Beruflich Dokumente
Kultur Dokumente
Pneumonia Pedia
Hochgeladen von
Krisia CastucianoCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pneumonia Pedia
Hochgeladen von
Krisia CastucianoCopyright:
Verfügbare Formate
PNEUMONIA
What is Pneumonia?
Pneumonia is a general term that refers to an infection of the lungs, which can be caused by a variety
of microorganisms, including viruses, bacteria, fungi, and parasites.
What causes Pneumonia?
Pneumonia is caused by a number of infectious agents, including viruses, bacteria and fungi.
The most common are:
Streptococcus pneumoniae the most common cause of bacterial pneumonia in children;
Haemophilus influenzae type b (Hib) the second most common cause of bacterial
pneumonia;
respiratory syncytial virus is the most common viral cause of pneumonia;
in infants infected with HIV, Pneumocystis jiroveci is one of the commonest causes of
pneumonia, responsible for at least one quarter of all pneumonia deaths in HIV-infected
infants.
Incubation
The incubation period (the length of time between exposure and feeling sick) for pneumonia varies,
depending on the type of virus or bacteria causing the infection. For instance, for RSV, this is 4 to 6
days; for influenza, 18 to 72 hours.
Duration
With treatment, most types of bacterial pneumonia can be cured within 1 to 2 weeks. Viral
pneumonia may last longer. Mycoplasmal pneumonia may take 4 to 6 weeks to resolve completely.
Contagiousness
The viruses and bacteria that cause pneumonia are contagious and usually found in fluid from the
mouth or nose of someone who's infected. Illness can spread when an infected person coughs or
sneezes on others, by sharing drinking glasses and eating utensils, and when someone touches the
used tissues or handkerchiefs of an infected person.
Risk Factors
indoor air pollution caused by cooking and heating with biomass fuels (such as wood or
dung)
living in crowded homes
parental smoking.
A child's immune system may be weakened by malnutrition or undernourishment, especially
in infants who are not exclusively breastfed.
Pre-existing illnesses, such as symptomatic HIV infections and measles, also increase a
child's risk of contracting pneumonia.
What are the signs and symptoms?
Symptoms vary depending on the age of the child and the cause of the pneumonia, but common
ones include:
fever
chills
cough
nasal congestion
unusually rapid breathing (in some cases, this is the only symptom)
Children younger than 2 months: Greater than or equal to 60 breaths/min
Children aged 2-11 months: Greater than or equal to 50 breaths/min
Children aged 12-59 months: Greater than or equal to 40 breaths/min
breathing with grunting or wheezing sounds
labored breathing that makes the rib muscles retract (when muscles under the ribcage or between
ribs draw inward with each breath) and causes nasal flaring
vomiting
chest pain
abdominal pain
decreased activity
loss of appetite (in older kids) or poor feeding (in infants), which may lead to dehydration
in extreme cases, bluish or gray color of the lips and fingernails
Someone with pneumonia in the lower part of the lungs near the abdomen might have fever and
abdominal pain or vomiting but no breathing problems.
Kids with pneumonia caused by bacteria usually becomes sick fairly quickly and will have a
sudden onset of a high fever and unusually rapid breathing.
Kids with pneumonia caused by viruses probably will have symptoms that appear more
gradually and are less severe, though wheezing can be more common in viral pneumonia.
Some types of pneumonia cause symptoms that give important clues about which germ is
causing the illness. For example, in older kids and adolescents, pneumonia due
to Mycoplasma (also called walking pneumonia) is notorious for causing a sore throat, headache,
and rash in addition to the usual symptoms of pneumonia.
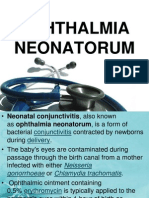
In infants, pneumonia due to chlamydia may cause conjunctivitis (pinkeye) with only mild
illness and no fever. When pneumonia is due to whooping cough (pertussis), a child may have
long coughing spells, turn blue from lack of air, or make the classic "whoop" sound when trying
to take a breath.
