Beruflich Dokumente
Kultur Dokumente
Prospective Case-Control Study of Encephalopathy in Children With
Hochgeladen von
Indra Ihsan0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
12 Ansichten4 SeitenEncephalopathy accounted for 0.5% of 5,400 patients admitted with dengue hemorrhagic fever (DHF) mortality rate was 22%, with the survivors experiencing a complete recovery. Magnetic resonance imaging scans showed cerebral edema in the majority of patients.
Originalbeschreibung:
Originaltitel
Prospective Case-control Study of Encephalopathy in Children With
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenEncephalopathy accounted for 0.5% of 5,400 patients admitted with dengue hemorrhagic fever (DHF) mortality rate was 22%, with the survivors experiencing a complete recovery. Magnetic resonance imaging scans showed cerebral edema in the majority of patients.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
12 Ansichten4 SeitenProspective Case-Control Study of Encephalopathy in Children With
Hochgeladen von
Indra IhsanEncephalopathy accounted for 0.5% of 5,400 patients admitted with dengue hemorrhagic fever (DHF) mortality rate was 22%, with the survivors experiencing a complete recovery. Magnetic resonance imaging scans showed cerebral edema in the majority of patients.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 4
848
Am. J. Trop. Med. Hyg., 65(6), 2001, pp. 848851
Copyright 2001 by The American Society of Tropical Medicine and Hygiene
PROSPECTIVE CASE-CONTROL STUDY OF ENCEPHALOPATHY IN CHILDREN WITH
DENGUE HEMORRHAGIC FEVER
B. V. CAM, L. FONSMARK, N. B. HUE, N. T. PHUONG, A. POULSEN, AND E. D. HEEGAARD
Department of Intensive Care, Pediatric Hospital No. 1, Ho Chi Minh City, Vietnam; Departments of Intensive Care, Pediatrics,
and Clinical Microbiology, University State Hospital, Rigshospitalet, Copenhagen, Denmark
Abstract. We present a prospective case-control study of 27 serologically conrmed dengue hemorrhagic fever
(DHF) patients with severe central nervous system symptoms. Dengue associated encephalopathy accounted for 0.5%
of 5,400 patients admitted with DHF. The mortality rate among children with encephalopathy was 22%, with the
survivors experiencing a complete recovery. Liver enzymes and bilirubin were signicantly elevated in the study
group. In analysis of the cerebrospinal uid (CSF), reverse transcriptasepolymerase chain reaction revealed dengue-
3-specic RNA in one evaluated case. Dengue-specic immunoglobulin M was detected in CSF in 14 of 22 assessable
patients, indicating a localized infection. Magnetic resonance imaging scans showed cerebral edema in the majority
of patients, although encephalitis-like changes were less common. There was an equal distribution of primary and
secondary infections. On the basis of previous reports and of the ndings of our study, DHF probably encompasses
an expanding clinical spectrum that infrequently involves encephalitis due to a direct neurotropic effect of dengue
virus.
INTRODUCTION
Dengue viruses are single-stranded RNA arboviruses and
members of the Flaviviridae family. Infection by any of the
4 serological types of dengue viruses (dengue-14) causes
dengue fever and dengue hemorrhagic fever (DHF), which
represents an increasingly important public health problem
in Western Pacic regions and in Southeast Asia. Unlike
most other arboviral diseases, dengue virus does not usually
cause neurologic symptoms. In recent years, we and others
have occasionally received DHF patients with symptoms of
encephalopathy.
110
The pathophysiology of the neurologic
symptoms in the reported cases have been attributed to ce-
rebral edema, anoxia, hemorrhage, hyponatremia, hepatic
failure, microcapillary hemorrhage, and release of toxic sub-
stances. Animal and clinical studies have recently suggested
a neurotropic potential of dengue virus leading to encepha-
litis in some cases.
5,6,11
We present a prospective case-control study of 27 sero-
logically conrmed DHF patients with severe central ner-
vous system (CNS) symptoms. The patients and the controls
underwent clinical and paraclinical examinations; the infor-
mation we gathered helped us elucidate contributing factors
in dengue-associated encephalitis.
