Beruflich Dokumente
Kultur Dokumente
Jurnal CT Scan
Hochgeladen von
Pungki Putra TamaraOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Jurnal CT Scan
Hochgeladen von
Pungki Putra TamaraCopyright:
Verfügbare Formate
Mild Head Injury: Criteria for Computed Tomography Scan
Garba, I.
1
Speelman, A.
2
Tabari, AM.
3
1
Department of Medical Radiography, Bayero University Kano, Nigeria
2
Department of Radiography, Cape Peninsula University of Technology, Cape Town,
South Africa
3
Department of Radiology, Aminu Kano Teaching Hospital, Kano, Nigeria
Corresponding Author:
Garba I.
Email: babaidi2003@yahoo.com, Phone Number: +2348034532750
ARTICLE INFO
Article history
Received March 5, 2009;
Revised November 15, 2009;
Accepted December 12, 2009
Available online, 2009
Keywords:
Mild head injury, clinical
risk factors, computed
tomography
Abstract
Background/Objective: Mild Head Injury (MHI) is the most common
type of head trauma, and forms a majority of the injuries seen in the trauma
unit (65-85%).
1
This study was aimed at using previously identified
clinical risk factors to determine which category of patients with MHI
would not need to undergo Computed Tomography (CT). This may serve
as cost saving measure to patients and hospitals likewise reduce collective
radiation dose to the population.
Methodology: A retrospective study conducted at the trauma unit of a
teaching hospital situated in the Cape Metropole. CT scan images of 50
patients aged 14 years and above who had MHI and undergone CT
examination were retrieved from the archive. Patients information, clinical
history and resultant CT findings were collated. Clinical risk factors were
correlated with abnormal and normal CT scan findings. Data were
analyzed using chi-square statistic at 95% confidence interval.
Results: Twenty three (46%) of the patients had abnormal CT findings,
and all presented with one or more of these risk factors; severe headache
(10%), skull fracture (20%), scalp injury (6%), loss of consciousness
(LOC)(8%) and intoxication(2%). The results were not statistically
significant when compared with the normal CT scans group. Four patients
(8%) with no risk factors had normal CT scans. All the patients presenting
with the clinical risk factors, of nausea and vomiting 6% (n=50), seizures
4% (n=50) had normal CT scan findings.
Conclusion: Certain clinical risk factors can be used to suggest the
probability of abnormal CT scan in patients with MHI. Patients with no
risk factors such as patients with confusion and disorientation are more
likely to have normal CT findings and may therefore be exempted from CT
examination. Further studies with larger sample size may be helpful in
validating these findings.
copyright@2009 jarn-xray
ISSN1115-7976
Vol.21
X-RAYS
Contents lists available at
Journal of Association of Radiographers of Nigeria
Journal homepage: www.jarn-xray.org
X-RAY
Garba I., Speelman A. and Tabari A.M./Journal of Association of Radiographers of Nigeria, Vol. 23, (2009) 7 15.
8
INTRODUCTION
Mild Head Injury (MHI) is commonly
defined as blunt trauma to the head, after
which the patient loses consciousness for
<15 min or has a short, post-traumatic
amnesia of <1 h, or both, as well as a
normal or minimally altered mental
status on presentation, indicated by a
Glasgow coma scale (GCS) score of 13
15.
1, 2
Loss of Consciousness (LOC) is
defined as a witness viewing the patient
in a state of unconsciousness and
reporting this fact to the emergency
medical personnel. Amnesia is defined
as a patient being unable to remember or
describe the incident that led to the head
trauma in the history taken directly by
the examining physician.
3
Recently, there have been debates in
medical literature as to which patient
requires CT scan after head trauma.
Historically low GCS score has been
used as a criterion for CT scans. While,
patients with GCS scores of 13 and
above believed to have only MHI, have
often simply observed. Research has
shown that a significant number of
patients with the GCS of 13 and above
had significant brain injuries, and early
CT scan is recommended in this group of
patients.
3, 4
Other studies have shown that, very few
patients with MHI and GCS score of >13
require intervention and most of the
abnormalities seen on CT scans are
minor. These have led to the possibility
of a less conservative approach with
regard to the patients management.
1
This study was aimed at using previously
identified clinical risk factors for the
South African context, to classify
patients with MHI and GCS score of 13
and above who may not need to undergo
CT scan. It is envisaged that this may
reduce medical costs to patients and
hospitals as well as contribute to the
reduction of the populations collective
dose from CT scans.
METHODOLOGY
Our study was retrospective and
conducted at the trauma unit of a
teaching hospital in Cape Town, South
Africa. Ethical clearance was obtained
from the Cape Peninsula University of
Technology (CPUT) ethics committee,
CT scan results of patients performed
between January and December 2008
were retrieved from the archive. Only
patients aged 14 years and above, with
MHI and who had undergone CT scans
of the brain were included in this study.