Prevention
Vaccines
Antibiotics
Antiviral
Keep your child away from anyone who has an upper respiratory tract infection.
If someone in your home has a respiratory infection or throat infection, keep his or her
drinking glasses and eating utensils separate from those of other family members, and
wash your hands frequently, especially if you are handling used tissues or dirty
handkerchiefs.
Diagnostic Exams
Auscultation by stethoscope
Cultures
Serology
Complete blood cell count (CBC)
Chest radiography
Ultrasonography
Treatment
Antibiotics - given by mouth as tablets or liquid
Pain relieving medications
Paracetamol to reduce fever
Antibiotics given intravenously (via a drip into a vein)
Oxygen therapy - to ensure the body gets the oxygen it needs
Intravenous fluids - to correct dehydration or if the person is too unwell to eat or drink
Physiotherapy - to help clear the sputum from the lungs.
Nursing Diagnoses
Ineffective airway clearance related to copious tracheobronchial secretions
Activity intolerance related to impaired respiratory function
Risk for deficient fluid volume related to fever and a rapid respiratory rate
Imbalanced nutrition: less than body requirements
Deficient knowledge about the treatment regimen and preventive health measures
Complications
Continuing symptoms after initiation of therapy
Shock
Respiratory failure
Atelectasis
Pleural effusion
Confusion
Nursing Care
Assess for:
Respiratory status including rate, depth, ease, shallow or irregular breathing, dyspnea, use
of accesory muscles, and diminished breath sounds, rhonchi or crackles on auscultation -
provides data baseline.
Changes in mental status, skin color, cyanosis - indicates possible decrease in
oxygenation.
Quality of cough and ability to raise secretions including consistency and characteristics
of sputum - removal of secretions prevents obstruction of airways and stasis leading to
further infection and consolidation of lungs; clearing airways facilitates breathing.
Monitor, record, describe:
Respiratory rate, quality and breath sounds q2-q4 - indicates airway resistance, air
movement, severity of disease.
ABGs, oximeter reading - decreased oxygen levels result in hypoxemia.
Administer:
Oxygen therapy via cannula - maintain optimal oxygen level.
Antitussives/expectorants (terpin hydrate, guaifenesin) - acts on bronchial cells to
increase fluid production and promote expectoration; guaifenesin reduces surface tension
of secretions; both relieve non-productive cough
Mucolytic (acetylcysteine) - decrease viscosity of mucus for easier removal.
Antibiotic (ampicillin, cephalexin) - acts by binding to cell wall organisms preventing
synthesis and destroying pathogens.
Perform or Provide:
Position of comfort in semi or high fowlers and change position q2h - facilitates
breathing and allows for full expansion of lungs.
Encourage coughing if sounds is moist; if dry and hacking, increase fluid intake and
administer cough suppressant - reduces continual irritation to throat and liquefies
secretions.
Coughing and deep breathing exercise q2h; use incentive spirometer 5-10 breaths if
tolerated - coughing clears airway by propelling secretions to mouth deep
breathing promotes ventilation and prolongs expiratory phase.
Assist with coughing by splinting chest; humidified air with cool mist - loosens
secretions and improves ventilation, moistens mucous membranes
Postural drainage and percussion PRN - mobilizes secretion.
Suction secretions if cough ineffective - removal if unable to bring up secretions.
Oral care after expectoration and provide tissues and bag for disposal - promotes comfort
and prevents transmission of organisms to others.
