Beruflich Dokumente
Kultur Dokumente
Atopic Dermatitis
Hochgeladen von
Mahmoud Abu SamraCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Atopic Dermatitis
Hochgeladen von
Mahmoud Abu SamraCopyright:
Verfügbare Formate
1) Atopic Dermatitis
Atopic dermatitis (AD) also known as atopic eczema or eczema is a type of dermatitis, an inflammatory,
relapsing, non-contagious and itchy skin disorder. It has been given names like "prurigo Besnier,"
"neurodermatitis," "endogenous eczema," "flexural eczema," "infantile eczema," and "prurigo diathsique".
Atopic dermatitis is very common worldwide and increasing in prevalence. It affects males and females equally
and accounts for 10%-20% of all referrals to dermatologists (doctors who specialize in the care and treatment
of skin diseases). Atopic dermatitis occurs most often in infants and children, and its onset decreases
substantially with age. Scientists estimate that 65% of patients develop symptoms in the first year of life, and
90% develop symptoms before the age of 5. Onset after age 30 is less common and often occurs after
exposure of the skin to harsh conditions. People who live in urban areas and in climates with low humidity
seem to be at an increased risk for developing atopic dermatitis.
About 10% of all infants and young children experience symptoms of the disease. Roughly 60% of these
infants continue to have one or more symptoms of atopic dermatitis even after they reach adulthood.
2) Causes of AD
The cause of atopic dermatitis is not known, but the disease seems to result from a combination of genetic
(hereditary) and environmental factors. There seems to be a basic hypersensitivity and an increased tendency
toward itching. Evidence suggests that the disease is associated with other so-called atopic disorders such as
hay fever (seasonal allergies) and asthma, which many people with atopic dermatitis also have. In addition,
many children who outgrow the symptoms of atopic dermatitis go on to develop hay fever or asthma. Although
one disorder does not necessarily cause another, they may be related, thereby giving researchers clues to
understanding atopic dermatitis. It is important to understand that food sensitivities do not seem to be a major
factor with most atopic dermatitis. This is an area of active research. Patients with atopic dermatitis seem to
have mild immune system weakness. They are predisposed to develop fungal foot disease and cutaneous
staphylococcal infections, and they can disseminate herpes simplex lip infections (eczema herpeticum
1
) and
smallpox vaccination (eczema vaccinatum
2
) to large areas of skin.
3) Characteristics of Atopic Dermatitis:
Atopic dermatitis (AD) is a chronic pruriginous inflammatory skin disease, characterized by intense dryness,
suggestive of an allergic diathesis of genetic origin. It is characterized by impaired skin barrier function,
resulting from a lipid deficiency in the intercorneocyte matrix, rendering the atopic skin more sensitive to
environmental allergens and facilitating their penetration. AD is characterized by two different, chronic,
stages: Eczema and Remission. Only the AD symptoms can be treated, as there is currently no curative
treatment. Eczema outbreaks combining sensations of dryness and squames
3
, with a rough appearance and
rash, located particularly in the vicinity of the lesions. It should be noted that there is an occasional risk of
superinfection of these lesions by the pathogenic flora, in particular by Staphylococcus aureus, when the
skin barrier is breached by pruritus or itching. The most recent studies show the involvement of one essential
factor: the NF kappa B factor, responsible for amplifying the inflammatory response. The NF kappa B factor
is a protein complex that controls transcription of DNA and is involved in cellular responses to stimuli such as
stress, cytokines, free radicals, ultraviolet irradiation. In brief, NF-B can be understood to be a protein
responsible for cytokine production and cell survival.
The mechanism of Atopic dermatitis witnesses an innate abnormality in the epidermal lipid metabolism
which leads to
1) A failure of the intercorneocyte cement due to a lack of: Ceramides, Essential fatty acids, Cholesterol
and cholesterol esters.
2) Shortage of filaggrins are filament-associated proteins which bind to keratin fibers in the epidermal cells.
The gene for filaggrin resides on Chromosome 1 (1q21.3). This gene was first identified as the gene
involved in ichthyosis vulgaris.
4
Also, the shortage of filaggrin results in the increase in skin pH which
encourages serine protease activity these are enzymes which digest lipid-processing enzymes and the
proteins that hold epidermal cells together. Serine proteases also generate active cytokines like IL-1a and
Il-1beta and promote skin inflammation.
3) Shortage of involucrin which contributes to the formation of a cell envelope that protects corneocytes in
the skin. Involucrin is synthesized in the stratum spinosum and cross linked in the stratum granulosum by
the transglutaminase enzyme that makes it highly stable. Thus it provides structural support to the cell,
thereby allowing the cell to resist invasion by micro-organisms.