The reason for excluding 14 years and
younger was because, the abnormalities
on CT scan are so common and severe in
patients below this age limit.
5
All CT
scans were performed on a Siemens
Somatom Balance (K1508) CT scanner
manufactured in Erlangen Germany.
Information derived from the patients
records include, age, sex, GCS score,
clinical request, clinical history and
resultant CT findings. The clinical
history recorded on the request forms
included, severe headache, nausea,
vomiting, suspected skull fracture, LOC,
seizures, scalp injury and intoxication
these were all considered as clinical risk
Garba I., Speelman A. and Tabari A.M./Journal of Association of Radiographers of Nigeria, Vol. 23, (2009) 7 15.
9
factors. However, clinical history of
confusion and disorientation were
regarded as non-risk factors based on the
literature reviewed.
1-4, 6,8
The
mechanisms of head injury were
classified as: assault, Motor Vehicle
Accident (MVA), Pedestrian Vehicle
Accident (PVA), and others ( for
example domestic accident (DA) or no
cause stated)
6
as recorded on the request
forms. Patients ages were classified on
the basis of the WHO age classifications
7
as: adolescent (14-18) years, young adult
(19-39) years, adult (40-59) years and
old adult (60 and above) years.
Clinical risk factors and mechanisms of
the head injury were correlated with
normal and abnormal CT scan groups
respectively. The distribution of GCS
scores were correlated with normal and
abnormal CT scan findings. Age
distribution of patients with abnormal
and normal CT scans. The distribution of
the abnormal CT scan findings in
patients with clinical risk factors were
also analyzed.
An abnormal CT scan was defined as
one showing an acute traumatic lesion
such as contusion, parenchymal
hematoma, epidural hematoma, subdural
hematoma, subarachnoid haemorrhage or
a skull fracture as described in the
literature.
4
Data were analyzed with the chi-square
binary analysis. Relative risk and Odd
ratio (at 95% confidence interval (CI)
were calculated with their corresponding
p values.
RESULTS
A total of 50 CT scan images were
evaluated. These were made up of 42
(84%) males and 8 (16%) females.
Subjects whose images were used were
aged between 14 and 100 years (mean
SD 33.5210.2 years). There were
23(46%) patients who had abnormal
scans (epidural haemorrhage (4%),
subdural haemorrhage (6%), skull
fracture (14%), contusion (16%),
subarachnoid haemorrhage (2%),
intraventricular haemorrhage (4%) and
27 (54%) patients had normal CT
findings.
No statistically significant difference
was noted between the abnormal and
normal CT scan groups with respect to
the mechanism of the head injury.
However, most of the injuries were
sustained as a result of assault 52% (n
=26), and the least was from others 20%
(n =10) (Table1).
Garba I., Speelman A. and Tabari A.M./Journal of Association of Radiographers of Nigeria, Vol. 23, (2009) 7 15.
10
Table 1: Mechanism of head injury versus abnormal CT scans.
Mechanism of head injury Abnormal
CT scans
n =23 (%)
Normal
CT
scans
n =27 (%)
P=value
Assault 12 (52) 14 (51.9) 0.9819
MVA/PVA 7 (30.4) 7 (25.9) 0.7234
Others (domestic accident or no cause stated) 4 (17.4) 6 (22.2) 0.6704
TOTAL 23 (100) 27(100)
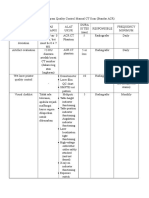
Table 2 compared patients with
abnormal and normal CT scans with
respect to the clinical risk factors. Severe
headache, suspected skull fracture, LOC,
scalp injury and intoxication were more
likely causes of abnormal CT scan
findings, even though, no statistically
significant difference was noted between
the two groups. About 46% of the
subjects with abnormal CT findings had
associated risk factors. Some 8% of the
subjects without risk factors had normal
CT findings. Patients presenting with the
clinical risk factors of nausea and
vomiting 6% (n =3), seizures 4% (n =2),
had normal CT scan findings.
Table 2: Comparison of Clinical Risk Factors in Normal and Abnormal CT scan Groups.
