Beruflich Dokumente
Kultur Dokumente
Tracheostomy PDF
Hochgeladen von
Veronica Gatica0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
262 Ansichten8 SeitenTracheostomy is done for airway obstruction, respiratory support, pulmonary hygiene, elimination of dead space, and treatment of obstructive sleep apnoea. A chest x-ray will alert the surgeon to tracheal deviation due to cervical and mediastinal tumours, or traction on the trachea due to fibrosis. If airway obstruction is as a consequence of laryngeal cancer, then one should
Originalbeschreibung:
Originaltitel
TRACHEOSTOMY.pdf
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenTracheostomy is done for airway obstruction, respiratory support, pulmonary hygiene, elimination of dead space, and treatment of obstructive sleep apnoea. A chest x-ray will alert the surgeon to tracheal deviation due to cervical and mediastinal tumours, or traction on the trachea due to fibrosis. If airway obstruction is as a consequence of laryngeal cancer, then one should
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
262 Ansichten8 SeitenTracheostomy PDF
Hochgeladen von
Veronica GaticaTracheostomy is done for airway obstruction, respiratory support, pulmonary hygiene, elimination of dead space, and treatment of obstructive sleep apnoea. A chest x-ray will alert the surgeon to tracheal deviation due to cervical and mediastinal tumours, or traction on the trachea due to fibrosis. If airway obstruction is as a consequence of laryngeal cancer, then one should
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 8
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD &
NECK OPERATIVE SURGERY
TRACHEOSTOMY Johan Fagan
Tracheostomy refers to the creation of a
communication between the trachea and
the overlying skin. This may be done either
by open or percutaneous technique. This
chapter will focus on the open surgical
technique in the adult patient.
I ndications
Tracheostomy is done for airway
obstruction, respiratory support (assisted
ventilation), pulmonary hygiene, elimina-
tion of dead space, and treatment of
obstructive sleep apnoea.
Preoperative evaluation
Level of obstruction: A standard
tracheostomy will not bypass obstruction
in the distal trachea or bronchial tree
Anatomy of the neck: The surgeon should
anticipate a difficult tracheostomy in
patients with short necks, thick necks, and
necks that cannot be extended due to e.g.
rheumatoid or osteoarthritis of the cervical
spine
Deviation of cervical trachea: A chest X-
ray will alert the surgeon to tracheal
deviation due to cervical and mediastinal
tumours, or traction on the trachea due to
fibrosis (Figure 1).
Figure 1: Tracheal deviation due to
tuberculosis
Coagulopathy: A coagulopathy should be
corrected prior to surgery. If not
completely corrected, then have
electrocoagulation available at surgery to
aid haemostasis
Cardiorespiratory status: Patients with
upper airway obstruction may have cor
pulmonale, or respiratory acidosis. Some
patients may be dependent on
physiological PEEP to maintain O
2
saturation, or an elevated pCO
2
to maintain
respiratory drive; relieving upper airway
obstruction with a tracheostomy may
paradoxically cause such patients to stop
breathing and become hypoxic.
Laryngeal cancer: If airway obstruction is
as a consequence of laryngeal cancer, then
one should attempt not to enter the tumour
during tracheostomy. This may require a
lower tracheostomy if tumour involves the
cervical trachea. It is prudent to send a
sample from the tracheal window for
histological examination as involvement
by tumour might be useful information for
the surgeon subsequently doing the
laryngectomy.
Tracheostomy procedure
A tracheostomy is best done in the
operating room with good lighting,
instrumentation, suction, and assistance.
Patients may cough on inserting the
tracheostomy tube; hence eye protection is
recommended to prevent transmission of
infections such as HIV and hepatitis.
Anaesthesia: Unless the patient can safely
be intubated or the patient be ventilated
with a mask, a tracheostomy should be
done under local anaesthesia. If there is
concern about the anaesthetists ability to
maintain an airway, then the surgeon
should be present during induction; the
2
skin, soft tissue and trachea (into the
lumen) should be infiltrated with local
anaesthesia with adrenaline before
induction; and a set of tracheostomy
instruments should be set out before
induction of anaesthesia so that an
emergency tracheostomy can be done if
required.
