Beruflich Dokumente
Kultur Dokumente
Role of Laparoscopic Cholecystectomy in The Early Management of Acute Gallbladder Disease
Hochgeladen von
Horacio Chacon0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
17 Ansichten6 SeitenThis study evaluated the role of laparoscopic surgery in the early management of acute gallbladder disease in a single large UK teaching hospital. 385 patients with gallstone disease (243 acute biliary pain, 142 acute cholecystitis) and 15 with acalculous disease were identified.
Originalbeschreibung:
Originaltitel
British Journal of Surgery Volume 92 Issue 5 2005 [Doi 10.1002%2Fbjs.4831] W. K. Peng; Z. Sheikh; S. J. Nixon; S. Paterson-Brown -- Role of Laparoscopic Cholecystectomy in the
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenThis study evaluated the role of laparoscopic surgery in the early management of acute gallbladder disease in a single large UK teaching hospital. 385 patients with gallstone disease (243 acute biliary pain, 142 acute cholecystitis) and 15 with acalculous disease were identified.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
17 Ansichten6 SeitenRole of Laparoscopic Cholecystectomy in The Early Management of Acute Gallbladder Disease
Hochgeladen von
Horacio ChaconThis study evaluated the role of laparoscopic surgery in the early management of acute gallbladder disease in a single large UK teaching hospital. 385 patients with gallstone disease (243 acute biliary pain, 142 acute cholecystitis) and 15 with acalculous disease were identified.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 6
Original article
Role of laparoscopic cholecystectomy in the early management
of acute gallbladder disease
W. K. Peng, Z. Sheikh, S. J. Nixon and S. Paterson-Brown
Department of Clinical and Surgical Sciences (Surgery), Royal Inrmary of Edinburgh, Little France Crescent, Edinburgh EH16 4SA, UK
Correspondence to: Mr S. Paterson-Brown (e-mail: spb@doctors.org.uk)
Background: This study evaluated the role of laparoscopic surgery in the early management of acute
gallbladder disease in a single large UK teaching hospital.
Methods: Details of all emergency admissions for acute gallbladder disease from January 2000 to
December 2001 were identied and additional information from the hospital records was reviewed
retrospectively.
Results: Three hundred and eighty-ve patients with gallstone disease (243 acute biliary pain, 142 acute
cholecystitis) and 15 with acalculous disease were identied. The conversion rate was higher during early
laparoscopic surgery for acute calculous cholecystitis than in operations for acute biliary pain (19 versus
4 per cent; P = 0002). In patients with acute calculous cholecystitis the conversion rate was signicantly
lower in operations within 48 h of admission (one of 26) than when surgery was delayed beyond 48 h (14
of 52) or subsequently carried out electively (seven of 21) (P = 0014). Elective surgery for previous acute
cholecystitis was associated with a higher conversion rate (seven of 21 patients) than elective surgery for
biliary pain (three of 65) (P = 0002).
Conclusion: Laparoscopic cholecystectomy for acute calculous cholecystitis should be performed, where
possible, within the rst 48 h of admission.
Paper accepted 11 August 2004
Published online 18 March 2005 in Wiley InterScience (www.bjs.co.uk). DOI: 10.1002/bjs.4831
Introduction
The value of early cholecystectomy for acute calculous
cholecystitis was well established in the prelaparoscopic
era
1,2
and early laparoscopic intervention has subsequently
been shown to provide an improved outcome
26
. In
spite of this, many hospitals in the UK do not
have a policy of early laparoscopic cholecystectomy
for acute gallbladder disease. This may partly be
related to ongoing concerns that conversion rates
are higher in the acute setting, partly to the fact
that not all emergency general surgeons are skilled
in laparoscopic cholecystectomy, and also to resource
restrictions in many hospitals regarding early access to
theatre for patients considered not to require urgent
surgery.
Conversion rates for early laparoscopic cholecys-
tectomy in patients with acute cholecystitis range
from 5 to 30 per cent, but optimal timing for early
operation is difcult to assess because most reports
did not compare surgery at different time inter-
val within the same admission, case mix differences
and patient selection. Laparoscopic cholecystectomy for
an acutely inamed gallbladder is technically more
demanding than surgery for acute biliary pain with-
out inammation (biliary colic), and the time inter-
val from admission to surgery may affect conversion
rates
79
.
Apart from obscure anatomy and bleeding, the reasons
for conversion to open surgery relate to the presence of
inammation in the acute setting and to adhesions in the
elective setting. Although the decision to convert should
not be considered as a complication, as the overall success-
ful and safe completion of the operation is the ultimate
goal, it would be useful to identify the circumstances under
which laparoscopic cholecystectomy might have the best
chance of successful completion. This study examined the
management of all patients admitted to the Royal Inrmary
of Edinburgh with acute gallbladder disease over 2 years
to evaluate the outcome of early laparoscopic surgery.
Copyright 2005 British Journal of Surgery Society Ltd British Journal of Surgery 2005; 92: 586591
Published by John Wiley & Sons Ltd
Early management of gallbladder disease 587
Patients and methods
Details of all patients admitted to the general surgical unit
of Edinburgh Royal Inrmary are recorded prospectively
using the Lothian Surgical Audit system. A total of
400 patients having an emergency admission for acute
gallbladder disease were identied between January 2000
and December 2001. This system records patients
diagnoses and operative details with specic codes, and
includes free text for the operation notes, discharge
summary and any clinic letters. Additional information
such as ultrasonography reports, blood results and
histological ndings were retrieved retrospectively from
patients notes or the hospital information system.
