Beruflich Dokumente
Kultur Dokumente
Gunshot Wounds To Face
Hochgeladen von
Khadim ShahOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Gunshot Wounds To Face
Hochgeladen von
Khadim ShahCopyright:
Verfügbare Formate
Gunshot Injuries:
Management of gunshot injuries to the face led in many ways to the development of modern maxillofacial
surgery, and it remains a cornerstone of the specialty of oral and maxillofacial surgery.
Ballistics:
Ballistics is the science of projectile motion.
A prerequisite to understanding the injuries caused by various firearms is knowledge of the language of
ballistics. The potential problems of a wound caused by a projectile can be better anticipated if one has some
knowledge of the weapon and projectile type that caused the wound.
Ballistic science seeks to explain the behavior of the projectile and is typically divided into three stages:
1. Internal (or interior) ballistics describes the forces that apply to a projectile from the time the propellant is
ignited to the time the projectile leaves the barrel. An important consideration is barrel length. In general,
longer barrels (rifles) allow the force of the propellant to act on the projectile longer and generate higher
velocities than do shorter-barreled weapons. In addition, a longer barrel serves to stabilize the bullet over
longer distances.
2. External ballistics refers to forces that act on the bullet in flight. The primary factors that govern external
ballistics are the weight and shape of the bullet.
3. Terminal ballistics is the study of bullet behavior once it impacts the target and is primarily concerned with
how much energy is transferred to the target material and the resultant damage. The science of terminal
ballistics is most important to the surgeon and is the most common source of controversy when discussing
ballistic wounding.
Attempts to reproduce the interaction of bullets with living tissue by using various target media such as
ballistic gel have led to many myths surrounding wounding and the stopping power of various bullets and
weapons. Similarly, surgeons have passed on many myths of their own regarding GSWs and the firearms that
cause them.
Classification Schemes
Classification of traumatic injuries is helpful in guiding treatment and, more importantly, tracking outcomes
for various treatment modalities. A number of trauma scoring systems and classifications for various injuries
have been developed and validated. Similarly, attempts have been made to classify GSWs to assist the surgeon
in selecting appropriate management strategies. Many of these classification schemes were developed on the
battlefield. Dissimilarities between civilian and military gunshot injuries, such as ammunition, wounding
potential of military weapons, and treatment objectives, make these classification schemes of little use in the
urban trauma center, which most commonly deals with low- to medium-velocity handgun injuries. Trauma
systems have attempted to incorporate gunshot injuries into existing classification and trauma scoring
systems. Unfortunately, current schemes have not proven beneficial in guiding treatment and judging
outcomes to develop ideal approaches. Attempts to distinguish GSWs as low or high velocity have suffered
from the shortcomings noted above. In addition, velocity is less critical than bullet type, mass, distance to
target, and specific vital organs involved because most civilian injuries are caused by low- or mediumvelocity
weapons.
One of the earliest and simplest classification schemes classifies GSWs as nonpenetrating (grazing or blast
wound), penetrating (bullet does not exit), perforating (in and out), and avulsive. The International Committee
of the Red Cross introduced the armed conflict classification system to improve information gathering and
communication regarding war wounds. Because of the diversity of battlefield weaponry, by necessity the
system ignores weapon type and instead concentrates on wound severity in terms of tissue damage and
anatomic structures involved. Gugala and Lindsey suggested a civilian gunshot injury classification scheme. It
takes into account energy (high or low), involvement of vital structures (neural and vascular), wound type
(nonpenetrating, penetrating, perforating), fracture (intra-articular and extra-articular), and contamination.
Primarily used in orthopedics, its usefulness in gunshot injuries to the head and neck is limited.
Shotgun Wounds
Because of their unique ballistic profile, shotgun injuries are often classified based on the distance to the
target. Shotgun pellets have significant aerodynamic resistance and give up substantial amounts of kinetic
energy during flight. In type I shotgun injuries (< 5 m), the pellets strike the target as a single mass, resulting
in massive kinetic energy transfer, tissue avulsion, and a high mortality rate (8590%). Patients that survive
suicide attempts with shotguns typically survive because, in an attempt to reach the trigger with the muzzle
under the chin or in the mouth, the head is hyperextended, which causes the pellets to create devastating
injuries to the face but avoid the cranium. Fragments of paper or plastic wadding may be found in the wound.
Type II injuries (512 m) usually result in much less tissue destruction. At these distances there is significant
dispersal of the pellets and loss of energy. Penetration may occur through deep fascia, but fractures are rare.
