Beruflich Dokumente
Kultur Dokumente
JPEN 14,38,8S A Tutorial On Enteral Access in Adult Patients in The Hospitalizeed Setting (NE)
Hochgeladen von
Jos Canales0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
33 Ansichten15 SeitenA tutorial On enteral access in Adult Patients in the hospitalized setting. Nutrition support remains a mainstay in the management of disease. The gastrointestinal tract is the preferred route of delivery.
Originalbeschreibung:
Originaltitel
JPEN 14,38,8S a Tutorial on Enteral Access in Adult Patients in the Hospitalizeed Setting (NE)
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenA tutorial On enteral access in Adult Patients in the hospitalized setting. Nutrition support remains a mainstay in the management of disease. The gastrointestinal tract is the preferred route of delivery.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
33 Ansichten15 SeitenJPEN 14,38,8S A Tutorial On Enteral Access in Adult Patients in The Hospitalizeed Setting (NE)
Hochgeladen von
Jos CanalesA tutorial On enteral access in Adult Patients in the hospitalized setting. Nutrition support remains a mainstay in the management of disease. The gastrointestinal tract is the preferred route of delivery.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 15
http://pen.sagepub.
com/
Nutrition
Journal of Parenteral and Enteral
http://pen.sagepub.com/content/38/3/282
The online version of this article can be found at:
DOI: 10.1177/0148607114522487
2014 38: 282 originally published online 5 February 2014 JPEN J Parenter Enteral Nutr
Keith R. Miller, Stephen A. McClave, Laszlo N. Kiraly, Robert G. Martindale and Matthew V. Benns
A Tutorial on Enteral Access in Adult Patients in the Hospitalized Setting
Published by:
http://www.sagepublications.com
On behalf of:
The American Society for Parenteral & Enteral Nutrition
can be found at: Journal of Parenteral and Enteral Nutrition Additional services and information for
http://pen.sagepub.com/cgi/alerts Email Alerts:
http://pen.sagepub.com/subscriptions Subscriptions:
http://www.sagepub.com/journalsReprints.nav Reprints:
http://www.sagepub.com/journalsPermissions.nav Permissions:
What is This?
- Feb 5, 2014 OnlineFirst Version of Record
- Mar 3, 2014 Version of Record >>
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
Journal of Parenteral and Enteral
Nutrition
Volume 38 Number 3
March 2014 282 295
2014 American Society
for Parenteral and Enteral Nutrition
DOI: 10.1177/0148607114522487
jpen.sagepub.com
hosted at
online.sagepub.com
Tutorial
Preface and Clinical Relevancy Statement
Nutrition support remains a mainstay in the management of
disease regardless of diagnosis and preexisting conditions.
Growing evidence has substantiated the role of nutrition sup-
port in improving patient outcomes and reducing duration of
hospitalization. When feasible, the gastrointestinal tract is the
preferred route of delivery and superior to the parenteral route
alone. As determined by nutrition assessment and evaluation,
many patients will prove unable to tolerate sufficient nutrition
support via the oral route. In these patients, alternative routes
of delivery should be considered prior to the initiation of par-
enteral support. A wide array of options are available to nutri-
tion support teams, and a comprehensive understanding of the
indications, contraindications, and complications inherent with
each access route provides clinicians with the information
needed to select the appropriate route in the individual patient.
Just as with any other treatment plan, an individualized
approach to the patient should be conducted prior to imple-
mentation. Careful nutrition assessment provides information
with regard to the likely duration of support.
Nutrition Support
Nutrition Assessment: Which Patients Should
Be Considered?
The typical medical/surgical ward and the intensive care unit
(ICU) often consist of heterogeneous populations, and it is
clear that these populations often have different needs. Multiple
nutrition screening tools are available to clinicians and include,
among others, the Nutritional Risk Screening (NRS)2002,
Mini Nutritional Assessment (MNA), Simplified Nutritional
Assessment Questionnaire (SNAQ), Subjective Global
Assessment (SGA), and Malnutrition Universal Screening
Tool.
1
Recent evidence suggests that combining nutrition
assessment with injury severity scores can help identify those
patients most likely to benefit from nutrition support.
2
Nutrition
risk stratification is an important principle that must be consid-
ered by all those involved in the care of the patient. Regardless
of the assessment tool that is used, the goal in all at-risk patients
is to initiate enteral support if possible in an early, safe, and
efficacious manner. As in all facets of patient care, continuous
reassessment and reevaluation are required in order for the cli-
nician to adapt the nutrition support plan to the changing con-
dition of the patient. During the assessment phase, a nutrition
support plan is generated and the patient is prepared for imple-
mentation through the establishment of appropriate enteral
access. Early enteral support should be the goal, and this prac-
tice has demonstrated improved patient outcomes in surgical,
critically ill, and trauma patients.
3-5
522487PENXXX10.1177/0148607114522487Journal of Parenteral and Enteral NutritionMiller et al
research-article2014
From the
1
University of Louisville, Louisville, Kentucky, and
2
Oregon
Health Sciences University, Portland, USA.
Financial disclosure: None declared.
Received for publication October 24, 2013; accepted for publication
January 13, 2014.
This article originally appeared online on February 5, 2014.
Corresponding Author:
Keith R. Miller, MD, Department of Surgery, University of Louisville,
ACB 2nd Floor, 550 South Jackson St, Louisville, KY 40202, USA.
Email: Krmill10@gwise.louisville.edu
A Tutorial on Enteral Access in Adult
Patients in the Hospitalized Setting
Keith R. Miller, MD
1
; Stephen A. McClave, MD
1
; Laszlo N. Kiraly, MD
2
;
Robert G. Martindale, MD
2
; and Matthew V. Benns, MD
1
Abstract
Enteral access is a cornerstone in the provision of nutrition support. Early and adequate enteral support has consistently demonstrated
improved patient outcomes throughout a wide range of illness. In patients unable to tolerate oral intake, multiple options of delivery are
available to the clinician. Access requires a multidisciplinary effort that involves nurses, dietitians, and physicians to be successful. These
techniques and procedures are not without morbidity and even mortality. A comprehensive understanding of the appropriate management
of these tubes and their inherent complications should be garnered by all those involved with nutrition support teams. This tutorial reviews
available options for enteral access in addition to commonly encountered complications and their management. (JPEN J Parenter Enteral
Nutr. 2014;38:282-295)
Keywords
enteral access; nutrition; nutrition support teams; nutrition support practice; adult; life cycle
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
Miller et al 283
Initial Approach: Nasoenteric Access
Options
Nasogastric access. The decision to attempt oral feeding or
transition directly to tube feedings is empiric and based on
clinical judgment with little guidance from the literature. Reas-
sessment and reevaluation are necessary as the clinical course
progresses and may result in a deviation from the original plan.
Adequate access can be achieved in most patients with mini-
mal intervention, with fewer patients requiring more complex
approaches (Figure 1). Depending on the inpatient setting,
there is a small subset of patients who will already have access
in place. This is clearly the minority, but these patients should
be recognized by the clinician early to avoid unnecessary inter-
ventions. Multiple access options are available for patients
determined to be at risk, who are unable to tolerate an early
progression to oral intake, and who do not have prior enteral
access in place.
An early opportunity for initiation of nutrition support is
afforded by using the hard plastic large-bore nasogastric tubes
usually placed for gastric decompression. This tube can pro-
vide decompression during the resuscitation and investigative
phases of the patients presentation and then allow for early
initiation of support as the patient stabilizes. Orogastric tubes
are limited by patient discomfort but can be used for short-term
access and are better tolerated in intubated and sedated patients.
Once determined to be appropriate candidates for the initiation
of enteral support, the naso- or orogastric tube provides tempo-
rary conduits for delivery that can be used immediately follow-
ing confirmation of appropriate placement.
Anecdotally, as the patient condition progresses, clinicians
are better able to predict the duration that enteral access will be
required (although these predictions remain empiric and
largely based on clinical judgment). Large-bore nasogastric
tubes should be replaced with smaller diameter and more pli-
able nasoenteric access within 57 days to potentially reduce
morbidity and improve patient discomfort. Nasoenteric feed-
ing tubes are commonly composed of silicone or polyurethane
and generally range from 812 French in size compared with
standard large-bore sump nasogastric tubes, which are 1418
French.
Pliable nasoenteric tubes can be placed with endoscopic
assistance or placed blindly with assistance of either promo-
tility agents or various signaling devices. As a rule, all tubes
should be confirmed to be in the appropriate location prior to
the initiation of enteral support. Confirmation is usually pro-
vided through imaging, which can add significant cost and
time to tube placement. Recent adjuncts have been developed,
including the use of carbon dioxide or pH sensors to confirm
intubation of the stomach rather than the pulmonary tree.
Sensitivity and specificity have been reported in 1 trial as high
as 86% and 99%, respectively.
6
Magnet devices to direct place-
ment have also been used with high success rates, reported
with regard to ensuring the tube is below the level of the dia-
phragm.
7
These options provide the clinician with multiple
options in confirming tube location prior to the initiation of
enteral feeding.
Postpyloric access. Patients intolerant of gastric feeding will
often tolerate feeding more distally in the gastrointestinal (GI)
tract. Self-propelling tubes that are placed blindly are designed
to assist in this endeavor. The design of these tubes includes
weights that theoretically facilitate peristaltic migration
through the pylorus to the small bowel. The weighted tubes
have failed to demonstrate any advantage with regard to place-
ment in randomized clinical trials.
8
Promotility agents (eg,
erythromycin) are often utilized to assist with these maneuvers
but are of questionable utility.
9
Bedside placement of postpylo-
ric tubes can be reasonably performed with success rates
approaching 80% with well-trained personnel.
10
In difficult
patients, more directed guidance can be accomplished with the
assistance of either endoscopy or fluoroscopy. Fluoroscopy has
been demonstrated to be more successful with regard to post-
pyloric placement and similar in cost compared with blindly
placed tubes. In addition, a reduced incidence of complications
and improved caloric delivery, particularly in the first 4 days
following tube placement, have also been demonstrated.
