Beruflich Dokumente
Kultur Dokumente
Name Other Name Etiologic Agent Pathognomonic Signs Incubation Signs & Symptoms Diagnostic Test Nursing Responsibilities
Hochgeladen von
Kristine Danielle DejeloOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Name Other Name Etiologic Agent Pathognomonic Signs Incubation Signs & Symptoms Diagnostic Test Nursing Responsibilities
Hochgeladen von
Kristine Danielle DejeloCopyright:
Verfügbare Formate
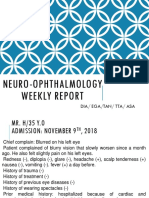
Dejelo, Kristine Danielle B.
BSNIII-A
Name Other Name Etiologic Agent Pathognomonic
Signs
Incubation Signs & Symptoms Diagnostic Test Nursing Responsibilities
Acquired Immune
Deficiency
Syndrome
AIDS Human
Immunodeficienc
y Virus
T4 less than
200mg/dl;
opportunistic
infections
Up to 10
years
Depression
diarrheal,
thrush,
weight loss,
lipodystrophy,
sinus infection,
fatigue, nausea &
vomiting,
lactic acidosis,
burning & tingling
sensation
EIA or ELISA (
enzyme-linked
immunosorbent assay)
Particle agglutination
(PA) test
Western blot analysis
Immunoflourescent test
Radio immune-
precipitation assay
(RIPA)
HIV antibody test
Health Education
Practice universal/
standard precaution
Prevention
Four Cs
1. Compliance
2. Counselling
3. Contact tracing
4. Condoms
Amoebiasis Amoebic
Dysentry
Entamoeba
histolytica
bloody mucoid
stool
3 to 4
weeks
Diarrheal
Colic
Nausea
Flatulence
Abdominal
distension
Dysentery
Anorexia
Weight loss and
weakness
Mild toxaemia
Stool exam
Blood exam
Proctoscopy/
sigmodoscopy
Observe Isolation &
enteric precaution
Provide health
education
Proper collection of
stool specimen
Skin Care
Mouth Care
Provide optimum
comfort
Diet
Anthrax Bacillus
Anthracis
A sore, especially
on the face, arms
or hands, that
starts as a raised
bump and
develops into a
painless ulcer
with a black area
in the center
One to five
days
Anthrax meningitis
Anthrax sepsis
Specimen tests
Chest x-ray
Careful history taking
Thorough physical
examination
Skin care,
psychological and
emotional support
Ascariasis Roundworm Ascaris vomiting, passing 2 months Cough, Stool for ova All members of the
Dejelo, Kristine Danielle B.
BSNIII-A
Infection Lumbricoides out of worm Fever
rales
blood- tinged
sputum,
nasal pruritus,
colicky preumbilical
pain
Severe abdominal
pain
Abdominal X- ray
Routine blood counts
family must be taught
on sanitary practices
Availability of toilet
facilities
Importance of personal
hygiene
Proper disposal of
diapers
Bacillary
Dysentery
Shigel
losis
Blood
flux
Shigella
flexneri
Shigella
boydii
Shigella
connei
Shigella
dysenteri
ae
small volume,
very bloody
stool, containing
many PMNs and
RBCs
3 to 5 days Fever
Tenesmus, nausea,
vomiting &
headache
Colicky or cramping
abdominal pain
Diarrhea with
bloody mucoid
stools
Rapid dehydration
& loss of weight
Fecalysis
Peripheral blood
examination
Blood culture
Maintain fluid &
electrolyte balance
Keep pt. warm and
comfortable
Restrict food until
nausea and vomiting
subsides
Proper personal hygiene
Botulism Clostridium
botulinum
bulbar palsy and
descending
paralysis, lack of
fever, and clear
senses and
mental status
("clear
sensorium")
12 to 36
hours
Diplopia & blurred
vision
Slurred speech
Muscle weakness
Lethargy
Poor muscle tone
Dry mouth
Fecalysis
enzyme-linked
immunosorbent
assays (ELISAs)
electrochemiluminesc
ent (ECL) tests
mouse inoculation or
feeding trials
Supportive care is
needs
In foodborne, emetics
and gastric lavage are
needed
In wound, exploration
&debridement of the
site need to be
undertaken
Candidiasis Moniliasis
Candidosi
s
Candida Albicans cheeselike
discharge
2 to 5 days Scaly skin
Nails are red &
swollen
Thrush
Whitish vaginal
discharge
Stool culture
Gram staining, for
vaginal discharge and
scaling
Avoid sharing utensils
Meticulous mouth care
Proper disposal of oral
secretions
Dejelo, Kristine Danielle B.
