Beruflich Dokumente
Kultur Dokumente
ESR Good Practice Guide For Ambulance Services and Their Commissioners
Hochgeladen von
MarcusMüllerOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
ESR Good Practice Guide For Ambulance Services and Their Commissioners
Hochgeladen von
MarcusMüllerCopyright:
Verfügbare Formate
EMERGENCY
SERVICES
REVIEW
Good Practice Guide for Ambulance Services
and their Commissioners
Emergency Services Review
Good Practice Guide for Ambulance Services
and their Commissioners
Author Jonathan Brotherton
Foreword Anthony C Marsh
Editors Claire Burden, Russell Emeny and Ian Merrick
The Emergency Services Review was co-ordinated by
NHS Interim Management and Support on behalf of the
Office of the Strategic Health Authorities
Thanks go to everyone involved with the project
Good practice guide for Ambulance Services
and their commissioners
CONTENTS
Section Page
Foreward 1
1. Introduction 2
2. Ambulance Service Commissioning 3
3. Whole System Working and Effective Partnerships 4
4. Operational Performance - Understanding Demand 6
5. Operational Performance - Aligning Resources to Demand 7
6. Operational Performance - The Call Cycle and Emergency
Operations Centres
9
7. Escalation 11
8. Summary 12
Appendix A - Bibliography 13
Appendix B - Emergency Access Algorithm 16
Appendix C - Example of Resource Escalatory Action Plan 17
The Emergency Services Review has produced a set of guidance and tools. The
following publication is part of this series of documents. The publications are:
A comparative review of international Ambulance Service best practice
Good practice guide for Ambulance Services and their commissioners
Good practice in delivering emergency care: A guide for local health communities
System resilience: A review of NHS emergency care performance during recent
winters
Intensive support diagnostic toolkit: Tools and user guide
These publications are all available in PDF from http://www.osha.nhs.uk. Please
contact programmes@osha.nhs.uk for hard copies or with any queries.
Good practice guide for Ambulance Services
and their commissioners
FOREWORD
The Emergency Services Review was instigated following the winter of 2008 to identify
a focused set of actions to support local health economies in the development of
resilient, sustainable and integrated emergency and urgent care systems. The review
has focussed on improving emergency ambulance service delivery through a
strengthened whole-system approach. This guide is one of a number of tools that are a
product of the review.
In acknowledgement of the excellent guidance notes and good practice that is available
for Ambulance Trusts and their Commissioners this paper does not attempt to introduce
additional new ways of working. The overriding aim is to support commissioner driven
delivery and maintenance of key national performance standards by bringing together
previously published guidance into a single point of reference. In doing this, a practical,
pragmatic and accessible guide has been created.
We all recognise the importance of providing an excellent level of service and I hope
that this document will support further improvements.
Anthony C Marsh
Chief Executive Officer
West Midlands Ambulance Service NHS Trust
National Professional Lead
Emergency Services Review Programme
1 Foreword
Good practice guide for Ambulance Services
and their commissioners
Introduction 2
1. INTRODUCTION
1.1 This document draws together and signposts the majority of relevant, published
UK Ambulance Service guidance. It is aimed at:
Ambulance Service Managers
o To highlight established good practice
o To share knowledge and expertise across the country
NHS Commissioners
o To highlight established models, techniques and efficiencies
o To foster innovation and efficiency through informed commissioning of
ambulance services
o To further ensure emergency care standards are commissioner-driven
and performance managed
Other partners in unscheduled care
o To advance improvements in unscheduled care pathways for the benefit
of patients and local health communities
1.2 We have carried out an extensive literature review and have also consulted
senior ambulance service leaders, ambulance commissioning specialists and
other ambulance service specialists. A full bibliography is contained in Appendix
A, with full URLs.
1.3 The most relevant sections have been sign posted for easy navigation.
Hyperlinks are included in the electronic version to take the reader to relevant
documents without the need to search Department of Health and NHS websites.
1.4 If you would like to comment on this guide, please email
jonathan.brotherton@southwest.nhs.uk.
Good practice guide for Ambulance Services
and their commissioners
3 Ambulance Service Commissioning
2. AMBULANCE SERVICE COMMISSIONING
2.1 Ambulance services should be commissioned to encourage shared ownership of
urgent care across healthcare systems. The system needs a congruent view of
urgent care requirements and priorities. Ambulance services should be
commissioned by a consortium of Primary Care Trusts (PCTs) with agreed
decision making processes and a lead commissioner. This is now common
practice, but must be universal, as described in the Guidance on the Standard
NHS Contract for Ambulance Services.