11,12
Disadvantages of this technique include delay in time until
placement and the potential need for patient transport. Endo-
scopically guided tubes allow for immediate assurance that the
tube is in the GI tract and allow for more distal guidance under
direct visualization. This can be accomplished using transnasal
endoscopy
13
(Figure 2) or with standard endoscopy using spe-
cialized techniques to transfer the wire from the oropharynx to
Figure 1. Most patients are amenable to less complex enteral
access strategies. However, as clinical complexity increases,
a small subset of patients will require more invasive measures
to achieve appropriate enteral access. PEG, percutaneous
endoscopic gastrostomy; PEGJ, PEG with jejunal extension; PEJ,
percutaneous endoscopic jejunostomy.
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
284 Journal of Parenteral and Enteral Nutrition 38(3)
the nasopharynx
13
(Figure 3).
14
Disadvantages include the
complications associated with endoscopy and sedation as well
as increased hospital costs.
Contraindications. Absolute contraindications to nasogas-
tric tube placement include certain patterns of facial fracture
(cribiform plate, nasal fractures), which can result in inadvertent
placement of the tube into the cranial vault. Proximal upper GI
malignancies, head and neck cancers, and esophageal divertic-
ula and strictures can preclude naso/orogastric tube placement
or predispose patients to morbid complications such as GI per-
foration. Although contraindications are rare, tube placement in
these patients should be performed only with the involvement
of appropriate clinicians, including those managing the primary
malignancy or those with advanced technical skills in endos-
copy or interventional radiology. Coagulopathies, either disease
related or medication induced, should trigger heightened aware-
ness for complication but generally do not preclude placement.
Complications and considerations. Risks associated with
placement in all patients without the above risk factors include
esophageal perforation, obstruction of normal sinus drainage
resulting in an increased incidence of sinusitis, and uninten-
tional placement into the bronchopulmonary tree. The rigidity
and large diameter of the standardly placed nasogastric tube
somewhat limits the duration that these tubes can be useful. One
study examined the incidence of middle ear effusions and altered
tympanometry in intubated patients with nasogastric tubes and
demonstrated that there was no increased incidence with 12 F
and 14 F tubes but there was with 18 F tubes.
15
Larger diam-
eter tubes are clearly more beneficial when decompression is
the goal but should be avoided in patients who are unlikely to
benefit from this feature. Sinusitis is often a difficult diagnosis to
make in the critically ill patient but appears to be closely linked
to the presence of nasogastric and nasoenteric tubes. Feeding
through nasogastric tubes in the setting of sedation or a patient
with a Glasgow Coma Score <7 have been demonstrated as
independent risk factors for nosocomial sinusitis in medical ICU
patients.
16
With regard to clinical relevance, 1 study suggested
sinusitis as the sole cause of fever of unknown etiology in as
many as 16% of surgical ICU patients, as demonstrated by imag-
ing, cultures, and clinical resolution with drainage.
17
In patients
with suspected infections and long-term nasoenteric tubes, prac-
titioners should actively rule out this potential complication.
Tube dislodgement and occlusion are not uncommon and
occur in 40%60% of patients.
18,19
Bridling techniques are use-
ful and can significantly reduce the incidence of unintentional
tube dislodgement with minimal morbidity.
19
Fortunately,
major complications from the use of nasoenteric tubes are rela-
tively uncommon. Potential major complications from nasoen-
teric tubes include esophageal perforation during placement,
malpositioning into the tracheobronchial tree or cranial vault,
mucosal ulceration and bleeding, sinusitis/rhinitis, submucosal
passage, aspiration, and stricture formation.
20
Nasogastric tube
syndrome (NGTS) is an interesting but rare complication com-
posed of the triad of nasoenteric intubation, throat pain, and
vocal cord paralysis. Vocal cord paralysis is often bilateral in
nature and is attributed to the edema, inflammation, and traction
generated by the presence of the tube. In a meta-analysis of
17 reported cases in the literature, symptoms began anywhere
from 12 hours to 2 weeks following tube placement and
Figure 2. Endoscopic-assisted nasoenteric tube placement.
(A) A guidewire is placed through the endoscope into the small
bowel. (B) A feeding tube is placed over the guidewire into the
small bowel. Reprinted with permission from Elsevier: DeLegge
MH. Enteral accessthe foundation of feeding: endoscopic
nasoenteric tube placement. Tech Gastrointest Endoscopy.
2011;3(1):22-29.
Figure 3. Technique for transferring wire from mouth out
through the nose, keeping the wire in position by pinning
it against the posterior wall of the pharynx. Reprinted with
permission from Elsevier: DeLegge MH. Enteral accessthe
foundation of feeding: endoscopic nasoenteric tube placement.
Tech Gastrointest Endoscopy. 2011;3(1):22-29.
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
Miller et al 285
consisted primarily of pain, stridor, dysphagia, and hoarseness.
21
Treatment consisted of antibiotics, parenteral steroids, and often
tracheostomy. This is mentioned only because it is a less well-
recognized and devastating complication directly attributable to
nasoenteric access and requires early and aggressive action to
prevent decompensation.
Blindly placed nasoenteric tubes have the obvious advantage
of generally avoiding conscious sedation and endoscopic inter-
vention. However, there is significant risk with blindly placed
nasoenteric tubes with regard to intubation of the tracheobron-
chial tree. In an informative recent review analyzing 5 contribut-
ing trials by Sparks et al,
22
9931 nasoenteric tubes were reviewed
with a malposition rate of 1.9%. Nearly 20% of the malposi-
tioned tubes resulted in a pneumothorax with 5 deaths attributed
to the complication. Also of interest, 60% of the malpositioned
tubes were in ventilated patients. In an attempt to reduce the
morbidity of nasoenteric tube placement, Marderstein et al
23
implemented a protocolized approach involving specialized
nasoenteric teams and limiting initial placement to 35 cm prior
to radiographic confirmation of location, which resulted in
reduced complications, particularly pneumothorax. Educational
endeavors include web-based training modules and have dem-
onstrated improvement in first-time success rates for the place-
ment of postpyloric tubes.
24
Serial films should clearly be
considered in patients with decreased mental status and history
of difficult tube placements. Mortality in these cases almost
exclusively involves initiating feeding through a tube in the tra-
cheobronchial tree. Blindly placed tubes must have confirma-
tory imaging to avoid these potentially fatal complications.
Ultimately, long-term feeding with nasogastric tubes has
been demonstrated to be less efficacious with regard to reduc-
ing weight loss in patients with head and neck cancer when
compared with gastrostomy.
25
Some of the major limitations of
long-term nasoenteric access are patient discomfort, tube
occlusion, and increased aspiration events. To allow for
improved patient tolerance, the tubes are generally smaller in
size, predisposing them to occlusion. Pulmonary aspiration
was 50% less with a percutaneous gastrostomy compared with
a nasoenteric tube in 1 trial.
26
In prospective trials in both
stroke patients and geriatric patients receiving long-term
enteral support, feeding through a gastrostomy resulted in
fewer aspiration events and improved tolerance compared with
nasoenteric feeding.
27,28
In conclusion, due to their inferiority
in nutrition delivery and inherent complication profile, stan-
dard naso/orogastric tubes should be viewed as short-term
access options for feeding less than 4 weeks duration as more
definitive measures are implemented.
Percutaneous Tubes: Surgical,
Endoscopic, and Radiologic Techniques
Should greater than 4 weeks of enteral access be thought nec-
essary, percutaneous and long-term access options should be
considered such as percutaneous endoscopic gastrostomy
(PEG), PEG with jejunal extension (PEGJ), direct percutane-
ous endoscopic jejunostomy (DPEJ), and surgical gastros-
tomy/jejunostomy. A small subset of complex surgical patients
as well as patients with end-stage liver disease, ascites, neu-
tropenia, and peritonitis will not be candidates for surgical
tubes, and longer term nasoenteric tubes may be the only
option. This is an important branch point in the treatment
algorithm and requires some foresight by the nutrition support
team (Figure 4).
The decision to pursue more permanent access can be facili-
tated through endoscopic, radiologic, or conventional surgical
approaches. Clinicians should be familiar with the options
available as well as the advantages, disadvantages, and compli-
cations associated with each approach (Table 1). Endoscopic
approaches offer the advantages of avoiding laparotomy and
general anesthesia, but there is no visualization of the other
intra-abdominal organs during placement (primarily the colon
and liver). An endoscope is inserted through the oropharynx,
past the esophagus, and into the stomach to allow for direct
needle access into the stomach. Transillumination and abdomi-
nal palpation must be clearly associated with indentation into
the stomach from the endoscopic viewpoint prior to catheter
access. Using a wire placed through the catheter, a tube is
either pushed or pulled through the dilated tract.
29
The same
principle is applied to percutaneous jejunal access, only the
endoscope must be advanced more distally into the jejunum,
which is then accessed with the finder needle (Figure 5).
30
Surgical approaches offer the advantage of direct visualiza-
tion of tube placement into the intended organ (stomach or
jejunum) but require a laparotomy or laparoscopy with the
potential for inherent complications (hernia, dehiscence, infec-
tion). During the surgical approach, the stomach or jejunum is
identified following a laparotomy incision, and the appropriate
tube is secured within the lumen of the targeted organ and
brought out through a separate stab incision. Variations in tech-
nique are important to understand in the event of inadvertent
removal and complication (Figure 6).
31
The standard Stamm
gastrostomy involves circumferential purse-string sutures sta-
bilizing the tube within the lumen of the stomach and fixing the
stomach to the posterior aspect of the anterior abdominal wall.
The Witzel technique involves creating a serosal tunnel as well
as an abdominal wall tunnel through which the tube passes and
is generally used when the target organ cannot be fixed to the
abdominal wall (eg, remnant stomach following Roux-en Y
gastric bypass). Utilization of specific surgical techniques is
largely surgeon and institution dependent. Witzel tubes, due to
their tunneled nature, are more difficult to replace and often
require radiologic assistance.