BSNIII-A
Chancroid Soft
Chancre
Soft sore
Sulcus
Mole
Haaemophilus
dicreyi
Painful ulcers
that have
irregular borders,
with a base which
bleeds and is
covered with a
grey material
3 to 5 days Lesions appear at
the groin or inner
thigh
Papule rapidly
ulcerates
During the healing
stage, phimosis may
develop
Gram stain of ulcer
exudate
Biopsy
Dark field
examination and
serologic test
Standard precaution
should be practiced
Check for drug allergy
Lotion, cream, or oil
should be applied on
lesions
Chlamydial
I nfections
Chlamydia
trachomatis
UTI; purulent
exudate,
generally less
viscous and
lighter in color
than gonorrhea
one to three
weeks
Cervicitis
Dysuria
Erythema
Tenderness of the
urethral meatus
Urinary frequency
Scrotal swelling
urethral discharge
Swab the site of
infection
Culture of aspirated
materials
ELISA
Direct fluorescent
antibody test
Practice universal
precaution
Suggest that both
partners should submit
for HIV testing
Check new-borns for
chlamydial infection
Chickenpox Varicella Herepes virus
varicellae
vesiculopopular
lesions
10 to 21
days
Mild fever and
malaise
Eruptive stage
Complement fixation
test
Microscopic
examination of
vesicular fluid
Respiratory isolation
Prevent secondary
infections
Cut fingernails short
Child must wear
mittens
Provide activities to
keep children occupied
Cholera El Tor Vibrio Cholerae
Vibrio coma
rice-watery stool 1 to3 days Acute, profuse
watery diarrhea
Rice water-like stool
Vomiting
Poor tissue turgor
Cold skin
Cyanosis
Breathing is rapid
and deep
Rectal swab
Dark field or phase
microscopy
Stool exam
Medical aseptic
protective care
Enteric isolation
V/S record properly
Proper preparation of
food
Observed
environmental
sanitation
Dengue Fever Breakbone
fever
Flavivirus
Arbovirus
purplish or
violaceous red
3 to 14
days
malaise and
anorexia
Tourniquet test
Platelet count
Pt. should be kept on a
mosquito free
Dejelo, Kristine Danielle B.
BSNIII-A
Hemorrha
gic fever
Dandy
fever
Infectious
Thromboc
ytopenic
Purpura
lesions with
blanched areas
about 1 cm or
less in size
fever and chills
nausea and vomiting
Petechial
Hemoconcentration
Occult blood
Haemoglobin
determination
environment
Keep pt.at rest during
bleeding
VS must be promptly
monitored
Observe for signs of
shock
Monitor vital signs
Put on trendelenburg
position
Diphtheria Corynebacterium
diptheriae
pseudomembrane
, Grayish-white,
leathery in
consistency.
2 to 5 days Fatigue
Malaise
Slight sore throat
Elevated temp.
Cervical adenitis
Body malaise
Bulls neck
Breathing difficulty
Husky voice
Increased heart rate
Stridor
Swelling of palate
Virulence test
Schick test
Molony test
Loeffler slant
Take full bed rest for at
least two weeks
Soft diet is recommend
Drink fruit juices rich in
vitamin C
Ice collar must be
applied
Nose and throat must be
taken care of
Encephalitis Brain fever Bacteria, viruses,
fungi, rickettsia,
toxins chemical
substance or
trauma
full or bulging
fontanel;
seizures, stupor,
coma, and related
neurological
signs
5 to 15 days Fever, chills,
headache, nausea,
and vomiting
Decreased IQ
Serious brain
damage
Stiff neck,
confusion, and
neurologic
manifestation
CSF analysis
Serological test
ELISA (IgM)
Polymerase chain
reaction
Provide comfort
Prevent complications
Monitor Intake and
Output
Filariasis Elephantiasis Wuchereria
bancrofi
Brugia
thickening of the
skin and
underlying
Eight to
twelve
months
On and off chills
Headache
Fever
Circulating filarial
antigen (CFA)
Patients history
Health education &
information
dissemination
Dejelo, Kristine Danielle B.
BSNIII-A
malayi
Brugia timori
Loa loa
tissues, especially
in the legs and
male genitals
Swelling,
Redness,Pain in the
scrotum
taking Environmental
sanitation
Psychological and
emotional support
Personal hygiene must
be encouraged
Course of the disease
must be explained
German Measles Rubella
Three-
day
measles
Rubella virus mild enanthem of
petechial lesions
(Forschei-mers
spots)
14to 21 days Intra uterine growth
retardation
Congenital rubella
syndrome
Blueberry muffin
skin
Lethargy and
hypothermia
Virus isolation and
identification
ELISA
Detection of rubella
antibodies
Pt. should be isolated
Pt. should be advised to
rets in bed
Room must be darken
to avoid photophobia
Take mild liquid but
nourishing diet
Eye should be irrigated
with normal saline
Ears must be taken care
of
Good ventilation
Encouraged to
increased oral fluid
intake
Gonorrhea Clap
Flores
blanca
s
Gleet
Neisseria
gonorrhoea or
gonococcus
thick purulent
discharge
21 days Burning sensation
and frequent
urination
Yellowish purulent
vaginal discharges
Dysuria with
purulent discharges
Rectal infection in
homosexual
Prostitis
Urethritis
Pelvic pain and
Inoculation of
specimen on Thayer-
Martin medium
Gram stains
Practice standard
precautions
All information on pts.
Must be confidential
Patient should be
isolated
Apply moist heat on the
affected side
Dejelo, Kristine Danielle B.