But what triggers AD..
Mutations of the gene encoding TLR2 are associated with severe forms of AD (with recurring bacterial
infections) as when an allergen crosses the epidermal barrier, it comes in contact with toll-like receptors
(TLRs) expressed by skin cells, the 1
st
line of defense against infections
Reduced activity of beta-defensins 2 and 3
5
. This reduction in the skin's natural antimicrobial peptides
6
is
induced by the strong presence of pro-inflammatory cytokines
7
(IL3,IL4,IL5,IL13) produced by the Th2
lymphocytes
8
Reduced innate immunity (beta-defensins 2 and 3) is why, in 90% of cases, atopic skin is colonized by
staphylococcus aureus bacteria. The toxins produced by S.aureus increase inflammation and cause the
production of specific IgEs. The ceramidases synthesized by S.aureus alter the skin's barrier function.
The hyper-reactivity of the immune system triggers the release of numerous pro-inflammatory
mediators and immunoglobulin E (IgE)
9
In the case of extrinsic or allergic atopy (actual AD), specific immunoglobulins Es (IgEs) are released Other
symptoms: rhinitis, asthma.etc.
Reactivity to environmental allergens:
Respiratory allergens: pet hairs (cats, dogs), pollen, dust mites
Food allergens: eggs, peanuts, milk, soya bean, wheat flour etc.
Contact allergens: perfume, nickel, latex etc.
4) Treatment to Atopic Dermatitis
1. Anti-inflammatory (dermocorticosteroids). This is used for short term only and during inflammatory
eczemas. They should be advised with a proper emollient since they induce dryness.
2. Antiseptic (Antibiotics only in case of super infection). They can't be used for so long or they will be
harming the cutaneous flora (bacterium that lives on top of the skin)
3. Anti Pruritus, anti- itching or Anti-histamines.
4. With severe cases, immunomodulators or topical immunosuppressive could be used.
1
is a rare but severe disseminated infection that generally occurs at sites of skin damage produced by, for example, atopic
dermatitis, burns, long term usage of topical steroids or eczema
2
is a rare severe adverse reaction to smallpox vaccination.
3
Squames begin life as normal cells in the lower layers of the epidermis but, as they travel towards the surface, they
progressively lose all recognizable contents.
4
Ichthyosis is characterised by persistently dry, thickened, rough, fish scale skin. There are at least 20 varieties of ichthyosis,
including inherited and acquired forms.
5
The beta defensins are antimicrobial peptides implicated in the resistance of epithelial surfaces to microbial colonization.
6
A peptide is a chemical compound containing two or more amino acids (amino acid polymers) that are coupled by a
peptide bond. This bond is a special linkage in which the nitrogen atom of one amino acid binds to the carboxyl carbon atom
of another.
7
Cytokines are cell signaling molecules that aid cell to cell communication in immune responses and stimulate the
movement of cells towards sites of inflammation, infection and trauma.
8
Lymphocytes are small white blood cells that play an role in the bodys immune response (that is, in the bodys fight
against germs and diseases).There are two main types of lymphocytes, known as B cells and T cells (also known as B
lymphocytes and T lymphocytes). The B cells produce antibodies that attack foreign molecules (germs and the toxins they
produce). The T cells are more complicated, but they can attack the bodys own cells when they are diseased (for example,
when the cells have been invaded by cancer or viruses).
Substances secreted by lymphocytes (called lymphokines) contribute to inflammation. Wherever there is chronic
inflammation in the body, lymphocytes are present.