32
Laparoscopy can reduce inci-
sion size and potentially postoperative pain but can be difficult
in patients who have undergone multiple prior abdominal oper-
ations. The decision to use laparoscopic vs open techniques is
largely dictated by surgeon preference and their individual
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
286 Journal of Parenteral and Enteral Nutrition 38(3)
experience with laparoscopy. The risk of complications from
general anesthesia and laparotomy varies widely and is some-
what dependent on the overall condition of the patient.
The radiologic technique involves insufflation of the stom-
ach through either an angiocatheter or nasogastric tube with air
and using a combination of ultrasound, computed tomography,
and fluoroscopy to gain wire access into the lumen of the stom-
ach (Figure 7).
33
Wide variation in technique is used, with
some deploying anchors to appose the stomach to the posterior
abdominal wall.
34
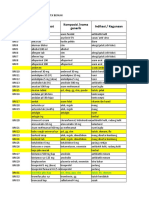
Can paent eat?
Nutrion Support
Indicated
Oral tolerant
Feed
Supplement
Oral intolerant
Decompression
needed?
Duraon of
access?
> 4 weeks
Endoscopic
access
feasible?
< 4 weeks
Nasoenteric
tube
Delayed
gastric
emptying
PEGJ/DPEJ
Surgical
candidate
Surgical
tube
Radiologic
tube
Yes No
No
Large-bore
nasogastric tube
Resoluon?
Feed through
large-bore tube
up to 5-7 days
Able to
eat?
Feed
Supplement
Yes
Yes
No
Yes
No
No Yes
Yes
No
Yes
No
PEG
Figure 4. An algorithm details the multiple factors that contribute to individualizing access options to appropriate patients. DPEJ,
direct percutaneous endoscopic jejunostomy; PEG, percutaneous endoscopic gastrostomy; PEGJ, PEG with jejunal extension.
Table 1. Comparison of the Various Enteral Access and Their Inherent Advantages and Disadvantages.
Tube Type Provider Absolute Contraindications Advantages Disadvantages
Large-bore nasogastric/orogastric Nurse Certain facial fractures/
trauma
Avoids sedation
Allows decompression
Blind placement
Patient discomfort
Blind nasoenteric feeding tubes Nurse/dietitian Certain facial fractures/
trauma
Avoids sedation
Cost
Blind placement
Endoscopic nasoenteric tubes Gastroenterologist
surgeon
No endoscopic access Visual confirmation Endoscopy
Percutaneous endoscopic
gastrostomy
Gastroenterologist
surgeon
No endoscopic access Long-term access Endoscopy
Percutaneous endoscopic
jejunostomy
Gastroenterologist
surgeon
Endoscopic access Long-term access
Distal feeding
Endoscopy
Radiologic gastrostomy Radiologist None No endoscopic access
required
Limited
availability
Surgical gastrostomy/jejunostomy Surgeon None Direct visualization General anesthesia
Laparotomy
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
287
F
i
g
u
r
e
5
.
S
c
h
e
m
a
t
i
c
o
f
d
i
r
e
c
t
p
e
r
c
u
t
a
n
e
o
u
s
e
n
d
o
s
c
o
p
i
c
j
e
j
u
n
o
s
t
o
m
y
(
D
P
E
J
)
p
l
a
c
e
m
e
n
t
p
r
o
c
e
d
u
r
e
.
(
A
)
T
h
e
e
n
t
e
r
o
s
c
o
p
e
i
s
a
d
v
a
n
c
e
d
u
n
t
i
l
t
r
a
n
s
i
l
l
u
m
i
n
a
t
i
o
n
i
s
a
c
h
i
e
v
e
d
.
(
B
)
A
d
i
s
c
r
e
t
e
i
n
d
e
n
t
a
t
i
o
n
s
h
o
u
l
d
b
e
r
e
p
r
o
d
u
c
i
b
l
e
w
i
t
h
d
i
r
e
c
t
d
e
p
r
e
s
s
i
o
n
a
t
t
h
e
s
i
t
e
o
f
t
r
a
n
s
i
l
l
u
m
i
n
a
t
i
o
n
.
(
C
)
T
h
e
s
o
u
n
d
i
n
g
a
n
e
s
t
h
e
s
i
a
n
e
e
d
l
e
i
s
i
n
s
e
r
t
e
d
a
t
t
h
e
s
i
t
e
o
f
d
e
p
r
e
s
s
i
o
n
/
t
r
a
n
s
i
l
l
u
m
i
n
a
t
i
o
n
a
n
d
a
d
v
a
n
c
e
d
u
n
t
i
l
i
t
i
s
s
e
e
n
t
o
e
n
t
e
r
t
h
e
j
e
j
u
n
a
l
l
u
m
e
n
u
n
d
e
r
e
n
d
o
s
c
o
p
i
c
v
i
s
u
a
l
i
z
a
t
i
o
n
.
(
D
)
T
h
e
n
e
e
d
l
e
/
c
a
n
n
u
l
a
i
s
i
n
s
e
r
t
e
d
a
l
o
n
g
s
i
d
e
t
h
e
s
o
u
n
d
i
n
g
n
e
e
d
l
e
.
(
E
)
W
i
t
h
t
h
e
n
e
e
d
l
e
r
e
m
o
v
e
d
f
r
o
m
w
i
t
h
i
n
t
h
e
i
n
d
w
e
l
l
i
n
g
c
a
n
n
u
l
a
,
t
h
e
i
n
s
e
r
t
i
o
n
w
i
r
e
i
s
a
d
v
a
n
c
e
d
t
h
r
o
u
g
h
t
h
e
c
a
n
n
u
l
a
a
n
d
g
r
a
s
p
e
d
b
y
t
h
e
a
w
a
i
t
i
n
g
s
n
a
r
e
t
h
a
t
e
x
t
e
n
d
s
f
r
o
m
t
h
e
t
i
p
o
f
t
h
e
e
n
d
o
s
c
o
p
e
.
(
F
,
G
)
T
h
e
s
c
o
p
e
i
s
t
h
e
n
r
e
m
o
v
e
d
,
a
n
d
t
h
e
i
n
s
e
r
t
i
o
n
w
i
r
e
i
s
w
i
t
h
d
r
a
w
n
w
i
t
h
i
t
s
o
t
h
a
t
1
e
n
d
o
f
t
h
e
i
n
s
e
r
t
i
o
n
w
i
r
e
e
x
t
e
n
d
s
f
r
o
m
t
h
e
m
o
u
t
h
a
n
d
t
h
e
o
t
h
e
r
e
n
d
e
x
t
e
n
d
s
f
r
o
m
t
h
e
a
b
d
o
m
i
n
a
l
w
a
l
l
.
(
G
,
H
)
T
h
e
a
t
t
a
c
h
m
e
n
t
l
o
o
p
o
f
t
h
e
p
u
l
l
-
t
y
p
e
g
a
s
t
r
o
s
t
o
m
y
f
e
e
d
i
n
g
t
u
b
e
i
s
t
e
t
h
e
r
e
d
t
o
t
h
e
m
o
u
t
h
e
n
d
o
f
t
h
e
i
n
s
e
r
t
i
o
n
w
i
r
e
,
a
n
d
t
h
e
a
s
s
e
m
b
l
y
i
s
p
u
l
l
e
d
i
n
t
e
r
n
a
l
l
y
u
n
t
i
l
t
h
e
f
e
e
d
i
n
g
t
u
b
e
h
a
s
t
r
a
v
e
r
s
e
d
t
h
e
j
e
j
u
n
a
l
a
n
d
a
b
d
o
m
i
n
a
l
w
a
l
l
s
a
n
d
i
s
p
u
l
l
e
d
u
p
s
n
u
g
l
y
.
R
e
p
r
i
n
t
e
d
w
i
t
h
p
e
r
m
i
s
s
i
o
n
f
r
o
m
E
l
s
e
v
i
e
r
:
G
i
n
s
b
e
r
g
G
G
.
D
i
r
e
c
t
p
e
r
c
u
t
a
n
e
o
u
s
e
n
d
o
s
c
o
p
i
c
j
e
j
u
n
o
s
t
o
m
y
.
T
e
c
h
G
a
s
t
r
o
i
n
t
e
s
t
E
n
d
o
s
c
o
p
y
.
2
0
1
1
;
3
(
1
)
:
4
2
-
4
9
.
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
288 Journal of Parenteral and Enteral Nutrition 38(3)
Complications and Considerations
The various complications of percutaneous access placement are
many. The reported major complication rate of PEG placement
is between 1% and 3%. DPEJ placement, which involves endo-
scopic placement of a tube within the jejunum as opposed to the
stomach, can be performed by experienced endoscopists but car-
ries a significantly higher major complication rate and has a
lower success rate.
35
This is due in part to the variability in loca-
tion and mobility of the targeted access point. In addition, the
risk of conscious sedation must be considered for both proce-
dures but is generally low. Complications associated with percu-
taneous endoscopic approaches include endoscopic trauma and
perforation of the GI tract, bleeding, skin and soft tissue infec-
tion, injury to intra-abdominal viscera such as the liver or colon,
tube dislodgement, and fistula creation. These complications are
discussed in further detail in subsequent sections.
Radiologic placement has many of the same risks as endoscop-
ically placed tubes (soft tissue infection, bleeding, injury to intra-
abdominal viscera, etc) with the exception of the absence of scope
trauma/perforation of the upper aerodigestive tract. The reported
major complication rate is below 8%, with minor complications in
up to 10% of patients.
36
Surgically placed tubes are associated
most commonly with skin and soft tissue infection, incisional her-
nia, bleeding, inadvertent removal, and complications associated
with general anesthesia. Issues with inadvertent injury to sur-
rounding intra-abdominal viscera should be exceedingly rare if
not eliminated. The incidence of complication for surgical gas-
trostomy has been reported as between 7% and 15%.
32
When sur-
gical enteral routes are deemed appropriate, multiple variants of
operative access to the GI tract are available.
In a randomized controlled trial comparing endoscopic,
laparoscopic-assisted, and open gastrostomy tube placement,
the laparoscopic-assisted approaches had an increased compli-
cation rate compared with the open and endoscopic techniques.