BSNIII-A
fever
Hepatitis A Infectiou
s
hepatitis
Catarrhal
jaundice
Hepatitis A virus Jaundice 15 to 0 days Flu like illness with
chills
Diarrhea, fatigue
and abn. Pain
Loss of appetite
Jaundice and dark
colored urine
HAV and HBV
Liver function test
Bile examination of
stool and urine
samples
SGOT, SGPT, ALT
IgM level
Pt. must be isolated
Encouraged to rest
Nutritional status must
be improve
Observe for melena
Optimum skin and oral
care
Hepatitis B Serum
hepatitis
Hepatitis B virus Jaundice 50 to 189
days
Fever, malaise and
anorexia
Nausea, vomiting,
abdominal pain,
Jaundice, dark urine
and pale stools
Complement fixation
test
Radio immune assay
hemaglutinin test
Liver function test
Bile examination in
blood and urine
Blood count
Serum transaminase-
SGOPT, SGPT, ALT
HBsAg
Hepatitis C Blood
borne
hepatitis
Non-A,
non-B
hepatitis
Hepatitis C virus Asymptomatic No vaccines are
available
Hepatitis D Hepatitis D virus
or delta virus
Jaundice Cannot exist without
hepatitis B
Hepatitis E Hepatitis E virus Fatigue, anorexia,
body malaise,
headache, arthralgia,
myalgia,
photophobia nausea
and vomiting
Changes in pts.
Smell and taste
Serum aspartate
aminotransferase
levels and serum
alanine amino
transferase
Serum alkaline
phosphatase levels
Serum bilirubin
Large meal must be
eaten in the morning
Provide diversional
activities
Encourage anorexic pts
to take juicesoccasional
ice chips to maintain
hydration
Dejelo, Kristine Danielle B.
BSNIII-A
Moderate grade
fever
levels
Prolonged
prothrombin time
Liver biopsy
Monitor weight daily
Observe stools for color
consistency and amount
Non Viral
Hepatitis
Toxic or drug
induced
hepatitis
Alcohol
overuse
Direct
hepatotoxici
ty
Idiosyncrati
c
hepatotoxici
ty
Cholesterol
reactions
Metabolic
and auto
immune
disorders
Jaundice Liver damage
symptoms
Herpes Simplex Virus of love Herpes simplex
virus
Common
infection of the
skin or mucosa,
may affect the
face and mouth
4 to 5 days Vesicular and
ulcerative lesions
Inflammation of the
gums
Excessive
salivation
Primary keratitis
Personal hygiene
Restoration of fluid
and electrolyte balance
Isolation of clients esp.
With those eczema
Practice universal
precaution
Herpes Zoster Shingles
Acute
posterior
Ganglioniti
s
Varicella
- zoster
Virus
lesions follow
peripheral nerve
pathway
13 to 17
days
Erthematou base of
the skin lesion
Painvarying
intensity
Fever, malaise,
anorexia, and
headache
Paralysis of the
facial nerve
Tissue culture
technique
Smear of vesicle fluid
microscopy
keep pt. comfortable
keep the pt. in strict
isolation
Apply cool, wet
dressing with NSS to
pruritic lesions
Efforts should be made
to prevent secondary
infection
Dejelo, Kristine Danielle B.
BSNIII-A
Prevent entrance of
microorg.
Assess the degree of
pain
Encourage sufficient
bed rest
Provide diversional
Activities
Hookworm
Disease
Ancylostomi
asis
Miners
disease
Egyptian
Chlorosis
Ancylostoma
duodenale
Necator
americanus
intensely pruritic
lesions
accompanied by
symptoms
40 to 100
days
Iron deficiency
anemia
Abn. Pain, diarrhea,
and urticarial
Malnourished and
undersized
Lazy, lack of energy
Perverted appetites
Pedal edema
Microscopic
examinations of feces
for the eggs
Blood exam reveals
eosinophilia
Diet high in calorie and
vitamins and minerals
Personal hygiene
should be maintained
I nfluenza La Grippe RNA- containing
myxoviruses
None 24 to 48
hours
Chilly sensation,
hyperpyrexia,
malaise, sore throat
coryza and myalgia
Severe aches and
pain at the back
GI symptoms and
vomiting
Blood examination
Viral serology
Stay at home
Drink plenty of fluids
Sponge fever down
with tepid water
Avian I nfluenza Bird flu Avian influenza
virus
Flu-like
symptoms
3 to 5 days Fever, sore throat,
cough, and in sever
case are pneumonia
Culture
polymerase chain
reaction testing
Antiviral drugs are
clinically effective
Leprosy Hansens
Disease
Hansenosis
Mycobacterium
leprae
one or more light
or slightly red
patches of skin
that appear on the
trunk or
extremities that
are less sensitive
5 and half
month to
years
Atrophy of the
muscles of the hand
Paralysis and
peripheral
anaesthesia
Loss of function
sweat glands
Tissue biopsy
Tissue smear
CBC
Isolation and medical
asepsis should be
carried out
Moral support and
encouragement
Full diet and
wholesome nutritious
Dejelo, Kristine Danielle B.