Ocular injuries can occur as well as embolization of lead pellets, but mortality is less (1520%). At distances >
12 m (type III), usually only the skin is penetrated and mortality is rare (05%). Because specific information
on shooting distances is not often available to the clinician, a system was suggested that evaluated the
maximum distance of pellet scatter. Type I injuries had > 25 cm of pellet scatter. Type II injuries had 10 to 25
cm of scatter. Type III injuries had < 10 cm of scatter and would roughly correspond to a type I injury in the
classification of Sherman and Parrish.24
This classification scheme was developed and applied to abdominal shotgun wounds in an attempt to guide
therapy.26 Again, the difficulty lies in applying this scheme, or any scheme, universally to GSWs involving
different anatomic sites and weapon types. It should be noted that rifle and shotgun injuries, although rare in
assaults, are frequently encountered in attempted suicide patients. A characteristic wound profile is seen
because of the head position assumed when the patient places the barrel of the weapon in the mouth or under
the chin and subsequently hyperextends to reach the trigger. Characteristic powder burns are seen at the
entrance wound. The face frequently takes the full effect of the blast, whereas lethal intracranial involvement
is avoided. If a high energy weapon such as a shotgun or rifle is used, the injury can be devastating with
significant tissue loss. Although classification schemes can serve useful purposes in research as well as clinical
practice, strict adherence to treatment algorithms based on wound classification can lead to mismanagement.
Importantly, information regarding types of firearm and other details of the shooting are frequently not
available, and clinical assessment of the wound remains the most reliable method for determining treatment
approaches.
Management
General Principles
On admission victims of gunshot injuries are best managed by standard advanced trauma life support (ATLS)
protocols. Even seemingly innocuous wounds deserve attention, given the erratic nature of the wounds.
Specific attention must be given to the possibility of multiple injuries; it is imperative to thoroughly inspect
the patient for multiple entrance and exit wounds. Visually disturbing but nonlife-threatening facial gunshot
injuries can distract medical personnel from other more subtle lethal injuries such as a penetrating thoracic
wound that entered through the back. Ophthalmologic and neurosurgical consultations are obtained when
indicated. Approximately 17% of patients with a GSW to the face have associated brain injuries, and 8% have
associated C-spine injuries. Eye injuries are present in approximately 13%. Certain considerations for gunshot
injuries should be emphasized.
Airway
Loss of the airway is the single most likely cause of death in an isolated GSW to the face. When confronted
with a patient with a facial GSW, surgeons should have a low threshold for establishing a definitive airway
through intubation or a surgical airway if intubation is not possible. Intubation either in the field or the
emergency department is required in 25 to 36% of patients. Wounds involving the mandible have the highest
rate of intubation (3753%), followed by those of the midface (1836%). Excluding patients that require
airway control for associated brain injuries, Demetriades and colleagues found that 17.4% of patients
required urgent airway control for facial injuries. Gunshot injuries to the neck may result in tracheal damage
and require an emergent surgical airway (cricothyroidotomy). Intubation with fiber-optic assistance is
possible, but paralytics should be avoided owing to the risk of expanding hematomas or massive edema.
Cricothyroidotomy or an awake tracheostomy is more appropriate in this setting. The need to convert an
intubated airway to a tracheostomy depends on several factors. Tracheostomy can make repair of injuries
involving the mandible and midface easier. Patients who will require multiple return trips to the operating
room for wound dbridements and second looks will benefit from the decreased risk of multiple intubations.
Delayed swelling can be anticipated with trauma to the upper aerodigestive tract including the tongue; this
may influence the decision to proceed with tracheostomy. Associated tracheal injuries are another indication
for tracheostomy. Lastly, multiple system injuries with anticipated long-term ventilation is an indication for
early tracheostomy. Most experienced surgeons would agree that it is rare to regret having performed a
tracheostomy, but tragic to regret not performing one.
Hemorrhage Control
Life-threatening hemorrhage is unusual in civilian gunshot injuries. Low-velocity handgun injuries typically
do not involve the great vessels. Demetriades and colleagues in Los Angeles reported only 7.5% of patients
with isolated gunshot wounds to the face to be in shock upon admission (systolic blood pressure < 90 mm
Hg). In their report 70 patients (28.3% of the total) required angiography, and 10 of these required
embolization. Overall the literature reports angiography in 17 to 63% of patients with a GSW to the face, with
positive findings in 15 to 51%. Indications for angiography include expanding hematoma and bleeding that
persists despite local measures. The most commonly involved vessels in these cases were the maxillary and
facial arteries. Gunshot injuries associated with high-velocity weapons or fractures, however, can result in
significant blood loss. Initial attempts to control hemorrhage in the emergency department center on direct
pressure and packing. Blind clamping should be avoided because of the attendant risk of damage to other
structures. Standard methods for epistaxis control such as Foley catheters or specially designed balloon
catheters will control most midface bleeding. In cases of mandible fractures, temporary reduction of the
fracture may be required. Penetrating injuries can require that the surgeon make difficult choices. Injuries at
the skull base may benefit from angiography and embolization.