2.2 The 2005 Department of Health report, Taking Healthcare to the Patient -
Transforming NHS Ambulance Services, contains a number of commissioning
recommendations including:
PCTs should integrate ambulance commissioning within their strategic
commissioning plans for all urgent and emergency care
The commissioning of NHS Direct, out of hours services, and other urgent
care services should be integrated to produce a coherent service model
SHAs should work with PCTs to ensure that Ambulance Trust resources are
included in capacity plans for primary care and for urgent care
2.3 Driving change: Good practice guidelines for PCTs on commissioning
arrangements for emergency ambulance services and non-emergency patient
transport services is designed to assist PCTs in leading the commissioning
process to achieve the necessary system reform outlined above.
2.4 World Class Commissioning (WCC) aims to improve the health and wellbeing of
people in England through improvements in the way that health and care
services are commissioned by PCTs. The new World Class Commissioning
support and development website brings together:
The latest WCC news
The most relevant WCC events and master classes
The best guidance, tools and case studies
A discussion forum to share ideas and concerns
2.5 Two useful documents demonstrate how the North West of England has adopted
the World Class Commissioning framework for the commissioning of Ambulance
Services:
World Class Commissioning of Ambulance Services in the North West
World Class Commissioning Competency Framework
2.6 The Primary Care Foundations Urgent Care a practical guide to transforming
same day care in General Practice has much to attract commissioners of
ambulance services. It has a suite of recommendations on pages 6 and 7. Case
studies two and eight highlight more appropriate use of ambulance services.
Good practice guide for Ambulance Services
and their commissioners
Whole System Working and Effective Partnerships 4
3. WHOLE SYSTEM WORKING AND EFFECTIVE PARTNERSHIPS
3.1 The Department of Healths Guidance on the Standard NHS Contract for
Ambulance Services explains how the Contract can be used as a tool for
assuring accountability between Providers and PCTs and for improving
performance. The guiding principles and expected behaviours in section 2
outline a whole system approach where effective partnerships are fundamental.
3.2 To commission and provide ambulance services that are safe and provide value
for money there needs to be:
An agreed vision for emergency and urgent care
An effective mechanism to enable a whole systems approach
3.3 The Health Care Commissions Not J ust a Matter of Time a review of urgent
and emergency care services in England is an extensive review focussing on
how services are accessed, delivered and managed across an area. It highlights
a lack of awareness and understanding of the range of new services that have
been introduced in recent years. It also identifies many of the problems patients
experience on the pathways they follow into urgent and emergency care. Where
patients are dealt with by the first service they contact, their care usually
proceeds smoothly. But where patients are transferred or referred between
services, they can experience problems. A summary of its recommendations are
contained in Next Steps on pages 52-60.
3.4 A vision for emergency and urgent care: the role of ambulance services, which
was published by the Ambulance Service Network, outlines the challenges facing
health services across the Western world: an ageing population; an increase in
long-term conditions; and changing expectations and demands from patients and
the public. Ambulance services have a vital role to play in addressing these
challenges and ensuring all patients get the right care, in the right place, at the
right time. This report outlines how ambulance services can work with the
commissioners and providers of health and social care to save lives, improve
health and tackle inequalities. There are also a set of urgent care case studies
on the Department of Health website that demonstrate whole system integration.
Good practice guide for Ambulance Services
and their commissioners
5 Whole System Working and Effective Partnerships
3.5 Pressures within emergency and urgent services affect the whole health and
social care system. Faster, more convenient access to emergency care cannot
be delivered and sustained without co-operation across the system. The
Emergency Care Networks Checklist (ECNs) provides a how to guide to create
this key mechanism for achieving and managing that co-operation. This checklist
reaffirms that availability of intelligent data is crucial to managing the emergency
care system. Ambulance Trusts providing demand and clinical data on actual
illness on a regular basis can support commissioners and ECNs to take
ownership of activity. Data provided at practice level can enable GPs and
Practice Based Commissioners (PBC) to support action to find appropriate
alternatives to hospital care. More specifically, Measuring the Benefits of the
Emergency Care Practitioner (ECP) details how ECNs can determine the
effectiveness of more recent initiatives such as the ECP role. It includes sections
on:
Quantifying the Benefits
Measuring Against Target
Cost Effectiveness of ECPs in the Emergency Pathway
Calculating the Business Case Return on Investment
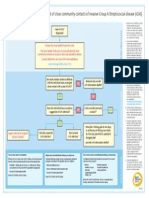
3.6 The Emergency Access Algorithm produced by the Emergency Services Review
(appendix B) outlines emergency and urgent care pathways. This algorithm can
help commissioners and providers to improve their understanding of access
pathways into emergency care systems; along with potential solutions to improve
access and reduce delays across the whole health and social care system.