The open technique took the longest to perform and had the
greatest delay in the initiation of feeding.
37
Decreased compli-
cation rates are generally reported when endoscopic techniques
are compared with surgical feeding tube placement. Overall,
regardless of the technique employed, complication rates are
generally low even given the high prevalence of malnutrition
and chronic disease states in this patient population.
38
One final point with regard to enteral access involves clini-
cian awareness. Should a patient be taken to the operating
room to undergo laparotomy for another reason, consideration
should be given to placing enteral access at the time of opera-
tion. This can result in the avoidance of unnecessary and tech-
nically demanding procedures should the patient ultimately
require access at a later time.
Contraindications
Percutaneous endoscopic approaches have become the preferred
approach to obtaining longstanding enteral access primarily due
Figure 6. Surgical techniques for enteral access: (A) cross-
sectional representation of a typical Stamm gastrostomy. (B)
Witzel tunnels are an alternative technique generally used
when apposition to the abdominal wall cannot be performed.
(C) Laparoscopic approaches can be performed. Reprinted
with permission from Elsevier: Allen JW, Spain DA. Open and
laparoscopic surgical techniques for obtaining enteral access.
Tech Gastrointest Endoscopy. 2001;3(1):50-54.
Figure 7. Computed tomography (CT)guided percutaneous
gastrostomy (PG). (A) The left lobe of the liver wraps over the
stomach, obviating a safe access route. There is also a small
amount of ascites. (B) A CT-guided lateral approach into the
stomach permits initial access. (C) The distended stomach
now permits access into the stomach for PG. Reprinted with
permission from Elsevier: vanSonnenberg E, Wittich GR,
Goodacre BW. Radiologic percutaneous gastrostomy and related
enterostomies. Tech Gastrointest Endoscopy. 2001;3(1):16-21.
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
Miller et al 289
to reduced costs, reduced complication rates, and the ability to
avoid the morbidity (pain, complications) of laparotomy. PEG
placement generally requires conscious sedation but has been
successfully performed with no sedation.
39
Fewer and fewer
absolute contraindications to PEG placement persist as clini-
cians continue to expand and refine the available techniques.
Special considerations include patients with surgically altered
gastric and upper GI anatomy, including gastric bypass, gastric
resections, and gastrojejunostomy. Prior laparotomy, particu-
larly those resulting in large ventral hernias requiring repair with
mesh or resulting from intra-abdominal catastrophes, can make
placement more technically difficult or prohibitive, but studies
have demonstrated similar safety and efficacy results in these
patients.
40-42
In patients with esophageal cancer, there is some
concern for inadvertent disruption of the gastroepiploic artery,
which is the primary supply to the gastric conduit following
esophagectomy, but this is reportedly a rare occurrence.
43
Although morbidly obese patients can also present significant
technical challenges, PEG placement has been demonstrated to
be both safe and feasible.
44
Patients with preexisting ventriculo-
peritoneal (VP) shunts were once thought to be poor candidates,
but retrospective data have not demonstrated an increased risk of
shunt infections with PEG placement.
45
Inability to pass the endoscope through the oropharynx or
esophagus remains an absolute contraindication to PEG or PEJ
placement for obvious reasons. Placing a PEG using the Russel
introducer technique and a narrow caliber endoscope is pos-
sible if a total obstruction is not present. In these patients,
options include surgical placement of a gastrostomy/jejunos-
tomy or placement using radiologic techniques. The availabil-
ity of interventional radiologists who are trained and willing to
use the radiographic techniques will largely dictate which
approach is feasible in most institutions.
Preexisting medical comorbidities must be considered.
Patients with advanced liver disease who undergo percutane-
ous enteral access have a 30-day mortality as high as 40%, with
the large majority of the mortalities observed in patients with
ascites.
46
Therefore, most would consider ascites to represent a
relative contraindication to PEG placement. Finally, there are
limited data with regard to PEG placement in adult patients
with neutropenia. A small study examining bone marrow trans-
plant patients in children found a 36% risk of infectious com-
plications in patients with neutropenia.
47
In general,
individualized risk-benefit analysis should be considered and
PEG placement should probably be avoided in neutropenic
adult patients.
47
Common Management Issues
Managing Newly Placed Tubes
Naso/orogastric tubes. The mainstays of management of
naso/orogastric tubes include adequate securing of the tube to
maintain the level of infusion as well as frequent flushing of
the tube to prevent occlusion. Tubes should be flushed regu-
larly and following the administration of medications. Once
the position of the tube has been confirmed, feeding can be
initiated immediately.
PEG/PEGJ/ DPEJ tubes. Following placement of percutane-
ous tubes, the external bolster should generally be left apposed
to the skin for at least 4 days. After 4 days, there should be
to 1 cm of laxity left between the entry point and the bumper of
the tube to prevent buried bumper syndrome.
48
In the long
term, commercially available devices allow the tube to exit
perpendicular to the abdominal wall. This avoids abnormal
traction and potential erosion of the tract by the tube. Several
randomized trials have demonstrated the safety of immediate
feeding after PEG placement.
49,50
After changes in patient posi-
tioning and edema at the placement site, the original PEG posi-
tion can change. Rechecking the tube position 2448 hours
after placement can avoid overtightening of the PEG bolster.
Altering the Level of Infusion
Although gastric feeds are tolerated well by most patients,
there are several appropriate clinical scenarios where more dis-
tal access is appropriate. Changing the level of infusion more
distally in the GI tract reduces reflux and aspiration but may
not reduce the incidence of pneumonia or improve caloric
delivery.
51
Tubes most commonly placed are gastric, duodenal
(postpyloric), and jejunal (distal to the ligament of Treitz).
Reasons for considering distal access include severe acute pan-
creatitis, true intolerance to gastric feeding, and diversion from
a surgically altered proximal gastric or duodenal anatomy.
Tubes placed at the bedside into the stomach will often migrate
more distally regardless of intention to do so. Determining the
appropriate level of infusion is often fluid, requires reassess-
ment, and may need alteration with changes in patient condi-
tion. Prior to PEG placement, it is often appropriate to trial the
patient on gastric feeds to ensure tolerance. Combination gas-
trojejunal feeding tubes are available for placement at the time
of laparotomy. A jejunal extension tube can be placed through
a preexisting PEG to facilitate more distal feeding while also
providing an avenue for gastric decompression when
necessary.
Who Should Put These Tubes In?
A multidisciplinary approach to placement of enteral access is
preferred. Nasoenteric tubes are generally placed by dietitians
and nurses, whereas percutaneous and surgically placed tubes
are performed by a wide array of physicians, including gastro-
enterologists, surgeons, radiologists, and medical intensivists.
If prolonged access is warranted and the patient is able to
undergo endoscopy, endoscopic gastrostomy or jejunostomy
performed by surgeons or gastroenterologists is the likely
choice. If the stomach is unable to be accessed endoscopically,
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
290 Journal of Parenteral and Enteral Nutrition 38(3)
radiologic techniques (interventional radiologists) and open
gastrostomy/jejunostomy (surgeons) are appropriate options.
Enteral Access and Liver Failure
As mentioned previously, patients with advanced liver disease
experience significant mortality when undergoing percutane-
ous enteral access procedures. This is particularly true in those
with ascites.
46
Nasoenteric access is the preferred route in
these patients for this reason. Ascites can preclude adequate
seal and lead to continued ascites leak and predispose the
patient to bacterial peritonitis. PEG placement is potentially
feasible if ascites is adequately drained through paracentesis
prior to placement and the patient is kept dry until an appro-
priate seal is formed. A seal can be facilitated through gastro-
pexy using T-fasteners at the time of placement and has been
described.
52
Esophageal varices are another potential compli-
cation associated with advanced liver disease. Management
decisions in these patients can prove quite difficult and should
generally be managed on an individualized basis. Patients
with nonbleeding esophageal varices should be fed through
nasoenteric access. However, in patients with actively bleed-
ing varices, nasoenteric tube placement should likely be
avoided.
53
Anticoagulation and Enteral Access
According to guidelines published by the American Society of
Gastrointestinal Endoscopy (ASGE), percutaneous enteral
access is considered a high-risk endoscopic procedure.
54
As
such, patients receiving therapeutic anticoagulation should
have their anticoagulants held for an appropriate period to
ensure normalization of coagulation parameters (57 days for
warfarin). For patients with high-risk conditions (heart valves,
etc), bridge therapy with heparin or low-molecular-weight
heparin can be considered. Anticoagulation can generally be
safely resumed within 1 day of uncomplicated percutaneous
enteral access.
Decisions regarding withholding antiplatelet therapy
depend highly on the underlying indications for which they are
prescribed. Any decision to hold therapy should be discussed
with the patients appropriate managing physician. In general,
patients on single-agent therapy with aspirin or nonsteroidal
anti-inflammatory drugs (NSAIDs) may continue these medi-
cations during the periprocedural period. Consideration should
be given to holding thienopyridines (eg, clopidigrel) for 5 days
prior to percutaneous enteral access if possible. Patients on
dual therapy should continue aspirin, and consideration should
be given to starting aspirin for patients on thienopyridine
monotherapy if it is to be held during the periprocedural period.
One recent study did not show a significant increase in bleed-
ing events with antiplatelet therapy held for shorter durations
and suggested 3 days prior to the procedure as a safe waiting
time.
55
Patients undergoing percutaneous enteral access will com-
monly be on prophylactic dosages of anticoagulants such as
low-molecular-weight heparin to prevent venous thromboem-
bolism. The bleeding risk for procedures on these agents is not
well studied, but it appears reasonable and safe to hold them
the day of the procedure and resume them the following day.
56
How Do You Address the Combative
Patient?
Combative and agitated patients present additional hurdles to
maintaining adequate enteral access as tubes can become dis-
lodged or entirely removed. ICU psychosis and recreational
drug or alcohol withdrawal are common situations resulting in
both airway and enteral access issues. Tube dislodgement is a
major contributor to reduced caloric provision in the ICU in
addition to requiring significant cost and resources for repeated
replacement.
