in rat s lipid perox-
i dat i on of cardi ac tissue is pr obabl y not responsi bl e
for the devel opment of cardi ot oxi ci t y. On the ot her
hand, lipid peroxi des have been det ect ed in serum of
rat s t reat ed with doxor ubi ci n (Thayer, 1984); these
possi bl y ori gi nat e from the liver ( Mi mnaugh e t al . ,
1981), since this organ is very well suited to suppor t
free radi cal f or mat i on from doxorubi ci n. Hypot het i -
cally, these peroxi des mi ght cont r i but e to cardi ot oxi -
city, since heart cells are known to be very sensitive
to exposure to lipid peroxi des ( Nor onha- Dut r a and
Steen, 1982). However, this possi bi l i t y awai t s further
verification.
4. FREE RADI CAL- I NDEPENDENT
MECHANI SMS OF TOXICITY
As doxor ubi ci n is active agai nst a wide variety of
cancers, while many t umor cell types, as poi nt ed out
above, are not likely to be killed via a free radi cal -
dependent mechani sm of cyt ot oxi ci t y, efficient
radi cal -i ndependent mechani sms of cyt ot oxi ci t y of
doxor ubi ci n must exist. The most widely st udi ed
nonr adi cal - dependent mechani sms of cyt ot oxi ci t y are
based on the capaci t y of this dr ug to i nt ercal at e i nt o
doubl e- st r anded DNA. It has been known for 20
years t hat ant hracycl i nes can give rise to an i nt ercal a-
tion compl ex with DNA (for review see Aubel -
Sadr on and Londos- Gagl i ar di , 1984). Possi bl y as a
consequence of this pr oper t y, doxor ubi ci n inhibits
bot h RNA and DNA synthesis, a process which
might be involved in its ant i t umor effect (Aubel -
Sadr on and Londos- Gagl i ar di , 1984). Non- DNA-
bi ndi ng deri vat i ves of doxorubi ci n, like AD-32, may
di rect l y i nt eract with the RNA pol ymerase to i nhi bi t
t ranscri pt i on ( Aubel - Sadr on and Londos- Gagl i ar di ,
1984).
Recently, a novel mechani sm by which doxor u-
bicin, as well as ot her i nt ercal at i ng drugs, may kill
t umor cells has been described; it is based on interfer-
ence with the DNA br eakage- r euni on react i on
medi at ed by t opoi somer ase II (Tewey e t al . , 1984a).
This mechani sm woul d explain, why in t umor cells
t reat ed with clinically rel evant doxor ubi ci n concen-
t rat i ons, bot h single- and doubl e- st r and prot ei n-
associ at ed DNA breaks are observed (Potmesil e t al . ,
1983, 1984). A maj or quest i on now is whet her this
react i on pl ays a domi nant role in the ant i t umor effect
of doxorubi ci n.
Evidence favori ng this possi bi l i t y is derived from a
compar i son of t reat ment s t hat i nhi bi t t opoi somer ase
II- medi at ed DNA damage and affect doxor ubi ci n
cyt ot oxi ci t y. Three condi t i ons are known t o i nhi bi t
t opoi somerase II i n v i t r o : low t emper at ur e (Liu e t al . ,
1983), high salt concent rat i ons (Tewey e t al . , 1984b;
Liu e t al . , 1983) and doxor ubi ci n concent rat i ons
exceeding a critical value between 0.5 and 2.5 #M
(Tewey e t al . , 1984b). For all three condi t i ons there
is evidence for a similar effect on doxor ubi ci n cyt o-
toxicity: (1) Incubat i on of cells at 0C t ot al l y abol -
ished doxor ubi ci n cyt ot oxi ci t y (Lane e t al . , 1987); (2)
high salt dr amat i cal l y prot ect ed agai nst doxor ubi ci n
cyt ot oxi ci t y at concent rat i ons very similar to t hose
i nhi bi t i ng t opoi somer ase II- dependent DNA damage
(Tabl e 2; Li u e t al . , 1983; Il i aki s and Lazar, 1987); (3)
high concent rat i ons of doxor ubi ci n are known to
i nhi bi t the i nduct i on of prot ei n-associ at ed DNA
st rand breaks (Potmesil e t a L, 1983) which is expected
to i nhi bi t its own cyt ot oxi ci t y. Indeed, cl onal survival
curves usually level off at relatively high concent ra-
t i ons of doxor ubi ci n (Barranco, 1984), possi bl y due
to this phenomenon. Toget her these dat a seem to be
consi st ent with a maj or role for interference with the
br eakage- r euni on react i on of t opoi somer ase II in the
mechani sm of cyt ot oxi ci t y of doxorubi ci n.
Such a mechani sm is furt her suppor t ed by the
observat i on t hat t opoi somer ase II- dependent DNA
damage is i nhi bi t ed by ouabai n (an i nhi bi t or of
cellular Na / K ATPase), and t hat this i nhi bi t i on
was closely correl at ed with decreased cyt ot oxi ci t y of
doxor ubi ci n in the presence of ouabai n (Lawrence,
1988). Interestingly, a decreased endogenous Na/
TABLE 2. Ef f ect o f Me di um Toni ci t y on Doxorubi ci n Cy t o -
t oxi ci t y and Topoisomerase I1 Ac t i v i t y
Interference with
Medium % Clonal survival topoisomerase II
tonicity after treatment activity
(mOsm) with doxorubicin (arbitrary units)
300 0.1 - -
500 5.0 + +
1000 70.0 + + + *
1300 100.0 ND
The tonicity of the medium can interfere with both
the cytotoxicity of doxorubicin (Liu et al., 1983) and the
activity of topoisomerase II (Iliakis and Lazar, 1987).
Tonicity was increased by adding NaCI. The asterisk
indicates that interference was still incomplete. ND, not
determined.