PATIENTS AND METHODS
A prospective case-control study was carried out at Chil-
drens Hospital No. 1, Ho Chi Minh City, Vietnam, October
1997October 1999. Informed consent was obtained from
parents or legal guardians; the hospital ethical review board
approved the project. Pending parental consent and a stable
hemodynamic condition, children aged 16 years with se-
rologically veried DHF and CNS symptoms admitted at the
intensive care unit were enrolled in the study. Possible CNS
symptoms included convulsions, spasticity, focal neurologi-
cal signs, and altered level of consciousness for 8 hr (i.e.,
drowsiness, lethargy, agitation, or coma). The next patient
admitted to the hospital without CNS symptoms but with the
same age and sex and an identical grade of DHF was in-
cluded in the control group. Children with chronic liver or
renal failure, purulent meningitis, cerebral malaria, cerebral
palsy, or epilepsy were excluded.
When the patient was included in the study, we estab-
lished the grade of DHF and the presence of hemorrhagic
symptoms, and we also took a medical history. A neurope-
diatrician evaluated the level of consciousness according to
the Glasgow Coma Score from Days 16. The neurological
status was evaluated until total recovery and for a minimum
of 3 months. Paraclinical tests included glucose, electrolytes,
carbamide, creatinine, bilirubin, aspartate aminotransferase
(AST), alanine aminotransferase (ALT), ammonium, and
prothrombin. Serological tests, including enzyme-linked im-
munosorbent assay and hemagglutination inhibition tests for
both dengue virus and Japanese encephalitis virus, were per-
formed. A lumbar puncture was carried out in members of
the study group, and the cerebrospinal uid (CSF) was an-
alyzed for the presence of protein, glucose, cells, and dengue
virusand Japanese encephalitis virus-specic antibodies.
Reverse transcriptase-polymerase chain reaction (RT-PCR)
and virus isolation were performed at the Pasteur Institute,
Ho Chi Minh City.
12
The study group underwent magnetic
resonance imaging (MRI) scans (evaluated by the same ra-
diologist), and children aged 1 year were additionally sub-
jected to a cerebral ultrasound scan. All patients in the study
and control groups received treatment according to the
World Health Organization guidelines for dengue fever.
RESULTS
Clinical characteristics. During the 2-year study period,
5,400 patients with DHF were admitted to the hospital, of
whom 224 were referred to the intensive care unit. A total
of 27 patients, 10 girls and 17 boys, with dengue encepha-
lopathy were enrolled in the study (incidence of 0.5%). The
median age was 7 years (range, 8 months to 15 years), in-
cluding 6 (22%) infants aged 1 year and 19 (70%) chil-
dren aged 6 years. When classifying the patients, 33%
had DHF grade II, 52% had DHF grade III, and 15% had
DHF grade IV. The control group matched the study group
for all these parameters. The time from onset of disease to
development of neurological symptoms showed a median of
849 ENCEPHALOPATHY IN DENGUE HEMORRHAGIC FEVER
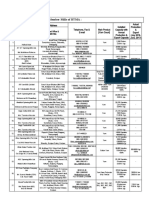
TABLE 1
Signicant paraclinical ndings in 27 patients with encephalopathy and 27 control patients*
Parameter (normal range) Study group Control group P value
Hematocrit (%)
Leukocytes (mm
3
)
Platelets (10
9
/L)
Glycemia (75105 mg %)
Serum sodium (135145 mmol/L)
31.4 7.7
8,378 4,244
76 54
84 43
135.3 5.9
35.5 5.5
5,648 2,440
60 26
106 21
131.8 3.5
0.027
0.005
0.168
0.024
0.011
Uremia (1540 mg %)
Creatinine (mol/L)
Aspartate aminotransferase (3138 U/L)
Alanine aminotransferase (3240 U/L)
48 25
60 41
2,751 3.855
984 777
35 15
50 27
234 485
81 152
0.021
0.346
0.001
0.001
Bilirubin total (1 mg %)
Alkaline phosphatase (350 U/L)
Prothrombin (70100%)
D-dimer (positive)
1.22 0.97
279 227
42 25
17
0.35 0.35
161 59
61 23
6
0.001
0.015
0.005
0.007
* Values are expressed as mean standard deviation. Students t-test was used for calculating all probabilities except D-dimer, for which the chi-square test was used.
6 days (range, 39 days). Twenty-six patients were in a
coma; of these, 21 experienced generalized convulsions and
1 had hemiplegia. Agitation was the inclusion criteria for the
remaining patient. The Glasgow Coma Score at inclusion
and the minimum score for the survivors showed a median
of 6 (range, 311) for both.