BSNIII-A
Epistaxis Special attention to
personal hygiene
Terminal disinfection
should be carried out
Leptospirosis Weils
disease
Canicola
fever
Hemorrh
agic
jaundice
Mud
fever
Swine
herd
disease
Leptospira
interrogans
orange eyes 6 to 15 days Fever last 4 to 7
days
Chills, headache
anorexia, abn. Pain
and severe
prostration
Iritis, shock, coma &
congestive heart
failure
BUN, Crea
ELISA
AST, ALT, GGT
Leptospira antigen-
antibody test (LAAT)
Leptospira antibody
test (LAT)
Isolate the patient
Urine must be properly
disposed
Darken the pts. Room
Observe meticulous
skin care to ease
pruritus
Eradicate rats and
rodents
Encourage oral fluid
intake
Malaria Ague Plasmodium
falciparum
Plasmodium
Vivax
Plasmodium
malariae
Plasmodium
ovale
fever and chills 12 days
for
falcipar
um
14 days
for
vivax
and
ovale
30 days
for p.
malariae
Paroxysms with
shaking
Rapidly rising fever
with severe
headache
Profuse sweating
Myalgia, with
feelings of
wellbeing between
Splenomegaly
Orthostatic
hypotension
Malarial smear
Rapid diagnostic test
(RDT)
Intake and output must
be closely monitored
Tepid sponges, alcohol
rubs, and ice caps on
the head during febrile
stages
Provide comfort and
psychological support
Encourage the patient
to take plenty of fluids
Bed and clothing
should be kept dry
Evaluate the degree of
anaemia
Watch out for bleeding
Measles Rubeola
Morbilli
Filterable virus Koplik s spots 10 to 12
days
Fever, catarrhal
symptoms
Cold to persistent
coughing
Nose and throat swab
Urinalysis
Blood exams ( CBC,
leukopenia,
Isolation is necessary
Control pts. High
temperature
Skin care is utmost
Dejelo, Kristine Danielle B.
BSNIII-A
Enanthems sign
Maculo popular rash
Anorexia and
irritability
Abdominal
tympanism, pruritus
and lethargy
The throat is red and
often extremely sore
leucocytosis)
Complement fixation
or hemogglutinin test
important
Oral and nasal hygiene
is very important
Oral and nodal hygiene
is a very important
Care of the eyes is
necessary
Meningitis Cerebrospinal
Fever
Pneumoccoc
us
Staphyloccoc
us
Streptococcu
s
nucchal rigidity 1 to 10 days Petechial, purpuric
or
ecchymosishaemorr
hages
Headache, fever,
vomiting and
meningeal
symptoms
Sinusarrhythmia
Irritability, photo
phobia, diplopia,
and other visual
problems
CSF analysis
Gram staining
Smear and blood
culture
Smear from petechial
Urine culture
Asses neurologic signs
often
Watch out for
deterioration of patients
condition
Monitor fluid balance
Watch out for ay side
effects of antibiotics
Position the patient
carefully to prevent
joint stiffness and neck
pain
Maintain adequate
nutrition and
elimination
Ensure the patients
comfort
Provide reassurance and
support to the pt. and
the family
Follow strict aseptic
technique when treating
patients with heal
wounds or skull
fractures
Isolation is necessary
Dejelo, Kristine Danielle B.
BSNIII-A
Mononucleosis Glandular
Fever
Kissing
disease
Epstein- Barr
virus (EBV)
Sore throat
usually
accompanied by
exudative
tonsillitis
30 to 50
days
Fatigue, anorexia,
inability to
concentrate, chilly
sensation and
headache
Fever that is usually
lasts for five days,
throat and enlarged
lymph nodes
Sore throat usually
accompanied by
exudative tonsillitis
Lymphocytosis
Positive for cephalin-
cholesterol
flocculation test
Increase in
transaminase 4 levels,
especially
SGOT,SGPT and
LDH
Increased in total
IgM levels
Oral secretions should
be properly disposed of.
Clients should be
cautioned to avoid
straining or to refrain
from any strenuous
activity
Cooling measures
should be taken for
febrile patients
Encourage soft diet and
increase fluid intake
Mumps Infectios
proritis
Epidemic
proritis
Paramyxo virus swollen parotid
glands
14 to 25
days
Sudden headache,
earache, loss of
appetite, fever and
swelling of the
parotid glands
Pain is r/t the
extent of swelling
of the gland
Temperature
usually remains
moderately
elevated
Occasionally
enlargement of the
glands
Compliment
fixation test
Hemaaggglutinatio
ninhibition test
Viral culture or the
isolation test
Serum amylase
determination is the
most useful test
Medical aseptic
protective care
Oral care and overall
personal hygiene are
a must
Bed restto avoid
complications
Diversion activities
are recommended
Soft and semi -solid
foods are easily
managed
Pediculosis Phthhiriasis Pediculous
humanous
var. capitis
Pediculus
humanos var.
corporis
Phthirus
pubis or
Itching and
crawling lice
8 10 days Itching
Plicapolonica
Vagabondia
Blepharitis
Good personal hygiene
Avoid contact w/
persons suffering from
pediculosis
Dejelo, Kristine Danielle B.