18
Nasoenteric tubes can be secured with a nasal bridle.
Commercially available magnetized devices are available for
use as opposed to the standard adhesive tape that is tradition-
ally applied. Magnetized kits offer the advantage of bedside
placement with minimal sedation and instrumentation of the
oropharynx. These are best placed at the time of tube place-
ment, taking advantage of conscious sedation or general anes-
thesia. A recent randomized controlled trial in 80 surgical
intensive care patients compared the bridling technique with
standard adhesive tape application. Only 18% of the bridled
tubes became dislodged vs 63% of the nonbridled tubes, result-
ing in significantly improved caloric provision (78% vs 62%
goal) in the bridled group.
19
Complications of the bridling
technique included nasal ulceration and epistaxis. This tech-
nique provides a practical and safe approach for securing the
access device.
Managing Complications
Wound Infection
Peristomal infections are a common concern but probably
occur in less than 1%2% of cases. Most cases consist of mild
superficial cellulitis that can be treated with antibiotics cover-
ing normal skin flora, although methicillin-resistant
Staphylococcus aureus (MRSA) is becoming increasingly
common.
57
Rarely cases will involve an abscess within the soft
tissue surrounding the tube and are best treated with local
drainage and subsequent wound care. Even more rarely,
abscesses develop in the deeper tissue planes and are not read-
ily apparent on visual inspection. Patients usually report exces-
sive pain around the tube and may exhibit signs of systemic
infection such as leukocytosis or fever. Computed tomography
(CT) scan can be helpful in the diagnosis of these abscesses.
They can usually be drained by extending the tube site skin
incision. Patients with percutaneous enteral access can also
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
Miller et al 291
develop necrotizing soft tissue infections at the tract site.
58,59
The treatment involves systemic antibiotics and prompt surgi-
cal debridement of affected tissues. Tube removal is usually
necessary. Fortunately, these cases are rare. Signs of infection
or leakage should also prompt consideration for the buried
bumper syndrome as described below.
The overall incidence of infections at PEG sites can be
decreased by the use of periprocedural antibiotics.
60,61
A single
intravenous (IV) dose of a first-generation cephalosporin 30
minutes prior to the procedure is acceptable. Recent studies
have also shown equivalence with a single oral dose of Bactrim
instilled into the PEG tube after placement.
62
Bleeding
Significant bleeding during percutaneous enteral access is
uncommon. Most bleeding represents disruption of superficial
blood vessels arising from the tube tract, which can be con-
trolled by tightening the bumper to apply direct pressure. An
excellent retrospective study examining more than 1500 PEG
insertions determined a GI bleeding incidence of around 3%
and bleeding directly attributable to PEG placement as 0.4%.
Heparin and length of hospitalization were 2 independent risk
factors identified. Alternative antiplatelet and anticoagulants
were not identified as independent risk factors despite being
held between 1 and 2 days prior to intervention. Nearly 10% of
the patients undergoing PEG placement were on clopidrogrel
in this study.
63
If excessive pressure is required, it should be
released within 2448 hours to avoid injury to the skin.
Ulceration with subsequent bleeding may also occur in the
stomach on the posterior wall opposite the PEG or underneath
the internal bolster. Abdominal wall and rectus sheath hemato-
mas can occur,
64
but these are usually self-limited and gener-
ally do not require intervention. There are case reports of aortic
perforation, gastric artery injury, and retroperitoneal hemor-
rhage during PEG placement.
65,66
Adherence to good technique
should limit risk to significant blood vessels, as they can gener-
ally be visualized endoscopically and with transillumination.
As previously discussed, coagulopathy should be corrected
and anticoagulants should be held during access procedures to
decrease the risk of bleeding complications. In addition, there
is recent evidence that the bleeding risk during PEG is increased
with the use of serotonin reuptake inhibitors.
67
Leakage
Peristomal leakage of gastric contents due to enlarging diameter
of the PEG tract is a common complication and reported in some
studies as high as 10%.
68
Most common causes are side torsion
on the tract wall causing ulceration at the skin and enlargement
of the hole. This can be corrected by using a commercial clamp-
ing device to secure the tube and prevent side pressure against
the walls of the tract. The second most common cause is lack of
an external bolster allowing the tube to migrate in and out,
thereby causing enlargement of the PEG tract (Figure 8).
69
Creating an external bolster or replacing the PEG usually cor-
rects this problem. A common pitfall, however, is excessive
tightening of the bolster to stop leakage (Figure 9).
69
This will
only lead to further skin breakdown and delay further wound
healing. Another common pitfall is replacing a leaking tube with
a larger diameter tube in the hopes of obtaining a better seal.
This only serves to further enlarge and distort the leaking tube
tract. In rare cases of persistent leakage, the site must be sacri-
ficed, and the tube may have to be replaced to a different skin
site, allowing the original site to close and heal.
Pneumoperitoneum
Pneumoperitoneum is relatively common after PEG place-
ment.
70,71
PEG placement represents a controlled perforation of
a hollow viscus, so some degree of pneumoperitoneum is
expected. It is caused by the distention of the stomach with
escape of air into the peritoneal space during endoscopy with
subsequent needle puncture. It is a benign condition but can
lead to diagnostic confusion for clinicians. If there are no asso-
ciated signs of peritonitis, it can simply be observed. Most
cases will resolve within 72 hours. If there is uncertainty, a
contrasted study through the tube or a CT scan can be obtained
to confirm position. Pneumoperitoneum should only be con-
sidered benign for newly placed enteral access. Patients with
mature tubes who present with free air should undergo the
same diagnostic considerations as any other patient.
Figure 8. Excessive torsion can enlarge the tube tract, resulting
in leakage and superficial excoriation. Reprinted with permission
from Elsevier: McClave SA, Chang WK. Complications of
enteral access. Gastrointest Endoscopy. 2003;58(5):745.
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
292 Journal of Parenteral and Enteral Nutrition 38(3)
Clogging/Tube Dysfunction
Tube clogging is a common and frustrating issue and can occur
with both medication administration as well as enteral formula.
The best management strategy is prevention. All medications
should be appropriately dissolved in liquid prior to administra-
tion. Certain medications such as bulking agents or resins
should never be placed through enteral access tubes. Tubes
should also be flushed with warm water after every use. If clog-
ging does occur, the tube can usually be irrigated using a syringe
to create pressure. Pancreatic enzymes dissolved in bicarbonate
and allowed to dwell in the tube prior to flushing may be also be
effective.
72
If clogging is persistent, guidewires or specially
designed tube brushes may be used. Occasionally, tubes will
have to be replaced for clogging, cracks, or general deteriora-
tion. This appears to be more common with silicone tubes (due
to fungal colonization) compared with polyurethane.
73
Persistent Fistula Following Removal
Following removal, most tube sites will close spontaneously
within 72 hours. The development of a persistent gastric fistula
is more common in children and may correlate with the dura-
tion of tube use.
74
Treatment often requires formal surgical
closure of the fistula. Minimally invasive techniques, includ-
ing gastric mucosa endoclipping, fibrin glue, and fistula tract
lining disruption using a curette or electrocautery device, have
also been described and may be attempted prior to proceeding
with surgery.
75-78
Anecdotally, placing a purse-string suture
beneath the skin in the subcutaneous tissue may be added to the
endoclipping of the mucosal defect to promote closure.
Buried Bumper Syndrome
Buried bumper syndrome occurs when the internal bolster of
the PEG erodes into the gastric wall as a long-term conse-
quence of excessive tightening of the bolsters.
79
The syndrome
is associated with pain, increased drainage, PEG site infection/
inflammation, and eventually an inability to feed through the
tube. Diagnosis is usually made by endoscopy or CT scan.
Treatment involves removal and replacement of the tube and
can be done through the same site, adding a commercial clamp-
ing device to hold the tube in place, prevent migration into the
mucosa, and allow for healing of the ulceration to take place.
Inadvertent Removal
Percutaneously and surgically placed tubes also can be dis-
lodged or removed during episodes of agitation and present
additional problems. An interesting recent retrospective review
of 563 PEGs over a 3-year period demonstrated an early
(within 7 days) dislodgement rate of 4.1% and total lifetime
dislodgement rate of almost 13%, with most occurring after
discharge from inpatient hospitalization. The average cost of
replacement was $1200.
80
Abdominal binders and clinical
restraints can be useful adjuncts following PEG placement and
prevent patient access to the majority of the tube. Tailoring the
tube at a length that allows adequate care but also restricts
access is advisable. Inadvertent removal is a relatively com-
mon and expensive problem. Management of tube removal
depends on the length of time the tube has been present and the
overall maturity of the tract. For tubes in place >4 weeks, blind
bedside tube replacement through the tube tract is generally
safe and easy. It should be attempted as soon as possible to
prevent the tube tract from closing. A similarly sized Foley
catheter is commonly available and makes for a great tempo-
rary replacement PEG. If enteric contents can be aspirated and
the tube flushes easily, a confirmatory radiographic study is not
necessary. For tubes in place <4 weeks, inadvertent removal
can create an emergent situation. If the stomach serosa has not
had time to adhere to the parietal peritoneum, tube removal
will cause it to fall away and leak into the peritoneal cavity.
Depending on clinician discretion, blind bedside replacement
can still be attempted but should be followed promptly with a
water-soluble contrast study to confirm position. For recently
placed tubes (<2 weeks), patients with inadvertent removal can
be treated with immediate endoscopy and replacement of the
tube through the same site. Prophylactic antibiotics and moni-
toring for signs of peritonitis and the need for surgical explora-
tion are recommended in these situations. If unable to replace
Figure 9. Commercial clamping devices can prevent
torsion within the tube tract and allow healing. Reprinted
with permission from Elsevier: McClave SA, Chang WK.
Complications of enteral access. Gastrointest Endoscopy.
2003;58(5):747.
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
Miller et al 293
the PEG immediately, the patient can be managed by nasogas-
tric aspiration, broad-spectrum antibiotics, and parenteral
nutrition. Surgical exploration is warranted if the patient dem-
onstrates signs of peritoneal leakage and early peritonitis.