In partial fulfillment
of the requirements in
Related Learning Experience
San Lazaro Hospital
Pneumonia
(Report)
Submitted to:
Ms. Romelyn Bautista, RN, MAN
Submitted by:
Ms. Krisia E. Castuciano, SN3
May 13, 2014
Holy Trinity University
College of Nursing and Health Sciences
Puerto Princesa City
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Drug Study - ErcefloraDokument4 SeitenDrug Study - ErcefloraKrisia Castuciano50% (2)
- 253 Complexes For Biomedis Trinity - DescriptionDokument74 Seiten253 Complexes For Biomedis Trinity - Descriptionjanhendrik4444100% (1)
- Structural and Dynamic Bases of Hand Surgery by Eduardo Zancolli 1969Dokument1 SeiteStructural and Dynamic Bases of Hand Surgery by Eduardo Zancolli 1969khox0% (1)
- BLS Aha - 2010 Refresher Course For Junior Clerks 2015Dokument28 SeitenBLS Aha - 2010 Refresher Course For Junior Clerks 2015Kalpana ShahNoch keine Bewertungen
- PamphletDokument2 SeitenPamphletapi-25931970033% (3)
- Biology Final Exam Grade 9Dokument2 SeitenBiology Final Exam Grade 9Yesha Shah100% (1)
- The Historical Foundation of The Philippine ChurchDokument18 SeitenThe Historical Foundation of The Philippine ChurchKrisia CastucianoNoch keine Bewertungen
- Individual Rating ScaleDokument2 SeitenIndividual Rating ScaleKrisia CastucianoNoch keine Bewertungen
- Final MagtulunganDokument35 SeitenFinal MagtulunganKrisia CastucianoNoch keine Bewertungen
- Ump SurgicalDokument1 SeiteUmp SurgicalKrisia CastucianoNoch keine Bewertungen
- Emergency Room DrugsDokument3 SeitenEmergency Room DrugsKrisia CastucianoNoch keine Bewertungen
- German MeaslesDokument2 SeitenGerman MeaslesKrisia CastucianoNoch keine Bewertungen
- Symptoms of RabiesDokument16 SeitenSymptoms of RabiesKrisia CastucianoNoch keine Bewertungen
- Random SamplingDokument1 SeiteRandom SamplingKrisia CastucianoNoch keine Bewertungen
- German MeaslesDokument2 SeitenGerman MeaslesKrisia CastucianoNoch keine Bewertungen
- A. Aegypti Clostridium Tetani: Rabies Virus Australian Bat LyssavirusDokument2 SeitenA. Aegypti Clostridium Tetani: Rabies Virus Australian Bat LyssavirusKrisia CastucianoNoch keine Bewertungen
- OPTALMIANEONATORUMDokument11 SeitenOPTALMIANEONATORUMKrisia CastucianoNoch keine Bewertungen
- Occupational TherapyDokument6 SeitenOccupational TherapyKrisia CastucianoNoch keine Bewertungen
- Drug Study OrthoDokument6 SeitenDrug Study OrthoKrisia CastucianoNoch keine Bewertungen
- Learning Activities - Docx FinaleDokument8 SeitenLearning Activities - Docx FinaleKrisia CastucianoNoch keine Bewertungen
- I. Patient'S Initial Database: Physical AssessmentDokument7 SeitenI. Patient'S Initial Database: Physical AssessmentKrisia CastucianoNoch keine Bewertungen
- Physical Assessment RaDokument8 SeitenPhysical Assessment RaKrisia CastucianoNoch keine Bewertungen
- Health Problem Objectives Activities Materials/ Resources Persons Involved Target DateDokument8 SeitenHealth Problem Objectives Activities Materials/ Resources Persons Involved Target DateKrisia CastucianoNoch keine Bewertungen
- Physical AssessmentDokument10 SeitenPhysical AssessmentKrisia CastucianoNoch keine Bewertungen
- Pa Title PageDokument1 SeitePa Title PageKrisia CastucianoNoch keine Bewertungen
- DR InstrumentsDokument16 SeitenDR InstrumentsKrisia Castuciano100% (1)
