Beruflich Dokumente
Kultur Dokumente
Pathogens - Training in Microbiological Analysis of Food As of Feb. 6
Hochgeladen von
clairealbertini0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
117 Ansichten54 SeitenMicrobial analysis of pathogens in food. FDA-BAM Method
Originaltitel
Pathogens_training in Microbiological Analysis of Food as of Feb. 6
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenMicrobial analysis of pathogens in food. FDA-BAM Method
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
117 Ansichten54 SeitenPathogens - Training in Microbiological Analysis of Food As of Feb. 6
Hochgeladen von
clairealbertiniMicrobial analysis of pathogens in food. FDA-BAM Method
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 54
FOOD AND NUTRITION RESEARCH INSTITUTE
DEPARTMENT OF SCIENCE AND TECHNOLOGY
Training Manual
Microbiological Analysis of Food
PATHOGENS
This Training Manual was developed by the Food Analytical Service Laboratory (Laboratory Services
Group) of FNRI-DOST for the purpose of its training courses. This cannot be reproduced in partial or full
without the approval of FNRI.
2
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Prepared By:
MICROBIOLOGY UNIT
FOOD ANALYTICAL SERVICE LABORATORY (FASL)
LABORATORY SERVICES GROUP (LSG)
2014
3
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
TABLE OF CONTENTS
INTRODUCTION.4
(Course Description, Objectives and Mechanics)
TOPICS
Topic 1. Introduction to Food Microbiology..6
Topic 2. General Laboratory Practices........................10
LABORATORY OBSERVATION....15
METHODS OF ANALYSIS
METHOD1. Detection of Salmonella ......18
METHOD 2. Enumeration of Staphylococcus aureus ....24
METHOD 3. Enumeration of Bacillus cereus .29
METHOD 4. Detection of Listeria monocytogenes...34
ANNEXES
ANNEX A Microbiology Laboratory Safety Guidelines .....40
ANNEX B Media Preparation.41
ANNEX C Biochemical tests..42
ANNEX D Workshops/Sample Worksheets...46
ANNEX E Training Schedule.53
4
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
INTRODUCTION
Duration: One (1) hour
Learning Objectives
General: To discuss the course objectives, course content, significance of the
course, schedule of training and expected output.
Specific: After the session, the participants should be able to:
1. enumerate the objectives of the course;
2. appreciate the importance of the course in detection and/or
enumeration of pathogens; and
3. give their expectations on the course and ensure that it will be
included in the training objectives.
Training Method: Lecture with visuals and discussion; Pre-evaluation (short quiz).
Materials Needed: Lecture presentation, blank CD, laptop computer and LCD
projector, blank cassette tapes and cassette recorder for
documentation, office supplies and materials, white board marker
and eraser, quiz papers.
Content: Introduction / Overview of the Course
Course Description:
This training on microbiological analysis of food describes the testing
procedures for detection and/or enumeration of specific pathogens such as
Salmonella, Listeria monocytogenes, Staphylococcus aureus, and Bacillus
cereus. It also includes a brief introduction about food microbiology, updates on
emerging foodborne pathogens and standard methods for their detection
according to regulations. Also, it highlights the preparation and use of quality
assurance program in a food testing laboratory.
Training Objectives:
After the session, the participants should be able to:
(a) explain the importance of microbiological analysis on food samples;
5
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
(b) identify the different procedures for laboratory quality assurance and
apply good laboratory practice in the laboratory;
(c) conduct proper sampling, sample preparation and sample storage;
(d) enumerate the laboratory requirements (e.g. equipment, facilities,
reagents, laboratory supplies), and the general principles of the test
methods; and
(e) conduct microbiological analysis to detect specific pathogens such as
Salmonella, Listeria monocytogenes, Bacillus cereus, and
Staphylococcus aureus from a given food sample in the laboratory.
Training Schedule (see attached)
Training Materials
1. LCD Projector
2. Lecture presentation/ materials
3. Blank CD
4. White Board/ White Board Marker/ Eraser
5. Sound System and Microphone (Lecture)
6. Laser pointer
7. Cassette recorder and blank cassette tapes for documentation
8. Office supplies and materials (bond paper, pens, pencils, etc.)
9. Equipment/facilities, reagents and lab. Supplies for the observation
training
10. Laboratory gown
Resource Persons / Trainers FASL staff
6
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Topic 1. INTRODUCTION TO FOOD MICROBIOLOGY
Duration: One (1) hour
Learning Objectives
General: To discuss updates/ knowledge on Food Microbiology
Specific: After the session, the participants should be able to:
1. discuss Food Microbiology and its importance;
2. discuss food contamination and food safety;
3. define the existing standards and regulatory offices in the
Philippines concerning the microbiological quality of food.
Training Method: Lecture with visuals and discussion.
Materials Needed: Lecture presentation, blank CD, laptop computer and LCD
projector, office supplies and materials, white board marker and
eraser.
Content: Food Microbiology
Definition and Scope of Food Microbiology
Food Microbiology encompasses the study of microorganisms, which have both
beneficial and deleterious effects on the quality, and safety of different food
products. It focuses on the general biology of the microorganisms that are found in
the foods including their growth characteristics, identification, and pathogenesis.
Specifically, food microbiology is mostly interested on areas such as food poisoning,
food preservation, food spoilage, and food legislation.
Basic Microbiology in a glance
Microbiology is the science that deals with the study of microorganisms including
algae, bacteria, fungi, protozoa and viruses. The most abundant of all are bacteria.
Bacteria are unicellular organisms that are relatively small (0.2 to 5 m). They
reproduce asexually and have specific nutritional requirements, temperature,
humidity, pH, etc. While bacteria are most often associated with spoilage and
poisoning, some species help in the food preservation. Meanwhile, foodborne fungi
include the molds and yeasts. Molds are filamentous fungi that grow in the form of
tangled mass spreading rapidly. Yeasts, on the other hand, are unicellular fungi
reproducing by budding.
7
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Parameters that affect growth of microorganisms in foods
The following is a list of parameters that can either result to promotion of
microorganisms growth or their inhibition in certain food products.
pH
Moisture Content (Water activity)
Oxidation-reduction potential
Nutrient content. And antimicrobial constituents
Biological structures
Storage temperature and relative humidity
Presence/absence of gases
Food Contamination
In the food production chain, there are several points by which food can become
contaminated such as from the farm, processors, retailers, and consumers. These
critical points must be considered during sampling and analysis.
Food Safety Concerns:
It is a fact that diseases caused by food borne pathogens create a public health
problem worldwide. Preventing these diseases is another issue. Globally, combined
institutions and sectors of various nations have committed to improve food safety.
Countries have set microbiological criteria for raw or finished processed products.
In the Philippines, the Food and Drug Administration (Department of Health)
issued guidelines for the assessment of microbiological quality of certain processed
foods under the FDA Circular no. 2013-010. The National Meat Inspection Service
(Department of Agriculture) also issued guidelines on the assessment of
microbiological quality of fresh, chilled and frozen meat under Memorandum
Circular 9-2008-05. Several standards specific for different food products are listed
under the Philippine National Standards for foods, which are complied and
regulated by the Bureau of Product Standards (Department of Trade & Industry).
Note: These Circulars and Standards are available online.
Emerging Pathogens
Salmonella sp.
Salmonellosis is one of the most common cause of infectious diseases
transmitted by contaminated poultry foods. A critical goal in food processing
plant and governmental control agencies is to prevent Salmonella
contamination of food products and this prevention depends to a great extent
on an adequate quality control program. Salmonella detection is still highly
8
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
dependent on employing appropriate culture media. Appropriate enrichment is
important in reviving cells that may be stressed during processing of the food.
Bacillus cereus
Bacillus cereus are Gram-positive, facultatively anaerobic, endospore forming
large rods widespread in the environment and are often isolated from soil and
vegetation.
It can implicate two types of illness. The first type, called diarrheal type, is
caused by consuming contaminated food. Inside the small intestine, the
bacterium produces an enterotoxin, a large molecular weight protein, which
leads to diarrhea. The other type, called vomiting or emetic type, is associated
with a different kind of toxin produced by B. cereus. The emetic toxin produced
is a low molecular weight, pH-stable and heat- and protease-resistant toxin
that leads to nausea and vomiting.
Diarrheal type of food poisoning is often associated with meats, milk,
vegetables and fish while the vomiting type outbreaks are implicated with rice
products and other starchy products.
Staphylococcus aureus
Staphylococcus aureus are small and spherical (cocci) Gram-positive,
catalase positive bacteria appearing in pairs, short chains or in grape-like
clusters and are widely distributed in the environment.
It is one of the most resistant non-spore forming human pathogen and can
survive for extended periods in aa dry state. It is a versatile pathogen, which is
the causative agent of Staphylococcal food posioning, toxic shock syndome,
pneumonia, post-operative wound infection and nosocomial bacterimia.
Importantly, it causes sporadic food poisoning episodes around the world and
the foods often implicated include meat and meat products; poultry and egg
products; salads; bakery products; and milk and dairy products.