Magnetic resonance imaging and ultrasound exami-
nations. Eighteen MRI scans were performed; the clinical
condition of the remaining 9 patients in the study group did
not allow for transportation to the outhospital MRI center.
Four patients showed no abnormal changes, 2 patients had
encephalitislike changes (edema and scattered focal lesions),
and 12 patients showed cerebral edema, one of whom had
intracranial hemorrhage and 2 of whom exhibited encephal-
itislike alterations. In children aged 1 year, cerebral ultra-
sound scans were normal; MRI showed encephalitis in one
and edema in 3 of these 6 patients.
Laboratory ndings. Because of severe coagulation dis-
orders or convulsions, lumbar puncture was performed in
only 22 patients; the control group was not subjected to this
procedure for ethical reasons. Protein, glucose, and cells in
the CSF were all normal. All liver enzyme (AST, ALT, and
alkaline phosphatase) and bilirubin levels were signicantly
elevated in members of the study group; serum sodium was
signicantly decreased in the control group (Table 1). Plate-
lets, serum potassium, ionized serum calcium, creatine, and
ammonia showed no statistical differences between the 2
groups of patients.
Microbiological ndings. All patients in the study and
control groups had an acute dengue infection as evidenced
by the nding of a positive hemagglutination inhibition test
and specic immunoglobulin (Ig) M or a 4-fold increase in
specic IgG. In the CSF, RT-PCR revealed dengue-3-specic
RNA in one evaluated case. Dengue-specic IgM was de-
tected in CSF in 14 (64%) of 22 assessable patients, and
Japanese encephalitis IgM was found in 7 of these patients,
but at a lower titer.
Follow-up. The mortality rate was 22%, with the survi-
vors experiencing a complete recovery of consciousness and
neurologic symptoms within a maximum of 7 days.
Comparison between the 14 CSF IgM-positive and 8 CSF
IgM-negative patients within the study group showed no sta-
tistical differences regarding clinical characteristics, MRI
scans, laboratory ndings, or outcome.
DISCUSSION
Dengue virus is a member of the Flaviviridae family,
which includes a number of neurotropic viruses such as Jap-
anese encephalitis virus, St. Louis encephalitis virus, and
tick-borne encephalitis virus. A growing number of case re-
ports regarding possible neurologic involvement in DHF
prompted us to investigate this relationship in a prospective
case-control study.
During the 2-year study period, patients with dengue-as-
sociated encephalopathy accounted for 0.5% of all patients
admitted with DHF. In a retrospective survey, Hendarto and
Hadinegoro
2
found an incidence of 6.2%, but contrary to the
patients included in our study, the reported patients appeared
to be only mildly affected, with just 14% in a state of stupor
or coma. In addition, a number of patients with DHF and
concurrent neurologic symptoms have been described, main-
ly as case reports or as part of minor series of patients with
unusual manifestations of DHF.
35,710,13,14
In previous reports of neurologic involvement in dengue
infections, the observed encephalopathy was thought to be
due to prolonged DHF with uid extravasation, cerebral ede-
ma, hyponatremia, and liver failure, renal failure, or both,
as opposed to encephalitis dened by a localized invasion
of the CNS. Recent reports, however, have demonstrated a
possible direct neurotropic effect of dengue virus. Animal
studies in mice showed a virus-induced, cytokine-mediated
breakdown of the blood-brain barrier.
11
A survey describing
9 patients with encephalitis in association with a dengue in-
fection detected involvement of the CNS in 4 patients by
the presence of virus or IgM antibodies in CSF.
10
In another
study, dengue virus was observed in the CSF in 5 of 6 pa-
tients presenting with encephalitis, indicating that virus may
cross the blood-brain barrier and directly invade the brain.
5
Search for viral RNA or viral isolation was negative in the
remaining patient, but specic IgM was found in the CSF.
5
Detection of IgM in CSF is indicative of viral replication in
CNS, but the titer is generally lower and short-lived when
compared with serum.
1
Finally, dengue viral antigens were
demonstrated by immunohistochemistry in CNS biopsies
from 5 fatal cases of dengue infection associated with en-
cephalopathy.
6
Results showed that inltration of virus-in-
fected macrophages could be one of the pathways by which
the virus may enter the brain in dengue encephalitis.
6
In
850 CAM AND OTHERS
accordance with these recent reports, we found 14 (64%) of
22 patients had dengue-specic IgM in the CSF, indicating
a localized infection in the CNS.
