Beruflich Dokumente
Kultur Dokumente
British Heart Asso - Heart Disease Summary
Hochgeladen von
nob2011nob0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
24 Ansichten2 SeitenBritish Heart Asso.heart Disease Summary
Originaltitel
British Heart Asso.heart Disease Summary
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenBritish Heart Asso.heart Disease Summary
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
24 Ansichten2 SeitenBritish Heart Asso - Heart Disease Summary
Hochgeladen von
nob2011nobBritish Heart Asso.heart Disease Summary
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 2
Cardiac imaging with MRI,
CT and Nuclear techniques
Factfile No.1 January 2010
Summary
Cardiac magnetic resonance (CMR) is the gold standard for assessing cardiac anatomy, function and mass
CMR is not the technique of choice for non invasive imaging of the coronary arteries
Computed tomography (CT) provides rapid, high quality non-invasive imaging of the coronary arteries
CT calcium scoring provides diagnostic and prognostic information on coronary artery disease
Nuclear imaging has a role in evaluating myocardial perfusion
Cardiac Positron Emission Tomography (PET) imaging with FDG is the gold standard for assessment of myocardial viability
Conventional X-ray angiography remains essential for coronary intervention (angioplasty)
Background
Non-invasive cardiac imaging* has developed rapidly over recent years
and is set to play an important role in the assessment of cardiac structure
and function in the future. Several different technologies are involved
and it is important that the optimal, most cost-effective test for each
individual clinical situation is chosen. There is currently no single non
invasive imaging technique that can provide all the information needed
to manage heart disease.
Cardiovascular Magnetic Resonance (CMR)
Magnetic Resonance (MR) imaging relies on differences in the way
tissues react to a magnetic field, based largely on their water content, to
generate an image. Differences in the way the field is applied can
produce different types of image and information. Consequently, the
image provided by MR is a composite of the data acquired, usually as a
series of digital data sets representing only a small portion of the whole
heart, and how it is handled (processed) by the computer. Data
acquisition requires the presence of the patient, but data processing can
take place at a later time. CMR has lagged behind MR imaging of other
organs because of artefacts induced by cardiac and respiratory
movements that occur during data acquisition. However, ECG and
respiratory gating (where data acquisition is synchronized with the
cardiac and respiratory cycle) coupled with increasingly rapid data
acquisition technologies now allow data sets to be acquired in a single
breath hold. From data acquired over 40-60 minutes CMR now delivers
high-resolution images in any imaging plane that can be processed to
provide two or three-dimensional static reconstructions or movie loops
in almost every patient.
What is CMR good at?
CMR provides outstanding anatomical and functional detail.
Consequently its main clinical uses are:
to characterise congenital heart disease and its complications
to measure right and left ventricular mass (CMR is the gold standard
for quantifying left ventricular hypertrophy)
to differentiate forms of cardiomyopathies, such as hypertrophic
cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy
and infiltrative diseases such as sarcoid and amyloid
to assess left and right ventricular function, regional wall motion
abnormalities, myocardial viability and myocardial perfusion. Areas
of myocardial infarction can be identified following administration
of intravenous gadolinium.
to identify stress induced myocardial ischaemia during infusions of
dobutamine or adenosine
*Some imaging procedures require the infusion or injection of agents to stress the
heart or those to enhance imaging such as nuclear imaging tests.
In addition, CMR has a role in the assessment of intra-cardiac masses and
quantifying intra- and extra-cardiac shunt flows. Because it can image
the entire aorta it is increasingly used for diagnosis and follow-up of
patients with several aortic pathologies e.g. dissection, Marfan and
aneurysm. However, although CMR can visualise the large proximal
portions of coronary arteries, such that it is used to diagnose rare
congenital anomalies of the coronaries, CMR currently cannot produce
images of sufficient quality to assess coronary artery disease.
What are the advantages of CMR over other imaging
techniques?
CMR provides higher resolution and clearer three dimensional images of
the heart than echocardiography, but at a substantially greater cost. It is
non-invasive, does not involve exposure to ionizing radiation and, unless
contrast agents are used, carries no known risks. It is highly reproducible
and therefore ideal for serial imaging.
What are the disadvantages of CMR?