BSNIII-A
pubic lice
Pertussis Whooping
Cough
Bordetella
pertussis
paroxysmal
coughs ending
with whoop
7to 14 days Catarrhal stage (
mucoidrhinorrea,
sneezing,
lacrimation, and dry
bronchial cough
Paroxysmal stage (
cough becomes
more spasmodic,
crowning inspiratory
whoop, and choking
on mucus)
Convalescent stage (
decrease in
paroxysms,
vomiting ceases)
Nasopharyngeal
swabs
Sputum culture
CBC (leucocytosis)
Isolation and medical
asepsis is necessary
Do not left unattended
Sunshine and fresh air
is important
Provide warm baths,
keep bed dry and free
from soiled linens,
Intake and output
should be closely
monitored
Pneumonia Streptococc
us
pneumonia
Staphylococ
cus aureus
Haemophilu
s influenza
Klebsiella
Pneumoniae
rusty sputum 1 to 3 days Sudden onset of
chills with rising
fever
There is stabbing
chest pain
aggravated by
respirations and
coughing
There is
paroxysmal or
choking cough
Pain in the
abdomen
Herpes may appear
on the lips
Body malaise
Diaphoresis
Convulsion and
vomiting
Chest X-ray
Sputum analysis
May be subjected to
blood/ serologic
exam
Maintain pts. airway
Teach pt. how tocough
Obtain sputum
specimens as needed
Maintain adequate
nutrition to offset
high- calorie nutrition
Provide calm
environment
Dispose secretions
properly
Dejelo, Kristine Danielle B.
BSNIII-A
Poliomyelitis Infantile
Paralysis
Heine-
Medin
Disease
Legio debilitans flaccid paralysis,
weakness or
paralysis and
reduced muscle
tone without
other obvious
cause
7 to 21 days Low lumbar pain
Occasional
vomiting
Transient paresis
Positive pandys
test
Less tendon reflex
Hypersensitivity
touch
Stool culture
Culture from CSF
Early swab
Carry out of enteric
isolation
Observe the patient
closely for signs of
paralysis
Perform neurologic
assessment
Check BP regularly
Watch for signs of
faecal impaction
Apply hot packs on the
affected limbs
Dispose excreta and
vomitus properly
Provide emotional
support
Maintain good
personal hygiene
Rabies Hydropho
bia
Lyssa
Rhabdo virus hydrophobia, a
morbid fear of
water
10 to 15
days
Fever, anorexia,
malaise, sore
throat,
copioussalivation,
lacrimation,
irritability, hyper
excitability,
apprehensiveness,
restlessness, mental
depression
Sensitive to light,
sound and
temperature
Delirium,
Aerophobia,
profuse drooling,
may exhibit
maniacal behaviour
Virus isolation from
the patients saliva
Fluorescent rabies
antibody (FRA)
Presence of Negri
bodies in the dogs
brain
Isolate the patient
Give emotional and
spiritual support
Provide optimum
comfort and provide a
quiet environment
Darken room
Pt. should not be
bathed and there must
be no running water in
the room
If IV med should be
given it must be
wrapped
Dejelo, Kristine Danielle B.
BSNIII-A
Loss of bowel and
urinary control,
progressive
paralysis,
tachycardia
Severe Acute
Respiratory
Syndrome
SARS Novel
coronavirus
Abnormal chest
x-ray and patchy
infiltrates in any
part of the lungs
Maximum
of 10 days
Sudden onset of
high-grade fever
Headache and
overall feeling of
discomfort and body
aches
Mild respiratory
symptoms at the
onset
Chest x-ray
Clinical
manifestations
Platelet and WBC
count
ELISA
Wear a mask if you
develop runny nose
Wash hands properly
and keep them clean
Build up a good
immunity
Scabies Sarcoptes Scabiei weeping itch 24 hours Itching
Lesions like
vesicles, papules and
pustules appears
Drop of oil over the
burrow, follow by
superficial scrapings
and examination of
expressed material
under a low power
microscope
Instruct clt. To apply
cream at bedtime, from
neck down to the toes
Contaminated clothing
or bedclothes should be
dry-cleaned or boiled
Advised pt. to report
any skin irritation
Schistosomiasis Bilharzia
sis
Snail
fever
Schistoma
Japonicum
Schistoma
mansoni
Schistoma
haematobiu
m
none At least 2
months
Swimmer itch
Low grade fever,
myalgia and cough
Bloody mucoid
stools
Becomes icteric and
jaundice
Fecalysis or direct
stool exam
Kato-katz technique
Liver and rectal
biopsy
ELIZA
Circumval precipitin
test (COPT)
confirmatory test
Proper waste disposal
Control of stray animals
Prohibition of people
from bathing in infested
streams
Syphilis Lues
Venereal
MorbusGa
llicus
Treponema
Pallidum
painless chancre
or ulceration
10 to 90
days
One or more
chancres in the
genitalia, anus,
nipples, tonsils or
Dark field
illumination test
Fluorescenttrepone
malantbody
Stress to the client the
importance of
completing the
treatment
Dejelo, Kristine Danielle B.