1
One patient also exhibited
dengue RNA when examined by RT-PCR. Interpretation of
PCR results in viral infections may be difcult, but patients
with a positive PCR result in CSF have a very high proba-
bility ratio for a possible diagnosis of viral infection of the
CNS.
15
On the basis of previous reports and of the ndings
of our study, DHF probably encompasses an expanding clin-
ical spectrum that infrequently involves encephalitis due to
a direct neurotropic effect of dengue virus.
Among members of Flaviviridae, antigenic cross-reactiv-
ity appears to involve a group-reactive antigen shared by all
members. In people with previous nondengue avivirus in-
fection such as Japanese encephalitis, these circulating low-
titered antibodies may show cross-reactivity to dengue virus.
Accordingly, dengue-specic IgM was detected in CSF in
14 of 22 assessable patients, whereas Japanese encephalitis
IgM was found in 7 of the 14 dengue-positive patients, but
at a lower titer. This suggests that detection of both specic
dengue and Japanese encephalitis antibodies should be car-
ried out in regions where these 2 viruses cocirculate.
16
The severity of neurologic disease caused by the different
dengue serotypes has been examined in a number of studies.
In conclusion, serotypes 2 and 3 have primarily been re-
ported to cause neurologic symptoms, and these patients may
experience both primary and secondary infections.
2,3,5,8,17
In
our study group, there was an equal distribution of primary
and secondary infections. Four patients with primary infec-
tion were infants in whom maternal antibodies may have
caused immune enhancement. We did not determine the den-
gue serotype, but at the time of the study, dengue-2 and
dengue-3 were the most prevalent in the community.
Computed tomography has been used to demonstrate ce-
rebral edema in a few patients with dengue-associated en-
cephalopathy.
5
Magnetic resonance imaging is superior to
computed tomography scans when demonstrating most CNS
lesions.
18,19
We present, for the rst time, MRI scans in a
cohort of patients with dengue encephalopathy. The majority
of patients had cerebral edema; encephalitislike changes
were less common. Possibly, the neurologic symptoms we
observed may only infrequently be caused by bleeding, be-
cause just one patient had intracranial hemorrhage.
Abnormal levels of liver enzymes in patients with DHF
are a common nding and may reect liver dysfunction.
20
It is reasonable to assume that DHF in some cases may
cause a hepatic encephalopathy, as reported numerous
times. As seen in Table 1, we found a signicant elevation
of liver enzymes (AST and ALT) that probably was a major
contributing factor in the development of the observed neu-
rologic symptoms. It is equally true, however, that we
found evidence of viral replication in CNS in a large pro-
portion of the patients we studied, which in our view jus-
ties the use of the term dengue-associated encephalitis.
Unfortunately, we do not know whether DHF patients with-
out neurologic symptoms have evidence of viral replication
in the CNS.
In conclusion, dengue encephalitis seems to be a true, al-
beit rare, entity. The patients are characterized by marked
depression of consciousness, signicantly elevated liver en-
zymes, and a substantial mortality; the survivors, on the oth-
er hand, experienced complete recovery. Pathophysiological
ndings include cerebral edema as well as specic IgM and
RNA in CSF.
Financial support: The Danish International Development Agency
supported this study as part of a 3-year program including studies
of prevention, diagnosis, and treatment of dengue fever in Vietnam.
Authors addresses: B. V. Cam, N. B. Hue, and N. T. Phuong, De-
partment of Intensive Care, Pediatric Hospital No. 1, 2 Su Van Hanh
St, District 10, Ho Chi Minh City, Vietnam. L. Fonsmark, Depart-
ment of Intensive Care, Section 3141, A. Poulsen, Department of
Pediatrics, Section 4064, E. D. Heegaard, Department of Clinical
Microbiology, Section 9301, University State Hospital, Rigshospi-
talet, Juliane Maries Vej, 2100 Copenhagen , Denmark.
REFERENCES
1. Chen WJ, Hwang KP, Fang AH, 1991. Detection of IgM anti-
bodies from cerebrospinal uid and sera of dengue fever pa-
tients. Southeast Asian J Trop Med Public Health 22: 659
663.
2. Hendarto SK, Hadinegoro SR, 1992. Dengue encephalopathy.
Acta Paediatr Jpn 34: 350357.