Positioning and draping: The patient is
placed in a supine position with neck
extended by a pillow or sandbag placed
under the shoulders in order to deliver the
trachea out of the thorax and to give the
surgeon adequate access to the cervical
trachea. Such extension may not be
possible in patients with neck injuries, or
rheumatoid and osteoarthritis of the
cervical spine. Some patients with
impending airway obstruction may not
tolerate a recumbent position; the
tracheotomy may then be done with the
patient in a sitting position with neck
extended. The skin of the anterior neck and
chest is sterilised and the neck draped. If
the tracheostomy is being done under local
anaesthesia, the face should not be
covered.
Surface landmarks: The tracheostomy is
created below the 1
st
tracheal ring, so as to
avoid subglottic stenosis as a result of
scarring. Therefore palpating to determine
the location of the cricoid cartilage is
important. When you run your fingers up
the midline of the neck starting inferiorly
at the sternal notch, you 1
st
encounter
prominence of the thyroid isthmus,
followed by the cricoid.
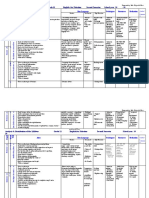
Minimum instruments: A minimum set of
instruments is demonstrated in Figure 2.
Figure 2: Minimum set of instruments
Skin incision: A horizontal incision is
made one fingerbreadth below the cricoid
prominence. This is cosmetically
preferable to a vertical midline incision.
The incision is carried through the skin and
the subcutaneous tissue. Note that the
platysma is generally absent in the midline.
Take care not to transect the anterior
jugular veins, which are just superficial to
the strap muscles within the investing
cervical fascia, and can be preserved and
retracted laterally (Figure 3). The
remainder of the dissection should remain
strictly in the midline in a vertical plane
to avoid injury to the inferior thyroid veins.
Figure 3: Exposure of anterior jugular
veins and cervical fascia
3
Infrahyoid strap muscles: Figure 4
illustrates the infrahyoid strap muscles.
Figure 4: Infrahyoid strap muscles
Identify the midline cervical fascial plane
between the sternohyoid muscles. Divide
this intermuscular plane by spreading with
a pair of scissors. Repeat this manoeuvre to
separate the sternothyroid muscles, and
retract the muscles laterally (Figure 5).
The trachea and cricoid can now be
palpated.
Figure 5: Retracting sternohyoid and
sternothyroid muscles to expose the
thyroid gland
Thyroid isthmus: The thyroid isthmus
overlies the 2
nd
/3
rd
tracheal rings. The
isthmus should be retracted superiorly to
expose the trachea (Figure 6). Only very
rarely does the thyroid isthmus need to be
doubly clamped, divided, and (suture)
ligated.
Figure 6: Thyroid retracted superiorly and
an inferiorly based flap cut (along red
lines) in anterior tracheal wall
Expose trachea: The infrathyroid trachea
is exposed anteriorly by carefully parting
overlying soft tissues with a pair of
scissors, taking care not to tear the inferior
thyroid veins. Ensure that the surgical field
is dry before proceeding, as it is difficult to
achieve haemostasis once the tracheostomy
tube has been inserted. Should there be
doubt about the location of the trachea, or
there be concern it being confused with the
carotid artery, aspirating air with a needle
attached to a syringe will confirm its
location.
Create tracheostoma: In the wake patient,
lignocaine may again be injected into
tracheal lumen prior to incising the trachea
and inserting the tube in order to reduce
coughing. Upward traction may be applied
to a tracheal hook inserted under a tracheal
ring to stabilise the trachea and deliver it
from the chest. The safest means to create
a tracheostomy in adults is by creating an
inferiorly based flap raised from the
anterior wall of the 3
rd
and 4
th
tracheal
rings. A silk traction suture is passed
through this anterior tracheal flap and
loosely secured to the skin (Figure 7).
Traction on the suture facilitates
reinsertion of the tracheostomy tube in
case of accidental decannulation.
Thyroid cartilage
Cricoid cartilage
Thyroid gland
Sternohyoid muscle
Sternothyroid muscle
4
Alternately one may remove an anterior
cartilage segment of the 2
nd
, 3
rd
or 4
th
tracheal rings.