Unfortunately, the time necessary to mobilize the angiography suite often makes this an impossible choice for
the unstable trauma patient in the middle of the night. For this reason, control of life-threatening hemorrhage
is typically best performed in the operating room. Ligation of multiple vessels is required. Tying off the
carotid is usually ineffectual and dangerous; an attempt should be made to control specific vessels. Lacerations
of the internal jugular artery are best controlled with ligation or repair. Packing and reduction of fractures
should be performed to control bleeding from the midface if possible. There is possibility of late
pseudoaneurysm formation and delayed hemorrhage, and selective angiography should be performed as
indicated. Additionally, the possibility of bullet or fragment embolization should be considered.
Penetrating Neck Injuries
Gunshot wounds involving the face may be associated with an entrance or exit wound in the neck, which is
divided into three zones originally described by Monson and colleagues from Cook County Hospital34:
Zone I is most commonly defined as the area from the clavicles to the cricoid cartilage. It contains the
inferior aspect of the trachea and esophagus along with the major vessels of the thoracic inlet: the common
carotid arteries, thyrocervical trunk, internal jugular veins, brachiocephalic trunk, subclavian arteries and
veins, thoracic duct, thyroid gland, and spinal cord.
Risk of injury to the great vessels is common in this area, and, consequently, injuries to zone I carry a high
mortality rate (approximately 12%). Some authors place the junction of zones I and II at the cricoid cartilage,
whereas others define it as being at the top of the clavicles.
Zone II represents the area from the cricoid cartilage to the angle of the mandible. It contains the common
carotid arteries, internal and external carotid arteries, internal jugular veins, larynx, hypopharynx, and cra-
nial nerves X, XI, and XII. It is the largest area and therefore the most commonly involved zone in penetrating
neck trauma.
Zone III spans the region from the skull base to the angle of the mandible.
It contains the carotid arteries, the internal jugular veins, and the pharynx along with multiple cranial nerves
exiting the skull base. It should be appreciated that gunshot wounds that involve mandibular fractures are
accompanied by injuries to zone III.
Van As and colleagues reported on 116 patients shot in the neck in South Africa. Of these, 70 suffered a direct
hit to the neck; in 46 patients the bullet traversed the face or chest first. Of the 116 patients 85 suffered some
vascular injury, although most were minor branches, 61 had some injury to the airway, and 32 had an injury
to the pharynx or esophagus. Many patients had more than one injury. Management strategies for
penetrating neck injuries are typically based on the zone(s) involved. Gunshot wounds to the head and neck
frequently involve projectiles that traverse or involve more than one zone. For this reason, surgeons may have
to modify management plans based on the situation at hand. Although a complete discussion of penetrating
neck trauma is beyond the scope of this chapter, general principles should be understood by surgeons
managing facial gunshot injuries.
Initially the patients stability from an airway and hemodynamic status guides the decision-making for
penetrating neck injuries. In the stable patient, a complete examination is part of the secondary survey of
ATLS. Signs of tracheal injury, such as subcutaneous emphysema, stridor, hoarseness, dysphonia, or
hemoptysis require urgent intervention. Hard signs of vascular injury, such as expanding hematoma, and
pulse or neurologic deficit, also signal the need for urgent management. In the absence of urgent
management needs, the surgeon must rule out occult injuries based on the zones involved.
Injuries to zone I can be associated with significant bleeding because of the large vessels in this area. This is
especially true with regard to injuries caused by highenergy weapons. Although serving to protect the vessels,
the clavicles are a hindrance to the application of direct pressure to the area and to rapid surgical exposure.
In the stable patient most surgeons advocate routine angiography and an evaluation of the esophagus via rigid
esophagoscopy or a barium swallow. The choice between barium swallow and esophagoscopy varies
according to the surgeons preference as both are reasonably accurate at diagnosing injury (90% and 86%,
respectively). In addition, there is some controversy regarding the appropriate contrast media.
Although meglumine diatrizoate causes less inflammatory response than does barium when it extravasates
into tissues owing to an esophageal perforation, it results in a severe chemical pneumonitis if aspirated.
For this reason, barium should be used if there is any impairment to the gag and cough reflexes; if there is a
leak, early operative intervention allows it to be washed out during surgery. Penetrating injuries to the left
neck, and rarely to the right, can result in a chyle leak. The surgeon should take care to exclude this at the
initial exploration, if possible, and to repair it by oversewing the duct with local tissues. It is useful to have the
anesthesiologist apply positive pressure and to place the patient in Trendelenburgs position.
Delayed management is much more difficult after the tissues have been exposed to chyle. Conservative
management with a diet of medium-chain triglycerides, which are not carried by the gut lymphatics, and
drainage should be attempted initially if the leak presents in the postoperative setting.
Exploration is indicated for leaks of > 400 to 500 cc/d for a week.
Penetrating injuries to zone II are the most common and are most amenable to surgical exploration, if
warranted. For asymptomatic patients, computed tomographic angiography is becoming an important tool for
screening and can assist in determining whether operative exploration is warranted. Patients can undergo
serial examinations over 24 hours if the angiography results are negative. Computed tomographic
angiography is faster and less invasive than angiography but is of lower specificity. It should also be noted
that injuries that have tamponaded themselves can be missed on either.