69,81
Liver Injury
The left lateral segment of the liver lies in close proximity to
the stomach and may be quite large in some patients or low
lying in other patient populations (eg, chronic obstructive pul-
monary disease). Liver injuries commonly occur with the tube
tract passing through the liver parenchyma prior to entering the
stomach and can lead to fistula formation.
82
Liver injuries are
most commonly associated with bleeding, either during place-
ment or at the time of removal. In many cases, injury may be
completely asymptomatic and diagnosed in delayed fashion.
When identified, tubes passing through the liver can be
removed surgically or endoscopically.
83,84
If surgical hemosta-
sis is not obtained, a period of observation for signs of bleeding
after removal is warranted. This complication may be pre-
vented by routinely percussing and marking the lower edge of
the liver prior to choosing the PEG site.
Colon Injury
The splenic flexure of the colon lies in close proximity to the
stomach and may overly portions of it in some patients. Injuries
to the colon usually involve the tube passing through the colon
prior to entering the stomach. Although possible, most injuries
do not lead to early onset peritonitis and are diagnosed in
delayed fashion. Patients may develop colocutaneous or gas-
trocolic fistulas that become evident only at the time of tube
removal.
85,86
Conservative measures are often successful in
obtaining closure (pulling the PEG tube and simply applying a
dressing over the tract site), but occasionally surgery is required
for definitive treatment.
Conclusion
The provision of adequate nutrition support in the hospital set-
ting is the standard of care. Enteral access in patients unable to
sustain volitional oral intake is a fundamental concept, allow-
ing the facilitation of appropriate support. As in any interven-
tion, forethought and consideration should be given to
successfully use the appropriate access option in a given
patient. Clinicians across disciplines should have a working
knowledge with regard to technique as well as the advantages
and disadvantages of the various enteral access options to opti-
mize outcomes and minimize unnecessary and higher risk
interventions. Finally, in the event that complications arise
from attempted access, clinicians should be aware of appropri-
ate management strategies to prevent further clinical deteriora-
tion and salvage attempts at ongoing support.
Further Reading
Allen JW, Spain DA. Open and laparoscopic surgical techniques for obtaining
enteral access. Tech Gastrointest Endosc. 2001;3(1):50-54.
DeLegge MH. Enteral accessthe foundation of feeding: endoscopic nasoen-
teric tube placement. Tech Gastrointest Endosc. 2001;3(1):22-29.
Ginsberg GG, Kochman M, Norton I, Gostout C. Clinical Gastrointestinal
Endoscopy. 2nd ed. Philadelphia, PA: Elsevier Saunders; 2005.
McClave SA, Chang WK. Complications of enteral access. Gastrointest
Endosc. 2003;58(5):739-751.
Glossary
APACHEAcute Physiology and Chronic Health Evaluation. A severity
of illness score used in the ICU that takes into account acute and chronic
illness to predict mortality.
Dobhoff tubea subtype of tube placed through the mouth or nose into the
GI tract.
DPEJdirect percutaneous endoscopic jejunostomy. Endoscopically
placed tube into the jejunum through the abdominal wall.
Fluoroscopyreal-time imaging modality using x-ray.
Frenchunit of measurement used in tube diameters equal to 1/3 mm.
GCSGlasgow Coma Score. A severity of derangement score used to
assess neurologic score in the ICU and in trauma patients.
ISSInjury Severity Score. A severity of illness score in trauma patients
used to predict mortality, morbidity, and length of hospitalization.
Nasoenteric accessbroad term to describe tubes placed through the
nose into the GI tract; includes nasogastric as well as nasojejunal
tubes.
Nasogastricplaced through the nose into the stomach.
Orogastricplaced through the mouth into the stomach.
PEGpercutaneous endoscopic gastrostomy. Endoscopically placed tube
into the stomach through the abdominal wall.
PEGJpercutaneous endoscopic gastrojejunostomy. An extension tube
placed through an existing PEG down into the jejunum.
Polyurethaneless compliant material used in tubes commonly utilized
for gastric decompression and replacement pegs.
Siliconemost common material used in feeding tubes, prone to fungal
colonization.
SOFASequential Organ Failure Assessment. A severity of illness score
assessing organ function used in the ICU to predict mortality.
References
1. Anthony PS. Nutrition screening tools for hospitalized patients. Nutr Clin
Pract. 2008;23:373-382.
2. Heyland DK, Dhaliwal R, Jiang X, Day AG. Identifying critically ill
patients who benefit the most from nutrition therapy: the develop-
ment and initial validation of a novel risk assessment tool. Crit Care.
2011;15(6):R268.
3. Osland E, Yunus RM, Khan S, Memon MA. Early versus traditional
postoperative feeding in patients undergoing resectional gastroin-
testinal surgery: a meta-analysis. JPEN J Parenter Enteral Nutr.
2011;35(4):473-487.
4. Marik PE, Zaloga GP. Early enteral nutrition in acutely ill patients:
a systematic review [published correction appears in Crit Care Med.
2002;30(3):725]. Crit Care Med. 2001;29(12):2264-2270.
5. Doig GS, Heighes PT, Simpson F, Sweetman EA. Early enteral nutrition
reduces mortality in trauma patients requiring intensive care: a meta-anal-
ysis of randomised controlled trials. Injury. 2011;42(1):50-56.
6. Munera-Seeley V, Ochoa JB, Brown N, et al. Use of a colorimetric car-
bon dioxide sensor for nasoenteric feeding tube placement in critical
care patients compared with clinical methods and radiography. Nutr Clin
Pract. 2008;23(3):318-321.
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
294 Journal of Parenteral and Enteral Nutrition 38(3)
7. Bercik P, Schlageter V, Mauro M, et al. Noninvasive verification of naso-
gastric tube placement using a magnet-tracking system: a pilot study in
healthy subjects. JPEN J Parenter Enteral Nutr. 2005;29(4):305-310.
8. Levenson R, Turner WW, Dyson A, et al. Do weighted nasoenteric feed-
ing tubes facilitate duodenal intubation? JPEN J Parenter Enteral Nutr.
1988;12(12):135-137.
9. van den Bosch S, Witteman E, Kho Y, Tan AC. Erythromycin to pro-
mote bedside placement of a self-propelled nasojejunal feeding tube in
non-critically ill patients having pancreatitis: a randomized, double-blind,
placebo-controlled study. Nutr Clin Pract. 2011;26(2):181-185.
10. Gatt M, MacFie J. Bedside postpyloric feeding tube placement: a pilot
series to validate this novel technique. Crit Care Med. 2009;37(2):523-527.
11. Prager R, Laboy V, Venus B, et al. Value of fluoroscopic assistance during
transpyloric intubation. Crit Care Med. 1986;14(2):151-152.
12. Huerta G, Puri VK. Nasoenteric feeding tubes in critically ill patients
(fluoroscopy versus blind). Nutrition. 2000;16(4):264-267.
13. DeLegge MH. Enteral accessthe foundation of feeding: endoscopic
nasoenteric tube placement. Tech Gastrointest Endosc. 2001;3(1):22-29.
14. Zhang L, Huang YH, Yao W, Chang H, Guo CJ, Lin SR. Transnasal
esophagogastroduodenoscopy for placement of nasoenteric feeding
tubes in patients with severe upper gastrointestinal diseases. J Dig Dis.
2012;13(6):310-315.
15. Gonzlez Pena M, Figuerola Massana E, Hernndez Gutirrez P, Rello
Condomines J. Middle ear effusion in mechanically ventilated patients:
effects of the nasogastric tube. Respir Care. 2013;58(2):273-278.
16. George DL, Falk PS, Umberto Meduri G, et al. Nosocomial sinusitis in
patients in the medical intensive care unit: a prospective epidemiological
study. Clin Infect Dis. 1998;27(3):463-470.
17. van Zanten AR, Dixon JM, Nipshagen MD, de Bree R, Girbes AR,
Polderman KH. Hospital-acquired sinusitis is a common cause of fever of
unknown origin in orotracheally intubated critically ill patients. Crit Care.
2005;9(5):R583-R590.
18. McClave SA, Sexton LK, Spain DA, et al. Enteral tube feeding in the
intensive care unit: factors impeding adequate delivery. Crit Care Med.
1999;27:1252-1256.
19. Seder CW, Stockdale W, Hale L, Janczyk RJ. Nasal bridling decreases
feeding tube dislodgment and may increase caloric intake in the surgi-
cal intensive care unit: a randomized, controlled trial. Crit Care Med.
2010;38(3):797-801.
20. Prabhakaran S, Doraiswamy VA, Nagaraja V, et al. Nasoenteric tube com-
plications. Scand J Surg. 2012;101(3):147-155.
21. Brousseau VJ, Kost KM. A rare but serious entity: nasogastric tube syn-
drome. Otolaryngol Head Neck Surg. 2006;135(5):677-679.
22. Sparks DA, Chase DM, Coughlin LM, Perry E. Pulmonary complications
of 9931 narrow-bore nasoenteric tubes during blind placement: a critical
review. JPEN J Parenter Enteral Nutr. 2011;35(5):625-629.
23. Marderstein E, Simmons R, Ochoa J. Effect of institutional protocols on
adverse events related to feeding tube placement in the critically ill. J Am
Coll Surg. 2004;199:39-50.
24. Lee JM, Fernandez F, Staff I, Mah JW. Web-based teaching module
improves success rates of postpyloric positioning of nasoenteric feeding
tubes. JPEN J Parenter Enteral Nutr. 2012;36(3):323-329.
25. Sobani ZU, Ghaffar S, Ahmed BN. Comparison of outcomes of enteral
feeding via nasogastric versus gastrostomy tubes in post operative patients
with a principle diagnosis of squamous cell carcinoma of the oral cavity. J
Pak Med Assoc. 2011;61(10):1042-1045.
26. McClave SA, Lukan JK, Stefater JA, et al. Poor validity of residual vol-
umes as a marker for risk of aspiration in critically ill patients. Crit Care
Med. 2005;33(2):324-330.
