Beruflich Dokumente
Kultur Dokumente
Risk Factors and Long-Term Health Consequences of Macrosomia
Hochgeladen von
Khuriyatun NadhifahOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Risk Factors and Long-Term Health Consequences of Macrosomia
Hochgeladen von
Khuriyatun NadhifahCopyright:
Verfügbare Formate
Journal of Biomedical Research, 2012, 26(4): 235-240
JBR
Research Paper
doi:10.7555/JBR.26.20120037
Abstract
We sought to determine risk factors associated with fetal macrosomia and to explore the long-term consequence
of infant macrosomia at the age of 7 years. A prospective population based cohort study was designed to examine
the associations between maternal and perinatal characteristics and the risk of macrosomia. A nested case-control
study was conducted to explore the long-term health consequence of infant macrosomia. The mean maternal age
of the macrosomia group was 24.743.32 years, which is slightly older than that in the control group (24.353.14
years, P = 0.000). The mean maternal body mass index (BMI) at early pregnancy was 22.752.81 kg/m
2
, which
was also higher than that in the control group (21.762.59 kg/m
2
, P = 0.000). About 64.6% of macrosomic ne-
onates were males, compared with 51.0% in the control group (P = 0.000). Compared with women with normal
weight (BMI: 18.5-23.9 kg/m
2
), women who were overweight (BMI: 24-27.9 kg/m
2
) or obese (BMI 28 kg/m
2
),
respectively, had a 1.69-fold (P = 0.000) and a 1.49-fold (P = 0.000) increased risks of having a neonate with
macrosomia, while light weight (BMI<18.5 kg/m
2
) women had an approximately 50% reduction of the risk. Fur-
thermore, macrosomia infant had a 1.52-fold and 1.50-fold risk, respectively, of developing overweight or obesity
at the age of 7 years (P = 0.001 and P = 0.000). Older maternal age, higher maternal BMI at early pregnancy and
male gender were independent risk factors of macrosomia. Macrosomic infant was associated with an increased
predisposition to develop overweight or obesity at the beginning of their childhood.
Keywords: risk factors, long-term, health consequences, macrosomia
Risk factors and long-term health consequences of macrosomia:
a prospective study in Jiangsu Province, China
Shouyong Gu
a
, Xiaofei An
b
, Liang Fang
a
, Xiaomin Zhang
c
, Chunyan Zhang
c
, Jingling Wang
c
, Qilan
Liu
d
, Yanfang Zhang
a
, Yongyue Wei
a
, Zhibin Hu
a
, Feng Chen
a
, Hongbing Shen
a,*
a
Department of Epidemiology and Biostatistics, School of Public Health, Nanjing Medical University, Nanjing, Jiangsu 210029,
China;
b
Department of Endocrinology, Jiangsu Province Hospital of Chinese Medicine, Nanjing, Jiangsu 210029, China;
c
Department of Science and Technology, Jiangsu Population and Family Planning Committee, Nanjing, Jiangsu 210008, China;
d
Genitalia Hygiene Research Center, Jiangsu Institute of Planned Parenthood Research, Nanjing, Jiangsu 210036, China.
Received 10 April 2012, Revised 08 May 2012, Accepted 24 May 2012, Epub 06 July 2012
This study was supported by grants from the Jiangsu Birth Defects
Intervention Program (No. JS200302) and the Natural Science Foundation
of Jiangsu Province (No. BK2008501).
*
Corresponding author: Hongbing Shen, M.D., Ph.D, Department of
Epidemiology and Biostatistics, School of Public Health, Nanjing
Medical University, 140 Hangzhong Road, Nanjing, Jiangsu 210029,
China, Tel/Fax: +86-25-86862745/+86-25-86527613, E-mail: hbshen@
njmu.edu.cn.
The authors reported no conflict of interest.
Available at http://elsevier.com/wps/find/journaldes-cription.cws_
home/723905/description#description.
c
2012 by the Journal of Biomedical Research. All rights reserved.
236
Gu S et al. / Journal of Biomedical Research, 2012, 26(4): 235-240
INTRODUCTION
Fetal macrosomia has attracted immense attention
because of the increased risk for both mothers and in-
fants. For mothers, it is well established that delivery
of a macrosomic newborn is a risk factor for protracted
labor, caesarean delivery and postpartum hemorrhage.
For macrosomic infants, short-term consequence is
birth trauma
[1]
, and long-term consequences include
increased predisposition to develop obesity and type 2
diabetes later in life
[2]
. Birth weight varies depending
on several maternal characteristics, including racial
origin, age, body mass index (BMI), parity and ciga-
rette smoking. It also depends on medical conditions,
such as pre-pregnancy diabetes mellitus
[3-5]
.
A trend toward a higher birth weight has been
demonstrated in most developed countries in recent
decades
[6-8]
. Chinese national health services survey
showed that birth weight increased from 3,186 g in
1993 to 3,300 g in 2008
[9]
. A rapid increase in the rate
of macrosomia has been reported in China. For ex-
ample, Bao et al.
[10]
found that the incidence of mac-
rosomia increased from 8.31% in 2001 to 10.50% in
2005 in the city of Harbin. In Shanghai, the rate of
macrosomia increased by 50% from 1989 to 1999
[11]
.
However, few studies were performed on the contri-
butions of risk factors to the increased incidence of
macrosomia and the long-term health risks in adult-
hood and even childhood. In the present study, a
population-based survey was therefore conducted to
examine risk factors for macrosomia in Jiangsu prov-
ince, China. We also explored the long-term health
consequences of infant macrosomia.
SUBJECTS AND METHODS
Subjects
Ninety-five communities were randomly selected
as surveillance spots by stratified cluster sampling in
Jiangsu province, China. All pregnant women in the
communities at the first trimester were investigated.
Each woman was assigned a unique identification
number when she was at the first prenatal care visit.
The women were followed up during their pregnancy,
delivery and immediate postpartum period by local
family planning service professionals. We collected
information on parental demographics, maternal med-
ical, reproductive history, and medical conditions dur-
ing pregnancy and pregnancy outcome (such as gesta-
tional age, birth weight, birth length, gender of baby,
and congenital anomalies). In 2010, we conducted a
cross-sectional study of birth cohort that consisted of
macrosomia and the controls delivered in 2003. All
information on the children's growth and development
(weight, height) were collected. The protocol was ap-
proved by the local institutional review boards of each
author's affiliated institutions, and all subjects pro-
vided signed informed consent.
