Beruflich Dokumente
Kultur Dokumente
Guidance On TB Patient Care For The Urban Poor (The RJPI Experience) 2014
Hochgeladen von
RITJATAPhOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Guidance On TB Patient Care For The Urban Poor (The RJPI Experience) 2014
Hochgeladen von
RITJATAPhCopyright:
Verfügbare Formate
1
Guidance on Tuberculosis
Patient Care for the Urban Poor
The RJPI Experience
2014
Research Institute of Tuberculosis
Japan Anti Tuberculosis Association Philippines,
Inc. (RJPI)
2nd Floor PTSI Bldg., 1853 Tayuman, St. Sta. Cruz,
Manila
2
Table of Contents
Acknowledgement 6
Acronyms 7
Background 8
Purpose of the Operational Guidelines 9
Target Audience 10
Diagram of RJPI Process of Private and Public Engagement and Collaboration 10
The Map of the Republic of the Philippines 11
The Map of District 1, Tondo, Manila 12
The Map of Payatas, Quezon, City 13
A. Planning and Preparation 14
1. Coordination / Consultative Meeting 14
2. Situational Assessment 15
B. Implementation 19
Strategy 1. Engagement of NGOs and other private organizations 20
Strategy 2. Capacity Building 21
a. Improving the supply side 21
b. Improving the Demand Side 24
Strategy 3. Advocacy, Communication, and Social Mobilization 24
a. Establishment of Referral Mechanism 25
b. Development of Recording Forms 26
c. Community Advocacy Campaign 28
3
d. Organize TB Support Group
29
e. Development of IEC Materials 30
C. Conducting Operations Research 30
D. Evaluation 32
1. Conducting on site Joint Monitoring and Evaluation 33
2. Program Evaluation 36
E. Scaling up Private and Public Mix Engagement and Collaboration 38
ANNEXES
Annex 1. Baseline Survey : Data Collection Form For Local Government Unit Health Centers 39
Annex 2. Baseline Survey : Data Collection Form For Non Government Organizations 43
Annex 3. A Sample Project Design Matrix 49
Annex 4. A Sample of Plan of Operations 51
Annex 5. Memorandum Of Agreement ( NGO DOTS Facility ) 56
Annex 6. Memorandum of Agreement ( NGO Referring Facility) 60
Annex 7. Assessment Sheet for Imaging Quality of Chest Radiography 64
Annex 8. CHV TB Symptomatic Referral Masterlist 65
Annex 9. NTP TB Symptomatic Referral Form 71
Annex 10. Modified Masterlist B 74
Annex 11. Contact Investigation Tool for Community Health Volunteers 78
Annex 12. MDR Suspect Referral Masterlist 80
Annex 13. MDR-TB Decentralized Masterlist 82
Annex 14. TB/ HIV Masterlist 84
4
Annex 15. A Sample Project Indicators
89
Annex 16. Monitoring Tools 94
a. Laboratory Case Finding Tool 97
b. Laboratory Checklist 98
c. Laboratory Feed Back Sheet 99
d. Validation Sheet for IPT 100
e. Validation Sheet for Child Screened 101
f. Validation Sheet for IPT Outcome 102
g. Quarterly Report on All TB Cases 103
h. TB Cases Treatment Outcome 106
i. Contact Investigation ( Modified Masterlist B ) 107
j. Validation Sheet on TB Diagnostic Committee 111
k. MDR TB Suspects Data Collection Form 112
l. TB Infection Control Monitoring Tool 113
m. Logistics Monitoring Form 114
n. Data Validation 115
o. Health Worker Interview ( DOTS facility ) 118
p. Patient Interview 120
q. NTP Monitoring Tool for Referring Facilities: Data Collection Form 121
r. NTP Monitoring Tool : Feedback Sheet
123
124
5
Developed by the Research Institute of Tuberculosis / Japan Tuberculosis Association,
Philippines, Inc. (RJPI)
Authors:
Akihiro Ohkado, RIT/JATA Philippines Inc., (RJPI) Manila, Philippines; Research Institute of
Tuberculosis (RIT) / Japan Anti Tuberculosis Association (JATA), Tokyo, Japan
Aurora Querri, RIT/JATA Philippines Inc., (RJPI) Manila, Philippines
Shoji Yoshimatsu, Research Institute of Tuberculosis (RIT) / Japan
Anti Tuberculosis Association (JATA), Tokyo, Japan
Leveriza Coprada, RIT/JATA Philippines Inc., (RJPI) Manila, Philippines
Evanisa Lopez, RIT/JATA Philippines Inc., (RJPI) Manila, Philippines
Gian Patrick Pili, RIT/JATA Philippines Inc., (RJPI) Manila, Philippines
Yuka Inoue, RIT/JATA Philippines Inc., (RJPI) Manila, Philippines
Akira Shimouchi, Research Institute of Tuberculosis (RIT) / Japan Anti Tuberculosis
Association (JATA), Tokyo, Japan
Funded by:
TB Control and Prevention Project in Socio-Economically Unprivileged Areas in Metro
Manila, The Philippines under the technical cooperation for grassroots projects of Japan
International Cooperation Agency (JICA), Japan:
The research project of the International Medical Center of Japan (IMCJ), A socio-medical
study for facilitating effective infectious diseases control in Asia funded by the International
Medical Cooperation Research Grant, the Ministry of Health, Labour and Welfare, Japan; and
the double barred cross seal donation of Japan Anti-Tuberculosis Association (JATA), Japan.
Citation: http://bit.ly/RJPIUrbanPoorGuidance
Contact information:
Akihiro Ohkado
Aurora Querri
Research Institute of Tuberculosis / Japan Anti Tuberculosis Association, Philippines, Inc.
(RJPI)
1853 Tayuman, St. Sta. Cruz, Manila, Metro Manila, the Philippines
Telephone Number: 02-740-8054
REFERENCES
6
Acknowledgement
We appreciate the significant contributions of the following organizations in enriching the RJPI
experience for the TB in the Urban Poor.
This Guidance on Tuberculosis Patient Care for the Urban Poor - The Research Institute for the
Tuberculosis Association Experience will not be put into writing without their collaborative
effort.
National Tuberculosis Control Program
Center for Health Development Metro Manila
Manila Health Department
Quezon City Health Department
Partner Organizations the Non-Government Organizations working within the project site
Other Partner Organizations
7
ACSM Advocacy Communication and Social Mobilization
CBO Community Based Organization
CHD-
MM
Center for Health Development- Metro Manila
CHV Community Health Volunteer
DOTS Directly Observed Treatment Short Course
FBO Faith Based Organization
FDS Free Discussion Session
HIV Human Immunodeficiency Virus
IEC Information Education Communication
IPT Isoniazid Preventive Therapy
JICA Japan International Cooperation Agency
LGU Local Government Unit
NGO Non Government Unit
NTP National Tuberculosis Control Program
NTRL National Tuberculosis Reference Laboratory
MDR-TB Multi Drug Resistant Tuberculosis
MHD Manila Health Department
MOA Memorandum of Agreement
OR Operational Research
PDM Project Design Matrix
PhilPACT Philippine Plan of Action to Control Tuberculosis
PLHIV People Living with HIV
PoOs Plan of Operations
QCHD Quezon City Health Department
RJPI Research Institute of Tuberculosis / Japan Anti Tuberculosis Association,
Philippines, Inc.
SLH San Lazaro Hospital
STI Sexually Transmitted Infection
TB Tuberculosis
TBCAP Tuberculosis Coalition Assessment Program
TBCTA Tuberculosis Coalition for Technical Assistance
TBIC Tuberculosis Infection Control
WHO World Health Organization
ACRONYMS
8
I. Background
Tuberculosis (TB) remains to be the global major public health problem for the past several
decades. The problem of TB is still predominant in the Philippines and its control is a
continuing concern of the National Tuberculosis Control Program (NTP). The Philippine Plan
of Action to Control TB (Phil PACT) was developed to systematically assess the TB burden and
TB control efforts in the Philippines in 2010. Likewise it is intended to serve as a road map in
reducing TB to a level where it is no longer a public health threat in the country (1). In the study
conducted by Tupasi et al., on the TB in the urban poor settlements in the Philippines, it was
noted that the prevalence of TB was 2.7 times in the urban than the general population (2). The
poor and vulnerable have longer pathway to health care than other social groups (3, 4). Studies
from a number of developing countries reveal that the poor have much less access to TB care
services than the nonpoor or can be excluded from TB care (5, 6 and 7). Emp, et al., observed
that TB services should also focus on the geographically poor areas such as slums or to specific
population group such as the homeless and the migrants who are likewise considered TB
vulnerable groups (8). In the study conducted by Murthy, et al., it concluded that engaging the
service providers used by the poor is substantial in reducing barriers to TB care (9).
The Research Institute of Tuberculosis / Japan Anti-Tuberculosis Association Philippines Inc,
(RJPI) was established in 2008, which aims to improve the access of the community people to
quality DOTS implementation through strengthening the linkage among the local government
units (LGUs) and non-governmental organizations (NGOs) in District I Tondo, Manila and
Payatas, Quezon City in Metro Manila, Philippines. The project as guided by the NTP and
Center for Health DevelopmentMetro Manila (CHD-MM) with the cooperation of the LGUs
and NGO partners identified the urban marginalized sector in District I-Tondo, Manila and
Barangay Payatas, in Quezon City as the strategic site of intervention. The RJPI has been
providing technical assistance since the first phase of the project through the Japan Ministry of
Foreign Affairs and now on its second phase through the grassroots project of Japan
International Cooperation Agency (JICA). The projects purpose of the RJPI is for the TB
infection and prevention and treatment to be implemented upon maintained quality DOTS
(Directly Observed Treatment, Short Course) program. For this purpose, the RJPI has been
conducting five kinds of activities in addition to assisting organizations concerned to maintain
quality DOTS program:
9
1. To strengthen Advocacy, Communication Social Mobilization (ACSM) about TB
and its treatment among community; the activities underneath this component
comprises of capacity building, encouraging partners and the community to
participate in advocacy campaigns, network and linkage with government and
NGOs and organization of TB support groups.
2. To assist governmental organizations (GOs) and NGOs to provide TB screening
(contact investigation for contacts) in the project areas; the project conducts
monitoring and evaluation and facilitated development of relevant recording
forms.
3. To support treatment failure and other retreatment TB patients to take anti-TB drug
susceptibility test (DST); the project ensures the multi-drug resistant TB (MDR
TB) suspect referred by the DOTS Facility was able to access the treatment center.
A DOTS Facility is a facility that provides TB care, management, treatment to
patients including diagnostics and serves as referring unit for MDR suspects. A
Treatment Center provides complete care, management, diagnostics and
treatment of MDR-TB patients.
4. To assist / support to provide TB screening among HIV positive patients at HIV
hospital (San Lazaro Hospital, Manila); the RJPI together with TB and HIV
experts from San Lazaro Hospital (SLH) facilitated the development of an
operational guideline for HIV infected TB patient care at the hospital and a
recording form was developed.
5. To assist / support to implement TB Infection Control (TBIC) at the health
facilities in the project area. The project oversees the TBIC health practices of
health staff through monitoring and evaluation visits.
II. Purpose of the Operational Guidelines
The purpose of the operational guidelines is to provide guidance to NGOs, Community Based
Organizations (CBOs) and NTP in implementing communitybased TB prevention,
management, care and support in urban poor settings. It describes activities for effective
collaboration among NTP, NGOs and CBOs. It is aligned with the Stop TB Partnership (10),
ENGAGE TB Approach (11) and PhilPACT Strategies (1) for engaging all health care
providers including NGOs as part of the public and private mix approach.
10
A. PLANNING AND
PREPARATION
Coordination / Consultative Meeting
Situational Assesment
B. IMPLEMENTATION
Engaging GOs , NGOs, and other
partners
Improving the supply side
Improving the demand side
C. CONDUCTING
OPERATIONAL
RESEARCH
D. EVALUATION
Joint Monitoring and Evaluation
Visits
Program Evaluation
Project Indicators
E. SCALING UP PRIVATE
AND PUBLIC MIX
ENGAGEMENT AND
COLLABORATION
III. Target Audience
This document is for the NGOs and other CBOs providing health care services that intend to
integrate community-based activities for TB prevention, management, care and support of
patients. The NTP is also an important audience of this document to assess and provide
recommendations and amendments to improve TB care in the community.
All community members in the community including women urban poor, youth, children,
elderly and family affected by TB could utilize this guide to generate demand for TB service.
IV. RJPI Process of Private and Public Mix Engagement and Collaboration
The diagram shown above represents the RJPI Collaboration Process in establishing and
strengthening linkage mainly between the GOs and NGOs. This is composed of five phases.
The first step is Planning and Coordination (consultative/conceptualization of the project),
followed by Implementation (actual execution of the activities based on the project design),
conducting operational research (documenting the current situation vis-a-vis resources and
absorptive capacity of the health staff to identify strategic interventions for the enhancement of
service delivery), then evaluation (regular assessment of the development of the project with
particular focus on its effectiveness and impact), and finally Scaling up of relevant organization
partnership (the success of a certain model or project introduced is replicated in other sites). The
Stop TB Partnership Six Point Agenda forges to engage all health care providers both the public
and private organizations to bring TB care services closer to the community (1). This process
could be adopted by private organizations which are willing to contribute to the NTP
11
The Map of the Philippines (12)
12
The Map of Project Sites
The project sites are in District-I, Tondo, Manila and Payatas, Quezon City. The project period
is from 2008-2014. The title of the project is TB Control and Prevention Project in Socio-
economically Unprivileged Areas in Metro Manila, the Philippines. Its focus is reaching the
underprivileged people in the community by bridging the gap through the networks among the
NGOs, CBOs and LGU in support of the NTP to improve the access to the quality DOTS
implementation.
1. Tondo Medical Center
2. Gat Andres Bonifacio Memorial Medical Center
3. Juan Posadas Health Center
4. Vitas Health Center
5. Canossa Health and Social Center Foundation Inc.
6. Velasquez Health Center
7. Aurora Quezon Health Center
8. Dagupan Health Center
9. Sto. Nino de Tondo Medical and Indigency Center
10. Bo. Fugoso Health Center
11. Parola Health Center
12. Tondo Foreshore Health Center
13. Bo. Magsaysay Health Center
14. Smokey Mountain Health Center
15. Youth With A Mission
16. Philippine Christian Foundation
17. Couples for Christ- Gawad Kalinga
18. San Pablo Apostol Clinic
19. Center for Community Transformation -Pritil
20. Encourage Families in Need and Care for Education
21. Center for Community Transformation -Parola
22. 4 People
23. Education Research Development Assistance-
Samahan ng Batang Nananambakan
24. Aspiring Citizen for Community Empowerment
25. Caritas
District-I Tondo, Manila
13
1. Lupang Pangako Health Center 4. Payatas Orione Foundation
2. St. Luigi Orione 5. Payatas A Health Center
3. Committee of German Doctors 6. Center for Community Transformation - Payatas
4. Payatas B Health Center
Payatas, Quezon City
14
A) PLANNING AND PREPARATION
The initial step in the RJPI process of engagement and collaboration is planning and preparation
of the project. The involvement of the NTP, CHD-MM including the City Health Offices is
significant in providing directions on how we will implement the project. Thus coordination and
consultation should be conducted at each level.
1. Coordination / Consultative Meeting
Initially we will have to coordinate the focal persons on when we plan to seek an audience with
them through a consultative meeting. A consultative meeting provides a venue to seek for expert
opinion on project conceptualization, For the RJPI experience; we solicited the advice of the
NTP and CHD-MM. Their participation is vital in the whole aspect of project implementation
and yet crucial at its preparation stage. The involvement of NTP / CHD-MM is specified in the
following stages in project planning and preparation.
Stages in the Preparation of the Project
a. Identifying goals: Goals are necessary in the preparatory phase of the engagement and
collaboration process. This is a guide that will direct the organization into the success of
the project. Most of the time, respective organization based their project goal which ought
to contribute to the broader social objective. Ultimately, the positive effect or impact that
we desire to achieve for the beneficiaries of the project must be the focus of the activity.
The RJPI goal is that TB infection prevention / treatment model is implemented by
maintaining quality DOTS services which is in line with the PhilPACT plan in reducing TB
mortality and morbidity. This aimed to improve the access of the TB services in the
community.
b. Identifying the beneficiaries: After the goal has been set, the identification of the
beneficiaries follows under the guidance of the NTP and CHD-MM. The beneficiaries are
the recipients of the intended positive effect from the implementation of the project. For the
RJPI project, they are the elderly, children and family or community members living in the
marginalized community who are experiencing impediments in accessing TB services.
c. Selecting a project site: When the beneficiaries had been identified, the next stage will be
selecting the project site. The project site refers to where we could strategically provide the
interventions that we will determine during the stakeholders analysis meeting as
mentioned below. In selecting a project site, we have to consider the performance of the
health facilities based on NTP indicators, extent of TB services they provide and other
baseline data which will be discussed in detail under situational assessment. The NTP and
CHD-MM who manages the data will guide us on where we could intervene.
15
d. Coordination with the Government Institution / City Health Office: After seeking the
expert opinions of NTP and CHD-MM, the next step is to coordinate with the government
institutions and to lay down the project plan again, through a consultative meeting.
Soliciting the advice of the City Health Office through their NTP Coordinators will help us
in arriving at a decision on where we could strategically place our interventions since they
know the intricacies and peculiarities of their sites and each of the health facilities. The
RJPI usually pays a courtesy visit to the City Health Office as part of coordination to
introduce RJPI project, the intention of possible collaboration and when to seek audience
with then through a consultative meeting.
2. Situational Assessment
This is the second part under the planning and preparation stage in the RJPI process of
development and collaboration. On this stage the RJPI employs the situational assessment in
order to have an accurate finding of the present situation of the area. Situational assessment is a
process utilized to systematically collect and evaluate the socio-cultural, economic and
geographical and health system data of each organization aimed at identifying the current TB
services strategies opportunities, strengths and barriers in providing quality TB care service in
the community.
a. Baseline Assessment of Health Facilities in the Proposed Project Sites
We need to collect and analyze the situation in the possible areas for further discussion
with the staff concerned. A baseline survey to identify all NGOs and private clinics
(mapping of existing GOs and NGOs), the extent of TB care and management and health
services they offer to the community and to identify their needs in providing quality TB
services will be conducted. This is composed of socio-demographic profile (relates to the
development / structure of each organization and the population characteristics in a certain
community), health resources (refers to materials, personnel, facilities and funds that can
be used for providing health care and services), health staff capacity (refers to the ability of
the health staff to perform quality TB services based on the number of TB trainings
received), NTP performance (the assessment of the program implementation vis-a-vis the
indicators set by the NTP including current activities and barriers to TB care). See baseline
Data Collection forms for LGUs and NGOs (Annexes 1 and 2).
16
b. Stakeholders Analysis Meeting
A stakeholders analysis meeting happens as a follow through activity, after the baseline
survey has been conducted. The activity has six phases and it aims to solicit inputs with the
partner institutions such as central and local governments (e.g., NTP, CHD-MM, MHD
and Quezon City Health Department (QCHD) and NGOs specifically in analyzing the
baseline data, to identify barriers on TB care access encountered, possible solutions and
interventions / strategies in order to address those barriers identified. It is also on this phase
that the Project Design matrix (PDM) is created.
Phases of Stakeholders Analysis Meeting
Phase 1 (Baseline Data Analysis): The baseline data obtained during the situational
assessment such as NTP performance and demographics will be presented to stakeholders
for analysis. By reviewing and evaluating the NTP performance together with the
acceptable performance target, we could better understand how the program is working.
Phase 2 (Identification of strengths of the GOs and NGOs on TB services): This
identified strength will be a medium for the sustainability and development of the project.
Phase 3 (Identification of barriers to access in TB Care): The stakeholders will identify
the different problems that they have encountered. The identified barriers are necessary in
developing core interventions for the project.
Phase 4 (Identification of strategies to address the barriers to TB Care): These relate
to the result of needs assessment. The strategies or interventions determined by the
stakeholders should correspond to the needs identified. Given the situation above, the
following strategies were recommended by the stakeholders to address the gaps to TB care
access. The identified strength in the second phase will be useful in making solution to the
problem. A thorough study in the strategies that will be used in the problem solving should
be necessary in order to cater the health needs, problems, and concerns that may surface
during the project implementation.
Phase 5 (Formulation of Project Design Matrix (PDM): After the systematic approach
in the identification of the strategies that will address the barriers of the TB care, the
agreed interventions will be now converted into a log frame or PDM. We need to formulate
a PDM to guide us how we are going to manage and implement the project. Without the
17
major components plans and strategies explicitly written on this document, there will be
confusion in running the project, hence its success would be uncertain. A log frame or
PDM specifies the goal, purpose, activities, inputs, assumptions, indicators for monitoring
/evaluation of a project. In concert with the PDM, is the formulation of the Plan of
Operations (PoOs) which exemplify the details of the activities, time, period, budget and
person-in-charge to perform the specified tasks. (See Annex 3 and 4: PDM and PoOs).
Both the PDM and PoOs are the pillars in planning, implementing, monitoring and
evaluating the project activities.
Phase 6 (Tasking and formulation of Memorandum of Agreement (MOA)): This is
the final phase on this activity. The designed PDM will be the heart of the MOA. The
MOA will be the avenue for the implementation of the project by both parties. All the
stakeholders involved in this project such as CHD-MM, City Health Offices (MHD and
QCHD) and NGO DOTS and Referring facilities, identify their tasks or roles /
responsibilities to formulate a MOA (See Annex 5 and 6).
18
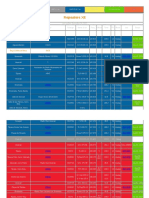
Example: Output of the Stakeholders Analysis conducted in 2008
RJPI Baseline Data Gathering
Location: District 1-Tondo, Manila and Payatas, Quezon City
Date: 2008
Particulars
District I-Tondo, Manila
Payatas, Quezon City
Socio-demographic profile
320,916 ( 47.5% Urban Poor )
128,736 (90% Urban
Poor )
Health Resources:
Shortage of NTP logistics such as TB medicine, reagents and other consumables
Lack of manpower and microscopy center
8 DOTS Referring Facilities to 12
3 Referring Facilities to 15
5 Microscopy Centers
3 DOTS Facilities to 6
1 Referring Facility
1 Microscopy Center to 6
NTP Performance 2007
New Smear Positive
Pulmonary TB ( NSP )
Case Notification Rate:
(CNR per 100,000
population)
127 ( 407/320916 ) 66 ( 85/128,736)
Cure Rate of NSP
76% ( 310/407 ) 74% ( 63/85)
Health Staff capacity :
NGO health staff and CHVs need training on NTP.
Issues / concerns/barriers:
Most of the NGO staff and CHVs need training, no referral system, no monitoring and
evaluation visits conducted and only some have network and linkage with the LGUs. This
part will be tackled comprehensively in the Stakeholders Analysis Meeting.
19
B) IMPLEMENTATION
This is the second step in the RJPI process of project development and collaboration. On this
step, the actual execution of the planned activities will be specified in the PDM. By this time,
the partner organizations have entered into a MOA. Implementation must be built with strong
commitment and camaraderie to be able to achieve the goal of the project. This stage is divided
into three strategies:
Stakeholders: Manila Health Department, Quezon City Health Department, NTP, CHD-MM,
RJPI
Output: The most common gap identified for the economic barriers are possibly lack of
transportation both by the patient and health staff, and unstable commitment by the health staff.
For the geographical barriers the gaps may be the distance of the health facility and frequent
relocation and demolition in the area. Accordingly, lack of knowledge on TB, stigma,
uncooperative patients and local authorities (e.g. barangay in the Philippines) maybe identified
by the health staff as socio-cultural barrier. For the health system barriers, lack of manpower,
untrained health staff and volunteers, lack of networking among the public and private sectors,
improper referral system, irregular monitoring, lack of equipment and the lack of health
volunteers as treatment partners are possibly identified by the health staff.
Needs: Training, referral system, logistics and regular monitoring and evaluation visits by
LGUs.
Strength: Health facilities in different capacities complement the health system i.e. The DOTS
facility, Referring Facilities, Community Health Volunteer, DOTS facilities
Strategies Identified: These relate to the result of needs assessment. The strategies or
interventions determined by the stakeholders should correspond to the needs identified. Given
the situation above, the following strategies were recommended by the stakeholders to address
the gaps to TB Care access: Capacity building, Network and linkage, ACSM activities and
conduct of operational researches.
20
Strategy 1. Engagement of NGOs and other private organizations: It is defined as a
commitment of mutual collaboration among the CHD-MM, City Health Offices (MHD/QCHD)
and partner organizations such as NGOs. The action of fulfilling the responsibilities, can
determine the success of the project. In this area, those NGOs identified during the mapping,
baseline data gathering and who expressed commitment to support the project are the ones
engaged. In engaging the NGOs / other private organizations, the steps below can be adopted:
Step 1 - Project Orientation. This is the initial step on NGO engagement. We need to
orient the other partner organizations to the project, its goal, objectives, the interventions as
well as the duties and responsibilities of each institution. The RJPI together with a
representative of MHD or QCHD visit the different identified NGO within the catchment
project site. The project is introduced to them together with the beneficial effects that it
intends to provide to the community. It is necessary for the RJPI to explain the duties and
responsibilities of the partner for the understanding and success of the project.
Step 2 Facility Capacity Review. The second step is to review the facilitys capacity in
providing TB care services. Again, the baseline data gathered during the situational
assessment will be utilized for this purpose. At this point, we will have to assess the facility
if they are suited as DOTS or Referring facility. The definition is described below:
NGO Referring Facility: refers to a nonprofit, voluntary citizens group which is
organized on a local, national or international level. The functions of this are (1) to find
presumptive TB in the community and refer them to a DOTS facility, (2) to conduct
contact investigation guided by the health worker staff, (3) to trace the interrupters or
defaulters of treatment, (4) to keep records or documents. To improve the case holding
activities, the CHVs sometimes take up the role as treatment partner and an educator to
motivate the TB patients to adhere with their treatment regimen until the end of the
treatment course.