228
H. G. KEIZER et al.
K + ATPa s e act i vi t y was obser ved in doxor ubi ci n-
resi st ant L5178Y cells ( Sugi mot o et al . , 1981). Fur -
t her mor e, cell t ypes f ound to be l ow in t opoi s omer as e
l I act i vi t y were rel at i vel y resi st ant to doxor ubi ci n
( Pot mesi l et al . , 1988). In a doxor ubi ci n- r es i s t ant
var i ant of P388 cells, r educed t opoi s omer as e II
act i vi t y was obs er ved (Defi l e et al . , 1989). Fur t he r a
cell line sel ect ed f or resi st ance t o VP-16-213, a not he r
ant i cancer dr ug t hat is consi der ed t o have t opoi s o-
mer ase II as an i mpor t a nt t ar get ( Ross et al . , 1984),
had a 10-fold l ower t opoi s omer as e II act i vi t y and was
cr oss- r esi st ant t o doxor ubi ci n ( Yal owi ch et al . , 1987).
In addi t i on, cells hyper sensi t i ve t o doxor ubi ci n
cont ai ned an el evat ed act i vi t y of t opoi s omer as e II
( Davi es et al . , 1988). Last l y, nucl ei of doxor ubi ci n-
resi st ant P388 cells showed less ant hr acycl i ne-
i nduced DNA br eaks af t er expos ur e t o doxor ubi ci n
t han nucl ei f r om sensi t i ve cells, pr obabl y as a
cons equence of r educed t opoi s omer as e II act i vi t y
( Capr ani co et al . , 1987).
In concl usi on, i nt er f er ence wi t h t opoi s omer as e II
act i vi t y is an at t r act i ve mechani s m in t he t umor i ci dal
act i on of doxor ubi ci n, but its r el at i ve i mpor t ance
r emai ns t o be est abl i shed.
5. S UMMAR Y AND CONCLUS I ONS
Doxor ubi c i n or doxor ubi c i n- i r on compl exes can
i ni t i at e t he f or ma t i on o f hydr oxyl r adi cal s af t er re-
duct i on of free doxor ubi ci n or af t er r educt i on or aut o-
oxi dat i on o f t he doxor ubi c i n- i r on compl ex. These
hydr oxyl r adi cal s can da ma ge cel l ul ar me mbr a ne s by
lipid per oxi dat i on or da ma ge cel l ul ar DNA. How-
ever, t he r el at i ve i mpor t ance o f such free radi cal
da ma ge in t he mechani s m of ki l l i ng t umor cells by
doxor ubi ci n is not cl ear, because doubl e- s t r anded
DNA, t o whi ch al mos t all i nt r acel l ul ar doxor ubi ci n
is bound, i nhi bi t s free r adi cal f or ma t i on f r om dox-
or ubi ci n whi l e d o x o r u b i c i n - i r o n compl exes have
never been det ect ed in cells t r eat ed wi t h doxor ubi ci n.
To i nvest i gat e t he possi bl e i nvol vement o f hy-
dr oxyl r adi cal s in t he mechani s m o f cyt ot oxi ci t y of
doxor ubi ci n, t wo appr oaches have been chosen. The
first is to try t o det ect OH r adi cal f or ma t i on under
condi t i ons t hat kill t he t u mo r cells and to i nvest i gat e
whet her OH r adi cal f or ma t i on cor r el at es wi t h t he
cyt ot oxi ci t y of doxor ubi ci n under var i ous condi t i ons.
The second is to i nvest i gat e t he effect of free r adi cal
scavenger s on t he cyt ot oxi ci t y of doxor ubi ci n. Un d e r
condi t i ons t hat kill t umor cells efficiently, no i nt r a-
cel l ul ar hydr oxyl r adi cal f or ma t i on can be det ect ed.
Onl y at r el at i vel y hi gh doxor ubi ci n concent r at i ons
was ext r acel l ul ar OH radi cal f or ma t i on det ect abl e.
Exper i ment s wi t h free r adi cal scavenger s show t hat
cer t ai n cell types, i ncl udi ng nor mal car di ac cells and
s ome t umor cell lines wi t h a r el at i ve defi ci ency in t hei r
ant i oxi dant def ense capaci t y, are ki l l ed by t hese
ext r acel l ul ar l y gener at ed radi cal s. However , f or t he
maj or i t y of t umor cells lines, free r adi cal i nvol vement
coul d not be de mons t r a t e d in t he mechani s m of
cyt ot oxi ci t y of doxor ubi ci n.
As doxor ubi ci n is act i ve agai nst a var i et y of solid
t umor s and l eukemi as, whi l e ma ny t umor cell t ypes
ar e not ki l l ed by a free r adi cal - dependent mechani s m
of cyt ot oxi ci t y, efficient nonr adi cal - dependent mech-
ani sms o f cyt ot oxi ci t y must al so exist. Si nce doxor u-
bi ci n at very l ow concent r at i ons has been shown t o
i nt er f er e wi t h t he act i vi t y of t opoi s omer as e II, resul t -
i ng in DNA st r and br eakage, whi l e bot h DNA st r and
br eakage and t opoi s omer as e II act i vi t y ar e cor r el at ed
wi t h t he cyt ot oxi ci t y o f doxor ubi ci n, i nt er f er ence
wi t h t opoi s omer as e II f or ms an at t r act i ve al t er nat i ve
f or free r adi cal - dependent mechani s ms of doxor u-
bi ci n cyt ot oxi ci t y agai nst t umor cells.
Acknowl edgement s- - Research in the authors' laboratories is
supported by the Dutch Cancer Society.
R EFER ENCES
ALEGRIA, A. E., SAMUNI, A., MITCHELL, J. B., R1ESZ, P. and
Russo, A. (1989) Free radicals induced by adriamycin-
sensitive and adriamycin-resistant cells: A spin-trapping
study. Biochemistry 28: 8653-8658.