Clinical Risk
Factors
Normal CT
scan
n =27 (%)
Abnormal CT
scan
n =23 (%)
Odds
ratio
(at 95%
CI)
Relative
risk (at
95% CI)
P values
Severe headache 5 (18.5) 5 (21.7) 0.8182 0.8519 0.7766
Nausea 1 (3.7) 0(0) 2.66 - 0.3512
Vomiting 2 (7.4) 0 (0) 4.608 - 0.1828
Suspected skull
fracture 7 (25.9) 10 (43.4) 0.455 0.5963 0.1916
LOC 3 (11.1) 4 (17.4) 0.5938 0.6389 0.5236
Seizures 2 (7.4) 0 (0) 4.608 - 0.1828
Scalp injury 3 (11.1) 3 (13) 0.8333 0.8519 0.834
Intoxication 0 (0) 1 (4.3) 0.2727 0.000 0.2737
Non-risk factors 4 (14.8) 0 (0) 9.000 - 0.0543
TOTAL 27 (100) 23 (100)
Contusions 8(34.8%) and skull fractures
7(30.4%) were the most frequent CT
findings respectively. The least CT
findings were subarachnoid haemorrhage
with a 1(4.3%) (Table 3).
Garba I., Speelman A. and Tabari A.M./Journal of Association of Radiographers of Nigeria, Vol. 23, (2009) 7 15.
11
Table 3: Distribution of abnormal CT scan findings
Abnormal CT findings Number of patients with clinical risk
factors n =23 (%)
Epidural hematoma 2 (8.7)
Subdural hematoma 3 (13.0)
Skull fracture only 7 (30.4)
Contusion 8 (34.8)
Subarachnoid haemorrhage 1 (4.3)
Intraventricular haemorrhage 2 (8.7)
TOTAL 23 (100)
The subjects aged 19-39 years had the
highest incidence of MHI 32(64%) and
the highest abnormal CT findings
18(78.3%). Subjects of 60 years and
above recorded the lowest incidence
(Table 4).
Table 4: Age distribution of MHI for CT scans
Age Abnormal CT scans
n =23 (%)
Number of patients
n =50 (%)
14-18 2 (8.7) 7 (14)
19-39 18 (78.3) 32 (64)
40-59 2 (8.7) 6 (12)
60 and above 1 (4.3) 5 (10)
TOTAL 23 (100) 50 (100)
Patients were divided into 3 groups
based on their GCS score, 15(32
patients), 14(14 patients) and 13(4
patients) (Table 5).
Table 5: Distribution of GCS in patients with normal and abnormal CT scans.
GCS score Abnormal CT
scans
n =23(46%)
Normal CT
scans
n =27(54%)
TOTAL
n =50(100%)
P = values
15 14(28%) 18(36%) 32(64%) 0.7984
14 7(14%) 7(14%) 14(28%) 0.7640
13 2(4%) 2(4%) 4(8%) 0.8725
DISCUSSION
Mild head injury is the most common
type of head trauma, and represents the
vast majority seen in the trauma unit (65-
85%).
1
Some authors have reported that,
a 10% reduction in the number of CT
scans of these patients would save more
than 20 million rands per annum, beside
the reduction in radiation dose.
8
Garba I., Speelman A. and Tabari A.M./Journal of Association of Radiographers of Nigeria, Vol. 23, (2009) 7 15.
12
Despite the high incidence and numerous
studies performed, there is much
controversy about correct evaluation of
these patents
9
. The question of how best
to define MHI is of great importance,
and is a source of controversy. Some of
these patients will harbour a life
threatening injury, while some may have
neurocognitive sequelae for days to
months after the head injury. The
challenge to the emergency physician is
to identify which patients will have acute
intracranial brain injury, and which
patients could be safely sent home.
10
Saboori et al
9
, reported that, some
clinical risk factors could be used to
predict the probability of abnormal CT
scans.
9
The use of these clinical risk
factors as predictor of intracranial
lesions in patients with MHI has been
evaluated in several studies. In two
studies it has been found that, selective
use of CT on the basis of clinical
findings such as severe headache,
vomiting and age over 60 years after
MHI with GCS score of >13 identified
96 percent and 98 percent respectively of
patients with abnormalities on CT
scans.
8
Similarly, Miller et al
2
studying the
clinical significance of risk factors like
severe headache, nausea, vomiting and
depressed skull fracture found that
significant number of patients with CT
abnormality had these risk factors
identified in our study. They concluded
that if CT scans in minor head injury
were done only on patients with these
risk factors there would be 61%
reduction in number of CT scan done,
and still identifying all patients who
require neurosurgical intervention. This
correlates with findings of this study, in
which severe headache, LOC, suspected
skull fracture; intoxication and scalp
injury were likely causes of abnormal
CT scan findings. In this study, however,
these risk factors identified 46% (n =23)
of the patients with abnormal CT scans
(Table 2). Similar findings have been
reported by the previous studies.
3,8, & 11
All the patients presented with risk
factors like nausea and vomiting 6% (n
=3), seizures 4% (n =2) had normal CT
scan findings (Table 2). Even though, all
the values were not statistically
significant, this could probably due to
our small sample size.
GCS is a numerical expression of the
severity of head injury that can be used
to correlate various levels of coma with
later clinical outcome.
12
Jagoda et al
10
reported that, the use of GCS score alone
is not a good predictor of underlying
brain/skull injury in patients with MHI.