NGO DOTS Facility: They function in the same way as the Local Government Unit
(LGU) DOTS centers do from case finding to case holding activities. NGO DOTS health
staff receives the same recording forms provided to the LGU DOTS such as MDR Suspect
Referral Masterlist, MDR Decentralized Masterlist, TB Symptomatic Masterlist, Modified
Masterlist B, etc.
21
Step 3 MOA signing. This defines the formal engagement of the NGOs as they affix
their signature and entered into a MOA with the CHD-MM, City Health Office and RJPI.
This signifies that they fully embrace the mission, tasks, interventions indicated on the
PDM and MOA. A sample MOA can be found on Annexes 5 and 6.
Strategy 2. Capacity Building: These are actions directed to improve knowledge, behaviours,
skills and techniques through training, sharing of information and transfer of knowledge among
each individual / partner organizations. The identified Health Care Workers (HCWs) and
Community Health Volunteers (CHVs) who need to be capacitated were trained in full
coordination with CHD-MM, MHD and QCHD to set a standard level in delivering quality TB
care in every health facilities. Consequently, it aims to strengthen and sustain the engagement of
each organization in implementing and scaling up communitybased TB activities. In capacity
building, there are two subjects that are in focus. The first one is supply side. These refers to the
health care provider, the person, institution or services it render to the community. The second
is the demand side which refers to the beneficiary of the health care delivery system, i.e., the
community members.
The following types of training were conducted both for the LGUs and NGOs in DOTS and
Referring Facilities:
a. Improving the Supply Side. This refers to the activity that would enhance the
competency or skills of health care workers and improve knowledge of CHVs to
provide quality DOTS services.
a.1 Improving the capacity of HCWs at DOTS Facility
Basic Directly Observed Treatment Short Course Chemotherapy Strategy
(DOTS) Training This is a four-day training to hone the knowledge, attitude and
skills needed by the doctors and nurses in providing quality TB Control Program
specifically in identifying presumptive TB, diagnosing and treating TB patients. It is
composed of lectures, group discussions/ presentations, workshops, role play and
plenary.
TB in Children Training This is a four-day training to enhance the skills and
knowledge of the doctors and nurses in identification, diagnosis and treatment of TB
in children. It is composed of lectures, group discussion, plenary and practical
examination on Tuberculin Skin Testing.
22
Basic Course on Direct Sputum Smear Microscopy (DSSM) for Medical
Technologist and Microscopist - This is a five-day training to improve the Medical
Technologists / Microscopists competence in performing sputum smear examinations
and additional knowledge on the NTP, laboratory technique on sputum smear
examination and quality assurance for sputum smear examination. It is composed of
lectures, discussions and practice exercises in proper smearing, staining and
microscopy reading.
Basic Training on DSSM for Laboratory Assistants This is a three-day training to
hone the skills of the laboratory assistants in the proper smearing and staining of
sputum specimen. It is composed of lectures and practise exercises in proper smearing
and staining of sputum specimen.
Chest Radiography Training
i. Training on Quality Chest Radiography Taking This is a four-day training to
improve radiologic technologists competence in performing accurate / standards in
chest radiography taking. It is composed of lectures and practice of the TBCAP
assessment tool (Annex 7) developed by Tuberculosis Coalition for Technical
Assistance (TBCTA) to ensure quality of chest radiography.
ii. Chest Radiography Appreciation Course This is a one and half day training
conducted among doctors and nurses to develop their skills in assessing the quality of a
good chest radiograph. It is composed of lectures and practice exercises by using the
TBCAP assessment tool (Annex 7) to ensure the quality chest radiography. After the
training, the doctors and nurses can now conduct prescreening on the quality chest
radiographs before referring those suggestive TB findings for Tuberculosis Diagnostic
Committees (TBDC) evaluation. Those identified with poor quality chest radiograph
will be requested to have another chest radiograph taken in another facility rather than
submitting to TBDC for evaluation knowing that it will be returned since the TBDC
could hardly interpret it due to its unacceptable quality. This will help in reducing
diagnosis delays as well as reading misinterpretations.
23
Training on HIV/TB
i. Training of Trainers This is a four-day training for TB coordinators, selected
doctors and nurses to equip them with knowledge and skills in imparting the basics of
STI, HIV AIDS education. It is composed of lecture and practical examination on
facilitation skills to become effective preceptors.
ii. Orientation to Health Care Workers (HCWs) This is a half-day or one day
orientation / for HCWs on the basics of STI, HIV and AIDS education for early
prevention and diagnosis of HIV and AIDS.
Training of Health Worker on Tuberculosis Infection Control (TBIC) This is a
two-day training for doctors, nurses and medical technologists to protect healthcare
workers since they are at risk of contracting TB infection. Likewise they are expected
to develop their TB Infection Control policy per health facility based on their TB
Infection Control Risk Assessment Plan. It is composed of lectures, demonstrations,
practical exercises, group discussion, work and site visit and evaluation of a TB
Facility.
Electronic TB Register (ETR) Training - This is a two to three days training of TB nurse to
enhance their skills and knowledge in the Standard Operating Guidelines of ETR, system
reporting, management of dispatch file, Internet and basic computer trouble shooting. It is
composed lectures and actual encoding of data.
a. 2 Improving capacity of CHVs in Referring Facility:
Orientation on Directly Observed Treatment (DOT) for Community Health
Volunteers - a one-half day orientation on DOT composed of lectures, role play
and group discussion which focuses on the following:
(1) Identifying TB presumptive (adult/ children)
(2) Patients drug intake supervision
(3) Contact Investigation
(4) Defaulter Tracing
(5) TB Infection Control practices
24
One of the important parts of this activity is the introduction of the referral
mechanism between the NGO Referring and DOTS Facilities. The steps on how
to identify/refer the TB symptomatic to the DOTS facilities and how to
accomplish the recording forms were tackled step by step. Please see Annexes 8.
The situation below illustrates the RJPI referral process:
The CHVs utilize two recording forms namely the CHV TB Symptomatic
Referral Masterlist (Annex 8) and NTP Referral Form (Annex9). The CHVs
accomplish half of the columns (1-11) of the said referral Masterlist, the process
of the TB symptomatic referral indicating the date when the patient is identified
as the TB symptomatic until he/she seeks consult. The remaining columns (12-
22) about the process from the diagnosis to treatment completion are updated by
the health staff every two weeks. The NTP Referral Form is utilized to refer TB
symptomatic to the DOTS facilities. The CHVs retrieved half of the
acknowledged referral form from the DOTS facility every week; however some
of the NGO referring facilities have agreements that they will retrieve the half of
the referral form after a month.
b. Improving Demand Side. In order to become successful in the implementation of the
project, we must create activities that will increase community TB awareness and
motivate them to participate in TB response. This is in turn would make them demand
for the needed services which is also beneficial to enhance TB Care policy. Thus, they
need to be empowered. This empowerment is discussed in strategy 3.
Strategy 3: Advocacy, Communication and Social Mobilization (ACSM). These are distinct
to one another but are used collectively to create more impact. This should capture the
policymakers, HCWs and the community to work hand in hand in support of NTP and its
related activities. The following are the activities conducted by the RJPI in the project sites to
improve case detection / treatment outcomes, reduce stigma / discrimination, empower the
community and mobilize political will / resources.
25
a. Establishment of Referral Mechanism
This is the process wherein a trained CHV oriented on Basic TB DOTS finds TB
symptomatic in the community and refer them to the nearest DOTS facility with proper
referral slip for diagnosis and treatment where appropriate. Once the trained CHV
identified TB symptomatic in the community she / he will register the name and basic
information on the CHV TB Symptomatic Referral Masterlist (Annex 8), and
afterwards shall accomplish the NTP Referral form (Annex 9) and hand it over to the
TB symptomatic. The purpose of the CHV TB Symptomatic Referral Masterlist is to
account the referrals done by the CHVs to the DOTS facilities and to ensure that all
patients referred by the CHVs accessed in the DOTS facilities. This recording
Masterlist are used by the trained CHVs to list all the identified TB symptomatic in the
community. This contains information from the time the TB symptomatic was
identified, assessed for TB, diagnosed as TB, initiated TB treatment including the
outcome. This is accomplished by CHVs and some columns are accomplished by
HCWs to update the progress of each TB symptomatic listed on this recording form.
The updating of this record is every two weeks. Sometimes the CHVs accompany the
patient in going to the DOTS facility for diagnosis. The CHVs will make a follow up
visit to the patient who did not access in the DOTS facility. Through the CHV
Masterlist and NTP referral forms we could document the contribution of the CHVs to
the NTP and the process of the referral mechanism itself.
The purpose of the NTP Referral form is to keep track of the care received by the
Patient of the actions taken by the health staff. Correspondingly, it works to review the
flow of the referral system. Consequently, this form should be accomplished
completely and accurately. It has two parts:
i. For the first part or the upper portion, it contains the basic details of the TB
symptomatic referred to the DOTS facilities such as the time of referral,
current signs / symptoms, previous treatment and the name of the referring unit
and CHVs.
ii. The second part or the lower portion, it is the actions taken by the receiving
DOTS facility. The CHVs retrieve the lower portion of this form from the
DOTS facility every two weeks to account the numbers of TB symptomatic
who were able to access the DOTS facility.
26
b. Development of Recording Forms and Enhancement of the NTP Monitoring Tool:
Development of Recording Forms: This refers to creating a tool to document the
current activities in the DOTS and referring facilities. This is necessary in data sage
guarding and accuracy of reports. The RJPI developed the CHV TB symptomatic
Referral Masterlist (Annex 8) and other recording forms in order to provide updates
and report to the NTP and Partner Organizations.
Enhancement of NTP Monitoring Tool: This refers to the incorporation of other
indicators specific to the project but pertinent to the NTP for the improvement of
existing tool and the program itself. The RJPI incorporated the following to the
existing NTP monitoring tool: (1) NTP Referring facility which covers from the time
TB symptomatic was identified, diagnose, treated including the treatment outcome;
(2) Contact investigation which focuses on all age groups, TB diagnosis yield /
treatment outcome; (3) MDR-TB which covers the referral of DOTS treatment center,
diagnosis and treatment; (4) TB Infection Control which focuses on the health
practice of health staff based on the National TBIC guidelines; and (5) Exit interview
for health staff / patients which covers how DOT is implemented on both perceptions
and how it can be improved. The side effects experienced by the patients are also
included in this activity.
Modified Masterlist B: The purpose of this is to identify and register all
household contacts of index TB cases (first one to contact TB in the household) for
early case detection and prompt initiation of treatment to reduce further transmission
of infection to others. Again, this should be accomplished completely and accurately
for ease of following up patients. This is an enhanced tool from the existing Masterlist
B of NTP which contains the information of index TB cases and their contacts which
covers all age groups, i.e., children and adults. The NGOs have been conducting
contact investigation among contacts or household members of their registered TB
cases (index cases) for the past several years. The contact investigation included all
age groups of contacts of index case; however, it was not documented. Currently, this
will serve as a relevant reference to improve contact investigation strategies. The
contacts with or without symptoms, are listed on this form including their diagnosis
and progress of treatment. Those under surveillance can likewise be tracked on this
form. Please see Annex 10.
27
Contact Investigation Tool for CHVs: This was developed for the CHVs to note
the TB household contacts that they have encouraged to go to the DOTS facility for
TB screening and evaluation. This tool came up after the CHVs and the NGO heads
of referring facilities agreed to assist the DOTS index cases, the name / age / signs /
symptoms of the household contacts and the date of their actual house visit (Annex
11). By reviewing the Modified Masterlist B together with the Contact
Investigation Tool for CHVs we can evaluate the contact investigation process and
find ways to enhance it.
MDR TB Suspect Referral Masterlist: The purpose of which is to document the
process of MDR Symptomatic Referrals to treatment center for possible policy
changes in improving access, turn-around time in diagnostics and prompt initiation of
treatment. The development of this Masterlist was based on the expressed need of
partner organizations. The DOTS facilities depend on the acknowledgement slips
returned by the treatment centers to track the number of the MDR suspects who were
able to access the treatment center. Through the development of the MDR Suspect
Referral Masterlist, the DOTS Facilities were able to officially document, track and
analyze the pathway of the MDR suspects. This covers the basic information of
patient, the dates the MDR suspect was referred to the treatment center including the
diagnostics performed, the diagnosis and treatment outcome (Please see Annex 12).
MDR-TB Decentralized Masterlist: The purpose of this is to account the number
of MDR-TB patients referred by the treatment center to the DOTS facility for
continuation and compliance of treatment. This came out as a recommendation of the
partner organization and covers the basic information of confirmed MDR-TB patients
who were decentralized to DOTS facilities. MDR-TB patients can be decentralized if
culture result is negative and the preference of the said patients to continue treatment
in the DOTS facilities or treatment sites. Currently, MDR-TB patients decentralized
by the treatment center are listed on this Masterlist. This document helps the HCWs
track the treatment outcomes of MDR-TB patients. Please see Annex 13.
The MDR-TB Suspect Referral Masterlist and MDR-TB Decentralized
Masterlist are currently utilized not just in the project sites but in the whole city of
Manila and Quezon City. This indicates a positive impact for the project.
28
TB / HIV Masterlist: This was developed by the RJPI and TB/HIV experts from
SLH to enhance the referral mechanism between the two departments at SLH. The
TB HIV Masterlist covers the identification of TB symptomatic of People Living
with HIV (PLHIV), diagnostics and treatment outcomes. From 2012, the TB and HIV
centers of SLH were able to document the number of PLHIV who were referred to
TB Center, were recommended for Isoniazid Preventive Therapy (IPT) or TB
treatment and started / completed treatment. Consequently, all referrals from the TB
Center were acknowledged and managed by the HIV Center where they were
screened and managed accordingly. The referral and recording systems were
institutionalized which facilitated the documentation and data analysis at SLH. Please
see Annex 14.
c. Community advocacy campaign: The RJPI initiated the conduct of community
assembly in 2010 which focuses on TB disease, how it is transmitted, when and
where to seek consult, including infection control measures and the important role of
the community leaders and other organizations in reducing the number of TB cases
within their family and the community. The target participants were officers of
Tricycle Operators and Drivers Association (TODA) together with people from the
community. The purpose of which is to create TB awareness in the community and to
encourage other organizations to participate in the TB activities. The TODA officers
and members actively participated on the TB response by referring and education
their passengers on symptoms of TB and where to access services. In addition to this
activity, the RJPI always joins the global community in celebrating the lung month
every August and World TB Day during March.
a. Community Assembly: This refers to the gathering of individuals who reside in
the same particular setting in order to tackle issue and concern that affect them. The
RJPI employs this community activity to share knowledge about TB and to increase
the awareness and improve the health seeking behaviour of the people in the
community.
a.1 Health Education: It is another intervention in providing the community
knowledge about TB. This can be conducted by groups through pre-clinic lectures or
bench conference and on oneone basis. There are different teaching methods to
deliver this activity such as role play, lecture discussion and learning exercises.
Usually, IEC materials such as flip chart are utilized and brochures provide to
intended participants to support the ideas they learned during the session.
29
a.2 Lung Month Celebration: It is an annual activity which celebrated every August
of the year in the Philippines. This activity stimulates the community to take care of
their health and their lungs. The purpose of this activity is to raise the awareness in
the prevention and control of Tuberculosis.
a.3 World TB Day: celebrated on the 24
th
of March every year was created to build
public awareness that tuberculosis today remains an epidemic in much of the world,
causing the deaths of nearly one-and-a-half million people each year, mostly in
developing countries. The partner organizations, barangay officials are invited on this
event including TB patients and their families. The usual activities are: TB patients
testimony, gallery presentation of health facility services, contests related to
increasing TB awareness, when and where to seek consult. The theme used every
three years is patterned after the WHO theme i.e Stop TB in my Lifetime (2010-2013)
and Reach the Three Million, A TB test, treatment and cure of all .(2014-2017). This
is where we based the criteria for activities such as slogan-making contest, poem-
making contest, song writing contests, etc.
d. Organize TB Task Force: The task force is composed of CHVs who are active in the
TB response. The purpose of which is to improve CHV performance in conducting
TB activities in the community. There are two (2) CHV task forces in the project
sites: one (1) for District I- Tondo and one (1) for Payatas, Quezon City. A CHV task
force meeting is being conducted twice a year. The agenda for the said meeting are:
presentation of accomplishment of each referring facilities, sharing of community
experience, gaps /good practices identified and possible solutions offered by each
facilities or CHVs with relatively good accomplishments. The RJPI facilitates and
provides technical support during those meetings.
Organize TB Support Group: TB support group is composed of previous TB
patients who were successfully treated. The purpose of this is to improve the health
care seeking behaviour of people in the community and mobilize them to take action
for their health. The TB support group conducts weekly house to house visit, follows
up interrupters of treatment and sometimes act as treatment partners of TB patients.
Ideally, all health facilities must create a TB support group to assist them in TB
activities. The RJPI facilitates the creation of TB support groups among DOTS
Facilities. After the DOTS Facilities have selected the members of their support
group, the RJPI will help them conduct the initial meeting concerning about the basic
facts about TB disease, how it is transmitted, objectives of having a support group and
30
the roles that they have to play once they become a member of the TB support group.
After which, the election of officers and members will be conducted. From then, the
subsequent meetings (i.e. activity updates, sharing of experience, and presentation of
TB support Group contribution to NTP) will be spearheaded by the DOTS facilities
and the RJPI will attend to provide technical support.
e. Development of Information Education, Communication (IEC) materials to seek
early consult: IEC materials such as poster, tarpaulin, stickers and flyers and video
are developed to facilitate community members to seek early consultation. The
purpose of this is to inform the community that seeking early consult at the DOTS
facility is important to detect TB cases early and for treatment to be initiated promptly
to reduce TB transmission in the family and community. The IEC materials need to
be field tested to the community and revision to be made accordingly based on the
comments raised by the community members.
C) CONDUCTING OPERATIONAL RESEARCH (OR)
One of the six-point agenda for TB Control developed by WHO and Stop TB Strategy (2010-
2016) is to enable and promote research (1). The project sees this as a vital component in
improving access to TB Care services. It helps the HCWs analyze their current operations,
existing problems and concerns, problems in decision making, interventions and optimize the
use of their resources. The following are the ORs so far conducted by the RJPI:
Example: This IEC material on the timing
and where to seek consult was converted into
a poster, tarpaulin and sticker. The posters /
tarpaulins were strategically placed in health
facilities, barangay stations and in the
community while the tarpaulin were
distributed to TODA and placed at the back of
their tricycles and stickers are placed inside
the tricycle. The stickers and flyers were
handed to the participants after thorough
explanation of its content during community
assemblies.
31
1.) Effectiveness of a training course on the quality assurance of chest radiography in the
Philippines
Chest radiography is regarded as a secondary tool in diagnosing TB among smear negative
cases with chest x-ray (CXR) findings. Unsatisfactory quality of CXR for diagnosing smear
negative leads to over and under diagnosis, resulting to mismanagement and waste of resources.
The RJPI provided training on Quality Chest Radiograph to ten facilities in Manila and nine
in Quezon City from 2009 to 2010. The aim of the study was to determine the effectiveness of a
training course in a quality chest radiograph. The study was conducted in 2011 participated by
36 from the training. After obtaining consent, the RJPI collected six CXR films composed of
three males and females among the participants. These were assessed by two senior radiologic
technologists using the TBCTA Tool Assessment Sheet (Annex 5). The factors assessed were
Identification marking, patient position, density, contrast, sharpness and presence of artefacts.
The significant improvement in the total score of the six assessment factors suggests a positive
impact of the training course (12).
Impact: This study is currently being utilized by the Philippine Association of Radiologic
Technologist (PART) for their research on developing a model intervention to sustain the
quality of chest radiograph in pulmonary TB and other lung diseases nationwide. The NTP,
together with the Center for Device Regulation Radiation Health and Research and the PART
recommended this training module for staff development and the formulation of quality control
mechanisms to assess and monitor the competence of radiologic staff.
Please check http://www.ncbi.nlm.nih.gov/pubmed/22640452 for the complete details of this
research.
2.) Health care seeking behaviour of Pulmonary Tuberculosis Patients in Socio-
Economically Depressed areas in the Philippines
The delay in diagnosis can be hazardous both to TB patients and community members since it
leads to the progression of the disease and continuous spread of bacilli to others. This study
described the current health care seeking behaviour in terms of delay to TB diagnosis and care
in new smear positive pulmonary TB patients in highly urbanized depressed areas in District I-
Tondo, Manila and Payatas, Quezon City. All new smear positive patients aged 15 years old and
above registered at the twelve DOTS facilities in District I and six in Payatas, Quezon City from
April 2010 to March 2011 were included in the study. The physician and nurses interviewed the
new smear positive patients using a structured questionnaire. This study revealed a half month
delay on the part of the health system and health providers and a one month delay on the part of
32
the client in Tondo and Payatas. This highlighted the importance of a short turnaround time
between diagnosis and prompt initiation of treatment to prevent TB transmission (13).
Impact: The patient, diagnosis and treatment delays noted on the health-care seeking behaviour
research was able to provide important data on how the TB services can be tailored to the needs
of the community and health system be improved and strengthened.
3) Tuberculosis Diagnostic Committees contribution to the National TB Program in
Manila and Quezon City
The RJPI conducted this study in 2011 to determine the current TB activities, obstacles and
possible solutions for improvements in the quality of diagnosis of smear negative PTB patients
in Manila and Quezon City. A record review was conducted, with interviews of 33 out of the 49
current members. During the 2
nd
and 3
rd
quarters of 2009, respectively 1142 and 1563 smear
negative cases were evaluated by the TBDCs in both cities. Of these, 53% in Manila and 65% in
Quezon City were classified as active TB patients. There were significant variations in the
percentage recommended for anti-TB treatment by the TBDC. The participation of its members
is based on commitment for program sustainability (14).
Impact: The TBDC study was able to elucidate the important role of peer review mechanism in
diagnosing smear negative PTB and ensuring judicious use of resources.
Please check:
http://www.ingentaconnect.com/content/iuatld/pha/2012/00000002/00000003/art00012 for the
complete details of this research.
D) EVALUATION
Monitoring and Evaluation Visits (M & E visits)
A Monitoring and Evaluation visit is one of the keys to improve the provision of TB care
services in the community. This provides an opportunity for the Monitoring Team to oversee the
performance of HCWs. During the visit, we can observe how DOT is being done, review
records and reports, and conduct exit interview among patients to give the monitoring team a
better grasp on how TB program is being implemented. More importantly, this is a good venue
to reinforce the HCWs good performance and correct inadequacies. Through the regular on-site
M & E visits, major problems could at least be prevented before it arises. It is important that the
team is prepared and HCWs are informed on when / where / how the on-site M & E visit will be
33
conducted. Likewise, there must be tool to make this activity effective and efficient. Please see
the step by step procedure in conducting M & E visits below:
1) Conducting on-site joint Monitoring/ Evaluation (M&E) Visits
a. Composition / Tasks: Monitoring Team
City/District NTP Coordinator: Oversees the work of the Monitoring Team.
Records review is conducted by the following on:
District Supervisor: Case Finding All Cases;
RJPI staff-1: TBDC and observes the infection control health practices of
HCWs;
RJPI staff-2: Case Finding, Laboratory Activities, and Contact Investigation;
RJPI staff-3: TB in Children and MDR Referrals;
RJPI staff-4: NGO referrals, treatment outcomes, interview;
RJPI staff-5: logistics and data validation.
b. Frequency:
M & E visits shall be conducted regularly on quarterly basis for those health
facilities with good performance and those which were not able to achieve the
program target, on a monthly basis.
c. Indicators:
These are parameters which will help the team to monitor how well the program is
being implemented and evaluate its progress. Likewise, this will be our guide in
determining the frequency of our M & E visits. Below are examples of indicators
utilized by the RJPI to monitor its project implementation.
No. of TB Symptomatic identified No. of TB symptomatic referrals,
Completion of INH Preventive Therapy (IPT), Treatment Success Rate of
New Smear Positive with low defaulter rate, and No. of MDR Suspect
Referrals to treatment center. Guideline about TB screening and IPT for
PLHIV at San Lazaro Hospital (SLH) is developed. A summary description
of these indicators is found in Annex 15.
d. Planning / Preparation (for the Monitoring and Evaluation)
Responsible Persons: Technical Coordinator/ Technical Officer
34
d.1 Coordinate with City / District NTP Coordinators / Supervisors and NGO Heads
regarding the purpose; proposed site / date of M & E visit. Remember that this is a
joint M & E visit and the participation of the NTP Coordinators / NGO Heads is
vital to be able to solve immediate concerns and come up with a consensual
solution.
d.2 Write a letter of permission to the City Health Office for the on-site M & E. The
purpose, method, date, time and name of the health facility to be visited should be
stated clearly.
d.3 Remind the City / District NTP Coordinators / Supervisors at least one week
before the scheduled visit. This will help ensure that there will be a responsible
person who will respond to the inquiries of the monitoring team and all pertinent
records / reports needed are in place during the visit at the health facility.
d.4 Prepare all the materials needed for this activity such as:
d.4.1 Monitoring Tool (Please see Annex 16)
d.4.2 pencil, ballpen, ruler, calculator
d.4.3 Laptop for data encoding
d.4.4 Camera for documentation purposes
e. Actual M & E Visit
e.1 Conducts records review based on their assigned tasks and validates them with
the health facility responsible person for any data inconsistencies (Responsible
Persons: Monitoring Team).
e.2 Utilizes a tool in monitoring the health practices of Health Care Workers
(HCWs) on TB infection control. The TBIC tool was developed by RJPI in
consultation with the partner organizations based on the DOH guidelines. The tool
is divided into four (4) levels of infection control such as managerial,
administrative, environmental and respiratory controls. There are specific health
practices underneath each level. Observation and interview of HCWs are the
Case Finding: Laboratory
Activities
MDR Suspect Referrals
0-4 years old on IPT Infection Control
TB in Children Screened Logistics
IPT Outcome Data Validation Tool
Contact Investigation Monitoring Tool for Referring Facility
Case Finding: All TB Cases
Treatment Outcome
Monitoring Tool Feedback Sheet with
carbon paper
TBDC
35
methods used to evaluate the health practices of HCWs trained on TBIC. For every
ideal health practices performed, letter Y is indicated and letter N for not done.