Good practice guide for Ambulance Services
and their commissioners
Operational Performance Understanding Demand 6
4. OPERATIONAL PERFORMANCE UNDERSTANDING DEMAND
4.1 The primary purpose of analysing call data is to understand demand. It assists
Ambulance Trusts in improving response times from when the call is connected
to the ambulance control room (call connect) to the time a vehicle arrives at
scene by best matching their resources to the natural patterns of demand. Such
analyses should be shared with commissioners to support decisions for further
investment, either in ambulance services or other community based options.
Operational planning needs to explicitly link with commissioned activity and the
resultant financial envelope attached to this, as per schedule 3 of the Standard
NHS Contract for Ambulance Services.
4.2 An analysis tool for Ambulance Trust data was developed by the Department of
Health in 2007 - Analysing ambulance call-cycle data for call connect target. The
purpose of this is to provide a structure for operational managers to identify the
causes of performance problems and to focus improvement effort in the places
where it will have the most benefit. It highlights where the main problems lie and
concentrates on the call cycle stages from call connect to vehicle arrive at scene.
This helps Trusts to improve call connect performance.
4.3 Further reference to the scope of this analysis tool is captured in section 3 of
Improving Ambulance Response Times: high impact changes and response time
algorithms for NHS Ambulance Services (High Impact Changes). There are
also good practice examples of understanding demand.
4.4 There are a number of other demand analysis tools and service improvement
options available to Ambulance Trusts. More recently, with developments in
computer aided dispatch systems (CAD), Ambulance Trusts have the opportunity
and capability to generate their own forecasts and deployment models.
Commercial options are also available and have been used successfully by a
number of Ambulance Trusts.
Good practice guide for Ambulance Services
and their commissioners
7 Operational Performance - Aligning Resources To Demand
5. OPERATIONAL PERFORMANCE - ALIGNING RESOURCES TO DEMAND
5.1 The process of managing emergency and urgent care demand in the local health
community is a shared responsibility of Commissioners and Providers. It should
be a key focus of ECNs. Taking Healthcare to the Patient - Transforming NHS
Ambulance Services defines an ambulance service that provides both high
quality call handling and clinical advice (hear and treat), and safe and effective
mobile healthcare (see and treat). The hear and treat and see and treat
models, along with accompanying examples of good practice, are outlined in
section 4 and appendix D. Further examples of good practice are in the case
studies section of Changing Times - Sustaining Long term Performance Against
Call Connect for NHS Ambulance services (Changing Times) and A vision for
emergency and urgent care - The role of ambulance services.
5.2 Effective matching of resources to demand is a fundamental requirement of
achieving Call Connect performance. Processes such as unit hour methodology
should continue to be used in driving efficiency. Section 2 of High Impact
Changes contains useful how to guides and good practice examples of:
The front loaded model - an increased proportion of fast response vehicles
and community response
Matching resources to demand the fundamental basics of having rosters
that reflect demand patterns
5.3 For further depth to this topic, the case studies section of Changing Times
includes reports and checklists on demand profiling of both call handling and
operational resources. Similarly Best Practice Guidelines on Ambulance
Operations Management contains straightforward yet effective recommendations
of demand-based cover that Ambulance Trusts may review against their own
current operations.
5.4 Changing models of care have significant workforce implications in terms of
development, structure and working patterns. The effective engagement and
management of people optimises a Trusts capacity to be successful in attaining
short term targets whilst delivering an agenda for sustainable long term change.
Changing Times contains more on effective engagement, with staff in its critical
success factors. There are also good practice examples in High Impact
Changes. Understanding the call cycle is key to engaging internal and external
partners in their contribution to making change for the better. These elements
are explored in 'Changing Times' Managing Information Checklist and Call
Management Cycle Algorithm.
Good practice guide for Ambulance Services
and their commissioners
Operational Performance - Aligning Resources To Demand 8
5.5 Ambulance Trusts typically develop their Community Response infrastructure
with a range of response models. These include Community First Responders,
staff responders, co-responder schemes (Police, Fire, Military Services, etc) and
strategically located automated external defibrillators (AEDs). High Impact
Changes (section 2) outlines some of the fundamentals of operating a
community response model. Changing Times highlights the need for community
response to be complimented by a strong governance framework and
organisational integration. This will optimise availability and utilisation whilst
maintaining the interest and commitment of those individuals involved.
Good practice guide for Ambulance Services
and their commissioners
9 Operational Performance - The Call Cycle and Emergency Operations Centres
6. OPERATIONAL PERFORMANCE - THE CALL CYCLE & EMERGENCY
OPERATIONS CENTRES
6.1 Ambulance Trusts should develop systems and processes that minimise delay in
their call-answering, call-processing and dispatch functions. The significant
improvements in computer aided dispatch systems need augmenting with local
knowledge and experience. Consistently successful EOCs will develop dispatch
guidelines and performance measures to ensure the right resource is dispatched
to the right patient at the earliest possible time.