This may perhaps provide an explanation
for the findings in this study in which,
28% (n=14) of the patients, with a GCS
score of 15 had abnormal CT scans
(Table 5).
Abdullatip et al in their study noted that,
most of the patients with MHI were
young-adults.
13
This is in line with
finding in the present study in which
patients in this age group represented
64% of the patients with MHI, and
78.3% of the patients with abnormal CT
findings (Table 4). However, most of the
Garba I., Speelman A. and Tabari A.M./Journal of Association of Radiographers of Nigeria, Vol. 23, (2009) 7 15.
13
mechanisms of the injuries were as a
result of assaults 52% (n =26) (Table
1).This might be due to the fact that,
young adults engaged themselves with
activities that could easily cause violence
like alcohol abuse and, or reckless
driving. Similar finding had also been
reported by Bordignon et al.
14
However,
more males 84% (n =42) presented with
MHI than females. This is in keeping
with findings from the previous
studies.
10, 13, 15 &16
Contusions 34.8% (n
=8) and skull fractures 30.4% (n =7)
were the most common abnormal CT
findings found in this study (Table 3),
which correlates with findings of
Bordignon et al.
14
The results show that, 46% (n =23) with
abnormal CT scan findings, and all had
one more of these clinical risk factors
namely; severe headache, LOC,
suspected skull fracture, scalp injury and
intoxication (Table 2). These included 14
patients with GCS score of 15, 7 patients
with GCS of 14, and 2 patients with
GCS of 13 (Table 5). Likewise, patients
with non-risk factors (confusion and
disorientation) 8% (n =4), had normal
CT findings in this study (Table 2). This
correlated with the result reported by
Heydel et al whereby all the patients
with positive CT scans had at least one
of the risk factors such as (headache,
vomiting, alcohol intoxication, and
seizures), and all the patients without
any of the risk factors had normal CT
scans.
8
It may therefore be necessary for CT
scan investigation in patients with MHI
to be preserved only for patients with
certain clinical risk factors such as
severe headache, suspected skull
fracture, intoxication, LOC, and scalp
injury, because, a significant number of
these patients have abnormal CT scan
findings. Whereas, those patients without
any of the clinical risk factors for MHI
should be exempted from CT scanning,
as the probability of abnormal CT scans
in this group of patients is a remote
possibility.
The limitation of our study includes:
small sample size used due to time
constrain, thus, the results were not
significant. Study with larger sample size
could be carried out to validate the
findings of this study.
CONCLUSION
The study has established clinical risk
factors that could be used to screen
patients with MHI that are likely to have
abnormal CT findings such as severe
headache, LOC, intoxication, scalp
injury or suspected skull fracture. Other
group of patients without any of these
factors may have normal CT findings
hence do not need to undergo CT scan.
ACKNOWLEDGEMENTS
We would like to thank Dr S. Candy
(Neuroradiologist), for taking her time to
go through our proposal, and guide
through the data collection process. Our
humble appreciations also, go to Dr
Alistair Hunter and Mr. Christoph
Trauernicht for their statistical help.
Garba I., Speelman A. and Tabari A.M./Journal of Association of Radiographers of Nigeria, Vol. 23, (2009) 7 15.
14
REFERENCES
1. Sleyman, T., Altug H., Abdulkadir
G., and Mustafa Y. Clinical Decision
Instruments for CT scan in Minor
Head Trauma. The Journal of
Emergency Medicine, 2008
34(3):253-259.
2. Lisa R.M., Shu B.C., Julio C.S and
Teresina M.H. The Use of Head
Computed Tomography in Elderly
Patients Sustaining Mild Head
Trauma. The Journal of Emergency
Medicine, 2003, 24(2):157-162.
3. Miller, E.C., Holmes, J.F., and
Derlet, R.W. Utilizing Clinical
Factors to Reduce Head CT scan
Ordering for Minor Head Trauma
Patients. The Journal of Emergency
Medicine, 1997 15(4):453-457.
4. Miller, E.C., Derlet R.W., Kinser D.
Minor Head Trauma: Is Computed
Tomography Always Necessary?
Ann Emergency Med, 1996, 27:290-
294.
5. Murgio, A., Patrick, P.D., Andrade,
F.A., Boettos, S., Leung, K.M.,
Munoz, S.M.A. International Study
of Emergency Department Care for
Paediatric Traumatic Brain Injury
and the Role of CT Scanning.
Childs Nerv Syst, 2001, 17:257-262.
6. Smits, M., Dippel, D.W.J., de Haan,
G.G., Dekker, H.M., Vos, P.E., Kool,
D.R., Nederkoorn, P.J., Hofmann,
P.A.M., Twijinstra, A., Tanghe,
H.I.J. and Hunink, M.G.M. External
Validation of the Canadian CT Head
Rule and the New Orleans Criteria
for CT Scanning in Patients with
Minor Head Injury. JAMA, 2005,
294(12):1519-1525.