CMR cannot be used in patients with large implanted metallic devices,
such as cardiac defibrillators or pacemakers (although there are some
MRI compatible pacing devices now available). However, patients with
modern mechanical heart valves or coronary artery stents can be
imaged safely.
CMR requires patients to lie inside a narrow tube for a considerable
amount of time. Consequently, some patients experience anxiety and
claustrophobia - this can sometimes be overcome by using sedation.
Image quality may be suboptimal in patients who are unable to hold
their breath or in those with an irregular heart rate, such as atrial
fibrillation. In patients with severe renal impairment gadolinium contrast
(used to image myocardial scarring) can lead to the rare complication of
nephrogenic systemic fibrosis.
State of the art CMR requires a highly trained multidisciplinary team,
including cardiologists, radiologists, radiographers and physicists. It is
therefore expensive and not yet available in all hospitals.
Cardiac Computed Tomography (CT)
Cardiac CT uses x-rays to build up 3D images of the heart. With modern
CT machines scans can be performed in under one second and can
provide remarkable levels of anatomical detail. CT imaging of the heart
can be performed either with or without intravenous contrast agents. As
with CMR, following acquisition, the CT datasets can be reformatted in
any orientation and can be viewed as cine loops for functional analysis
of ventricular function. Software allows semi-automated extraction of
the coronary arteries and the production of 3D volumetric datasets. Total
scan time for a cardiac CT is about 15 minutes.
Factfile is an information resource produced by the British Heart Foundation for GPs based on up to
date clinical evidence and expert opinion. As a digest of many data sources, it is necessarily the
culmination of assessments made by the BHFs medical professionals and should not be taken as a
definitive statement of correct clinical practice in any given situation. Consequently, the BHF is not
able to give any warranties in relation to particular clinical decisions taken or courses of treatment or
action pursued based upon information contained in the Factfiles.
This is the final printed Factfile you will receive.
To register for our electronic mailing please visit our website bhf.org.uk/factfiles.
To send us your comments or suggestions visit
bhf.org.uk/factfiles
British Heart Foundation
Greater London House
180 Hampstead Road
London
NW1 7AW
Telephone: 020 7554 0000
British Heart Foundation 2009, a registered charity in England and Wales (225971) and in Scotland (SC039426)
What is cardiac CT good at?
Coronary calcium scoring for suspected coronary artery disease
nearly all atherosclerotic plaques contain some calcium. Low dose,
non-contrast CT scans of the heart can quantify the amount and
distribution of calcium in the coronary arteries. There is a direct
correlation between the extent of calcium in the coronary arteries
and the risk of future cardiac events.
Diagnosis and assessment of coronary artery disease contrast
enhanced CT of the coronary arteries enables visualization of the
artery lumen, atherosclerotic plaques and stenoses. When combined
with calcium score, CT coronary angiography has a very high
negative predictive value (approaching 100%) for ruling out
coronary artery disease.
Assessment of patency of bypass grafts and anomalous coronary
arteries CT allows accurate assessment of coronary bypass graft
occlusion and patency, along with evaluation of the course of
anomalous coronary arteries.
Assessment of left ventricular mass and function accurate
assessment of stroke volume, ejection fraction and wall motion
abnormalities can be obtained.
Assessment of cardiac morphology CT can be used to assess
complex congenital heart disease; cardiac masses; thrombus;
pericardial disease; pulmonary and aortic pathology.
What are the advantages of CT over other imaging
techniques?
CT provides rapid, high quality imaging of the coronary arteries not
matched by any other non-invasive technique and is the only technique
able to provide a calcium score. CT scanning is less claustrophobic than
MRI and can be used in most patients who are precluded from having
CMR.
What are the disadvantages of CT?
The main disadvantage of cardiac CT is the dose of radiation, which is
dependent on the type of imaging undertaken, but is currently around
the same as a conventional x-ray angiogram (4-6mSv) for a full cardiac
investigation. The dose has fallen rapidly as the technology has
developed and is likely to fall still further in the future. As with routine X-
ray angiography, nephrotoxic iodinated contrast agents should be used
with caution in patients with impaired renal function.