27. Norton B, Homer-Ward M, Donnelly MT, Long RG, Holmes GK. A
randomised prospective comparison of percutaneous endoscopic gas-
trostomy and nasogastric tube feeding after acute dysphagic stroke. BMJ.
1996;312(7022):13-16.
28. Dwolatzky T, Berezovski S, Friedmann R, et al. A prospective compari-
son of the use of nasogastric and percutaneous endoscopic gastrostomy
tubes for long-term enteral feeding in older people. Clin Nutr. 2001;20(6):
535-540.
29. Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparot-
omy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):
872-875.
30. Ginsberg GG. Direct percutaneous endoscopic jejunostomy. Tech
Gastrointest Endosc. 2001;3(1):42-49.
31. Allen JW, Spain DA. Open and laparoscopic surgical techniques for
obtaining enteral access. Tech Gastrointest Endosc. 2001;3(1):50-54.
32. Khaodhiar L, Blackburn G. Enteral nutrition support. In: Fischer JE
et al. Mastery of surgery, 4th ed. Philadelphia, PA; Lippincott Williams &
Wilkins, 2001: 45-55.
33. vanSonnenberg E, Wittich GR, Goodacre BW. Radiologic percutane-
ous gastrostomy and related enterostomies. Tech Gastrointest Endosc.
2001;3(1):16-21.
34. Shin JH, Park AW. Updates on percutaneous radiologic gastrostomy/gas-
trojejunostomy and jejunostomy. Gut Liver. 2010;4(suppl 1):S25-S31.
35. Maple JT, Petersen BT, Baron TH, Gostout CJ, Wong Kee Song LM,
Buttar NS. Direct percutaneous endoscopic jejunostomy: outcomes in 307
consecutive attempts. Am J Gastroenterol. 2005;100(12):2681-2688.
36. Wollman B, DAgostino HB, Walus-Wigle JR, Easter DW, Beale A.
Radiologic, endoscopic, and surgical gastrostomy: an institutional evalua-
tion and meta-analysis of the literature. Radiology. 1995;197:699-704.
37. Bankhead RR, Fisher CA, Rolandelli RH. Gastrostomy tube placement
outcomes: comparison of surgical, endoscopic, and laparoscopic methods.
Nutr Clin Pract. 2005;20(6):607-612.
38. Ljungdahl M, Sundbom M. Complication rate lower after percutaneous
endoscopic gastrostomy than after surgical gastrostomy: a prospective,
randomized trial. Surg Endosc. 2006;20(8):1248-1251.
39. Steed H, Barrett D, Emm C, et al. Unsedated percutaneous endoscopic
gastrostomy insertion: a safe, effective, and well-tolerated method. JPEN
J Parenter Enteral Nutr. 2012 Mar;36(2):231-234.
40. Stellato TA, Gauderer MW, Ponsky JL. Percutaneous endoscopic gastros-
tomy following previous abdominal surgery. Ann Surg. 1984;200:46-50.
41. Stiegmann GV, Goff JS, Silas D, Pearlman N, Sun J, Norton L. Endoscopic
versus operative gastrostomy: final results of a prospective, randomized
trial. Gastrointest Endosc. 1990;36:1-5.
42. Eleftheriadias E, Kotzampassi K. Percutaneous endoscopic gastrostomy
after abdominal surgery. Surg Endosc. 2001;15:213-216.
43. Stockeld D, Fagerberg J, Granstrom L, et al. Percutaneous endoscopic
gastrostomy for nutrition in patients with oesophageal cancer. Eur J Surg.
2001;167:839-844.
44. Bochicchio GV, Guzzo JL, Scalea TM. Percutaneous endoscopic gastros-
tomy in the supermorbidly obese patient. JSLS. 2006;10(4):409-413.
45. Kim JS, Park YW, Kim HK, et al. Is percutaneous endoscopic gastros-
tomy tube placement safe in patients with ventriculoperitoneal shunts?
World J Gastroenterol. 2009;15:3148-3152.
46. Baltz JG, Argo CK, Al-Osaimi AM, Northup PG. Mortality after percu-
taneous endoscopic gastrostomy in patients with cirrhosis: a case series.
Gastrointest Endosc. 2010;72(5):1072-1075.
47. Kaur S, Ceballos C, Bao R, Pittman N, Benkov K. Percutaneous endo-
scopic gastrostomy tubes in pediatric bone marrow transplant patients.
J Pediatr Gastroenterol Nutr. 2013;56(3):300-303.
48. Chung RS, Schertzer M. Pathogenesis of complications of percutane-
ous endoscopic gastrostomy: a lesson in surgical principles. Am Surg.
1990;56(3):134-137.
49. McCarter TL, Condon SC, Aguilar RC, Gibson DJ, Chen YK. Randomized
prospective trial of early versus delayed feeding after percutaneous endo-
scopic gastrostomy placement. Am J Gastroenterol. 1998;93(3):419-421.
50. Stein J, Schulte-Bockholt A, Sabin M, Keymling M. A randomized
prospective trial of immediate vs. next-day feeding after percutaneous
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
Miller et al 295
endoscopic gastrostomy in intensive care patients. Intensive Care Med.
2002;28(11):1656-1660.
51. McClave SA, Demeo MT, Delegge MH, et al. North American Summit
on aspiration in the critically ill patient: consensus statement. JPEN J
Parenter Enteral Nutr. 2002;26:S80-S85.
52. Wejda BU, Deppe H, Huchzermeyer H, Dormann AJ. PEG place-
ment in patients with ascites: a new approach. Gastrointest Endosc.
2005;61(1):178-180.
53. Hbuterne X, Vanbiervliet G. Feeding the patients with upper gastrointes-
tinal bleeding. Curr Opin Clin Nutr Metab Care. 2011;14(2):197-201.
54. Anderson MA, Ben-Menachem T, Gan SI, et al; ASGE Standards of
Practice Committee. Management of antithrombotic agents for endo-
scopic procedures. Gastrointest Endosc. 2009;70(6):1060-1070.
55. Lozoya-Gonzalez D, Pelaez-Luna M, Farca-Belsaguy A, Salceda-
Otero JC, Vazquez-Ballesteros E. Percutaneous endoscopic gastros-
tomy complication rates and compliance with the American Society for
Gastrointestinal Endoscopy guidelines for the management of antithrom-
botic therapy. JPEN J Parenteral Enteral Nutr. 2012;36(2):226-230.
56. Barton CA, McMillian WD, Osler T, et al. Anticoagulation manage-
ment around percutaneous bedside procedures: is adjustment required? J
Trauma Acute Care Surg. 2012;72(4):815-820.
57. Chaudhary KA, Smith OJ, Cuddy PG, Clarkston WK. PEG site infections:
the emergence of methicillin resistant Staphylococcus aureus as a major
pathogen. Am J Gastroenterol. 2002;97(7):1713-1716.
58. Cave DR, Robinson WR, Brotschi EA. Necrotizing fasciitis following
percutaneous endoscopic gastrostomy. Gastrointest Endosc. 1986;32(4):
294-296.
59. Martindale R, Witte M, Hodges G, Kelley J, Harris S, Andersen C.
Necrotizing fasciitis as a complication of percutaneous endoscopic gas-
trostomy. JPEN J Parenter Enteral Nutr. 1987;11(6):583-585.
60. Lipp A, Lusardi G. Systemic antimicrobial prophylaxis for per-
cutaneous endoscopic gastrostomy. Cochrane Database Syst Rev.
2006;(4):CD005571.
61. Banerjee S, Shen B, Baron TH, et al; ASGE Standards of Practice
Committee. Antibiotic prophylaxis for GI endoscopy. Gastrointest
Endosc. 2008;67(6):791-798.
62. Blomberg J, Lagergren P, Martin L, Mattsson F, Lagergren J. Novel
approach to antibiotic prophylaxis in percutaneous endoscopic gastros-
tomy (PEG): randomised controlled trial. BMJ. 2010;341:c3115.
63. Singh D, Laya AS, Vaidya OU, Ahmed SA, Bonham AJ, Clarkston WK.
Risk of bleeding after percutaneous endoscopic gastrostomy (PEG). Dig
Dis Sci. 2012;57(4):973-980.
64. Ubogu EE, Zaidat OO. Rectus sheath hematoma complicating percuta-
neous endoscopic gastrostomy. Surg Laparosc Endosc Percutan Tech.
2002;12(6):430-432.
65. Lau G, Lai SH. Fatal retroperitoneal haemorrhage: an unusual com-
plication of percutaneous endoscopic gastrostomy. Forensic Sci Int.
2001;116(1):69-75.
66. Chong C, Derigo L, Brown D. Massive gastric bleeding: a rarely seen sub-
acute complication of percutaneous endoscopic gastrostomy. Intern Med
J. 2007;37(11):787-788.
67. Richter JA, Patrie JT, Richter RP, et al. Bleeding after percutaneous endo-
scopic gastrostomy is linked to serotonin reuptake inhibitors, not aspirin
or clopidogrel. Gastrointest Endosc. 2011;74(1):22-34.e1.
68. Blomberg J, Lagergren J, Martin L, Mattsson F, Lagergren P.
Complications after percutaneous endoscopic gastrostomy in a prospec-
tive study. Scand J Gastroenterol. 2012;47(6):737-742.
69. McClave SA, Chang WK. Complications of enteral access. Gastrointest
Endosc. 2003;58(5):739-751.
70. Dulabon GR, Abrams JE, Rutherford EJ. The incidence and signifi-
cance of free air after percutaneous endoscopic gastrostomy. Am Surg.
2002;68(6):590-593.
71. Wiesen AJ, Sideridis K, Fernandes A, et al. True incidence and clinical
significance of pneumoperitoneum after PEG placement: a prospective
study. Gastrointest Endosc. 2006;64(6):886-889.
72. Sriram K, Jayanthi V, Lakshmi RG, George VS. Prophylactic locking of
enteral feeding tubes with pancreatic enzymes. JPEN J Parenter Enteral
Nutr. 1997;21(6):353-356.