ARCAMONE, F., CASSINELLI, G. and FRANCESCHI, G. (1972)
Structure and physicochemical properties of adriamycin
(doxorubicin). In: Int. Syrup. Adriamycin, pp. 9-22,
CARTER, S. K., DIMARCO, A. and GnIONE, M. (eds)
Springer, New York.
AUBEL-SADRON, G. and LONDOS-GAGLIARDI, D. (1984)
Daunorubicin and doxorubicin, anthracycline antibiotics,
a physicochemical and biological review. Biochimie 66:
333-352.
AVERBUCH, S. O., GAUD1ANO, G., KOCH, T. H. and BACHUR,
N. R. 0985) Radical dimer rescue of toxicity and im-
proved therapeutic index of adriamycin in tumor-bearing
mice. Cancer Res. 45: 620045204.
BABSON, J. R., ABELL, N. S. and REED, D. J. (1981) Protective
role of the glutathione redox cycle against adriamycin-
mediated toxicity in isolated hepatocytes. Biochem.
Pharmac. 30: 2299-2304.
BACHUR, N. R., GORDON, S. L. and GEE, M. V. (1977)
Anthracycline antibiotic augmentation of microsomal
electron transport and free radical formation. Molec.
Pharmac. 13: 901-910.
BACHUR, N. R., GORDON, S. L. and GEE, M. V. (1978) A
general mechanism for microsomal activation of quinone
anticancer agents to free radicals. Cancer Res. 38:
1745-1750.
BACHUR, N. R., GEE, M. V. and FRIEDMAN, R. D. (1982)
Nuclear catalyzed antibiotic free radical formation.
Cancer Res. 42: 1078-1081.
BARRANCO, S. C. (1984) Cellular and molecular effects of
adriamycin on dividing and nondividing cells. Pharmac.
Ther. 24: 303-319.
BATES, D. A. and WINTERBOURN, C. C. (1982) Deoxyribose
breakdown by the adriamycin semiquinone and H202:
evidence for hydroxyl radical participation. FEBS Let t .
145: 137-142.
BERLIN, V. and HASELTINE, W. A. (1981) Reduction of
adriamycin to a semiquinone-free radical by NADPH
cytochrome P-450 reductase produces DNA cleavage in a
reaction mediated by molecular oxygen. J. biol. Chem.
256: 4747-4756.
Bozzl, A., MAVELLI, I., MONDOVl, B., STROM, R. and
ROTILIO, G. (1981) Differential cytotoxicity of dauno-
mycin in tumor cells is related to glutathione dependent
hydrogen peroxide metabolism. Biochem. J. 194:369 372.
BROXTERMAN, H. J., PINEDO, H. M., KUIPER, C. M.,
SCHUtJRHU~S, G. J. and LANKELMA, J. (1989) Glycolysis in
P-glycoprotein overexpressing human tumor cell lines.
Effect of resistance modifying agents. FEBS Let t . 247:
405-4 10.
CAPRANICO, G., RIVA, A., TINELLI, S., DASDIA, T. and
ZUNINO, F. (1987) Markedly reduced levels of anthracy-
Doxorubicin (Adriamycin)
229
cline-induced DNA st rand breaks in resistant P388
leukemia cells and isolated nuclei. Cancer Res. 47:
3752-3756.
CERVANTES, A., PINEDO, H. M., LANKELMA, J. and
SCHtJURHUIS, G. J. (1988) The role of oxygen-derived free
radicals in the cytotoxicity of doxorubicin in multidrug
resistant and sensitive human ovarian cancer cells. Cancer
Lef t . 41: 169-177.
DAVIES, K. J. A., DOROSHOW, J. H., CHAN, T. M. and
HOCHSTEIN, P. (1983a) Mi t ochondri al reduction of an-
thracyclines: Oxygen radical product i on at the expense of
ATP. In: Ox y Radi cal s and their Scavenger Sys t ems ,
Vol. H: Cellular and Medi cal Aspect s, pp. 313-316,
GREENWALD, R. A. and COHEN, G. (eds) Elsevier, New
York.
DAVIES, K. J. A., DOROSHOW, J. H. and HOCHSTEIN, P.
(1983b) Mi t ochondri al NADH dehydrogenase-catalyzed
oxygen radical product i on by adriamycin, and the relative
inactivity of 5-iminodaunorubicin. FEBS Let t . 153:
227-230.
DAVIES, S. M., ROBSON, C. N., DAVIES, S. L. and HICKSON, I.
D. (1988) Nuclear topoisomerase II levels correlate with
the sensitivity of mammal i an cells to intercalating agents
and epipodophylotoxins. 3. biol. Chem. 263:17724-17729.
DEFFIE, A. M., BATRA, I. K. and GOLDBERG, G. J. (1989)
Direct correlation between DNA topoisomerase II
activity and cytotoxicity in adriamycin-sensitive and
-resistant P388 leukemia cell lines. Cancer Res. 49: 58~2.
DOROSHOW, J. H. (I 983a) Effect of anthracycline antibiotics
on oxygen radical format i on in rat heart. Cancer Res. 43:
460-472.
DOROSHOW, J. H. (1983b) Anthracycline antibiotic-
stimulated superoxide, hydrogen peroxide, and hydroxyl
radical product i on by NADH dehydrogenase. Cancer
Res. 43: 4543-4551.
DOROSHOW, J. H. (1986a) Prevention of doxorubicin-
induced killing of MCF-7 human breast cancer cells by
oxygen radical scavengers and iron chelating agents.
Bi ochem. biophys. Res. Commun. 135: 330-335.
DOROSHOW, J. H. (1986b) Role of hydrogen peroxide and
hydroxyl radical format i on in the killing of Ehrlich t umor
cells by anticancer quinones. Proc. natn. Acad. Sci. U. S. A.
83: 4514-4518.
DOROSHOW, J. H., LOCKER, G. Y. and MYERS, C. E. (1980)
Enzymatic defenses of the mouse heart against reactive
oxygen metabolites; alterations produced by doxorubicin.