Some surgeons recommend the use of a barium swallow or rigid esophagoscopy, whereas others recommend
observation only if the index of suspicion for injury is low, as with wounds from low-energy guns. If patients
have associated mandible fractures, the neck can be explored while the mandible fractures are exposed for
fixation. Imaging is required in zone III injuries if the patient is stable. Diagnosis of vascular injuries at the
skull base typically requires angiography,which can also allow intervention if indicated. Injuries to zone III
are rarely amenable to surgical intervention. Overall, angiography remains the gold standard for exploration
of vascular injuries of the neck. In Van As and colleagues report, 89 patients underwent angiography for
GSWs to the neck; results were positive in 12 patients, with most lesions occurring in the common carotid
followed by the internal and external carotids (3 cases each), the vertebral artery (2 cases), and the subclavian
artery (1 case). Currently ultrasonography is gaining popularity as a rapid noninvasive technique for the
evaluation of a variety of traumatic injuries in the emergency department. Ginzburg and colleagues evaluated
the usefulness of duplex ultrasonography to evaluate vascular injuries in a double-blind study using
angiography as a control. They reported a 100% true-negative rate, 100% sensitivity, and 85% specificity in
detection of arterial injury. Ultrasonography will most likely continue to grow in popularity as a screening
tool because of its cost and the speed at which it can be performed. Further improvements in noninvasive
vascular evaluation techniques, such as helical computed tomographic angiography and ultrasonography,
will reduce the number of patients undergoing traditional angiography and improve patient selection for
nonoperative management.
Nutrition
The majority of civilian gunshot wounds affect young healthy males. Nutritional status becomes an issue only
in patients whose injuries preclude oral alimentation for an extended period (> 4 or 5 d). Feeding via
nasogastric intubation allows bypass of the oral cavity and improved hygiene in the early days following
injury. Consideration should be given to percutaneous endoscopic gastrostomy if long term bypass of the oral
cavity is necessary, the patient will be unable to eat, or the patient has a preexisting nutritional deficit.
Imaging
Following the ATLS protocol, standard C spine and chest radiographs should be obtained. These can be
valuable for visualizing the bullet fragments and in gaining some insight into the path of the bullet. It is
important to recall, however, that projectiles rarely follow a straight path once they enter tissue. The ability to
obtain accurate three dimensional images in a rapid fashion has been one of the most important advances in
dealing with gunshot injuries to the face. Spiral computed tomography combined with three-dimensional
reconstructions allows the surgeon an unparalleled view of the extent of damage to the maxillofacial skeleton,
which lies beneath the skin. Although it does not accurately demonstrate the amount of soft tissue damage,
clinical inspection combined with three-dimensional imaging allows an accurate assessment. As discussed
previously, the importance of temporary cavitation and emphasis on the amount of devitalized tissue distant
from the primary wound has probably been overstated in the past. Computed tomographic angiography can
also be useful in certain situations for evaluating vascular damage, especially in cases of penetrating neck
injuries. It should be remembered, however, that angiography remains the gold standard to evaluate the
vasculature. Also, angiography allows the ability to intervene with embolization of active bleeding vessels that
are difficult to approach surgically. Patients who are not sufficiently stable for imaging should be stabilized in
the operating room, and definitive repair should be deferred until appropriate imaging can be obtained.
Operative Procedure
Paralleling the evolution of firearms has been development in the management of gunshot injuries to the head
and neck. The earliest surgeons dealing with gunshot injuries blamed complications on gunpowder that
would later be ascribed to contamination and infections. The mystique that surrounded gunshot injuries
persists in some ways to modern times in surgical dogma that is passed down. During World
War I, high-energy close-range gunshot and shrapnel wounds to the face necessitated the development of
maxillofacial surgery.
Kazanjian and Converse described their approach to gunshot wounds as three phases consisting of initial
dbridement and suturing, immobilization of bony fragments with splints and ligatures, and, finally,
reconstruction following healing of the soft tissue.39 Many of the principles developed at that time persist
today, with surgeons advocating a phased approach with delayed closure of wounds, dbridement of tissue,
and secondary reconstruction. Many surgeons still advocate closed reduction and division of care into early
(first 10 d), intermediate (1060 d), and late (> 60 d) phases. The different nature of civilian gunshot wounds
and improved management techniques have led to a reappraisal of staged approaches, and current
management principles should more properly be considered a continuum that is based on the wound and
patient profile. The successful application of rigid fixation principles to blunt traumatic injuries resulted in
incorporation of these techniques to gunshot injuries. Early surgeons understood the importance of
immobilization on the healing of GSWs but lacked the ability to truly immobilize bony structures of the face.
The development of rigid fixation techniques and their application to GSWs was an important advance. Early
concerns regarding placement of hardware into contaminated sites proved unfounded. By allowing the early
stabilization of bone segments, percolation of contaminated oral fluids was prevented, primary bone healing
was made possible, and the effects of scar contracture were minimized. This has led most surgeons to advocate
early definitive repair of the majority of civilian gunshot wounds, which generally are inflicted with low-
velocity weapons.