BSNIII-A
eyelids
Alopecia, nails
become brittle,
Splenomegaly,
hepatomegaly
absorption test
VDRL slide test and
rapid plasma reagent
test
CSF analysis
Practice universal
precaution
Instruct to individuals
to inform their partner
that they should be
tested and if necessary
treated
Tetanus Lockjaw Clostridium
tetani
locked jaw or
trismus
3 days to 3
weeks
Hypostatic
pneumonia
Hypoxia
Atelectasis
Transitory
hallucination
Hyper salivation,
diaphoresis,
tachycardia
Laceration of the
tongueand buccal
mucosa
Intra muscular
hematoma
physical exam
medical and
immunization
history
signs and symptoms
Active immunization
with tetanus toxoid for
adults and pregnant
women
DPT for babies and
children
Tuberculosis Kochs
disease
Phthisis
Consupm
tion
disease
Mycobacteri
um
tuberculosis
M.
Africanum
M. Bovis
initially
asymptomatic
2 to 10
weeks
Afternoon rise in
temperature
Night sweating
Body malaise and
weight loss
Dry productive
cough
Dyspnea and
hoarseness of voice
Sputum analysis for
AFB ( confirmatory
test)
Chest X-ray
Tuberculin testing
(Mantaux test PPD,
Tine test OT, heaf
test LT)
Maintain respiratory
isolation,
Admin meds. As
ordered
Always check sputum
for bloodor purulent
expectoration
Encourage to verbalize
feelings
Teach about PTB
Advised to get plenty
of rest
Be alert for signs of
drug reaction
Dejelo, Kristine Danielle B.
BSNIII-A
Typhoid Fever Salmonella
typhosaor typhi
3 cardinal signs:
ladderlike fever,
rose spots,
spleenomegaly
5 to 40 days Headache, chilly
sensation and
aching all over the
body
Nausea, vomiting
and diarrhea
Tongue protrudes,
becoming dry and
brown
Coma vigil
Typhidot
confirmatory
ELISA
Widal test
Rectal swab
Isolation by the
medical aseptic
technique
Maintain or restore
fluid and electrolyte
balance
Monitor patients vital
signs
Maintained good
personal hygiene
Watch out for signs of
intestinal bleeding
Terminal and
concurrent disinfection
Das könnte Ihnen auch gefallen
- Wings of Arian - Devri WallsDokument528 SeitenWings of Arian - Devri WallsJoseph Dela Cruz100% (4)
- Elicityl - OligoTech - Human Milk Oligosaccharides HMOs - 2011v2Dokument4 SeitenElicityl - OligoTech - Human Milk Oligosaccharides HMOs - 2011v2pascalsalvaNoch keine Bewertungen
- Communicacable Diseases in The Digestive System: Peter John P. Gono, RN, ManDokument97 SeitenCommunicacable Diseases in The Digestive System: Peter John P. Gono, RN, ManGardoke Jr. M. LansonNoch keine Bewertungen
- Communicable DiseasesDokument7 SeitenCommunicable DiseasesRaisa Robelle Quicho100% (1)
- 408.gastrointestinal Infections and Food Poisoning - RevDokument93 Seiten408.gastrointestinal Infections and Food Poisoning - RevDawn FelicianoNoch keine Bewertungen
- Hema Lesson ADokument31 SeitenHema Lesson AEbiNoch keine Bewertungen
- Vdocument - in - Acute Abdomen 55849be833f54Dokument84 SeitenVdocument - in - Acute Abdomen 55849be833f54DAveyNoch keine Bewertungen
- Typhoid FeverDokument27 SeitenTyphoid FeverDonn Alcayde100% (2)
- Problem 3 - VarlaDokument75 SeitenProblem 3 - VarlavarlavarleyNoch keine Bewertungen
- Gil P. Soriano, RN, MhpedDokument24 SeitenGil P. Soriano, RN, MhpedGil Platon SorianoNoch keine Bewertungen
- Child Care ModuleDokument6 SeitenChild Care ModuleMiriam D. GutierrezNoch keine Bewertungen
- Neonatal SepsisDokument20 SeitenNeonatal SepsisNilanduniNoch keine Bewertungen
- Referat Demam TifoidDokument30 SeitenReferat Demam TifoidBening IrhamnaNoch keine Bewertungen
- Alawiya, Jamal Tango P.Dokument18 SeitenAlawiya, Jamal Tango P.Jamal P. AlawiyaNoch keine Bewertungen
- Gastrointestinal Communicable DiseasesDokument7 SeitenGastrointestinal Communicable DiseasesFreeNursingNotes100% (1)
- Urinary Tract Infection: Mentor DR - SaralaDokument53 SeitenUrinary Tract Infection: Mentor DR - SaralaMimi Suhaini SudinNoch keine Bewertungen
- Acute GastroenteritisDokument35 SeitenAcute GastroenteritisAdil ShabbirNoch keine Bewertungen
- Acute DiarrheaDokument32 SeitenAcute Diarrheashesh100% (1)
- STDDokument49 SeitenSTDArnzz AgbulosNoch keine Bewertungen
- Admitting Conference: Bantasan, Anna Lee Clinical ClerkDokument63 SeitenAdmitting Conference: Bantasan, Anna Lee Clinical ClerkAnna Lee BantasanNoch keine Bewertungen