The diagnosis of acute calculous cholecystitis in
patients operated on during an acute admission was
based on histological evidence of acute inammatory
cells. When the patient did not have early surgery,
the diagnosis of acute cholecystitis was based on
clinical features (right upper quadrant tenderness with
or without fever) and ultrasonographic conrmation of
gallstones, with either ultrasonographic features suggestive
of inammation (gallbladder wall thickness of more than
3 mm, oedematous wall, emphysematous wall, gallbladder
distension, pericholecystic uid, positive sonographic
Murphys sign) and/or leucocytosis greater than11 10
9
/l.
The diagnosis of acute biliary pain was made if
ultrasonographic, laboratory or histological ndings did
not reveal any sign of acute inammation. Bacteriological
specimens were not collected routinely at operation.
Patients with gallstone pancreatitis and gallstone ileus were
excluded from the study.
Statistical analysis
The Wilcoxon sum-of-rank test was used to analyse two-
sample unpaired quantitative data, and three-sample data
were analysed with the non-parametric Kruskal Wallis
test. Qualitative data were analysed using Fishers exact
(two-tailed P value) test. P < 0050 was considered
statistically signicant.
Results
Of the 400 patients identied, 385 (962 per cent) had acute
gallstone disease and 15 (38 per cent) had acute acalculous
cholecystitis. Some 142 (369 per cent) of the patients with
acute gallstone disease had acute cholecystitis and 243
(631 per cent) had acute biliary pain.
Management and outcome
Of the 142 patients (85 women; 599 per cent) with acute
calculous cholecystitis, 89 (627 per cent) had cholecys-
tectomy during the same acute admission. Laparoscopic
cholecystectomy was attempted in 78 patients (88 per cent)
and 11 (12 per cent) had open cholecystectomy. Percuta-
neous cholecystostomy was performed in four patients who
did not have early cholecystectomy. In total, 53 patients
were discharged home without early surgery, of whom
three had follow-up in another hospital, 21 proceeded to
elective surgery, 18 remained well and did not undergo
surgery, and 11 required further emergency admission
(three with acute cholecystitis, seven with acute biliary
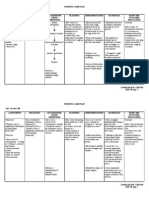
pain and one with gallstone pancreatitis). Table 1 shows the
histological ndings in patients who had early surgery, and
Table 2 lists the ultrasonographic and laboratory ndings
in patients who were discharged without early surgery.
Two elderly patients who were deemed unt for chole-
cystectomy because of signicant co-morbidity died from
multiorgan failure.
Of the 243 patients (164 women; 675 per cent)
with acute biliary pain, 87 (358 per cent) had early
cholecystectomy during the same acute admission; 85
Table 1 Histological ndings in patients with acute calculous
cholecystitis who underwent early surgery
No. of patients
(n = 89)
Acute inammation 63 (71)
Gangrene 17 (19)
Empyema 5 (6)
Gangrene with empyema 2 (2)
Perforated gallbladder 2 (2)
Values in parentheses are percentages.
Table 2 Ultrasonographic and laboratory ndings in patients with
acute calculous cholecystitis who were discharged without early
surgery
No. of patients
(n = 53)
Gallbladder wall thickened >3 mm 37 (70)
Oedematous wall 11 (21)
Pericholecystitic uid 5 (9)
Positive sonographic Murphys sign 3 (6)
Sludge within gallbladder 2 (4)
Distended gallbladder 1 (2)
Emphysematous wall 1 (2)
Intrahepatic abscess related to cholecystitis 1 (2)
Leucocytosis 48 (91)
Values in parentheses are percentages.
Copyright 2005 British Journal of Surgery Society Ltd www.bjs.co.uk British Journal of Surgery 2005; 92: 586591
Published by John Wiley & Sons Ltd
588 W. K. Peng, Z. Sheikh, S. J. Nixon and S. Paterson-Brown
had attempted laparoscopic cholecystectomy and two
had an open operation owing to signicant previous
abdominal surgery. Seventeen patients discharged without
undergoing surgery were followed up in other hospitals,
66 proceeded to elective laparoscopic cholecystectomy
(65 laparoscopic, one open), 53 remained well with
conservative management and 20 required a further
emergency admission. There was no death in this group.
Of patients who did not have an early operation, 20
(128 per cent) of 156 with acute biliary pain and 11
(21 per cent) of 53 with acute cholecystitis required a
further emergency readmission (P = 0181).
Of the 15 patients (seven women) with acute acalculous
cholecystitis, six had surgery during the same acute
admission (three attempted laparoscopic and three open
cholecystectomies). Percutaneous cholecystostomy was
performed in one patient who did not have early
cholecystectomy. Nine patients were discharged; three
proceeded to elective surgery at a later date, ve remained
well with conservative management, and one required a
further emergency admission. There were three deaths in
this group of patients, two from septic shock and one from
pulmonary embolism (one of these deaths occurred after
elective surgery).
Effect of age
The mean age of patients with acute calculous cholecystitis
was 58 (range 1499) years and that of patients with
acute biliary pain was 55 (range 1695) years (P 0097).
Patients with acute acalculous cholecystitis had a mean age
of 62 (range 3297) years. Patients operated on at the rst
admission for acute calculous cholecystitis (P 0002) or
acute biliary pain (P 00003) were signicantly younger
than whose in whom surgery was deferred (Table 3).