6.2 To achieve this, the 999 call management cycle can be broken down into
component parts to identify activities that dont add value. Key performance
indicators (KPIs) need to be established for each component, with performance
monitoring mechanisms and triggers put in place. The call management cycle
algorithm contained in Changing Times shows a range of possible high-impact
changes, both operationally and EOC based, that trusts can make to achieve
sustained performance improvement and improved patient care. The Response
Times Algorithm contained in High Impact Changes also offers guidance on call
cycle management as well as indicative times for each component against which
to benchmark a Trust and / or set as an internal KPI.
6.3 A lack of EOC leadership 24 hours a day was highlighted as a key risk in
Changing Times. Such leadership needs to ensure adequate focus on
performance against internal KPIs where variation is monitored, understood and
minimised. Setting internal targets encourages staff to better their individual and
team performance. The objective should be to challenge the best performing
individual or team and not accept that achieving the target is enough. Real-time
management information provides early indicators that a system or process is
under pressure. Early intervention in a pressured system or process can prevent
crisis management. Avoiding crisis management reduces variation in the long
term. Changing Times also contains an extensive case study on a programme
of EOC improvements made by one Trust.
6.4 Section 2 of High Impact Changes contains useful how to guides and good
practice examples of dynamic deployment plans (moving resources closer to the
predicted source of the next call). Such deployment plans require robust
communications to exist between operational managers and the EOC, with
success largely dependant on a regular review process that includes the
operations team.
6.5 Supporting reference material on Emergency Operations Centres can be found in
the Ambulance Improvement Checklist.
Good practice guide for Ambulance Services
and their commissioners
Operational Performance - The Call Cycle and Emergency Operations Centres 10
6.6 A part of the call cycle that Ambulance Trusts have limited control over is the
handover time at hospitals. Delays in the handover of care between the
ambulance and the hospital services represent a poor patient experience. The
Southwest SHA document, Ensuring Timely Handover of Patient Care, provides
Commissioners, Acute Trusts, Ambulance Trusts and Primary Care providers
with an improvement framework. It highlights the key issues with current
systems and offers practical guidance. The 14 recommendations for action
contained in appendix 1 should ensure timely handover of patient care. Further
good practice on managing hospital handover is contained on page 24 of
Changing Times.
Good practice guide for Ambulance Services
and their commissioners
11 Escalation
7. ESCALATION
7.1 Year round capacity planning and accompanying escalation plans are recognised
as essential for all health care organisations. Resourcing Escalatory Action
Plans (REAP) have been adopted by all Ambulance Service Trusts in England, to
ensure a structured set of arrangements when normal operating functions are
challenged, either through loss of staff, resources, or external factors including
periods of high demand. Each Trust will have a variety of strategic and tactical
options in their REAP that are most suitable to deal with the situation. The profile
of REAP status must be consistently high and as such they need to be routinely
shared with the nominated leads across the local health community who
understand their impact.
7.2 REAP can have a tendency to focus on internal capacity and escalation
processes. REAP management can be enhanced where escalation plans are
integrated across local health economies. Step 8 of the Emergency Care
Network Checklist and checklist 2 of Driving change: Good practice guidelines for
PCTs on commissioning arrangements for emergency ambulance services and
non-emergency patient transport services explain the requirement for, and key
components of, local health community escalation plans. Appendix C includes
an example of a REAP.
7.3 One of the obvious symptoms during periods of pressure is ambulance handover
delays. The table in Figure 2 of Ensuring Timely Handover of Patient Care
illustrates a suggested local health community escalation plan for handover
delays.
Good practice guide for Ambulance Services
and their commissioners
Summary 12
8. SUMMARY
8.1 A key to success is a shared vision of patient care and a commitment to whole
system commissioning of emergency and urgent care.
8.2 Emergency Care Networks are a tested model and provide the opportunity for
effective, collective progress in reducing delays and improving outcomes for
patients. Providers need to engage with the Networks and seek shared solutions
to difficult issues.
8.3 System intelligence, both qualitative and quantitative, needs to be accessible and
measures need to be achievable and tangible. Pursuing targets should not be a
sufficient objective for a network working in partnership to provide high quality
patient care.
8.4 We hope that you have found this guide helpful and wish you well in working with
colleagues across the health and social care services to provide safe and
effective emergency and urgent care.