An operative plan for a gunshot injury to the face is best formulated after characterization of the wound as
low or high energy. The surgeon facing a gunshot injury should consider the concept introduced by Manson
for evaluation of four components: soft tissue injury, bone injury, soft tissues loss (true avulsion), and bone
loss. After evaluation of the wound, a decision is made regarding early definitive repair versus the need for
delayed repair. The majority of civilian gunshot wounds resulting from assaults can be managed with early
definitive repair because these injuries usually result in injury to the soft tissue and bone but rarely loss of
these tissues. Impressive soft tissue injuries are usually not avulsive, and most can be closed primarily.
Extensive dbridement of soft tissue is not indicated.
Wound debris should be removed, and wounds should be lavaged with normal saline. Antibiotic solutions
such as saline and bacitracin (50,000 U/L) have not been shown to be more effective than normal saline but
are still popular. A pulsating irrigator is useful to mechanically agitate debris from the tissue.Obvious
devitalized and loose teeth should be removed. Fractures are reduced and fixed rigidly. Otherwise, teeth
should be maintained if possible to aid in restoration of occlusion and proper jaw relations. Drains are often
indicated; whether closed suction or Penrose is used depends on the wound. Pressure dressings can also be
used to minimize dead space. In cases of true soft tissue avulsion, a decision must be made regarding whether
primary flaps or grafting is indicated. In wounds that are relatively clean, local flaps and skin grafts may be
appropriate. In grossly contaminated wounds, delayed closure or grafting may be necessary. Closing mucosa
to skin can be a useful technique, but many cases can be managed with dressing changes and incorporation of
an early flap procedure. Free tissue transfer, although useful, should be delayed until the initial phase of
wound healing, when its accompanying vascular spasm and attendant hypercoagulable state has decreased.
In wounds with extensive soft and hard tissue damage and true loss of soft and hard tissue, an approach using
early stabilization of bone fragments with maxillomandibular fixation, external fixation, or internal fixation
with reconstruction plates combined with conservative management of soft tissue is indicated. In this era of
rigid internal fixation, the utility of maxillomandibular fixation should not be overlooked. In addition,
external fixation devices are still useful in select cases. Second-look operations with conservative wound
washouts and dbridement of only obviously dead tissue, which have gained popularity in orthopedics, have
great utility in injuries to the maxillofacial skeleton. Second dbridements should be performed 24 to 48
hours after the initial surgery. This allows for the maintenance of tissue considered borderline, which can be
excised if it truly becomes devitalized. Skin grafts can be used as permanent or temporary replacement for
missing tissue to reduce deformity from scar contracture. Once the soft tissues have stabilized, a decision can
be made regarding early replacement of lost tissues with free tissue transfer or delayed reconstruction. In
general, earlier repair leads to improved outcomes with less scar contracture and resultant deformity. Bone
grafts at the time of initial surgery may be indicated in the midface. Again, management strategies should be
considered a continuum that is modified as necessary rather than strict distinct stages.
Contamination
It should be remembered that projectiles from firearms are not sterile. This fact is well known to those who
have dipped their bullets in feces prior to assassination attempts but lost on clinicians who have taught that
gunshot wounds are indeed sterile. The heat generated by the discharge of the propellant as well as the
friction between the bullet and barrel is not sufficient to sterilize the bullet. Contamination can occur from
the bullet and also from skin flora and foreign bodies (clothing) carried into the wound. Historically,
streptococcal bacteremia was the most important cause of death on the battlefield in the preantibiotic era.
Wounds in which the bullet traverses the aerodigestive tract or paranasal sinuses are at particular risk.
Devitalized tissue and vascular congestion leads to an ideal environment for bacterial growth. Prophylactic
coverage with broad-spectrum antibiotics, typically a second-generation cephalosporin, and tetanus
prophylaxis, when indicated, should be initiated in all gunshot wounds.
Extensive surgical dbridement is rarely indicated in wounds consistent with low velocity projectiles to
prevent infection. Removal of projectiles, a well-worn tradition in Hollywood, is less commonly indicated in
reality. The need for the removal of bullets must be balanced against the real risk of increasing damage.
Lead toxicity is a rare complication that does not typically justify the routine removal of bullet fragments.
Removal of intra-articular bullet fragments should be considered when the increased risk of lead toxicity is
associated with fragments within joint spaces and the potential for long term deterioration of the joint.48
Finally, consideration may be given to the removal of brass- or copper-jacketed bullets that are in close
proximity to central or major peripheral nerves because of potential neurotoxicity. It is important to
remember that bullet fragments are potential evidence and an appropriate chain of custody is required. Most
hospitals have a protocol in place to ensure that this chain is unbroken from the time they are retrieved to
when they are logged in as evidence. This usually involves a police officer or other designee taking direct
possession of the bullet or fragments in the operating room or nearby. Documentation of injuries with
photographs can aid in reconstructing the events leading to the injury and recording where fragments were
retrieved. Since some assaults have injury patterns similar to suicides, it is important to consider this chain of
custody because subsequent investigations may reveal that an apparent suicide was actually an assault.