Figure 7: Flap reflected inferiorly with
traction suture attached to flap
Insertion of tracheostomy tube: The
surgeon assesses the size of the trachea,
and selects the largest sized cuffed
tracheostomy tube that will comfortably fit
the tracheal lumen. Inject air into the
tracheostomy inflatable cuff to test the
integrity of the cuff. Insert the introducer
into the tracheostomy tube. If the patient
has been intubated, the anaesthetist is
asked to slowly withdraw the endotracheal
tube, so that the tracheostomy tube can be
inserted under direct vision. Advance the
tube into the trachea while applying
traction to the silk traction suture attached
to the tracheal flap. Ensure that the tube
has been inserted into the tracheal lumen,
and not a false passage in the paratracheal
soft tissues. Inflate the cuff, attach the
anaesthetic tubing, and hand-ventilate until
one has confirmed correct placement of the
tube within the trachea (Figure 8). Do not
suture the skin tightly around the
tracheostomy tube, as this can promote
surgical emphysema.
Securing the tracheostomy tube: Tapes are
threaded through the holes in the flanges of
the tracheostomy tube, passed around the
neck, and tied, with the neck flexed. If the
ties are placed with the neck extended,
they are too loose when the patient flexes
the neck.
Epiglottis
Glottis
Thyroid cartilage
Cricoid
Thyroid gland
Innominate artery
Sternum
Figure 8: Position of tracheostomy tube
The ties should be tight enough to admit no
more than a single finger under the tape
(Figure 9).
Figure 9: Tracheostomy tube secured with
Velcro tape
It is prudent to suture the tracheotomy tube
to the skin for the first few days to allow
maturation of the tracheocutaneous tract.
The sutures can then be removed and
traditional tracheotomy tapes can then be
used. Following free microvascular
transfer flap reconstruction, tracheostomy
tapes should be avoided; the tracheostomy
should preferably be sutured to the
suprastomal skin, as tracheal tapes may
cause jugular vein compression,
thrombosis, and venous outflow
obstruction and flap failure.
Back wall of trachea
Inferiorly based tracheal
flap
Traction suture
anchoring flap
5
Pitfalls
High tracheostomy: It is important not to
place the tracheotomy above the 2
nd
tracheal ring, as inflammation may cause
subglottic oedema, chondritis of the cricoid
cartilage, and subglottic stenosis.
Low tracheostomy: A tracheotomy should
not be placed below the 4
th
tracheal ring
as:
The distance between the skin and the
trachea increases inferiorly, which
makes tracheal intubation more
difficult
A low tracheostomy may compress and
erode the innominate artery which
passes between the manubrium sterni
and the trachea (Figure 8). This may
cause innominate artery erosion and
fatal haemorrhage. This may be
preceded by a so-called sentinel
bleed
Paratracheal false tract: Inadvertent
extratracheal placement of the
tracheostomy tube can be fatal. It is
recognised by the absence of breath sounds
on auscultation of the lungs, high
ventilatory pressures, failure to ventilate
the lungs, hypoxia, absence of expired
CO
2
, surgical emphysema, and an inability
to pass a suction catheter down the
bronchial tree, and on chest X-ray.
Surgical emphysema, pneumomediastinum,
and pneumothorax: Injury to the pleural
domes is more likely to occur in children,
struggling patients and patients on positive
pressure ventilation. It can be complicated
by a tension pneumothorax. Hence
auscultation of the chest and a CXR should
be performed after tracheostomy,
especially in ventilated patients. Surgical
emphysema may also be promoted by
suturing the tracheostomy wound around
the tracheostomy tube.
Airway fire: Do not enter the trachea with
diathermy, as this may cause an airway fire
in a patient being ventilated with a high
concentration of oxygen.
Choice of Tracheostomy Tube
A variety of tube designs and materials are
available. The choice of tube should
conform to the indication for which it is to
be used. All tubes should have an inner
cannula; this can safely be removed and
cleaned without a need to remove the outer
cannula and hence endanger the airway.