3. Hommel D, Talarmin A, Deubel V, Reynes JM, Drouet MT,
Sarthou JL, Hulin A, 1998. Dengue encephalitis in French
Guiana. Res Virol 149: 235238.
4. Kho LK, Sumarmo, Wulur H, Jahja EC, Gubler DJ, 1981. Den-
gue hemorrhagic fever accompanied by encephalopathy in Ja-
karta. Southeast Asian J Trop Med Public Health 12: 8386.
5. Lum LC, Lam SK, Choy YS, George R, Harun F, 1996. Dengue
encephalitis: a true entity? Am J Trop Med Hyg 54: 256259.
6. Miagostovich MP, Ramos RG, Nicol AF, Nogueira RM, Cuzzi-
Maya T, Oliveira AV, Marchevsky RS, Mesquita RP, Schatz-
mayr HG, 1997. Retrospective study on dengue fatal cases.
Clin Neuropathol 16: 204208.
7. Nimmannitya S, Thisyakorn U, Hemsrichart V, 1987. Dengue
haemorrhagic fever with unusual manifestations. Southeast
Asian J Trop Med Public Health 18: 398406.
8. Row D, Weinstein P, Murray-Smith S, 1996. Dengue fever with
encephalopathy in Australia. Am J Trop Med Hyg 54: 253
255.
9. Thakare J, Walhekar B, Banerjee K, 1996. Hemorrhagic mani-
festations and encephalopathy in cases of dengue in India.
Southeast Asian J Trop Med Public Health 27: 471475.
10. Solomon T, Dung NM, Vaughn DW, Kneen R, Thao LT, Raeng-
sakulrach B, Loan HT, Day NP, Farrar J, Myint KS, Warrell
MJ, James WS, Nisalak A, White NJ, 2000. Neurological
manifestations of dengue infection. Lancet 355: 10531059.
11. Chaturvedi UC, Dhawan R, Khanna M, Mathur A, 1991. Break-
down of the blood-brain barrier during dengue virus infection
of mice. J Gen Virol 72 (Pt. 4): 859866.
12. Lanciotti RS, Calisher CH, Gubler DJ, Chang GJ, Vorndam AV,
1992. Rapid detection and typing of dengue viruses from clin-
ical samples by using reverse transcriptase-polymerase chain
reaction. J Clin Microbiol 30: 545551.
13. Patey O, Ollivaud L, Breuil J, Lafaix C, 1993. Unusual neuro-
logic manifestations occurring during dengue fever infection.
Am J Trop Med Hyg 48: 793802.
14. Strobel M, Lamaury I, Contamin B, Jarrige B, Perez JM, Steck
AJ, Goursaud R, 1999. Dengue fever with neurologic expres-
sion. Three cases in adults (in French). Ann Med Intern (Par-
is) 150: 7982.
15. Jeffery KJ, Read SJ, Peto TE, Mayon-White RT, Bangham CR,
1997. Diagnosis of viral infections of the central nervous sys-
tem: clinical interpretation of PCR results. Lancet 349: 313
317.
16. Innis BL, Nisalak A, Nimmannitya S, Kusalerdchariya S,
Chongswasdi V, Suntayakorn S, Puttisri P, Hoke CH, 1989.
An enzyme-linked immunosorbent assay to characterize den-
gue infections where dengue and Japanese encephalitis co-
circulate. Am J Trop Med Hyg 40: 418427.
851 ENCEPHALOPATHY IN DENGUE HEMORRHAGIC FEVER
17. Sistayanarain A, Maneekarn N, Polprasert B, Sirisanthana V,
Makino Y, Fukunaga T, Sittisombut N, 1996. Primary se-
quence of the envelope glycoprotein of a dengue type 2 virus
isolated from patient with dengue hemorrhagic fever and en-
cephalopathy. Southeast Asian J Trop Med Public Health 27:
221227.
18. Gilman S, 1998. Imaging the brain. Second of two parts. N Engl
J Med 338: 889896.
19. Gilman S, 1998. Imaging the brain. First of two parts. N Engl
J Med 338: 812820.