Women with multiple pregnancies, preterm births,
and insufficient information on birth weight at term
were not included in this present study. Cases with
congenital malformations and low birth weight were
excluded from the study. Any normal singleton baby
delivered at term that weighed 4,000 g or more was
classified as macrosomic, irrespective of gestational
age
[12]
. We carried out a comparison of factors related
to macrosomia between 2,488 macrosomic newborns
and a control group of 18,827 newborns, who weighed
from 2,500 g to 3,999 g, using an unmatched case-
control study design. We also performed a comparison
of the development at the age of 7 years between 700
children with macrosomia and a control group of 5137
with normal birth weight from the birth cohort, by us-
ing an unmatched nested case-control study design.
The study was approved by Jiangsu population and
family planning committee. Written informed consent
was obtained from the participants or their legal sur-
rogates.
We examined risk factors for macrosomia in the
context of maternal age, maternal education, maternal
residence, maternal BMI at early pregnancy (within
12 weeks of gestation), maternal smoking/drinking
during pregnancy, and infant gender. Maternal edu-
cation was categorized as elementary school or less,
junior middle school, high school or above. Maternal
BMI at early pregnancy was based on measured height
and weight at the first prenatal visit during the first
trimester. According to the Group of China Obesity
Task Force reference
[13]
, maternal BMI was grouped
into four categories: < 18.5 kg/m
2
, 18.5-23.9 kg/m
2
,
24-27.9 kg/m
2
, and 28 kg/m
2
; BMI for boys at the
age of 7 years was grouped into three categories: nor-
mal (< 17.4 kg/m
2
), overweight (17.4-19.2 kg/m
2
), and
obesity (19.2 kg/m
2
); BMI for girls at the age of 7
years was grouped into three categories: normal (<
17.2 kg/m
2
), overweight (17.2-18.9 kg/m
2
), and obes-
ity ( 18.9 kg/m
2
).
Statistical analysis
Continuous data were described as meanstandard
deviation (SD), and categorical data were described
as proportion. Continuous variables in two independ-
ent groups were compared by Student's t test. The
chi-square test and rank sum test were used when
comparing dichotomous and rank data separately.
Logistic regression was used to examine the associa-
Risk factors and long-term health consequences of macrosomia
237
tions between maternal and perinatal characteristics
and the risk of macrosomia. Odds ratio (OR) with
95% confidence interval (95% CI) for each candidate
factor was calculated. P < 0.05 was considered as
statistically significant. Statistical analyses were con-
ducted using SAS Version 9.13 (SAS Institute Inc.,
Cary, NC, USA).
RESULTS
There were 27,001 live births from December 1,
2002 to May 31, 2005 in our study sites. We excluded
5149 births with congenital malformations, or miss-
ing birth weight, or gestational age values outside the
range of 20-44 weeks. After exclusion of 537 mul-
tiple births and low birth weight infants (< 2,500 g),
there were 21,315 live-born singletons 37 gesta-
tional weeks. In total, 21,315 maternal and neona-
tal records were analyzed. Among these newborns,
2,488 (11.67%) had macrosomia, and 417 (1.96%)
had a birth weight of 4500 g. The mean weight of
all newborns was 3,468419 g. The mean weight of
newborns in the macrosomia group and in the non-
macrosomia group was 4,207347 and 3,371318 g,
respectively.
Table 1 shows maternal and fetal characteris-
tics between the macrosomia and control groups.
The mean maternal age of the macrosomia group
was 24.743.32 years, which was older than that
in the control group (24.353.14 years, P = 0.000).
The mean maternal BMI at early pregnancy was
22.752.81 kg/m2, which was also higher than that
in the control group (21.762.59 kg/m
2
, P = 0.000).
About 62.5% of the macrosomic neonates were males,
compared with 51.0% in the control group (P = 0.000).
There was no statistical difference in maternal resi-
dence, maternal education, and smoking (or drinking)
during pregnancy.
By univariate logistic regression analyses, we found
that maternal age at delivery, first trimester maternal
BMI, and infant male gender were significantly associated
with the risk of neonate macrosomia (Table 2). There
was no statistically significant association between
macrosomia risk and other factors such as maternal
residence and maternal education. Multiple logistic
regression analyses showed that maternal age at de-
livery, first trimester maternal BMI and infant gender
were independent risk factors for macrosomia. Com-
pared with women with normal weight (BMI: 18.5-23.9
kg/m
2
), women who were overweight (BMI: 24-27.9
kg/m
2
) and obese (BMI 28 kg/m
2
), respectively, had
a 1.69-fold (95%CI: 1.51-1.88) and a 1.49-fold (95%CI:
1.31-1.69) risk of delivering a neonatal macrosomia.
Compared with female newborns, male newborns had a
1.61-fold (95%CI: 1.47-1.75) risk of being macrosomic.
In the nested case-control analysis by 2010, the
mean weight for boys in the macrosomia group
was 25.473.68 kg and in the control group was
24.633.87 kg. The difference between the two
groups was statistically significant (P = 0.000). Simi-
larly, the mean weight of the girls in the macrosomia
group was heavier than that in the control group
(24.433.61 kg versus 23.483.56 kg, P = 0.000).
*
for Student's t-test;
**
for Chi-squared test. BMI: body mass index.
Table 1 Maternal and fetal characteristics in the control group and the macrosomia group
Maternal characteristics
Maternal age at delivery
Maternal BMI at early pregnancy (kg/m
2
)
Infant gender
Male
Female
Maternal residence
Urban area
Rural area
Maternal education
Elementary school or less
Junior school
High school or above
Smoking during pregnancy
No
Yes
Drinking during pregnancy
No
Yes
Macrosomia (n=2488)
24.743.32
22.752.81
1,556(64.64%)
0,928(37.36%)
,0505(20.30%)
1,983(79.70%)
0,334(13.45%)
1,309(52.72%)
,0840(33.83%)
2,473(99.40%)
,015(0.60%)
2,426(98.14%)
,046(1.86%)
Control (n=18827)
24.353.14
21.762.59
09,575(51.00%)
09,198(49.00%)
03,631(19.29%)
15,196(80.71%)
02,571(13.69%)
09,992(53.20%)
06,219(33.11%)
18,664(99.22%)
,0150(0.78%)
18,337(98.48%)
0,284(1.52%)
P
0.000
**
0.000
**
0.000
**
0.231
**
0.768
**
0.772
**
0.202
**
238
Gu S et al. / Journal of Biomedical Research, 2012, 26(4): 235-240
The mean BMI of boys and girls in the macrosomia
group was higher than in the non-macrosomia group
(boys, 17.312.43 kg/m
2
vs 16.872.34 kg/m
2
, P =
0.000; girls, 16.772.04 kg/m
2
vs 16.302.12 kg/m
2
, P =
0.000). Compared with the non-macrosomia group,
macrosomic infant had a 1.52-fold (P = 0.001) and
1.50-fold (P = 0.000) risk, respectively, to develop-
ing overweight or obesity at the age of 7 years. After
stratification by gender, we found that male macro-
somia had a 1.53-fold and a 1.49-fold risk of devel-
oping overweight and obesity at the age of 7 years,
respectively. The risk of developing overweight and
obesity in female macrosomia was significantly higher
than that in the female unaffected group (OR=1.45;
95%CI: 1.06-1.99).