The following factors may influence the
choice of tube:
Tube diameter: Because airway resistance
is related to the 4
th
power of the radius
with laminar flow, and the 5
th
power of the
radius with turbulent flow, it is important
to select a tube that that fits the trachea
snugly. A range of sizes should be
available. It also underscores the
importance of keeping the tube clean, as
accumulation of mucus increases airway
resistance not only by reducing the
diameter, but also by causing turbulent air
flow.
Tracheal seal: A cuffed, plastic
tracheostomy tube is used to create a seal
with the trachea in patients on positive
pressure ventilation, and with fresh
tracheostomy wounds (Figure 10) to
prevent saliva or blood entering the lower
airways. The cuffed tube may be replaced
with an uncuffed tube, either plastic or
metal (Figure 11) in patients who do not
require positive pressure ventilation once
the tract between the skin and the trachea
has become well defined by granulation
tissue at 48hrs, and tracheostomal bleeding
has settled.
6
Figure 10: Plastic low pressure cuffed
tracheostomy tube with outer cannula,
inner cannula and introducer (L to R)
Figure 11: Metal tracheostomy tube with
outer cannula, inner cannula and
introducer (L to R)
Tube length: Patients with very thick necks
can be fitted with a tracheostomy tube with
a flange that can be adjusted up or down
the shaft of the tube (Figure 12). Tube
length may also need to be adjusted when
the carina is close to the tracheostoma or
with tracheal stenosis or tracheamalacia
distal to the tracheostoma that needs to
stented by the tube. Chest and neck X-rays
are of value to determine the required
length.
Tube shape: Laryngectomy patients
require shorter tubes with a gentler
curvature to conform to the stoma and the
trachea.
Figure 12: Tracheostomy tube with
adjustable flange
Neck Flange: The neck flange should
conform to the shape of the neck and fit
snugly against the skin to avoid excessive
tube movement, accidental decannulation,
and soft tissue trauma.
Tube material: Metal tubes are thinner
walled, and hence have a better ratio of
outer to inner wall diameter, thereby
optimising airway resistance.
Phonation: Patients with uncuffed tubes or
fenestrated tubes (Figure 13) can phonate
by occluding the end of the tracheostomy
tube with a finger which permits air to
bypass the tube and to pass through the
larynx.
Figure 13: Fenestrated tracheostomy tube
7
Speaking valves fitted to the ends of
tracheostomy tubes are one-way valves
that open on inspiration, but close on
expiration, thereby directing expired air
through the larynx and permit hands-free
speech (Figure14).
Figure 14: Speaking valve that fits onto the
end of a tracheostomy tube and permits
hands-free speech
Fenestrated tubes with speaking valves are
particularly well suited to patients with
obstructive sleep apnoea, as they can have
normal speech by day with the valve in
place, but uncap the tracheostomy tube at
night to ensure unobstructed breathing.
Postoperative care
Pulmonary oedema: This may occur
following sudden relief of airway
obstruction and reduction in high
intraluminal airway pressures. It may be
corrected by CPAP or positive pressure
ventilation.
Respiratory arrest: This may occur
immediately following insertion of the
tracheostomy tube, and is attributed to the
rapid reduction in arterial pCO
2
following
restoration of normal ventilation, and
hence loss of respiratory drive.
Humidification: Tracheostomy bypasses
the nose and upper aerodigestive tract
which normally warms, filters, and
humidifies inspired air. To avoid tracheal
desiccation and damage to the respiratory
cilia and epithelium, and obstruction due to
mucous crusting, the tracheostomy patient
needs to breathe humidified warm air by
means of a humidifier, heat and moisture
exchange filter, or a tracheostomy bib.
Pulmonary Toilette: The presence of a
tracheostomy tube and inspiration of dry
air irritates the mucosa and increases
secretions. Tracheostomy also promotes
aspiration of saliva and food as tethering of
the airway prevents elevation of the larynx
during swallowing. Patients are unable to
clear secretions as effectively as
tracheostomy prevents generation of
subglottic pressure, hence making
coughing and clearing secretions
ineffective; it also disturbs ciliary function.
Therefore secretions need to be suctioned
in an aseptic and atraumatic manner.