7. World Health Organization (WHO).
Provisional Guidelines on Standard
International Age Classification.
Department of International
Economic and Social Affairs. Series
M, No. 74. United Nations, New
York, 1982.
8. Haydel, M.J., Preston, C.A., Mills,
T.J., Luber, S., Blaudeau, E., and
Deblieux, P.M.C. Indication for
Computed Tomography in Patients
with Minor Head Injury. The New
England Journal of Medicine, 2000,
343:100-5.
9. Saboori M., Ahmadi, J. And
Farajzadegan, Z. Indications for
Brain CT in Patients with Minor
Head Injury. Clinical Neurology and
Neurosurgery, 2007, 109:399-405
10. Jagoda, A.S., Bazarian, J.J., Bruns, Jr
J., Cantrill S.V, Gean, A.D., Howard,
P.K., Riggio, J.G.S, Wright, D.W.,
Wears R.L., Bakshy, A., and
Burgess, P. Clinical Policy:
Neuroimaging and Decision making
in Adult Mild Traumatic Brain Injury
in the Acute Setting. Ann Emergency
Medicine, 2008, 52:714-748.
11. Borczuk, P. Predictors of Intracranial
Injury in patients with Mild Head
Trauma. Ann Emergency Medicine,
1995, 25:731-736.
12. Zimmerman, R.A., Gibby, W.A. and
Carmody, R.F. .Neuroimaging
Clinical and Physical Principles.
Springer-Verlag New York Inc. New
York NY USA, 2000.
13. Abdul-latip, L.S., Alias, N.A.A,
Ariff, A.R., Shuaib, I.L., Abdullah, J
and Naing, N.N. CT in Minor Head
Trauma: A guide for Rural Doctors.
Garba I., Speelman A. and Tabari A.M./Journal of Association of Radiographers of Nigeria, Vol. 23, (2009) 7 15.
15
Journal of Clinical Neuroscience,
2004, 11(8):835-839.
14. Bordignon, K.C., and Arruda, W.O.
CT scans Findings in Head Trauma.
Arq Neuropsiquiatr, 2002, 60(2-
A):204-210.
15. Udgiri, .N.R., Tewari, M.K.,
Dwarakanath, S., Khandelwal, N.,
and Sharma, B.S. Role of Computed
Tomography in Minor Head Injury.
Indian Journal of Neurotrauma,
2004, 1(1):33-36.
16. Vilke, G.M., Chan, T.C., and Guss,
D.A. Use of Complete Neurological
Examination to Screen for
Significant Intracranial
Abnormalities in Minor Head Injury.
American Journal of Emergency
Medicine, 2000, 18:159-163.
17. Geijertam, J.L., Britton, M. Mild
Head Injury: Reliabilty of Early
Computed Tomographic Findings in
Triage for Admission. Emergency
Medicine Journal, 2005;22:103-107.
Das könnte Ihnen auch gefallen
- FORM QC MRI AcceptTesting 0604Dokument4 SeitenFORM QC MRI AcceptTesting 0604Yuda FhunkshyangNoch keine Bewertungen
- Boysen-Osborn (2018) PDFDokument11 SeitenBoysen-Osborn (2018) PDFBryan TorresNoch keine Bewertungen
- David Jenkins - Radiographic Photography and Imaging Processes - Springer Netherlands (1980)Dokument307 SeitenDavid Jenkins - Radiographic Photography and Imaging Processes - Springer Netherlands (1980)Carlos Hernández100% (2)
- Normal Tissue Constraint Guidelines: AppendixDokument4 SeitenNormal Tissue Constraint Guidelines: AppendixbigskyNoch keine Bewertungen
- Burdock Root AeroponicDokument8 SeitenBurdock Root AeroponicNelson RiddleNoch keine Bewertungen
- Consumer Behaviour Towards Healtth Care ProductsDokument46 SeitenConsumer Behaviour Towards Healtth Care ProductsJayesh Makwana50% (2)
- Jurnal Basic MriDokument11 SeitenJurnal Basic MrikonkonataNoch keine Bewertungen
- JRI 13 Full PDFDokument76 SeitenJRI 13 Full PDFAGNES TRIANA BASJANoch keine Bewertungen
- Comparing SPIR and SPAIR Fat Suppression Techniques in Magnetic Resonance Imaging (MRI) of Wrist JointDokument6 SeitenComparing SPIR and SPAIR Fat Suppression Techniques in Magnetic Resonance Imaging (MRI) of Wrist JointRini IndratiNoch keine Bewertungen
- Tabel QC CT ScanDokument6 SeitenTabel QC CT ScanbayuNoch keine Bewertungen