Presence of common bile duct stones
Overall 11 (77 per cent) of 142 patients with acute
calculous cholecystitis and 40 (165 per cent) of 243
with acute biliary pain were found to have common
Table 3 Patient age and timing of surgery
Mean (range) age (years)
Early surgery Discharged P*
Acute calculous cholecystitis 54 (1488) 64 (2799) <0002
Acute biliary pain 49 (1686) 58 (1995) <0001
P* <005 <005
*Wilcoxon sum-of-rank test.
bile duct stones. Thirty-two patients in whom there
was a high suspicion of choledocholithiasis (signicantly
abnormal liver function test results and/or an abnormal
biliary tree on ultrasonography) underwent preoperative
endoscopic retrograde cholangiopancreatography (ERCP).
The remaining 19 patients had selective intraoperative
cholangiography according to clinical data, operative
ndings and consultant preference; the methods of
stone retrieval were postoperative ERCP (11 patients),
laparoscopic exploration of the common bile duct with
choledochoscopy (four), conversion to open surgery (two),
and in two patients the small lling defect found on
cholangiography was left alone.
Laparoscopic conversion rate
Laparoscopic cholecystectomy was converted to open
surgery in 15 (19 per cent) of 78 patients having early
operation for acute cholecystitis, compared with three
(4 per cent) of 85 patients with acute biliary pain
(P = 0002). One of three patients undergoing early
laparoscopic cholecystectomy for acalculous cholecystitis
required conversion. After non-operative early treatment
and subsequent readmission for elective cholecystectomy,
the conversion rate was 33 per cent (seven of 21) in patients
with previous acute calculous cholecystitis compared with
5 per cent (three of 65) in those with previous acute biliary
pain (P = 0002). There were no conversions in the three
patients who had elective laparoscopic cholecystectomy
for previous acute acalculous cholecystitis. There was no
signicant difference in the conversion rate for early and
delayed laparoscopic cholecystectomy for acute calculous
cholecystitis (P = 0240) or acute biliary pain (P = 1000).
Reason for conversion
Thirteen of the 15 patients with acute calculous
cholecystitis who required conversion in the early setting
had severe inammation that obscured the plane of
dissection and anatomy around Calots triangle; conversion
was necessary in the other two patients because of bile duct
stones (one patient) and uncontrolled bleeding (one). In
the elective setting all seven conversions were required
because dense adhesions were present. As three patients
had undergone previous abdominal surgery, adhesions
discovered during cholecystectomy could not be attributed
solely to previous acute cholecystitis.
Among patients with acute biliary pain, three conver-
sions were required in the early setting because of obscure
anatomy with injury to a grossly dilated common hepatic
duct (one patient), adhesions (one) and common bile duct
Copyright 2005 British Journal of Surgery Society Ltd www.bjs.co.uk British Journal of Surgery 2005; 92: 586591
Published by John Wiley & Sons Ltd
Early management of gallbladder disease 589
stone (one). In elective surgery, the reasons were common
bile duct stone in one patient and adhesions in two patients
who had undergone previous abdominal surgery.
Conversion was necessary in one patient with acute
acalculous cholecystitis because of severe inammation.
Timing of laparoscopic surgery
For acute gallstone cholecystitis, the conversion rate
was signicantly higher when surgery was carried out
more than 48 h after admission or later as an elective
procedure. Of the 26 patients undergoing laparoscopic
cholecystectomy within 48 h of admission, one required
conversion (owing to a bile duct stone), compared with
14 of the 52 patients having early surgery after 48 h and
seven of the 21 operated on electively at a later date
(P = 0014) (Table 4). When only conversions required for
inammation or adhesions were considered and patients
who had undergone abdominal surgery previously were
excluded, the conversion rates were none of 25, 13 of 51
and four of 18 respectively (P = 0005) (Table 4).
There was no signicant difference in the conversion
rate between patients with acute cholecystitis operated on
within 48 h of admission (one of 26) and those with acute
biliary pain who had surgery in either the acute (three of
85) or the elective (three of 65) setting (P = 1000). There
was no signicant difference in the mean age (40 versus
51 versus 59 years; P = 0117) or male : female sex ratio
(17 : 9 versus 31 : 21 versus 12 : 9; P = 0890) of patients
undergoing surgery within 48 h, after 48 h, or later as an
elective patient (Table 4).
Complications and hospital stay
Operations for acute calculous cholecystitis carried out
within 48 h of admission were associated with a lower
overall rate of complications than surgery undertaken after
48 h (11 of 52) or (six of 21) (Table 4). There was a higher
rate of postoperative bile leakage in early operations after
Table 4 Comparison of patients with acute calculous cholecystitis who had laparoscopic cholecystectomy before and after 48 h of
admission, and those who had elective surgery
Timing of surgery
Early (n = 78)
<48 h
(n = 26)
>48 h
(n = 52)
Elective
(n = 21) P
LC requiring conversion 1 14 7 0014
LC requiring conversion owing to inammation or adhesions 0 of 25 13 of 51 4 of 18 0005
Histological ndings
Acute inammation 16 42 2
Empyema 1 4 1
Gangrene 9 5 0
Perforation 0 1 1
Chronic inammation 0 0 17
Consultant : trainees ratio
Attempted LCs 3 : 23 6: 46 6: 15 >0100
Converted LCs 0 : 01 0: 14 2: 05 1000
Median (range) hospital stay (nights) 3 (112) 6 (320) 7 (315)* <0001
Total no. of complications 3 11 6
Intraoperative
Bleeding 0 1 0
Gallbladder puncture (bile or stone spillage) 0 3 2
Small tear at falciform ligament 0 0 1
Postoperative
Cardiac event 1 1 0
Hypoxia 2 0 0
Pulmonary embolism 0 0 1
Bile leak 0 4 1 0400
Ileus 0 1 0
Urinary retention 0 1 0
Diarrhoea 0 0 1
*Includes both acute and elective admissions. LC, laparoscopic cholecystectomy. Excluding patients who had undergone abdominal surgery previously.
