Beruflich Dokumente
Kultur Dokumente
The Role of Radiotherapy in Cancer Treatment
Hochgeladen von
arakbae0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
113 Ansichten9 SeitenThe role of radiotherapy in cancer treatment
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenThe role of radiotherapy in cancer treatment
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
113 Ansichten9 SeitenThe Role of Radiotherapy in Cancer Treatment
Hochgeladen von
arakbaeThe role of radiotherapy in cancer treatment
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 9
The Role of Radiotherapy in Cancer Treatment
Estimating Optimal Utilization from a Review of Evidence-Based Clinical Guidelines
Geoff Delaney, M.B.B.S, M.D.
1,2
Susannah Jacob, M.B.B.S., M.D., M.H.A.
1
Carolyn Featherstone, M.B.Ch.B.
1
Michael Barton, M.B.B.S.
1,2
1
Collaboration for Cancer Outcomes Research and
Evaluation (CCORE), Liverpool Hospital, Sydney,
Australia.
2
University of New South Wales, Sydney, Austra-
lia.
This project was funded by a grant from the
Australian Commonwealth Department of Health
and Ageing.
The authors thank the members of the steering
committee of the Australian National Cancer Con-
trol Initiative and the forty-two reviewers involved
in this project for their comments on the study
design and decision trees.
Carolyn Featherstones current address: Beatson
Oncology Centre, Glasgow, Scotland, United King-
dom.
Address for reprints: Geoff Delaney, M.B.B.S.,
M.D., Collaboration for Cancer Outcomes, Re-
search and Evaluation, Liverpool Hospital,
Locked Bag 7103, Liverpool BC, NSW 1871,
Australia; Fax: (011) 61 2 9828 5299; E-mail:
Geoff.Delaney@swsahs.nsw.gov.au
Received February 14, 2005; revision received
April 25, 2005; accepted May 25, 2005.
Radiotherapy utilization rates for cancer vary widely internationally. It has previ-
ously been suggested that approximately 50% of all cancer patients should receive
radiation. However, this estimate was not evidence-based. The aim of this study
was to estimate the ideal proportion of new cases of cancer that should receive
radiotherapy at least once during the course of their illness based on the best
available evidence. An optimal radiotherapy utilization tree was constructed for
each cancer based upon indications for radiotherapy taken from evidence-based
treatment guidelines. The proportion of patients with clinical attributes that indi-
cated a possible benet from radiotherapy was obtained by adding epidemiologic
data to the radiotherapy utilization tree. The optimal proportion of patients with
cancer that should receive radiotherapy was then calculated using TreeAge (Tree-
Age Software, Williamstown, MA) software. Sensitivity analyses using univariate
analysis and Monte Carlo simulations were performed. The proportion of patients
with cancer in whom external beam radiotherapy is indicated according to the best
available evidence was calculated to be 52%. Monte Carlo analysis indicated that
the 95% condence limits were from 51.7% to 53.1%. The tightness of the con-
dence interval suggests that the overall estimate is robust. Comparison with actual
radiotherapy utilization data suggests a shortfall in actual radiotherapy delivery.
This methodology allows comparison of optimal rates with actual rates to identify
areas where improvements in the evidence-based use of radiotherapy can be
made. It provides valuable data for radiotherapy service planning. Actual rates
need to be addressed to ensure better radiotherapy utilization. Cancer 2005;104:
112937. 2005 American Cancer Society.
KEYWORDS: radiotherapy utilization, cancer, evidence-based.
T
he planning of efcient and equitable treatment services for a
population requires a rational and defensible estimate of demand.
This has particular relevance for planning services that require sig-
nicant capital expenditure such as radiotherapy. Radiotherapy is an
essential mode of cancer treatment and contributes to the cure or
palliation of many cancer patients. Radiotherapy facilities have high
capital costs and their operation is staff intensive. In this project, we
have undertaken to calculate a rational estimate of need for radio-
therapy, based on the occurrence of each type of cancer, the evi-
dence-based indication for radiotherapy in the treatment of each type
of cancer, and the probability that radiotherapy will be chosen as a
form of treatment.
The radiotherapy utilization rate is dened as the proportion of a
dened population of patients with cancer that receives at least one
course of radiotherapy during their lifetime. Previous reports from
Australian Commonwealth and State agencies have proposed that
50% of all new cases of notiable cancer in Australia should be treated
1129
2005 American Cancer Society
DOI 10.1002/cncr.21324
Published online 3 August 2005 in Wiley InterScience (www.interscience.wiley.com).
with external beam radiotherapy.
15
(Notiable can-
cers are cancers for which registry data are available.)
Although this gure is based almost entirely on expert
opinion, it is currently accepted as the guide for esti-
mating utilization and is used to plan for the distribu-
tion and number of linear accelerators. However, its
validity is questionable, and it is not responsive to
changing clinical indications. There are signicant
variations in actual radiotherapy utilization rates re-
ported in Australia, the United States, Canada, and the
Nordic countries, where utilization ranges from 20
55% of all new cancer cases.
611
These variations stress
the importance of using rigorous evidence-based
methods to estimate an optimal radiotherapy utiliza-
tion rate that can act as a benchmark against which
actual utilization rates can be compared.
This report estimates an ideal rate of radiotherapy
utilization for cancer in Australia based on the inci-
dence of each type of cancer, the evidence-based in-
dication for radiotherapy in the treatment of that can-
cer, and the proportion of cancer patients included in
that indication for radiotherapy.
The authors of the current study have previously
published optimal radiotherapy utilization rates for
breast carcinoma,
12
lung carcinoma,
13
melanoma,
14
gastrointestinal cancers,
15
genitourinary cancers,
16
head and neck cancers,
17
gynecologic cancers,
18,19
he-
matologic malignancies,
20,21
central nervous system
tumors, unknown primary cancers, and thyroid carci-
nomas.
22
This article reports the estimated overall op-
timal radiotherapy utilization rate for all registered
cancers in Australia and compares the optimal rate
with known actual rates of radiotherapy utilization.
Objectives
The objectives of this study were:
To estimate the ideal proportion of new cases of no-
tiable cancer that should receive megavoltage
external-beam radiotherapy at some time during
the course of their illness using the best available
evidence.
To develop a model of radiotherapy utilization that
can be used to estimate the effect of future
changes in the relative distribution of tumor sites,
changes in stage at presentation, and changes in
indications for radiotherapy on the optimal radio-
therapy utilization rate.
To compare the estimated optimal rates with actual
rates of radiotherapy use.
MATERIALS AND METHODS
In this study, an indication for radiotherapy was
dened as a clinical situation in which radiotherapy
was recommended as the treatment of choice on the
basis of published evidence that radiotherapy has a
superior clinical outcome compared to alternative
treatment modalities (including no treatment) and
where the patient was suitable to undergo radiother-
apy based on an assessment of performance status
indicators and the presence or absence of comorbidi-
ties. The superiority of radiotherapy over other treat-
ment options could be because of better survival, local
control, or toxicity proles. The study was limited to
all notiable cancers with an incidence of 1% of the
Australian cancer population. Notiable cancers are
cancers for which registry data are available. In Aus-
tralia this includes ductal carcinoma in situ of the
breast but does not include nonmelanomatous skin
cancers and benign tumors.
