Beruflich Dokumente
Kultur Dokumente
Acute Abdomen
Hochgeladen von
YS NateCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Acute Abdomen
Hochgeladen von
YS NateCopyright:
Verfügbare Formate
1
Week III
MODULE OF SKILL LABORATORY PRACTICE
BLOCK : GASTRO-INTESTINAL SYSTEM
TOPIC : CLINICAL EXAM OF SURGICAL DISEASE/
DISORDERS OF THE ACUTE ABDOMEN
I. GENERAL OBJECTIVE
After finishing skill practice of Clinical examination of surgical diseases and disorders of the
abdomen, the student will be able to perform history taking and physical examination of
surgical diseases and disorders of the abdomen correctly.
II. SPECIFIC OBJECTIVES
At the end of skill practices, the student will be able to perform clinical examination of acute
abdomen correctly.
III. SYLLABUS DESCRIPTION
3.1 Sub Module Objective
After finishing skill practice of examination of acute abdomen, the student will be
able to perform history taking and physical examination of acute abdomen correctly.
3.2 Expected Competencies
a. Students perform history taking of acute abdomen. (P5)
b. Students perform physical examination of acute abdomen.(P5)
3.1 Topics
1. History taking of acute abdomen.
2. Physical examination of acute abdomen.
3.2 Methods
a. Presentation
b. Demonstration
c. Coaching
d. Self practices
3.3 Laboratory Facilities
1. Skills Laboratory
2. Clinical Instructors
3. Student Learning guide
4. Instructor guide
5. References
6. Equipment
7. Standardized patient
2
3.4 Venue
Skills Laboratory Faculty of Medicine of Universitas Padjadjaran, Bandung, at
A.5.1.1 Building, Jatinangor Campus.
3.5 Organizer
Clinical Skills Program of Gastro-intestinal System, Faculty of Medicine Universitas
Padjadjaran, Dr Hasan Sadikin Hospital.
3.6 Evaluation
a. Skill demonstration
b. Point nodal evaluation
c. OSCE
IV. Equipment arrangement
All equipment required for this topic includes:
1. Multimedia equipment
2. Examination couch
3. Table
4. Chairs
5. Stethoscope
6. Pelvic models
7. Supporting equipment and facilities
1. Water tap with running water
2. Wash basin
3
V. LEARNING GUIDE OF ACUTE ABDOMEN
A. HISTORY TAKING
No. Procedure Performance Scale
Comment
1 2 3
Introduction
1. Greet the patient, and develop a warm
and helpful environment
2. Introduce yourself to the patient
Patient Identity
3. Ask the patient politely concerning
his/her:
name
age
4. Record the gender:
Male
Female
5. Ask the marital status of the patient
(especially for female)
Chief complaint
6. Ask the patient regarding why the
patient comes to you.
7. Pain:
Onset
Site at onset
Site at present
Severity
Aggravating factors
Relieving factors
Duration
Progress
Type of pain
Radiation
4
Other related symptoms
8. Ask the patient concerning
related/concomitant symptoms of:
9.1.Gastro-intestinal functions:
Nausea
Vomiting
Loss of appetite
Faintness
Previous indigestion (habitual)
Jaundice
Bowel habit:
o Constipation?
o Diarrhoea?
o Color of the stool?
o Presence or absence of
blood and mucus (slime)
9.2.Urinary function:
Micturition: amount of urine,
lower abdominal discomfort,
color of urine
9.3.Gynaecological function: (Female)
Menstrual function
Delayed or miss period
Abnormal bleeding or discharge
(color, quantity)
9. Previous history of :
Previous similar pain
Previous abdominal surgery
Previous major illness: incl.
fever, abdominal injury.
Drugs
Allergies
5
B. PHYSICAL EXAMINATION
No. Procedure Performance Scale
Comment
1 2 3
Preparation
1. Check all the equipment required and
have a good light:
Examination couch
Stethoscope
2. Explain the procedure and its goals to the
patient.