DISCUSSION
The present study has confirmed that the birth of
macrosomic neonates was related to certain maternal
and fetal characteristics in Chinese population. The
results that the risk for macrosomia increases with
maternal BMI at early pregnancy, maternal age and
male gender are compatible with the findings of other
investigators. Recent studies have suggested that high
pre-pregnancy BMI was the most important predic-
tor of delivering an infant with macrosomia
[14-18]
. The
magnitude of effect of maternal BMI on the risk of
macrosomia in non-diabetic pregnancies varies con-
BMI: body mass index.
Table 2 Univariate logistic regression analysis for the association of macrosomia
Maternal and fetal characteristics
Maternal age at delivery
Maternal BMI at early pregnancy (kg/m
2
)
< 18.5
18.5-23.9
24-27.9
> 28
Infant gender
Male
Female
Maternal residence
Urban area
Rural area
Maternal education
Elementary school or less
Junior school
High school or above
Smoking during pregnancy
No
Yes
Drinking during pregnancy
No
Yes
Macrosomia (n=2,488)
24.743.32
,080(3.22%)
1,519(61.05%)
,0540(21.70%)
0,349(14.03%)
1,556(64.64%)
,0928(37.36%)
,0505(20.30%)
1,983(79.70%)
,0334(13.45%)
1,309(52.72%)
,0840(33.83%)
2,473(99.40%)
,015(0.60%)
2,426(98.14%)
,046(1.86%)
Control (n=18,827)
24.353.14
1,388(7.37%)
12,830(68.15%)
02,631(13.97%)
01,978(10.51%)
09,575(51.00%)
09,198(49.00%)
03,631(19.29%)
15,196(80.71%)
02,571(13.69%)
09,992(53.20%)
06,219(33.11%)
18,664(99.22%)
,0150(0.78%)
18,337(98.48%)
,0284(1.52%)
OR(95%CI)
1.04(1.02-1.05)
0.49(0.39-0.61)
Ref
1.73(1.56-1.93)
1.49(1.31-1.69)
Ref
0.62(0.57-0.68)
Ref
0.94(0.85-1.04)
Ref
1.01(0.89-1.15)
1.04(0.91-1.19)
Ref
0.84(0.25-2.77)
Ref
1.23(0.89-1.68)
P
0.000
0.000
-
0.000
0.000
-
0.000
-
0.231
-
0.898
0.909
-
0.772
-
0.202
BMI: body mass index.
Table 3 Long-term health consequences of macrosomia for children at the age of 7 years
BMI
Normal
Overweight
Obesity
Normal
Overweight
Obesity
Normal
Overweight
Obesity
Macrosomia (n=700)
259(60.66%)
099(23.19%)
069(16.15%)
183(67.03%)
058(21.24%)
032(11.73%)
442(63.14%)
157(22.43%)
101(14.43%)
Control (n=5137)
1,838(69.99%),,
,459(17.52%)
,328(12.49%)
1,873(74.56%),,
,408(16.24%)
231(9.20%),
3,711(72.24%),,
,867(16.88%)
,559(10.88%)
OR (95%CI)
-
1.53(1.19-1.97)
1.49(1.14-1.99)
-
1.45(1.06-1.99)
1.42(0.95-2.11)
-
1.52(1.24-1.86)
1.50(1.19-1.92)
P
-
0.001
0.007
-
0.019
0.087
-
0.001
< 0.001
Male
Female
Total
Risk factors and long-term health consequences of macrosomia
239
siderably between different studies and has been re-
ported to range from 1.4- to 18-fold. Our result on
maternal BMI at early pregnancy is consistent with
these reports. We also found that mothers deliver-
ing macrosomic infants were significantly older (P =
0.000). This finding agrees with most domestic and
foreign scholars' reports
[10,19-21]
. However, Adesina
et al.
[22]
in Ibadan, Nigeria, did not find any signifi-
cant difference in maternal age. There was a male
predominance (64.6%) in our study group. This was
also reported by Wollschlaeger
[19]
from Germany and
Tomic
[23]
from Bosnia.
Furthermore, we found that macrosomic infants had
an increased predisposition to develop overweight and
obesity. Compared with the non-macrosomia group,
macrosomic infant had a 1.52-fold (P = 0.001) and
1.50-fold (P = 0.000) risk, respectively, of develop-
ing overweight or obesity at the age of 7 years. This
is also illustrated by the data indicating that exposure
to a diabetic state in utero, apparently independent of
genetic factors, increases the risk of obesity and dia-
betes in the next generation
[24-26]
. Catalano pointed out
that a vicious cycle may be established with profound
consequences for the health of future generations
[27]
.
Our study has important significance. The popula-
tion is a large sample of 21,315 mother-child pairs,
and the children were prospectively followed and
assessed for obesity 7 years after birth. On the other
hand, this study also has some limitations. Our sur-
veillance data did not record gestational age based on
ultrasound dating. Gestational age based on the first
date of last menstrual period has errors, particularly
among preterm and post term births
[28]
. In addition,
pre-pregnancy BMI and weight gain during pregnan-
cy were not recorded routinely in this study. We used
maternal height and weight during the first trimester
to calculate early pregnancy BMI, which was affected
by both gestational weight gain and pre-pregnancy
BMI. Finally, although reduction of maternal smok-
ing during pregnancy is an important factor for mac-
rosomia increase in developed countries
[14,17,29,30]
, we
did not find statistically significant association be-
tween smoking in pregnancy and macrosomia. The
prevalence of smoking in pregnancy in our population
was too low (0.77%; 165 out of 21,315 women) to
analyze its relationship with the occurrence of mac-
rosomia.