- NephrocystinosisDokument31 SeitenNephrocystinosisEmily EresumaNoch keine Bewertungen
- Ramel Pedro D. Tadong Post-Graduate Intern Department of PediatricsDokument5 SeitenRamel Pedro D. Tadong Post-Graduate Intern Department of PediatricsJim Christian EllaserNoch keine Bewertungen
- Morning Report Mrs AlbineDokument50 SeitenMorning Report Mrs AlbineTito Haposan TobingNoch keine Bewertungen
- Locally Endemic DiseasesDokument23 SeitenLocally Endemic DiseasesERMIAS, ZENDY I.Noch keine Bewertungen
- Communicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistDokument846 SeitenCommunicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistGrn Mynjrkxz100% (1)
- NCM 112 LEC Topic 14 Communicable DiseasesDokument6 SeitenNCM 112 LEC Topic 14 Communicable DiseasesViviene Faye FombuenaNoch keine Bewertungen
- Causes of Henoch-Schönlein Syndrome NephritisDokument6 SeitenCauses of Henoch-Schönlein Syndrome NephritisJimae Rose BaculaNoch keine Bewertungen
- 08 Common Problems That Develop During InfancyDokument48 Seiten08 Common Problems That Develop During InfancyLorelie AsisNoch keine Bewertungen
- History Taking PediatricDokument27 SeitenHistory Taking PediatricIvan DanusaputraNoch keine Bewertungen
- Case 1 Pedia Henoch Schonlein PurpuraDokument45 SeitenCase 1 Pedia Henoch Schonlein PurpuraJefferson Gumiran100% (1)
- Nursing Case Study Acute GastroDokument8 SeitenNursing Case Study Acute GastroEdilyn BalicaoNoch keine Bewertungen
- Clinical Presentation On Child With Neonatal SepsisDokument37 SeitenClinical Presentation On Child With Neonatal SepsisSREEDEVI T SURESHNoch keine Bewertungen
- Disease Info TobeprintedDokument15 SeitenDisease Info TobeprintedJack BangcoyoNoch keine Bewertungen
- Joel Vasanth PeterDokument38 SeitenJoel Vasanth PeterJoelPeterNoch keine Bewertungen
- Acute Pyelonephritis: University of La Salette College of Nursing Santiago CityDokument22 SeitenAcute Pyelonephritis: University of La Salette College of Nursing Santiago CityZNEROLNoch keine Bewertungen
- CPG On AID PPT PresentationDokument83 SeitenCPG On AID PPT Presentationsharmaine peroNoch keine Bewertungen
- Typhoid Fever: Dr. Dur Muhammad Khan (Mrcp. FRCP)Dokument52 SeitenTyphoid Fever: Dr. Dur Muhammad Khan (Mrcp. FRCP)Osama HassanNoch keine Bewertungen
- Clinical Presentation On ADDDokument39 SeitenClinical Presentation On ADDSREEDEVI T SURESHNoch keine Bewertungen
- PX-F B - CompleteDokument8 SeitenPX-F B - CompleteyayayanizaNoch keine Bewertungen
- G.I DiseasesDokument50 SeitenG.I DiseasesEdelou Alegria JumawanNoch keine Bewertungen
- Altered Genitourinary/Renal FunctionDokument14 SeitenAltered Genitourinary/Renal FunctionAshleyNoch keine Bewertungen
- Enteric Fever 3Dokument33 SeitenEnteric Fever 3Grethel H SobrepeñaNoch keine Bewertungen
- Enteric FeverDokument20 SeitenEnteric FeverLusi UtamiNoch keine Bewertungen
- CYSTIC FIBROSIS by DR Huma Bashir PDFDokument36 SeitenCYSTIC FIBROSIS by DR Huma Bashir PDFAreej TasadaqNoch keine Bewertungen
- Disorders of The Digestive SystemDokument108 SeitenDisorders of The Digestive SystemNina Lao CamamaNoch keine Bewertungen
- Gastroenteritis in ChildrenDokument48 SeitenGastroenteritis in ChildrenKelsingra FitzChivalry FarseerNoch keine Bewertungen
- Asculitis Syndromes: Emily B. Martin, MD Rheumatology Board Review April 9, 2008Dokument54 SeitenAsculitis Syndromes: Emily B. Martin, MD Rheumatology Board Review April 9, 2008Miguel M. Melchor RodríguezNoch keine Bewertungen
- Morport 12 Des 17Dokument31 SeitenMorport 12 Des 17Cindhy Karania Metta SilavattoNoch keine Bewertungen
- Paediatric Diarrhoea - Lee Way SeahDokument42 SeitenPaediatric Diarrhoea - Lee Way SeahayunisallehNoch keine Bewertungen
- 04 - Typhoid FeverDokument35 Seiten04 - Typhoid Feversoheil100% (1)
- Acute DiarrhoealDokument104 SeitenAcute DiarrhoealRahul NetragaonkarNoch keine Bewertungen
- Pediatrics NotesDokument96 SeitenPediatrics NotesErwin Jake TagubaNoch keine Bewertungen