Fishers exact (two-tailed) test; Kruskal Wallis test.
Copyright 2005 British Journal of Surgery Society Ltd www.bjs.co.uk British Journal of Surgery 2005; 92: 586591
Published by John Wiley & Sons Ltd
590 W. K. Peng, Z. Sheikh, S. J. Nixon and S. Paterson-Brown
48 h than for surgery within 48 h or elective operations,
but the difference was not signicant (P = 0400) (Table 4).
Total hospital stay was signicantly shorter for patients
with acute calculous cholecystitis when the operation was
carried out within 48 h than for those who had surgery
after 48 h or elective operation (P < 0001) (Table 4).
Outcome of surgery by trainees and consultants
Eighty-four (85 per cent) of the 99 laparoscopic procedures
for acute calculous cholecystitis (in both acute and elective
settings) were performed by trainees (supervised and
unsupervised), but no signicant difference in conversion
rate was found between trainees and consultants in either
setting (Table 4). Neither was there a signicant difference
in the conversion rate of laparoscopic operations (early or
delayed) for acute biliary pain carried out by trainees (three
of 118; 25 per cent) or consultants (three of 32; 9 per cent)
(P = 0112).
Discussion
This study has conrmed and further claried the
results of other reports
3,5,6,10,11
showing the benets
of early laparoscopic cholecystectomy in patients with
acute calculous gallbladder disease. There is now good
evidence to support early operative management
1,36,10,11
in patients t for surgery, which should be carried out
laparoscopically within 48 h of admission, where possible.
If the patient is unable to undergo surgery within 48 h,
it is still worth proceeding with the operation within the
same acute setting as, owing to the formation of dense
inammatory adhesions, the conversion rate is similar to
that for patients returning at a later date for an elective
procedure. The higher complication rate in patients
undergoing delayed surgery either more than 48 h after
admission or subsequently as an elective procedure also
supports a policy of early surgery. Furthermore, early
operation in these patients may avoid the subsequent
need for readmission and emergency surgery following
discharge, which occurred in 21 per cent of patients in the
present study.
There is good evidence from randomized trials
in support of early laparoscopic cholecystectomy
3,5
.
However, the ideal interval from admission to early
surgery has yet to be agreed universally. Differences
in the conclusions of various studies may be explained
by methodological variations, such as the time interval
being from onset of symptoms to surgery or from time
of admission to surgery. In addition, some studies have
combined data from patients with acute cholecystitis and
those with simple acute biliary pain but no inammation.
Most studies have reported an optimal delay to surgery of
between 72 and 96 h
79,1215
, but some found no effect of
a prolonged delay on conversion rate
16,17
. Consistent with
the present results, an optimal maximum delay of 48 h was
proposed in two other studies
7,18
.
This study has demonstrated a difference in the
early operative intervention rate between patients with
inammatory cholecystitis (627 per cent) and those with
pain but no inammation (358 per cent). There was a clear
tendency to defer surgery in older patients in both groups,
but this does not explain the differing rates of operation
as patients with pain but no inammation were generally
younger. There were no other apparent differences in case
mix between these two groups, although a prospective
quantitative risk assessment was not undertaken. A
dedicated 24-h emergency operating theatre was available
throughout this study, but demand on its use meant that
it was not always available during the standard working
day; as a result, many patients with simple biliary pain
whose symptoms settled quickly were discharged, to return
for elective surgery at a later date. Interestingly, deferred
surgery in patients with no inammation was not associated
with an increased conversion rate, whereas deferment
of inamed cases appeared to increase the subsequent
technical difculty rather than reduce it. Thus the widely
held concept of delaying surgery to allow inammation to
settle and ease subsequent surgery appears to be awed.
During this study, patients were managed by a general
on-call team that included some consultants whose elective
practice did not encompass laparoscopic cholecystectomy;
this undoubtedly inuenced the practice of early or
delayed cholecystectomy. In August 2002, Edinburgh
developed a specialist on-call service for both upper and
lower gastrointestinal emergencies, and the results of
an early audit have demonstrated a much higher early
cholecystectomy rate. Similar results have also been shown
by surgeons in Portsmouth, UK
19
.
There is, of course, a group of patients with calculous
or acalculous cholecystitis who are not t for early
cholecystectomy, in whom management often poses a
challenge to the surgeons. Recent reports have suggested
that these high-risk patients, who are often ill from other
conditions, should be managed by cholecystostomy in
the rst instance
20
; they may not require subsequent
cholecystectomy at all, particularly those without stones
21
.
This is certainly becoming the authors policy, except
where the patients clinical conditionimproves rapidly after
the initial non-operative management and conrmation of
diagnosis.
Copyright 2005 British Journal of Surgery Society Ltd www.bjs.co.uk British Journal of Surgery 2005; 92: 586591
Published by John Wiley & Sons Ltd
Early management of gallbladder disease 591
The present study has identied clear differences in
outcome of early and delayed surgery for acute calculous
cholecystitis and acute biliary pain. Patients with acute
biliary pain obviously benet from early surgery to avoid
recurrent admission, although laparoscopic operations in
the acute and elective setting were associated with a similar
conversion rate. Local resources, and perhaps patient and
surgeon preferences, will dictate which route is taken.