Cleaning the tube: Airway resistance is
related to the 4
th
power of the radius with
laminar flow, and the 5
th
power of the
radius with turbulent flow. Therefore even
a small reduction of airway diameter
and/or conversion to turbulent airflow as a
result of secretions in the tube can
significantly affect airway resistance.
Therefore regular cleaning of the inner
cannula is required using a pipe cleaner or
brush.
Securing the tube: Accidental decannula-
tion and failure to quickly reinsert the tube
may be fatal. This is especially
problematic during the 1
st
48hrs when the
tracheocutaneous tract has not matured and
attempted reinsertion of the tube may be
complicated by the tube entering a false
tract. Therefore the tightness of the
tracheostomy tapes should be regularly
checked. Traction sutures on the tracheal
flap facilitate reinsertion of the
tracheotomy tube.
Cuff pressures: When tracheostomy tube
cuff pressures against the tracheal wall
mucosa exceed 30cm H
2
0, mucosal
capillary perfusion ceases, ischaemic
damage ensues and tracheal stenosis may
result. Mucosal injury has been shown to
8
occur within 15 minutes. Therefore cuff
inflation pressures of >25cm H
2
0 should be
avoided. A number of studies have
demonstrated the inadequacy of manual
palpation of the pilot balloon as a means to
estimate appropriate cuff pressures.
Measures to prevent cuff related injury
include:
Only to inflate the cuff if required
(ventilated, aspiration)
Minimal Occluding Volume Technique:
Deflate the cuff, and then slowly
reinflate until one can no longer hear
air going past the cuff with a
stethoscope applied to the side of the
neck near the tracheostomy tube
(ventilated patient)
Minimal Leak Technique: The same
procedure as above, except that once
the airway is sealed, slowly to
withdraw approximately 1ml of air so
that a slight leak is heard at the end of
inspiration
Pressure gauge: Regular or continuous
monitoring of cuff pressures
Decannulation
The tracheostomy tube can be removed
once the cause of the airway obstruction
has been resolved. If any doubt exists
about the adequacy of the airway, e.g.
following pharyngeal or laryngeal surgery,
then the tracheostomy tube is first
downsized and plugged, so that the patient
can breathe freely past the tube. The tube
is then plugged. The patient should be
under close observation during this time,
and may be monitored with pulse
oximetry. If the patient can tolerate the
tracheostomy tube being plugged
overnight, it can then be removed. The
tracheostomy wound is covered with an
occlusive dressing, and generally heals
over a matter a week.
Author & Editor
Johan Fagan MBChB, FCORL, MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za
THE OPEN ACCESS ATLAS OF
OTOLARYNGOLOGY, HEAD &
NECK OPERATI VE SURGERY
www.entdev.uct.ac.za
The Open Access Atlas of Otolaryngology, Head &
Neck Operative Surgery by Johan Fagan (Editor)
johannes.fagan@uct.ac.za is licensed under a Creative
Commons Attribution - Non-Commercial 3.0 Unported
License
Das könnte Ihnen auch gefallen
- A Manual of the Operations of Surgery: For the Use of Senior Students, House Surgeons, and Junior PractitionersVon EverandA Manual of the Operations of Surgery: For the Use of Senior Students, House Surgeons, and Junior PractitionersNoch keine Bewertungen
- Anesthesia in Thoracic Surgery: Changes of ParadigmsVon EverandAnesthesia in Thoracic Surgery: Changes of ParadigmsManuel Granell GilNoch keine Bewertungen