The indications for radiotherapy for each cancer
site were derived from treatment guidelines issued by
national and international institutions or specialist
groups and published (including on the Internet) be-
fore December 2003. If guidelines did not exist for
particular cancer types and tumor sites, or where the
guidelines did not adequately address radiotherapy
use, other sources of evidence were identied. These
included treatment reviews, randomized controlled
trials, population-based studies of care, and single-
institution studies.
The evidence for indications for radiotherapy was
classied using the Australian National Health and
Medical Research Council (NHMRC) hierarchy of lev-
els of evidence (Table 1), with only the highest level of
evidence being used for each indication for radiother-
apy.
23
As our purpose was to make recommendations
for radiotherapy services in Australia, the highest pri-
ority was given to Australian evidence-based clinical
practice guidelines issued by national institutions
such as the NHMRC or the National Breast Cancer
Centre. If these did not exist, then guidelines from
other countries were used wherever possible.
Radiotherapy utilization trees for individual can-
cer sites were constructed based upon the treatment
TABLE 1
Levels of Evidence for Indications for Radiotherapy
23
Level of evidence Description
I Systematic review of all relevant randomized studies
II At least 1 properly conducted randomized trial
III Well designed controlled trials without randomization
a
IV Case series
a
These include trials with pseudo-randomization where a awed randomization method occurred
(e.g., alternate allocation of treatments) or comparative studies with either comparative or historical
controls.
1130 CANCER September 15, 2005 / Volume 104 / Number 6
recommendations obtained from evidence-based
treatment guidelines. We used decision analysis soft-
ware (TreeAge Data version 3.5, TreeAge Software,
Williamstown, MA) to illustrate the indications for ra-
diotherapy in a diagrammatic form (as a tree), to per-
form basic calculations such as multiplication of fac-
tors and summation of the results, and to perform
sensitivity analyses of variability. Parameters can be
readily adjusted in the tree if indications for radiother-
apy or epidemiologic data distributions change in the
future and the software can then rapidly calculate the
adjusted utilization rates.
The utilization trees depict the clinical conditions
for which radiotherapy is indicated. Each terminal
branch of the tree shows whether or not radiotherapy
is recommended for a particular type of cancer in
individuals with specic clinical attributes. In some
circumstances, the indication for radiotherapy oc-
curred in the initial stages of management. In other
circumstances, radiotherapy was given later in the
disease course (for instance, in patients who devel-
oped a local recurrence and who had not previously
had an indication for treatment with radiotherapy).
Similar methodology has been used by others.
6,2426
This is the rst published report of an analysis of all
cancers.
The purpose of our project was to determine the
proportion of all cancer patients who have at least one
indication for radiotherapy at some time in the course
of their illness. Patients requiring radiotherapy were
therefore counted only once, even if they had multiple
indications at different stages in their illness.
The radiotherapy utilization trees also depict the
proportion of patients represented by each branch
point of the tree. The relative quality of epidemiologic
data from various sources was ranked according to a
scoring system that gave greatest importance to Aus-
tralian population-based data. Population-based
datasets from other countries were also used. Popula-
tion-based databases were preferred because they
were considered less likely to be affected by referral or
selection bias (compared with hospital-based data-
bases) and, therefore, were more likely to be represen-
tative of the entire population of patients with cancer.
Table 2 shows the hierarchy of quality of epidemio-
logic data used.
The proportion of patients for whom radiotherapy
would be recommended was calculated for each can-
cer site by calculating the frequency of each indication
for radiotherapy and then summing the frequencies to
give the total optimal rate of use. The overall optimal
radiotherapy utilization rate was calculated by sum-
ming the optimal utilization rates derived for each
cancer site, calculated as a proportion of all cancers.
As this project involved determining estimates for
optimal radiotherapy utilization for all notiable can-
cers with an incidence of 1%, the remaining cancers
that have an incidence of 1% have been called
other cancers in the radiotherapy utilization tree
and comprise 2% of the entire cancer population ac-
cording to the Australian Institute of Health and Wel-
fare report.
27
These cancers include pediatric cancers,
sarcomas of soft tissue and bone, cancers of the me-
diastinum, orbit, peritoneum, retroperitoneum, penis,
and pleura as well as other rare malignancies. Some of
these malignancies are commonly treated with radio-
therapy (such as soft tissue sarcomas), and others are
rarely treated with radiation (e.g., peritoneal and pleu-
ral tumors). For the purpose of the current study,
specic radiotherapy utilization trees were not con-
structed for each of these uncommon cancers. We
assumed that the requirement for radiotherapy for
this miscellaneous group was 50% and then per-
formed sensitivity analysis where the use of radiother-
apy for other cancers ranges between 0% and 100%.
This is included in the sensitivity analysis performed
for the entire radiotherapy decision tree and is de-
scribed later.
For some branches of the trees, there was a rela-
tive lack of high quality epidemiologic data, and, for
some other branches, epidemiologic data differed sig-
nicantly across different data sources of equal qual-
ity. Monte Carlo simulations were performed to assess
the impact on the radiotherapy utilization rate that
would result from variations in epidemiologic data,
different probabilities of benet from treatment, or
uncertainty in the indication for radiotherapy. Monte
Carlo simulations are based upon random sampling of
variables from discrete and continuous distributions
using individual trial data. Observing the statistical
TABLE 2
Hierarchy of Epidemiologic Data
a
Quality of
source Source Type
Australian National Epidemiological data
Australian State Cancer Registry
Epidemiologic databases from other large international groups
(e.g. SEER)
Results from reports of a random sample from a population
Comprehensive multiinstitution database
Comprehensive single-institution database
Multiinstitution reports on selected groups (e.g. multiinstitution
clinical trials)
Single-institution reports on selected groups of cases
Expert opinion
a
Modied from Tyledsley et al.
6
Radiotherapy Utilization in Cancer/Delaney et al. 1131
properties of many trials using random sampled val-
ues allows additional insight into performance of a
model. The main weakness of the Monte Carlo anal-
ysis, in the current study, is that the relative impor-
tance of all of data used is weighted by study size and
may not necessarily be ranked by study quality, which
was impossible to assess for each dataset.
Funding and Peer Review
The project was funded by the Department of Health
and Ageing of the Australian Government and super-
vised by the National Cancer Control Initiative (NCCI).
An expert steering committee was convened for this
project by the NCCI with representation from major
nongovernmental cancer organizations, consumers,
epidemiologists, radiation and medical oncologists,
surgeons, palliative care specialists, and experts in
evidence and treatment guidelines.
A multidisciplinary panel of expert reviewers was
established, comprising ninety-one nationally recog-
nized oncology experts from the elds of medical,
surgical, and radiation oncology, palliative care, and
oncology nursing. Forty-two of these reviewers pro-
vided comments, and 43% of reviewers were from
nonradiation oncology specialties also commented.