9
IgE: specific antibodies synthesized during the allergic reaction.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- String Harmonics in Ravel's Orchestral WorksDokument97 SeitenString Harmonics in Ravel's Orchestral WorksYork R83% (6)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- FeedbackDokument101 SeitenFeedbackRupsi Kumar75% (4)
- Getting To Yes Book SummaryDokument5 SeitenGetting To Yes Book SummaryAnthony Chan67% (3)
- Negotiating With Difficult People and Difficult BehavioursDokument19 SeitenNegotiating With Difficult People and Difficult BehavioursMahmoud Abu SamraNoch keine Bewertungen
- Perspective in PharmacyDokument3 SeitenPerspective in PharmacyAgniez Hannah Permites100% (4)
- A Course in KettlebellsDokument40 SeitenA Course in KettlebellsMagoots100% (1)
- Physics Project On Circular MotionDokument22 SeitenPhysics Project On Circular Motionishan67% (3)
- Jarratt Davis: How To Trade A Currency FundDokument5 SeitenJarratt Davis: How To Trade A Currency FundRui100% (1)
- Sales Presentation Evaluation SheetDokument1 SeiteSales Presentation Evaluation SheetNilabjo Kanti PaulNoch keine Bewertungen
- ActivistDokument1 SeiteActivistMahmoud Abu SamraNoch keine Bewertungen
- Bioderma expenses sheet group costs 2016Dokument2 SeitenBioderma expenses sheet group costs 2016Mahmoud Abu SamraNoch keine Bewertungen
- Assessment BriefDokument4 SeitenAssessment BriefMahmoud Abu Samra0% (1)
- Writing - Paraphrasing - JS & SCDokument4 SeitenWriting - Paraphrasing - JS & SCMahmoud Abu SamraNoch keine Bewertungen
- Agenda For New Kams & Mrs Day/Date/Time Topic: Hydrabio & Dehydrated Skin - CicabioDokument3 SeitenAgenda For New Kams & Mrs Day/Date/Time Topic: Hydrabio & Dehydrated Skin - CicabioMahmoud Abu SamraNoch keine Bewertungen
- SCE Commission Structure and Ranking Criteria Proposal for 2016Dokument8 SeitenSCE Commission Structure and Ranking Criteria Proposal for 2016Mahmoud Abu SamraNoch keine Bewertungen
- Curriculum Design Form: Physician Partnership Training ProgramDokument6 SeitenCurriculum Design Form: Physician Partnership Training ProgramMahmoud Abu SamraNoch keine Bewertungen
- Session/Topic Exercise/Resources Time Frame: Day OneDokument7 SeitenSession/Topic Exercise/Resources Time Frame: Day OneMahmoud Abu SamraNoch keine Bewertungen
- ENGL-101 - General Weekly Syllabus - Fall 2013Dokument2 SeitenENGL-101 - General Weekly Syllabus - Fall 2013Mahmoud Abu SamraNoch keine Bewertungen
- Anatomy Ch. 5Dokument62 SeitenAnatomy Ch. 5Mahmoud Abu SamraNoch keine Bewertungen
- Mahmoud Abdel Hameed November Expense ReportDokument2 SeitenMahmoud Abdel Hameed November Expense ReportMahmoud Abu SamraNoch keine Bewertungen
- 27 How To Make Water in Oil EmulsionsDokument1 Seite27 How To Make Water in Oil EmulsionsEmontevideo100% (2)
- 00 B 4952 BB 1400 CB 0 A 1000000Dokument8 Seiten00 B 4952 BB 1400 CB 0 A 1000000Mahmoud Abu SamraNoch keine Bewertungen
- Difficult Situation: So, Based On This Given Information, Meet Both of Them and NegotiateDokument4 SeitenDifficult Situation: So, Based On This Given Information, Meet Both of Them and NegotiateMahmoud Abu SamraNoch keine Bewertungen
- This One Is Big and in Discovery Gardens (7elwa Ya 7oda) It Includes All Rates and It's One Bedroom ApartmentDokument4 SeitenThis One Is Big and in Discovery Gardens (7elwa Ya 7oda) It Includes All Rates and It's One Bedroom ApartmentMahmoud Abu SamraNoch keine Bewertungen
- Presentation Evaluation ChecklistDokument1 SeitePresentation Evaluation ChecklistMahmoud Abu SamraNoch keine Bewertungen
- New Tools Questionnaire International Markets - EVDokument9 SeitenNew Tools Questionnaire International Markets - EVMahmoud Abu SamraNoch keine Bewertungen
- EnvelopeDokument1 SeiteEnvelopeMahmoud Abu SamraNoch keine Bewertungen
- White Objective PatentDokument2 SeitenWhite Objective PatentMahmoud Abu SamraNoch keine Bewertungen