- Loa LoaDokument28 SeitenLoa LoaKrisia CastucianoNoch keine Bewertungen
- Loa LoaDokument28 SeitenLoa LoaKrisia CastucianoNoch keine Bewertungen
- AntacidsDokument29 SeitenAntacidsKrisia CastucianoNoch keine Bewertungen
- Antenatal Care: Muhammad Wasil Khan and Ramsha MazharDokument55 SeitenAntenatal Care: Muhammad Wasil Khan and Ramsha MazharmarviNoch keine Bewertungen
- Introduction To HemostasisDokument16 SeitenIntroduction To HemostasisRaiza RuizNoch keine Bewertungen
- Jimma University: Institute of Health Faculty of Health Science School of PharmacyDokument69 SeitenJimma University: Institute of Health Faculty of Health Science School of PharmacyMaህNoch keine Bewertungen
- CT and MRI of Abdomen and PelvicDokument1.691 SeitenCT and MRI of Abdomen and PelvicĐức Khang NguyễnNoch keine Bewertungen
- Eating Disorders Eating Disorders OverviewDokument12 SeitenEating Disorders Eating Disorders OverviewGiancarlo CrespoNoch keine Bewertungen
- NCP EsrdDokument9 SeitenNCP EsrdMarisol Dizon100% (1)
- DementiaDokument26 SeitenDementianadya100% (4)
- Chapter 21 - Nursing Care of The Family During The Postpartum PeriodDokument11 SeitenChapter 21 - Nursing Care of The Family During The Postpartum PeriodJill Hill100% (3)
- SchizophreniaDokument67 SeitenSchizophreniaHazirah Mokhtar100% (1)
- نموذج انقاذ حياة الجديدDokument2 Seitenنموذج انقاذ حياة الجديدraad_alghamdi_1Noch keine Bewertungen
- Patients-RightsDokument1 SeitePatients-Rightsadalacse2016Noch keine Bewertungen
- A Guide To Clinical Case Study and Its PresentationDokument13 SeitenA Guide To Clinical Case Study and Its PresentationVince Troy AquinoNoch keine Bewertungen
- Elementary Reading Comprehension Test 02 PDFDokument4 SeitenElementary Reading Comprehension Test 02 PDFroxanaNoch keine Bewertungen
- Health FormsDokument5 SeitenHealth FormsBianca Louise SengcoNoch keine Bewertungen
- PRN Effectiveness PresentationDokument14 SeitenPRN Effectiveness Presentationapi-457177638Noch keine Bewertungen
- 1 - Patient Evaluation, Diagnosis and Treatment PlanningDokument5 Seiten1 - Patient Evaluation, Diagnosis and Treatment PlanningMohammed100% (1)
- DosulepinDokument4 SeitenDosulepinbrickettNoch keine Bewertungen
- Leah Valenti ResumeDokument2 SeitenLeah Valenti Resumeapi-404670973Noch keine Bewertungen
- Https Cghs - Nic.in Reports View Hospital - JSPDokument36 SeitenHttps Cghs - Nic.in Reports View Hospital - JSPRTI ActivistNoch keine Bewertungen
- Nutrition Month 2011: Isulong Ang Breastfeeding - Tama, Sapat at Eksklusibo! (Tsek) ProgramDokument22 SeitenNutrition Month 2011: Isulong Ang Breastfeeding - Tama, Sapat at Eksklusibo! (Tsek) Programセル ZhelNoch keine Bewertungen
- Steroids Other Appearance Performance Enhancing Drugs Apeds Research ReportDokument34 SeitenSteroids Other Appearance Performance Enhancing Drugs Apeds Research ReportFit and LiftNoch keine Bewertungen
- Treatment MGRDokument12 SeitenTreatment MGRMod AntbugNoch keine Bewertungen
- Nursing Care Plan Guide: Subjective DataDokument1 SeiteNursing Care Plan Guide: Subjective DataJan Oliver YaresNoch keine Bewertungen
- Case Study 5 (Respiratory) - COPDDokument6 SeitenCase Study 5 (Respiratory) - COPDSamantha AquinoNoch keine Bewertungen
- Nursing DiagnosisDokument3 SeitenNursing DiagnosislesternNoch keine Bewertungen