In conclusion, older maternal age, higher maternal
BMI at early pregnancy and male gender are independ-
ent risk factors of macrosomia. Macrosomic infants
show an increased predisposition to develop overweight
or obesity at the beginning of their childhood.
Acknowledgements
We sincerely appreciated the assistance with data
collection provided by the family planning service
professionals, data managers and other staff of the
95 surveillance spots, and the Jiangsu Population and
Family Planning Committee.
References
[1] Savona-Ventura C, Chircop M. Determinant for macro-
somia in a Mediterranean island community. Int J Diabet
Metab 2004; 12: 44-8.
[2] Savona-Ventura C, Chircop M. Birth weight influence on
the subsequent development of gestational diabetes mel-
litus. Acta Diabetologica 2003; 40: 101-4.
[3] Gardosi J, Mongelli M, Mul T. Intrauterine growth re-
tardation; in Steegers EAP, Eskes TKAB, Symonds EM
(eds): Preventive care in obstetrics and gynaecology.
Baillieres Clin Obstet Gynaecol 1995; 9: 445-643.
[4] Gardosi J. New definition of small for gestational age
based on fetal growth potential. Horm Res 2006; 65(S3):
15-8.
[5] Wen SW, Goldenberg RL, Cutter GR, Hoffman HJ,
Cliver SP, Davis RO, et al. Smoking, maternal age, fe-
tal growth, and gestational age at delivery. Am J Obstet
Gynecol 1990; 162: 53-8.
[6] Ananth CV, Wen SW. Trends in fetal growth among sin-
gleton gestations in the United States and Canada, 1985
through 1998. Semin Perinatol 2002; 26: 260-7.
[7] Schack-Nielsen L, Mlgaard C, Srensen TI, Greisen
G, Michaelsen KF. Secular change in size at birth from
1973 to 2003: national data from Denmark. Obesity
(Silver Spring) 2006; 14: 1257-63.
[8] Lahmann PH, Wills RA, Coory M. Trends in birth size
and macrosomia in Queensland, Australia, from 1988 to
2005. Paediatr Perinat Epidemiol 2009; 23: 533-41.
[9] Center for Health Statistics and Information, MOH. An
analysis report of national health services survey in
China. Chinese Peking Union Medical College Press (In
Chinese) 2008: 88.
[10] Bao C, Zhou Y, Jiang L, Sun C, Wang F, Xia W, et al.
Reasons for the increasing incidence of macrosomia in
Harbin, China. BJOG 2011; 118: 93-8.
[11] Zhu L, Qin X, Qian S. Macrosomia and associated risk
factors in Shanghai. Chin J Birth Heredity (In Chinese)
2001; 9: 81-3.
[12] Schwarz R, Teramo KA. What is the significance of
macrosomia? Diabetes Care 1999; 22: 1201-5.
[13] Group of China Obisity Task Force. Body mass index
reference norm for screening overweight and obesity in
Chinese children and adolescents. Chin J Epidemiol (In
Chinese) 2004; 25: 97-102.
[14] Surkan PJ, Hsieh CC, Johansson AL, Dickman PW, Cn-
attingius S. Reasons for Increasing Trends in Large for
Gestational Age Births. Obstet Gynecol 2004; 104: 720-6.
240
Gu S et al. / Journal of Biomedical Research, 2012, 26(4): 235-240
[15] Neggers Y, Goldenberg RL, Cliver SP, Hoffman MA &
Cutter GR.The relationship between maternal and neo-
natal anthropometric measurements in term newborns.
Obstet Gynecol 1995; 85: 192-6.
[16] Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M,
Beard RW, et al. Maternal and prepregnancy outcome:
a study of 287 213 pregnancies in London. Int J Obes
Relat Metab Disord 2001; 25: 1175-82.
[17] Bergman RL, Richter R, Bergman KE, Plagemann A,
Brauer M & Dudenhausen JW. Secular trends in neo-
natal macrosomia in Berlin: influences of potential
determinants. Paediatr Perinat Epidemiol 2003; 17:
244-9.
[18] rskau J, Henriksen TB, Kesmodel U, Secher NJ. Ma-
ternal characteristics of lifestyle factors and risk of de-
livering high birth weight infants. Obstet Gynecol 2003;
102: 115-20.
[19] Wollschlaeger K, Nieder J, Kppe I, Hartlein K. A study
of fetal macrosomia. Arch Gynecol Obstet 1999; 263: 51-5.
[20] Kamanu CL, Onwere S, Chigbu B, Aluka C, Okoro O,
Obasi M. Fetal macrosomia in African women: A study
of 249 cases. Arch Gynecol Obstet 2009; 279: 857-61.
[21] Akin Y, Comert S, Turanc C, Picak A, Agzikuru T, Te-
latar B. Macrosomic newborns:A 3-year review. Turk J
Pediatr 2010; 52: 378-82.
[22] Adesina AO, Olayemi O. Fetal macrosomia at the Uni-
versity College Hospital, Ibadan:A 3-year review. J Ob-
stet Gynecol 2003; 23: 30-3.
[23] Tomic V, Bosnjak K, Petrov B, Dikic M, Knezevic D.
Macrosomic births at Mostar Clinical Hospital: a 2-year
review. Bosn J Basc Med Sci 2007; 7: 271-4.
[24] Dabelea D, Hanson RL, Lindsay RS, Pettitt DJ, Impraa-
tore G, Gabir MM, et al. Intrauterine exposure to diabe-
tes conveys risks for type 2 diabetes and obesity. Dia-
betes 2000; 49: 2208-11.
[25] Dabelea D, Pettitt DJ. Intrauterine diabetic environment
confers risks for type 2 diabetes mellitus and obesity in
the offspring, in addition to genetic susceptibility. JPEM
2001; 14: 1085-91.
[26] Waterland RA, Garza C. Potential mechanisms of meta-
bolic imprinting thatleads to chronic disease. Am J Clin
Nutr 1999; 69(2): 179-97.
[27] Catalano PM. Obesity and pregnancy - the propagation
of a vicious cycle. JCEM 2003; 88: 3505-6.
[28] Kramer MS, McLean FH, Boyd ME, Usher RH. The va-
lidity of gestational age estimation by menstrual dating
in term, preterm, and postterm gestations. JAMA 1988;
260: 3306-8.
[29] Michael KS, Isabelle M, Yang Hong, Platt RW, Rob-
ert U, Helen MN, et al. Why are babies getting bigger?