Cardiac Nuclear Imaging - Single Photon Emission Computed
Tomography (SPECT) and Cardiac Positron Emission Tomography
and (PET)
Cardiac SPECT and PET are both non-invasive nuclear imaging
techniques. They rely on intravenous administration of radiotracers that
are extracted by normal myocardium, such as thallium and sestamibi for
SPECT and Fluorodeoxyglucose (FDG) for PET. Images are derived from
radioactive emission data acquired using either a gamma camera
(SPECT) or a PET scanner and processed to provide an image of the
radiotracer distribution in the myocardium. Both techniques generate
low resolution, high sensitivity 3D images of radiotracer distribution
within the myocardium. Their primary role is therefore in the quantative
assessment of myocardial perfusion and myocardial viability. They have
no role in anatomical imaging.
Both SPECT and PET data can be acquired during pharmacological stress
(adenosine, dipyridamole) to determine whether there are inducible
areas of ischaemia within the myocardium. Assessment of myocardial
ischaemia by SPECT involves comparing tracer distribution during stress
with that at rest. A mismatch indicates reversible ischaemia, whereas a
fixed defect indicates myocardial infarction. Consequently a SPECT
myocardial perfusion study requires two imaging sessions separated by
sufficient time to allow for decay of the previous dose. Cardiac SPECT is
much more widely available than PET and uses tracers with long half-
lives. In contrast cardiac PET is less available and uses short half life tracers
whose short half-life requires that they have to be generated near to the
scanner and used within a short time of production. The advantage of
PET is its ability to use many different tracers to interrogate several
aspects of myocardial pathophysiology. Whilst SPECT is available in most
UK hospitals, cardiac PET remains predominantly a research tool
confined to major academic centres.
Total scanning time is usually around 30 minutes. The data are displayed
in the three standard cardiac planes and may include both static and
dynamic images. Images can be read both qualitatively and
quantitatively.
Newly designed combined PET/CT scanners provide the opportunity to
acquire complimentary anatomical data such as CT coronary
angiography and functional data such as perfusion in a single imaging
session. This hybrid technique at present remains a research tool.
What is nuclear imaging good at?
Assessment of myocardial perfusion (SPECT)
Assessment of left ventricular ejection fraction
Assessment myocardial viability (PET) FDG-PET can identify viable
myocardium that is functioning poorly as a result of reduced
perfusion (hibernating myocardium) that would benefit from
revascularization.
What are the advantages of nuclear imaging over other imaging
techniques?
Cardiac PET imaging with FDG is the gold standard for assessment of
myocardial viability. Cardiac SPECT is relatively cheap and widely
available.
What are the disadvantages of nuclear imaging?
As with cardiac CT, nuclear imaging involves ionizing radiation. For
example, the radiation dose for a SPECT perfusion study is approximately
15mSv for a thallium scan. Consequently, nuclear imaging is not
appropriate for serial follow up studies.
Summary
Non invasive cardiac imaging is fast becoming the first line investigation
in the diagnosis and management of patients with heart disease.
Currently, there is no single technique that can provide all the
information that might be needed and choice of technique is dictated
by the question to be resolved and local availability and expertise. Both
cardiac MR and CT are set to become part of routine cardiac disease
management.
Further reading
1. Bandettini WP, Arai AE. Advances in clinical applications of cardiovascular magnetic resonance imaging. Heart 2008;94:1485-1495.
2. Roberts WT, Bax JJ, Davies LC et al. Cardiac CT and CT coronary angiography: technology and application. Heart 2008;94:781-792.