Listeria monocytogenes
Listeria monocytogenes was discovered as a pathogen of animals and
humans in the 1930s. As far as humans are concerned the organism was
initially identified as a cause of abortion in early pregnancy, stillbirth, or of
septicemia after an uneventful birth. Ecological surveys have demonstrated
that Listeria in general, and L. monocytogenes in particular, are naturally
occurring in a wide variety of domestic animals, particularly sheep and
chickens. L. monocytogenes has four attributes: the elevated heat resistance,
the ability for relatively rapid growth at refrigeration temperatures, a marked
tolerance of reduced pH values, and growth in the presence of over 5%
sodium chloride. L. monocytogenes have been isolated from raw staple foods
including chicken,red meat, seafood, and, of course, raw milk
Escherichia coli 0157:H57
Clostridium perfringens
Clostridium botulinum
9
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Campylobacter
Yersinia
References:
Jay, J., M.J. Loesnner & D.A Golden. (2005). Modern Food Microbiology.(7
th
ed).
USA: Springer Science Business Media.
Lampel, K.A., Al-Khaldi, S. and Cahill, S.M. Bad Bug Book: Handbook of
Foodborne Pathogenic Microorganisms and Natural Toxins. Food and
Drug Administration, USA:2012. 2nd edition.
10
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Topic 2. GENERAL LABORATORY PRACTICES
Duration: One (1) hour lecture and one (1) hour laboratory
Learning Objectives
General: To discuss the guidelines to follow in the laboratory during the
conduct of microbiological analyses of pathogens.
Specific: After the session, the participants should be able to:
1. explain the significance and principles of laboratory quality assurance;
2. apply good laboratory practice and quality assurance in the laboratory;
and
3. identify the different monitoring procedures involved in a food
processing environment and explain the purpose of each practice.
Identify and understand the quality control procedures
employed in the analysis; and
Implement the quality control procedures in the laboratory.
Training Method: Lecture with visuals, Discussion and Laboratory Demo/Tour.
Materials Needed: Lecture presentation, blank CD, laptop computer and LCD projector,
blank cassette tapes and cassette recorder for documentation, office
supplies and materials, white board marker and eraser.
Content: General Laboratory Practices
Basic Food Microbiology Skills
In testing for pathogens, it is a must that the analyst is familiar and has gained
skills on the following concepts:
1. Materials and Media Preparation (Refer to Annex D: Workshop 1)
2. Food Sampling and Preparation of Food Homogenate
3. Identification and Confirmation of Isolates
Plating skills such as Streaking for Isolation, Pour and spread plating for
enumeration are necessary in this training. Isolation of cultures is an important
step in confirming and identifying if such are the target organisms. Isolated
cultures are used in a series of biochemical and confirmation tests.
4. Gram staining, Spore Staining and Microscopy
11
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Gram staining, which is an initial step in microbial identification, is a useful aide
in differentiating the major groups of bacteria based on their cell wall
composition: the Gram positive and Gram negative bacteria. It also helps in
morphological characterization of isolates.
5. Observation and Interpretation of results
A good analyst is able to observe and properly interpret results. This is gained
through adequate training and experience.
Good Laboratory Practice
Good Laboratory Practice (GLP) describes how microbiologist and other technical
staff conduct analytical work. It includes planning, monitoring, recording, archiving
and reporting results. The goal of GLP is to get the right results. It is a must to
make all necessary preparations:
Before analysis
Make a plan of all activities such as locating the samples, reviewing the
up-to-date copy of the method available, checking that all equipment are
in good working conditions, assuring that all materials, glass ware, and
other supplies are available, sterile and properly dried, if necessary,
checking that the environmental conditions specifications are met,
ensuring that the working area is clean and disinfected, and all other
quality assurance measures are performed and results have passed the
conditions.
During analysis
Note that samples are ready (thawed out properly, if needed). Sampling
and entire analysis must be done aseptically. It is important that the
method is followed exactly as it is written. Observations and/or readings,
colony counts, biochemical reactions should be clearly and directly
recorded on the worksheets. During analysis, reference working cultures
should be used as positive and negative controls. Blank controls must
also be used to ensure sterility of the environment or of the media being
used.
After analysis
After analysis, results must be calculated accurately once all data are
recorded properly. All the laboratory glass ware and supplies used in the
analysis should be washed as soon as possible, decontaminating prior to
washing, if potential microorganisms are present. Hazardous chemicals and
decontaminated media should be disposed properly by rinsing and/or
12
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
decontamination. Equipment used must also be cleaned and/or disinfected
carefully after the work has been conducted. Samples analyzed must be
retained for a specific period of time until Report of Analysis has been
released to the customer, or as specified to the laboratorys quality manual.
Reporting the Results
Results should be translated into clear information in such a way that the
customer can understand it. Also, these must be expressed to the correct
number of significant figures or decimal places and mode of expression.
Quality Assurance in the Laboratory
General Laboratory Operations: Components of the QA program
Sample Management
Laboratory Standard Operating Procedures
Personnel
Facilities
Equipment and Instrumentation
Laboratory Glassware
Media and Reagents
Record keeping
General Safety Guidelines
The general safety guidelines being followed and implemented in the Food
Analytical Service Laboratory are written on the appendix A.
Sampling
Obtaining a proper sample for the conduct of analytical testing is of first priority.
A sample is required to be a representative of the entire lot of the food material
being evaluated. The sample must also be of proper type for the determination to
be made or for the requested analytical parameters. Lastly, the sample must be
protected against contamination and improper handling.
An appropriate sampling plan should be obtained and described by the person
acquiring and submitting the samples to the laboratory. This includes procedures
of collecting, labeling, transporting, storing and preparing samples for analysis.
Detailed sampling plans for specific food types are described in literatures.
A proper sample subjected to analysis is very important such that
laboratory results and their interpretation will only be considered valid if
13
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
samples submitted to the laboratory are representative of the lot/batch
under study or investigation.
Steps
Sample Collection
In collecting the sample, the physical state 9form, shape, particle size)
of the food product must be considered to ensure that the number of units
will be representative and/or statistically significant for its intended use.
Sample Handling and Storage
Prior to shipment, samples must be stored properly. For frozen
products, store at -20
0
C. For refrigerated products, store at 4
0
C. During
transport, an insulated material must be used. Dry products, on the other
hand, can be packed in a cardboard box-stacked and positioned
appropriately to prevent breakage. If possible, these samples must be
submitted with its original unopened packaging and be delivered to the
laboratory as soon as possible. Also, samples must be labeled properly,
clearly, and completely.
Receipt of Samples
Upon receipt, the general conditions of the sample must be noted.
Personnel receiving the sample must label and record them accurately.
Analysts must be able to analyze them immediately, if possible or if not,
be stored properly and appropriately.
Preparation of Food Homogenate for Analysis
During the preparation of food homogenate from the original sample,
aseptic conditions must be followed. Surrounding working areas must be
cleaned and disinfected as well as the hands of the analysts.
Liquid samples are thoroughly shaken while dry samples are mixed to
obtain an even distribution of microorganisms in the sample. Samples are
weighed accurately and are mixed with the appropriate diluents. Mixing of
the analytical unit to produce a food homogenate can be done by blending
or stomaching. It must be noted that upon obtaining the food homogenate,
all dilutions and inoculation of the sample to the appropriate media must
be done within 15 minutes.
Several food types require specific procedures for sampling. Consult
literatures for such.
14
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
The Use of Working Microbial Cultures during analysis
The use of positive control cultures, as well as negative control cultures, is
absolutely necessary to verify that the analysis will detect the target organism.
Microbial Monitoring of Laboratory Environment
Like the food processing environment, the food microbiology laboratory
environment must also be monitored such that sampling sites, which are possible
to harbor microorganisms that may directly or indirectly contaminate the food
product, are selected. This is especially true when working with enriched cultures
or highly contaminated samples. Monitoring is performed to verify the
effectiveness of cleaning and disinfection practices and to determine the presence
of pathogens in the working environment. Several equipment and critical work
surfaces should be included in the routine monitoring. Strategies include Surface
Contact methods and Air sampling methods.
Conclusion
The application of all the principles discussed achieves the following:
Prevention of cross-contamination of samples being examined
Protection of the personnel against infection and protection of the
environment against contamination
Assurance of the correctness of data generated from analyses through
monitoring and verification of QA system
Expression of suitability for use of the analytical procedures
References
Andrews, W.H. & Hammack, T.S. (2003). Chapter 1: Food Sampling and Preparation
of Food Homogenate. Bacteriological Analytical Manual. Retrieved from
http://www.fda.gov/Food/FoodScienceResearch/LaboratoryMethods/ucm063335.htm
Downes, F & Ito, K. (2001). Compendium of Methods for Microbiological
Examination of Foods. (4
th
ed). Washington, DC: American Public Health
Association.
15
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
LABORATORY OBSERVATION- MICROBIOLOGICAL ANALYSIS OF
FOOD : Test for Pathogens
Duration: Fifteen (15) hours laboratory
Learning Objectives
General: To discuss the techniques and quality control procedures employed
in the detection and/or enumeration of pathogens such as Salmonella
sp., Listeria monocytogenes, Staphylococcus aureus, Bacillus cereus.
Specific: After the session, the participants should be able to:
1. Follow the procedures of the test methods, apply good laboratory
practices and conduct microbial analysis in the laboratory
properly.
2. Apply and implement quality control procedures in the
laboratory
Training Method: Observation training in the Food Analytical Service Laboratory on
microbiological analysis.
Method 1 Detection of Salmonella sp.