- TracheostomyDokument8 SeitenTracheostomyShar CatedralNoch keine Bewertungen
- TracheostomyDokument63 SeitenTracheostomyAyesha FayyazNoch keine Bewertungen
- Tracheostomy: As. Univ. Dr. Andrei Cristian Bobocea As. Univ. Dr. Serban Radu MatacheDokument21 SeitenTracheostomy: As. Univ. Dr. Andrei Cristian Bobocea As. Univ. Dr. Serban Radu MatacheIoana VasileNoch keine Bewertungen
- TracheostomyDokument10 SeitenTracheostomyanitaabreu123Noch keine Bewertungen
- Tracheostomy 191224152833Dokument106 SeitenTracheostomy 191224152833Dimas SevantoNoch keine Bewertungen
- Chest Tube ThoracostomyDokument6 SeitenChest Tube ThoracostomyRhea Lyn LamosteNoch keine Bewertungen
- CricothyroidotomyDokument38 SeitenCricothyroidotomyAlsalman AnamNoch keine Bewertungen
- Chest Tube InsertionDokument4 SeitenChest Tube InsertionHugo ARNoch keine Bewertungen
- Tension PneumothoraxDokument3 SeitenTension PneumothoraxariefNoch keine Bewertungen
- Cricothyroidotomy and Needle CricothyrotomyDokument10 SeitenCricothyroidotomy and Needle CricothyrotomyunderwinefxNoch keine Bewertungen
- TracheostomyDokument27 SeitenTracheostomynahidanila439Noch keine Bewertungen
- Minor Surgical Procedures...Dokument10 SeitenMinor Surgical Procedures...Silinna May Lee SanicoNoch keine Bewertungen
- Total LaryngectomyDokument14 SeitenTotal LaryngectomyDr. T. BalasubramanianNoch keine Bewertungen
- Total LaryngectomyDokument15 SeitenTotal LaryngectomyKumaran Bagavathi RagavanNoch keine Bewertungen
- Tube Thoracostomy Chest Tube Implantation and Follow Up: Review ArticleDokument10 SeitenTube Thoracostomy Chest Tube Implantation and Follow Up: Review ArticleAnasthasia hutagalungNoch keine Bewertungen
- Total LaryngectomyDokument15 SeitenTotal LaryngectomyAdi SitaruNoch keine Bewertungen
- Tracheostomy: Presented By: Barte, Hannah Aida D. Balamurugan, RameebhaDokument21 SeitenTracheostomy: Presented By: Barte, Hannah Aida D. Balamurugan, RameebhaThakoon Tts100% (1)
- Tracheostomy Operating TechniqueDokument34 SeitenTracheostomy Operating TechniqueIsa BasukiNoch keine Bewertungen
- TracheostomyDokument4 SeitenTracheostomyNapieh Bulalaque PolisticoNoch keine Bewertungen
- Assignment On TreacheostomyDokument7 SeitenAssignment On Treacheostomysantosh kumarNoch keine Bewertungen
- TracheostomyDokument3 SeitenTracheostomyJon AsuncionNoch keine Bewertungen
- TracheotomyDokument19 SeitenTracheotomyKarina BundaNoch keine Bewertungen
- Filosso 2017Dokument11 SeitenFilosso 2017Allison DiêgoNoch keine Bewertungen
- Tracheostomy in Palliative CaraDokument9 SeitenTracheostomy in Palliative CarameritaNoch keine Bewertungen
- Annrcse01509 0sutureDokument3 SeitenAnnrcse01509 0sutureNichole Audrey SaavedraNoch keine Bewertungen
- Chest TubeDokument18 SeitenChest TubeAyu MasturaNoch keine Bewertungen
- TracheostomyDokument28 SeitenTracheostomyprivatejarjarbinksNoch keine Bewertungen
- Tracheal TraumaDokument3 SeitenTracheal TraumaWalid DarwicheNoch keine Bewertungen
- Pneumothorax GuidelineDokument8 SeitenPneumothorax GuidelineIonut - Eugen IonitaNoch keine Bewertungen
- Vertical Partial Laryngectomy An AtlasDokument14 SeitenVertical Partial Laryngectomy An AtlasDr. T. Balasubramanian100% (2)
- Anatomy of TracheostomyDokument4 SeitenAnatomy of TracheostomyShahabuddin ShaikhNoch keine Bewertungen