Where separate emergency and elective surgical teams
are available, as is becoming increasingly common in the
UK
22
, early surgery undoubtedly provides efcient use of
resources and helps to minimize waiting lists.
Finally, although there was no difference in conversion
rates between consultants and trainees, the majority of
operations performed by trainees were closely supervised
by consultants and the results should be interpreted
accordingly.
References
1 van der Linden W, Sunzel H. Early versus delayed operation
for acute cholecystitis. A controlled clinical trial. Am J Surg
1970; 120: 713.
2 McArthur P, Cuschieri A, Sells RA, Shields R. Controlled
clinical trial comparing early with interval cholecystectomy
for acute cholecystitis. Br J Surg 1975; 62: 850852.
3 Wilson RG, Macintyre IM, Nixon SJ, Saunders JH,
Varma JS, King PM. Laparoscopic cholecystectomy as a safe
and effective treatment for severe acute cholecystitis. BMJ
1992; 305: 394396.
4 Lo CM, Liu CL, Lai EC, Fan ST, Wong J. Early versus
delayed laparoscopic cholecystectomy for treatment of acute
cholecystitis. Ann Surg 1996; 223: 3742.
5 Lo CM, Liu CL, Fan ST, Lai EC, Wong J. Prospective
randomized study of early versus delayed laparoscopic
cholecystectomy for acute cholecystitis. Ann Surg 1998; 227:
461467.
6 Lai PB, Kwong KH, Leung KL, Kwok SP, Chan AC,
Chung SC et al. Randomized trial of early versus delayed
laparoscopic cholecystectomy for acute cholecystitis. Br J
Surg 1998; 85: 764767.
7 Madan AK, Aliabadi-Wahle S, Tesi D, Flint LM,
Steinberg SM. How early is early laparoscopic treatment of
acute cholecystitis? Am J Surg 2002; 183: 232236.
8 Koo KP, Thirlby RC. Laparoscopic cholecystectomy in
acute cholecystitis. What is the optimal timing for operation?
Arch Surg 1996; 131: 540545.
9 Rattner DW, Ferguson C, Warshaw AL. Factors associated
with successful laparoscopic cholecystectomy for acute
cholecystitis. Ann Surg 1993; 217: 233236.
10 Papi C, Catarci M, DAmbrosio L, Gili L, Koch M,
Grassi GB et al. Timing of cholecystectomy for acute
calculous cholecystitis: a meta-analysis. Am J Gastroenterol
2004; 99: 147155.
11 Cheema S, Brannigan AE, Johnson S, Delaney PV,
Grace PA. Timing of laparoscopic cholecystectomy in acute
cholecystitis. Ir J Med Sci 2003; 172: 128131.
12 Eldar S, Sabo E, Nash E, Abrahamson J, Matter I.
Laparoscopic cholecystectomy for acute cholecystitis:
prospective trial. World J Surg 1997; 21: 540545.
13 Eldar S, Sabo E, Nash E, Abrahamson J, Matter I.
Laparoscopic versus open cholecystectomy in acute
cholecystitis. Surg Laparosc Endosc 1997; 7: 407414.
14 Pessaux P, Tuech JJ, Rouge C, Duplessis R, Cervi C,
Arnaud JP. Laparoscopic cholecystectomy in acute
cholecystitis. A prospective comparative study in patients
with acute vs. chronic cholecystitis. Surg Endosc 2000; 14:
358361.
15 Garber SM, Korman J, Cosgrove JM, Cohen JR. Early
laparoscopic cholecystectomy for acute cholecystitis. Surg
Endosc 1997; 11: 347350.
16 Knight JS, Mercer SJ, Somers SS, Walters AM, Sadek SA,
Toh SK. Timing of urgent laparoscopic cholecystectomy
does not inuence conversion rate. Br J Surg 2004; 91:
601604.
17 Bhattacharya D, Senapati PS, Hurle R, Ammori BJ. Urgent
versus interval laparoscopic cholecystectomy for acute
cholecystitis: a comparative study. J Hepatobiliary Pancreat
Surg 2002; 9: 538542.
18 Willsher PC, Sanabria JR, Gallinger S, Rossi L, Strasberg S,
Litwin DE. Early laparoscopic cholecystectomy for acute
cholecystitis: a safe procedure. J Gastrointest Surg 1999; 3:
5053.
19 Mercer SJ, Knight JS, Toh SK, Walters AM, Sadek SA,
Somers SS. Implementation of a specialist-led service for the
management of acute gallstone disease. Br J Surg 2004; 91:
504508.
20 Lo LD, Vogelzang RL, Braun MA, Nemcek AA Jr.
Percutaneous cholecystostomy for the diagnosis and
treatment of acute calculous and acalculous cholecystitis.
J Vasc Interv Radiol 1995; 6: 629634.
21 Sugiyama M, Tokuhara M, Atomi Y. Is percutaneous
cholecystostomy the optimal treatment for acute cholecystitis
in the very elderly? World J Surg 1998; 22: 459463.
22 Addison PDR, Getgood A, Paterson-Brown S. Separating
elective and emergency surgical care (the emergency team).
Scott Med J 2001; 46: 4850.