3. Hengel FM, Higuchi T, Javadi MS, Lautamki R. Cardiac Positron Emission Tomography. J Am Coll Cardiol 2009;54(1):1-15.
Das könnte Ihnen auch gefallen
- Econometrics Notes-1Dokument28 SeitenEconometrics Notes-1nob2011nobNoch keine Bewertungen
- How To Write Great EssaysDokument127 SeitenHow To Write Great Essaysa100% (25)
- Acute Pancreatitis GuidelinesDokument10 SeitenAcute Pancreatitis GuidelinesDaniel RusieNoch keine Bewertungen
- Minimal Change GNDokument2 SeitenMinimal Change GNnob2011nobNoch keine Bewertungen
- MCQs in BasicDokument87 SeitenMCQs in Basictausif0675% (4)
- Fast Track Surgery - Trauma OrthoDokument40 SeitenFast Track Surgery - Trauma Orthonob2011nobNoch keine Bewertungen
- NICE - Dementia (Quick Reference)Dokument28 SeitenNICE - Dementia (Quick Reference)Mohd RamadhanNoch keine Bewertungen
- Mrcs ExamsDokument10 SeitenMrcs Examsnob2011nobNoch keine Bewertungen
- Last Minute CPSDokument11 SeitenLast Minute CPSnob2011nobNoch keine Bewertungen
- Coeli AcDokument9 SeitenCoeli AcSamir MustafaNoch keine Bewertungen
- Guideline Management Atrial FibrilationDokument61 SeitenGuideline Management Atrial FibrilationDeni Andre Atmadinata100% (1)
- Actinic Keratoses GuidelinesDokument9 SeitenActinic Keratoses Guidelinesnob2011nobNoch keine Bewertungen
- COPD TextbookDokument10 SeitenCOPD Textbooknob2011nobNoch keine Bewertungen
- GP Clinical Survival GuideDokument30 SeitenGP Clinical Survival Guidenob2011nobNoch keine Bewertungen
- Actinic Keratoses GuidelinesDokument9 SeitenActinic Keratoses Guidelinesnob2011nobNoch keine Bewertungen
- ENT Exam-TZAR DOHNS Report 2011-860056v1-UbayasiriDokument2 SeitenENT Exam-TZAR DOHNS Report 2011-860056v1-Ubayasirinob2011nob0% (1)
- Surgery MCQ 2004Dokument24 SeitenSurgery MCQ 2004nob2011nob100% (1)
- Basic Science Notes MRCP AssDokument9 SeitenBasic Science Notes MRCP AssUm HamoOdNoch keine Bewertungen
- Medical Mnemonics: FOR Medicine & SurgeryDokument62 SeitenMedical Mnemonics: FOR Medicine & SurgeryShailen ShakyaNoch keine Bewertungen
- EconomicsDokument24 SeitenEconomicsnob2011nobNoch keine Bewertungen
- Fast Track Surgery - Trauma OrthoDokument40 SeitenFast Track Surgery - Trauma Orthonob2011nobNoch keine Bewertungen
- Econometrics Notes-1Dokument28 SeitenEconometrics Notes-1nob2011nobNoch keine Bewertungen
- EMQs for Medical Students Volume 2 GastroenterologyDokument30 SeitenEMQs for Medical Students Volume 2 Gastroenterologynob2011nob100% (1)
- Mrcs NotesDokument24 SeitenMrcs Notesnob2011nob67% (3)
- Intercollegiate MRCS SyllabusDokument88 SeitenIntercollegiate MRCS Syllabuskelly_ann23Noch keine Bewertungen
- Vit DDokument5 SeitenVit DShrikant Hemant JoshiNoch keine Bewertungen
- Physiology NotesDokument3 SeitenPhysiology Notesnob2011nob0% (1)
- Med Surg Finals 2e BOOK PDFDokument51 SeitenMed Surg Finals 2e BOOK PDFJa Gh75% (4)
- SURGERY Important NotesDokument14 SeitenSURGERY Important Notesnob2011nobNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- RadiologistDokument4 SeitenRadiologistdenchas100% (2)
- Medical Imaging Units SpecsDokument12 SeitenMedical Imaging Units Specsar nedungadiNoch keine Bewertungen
- Single Photon Emission Computed TomographyDokument6 SeitenSingle Photon Emission Computed TomographyGanesh JagdaleNoch keine Bewertungen
- Edan MONITOR ACCESSORIES PDFDokument11 SeitenEdan MONITOR ACCESSORIES PDF高伟Noch keine Bewertungen
- Monitor DesfibriladorDokument72 SeitenMonitor DesfibriladoryimelNoch keine Bewertungen