- Atopic DermatitisDokument4 SeitenAtopic DermatitisMahmoud Abu SamraNoch keine Bewertungen
- New Expenses SheetDokument2 SeitenNew Expenses SheetMahmoud Abu SamraNoch keine Bewertungen
- Sebium Range for Oily Acne-Prone Skin CareDokument1 SeiteSebium Range for Oily Acne-Prone Skin CareMahmoud Abu SamraNoch keine Bewertungen
- Skin Structure: Layers, Cells & FunctionsDokument1 SeiteSkin Structure: Layers, Cells & FunctionsMahmoud Abu SamraNoch keine Bewertungen
- Sun and Skin (Photoderm)Dokument5 SeitenSun and Skin (Photoderm)Mahmoud Abu SamraNoch keine Bewertungen
- SerumDokument1 SeiteSerumMahmoud Abu SamraNoch keine Bewertungen
- This One Is Big and in Discovery Gardens (7elwa Ya 7oda) It Includes All Rates and It's One Bedroom ApartmentDokument4 SeitenThis One Is Big and in Discovery Gardens (7elwa Ya 7oda) It Includes All Rates and It's One Bedroom ApartmentMahmoud Abu SamraNoch keine Bewertungen
- T&DChap 011Dokument25 SeitenT&DChap 011SandrakalaaSivaguruNoch keine Bewertungen
- ICTMS 2013 - Program ScheduleDokument3 SeitenICTMS 2013 - Program ScheduleSantanu DasNoch keine Bewertungen
- Sidak 2008 FAQsDokument3 SeitenSidak 2008 FAQssikhswimNoch keine Bewertungen
- Dreams PDFDokument8 SeitenDreams PDFapi-266967947Noch keine Bewertungen
- TOS-GRADE-10 EnglishDokument2 SeitenTOS-GRADE-10 EnglishPRINCESS VILLASANTANoch keine Bewertungen
- Crafting Your Keto Diet MindsetDokument3 SeitenCrafting Your Keto Diet MindsetoculosoakleyNoch keine Bewertungen
- Evolution and Diversity of Coleochaete, Charales, and Green PlantsDokument4 SeitenEvolution and Diversity of Coleochaete, Charales, and Green PlantsAndrei PusungNoch keine Bewertungen
- Arp ReflectionDokument3 SeitenArp Reflectionapi-317806307Noch keine Bewertungen
- Analyze Financial Performance with Ratio AnalysisDokument4 SeitenAnalyze Financial Performance with Ratio AnalysisKartikeyaDwivediNoch keine Bewertungen
- Swadhin Bangla Betar KendraDokument21 SeitenSwadhin Bangla Betar KendraMusfiqur Rahman ApuNoch keine Bewertungen
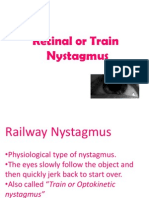
- NystgmusDokument16 SeitenNystgmusCheska Justine San JuanNoch keine Bewertungen
- Progressivism Lesson 3 The PresidentsDokument3 SeitenProgressivism Lesson 3 The Presidentsapi-302923213Noch keine Bewertungen
- 22-Submission File-35-1-10-20190811Dokument3 Seiten22-Submission File-35-1-10-20190811DhevNoch keine Bewertungen
- Fuentes CAED PortfolioDokument32 SeitenFuentes CAED PortfoliojsscabatoNoch keine Bewertungen
- Butterfly Court SpreadsDokument24 SeitenButterfly Court SpreadsAbigaïl EnderlandNoch keine Bewertungen
- Mabvax v. Harvey Kesner MTD 05-09-2019 OrderDokument49 SeitenMabvax v. Harvey Kesner MTD 05-09-2019 OrderTeri BuhlNoch keine Bewertungen
- Marketing Management: Amit Pandey +91-7488351996Dokument15 SeitenMarketing Management: Amit Pandey +91-7488351996amit pandeyNoch keine Bewertungen
- Toan Bo Cac Bai Ktra E11CBDokument13 SeitenToan Bo Cac Bai Ktra E11CBNguyễn Thị Huyền Phương0% (1)
- Africa S Top 15 Cities in 2030Dokument10 SeitenAfrica S Top 15 Cities in 2030loca018Noch keine Bewertungen
- Community-Acquired Pneumoniaandhospital-Acquiredpneumonia: Charles W. Lanks,, Ali I. Musani,, David W. HsiaDokument15 SeitenCommunity-Acquired Pneumoniaandhospital-Acquiredpneumonia: Charles W. Lanks,, Ali I. Musani,, David W. HsiaMajo EscobarNoch keine Bewertungen
- Guide Number 5 My City: You Will Learn To: Describe A Place Tell Where You in The CityDokument7 SeitenGuide Number 5 My City: You Will Learn To: Describe A Place Tell Where You in The CityLUIS CUELLARNoch keine Bewertungen
- Propaganda AssignmentDokument3 SeitenPropaganda Assignmentapi-653920203Noch keine Bewertungen
- Karakteristik Morfologik Kambing Spesifik Lokal Di Kabupaten Samosir Sumatera UtaraDokument6 SeitenKarakteristik Morfologik Kambing Spesifik Lokal Di Kabupaten Samosir Sumatera UtaraOlivia SimanungkalitNoch keine Bewertungen