Specialized Structures
Facial Nerve
Damage to the facial nerve is present in only 3 to 6% of civilian GSWs to the face. This is most likely because
low energy weapons are involved in most of these cases. However, such damage is not uncommon in injuries
inflicted by higher velocity firearms. Careful documentation at the earliest possible opportunity is important.
If a functioning nerve becomes nonfunctional secondary to swelling, the surgeon can be reasonably confident
that function will return. Obvious transection of the nerve requires repair. In heavily contaminated wounds,
repair should be delayed for 48 to 72 hours, given the possibility that grafts will be required to span damaged
segments. Beyond 72 hours distal branches of the facial nerve will not respond to a nerve stimulator, making
their identification difficult. If possible, tagging the branches with suture at the initial surgery is invaluable.
Extensive damage to the proximal nerve may require a temporal bone dissection to identify a viable proximal
nerve for grafting.
Injuries distal to a line dropped vertically from the lateral canthus (zone of arborization) do not typically
require repair because of the multiple interconnections distal to this line and the reasonable expectation of
return of function, even if the nerve is temporarily nonfunctioning.
Salivary Ducts
Transected salivary ducts may be repaired or ligated depending on the amount of damage. The parotid duct
can be repaired over an intravenous catheter or polymeric silicone tubing, which is then sutured to the buccal
mucosa. It is best to avoid bringing the tubing out of the mouth because of the tendency for it to be dislodged.
In injuries that penetrate the parotid-masseteric fascia, there is a potential for development of a sialocele or
fistula. These typically resolve with drainage and pressure dressings. Aspiration may be required multiple
times, and, rarely, antisialagogues may be indicated. In addition, removal of any associated foreign bodies may
be necessary to resolve the fistula and hasten healing. Dermal grafts can be used at the time of repair.
Controversies: Delayed versus Early Management and Closed versus Open Fracture Management
Proponents exist both for closed management of fractures with delayed reconstruction as well as aggressive
early management with open reduction of fractures and replacement of missing tissue as soon as possible.
Both groups point to failures and shortcomings of the other to justify their approach. Advocates of delayed
repair point to a higher incidence of infection and to benefits of closed treatment, whereas those advocating
more aggressive management report improved functional and esthetic outcomes. Since neither approach is
likely to ever be subjected to a randomized trial measuring outcomes, surgeons must base their treatment
decisions on a critical review of the literature and their own experience. As with most arguments in surgical
science, the truth most likely lies somewhere in the middle. Certainly the advantages of aggressive early
management are appealing.
Early return to function and decreased numbers of revision surgeries are laudable goals. Currently techniques
involving open reduction and fixation of fractures resulting from GSWs seem to be gaining in popularity, and
patients are less likely to be treated with closed reduction. Given that most of these injuries are low energy,
this is acceptable. The main disadvantage of open reduction is infection, which primarily affects the mandible.
The reported rate of infection with open reduction and fixation of mandible fractures resulting from a
gunshot is around 16 to 17%.54 However, rigid fixation can frequently be maintained in the event of wound
problems and still serves to stabilize mandibular segments.
Surgeons should avoid the application of a set protocol to every GSW situation and should instead rely on a
careful appraisal of the wound and decide on the amount of early repair that is indicated.
Bone Grafting
Bone grafts are frequently required in the management of GSWs to the face, whether for replacement of true
loss of bone (avulsive injuries) or in cases in which comminuted and misplaced fragments need to be replaced
or reinforced. Reconstruction with bone grafts gained popularity in World War I, and much of what we know
about the healing of free bone grafts was learned following their introduction for late reconstruction of
gunshot injuries in wartime. Iliac bone grafts were popular for late reconstruction.
Surgical dogma was against early or primary bone grafting and stipulated waiting until soft tissue healing
had occurred. More recently the use of bone grafts in the early setting has gained popularity. Gruss and
colleagues have published extensively on their success with early bone grafting to stabilize and support soft
tissues, and to decrease scar contracture and distortion. The use of cranial bone in blunt injuries was extended
to include GSWs with some success. Currently many surgeons advocate the use of primary bone grafting in
the midface. Some surgeons also advocate immediate bone grafting of mandible defects. Most agree, however,
that delayed grafting of discontinuity defects of the mandible is still indicated because of the high risk of
exposure and loss of bone grafts in this site, and that immediate grafting in the mandible should be avoided.
Clark and colleagues reported a 35% incidence of wound complications in patients undergoing immediate
reconstruction of significantly comminuted mandible fractures resulting from GSWs. Conversely, primary
bone grafting was uniformly successful in the cranium and midface.