Good practice guide for Ambulance Services
and their commissioners
13 Appendix A Bibliography
APPENDIX A
BIBLIOGRAPHY
L
i
n
k
/
A
v
a
i
l
a
b
l
e
f
r
o
m
h
t
t
p
:
/
/
w
w
w
.
p
r
i
m
a
r
y
c
a
r
e
f
o
u
n
d
a
t
i
o
n
.
c
o
.
u
k
/
p
a
g
e
9
/
p
a
g
e
1
9
/
p
a
g
e
1
9
.
h
t
m
l
h
t
t
p
:
/
/
w
w
w
.
s
e
f
t
o
n
p
c
t
.
n
h
s
.
u
k
/
L
i
b
r
a
r
y
/
B
e
t
t
e
r
_
L
i
f
e
_
B
e
t
t
e
r
_
H
e
a
l
t
h
/
P
l
a
n
n
i
n
g
_
f
o
r
_
b
e
t
t
e
r
_
f
u
t
u
r
e
/
N
W
A
S
%
2
0
W
O
R
L
D
%
2
0
C
L
A
S
S
%
2
0
C
O
M
M
I
S
S
I
O
N
I
N
G
%
2
0
v
4
.
p
d
f
h
t
t
p
:
/
/
w
w
w
.
s
e
f
t
o
n
p
c
t
.
n
h
s
.
u
k
/
L
i
b
r
a
r
y
/
B
e
t
t
e
r
_
L
i
f
e
_
B
e
t
t
e
r
_
H
e
a
l
t
h
/
P
l
a
n
n
i
n
g
_
f
o
r
_
b
e
t
t
e
r
_
f
u
t
u
r
e
/
N
W
A
S
%
2
0
W
O
R
L
D
%
2
0
C
L
A
S
S
%
2
0
C
O
M
M
I
S
S
I
O
N
I
N
G
%
2
0
v
4
.
p
d
f
h
t
t
p
:
/
/
w
c
c
.
n
e
t
w
o
r
k
s
.
n
h
s
.
u
k
/
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
0
9
1
4
5
1
?
I
d
c
S
e
r
v
i
c
e
=
G
E
T
_
F
I
L
E
&
d
I
D
=
1
7
9
6
7
2
&
R
e
n
d
i
t
i
o
n
=
W
e
b
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
4
1
1
4
2
6
9
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
4
1
1
2
3
0
7
D
a
t
e
P
u
b
l
i
s
h
e
d
M
a
r
-
0
9
J
a
n
-
0
9
J
a
n
-
0
9
D
e
c
-
0
8
J
u
n
-
0
5
A
u
t
h
o
r
/
O
r
i
g
i
n
a
t
o
r
T
h
e
P
r
i
m
a
r
y
C
a
r
e
F
o
u
n
d
a
t
i
o
n
S
e
f
t
o
n
P
C
T
S
e
f
t
o
n
P
C
T
N
H
S
N
e
t
w
o
r
k
s
D
e
p
t
o
f
H
e
a
l
t
h
D
e
p
t
o
f
H
e
a
l
t
h
N
a
m
e
o
f
P
u
b
l
i
c
a
t
i
o
n
U
r
g
e
n
t
C
a
r
e
:
a
p
r
a
c
t
i
c
a
l
g
u
i
d
e
t
o
t
r
a
n
s
f
o
r
m
i
n
g
s
a
m
e
d
a
y
c
a
r
e
i
n
G
e
n
e
r
a
l
P
r
a
c
t
i
c
e
W
o
r
l
d
C
l
a
s
s
C
o
m
m
i
s
s
i
o
n
i
n
g
o
f
A
m
b
u
l
a
n
c
e
S
e
r
v
i
c
e
s
i
n
t
h
e
N
o
r
t
h
W
e
s
t
W
o
r
l
d
C
l
a
s
s
C
o
m
m
i
s
s
i
o
n
i
n
g
C
o
m
p
e
t
e
n
c
y
F
r
a
m
e
w
o
r
k
W
o
r
l
d
c
l
a
s
s
c
o
m
m
i
s
s
i
o
n
i
n
g
s
u
p
p
o
r
t
a
n
d
d
e
v
e
l
o
p
m
e
n
t
w
e
b
s
i
t
e
G
u
i
d
a
n
c
e
o
n
t
h
e
S
t
a
n
d
a
r
d
N
H
S
C
o
n
t
r
a
c
t
f
o
r
A
m
b
u
l
a
n
c
e
S
e
r
v
i
c
e
s
T
a
k
i
n
g
H
e
a
l
t
h
c
a
r
e
t
o
t
h
e
P
a
t
i
e
n
t
-
T
r
a
n
s
f
o
r
m
i
n
g
N
H
S
A
m
b
u
l
a
n
c
e
S
e
r
v
i
c
e
s
D
r
i
v
i
n
g
c
h
a
n
g
e
:
G
o
o
d
p
r
a
c
t
i
c
e
g
u
i
d
e
l
i
n
e
s
f
o
r
P
C
T
s
o
n
c
o
m
m
i
s
s
i
o
n
i
n
g
a
r
r
a
n
g
e
m
e
n
t
s
f
o
r
e
m
e
r
g
e
n
c
y
a
m
b
u
l
a
n
c
e
s
e
r
v
i
c
e
s
a
n
d
n
o
n
-
e
m
e
r
g
e
n
c
y
p
a
t
i
e
n
t
t
r
a
n
s
p
o
r
t
s
e
r
v
i
c
e
s
P
a
g
e
N
o
.