Comparison with Actual Radiotherapy Utilization Rates
Actual radiotherapy utilization rates were obtained
from published and unpublished sources covering the
years 1990 to 2001. These actual rates were tabulated
and compared with estimated optimal radiotherapy
utilization rates.
RESULTS
Recommended optimal radiotherapy utilization rates
and optimal radiotherapy utilization trees for breast,
12
lung,
13
skin (melanoma),
14
genitourinary,
16
gastroin-
testinal,
15
gynecologic,
18,19
and head and neck can-
cers,
17
hematologic malignancies,
20,21
and central ner-
vous system, thyroid, and unknown primary site
tumors
22
have been reported in detail elsewhere. A
summary of the calculated ideal radiotherapy utiliza-
tion rates for the various tumor sites are presented in
Table 3 along with the proportion of cancer that each
tumor site composes in Australia.
Overall Optimal Radiotherapy Utilization Rate
The optimal radiotherapy utilization rates in Table 3
varied from a low recommended rate of 0% for liver
cancer patients to a high rate of 92% for patients with
central nervous system tumors. The recommended
TABLE 3
Optimal Radiotherapy Utilization Rate by Cancer Type
Tumor type
Proportion of
all cancers
Proportion of
patients receiving
radiotherapy
Patients receiving
radiotherapy
(% of all cancers) Reference
Breast 0.13 83 10.8 Delaney et al.
12
Lung 0.10 76 7.6 Delaney et al.
13
Melanoma 0.11 23 2.5 Delaney et al.
14
Prostate 0.12 60 7.2 Delaney et al.
16
Gynecologic 0.05 35 1.8 Delaney et al.
18,19
Colon 0.09 14 1.3 Delaney et al.
15
Rectum 0.05 61 3.1 Delaney et al.
15
Head and neck 0.04 78 3.1 Delaney et al.
17
Gall bladder 0.01 13 0.1 Delaney et al.
15
Liver 0.01 0 0.0 Delaney et al.
15
Esophageal 0.01 80 0.8 Delaney et al.
15
Stomach 0.02 68 1.4 Delaney et al.
15
Pancreas 0.02 57 1.1 Delaney et al.
15
Lymphoma 0.04 65 2.6 Featherstone et al.
20
Leukemia 0.03 4 0.1 Featherstone et al.
21
Myeloma 0.01 38 0.4 Featherstone et al.
21
Central nervous system 0.02 92 1.8 Delaney et al.
22
Renal 0.03 27 0.8 Delaney et al.
16
Bladder 0.03 58 1.7 Delaney et al.
16
Testis 0.01 49 0.5 Delaney et al.
16
Thyroid 0.01 10 0.1 Delaney et al.
22
Unknown primary 0.04 61 2.4 Delaney et al.
22
Other 0.02 50 1.0 See citations in text
Total 1.00 - 52.3
1132 CANCER September 15, 2005 / Volume 104 / Number 6
overall optimal radiotherapy utilization rate was cal-
culated to be 52.3%.
Sensitivity Analysis
Some variables in the utilization tree were associated
with signicant uncertainties, which can be catego-
rized as follows:
1. Uncertainty in the data where the values of epi-
demiologic data obtained from multiple sources
differed signicantly. Typically these were near
the terminal ends of the tree where large studies
on incidence rates were lacking.
2. Uncertainty in the indication for radiotherapy
where guidelines had no specic criteria, or con-
icting criteria, for consideration of radiotherapy.
For example, one guideline for breast cancer rec-
ommended radiotherapy for postmastectomy pa-
tients with 3 axillary nodes involved, but also
advocated consideration of radiotherapy in all
patients with nodal involvement.
28
Other guide-
lines either mention that radiotherapy in patients
with involvement of less than 4 axillary lymph
nodes is controversial
29
or avoid the issue com-
pletely.
30
3. Uncertainty in the choice between radiotherapy
and other treatment options of equal efcacy,
such as surgery, observation, or radiotherapy for
localized prostate adenocarcinoma.
The actual branchpoints where these uncertain-
ties existed have been described in reports of each
specic cancer sites radiotherapy utilization trees.
Sensitivity analysis allows an assessment of the effect
that data uncertainty may have on the overall radio-
therapy utilization estimate. Two different types of
sensitivity analyses were performed. One-way sensi-
tivity analyses allowed assessment of the effect of
varying the value of each variable on the overall model
in a univariate fashion. One-way sensitivities were
presented for each of the decision trees where uncer-
tainty existed and are not repeated here.
1217,1922
For
a more global multivariate-type assessment, Monte
Carlo simulations can be performed to assess the ef-
fect of multiple uncertainties on the overall radiother-
apy utilization rate. Monte Carlo simulations are
based upon random sampling of variables from dis-
crete and continuous distributions using individual
trial data. Multivariate sensitivity analysis using Monte
Carlo analysis on 10
4
simulations indicates that the
95% condence limits for our optimal radiotherapy
estimate were 51.7% and 53.1%.
Comparison with Actual Radiotherapy Utilization Rates
Table 4 shows the actual rates of radiotherapy utiliza-
tion from population-based reports from Sweden, the
United Kingdom, the United States and some national
and state patterns of care studies in Australia.
5,3139
DISCUSSION
We have used an evidence-based technique to calcu-
late an overall estimate of optimal radiotherapy utili-
zation of 52.3% for all notiable cancer in Australia.
This nal estimate is remarkably precise (as measured
by the tight condence limits) despite uncertainty ex-
isting in relation to data for some indications for ra-
diotherapy and occasional uncertainty between treat-
ment options of approximately equal efcacy. The
tight condence interval may be explained by the fact
that good quality data existed for the initial branches
of the tree (for example, data such as tumor type and
stage at presentation). Most of the uncertainty existed
in the distal or near-terminal branches of the tree and,
therefore, affected only very small proportions of the
cancer population and had little effect on the overall
estimate. In addition, the effect of these variations was
such that some would increase the overall utilization
rate whereas others would reduce it, so that, to a large
extent, they cancelled out each other.
The model of radiotherapy utilization developed
in this project has many benets.
1. It provides a benchmark for planning radiotherapy
services on a population basis.The results from this
study can be useful in the planning of appropriate
radiotherapy services for a given population using
the following calculations.
For every 1000 cancer cases in a population, 523
patients would need radiation as an optimal part of
their management based upon the results of this
project (calculated optimal radiotherapy utilization
rate of 52.3%). A further 120 patients, of the above 523
patients, will require retreatment (based upon an ac-
tual retreatment rate of 23%).
40
This means that an
estimated 643 courses of treatment will be required for
every 1000 cancer patients diagnosed with a registered
cancer. These calculations are summarized in Table 5.
This will allow population-based estimates for the
number of possible treatment courses (and, therefore,
the amount of resources) that should be provided for
any particular area. This study was performed for the
Australian government and was viewed as a study that
would provide an evidence-based planning target.