Method 2 Enumeration of Staphylococcus aureus
Method 3 Enumeration of Bacillus cereus
Method 4 Detection of Listeria monocytogenes
Materials Needed: Laboratory supplies, Culture media/reagents, equipment for
microbiological analysis, notebook, calculator, laboratory gown,
Working Reference Cultures, Worksheets
16
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
METHODS
OF
ANALYSIS
17
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
CONTENTS
Method 1 Detection of Salmonella sp.
(FDA BAM-5, 2007)
Method 2 Enumeration of
Staphylococcus aureus
(FDA BAM-12, 2001)
Method 3 Enumeration of
Bacillus cereus
(FDA BAM-14, 2001)
Method 4 - Detection of
Listeria monocytogenes
(FDA BAM-10, 2011)
18
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
METHOD 1
Detection of
Salmonella sp.
(Culture based method)
19
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Method 1 Detection of Salmonella sp.
1. PURPOSE/SCOPE
This method of analysis is intended to detect the presence of Salmonella sp. in a
given food sample. This involves the enrichment of a portion of the sample, then
inoculation to selective secondary enrichment broths, then streaking to selective
agars. After which, confirmatory tests are performed using classical biochemical
tests.
2. SAFETY and PRECAUTIONS
2.1 Perform method in aseptic conditions, using Biological Safety Cabinet
(Class II).
2.2 Wear proper laboratory attire: laboratory gown, mask, hair cap, gloves,
closed shoes.
2.3 Precautions in media preparation and conventional culture procedure
must be observed and considered for the reliable isolation of the target
organism.
3. REFERENCES
3.1 FDA Bacteriological Analytical Manual, Chapter 5: Salmonella. 2011
3.2 Compendium of Methods for the Microbiological Examination of Foods. 4
th
ed.
3.3 Modern Food Microbiology. J. M. Jay. 1996. 5
th
edition.
4. DEFINITION
Salmonella are small, gram-negative, non-sporing rods which are widely
distributed in nature. They are the most important species responsible for
foodborne gastroenteritis. Generally, they are unable to ferment lactose, sucrose,
or salicin, although glucose and certain other sugars are fermented, with H2S
production.
20
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
5. PRINCIPLE
This culture based method is a qualitative test, which determines the presence or
absence of Salmonella in a given sample. It starts with the pre-enrichment step
using a non selective medium to resuscitate Salmonella organisms, which are
usually in low numbers in food. This is followed by selective enrichment step,
using two selective medium, to increase recovery of Salmonella. Then, three
selective agar are used for isolation of colonies. These selective media enable
the distinction of Salmonella from non-Salmonella bacteria. Subsequently,
biochemical screening is performed to characterize isolates. However, complete
identification should not be solely based on the biochemical tests since
Salmonella do not always produce typical biochemical reactions.
6. CULTURE MEDIA AND REAGENTS
All media shall be of recognized of quality. The reagent water used shall be
distilled water. Note: Culture media and reagent water should undergo quality
control check (intermediate) before use.
6.1 Lactose broth
6.2 Bactopeptone Water
6.3 Tetrathionate Broth
6.4 Rappaport-Vassiliadis Broth
6.5 Xylose Lysine Decarboxylase Agar
6.6 Bismuth Sulfite Agar
6.7 Hektoen Enteric Agar
6.8 Triple Sugar Iron Agar
Dispensed in slant positions to tubes
6.9 Lysine Iron Agar
Dispensed in slant positions to tubes. Prepare with a deep butt (4cm).
6.10 Phenol Red Broth with sugar solutions (glucose, sucrose, dulcitol,
lactose)
Prepare the phenol red broth base with 0.5% sugar solutions.
6.11 MacConkey Agar
6.12 Tryptone broth
6.13 Trypticase soy broth/Nutrient broth
6.14 MR-VP Broth
6.15 SIM Medium
6.16 Simmons Citrate Agar
6.17 Urea broth
6.18 Lysine decarboxylase broth
21
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
6.19 Kovacs Reagent
6.20 VP Reagents
6.21 Methyl red indicator
6.22 0.85% Physiological saline solution
6.23 API 20E kit
7. EQUIPMENT AND MATERIALS
7.1 Biological Safety Cabinet
7.2 Waterbath, at 43 + 2
0
C; for RV incubation
7.3 Stomacher
7.4 Top Loading Balance, calibrated
7.5 Hotplate/Microwave Oven, for melting solidified culture medium
7.6 Incubator, set at 35
0
C
7.7 Sterile pipettes
7.8 Sterile plates
7.9 Sterile tubes
7.10 Sterile wide mouth, screw cap jars/bottles
7.11 Inoculating loop and loop sterilizer
7.12 Autoclave
8. PROCEDURE
8.1 Preparation of Sample Homogenate
8.1.1 Refer to Topic 3: Sampling
8.1.2 Measure 25 analytical unit from the food sample aseptically.
8.2 Pre - enrichment
8.2.1 Mix the 25 g or ml of food sample with 225 ml of Lactose broth (or
the appropriate diluent) in a sterile container.
8.2.2 Incubate for 18-24 hours at 35
0
C.
8.3 Selective enrichment
8.3.1 Transfer 1.0ml of the incubated homogenate to 10mL freshly
prepared Tetrathionate broth. Incubate for 24 hours at 35
0
C.
22
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
8.3.2 Inoculate also 0.1ml of the homogenate to 10mL RV broth. Incubate
at 43
0
C waterbath for 24 hours.
8. 4 Inoculation to selective media
8.4.1 After incubation, streak for isolation a loopful of inoculum from TT
broth to each selective medium: XLDA, BSA, and HEA.
8.4.2 Do the same for each loopful from RV broth.
8.4.3 Invert the plates and incubate at 35
0
C for 18-24 hours.
8.5 Reading of plates
8.5.1 After incubation, observe plates for growth of typical Salmonella.
XLDA: colorless colonies with or without black center
BSA:
HEA: blue to blue green colonies with or without black center
8.5.2 If plates have mixed cultures, re-streak to MacConkey Agar to get a
pure isolate.
9. CONFIRMATION OF RESULTS
9.1 Pick at least 2 colonies from each selective agar.
9.2 Inoculate each isolate to TSI (streak then stab) and LIA (double stab then
streak) tubes. Incubate for 24 hours at 35
0
C.
9.3 Observe for red (alkaline) slant and yellow (acid) butt in TSI; purple
(alkaline) reaction in LIA butt of tube.
9.4 Subject the presumptive TSI cultures to urease test.
9.5 Test urease-negative cultures with the following biochemical tests: lysine
decarboxylase test and dulcitol fermentation test.
23
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
9.6 From the TSI culture, inoculate small growth to tryptone broth and perform
KCN, Malonate and Indole test.
9.7 When isolates are not conclusive of Salmonella, additional biochemical
tests may be performed such as lactose and sucrose fermentation tests,
MR-VP and citrate test.
9.8 As an alternative, available commercial kits can be used for rapid
identification of Salmonella.
9 REPORTING OF RESULTS
Report as Positive or Negative for Salmonella per 25 g of the given food
sample.
24
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
METHOD 2
Enumeration of
Staphylococcus aureus
(Direct Plate Count
method)
25
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Method 2 Enumeration of Staphylococcus aureus
1. PURPOSE/SCOPE
1.1 This method of analysis is intended to enumerate the coagulase-positive
Staphylococcus aureus in food samples. Since Staphylococcus aureus is
highly vulnerable to destruction by heat treatment and many sanitizing
agents. Foods must be examined for S.aureus to confirm if the organism
is the causative agent of foodborne illness, to determine whether a
food/food ingredient is a potential source of enterotoxigenic staphylococci,
and to demonstrate post-processing contamination.
2. SAFETY and PRECAUTIONS
2.1 Perform method in aseptic conditions, using Biological Safety Cabinet
(Class II).
2.2 Wear proper laboratory attire: laboratory gown, mask, hair cap, gloves,
closed shoes.
3. REFERENCES
3.1 FDA Bacteriological Analytical Manual, Chapter 10: Staphylococcus
aureus. 2001.
3.2 Compendium of Methods for the Microbiological Examination of Foods. 4
th
ed.
4. DEFINITION
Staphylococcus aureus are gram positive cocci. Their presence indicates
potential public health hazard since many strains produce enterotoxins causing
food poisoning if ingested.
5. PRINCIPLE
This direct plate count method is suitable for the analysis of foods in which more
than 100 S.aureus cells per gram may be expected.
26
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
6. CULTURE MEDIA AND REAGENTS
All media shall be of recognized of quality. The reagent water used shall be
distilled water. Note: Culture media and reagent water should undergo quality
control check (intermediate) before use.
6.1 Baird Parker Agar
Prepare as described in the Manufacturers Instructions. Separately
prepare the agar base in the appropriate amount and sterilize at 121
0
C for
15 minutes. Cool the agar at 45
0
C through circulating water bath and
aseptically add the egg yolk tellurite emulsion in proportion. Mix and
dispense about 18 to 20 ml in Petri dishes. Dry the plates prior to use.
6.2 Bactopeptone Water
Dissolve 1 gram of BPW in 1.0 L distilled water. Dispense 225 ml and 90
ml to dilution bottles. Sterilize by moist heat at 121
0
C for 15 minutes.
6.3 Brain heart infusion broth
6.4 Trypticase soy agar
6.5 Coagulase plasma (rabbit) with EDTA
6.6 Hydrogen peroxide, 3% for catalase test
6.7 Phenol red broth base with agar, or any carbohydrate fermentation
medium; with Glucose and Mannitol sugar solutions
Prepare 0.5% filter sterilized sugar solutions and aseptically add to phenol
red agar (sterilized and dispensed in tubes).