3
3
3
3
3
,
4
3
,
7
3
,
1
1
Good practice guide for Ambulance Services
and their commissioners
Appendix A Bibliography 14
L
i
n
k
/
A
v
a
i
l
a
b
l
e
f
r
o
m
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
H
e
a
l
t
h
c
a
r
e
/
U
r
g
e
n
t
c
a
r
e
/
D
H
_
4
1
1
9
5
6
1
h
t
t
p
:
/
/
w
w
w
.
c
q
c
.
o
r
g
.
u
k
/
_
d
b
/
_
d
o
c
u
m
e
n
t
s
/
N
o
t
_
j
u
s
t
_
a
_
m
a
t
t
e
r
_
o
f
_
t
i
m
e
_
-
_
A
_
r
e
v
i
e
w
_
o
f
_
u
r
g
e
n
t
_
a
n
d
_
e
m
e
r
g
e
n
c
y
_
c
a
r
e
_
s
e
r
v
i
c
e
s
_
i
n
_
E
n
g
l
a
n
d
_
2
0
0
8
1
0
1
5
5
9
0
1
.
p
d
f
h
t
t
p
:
/
/
w
w
w
.
s
k
i
l
l
s
f
o
r
h
e
a
l
t
h
.
o
r
g
.
u
k
/
~
/
m
e
d
i
a
/
R
e
s
o
u
r
c
e
-
L
i
b
r
a
r
y
/
P
D
F
/
E
C
P
_
B
e
n
e
f
i
t
s
_
d
o
c
u
m
e
n
t
_
J
u
n
e
_
0
7
.
a
s
h
x
h
t
t
p
:
/
/
w
w
w
.
n
h
s
c
o
n
f
e
d
.
o
r
g
/
P
u
b
l
i
c
a
t
i
o
n
s
/
D
o
c
u
m
e
n
t
s
/
A
v
i
s
i
o
n
f
o
r
e
m
e
r
g
e
n
c
y
a
n
d
u
r
g
e
n
t
c
a
r
e
.
p
d
f
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
4
0
8
6
9
3
9
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
0
9
1
4
5
1
?
I
d
c
S
e
r
v
i
c
e
=
G
E
T
_
F
I
L
E
&
d
I
D
=
1
7
9
3
1
3
&
R
e
n
d
i
t
i
o
n
=
W
e
b
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
0
7
6
9
6
6
D
a
t
e
P
u
b
l
i
s
h
e
d
M
a
r
c
h
-
0
7
S
e
p
-
0
8
J
u
n
-
0
7
J
u
n
-
0
8
J
u
l
-
0
4
D
e
c
-
0
8
J
u
l
y
-
0
7
A
u
t
h
o
r
/
O
r
i
g
i
n
a
t
o
r
D
e
p
t
o
f
H
e
a
l
t
h
H
e
a
l
t
h
C
a
r
e
C
o
m
m
i
s
s
i
o
n
S
k
i
l
l
s
f
o
r
H
e
a
l
t
h
N
H
S
C
o
n
f
e
d
e
r
a
t
i
o
n
D
e
p
t
o
f
H
e
a
l
t
h
D
e
p
t
o
f
H
e
a
l
t
h
D
e
p
t
o
f
H
e
a
l
t
h
N
a
m
e
o
f
P
u
b
l
i
c
a
t
i
o
n
U
r
g
e
n
t
C
a
r
e
C
a
s
e
S
t
u
d
i
e
s
N
o
t
J
u
s
t
a
M
a
t
t
e
r
o
f
T
i
m
e
-
A
R
e
v
i
e
w
o
f
U
r
g
e
n
t
&
E
m
e
r
g
e
n
c
y
C
a
r
e
S
e
r
v
i
c
e
s
i
n
E
n
g
l
a
n
d
M
e
a
s
u
r
i
n
g
t
h
e
B
e
n
e
f
i
t
s
o
f
t
h
e
E
m
e
r
g
e
n
c
y
C
a
r
e
P
r
a
c
t
i
t
i
o
n
e
r
A
v
i
s
i
o
n
f
o
r
e
m
e
r
g
e
n
c
y
a
n
d
u
r
g
e
n
t
c
a
r
e
-
T
h
e
r
o
l
e
o
f
a
m
b
u
l
a
n
c
e
s
e
r
v
i
c
e
s
E
m
e
r
g
e
n
c
y
C
a
r
e
N
e
t
w
o
r
k
s
C
h
e
c
k
l
i
s
t
S
t
a
n
d
a
r
d
N
H
S
C
o
n
t
r
a
c
t
f
o
r
A
m
b
u
l
a
n
c
e
S
e
r
v
i
c
e
s
A
n
a
l
y
s
i
n
g
a
m
b
u
l
a
n
c
e
c
a
l
l
c
y
c
l
e
d
a
t
a
f
o
r
c
a
l
l
c
o
n
n
e
c
t
P
a
g
e
N
o
.