The letter Y stands for yes and letter N for no. The ideal health practices
are then summarized per level of TBIC and per health facility. The HCWs are
expected to perform 50% of the ideal health practices per level of infection control.
There are five (5) ideal health practices under the managerial and administrative
levels. There are six (6) ideal health practices under environmental and four (4) for
respiratory controls (i.e. 3 ideal health practices out of five (5) were performed
under the managerial level 60%). After computing per level of IC and per health
facility, the health facilities are grouped into two (2)- ratings 1 and 2. A health
facility with rating 1 means that less than 50% of the health practices are performed
while rating 2 means 50% or more of those were performed or accomplished.
e.3 Conducts exit interview to patients/HCWs where appropriate (Responsible
Persons: Community Development Officer)
e.4 Provide Feedback to the HCWs. The findings together with the proposed
recommendations (conferred with the HCW concerned during the validation) are
presented to the HCWs. This is also a form of brainstorming to specifically discuss
the challenges encountered by the HCWs in their course of implementation.
Moreover, actions to address the challenges and ways of maintaining the good
performance are dealt at hand. The recognition of the HCWs collaborative efforts
in improving the quality of TB Care services can serve as a motivating factor to
them while pointing out the bottlenecks; make them more sensible in their actions.
The original copy of the feedback sheet signed by both the HCWs and the
monitoring team is provided to the HCWs while the carbon copy is left for the
team. The feedback sheet corresponds as reference for the next visit. With the
Integrated TB Information System (ITIS) in place, the monitoring team perceives
efficiency in generating reports and analysis of data. This could also facilitate
effective M & E visits (Responsible Persons: Assigned member of the Monitoring
Team).
36
2) Program Evaluation
This is an assessment of program performance of GOs and NGOs semi-annually or
annually. All stakeholders are invited including the NTP, CHD-MM, and sometimes the TB
patients. Each partner organization will have to present their accomplishment for the
specified period based on the NTP and project indicators. Apart from looking at statistics,
reviewing / analysing the data, it is also a good venue to share the experiences of each
organization and how they were able to address the challenges they encountered in the
course of implementation. The presence of NTP, CHD-MM and the City Health
representatives is significant in providing directions on how the project could further
improve. Consequently, regular activity such as this keeps the camaraderie and stewardship
of the stakeholders.
Example by RJPI:
Annual Program Evaluation Workshop - January 30, 2009
Attendees: All stakeholders, NTP, CHD-MM, MHD, QCHD, NGOs and WHO
Findings: GOs and NGOs presented their accomplishment and noted an
improvement in case finding / case holding activities, program implementation
improved through capacity building of staff / installing of microscopy center in
Payatas. The CHVs are active in finding TB symptomatic but their contributions
were not documented.
Recommendations: Develop a CHV TB Symptomatic Referral Masterlist and
referral form to document the accomplishment / contribution of CHVs
Annual Program Evaluation Workshop - February 22-24, 2010
Attendees: All stakeholders, NTP, CHD-MM, MHD, QCHD, NGOs, PTSI and a
TB Patient.
Findings: Need to improve turn-around time in DSSM from 3 days to 2 days
revise the CHV TB Symptomatic Masterlist/ TB Symptomatic Referral
Form.
Recommendation : Capacitate the CHVs as Laboratory Assistants to improve
DSSM turn-around time to reduce delay in diagnosis.
: CHV TB Symptomatic Masterlist shall include the TB diagnosis and
Treatment Outcome parts.
37
: CHV TB Symptomatic Referral Form shall include questions on
finding MDR suspects (i.e. previous intake of TB drugs), TB
symptomatic serial number for ease of monitoring and the specific
actions taken by the receiving DOTS facility.
Annual Program Evaluation - February 14- 16, 2011
Attendees: All stakeholders, NTP, CHD-MM, MHD, QCHD and NGOs
Findings: Decreased in the number of TB symptomatic referred by CHVs
There are no M & E tools to cover TB infection Control, MDR and
Contact investigation.
Recommendations : Conduct a FGD among CHVs to investigate possible reasons
of the decline of the referred.
: Develop a TB Infection Control Checklist based on National
Guidelines.
: Create Contact Investigation/ MDR M & E tool based on project
indicators
Annual Program Evaluation Workshop February 16-17, 2012
Attendees : All stakeholders, NTP, CHD-MM, MHD, QCHD and NGOs
Findings : NSP Success Rate not achieved for both project sites
High Defaulter/ Transferred out rates
Recommendations : Conduct a FGD among HCWs and orient them on IPCC
: Conduct program evaluation twice a year (semi-annual and
annually) to identify gaps/ solutions encountered for the past six
months and give HCWs more time to improve their performance
before the year ends.
Semi- Annual Evaluation : QCHD with NGOs -July 19-20, 2012
MHD with NGOs- August 29-31, 2013
Findings: No training on infection control conducted among HCWs
: No documentation on the number of MDR Suspects referred / access to
treatment center.
Recommendations : Train HCWs on Infection Control
: Develop MDR Suspect referral Masterlist
: Enhance Masterlist B, i.e., the adult contacts of a registered TB case
should be listed and progress of consultation should be tracked.
38
Annual Program evaluation Workshop January 30-31, 2013
Attendees: All stakeholders, NTP, CHD-MM, MHD, QCHD and NGOs
Findings : Improved turnaround time in DSSM from 5 days to 2 days
: Treatment Success rate did not achieve the program target due to high
defaulter and transferred out rates
Recommendations : Conduct IPCC among HCWs.
E) SCALING UP PRIVATE AND PUBLIC MIX ENGAGEMENT AND
COLLABORATION
This is the final step in the RJPI process of project development and collaboration. Once the
GO and NGO partnership is successful, it is ready on its take off to expand to other areas.
Expanding to other sites requires careful planning and evaluation of the model introduced. It
should be integrated with the overall objective for an effective expansion. Important persons
like our current partners who were part of this promising collaboration should be included
and not to be taken for granted. Sustaining the involvement of our current partner will be the
key in expanding; they will share their experience for effective planning and preparation for
the expansion. Lessons learned must be taken into consideration to enhance the program
implementation. Ownership must be instilled in the GOs and NGOs framework to keep the
sustainability of the activities.
The RJPI introduced the NGO referral mechanism and was able to accelerate service points
in the community. Seeing the contributions of these NGOs who mainstreamed TB services
in their program, the City Health Offices included in their sustainability plan to continue M
& E visits among the NGOs engaged by the project.
39
Annex 1: BASELINE SURVEY Data Collection Form for Local Government Unit Health
Centers
Name of Health Center (Facility):_____________________________________________________
Address:________________________________________________________________________
Telephone Nos. : ________________________ Fax No:_________________
Contact Person (Physician In Charge /Nurse): ________________ Mobile No.: _______________
Population coverage: __________________
No. of Barangays (Bgy) Covered: ______Depressed Bgy: _________Non-Depressed Bgy: ______
No. of Depressed Population: _________ No. of Non- Depressed Population: ________
No. of Health staff: ____________ (Pls. enumerate names below)
No. of Barangay Health Workers (BHWs): _________________ (Pls. enumerate names below)
No. of Community Health Team (CHT) volunteers: ___________
NO. NAME DESIGNATION TB Trainings/Orientation
1
2
3
4
5
6
7
8
9
10
11.
12.
13
14
15
40
QUESTIONNAIRE:
1. When was your health facility established? ________________________________
2. Do you have current partner NGOs or private health facility? ___ Yes ___ No
If yes, what kind of assistance or partnership you share in terms of health service network? _____________________
3. How many possible partner NGOs or private facility you have in your catchment population?
4. Is this a microscopy center? ___ Yes ___ No
If no, where do you send the sputum for examination? ____________________
Schedule of Sputum collection: ________________________
Schedule of Transport of Sputum Specimen or stained smear slides: _________
5. Do you conduct contact investigation? ___ Yes ___ No
If yes, do you utilize a Masterlist for this? ___ Yes ___ No
What age groups are covered by the contact investigation? _____________
6. Health education/promotion: ____ Yes ____ No
7. Do you utilize a Masterlist for referrals of MDR Suspects to Treatment Center?
8. Do you have MDR decentralized case as of now? ___ Yes ___ No
If yes, do you utilize a Masterlist for this? _____________________
9. Do you have any problems in the implementation of DOTS strategy? ____ Yes ___ No
If yes, what are the problems encountered during the implementation of DOTS strategy?
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
10. Do you have any idea or roughly could you estimate the percentage population of the following? :
Roman Catholic: _______ Muslims: ______
Protestants: ___________ Iglesia Ni Cristo (Church of Christ): _______
Others: _______________
Name of Private Facility
Classification
(NGO or Private Clinic)
Kind of services offered
TB Trainings/Orientation
41
BASELINE DATA
A. Case Finding
a. No. Of TB symptomatic examined ______________
b. No. With 3 sputum specimen __________________
c. Three sputum collection rate __________________
d. No. of Smear positive discovered _______________
e. Positivity Rate ______________________________
B. Population________________________________________
New Smear Positive Cases ___________________________
Case Notification Rate ______________________________
Case Detection Rate ________________________________
C. Case Holding
a. New Smear Positive Cases ____________________
b. New Smear Negative Cases ___________________
c. New Smear Negative Cases ( ODT ) _____________
d. Relapse __________________
e. Treatment Failure __________
f. Return After Default ________
g. Transfer In ________________
h. Other Positive _____________
i. Other Negative ____________
j. Extra Pulmonary ___________
k. Total patient initiated to Treatment
D. Treatment Outcome (registered in _____Q of _____ Year)
New Smear Positive Cases No. Percentage
Initiated to Treatment
Cured
Treatment Completed
Success
Died
Failed
Defaulted
Transfer out
New Smear Negative Cases (Treatment Outcome category same as applied to New smear positive cases except for
Cured)
New Smear Negative Cases ( Other Diagnostic Test) (Treatment Outcome category same as applied to New smear
negative cases)
Relapse(Treatment Outcome category same as applied to New smear positive cases)
Return After Default(Treatment Outcome category same as applied to New smear positive cases)
Treatment Failure(Treatment Outcome category same as applied to New smear positive cases)
Other Positive(Treatment Outcome category same as applied to New smear positive cases)
Other Negative(Treatment Outcome category same as applied to New smear negative cases)
Extra Pulmonary(Treatment Outcome category same as applied to New smear negative cases)
42
E. TBDC Report ( ___Q ____Year)
a. Total No. of Smear negative / CXR suggestive TB symptomatic referred to TBDC _______________
TBDC Diagnosis:
b. Total number of active TB case diagnosed by TBDC ______________
i. Classification of active TB cases diagnosed by TBDC________
1. New _______
2. Retreatment _______
3. Total _____________
c. Total number of inactive TB patients __________
d. Total number of patients diagnosed as other lung disease_________
e. Total number of patients evaluated by TBDC this quarter_________
f. Total number of patients recommended by the TBDC for anti TB treatment______
g. No. Initiated to treatment ________
h. Other Recommendations :
i. Surveillance___________
ii. Repeat Chest X-ray ___________
iii. CT Scan ___________
iv. For AP Lateral View __________
F. Children 0-4 yrs old on IPT
i. TB Exposure:_________
j. TB Infection : ________
k. Total _______________
G. IPT Outcome ( ___Q ____Year)
TB Exposure No. Percentage
Initiated to Treatment
Treatment Completed
Died
Failed
Defaulted
Transfer out
TB Infection
Initiated to Treatment
Treatment Completed
Died
Failed
Defaulted
Transfer out
Total Cases
Initiated to Treatment
Treatment Completed
Died
Failed
Defaulted
Transfer out
H. MDR Suspect Referrals
l. No. of MDR suspects registered:__________
m. No. of MDR suspects referred to treatment center _________
n. No. of MDR suspects screened at the treatment center ________
o. No. of confirmed MDR cases ___________
p. No. of MDR cases initiated to treatment :________
q. No. of MDR cases decentralized _____________
43
Annex 2: BASELINE SURVEY Data Collection Form for NonGovernment Organizations
Name of the Health/Facility Organization: __________________________________________
Address: ____________________________________________________________________
Telephone Nos. : ________________________ Fax No. : ___________________
Contact Person: _________________________ Mobile No.: __________________
Population coverage: ____________________
No. of Bgys. Covered: ____________ Depressed Bgy:________ Non-Depressed Bgy: _______
No. of Depressed Population__________ No. of Non- Depressed Population____________
QUESTIONNAIRE:
1. When was your organization established? _____________________________________
2. Is your organization an independent organization? ______________________________
3. Does your organization received grants from other private organization? __Yes __No
If yes, what kind of grant? __________________________________________________
4. Does your organization receive grants from the government? __ Yes __ No
If yes, what kind of grant or assistance? _____________________
5. What are the services provided by the health facility/organization?
a._______________________________________
b. ______________________________________
c. ______________________________________
d. ______________________________________
e. ______________________________________
f. ______________________________________
6. Does your organization have clinic for patients? ___ Yes ___ No
7. If yes, how many staff do you have in the clinic? ___________ (Please enumerate below)
NO. NAME DESIGNATION TB Training/s Conducted by:
1
2
3
4
5
6
44
8. Do you have a volunteer staff? ___ Yes ___ No
If yes, how many? ________________________
9. Are you providing services for :
Adult TB cases? ___ Yes ___ No
TB in Children: ___ Yes ___ No
MDR TB: ___ Yes ___ No
10. When did your organization start providing TB services? _________________________
11. Are the staffs aware of the DOTS strategy of NTP? ___ Yes ___ No
12. Are the staffs following the DOTS strategy of NTP? ___ Yes ___ No
a. If yes, since when? _____________________________________________________
b. If no, are you willing to adopt the DOTS strategy? ___ Yes ___ No
13. What service/s is your clinic providing for TB patients?
a. Diagnosis: Sputum examination: ____ Chest X-ray: _____ PPD:_____ Others:_____
b. Treatment: Free TB medicines: ______ Prescribed medicines: ___________
If anti-TB medicines are for free, where do you get it? __________________
If anti-TB medicines are prescribed, what kind of medicines?_____________
And for how long? ___________________________________________
14. Do you conduct contact investigation? ___ Yes ___ No
If yes, do you utilize a Masterlist for this?
What age groups are covered by the contact investigation? _____________
15. Health education/promotion: ____ Yes ____ No
16. Are the diagnostic work-ups for free? ____ Yes ____ No
If No, how much? Sputum examination: ______ CXR: _______ PPD: ____
No. Name Function/s TB Trainings/Orientation Conducted By:
1
2
3
4
45
17. Does your organization have a laboratory? ____ Yes ____ No
If yes, what services are being provided by the laboratory?
______________________________________________________________________________________________________
__________________________________________________________________________________________________
18. If your clinic is providing sputum microscopy, who does the quality assurance of the smear?
_________________________________________________________________
19. If your clinic is not providing diagnostic work-ups for the following where do you refer the patient?
a. Sputum Microscopy ___________________________________
b. Chest X-ray __________________________________________
c. PPD ________________________________________________
d. Others ______________________________________________
20. If you are providing treatment services for the TB patients, are you doing DOT in the whole course of treatment?
________________________________________________
a. If you are not doing DOT, how frequent is the follow-up of the TB patients? ________________________
21. If you are doing DOTS, are you following the standard recording system provided by the NTP (DOH)? __ Yes __No
If yes, what reporting forms, do you utilize? _______________________________
a. If yes, who does the recording? _____________________
b. If no, do you have a recording system of your own? ____ Yes ____ No
c. If no, are you willing to adopt the standard recording format of the DOH? ____ Yes ____ No
22. If you are not providing services for TB patients, where do you refer them?
a. Health Center: ________________________________________________________
b. Hospital: ___________________________________________________________
c. Private clinic: _________________________________________________________
23. Does your organization have collaboration with other private organization? ___ Yes ___No
If yes, what organization?
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
______________________________________________________________________________________________________
24. Does your organization have collaboration with the government? ____ Yes ____ No
If yes: ___ National or _____ local
25. If your organization has volunteers, do they receive incentives? ___ Yes ____ No
If yes, what kind of incentive, do they receive?
______________________________________________________________________________________________
46
If no incentives are provided, how do you motivate them to stay as volunteer?
______________________________________________________________________________________________________
__________________________________________________________________________________________________
26. Do you have any problems in the implementation of DOTS strategy? __ Yes __No
If yes, what are the problems encountered during the implementation of DOTS strategy?
______________________________________________________________________________________________________
__________________________________________________________________________________________________
27. Nutritional Status
a. Are you aware of the nutritional status of your Adult TB patients? ___ Yes ___ No
b. Are you aware of the nutritional status of your TB in Children? ___ Yes ___ No
28. Do you have any idea or roughly could you estimate the percentage population of the following? :
a. Roman Catholic: ___________
b. Muslims: _____________
c. Iglesia ni Cristo (Church of Christ): ____________
d. Protestants: _______________
e. Others: ___________
47
BASELINE DATA
A. Case Finding
a. No. Of TB symptomatic examined ______________
b. No. With 3 sputum specimen __________________
c. Three sputum collection rate __________________
d. No. of Smear positive discovered _______________
e. Positivity Rate ______________________________
B. Population________________________________________
New Smear Positive Cases ___________________________
Case Notification Rate ______________________________
Case Detection Rate ________________________________
C. Case Holding
a. New Smear Positive Cases ____________________
b. New Smear Negative Cases ___________________
c. New Smear Negative Cases ( ODT ) _____________
d. Relapse __________________
e. Treatment Failure __________
f. Return After Default ________
g. Transfer In ________________
h. Other Positive _____________
i. Other Negative ____________
j. Extra Pulmonary ___________
k. Total patient initiated to Treatment
D. Treatment Outcome ( __Q, _____Year)
New Smear Positive Cases No. Percentage
Initiated to Treatment
Cured
Treatment Completed
Success
Died
Failed
Defaulted
Transfer out
New Smear Negative Cases (Treatment Outcome category same as applied to New smear positive cases except for
Cured)
New Smear Negative Cases (Other Diagnostic Test) (Treatment Outcome category same as applied to New smear
negative)
Relapse (Treatment Outcome category same as applied to New smear positive cases)
Return After Default (Treatment Outcome category same as applied to New smear positive cases)
Treatment Failure (Treatment Outcome category same as applied to New smear positive cases)
Other Positive (Treatment Outcome category same as applied to New smear positive cases)
Other Negative (Treatment Outcome category same as applied to New smear negative cases)
Extrapulmonary (Treatment Outcome category same as applied to New smear positive cases)
48
E. TBDC Report 2012
a. Total No. of Smear negative / x-ray positive TB symptomatic referred to TBDC _______________
TBDC Diagnosis:
b. Total number of active TB case diagnosed by TBDC ______________
i. Classification of active TB cases diagnosed by TBDC________
1. New _______
2. Retreatment _______
3. Total
c. Total number of inactive TB patients __________
d. Total number of patients diagnosed as other lung disease_________
e. Total number of patients evaluated by TBDC this quarter_________
f. Total number of patients recommended by the TBDC for anti TB treatment______
g. No. Initiated to treatment ________
h. Other Recommendations :
i. Surveillance___________
ii. Repeat Chest X-ray ___________
iii. CT Scan ___________
iv. For AP Lateral View __________
F. Children 0-4 yrs old on IPT
a. TB Exposure:_________
b. TB Infection : ________
c. Total _______________
G. IPT Outcome ( 2011)
TB Exposure No. Percentage
Initiated to Treatment
Treatment Completed
Died
Failed
Defaulted
Transfer out
TB Infection
Initiated to Treatment
Treatment Completed
Died
Failed
Defaulted
Transfer out
Total Cases
Initiated to Treatment
Treatment Completed
Died
Failed
Defaulted
Transfer out
H. MDR Suspect Referrals
a. No. of MDR suspects registered:__________
b. No. of MDR suspects referred to treatment center _________
c. No. of MDR suspects screened at the treatment center ________
d. No. of confirmed MDR cases ___________
e. No. of MDR cases initiated to treatment :________
f. No. of MDR cases decentralized ________
49
Annex 3: A Sample Project Design Matrix
Project Name: TB Control and Prevention Project in Socio-economically Unprivileged Areas in Metro Manila, the Philippines
Project Areas: Metro Manila, Philippines and Payatas Quezon City
Beneficiaries
1. Number of all Tuberculosis patients in Tondo, Manila and Payatas in Quezon city :1200 TB cases per year
2. Number of people who have close contact to the above (no. of family contacts 4 per new smear positive
patient assuming 800/year burden) 3200 per year
3. Number of Treatment Failure/Retreatment patients in Tondo, Manila and Payatas in Quezon City : 160
retreatment cases per year
4. No. of HIV positive outpatients at San Lazaro Hospital : 600 HIV positive patients
Ver.1 Date: Jan 13, 2011
Ver.2 Date: Feb 17 2012
Ver.3 Date: Dec 6, 2012
Duration: June 2011-May
2014
NARRATIVE SUMMARY
OBJECTIVELY VERIFIABLE INDICATORS
MEANS OF
VERIFICATION
IMPORTANT
ASSUMPTIONS OVERALL GOAL
Tuberculosis morbidity
and mortality in Tondo,
Manila and Payatas, QC is
decreased in 2015
1. TB mortality rate will be decreased from 38.2/100,000 in 1990
to 19.1/100,000 in 2015 (50% reduction)
WHO Report
Continuous support of
government health
services at all levels to TB
program
HIV/AIDS will not spread
so rapidly
Standard living conditions
of the population will not
drastically worsen
2. TB Morbidity is decreased (or maintained) as follows:
2.1 Incidence of new smear positive TB will be decreased (or
maintained) from 131/100,000 population to 130/100,000 by
2015
WHO report
NTP Report
(DOH)
2.2 Prevalence of new smear positive TB will be decreased from
3.1/1000 in 1997 to 2.0/1000 by 2015
WHO Report
TB prevalence
survey report
(DOH)
3. Prevalence of MDR-TB of new TB Patient will be decreased
from 3.8% in 2003 to 3.0% in 2015.
National Drug
Resistance
Survey Data
(DOH)
Project Purpose
Tuberculosis Infection
prevention/treatment
model is implemented
upon maintained quality
DOTS programme
1. Treatment success rate of New Smear Positive PTB patients is
90% with low defaulter rate (i.e., below 5%)
City Health
Department
Report
Project activities
report
Monitoring
report
Continuous support of
central and local
government health
services at all levels to TB
program
2. No. of registered New Sm+ TB Patients and New Sm- has been
increased by 5% and 10% respectively in 2013. (baseline 2011)
3.Completion rate of INH Preventive Therapy (IPT) is at least 80%
in 2013
4.treatment success rate among retreatment patients doesn't
get worse than the level of 2010(no MDR case)
5. Number of referrals is increased with access rate of 55%.
NARRATIVE SUMMARY
OBJECTIVELY VERIFIABLE INDICATORS
MEANS OF
VERIFICATION
IMPORTANT
ASSUMPTIONS Outputs
1. Advocacy,
Communication, Social
Mobilization (ACSM)
about TB and treatment
among community is
strengthened
1. No of Participants to community assembly is 1, 500 for three
years
Project Activity
report
2. No of Facilities attended to Advocacy Campaign is at least 30
per advocacy campaign
3. No of Participants to Advocacy Campaign is at least 400 per
event
4. No. of TB suspects identified is increased by 10 % in 2013
(Baseline 2011)
5. Knowledge on TB through CHV Training is improved (80%
participants will get score 17 and above. (full score is 25))
2. TB Screening
(Contact investigation for
contacts) is provided in
the project areas
1. No. of facilities that contributed to contact investigation is
more than 25 for three years
Project Activity
report
Sufficient TST kits and
INH for IPT are provided
to the project sites by
DOH/NTP
2. No. of identified TB patients by contact tracing is at least 200
for three years
3. No. of patients on INH Preventive Therapy (IPT) is 700 for
three years.