Radiotherapy Utilization in Cancer/Delaney et al. 1133
2. Modeling the effect that changes to a particular
cancer incidence or changes in stage distribution
have on the overall recommended radiotherapy
utilization rate is another benet.
It is possible to easily modify the model should
there be changes in the relative incidence of certain
cancers, a change in the stage distribution, or a
change in treatment recommendations. The model
can also be used to estimate the optimal radiotherapy
utilization rate for other countries that may have dif-
TABLE 4
Comparison of Optimal with Actual Radiotherapy Utilization Rates
Cancer site
% Optimal
radiotherapy
utilization rate
Actual radiotherapy utilization rates
% Sweden
National
2001
31
% USA
% UK
(NYCRIS)
1999
34
% Australia
SEER 1995
2000
32
ACS
a
2001
33
National
1995
35
2000
36
NSW
2000
5
VIC
2000
37
1993
38
SA
a
1990
1994
39
Breast cancer 83 81 42 44 54 41 71 24 40
Lung cancer 76 71 39 36 - - 49 44 38
Melanoma 23 23 2 1 - - 13 - 2
Prostate 60 51 27 41 16 - - - 44
Kidney 27 63 8 4 9 - - - 11
Urinary bladder 58 17 4 3 26 - - - 26
Testis 49 48 40 - NR - - - 43
Esophagus 80 73 54 - 31 - - - 47
Stomach 68 7 15 - 4 - - - 6
Pancreas 57 6 16 - 4 - - - 4
Liver 0 - 3 - 3 - - - 3
Gall bladder 13 9 14 - 9 - - - 5
Colon 14 6 2 1 2 3 - - 3
Rectum 61 56 40 41 33 38 - - 17
Oral cavity 74 94
b
NR - - - - - 44
c
Lip 20 22 8 - - - - - 2
Larynx 100 100 75 - - - - - 80
Oropharynx 100 100 70 - - - - - -
Salivary gland 87 60 55 - - - - - -
Hypopharynx 100 39 74 - - - - - -
Paranasal sinuses 100 100 NR - - - - - -
Nasopharynx 100 100 84 - - - - - -
Unknown primary
(head & neck)
90 NR - - - - - - -
Uterus 46 64 22 25 - - - - 26
Cervix 58 83 44 33 - - - - 41
Central nervous
system
92 37 59 - - - - - 52
Lymphoma 65 40 - - - - - - 24
Leukemia 4 8 - - - - - - 6
Myeloma 38 82 - - - - - - 34
All cancers 52 43 24 - - - - - 25
NR: Not reported; ACS: American College of Surgeons; SEER: Surveillance, Epidemiology and End Results database (National Cancer Institute); NYCRIS: Northern and Yorkshire Cancer Registry and Information
Service; NSW: the state of New South Wales; VIC: the state of Victoria; SA: the state of South Australia.
a
First treatment only.
b
Includes brachytherapy.
c
Includes salivary glands.
TABLE 5
Estimated Optimal Number of Courses of Treatment per 1000
Registered Cancers
Percentage
Total
no.
New registered cancers N/A 1000
Patients requiring radiation 52.3 523
Retreatments 23 120
Total number of courses of radiotherapy required 643
1134 CANCER September 15, 2005 / Volume 104 / Number 6
fering cancer-specic proportions. For example, if an-
other country with a very different cancer incidence
prole were to use the model, then the only require-
ment to recalculate the optimal radiotherapy utiliza-
tion rate would be to alter the incidence of each of the
cancers in the tree and recalculate. Similarly, a change
in stage distribution of cancer due to development of
superior staging investigations (such as positron emis-
sion tomography in nonsmall cell lung cancer), or
following the introduction of a screening program
could easily be incorporated into the model.
3. This model provides a benchmark for service deliv-
ery.
The radiotherapy utilization trees that have been
developed for each of the tumor sites are a diagram-
matic representation of optimal evidence-based can-
cer care from a radiotherapy perspective. Epidemio-
logic data from patterns of care studies will allow
comparisons to be made between the actual rates of
radiotherapy delivery and the evidence-based ideal
rate. Analysis of the distributions of tumor stage, his-
tology, age, performance status, and other factors will
better dene any discrepancy between the actual and
ideal utilization rates.
Table 4 compares optimal radiotherapy utilization
rates with available rates of actual radiotherapy utili-
zation obtained from population-based data. The ta-
ble highlights the paucity of the data on actual radio-
therapy utilization, the high variability of the actual
radiotherapy rates across different regions, and the
general shortfall in radiotherapy use for most major
tumor sites including the common tumor sites that
have well known evidence-based treatment guidelines
(e.g., breast cancer). These data are not subdivided by
the various stages or other clinical attributes that
would make a direct comparison between the optimal
trees and the actual practice, although future studies
may be designed to identify subgroups of patients so
that, when shortfalls in radiotherapy are identied,
specic details as to types of patients where the short-
falls are greatest may help direct quality improvement
programs to the areas of most gain.
4. This model can determine optimal rates and re-
sources for other treatment modalities.
The methodology used here could be readily
adapted to consider other treatments (such as surgery,
chemotherapy, or palliative care) for cancer. It could
also be used to plan other services if criteria for se-
lecting appropriate patients were known for that par-
ticular service. For instance, if we knew the factors
that predict the need for palliative care referral, or
cancer genetics services, then resource planning could
be assisted by calculating the optimal utilization rate
in a similar fashion to that described here for radio-
therapy.
5. This model may be used to predict future radio-
therapy workload.
The radiotherapy utilization tree predicts whether
patients should receive any radiotherapy but does not
assess whether the treatment intent would be pallia-
tive or radical, and the tree predicts neither the num-
ber of fractions of treatment required nor the com-
plexity of the patients care. Various models of
complexity have been reported in the literature that
may be used in future studies so that even more ac-
curate predictions of radiotherapy workload could be
determined by calculating the actual number of treat-
ment fractions that may be expected for a given pop-
ulation.
Some Limitations of the Study Were Identied
Quality of data
The current study has identied areas where good
quality epidemiologic data (based on stage, perfor-
mance status, etc.) were lacking. We have overcome
the problem by performing modeling and sensitivity
analyses to indicate the relatively minor effect that any
of these uncertainties could have on overall utilization
rate.
1217,1922
Skin cancer and benign diseases provide workload for
radiation oncology departments but are not included as
registered cancers and, therefore, have not been factored
into the model
Notiable cancers are cancers for which statutory re-
quirements exist to notify a state cancer registry. Stat-
utory notication in Australia excludes nonmelano-
matous skin cancers and benign tumors but includes
ductal carcinoma in situ of the breast. A limitation of
the study is that there are other uses for radiotherapy
that are not included in this estimate and that will
need consideration when planning radiotherapy re-
sources. Radiotherapy has an established role in man-
agement of nonmalignant conditions (benign tumors
and noncancerous conditions) as well as a role in the
management of nonregistered cancers such as non-
melanomatous skin cancers. The overall need for ra-
diotherapy resources is difcult to estimate for these
nonregistered conditions, as the overall incidence of
these conditions is unknown, and evidence-based
treatment guidelines do not exist for most of these
conditions. Data obtained from selected hospitals in
Australia show that around 11% of patients who re-
ceive external beam radiotherapy are treated for non-
Radiotherapy Utilization in Cancer/Delaney et al. 1135
notiable conditions.