4
4
5
4
,
7
5
,
1
1
6
6
Good practice guide for Ambulance Services
and their commissioners
15 Appendix A Bibliography
L
i
n
k
/
A
v
a
i
l
a
b
l
e
f
r
o
m
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
0
7
3
6
8
3
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
4
1
1
2
3
0
5
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
0
8
6
2
9
6
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
4
0
8
5
1
7
8
h
t
t
p
:
/
/
w
w
w
.
d
h
.
g
o
v
.
u
k
/
e
n
/
P
u
b
l
i
c
a
t
i
o
n
s
a
n
d
s
t
a
t
i
s
t
i
c
s
/
P
u
b
l
i
c
a
t
i
o
n
s
/
P
u
b
l
i
c
a
t
i
o
n
s
P
o
l
i
c
y
A
n
d
G
u
i
d
a
n
c
e
/
D
H
_
0
8
9
0
7
2
D
a
t
e
P
u
b
l
i
s
h
e
d
A
p
r
-
0
7
J
u
n
-
0
5
J
u
l
-
0
8
O
c
t
-
0
4
O
c
t
-
0
8
A
u
t
h
o
r
/
O
r
i
g
i
n
a
t
o
r
D
e
p
t
o
f
H
e
a
l
t
h
D
e
p
t
o
f
H
e
a
l
t
h
D
e
p
t
o
f
H
e
a
l
t
h
N
H
S
S
o
u
t
h
W
e
s
t
N
a
m
e
o
f
P
u
b
l
i
c
a
t
i
o
n
I
m
p
r
o
v
i
n
g
A
m
b
u
l
a
n
c
e
R
e
s
p
o
n
s
e
T
i
m
e
s
:
H
i
g
h
I
m
p
a
c
t
C
h
a
n
g
e
s
a
n
d
R
e
s
p
o
n
s
e
T
i
m
e
s
A
l
g
o
r
i
t
h
m
s
f
o
r
N
H
S
A
m
b
u
l
a
n
c
e
S
e
r
v
i
c
e
s
B
e
s
t
P
r
a
c
t
i
c
e
G
u
i
d
e
l
i
n
e
s
o
n
A
m
b
u
l
a
n
c
e
O
p
e
r
a
t
i
o
n
s
M
a
n
a
g
e
m
e
n
t
C
h
a
n
g
i
n
g
T
i
m
e
s
-
S
u
s
t
a
i
n
i
n
g
L
o
n
g
t
e
r
m
P
e
r
f
o
r
m
a
n
c
e
A
g
a
i
n
s
t
C
a
l
l
C
o
n
n
e
c
t
f
o
r
N
H
S
A
m
b
u
l
a
n
c
e
s
e
r
v
i
c
e
s
A
m
b
u
l
a
n
c
e
I
m
p
r
o
v
e
m
e
n
t
C
h
e
c
k
l
i
s
t
E
n
s
u
r
i
n
g
T
i
m
e
l
y
H
a
n
d
o
v
e
r
o
f
P
a
t
i
e
n
t
C
a
r
e
P
a
g
e
N
o
.
6
,
7
,
8
7
7
,
8
9
1
0
,
1
1
Good practice guide for Ambulance Services
and their commissioners
APPENDIX B
EMERGENCY ACCESS ALGORITHM
Appendix B - Emergency Access Algorithm 16
Good practice guide for Ambulance Services
and their commissioners
APPENDIX C
AN EXAMPLE OF A RESOURCE ESCALATORY PLAN
REAP - Resource Escalatory Action Plan
These action cards should be read in conjunction with the WMAS REAP Level Matrix (ver1.2)
Levels 1 to 5
LEVEL 1
Actions
Ensure appropriate EOC cover
Assess RRV staffing, back fill from core other core areas
Ensure RRVs are at standby points
Active liaison with EOC on ambulance standby arrangements
Monitor and manage leave
Monitor and manage mobilisation times
Monitor and manage job cycle times
Monitor and manage activation times
Monitor and manage sickness
Monitor and manage all abstractions
Monitor and manage hours produced
Monitor and manage predicted staffing
Ensure Ops management (GSM and ISO) cover
Ensure proportionate cover of Ambulance vs RRV
Ensure provision of management cover at vulnerable timings (morning/evening changeover
and Fri/Sat evenings until 0400hrs)
Ensure routine mobile management (GSM/ISO) presence at hospitals
Ensure good utilisation of ECPs
Look at predicted single staff and pair-up in advance.