J. clin. Invest. 65: 128-135.
DOROSHOW, J. H., LOCKER, G. Y., IFRIM, I. and MYERS, C. E.
(1981) Prevention of doxorubicin cardiac toxicity in the
mouse by N-acetylcysteine. J. di n. Invest. 68: 1053-1064.
ELIOT, H., GIANNI, L. and MYERS, C. (1984) Oxidative
destruction of DNA by the adri amyci n-i ron complex.
Bi ochemi st ry 23: 928-936.
ERTTMANN, R., ERB, N., STEINHOFF, A. and LANDBECK, G.
(1988) Pharmacokinetics of doxorubicin in man: dose and
schedule dependence. J. Cancer Res. clin. Oncol. 114:
509-513.
FREEMAN, R. W., MACDONALD, J. S., OLSON, R. D., BOERTH,
R. C., OATES, J. A. and HARBISON, R. D. (1980)
Effect of sulfhydryl-containing compounds on the anti-
t umor effects of adriamycin. Toxi c. appl. Pharmac. 54:
168-175.
FUJITA, K., SHINPO, K., YAMADA, K., SATO, T., NIIMI, H.,
SHAMOTO, M., NAGATSU, T., TAKEUCHI, T. and UMEZAWA,
H. (1982) Reduction of adriamycin toxicity by ascorbate
in mice and Gui nea pigs. Cancer Res. 42: 309-316.
GELVAN, D. and SAMUNI, A. (1988) Reappraisal of the
association between adriamycin and iron. Cancer Res. 48:
5645-5649.
GIANNI, L., ZWEIER, J. L., LEVY, A. and MYERS, C. E. (1985)
Characterization of the cycle of iron-mediated electron
transfer from adriamycin to molecular oxygen. J. biol.
Chem. 260: 6820~i826.
GIANNI, U, VIGANO, L., LANZI, C., NIGGELER, M. and
MALATESTA, V. (1988) Role of daunosami ne and hydroxy-
acetyl side chain in reaction with i ron and lipid peroxida-
tion by anthracyclines. J. nam. Cancer Inst. 80:
l l 04-1111.
GIGLI, M., DOGLIA, S. M., MILLOT, J. M., VALENTINI, L. and
MANFAIT, M. (1988) Quant i t at i ve study of doxorubicin in
living cell nuclei by microspectrofluorometry. Biochim.
biophys. Act a 950: 13-20.
GLAZER, R. I., HARTMAN, K. D. and RICHARDSON, C. L.
(1982) Cytokinetic and biochemical effects of 5-
i mi nodaunorubi ci n in human colon carcinoma in culture.
Cancer Res. 42: 117-121.
GOODMAN, J. and HOCHSTEIN, P. (1977) Generat i on of free
radicals and lipid peroxidation by redox cycling of
adriamycin and daunomycin. Bi ochem. biophys. Res.
Commun. 77: 797-803.
GREEN, M. D., SPEYER, J. L. and MUGGIA, F. M. (1984)
Cardiotoxicity of anthracyclines. Eur. J. Cancer clin.
Oncol. 20: 293-296.
GRIFFITH, O. W. and MEISTER, A. (1979) Glutathione: inter-
organ translocation, turnover, and metabolism. Proc.
natn. Acad. Sci. U. S. A. 76: 5606-5610.
GUTI~R~Z, P. L., GEE, M. V. and BACHUR, N. R. (1983)
Kinetics of anthracycline antibiotic free radical format i on
and reductive glycosidase activity. Archs Biochem. Bi o-
phys. 223: 68-75.
GUTTERIDOE, J. M. C. (1982) The role of superoxide and
hydroxyl radicals in phospholipid peroxidation catalysed
by iron salts. FEBS Let t . 150: 454~58.
GUTTERIDGE, J. M. C. (1983) Adriamycin-iron catalysed
phospholipid peroxidation: a reaction not involving
reduced adriamycin or hydroxyl radicals. Biochem. Phar-
mac. 32: 1949-1952.
GUTTERIDGE, J. M. C. (1984) Lipid peroxidation and possi-
ble hydroxyl radical format i on stimulation by the self-
reduction of a doxorubi ci n-i ron (III) complex. Biochem.
Pharmac. 33: 1725-1728.
GUTTERIDGE, J. M. C. and TOEG, D. (1982) Adriamycin-
dependent damage to deoxyribose: a reaction involving
iron, hydroxyl and semiquinone free radicals. FEBS Let t .
149: 228-232.
HAMILTON, T. C., WINKER, M. A., LOUIE, K. G., BATIST, G.,
BEHRENS, B. C., TSURUO, T., GROTZINGER, K. R., MCKOY,
W. M., YOUNG, R. C. and OZOLS, R. F. (1985) Augment a-
tion of adriamycin, melphalan, and cisplatin cytotoxicity
in drug-resistant and -sensitive human ovarian carcinoma
cell lines by but hi oni ne sulfoximine mediated glutathione
depletion. Bi ochem. Pharmac. 34: 2583-2586.
ILIAKIS, G. and LAZAR, W. (1987) Effect of sodium chloride
concent rat i on on adriamycin and N-trifluoroacetyladri-
amycin-14-valerate(AD32)-induced cell killing and DNA
damage in Chinese hamst er V79 cells. Cancer Res. 47:
1853-1858.
JOHNSON, B. A., CHEANG, M. S. and GOLDENBERG, G. J.
(1986) Compari son of adriamycin uptake in chick embryo
heart and liver cells and murine L5178Y lymphoblasts in
vitro: role of drug upt ake in cardiotoxicity. Cancer Res.
46: 218-223.