7. EQUIPMENT AND MATERIALS
7.1 Biological Safety Cabinet
7.2 Waterbath
7.3 Stomacher
7.4 Top Loading Balance, calibrated
7.5 Hotplate/Microwave Oven, for melting solidified culture medium
7.6 Incubator, set at 35
0
C
7.7 Sterile pipettes
7.8 Sterile plates
7.9 Sterile tubes
7.10 Sterile wide mouth, screw cap jars/bottles
27
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
7.11 Inoculating loop and loop sterilizer
7.12 Autoclave
8. PROCEDURE
8.1 Preparation of Sample Homogenate
8.1.1 Refer to Topic 3: Sampling
8.1.2 Mix the 25 g or mL food sample to 225 mL Buffered peptone water
and stomached for 30 seconds.
8.2 Dilution and Inoculation
8.2.1 Prepare decimal dilutions and shake dilutions vigorously for 25
times.
8.2.2 Inoculate 1mL sample suspension to 3 BPA plates distributing
inoculum equitably (0.3. 0.3, 0.4 mL).
8.2.3 Spread inoculum over surface of agar plate using sterile bent glass
rod. Retain plates in upright position until inoculum is absorbed by
the agar.
8.2.4 Invert plates and incubate for 44-48 hours at 35
0
C.
8.3 Counting and Recording Colonies
8.3.1 Observe for typical appearance of S. aureus which is circular,
smooth convex, moist, 2-3mm in diameter, gray to jet-black with off
white margin, surrounded by opaque zone, and with an outer clear
zone.
When touched with inoculating needle, colonies have buttery or
gummy consistency.
8.3.2 Select plates with 20-200 colonies. If plates have different types of
colonies, count colonies for each type, and record separately.
8. 4 Coagulase test
28
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
8.4.1 Transfer suspect S. aureus colonies into small tubes with 0.2-0.3 ml
BHI broth and emulsify thoroughly.
8.4.2 Inoculate TSA slant with the BHI suspension, for ancillary tests.
Retain these slant cultures at room temperature.
8.4.3 Incubate BHI tubes at 35
0
C for 18-24 hours.
8.4.4 Add 0.5 ml reconstituted coagulase plasma with EDTA to the BHI
culture and mix thoroughly. Incubate at 35
0
C and examine
periodically for a total of 6 hours. Observe for clotting.
8.4.5 Only firm and complete clotting is considered as positive for S.
aureus.
8.5 Ancillary tests
8.5.1 If partial clotting is observed, further testing is a must.
8.5.2 Using the growth from the TSA slant, perform Gram staining (for
microscopic observation), catalase test, anaerobic utilization of
glucose and mannitol, lysostaphin sensitivity, and thermostable
nuclease production.
8.6 Computing of results
8.6.1 Add number of colonies on triplicate plates represented by colonies
giving positive coagulase test and multiply by dilution factor. Use the
formula below for computation.
=
9. REPORTING RESULTS
Report as CFU per gram or ml of Staphylococccus aureus
29
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
METHOD 3
Enumeration of
Bacillus cereus
(Direct Plate Count
method)
30
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Method 3 Enumeration of Bacillus cereus
1. PURPOSE/SCOPE
This method of analysis is intended to enumerate Bacillus cereus. This
organism causes food poisoning when foods are prepared and held without
adequate refrigeration for several hours before serving. B.cereus is widely
distributed in nature and can be isolated from a variety of foods.
2. SAFETY and PRECAUTIONS
2.1 Perform method in aseptic conditions, using Biological Safety Cabinet
(Class II).
2.2 Wear proper laboratory attire: laboratory gown, mask, hair cap, gloves,
closed shoes.
3. REFERENCES
3.1 FDA Bacteriological Analytical Manual, Chapter 3: Aerobic Plate Count.
2001.
3.2 Compendium of Methods for the Microbiological Examination of Foods. 4
th
ed.
4. DEFINITION
Bacillus cereus is an aerobic spore forming bacterium commonly found in soil,
on vegetables, and in many raw and processed foods.
5. PRINCIPLE
Plate count method for enumerating Bacillus cereus in food samples make use of
MYP culture medium, which produces colonies of the target organism
surrounded by precipitate zone. This indicates lecithinase production. B.cereus,
in most instances, produces very strong reaction in egg yolk agar, which is
characterized by a wide zone of turbidity surrounding the individual colonies after
20-24 hour incubation.
31
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
6. CULTURE MEDIA AND REAGENTS
All media shall be of recognized of quality. The reagent water used shall be
distilled water. Note: Culture media and reagent water should undergo quality
control check (intermediate) before use.
6.1 Mannitol yolk polymyxin agar or Bacara agar
Prepare as described in the Manufacturers Instructions. Prepare
agar base separately by dissolving dehydrated medium to the appropriate
volume of water. Sterilize at 121
0
C for 15 minutes. Cool agar at 45
0
C
through circulating water bath and aseptically add 50% egg yolk emulsion
and the Polymyxin B solution in appropriate amounts.
6.2 Bactopeptone Water
Dissolve 1 gram of BPW in 1.0 L distilled water. Dispense 225 ml and 90
ml to dilution bottles. Sterilize by moist heat at 121
0
C for 15 minutes.
6.3 50% egg yolk emulsion
6.4 Polymyxin B solutions
6.5 Phenol red glucose broth
6.6 Tyrosine agar
Prepare Nutrient agar and sterilize at 121
0
C for 15 minutes.
Prepare also Tyrosine solution and sterilize at same conditions.
Aseptically add tyrosine to the nutrient agar and dispense in tubes (and
dry it in slants).
6.7 Trypticase soy-sheep blood agar
Prepare trypticase soy agar and sterilize at 121
0
C for 15 minutes. After
sterilization and cooling, aseptically add 5ml of defibrinated sheep blood
to 100 ml agar. Dispense in plates.
6.8 Motility medium
6.9 Nitrate broth, and nitrite detection reagents
6.10 Lysozyme broth
6.11 Modified VP medium, and VP Reagents
6.12 Gram stain kit
7. EQUIPMENT AND MATERIALS
7.1 Biological Safety Cabinet
7.2 Waterbath
7.3 Stomacher
7.4 Top Loading Balance, calibrated
7.5 Hotplate/Microwave Oven, for melting solidified culture medium
32
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
7.6 Incubator, set at 30
0
C
7.7 Sterile pipettes
7.8 Sterile plates
7.9 Sterile tubes
7.10 Sterile wide mouth, screw cap jars/bottles
7.11 Inoculating loop and loop sterilizer
7.12 Autoclave
8. PROCEDURE
8.1 Preparation of Sample Homogenate
8.1.1 Refer to Topic 3: Sampling
8.1.2 Mix the 25 g or mL food sample to 225 mL Buffered peptone water
and stomached for 30 seconds.
8.2 Dilution and Inoculation
8.2.1 Prepare decimal dilutions and shake dilutions vigorously for 25
times.
8.2.2 Inoculate 0.1mL sample suspension to properly dried duplicate MYP
agar plates with each dilution of sample.
8.2.3 Spread inoculum over surface of agar plate using sterile bent glass
rod. Retain plates in upright position until inoculum is absorbed by
the agar.
8.2.4 Invert plates and incubate for 18-24 hours at 30
0
C.
8.3 Counting and Recording Colonies
8.3.1 Observe for pink colonies surrounded by precipitate zone (indicating
lecithinase production). Color becomes intense after additional
incubation.
8.3.2 Select plates with 15-150 colonies. Pick at least 5 presumptive
B.cereus colonies and transfer to Nutrient agar slants. Incubate
slants 24 hours at 30
0
C
33
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
8. 4 Confirmatory tests
8.4.1 Gram stain
Prepare gram-stained smears from slants and examine
microscopically. B.cereus appear as large Gram positive bacilli in
short to long chains; with ellipsoidal spores, centrally to
subterminally located; do not swell sporangium.
8.4.2 Other tests
Transfer 3mm loopful of culture from each slant to a sterile tube
containing phosphate buffered dilution water and suspend it. Use
the suspended culture to inoculate on the ff media for confirmatory
tests: Phenol red glucose broth, tyrosine agar, nitrate broth, modified
VP medium, and lysozyme broth.
8.6 Computing of results
8.6.1 Calculate number of Bacillus cereus cells per gram or ml of sample
using the formula below:
= .
.
9. REPORTING RESULTS
Report as CFU per gram or ml of Staphylococccus aureus
34
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
METHOD 4
Detection of
Listeria monocytogenes
(Culture based method)
35
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Method 4 Detection of Listeria monocytogenes
1. PURPOSE/SCOPE
This method of analysis is intended to detect the presence of Listeria
monocytogenes in a given food sample. It allows the analysis of foods that
contain injured L.monocytogenes cells and high populations of contaminants.
The target organism is known to be universally occurring in food and is a
well known hazard causing listeriosis, which often leads to severe
consequences, particularly in susceptible subpopulations.
2. SAFETY and PRECAUTIONS
Note: The organism to be handled is highly virulent in nature so, strict
safety precautions are demanded when working.
2.1 Perform method in aseptic conditions, using Biological Safety Cabinet
(Class II).
2.2 Wear proper laboratory attire: laboratory gown, mask, hair cap, gloves,
closed shoes.