Copyright 2005 British Journal of Surgery Society Ltd www.bjs.co.uk British Journal of Surgery 2005; 92: 586591
Published by John Wiley & Sons Ltd
Das könnte Ihnen auch gefallen
- 2012 OiteDokument256 Seiten2012 Oiteaddison wood100% (4)
- Acute Kidney InjuryDokument49 SeitenAcute Kidney InjuryfikasywNoch keine Bewertungen
- Restoration of The Worn Dentition. Part 2Dokument7 SeitenRestoration of The Worn Dentition. Part 2Isharajini Prasadika Subhashni GamageNoch keine Bewertungen
- Tuesday 14 January 2020: BiologyDokument24 SeitenTuesday 14 January 2020: Biologysham80% (5)
- Variation in The Use of Laparoscopic Cholecystectomy For Acute CholecystitisDokument5 SeitenVariation in The Use of Laparoscopic Cholecystectomy For Acute CholecystitisAziz EzoNoch keine Bewertungen
- 1 s2.0 S2667008923000253 MainDokument4 Seiten1 s2.0 S2667008923000253 Mainal malikNoch keine Bewertungen
- Original Article Reasons of Conversion of Laparoscopic To Open Cholecystectomy in A Tertiary Care InstitutionDokument5 SeitenOriginal Article Reasons of Conversion of Laparoscopic To Open Cholecystectomy in A Tertiary Care InstitutionLuis Carlos Moncada TorresNoch keine Bewertungen
- Journal ReadingDokument8 SeitenJournal ReadingAnonymous Uh2myPxPHNoch keine Bewertungen
- C Reactive Protein An Independent Predictor of Difficult Emergency CholecystectomyDokument10 SeitenC Reactive Protein An Independent Predictor of Difficult Emergency Cholecystectomysarjan kunwarNoch keine Bewertungen
- Outcomes of Early Versus Delayed Cholecystectomy in Patients With Mild To Moderate Acute Biliary Pancreatitis: A Randomized Prospective StudyDokument36 SeitenOutcomes of Early Versus Delayed Cholecystectomy in Patients With Mild To Moderate Acute Biliary Pancreatitis: A Randomized Prospective StudyAnonymous Uh2myPxPHNoch keine Bewertungen
- Acute Cholecystitis: Computed Tomography (CT) Versus Ultrasound (US)Dokument11 SeitenAcute Cholecystitis: Computed Tomography (CT) Versus Ultrasound (US)deahadfinaNoch keine Bewertungen
- Management of Acute Cholecystitis in UK Hospitals: Time For A ChangeDokument4 SeitenManagement of Acute Cholecystitis in UK Hospitals: Time For A ChangeRana BishwoNoch keine Bewertungen
- Chapter 10Dokument9 SeitenChapter 10Kanishka SamantaNoch keine Bewertungen
- Post-Portoenterostomy Triangular Cord Sign Prognostic Value in Biliary Atresia: A Prospective StudyDokument4 SeitenPost-Portoenterostomy Triangular Cord Sign Prognostic Value in Biliary Atresia: A Prospective StudyWisnu Karya SanjayaNoch keine Bewertungen
- Pattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?Dokument4 SeitenPattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?neildamiNoch keine Bewertungen
- Per-Operative Conversion of Laparoscopic Cholecystectomy To Open Surgery: Prospective Study at JSS Teaching Hospital, Karnataka, IndiaDokument5 SeitenPer-Operative Conversion of Laparoscopic Cholecystectomy To Open Surgery: Prospective Study at JSS Teaching Hospital, Karnataka, IndiaSupriya PonsinghNoch keine Bewertungen
- 6870 FTPDokument10 Seiten6870 FTPAkreditasi Sungai AbangNoch keine Bewertungen
- Percutaneous Abscess Drainage in Patients With Perforated Acute Appendicitis: Effectiveness, Safety, and Prediction of OutcomeDokument8 SeitenPercutaneous Abscess Drainage in Patients With Perforated Acute Appendicitis: Effectiveness, Safety, and Prediction of Outcomereza yunusNoch keine Bewertungen
- Jurnal 3 AppDokument4 SeitenJurnal 3 AppmaulidaangrainiNoch keine Bewertungen
- BLL 2016 06 328Dokument4 SeitenBLL 2016 06 328alifandoNoch keine Bewertungen
- Risk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryDokument31 SeitenRisk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryWielda VeramitaNoch keine Bewertungen
- Anesthesiaforemergency Abdominalsurgery: Carol Peden,, Michael J. ScottDokument13 SeitenAnesthesiaforemergency Abdominalsurgery: Carol Peden,, Michael J. ScottJEFFERSON MUÑOZNoch keine Bewertungen
- Surgical Management of Acute CholecystitisDokument17 SeitenSurgical Management of Acute Cholecystitisgrayburn_1Noch keine Bewertungen
- IMU Learning Outcome: Psychomotor SkillsDokument11 SeitenIMU Learning Outcome: Psychomotor SkillsRameshNoch keine Bewertungen
- Spontaneous Passage of Bile Duct Stones: Frequency of Occurrence and Relation To Clinical PresentationDokument4 SeitenSpontaneous Passage of Bile Duct Stones: Frequency of Occurrence and Relation To Clinical PresentationBenny KurniawanNoch keine Bewertungen