41
It remains important to con-
sider this additional workload in resource planning.
Other forms of radiotherapy have not been considered
Inclusion of other forms of radiotherapy such as
brachytherapy (interstitial and intracavitary) and/or
with radioactive isotopes (iodine, yttrium, samarium,
strontium, etc.) are beyond the scope of this article.
However, these other forms of radiotherapy should be
considered when planning radiotherapy resources
and could be the subject of further study.
Controversies in the recommended use of radiotherapy
Despite using treatment guidelines to determine indi-
cations for radiotherapy, there are many areas where
the role of radiotherapy remains poorly dened or
where the indications for the use of radiotherapy re-
main vague. This is mainly due to poor evidence and
the lack of good quality trials. We have identied some
areas where future research would be useful. The
model is easily amended should new evidence for or
against the use of radiotherapy for a specic clinical
situation emerge.
The effect of patient choice considerations
We did not consider the effect of patient choice be-
cause of the risk that the studies reporting patient
preference might have been confounded by availabil-
ity of radiotherapy to the study population. Little or no
data are presented in these studies to judge whether
access to resources was factored into the decision for
or against radiotherapy when alternative treatment
options were available.
Rare indications for radiotherapy have not been included
in the overall estimate
In many cancers there will be a small proportion of
patients who may appropriately receive radiotherapy
for rare indications, usually for metastases such as
symptomatic lung, soft tissue, or subcutaneous metas-
tases. They were not included because incidence data
were not available and the proportions of patients
with symptoms that required radiotherapy could not
be estimated. Although only of small overall impact in
their own right, the cumulative total of these indica-
tions could increase the overall radiotherapy utiliza-
tion estimate by 12% at the most.
Conclusions
The overall estimate for radiotherapy utilization is
52.3% based upon the best available evidence. Al-
though the scope of this study is conned to exploring
the optimal utilization of external beam megavoltage
radiotherapy for notiable cancers, the overall esti-
mate provides a useful tool for assisting in planning
adequate radiotherapy resources. Population-based
data from the United States, the United Kingdom,
Sweden, and Australia suggest that there is a signi-
cant shortfall between the optimal rate and the pro-
portion of patients currently treated with radiotherapy
that warrants further research and action.
REFERENCES
1. National Health and Medical Research Council. Beam and
isotope radiotherapyA report of the Australian Health
Technology Advisory Committee. Publication no. 2036. Can-
berra: Commonwealth Department of Health and Family
Services, 1996.
2. Statewide Services Development Branch. Radiotherapy
management information system. State health publication
no.(SSDB) 980139. Sydney: NSW Health Department, 1997.
3. Statewide Services Development Branch. Radiotherapy
management information system. State health publication
no. (SSDB) 970069. Sydney: NSW Health Department, 1996.
4. Statewide Services Development Branch. Radiotherapy
management information system. State health publication
no. (SSDB) 980139. Sydney: NSW Health Department, 1998.
5. Statewide Services Development Branch. NSW radiotherapy
management information system report 2000. Sydney: NSW
Health Department, 2001.
6. Tyldesley S, Boyd C, Shulze K, Walker H, Mackillop WJ.
Estimating the need for radiotherapy for lung cancer: an
evidence-based, epidemiologic approach. Int J Radiat Oncol
Biol Phys. 2001;49:973985.
7. Mackillop WJ, Dixon P, Zhou Y, et al. Variations in the
management and outcome of non-small cell lung cancer in
Ontario. Radiother Oncol. 1994;32:105115.
8. Mackillop WJ, Groome PA, Zhang-Solomons J, et al. Does a
centralized radiotherapy system provide adequate access in
care? J Clin Oncol. 1997;15:12611271.
9. Lote K, Moller T, Nordman E, et al. Resources and produc-
tivity in radiation oncology in Denmark, Finland, Iceland,
Norway and Sweden during 1987. Acta Oncol. 1991;30:555
561.
10. Denham JW. How do we bring an acceptable level of radio-
therapy services to a dispersed population? Australas Radiol.
1995;39:171173.
11. Barton MB. Radiotherapy utilisation in New South Wales
from 1996 to 1998. Australas Radiol. 2000;44:483484.
12. Delaney G, Barton B, Jacob S. Estimation of an optimal
radiotherapy utilization rate for breast carcinoma: a review
of the evidence. Cancer. 2003;98:19771986.
13. Delaney G, Barton M, Jacob S, Jalaludin B. A model for
decision making for the use of radiotherapy in lung cancer.
Lancet Oncol. 2003;4:120128.
14. Delaney G, Barton M, Jacob S. Estimation of an optimal
radiotherapy utilization rate for melanoma. A review of the
evidence. Cancer. 2004;100:12931301.
15. Delaney G, Barton M, Jacob S. Estimation of an optimal
radiotherapy utilization rate for gastrointestinal cancer: A
review of the evidence. Cancer. 2004;101:657670.
16. Delaney G, Jacob S, Barton M. Estimating the optimal ex-
ternal beam radiotherapy utilization rate for genitourinary
malignancies. Cancer. 2005;103:462473.
17. Delaney G, Jacob S, Barton M. Estimation of an optimal
external beam radiotherapy utilization rate for head and
neck carcinoma. Cancer. 2005;103:22162227.
1136 CANCER September 15, 2005 / Volume 104 / Number 6
18. Delaney G, Jacob S, Barton M. Estimation of an optimal
radiotherapy utilization rate for gynecologic cancer: part
I-malignancies of the cervix, ovary, vagina, and vulva. Can-
cer. 2004;101:671681.
19. Delaney G, Jacob S, Barton M. Estimation of an optimal
radiotherapy utilization rate for gynecologic cancer: part
II-carcinoma of the endometrium. Cancer. 2004;101:682
692.
20. Featherstone C, Delaney G, Jacob S, Barton M. Estimating
the optimal utilization rates of radiotherapy for hematologic
malignancies from a review of the evidence: part I-lym-
phoma. Cancer. 2005;103:383392.
21. Featherstone C, Delaney G, Jacob S, Barton M. Estimating
the optimal utilization rates of radiotherapy for hematologic
malignancies from a review of the evidence: part II-leuke-
mia and myeloma. Cancer. 2005;103:393401.
22. Delaney G, Jacob S, Barton M. Estimating the optimal ra-
diotherapy utilization for cancer of the central nervous sys-
tem, thyroid cancer, and cancer of unknown primary origin
from evidence-based clinical guidelines. Cancer. in press.