20. Nguyen TL, Nguyen TH, Tieu NT, 1997. The impact of dengue
haemorrhagic fever on liver function. Res Virol 148: 273277.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Journal Pone 0138465Dokument16 SeitenJournal Pone 0138465Indra IhsanNoch keine Bewertungen
- Sistematik ReviewDokument4 SeitenSistematik ReviewIndra IhsanNoch keine Bewertungen
- Pogatzki Zahn2017Dokument16 SeitenPogatzki Zahn2017Indra IhsanNoch keine Bewertungen
- Pogatzki Zahn2017Dokument16 SeitenPogatzki Zahn2017Indra IhsanNoch keine Bewertungen
- Acute Kidney Injury in Dengue Virus Infection: MinireviewDokument5 SeitenAcute Kidney Injury in Dengue Virus Infection: MinireviewIndra IhsanNoch keine Bewertungen
- Acute Respiratory Distress Syndrome: A Rare Complication in Pediatric Diabetic KetoacidosisDokument3 SeitenAcute Respiratory Distress Syndrome: A Rare Complication in Pediatric Diabetic KetoacidosisIndra IhsanNoch keine Bewertungen
- Severe Sepsis and Septic Shock - RiversDokument28 SeitenSevere Sepsis and Septic Shock - RiversMihai SalceanuNoch keine Bewertungen
- Mi Kro AlbuminuriaDokument5 SeitenMi Kro AlbuminuriaIndra IhsanNoch keine Bewertungen
- Case Report Aki N RabdoDokument4 SeitenCase Report Aki N RabdoIndra IhsanNoch keine Bewertungen
- Cold Spring Harb Perspect Med-2012-ThurstonDokument14 SeitenCold Spring Harb Perspect Med-2012-ThurstonIndra IhsanNoch keine Bewertungen
- Predictor OutcomesDokument3 SeitenPredictor OutcomesIndra IhsanNoch keine Bewertungen
- Aminofilin and Critical IllDokument9 SeitenAminofilin and Critical IllIndra IhsanNoch keine Bewertungen
- WHO 2015 - Mal TX Guidelines - 9789241549127 - Eng PDFDokument318 SeitenWHO 2015 - Mal TX Guidelines - 9789241549127 - Eng PDFDody ChandraNoch keine Bewertungen
- Syok Pediatrics PDFDokument8 SeitenSyok Pediatrics PDFSri Juliana NasutionNoch keine Bewertungen
- Format Diskusi Bed Site TeachingDokument1 SeiteFormat Diskusi Bed Site TeachingIndra IhsanNoch keine Bewertungen
- Breathing GuidelineDokument114 SeitenBreathing GuidelineMedico Nol DelaphanNoch keine Bewertungen
- Eng PDFDokument34 SeitenEng PDFAkbar RihansyahNoch keine Bewertungen
- Protocol ADSDokument13 SeitenProtocol ADSIndra IhsanNoch keine Bewertungen
- 1535Dokument2 Seiten1535Indra IhsanNoch keine Bewertungen
- Ten KasusDokument4 SeitenTen KasusIndra IhsanNoch keine Bewertungen
- Format Diskusi Bed Site TeachingDokument1 SeiteFormat Diskusi Bed Site TeachingIndra IhsanNoch keine Bewertungen
- 12 CompleteDokument154 Seiten12 CompleteIndra IhsanNoch keine Bewertungen
- Viz., Chloramphenicol, Amoxycillin And: Cefotaxime in Multi Drug Resistant Typhoid FeverDokument4 SeitenViz., Chloramphenicol, Amoxycillin And: Cefotaxime in Multi Drug Resistant Typhoid FeverIndra IhsanNoch keine Bewertungen
- Angiopoietin-1 and - 2 Biomarkers For Infectious Diseases That Compromise Endothelial IntegrityDokument20 SeitenAngiopoietin-1 and - 2 Biomarkers For Infectious Diseases That Compromise Endothelial IntegrityIndra IhsanNoch keine Bewertungen
- NCHS, USaDokument8 SeitenNCHS, USaIndra IhsanNoch keine Bewertungen
- Dengue and Liver Disease: Ira ShahDokument3 SeitenDengue and Liver Disease: Ira ShahIndra IhsanNoch keine Bewertungen
- Dengue EncephalopathyDokument2 SeitenDengue EncephalopathyIndra IhsanNoch keine Bewertungen
- Pa To GenesisDokument19 SeitenPa To GenesisIndra IhsanNoch keine Bewertungen