JULICHER, R. H. M., VAN DER LAARSE, A., STERRENBERG, L.,
BLOYS VAN TRESLONG, C. H. F., BAST, A. and NOORDHOEK,
J. (1985) The involvement of an oxidative mechanism in
the adriamycin induced toxicity in neonatal rat heart cell
cultures. Res. Commun. Chem. Pat h. Pharmac. 47: 35-47.
KALYANARAMAN, B., PEREZ-REYES, E. and MASON, R. P.
(1980) Spin-trapping and direct electron spin resonance
investigations of the redox metabolism of qui none anti-
cancer drugs. Biochem. biophys. Act a 630: 119-130.
KEIZER, H. G., VAN RIJN, J., PINEDO, H. M. and JOENJE, H.
(1988) Effect of endogenous glutathione, superoxide
dismutases, catalase, and glutathione peroxidase on adri-
amycin tolerance of Chinese hamst er ovary cells. Cancer
Res. 48: 4493-4497.
230 H. G. KEIZER et al.
KEIZER, H. G., DE LEEUW, S. J., VAN RIJN, J., PINEDO, H. M.
and JOENJE, H. (1989a) Effect of artificial electron accep-
tors on the cytotoxicity of mitomycin C and doxorubicin
in human lung t umor cells. Eur. J. Cancer clin. Oncol. 25:
1113-1118.
KEIZER, H. G., SCnUURHUIS, G. J., BROXTERMAN, H. J.,
LANKELMA, J., SCHOONEN, W. G. E. J., VAN RIJN, J.,
P1NEDO, H. M. and JOENJE, H. (1989b) Correl at i on of
multidrug resistance with decreased drug accumulation,
altered subcellular drug di st ri but i on and increased P-
glycoprotein expression in cultured SW-1573 human lung
t umor cells. Cancer Res. 49: 2988-2993.
KENNEDY, K. A., SIEGFRIED, J. M., SARTORELLI, A. C. and
TRITTON, T. R. (1983) Effects of anthracyclines on oxy-
genated and hypoxic t umor cells. Cancer Res. 43: 54-59.
KRAMER, R, A., ZAKHER, J. and KIM, G. (1988) Role of the
gl ut at hi one redox cycle in acquired and de novo multi-
drug resistance. Science 241: 694-697.
LAMPIDIS, T. J., JOHNSON, L. V. and ISRAEL, M. (1981) Effects
of adriamycin on rat heart cells in culture: increased
accumulation and nucleoli fragment at i on in cardiac
muscle v. non-muscle cells. J. molec, cell. Cardiol. 13:
913-924.
LANE, P., VICHI, P., BAIN, D. L. and TRITTON, T. R. (1987)
Temperat ure dependence studies of adriamycin upt ake
and cytotoxicity. Cancer Res. 47: 4038-4042.
LAWRENCE, T. S. (1988) Reduction of doxorubicin cytotox-
icity by ouabain: correlation with topoisomerase-induced
DNA st rand breakage in human and hamst er cells.
Cancer Res. 48: 725-730.
LAZZAR1NO, G., VIOLA, A. R., MULLER1, L., ROTILIO, G. and
MAVELLI, I. (1987) Prevention by fructose-l, 6-biphos-
phat e of cardiac oxidative damage induced in mice by
subchroni c doxorubicin treatment. Cancer Res. 47:
651 lq5516.
LIU, L. F., ROWE, T. C., YANG, L., TEWEY, K. M. and CHEN,
G. L. (1983) Cleavage of DNA by mammal i an DNA
topoisomerase II. J. biol. Chem. 258: 15365-15370.
MEIJER, C., MULDER, N . H. , TIMMER-BOSSCHA, H., ZIJLSTRA,
J. G. and DE VR1ES, E. G. E. (1987) Role of free radicals
in an adriamycin-resistant human small cell lung cancer
cell line. Cancer Res. 47: 4613-4617.
MEREDITH, M. J. and REED, D. J. (1983) Depletion in vitro
of mi t ochondri al gl ut at hi one in rat hepatocytes and
enhancement of lipid peroxidation by adriamycin and
1,3-bis(2-chloroethyl)-l-nitrosourea (BCNU). Biochem.
Pharmac. 32: 1383-1388.
MIMNAUGH, E. G. (1986) Pot ent i at i on by reduced gluta-
t hi one of Adriamycin-stimulated lipid peroxidation in
kidney microsomes. Biochem. Pharmac. 35: 4337-4339.
MIMNAUGH, E. G., TRUS8, M. A. and GRAM, T. E. (1981)
Stimulation by adriamycin of rat heart and liver micro-
somal NADPH- dependent lipid peroxidation. Biochem.
Pharmac. 30: 2797-2804.
MIMNAUG8, E. G., TRUS8, M. A., GINSaURG, E. and GRAM,
T. E. (1982) Differential effects of anthracycline drugs on
rat heart and liver microsomal reduced nicotinamide
adenine dinucleotide phosphat e-dependent lipid peroxi-
dation. Cancer Res. 42: 3574-3582.
MIMNAUGH, E. G., GRAM, T. E. and TRUSH, M. A. (1983)
Stimulation of mouse heart and liver microsomat lipid
peroxidation by anthracycline anticaneer drugs: charac-
terization and effects of reactive oxygen scavengers.
J. Pharmac. e.xp. Ther. 226: 806-816.
MIMNAUGH, E. G., KENNEDY, K. A., TRUSH, M. A. and
SINHA, B. K. (1985a) Adriamycin-enhanced membrane
lipid peroxidation in isolated rat nuclei. Cancer Res. 45:
3296-3304.
MIMNAUGH, E. G., TRUSH, M. A., BHATNAGAR, M. and
GRAM, T. E. (1985b) Enhancement of reactive oxygen-
dependent mi t ochondri al membrane lipid peroxidation by
the anticancer drug adriamycin. Biochem. Pharmac. 34:
847-856.
MIMNAUGH, E. G., TRUSH, M. A. and GRAM, T. E. (1986) A
possible role for membrane lipid peroxidation in ant hra-
cycline nephrotoxicity. Biochem. Pharmac. 35: 4327-4335.