- Karakteristik Film Sinar-X Yang Digunakan Pada RadiologiDokument13 SeitenKarakteristik Film Sinar-X Yang Digunakan Pada Radiologifikal 'sNoch keine Bewertungen
- AI PKL 1 - Calcaneus - Put AyDokument17 SeitenAI PKL 1 - Calcaneus - Put AyYusuf Erlangga AWNoch keine Bewertungen
- AAPM 34 - MRI Acceptance TestDokument16 SeitenAAPM 34 - MRI Acceptance TestmahbodsedNoch keine Bewertungen
- Makalah CR DR Dan CT ScanDokument11 SeitenMakalah CR DR Dan CT ScanRenolia WidyaningrumNoch keine Bewertungen
- Spesifikasi PHILIPS Ultrasound System EPIQ 5 WHC BasicDokument2 SeitenSpesifikasi PHILIPS Ultrasound System EPIQ 5 WHC BasichsNoch keine Bewertungen
- Loopography Examination For Colon Cancer 7c394e77Dokument11 SeitenLoopography Examination For Colon Cancer 7c394e77N. Camelya FirdausNoch keine Bewertungen
- Bontrager S Handbook ofDokument1 SeiteBontrager S Handbook ofYoga SaputraNoch keine Bewertungen
- Radlink PET and Cardiac Imaging Centre - PhilipsDokument1 SeiteRadlink PET and Cardiac Imaging Centre - PhilipsRadlinkSingaporeNoch keine Bewertungen
- Dual Source CT Imaging PDFDokument275 SeitenDual Source CT Imaging PDFAnisa SetiawatiNoch keine Bewertungen
- Ai Pengujian Lead ApronDokument8 SeitenAi Pengujian Lead Apronwildan sanjayaNoch keine Bewertungen
- Computed Tomography HUDokument7 SeitenComputed Tomography HUAnonymous 0XPHreGPNoch keine Bewertungen
- Emergency Radiology PDFDokument41 SeitenEmergency Radiology PDFRobiul AlamNoch keine Bewertungen
- Review Jurnal RadiologiDokument10 SeitenReview Jurnal RadiologiM Benni KadapihNoch keine Bewertungen
- Makalah Bahasa InggrisDokument8 SeitenMakalah Bahasa InggrisNorhikmahNoch keine Bewertungen
- Analisis Efisiensi Celah Shutter Kolimator Tabung Sinar X Di Tiga Instalasi Radiologi Lahan PKL Prodi D3 Radiologi Unisa YogyakartaDokument7 SeitenAnalisis Efisiensi Celah Shutter Kolimator Tabung Sinar X Di Tiga Instalasi Radiologi Lahan PKL Prodi D3 Radiologi Unisa YogyakartaNoveliaNoch keine Bewertungen
- 2016 Merrill's Atlas of Radiographic Positioning (1) - 1476-1515 PDFDokument40 Seiten2016 Merrill's Atlas of Radiographic Positioning (1) - 1476-1515 PDFhanna adkhillahNoch keine Bewertungen
- Makalah MyelografiDokument8 SeitenMakalah Myelografi16 generation Radiology100% (1)
- Chat GPTDokument2 SeitenChat GPTGerardoMadrizNoch keine Bewertungen
- Pengukuran Laju Paparan Radiasi Pada Ruang Ct-Scan: PKU Sukoharjo. Poltekkes Kemenkes SemarangDokument10 SeitenPengukuran Laju Paparan Radiasi Pada Ruang Ct-Scan: PKU Sukoharjo. Poltekkes Kemenkes SemarangZmaNoch keine Bewertungen
- 4.menajemen Dokter Penunjang Radiologi, Clinical Reasoning SM 7. 2011Dokument35 Seiten4.menajemen Dokter Penunjang Radiologi, Clinical Reasoning SM 7. 2011Pradipta SuarsyafNoch keine Bewertungen
- Cervical Proyeksi Ap Open MouthDokument17 SeitenCervical Proyeksi Ap Open MouthAgil SarengatNoch keine Bewertungen
- Agfa CR 10 XDokument4 SeitenAgfa CR 10 XSandyKarittokNoch keine Bewertungen
- Role of Automated Breast Ultrasound in Diagnostic and Early Detection 5-1Dokument47 SeitenRole of Automated Breast Ultrasound in Diagnostic and Early Detection 5-1Dokdem AjaNoch keine Bewertungen
- Kel - 3 Uretrocystografi Bipolar TRO 16 ADokument22 SeitenKel - 3 Uretrocystografi Bipolar TRO 16 A16 generation Radiology100% (3)
- Laporan Automatic ProcessingDokument21 SeitenLaporan Automatic ProcessingVeny KzahroNoch keine Bewertungen
- FistulografiDokument11 SeitenFistulografiAisa MaulidianaNoch keine Bewertungen
- Jurnal Radiografi Pelvis Judeth ViewDokument12 SeitenJurnal Radiografi Pelvis Judeth ViewKresensia0% (1)