2.3 Be especially mindful of generating aerosols during blending and mixing
procedures and be meticulous in rinsing work areas often with
bactericidal solutions.
2.4 Pregnant women or other immune-compromised personnel are prohibited
from entering laboratories in which L.monocytogenes will be analyzed.
3. REFERENCES
3.1 FDA Bacteriological Analytical Manual, Chapter 10: Detection and
Enumeration of Listeria monocytogenes. 2011
3.2 Compendium of Methods for the Microbiological Examination of Foods. 4
th
ed.
4. DEFINITION
Listeria monocytogenes is a short, gram-positive, nonsporeforming rod-shaped
bacterium that appears coccoidal in older cultures. It thrives under anaerobic to
36
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
microaerophilic conditions, preferring 10% carbon dioxide environment. It grows
over a pH range of 5 to 9.6.
5. PRINCIPLE
Successful isolation of Listeria monocytogenes depends on the choice of
method sensitive to the recovery of low-level contamination. This method
employs pre-enrichment media incubated at 35
0
C followed by plating on
selective/differential agars. Numerous taxonomic tests are required for
confirmation. This method also utilizes the distinct ability of the organism to
display resistance to many antibiotics, which are incorporated at the pre-
enrichment medium.
6. CULTURE MEDIA AND REAGENTS
All media shall be of recognized of quality. The reagent water used shall be
distilled water. Note: Culture media and reagent water should undergo quality
control check (intermediate) before use.
6.1 Buffered Listeria Enrichment broth
6.2 Selective supplements for BLEB
Prepare the following supplements as stock solutions and filter-sterilize
them: Acriflavin HCl (10mg/L), Nalidixic acid, Sodium salt (40mg/L),
Cycloheximide (50mg/L). Store at 4
0
C and protect from light. Aseptically
add to enrichment after 4 hr incubation (Refer to procedures below).
6.3 Oxford Medium
6.4 CHROMagar Listeria
6.5 3% Hydrogen peroxide, for catalase test
6.6 Sheep blood agar
Prepare Blood base no.2 as recommended and sterilize at 121
0
C for 15
minutes. Cool to 50
0
C and aseptically add 5% defibrinated sheep blood.
Dispense in plates.
6.7 Gram stain kit
6.8 Carbohydrate fermentation medium, with sugar stock solutions
Prepare carbohydrate fermentation medium (Purple carbohydrate
fermentation broth base), dispense 2.5 ml into tubes with fermentation
tubes and sterilize at 118
0
C for 10 minutes.
Prepare 0.5% solutions of dextrose, esculin, maltose, rhamnose,
mannitol and xylose. Filter sterilize each solution.
Aseptically add each solution to a tube.
37
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
6.9 Nitrate broth, and Nitrite detection reagents
6.10 Trypticase soy agar with 0.6% yeast extract (TSAYE)
6.11 Trypticase soy broth with 0.6% yeast extract (TSBYE)
6.12 SIM Medium
6.13 API Listeria
7. EQUIPMENT AND MATERIALS
7.1 Biological Safety Cabinet
7.2 Waterbath
7.3 Stomacher
7.4 Top Loading Balance, calibrated
7.5 Hotplate/Microwave Oven, for melting solidified culture medium
7.6 Incubators, set at 30
0
C and 35
0
C
7.7 Sterile pipettes
7.8 Sterile plates
7.9 Sterile tubes
7.10 Sterile wide mouth, screw cap jars/bottles
7.11 Inoculating loop and loop sterilizer
7.12 Autoclave
8. PROCEDURE
8.1 Preparation of Sample Homogenate
Refer to Topic 3: Sampling
8.2 Enrichment
8.2.1 Mix the 25 g of food sample with 225 ml of Buffered Listeria
enrichment broth in a sterile container.
8.2.2 Incubate for 4 hours at 35
0
C.
8.2.3 Aseptically add the selective supplements after 4 hours incubation
and continue incubation up to 48 hours.
8.3 Inoculation
8.3.1 Streak a loopful of the incubated homogenate to OXA agar and also
to CHROMagar Listeria, as an option.
38
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
8.3.2 Incubate plates at 35
0
C for 24-48 hours.
8.3.3 Observe for black colonies with black halo due to esculin hydrolysis
in OXA medium. For CHROMagar, observe Listeria monocytogenes
for blue to blue-green colonies.
8. 4 Isolation
8.4.1 Pick at least 5 isolates and streak for isolation to TSAYE plates.
8.4.2 Incubate TSAYE plates at 30
0
C (if motility will be observed by wet
mount) or at 35
0
C.
8.4.3 Use these cultures for confirmatory tests. Prepare also Gram-
stained smears from 16-24 hr cultures. Listeria are short gram
positive rods.
9. CONFIRMATION OF RESULTS
9.1 Using the TSAYE cultures, perform the ff tests: catalase test and motility
test. Listeria spp. are catalase positive. In motility test using wet mount,
Listeria spp. can be observed as short, slim rods with tumbling motility. On
the other hand, if SIM is used, umbrella-like growth pattern will be observed
at 7 days room temperature incubation.
9.2 Perform hemolysis test. Listeria monocytogenes produces a slightly
cleared zone around the stab, indicating -hemolysis. If results are
questionable, perform CAMP test.
9.3 From the TSAYE culture, transfer a loopful to TSBYE and incubate at 35
0
C
for 24 hrs. Use this to inoculate carbohydrate fermentation media.
Positively reacting Listeria monocytogenes should produce acid but no gas
in dextrose, esculin, rhamnose and maltose; and must be negative for
mannitol and xylose.
9.4 As an alternative, pure isolates can already be used directly for API Listeria
for identification.
10 REPORTING RESULTS
Report as Positive or Negative for Listeria monocytogenes per 25 g of the
given food sample.
39
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX
A Microbiology Laboratory Safety
Regulations
B Media Preparation
C Biochemical Tests
D Workshops
E Training Schedule
40
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX A
MICROBIOLOGY LABORATORY SAFETY REGULATIONS
1. Make a plan of all the activities and make all necessary preparations before
conducting analysis or laboratory work. Read the Standard Operating
Procedures, if not yet familiar.
2. Observe safety precautions at all times.
3. Wear protective clothing (laboratory gown) when entering the laboratory. Also,
Do not wear lab clothing outside the lab
4. Do not eat, drink, chew, or smoke anything in the lab
5. Never, never, never mouth pipette
6. Keep your hands away from your face
7. Always wash your hands before and after analysis (especially after working with
the cultures).
8. Clean and sanitize all working areas by wiping them down with an appropriate
disinfectant (70% alcohol) before and after analysis.
9. Keep the laboratory equipment inside the microbiology lab. When using
instruments and equipment, read and follow the equipment operations manual.
10. Decontaminate used bottles, Petri dishes, test tubes, flasks, and other materials
that may contain potential microorganisms before washing and/or disposal.
Dispose wastes, chemicals and decontaminated cultures/materials properly and
safely.
11. In cases of spills, use forceps and cotton for wiping. Disinfect the affected areas.
Discard cotton/residues into an autoclavable bag. Flame the forceps.
12. Always work with at least another person nearby. Never work alone in the
laboratory.
13. Implement good housekeeping practices to reduce chance of accidents.
14. Follow
15. Label samples, cultures, reagents, and media with permanent markers.
16. Use proper transport vessels (test tube racks) for moving cultures in the
laboratory, and store vessels containing cultures in a leak-proof container when
work with them is complete. Laso, use safety carriers for transporting large
containers of chemicals.
17. Notify safety officer (or supervisor) of all spills, unsafe practices, and accidents.
18. If you do not understand or you are in doubt, PLEASE ASK.
Reference:
Food Microbiology: The Laboratory (by Phyllis Entis)
41
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX B
MEDIA PREPARATION
Basic Steps in Media Preparation;
1. Weigh carefully the proper amount of dehydrated medium
2. Place the requisite amount of distilled water into a suitable container
3. Add the weighed dehydrated medium to part of the water. Mix
4. Add the remaining water and mix again.
5. Check pH and adjust if necessary
6. Heat to boiling to complete dissolution using microwave, hot plate or water bath.
7. Stir often to prevent overheating and burning
8. Distribute medium to appropriate containers, making sure that the amount of
medium per container is no more than 2/3 of the containing volume of the
container.
9. Sterilize at 121
0
C for 15 minutes or according to the recommended procedures of
the medium.
10. Melt and hold media at 44 to 46
0
C until ready to use, but not exceeding 3 hours.
Reference:
Standard Methods for the Examination of Dairy Products
American Public Health Association
Chapter 4: Media and Dilution Water Preparation/
42
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX C
BIOCHEMICAL and OTHER CONFIRMATORY TESTS
Anaerobic utilization of Glucose and Mannitol
Inoculate tube of carbohydrate fermentation medium containing glucose and mannitol(0.5%). Immediately
inoculate each tube heavily with wire loop. Make certain inoculum reaches bottom of tube. Cover surface
of agar with layer of sterile paraffin oil at least 25 mm thick. Incubate 5 days at 37C. Run controls
simultaneously (positive and negative cultures and medium controls).
Acid is produced anaerobically if indicator changes to yellow throughout tube, indicating presence
of S. aureus. S. aureus is usually positive in mannitol but some strains are negative.