3. Treatment failure and
other Retreatment TB
patients take anti-TB Drug
Susceptibility Test (DST)
No. of (referred) retreatment TB patients who access the
treatment center is at least 90%
Project
Activities Report
Sufficient number of
second line anti-TB Drugs
are provided to the
project sites by GF
through DOH
50
4. TB Screening among
HIV Positive Patients is
provided and
mechanisms for newly
diagnosed HIV+/TB
patients at San Lazaro
Hospital are in place
1. Guideline about TB Screening and IPT for HIV positive Patients
at SLH is made
San Lazaro
Hospital Project
Report
Project activities
report
Cooperation and
support from NGO and
CHVs are maintained
Governmental Budget
for PPD, INH and TB
drugs are allocated and
stably distributed by
DOH
2. No. of TB Patients identified by TB Screening among HIV
positive patients is available
3. No of HIV positive patients with IPT and IPT completed HIV
positive patients is available
5. Tuberculosis Infection
Control is implemented
at the health facilities in
the project areas
1. Facilities implementing the Infection Control Policy of DOH
achieved at least 50% per level of infection control
Project activities
report
DOH will endorse the
DOH TB Infection Control
Guidelines to LGUs
ACTIVITIES PRE-CONDITION
1. Advocacy, Communication, Social Mobilization (ACSM) about TB and treatment among community is
strengthened
Input
Japan
1. Dispatch of Japanese
Experts
2. Provide Training
Materials
Philippines
1.DOH or Health Office
Personnel
2 NGO Staffs and CHVs.
3. Provide the facility
1.1 Conduct training on Interpersonal Communication Course (IPCC, VCT, PICT)
1.2 Strengthen networking
i. Conduct TB Support Group Meeting (Cured TB Patients Meeting)
ii. Facilitate TB Task force meeting (CHVs Meeting)
iii. Facilitate Barangay chair and committee on health advocacy on TB
1.3 Conduct Advocacy Campaign
i. Lung Month (August)
ii. World TB Day (March)
1.4 Conduct Health Education to community members
1.5 Program Evaluation Workshop with all TB Stakeholders in the project areas
1.6 Disseminate IEC materials on TB care in the community
2. TB Screening (Contact investigation for contacts including kids and adults) is provided in the project areas
2.1 Conduct workshop for situation analysis for TB contact investigation
2.2 Conduct Training on Contact investigation and IPT
2.3 Conduct Chest radiography Training
i. Conduct Training on Quality Chest radiography Taking
ii. Conduct appreciation course on QCXR reading for primary health care physicians
iii. Establish a monitoring and evaluation mechanism with a checklist on quality chest radiography taking
2.4 Conduct monitoring and Evaluation on Contact Tracing and IPT for contacts
3. Treatment failure/Retreatment TB patients take anti TB Drug Susceptibility Test in the direction of the
NTP/PMDT policy and strategy
3.1 Conduct Analysis Workshop based on the case study of Treatment failure / Retreatment TB patients
3.2 Conduct Workshop on developing a system that treatment failure / Retreatment TB patients take drug
susceptibility test for the early treatment
3.3 Conduct orientation on recording of referral of MDR suspects to treatment center
3.4 Develop Logbook for tracking Treatment Failure / Retreatment patients
3.5 Conduct Monitoring and Evaluation on care of treatment failure/ Retreatment TB patients
3.6 Conduct training on management including TB Diagnostics and care of MDR TB patients
4. TB Screening among HIV Positive Patients at San Lazaro Hospital is provided.
4.1 Develop TB Screening and IPT guidelines and its training modules among HIV Positive Patients at San Lazaro
Hospital
4.2 Conduct Training on TB Screening and IPT for HIV/AIDS Patients
4.3 HIV/TB Training
4.4 Conduct Chest radiography Training (same as 2.3)
4.5 Conduct Monitoring and Evaluation on TB Screening and IPT for HIV Positive Patients (Consultative program
review)
5.Tuberculosis Infection Control is implemented at the health facilities in the project areas
5.1 Conduct workshop on developing infection control guidelines (including NTRL/DOH-NTP - UPCPH) in health
facilities in Manila City and Quezon City
5.2 Develop IEC materials on Infection control in health facilities
5.3 Conduct training on Infection Control in health facilities
i. Facilities with only outpatients
ii. Facilities with capacities of hospitalization
5.4 Develop Monitoring and Evaluation Checklist
5.5 Conduct Monitoring and Evaluation after TB Infection Control Training
51
Project Goal Tuberculosis Infection prevention/treatment model is implemented upon maintained quality DOTS programme
Activities
2011 2012 2013 2014
2
nd
Q 3
rd
Q 4
th
Q 1
st
Q 2
nd
Q 3
rd
Q 4
th
Q 1
st
Q 2
nd
Q 3
rd
Q 4
th
Q 1
st
Q 2
nd
Q
6 7 8 9 10 11 12 1 2 3 4 5 6 7 8 9 10 11 12 1 2 3 4 5 6 7 8 9 10 11 12 1 2 3 4 5 6
1.Advocacy, Communication, Social Mobilization(ACSM) about TB and treatment among community is strengthened
1.1 Conduct training on
Interpersonal
Communication
Course(IPCC, VCT, PICT)
Plan
Conduct
1.2 Strengthen networking
i. Conduct TB Support
Group Meeting
Plan
Conduct
ii. Facilitate TB Task
force meeting(CHVs
Meeting)
Plan
Conduct
iii. Barangay chair and
committee on health
advocacy on TB
Plan
Conduct
1.3 Conduct Advocacy Campaign
i. Lung Month
(August)
Plan
Conduct
ii. World TB Day
(March)
Plan
Conduct
1.4 Conduct Health
Education to
community members
Plan
Conduct
1.5 Program Evaluation
Workshop with all TB
Stakeholders in project
areas
Plan
Conduct
1.6 Development of IEC
materials
Plan
Conduct
Annex 4: A Sample of Plan of Operations
(PoOs)
52
2. TB Screening (Contact investigation for contacts including kids and adults) is provided in the project areas.
2.1 Conduct workshop
for situation analysis for
contact investigation
Plan
Conduct
2.2 Conduct Training on
Contact investigation
and IPT
Plan
Conduct
2.3 Conduct Chest radiography Training
i. Conduct Training
on Chest radiography
Taking
Plan
Conduct
ii. Appreciation
course on QCXR reading
for primary health care
physicians
Plan
Conduct
iii. Establishment of
monitoring and
evaluation mechanism
with a checklist on
quality chest
radiography taking
Plan
Conduct
2.4 Monitoring and
Evaluation on Contact
Tracing and IPT for
contacts
Plan
Conduct
3. Treatment failure TB patients take anti TB Drug Susceptibility Test in the direction of the NTP/PMDT policy and strategy
3.1 Conduct Analysis
Workshop based on the
case study of
Treatment failure TB
patients
Plan
Conduct
3.2 Conduct Workshop
on developing a system
that treatment failure
TB patients take drug
susceptibility test for
the early treatment
Plan
Conduct
53
3.3 Conduct
orientation on
recording of referral of
MDR suspects to
treatment center
Plan
Conduct
3.4 Develop Logbook
for tracking Treatment
Failure patients
Plan
Conduct
3.5 Monitoring and
Evaluation on care of
treatment failure TB
patients
Plan
Conduct
3.6 Conduct training on management including TB Diagnostics and care of MDR TB patients
i. Basic TB DOTS
Training
Plan
Conduct
ii. DSSM Training for
Med Tech
Plan
Conduct
iii. CHV Training
Plan
Conduct
iv. MDR Training
Plan
Conduct
4. TB Screening among HIV Positive Patients is provided and mechanisms for newly diagnosed HIV+/TB patients at San Lazaro Hospital are in place
4.1 Develop TB
Screening and IPT
guidelines and its
training modules
among HIV Positive
Patients at San Lazaro
Hospital
Plan
Conduct
54
4.2 Conduct Training
on TB Screening and
IPT for HIV/AIDS
Patients
Plan
Conduct
4.3 HIV/TB Training
Plan
Conduct
4.4 Conduct Chest radiography Training
4.5 Monitoring and
Evaluation on TB
Screening and IPT for
HIV Positive
Patients(Consultative
program review)
Plan
Conduct
5. Tuberculosis Infection Control is implemented at the health facilities in the project areas.
5.1 Conduct
workshop on
developing infection
control guidelines
(including
NTRL/DOH-NTP -
UPCPH) in health
facilities in Manila
City and Quezon City
Plan
Conduct
55
5.2 Develop IEC
materials on
Infection control in
health facilities( a.
Audio- Visual b.
Tarpaulin)
Plan
Conduct
5.3 Conduct training on Infection Control in health facilities
i. Facilities with
only outpatients
Plan
Conduct
ii. Facilities with
capacities of
hospitalization
Plan
Conduct
5.4 Develop
Monitoring and
Evaluation Checklist
Plan
Conduct
5.5 Monitoring and
Evaluation after TB
Infection Control
Training
Plan
Conduct
56
MEMORANDUM OF AGREEMENT
KNOW ALL MEN BY THESE PRESENTS:
This AGREEMENT is made and entered into by and among:
The RIT/ Japan Anti-Tuberculosis Association Philippines, Inc., a non government, non-profit organization
with postal address at 2
nd
Floor PTSI Building, #1853 Tayuman St. Corner Rizal Avenue, Sta Cruz, Manila, Philippines,
duly represented by __________________ in his capacity as President and Chairman of the Board, hereinafter
referred to as
RJPI
and
The CENTER FOR HEALTH DEVELOPMENT METRO MANILA, a government agency created and existing
under the laws of the Republic of the Philippines, with principal office at Welfareville Compound, Brgy. Addition Hills,
Mandaluyong City, represented by ___________________ , in her capacity as the Director IV of Center for Health
Development Metro Manila, herein referred to as CHD-MM
and
The ___________________, local government health department, with principal office at the Quezon City
Hall, Quezon City, represented by ______________, in her capacity as the City Health Officer of Manila Health
Department, herein referred to as MHD
and
The __________________________ a non-government organization with clinic address at Payatas, Quezon City,
represented by _____________________, Executive Director of __________________, herein referred to as the
DOTS Facility.
WITNESSETH:
WHEREAS, the 1987 Constitution mandates the State to protect and promote the right to health of the people and
instill health consciousness among them;
WHEREAS, the DOH as the lead agency for health is responsible for ensuring access to basic public health services to
all Filipinos through the provision of quality and accessible health care;
WHEREAS, the CHD-MM promotes prevention and cure of infectious diseases including Tuberculosis within Metro
Manila
WHEREAS, the RIT/Japan Anti Tuberculosis Association aims to contribute for the provision of quality TB services for
the community.
WHEREAS, the DOTS strategy of the National Tuberculosis Program of the Department of Health is being
implemented by the Manila Health Department;
Annex 5: MEMORANDUM OF AGREEMENT
(NGO DOTS FACILITY)
57
WHEREAS, St. Luigi Orione Foundation Inc, likewise promotes quality care for TB patients;
WHEREAS, consistent with the mandate of the Constitution, the herein contracting parties hereby acknowledge their
joint responsibility and undertaking in the pursuit of providing quality TB services which are available, accessible and
affordable to the community.
NOW THEREFORE, premises considered, the parties have agreed to enter into and bind themselves into this
Agreement, in accordance with the ensuing stipulations;
I. OBJECTIVES:
The objectives of this Memorandum of Agreement are:
1. To identify and establish the roles and responsibilities of the partners in the organization in the delivery
of quality TB care.
2. To develop the capacity of health workers to diagnose and treat TB and implement the NTP through the
DOTS Strategy.
3. To provide diagnostic and treatment services for TB patients following the NTP DOTS Strategy.
4. To establish and strengthen the collaboration and networking among public and non-government
organizations.
II. ROLES and RESPONSIBILITIES:
1. Center for Health Development, Metro Manila shall:
a. Provide training and updates on NTP.
b. Oversee project implementation in coordination with RIT/Japan Anti- Tuberculosis Association
Philippines, Inc. and MHD.
c. Provide overall monitoring of the program implementation.
d. Provide NTP drugs and other logistics (reagents, sputum cups, glass slides, and recording forms) to
the DOTS facility.
e. Provide NTP drugs and other logistics (reagents, sputum cups, glass slides, and recording forms) to
the DOTS facility.
2. The RIT/Japan Anti- Tuberculosis Association Philippines, Inc. shall:
a. Provide training funds and assist the DOH -CHD MM, MHD in the provision of training and updates
about TB and TB related matters to the DOTS facility.
b. Coordinate the quarterly consultation meeting with DOH-CHD-MM, MHD and the DOTS Facility.
c. Assist the DOTS facility in conducting its advocacy and health promotion campaign.
d. Assist the DOTS facility and other partners in the establishment of community organization in the
area.
e. Assist the DOH-CHD-MM and MHD in monitoring, supervising and evaluating the program
implementation and recommend corrective measures in the designated DOTS facility.
f. Provide some equipment which can be utilized by the DOTS facility for the implementation of the
program.
g. Conduct operational researches in coordination with the partners to monitor and
and evaluate the program implementation in the area.
3. The Quezon City Health Department shall:
a. Assist DOH-CHD-MM and RIT/JATA Philippines Inc. in the provision of training of the health staff of
the DOTS facility on TB.
58
b. Facilitate the quarterly consultation meeting with DOH-CHD-MM, RIT/JATA Philippines, Inc. and the
DOTS Facility.
c. Conduct supervision, monitoring and evaluation of the program implementation of the DOTS facility.
d. Implement quality assurance activities of sputum smear microscopy.
e. Facilitate the review of Smear negative, X-ray Positive PTB referred by the DOTS facility through the
TBDC.
f. Assist in the planning and evaluation of the project of RIT/JATA Philippines, Inc.
g. Ensure that all NTP supplies in coordination with DOH-CHD-MM are available at the DOTS facility.
4. The ( Name of DOTS Facility ), Inc. shall:
a. Conduct TB Case finding activities.
All TB symptomatic must undergo sputum examination with or without x-ray result.
3 sputum specimens must be collected and submitted.
b. Ensure that all identified TB patients shall take his/her medicines daily (Tutok Gamutan).
c. Implement proper recording and reporting system.
d. Submit AFB slides to Manila NTP coordinators for quality assurance.
e. Submit NTP quarterly and annual reports to MHD and copy furnish RIT/Japan Anti-Tuberculosis
Association Philippines, Inc.
f. Conduct defaulter tracing by trained health volunteers.
g. Ensure management of NTP logistics.
h. Conduct health promotion and advocacy campaign for TB.
i. Actively participate in the consultative workshops and Program Implementation Review (PIR) which
will be conducted by RIT/Japan Anti-Tuberculosis Association Philippines, Inc. in collaboration with
DOH-CHD-MM and MHD.
III. Period of Cooperation :
The period of cooperation shall commence on the date of signing of the document as agreed by all
parties concerned.
IV. Duration and Renewal:
This agreement shall take effect upon signing of the document. Prior to its effect, however, all
parties shall take all necessary steps to ensure performance and compliance of the undertakings.
This agreement shall be in abeyance with the possibility of extension, unless otherwise terminated
by any party. Revision or amendment of this Agreement, however, shall require consultation and the
consent of all parties.
In case of ambiguity of any provision of this agreement or conflict of interpretation by the parties,
the interpretation which is for the best interest of the people shall prevail with the Department of
Health facilitating and mediating the process for clarity.
V. Penalties and Guaranties:
1. Any partners shall have the right to terminate this agreement at any time with 30 days notice in
writing indicating reasons for the same to all partners.
2. If a partner wishes to continue the contract, it must respond in writing within 30 days of receipt of
the termination notice.
3. If a resolution among the partners is not possible, then the Department of Health shall attempt to
resolve the dispute. The Department of Health will make the final decision on this matter, if
necessary.
4. Failure to implement the project as agreed upon may lead to termination of this agreement
59
________________________ ________________________
(Name of Executive Director) (Name of City Health Officer )
Designation City Health Officer
Name of Organization Quezon City Health Department
_____________________________________ _____________________________________
Name of the President Name of Regional Director
President, Chair of the Board Director IV
RIT/Japan Anti-Tuberculosis Association Center for Health Development-Metro
Philippines, Inc. Manila
SIGNED IN THE PRESENCE OF
_______________________ _____________________
Name of DED Name of Administrator
Deputy Executive Director Administrator
RIT/Japan Anti-Tuberculosis Association RIT/Japan Anti-Tuberculosis Association
Philippines, Inc. Philippines, Inc
ACKNOWLEDGEMENT
REPUBLIC OF THE PHILIPPINES )
CITY OF MANILA ) S.S.
BEFORE ME, this _______ day of ________ personally appeared:
CTC No. Issued at/on
Name of the Head of the Organization __________ __________________
Name of City Health Officer __________ __________________
Name of the President of BOT __________ __________________
Name of the Regional Director __________ __________________
WITNESS MY HAND AND SEAL on the date and place above written.
Doc. No. __________
Page No. __________
Book No. __________
Series of __________
60
MEMORANDUM OF AGREEMENT
KNOW ALL MEN BY THESE PRESENTS:
This Agreement is made and entered into by and among:
The RIT/ Japan Anti-Tuberculosis Association Philippines, Inc., a non government non-profit organization
with postal address at 2
nd
Floor PTSI Building, #1853 Tayuman St. Corner Rizal Avenue, Sta Cruz, Manila, Philippines,
duly represented by ___________________________
In his capacity as President and Chairman of the Board, hereinafter referred to as
RJPI
and
The CENTER FOR HEALTH DEVELOPMENT METRO MANILA, a government agency created and existing under
the laws of the Republic of the Philippines, with principal office at Welfareville Compound, Brgy. Addition Hills,
Mandaluyong City, represented by_________________, in her capacity as the Director IV of Center for Health
Development Metro Manila, herein referred to as CHD-MM
and
The Manila Health Department, local government health department, with principal office at the Quezon City
Hall, Quezon City, represented by _____________, in her capacity as the City Health Officer of Manila Health
Department, herein referred to as MHD
and
The Name of Ref Fac, a non-government organization with address at (Address) represented by
MS._________, Executive Director of ________________________________________, herein referred to as the
Referring Facility
WITNESSETH:
WHEREAS, the 1987 Constitution mandates the State to protect and promote the right to health of the people and
instill health consciousness among them;
WHEREAS, the DOH as the lead agency for health is responsible for ensuring access to basic public health services to
all Filipinos through the provision of quality and accessible health care;
WHEREAS, the CHD-MM promotes prevention and cure of infectious disease including Tuberculosis within Metro
Manila.
WHEREAS, the RIT/ Japan Anti Tuberculosis Association aims to contribute for the provision of quality TB services for
the community.
WHEREAS, the DOTS strategy of the National Tuberculosis Program of the Department of Health is being
implemented by the Manila Health Department;
Annex 6: MEMORANDUM OF AGREEMENT
(NGO REFERRING FACILITY)
61
WHEREAS, _______________, likewise promotes quality care for TB patients;
WHEREAS, consistent with the mandate of the Constitution, herein contracting parties hereby acknowledge their
joint responsibility and undertaking in the pursuit of providing quality TB Services which are available, accessible and
affordable to the community.
NOW THEREFORE, premises considered, the parties have agreed to enter into and bind themselves into this
Agreement, in accordance with the ensuing stipulations;
I. OBJECTIVES:
The objectives of this Memorandum of Agreement are:
1. To identify and establish the roles and responsibilities of the partners in the organization in the delivery of
quality TB care.
2. To develop the capacity of health workers to identify and refer TB symptomatics and provide treatment
services for TB patients following the NTP DOTS Strategy.
3. To establish and strengthen the collaboration and networking among public and non-government
organizations.
II. ROLES and RESPONSIBILITIES:
1. Center for Health Development, Metro Manila shall:
a. Provide training and updates on NTP.
b. Oversee project implementation in coordination with RIT/Japan Anti- Tuberculosis Association
Philippines, Inc. and MHD
c. Provide overall monitoring of the program implementation.
d. Assist in the planning and evaluation of the project of RIT/JATA Philippines, Inc.
2. The RIT/Japan Anti- Tuberculosis Association Philippines, Inc. shall:
a. Provide training funds and assist the DOH CHD MM, MHD in the provision of training and updates
about TB and TB related matters to the DOTS facility.
a. Coordinate the quarterly consultation meeting with DOH-CHD-MM, MHD and the DOTS Facility.
c. Assist the Referring facility in conducting its advocacy and health promotion campaign.
d. Assist the Referring facility and other partners in the establishment of community organization in the
area.
e. Assist the DOH-CHD-MM and MHD in monitoring supervising and evaluation the program
implementation and recommend corrective measures in the designated DOTS facility.
f. Provide some equipment and NTP logistics like forms which can be utilized by the Referring facility for
the implementation of the program.
g. Conduct operational researches in coordination with the partners to monitor and evaluate the program
implementation in the area.
3. The Manila Health Department shall:
a. Assist CHD-MM and RIT/JATA Philippines Inc. in the provision of training of the health staff and
volunteers of the Referring facility on TB
b. Facilitate the quarterly consultation meeting with CHD-MM, RIT/JATA Philippines, Inc and the DOTS
Facility.
c. Conduct supervision, monitoring of the Referring facility
d. Assist in the planning and evaluation of the project of RIT/JATA Philippines, Inc.
4. The Name of (Referring Facility), shall:
a. Identify and refer TB symptomatics to the designated DOTS Facility in the area.
b. Act as treatment partners of DOTS and ensure that all identified TB patients shall take his/her
medicines daily (Tutok Gamutan).
62
c. Implement proper recording and reporting system.
d. Conduct defaulter tracing by trained health volunteers.
e. Conduct health promotion and advocacy campaign for TB.
f. Actively participate in the consultative workshops and Program Implementation Review (PIR) which will
be conducted by RIT/Japan Anti-Tuberculosis Association Philippines, Inc, in collaboration with DOH-CHD-
MM and MDH
III. Period of Cooperation:
The period of cooperation shall commence on the date of signing of the document as agreed by all
parties concerned.
IV. Duration and Renewal:
This agreement shall take effect upon signing of the document. Prior to its effect, however, all
parties shall take all necessary steps to ensure performance and compliance of the undertakings.
This agreement shall be in abeyance with the possibility of extension unless otherwise terminated by
any party. Revision or amendment of this Agreement, however, shall require consultation and the
consent of all parties.
In case of ambiguity of any provision of this agreement or conflict of interpretation by the parties,
the interpretation which is for the best interest of the people shall prevail with the Department of Health
facilitating and meditating the process for clarity.
V. Penalties and Guaranties:
1. Any partners shall have the right to terminate this agreement at any time with 30 days notice in writing
indicating reasons for the same to all partners.
2. If a partner wishes to continue the contract, it must respond in writing within 30 days of receipt of
termination notice.
3. If a resolution among the partners is not possible, then the Department of Health shall attempt to
resolve the dispute. The Department of Health will make the final decision on this matter, if necessary.
4. Failure to implement the project as agreed upon may lead to termination of the agreement.
SIGNED IN THE PRESENCE OF:
____________________________ MS._____________________
Executive Director TB Coordinator RIT/Japan Anti-
Tuberculosis Association Philippines, Inc. Ref Facility
ACKNOWLEDGEMENT
REPUBLIC OF THE PHILIPPINES )
CITY OF MANILA ) S.S
BEFORE ME, this _________ day of ___________ personally appeared:
63
CTC No. Issued at/on
Name of the Head of the Organization ___________ ___________
Name of the City Health Officer ___________ ___________
Name of the President of BOT ___________ ___________
Name of the Regional Director ___________ ___________
WITNESS MY HAND AND SEAL on the date and place above written.
Doc. No. _______
Page No. _______
Book No. _______
Series of _______
DR._____________________ ___________________________
Executive Director City Health Officer
Manila Health Department
_____________________ ___________________________
President Director IV
RIT/Japan Anti-Tuberculosis Association Center for Health Development-Metro Manila
Philippines, Inc.
64
Date: ______/ ______/ _________
Name of Facility: ______________________ Date when film was taken: ____/ _____/ ________
Patient Name or ID number: _____________________________________
1) Identification marking of the patient 1. Good 2. Fair 3. Poor
2) Patient Positioning
Good is the score of 0 or 1 excluding items i or ii.
Fair is neither Good nor Poor
Poor is a score of 5 or more, or any score with both
i and ii
Please check the following 7 items:
i. Defective lung fields Yes or No
ii. Poor Inspiration Yes or No
iii. Oblique positioning Yes or No
iv. Position of clavicles Yes or No
v. Position of scapulas Yes or No
vi. symmetric density of lungs Yes or No
vii. Foreign substance Yes or No
1. Good 2. Fair 3. Poor
3) Density
Sub Total Score
1. Good (4-5)
2. Fair (6-9)
3. Poor (10-12)
1. Lung Field
1. good 2. fair 3. poor
If 2 or 3, please specify your reason: i. Excessive ii. Insufficient
2. Lung Periphery
1. good 2. fair 3. poor
If 2 or 3, please specify your reason: i. Excessive ii. Insufficient
3. Mediastinum
1. Good 2. fair 3. poor
If 2 or 3, please specify your reason: i. Excessive ii. Insufficient
4. Cardiac Shadow 1. Good 2. fair 3. poor
If 2 or 3, please specify your reason: i. Excessive ii. Insufficient
4) Contrast
Sub Total Score
1. Good (4-5)
2. Fair (6-9)
3. Poor (10-
12)
1. Lung Field 1. good 2. fair 3. poor
2. Lung Periphery 1. good 2. fair 3. poor
3. Mediastinum 1. good 2. fair 3. poor
4. Cardiac Shadow 1. good 2. fair 3. poor
5) Sharpness 1. Good 2. Fair 3. Poor
6) Artifacts
If 2 or 3, please indicate the place
Of artifacts on this figure:
Excellent: 6 or 7 Good: 8-11 without any Poor/ Present
Fair: 8-13 Poor/Presents or less Poor: 14-18 or with 3 Poor/ Presents or more
Radiation protection for the gonad Gonads are protected Gonads are NOT protected
Comments Assessor
Citation: http://www.tbrieder.org/publications/books_english/radiography.pdf
1. None
2. Slight
3. Present
Assessment Result: Total Score for the 6 Factors is _______ (6-18)
Annex 7: Assessment Sheet for Imaging Quality of Chest Radiography
65
Annex 8: CHV TB Symptomatic Masterlist
Referral
No.
(1)
Date of
Registration
(2)
Name of TB
Symptomatics
(3)
Complete Address
(4)
Bgy
(5)
Contact
No.
(6)
Age
(7)
Sex
(8)
Date
Identified
(9)
Date
Referred
(10)
Date
Consulted
(11)
TB Case
(Y/N), If Y,
Case No.
(12)
Class
(P/EP)
(13)
Type
(N/R/TI/
TF/RAD/O)
(14)
Cat
(I/II/III)
(15)
Type of Patient
Treatment Outcome
Cured
Treatment
Completed Died Failed Default Transfer out
New Smear Positive
New Smear Negative
Relapse
Treatment Failure
Return After Default
Other Positive
Other Negative
*left portion of the Masterlist
*bottom portion of the Masterlist (summary table)
66
Date/ Result
of DSSM
(16)
Date/ Result
of other
exam
(17)
Date/ CXR
result
(18)
TBDC Decision
(19)
Treatment
Initiated (Y/N)
(20)
Treatment Partners
(1:HW/2:BHW/3:CHV/4:FM/5:Others)
(21)
Treatment Outcome
(22)
Remarks
(23) Cured Comp Died Failed Defaulted Transout
No. of TB Symptomatics
Identified
No. of TB
Symptomatics
Referred
No. of TB
Symptomatics
Consulted
No. of True TB
Symptomatics
No. of TB
Symptomatics
with DSSM
No. of
Symtomatics
with other
Bacteriologic
Exam
Total No. of
TB Cases
Diagnosed
TB Cases Diagnosed
Total No.
of TB
Cases
Initiated
Tx
No. of TB
patients
with
Treatment
Partners
Pulmonary
EP
New (N) Relapse T.Failure RAD Other Other
N+ N- R TF RAD O+ O-
No. by
Type
1:
2:
3:
4:
5:
6:
Initiated
Treatment
*right portion of the Masterlist
*bottom portion of the Masterlist (summary table)
67
The following are the information needed for each item on the CHV TB Symptomatic Referral Masterlist:
(1) Serial Number assigned to a TB Symptomatic after registration
(2) Exact date when the patient was registered in the CHV TB Referral Masterlist
(3) Patients full name (family name first in bold capital letters, followed by given or first name)
(4) Patients complete address (street name (ALL CAPITAL LETTERS) first, then number, including nearest landmark (if available), to easily
locate the patient
(5) The Barangay name or number where the patient resides including the zone number where appropriate
(6) Landline Number/cell phone numbers of the patient/relatives/significant others who can help locate the patient.