MOORE, H. W. (1977) Bioactivation as a model for drug
design bioreductive alkylation. Science 197:527 532.
MROSS, K., MAESSEN, P., VAN DER VIJGH, W. J. F., GALL, H.,
BOVEN, E. and PINEDO, H. M. (1988) Pharmacokinetics
and metabolism of epidoxorubicin and doxorubicin in
humans. J. din. Oncol. 6: 517-526.
MUINDI, J. R. F., SINHA, B. K., GIANII, L. and MYERS, C. E.
(1984) Hydroxyl radical product i on and DNA damage
induced by ant hracycl i ne-i ron complex. FEBS Lett. 172:
226-230.
MUINDI, J., S1NHA, B. K., GIANNI, L. and MYERS, C. (1985)
Thiol-dependent DNA damage produced by anthracy-
cline-iron complexes; the structure-activity relationships
and molecular mechanisms. Molec. Pharmac. 27:
356-365.
MULIAWAN, H., SCHEULEN, M. E. and KAPPUS, H. (1980)
Acute adriamycin t reat ment of rats does not increase
et hane expiration. Res. Commun. Chem. Path. Pharmac.
3 0 : 5 0 9 - 5 1 9 .
MYERS, C. E., LISS, R. H., IFRIM, 1., GROTZINGER, K. and
YOUNG, R. C. (1977) Adriamycin: the role of lipid perox-
idation in cardiac toxicity and t umor response. Science
197: 165-167.
MYERS, C. E., GIANN1, L., S1MONE, C. B., KLECKER, R. and
GREENE, R. (1982) Oxidative destruction of erythrocyte
ghost membranes catalyzed by the doxorubi ne iron
complex. Biochemistry 2 1 : 1 7 0 7 1713.
NEWMAN, R. A., HACKER, M. P. and KRAKOEE, L H. (1981)
Amel i orat i on of adriamycin and daunorubi ci n myo-
cardial toxicity by adenosine. Cancer Res. 41: 3483-3488.
NOHL, H. and JORDAN, W. (1983) OH' -generat i on by adri-
amycin semiquinone and H202: an explanation for the
cardiotoxicity of anthracycline antibiotics. Biochem. bio-
phys. Res. Commun. 114: 197-205.
NORONHA-DUTRA, A. A. and STEEN, E. M. (1982) Lipid
peroxidation as a mechani sm of injury in cardiac my-
ocytes. Lab. Invest. 47: 346 353.
OLSON, H. M. and CAPEN, C. C. (1977) Subacute cardio-
toxicity of adriamycin in the rat. Biochemical and ultra-
structural investigations. Lab. Invest. 37: 386-394.
OLSON, R. D., MACDONALD, J. S., VAN BOXTEL, C. J.,
BOERTH, R. C., HARB1SON, R. D., SLON1M, A. E., FREEMAN,
R. W. and OATES, J. A. (1980) Regulatory role of gluta-
thione and soluble sulfhydryl groups in the toxicity of
adriamycin. 3. Pharmac. exp. TheE. 215: 450-454.
PAN, S.-S. and BACHUR, N. R. (1980) Xant hi ne oxidase
catalyzed reductive cleavage of anthracycline antibiotics
and free radical formation. Molec. Pharmae. 17: 95--99.
PAN, S.-S., PEDERSEN, L. and BACHUR, N. R. (1981) Compar-
ative flavoprotein catalysis of anthracycline antibiotic:
reductive cleavage and oxygen consumption. Molec.
Pharmac. 19: 184 186.
PANNEERSELVAM, M., I~REDEI-IORST, R. and VOGEL, C. W.
(1987) Cell surface cytotoxic effect of immobilized
doxorubicin is target cell-dependent and involves oxygen
radical formation. Proc. Am. Ass. Cancer Res. 28: 267.
PORTA, E. A., JOUN, N. S., MATSUMURA, L., NAKASONE, B.
and SABLAN, H. (1983) Acute adriamycin cardiotoxicity in
rats. Res. Commun. Chem. Path. Pharmac. 41: 125 137.
POTMESIL, M., KIRSCHENBAUM, S., ISRAEL, M., LEVIN, M.,
KrmTARPAL, V. K. and SILBER, R. (1983) Relationship of
Adriamycin concent rat i ons to the DNA lesions induced
in hypoxic and euoxic LI210 cells. Cancer Res. 43:
3528-3533.
POTMESIL, M., ISRAEL, M. and SILVER, R. (1984) Two
mechanisms of Adri amyci n-DNA interaction in L1210
cells. Biochem. Pharmac. 33: 3137 3142.
POTMESIL, M., HSIANG, Y, H,, LIU, L. F,, BANK, B.,
GROSSBERG, H., KIRSCHENBAUM, S., F'ORLENZAR, T. J.,
PENZINER, A., KANGANIS, D., KNOWLES, D., TRAGANOS, F'.
Doxorubicin (Adriamycin) 231
and SILVER, R. (1988) Resistance of human leukemic and
normal lymphocytes to drug-induced DNA cleavage and
low levels of DNA topoisomerase II. Cancer Res. 48:
3537-3543.
RAJAGOPALAN, S., POLITI, P. M., SINHA, B. K. and MYERS, C.
E. (1988) Adriamycin-induced free radical format i on in
the perfused rat heart: implications for cardiotoxicity.
Cancer Res. 48: 4766-4769.
RAMU, A., COHEN, L. and GLAUBIGER, D. (1984) Oxygen
radical detoxification enzymes in doxorubicin-sensitive
and -resistant P388 murine leukemia cells. Cancer Res. 44:
1976-1980.
ROGERS, K. E. and T6K~S, Z. A. (1984) Novel mode of
cytotoxicity obt ai ned by coupling inactive Anthracycline
to a polymer. Bi ochem. Pharmac. 33: 605~08.