Temporal trends in fetal growth and its determinants. J
Pediatr 2002; 141: 538-42.
[30] rskou J, Henriksen TB, Kesmodel U, Secher NJ. Ma-
ternal characteristics and lifestyle factors and the risk
of delivering high birth weight infants. Obstet Gynecol
2003; 102: 115-20.
Das könnte Ihnen auch gefallen
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsVon EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNoch keine Bewertungen
- Secular Trends of Macrosomia in Southeast China, 1994-2005: Researcharticle Open AccessDokument9 SeitenSecular Trends of Macrosomia in Southeast China, 1994-2005: Researcharticle Open AccesskymalogaNoch keine Bewertungen
- 6 UN Reddy EtalDokument6 Seiten6 UN Reddy EtaleditorijmrhsNoch keine Bewertungen
- InformaciónDokument6 SeitenInformaciónVIOLETA JACKELINE ARMAS CHAVEZNoch keine Bewertungen
- Association Between Gestational Diabetes Mellitus.46Dokument7 SeitenAssociation Between Gestational Diabetes Mellitus.46Frank MacíasNoch keine Bewertungen
- 08 AimukhametovaDokument10 Seiten08 AimukhametovahendraNoch keine Bewertungen
- Jog 12115Dokument7 SeitenJog 12115niko4eyesNoch keine Bewertungen
- DownloadDokument6 SeitenDownloadKai GgNoch keine Bewertungen
- Effects of prepregnancy dietary patterns on infant birth weight a prospective cohort studyDokument11 SeitenEffects of prepregnancy dietary patterns on infant birth weight a prospective cohort studyLola SantiaNoch keine Bewertungen
- Maternal and Fetal Outcomes of Obese Pregnant Women: A Prospective Cohort StudyDokument5 SeitenMaternal and Fetal Outcomes of Obese Pregnant Women: A Prospective Cohort StudyCostin VrabieNoch keine Bewertungen
- ArticleDokument8 SeitenArticleAstrid Abrahams PakelNoch keine Bewertungen
- Diabetic MaternlaDokument4 SeitenDiabetic MaternlaAde Gustina SiahaanNoch keine Bewertungen
- Pregnancy Exercise Overweight MetaanalysisDokument11 SeitenPregnancy Exercise Overweight MetaanalysisAisleenHNoch keine Bewertungen
- McKay Et Al PAFs Complete Cases PDFDokument10 SeitenMcKay Et Al PAFs Complete Cases PDFAnonymous oAoEj7pzNoch keine Bewertungen
- Maternal and Perinatal Maternal and Perinatal Outcome of Maternal Obesity Outcome of Maternal Obesity at RSCM in 2014-2019 at RSCM in 2014-2019Dokument1 SeiteMaternal and Perinatal Maternal and Perinatal Outcome of Maternal Obesity Outcome of Maternal Obesity at RSCM in 2014-2019 at RSCM in 2014-2019heidi leeNoch keine Bewertungen
- Andres, 2015Dokument7 SeitenAndres, 2015Daniela Patricia Alvarez AravenaNoch keine Bewertungen
- Research ArticleDokument11 SeitenResearch ArticlemalyaNoch keine Bewertungen
- Metgud Factors Affecting Birth Weight of A Newborn - A Community Based Study in Rural Karnataka, IndiaDokument4 SeitenMetgud Factors Affecting Birth Weight of A Newborn - A Community Based Study in Rural Karnataka, IndiajanetNoch keine Bewertungen
- Risk Factors and Outcomes of Fetal Macrosomia in A Tertiary Centre in Tanzania: A Case-Control StudyDokument8 SeitenRisk Factors and Outcomes of Fetal Macrosomia in A Tertiary Centre in Tanzania: A Case-Control StudyMarianella Saravia LopezNoch keine Bewertungen
- Ehrenberg2009 PDFDokument5 SeitenEhrenberg2009 PDFAhmad TriadiNoch keine Bewertungen
- Breast vs. Bottle: Differences in The Growth of Croatian InfantsDokument9 SeitenBreast vs. Bottle: Differences in The Growth of Croatian InfantsBernadette Grace RetubadoNoch keine Bewertungen
- Jurnal Internasional Nuzulia Rahmah 1Dokument10 SeitenJurnal Internasional Nuzulia Rahmah 1nzlNoch keine Bewertungen
- Protocol - PaedsDokument3 SeitenProtocol - PaedsShradha PrakashNoch keine Bewertungen
- Labor and Delivery Experiences of Mothers with Suspected Large BabiesDokument5 SeitenLabor and Delivery Experiences of Mothers with Suspected Large BabiesAlleyan Hannah DenumNoch keine Bewertungen
- D'Souza-2019-Maternal Body Mass Index and PregDokument17 SeitenD'Souza-2019-Maternal Body Mass Index and PregMARIATUL QIFTIYAHNoch keine Bewertungen
- The Effect of Obesity On Pregnancy and Its Outcome in The Population of Oman, Seeb ProvinceDokument12 SeitenThe Effect of Obesity On Pregnancy and Its Outcome in The Population of Oman, Seeb ProvinceHazley ZeeNoch keine Bewertungen
- Predictive factors for preeclampsiaDokument5 SeitenPredictive factors for preeclampsiaTiti Afrida SariNoch keine Bewertungen
- Being Macrosomic at Birth Is An Independent Predictor of Overweight in Children: Results From The IDEFICS StudyDokument9 SeitenBeing Macrosomic at Birth Is An Independent Predictor of Overweight in Children: Results From The IDEFICS StudySayuri BenitesNoch keine Bewertungen
- Article in Press: Effects of Central Obesity On Maternal Complications in Korean Women of Reproductive AgeDokument8 SeitenArticle in Press: Effects of Central Obesity On Maternal Complications in Korean Women of Reproductive AgeMhmmd FasyaNoch keine Bewertungen
- ResearchDokument20 SeitenResearchtedypsNoch keine Bewertungen
- The Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaDokument8 SeitenThe Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaAndres GallegosNoch keine Bewertungen
- Hubungan Makrosomia Dengan Kejadian Obesitas Pada Anak Yang Lahir Di Rsud Margono Soekardjo Purwokerto Periode Januari - Desember 2010Dokument9 SeitenHubungan Makrosomia Dengan Kejadian Obesitas Pada Anak Yang Lahir Di Rsud Margono Soekardjo Purwokerto Periode Januari - Desember 2010iraNoch keine Bewertungen
- 5625 21893 2 PBDokument8 Seiten5625 21893 2 PBIndah 15Noch keine Bewertungen