73. Blacka J, Donoghue J, Sutherland M, et al. Dwell time and functional fail-
ure in percutaneous endoscopic gastrostomy tubes: a prospective random-
ized-controlled comparison between silicon polymer and polyurethane
percutaneous endoscopic gastrostomy tubes. Aliment Pharmacol Ther.
2004;20(8):875-882.
74. El-Rifai N, Michaud L, Mention K, et al. Persistence of gastrocutaneous
fistula after removal of gastrostomy tubes in children: prevalence and
associated factors. Endoscopy. 2004;36(8):700-704.
75. Gonzalez-Ojeda A, Avalos-Gonzalez J, Mucino-Hernandez MI, et al.
Fibrin glue as adjuvant treatment for gastrocutaneous fistula after gastros-
tomy tube removal. Endoscopy. 2004;36(4):337-341.
76. Hameed H, Kalim S, Khan YI. Closure of a nonhealing gastrocutanous
fistula using argon plasma coagulation and endoscopic hemoclips. Can J
Gastroenterol. 2009;23(3):217-219.
77. Teitelbaum JE, Gorcey SA, Fox VL. Combined endoscopic cautery and
clip closure of chronic gastrocutaneous fistulas. Gastrointest Endosc.
2005;62(3):432-435.
78. Peter S, Geyer M, Beglinger C. Persistent gastrocutaneous fistula after
percutaneous gastrostomy tube removal. Endoscopy. 2006;38(5):539-540.
79. Klein S, Heare BR, Soloway RD. The buried bumper syndrome: a com-
plication of percutaneous endoscopic gastrostomy. Am J Gastroenterol.
1990;85(4):448-451.
80. Rosenberger LH, Newhook T, Schirmer B, Sawyer RG. Late accidental
dislodgement of a percutaneous endoscopic gastrostomy tube: an under-
estimated burden on patients and the health care system. Surg Endosc.
2011;25(10):3307-3311.
81. Galat SA, Gerig KD, Porter JA, Slezak FA. Management of premature
removal of the percutaneous gastrostomy. Am Surg. 1990;56(11):733-
736.
82. Chaer RA, Rekkas D, Trevino J, Brown R, Espat J. Intrahepatic placement
of a PEG tube. Gastrointest Endosc. 2003;57(6):763-765.
83. Fyock CJ, Kethu SR. PEG placement causing liver perforation. J Clin
Gastroenterol. 2009;43(4):385.
84. Shaw J, Casey K. A PEG tube through the liver. Am J Gastroenterol.
2009;104(5):1323-1324.
85. Saltzberg DM, Anand K, Juvan P, Joffe I. Colocutaneous fistula: an
unusual complication of percutaneous endoscopic gastrostomy. JPEN J
Parenter Enteral Nutr. 1987;11(1):86-87.
86. Berger SA, Zarling EJ. Colocutaneous fistula following migration of PEG
tube. Gastrointest Endosc. 1991;37(1):86-88.
at UNIV FED DO RIO DE JANEIRO on March 13, 2014 pen.sagepub.com Downloaded from
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- International Journal of Nursing StudiesDokument8 SeitenInternational Journal of Nursing StudiesJos CanalesNoch keine Bewertungen
- E144 Vol. 52 No. 6 December 2016 Selected AbstractsDokument2 SeitenE144 Vol. 52 No. 6 December 2016 Selected AbstractsJos CanalesNoch keine Bewertungen
- 1 s2.0 S0020748919302093 MainDokument7 Seiten1 s2.0 S0020748919302093 MainjoscanalesNoch keine Bewertungen
- Stigma and Mental Health Challenges in Medical StudentsDokument1 SeiteStigma and Mental Health Challenges in Medical StudentsJos CanalesNoch keine Bewertungen
- BBL Sensi-Disc Antimicrobial Susceptibility Test Discs: (Testblättchen Zur Antimikrobiellen Empfindlichkeitsprüfung)Dokument8 SeitenBBL Sensi-Disc Antimicrobial Susceptibility Test Discs: (Testblättchen Zur Antimikrobiellen Empfindlichkeitsprüfung)Ivan Ro-RoNoch keine Bewertungen
- The Eff Ect of Iron Overload On Red Blood Cell MorphologyDokument1 SeiteThe Eff Ect of Iron Overload On Red Blood Cell MorphologyJos CanalesNoch keine Bewertungen
- APT 13,38,1156 Evidence Based Dietary Advice For Patients With Inflammatory Bowel Disease (EII) (NE) (NPT)Dokument16 SeitenAPT 13,38,1156 Evidence Based Dietary Advice For Patients With Inflammatory Bowel Disease (EII) (NE) (NPT)Jos CanalesNoch keine Bewertungen
- Metabolic and Body Composition Factors in Subgroups of Obesity: What Do We Know?Dokument7 SeitenMetabolic and Body Composition Factors in Subgroups of Obesity: What Do We Know?Jos CanalesNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Case Study On DehydrationDokument4 SeitenCase Study On DehydrationDustin Dela CruzNoch keine Bewertungen
- Antenatal CareDokument23 SeitenAntenatal Caremalaika khanNoch keine Bewertungen
- Nadira Duwi 3191028 Naufal HafidDokument61 SeitenNadira Duwi 3191028 Naufal HafidNadira RaraNoch keine Bewertungen
- Seminar Conduction System of HeartDokument61 SeitenSeminar Conduction System of HeartKirtishAcharyaNoch keine Bewertungen
- Pharmaceutical Assasination (Partial)Dokument14 SeitenPharmaceutical Assasination (Partial)jamie_clark_2100% (2)
- DRUG STUDY Setera Case 8Dokument10 SeitenDRUG STUDY Setera Case 8Ceria Dorena Fe SeteraNoch keine Bewertungen
- LipaseDokument28 SeitenLipaseshar12100% (1)
- Cognitive-Behavioral Therapy For ADHD in Adolescents Clinical ConsiderationsDokument11 SeitenCognitive-Behavioral Therapy For ADHD in Adolescents Clinical Considerationsdmsds100% (1)
- Subject - Obstetrics and Gynecology Batch - BBA (HA) IV Sem. Submit To - Dr. Jyoti Joshi Ma'am Submit by - Shivam Rajput & Umesh ChoyalDokument19 SeitenSubject - Obstetrics and Gynecology Batch - BBA (HA) IV Sem. Submit To - Dr. Jyoti Joshi Ma'am Submit by - Shivam Rajput & Umesh ChoyaldevNoch keine Bewertungen
- EBUS Kazuhiro YasufukuDokument27 SeitenEBUS Kazuhiro YasufukuOrion JohnNoch keine Bewertungen
- Recent Advances in Diagnosis, Treatment and Prevention of Hepatocellular Carcinoma (HCC)Dokument65 SeitenRecent Advances in Diagnosis, Treatment and Prevention of Hepatocellular Carcinoma (HCC)amal.fathullahNoch keine Bewertungen
- 1.Dr - Haerani Rasyid-Simposium Prinsip Terapi Nutrisi DialisisDokument41 Seiten1.Dr - Haerani Rasyid-Simposium Prinsip Terapi Nutrisi DialisisZaza ZunitaNoch keine Bewertungen
- Surgery History and PhysicalDokument23 SeitenSurgery History and PhysicalBilal RowaihiNoch keine Bewertungen
- TRS 987Dokument286 SeitenTRS 987NGOTTANoch keine Bewertungen
- Manual Muscle Test (MMT) : Ajith C Student of Department of Physio Kmch-CoptDokument80 SeitenManual Muscle Test (MMT) : Ajith C Student of Department of Physio Kmch-Coptayesha solNoch keine Bewertungen
- Abstract Leftsidest SetDokument1.047 SeitenAbstract Leftsidest Setpokharelriwaj82Noch keine Bewertungen
- Antenatal Care Draft Assessment Tool2Dokument14 SeitenAntenatal Care Draft Assessment Tool2Vin BitzNoch keine Bewertungen
- Post Graduate Diploma in Clinical Cardiology (PGDCC) : Mcc-004: Common Cardio-Vascular Diseases - IiDokument8 SeitenPost Graduate Diploma in Clinical Cardiology (PGDCC) : Mcc-004: Common Cardio-Vascular Diseases - IiBoda JyothiNoch keine Bewertungen
- Ultrasonography of The EyeDokument8 SeitenUltrasonography of The Eyetaner_soysurenNoch keine Bewertungen
- Literature ReviewDokument11 SeitenLiterature Reviewapi-691127747Noch keine Bewertungen
- Amniotic Fluid EmbolismDokument13 SeitenAmniotic Fluid EmbolismMARIANN JEAN ANDREA CULANAG MATALINESNoch keine Bewertungen
- Immunology Review For FPGEEDokument8 SeitenImmunology Review For FPGEEMina MinawyNoch keine Bewertungen
- 88 FinalDokument4 Seiten88 FinalEshiebel OrganistaNoch keine Bewertungen
- Primitive ReflexesDokument10 SeitenPrimitive Reflexesbun_yulianaNoch keine Bewertungen
- Focus On Adult Health Medical Surgical Nursing Pellico Edition Test BankDokument8 SeitenFocus On Adult Health Medical Surgical Nursing Pellico Edition Test BankCarolineAndersoneacmg100% (33)
- Kebutuhsn Implan Urologi Desember 2021 - November 2022 - 3Dokument32 SeitenKebutuhsn Implan Urologi Desember 2021 - November 2022 - 3Ilham ApriansyahNoch keine Bewertungen
- Gait AnalysisDokument2 SeitenGait AnalysisIvin KuriakoseNoch keine Bewertungen
- Renal Dosing Protocol - Renal Dosing ProtocolDokument3 SeitenRenal Dosing Protocol - Renal Dosing Protocoldjwa163Noch keine Bewertungen
- Nama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, DemamDokument52 SeitenNama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, Demamrio1995Noch keine Bewertungen
- Introduction To Language and Linguistics BIT10703 Ahmad Taufik Hidayah Bin AbdullahDokument5 SeitenIntroduction To Language and Linguistics BIT10703 Ahmad Taufik Hidayah Bin AbdullahMuhammad Ikhwan RosmanNoch keine Bewertungen