23. National Health and Medical Research Council. Guide to the
development, implementation and evaluation of clinical
practice guidelines. Appendix B, 56. Canberra: National
Health and Medical Research Council, 1998.
24. Foroudi F, Tyldesley S, Walker H, Mackillop WJ. An evi-
dence-based estimate of appropriate radiotherapy utiliza-
tion rate for breast cancer. Int J Radiat Oncol Biol Phys.
2002;53:12401253.
25. Foroudi F, Tyldesley S, Barbera L, Huang J, Mackillop WJ. An
evidence-based estimate of the appropriate radiotherapy
utilization rate for colorectal cancer. Int J Radiat Oncol Biol
Phys. 2003;56:12951307.
26. Foroudi F, Tyldesley S, Barbera L, Huang J, Mackillop WJ.
Evidence-based estimate of appropriate radiotherapy utili-
zation rate for prostate cancer. Int J Radiat Oncol Biol Phys.
2003;55:5163.
27. Australian Institute of Health and Welfare (AIHW) and Aus-
tralasian Association of Cancer Registries (AACR). Cancer in
Australia 1998. CAN 12. 2001. Cancer Series No 17. Can-
berra: AIHW and AACR, 2001.
28. National Comprehensive Cancer Network. National practice
guidelines in oncology-breast cancer. Version 2. Available
from URL: www.nccn.org. 2002. [Accessed February 21,
2003].
29. National Cancer Institute. PDQ cancer information summa-
ries: Treatment of breast cancer. Available from URL:
www.nci.nih.gov. 2003. [Accessed February21, 2003].
30. NHMRC National Breast Cancer Centre. Clinical practice
guidelines for the management of advanced breast cancer.
National Health and Medical Research Council. Kings Cross:
NHMRC National Breast Cancer Centre, 2001.
31. Moller TR, Brorsson B, Ceberg J, et al. A prospective survey
of radiotherapy practice 2001 in Sweden. Acta Oncol. 2003;
42:387410.
32. National Cancer Institute (Cancer Statistics Branch). SEER
Stat 5.0. Surveillance, Epidemiology and End Results cancer
incidence public-use database, 19732000. Bethesda: US
Department of Health and Human Services, 2002.
33. American College of Surgeons. National Cancer Database.
Available from URL: http://www.facs.org.dept/cancer/
ncdb/whatsncdb.html [accessed on November 25, 2003].
34. Northern and Yorkshire Cancer Registry and Information
Service (NYCRIS). Northern and Yorkshire Cancer Networks.
A report on incidence and management for the main sites of
cancer 1999. Available from URL: http://www.nycris.
org.uk/. 2002. [Accessed on November 25, 2003].
35. Hill D, Jamrozik K, White V, Collins J, et al. Surgical Man-
agement of Breast Cancer in Australia in 1995. Kings Cross,
NHMRC National Breast Cancer Centre, 1999.
36. Clinical Governance Unit. The National Colorectal Cancer
Care Survey. Australian clinical practice in 2000. Melbourne:
National Cancer Control Initiative, 2002.
37. Hill DJ, White VM, Giles GG, Collins JP, Kitchen PR. Changes
in the investigation and management of primary operable
breast cancer in Victoria. Med J Aust. 1994;161:110118.
38. Richardson GE, Thurseld VJ, Giles GG. Reported manage-
ment of lung cancer in Victoria in 1993: comparison with
best practice. MJA. 2000;172:321324.
39. Luke C, Chapman P, Priest K, Roder D. Use of radiotherapy
in the primary treatment of cancer in South Australia. Aus-
tralas Radiol. 2003;47:161167.
40. Statewide Services Development Branch. Radiotherapy
management information system report 2003. Sydney: NSW
Health Department, 2004.
41. Barton M, Frommer M, Olver I, Cox C, Crowe P, et al. A
cancer services framework for Victoria and future directions
for the Peter MacCallum Cancer Institute. Available from
URL: http://www.health.vic.gov.au/cancer/docs/vcsnalre-
port.pdf. 2003. [Accessed January 10, 2005].
Radiotherapy Utilization in Cancer/Delaney et al. 1137
Das könnte Ihnen auch gefallen
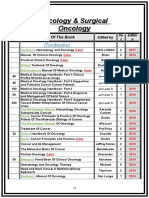
- Guideline Fracionamentos Alternativos - UKDokument84 SeitenGuideline Fracionamentos Alternativos - UKMarco Antonio SantanaNoch keine Bewertungen
- The American Cancer Society's Principles of Oncology: Prevention to SurvivorshipVon EverandThe American Cancer Society's Principles of Oncology: Prevention to SurvivorshipThe American Cancer SocietyNoch keine Bewertungen
- 2012 - Handbook of Treatment Planning in Radiation Oncology OCRDokument127 Seiten2012 - Handbook of Treatment Planning in Radiation Oncology OCRRoxana MacarieNoch keine Bewertungen
- Brfo193 Radiotherapy Dose Fractionation Third-Edition PDFDokument137 SeitenBrfo193 Radiotherapy Dose Fractionation Third-Edition PDFMed MedNoch keine Bewertungen
- Part 2 Week 9 - Treatment PlanningDokument50 SeitenPart 2 Week 9 - Treatment PlanningdanNoch keine Bewertungen
- Icru 58Dokument45 SeitenIcru 58Zoran MirkovNoch keine Bewertungen
- The Lecture: "Tumours of The Mammary Gland."Dokument21 SeitenThe Lecture: "Tumours of The Mammary Gland."top theNoch keine Bewertungen
- Understanding BrachytherapyDokument28 SeitenUnderstanding Brachytherapyqwertu132Noch keine Bewertungen
- Mammography - Procedure, Test, Pain, Time, Types, Risk, Cancer, RateDokument4 SeitenMammography - Procedure, Test, Pain, Time, Types, Risk, Cancer, RateMassimo RiserboNoch keine Bewertungen
- Rtog 0813 Marina CousinsDokument22 SeitenRtog 0813 Marina Cousinsapi-426094285Noch keine Bewertungen
- Sources, Fields, Measurements, and Applications: Radiation Dosimetry, Vol. 3Von EverandSources, Fields, Measurements, and Applications: Radiation Dosimetry, Vol. 3Frank H. AttixNoch keine Bewertungen
- Diagnostic Reference Level in Lumbar Radiography in Abidjan, Côte D'ivoireDokument5 SeitenDiagnostic Reference Level in Lumbar Radiography in Abidjan, Côte D'ivoiretheijesNoch keine Bewertungen