- Body Mass Index at Age 18 - 20 and Later Risk of Spontaneous Abortion in The Health Examinees Study (HEXA)Dokument8 SeitenBody Mass Index at Age 18 - 20 and Later Risk of Spontaneous Abortion in The Health Examinees Study (HEXA)Faradiba NoviandiniNoch keine Bewertungen
- Muest RaDokument13 SeitenMuest RaBruno LinoNoch keine Bewertungen
- 521 2345 1 PB Converted 1Dokument14 Seiten521 2345 1 PB Converted 1prabuNoch keine Bewertungen
- Nutrients 09 00221 v2Dokument11 SeitenNutrients 09 00221 v2Firman FajriNoch keine Bewertungen
- Fibroid TumorsDokument5 SeitenFibroid TumorscacingpandoraNoch keine Bewertungen
- Early Life Risk Factors For ObesityDokument13 SeitenEarly Life Risk Factors For Obesitybarragan-prosisaNoch keine Bewertungen
- Obesidad y EmbarazoDokument5 SeitenObesidad y EmbarazolandabureNoch keine Bewertungen
- Fetal Macrosomia : Its Maternal and Neonatal ComplicationsDokument6 SeitenFetal Macrosomia : Its Maternal and Neonatal ComplicationsTheresia Herestuwito NaruNoch keine Bewertungen
- Influence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenDokument5 SeitenInfluence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenIvana YunitaNoch keine Bewertungen
- Influence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenDokument5 SeitenInfluence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenAnonymous h0DxuJTNoch keine Bewertungen
- Elderly PrimigravidaDokument7 SeitenElderly PrimigravidaAnonymous mvNUtwidNoch keine Bewertungen
- Makrosomia and Childhood ObesityDokument11 SeitenMakrosomia and Childhood ObesityRiki SubagjaNoch keine Bewertungen
- Periodontal Disease and Adverse Pregnancy OutcomeDokument3 SeitenPeriodontal Disease and Adverse Pregnancy OutcomeWilliam JensenNoch keine Bewertungen
- Nursing Research PaperDokument24 SeitenNursing Research Paperapi-455624162Noch keine Bewertungen
- Proforma Synopsis For Registration of SubjectDokument15 SeitenProforma Synopsis For Registration of SubjectTamilArasiNoch keine Bewertungen
- Jurnal 05Dokument5 SeitenJurnal 05Jojo McalisterNoch keine Bewertungen
- Woobaidal 2016Dokument19 SeitenWoobaidal 2016Visa LaserNoch keine Bewertungen
- Sciencedirect: Sara Dokuhaki, Maryam Heidary, Marzieh AkbarzadehDokument8 SeitenSciencedirect: Sara Dokuhaki, Maryam Heidary, Marzieh AkbarzadehRatrika SariNoch keine Bewertungen
- Obesity and PregnancyDokument6 SeitenObesity and PregnancyBudiarto BaskoroNoch keine Bewertungen
- Maternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyDokument7 SeitenMaternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyKhuriyatun NadhifahNoch keine Bewertungen
- Early Prediction of Preterm Birth For Singleton, Twin, and Triplet PregnanciesDokument6 SeitenEarly Prediction of Preterm Birth For Singleton, Twin, and Triplet PregnanciesNi Wayan Ana PsNoch keine Bewertungen
- (2023) - Relationship Between Diet Quality and Maternal Stool Microbiota in The MUMS Australian Pregnancy CohortDokument12 Seiten(2023) - Relationship Between Diet Quality and Maternal Stool Microbiota in The MUMS Australian Pregnancy CohortVisa LaserNoch keine Bewertungen
- 9 PDFDokument9 Seiten9 PDFAnggun SetiawatiNoch keine Bewertungen
- Jurnal ViolenceDokument6 SeitenJurnal ViolenceIris BerlianNoch keine Bewertungen
- Babies Born To Obese Mothers: What Are The Characteristics and Outcomes?Dokument8 SeitenBabies Born To Obese Mothers: What Are The Characteristics and Outcomes?IJPHSNoch keine Bewertungen
- 2.jurnal Kepkel4Dokument7 Seiten2.jurnal Kepkel4Himatul AliyahNoch keine Bewertungen
- Risk Factors for Macrosomia and Labor OutcomesDokument8 SeitenRisk Factors for Macrosomia and Labor OutcomesKhuriyatun NadhifahNoch keine Bewertungen
- DM TyroidDokument10 SeitenDM TyroidKhuriyatun NadhifahNoch keine Bewertungen
- Effect of Glimepiride Compared With Glibenclamide On Post Prandial Blood Sugar in Type II Diabetes Mellitus PatientsDokument4 SeitenEffect of Glimepiride Compared With Glibenclamide On Post Prandial Blood Sugar in Type II Diabetes Mellitus PatientsKhuriyatun NadhifahNoch keine Bewertungen
- Dasar Dasar Interpretasi Ekg Radityo Prakoso Hary S MuliawanDokument69 SeitenDasar Dasar Interpretasi Ekg Radityo Prakoso Hary S MuliawanAndi Rizki AyuNoch keine Bewertungen
- Diabetes and MacrosomiaDokument35 SeitenDiabetes and MacrosomiaKhuriyatun NadhifahNoch keine Bewertungen
- J. Pediatr. Psychol. 2013 Maas Van Schaaijk 30 40Dokument11 SeitenJ. Pediatr. Psychol. 2013 Maas Van Schaaijk 30 40Khuriyatun NadhifahNoch keine Bewertungen
- Adverse Maternal Outcomes Associated With Fetal Macrosomia: What Are The Risk Factors Beyond Birthweight?Dokument6 SeitenAdverse Maternal Outcomes Associated With Fetal Macrosomia: What Are The Risk Factors Beyond Birthweight?Khuriyatun NadhifahNoch keine Bewertungen
- Maternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyDokument7 SeitenMaternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyKhuriyatun NadhifahNoch keine Bewertungen
- Risk factors macrosomia study acknowledgement addedDokument1 SeiteRisk factors macrosomia study acknowledgement addedKhuriyatun NadhifahNoch keine Bewertungen
- Risk factors for macrosomia in Latina womenDokument7 SeitenRisk factors for macrosomia in Latina womenKhuriyatun NadhifahNoch keine Bewertungen
- Risk factors for fetal macrosomia: positive oral glucose challenge testDokument7 SeitenRisk factors for fetal macrosomia: positive oral glucose challenge testKhuriyatun NadhifahNoch keine Bewertungen