(7) Patients age in years
(8) Patients gender (M for male and F for female)
(9) Exact date when the patient was identified as TB Symptomatic
(10) Exact date when the patient was referred to a DOTS Facility for DSSM/diagnosis/Result of sputum examination
(11) Exact date when the patient was seen/ examined by the physician
COLUMNS 12 TO 23 to be filled-out by the Nurse at the DOTS Facility
(12) Patient case number seen in the NTP registry if referral enrolled for treatment. N if not TB case.
(13) Classification of TB according to location. (pulmonary / Extra-pulmonary).
(14) Type of patient enrolled. (New, Transferred-in, Treatment Failure, Return after default and other).
(15) Category of treatment for the treatment regimen to be given to patient.
(16) Exact date and result of sputum exam of patient.
(17) Exact date and result of other examination. (e.g. skin test.. etc.
(18) Exact date and result of chest X-ray.
(19) Decision of TB Diagnostic Committee for the patient treatment.
(20) Y if the patient starts treatment on TB and N if not treated for TB.
(21) Indicate the Name and position of Treatment partner.
(22) Indicate the exact date of last drug intake on the outcome of treatment.
(23) Remarks- This refers to any actions taken on the patients behalf. Any observation or comment made by CHVs or HCWs that needs
attention. This column can be utilized by both the CHVs and HCWs. You can also indicate reason/s that arise/s from the time of referral, course
of treatment and outcome of treatment. (Ex. Refused to go to DOTS Facility Did not submit second sputum specimen).
Summary Table to be filled-out by the Nurse at the DOTS Facility
HOW TO REGISTER IN THE CHV REFERRAL MASTERLIST
COLUMN 1: Serial Number
Assign a new number to each patient being registered.
10-001 where:
10- Refers to the last 2 digits of the current year Ex. 10 for 2010
001- Patients serial number based on the CHV Referral Masterlist of the current year.
The patients serial number should start with 001 at the beginning of every year. Assign the next number in the last 3 digits every time you
register a new patient.
Example:
Today is April 12, 2010 and you are registering 4 patients in the CHV Masterlist. The last serial number in the CHV TB Referral Masterlist is 10-
013.
The Serial Number of the next patients will be:
COLUMN 2: Date of Registration
Write the date when you register a patient in the CHV TB Referral Masterlist.
The month and day should be written as: month/day/year.
Example: 04/12/10
COLUMN 3: Name of TB Symptomatic
Write the patients full name (family name first in bold capital letters, followed by given or first name)
Example:
QUERRI, Aurora Archangel
Patient 1 10-014
Patient 2 10-015
Patient 3 10-016
Patient 4 10-017
68
COLUMN 4: Complete Address
Write the patients complete address, including nearest landmark (if available), to easily locate the patient.
Example: a. CENTRAL AVENUE. Blk 8 Lot 1 QC Ville Subdivision, Quezon City (Aqua soft water refilling station, across)
COLUMN 5: Barangay/Zone Number
Write the Name of the Barangay or the Number of the Bgy where the patient resides.
Example:
Bgy /Zone Bgy/Zone
Central 95 /8
COLUMN 6: Contact Number
Landline Number /or cellphone numbers of the patient/relatives/significant others who can help locate the patient.
Example: If this is the contact number of the patient, we write:
0920-9033582 or 740-8054 /0920-9033582
For Contact Numbers of Relative/Friends/Significant Others (Other than the patient), we write:
Teddy (Relative) - 0920-143-4452 or Teddy (Relative)-143-5254
COLUMN 7: Age
Write the patients age in years.
Example: 36 y/o
COLUMN 8: Sex
Patients gender (M for male and F for female)
COLUMN 9: Date Identified
Write the Exact date when the patient was identified as TB Symptomatic. The month, day and year should be written as:
04/12/10 where : 04- stands for April, 12- stands for day of the month and 10- stands for the last two digits of the current year.
COLUMN 10: Date Referred
Write the Exact date when the patient was referred to a DOTS Facility for DSSM/diagnosis. The month, day and year should be written as:
04/12/10 where : 04- stands for April, 12- stands for day of the month and 10- stands for the last two digits of the current year.
04/13/10 where : 04- stands for April, 13- stands for day of the month and 10- stands for the last two digits of the current year.
(YOU WILL HAVE TO MAKE USE OF THE REFERRAL FORM WHENEVER YOU REFER THUS; THE COLUMN DATE REFERRED SHOULD MATCH
THE DATE WHEN YOU ACTUALLY REFERRED THE PATIENT WHICH IS REFLECTED IN THE REFERRAL FORM THE PATIENT WHICH IS REFLECTED
IN THE REFERRAL FORM.)
COLUMN 11: Date Consulted/Assessed
The exact date when the patient was seen/ examined by the physician or:
the exact date when the patient was assessed by the nurse or midwife.
The month, day and year should be written as:
04/12/10 where : 04- stands for April, 12- stands for day of the month and 10- stands for the last two digits of the current year.
04/13/10 where : 04- stands for April, 13- stands for day of the month and 10- stands for the last two digits of the current year.
Remarks
This refers to any actions taken on the patients behalf. Any observation or comment made by CHVs or HCWs that needs attention.
This column can be utilized by both the CHVs and HCWs. You can also indicate reason/s that arise/s from the time of referral, course of
treatment and outcome of treatment. (Ex. Refused to go to DOTS Facility Did not submit second sputum specimen).
Note: The CHVs accomplish COLUMNS 1- 11 AND 24 ONLY.
The NURSES accomplish/update COLUMNS 12- 24
69
COLUMN 12: TB Case (TB Case No. /N):
If the patient was diagnosed as TB Case, write the TB CASE NO.
If the patient is not a TB case, write N.
COLUMN 13: Classification of TB (P/EP):
Write P for Pulmonary TB and EP for Extra Pulmonary TB as defined on the Manual of Procedures (MOP).
COLUMN 14: Type of Patient (N/R/TF/RAD/O):
Indicate the following for:
N New TB Patient/ R- Relapse/ TF Treatment Failure /RAD- Return After Default/ O (+)- for Other (+)/ O (-) - for Other (-)
N.B.: Type of patient as defined on the MOP.
COLUMN 15: Category of Treatment (I,II,III):
Write I- for Category I
Write II- for Category II
Write III- for Category III
N.B.: Category of patient as defined on the MOP.
COLUMN 16: Date/Result of DSSM (+)/0) :
Record the DATE over the RESULT OF DSSM where appropriate:
Ex. For DSSM Positive: 05/28/2012 over +2 or for DSSM Negative: 05/28/2012 over O
N.B.: Record the DSSM result as specified on the MOP.
COLUMN 17: Date/Result of Other Examination (Ex. Culture etc.)
Record the DATE over the RESULT OF the EXAMINATION where appropriate:
COLUMN 18: Date/CXR Result:
Record the DATE over the Chest X-Ray Result where appropriate:
Example: if done: 05/28/2012 over PTB Minimal *Note:IF NOT DONE: Write N for No or None
COLUMN 19: TBDC Decision (Y/N)
Write Y for Yes if it passed through the TBDC.
Write N for No if it did not pass through the TBDC.
N.B.: Based on the stipulations on the MOP for the Smear Negative Cases with TB Chest X-Ray Findings.
COLUMN 20: Treatment Initiated (Date of Treatment/N):
Treatment refers to anti-TB treatment received by the patient.
If the patient was initiated with anti-TB treatment, write the EXACT DATE THE PATIENT WAS PLACED ON TREATMENT. Ex. 05/31/2012
Write N for No if treatment was not initiated and INDICATE THE REASON/S ON THE Remarks column.
COLUMN 21: Treatment Partner (HW/BHW/CHV/FM/Others):
Indicate the following where appropriate:
1- if the treatment partner is a health worker
2- if the treatment partner is a Barangay Health Worker
3- if the treatment partner is a Community Health Volunteer.
4- if the treatment partner is a Family Member. Reminder: Least priority as a Treatment Partner.
5- refers to the treatment partner apart from No. 1-4 and 6. Example friend or neighbour trained to
become a Treatment partner.
70
COLUMN 22: Treatment Outcome (Cured/Completed/Died/Failed/Defaulted/Transferred Out):
Write the date on the columns specific for the treatment outcome of the patient.
Cured Completed Died Failed Defaulted Transferred Out
05/31/2012
N.B.: The Treatment Outcome as specified on the MOP.
COLUMN 23: Remarks:
Any observation or comment made by CHVs or HCWs that needs attention. This column can be utilized by both the CHVs and HCWs. You can
also indicate reason/s that arise/s from the time of referral, course of treatment and outcome of treatment. (Ex. Refused to go to DOTS Facility
Did not submit second sputum specimen).
*Summary Table to be filled-out by the Nurse at the DOTS Facility
71
Annex 9: NTP Symptomatic Referral Form
Upper part: (To be accomplished by the referring unit/ NGO)
TB Symptomatic [ ] Yes [ ] No
TB Symptomatic Serial No.____
Date: _________
Please facilitate completion of information of patient bearing this referral form
Name of Referring unit/ NGO: Tel no:
Fax no.
Mobile no:
Email:
Full address of Referring unit/ NGO:
Name of Receiving DOTS Facility: Tel no:
Fax no.
Mobile no:
Email:
Full address of receiving DOTS Facility:
Name of Patient: Age: Sex: ( )M ( )F
Full address of Patient: Tel no. Mobile:
Dati na bang nakainom ng gamot laban sa tuberculosis o TB? [ ]Oo [ ]Hindi
Signs/Symptoms (Palatandaan/Sintomas) (Lagyan ng tsek ang kahon ayon sa nararamdaman ng pasyente)
[ ] Ubo ng 2 linggo o higit pa [ ] pananakit ng dibdib o likod
[ ] lagnat [ ] pagbaba ng timbang
[ ] dura na may dugo
Printed Name & Signature of Referring Staff: Designation: Date/Time
Referred:
Lower part: (To be accomplished by Receiving DOTS Facility)
Date/ Time Referral Received:_______________________
Name of Receiving DOTS Facility: Tel no.
Fax no
Email:
Full address of receiving DOTS Facility:
Mobile no.
Name of Patient Age Sex: ( )M ( )F
Full address of Patient: Tel no. Mobile:
Dati na bang nakainom ng gamut laban sa tuberculosis o TB? [ ]Oo [ ]Hindi
Kailan: ___buwan/____(araw)/(taon)
Pangalang ng gamot:________________________
Action Taken:
[ ] DSSM, write date/ results:________ [ ] Referred to Treatment Center
[ ] TST, write date/ results:__________ (Pls Specify name:_____________)
[ ] Others:______________________________________________________ (Pls Specify)
Printed Name of Receiving DOTS Facility staff and signature: Designation:
72
The following are the information needed for each item on the NTP Symptomatic Referral Form:
Upper Part to be ACCOMPLISHED BY THE CHV and left at the DOTS Facility
(1) Exact Date the patient was referred (Ex. 05/28/2012)
(2) The Name of the Referring Unit/NGO/or Group who referred the patient to the DOTS Facility
(Ex. TB Life Savers (TB Support Group of T.F. H.C.) or CCT Parola)
(3) Full address of the referring Unit/NGO/or Group who referred the patient to the DOTS Facility
(4) Telephone No/Fax No./Mobile No. of the referring unit/NGO/ or group who referred the patient to the DOTS Facility
(5) Email address of the referring unit//NGO/ or group who referred the patient to the DOTS Facility
(6) Name of DOTS Facility who received referral (Ex. Vitas Health Center /Canossa)
(7) Full address of the DOTS Facility who received referrals
(8) Telephone No/Fax No./Mobile No. of the DOTS Facility
(9) Email address of the DOTS Facility
(10) Patients full name (family name first in bold capital letters, followed by given or first name)
(11) Patients age in years (38 y/o)
(12) Patients gender (M for male and F for female)
(13) Patients complete address (street name (ALL CAPITAL LETTERS) first, then number, including nearest landmark (if available), to easily
locate the patient.
Write the patients complete address, including nearest landmark (if available), to easily locate the patient.
Example:
a. CENTRAL AVENUE . Blk 8 Lot 1 QC Ville Subdivision, Quezon City (Aqua soft water refilling station, across)
(14) The Barangay name or number where the patient resides including the zone number where appropriate
Write the Name of the Barangay or the Number of the Bgy where the patient resides.
Example:
Bgy /Zone Bgy/Zone
Central 95 /8
(15) Landline Number/cell phone number of the patient/relatives/significant others who can help locate the patient.
(16) History of Anti-TB Treatment (Y/N)
(17) Sign/Symptoms of the patient (Guided Put a check mark on the S/S)
( ) cough of two weeks or more ( ) chest/back pain)
( ) Fever ( ) weight faltering
( ) blood tinged sputum/or hemoptysis
(18) Name /Signature of the Referring Staff
(19) Designation of the staff who referred to the DOTS Facility
73
(20) Exact date and Time when the patient was referred
N.B.: THE RIGHT UPPER CORNER OF THE UPPER PART WILL BE UPDATED BY THE NURSES.
Lower Part (To be accomplished by the RECEIVING DOTS FACILITY and will be returned to the Referring Unit)
(1)Date/Time the referral was received by the DOTS Facility
(2) Name of the receiving DOTS Facility
(3) Full address of the receiving DOTS Facility
(4) Telephone No/Fax No./Mobile No. of the receiving DOTS Facility
(5) Email address of the receiving DOTS Facility
(6) Patients full name (family name first in bold capital letters, followed by given or first name)
(7) Patients age in years
(8) Patients gender (M for male and F for female)
(9) Patients complete address (street name (ALL CAPITAL LETTERS) first, then number, including nearest landmark (if available), to easily
locate the patient (same as above)
(10) The Barangay name or number where the patient resides including the zone number where appropriate (same as above)
(11) Landline Number/cell phone numbers of the patient/relatives/significant others who can help locate the patient.
(12) History of Anti-TB Treatment /Date and Name of Medicines taken
History of TB Treatment - Put a check mark ( ) Yes or ( ) No
Date of TB Treatment- Specify Month/Day/Year
Name of Medicine Taken - Specify the name/names of the medicine taken
(13) Action Taken (Guided- Put a check part/specify)
( ) DSSM, write date/results: _______________
( ) TST, write date/results: _________________
( ) Others: specify ________________________
( ) Referred to Treatment Center, specify the name of the Treatment Center
(18) Name /Signature of the DOTS Facility Staff who attended the patient
(14) Designation of the DOTS Facility staff who attended the patient
N.B.: THE RIGHT UPPER CORNER OF THE UPPER PART WILL BE UPDATED BY THE NURSES.
TB Symptomatic Put a check mark if ( ) Yes TB Symptomatic based on the MOP criteria for Adult and Children. Put a check mark if ( ) No-
patient is not classified as TB Symptomatic.
TB Symptomatic Serial No. Just copy this information from TB Symptomatic Masterlist
(12-001- Current year then patients case number as TB Symptomatic.
74
Annex 10: Modified Masterlist B
Date when
TB case was
registered
(1)
TB
Case
No of
Index
case
(2)
Sputum/
TST result
of
Registere
d Case
before
treatment
(3)
Name of
Contacts
(4)
Age
(5)
Sex
(6)
Address
(7)
Clinical Signs & Symptom (Check)
(8)
Date
Evaluated
(9)
TB
Sympt
(10)
Diagnostic Procedure
(11) Cough
2wks
or
more
Fever Loss
of
appet
ite
Non
Response
to
antibiotic
Failure
to regain
previous
state of
health
Child has loss
his normal
energy/activity
DSSM
CXR
Result/
TBDC
Recomm
endation
TST
*left portion of the Masterlist
75
TB Case
Number
(12)
Classification
of TB
(13)
TYPES OF TB
(14)
TREATMENT OUTCOME
(15)
Treatment
Partner
(16)
Remarks
(17)
New Retreatment Cases
Trans-
In
Sm+ Sm- Relapse
Treatment
Failure
RAD
Other
Cured
Completed
Treatment
Died Failed Defaulted
Transferred
out
Total No.
Evaluated + -
*right portion of the Masterlist
76
HOW TO ACCOMPLISH THE MODIFIED MASTERLIST B
COLUMN 1: Date when TB case was registered
Write the date when the index case was registered on the TB Register.
The month and day should be written as: month/day/year.
Example: 04/12/10
COLUMN 2: TB Case No. of Index case
Write the TB case number of the index case registered on the TB Register.
Example: 13501003
COLUMN 3: Sputum/TST result of Registered Case before treatment
Write the result of the Sputum/TST of the index case registered on the TB Register before treatment
Example: + (positive)
COLUMN 4: Name of Contacts
Write the full name of the household contacts of the Index case (family name first in bold capital letters, followed by given or first name and
middle Initial.)
Example: MANAPAT, Paeng M.
COLUMN 5: Age
Write the age in years of the registered household contacts.
Example: 36 y/o
COLUMN 6: Sex
Write the gender of the registered household contacts (M for male and F for female)
COLUMN 7: Address
Write the complete address of the registered household contacts, including nearest landmark (if available), to easily locate them.
Example: a. CENTRAL AVENUE . Blk 8 Lot 1 QC Ville Subdivision, Quezon City (Aqua soft water refilling station, across)
COLUMN 8: Clinical Signs and Symptom ( Please Check)
Put check () mark on a column with the specified signs and symptoms of those registered household contacts where appropriate.
COLUMN 9: Date Evaluated
Write the date when the household contacts were evaluated
Example: 4/15/10
COLUMN 10: TB Symptomatic
Write Yes, if the household contacts were classified as TB Symptomatic and put a No, if not TB Symptomatic
COLUMN 11: Diagnostic Procedure
Write the date and the result of the diagnostic procedures done to the household contacts as per Physicians request. Upper portion : result,
lower portion : date the diagnostic procedures was done
Example: DSSM- (2+) / 4/15/10
CXR Result/TBDC Recommendation- Minimal PTB/Anti-TB Treatment or Cat III / 4/15/2010
TST- (10mm) / 4/15/10
COLUMN 12: TB Case Number
Write the TB Case Number of the household contact who initiated treatment. This is indicated on the TB Register.
Example: 13501010
COLUMN 13: Classification of TB
Write P for Pulmonary TB and EP for Extra Pulmonary TB as defined on the Manual of Procedures (MOP).
77
COLUMN 14: TYPES of Patient
Put a check () mark on the household contact who initiated treatment based on the following types of patient as specified in the column.
New Smear
Positive
New Smear
Negative
Relapse
Treatment
Failure
Return After
Default
Other Positive
Other Negative
Trans-in
N.B.: Types of patient as defined on the MOP
Data source: NTP TB Register
COLUMN 15: Treatment Outcome
Write the date on the columns specific for the treatment outcome of the patient.
Cured Completed Died Failed Defaulted Transferred Out
05/31/2012
N.B: Treatment outcome of patient as defined on the MOP
Data source: NTP TB Register
COLUMN 16: Treatment Partner
Write the full name (family name first in bold capital letters, followed by given or first name and middle Initial) of the treatment partner
responsible for DOTS to the diagnosed TB patient.
Example: LUPONG, Rona S. / CHV
FRIAS, Teddy F. / Nurse
COLUMN 17: Remarks
Any observation / comment made by HCWs that needs attention. You can also indicate reason/s that arise/s , course of treatment and its
outcome, and the date when the comment / action taken was noted. (Ex. 5/31/2012. Refused to go to DOTS Facility, Did not submit second
78
Annex 11: CHVs Contact Investigation Tool
Name of referring facility: ______________________________
(Month) ________ (Year) _________
Submitted By:
_________________________
(Name of CHW/ BHW
No.
(1)
Name of
Patient
(2)
Address
(3)
Name of
Contacts
(4)
Age
(5)
Sex
(6)
Date of Visited in the
community
(7)
Name of requesting
Health Facility
(8)
Date referred
(9)
TB screening No./TB
Symptomatic Serial No.
(10)
Remarks
(11)
79
HOW TO ACCOMPLISH THE CHVS CONTACT INVESTIGATION TOOL
UPPER MIDDLE PORTION:
Name of Referring Facility: Indicate the name of the referring facility
Month/ Year: Indicate the Month/Year the contact investigation was conducted
Note: COLUMNS 1-9 to be accomplished by the CHVs (assisted by the Nurses)
COLUMN 1- Case Number of patient
Write the last two digits of the current year and the patients case number
Example: 12- 010 (10
th
patient listed on the Contact Investigation Tool).
COLUMN 2- Name of Patient
Write the patients full name (family name first in bold capital letters, followed by given or first name)
Example: Corona, Ana
COLUMN 3- Address
Write the patients complete address, including nearest landmark (if available), to easily locate the patient.
Example:
a. CENTRAL AVENUE . Blk 8 Lot 1 QC Ville Subdivision, Quezon City (Aqua soft water refilling station, across)
Indicate also the Barangay/Zone Number
Write the Name of the Barangay or the Number of the Bgy where the patient resides.
Example:
Bgy /Zone Bgy/Zone
Central 95 /8
COLUMN 4- Name of Contacts
List all the names of the household contacts (Adult/children) with or without symptoms.
COLUMN 5- Ages
Write the patients age in years.
Example: 36 y/o
COLUMN 6- Sex
Patients gender (M for male and F for female)
COLUMN 7- Name of Requesting Health Facility
Indicate the name of the Health facility that requested for the referring facility to list /validate the names of household contacts of the index
patient.
COLUMN 8- Date of Follow-up visit in the Community
Write the date of actual follow-up visit of the CHV to the house of the index patient.
COLUMN 9- Date Referred back to the Health Facility
Write the date when the household contacts of the index patient were referred back to the DOTS Facility. (Month/Day/Year)
COLUMNS TO BE UPDATED BY THE NURSES:
COLUMN 10- TB Screening No./TB Symptomatic Serial No.
Indicate the screening number/TB Symptomatic Serial number of patients where appropriate.
COLUMN 11- Remarks
This refers to any actions taken on the patients behalf. Any observation or comment made by CHVs or HCWs that needs attention. This
column can be utilized by both the CHVs and HCWs. You can also indicate reason/s that arise/s from the time of referral, course of treatment
and outcome of treatment. (Ex. Refused to go to DOTS Facility Did not submit second sputum specimen).
Write the date and action taken: ex. 5/29/2012- pt. refused to go to DOTS Facility.
80
Annex 12: MDR TB SUSPECT MASTERLIST
Name of Health Center/District:_________________ Quarter/ Year: ____________
No.
NAME
(1)
AGE
/
SEX
(2)
ADDRESS
(3)
BGY
/
FAM #
(4)
TYPE OF
PATIENT*
(USE
CODE)
(5)
REFERRED
(YES-WRITE
DATE
NO-WRITE
REASON)
(6)
Name of Treatment
Center/ Satellite
Treatment Center
Referred to
(7)
DATE
SCREENED
AT TX
CENTER
(8)
RECOMMENDATION/ DATE INITIATED TX
(9)
REMARKS/
Treatment
Outcome/ Date
(10)
Start CAT
II
Regimen
Mod CAT
II
Start SR For CAT
IV
*Type of Patient: 1 Category I Failure 5 Return After Default (RAD) 7 Non-Converter of Category II
2 Category II Failure 6 Other 8 Symptomatic Contact of a suspected/confirmed MDR-TB patient
3 Category I Relapse 6.1 Non-DOTS 9 HIV Patient
4 Category II Relapse 6.2 Other (+) 10 MDR-TB/ DR-TB Patient (with DST result)
6.3 Other (-)
81
HOW TO ACCOMPLISH THE MDR-TB SUSPECT MASTERLIST
Upper Portion:
(1) Name of Health Center/District Ex. Vitas HC/District I
(2) Quarter/ Year The current quarter / year the patients were registered
COLUMN 1 Name of MDR Suspect Identified-
Write the patients full name (family name first in bold capital letters, followed by given or first name)
COLUMN 2 - Age/Sex of the MDR Suspect-
Indicate the age. For the gender or sex- Indicate M for Male and F for Female Ex- 38 y/o- F
COLUMN 3- Address of the MDR Suspect
Write the patients complete address, including nearest landmark (if available), to easily locate the patient.
Example: a. CENTRAL AVENUE . Blk 8 Lot 1 QC Ville Subdivision, Quezon City (Aqua soft water refilling station, across)
COLUMN 4- Bgy/ Family Number:
Write the Name of the Barangay or the Number of the Bgy where the patient resides.
Bgy /Zone (Quezon City) Bgy/Zone (Manila)
Central 95 /8
Write the Family Number (designated by Health Center for the current year).
COLUMN 5 Type of Patient
Refers to the Category status of the Patient (Refer to the List of type of Patient)
COLUMN 6 - Referred
If the MDR-TB Suspect was referred to Treatment Center- Write the date as: month/day/year
If the patient was not referred to the treatment center, indicate: the reason
COLUMN 7 Name of Treatment Center/Treatment Satellite-
Specify the Name of the Treatment Center or Treatment Satellite where you refer the MDR Suspect.
For Columns 8- 10- DOTS Facility shall update with the Treatment Center or Treatment Satellite
COLUMN 8 - Date Screened at Treatment Center-
Write the Month/Day/ Year the MDR Suspect was screened at the Treatment Center
COLUMN 9 - Recommendation/Date Initiated Treatment
Write the date the patient was initiated treatment on the columns specific for the recommendation provided by the consilium
COLUMN 10 Remarks any observation / comment made by HCWs that needs attention. You can also indicate reason/s that arise/s , course of
treatment and its outcome, and the date when the comment / action taken was noted. (Ex. 5/31/2012. Refused to go to DOTS Facility, Did
not submit second sputum specimen.