- 18-Oncology & Radiation OncologyDokument3 Seiten18-Oncology & Radiation OncologyIbrahimFikryNoch keine Bewertungen
- Review of Electron Beam Therapy PhysicsDokument36 SeitenReview of Electron Beam Therapy PhysicsMaría José Sánchez LovellNoch keine Bewertungen
- Physics of Radiation - Lec1Dokument10 SeitenPhysics of Radiation - Lec1شبكة المستقبلNoch keine Bewertungen
- Treatment Planning Heterogeneity Vs Homogeneity Lung ProjectDokument13 SeitenTreatment Planning Heterogeneity Vs Homogeneity Lung Projectapi-299138743Noch keine Bewertungen
- London Cancer Breast Radiotherapy Guidelines 2017 Version 4Dokument17 SeitenLondon Cancer Breast Radiotherapy Guidelines 2017 Version 4Novi WiarniNoch keine Bewertungen
- Innovative Radiotherapy Techniques for Prostate CancerVon EverandInnovative Radiotherapy Techniques for Prostate CancerNoch keine Bewertungen
- Three-Dimensional Conformal Radiation Therapy (3DCRT) For Prostate CancerDokument34 SeitenThree-Dimensional Conformal Radiation Therapy (3DCRT) For Prostate CancerMuhammad Safwan Ahmad FadzilNoch keine Bewertungen
- QUANTEC RT ConstraintsDokument41 SeitenQUANTEC RT ConstraintsNika Topuria100% (2)
- NRG Protocol Radiation Therapy Template - GYN - Endometrial Cancer - FinalDokument12 SeitenNRG Protocol Radiation Therapy Template - GYN - Endometrial Cancer - FinalarifpharmjuNoch keine Bewertungen
- Image Guided Radiotherapy Technique - IGRTDokument13 SeitenImage Guided Radiotherapy Technique - IGRTbadusha vpNoch keine Bewertungen
- Plan Evaluation in External Beam Radiotherapy: BY Sidhartha Dev Pattanaik Resident Medical Physicist HBCH/MPMMCC, VaranasiDokument56 SeitenPlan Evaluation in External Beam Radiotherapy: BY Sidhartha Dev Pattanaik Resident Medical Physicist HBCH/MPMMCC, VaranasiSidhartha DevNoch keine Bewertungen
- New Advanced in RadiotherapyDokument49 SeitenNew Advanced in RadiotherapyIndonesian Journal of CancerNoch keine Bewertungen
- Curriculum Physics RadiologyDokument156 SeitenCurriculum Physics Radiologydrzalie70Noch keine Bewertungen
- Haris Linear AcceleratorDokument66 SeitenHaris Linear AcceleratorHarisrahmanNoch keine Bewertungen
- Linear Quadratic (LQ) Model & Biological Based Treatment Planning - Dr. Manoj GuptaDokument60 SeitenLinear Quadratic (LQ) Model & Biological Based Treatment Planning - Dr. Manoj GuptaSudhan Rajan100% (3)
- Oncology NotesDokument5 SeitenOncology NotesLucky GomezNoch keine Bewertungen
- Prostate Radiotherapy - Current Standards and Future DirectionsDokument40 SeitenProstate Radiotherapy - Current Standards and Future Directionsvikram_bansal84Noch keine Bewertungen
- Radiation Therapy Case Study 2Dokument11 SeitenRadiation Therapy Case Study 2api-278170649Noch keine Bewertungen
- Gastrointestinal and Hepatobiliary Radiology ResourcesDokument3 SeitenGastrointestinal and Hepatobiliary Radiology Resourcesarsalanraza1978Noch keine Bewertungen
- Iaea TRS 430Dokument302 SeitenIaea TRS 430Alvaro Hermosilla ManríquezNoch keine Bewertungen
- MammogramDokument92 SeitenMammogramVasu Reddy ChallaNoch keine Bewertungen
- Clinical PET/MRIVon EverandClinical PET/MRIOnofrio Antonio CatalanoNoch keine Bewertungen
- IMRT Basics: R. Alfredo C. Siochi, Ph.D. Juan Carlos Celi, PH.DDokument3 SeitenIMRT Basics: R. Alfredo C. Siochi, Ph.D. Juan Carlos Celi, PH.DSantanu SamantaNoch keine Bewertungen
- Intraoperative RadiotherapyDokument42 SeitenIntraoperative RadiotherapyDr Sasikumar SambasivamNoch keine Bewertungen
- 103manual QAP Radiologi Pindaan Januari 2019Dokument115 Seiten103manual QAP Radiologi Pindaan Januari 2019UMGC Sri RampaiNoch keine Bewertungen
- The Timely Delivery of Radical Radiotherapy: Guidelines For The Management of Unscheduled Treatment InterruptionsDokument39 SeitenThe Timely Delivery of Radical Radiotherapy: Guidelines For The Management of Unscheduled Treatment InterruptionsshreyaNoch keine Bewertungen
- Icru 89Dokument274 SeitenIcru 89Jose Miguel Oyarzun SilvaNoch keine Bewertungen
- Radiod MasterDokument149 SeitenRadiod MasterAhmeid Eid0% (1)
- Radiotherapy SARP PDFDokument5 SeitenRadiotherapy SARP PDFskNoch keine Bewertungen
- Anatomy Imaging For Radiotherapy PDFDokument41 SeitenAnatomy Imaging For Radiotherapy PDFIkang FauziNoch keine Bewertungen
- Radiation Oncology: DR - Durgesh Mishra Dy - Cmo, MJPJAY, MahDokument13 SeitenRadiation Oncology: DR - Durgesh Mishra Dy - Cmo, MJPJAY, MahKASATSANoch keine Bewertungen
- ESUR Guidelines On Contrast MediaDokument10 SeitenESUR Guidelines On Contrast MediatsimitselisNoch keine Bewertungen
- 10 Intraoperative RadiotherapyDokument11 Seiten10 Intraoperative RadiotherapyDgek LondonNoch keine Bewertungen
- Intraoperative Irradiation Techniques and ResultsDokument533 SeitenIntraoperative Irradiation Techniques and ResultsTELLY GONZALO ROMERO BRIOSONoch keine Bewertungen
- ILRT Dr. Sarbani-1 PDFDokument48 SeitenILRT Dr. Sarbani-1 PDFdurgesh kumar100% (1)
- SBRT PDFDokument14 SeitenSBRT PDFrubenNoch keine Bewertungen
- Plan EvaluationDokument56 SeitenPlan EvaluationSidhartha DevNoch keine Bewertungen
- Application of Radiobiology in RTDokument61 SeitenApplication of Radiobiology in RTnilesh kumarNoch keine Bewertungen
- IMRT by Musaib MushtaqDokument44 SeitenIMRT by Musaib MushtaqDr. Musaib MushtaqNoch keine Bewertungen
- Hendees Radiation Therapy PhysicsDokument3 SeitenHendees Radiation Therapy PhysicsRajeev GuptaNoch keine Bewertungen
- Women's Imaging: MRI with Multimodality CorrelationVon EverandWomen's Imaging: MRI with Multimodality CorrelationMichele A. BrownBewertung: 5 von 5 Sternen5/5 (1)