- Adverse Maternal Outcomes Associated With Fetal Macrosomia: What Are The Risk Factors Beyond Birthweight?Dokument6 SeitenAdverse Maternal Outcomes Associated With Fetal Macrosomia: What Are The Risk Factors Beyond Birthweight?Khuriyatun NadhifahNoch keine Bewertungen
- Risk factors for fetal macrosomia: positive oral glucose challenge testDokument7 SeitenRisk factors for fetal macrosomia: positive oral glucose challenge testKhuriyatun NadhifahNoch keine Bewertungen
- J. Pediatr. Psychol. 2013 Maas Van Schaaijk 30 40Dokument11 SeitenJ. Pediatr. Psychol. 2013 Maas Van Schaaijk 30 40Khuriyatun NadhifahNoch keine Bewertungen
- 21 Corr Study of EndothelialDokument2 Seiten21 Corr Study of EndothelialKhuriyatun NadhifahNoch keine Bewertungen
- J. Pediatr. Psychol. 2013 Maas Van Schaaijk 30 40Dokument11 SeitenJ. Pediatr. Psychol. 2013 Maas Van Schaaijk 30 40Khuriyatun NadhifahNoch keine Bewertungen
- 21 Corr Study of EndothelialDokument2 Seiten21 Corr Study of EndothelialKhuriyatun NadhifahNoch keine Bewertungen
- Risk Factors for Macrosomia and Labor OutcomesDokument8 SeitenRisk Factors for Macrosomia and Labor OutcomesKhuriyatun NadhifahNoch keine Bewertungen
- Adverse Maternal Outcomes Associated With Fetal Macrosomia: What Are The Risk Factors Beyond Birthweight?Dokument6 SeitenAdverse Maternal Outcomes Associated With Fetal Macrosomia: What Are The Risk Factors Beyond Birthweight?Khuriyatun NadhifahNoch keine Bewertungen
- Risk factors for fetal macrosomia: positive oral glucose challenge testDokument7 SeitenRisk factors for fetal macrosomia: positive oral glucose challenge testKhuriyatun NadhifahNoch keine Bewertungen
- Maternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyDokument7 SeitenMaternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyKhuriyatun NadhifahNoch keine Bewertungen
- Risk factors for macrosomia in Latina womenDokument7 SeitenRisk factors for macrosomia in Latina womenKhuriyatun NadhifahNoch keine Bewertungen
- The Basic Philosophical and Theological Notions of Saint Augustine - John C. Cooper PDFDokument21 SeitenThe Basic Philosophical and Theological Notions of Saint Augustine - John C. Cooper PDFjusrmyrNoch keine Bewertungen
- Credit Suisse AI ResearchDokument38 SeitenCredit Suisse AI ResearchGianca DevinaNoch keine Bewertungen
- Configure Initial ISAM Network SettingsDokument4 SeitenConfigure Initial ISAM Network SettingsnelusabieNoch keine Bewertungen
- Public Policy For Nigerian EnviromentDokument11 SeitenPublic Policy For Nigerian EnviromentAbishai Auta GaiyaNoch keine Bewertungen
- Court of Appeals: DecisionDokument11 SeitenCourt of Appeals: DecisionBrian del MundoNoch keine Bewertungen
- 1 Minute Witness PDFDokument8 Seiten1 Minute Witness PDFMark Aldwin LopezNoch keine Bewertungen
- Causes of WWI: Alliances, Militarism & AssassinationDokument4 SeitenCauses of WWI: Alliances, Militarism & AssassinationJoshua De Leon TuasonNoch keine Bewertungen
- Recommender Systems Research GuideDokument28 SeitenRecommender Systems Research GuideSube Singh InsanNoch keine Bewertungen
- BiblicalDokument413 SeitenBiblicalMichael DiazNoch keine Bewertungen
- Entrepreneurship - Quarter 2 - Week 1-3 - 4 M's of Production and - Business ModelDokument6 SeitenEntrepreneurship - Quarter 2 - Week 1-3 - 4 M's of Production and - Business ModelJude Del RosarioNoch keine Bewertungen
- The Ramayana and The Sacred Palm Trees of Sumeria, Mesopotamia, Assyria and PhoeniciaDokument7 SeitenThe Ramayana and The Sacred Palm Trees of Sumeria, Mesopotamia, Assyria and PhoeniciaNeeta RainaNoch keine Bewertungen
- Intern - Annapolis PharmaceuticalsDokument34 SeitenIntern - Annapolis Pharmaceuticalsjoycecruz095Noch keine Bewertungen
- Final Project On Employee EngagementDokument48 SeitenFinal Project On Employee Engagementanuja_solanki8903100% (1)
- Molly C. Dwyer Clerk of CourtDokument3 SeitenMolly C. Dwyer Clerk of CourtL. A. PatersonNoch keine Bewertungen
- Young Man Seeks Book to Contact Girl He MetDokument1 SeiteYoung Man Seeks Book to Contact Girl He MetJessie WattsNoch keine Bewertungen
- Q3 Week 7 Day 2Dokument23 SeitenQ3 Week 7 Day 2Ran MarNoch keine Bewertungen
- StoreFront 3.11Dokument162 SeitenStoreFront 3.11AnonimovNoch keine Bewertungen
- 04 - JTC Template On Project ProposalDokument10 Seiten04 - JTC Template On Project Proposalbakelm alqamisNoch keine Bewertungen
- Basics of OncologyDokument64 SeitenBasics of OncologyCiubotaru Diana -MariaNoch keine Bewertungen
- CSEC English SBA GuideDokument5 SeitenCSEC English SBA GuideElijah Kevy DavidNoch keine Bewertungen
- APEC ArchitectDokument6 SeitenAPEC Architectsarah joy CastromayorNoch keine Bewertungen
- Ecomix RevolutionDokument4 SeitenEcomix RevolutionkrissNoch keine Bewertungen
- AdmitCard 1688037Dokument1 SeiteAdmitCard 1688037P.Supreeth ReddyNoch keine Bewertungen
- Introduction To Opengl/Glsl and WebglDokument46 SeitenIntroduction To Opengl/Glsl and Webglanon_828313787Noch keine Bewertungen
- 40 Energising BreathsDokument1 Seite40 Energising BreathsOwlbearNoch keine Bewertungen
- PCC ConfigDokument345 SeitenPCC ConfigVamsi SuriNoch keine Bewertungen
- Final Portfolio Cover LetterDokument2 SeitenFinal Portfolio Cover Letterapi-321017157Noch keine Bewertungen
- Eng10 LPQ3_4 Coherence and CohesionDokument2 SeitenEng10 LPQ3_4 Coherence and CohesionNiña RasonableNoch keine Bewertungen
- Marcos & Sumulong Highway, Rizal Applicant'S Information Sheet (Non-Academic)Dokument2 SeitenMarcos & Sumulong Highway, Rizal Applicant'S Information Sheet (Non-Academic)dummy testerNoch keine Bewertungen
- Condicional Perfecto Continuo interrogativo guíaDokument2 SeitenCondicional Perfecto Continuo interrogativo guíaMaxi RamirezNoch keine Bewertungen