ROGERS, K. E., CARR, B. I. and TOKES, Z. A. (1983)
Cell surface-mediated cytotoxicity of polymer-bound
Adramyci n against drug-resistant hepatocytes. Cancer
Res. 43: 2741 2748.
Ross, K. L., AKMAN, S. A., SIK1C, B. I. and DOROSHOW, J. H.
(1988) Free radical detoxifying enzymes in adriamycin-
resistant cell lines. Proc. Am. Ass. Cancer Res. 29: 503.
ROSS, W. E. and SMITH, M. C. (1982) Repair of deoxyribonu-
cleic acid lesions caused by Adriamycin and ellipticine.
Bi ochem. Pharmac. 31:1931 1935.
Ross, W., ROWE, T., GLISSON, B., YALOWICH, J. and LID, L.
(1984) Role of topoisomerase II in mediating epipodo-
phyllotoxin-induced DNA cleavage. Cancer Res. 44:
5857 5860.
ROWLEY, D. A. and HALLIWELL, B. (1983) DNA damage
by superoxide-generating systems in relation to the mech-
anism of action of the ant i -t umor antibiotic Adriamycin.
Biochim. biophys. Act a 761: 86-93.
SATO, S., IWAIZUMI, M., HANDRA, K. and TAMURA, Y. (1977)
Electron spin resonance study on the mode of generation
of free radicals of daunomycin, adriamycin, and carbo-
quone in NAD(P)H-mi crosome system. Gann 68:
603~08.
SINHA, B. K. and CHIGNELL, C. F. (1979) Binding mode of
chemically activated semiquinone free radicals from
qui none anticancer agents to DNA. Chem. Biol. Interact.
28: 301-308.
SINHA, B. K. and LEWIS GREGORY, J. (1981) Role of one-
electron and two-electron reduction products of
adriamycin and daunomyci n in deoxyribonucleic acid
binding. Bi ochem. Pharmac. 30: 2626-2629.
SINHA, B. K., TRUSH, M. A., KENNEDY, K. A. and
MIMNAUGH, E. G. (1984) Enzymatic activation and
binding of adriamycin to nuclear DNA. Cancer Res. 44:
2892 2896.
SINHA, B. K., KATKI, A. G., BATIST, G., COWAN, K. H. and
MYERS, C. E. (1987a) Adriamycin-stimulated hydroxyl
radical format i on in human breast t umor cells. Biochem.
Pharmac. 36: 793 796.
SINHA, B. K., KATKI, A. G., BATIST, G., COWAN, K. H. and
MYERS, C. E. (1987b) Differential format i on of hydroxyl
radicals by Adriamycin in sensitive and resistant MCF-7
human breast t umor cells: implications for the mechanism
of action. Bi ochemi st ry 26: 3776 3781.
STERRENBERG, t . , JULICHER, R. H. M., GOOSSENS, P. A. L.,
BAST, A. and NOORDHOEK, J. (1985) Anthracycline-
induced oxygen consumpt i on and oxidative damage in rat
liver microsomes are not necessarily coupled: a study
with 8 structurally related anthracylines. Free Rad. Res.
Commun. 1: 41-54.
SUGIMOTO, Y., NISHIMURA, T., SUZUKI, H. and TANAKA, N.
(1981) Al t erat i on of membrane-associated enzymes in
drug-resistant sublines of mouse l ymphobl ast oma
L5178Y cells. J. Ant i bi ot i cs 34: 1200-1205.
SUG1OKA, K. and NAKANO, M. (1982) Mechanism of
phospholipid peroxidation induced by ferric ion-ADP-
adriamycin-co-ordination complex. Biochim. biophys.
Act a 713: 333-343.
SVINGEN, B. A. and PowIs, G. (1981) Pulse radiolysis studies
of ant i t umor quinones: radical lifetimes, reactivity with
oxygen, and one-electron reduction potentials. Archs
Biochem. Biophys. 2119:119-126.
TEWEY, K. M., CHEN, G. L., NELSON, E. M. and LIU, L. F.
(1984a) Intercalative ant i t umor drugs interfere with the
breakage-reunion reaction of mammal i an DNA topoiso-
merase II. J. biol. Chem. 259: 9182-9187.
TEWEY, K. M., ROWE, T. C., YANG, L., HALLIGAN, B. D. and
LIu, L. F. (1984b) Adriamycin-induced DNA damage
mediated by mammal i an DNA topoisomerase II. Sci ence
226: 466-468.
THAYER, W. S. (1984) Serum lipid peroxides in rats treated
chronically with adriamycin. Bi ochem. Pharmac. 33:
2259-2263.
THORNALLEY, P. J. and DODD, N. J. F. (1985) Free radical
product i on from normal and adriamycin-treated rat
cardiac sarcosomes. Bi ochem. Pharmac. 34: 669~574.
TRITTON, T. R. and YEE, G. (1982) The anticancer agent
Adriamycin can be actively cytotoxic without entering
cells. Sci ence 217: 248-250.
WADLER, S., GREEN, M. D. and MUGGIA, F. M. (1986)
Synergistic activity of doxorubicin and the bisdioxopi-
perazine (+)-l, 2-Bis(3, 5-dioxopiperazinyl-l-yl)propane
( ICRF 187) against the routine sarcoma Sl 80 cell line.
Cancer Res. 46: 1176- I 181.
WINTERBOURN, C. C., GUTTERIDGE, J. M. C. and HALLIWELL,
B. (1985) Doxorubicin-dependent lipid peroxidation at
low partial pressures of 02. J. Free Rad. Biol. Med. 1:
43-49.
YALOWICH, J. C., ROBERTS, D., BENTON, S. and PARGANAS, E.
(1987) Resistance to etoposide (VP-16) in human
leukemia K562 cells is associated with altered DNA
topoisomerase II (TOPO II) activity and rapid reversal of
drug-induced DNA damage. Proc. Am. Ass. Cancer Res.