- APBI Journal Club PowerPointDokument20 SeitenAPBI Journal Club PowerPointRegan Ward HimeNoch keine Bewertungen
- Notes On PET-CT - FinalDokument12 SeitenNotes On PET-CT - FinalAbhi SachdevNoch keine Bewertungen
- Csi Plan Writeup Portion Turn in PDFDokument13 SeitenCsi Plan Writeup Portion Turn in PDFapi-481226212Noch keine Bewertungen
- World Journal of Surgical Oncology: Abnormal HCG Levels in A Patient With Treated Stage I Seminoma: A Diagnostic DilemmaDokument3 SeitenWorld Journal of Surgical Oncology: Abnormal HCG Levels in A Patient With Treated Stage I Seminoma: A Diagnostic DilemmaarakbaeNoch keine Bewertungen
- 90 6601867aDokument7 Seiten90 6601867aarakbaeNoch keine Bewertungen
- Macros Roimanager3dDokument2 SeitenMacros Roimanager3darakbaeNoch keine Bewertungen
- The Role of Radiotherapy in Cancer TreatmentDokument9 SeitenThe Role of Radiotherapy in Cancer TreatmentarakbaeNoch keine Bewertungen
- MiR-210 As A Marker of Chronic Hypoxia, But Not A Therapeutic Target in Prostate CancerDokument6 SeitenMiR-210 As A Marker of Chronic Hypoxia, But Not A Therapeutic Target in Prostate CancerarakbaeNoch keine Bewertungen
- Biosains Vol 14 No 2 Mei 2012-7Dokument7 SeitenBiosains Vol 14 No 2 Mei 2012-7arakbaeNoch keine Bewertungen
- Ablative Therapies of The BreastDokument23 SeitenAblative Therapies of The BreastarakbaeNoch keine Bewertungen
- Design, Implementation and Validation of A Motorized Wedge Filter For A Telecobalt Machine (Bhabhatron-II)Dokument7 SeitenDesign, Implementation and Validation of A Motorized Wedge Filter For A Telecobalt Machine (Bhabhatron-II)arakbaeNoch keine Bewertungen
- Monte Carlo Simulation of A Theratron Elite100 TelecobaltDokument10 SeitenMonte Carlo Simulation of A Theratron Elite100 TelecobaltarakbaeNoch keine Bewertungen
- 2012 Karshaniya YavaguDokument4 Seiten2012 Karshaniya YavaguRANJEET SAWANTNoch keine Bewertungen
- Учебный предметDokument2 SeitenУчебный предметorang shabdizNoch keine Bewertungen
- Procedure For Non Hazardous Waste ManagementDokument6 SeitenProcedure For Non Hazardous Waste ManagementPaddyNoch keine Bewertungen
- Earthing SystemsDokument6 SeitenEarthing SystemsRob PettitNoch keine Bewertungen
- CrumpleZonesSE (Edit)Dokument12 SeitenCrumpleZonesSE (Edit)Dah Unknown MarksmenNoch keine Bewertungen
- Bagi CHAPT 7 TUGAS INGGRIS W - YAHIEN PUTRIDokument4 SeitenBagi CHAPT 7 TUGAS INGGRIS W - YAHIEN PUTRIYahien PutriNoch keine Bewertungen
- FORM Module IpsDokument10 SeitenFORM Module IpsRizalNoch keine Bewertungen
- 30 Risk and InsuranceDokument4 Seiten30 Risk and InsuranceSiti Nur Ain RamliNoch keine Bewertungen
- Task 3: New - HTMLDokument12 SeitenTask 3: New - HTMLGONELA SAI LOKESH (RA2011028010100)Noch keine Bewertungen
- Livro Spectrochemical AnalysisDokument9 SeitenLivro Spectrochemical AnalysisRicardo PossebonNoch keine Bewertungen
- Refrigerant Unit Lab ReportDokument19 SeitenRefrigerant Unit Lab Reportakmal100% (2)
- Directorate of Technical Education, Maharashtra StateDokument47 SeitenDirectorate of Technical Education, Maharashtra StatePandurang GunjalNoch keine Bewertungen
- English Lesson Plan Form 4 (Literature: "The Living Photograph")Dokument2 SeitenEnglish Lesson Plan Form 4 (Literature: "The Living Photograph")Maisarah Mohamad100% (3)
- IAU Logbook Core 6weeksDokument7 SeitenIAU Logbook Core 6weeksbajariaaNoch keine Bewertungen
- Application of SPACE MatrixDokument11 SeitenApplication of SPACE Matrixdecker444975% (4)
- High School Department PAASCU Accredited Academic Year 2017 - 2018Dokument6 SeitenHigh School Department PAASCU Accredited Academic Year 2017 - 2018Kevin T. OnaroNoch keine Bewertungen
- Digital Control Engineering 2nd Edition Fadali Solutions Manual PDFDokument3 SeitenDigital Control Engineering 2nd Edition Fadali Solutions Manual PDFMohammed SalahNoch keine Bewertungen
- Lesson Plan - Sight Word ObservationDokument2 SeitenLesson Plan - Sight Word Observationapi-253277023Noch keine Bewertungen
- Simulation of 1,3-Butadiene Extractive Distillation Process Using N-Methyl-2-Pyrrolidone SolventDokument7 SeitenSimulation of 1,3-Butadiene Extractive Distillation Process Using N-Methyl-2-Pyrrolidone SolventAA0809Noch keine Bewertungen
- Statistics For Criminology and Criminal Justice (Jacinta M. Gau)Dokument559 SeitenStatistics For Criminology and Criminal Justice (Jacinta M. Gau)Mark Nelson Pano ParmaNoch keine Bewertungen
- How To Spend An Hour A Day in Prayer - Matthew 26:40-41Dokument1 SeiteHow To Spend An Hour A Day in Prayer - Matthew 26:40-41Steve GainesNoch keine Bewertungen
- Adel Lock ManualDokument1 SeiteAdel Lock Manual24245677843Noch keine Bewertungen
- Valuing Construction Variation by Using PWA, FIDIC, ICWMF and CEDA Fluctuation Formula MechanismDokument5 SeitenValuing Construction Variation by Using PWA, FIDIC, ICWMF and CEDA Fluctuation Formula MechanismAzman YahayaNoch keine Bewertungen
- 250 Conversation StartersDokument28 Seiten250 Conversation StartersmuleNoch keine Bewertungen
- Different Art TechniquesDokument39 SeitenDifferent Art TechniquesRommel LegaspiNoch keine Bewertungen
- Electrostatics Practice ProblemsDokument4 SeitenElectrostatics Practice ProblemsMohammed Aftab AhmedNoch keine Bewertungen
- Factsheet AMRT 2023 01Dokument4 SeitenFactsheet AMRT 2023 01arsyil1453Noch keine Bewertungen
- Unit 12 BriefDokument7 SeitenUnit 12 Briefapi-477397447Noch keine Bewertungen
- Bachelors of Engineering: Action Research Project - 1Dokument18 SeitenBachelors of Engineering: Action Research Project - 1manasi rathiNoch keine Bewertungen
- VectorCAST QA Factsheet ENDokument2 SeitenVectorCAST QA Factsheet ENChaos XiaNoch keine Bewertungen