- MedSurg NotesDokument57 SeitenMedSurg NotesCHRISTOFER CORONADONoch keine Bewertungen
- Tracheostomy: Berlian Chevi A. 20184010030Dokument26 SeitenTracheostomy: Berlian Chevi A. 20184010030Berlian Chevi e'Xgepz ThrearsansNoch keine Bewertungen
- Chest Tube InsertionDokument3 SeitenChest Tube InsertionprofarmahNoch keine Bewertungen
- Tracheostomy: Continuing Education ActivityDokument9 SeitenTracheostomy: Continuing Education ActivityUlul IsmiNoch keine Bewertungen
- Chest Tube InsertionDokument2 SeitenChest Tube InsertionmusicaBGNoch keine Bewertungen
- Tracheostomy: Dr. Amar KumarDokument18 SeitenTracheostomy: Dr. Amar KumarSudhanshu ShekharNoch keine Bewertungen
- Thoracocentesis: Nadja E. SigristDokument4 SeitenThoracocentesis: Nadja E. SigristDwi AnaNoch keine Bewertungen
- Chest Tubes and ThoracentesisDokument18 SeitenChest Tubes and ThoracentesisecleptosNoch keine Bewertungen
- Schellenberg 2018Dokument13 SeitenSchellenberg 2018Juan Jesús Espinoza AmayaNoch keine Bewertungen
- ThoracentesisDokument10 SeitenThoracentesisGabriel Friedman100% (1)
- Chest Tube Placement (Adult)Dokument8 SeitenChest Tube Placement (Adult)Ariane Joyce SalibioNoch keine Bewertungen
- TracheostomyDokument58 SeitenTracheostomylissajanet1016100% (1)
- Percutaneous Tracheostomy: A Comprehensive Review.Dokument11 SeitenPercutaneous Tracheostomy: A Comprehensive Review.Hitomi-Noch keine Bewertungen
- Chest Drains Learning ResourceDokument22 SeitenChest Drains Learning ResourceSiriporn TalodkaewNoch keine Bewertungen
- Chapter 132 Total Penectomy. Hinman. 4th Ed. 2017Dokument3 SeitenChapter 132 Total Penectomy. Hinman. 4th Ed. 2017Urologi JuliNoch keine Bewertungen
- Howard B. Seim III, DVM, DACVS Colorado State University: WWW - VideovetorgDokument4 SeitenHoward B. Seim III, DVM, DACVS Colorado State University: WWW - VideovetorgIkhsan HidayatNoch keine Bewertungen
- Supraglottic LaryngectomyDokument5 SeitenSupraglottic LaryngectomyCarlesNoch keine Bewertungen
- ThoracentesisDokument12 SeitenThoracentesisAnusha Verghese0% (1)
- Amit Tracheostomy Presentation 12 Aug 2010Dokument59 SeitenAmit Tracheostomy Presentation 12 Aug 2010Amit KochetaNoch keine Bewertungen
- TracheostomyDokument35 SeitenTracheostomyAbdur Raqib100% (1)
- TracheostomyDokument6 SeitenTracheostomynamithaNoch keine Bewertungen
- Thoracic Incisions PDFDokument14 SeitenThoracic Incisions PDFalbimar239512Noch keine Bewertungen
- Assisting With Chest Tube InsertionDokument5 SeitenAssisting With Chest Tube InsertionLoveSheryNoch keine Bewertungen
- Anesthetic Implications of Zenker's Diverticulum: Somasundaram Thiagarajah, Erwin Lear, and Margaret KehDokument3 SeitenAnesthetic Implications of Zenker's Diverticulum: Somasundaram Thiagarajah, Erwin Lear, and Margaret KehMatthew JohnsonNoch keine Bewertungen
- Tracheostomy DR KVLN Rao PDFDokument33 SeitenTracheostomy DR KVLN Rao PDFVenkata Krishna Kanth ThippanaNoch keine Bewertungen
- Difficult Acute Cholecystitis: Treatment and Technical IssuesVon EverandDifficult Acute Cholecystitis: Treatment and Technical IssuesNoch keine Bewertungen
- Break The Cycle Activity GuidesDokument19 SeitenBreak The Cycle Activity GuidesJuanmiguel Ocampo Dion SchpNoch keine Bewertungen
- 3 5 18 950 PDFDokument3 Seiten3 5 18 950 PDFBang AthanNoch keine Bewertungen
- Registrars Manual On Band DDokument32 SeitenRegistrars Manual On Band DkailasasundaramNoch keine Bewertungen