- Prospective Case-Control Study of Encephalopathy in Children WithDokument4 SeitenProspective Case-Control Study of Encephalopathy in Children WithIndra IhsanNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- OSCE - Chest PainDokument2 SeitenOSCE - Chest PaincgalongNoch keine Bewertungen
- Student WorkDokument7 SeitenStudent Workapi-316130138Noch keine Bewertungen
- Sangita Das 2Dokument3 SeitenSangita Das 2ettanpsNoch keine Bewertungen
- Pre Columbian Art Including Selection of LempertzDokument148 SeitenPre Columbian Art Including Selection of LempertzAQQUIROGA50% (2)
- Review of Indigenous Sheep Breeds Production Systems in EthiopiaDokument7 SeitenReview of Indigenous Sheep Breeds Production Systems in EthiopiaInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- The 12 Days of ChristmasDokument2 SeitenThe 12 Days of ChristmasCarla Muss-JacobsNoch keine Bewertungen
- Esthetic Rehabilitation of A Severely Worn Dentition With MIPPDokument22 SeitenEsthetic Rehabilitation of A Severely Worn Dentition With MIPPKarla Margine PérezNoch keine Bewertungen
- Un SMP 2016Dokument27 SeitenUn SMP 2016SmpMugaruNoch keine Bewertungen
- Reading Comprehension For Grade 3 PDFDokument6 SeitenReading Comprehension For Grade 3 PDFIVAN CONRADNoch keine Bewertungen
- CASE PRE (Intrapartum)Dokument6 SeitenCASE PRE (Intrapartum)teuuuuNoch keine Bewertungen
- Military Working Dog ProgramDokument155 SeitenMilitary Working Dog Programjojo2486100% (3)
- Lion and Tiger Hybrid: Liger: Presented By: Harsh Salunkhe Xi ScienceDokument14 SeitenLion and Tiger Hybrid: Liger: Presented By: Harsh Salunkhe Xi ScienceHarsh SalunkheNoch keine Bewertungen
- Artificial Salmon SpawningDokument28 SeitenArtificial Salmon SpawningjimborenoNoch keine Bewertungen
- Zak's Class SystemDokument115 SeitenZak's Class SystemGeorge Quail100% (2)
- Lapbook About CanadaDokument45 SeitenLapbook About CanadaTanyaHrabovaNoch keine Bewertungen
- Psychology of ThinkingDokument19 SeitenPsychology of ThinkingDiyana HalimNoch keine Bewertungen
- Chapter 7 Study GuideDokument4 SeitenChapter 7 Study GuidejbradeeNoch keine Bewertungen
- Medical Form For NimDokument1 SeiteMedical Form For NimvishalNoch keine Bewertungen
- List of Yarn Manufacturing Member Mills of BTMADokument26 SeitenList of Yarn Manufacturing Member Mills of BTMAMd. Monowarul IslamNoch keine Bewertungen
- Annotatedbib2 DebockDokument2 SeitenAnnotatedbib2 Debockapi-282281003Noch keine Bewertungen
- Flower Crochet Ebook - 294885.PDF (Pdfdrive)Dokument125 SeitenFlower Crochet Ebook - 294885.PDF (Pdfdrive)Lhen Pranciliso100% (1)
- Module TP AzzuraDokument80 SeitenModule TP AzzuraNOOR SHAREEZA AZZURA BINTI SHAHRUDDIN MoeNoch keine Bewertungen
- Hematology 1 MidtermsDokument31 SeitenHematology 1 Midtermsella SyNoch keine Bewertungen
- Coral ReefsDokument13 SeitenCoral Reefsapi-252647924Noch keine Bewertungen
- امتحان اللغة الانجليزية سادس ف2-د2 2014-2015مDokument14 Seitenامتحان اللغة الانجليزية سادس ف2-د2 2014-2015مMundhir Al-KhusaibiNoch keine Bewertungen
- Fausto & Costa - Cambridge - Anthropology - 2013Dokument7 SeitenFausto & Costa - Cambridge - Anthropology - 2013Paulo BüllNoch keine Bewertungen
- Explorers 4 Unit 6 Under The Sea 2Dokument3 SeitenExplorers 4 Unit 6 Under The Sea 2Gregorio CuadradoNoch keine Bewertungen
- Animation Changelog 12.25.2022Dokument3 SeitenAnimation Changelog 12.25.2022Miguel CortesNoch keine Bewertungen
- AMCAT CocubesDokument35 SeitenAMCAT CocubesMuthyala Akhil100% (6)
- The Five Human SensesDokument17 SeitenThe Five Human SensesAntonio Gonzalez100% (1)