3. Wash your hands with antiseptic soap
4. Dry and warm your hands with tissues
Implementation
A General Examination:
5. General appearance:
Consciousness
Mood: distressed? Anxious?
Immobile
Move cautiously
Colour: Pallor? Flushing?
Jaundice? Cyanosis?
6. Examine the vital signs:
Temperature
Pulse rate
Blood Pressure
Respiratory rate
7. Perform other systems examination,
including cardio-pulmonary system.
8. Ask the patient politely to expose his/her
abdomen.
B. Abdominal Examination:
Inspection
9. Inspect the movement:
Respiratory movement
Visible bowel peristaltic
6
10. Is there any scar on the skin of the
abdomen?
11. Is there any abdominal distention?
Flatus?
Fluid?
Fetus?
12. Is there any rashes and discoloration?
Cullens sign
Gray Turners sign
Ecchymosis of the abdominal wall
13. Is there any masses:
Tumors?
Hernial sites?
Masses with pulsation?
Auscultation
14. Using stethoscope, and place it gently on
the abdomen, listen to the bowel sounds
and bruit at least for one minute:
Absent?
High pitched and hyperactive?
Metallic sound?
Vascular bruit?
Palpation
15. Ask the patient to locate the site of
maximum pain with the tip of a finger.
16. Using the palmar surface of your fingers,
gently palpate the abdomen, starting from
a site farthest from the area of maximum
pain, move gradually towards it. While
palpating, look to the face expression of
the patient, and look for any signs of :
Tenderness
Rebound tenderness
Muscle guarding
Rigidity
Murphys sign
Rovsings sign
Psoas and Obturators sign
Swelling or masses
Expansile pulsation
Hernial orifices
Scrotum in male
7
Percussion
16\7
.
Place the palmar aspect of your left hand
on the abdomen, and gently percuss its
dorsal aspect with the tip of the middle
finger of the right hand, moving all
around the abdominal region:
Is it tymphanitic?
Is it Dull?
Is there any shifting dullness?
Site of liver dullness? and is it
disappeared?
Digital Rectal Examination
18. Put on surgical hand gloves and ask the
patient to expose his/her buttock and anus,
and place the patient in lithotomic
position.
19. Apply lubricating jelly on to the right
index finger.
20. Gently insert your right index finger into
the anus, move toward the anal canal
slowly, and evaluate the followings:
Anal margin: piles?
Mucosal surface of the anal canal
and the ampulla (collapsed?)
Sites of any pain elicited
Masses or swelling: consistency,
location, surface, fixity to the
surroundings.
Bowel contents: consistency of
faeces? Mucus? Blood?
21. Perform bimanual palpation in female
patient to examine the uterus, pelvic
cavity and adnexa.
22. Remove the gloves and wash your hands.
Write up
23. Write up all significant findings in the
medical record.
24. Conclude your diagnosis and differential
diagnosis, and order any necessary special
investigations
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- 04 Talent Pro User Manual EN-rev1Dokument45 Seiten04 Talent Pro User Manual EN-rev1Mai Thanh Sơn75% (4)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Fundamentals of Nursing Chapter ExamDokument13 SeitenFundamentals of Nursing Chapter ExamAlfred Benjamin Cajita100% (4)