CAMP Test
Streak weakly -hemolytic S. aureus and R. equi vertically on sheep blood agar. Separate vertical streaks
so that test strains may be streaked horizontally between them without quite touching them. After 24- and
48-h incubation at 35 C, examine plates for hemolysis in the zone of influence of the vertical streaks.
Hemolysis of L. monocytogenes is enhanced near the S. aureus streak;
Catalase Test
Use growth from TSA slant for catalase test on glass slide or spot plate, and illuminate properly to
observe production of gas bubbles.
Citrate Test
Inoculate this agar, using needle containing growth from unclassified TSI agar slant. Inoculate by
streaking slant and stabbing butt. Incubate 96 2 h at 35C. Read results as follows:
Positive--presence of growth, usually accompanied by color change from green to blue.
Negative--no growth or very little growth and no color change.
Most cultures of Salmonella are citrate-positive.
Hemolysis test
Inoculate heavily (from TSAye colony) 5% sheep blood agar by stabbing plates that have been poured thick and dried
well (check for moisture before using). Draw grid of 20-25 spaces on plate bottom. Stab one culture per grid space.
Always stab positive controls and negative control. Incubate for 24-48 h at 35 C. Attempt to stab as near to bottom
of agar layer as possible, without actually touching bottom of agar layer and possibly fracturing the agar.
Indole Test
Transfer 5 ml of 24 h tryptophane broth culture to empty test tube. Add 0.2-0.3 ml Kovacs' reagent.
Record intermediate shades of orange and pink as .
Most Salmonella cultures give negative test (lack of deep red color at surface of broth).
KCN Test
43
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Transfer 3 mm loopful of 24 h tryptophane broth culture to KCN broth. Heat rim of tube so that good seal
is formed when tube is stoppered with wax-coated cork. Incubate 48 2 h at 35C but examine after 24 h.
Interpret growth (indicated by turbidity) as positive.
Most Salmonella species do not grow in this medium, as indicated by lack of turbidity.
Lysine Decarboxylase Test
Inoculate broth with small amount of growth from TSI slant suspicious for Salmonella . Replace cap tightly
and incubate 48 2 h at 35C but examine at 24 h intervals. Negative test is indicated by yellow color
throughout medium. If medium appears discolored (neither purple nor yellow) add a few drops of 0.2%
bromcresol purple dye and re-read tube reactions.
Salmonella species cause alkaline reaction indicated by purple color throughout medium.
Lysostaphin Sensitivity
Transfer isolated colony from agar plate with inoculating loop to 0.2 ml phosphate-saline buffer, and
emulsify. Transfer half of suspended cells to another tube (13 x 100 mm) and mix with 0.1 ml phosphate-
saline buffer as control. Add 0.1 ml lysostaphin (dissolved in 0.02 M phosphate-saline buffer containing
1% NaCl) to original tube for concentration of 25 g lysostaphin/ml. Incubate both tubes at 35C for not
more than 2 h. If turbidity clears in test mixture, test is considered positive. If clearing has not occurred in
2 h, test is negative.
S. aureus is generally positive.
Lysozyme Sensitivity
Inoculate 2.5 ml of nutrient broth containing 0.001% lysozyme with 2 mm loopful of culture. Also inoculate
2.5 ml of plain nutrient broth as positive control. Incubate tubes 24 h at 35C. Examine for growth in
lysozyme broth and in nutrient broth control. Incubate negative tubes for additional 24 h before
discarding.
Bacillus cereus grow in the presence of 0.001% lysozyme
Malonate Test
Transfer 3 mm loopful of 24 h tryptone broth culture to malonate broth. Incubate 48 2 h at 35C, but
examine after 24 h.
Most Salmonella species cultures give negative test (green or unchanged color) in this broth.
Motility Test for B.cereus
Inoculate BC motility medium by stabbing down the center with 3 mm loopful of 24 h culture suspension.
Incubate tubes 18-24 h at 30C and examine for type of growth along stab line. Motile organisms produce
diffuse growth out into the medium away from the stab. Non-motile organisms produce growth only in and
along stab.
Most strains of B. cereus are motile by means of peritrichous flagella. A few B. cereus strains are also
non-motile.
Motility Test for L.monocytogenes
Inoculate SIM or MTM from TSBye. Incubate for 7 days at room temperature. Observe daily.
44
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Listeria spp. are motile, giving a typical umbrella-like growth pattern.
MR-VP test
Inoculate medium with small amount of growth from each unclassified TSI slant suspected to contain
Salmonella. Incubate 48 2 h at 35C.
1) Perform Voges-Proskauer (VP) test at room temperature as follows: Transfer 1 ml 48 h culture to
test tube and incubate remainder of MR-VP broth an additional 48 h at 35C. Add 0.6 ml -
naphthol and shake well. Add 0.2 ml 40% KOH solution and shake. To intensify and speed
reaction, add a few crystals of creatine. Read results after 4 h; development of pink-to-ruby red
color throughout medium is positive test.
Most cultures of Salmonella are VP-negative, indicated by absence of development of pink-to-red
color throughout broth.
2) Perform methyl red test as follows: To 5 ml of 96 h MR-VP broth, add 5-6 drops of methyl red
indicator. Read results immediately. A distinct yellow color is negative test.
Most Salmonella cultures give positive test, indicated by diffuse red color in medium.
Modified VP Test
Inoculate 5 ml medium with 3 mm loopful of culture and incubate tubes 48 2 h at 35C. Test for
production of acetylmethyl-carbinol by pipetting 1 ml culture into 16 125 mm test tube and adding 0.6
ml alpha-naphthol solution and 0.2 ml 40% potassium hydroxide. Shake, and add a few crystals of
creatine. Observe results after holding for 1 h at room temperature. Test is positive if pink or violet color
develops.
Bacillus cereus shows positive VP reaction.
Nitrate Test
Inoculate 5 ml broth with 3 mm loopful of culture. Incubate tubes 24 h at 35C. To test for nitrite, add 0.25
ml each of nitrite test reagents A and C to each culture. An orange color, which develops within 10 min,
indicates that nitrate has been reduced to nitrite.
Bacillus cereus reduce nitrate to nitrite. On the other hand, Listeria monocytogenes cannot reduce
nitrates to nitrite.
Phenol Red Glucose test
Inoculate 3 mL broth with 2 mm loopful of culture. Incubate tubes anaerobically 24 h at 35C in GasPak
anaerobic jar. Shake tubes vigorously and observe for growth as indicated by increased turbidity and
color change from red to yellow, which indicates that acid has been produced anaerobically from glucose.
A partial color change from red to orange/yellow may occur, even in uninoculated control tubes, due to a
pH reduction upon exposure of media to CO2 formed in GasPak anaerobic jars.
Bacillus cereus grow and produce acid from glucose anaerobically.
Sugar Fermentation for L.monocytogenes
From TSBye culture, inoculate the following carbohydrates as 0.5% solutions in purple carbohydrate
broth (the use of Durham tubes is optional): dextrose, esculin, maltose, rhamnose, mannitol, and xylose.
Incubate 7 days at 35 C.
Positively reacting Listeria spp. produce acid with no gas.
45
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Listeria monocytogenes should be positive for dextrose, esculin, rhamnose, and maltose but negative for
mannitol and xylose.
Sugar Fermentation Tests for Salmonella spp.
Inoculate broth with small amount of growth from TSI culture. Replace cap loosely and incubate 48 2 h
at 35C, but examine after 24 h. Production of acid should be interpreted as a positive reaction. Negative
test is indicated by no gas formation in inner fermentation vial and red (with phenol red as indicator) or
purple (with bromcresol purple as indicator) color throughout medium.
Most Salmonella species give positive tests in dulcitol but negative in lactose and sucrose.
Thermostable nuclease production
Prepare microslides by spreading 3 ml toluidine blue-deoxyribonucleic acid agar on the surface of each
microscope slide. When agar has solidified, cut 2 mm diameter wells (10-12 per slide) in agar and remove
agar plug by aspiration. Add about 0.01 ml of heated sample (15 min in boiling water bath) of broth
cultures used for coagulase test to well on prepared slide. Incubate slides in moist chamber 4 h at 35C.
Development of bright pink halo extending at least 1 mm from periphery of well indicates a positive
reaction for Bacillus cereus.
Tyrosine decomposition
Inoculate entire surface of tyrosine agar slant with 3 mm loopful of culture. Incubate slants 48 h at 35C.
Observe for clearing of medium near growth, which indicates that tyrosine has been decomposed.
Examine negative slants for obvious signs of growth, and incubate for a total of 7 days before considering
as negative.
Bacillus cereus decomposes L-tyrosine.
Urease test
With sterile needle, inoculate growth from each presumed-positive TSI slant culture into tubes of urea
broth. Include control tubes (uninoculated). Incubate 24 2 h at 35C.
Urea broth turn purple-red as a positive test result. Salmonella species are negative for this test, showing
no color change in the broth.
Wet Mount Motility
Pick typical colony from culture plate incubated at 30C or less and examine by wet mount, using 0.85%
saline for suspending medium and oil immersion objective of phase-contrast microscope. Choose a
colony with enough growth to make a fairly heavy suspension; emulsify thoroughly. If too little growth is
used, the few cells present will stick to the glass slide and appear non-motile.
Listeria spp. are slim, short rods with slight rotating or tumbling motility.