82
Annex 13: MDR- TB Decentralized Masterlist
Name of Health Facility/ District: _________________________ Year: _________________
Name
(1)
AGE/
SEX
(2)
ADDRESS
(3)
BRGY/
Fam #
(4)
DIAGNOSIS
(3)
Newly master listed
(NEW)/Carry-over
from last year (CO)
(6)
DATE PATIENT WAS
DECENTRALIZED
(7)
TREATMENT
CENTER/
SATELLITE TC
(8)
STATUS OF PATIENT
AT THE END OF THE
QUARTER*
(9)
TREATMENT
OUTCOME/DATE
(10)
Remarks
(11)
Q1
Q2
Q3
Q4
83
HOW TO ACCOMPLISH THE MASTERLIST OF DECENTRALIZED MDR-TB/DR-TB PATIENTS
UPPER PART
Name of Health Center/District: Write the name of the Health Center/District
Year: Write the current year
COLUMNS 1-11
COLUMN 1 - Name:
Write the full name (family name first in bold capital letters, followed by given or first name) of the patient decentralized at the DOTS facility
Example: CORONA, Ronaldo
COUMN 2 - Age/ sex:
Write the patients age in years and gender or sex Mfor Male and F for Female of the patient decentralized at the DOTS facility.
COLUMN 3- Address:
Write the patients complete address, including nearest landmark (if available), to easily locate the patient.
Example: a. CENTRAL AVENUE . Blk 8 Lot 1 QC Ville Subdivision, Quezon City (Aqua soft water refilling station, across)
COLUMN 4- Barangay/ Family Number:
Indicate the Bgy. No./Family Number (assigned by the HC for the current year)
COLUMN 5 - Diagnosis:
Write the diagnosis as indicated on the MDR TB/DR-TB Decentralized acknowledgment form
COLUMN 6 Newly masterlisted/ Carry over from last year:
Write New if the patient is newly masterlisted.
Write CO if the patient is carry-over from last year
COLUMN 7- Date patient was decentralized:
Write the date the patient was decentralized as specified on the MDR-TB/DR-TB Decentralized
Acknowledgement Form (Month/Date/Year)
COLUMN 8- Treatment Center/ Satellite Treatment Center:
Indicate the name of the treatment center and /or the Satellite Treatment Center who referred the MDR-TB/DR-TB patient to DOTS Facility (or
Treatment Site)
COLUMN 9- Status of Patient at the end of the quarter:
Use the code below in updating this column as follows:
A- Patient still on Treatment
B- Patient referred back to TC/STC
C- Patient lost to follow-up
D- Others
E-
COLUMN 10 Treatment Outcome/ Date:
Write the Outcome (based on the standard definition on the PMDT Manual of Procedure) and Date of Treatment.
Example: Month/Day/Year
COLUMN 11- Remarks:
Remarks- This refers to any actions taken on the patients behalf. Any observation or comment made by HCWs that needs attention. Indicate
remarks where appropriate.
Write the date and action taken: ex. 5/29/2012- Patient refused to take medicine.
84
Annex 14: TB HIV Masterlist
Reference
No
(1)
Date
of
Registr
ation
(2)
H4
Cod
e
No.
(3)
Alias
(4)
Name of Patient
(5)
Complete
Address
(6)
Age
(7)
Sex
(8)
SACCL Code
and Date
Confirmed
with HIV
(9)
Date
Referred
to NTP
(10)
S/Sx 1)cough
2)fever, 3)wt.
loss 4)night
sweats
(11)
Date/Result of Diagnostic Test (12)
CD4
Count/
Date
(13)
DSSM Gene
Expert/MDR
Cult
ure
DST Radiogr
aphic
Exams
No.
Confirmed
with HIV
No. of TB
Symptomatics
Referred to
NTP
No. of TB
Symptom
atics with
DSSM
No. of
Symptomatic
s with other
Bacteriologic
Exam
Total No.
of TB Cases
Diagnosed
TB Cases Diagnosed
Total No. of
TB Cases
Initiated Tx
Pulmonary
EP
New (N) Relapse Trans-in Tx Failure RAD Other
(N+) (N-) (R) (TI) (TF) (RAD) (O-) (O+)
No. by
Type
Initiated
Treatment
*left portion of the Masterlist
*bottom portion of the Masterlist (summary table)
85
w/
ARV
(Y/N)
(14)
Date
Started
ARV
Regimen
(15)
TBDC
Decision
w/ Date
(16)
TB Case
(Y/N) If Y,
Case No.
(17)
Class.
(P/EP)
(18)
FNAB
(Y/N)
(19)
Type
(N/R/TI/TF/
RAD/O)
(20)
Cat.
(I/II/III/IV)
(21)
Date
Initiated
(22)
Anti-TB
Regimen
(23)
Name
of Tx
Center
(24)
Treatment Outcome
(with Date)
(25)
Remarks
(26) Cured Comp Died Failed Default Transout
Type of Patient Treatment Outcome
New Smear
Positive
Cured Completed Died Failed Default Transout
New Smear
Negative
Relapse
Treatment Failure
Return After
Default
Other Positive
Other Negative
*right portion of the Masterlist
*bottom portion of the Masterlist (summary table)
86
HOW TO ACCOMPLISH THE TB HIV MASTERLIST
Columns:
COLUMN 1: Reference Number
Write the reference number of the patient indicated on the referral slip of TB Center
Example: Patient 1: 13-001
Patient 2: 13-002
COLUMN 2: Date of Registration
Write the exact date when the patient registered on the TB HIV Masterlist.
Example: 5/20/13
COLUMN 3: H4 Code No.
Write the H4 Code based on the time patient was registered in masterlist of HIV center
old patient : those registered before 2012
new patient: those registered from 2013
Example: Patient 1: 11-001
Patient 2: 12-056
COLUMN 4: Alias
Write the Alias name as preferred by the patient.
COLUMN 5: Name of Patient
Write the full name (family name first in bold capital letters, followed by given or first name and middle Initial.)
Example: LAUREATA, Bangs L.
COLUMN 6: Complete Address
Write the complete address of the registered patient, including nearest landmark (if available), to easily locate.
Example: a. CENTRAL AVENUE . Blk 8 Lot 1 QC Ville Subdivision, Quezon City (Aqua soft water refilling station, across)
COLUMN 7: Age
Write the age in years of the registered patient.
Example: 36 y/o
COLUMN 8: Sex
Write the gender of the registered patient (M for male and F for female)
Column 9: SACCL (or SLH NRL) Code and Date Confirmed with HIV
Write the date when the patient was confirmed with HIV and the SACCL code of the patient from SLH National Reference Laboratory.
COLUMN 10: Date referred to NTP (or TB Center)
Write the date when the patient referred to TB Center with Proper referral.
COLUMN 11: Signs /symptoms 1) cough, 2) fever, 3) wt. loss, 4) night sweats
Write the number indicated above for the signs and /symptoms of the patient
Example: 1, means cough, 3 means weight loss
87
COLUMN 12: Date/Result of Diagnostic Test
Write the result of the examination over the date where appropriate
Example
DSSM Gene Expert Culture DST Radiographic
Examination
2+ MTB
Positive
RIF
Susceptible
(0) Susceptible
1/24/2012 2/29/2012 3/21/2012 6/20/2012 1/25/2012
COLUMN 13: CD4 Count/Date
Record the CD4 Count of the patient and date
Example:
COLUMN 14: w/ ARV (Y/N)
Write Y, if the patient is taking Anti Retroviral Drug ( ARV ) and N, if without ARV
COLUMN 15: Date started ARV Regimen
Write the date when the patient started for ARV Regimen
COLUMN 16: TB Diagnostic Committee ( TBDC ) decision with Date
Write the result and the date of TBDC as indicated on the TBDC Form.
Example: Anti-TB treatment
5/23/13
COLUMN 17: TB Case (Y/N), If Y, Case No.
Write Y and record the TB Case Number of the patient diagnosed as TB. and
N, if not diagnosed with TB.
COLUMN 18: Classification (P/EP)
Write P for Pulmonary TB and EP for Extra Pulmonary TB as defined on the Manual of Procedures (MOP).
COLUMN 19: Fine Needle Aspiration Biopsy (FNAB) (Y/N)
Write Y, if the patient underwent FNAB and N, if not
COLUMN 20: Type (N/R/TI/TF/RAD/O)
Write the type (code) of the TB patient initiated to treatment
a. New Patient (N)
New Smear Positive
New Smear Negative
b. Relapse ( R)
c. Treatment Failure ( TF )
d. Other Positive ( O+)
e. Other Negative ( O-)
f. Transfer In ( TI )
N.B.: Types of patient as defined on the MOP
COLUMN 21: Cat. (I/II/III/IV) Write the prescribed treatment regimen by Category Write I- for Category I
Write II- for Category II
Write III- for Category III
Write IV- for confirmed MDR-TB
COLUMN 22: Date Treatment Initiated
Write the date when the patient started for treatment on TB.
88
COLUMN 23: Anti-TB REGIMEN
Record the treatment regimen based on the following code
Example: R: Rifampicin, H: Isoniazid, E : Ethambutol, Z: Pyrazinamide
COLUMN 24: Name of Treatment Center
Write the name of the treatment center where the patient referred for MDR Screening
Example: PTSI KASAKA, SLH PMDT Center and others
COLUMN 25: Treatment Outcome (with date)
Write the date on the columns specific for the treatment outcome of the patient.
Cured Completed Died Failed Defaulted Transferred Out
12/31/2012
COLUMN 26: Remarks
This refers to any actions taken on the patients behalf. Any observation or comment made by HCWs that needs attention. Indicate remarks
where appropriate.
Write the date and action taken: ex. 5/29/2012- Patient refused to take medicines
89
Annex 15: Sample Project Indicators
Summary description of Indicators:
INDICATOR
DEFINITION
FORMULA
FREQUENCY OF
DATA COLLECTION
SOURCE
PROPOSED TARGET
1.Number of TB
symptomatic identified
is increased by 10% in
2013
Those with two
weeks cough
examined under
Direct Sputum
Smear Microscopy
(DSSM)
No. of TB
symptomatic
examined 2011
minus 2013
No. of TB
symptomatic 2011
X 100
Quarterly
Laboratory Register
No. of TB
Symptomatic
Tondo: 4852
Payatas: 2413
2. No. of referrals is
increased with
acceptance rate of 55%
About 55% of the
TB symptomatic
referred by CHVs(
referring facilities)
to DOTS facilities
were able to seek
consult at the
DOTS Facilities
No. of TB
Symptomatic who
seek consult at the
DOTS Facilities
No. of TB
Symptomatic
Referred by CHVs to
DOTS facilities
X 100
Quarterly CHV Referral
Masterlist
and
NTP Referral Form
Referral Acceptance
Rate: 55%
3. Completion Rate of
INH Preventive Therapy
is at least 80% in 2013
No. of 0-4 years
old initiated on
IPT who
completed
treatment
No. 0-4 yrs old who
completed
treatment on IPT
No. who initiated
treatment on IPT
x 100
Quarterly IPT Register Completion Rate of
80%
4. Treatment Success
Rate of New Smear
Positive is 90% with Low
defaulter Rate (i.e.
below 5%)
The combination
of cured and
completed
treatment among
New Smear
Positive is 90%
Cured + Treatment
Completed among
New Smear Positive
cases
Total New Smear
Positive Cases
Initiated Treatment
x 100
Quarterly TB Register At least 90 %
5.No. of referred
retreatment TB patients
or MDR suspects who
access the treatment
center is at least 90%
Number of MDR
suspects
identified by the
DOTS Facility who
were screened
(access) at the
Treatment Center.
Number of MDR
suspects who access
the treatment center
Total number
registered on MDR
Suspect Masterlist /
referred to
treatment center
x 100
Quarterly MDR Suspect
Masterlist
90% of those listed
on MDR Suspect
Masterlist were able
to access and
undergo culture and
DST
90
Indicator 1: No. of TB symptomatics identified is increased by 10 % in 2013 (Baseline 2011) Achieve or not?
6. Guideline about TB
screening and IPT for
PLHIV at SLH is
developed
Operational
guideline for TB
and HIV was
developed by
RJPI together
with TB and HIV
experts of SLH
Drafted in 2012.
Finalized and
endorsed in 2013.
Printed out in
2014.
7.Facilities
implementing
infection control
policy of DOH
achieved at least 50%
per level of infection
control
Four levels of
TBIC such as
Managerial,
Administrative,
Environmental
and Respiratory
Controls are
being monitored
with specific
health practice
parameters
based on the
DOH Guidelines
No. of health
practices
performed/
standard
parameter for
each level of
infection control X
100
2011: The TBIC
monitoring
checklist was
develop by RJPI
based on the WHO
Infection Control
Guidelines (3 levels
of Infection
Control) and
incorporated on
the NTP
monitoring tool
2012: TBIC
monitoring
checklist was
revised based on
the NTP Guidelines
on TB and Other
Airborne Infectious
Diseases. This
covers four (4)
levels on TBIC
namely:
managerial,
administrative,
environmental and
respiratory
controls.
Health Facility
TB Symptomatic
2008 2009 2010 2011 2012
LGU 2242 2386 2765 3275 3726
NGO 597 804 834 1136 881
Tondo 2839 3190 3599 4411 4607
91
There was a 60% increase in the number of TB symptomatic from 2008 to 2012 (from 4363 to 6998). The contribution of the NGO DOTS also
increased from 25% in 2007 to 30% in 2012. The participation of the NGOs in case finding activities was able to accelerate the service points in
the community.
Indicator 2. Number of referrals is increased with the acceptance rate of 55%
The 2010 and 2012 data showed, the actual number of TB symptomatic referred decreased from 357 to 347; the Access Rates to DOTS
Facilities significantly improved from 53% to 61% (p=0.03); and Examination Yield improved significantly from 40% to 60% (p < 0.01). The CHVs
were able to bridge the gap between the community and DOTS facility.
Indicator 3. Completion Rate of INH Preventive Therapy is at least 80%
The IPT Completion Rate in 2010 and 2011 was 90% and 92% in District I, Tondo. In Payatas, this was at 100% from 2010 to 2012.
LGU 1046 962 949 925 1179
NGO 478 736 803 1266 1212
Payatas 1524 1698 1752 2191 2391
No. of TB Symptomatics
Identified
No. Referred to DOTS
Facility
No. Accessed to DOTS Facility Access Rate
2010 2011 2012 2010 2011 2012 2010 2011 2012 2010 2011 2012
Tondo 344 390 314 315 354 274 162 190 165 51 54 60
Payatas 42 97 73 42 97 73 26 52 46 62 54 63
Total 386 487 387 357 451 347 188 242 211 53 54 61
Health Facilities IPT Completion Rate
2010 2011
GO 85.8% (97/113) 88.3 % (151/171)
NGO 95.9% (70/73) 97.8% (92/94)
Tondo 89.7 % (167/ 186) 91. 6 % (243/265)
GO 100% (7/7) 100% (6/6)
NGO 100% (19/19) 100% (37/37)
Payatas 100 % (26/26) 100% (43/43)
92
Indicator 4: Treatment Success Rate of New Smear Positive PTB patient is 90% with low Defaulter Rate (i.e. below 5%)
The treatment success rate of new smear positive pulmonary tuberculosis cases was maintained in District I- Tondo at 84.2 % in 2008 and at
84.4% in 2011 (p=0.47). Although this decreased in Payatas from 90% in 2008 to 88% in 2011, this was not statistically significant (p=0.16).
This is being closely monitored by RJPI.
Indicator 5: No. of referred retreatment TB patients who access the treatment center is at least 90%.
In 2012, RJPI developed the Multi-Drug Resistant (MDR)-TB Suspect Masterlist to record, track and analyze the MDR Suspect Referral
Pathway. Initial data showed the Access Rate to be at 92.3%. This could provide relevant data to NTP to enhance policy on Programmatic
Management of Drug Resistant TB (PMDT).
Health Facilities Treatment Success Rate (New Smear Positive) Defaulter Rate (New Smear Positive)
2008 2009 2010 2011 2008 2009 2010 2011
GO 79.9
(299/374)
85
(345/406)
86
(386/449)
81.7
(379/464)
10.4
(39/374)
6.4
(26/406)
6 (27/449) 6.7
(31/464)
NGO 94.7
(144/152)
89.3
(151/169)
96.8
(150/155)
92.4
(145/157)
0.7
(1/152)
3.6
(6/169)
1.9
(3/155)
1.3
(2/157)
Tondo 84.2
(443/526)
86.3
(496/575)
89
(536/604)
84.4
(524/621)
7.6
(40/526)
5.6
(32/575)
5 (30/604) 5.3
(33/621)
GO
88 (66/75) 85.3
(93/109)
92.3
(108/117)
92.1
(93/101)
2.7 (2/75) 10.1
(11/109)
1.7
(2/117)
4.0
(4/101)
NGO
93.5 (43/46) 80 (72/90) 83.7 (77/92) 83.2
(89/107)
0 (0/46) 8.9 (8/90) 7.6 (7/92) 3.7
(4/107)
Payatas
90.1
(109/121)
82.9
(165/199)
88.5
(185/209)
87.5
(182/208)
1.7
(2/121)
9.5
(19/199)
4.3
(9/209)
3.8(8/208)
Project Site Health Facilities Indicator 2010 2011 2012
Tondo
GO
referred 95 190 218
screened 94 187 197
confirmed 8 29 19
NGO
referred 55 59 61
screened *58 59 61
confirmed 3 4 3
Payatas
GO
referred 51 48 43
screened 51 48 41
confirmed 0 3 2
NGO
referred 14 44 42
screened 14 44 37
confirmed 2 5 4
Access Rate (screened/ referred) 99.5%(214/215) 99.1% (338/341) 92.3% (336/364)
93
Indicator no. 6: San Lazaro Hospital (SLH)
TB screening among People Living with HIV (PLHIV) is provided and mechanisms for newly diagnosed HIV+/TB patients at San
Lazaro Hospital (SLH) are in place
Guideline about TB screening and IPT for PLHIV at SLH is made
The SLH draft guideline was developed in 2012. San Lazaro Hospital will revise the draft guideline based on the national
guideline. National guideline on TB/HIV will be released within this year.
No. of TB patients identified by TB screening among HIV positive patient is available
No. of HIV positive patients with IPT and IPT completed PLHIV is available
The RJPI facilitated the development Guidelines on the Collaborative Approach of TB/HIV Prevention and Control in San Lazaro Hospital and
strengthen the referral mechanism between the TB and HIV Centers.
Indicator 7: Facilities implementing Infection Control (IC) Policy of DOH achieved at least 50% per level of Infection Control
The TB Infection Control (TBIC) parameters were incorporated to the monitoring tool to document the health practices of HCWs. This could be
an important reference to improve policy on TBIC.
Indicator
*New (Jan-Dec 2012)
*Old (Before 2012)
Total
Patients screened for TB 468 65
533
Referred to TB ward 110 65
175
TB case (CAT1) 37 15
52
TB case (CAT2) 18 11
29
TB case (CAT3) 5 3
8
TB case (CAT4) 3 2
5
EPTB 2 2
4
IPT 1 2
3
Surveillance 18 20
38
Death 21 8
29
Trans out 1 2 3
LEVEL OF TB INFECTION CONTROL
Tondo
LGU(4/10)
Tondo
NGO(2/2) Payatas LGU(3/3) Payatas NGO(3/3)
Managerial Control 20% 40% 40% 40%
Administrative Control 40% 40% 20% 60%
Environmental Control 50% 67% 67% 83%
Personal Protective Equipment (PPE) 50% 75% 75% 100%
94
Annex 16: Monitoring Tools for Data Collection
NTP Monitoring Tool: The existing monitoring tool was enhanced for a more comprehensive monitoring and
evaluation program implementation. The recording forms are designed to collect additional information that is
specific to the project but may be relevant to analyze the current activities and interventions of the NTP. The said
tools are described below:
1. Laboratory Data Collection Forms:
a. Laboratory Case Finding Tool: This is covers the number of TB symptomatic examined, sputum
completely submitted and smear positive discovered. Count the said data on the Laboratory Register
and tick on this tool accordingly. The sputum for diagnosis and follow-up are written on this register.
b. Laboratory Checklist: This contains guide questions both on the operations and technical aspect of the
microscopy services. This looks at the effectiveness and efficiency of the medical technologists or
Microsopists including the quality of diagnostic services. Observe all the parameters indicated on the
sheet. Put a check on the Yes column if it meets the standard parameter for diagnostic services and
No if otherwise.
c. Laboratory Feedback Sheet: This sheet summarizes the gaps and recommended solutions observed
during the visit. It is written in narrative form and may be supported by statistics. Write all your findings,
interpretation of findings and actions taken on appropriate columns. The results/follow-up column will
be updated on the next visit to note status of previous recommendation.
2. TB in Children Data Collection Form:
a. Validation Sheet for IPT: This is a counting sheet to monitor the number of 0 - 4 years old initiated on
IPT. Use the IPT Register to count the needed data and tick on appropriate columns (i.e TB Exposure or
TB Infection). Write this information on the quarter being evaluated (i.e. 1
st
Quarter, 2
nd
Quarter, 3
rd
Quarter or 4
th
Quarter).
b. Validation Sheet for Children Screened: This comprises the children (0-14 years old) who were screened
for TB symptoms as walk in clients or household contacts of the Index TB Case. Use Masterlist A
to count those screened as walk-in and Masterlist B for the household contacts. Tick appropriately on
the quarter being evaluated, per indicator and age-group (0-4 y/o, 5-9 y/o and 10- 14 y/o).
c. Validation Sheet for IPT Outcome: This validates the treatment outcome of 0-4 years old initiated on IPT
for the past 12- 18 months. Use the IPT Register for the quarter or year being evaluated. Tick the
indicated treatment outcome (Completed, Defaulted, Died, Failed and Transferred Out) on the columns
provided on this sheet.
3. Case Holding: This form has four (4) parts: All TB Cases registered during the quarter per age- group,
Breakdown of New Pulmonary Smear Positive by Age and Sex, Treatment Regimen and the Summary of
Children with Extra Pulmonary TB (EPTB).
a. The first part covers the Pulmonary TB Cases per patient type and age-group including the Extra
Pulmonary TB (EPTB) Cases. The New Smear Negative column is further subdivided into groups: those
who underwent DSSM and Other Diagnostic Tests (ODT: i.e. TST or CXR) while the EPTB case is divided
into Less Severe and Severe. Tick per patient type and age-group.
95
b. The second part provides information on which gender and age-group are more infectious. Tick the New
Pulmonary Smear Positive initiated on treatment based on gender and age-group.
c. The third part comprises of treatment regimen provided. Tick on appropriate columns (Category I, II or
III).
d. The fourth part covers severity of EPTB among children (0-14 years old). Tick per age group and based
on severity of illness (Less Severe and Severe).
Use the TB Register for the quarter being evaluated and tick accordingly.
4. TB Cases Treatment Outcome: This is a counting sheet for the outcomes of all TB Cases initiated on
treatment for the past 12- 18 months. This form is divided per patient-type, age-group and treatment
outcome (cured, completed, defaulted, failed, died and transferred out). Tick accordingly. Use the TB
Register for the quarter or year being evaluated.
5. Contact Investigation: This tool provides a detailed account of the screening pathway of the Household
contacts of Index TB Case. The steps in the pathway are: TB symptom screening, diagnostic examination
done, diagnosis, initiation of IPT or Anti-TB Treatment and treatment outcome. Use the Masterlist B (for
LGUs) and Modified Masterlist B (for NGO DOTS). Tick accordingly.
6. Validation Sheet on TB Diagnostic Committee: The patient recommended for TBDC evaluation should be
counted on this form. Use the TBDC Masterlist for the quarter being evaluated. Tick on appropriate columns
based on age, recommendation of TBDC, whether active or inactive or other conditions (Other Lung Disease,
Repeat CXR, etc). The column for the active cases is further subdivided per category of treatment
(Category I, II, or III). Tick accordingly.
7. MDR TB Suspects Data Collection Form: All the retreatment TB patients or other patients classified as MDR
TB Suspect and referred to the treatment center for screening are counted on this form. This form comprises
the referral pathway of MDR-TB Suspect to the Treatment Center. The steps in the referral pathway are: (1)
identification of MDR TB Suspect; (2) Referral to Treatment Center; (3) Access of patient to the Treatment
Center; (4) Diagnostic Examination; (5) Diagnosis; and (6) Initiation of Treatment. The MDR-TB confirmed
cases started on treatment by the Treatment Center that were decentralized to continue medication at the
DOTS Facility are counted on this sheet. There are two (2) instances by which an MDR-TB patient can be
decentralized to DOTS Facility: (1) Identified /Referred by the Treatment Center and (2) Identified by the
DOTS Facility and referred back by the Treatment Center. The MDR TB treatment package is provided by the
Treatment Center for the whole course of treatment.
Use the MDR-TB Suspect Masterlist for this purpose. Tick accordingly.
8. TB Infection Control Monitoring Tool: This is a checklist to monitor the infection control practices by the
HCWs. This is divided into four (4) levels of infection control namely: managerial, administrative,
environmental and respiratory control. Ideal Infection Control (IC) practices are indicated per level of
infection control. Put a check on the Yes column if appropriate IC practices were carried out by the HCWs
and No if otherwise.
9. Logistics Monitoring Form: The actual count of available NTP medicines and supplies are reflected on this
sheet. Count all the medicines in the stock room and write the number of available medicine and expiry
dates accordingly. You can compare the actual count with their stock card.
96
10. NTP Data Quality Assurance Tool: This part is divided into three (3) parts: Data Validation and Interview of
HCWs and Patient.
a. Data Validation: This is checklist to verify data and assess its accuracy and completeness. The laboratory
register together with the TB Register and treatment card or other TB recording forms are cross-checked
to assess the accuracy and data completeness. Tick for the parameters done appropriately and
otherwise tick No.
b. Interview of HCW: This consists of series of questions to look into the quality of the current NTP
activities and interventions carried out by the HCWs. The assigned member of the monitoring team will
ask questions and document the responses of the HCW on this sheet. Validate the responses of the HCW
based on the existing data and observations. Reinforce the positive actions done and correct actions not
parallel to the NTP protocol.
c. Interview of Patient: This consists of list of questions for patients regarding his/her clinical course,
treatment regimen, perception on DOTS implementation and convenience of transportation going to the
DOTS facility. The assigned member of the monitoring team will ask questions and document the
responses of the patient on this sheet. Validate the responses of the patient based on the existing data
and observations. Reinforce the positive actions done and correct misconceptions on the health system
and NTP.