- Complete Data Interpretation For The MRCP (S. Hughes) (Z-Library)Dokument289 SeitenComplete Data Interpretation For The MRCP (S. Hughes) (Z-Library)YS NateNoch keine Bewertungen
- Adult Non Verbal Pain Scale UpdatedDokument15 SeitenAdult Non Verbal Pain Scale UpdatedGay PopNoch keine Bewertungen
- Arndt - First Lessons in Symptomatology of Leading Homeopathic RemediesDokument85 SeitenArndt - First Lessons in Symptomatology of Leading Homeopathic Remediesaruen79Noch keine Bewertungen
- Brad Whisnant Five Element WebinarDokument27 SeitenBrad Whisnant Five Element WebinarRodrigo Bittencourt93% (15)
- CD015311.ms en Ms TDokument2 SeitenCD015311.ms en Ms TYS NateNoch keine Bewertungen
- CD014799.pub2.ms en Ms TDokument2 SeitenCD014799.pub2.ms en Ms TYS NateNoch keine Bewertungen
- CD001423.pub4.ms en Ms TDokument1 SeiteCD001423.pub4.ms en Ms TYS NateNoch keine Bewertungen
- CD009124.pub3.ms en Ms TDokument2 SeitenCD009124.pub3.ms en Ms TYS NateNoch keine Bewertungen
- CD003212.pub4.ms en Ms TDokument2 SeitenCD003212.pub4.ms en Ms TYS NateNoch keine Bewertungen
- CD013558.pub2.ms en Ms TDokument2 SeitenCD013558.pub2.ms en Ms TYS NateNoch keine Bewertungen
- CD009604.pub2.ms en Ms TDokument2 SeitenCD009604.pub2.ms en Ms TYS NateNoch keine Bewertungen
- CD004065.pub4.ms en Ms TDokument2 SeitenCD004065.pub4.ms en Ms TYS NateNoch keine Bewertungen
- CD012788.pub2.ms en Ms TDokument2 SeitenCD012788.pub2.ms en Ms TYS NateNoch keine Bewertungen
- CD006161.pub3.ms en Ms TDokument2 SeitenCD006161.pub3.ms en Ms TYS NateNoch keine Bewertungen
- Auto Form 1 Oct 2022. Version 3.1Dokument1 SeiteAuto Form 1 Oct 2022. Version 3.1YS NateNoch keine Bewertungen
- Chew Guan HinDokument11 SeitenChew Guan HinYS NateNoch keine Bewertungen
- Cinacalcet For The Treatment of Secondary Hyperparathyroidism in Patients With End-Stage Renal Disease On Maintenance Dialysis TherapyDokument31 SeitenCinacalcet For The Treatment of Secondary Hyperparathyroidism in Patients With End-Stage Renal Disease On Maintenance Dialysis TherapyYS NateNoch keine Bewertungen
- Basic Echo HaemodynamicsDokument47 SeitenBasic Echo HaemodynamicsYS NateNoch keine Bewertungen
- DocScanner 12 Apr 2023 15-46Dokument2 SeitenDocScanner 12 Apr 2023 15-46YS NateNoch keine Bewertungen
- Dudley CCG Mrsa Guideline Review v40 1597073282Dokument23 SeitenDudley CCG Mrsa Guideline Review v40 1597073282YS NateNoch keine Bewertungen
- NIH Guideline 2021Dokument116 SeitenNIH Guideline 2021YS NateNoch keine Bewertungen
- Acv AjemDokument3 SeitenAcv AjemYS NateNoch keine Bewertungen
- TCM Card-One Sided PDFDokument1 SeiteTCM Card-One Sided PDFYS NateNoch keine Bewertungen
- Medical Chinese Session 1Dokument3 SeitenMedical Chinese Session 1YS NateNoch keine Bewertungen
- Guidelines For Use: Workplace Words and Phrases - Mandarin (Chinese)Dokument6 SeitenGuidelines For Use: Workplace Words and Phrases - Mandarin (Chinese)YS NateNoch keine Bewertungen
- Medical-Chinese Booklet PDFDokument36 SeitenMedical-Chinese Booklet PDFYS NateNoch keine Bewertungen
- Medicial Terminology Origins ApproachDokument454 SeitenMedicial Terminology Origins ApproachMonica LuceroNoch keine Bewertungen
- Guideline For Research Proposal 2021Dokument35 SeitenGuideline For Research Proposal 2021farahafiqahNoch keine Bewertungen