- Predictive Factors For Conversion of Laparoscopic CholecystectomyDokument4 SeitenPredictive Factors For Conversion of Laparoscopic CholecystectomyGilang IrwansyahNoch keine Bewertungen
- Diagnosing Acute CholecystitisDokument2 SeitenDiagnosing Acute CholecystitisJorelle NunagNoch keine Bewertungen
- Art07 PDFDokument6 SeitenArt07 PDFadan2010Noch keine Bewertungen
- Choledochal CystDokument5 SeitenCholedochal CystZulia Ahmad BurhaniNoch keine Bewertungen
- Operations Patients Hepatic: Clarification of Risk Factors in With CirrhosisDokument7 SeitenOperations Patients Hepatic: Clarification of Risk Factors in With CirrhosisdaviddchandraNoch keine Bewertungen
- Liver A BSC DrainDokument8 SeitenLiver A BSC DrainAngelica AmesquitaNoch keine Bewertungen
- Laparoscopic Cholecystectomy For Acute !!!!Dokument9 SeitenLaparoscopic Cholecystectomy For Acute !!!!Anca FlorescuNoch keine Bewertungen
- Complikasi LaparosDokument5 SeitenComplikasi LaparosVirdo_pedroNoch keine Bewertungen
- Pattern of Acute Intestinal Obstruction Is There A PDFDokument3 SeitenPattern of Acute Intestinal Obstruction Is There A PDFMaría José Díaz RojasNoch keine Bewertungen
- JurnalDokument9 SeitenJurnalFrans 'cazper' SihombingNoch keine Bewertungen
- Jurnal 4Dokument7 SeitenJurnal 4Ega Gumilang SugiartoNoch keine Bewertungen
- RectopexyDokument7 SeitenRectopexyInzamam Ul HaqNoch keine Bewertungen
- Duct Cholecystectomy: Major LaparoscopicDokument10 SeitenDuct Cholecystectomy: Major LaparoscopicShahnawaz AhangarNoch keine Bewertungen
- Pancreatic ®stula After Pancreatic Head ResectionDokument7 SeitenPancreatic ®stula After Pancreatic Head ResectionNicolas RuizNoch keine Bewertungen
- Jurnal 3Dokument3 SeitenJurnal 3Ega Gumilang SugiartoNoch keine Bewertungen
- Appendicitis After Liver Transplantation Presentation of JournalDokument16 SeitenAppendicitis After Liver Transplantation Presentation of JournalIndah JamtaniNoch keine Bewertungen
- Case Report: Cholecystomegaly: A Case Report and Review of The LiteratureDokument5 SeitenCase Report: Cholecystomegaly: A Case Report and Review of The LiteratureAnti TjahyaNoch keine Bewertungen
- Rheumatology Journal Club Gut Vasculitis: by DR Nur Hidayati Mohd SharifDokument36 SeitenRheumatology Journal Club Gut Vasculitis: by DR Nur Hidayati Mohd SharifEida MohdNoch keine Bewertungen
- Transanal Endorectal PullthroughDokument8 SeitenTransanal Endorectal PullthroughMuhammad Harmen Reza SiregarNoch keine Bewertungen
- Liver Test Patterns in Patients With Acute Calculous Cholecystitis and or CholedocholithiasisDokument8 SeitenLiver Test Patterns in Patients With Acute Calculous Cholecystitis and or Choledocholithiasismari3312Noch keine Bewertungen
- 14 146 v13n6 2014 RiskCarcinogenesisDokument8 Seiten14 146 v13n6 2014 RiskCarcinogenesisDaphne Ongbit JaritoNoch keine Bewertungen
- Post-Cholecystectomy Acute Injury: What Can Go Wrong?Dokument7 SeitenPost-Cholecystectomy Acute Injury: What Can Go Wrong?Ramyasree BadeNoch keine Bewertungen
- Colovesical FistulaDokument4 SeitenColovesical FistulaNisaNoch keine Bewertungen
- Annals of Medicine and Surgery: Case ReportDokument4 SeitenAnnals of Medicine and Surgery: Case ReportDimas ErlanggaNoch keine Bewertungen
- Laproscopic Vagotony PaperDokument4 SeitenLaproscopic Vagotony Paperpeter_mrNoch keine Bewertungen
- Safe Laparoscopic Cholecystectomy FinaleDokument5 SeitenSafe Laparoscopic Cholecystectomy FinalenipolinNoch keine Bewertungen
- Serosal Appendicitis: Incidence, Causes and Clinical SignificanceDokument3 SeitenSerosal Appendicitis: Incidence, Causes and Clinical SignificancenaufalrosarNoch keine Bewertungen
- Laparoscopic Appendectomy PostoperativeDokument6 SeitenLaparoscopic Appendectomy PostoperativeDamal An NasherNoch keine Bewertungen
- Liang 2008Dokument6 SeitenLiang 2008Novi RobiyantiNoch keine Bewertungen
- Loozen 2017Dokument5 SeitenLoozen 2017Dheana IsmaniarNoch keine Bewertungen
- Colecistitis Aguda CirurgiaDokument7 SeitenColecistitis Aguda Cirurgiajoseaugustorojas9414Noch keine Bewertungen
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Dokument5 SeitenLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaNoch keine Bewertungen
- Cheema2003 Article TimingOfLaparoscopicCholecysteDokument4 SeitenCheema2003 Article TimingOfLaparoscopicCholecysteBandac AlexandraNoch keine Bewertungen