- Kırşehir Ahi Evran Üniversitesi Sağlık Bilimleri Enstitüsü: Neonatal Sepsis & MeningitisDokument40 SeitenKırşehir Ahi Evran Üniversitesi Sağlık Bilimleri Enstitüsü: Neonatal Sepsis & MeningitisAli FalihNoch keine Bewertungen
- Typhoid FeverDokument46 SeitenTyphoid Feverdeskichinta50% (2)
- Infectious Disease SummarizeDokument7 SeitenInfectious Disease SummarizeKris Joy Limpiada100% (1)
- BHW Training Adult CareDokument123 SeitenBHW Training Adult CareWilma BeraldeNoch keine Bewertungen
- National Antibiotic Pedia GuidelinesDokument149 SeitenNational Antibiotic Pedia GuidelinesGg GreyNoch keine Bewertungen
- Digestive DiseasesDokument10 SeitenDigestive Diseaseskate_5182178Noch keine Bewertungen
- Crohn's DiseaseDokument38 SeitenCrohn's Diseasetintukmathew100% (1)
- BST Sore ThroatDokument57 SeitenBST Sore ThroatAru VinNoch keine Bewertungen
- Assesment C&G Prepare, Cook and Finish EggsDokument6 SeitenAssesment C&G Prepare, Cook and Finish Eggsعلي صالحNoch keine Bewertungen
- Med-RM - Zoo - SP-4 - Ch-17 - Strategies For Enhancement in Food ProductionDokument22 SeitenMed-RM - Zoo - SP-4 - Ch-17 - Strategies For Enhancement in Food Productionkrish masterjeeNoch keine Bewertungen
- Isopod BehaviorDokument4 SeitenIsopod BehaviorCody Griffin100% (1)
- Brain Imaging Technologies and Their Applications in NeuroscienceDokument45 SeitenBrain Imaging Technologies and Their Applications in NeuroscienceNeea AvrielNoch keine Bewertungen
- Problems and SolutionsDokument268 SeitenProblems and SolutionsMajid Mohammadi100% (1)
- Link To Publication in University of Groningen/UMCG Research DatabaseDokument54 SeitenLink To Publication in University of Groningen/UMCG Research DatabaseSrood TalibNoch keine Bewertungen
- 11.2 MovementDokument24 Seiten11.2 MovementAndyChoNoch keine Bewertungen
- How To Tell Wild Animals Q&ADokument4 SeitenHow To Tell Wild Animals Q&AUjwal vandana JhaNoch keine Bewertungen
- Quarter 4 - CompleteDokument115 SeitenQuarter 4 - Completemaria luisa mendozaNoch keine Bewertungen
- Fate of The Embryonic Germ LayersDokument3 SeitenFate of The Embryonic Germ Layersmalav1989Noch keine Bewertungen
- Road Encounters PDFDokument23 SeitenRoad Encounters PDFFederico Carrera BuronneNoch keine Bewertungen
- 1933 ConventionDokument4 Seiten1933 Conventionapi-301726216Noch keine Bewertungen
- Christofilou Tellina AnimalsDokument8 SeitenChristofilou Tellina Animalsapi-263384917Noch keine Bewertungen
- Case Report CMV RetinitisDokument27 SeitenCase Report CMV RetinitistaniamaulaniNoch keine Bewertungen
- Mandala Effects by Maryanne JohnsonDokument38 SeitenMandala Effects by Maryanne JohnsonKaren MersonNoch keine Bewertungen
- Zitelli Picture Review - GeneticsDokument101 SeitenZitelli Picture Review - GeneticsEllagEszNoch keine Bewertungen
- Supplementary Reading Exercise-1Dokument5 SeitenSupplementary Reading Exercise-1MuiesNoch keine Bewertungen
- Form 2 Science (Objective)Dokument10 SeitenForm 2 Science (Objective)Audrey Tening JNoch keine Bewertungen
- Struktur Organisasi Puskesmas DoneDokument19 SeitenStruktur Organisasi Puskesmas Donepuskesmas kepulunganNoch keine Bewertungen
- Happicuppa - English LiteratureDokument8 SeitenHappicuppa - English LiteratureNecolyn UbaNoch keine Bewertungen
- Bedroom TitanDokument70 SeitenBedroom TitanCamillo Granata100% (3)
- Lot F Chapter 4 QuestionsDokument3 SeitenLot F Chapter 4 QuestionsKanta EngNoch keine Bewertungen
- Best Books Years 7Dokument7 SeitenBest Books Years 7MagelicanNoch keine Bewertungen
- Worksheet For Morgan - Carter Laboratory #25 "Animal Development"Dokument9 SeitenWorksheet For Morgan - Carter Laboratory #25 "Animal Development"HyenaNoch keine Bewertungen
- Caning Dictionary Jun 16Dokument36 SeitenCaning Dictionary Jun 16Hakki YazganNoch keine Bewertungen
- Leishmania SPPDokument9 SeitenLeishmania SPPanalyn123Noch keine Bewertungen
- THBT Animal Testing Should Be BannedDokument3 SeitenTHBT Animal Testing Should Be BannedFabio RizalNoch keine Bewertungen
- Synonyms and Antonyms Reading Comprehension Exercises TBL Task Based Lea - 135200Dokument3 SeitenSynonyms and Antonyms Reading Comprehension Exercises TBL Task Based Lea - 135200Oyuki Torres ChoraNoch keine Bewertungen