- Pain ManagementDokument17 SeitenPain Managementa bNoch keine Bewertungen
- Randomized, Placebo-Controlled Comparison of Amitriptyline, Duloxetine, and Pregabalin in Patients With Chronic Diabetic Peripheral Neuropathic PainDokument8 SeitenRandomized, Placebo-Controlled Comparison of Amitriptyline, Duloxetine, and Pregabalin in Patients With Chronic Diabetic Peripheral Neuropathic PainTriNoch keine Bewertungen
- Old CartsDokument3 SeitenOld CartsinggitluthfiazahraNoch keine Bewertungen
- Nursing Care Plan: Saint Paul University PhilippinesDokument6 SeitenNursing Care Plan: Saint Paul University PhilippinesChristian UmosoNoch keine Bewertungen
- Protocol AkashDokument37 SeitenProtocol AkashAkash KanojiaNoch keine Bewertungen
- 17uchs05 Pharmaceutical ChemistryDokument46 Seiten17uchs05 Pharmaceutical ChemistryVadivelanNoch keine Bewertungen
- Outpatient Interventions With Suicidal Patients: Promoting Acceptance and Value-Based Problem SolvingDokument48 SeitenOutpatient Interventions With Suicidal Patients: Promoting Acceptance and Value-Based Problem SolvingsoniaNoch keine Bewertungen
- Nursing Care Plan Format Name: - Medical Diagnosis: Tetanus DateDokument2 SeitenNursing Care Plan Format Name: - Medical Diagnosis: Tetanus DateSheryl Ann Barit PedinesNoch keine Bewertungen
- Emotional Release Deepak ChopraDokument4 SeitenEmotional Release Deepak ChopraXa SancleNoch keine Bewertungen
- LifeWave X39 Pilot Demuestra Cambios Ligeros ActivadosDokument12 SeitenLifeWave X39 Pilot Demuestra Cambios Ligeros Activadosave_fenix_mileniumNoch keine Bewertungen
- Fulltext 1 To 33Dokument135 SeitenFulltext 1 To 33RAY RAMIREZNoch keine Bewertungen
- Ahad PSY101 Lab ReportDokument10 SeitenAhad PSY101 Lab ReportAbdullah Al AhadNoch keine Bewertungen
- Haad Questions (2018)Dokument54 SeitenHaad Questions (2018)SAHYA TRADCO100% (1)
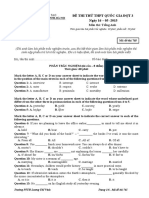
- De Thi ThuDokument6 SeitenDe Thi ThuQuynh TrangNoch keine Bewertungen
- Nyeri Kepala IAFKU, DR Betty, SPSDokument43 SeitenNyeri Kepala IAFKU, DR Betty, SPSMuhammad AsrizalNoch keine Bewertungen
- NCP MeningitisDokument6 SeitenNCP MeningitisSkyerex67% (3)
- ASKEP ANEMIA APLASTIK - Id.enDokument26 SeitenASKEP ANEMIA APLASTIK - Id.enNovia FerginaNoch keine Bewertungen
- Axinerve NP MonographDokument12 SeitenAxinerve NP MonographShama Safiana100% (1)
- Dosen Program Studi Keperawatan, Stikes Wiyata Husada SamarindaDokument9 SeitenDosen Program Studi Keperawatan, Stikes Wiyata Husada SamarindaNana MuktiNoch keine Bewertungen
- Kent Materia MedicaDokument694 SeitenKent Materia MedicaIlyas78692110100% (6)
- Cruelty's Rewards - The Gratifications of Perpetrators and Spectators Victor NellDokument48 SeitenCruelty's Rewards - The Gratifications of Perpetrators and Spectators Victor NellTernassNoch keine Bewertungen
- NEW GUIDELINES - CDC Softens Opioid Prescribing Guidelines For DoctorsDokument100 SeitenNEW GUIDELINES - CDC Softens Opioid Prescribing Guidelines For DoctorsDan LehrNoch keine Bewertungen
- Referral Letter To Specialist From Admitted PatientDokument52 SeitenReferral Letter To Specialist From Admitted PatientyazzNoch keine Bewertungen
- Psychosocial Aspect of PainDokument21 SeitenPsychosocial Aspect of PainLaiba WarisNoch keine Bewertungen