Rigid fixation maintains the mandibular segments. Even if the titanium plate becomes exposed, wound care
will allow it to be maintained until definitive reconstruction. In summary, primary bone grafting in the early
phase of gunshot wound management can be useful, but it should be limited to the upper and midface.
Maintenance of mandibular segments with rigid reconstruction plates combined with delayed grafting or free
flap reconstruction offers a predictable result, and in most cases primary grafting of the mandible is not
indicated.
Late Reconstruction
Delayed bone reconstructions frequently suffer from a scarred hypovascular environment that does not
support the graft. In addition, there is typically a deficiency in soft tissue that becomes more pronounced
when wounds are opened. In these cases vascularized tissue transfer offers the ability to import soft tissue
and/or bone into the site. As noted previously, free tissue transfer is usually delayed until after the acute
setting to decrease the incidence of flap loss secondary to clotting of the vascular pedicle. Preoperative
angiography often is beneficial to identify appropriate vessels in the neck. Vascularized bone grafts can
support osseointegrated implants to complete the reconstruction. Anthony and colleagues reported on the use
of the fibula in patients in whom previous reconstructive attempts for gunshot injuries had failed.
Both cases involved secondary reconstructions. Some surgeons have advocated delayed reconstruction in
gunshot wounds that resulted from suicide attempts because of the potential for repeat suicide attempts,
arguing that there is a high rate of recidivism and that patients should be stabilized psychologically for some
period of time prior to undertaking an extensive (and expensive) reconstructive effort.
However, Cusick and colleagues found an incidence of only 8% confirmed mortality in the follow-up of 91
patients who had attempted suicide. All were patients who had long-standing chronic mental illness.
De Leo and colleagues found a higher rate in an elderly European population. In a 1-year follow-up, they
found 24% had attempted suicide again, with approximately half being successful in their second attempt.
With modern techniques, however, primary reconstruction has become more attractive in most patients who
have self-inflicted gunshot wounds. It should be noted, however, that some authors still recommend delayed
reconstructive efforts. Siberchicot and colleagues reviewed 165 patients with selfinflicted gunshot injuries
between 1982 and 1996 and suggested that delayed definitive reconstruction was more likely to achieve
satisfactory results in appearance and function.
Conclusions
The development of firearms heralded a new era in surgery as well as warfare. Evolution of more efficient
weapons continues to force surgeons to improve techniques.
Similarly, improvement in the management of GSWs to the face has paralleled the advancement of oral and
maxillofacial surgery. Advances by Varaztad Kazanjian, the miracle man of the Western front during World
War I, continued through the wars of the twentieth century.
Improvements in casualty management and triage in the Korean and Vietnam conflicts led to increased
survival of those with devastating facial injuries. Techniques and skills developed by oral and maxillofacial
surgeons in the management of these injuries translated directly to other areas such as bone grafting, and
promoted the growth and expanding scope of the specialty. These efforts are continued today in urban trauma
centers dealing with gunshot injuries to the face.
Improvements in imaging and fixation techniques have resulted in an evolution in management, with an
emphasis on earlier repair and a focus on improvement in quality of life.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
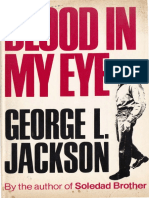
- Jackson, George - Blood in My Eye PDFDokument219 SeitenJackson, George - Blood in My Eye PDFregan100% (7)
- Pamphlet The Invisible House of Rothschild by Zahirebrahim PDFDokument70 SeitenPamphlet The Invisible House of Rothschild by Zahirebrahim PDFpkemalss50% (2)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- High Yield EmbryologyDokument49 SeitenHigh Yield EmbryologyKhadim Shah0% (5)
- Project Manequin and Underground Bases PDFDokument92 SeitenProject Manequin and Underground Bases PDFArizonaMilitia100% (1)
- Cyberpunk 2020 - Advanced Hit Location SheetDokument1 SeiteCyberpunk 2020 - Advanced Hit Location Sheetcp_jail100% (7)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- 1000 MCQ Bank QuestionsDokument157 Seiten1000 MCQ Bank Questionsapi-2629165193% (59)