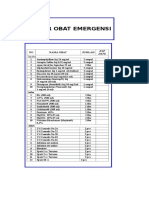
- Daftar Harga Produk PT Galoeh Husada Farma 2021: No Nama Barang Nama Produk PT GHF Satuan Hna+Ppn KeteranganDokument2 SeitenDaftar Harga Produk PT Galoeh Husada Farma 2021: No Nama Barang Nama Produk PT GHF Satuan Hna+Ppn Keteranganpuskesmas tarokanNoch keine Bewertungen
- Nama Alat Merk Type Rehab Medik: Daftar Alat Kalibrasi Rsi At-TinDokument14 SeitenNama Alat Merk Type Rehab Medik: Daftar Alat Kalibrasi Rsi At-Tineka febriNoch keine Bewertungen
- Correct Selection of Pitch in CT JACR 415Dokument2 SeitenCorrect Selection of Pitch in CT JACR 415Merim JusufbegovicNoch keine Bewertungen
- Introduction To Medical Imaging SystemsDokument13 SeitenIntroduction To Medical Imaging SystemsYousef Ahmad2Noch keine Bewertungen
- Kegiatan Kalibrasi Tahun: 2022: Puskesmas GUNUNG KALERDokument2 SeitenKegiatan Kalibrasi Tahun: 2022: Puskesmas GUNUNG KALERNova ArdiantoNoch keine Bewertungen
- Daftar Obat Alkes Trolley EmergencyDokument15 SeitenDaftar Obat Alkes Trolley EmergencyPRIHATINNoch keine Bewertungen
- Intrnoduction To Medical Imaging (ENG)Dokument40 SeitenIntrnoduction To Medical Imaging (ENG)علاء الدين العولقيNoch keine Bewertungen
- Infant T-Piece Resuscitator with Air/O2 Blender & PIP/PEEP ControlDokument1 SeiteInfant T-Piece Resuscitator with Air/O2 Blender & PIP/PEEP ControlDavid Gnana DuraiNoch keine Bewertungen
- Information For Consumers - Magnetic Resonance Angiography (MRA)Dokument5 SeitenInformation For Consumers - Magnetic Resonance Angiography (MRA)ChemistixNoch keine Bewertungen
- Price List Isamed'19Dokument10 SeitenPrice List Isamed'19yohandaNoch keine Bewertungen
- Final - Specifications of Stereotactic FrameDokument2 SeitenFinal - Specifications of Stereotactic FrameadeshdrNoch keine Bewertungen
- 18 SmallyDokument6 Seiten18 Smallyjangkrik21Noch keine Bewertungen
- CTTN Radiology Cibinong 1Dokument5 SeitenCTTN Radiology Cibinong 1arikamanjayaNoch keine Bewertungen
- Usulan Alkes 2023Dokument10 SeitenUsulan Alkes 2023Vitananda Tiara MaharaniNoch keine Bewertungen
- Introduction To Clinical Radiology: The Breast: Priscilla J. Slanetz MD, MPH Assistant Professor of RadiologyDokument10 SeitenIntroduction To Clinical Radiology: The Breast: Priscilla J. Slanetz MD, MPH Assistant Professor of Radiologydrqazi777Noch keine Bewertungen
- Previous Question Paper 1 DMITDokument8 SeitenPrevious Question Paper 1 DMITMahesh BodaNoch keine Bewertungen
- Nemio Brochure MCAUS0642Dokument4 SeitenNemio Brochure MCAUS0642Engineer AwaisNoch keine Bewertungen
- March: Operating Room 1 ItemDokument16 SeitenMarch: Operating Room 1 ItemJoybee ThiamNoch keine Bewertungen
- Operating Room Requisition SlipDokument2 SeitenOperating Room Requisition SlipAnna Margarett Mutia CaballarNoch keine Bewertungen
- Ups Imagen Guia de DiseñoDokument591 SeitenUps Imagen Guia de DiseñoJersson Monge RiveroNoch keine Bewertungen
- Vendor MR Acronyms ConversionDokument6 SeitenVendor MR Acronyms Conversionhgaucher100% (4)
- Ecdoc 100005411Dokument3 SeitenEcdoc 100005411Anka Yatçılık - BodrumNoch keine Bewertungen
- Sti - Pricelist AcDokument2 SeitenSti - Pricelist AcGriya Ayu SkincareNoch keine Bewertungen
- Book of Extended SynopsesDokument671 SeitenBook of Extended Synopsesjiar001Noch keine Bewertungen
- BASIC COMPUTER OPERATIONS AND MEDICAL DATADokument9 SeitenBASIC COMPUTER OPERATIONS AND MEDICAL DATAEslamdasoky 223366Noch keine Bewertungen