28: 277.
YODA, Y., NAKAZAWA, M., ABE, T. and KAWAKAMI, Z.
(1986) Prevention of doxorubicin myocardial toxicity
in mice by reduced glutathione. Cancer Res. 46:
2551-2556.
YOUNG, R. C., OZOLS, R. F. and MYERS, C. E. (1981) The
anthracycline antineoplastic drugs. Ne w Engl. J. Med.
305: 139-153.
ZWEIER, J. L. (1983) Reduction of 02 by iron-adriamycin.
J. biol. Chem. 259: 6056-6058.
ZWEIER, J. L. (1985) Iron-mediated format i on of an oxidized
adriamycin free radical. Biochim. biophys. Act a 839:
209-213.
ZWE1ER, J. L., GIANNI, L., MUINDI, J. and MYERS, C. E.
(1986) Differences in O 2 reduction by the iron complexes
of adriamycin and daunomycin- the importance of the
sidechain hydroxyl group. Biochim. biophys. Act a 884:
326-336.
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- ISBN Book Abstract ICONMIN 2020Dokument91 SeitenISBN Book Abstract ICONMIN 2020Lini Anisfatus SholihahNoch keine Bewertungen
- Surgical Sponges - Towels WebDokument20 SeitenSurgical Sponges - Towels WebDa Josh MarienellaNoch keine Bewertungen
- Supervivencia Dental A Largo Plazo Después Del Tratamiento Regenerativo de Defectos IntraóseosDokument7 SeitenSupervivencia Dental A Largo Plazo Después Del Tratamiento Regenerativo de Defectos IntraóseosAgustin BuryakNoch keine Bewertungen
- WD D-Healthy TravelerDokument6 SeitenWD D-Healthy TravelercjNoch keine Bewertungen
- CBME Time Table Phase - II 2022Dokument36 SeitenCBME Time Table Phase - II 2022IrfanNoch keine Bewertungen
- M&E Training ManualDokument45 SeitenM&E Training Manualsheittie100% (1)
- Social Perspectives - Unit 10 - Task 1 - Copy 123Dokument13 SeitenSocial Perspectives - Unit 10 - Task 1 - Copy 123zxko24Noch keine Bewertungen
- Increased Intracranial PressureDokument10 SeitenIncreased Intracranial Pressureapi-3822433100% (10)
- Cancer and Oncology Nursing NCLEX Practice Quiz ANSDokument5 SeitenCancer and Oncology Nursing NCLEX Practice Quiz ANSyanyan cadizNoch keine Bewertungen
- 1078-Texto Del Artículo-2743-1-10-20171030 PDFDokument12 Seiten1078-Texto Del Artículo-2743-1-10-20171030 PDFRichard Copa AliNoch keine Bewertungen
- AmyloidosisDokument15 SeitenAmyloidosisNicoletta OrphanouNoch keine Bewertungen
- Introduction To Medical Microbiology, Parasitology & Immunology - Oct 2022Dokument16 SeitenIntroduction To Medical Microbiology, Parasitology & Immunology - Oct 2022Esther WanjukiNoch keine Bewertungen
- Presentation DiarrheaDokument23 SeitenPresentation DiarrheaVenkatesh KS 233Noch keine Bewertungen
- Medical Cannabis For The Treatment of DementiaDokument24 SeitenMedical Cannabis For The Treatment of DementiaLorina BoligNoch keine Bewertungen
- Basic Ethical Principles 1. StewardshipDokument5 SeitenBasic Ethical Principles 1. Stewardshipmitsuki_sylph83% (6)
- PERFORMING CPT (Percussion, Vibaration, Postural DrainageDokument6 SeitenPERFORMING CPT (Percussion, Vibaration, Postural DrainageBianx Flores DosdosNoch keine Bewertungen
- COVID-19 Vaccine - Quick Information For PharmaciesDokument18 SeitenCOVID-19 Vaccine - Quick Information For PharmaciesDaxaNoch keine Bewertungen
- NCP Dengue Fever Hyperthermia and Acute PainDokument4 SeitenNCP Dengue Fever Hyperthermia and Acute PainJordz PlaciNoch keine Bewertungen
- GR.6 Practical ResearchDokument4 SeitenGR.6 Practical ResearchRovi Gie ArabitNoch keine Bewertungen
- UnaniDokument16 SeitenUnaniRahul Banik888Noch keine Bewertungen
- Epilepsi 1Dokument12 SeitenEpilepsi 1Ima SoniaNoch keine Bewertungen
- I 693instrDokument11 SeitenI 693instrShivana SeeramNoch keine Bewertungen
- INR Price ListDokument56 SeitenINR Price ListBINISHNoch keine Bewertungen
- An Ethnobotanical Survey of Medicinal Plants Used in Terai Forest of Western NepalDokument15 SeitenAn Ethnobotanical Survey of Medicinal Plants Used in Terai Forest of Western NepalLeandro DouglasNoch keine Bewertungen
- Hypertension LecturesDokument65 SeitenHypertension LecturesAdebisiNoch keine Bewertungen
- InsuracneDokument4 SeitenInsuracnesathishbabuNoch keine Bewertungen
- Saunders Lumbar TractionDokument12 SeitenSaunders Lumbar TractionIra AdventiaNoch keine Bewertungen
- Role of Nurse Hospitalized ChildDokument29 SeitenRole of Nurse Hospitalized ChildAjay Remya100% (2)
- Nursing Care Plan Surgical PDFDokument2 SeitenNursing Care Plan Surgical PDFDanielle Audrey100% (2)
- Appropriate Maximum Phlebotomy Volumes: Neonate, Infant and Pediatric PopulationDokument2 SeitenAppropriate Maximum Phlebotomy Volumes: Neonate, Infant and Pediatric PopulationEthiopia HagereNoch keine Bewertungen