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindVon EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindBewertung: 4.5 von 5 Sternen4.5/5 (1)
- Meat Is for Pussies: A How-To Guide for Dudes Who Want to Get Fit, Kick Ass, and Take NamesVon EverandMeat Is for Pussies: A How-To Guide for Dudes Who Want to Get Fit, Kick Ass, and Take NamesBewertung: 3.5 von 5 Sternen3.5/5 (8)
- Chakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.Von EverandChakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.Bewertung: 4 von 5 Sternen4/5 (2)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisVon EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisBewertung: 3 von 5 Sternen3/5 (2)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeVon EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeBewertung: 4.5 von 5 Sternen4.5/5 (110)
- What No One Tells You: A Guide to Your Emotions from Pregnancy to MotherhoodVon EverandWhat No One Tells You: A Guide to Your Emotions from Pregnancy to MotherhoodBewertung: 4.5 von 5 Sternen4.5/5 (30)
- How Bad Do You Want It?: Mastering the Pshchology of Mind over MuscleVon EverandHow Bad Do You Want It?: Mastering the Pshchology of Mind over MuscleBewertung: 4.5 von 5 Sternen4.5/5 (127)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingVon EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingBewertung: 4.5 von 5 Sternen4.5/5 (66)
- The Yogi Code: Seven Universal Laws of Infinite SuccessVon EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessBewertung: 4.5 von 5 Sternen4.5/5 (104)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerVon EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerBewertung: 4 von 5 Sternen4/5 (5)
- Brain Body Diet: 40 Days to a Lean, Calm, Energized, and Happy SelfVon EverandBrain Body Diet: 40 Days to a Lean, Calm, Energized, and Happy SelfBewertung: 5 von 5 Sternen5/5 (2)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesVon EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesNoch keine Bewertungen
- The Menopause Manifesto: Own Your Health With Facts and FeminismVon EverandThe Menopause Manifesto: Own Your Health With Facts and FeminismBewertung: 4 von 5 Sternen4/5 (18)
- Relentless: From Good to Great to UnstoppableVon EverandRelentless: From Good to Great to UnstoppableBewertung: 5 von 5 Sternen5/5 (779)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsVon EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsBewertung: 5 von 5 Sternen5/5 (95)
- All in Her Head: The Truth and Lies Early Medicine Taught Us About Women’s Bodies and Why It Matters TodayVon EverandAll in Her Head: The Truth and Lies Early Medicine Taught Us About Women’s Bodies and Why It Matters TodayBewertung: 5 von 5 Sternen5/5 (2)
- ADHD Women: A Holistic Approach To ADHD ManagementVon EverandADHD Women: A Holistic Approach To ADHD ManagementBewertung: 5 von 5 Sternen5/5 (4)
- What to Expect When You’re Expecting (5th Edition)Von EverandWhat to Expect When You’re Expecting (5th Edition)Bewertung: 5 von 5 Sternen5/5 (1)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!Von EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Bewertung: 4.5 von 5 Sternen4.5/5 (22)
- Perimenopause Power: Navigating your hormones on the journey to menopauseVon EverandPerimenopause Power: Navigating your hormones on the journey to menopauseBewertung: 4 von 5 Sternen4/5 (2)
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouVon EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouNoch keine Bewertungen
- A Radical Guide for Women with ADHD: Embrace Neurodiversity, Live Boldly, and Break Through BarriersVon EverandA Radical Guide for Women with ADHD: Embrace Neurodiversity, Live Boldly, and Break Through BarriersBewertung: 4.5 von 5 Sternen4.5/5 (71)
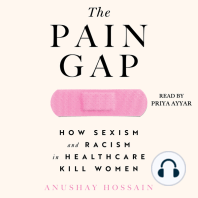
- The Pain Gap: How Sexism and Racism in Healthcare Kill WomenVon EverandThe Pain Gap: How Sexism and Racism in Healthcare Kill WomenBewertung: 4 von 5 Sternen4/5 (153)
- Younger Next Year, 2nd Edition: Live Strong, Fit, Sexy, and Smart-Until You're 80 and BeyondVon EverandYounger Next Year, 2nd Edition: Live Strong, Fit, Sexy, and Smart-Until You're 80 and BeyondBewertung: 4 von 5 Sternen4/5 (110)
- I'll Start Again Monday: Break the Cycle of Unhealthy Eating Habits with Lasting Spiritual SatisfactionVon EverandI'll Start Again Monday: Break the Cycle of Unhealthy Eating Habits with Lasting Spiritual SatisfactionBewertung: 4.5 von 5 Sternen4.5/5 (123)
- If You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsVon EverandIf You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsBewertung: 4.5 von 5 Sternen4.5/5 (7)
- Calisthenics: 12 Effective Exercises to Build Calisthenics Body in 14 DaysVon EverandCalisthenics: 12 Effective Exercises to Build Calisthenics Body in 14 DaysBewertung: 3 von 5 Sternen3/5 (5)
- The Strength and Conditioning Bible: How to Train Like an AthleteVon EverandThe Strength and Conditioning Bible: How to Train Like an AthleteNoch keine Bewertungen
- Sacred Womb Healing Meditation Divine feminine alignment: heal ancestral traumas deep wounds, release blocked sexual energies, flow to creativity, overcome the energies of birthing, joy love happyVon EverandSacred Womb Healing Meditation Divine feminine alignment: heal ancestral traumas deep wounds, release blocked sexual energies, flow to creativity, overcome the energies of birthing, joy love happyBewertung: 5 von 5 Sternen5/5 (1)