- Pictorial Essay: Multidetector CT Urography With Abdominal Compression and Three-Dimensional ReconstructionDokument13 SeitenPictorial Essay: Multidetector CT Urography With Abdominal Compression and Three-Dimensional ReconstructionHarley Alejo MNoch keine Bewertungen
- Computed Tomography Scan (CT Scan) : Dr. Ifeanyi Ukachukwu Consultant Diagnostic and Interventional RadiologistDokument48 SeitenComputed Tomography Scan (CT Scan) : Dr. Ifeanyi Ukachukwu Consultant Diagnostic and Interventional RadiologistifeanyiukNoch keine Bewertungen
- Artikel Ilmiah Teknik Radiografi Cranium Ada Kasus FrakturDokument13 SeitenArtikel Ilmiah Teknik Radiografi Cranium Ada Kasus FrakturLia NurNoch keine Bewertungen
- 7@myelografiDokument39 Seiten7@myelografierly indrianiNoch keine Bewertungen
- Pengujian Kolimator Dengan Metode Collimator Test Tool Pada Pesawat SinarDokument10 SeitenPengujian Kolimator Dengan Metode Collimator Test Tool Pada Pesawat Sinarmak cretNoch keine Bewertungen
- Radiology Notes (1-36)Dokument83 SeitenRadiology Notes (1-36)el spin artifactNoch keine Bewertungen
- Jurnal MRCPDokument18 SeitenJurnal MRCPMaharani Eka SaputriNoch keine Bewertungen
- RPDIR-L16.2 Fluoroscopy Doses WEBDokument46 SeitenRPDIR-L16.2 Fluoroscopy Doses WEBNur Qina100% (1)
- Angiografi Femoralis-1Dokument24 SeitenAngiografi Femoralis-1Sepahit Kopi Hitam100% (1)
- Standar Kualitas Gambar Radiografi PDFDokument30 SeitenStandar Kualitas Gambar Radiografi PDFAdhitia DarmansyahNoch keine Bewertungen
- Chapter 1Dokument11 SeitenChapter 116 generation Radiology100% (2)
- Truebeam CollimationDokument6 SeitenTruebeam Collimationzhen yongjieNoch keine Bewertungen
- Abdomen CTDokument26 SeitenAbdomen CTAnto BijuNoch keine Bewertungen
- Teknik Pemeriksaan CT Scan Sinus ParanasalDokument22 SeitenTeknik Pemeriksaan CT Scan Sinus ParanasalmhyamannanNoch keine Bewertungen
- Y3. INTRODUCTION TO MEDICAL IMAGING. Part 1Dokument40 SeitenY3. INTRODUCTION TO MEDICAL IMAGING. Part 1Jonathan YeohNoch keine Bewertungen
- E-Cube Line Up CatalogDokument16 SeitenE-Cube Line Up CatalogJose QuiscaNoch keine Bewertungen
- 47 421 1 PB PDFDokument8 Seiten47 421 1 PB PDFRien Gloria SihombingNoch keine Bewertungen
- Mammography - Procedure, Test, Pain, Time, Types, Risk, Cancer, RateDokument4 SeitenMammography - Procedure, Test, Pain, Time, Types, Risk, Cancer, RateMassimo RiserboNoch keine Bewertungen
- Viner 2005 Forensic Radiography in South AfricaDokument24 SeitenViner 2005 Forensic Radiography in South Africah8517Noch keine Bewertungen
- Chapter 3 VerbsDokument13 SeitenChapter 3 Verbs16 generation Radiology100% (2)
- Jurnal Pemeriksaan LopografiDokument5 SeitenJurnal Pemeriksaan LopografiDwi Ajeng Risqy HasanahSyamNoch keine Bewertungen
- Pit Pdsri 2019 Announce r3Dokument6 SeitenPit Pdsri 2019 Announce r3anggiayunandaNoch keine Bewertungen
- Medical Imaging: Principles, Detectors, and ElectronicsVon EverandMedical Imaging: Principles, Detectors, and ElectronicsNoch keine Bewertungen
- Atlas of Hybrid Imaging Sectional Anatomy for PET/CT, PET/MRI and SPECT/CT Vol. 2: Thorax Abdomen and Pelvis: Sectional Anatomy for PET/CT, PET/MRI and SPECT/CTVon EverandAtlas of Hybrid Imaging Sectional Anatomy for PET/CT, PET/MRI and SPECT/CT Vol. 2: Thorax Abdomen and Pelvis: Sectional Anatomy for PET/CT, PET/MRI and SPECT/CTNoch keine Bewertungen
- Anoplastia Percutanea 2022Dokument11 SeitenAnoplastia Percutanea 2022Sandra Cárdenas HilasacaNoch keine Bewertungen
- Statistical EstimationDokument37 SeitenStatistical EstimationAmanuel MaruNoch keine Bewertungen