- The Best of Greyhawk PresentsDokument22 SeitenThe Best of Greyhawk PresentsElijah FlemingNoch keine Bewertungen
- DIN13 ISO Metric Threads enDokument1 SeiteDIN13 ISO Metric Threads enwagner jrNoch keine Bewertungen
- The 100 Best History Books of All TimeDokument23 SeitenThe 100 Best History Books of All TimeDavid DiógenesNoch keine Bewertungen
- Oralpatho MCQDokument0 SeitenOralpatho MCQkainath0150% (2)
- Soviet Aims in Korea and The Origins of The Korean War, 1945-1950 New Evidence From Russian ArchivesDokument37 SeitenSoviet Aims in Korea and The Origins of The Korean War, 1945-1950 New Evidence From Russian ArchivesoraberaNoch keine Bewertungen
- Winston ChurchillDokument13 SeitenWinston ChurchillJulianNoch keine Bewertungen
- Oral Pathology McqsDokument3 SeitenOral Pathology McqsAdel Abdel-Azim79% (19)
- Management of Nerve Injuries: Abstract and IntroductionDokument6 SeitenManagement of Nerve Injuries: Abstract and IntroductionKhadim ShahNoch keine Bewertungen
- Rubber DamDokument2 SeitenRubber DamKhadim ShahNoch keine Bewertungen
- Of An Ulcer: Break in The Continuity of Surface Epithelium With Superadded InfectionDokument5 SeitenOf An Ulcer: Break in The Continuity of Surface Epithelium With Superadded InfectionKhadim ShahNoch keine Bewertungen
- Chapter 2Dokument12 SeitenChapter 2Khadim ShahNoch keine Bewertungen
- CH 07Dokument33 SeitenCH 07Khadim ShahNoch keine Bewertungen
- Chapter 2Dokument12 SeitenChapter 2Khadim ShahNoch keine Bewertungen
- Oral PathologyDokument3 SeitenOral PathologyKhadim Shah0% (1)
- Chapter 49: The Submandibular RegionDokument2 SeitenChapter 49: The Submandibular RegionKhadim ShahNoch keine Bewertungen
- Conversion of Galvanometer Into VoltmeterDokument1 SeiteConversion of Galvanometer Into VoltmeterKhadim ShahNoch keine Bewertungen
- LighthouseDokument2 SeitenLighthouseВлад «Befly» МирошниченкоNoch keine Bewertungen
- Jurnal Triangle SpiderDokument17 SeitenJurnal Triangle SpiderZuhdi Mahendra KotoNoch keine Bewertungen
- The Art of Commitment by Robert Schelling.Dokument29 SeitenThe Art of Commitment by Robert Schelling.Gregory DavisNoch keine Bewertungen
- Does It Matter? - A Critical AnalysisDokument3 SeitenDoes It Matter? - A Critical AnalysisGina M CorreaNoch keine Bewertungen
- Ferdinand Porsche BiographyDokument2 SeitenFerdinand Porsche BiographyAnonymous umabEI6Noch keine Bewertungen
- Hero Tiers: Team & Hero Tier ListDokument6 SeitenHero Tiers: Team & Hero Tier ListLan SarawakNoch keine Bewertungen
- Metro Manila: International Humanitarian Law, Genocide, and Other Crimes Against Humanity"Dokument24 SeitenMetro Manila: International Humanitarian Law, Genocide, and Other Crimes Against Humanity"FrancisC.PostradoNoch keine Bewertungen
- Maaswj 866Dokument8 SeitenMaaswj 866Hornet133Noch keine Bewertungen
- ABSL Paper Eng-InsideDokument5 SeitenABSL Paper Eng-Insideအာ ကာNoch keine Bewertungen
- NotesDokument6 SeitenNotesRonnie MonivaNoch keine Bewertungen
- Basic Guide To War of Emperium: ROM EditionDokument48 SeitenBasic Guide To War of Emperium: ROM EditionL M AkhiruddinNoch keine Bewertungen
- Warhammer 40000 Deathwatch enDokument3 SeitenWarhammer 40000 Deathwatch enSebastianoPedrettiNoch keine Bewertungen
- Today's Fallen Heroes Thursday 16 August 1917 (4119)Dokument88 SeitenToday's Fallen Heroes Thursday 16 August 1917 (4119)MickTierneyNoch keine Bewertungen
- Skills Practiced: Scanning & Skimming Task Types: Matching Multiple Choice Sentence Completion Main Idea Yes/No/NGDokument8 SeitenSkills Practiced: Scanning & Skimming Task Types: Matching Multiple Choice Sentence Completion Main Idea Yes/No/NGNhung TrầnNoch keine Bewertungen
- RULES-DW-Dungeon World Cheat Sheets - Google DocumentenDokument8 SeitenRULES-DW-Dungeon World Cheat Sheets - Google Documentenkris rendersNoch keine Bewertungen
- Booklet 5 - 231118 - 183901Dokument188 SeitenBooklet 5 - 231118 - 183901Solange RiofrioNoch keine Bewertungen
- Currunt Affairs 09 and 10Dokument47 SeitenCurrunt Affairs 09 and 10trohankNoch keine Bewertungen
- PAKISTAN - RUSSIA Relations in The Post Cold War EraDokument12 SeitenPAKISTAN - RUSSIA Relations in The Post Cold War EradanielNoch keine Bewertungen
- Chuyên Nguyễn Trãi 11 DHBBDokument18 SeitenChuyên Nguyễn Trãi 11 DHBBHung Cg NguyenNoch keine Bewertungen
- SkenderbegDokument2 SeitenSkenderbegzoranlac7Noch keine Bewertungen
- Listado TNT Games 58448933 54388621Dokument12 SeitenListado TNT Games 58448933 54388621Yasmany FargiéNoch keine Bewertungen