97
Laboratory Data Collection Forms
Laboratory Case Finding Tool
Name of Health Facility:________________
Date:________________
1. No. of TB Symptomatic examined
0-4 yrs old
5-9 yrs old
10-14 yrs.old
15yrs old and above
Total
2. No. of TB Symptomatic with 3 sputum specimen
0-4 yrs old
5-9 yrs old
10-14 yrs.old
15yrs old and above
Total
3. Three sputum collection rate
4. No. of Smear Positive Discovered
0-4 yrs old
5-9 yrs old
10-14 yrs.old
15yrs old and above
Total
5. Positivity Rate
6. No. of TB Symptomatic with doubtful result
0-4 yrs old
5-9 yrs old
10-14 yrs .old
15yrs old and above
Total
7. No. of TB Symptomatic as smear negative
0-4 yrs old
5-9 yrs old
10-14 yrs.old
15yrs old and above
Total
Treatment Follow up
8. No. of Follow up examinations done
0-4 yrs old
5-9 yrs old
10-14 yrs.old
15 yrs old and above
98
Laboratory Checklist
Name of Laboratory:__ ____________________ District: _________ Date: __________
Med. Tech: ______________________________
Lab Aides: ______________________________
SECTIONS
CHECKLISTS
Yes
No
OPERATIONAL
1) SOP
Is a Standard Operating Procedure manual present inside the Laboratory?
2)LABORATORY
SET UP
Is there a separate area for TB microscopy?
Are there separate tables for smear preparation and microscopy?
Is there a power supply available?
Ample water supply?
Does the laboratory area have adequate ventilation?
3)STAFFING Has all the staff received formal training in TB testing? (Proportion)
4)EQUIPMENT
Is the microscope in good working condition?
Is a spare bulb available in the laboratory?
5) LOGISTICS Does the laboratory have stocks of stains, slides etc.
6) LABORATORY
SAFETY
Does the laboratory use disinfectant recommended by the NTRL?
How are used sputum containers disposed of? Is it Disinfected? Autoclaved? Buried?
Burned?
TECHNICAL
1) SPECIMEN
COLLECTION
Are specimens collected outdoor?
Does the patient receive proper instruction from a nurse or Med-Tech before collection?
Is the specimen container properly labelled before collection?
Is the label located at the containers body, and not at the lid?
Is the specimen quality checked before being sent to the laboratory?
Is the sputum container used recommended by the NTRL?
Are samples forwarded to the laboratory as soon as possible after collection?
2) RECORDING AND
REPORTING
Do/es the Laboratory staff use the specified Laboratory request form and Laboratory
register?
Are the forms / register neat, legible and up to date?
3) MICROSCOPY
EQA
Are all smears approximately 3cm x2cm?
Are all stain solutions inside expiry date?
Is the carbol fuchsin stain heated and left in contact with the smear for at least 5 mins.?
Are positive slides used in accordance with the scale provided by the NTRL/WHO?
Are the completed slides stored in a box in the same sequence as the register?
Are the completed slides cleaned with xylene before storage?
Are the completed slides left standing up (dripping) to get rid of the oil?
Are all positive and negative smear slides chronologically stored in a storage box for
EQA?
Are the feedback sheets filed neatly?
COMMENT
99
Laboratory Feedback Sheet
Microscopy
Center :
___________ Month : ____________ Year : ___________
Findings
Interpretation
ACTIONS TAKEN
RESULTS/FOLLOW - UP
100
TB in Children Data Collection Form
Validation Sheet for IPT
Children 0-4 yrs. OLD for IPT
1Q
2Q
3Q
4Q
TOTAL
1. TB Exposure
2. TB Infection
TOTAL
101
Validation Sheet for Children Screened
Name of Health Facility: __________________________
Source of data: Masterlist A and Masterlist B
Screening Activities
1Q On
IPT
TB
Disease
2Q On
IPT
TB
Disease
3Q On
IPT
TB
Disease
4Q On IPT TB
Disease
TOTAL Total
On IPT
Total TB
Disease
1. Total Number of children 0-14 yrs. Old listed in
Masterlist A
a. No. of TB Symptomatic children 0-4 yrs old
b. No. of TB Symptomatic children 5-9 yrs old
c. No. of TB Symptomatic children 10-14 yrs old
2. Total number of children 0-14 yrs old listed in
Masterlist B
2.1 Total number of child contacts 0-14 yrs
evaluated
a. No of children 0-4 yrs old
b. No. of TB Symptomatic children 5-9 yrs old
c. No. of TB Symptomatic children 10-14 yrs old.
TOTAL NUMBER OF CHILDREN SCREENED
102
Validation Sheet for IPT Outcome
TB Exposure
Total Number of
Patient Initiated to
Treatment
Completed
IPT % Defaulted % Died % IPT Failed %
Trans-
out %
Total No.
Evaluated
Health Facilities
TB Infection
Total Number of
Patient Initiated to
Treatment
Completed
IPT % Defaulted % Died % IPT Failed %
Trans-
out %
Total No.
Evaluated
Health Facilities
103
Case Holding
QUARTERLY REPORT ON ALL TB CASES
Name of DOTS Facility:_______________________ ____Quarter of the Year__________
A. All TB Cases registered during the quarter by Age-Group:
0-4 years old
TYPES OF
PATIENTS
New Sm(+)
(1)
Relapse
(2)
Trans-in
(3)
RAD
(4)
Treatment
Failure
(5)
Other
(6)
Reported as New Smear
Negative
(7)
EPTB
(8)
Positive Negative New Sm (-) ODT Less Severe Severe
M F M F M F M F M F M F M F M F M F M F M F
Public
Private
SUBTOTAL
104
5-9 YEARS OLD
TYPES OF
PATIENTS
New Sm(+)
(1)
Relapse
(2)
Trans-in
(3)
RAD
(4)
Treatment
Failure
(5)
Other
(6)
Reported as New Smear
Negative
(7)
EPTB
(8)
Positive Negative New Sm (-) ODT Less Severe Severe
M F M F M F M F M F M F M F M F M F M F M F
Public
Private
SUBTOTAL
10-14 YEARS OLD
TYPES OF
PATIENTS
New Sm(+)
(1)
Relapse
(2)
Trans-in
(3)
RAD
(4)
Treatment
Failure
(5)
Other
(6)
Reported as New Smear
Negative
(7)
EPTB
(8)
Positive Negative New Sm (-) ODT Less Severe Severe
M F M F M F M F M F M F M F M F M F M F M F
Public
Private
SUBTOTAL
15 YEARS OLD
TYPES OF PATIENTS New Sm(+)
(1)
Relapse
(2)
Trans-in
(3)
RAD
(4)
Treatment
Failure
(5)
Other
(6)
Reported as New Smear
Negative
(7)
EPTB
(8)
Positive Negative New Sm (-) ODT Less Severe Severe
M F M F M F M F M F M F M F M F M F M F M F
Public
Private
SUBTOTAL
105
B. Breakdown of New Pulmonary Smear-Positive by Age and Sex
C. Treatment Regimen Given
D. Summary of Children with Extra pulmonary TB:
Source of Data: TB Register
0-4 5-9 10-14 15 y/o TOTAL
M F M F M F M F M F TOTAL
Cat I Cat II Cat III
Cases Initiated Treatment
Age-Group
Extrapulmonary TB
Less Severe Severe
0-4 yrs
5-9 yrs
10-14 yrs
Total
106
TB Cases Treatment Outcome
NAME OF CHD: ____________ QUARTER: 1ST 2ND DATE:
NAME OF PHO/CHO:
3RD 4TH
NAME OF DOTS FAC: YEAR:
PREPARED BY:
Total Number of Pulmonary TB
cases (Copy the total # reported
in the Casefinding report during
the same quarter)
Cured
Completed
Treatment
Died Failed Defaulted Transout Total
1. New Cases
1.1 Smear (+)
a. 0-4
b. 5-9
c. 10-14
d. 15 above
Total
1.2 Smear (-)
a.0-4
b. 5-9
c. 10-14
d. 15 above
Total
1.3 ODT
a. 0-4
b. 5-9
c. 10-14
Total
2. Retreatment
2.1 Relapse
2.2 Tx Failure
2.3 RAD
2.4. Others
2.4.1 Other (+)
a. 0-4
b. 5-9
c. 10-14
d. 15 above
Total
2.4.2 Other (-)
a. 0-4
b. 5-9
c. 10-14
d. 15 above
Total
4. Trans-in
5. EPTB
Grand Total
107
Contact Investigation
Smear Positive Smear Negative
1. No. Index Case
2. Total No. of Contacts
2.1 ( 0-4 y/o)
2.2 (5-9 y/o )
2. 3 (10-14 y/o)
2. 4 (15 y/o and above )
3. No. Evaluated
3.1 ( 0-4 y/o)
3.2 (5-9 y/o )
3.3 (10-14 y/o)
3.4 (15 y/o and above )
4. Reasons why Patients are "Not Evaluated"
4. 1 HCWs' understanding is that the patients should go to the health facility for evaluation
4. 2 Patient refused to go the DOTS Facility
4.3 Patient used fictitious address
4.4 conflict schedule
5. SIGNS AND SYMPTOMS
5.1 No signs and symptoms
5. 2 W/ only 1 clinical S/S
5. 3 W/ 2 Clinical S/S
5. 4 W/ 3 Clinical S/S
5. 5 W/ > 3 Clinical S/S
6. No. Classified as TB Symptomatics
6.1. Reasons for the classification as TB Symptomatic
a. Met the 3 out of 6 Criteria (9 Y/o and below)
b. Cough of two weeks or more (10 y/o and above)
c. Based on the clinical judgment of the medical officer
d. Others: pls specify /enumerate :
7. No. classified as "Not TB Symptomatic"
8. Diagnostic Procedures:
8. 1 Total No. Examined by DSSM
8.1.1 Total No. w/ Less than 2 sputum specimen
a. Refused to complete
a.1 Interventions
a.2 Result of Intervention
b. No money to pay the transportation
b.1 Interventions
b.2 Result of Intervention
c. Long waiting time at the DOTS facility
c.1 Interventions
c.2 Result of Intervention
d. No CHV companion to go to the DOTS facility
d.1 Interventions
d.2 Result of Intervention
e. Others :( pls. specify and enumerate )
e.1 Interventions
e.2 Result of Intervention
8.1.2 Total no. W/ 2 sputum specimen
8.2 Total No. who underwent CXR
8.2.1 Total No. of Patient came in with CXR Result
a. 0-4 y/o
b. 5-9 y/o
c. 10-1 4 y/o
d. 15 y/o and above
8.2.2 Total No. of Patient requested by MD for CXR
a. 0-4 y/o
b. 5-9 y/o
c. 10-1 4 y/o
d. 15 y/o and above
8.2.3 Total No. of Patient requested by MD for CXR and done
a. 0-4 y/o
b. 5-9 y/o
c. 10-1 4 y/o
d. 15 y/o and above
108
Smear Positive Smear Negative
8. 3 Tuberculin Skin Testing
8.3.1 No. of TST administered
a. 0-4 y/o
b. 5-9 y/o
8.3.2 No. of TST requested but not done
a. 0-4 y/o
b. 5-9 y/o
8.3.3 No. of TST administered and read
a. 0-4 y/o
b. 5-9 y/o
9. Results
9.1 Bacillary Status (a + c=9.1.2)
a. No. of Smear ( + ) cases
b. Positivity Rate
c. No. of Smear ( - ) Cases
9. 2 CXR (9.2.1-9.2.3)
9.2.1 Total No. of cases submitted to TBDC
i. 0-4 y/o
II. 5-9 y/o
III. 10-14 y/o
IV. 15 y/o and above
9.2. 2 W/ TBDC recommendation
I. Active
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
II. Inactive
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
III. Other Lung Disease
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
IV. Total W/ Other recommendations (Please specify/enumerate on separate sheet )
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
9. 3 No. of TST performed
9.3.1 No. of ( + ) cases
a. 0-4 y/o
b. 5-9 y/o
9.3.2 No. of ( - ) cases
a. 0-4 y/o
b. 5-9 y/o
9.3.3 Not read
10. CASE HOLDING
10.1 TB Exposure
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
10.2 TB Infection
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
10.3 Total No. of TB Disease
10.3.1 Total No. of Pulmonary Cases
I. No. New Smear ( + ) Cases
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
109
Smear Positive Smear Negative
d. 15 y/o and above
II. No. of New Smear ( - ) Cases
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
III. No. of Relapse Cases
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
IV. No. of Treatment Failure Cases
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
IV. No. of RAD Cases
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
V. No. of Other ( + ) Cases
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
VI. No. of Other ( - ) Cases
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
VII. No. of Transferred - In Cases
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
10.3.2 Total No. of Extra Pulmonary TB Disease
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
11. Treatment
11.1 IPT
a. No. Recommended for IPT
b. No. Initiated Treatment
c. Not Initiated
c. 1 REASONS
c.1.1 No INH
c.1.2 Refused treatment
c.1.3 Not requested by MD
c..1.4 Not aware of the protocol (specify who)
c..1.5 Others (Pls. specify /separate sheet)
11.2 Anti- TB Treatment
a. Recommended for Treatment
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
b. No. Initiated Treatment
a. 0-4 y/o
b. 5-9 y/o
c. 10-14 y/o
d. 15 y/o and above
c. Not Initiated
c. 1 REASONS
c.1.1 No Anti-TB Drug
c.1.2 Refused treatment
c.1.3 Not requested by MD
c..1.4 Not aware of the protocol (specify who)
110
c..1.5 Others (Pls. specify /separate sheet)
12. Total No. w/ Treatment Partners (12.2 letter B)
a. HCW
b. BHW
c. CHV
d. Parent/Guardian
13.Treatment Outcome _____ Qtr _____Year
13.1 IPT
a. Treatment Completed
b. Died
c. Failed
d. Defaulted
d.1 Went home to province without prior notice
d. 2 No companion to go to the DOTS facility
d. 3 Due to allergic reactions
d. 4 Refused to complete the treatment
e. Transferred- Out
13.2 Anti- TB Treatment
13. 2. 1 Total No. of New Smear ( + ) Cases
a. Cured
b. Treatment Completed
c. Died
d. Failed
e. Defaulted
e.1 Went home to province without prior notice
e. 2 No companion to go to the DOTS facility
e. 3 Due to allergic reactions
e. 4 Refused to complete the treatment
f. Transferred- Out
Reasons: Please specify
13.2.2 Total No. New Smear ( - ) Cases
a. Treatment Completed
b. Died
c. Failed
d . Defaulted
d.1 Went home to province without prior notice
d. 2 No companion to go to the DOTS facility
d. 3 Due to allergic reactions
d. 4 Refused to complete the treatment
e. Transferred- Out
13.2.3 Total No. of Relapse Cases Initiated Treatment
a. Cured
b. Treatment Completed
c. Died
d. Failed
e. Defaulted
e.1 Went home to province without prior notice
e. 2 No companion to go to the DOTS facility
e. 3 Due to allergic reactions
e. 4 Refused to complete the treatment
f. Transferred- Out
13. 2. 4 Total No. of Treatment Failure Cases
(Treatment Outcome Category as applied in 14.2.1 )
13.2. 5 Total No. Return After Default Cases Initiated Treatment (Treatment Outcome Category as
applied in 14.2.1)
13.2.6 Total No. of Other ( + ) Cases Initiated Treatment (Treatment Outcome Category as applied
in 14.2.1 )
13.2.7 Total No. of Other ( - ) cases initiated Treatment (Treatment Outcome Category as applied
in 14.2.2)
111
Validation Sheet on TB Diagnostic Committee
Health Facility:__________________ Date:_______________________ Qtr ______ Year: ______
Prepared by:_____________
AGE-GROUP Legend TREATMENT REGIMEN RECOMMENDED BY TBDC Inactive Other Lung Disease Rpt X-ray Reason Normal
CXR
Others
I III Total New II Grand Total
0-4
Recomme
nded for
Treatment
Initiated
Treatment
(Double Tick)
5-9
Recomme
nded for
Treatment
Initiated
Treatment
(Double Tick)
10-14
Recomme
nded for
Treatment
Initiated
Treatment
(Double Tick)
15 and
above
Recomme
nded for
Treatment
Initiated
Treatment
(Double Tick)
112
MDR TB Suspects Data Collection Form
RESEARCH INSTITUTE OF TUBERCULOSIS/ JAPAN ANTI TUBERCULOSIS ASSOCIATION, PHILIPPINES
MONITORING TOOL
Name of Facility:
A. No. of MDR Suspects
Registered
0-4 yrs old
5-9 yrs old
10-14 yrs old
15 yrs old and above
Total
Referred
0-4 yrs old
5-9 yrs old
10-14 yrs old
15 yrs old and above
Total
Screened
0-4 yrs old
5-9 yrs old
10-14 yrs old
15 yrs old and above
Total
Confirmed
0-4 yrs old
5-9 yrs old
10-14 yrs old
15 yrs old and above
Total
Initiated Treatment
0-4 yrs old
5-9 yrs old
10-14 yrs old
15 yrs old and above
Total
Decentralized (Identified from the HC)
0-4 yrs old
5-9 yrs old
10-14 yrs old
15 yrs old and above
Total
Decentralized (Patients from Treatment Centers)
0-4 yrs old
5-9 yrs old
10-14 yrs old
15 yrs old and above
Total
113
TB Infection Control Monitoring Tool
Levels of Infection Control
YES NO REMARKS
Total
Total
Total
TB INFECTION CONTROL
1. Managerial Control
a. TB Infection Control guidelines/updates discussed within the quarter
b. Any person in-charge to discuss the guidelines?
c. TB Infection Control Training conducted annually among HCWs
d. Proper disposal of sputum cups, applicator sticks, masks etc.
e. Conduct of regular health education on TB infection Control in health facility (pre-clinic lectures , etc.)
CONSOLIDATED
2. Administrative Control
a. Annual Health-screening conducted among HCWs?
b. HCWs separates patients with cough from other patients
c. Any particular schedule for sputum collection?
d. Any particular schedule for TB patients' drug collection?
e. Signage for cough etiquette/standard precaution
CONSOLIDATED
3. Environmental Control
a. HCWs talk to patients in a well ventilated area/room
b. Utilize uni-directional airflow (ex. improvised mechanical ventilation- Electric fan directed at air exhaust
points - windows /doors)
c. Use of short curtains rather than long ones (short curtains allow good ventilation (natural ventilation) better
than the ones utilizing long curtains thus diluting droplet nuclei)
d. Conduct sputum collection/induction in a well ventilated area
e. Is there any one in-charge of monitoring
f. Is there any responsible person for cleaning the windows, lab equipment etc?
CONSOLIDATED
4. Personal Protective Equipment (PPE)
a. HCWs use N-95 mask, surgical masks or ordinary masks
b. Patients use surgical mask/cloth masks
c. Hand hygiene after caring for patients
d. HCWs instruct TB patients about cough Etiquette/Respiratory Hygiene
CONSOLIDATED
OVERALL
114
Logistics Monitoring Form
Summary
Health Facilities/ Date
Stock Card
Sputum cups
reagent
applicator stick
glass slides
disinfectant
gloves(pairs)
surgical masks
N95 masks
Cat I/ Kit
Cat Kit
FDC-A
FDC-B
Isoniazid(tab)
Rifampicin(tab)
Pyrazinamide (tab)
Ethambutol(tab)
Streptomycin(vial)
Gauge 23 needle/syringe
TB KIDS Kit
Isoniazide(bottle)
Rifampicin(bottle)
Pyrazinamide(bottle)
PPD vials
Gauge 26 needle/ syringe
115
NTP Data Quality Assurance Tool
Data Validation
Health Facility:______________________ Date:______________
I. VERIFICATION: Accuracy of Data Yes No Remarks
1. TB Laboratory Register and TB Register
a. All smear (+) registered in TB Lab during the last 2 quarters is registered in the TB register?
b. Date of Examination Results for sputum diagnosis and follow-up are consistent for both
registers
2. TB Treatment Card and TB Register
a. All patients under treatment are registered?
b. Are the following data consistent for both registers?
b.1 General patient information, TB Case no., Type of Patient, classification, regimen
b.2 Date of Examination Result for diagnosis and sputum follow-up
b.3 Treatment Outcome
3. TB Treatment Cared and TB ID Card (Patient/Tx Partner)
a. Are the following data consistent for both NTP Cards?
a.1 General patient information. TB Case no., Type of patient, classification regimen
a.2 Date of Examination Result for diagnosis and sputum follow-up
a.3 Treatment Outcome
a.4 Regularity of Drug collection
4. Monthly (Quarterly) NTP Reports (CF,TrOc,TBDC,TB in Children)
a. Are all NTP reports filed neatly?
b. Do the figures reported match to those counted by monitoring team?
II. REVIEW: Date Completeness
1. TB Laboratory Register
a. General Information (Name,address,etc)
b. Filed-out TB Case No. sputum follow-ups
c. Filed Summary of Cases at the bottom of the register
1. Treatment Card
a. General patient information, TB Case no., Type of patient, classification, regimen
II. REVIEW: Data Completeness
b. All TB patients are under DOTS?
c. Treatment Outcome
d. Regularity of Drug Collection
2. Request for Sputum Exam Form
a. Filed-out all information
b. Filed-out TB case no. for follow-up exam?
3. TB Symptomatic Masterlist
a. Filed-out all information
4. Referral Slip
a. Existing (NTP Referral Form and MDR Referral Form)
b. Filed-out all information
5. TB Register
a. General patient information, TB Case no., Type of patient, classification, regimen
b. Sputum follow-up exam: Date/frequency?
c. Treatment Outcome
d. Filed-out Summary of Cases located at the bottom of the register
116
6. TB ID Card (Patient/Tx Partner)
a. General patient information, TB Case no., Type of Patient, classification, regimen
b. Date of Examination Result for diagnosis and sputum follow-up
c. Treatment Outcome
d. Regularity of Drug Collection
III. TB INFECTION CONTROL
1. Administrative Control
a. TB infection control guidelines/updates discussed within the quarter
b. Any person in-charge to discuss the guidelines?
c. Annual Health-screening conducted among HCWs?
d. HCEs separates patients with cough from other patients
f. Any particular schedule for sputum collection?
g. Any particular schedule for TB patients drug collection?
h. Proper disposal of sputum cups, applicator sticks, masks etc.
IV. TB INFECTION CONTROL
i. Signage for cough etiquette/standard precaution
j. Conduct of regular health education on TB infection Control in health facility (pre-clinic
lectures, etc.)
2. Environment Control
a. HCWs talk to patients in a well ventilated area/room
b. Utilize uni-directional airflow (ex. Improvised mechanical ventilation-Electric fan directed at
air exhaust points windows/doors)
c. Use of short curtains rather than long ones (short curtains allow good ventilation (natural
ventilation) better than the ones utilizing long curtains thus diluting droplet nuclei)
d. Conduct sputum collection induction in a well ventilated area
e. Is there any on in-charge of monitoring
f. Is there any responsible person for cleaning the windows, lab equipment etc.?
3. Personal Protective Equipment (PPE)
a. HCWs use N-95 mask, surgical masks or ordinary masks
b. Patients use surgical mask/ Cloth mask
c. Hand hygiene after caring for patients
d. HCWs instruct TB patients about cough Etiquette/Respiratory Hygiene
V. LOGISTICS
A. Laboratory
a. sputum cups
b. reagent
c. applicator stick
d. glass slides
f. xylene
g. disinfectant
h. gloves
i. masks
1. surgical masks
2/ N-95
j. Reporting Forms
B. NTP Drugs
l. Adult
a. FDC-A
117
b. FDC-B
c. Single drug Formulation
c.1 Rifampicin
c.2 Pyrazinamide
c.3 Ethambutol
d. Streptomycin
e. Gauge 23 needle/syringe
II. Children
a. TB Kit I
b. TB Kit II
c. Single Drug Formulation
c.1 Rifampicin
c.2 Pyrazinamide
c.3 Ethambutol
d. PPD Vials
e. Gauge 26 needle/ syringe
f. Hub cutter
g. cotton balls
h. alcohol
PREPARED BY: NOTED BY:
REMARKS:
118
Health Worker Interview (DOTS Facility)
Name of Health Worker: _________________ Designation: _____________
Date of Interview: ____________
A. Case Finding/ Case Holding
1. When do you register TB symptomatic on TB symptomatic Masterlist?
2. When do you register TB symptomatic on TB laboratory register?
3. When do you register retreatment cases on MDR Referral Masterlist?
4. When do you register TB Patients?
5. Who is the responsible person in filling-out the following records?
a. TB Symptomatic Masterlist
b. TB Laboratory register
c. MDR Referral Masterlist
d. NTP Register
e. Treatment Card
6. In the absence of the responsible person, who fills out the said records?
7. Is there a file for the following?
7.1 NTP Referral Form
7.1.1 Sent out (Copy slips of sent out)
7.1.2 Acknowledgement (copy of returned slips with action taken)
7.2 Acknowledgement referrals from the Referring NGO Units
7.3 MDR Referrals
7.3.1 Sent out (Copy slips of sent out)
7.3.2 Acknowledgement (copy of returned slips with action taken)
7.4 Qtr/ Annual Reports?
7.4.1 Quarterly Reports
7.5.1 Annual Reports
8. Do you have a particular schedule for DOT of Patients?
9. When is the schedule for DOT of patients?
10. Who supervises the drug intake of patients in the health facility?
11. Are there patients taking anti-TB drugs in their houses? Who supervises their treatment?
12. Are there patients taking anti-TB drugs other than the two facilities mentioned above? Who supervises their
treatment?