- NMI Application Form (NCLEX Scores Transfer)Dokument2 SeitenNMI Application Form (NCLEX Scores Transfer)Ramon Carlo Almiranez100% (1)
- Voice Over Script For Pilot TestingDokument2 SeitenVoice Over Script For Pilot TestingRichelle Anne Tecson ApitanNoch keine Bewertungen
- Real-Time Health Care Monitoring System Using Iot: International Journal of Engineering & TechnologyDokument5 SeitenReal-Time Health Care Monitoring System Using Iot: International Journal of Engineering & TechnologyShaik JunaidNoch keine Bewertungen
- School Form 2 (SF2) Daily Attendance Report of LearnersDokument4 SeitenSchool Form 2 (SF2) Daily Attendance Report of LearnersRyan A. CabalidaNoch keine Bewertungen
- Introduction and Analytical Report PDFDokument111 SeitenIntroduction and Analytical Report PDFJoão Pedro GarciaNoch keine Bewertungen
- Story of ChangeDokument3 SeitenStory of ChangeSend Sierra LeoneNoch keine Bewertungen
- Below The Breadline: The Relentless Rise of Food Poverty in BritainDokument28 SeitenBelow The Breadline: The Relentless Rise of Food Poverty in BritainOxfamNoch keine Bewertungen
- MDSAP QMS ManualDokument43 SeitenMDSAP QMS ManualmamjaguarNoch keine Bewertungen
- 33 Pol BRF Food Models enDokument36 Seiten33 Pol BRF Food Models enthuyetnnNoch keine Bewertungen
- Analysis of Shift in Consumption of Carbonated Beverages To Healthy DrinksDokument26 SeitenAnalysis of Shift in Consumption of Carbonated Beverages To Healthy DrinksAntara JasrotiaNoch keine Bewertungen
- CrimPro Cases People Vs LlantoDokument7 SeitenCrimPro Cases People Vs LlantoFatmah Azimah MapandiNoch keine Bewertungen
- BB - Self AuditDokument18 SeitenBB - Self AuditFe Rackle Pisco JamerNoch keine Bewertungen
- Contemporary Management of Major Haemorrhage in Critical CareDokument13 SeitenContemporary Management of Major Haemorrhage in Critical CareYo MeNoch keine Bewertungen
- Allergist OIT Packet 180913 NutsDokument74 SeitenAllergist OIT Packet 180913 Nutsmuaz.rizviNoch keine Bewertungen
- 2nd Year Medical BooksDokument3 Seiten2nd Year Medical Bookskent_mazawNoch keine Bewertungen
- Bar Coding Near MissDokument8 SeitenBar Coding Near Missenorth1234Noch keine Bewertungen
- Sistem Pakar Diagnosis Penyakit Pada Ayam Dengan Menggunakan Metode Dempster ShaferDokument11 SeitenSistem Pakar Diagnosis Penyakit Pada Ayam Dengan Menggunakan Metode Dempster ShaferYata RinNoch keine Bewertungen
- Training 11 Add 3 enDokument44 SeitenTraining 11 Add 3 enBela CruzNoch keine Bewertungen
- CPB Online Medical Billing Syllabus - 11th - 4!17!13Dokument2 SeitenCPB Online Medical Billing Syllabus - 11th - 4!17!13Kian GonzagaNoch keine Bewertungen
- The Girl With Green Eyes by John EscottDokument10 SeitenThe Girl With Green Eyes by John EscottAyman Charoui essamadiNoch keine Bewertungen
- Mosh RoomDokument21 SeitenMosh RoomBrandon DishmanNoch keine Bewertungen
- ARTIGO 2002 - Clarke, D. M., & Kissane, D. W. (2002) - Demoralization: Its Phenomenology and Importance.Dokument11 SeitenARTIGO 2002 - Clarke, D. M., & Kissane, D. W. (2002) - Demoralization: Its Phenomenology and Importance.GTGTNoch keine Bewertungen
- Pollution of The WaterDokument25 SeitenPollution of The WaterJeprox Martinez100% (1)
- Cbse Term 1 Final Exam Instructions 2021-21Dokument9 SeitenCbse Term 1 Final Exam Instructions 2021-21Eshaan123thebestNoch keine Bewertungen
- Vieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMDokument17 SeitenVieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMFranciscoNoch keine Bewertungen
- Research ProposalDokument3 SeitenResearch Proposalapi-446880170Noch keine Bewertungen