- Management of Perforated Peptic Ulcer in A District General HospitalDokument5 SeitenManagement of Perforated Peptic Ulcer in A District General HospitalNurul Fitrawati RidwanNoch keine Bewertungen
- 012011SCNA3Dokument14 Seiten012011SCNA3mariafmhNoch keine Bewertungen
- Tube IleostomyDokument5 SeitenTube IleostomyabhishekbmcNoch keine Bewertungen
- Acute Intestinal ObstructionDokument9 SeitenAcute Intestinal ObstructionRoxana ElenaNoch keine Bewertungen
- Atlas of Laparoscopic Gastrectomy for Gastric Cancer: High Resolution Image for New Surgical TechniqueVon EverandAtlas of Laparoscopic Gastrectomy for Gastric Cancer: High Resolution Image for New Surgical TechniqueNoch keine Bewertungen
- Histological Comparison of Pulpal Inflamation in Primary Teeth With Occlusal or Proximal CariesDokument8 SeitenHistological Comparison of Pulpal Inflamation in Primary Teeth With Occlusal or Proximal CariesGilmer Solis SánchezNoch keine Bewertungen
- Functional Gastrointestinal Disorders History Pathophysiology Clinical Features and Rome IVDokument20 SeitenFunctional Gastrointestinal Disorders History Pathophysiology Clinical Features and Rome IVwenyinriantoNoch keine Bewertungen
- Community Nursing Care PlanDokument6 SeitenCommunity Nursing Care Plantansincos93% (14)
- REAL in Nursing Journal (RNJ)Dokument8 SeitenREAL in Nursing Journal (RNJ)Anonymous 8hlR5KvNoch keine Bewertungen
- Day 1 - GynacologyDokument204 SeitenDay 1 - GynacologyTingting GeNoch keine Bewertungen
- Sars-Cov-2 & Influenza AB & RSV Antigen Combo Test Kit (Self-Testing)Dokument2 SeitenSars-Cov-2 & Influenza AB & RSV Antigen Combo Test Kit (Self-Testing)Ignacio PerezNoch keine Bewertungen
- (S-W5-Sun-Gen.S) (By Dr. Emad) Gall Bladder 1Dokument28 Seiten(S-W5-Sun-Gen.S) (By Dr. Emad) Gall Bladder 1Haider Nadhem AL-rubaiNoch keine Bewertungen
- Digestive WorksheetDokument8 SeitenDigestive WorksheetBrandon KnightNoch keine Bewertungen
- Psychological Complication in PuerperiumDokument17 SeitenPsychological Complication in Puerperiumbaby100% (2)
- Cost Per Test PC400 2020Dokument10 SeitenCost Per Test PC400 2020fischaNoch keine Bewertungen
- Funda DemoDokument10 SeitenFunda DemoariadnebabasaNoch keine Bewertungen
- Media Release - COVID-19Dokument2 SeitenMedia Release - COVID-19Executive Director100% (2)
- Grand Halad Sa Kapamilya: List of ServicesDokument2 SeitenGrand Halad Sa Kapamilya: List of ServicesLeo LastimosaNoch keine Bewertungen
- World AIDS Day 2023-21797Dokument3 SeitenWorld AIDS Day 2023-21797shyamNoch keine Bewertungen
- Endocrine PancreasDokument21 SeitenEndocrine Pancreaslacafey741Noch keine Bewertungen
- Upper GI Drugs (Pod Pharm 2023, Thatcher)Dokument39 SeitenUpper GI Drugs (Pod Pharm 2023, Thatcher)8jm6dhjdcpNoch keine Bewertungen
- Therapeutic Plasma Exchange in Thrombotic Thrombocytopenic PurpuraDokument9 SeitenTherapeutic Plasma Exchange in Thrombotic Thrombocytopenic Purpurasugi9namliNoch keine Bewertungen
- Trauma in Early Childhood: A Neglected PopulationDokument20 SeitenTrauma in Early Childhood: A Neglected PopulationFrancisca AldunateNoch keine Bewertungen
- ADR Notes KINJAL S. GAMITDokument13 SeitenADR Notes KINJAL S. GAMITKinjal GamitNoch keine Bewertungen
- 33rd IACDE National Conference 2018 - VijayawadaDokument5 Seiten33rd IACDE National Conference 2018 - VijayawadaHari PriyaNoch keine Bewertungen
- CBCT-Scan in DentistryDokument24 SeitenCBCT-Scan in DentistryBilly Sam80% (5)
- 8 Cns StimulantsDokument46 Seiten8 Cns StimulantslouradelNoch keine Bewertungen
- First Aid For The Usmle Step 1 2022-Mcgraw-Hill Education 2022Dokument1 SeiteFirst Aid For The Usmle Step 1 2022-Mcgraw-Hill Education 2022Beto RendonNoch keine Bewertungen
- Ebook John Murtaghs General Practice Companion Handbook PDF Full Chapter PDFDokument67 SeitenEbook John Murtaghs General Practice Companion Handbook PDF Full Chapter PDFroberto.duncan209100% (27)
- What? Who?: DR - Mabel Sihombing Sppd-Kgeh DR - Ilhamd SPPD Dpertemen Ilmu Penyakit Dalam Rs - Ham/Fk-Usu MedanDokument45 SeitenWhat? Who?: DR - Mabel Sihombing Sppd-Kgeh DR - Ilhamd SPPD Dpertemen Ilmu Penyakit Dalam Rs - Ham/Fk-Usu MedanM Rizky Assilmy LubisNoch keine Bewertungen
- Lesson Plan On Nursing Care of A Patient With Acute Renal FailureDokument17 SeitenLesson Plan On Nursing Care of A Patient With Acute Renal FailurePriyanka NilewarNoch keine Bewertungen