13. How do you allocate the medicines for them?
a. Health Facility-based
b. Community-based
c. Others
14. What immediate actions are taken to defaulters?
15. How do you follow-up defaulters?
16. Who makes the list of defaulters? Any particular format?
17. Who follows up the identified defaulters?
18. When do you usually follow-up the defaulters?
B. Health Education
1. What Health Education Activities do you conduct?
a. One on one counseling
b. Pre-clinic lectures
c. Bench conference
d. Mothers class
e. Community assembly
f. Others
2. Who conducts the health education?
119
a. One on one counseling
b. Pre-clinic lectures
c. Bench conference
d. Mothers class
e. Community assembly
f. Others
3. When do you conduct the following?
a. One on one counseling
b. Pre-clinic lectures
c. Bench conference
d. Mothers class
e. Community assembly
f. Others
4. Is there a specific schedule for NTP?
5. What are the topics?
6. Is TB Infection Control included on those activities mentioned above?
7. Do you have attendance sheets for these?8. Do you have a narrative report on those activities mentioned above?
(Documentation)
(NOTE: TO BE ACCOMPLISHED ON A SEPARATE SHEET)
120
PATIENT INTERVIEW
Date of Interview:____________________
( ) y.o M/F Smear (+)/(-) P/EP
New/ Ret Reg.I/II/III Date Tx Started:_________________
Health Facility:_____________________
Treatment Partner: PHN/RM/BHW/CHV/FM/Others:___________
A. CONCERNING HIS/HER CLINICAL COURSE:
1. Do you know the name of your disease?
2. What kind of disease is it? Whats the cause of it? Is it infectious?
3. Where do you think you got TB?
4. What kind of symptoms did you have before diagnosis? And when did it start?
5. When and where did you consult first regarding your symptoms?
6. When and where were you diagnosed TB?
7. Were you diagnosed with TB before?
8. What did you feel when you were diagnosed of TB?
9. Any other patients among family (household) members?
10. Do you work now?
B. CONCERNING HIS/ HER TREATMENT REGIMEN:
1. Were you referred to the treatment center (ex. PTSI, etc.) prior to the start of this treatment?
2. How many kinds of medicine (drugs) are you taking?
3. How long are you going to take the medicines (drugs) altogether?
4. Who supervises your drug intake?
5. How often does your treatment partner supervise your drug intake?
6. How does it feel being supervised by a treatment partner (on a daily basis)?
7. What will happen to you if you quit taking the medicines (drugs)?
8.1 Do you want to complete your treatment?
8.2 Why do you want to complete the full course of your treatment?
9. How did you know this health facility?
10. Who decided that you are going to have your treatment here/ or at your treatment partners place for the daily intake of
drugs?
11. Are you committed to complete the whole course of treatment?
11.1 What is the importance of completing the whole course of treatment?
12. What are the side-effects of the medicines (drugs)?
13.1 Did you experience any side-effects?
13.2 If yes, to whom did you tell first?
13.3 What was his/ her advice?
14. Do you know how many times are you going to submit the sputum specimen?
15. What is the result of your sputum exam before you started on treatment?
16. When is your sputum follow-up or when are you going to submit sputum specimen (again)?
17. What is the importance of sputum follow-up?
C. CONCERNING THE CONVENIENCE OF HIS/ HER TRANSPORTATION:
c.1 Health Facility
c.1.1 How often do you go here?
c.1.2 How do you get here?
c.1.3 How much is the fare from your place to this health facility?
c.1.4 What time do you usually come here?
c.2 Treatment Partners Place:
c.2.1 How do you go to your treatment partners house to take medicine (everyday)?
c.2.2 How long does it take?
c.2.3 How much?
c.2.4 What time do you usually go to your treatment partners house?
c.2.5 Do you go alone or accompanied by husband/ wife/ family member ( )/ others ( )
c.2.6 Do you have any difficulties in going to your treatment partners house every day?
c.2.7 (or) Does your treatment partner comes to your house to supervise your drug intake?
If yes: c.2.7.1 How often does she come to your house?
c.2.7.2 What time does he/ she usually comes to your place?
121
NTP MONITORING TOOL FOR REFERRING FACILITIES: Data Collection Form
Adult Children Total
1. TB Symptomatics
1.1 No. Identified
1.2 No. referred to a DOTS facility (with referral forms)
1.3 No. accessed and consulted at DOTS facility
TB Symptomatics Access Rate (AR, %) = (1.3/1.2)* 100 = [TB Symptomatic who accessed/consulted at DOTS
facility
1.4 No. who failed to seek consult at DOTS Facility
Reasons:
Refused to seek consult
Went home to province
No transportation
No companion
Other reasons: specify _____________
1.5 No. underwent DSSM
1.5.1 Smear Positive
1.5.2 Smear Negative
1.6 No. underwent TST
1.6.1 TST Positive
1.6.2 TST Negative
1.7 No. underwent other bacteriological exam.
a. TB Symptomatics Examined Rate (with DSSM) (ER, %)
=(1.5/1.2)*100 = [TB Symptomatic who underwent DSSM] / [TB Symptomatic referred]* 100
b. TB Symptomatics Examined Rate (with TST) (ER, %)
=(1.6/1.2)* 100 = [TB Symptomatic who underwent DSSM] / [TB Symptomatic referred] * 100
c. TB Symptomatics Examined Rate (with DSSM) (ER, %)
=(1.6/1.3)* 100 = [TB Symptomatic who underwent DSSM] / [TB Symptomatic accessed and consulted]* 100
d. TB Symptomatics Examined Rate (with TST) (ER, %)
=(1.6/1.3)* 100 = [TB Symptomatic who underwent DSSM] / TB Symptomatic
2. TB Diagnosis
2.1 Total number of diagnosed as TB:
3. Initiated Treatment
3.1 Total number of TB cases initiated treatment
3.1.1 Total number of PTB:
3.1.1.1 New Smear + PTB (N+)
3.1.1.2 New Smear PTB (N-)
a. New Smear Negative
b. Other Diagnostic Test (ODT)
3.1.1.3 Relapsed (R)
3.1.1.4 Treatment Failure (TF)
3.1.1.5 Return After Default (RAD)
3.1.1.6 Other + (O+)
3.1.1.7 Other (O-)
3.1.2 Total Number of Extra-Pulmonary TB:
4. Treatment Partners of TB Patients
4.1 Total number of TB Patients under DOTS
4.1.1: Health Workers
4.1.2: BHWs
4.1.3: CHVs
4.1.4: FMs
4.1.5: Others
122
5. Treatment Outcome ____Qtr of ____Yr
5.1 New smear (+) PTB
Total initiated Treatment
cured
Completed treatment
Died
Failed
Defaulted
Reasons for Treatment Default
Went home to province
Refused to continue treatment
Other reasons
Transferred out
5.2 Relapsed (Treatment Outcome applied 5.1)
5.3 New Smear (-) PTB (treatment outcome applied same as 5.1 except cured)
5.4 Other Diagnostic Test Categorized as New Smear (-) PTB ( treatment outcome applied same as 5.3)
5.5 Treatment Failure (treatment outcome applied same as 5.1)
5.6 RAD (treatment outcome applied same as 5.1)
5.7 Other (+) PTB (treatment outcome applied same as 5.1)
5.8 Other (-) PTB (treatment outcome applied same as 5.3)
5.3 Extra PTB ( treatment outcome applied same as 5.3)
6. Others
6.1 Underwent MDR Screening
6.1.1 Positive for MDR
6.1.2 Negative for MDR
6.2 No. of trained Community Health Volunteer
6.2.1 No. of Active Community Health Volunteer
6.2.2 No. of Inactive Community Health Volunteer
6.2.2.1 Reasons for being inactive
6.2.2.2 Interventions Done
123
NTP Monitoring Tool Feedback Sheet
Health Facility: ________________________
Date / Time: __________________________
Responsible Person: (RJPI Staff) ________________________
FINDINGS RECOMMENDATIONS
1.
2.
3.
4.
5.
RESPONDENTS: MONITORING TEAM:
1. _______________________________ 1. ______________________________
2. _______________________________ 2. ______________________________
3. _______________________________ 3. ______________________________
4. _______________________________ 4. ______________________________
5. _______________________________ 5. ______________________________
6. _______________________________ 6. ______________________________
7. _______________________________ 7. ______________________________
8. _______________________________ 8. ______________________________
124
REFERENCES:
1. 2010-2016 Philippine Plan of Action to Control Tuberculosis, Health Sector Reform Agenda Monographs.
Manila, Republic of the Philippines, Department of Health (DOH HSRA Monograph No.11) 2009:7.
2. Tupasi T, Radhakrisha S, Quelapio M, et al. Tuberculosis in the Urban Poor Settlements in the Philippines.
Int J Tuberc Lung Dis 2000; 4 (1): 4- 11.
3. Kamolratanakul P, Sawert H, Kongsin S, et al. Economic Impact of Tuberculosis at the
household level. Int J Tuberc Lung Dis 1999; 3 (7): 596- 602.
4. Rajeswari R, Balasubramanian V, Muniyandi M, et al. Socio-economic impact of tuberculosis on patients and
family in India. Int J Tuberc Lung Dis 1999; 3 (10): 869-877.
5. Beyers N, Gie R, Schaaf H, et al. Delay in the diagnosis, notification and initiation of treatment and
compliance in children with tuberculosis. Int J Tuberc Lung Dis 1994; 75 (4) :260- 265.
6. Singh V, Jaiswal A, Porter J, et al. TB Control, Poverty, and Vulnerability in Delhi, India. Tropical Medicine
and International Health 2002; 7 (8): 693- 700.
7. Balasubramanian V, Oommen K, Samuel R. DOT or not? Direct observation of anti-tuberculosis treatment
and patient outcome, Kerala state, India. Int J Tuberc Lung Dis 2000; 495 (5): 409-413.
8. Kemp J, Boxshall M, Nhlema B, et al. Application of a Geographical Information System (GIS) to examine
the relationship between the socio-economic status and access to care for TB in urban Lilongwe. Int J Tuberc
Lung Dis 2001: 5:11 Supplement 1 S167 (abstract).
9. Murthy K, Friedman T, Yazdani A, et al. Public private partnership in Tuberculosis control: experience in
Hyderabad, India. Int J Tuberc Lung Dis 2001;5 (4): 354-359.
10. The Stop TB Strategy: Building on and enhancing DOTS to meet the TB- related Millennium Development
Goals. WHO/HTM/STB/2006.37.
11. Getahun H, Joseph T, Tomascovic L, et al. Engage-TB Integrating community-based tuberculosis activities
into the work of non-governmental and other civil society organizations: operational guidance World Health
Organization 2012.12.
12. Map of the Philippines, Metro Manila, Tondo District 1, and Payatas, Quezon City:
en.wikipedia.org/wiki/Metro_Manila..
13. Ohkado A, Poblete R, Mercader M, et al. Effectiveness of a Training Course on the Quality Assurance of
Chest Radiography in the Philippines. Int J Tuberc Lung Dis 2012;16: 379-383.
14. Ohkado A, Querri A, Poblete R, et al. Health Care Seeking Behaviour of Pulmonary Tuberculosis Patients in
Socio- economically Depressed Areas in the Philippines.Union 2012, Kuala Lumpur, Malaysia; Abstract PC-
333- 15.
15. Querri A, Ohkado A, Poblete R, et al. Tuberculosis Diagnostic Committees contribution to the National TB
Control Program in Manila and Quezon Cities. Public Health Action 2012; Vol 2 No.3.
Das könnte Ihnen auch gefallen
- National Tuberculosis Control Program Manual of Procedures 5th EditionDokument192 SeitenNational Tuberculosis Control Program Manual of Procedures 5th EditionBlue Pielago100% (9)
- Manual of Procedures NTP 5th EditionDokument172 SeitenManual of Procedures NTP 5th EditionMercuryCas100% (3)
- Phil PactDokument116 SeitenPhil PactCecilia Acuin100% (1)
- Ntcp-Mop TB CPG 2015Dokument192 SeitenNtcp-Mop TB CPG 2015Val Constantine Say CuaNoch keine Bewertungen
- HTTPWWW - Ntp.doh - gov.PhdownloadsNTP MOP 5th Edition PDFDokument192 SeitenHTTPWWW - Ntp.doh - gov.PhdownloadsNTP MOP 5th Edition PDFMa Zenaida RamosNoch keine Bewertungen
- NTCP MOP 5e FinalDokument192 SeitenNTCP MOP 5e FinalcharmainegoNoch keine Bewertungen
- Action Falling Short To End Tuberculosis EpidemicDokument4 SeitenAction Falling Short To End Tuberculosis EpidemicKapitan TutanNoch keine Bewertungen
- National Tuberculosis Program MOPDokument192 SeitenNational Tuberculosis Program MOPlpanatalioNoch keine Bewertungen
- Islands of Tuberculosis Elimination: An Evaluation of Community-Based Active Case Finding in North Sumatra, IndonesiaDokument12 SeitenIslands of Tuberculosis Elimination: An Evaluation of Community-Based Active Case Finding in North Sumatra, IndonesiaRahmadika NofriNoch keine Bewertungen
- Department of Health - National Tuberculosis Control Program - 2012-02-08Dokument5 SeitenDepartment of Health - National Tuberculosis Control Program - 2012-02-08daryl ann dep-asNoch keine Bewertungen
- TB Prev CTRL Program 4.5.2021Dokument123 SeitenTB Prev CTRL Program 4.5.2021JeslineNoch keine Bewertungen
- National Tuberculosis Program: NTP Manager: Dr. Anna Marie Celina G. GarfinDokument9 SeitenNational Tuberculosis Program: NTP Manager: Dr. Anna Marie Celina G. GarfinNorjetalexis Maningo CabreraNoch keine Bewertungen
- TB Caravan: A Mobile Active Case-Finding StrategyDokument22 SeitenTB Caravan: A Mobile Active Case-Finding StrategyMajo Napata100% (1)
- Tropicalmed 05 00026 v4Dokument13 SeitenTropicalmed 05 00026 v4D BasavarajaNoch keine Bewertungen
- National Tuberculosis Control ProgramDokument3 SeitenNational Tuberculosis Control ProgrampeterjongNoch keine Bewertungen
- Situational Analysis of Tuberculosis Elimination Program in Greater Manila Using Communities, Rights, and Gender (CRG) ToolsDokument65 SeitenSituational Analysis of Tuberculosis Elimination Program in Greater Manila Using Communities, Rights, and Gender (CRG) ToolsMeljoy AcdalNoch keine Bewertungen
- Revised National Tuberculosis Control Programme (RNTCP) Milestones and AchievementsDokument24 SeitenRevised National Tuberculosis Control Programme (RNTCP) Milestones and Achievementsarunjv1234100% (1)
- Tropicalmed 04 00134 PDFDokument16 SeitenTropicalmed 04 00134 PDFAbhijit DeyNoch keine Bewertungen
- 2013 Manual of Procedures For The National Tuberculosis Program, PhilippinesDokument134 Seiten2013 Manual of Procedures For The National Tuberculosis Program, PhilippinesMark Johnuel Duavis100% (9)
- Use of Digital Technology To Enhance Tuberculosis Control: Scoping ReviewDokument15 SeitenUse of Digital Technology To Enhance Tuberculosis Control: Scoping Reviewahmad habibNoch keine Bewertungen
- PNG National Tuberculosis Management Protocol 2011Dokument46 SeitenPNG National Tuberculosis Management Protocol 2011Issey Mari Tiongco100% (3)
- Tulloch2015 Article PatientAndCommunityExperiencesDokument9 SeitenTulloch2015 Article PatientAndCommunityExperiencesNamira Firdha KNoch keine Bewertungen
- Global TB Network - Working Together To Eliminate TuberculosisDokument3 SeitenGlobal TB Network - Working Together To Eliminate TuberculosisCylla RevataNoch keine Bewertungen
- 2014 AIDS Epidemic Model - Impact Modeling and AnalysisDokument108 Seiten2014 AIDS Epidemic Model - Impact Modeling and AnalysisFritz MaandigNoch keine Bewertungen
- Thailand Progress Towards Ending AIDSDokument83 SeitenThailand Progress Towards Ending AIDSindahNoch keine Bewertungen
- 2017 Article 4627Dokument10 Seiten2017 Article 4627ristaseptiawatiningsihNoch keine Bewertungen
- The Global Fund in Myanmar: Scaling Up The Tuberculosis ControlDokument2 SeitenThe Global Fund in Myanmar: Scaling Up The Tuberculosis ControlsithusoemoeNoch keine Bewertungen
- 2013 Manual of Procedures for the National TB Control ProgramDokument134 Seiten2013 Manual of Procedures for the National TB Control ProgramCarlo Giorgio DC CerezoNoch keine Bewertungen
- ntp2013 PDFDokument134 Seitenntp2013 PDFMissDyYournurseNoch keine Bewertungen
- Capstone Proposal Tanauan GroupDokument9 SeitenCapstone Proposal Tanauan GroupburdeosmaelnoraNoch keine Bewertungen
- India's National AIDS Control Programme (NACPDokument7 SeitenIndia's National AIDS Control Programme (NACPViswa GiriNoch keine Bewertungen
- Lepto Spiros IsDokument17 SeitenLepto Spiros IsIin IndrayaniNoch keine Bewertungen
- National Health ProgrammesDokument12 SeitenNational Health ProgrammesRAJU100% (2)
- GESI - From NACO - CleanDokument35 SeitenGESI - From NACO - CleanMatin Ahmad KhanNoch keine Bewertungen
- 1.2.1 Prevention of MDR-TBDokument24 Seiten1.2.1 Prevention of MDR-TBGunjan UpadhyayNoch keine Bewertungen
- Filipino OT Telehealth ExperiencesDokument5 SeitenFilipino OT Telehealth ExperiencesAr-jay PorrasNoch keine Bewertungen
- Annual Report 2011 HIV NATDokument92 SeitenAnnual Report 2011 HIV NATIs-ma PontiNoch keine Bewertungen
- App-Ramb Out 2019Dokument6 SeitenApp-Ramb Out 2019griloucuraNoch keine Bewertungen
- Revised National TB Control Programme (RNTCPDokument12 SeitenRevised National TB Control Programme (RNTCPViswa GiriNoch keine Bewertungen
- TeleHealth Final ManuscriptDokument127 SeitenTeleHealth Final ManuscriptMaxine JeanNoch keine Bewertungen
- PDF en InglésDokument6 SeitenPDF en InglésKwadwo Oti BoatengNoch keine Bewertungen
- World Bank HIV/AIDS Program Development Project (II) in Nigeria, An Exploration of TB and TB/HIV OptionsDokument29 SeitenWorld Bank HIV/AIDS Program Development Project (II) in Nigeria, An Exploration of TB and TB/HIV OptionsChukwu JanefrancesNoch keine Bewertungen
- Social Marketing On Dengue Hemorrhagic Fever and TDokument14 SeitenSocial Marketing On Dengue Hemorrhagic Fever and TdayafterNoch keine Bewertungen
- 1 Line Treatment Outcomes of The New Pulmonary Bacteriologically Confirmed TB Cases (2012 Cohort, %)Dokument34 Seiten1 Line Treatment Outcomes of The New Pulmonary Bacteriologically Confirmed TB Cases (2012 Cohort, %)ComingSoonNoch keine Bewertungen
- Program Implementation Review - Block 5Dokument20 SeitenProgram Implementation Review - Block 5jollyhotdog89Noch keine Bewertungen
- Telemedicine FinalDokument13 SeitenTelemedicine FinalVictoria PicacheNoch keine Bewertungen
- Tuberculosis preventive treatment WHO 2024Dokument7 SeitenTuberculosis preventive treatment WHO 2024AbrahamKatimeNoch keine Bewertungen
- 35 - Mann - IJTLD - 2010Dokument7 Seiten35 - Mann - IJTLD - 2010Syifa KhairaniNoch keine Bewertungen
- Country Progress ReportDokument19 SeitenCountry Progress Reportprk1234Noch keine Bewertungen
- Revealed That: Among New and Among Re-Treatment TB Cases Had MDR-TBDokument32 SeitenRevealed That: Among New and Among Re-Treatment TB Cases Had MDR-TBComingSoonNoch keine Bewertungen
- Interim Policy On Collaborative Tb/Hiv ActivitiesDokument18 SeitenInterim Policy On Collaborative Tb/Hiv ActivitiesrYanDYNoch keine Bewertungen
- STI-Report 7Dokument28 SeitenSTI-Report 7Hariraj SNoch keine Bewertungen
- National Tuberculosis Control ProgramDokument4 SeitenNational Tuberculosis Control ProgramSlepy chngNoch keine Bewertungen
- Exploring Strategies To Improve The Performance of Community Health Volunteers For Tuberculosis Care and Prevention: A Qualitative StudyDokument8 SeitenExploring Strategies To Improve The Performance of Community Health Volunteers For Tuberculosis Care and Prevention: A Qualitative StudyTIENDUONGNoch keine Bewertungen
- Learning Task 2 - An EvaluationDokument4 SeitenLearning Task 2 - An EvaluationAyeng MonterdeNoch keine Bewertungen
- Care For Vulnerable Populations During COVID-19 PandemicVon EverandCare For Vulnerable Populations During COVID-19 PandemicNoch keine Bewertungen
- Safe and Clean Care: Infection Prevention and Control for Health and Social Care StudentsVon EverandSafe and Clean Care: Infection Prevention and Control for Health and Social Care StudentsNoch keine Bewertungen
- SARS-CoV-2 Viral Outbreak Investigation: Laboratory Perspective: Clinical Updates in COVID-19Von EverandSARS-CoV-2 Viral Outbreak Investigation: Laboratory Perspective: Clinical Updates in COVID-19Bewertung: 3 von 5 Sternen3/5 (1)
- SARS-CoV-2 Viral Outbreak Investigation: Laboratory PerspectiveVon EverandSARS-CoV-2 Viral Outbreak Investigation: Laboratory PerspectiveNoch keine Bewertungen
- Handbook of Emergency Disposal and Management of Medical Waste in ChinaVon EverandHandbook of Emergency Disposal and Management of Medical Waste in ChinaNoch keine Bewertungen
- Groundwater Control For Cross PassagesDokument6 SeitenGroundwater Control For Cross PassageskrainajackaNoch keine Bewertungen
- Firewalker Spell and Ability GuideDokument2 SeitenFirewalker Spell and Ability GuideRon Van 't VeerNoch keine Bewertungen
- OCFINALEXAM2019Dokument6 SeitenOCFINALEXAM2019DA FT100% (1)
- Choi, J H - Augustinian Interiority-The Teleological Deification of The Soul Through Divine Grace PDFDokument253 SeitenChoi, J H - Augustinian Interiority-The Teleological Deification of The Soul Through Divine Grace PDFed_colenNoch keine Bewertungen
- Artificial IntelligenceDokument1 SeiteArtificial IntelligenceTeresaNoch keine Bewertungen
- Rizal's First Return Home to the PhilippinesDokument52 SeitenRizal's First Return Home to the PhilippinesMaria Mikaela MarcelinoNoch keine Bewertungen
- Pengayaan Inisiasi 6-SynonymyDokument35 SeitenPengayaan Inisiasi 6-SynonymyAriNoch keine Bewertungen
- Official Correspondence in English CompleteDokument55 SeitenOfficial Correspondence in English Completeyadab rautNoch keine Bewertungen
- Anti Viral DrugsDokument6 SeitenAnti Viral DrugskakuNoch keine Bewertungen
- Volleyball ReflectionDokument1 SeiteVolleyball ReflectionJake Santos100% (1)
- Le Nu Spa Employee HandbookDokument34 SeitenLe Nu Spa Employee Handbookhamzeh abo hammourNoch keine Bewertungen
- Lived Experiences of Science Teachers of Pangasinan Ii in The New Normal Education: A Phenomenological StudyDokument10 SeitenLived Experiences of Science Teachers of Pangasinan Ii in The New Normal Education: A Phenomenological StudyIJAR JOURNALNoch keine Bewertungen
- Understanding PersonalityDokument318 SeitenUnderstanding PersonalityRoxanna12100% (1)
- The Art of Communication PDFDokument3 SeitenThe Art of Communication PDFHung Tran JamesNoch keine Bewertungen
- EN4264 Final Essay - GeraldineDokument25 SeitenEN4264 Final Essay - GeraldineGeraldine WongNoch keine Bewertungen
- Munslow, A. What History IsDokument2 SeitenMunslow, A. What History IsGoshai DaianNoch keine Bewertungen
- Alan Ross CV Expert Road Safety AdviserDokument4 SeitenAlan Ross CV Expert Road Safety AdviserAnna Sophia YorkNoch keine Bewertungen
- Methods of GeographyDokument3 SeitenMethods of Geographyramyatan SinghNoch keine Bewertungen
- Sample Progress Report ASTDokument1 SeiteSample Progress Report ASTzulkefli90Noch keine Bewertungen
- The Names & Atributes of Allah - Abdulillah LahmamiDokument65 SeitenThe Names & Atributes of Allah - Abdulillah LahmamiPanthera_Noch keine Bewertungen
- Chemistry The Molecular Science 5th Edition Moore Solutions Manual 1Dokument36 SeitenChemistry The Molecular Science 5th Edition Moore Solutions Manual 1josephandersonxqwbynfjzk100% (27)
- Repeaters XE PDFDokument12 SeitenRepeaters XE PDFenzzo molinariNoch keine Bewertungen
- Advproxy - Advanced Web Proxy For SmoothWall Express 2.0 (Marco Sondermann, p76) PDFDokument76 SeitenAdvproxy - Advanced Web Proxy For SmoothWall Express 2.0 (Marco Sondermann, p76) PDFjayan_Sikarwar100% (1)
- Doubles and Doppelgangers: Religious Meaning For The Young and OldDokument12 SeitenDoubles and Doppelgangers: Religious Meaning For The Young and Old0 1Noch keine Bewertungen
- Eclipse Phase Ghost in The ShellDokument27 SeitenEclipse Phase Ghost in The ShellMeni GeorgopoulouNoch keine Bewertungen
- Semester 3 SyllabusDokument12 SeitenSemester 3 SyllabusFuggi JaanNoch keine Bewertungen
- Myanmar Thilawa SEZ ProspectusDokument92 SeitenMyanmar Thilawa SEZ ProspectusfrancistsyNoch keine Bewertungen
- 1603 Physics Paper With Ans Sol EveningDokument8 Seiten1603 Physics Paper With Ans Sol EveningRahul RaiNoch keine Bewertungen
- Jeff Roth CVDokument3 SeitenJeff Roth CVJoseph MooreNoch keine Bewertungen
- FINAL Conflicts 2019 Official Guidelines PDFDokument48 SeitenFINAL Conflicts 2019 Official Guidelines PDFxsar_xNoch keine Bewertungen