Reference:
Bacteriological Analytical Manual Online
(www.fda.gov/Food/FoodScienceResearch/Laboratory/Methods/BacteriologicalAnalyticalManualBAM.htm)
46
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX D.1
WORKSHOP 1 : MEDIA PREPARATION
SAMPLE MEDIA PREPARATION LOGSHEET
Test for
Pathogen
Name of
Medium
Brand
Lot
Number
Amount
weighed
(g)
Volume
of water
used
(ml)
pH
Sterility Control
Desired
incubation
Temp
Room
Temp
+ -
Diluent BPW
Bacillus cereus
Staphylococcus
aureus
Salmonella
Listeria
monocytogenes
pH of distilled water used: ______________
Prepared by: ___________________
Date: _________________________
47
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX D.2
WORKSHOP 2 : ENVIRONMENT MONITORING
SAMPLE ENVIRONMENT MONITORING LOGSHEET
Table 1. Monitoring of Microbiology Laboratory
DAY Date
Relative
Humidity
Temperature Recorder Remarks
1
2
3
4
5
Table 2. Air Environment Sampling in the Microbiology Laboratory using Open Plate Method
Sampling Sites Media Used
Incubation
(Time and Temp.)
Results
(CFU per plate)
Remarks
(PASS/FAIL)
Checked by
WORKSHOP 3 : BASIC MICROBIOLOGY SKILLS
ACTIVITY WORKSHEET
Activity 1 Gram Staining
Gram Staining is a basic procedure necessary to the physical characterization of bacteria. It aims
to differentiate organisms based on their cell wall structure. Gram positive bacteria possess thick
peptidoglycan layer and appear as blue to purple. Meanwhile, Gram negative bacteria have thin
peptidoglycan layer and appear pink to red.
Table 1. Protocol of Gram Staining (Gephardt et al, 1981, Feedback from ASMCUE participants, ASMCUE , 2005)
Reagents Time Purpose
Primary Stain
1 minute
Mordant
1 minute
Decolorizing Agent
15 seconds
Counterstain
30 sec- 1 minute
48
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
Activity 2 Spore Staining
Some bacteria such as Bacillus cereus possess primary structures that could not easily be stained
using the typical staining reagents and protocols. Endospore is an example of a structure possessed by
B.cereus. Detection of endospores aid in proper identification and differentiation of several microbial
groups.
Spore staining is a procedure that differentiates vegetative cells from the bacterial endospores.
In this activity, Schaeffer-Fulton method will be used.
Table 2. Protocol of Endospore Staining (Schaeffer-Fulton Method)
Reagents Procedure Purpose
Primary Stain Steam for 5 minutes
Decolorizing agent Wash
Counter stain 30 seconds
Activity 3 Microscopy
Figure 1. Organism: _______________ Figure 2. Organism: ________________
Gram reaction: ___________ Gram reaction: ____________
Figure 3. Organism: __________________
49
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX D.3
WORKSHOP 4 : ENUMERATION OF Bacillus cereus
SAMPLE WORKSHEET
Sample Name: _____________________
Sample Code: ______________________
Bacillus cereus CFU/gram or ml: ____________
Computation:
Analyzed by: ___________________ Checked by: ___________________ Date: _____________
Date received:
Date analysis started:
Date analysis finished:
___________________
___________________
___________________
Dilution
MYPA
GRAM
STAIN
SPORE
STAIN
Confirmatory tests
A B
Colony
Characteristics
G
l
u
c
o
s
e
(
A
n
a
e
r
o
b
i
c
)
T
y
r
o
s
i
n
e
N
i
t
r
a
t
e
V
P
L
y
s
o
z
y
m
e
H
e
m
o
l
y
s
i
s
(
+
)
B
.
c
e
r
e
u
s
10
0
10
-1
10
-2
10
-3
10
-4
CONTROLS
Blank
(+)
(-)
50
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
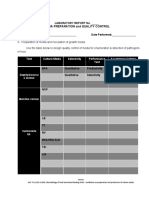
ANNEX D.4
WORKSHOP 5: ENUMERATION OF Staphylococcus aureus
SAMPLE WORKSHEET
Sample Name: _____________________
Sample Code: ______________________
Staphylococcus aureus CFU/gram or ml: ____________
Computation:
Analyzed by: ___________________ Checked by: ________________ Date: _____________
Date received:
Date analysis started:
Date analysis finished:
___________________
___________________
___________________
Dilution
BPA
COAGULASE
TEST
GRAM
STAIN
CATALASE
TEST
Ancillary tests
Counts
Colony
characteristics
G
l
u
c
o
s
e
(
A
n
a
e
r
o
b
i
c
)
M
a
n
n
i
t
o
l
(
A
n
a
e
r
o
b
i
c
)
L
y
s
o
s
t
a
p
h
i
n
T
h
e
r
m
o
n
u
c
l
e
a
s
e
10
0
0.3
0.3
0.4
10
-1
0.3
0.3
0.4
10
-2
0.3
0.3
0.4
10
-3
0.3
0.3
0.4
10
-4
0.3
0.3
0.4
CONTROLS
Blank
(+)
(-)
51
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX D.5
WORKSHOP 6: DETECTION OF PATHOGENS
Salmonella spp.
SAMPLE WORKSHEET
Sample Name: _____________________
Sample Code: ______________________
Salmonella spp. per 25 gram or ml: ____________
Analyzed by: ___________________ Checked by: ___________________ Date: _____________
Date received:
Date analysis started:
Date analysis finished:
___________________
___________________
___________________
Colony
characteristics
MAC
Urease
Test
Biochemical tests
S
a
l
m
o
n
e
l
l
a
s
p
p
TSI LIA
L
y
s
i
n
e
D
e
c
a
r
b
o
x
y
l
a
s
e
D
U
l
c
i
t
o
l
K
C
N
M
a
l
o
n
a
t
e
I
n
d
o
l
e
L
a
c
t
o
s
e
S
u
c
r
o
s
e
M
R
V
P
C
i
t
r
a
t
e
BSA
TT
RV
XLDA
TT
RV
HEA
TT
RV
CONTROLS
Blank
(+)
(-)
52
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX D.6
WORKSHOP 6: DETECTION OF PATHOGENS
Listeria monocytogenes
SAMPLE WORKSHEET
Sample Name: _____________________
Sample Code: ______________________
Listeria monocytogenes per 25 gram or ml: ____________
Analyzed by: ___________________ Checked by: ___________________ Date: _____________
Date received:
Date analysis started:
Date analysis finished:
___________________
___________________
___________________
Colony
characteristics
GRAM
STAIN
Catalase
test
Motility
test
H
e
m
o
l
y
s
i
s
C
M
A
P
t
e
s
t
Carbohydrate utilization
L
i
s
t
e
r
i
a
m
o
n
o
c
y
t
o
g
e
n
e
s
D
e
x
t
r
o
s
e
E
s
c
u
l
i
n
M
a
l
t
o
s
e
R
h
a
m
n
o
s
e
M
a
n
n
i
t
o
l
X
y
l
o
s
e
OXA
CHROM
agar
CONTROLS
Blank
(+)
(-)
53
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
ANNEX E
TRAINING SCHEDULE
Schedule Content Staff Involved
DAY 1
8:00-8:30 Welcome ceremony : Introduction to speakers and participants CSM
8:30-9:00
Course objectives/mechanics/schedule
Pre evaluation
9:00-10:00 TOPIC 1: Introduction to Food Microbiology CETC
10:00-10:15 Health Break
10:15-11:15 TOPIC 2: General Laboratory Practices CETC
11:15-11:30 Lab tour
11:30-12:00 Sample Preparation CETC
12:00-1:00 Lunch break
1:00-3:00
Workshop 1: Media Preparation
Workshop 2: Environment Monitoring (Open Plate & Use of Swab
Technique in Sampling)
CETC/CSM
3:00-3:15 Health Break
3:15-4:30
Workshop 3: Gram & Spore Staining & Microscopy
CETC/CSM
DAY 2
8:30-9:30
PRE-LAB: Isolation and detection of pathogens:
Salmonella spp. and Listeria monocytogenes
CSM
9:30-10:30 Laboratory Proper: Enrichment and Selective Enrichment CETC/CSM
10:30-10:45 Health break
10:45-12:00 Laboratory Continuation CETC/CSM
12:00-1:00 Lunch Break
1:00-2:00 Streak plating for Isolation CSM
2:00-3:15 Biochemical and Confirmatory tests for Salmonella CSM
3:15-3:30 Health break
3:30-4:30 Confirmatory tests for Listeria monocytogenes CSM
DAY 3
8:30-9:00 PRE-LAB: Enumeration of Staphylococcus aureus CETC
9:00-10:30
Laboratory Proper
Enumeration of Staphylococcus aureus
CETC
10:00-10:15 Health Break
10:15-12:00
Continuation of Laboratory :
Coagulase test and Ancillary test for S.aureus
CETC
54
Training in Microbiological Analysis of Food
Food Analytical Service Laboratory
Food and Nutrition Research Institute
Department of Science and Technology
12:00-1:00 Lunch Break
1:00-2:00 PRE-LAB: Enumeration of Bacillus cereus
2:00-3:00
Laboratory Proper on Enumeration of Bacillus cereus with
Exercise on Sampling
CETC
3:00-3:15 Health break
3:15-4:30 Continuation of B. cereus CETC
DAY 4
8:30-9:00 Biochemical Tests for Bacillus cereus CETC