- SR.# Weight (KG) Height (FT) Age (Yrz) Others RecommendationsDokument2 SeitenSR.# Weight (KG) Height (FT) Age (Yrz) Others RecommendationsshaniNoch keine Bewertungen
- Acuna - ENG 2089 AAEDokument2 SeitenAcuna - ENG 2089 AAERishi GolaniNoch keine Bewertungen
- Position PaperDokument2 SeitenPosition Paperiscream230% (1)
- Treatment and Prognosis of Febrile Seizures - UpToDateDokument14 SeitenTreatment and Prognosis of Febrile Seizures - UpToDateDinointernosNoch keine Bewertungen
- 5 Cover Letter Samples For Your Scientific ManuscriptDokument11 Seiten5 Cover Letter Samples For Your Scientific ManuscriptAlejandra J. Troncoso100% (2)
- YakultDokument15 SeitenYakultMlb T. De TorresNoch keine Bewertungen
- Gap AnalysisDokument9 SeitenGap Analysisapi-706947027Noch keine Bewertungen
- Power Development Through Complex Training For The.3Dokument14 SeitenPower Development Through Complex Training For The.3PabloAñonNoch keine Bewertungen
- Meditation ScriptDokument9 SeitenMeditation Scriptapi-361293242100% (1)
- Form2a 1Dokument2 SeitenForm2a 1ghi YoNoch keine Bewertungen
- Department of ICT Technology - DBMS Section: Level - IVDokument125 SeitenDepartment of ICT Technology - DBMS Section: Level - IVEsubalewNoch keine Bewertungen
- BLS Provider: Ma. Carmela C. VasquezDokument2 SeitenBLS Provider: Ma. Carmela C. VasquezPatricia VasquezNoch keine Bewertungen
- MSDS PDFDokument5 SeitenMSDS PDFdang2172014Noch keine Bewertungen
- Nzmail 18821014Dokument26 SeitenNzmail 18821014zeljkogrNoch keine Bewertungen
- Nutritional Interventions PDFDokument17 SeitenNutritional Interventions PDFLalit MittalNoch keine Bewertungen
- Analysis & Distribution of The Syllabus Grade 11 English For Palestine Second Semester School Year: 20 - 20Dokument3 SeitenAnalysis & Distribution of The Syllabus Grade 11 English For Palestine Second Semester School Year: 20 - 20Nur IbrahimNoch keine Bewertungen
- Nah Incarcerated HerniaDokument4 SeitenNah Incarcerated Herniafelix_the_meowNoch keine Bewertungen
- How To File A Claim-For GSISDokument2 SeitenHow To File A Claim-For GSISZainal Abidin AliNoch keine Bewertungen
- Tano Vs SocratesDokument3 SeitenTano Vs SocratesNimpa PichayNoch keine Bewertungen
- Golf Proposal 09Dokument7 SeitenGolf Proposal 09nrajentranNoch keine Bewertungen
- Viroguard Sanitizer SDS-WatermartDokument7 SeitenViroguard Sanitizer SDS-WatermartIshara VithanaNoch keine Bewertungen
- PARCO Project HSE Closing ReportDokument22 SeitenPARCO Project HSE Closing ReportHabib UllahNoch keine Bewertungen
- Clinical Practice Guidelines: High-Grade Glioma: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDokument9 SeitenClinical Practice Guidelines: High-Grade Glioma: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpSiva SubramaniamNoch keine Bewertungen
- 3M Disposable Filtering Facepiece Respirator Fitting Poster English and SpanishDokument2 Seiten3M Disposable Filtering Facepiece Respirator Fitting Poster English and SpanishTrunggana AbdulNoch keine Bewertungen
- Rdramirez Aota 2018 Poster For PortfolioDokument1 SeiteRdramirez Aota 2018 Poster For Portfolioapi-437843157Noch keine Bewertungen
- ProVari ManualDokument16 SeitenProVari ManualPatrickNoch keine Bewertungen
- The Ethics of Helping Transgender Men and Women Have ChildrenDokument16 SeitenThe Ethics of Helping Transgender Men and Women Have ChildrenAnonymous 75M6uB3OwNoch keine Bewertungen