9:00-10:30 POST-LAB: Bacillus cereus CETC
10:30-10:45 Health Break
10:45-12:00 POST Lab Salmonella CSM
12:00-1:00 Lunch Break
1:00-3:00 Ancillary Tests for S. aureus CETC
3:15-3:30 Health Break
3:30-4:30
Observation of plates (Pathogens)
POST-LAB: Listeria monocytogenes
CSM
DAY 5
8:30-9:30 Observation of all plates and tubes CSM
9:30-9:45 Health Break
9:45-10:15
Quality Assurance in the Laboratory
Observation of results of workshops
CSM
10:15-12:00 Interpretation of Results CETC/CSM
12:00-1:00 Lunch Break
1:00-3:00
Post Evaluation of Participants with Discussion
Health break
Post Evaluation
CETC/CSM
TOTAL no. of
hours
30 hours
Das könnte Ihnen auch gefallen
- Pathogens - TRAINING IN MICROBIOLOGICAL ANALYSIS OF FOODDokument52 SeitenPathogens - TRAINING IN MICROBIOLOGICAL ANALYSIS OF FOODclairealbertiniNoch keine Bewertungen
- Flowchart - Media QCDokument1 SeiteFlowchart - Media QCclairealbertiniNoch keine Bewertungen
- HACCP Decision Tree PDFDokument1 SeiteHACCP Decision Tree PDFclairealbertiniNoch keine Bewertungen
- Module 1 - Water - TRAINING IN MICROBIOLOGY PDFDokument40 SeitenModule 1 - Water - TRAINING IN MICROBIOLOGY PDFclairealbertiniNoch keine Bewertungen
- Media Function Incubation Control Strains Referenc e Media Method of Control Criteria Characteristic ReactionsDokument2 SeitenMedia Function Incubation Control Strains Referenc e Media Method of Control Criteria Characteristic ReactionsclairealbertiniNoch keine Bewertungen
- Ethical and Professional Practices For The Sensory Analysis of FoodsDokument3 SeitenEthical and Professional Practices For The Sensory Analysis of Foodsclairealbertini100% (1)
- Media Preparation and Quality ControlDokument3 SeitenMedia Preparation and Quality ControlclairealbertiniNoch keine Bewertungen
- Same-Different Test Analysis Using Chi-SquareDokument4 SeitenSame-Different Test Analysis Using Chi-SquareclairealbertiniNoch keine Bewertungen
- SOP 4.3 1 0 Control of DocumentsDokument4 SeitenSOP 4.3 1 0 Control of DocumentsclairealbertiniNoch keine Bewertungen
- Building-Up Competency On Color Analysis Using Visual Evaluation - Article For FNRI 2017 Annual Report - ColorDokument3 SeitenBuilding-Up Competency On Color Analysis Using Visual Evaluation - Article For FNRI 2017 Annual Report - ColorclairealbertiniNoch keine Bewertungen
- SOP-5.10 - Conduct of Sensory Evaluation (With IQC)Dokument8 SeitenSOP-5.10 - Conduct of Sensory Evaluation (With IQC)clairealbertini100% (5)
- Monthly Performance Output Report Form 2Dokument1 SeiteMonthly Performance Output Report Form 2clairealbertiniNoch keine Bewertungen
- Procedure For Isolation of Listeria MonocytogenesDokument5 SeitenProcedure For Isolation of Listeria MonocytogenesclairealbertiniNoch keine Bewertungen
- Standard Operating Procedures On Assessment of Staff Training and CompetencyDokument4 SeitenStandard Operating Procedures On Assessment of Staff Training and Competencyclairealbertini50% (6)
- Enhanced Sensory Evaluation Laboratory SoftwareDokument2 SeitenEnhanced Sensory Evaluation Laboratory SoftwareclairealbertiniNoch keine Bewertungen
- SOP-4.3-2-0 Creation, Revision and Approval of DocumentsDokument4 SeitenSOP-4.3-2-0 Creation, Revision and Approval of DocumentsclairealbertiniNoch keine Bewertungen
- SOP-5.2-2-0 Recruitmen, Screening and Selection of Candidate Sensory PanelistsDokument2 SeitenSOP-5.2-2-0 Recruitmen, Screening and Selection of Candidate Sensory Panelistsclairealbertini67% (3)
- Sensory Science 101 by IFT - How Do We TasteDokument13 SeitenSensory Science 101 by IFT - How Do We TasteclairealbertiniNoch keine Bewertungen
- Steps in Sensory EvaluationDokument1 SeiteSteps in Sensory Evaluationclairealbertini100% (1)
- Sensory Science 101 by IFT - How Do We SmellDokument11 SeitenSensory Science 101 by IFT - How Do We SmellclairealbertiniNoch keine Bewertungen
- Personnel Training Plan and Record On Equipment OperationDokument1 SeitePersonnel Training Plan and Record On Equipment Operationclairealbertini100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Presentation - Factors Affecting ClimateDokument16 SeitenPresentation - Factors Affecting ClimateAltoverosDihsarlaNoch keine Bewertungen
- Studovaný Okruh: Physical Therapist Sample Test Questions (G5+)Dokument8 SeitenStudovaný Okruh: Physical Therapist Sample Test Questions (G5+)AndreeaNoch keine Bewertungen
- Benefits of Silicone Coated Glass InsulatorsDokument10 SeitenBenefits of Silicone Coated Glass InsulatorsMuhammad Waseem AhmadNoch keine Bewertungen
- MSDS Lubriplate 105Dokument2 SeitenMSDS Lubriplate 105mackyyo0% (1)
- Subquery ProblemDokument9 SeitenSubquery ProblemAbhi RamNoch keine Bewertungen
- Workshop Manual Transporter 2016 19-29Dokument157 SeitenWorkshop Manual Transporter 2016 19-29samueleNoch keine Bewertungen
- Optical Fiber Communication Unit 3 NotesDokument33 SeitenOptical Fiber Communication Unit 3 NotesEr SarbeshNoch keine Bewertungen
- TDS Shell Spirax s6 Gxme 75w-80Dokument2 SeitenTDS Shell Spirax s6 Gxme 75w-80rstec pyNoch keine Bewertungen
- For Hand Grip Strength: NormsDokument7 SeitenFor Hand Grip Strength: NormsPraneethaNoch keine Bewertungen
- Signage Method of Statement and Risk AssessmentDokument3 SeitenSignage Method of Statement and Risk AssessmentNajmal AmanNoch keine Bewertungen
- Manual Gavita Pro 600e SE EU V15-51 HRDokument8 SeitenManual Gavita Pro 600e SE EU V15-51 HRwhazzup6367Noch keine Bewertungen
- ICSE Class 10 HRJUDSK/Question Paper 2020: (Two Hours)Dokument9 SeitenICSE Class 10 HRJUDSK/Question Paper 2020: (Two Hours)Harshu KNoch keine Bewertungen
- Installation Manual (DH84309201) - 07Dokument24 SeitenInstallation Manual (DH84309201) - 07mquaiottiNoch keine Bewertungen
- Pet 402Dokument1 SeitePet 402quoctuanNoch keine Bewertungen
- Soal 2-3ADokument5 SeitenSoal 2-3Atrinanda ajiNoch keine Bewertungen
- Data Performance 2Dokument148 SeitenData Performance 2Ibnu Abdillah MuhammadNoch keine Bewertungen
- People vs. MediosDokument10 SeitenPeople vs. MediostheresagriggsNoch keine Bewertungen
- The Ego and Analysis of Defense-Jason Aronson, Inc. (2005) Paul GrayDokument356 SeitenThe Ego and Analysis of Defense-Jason Aronson, Inc. (2005) Paul GrayClinica MonserratNoch keine Bewertungen
- Depression List of Pleasant ActivitiesDokument3 SeitenDepression List of Pleasant ActivitiesShivani SinghNoch keine Bewertungen
- PD 984Dokument38 SeitenPD 984mav3riick100% (2)
- 1 BSC Iriigation Engineering 2018 19 Std1Dokument70 Seiten1 BSC Iriigation Engineering 2018 19 Std1Kwasi BempongNoch keine Bewertungen
- Qualification of Analytical Instruments For Use in Pharmaceutical Industry-A Scientific ApproachDokument23 SeitenQualification of Analytical Instruments For Use in Pharmaceutical Industry-A Scientific Approachmicrobioasturias100% (4)
- Quality Assurance Kamera GammaDokument43 SeitenQuality Assurance Kamera GammawiendaintanNoch keine Bewertungen
- Product Sheet - Parsys Cloud - Parsys TelemedicineDokument10 SeitenProduct Sheet - Parsys Cloud - Parsys TelemedicineChristian Lezama Cuellar100% (1)
- Liquid Enema ProcedureDokument3 SeitenLiquid Enema Procedureapi-209728657Noch keine Bewertungen
- Leadership PresentationDokument10 SeitenLeadership Presentationapi-404415990Noch keine Bewertungen
- Fittings: Fitting Buying GuideDokument2 SeitenFittings: Fitting Buying GuideAaron FonsecaNoch keine Bewertungen
- Pentacam Four Maps RefractiveDokument4 SeitenPentacam Four Maps RefractiveSoma AlshokriNoch keine Bewertungen
- AQ-101 Arc Flash ProtectionDokument4 SeitenAQ-101 Arc Flash ProtectionYvesNoch keine Bewertungen
- High CarbonDokument2 SeitenHigh CarbonKarisoNoch keine Bewertungen