Review predicted RRV cover and fill all gaps. Use singles off other delivery areas as
necessary.
Resource Centres to chase overtime opportunities to staff and bank staff robustly.
EOC to maintain robust dynamic-deployment regime for vehicles.
Consider placing operational management liaison in EOC to manage standby.
17 Appendix C - An Example Of A Resource Escalatory Action Plan `
Good practice guide for Ambulance Services
and their commissioners
Appendix C - An Example Of A Resource Escalatory Action Plan 18
LEVEL 2
Actions as per Level 1, plus
Increase local monitoring at Locality and Divisional level to ensure efficiency
Ensure GSM/ISOs visit busy hospitals regularly
Grant no more short notice leave (under 48 hours)
Critically review abstractions and recall where appropriate
Stringent local monitoring of VOR
Increase focus on EOC staffing
LEVEL 3
Actions as per Level 1 & 2, plus
Consider the use of PTS resources to support A&E operations at critical times
Station Management Teams to cold call staff to encourage extra overtime
Consider if Operational Supervisor staff should only provide cover for vehicles
Training and Education function to provide Trainers for shifts
Cancel non essential meetings.
Operational management to staff vehicles for additional hours
Recall all non essential abstractions
Review planned stadia cover and consider cover options (ie Training Dept cover etc)
Consider extended hours of Fleet Support Services
Consider extended use of VAS
Review non essential training and consider re-scheduling
Consider Logistics / Make Ready to re-equip vehicles at hospitals
Contact St J ohn, Red Cross and PTS for additional vehicles
Place ALOs at busy hospitals to solve issues
Consider non-A/E Ops managers for above role
Consider staffing additional RRVs
Messages to media about pressures and using the Service wisely
LEVEL 4
Actions as per Level 1 & 2 & 3, plus
Establish GOLD Command team to manage recovery
Consider internal Major Incident. Advise SHA & Trust Board
All Operational Managers available managers to be redeployed to staff vehicles
Review planned leave and negotiate rescheduling
Consider buy back of committed leave
Cancel all training for existing staff
Cancel all non-REAP related meetings
All clinically trained staff to return to covering vehicles by default
Good practice guide for Ambulance Services
and their commissioners
19 Appendix C - An Example Of A Resource Escalatory Action Plan
Deploy Doctors to EOC to assist with triage of Cat B/C calls
All non-essential vehicle maintenance / repair to be rescheduled
LMS to provide drivers outside of normal hours to move vehicles as required
Training and Education to provide support by freeing up all clinical staff and vehicle
resources.
Consider placing an Ambulance Liaison Officer in West Mids Police Control at peak
periods - to co-ordinate and advise on Ambulance requests (at peak periods)
Liaison with PCTs to explore options for additional support
Chief Operating Officer to issue bulletin on the position
Use alternative methods to cover all Cat C work (non-response)
Consider mutual aid
LEVEL 5
Actions as per Level 1 & 2 & 3 & 4, plus
Declare internal Major Incident. Advise SHA and Trust Board
Introduce a No Send policy
Consider splitting A&E crews to work with PTS colleague
Implement extensive mutual aid
Cancel all Cat C work. Find other cover for lower priority Cat B work
Cancel all PTS and non essential work and redeploy resources to support A&E ops
Cancel all event and stadia cover
High profile media campaign to discourage inappropriate use
Paramedics/ECPs/Technicians to be authorised to refuse conveyance after assessment
Remove operational vehicles from UOC and re-deploy to EOC
Use trainees to support operations
Open workshops at night to increase daytime fleet
Ops Managers to carry cash float to allow quick solutions
All managers to assist with additional ambulance cover
Good practice guide for Ambulance Services
and their commissioners
Good practice guide for Ambulance Services
and their commissioners
Appendix C - An Example Of A Resource Escalatory Action Plan 20 Appendix C - An Example Of A Resource Escalatory Action Plan 20
Office of the Strategic Health Authorities
Southside, 105 Victoria Street
London SW1E 6QT
T: 020 7932 3700
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Case Study Acute PancreatitisDokument62 SeitenCase Study Acute PancreatitisAilyne A. CleofeNoch keine Bewertungen
- Epilepsy PresentationDokument10 SeitenEpilepsy Presentationapi-346838508Noch keine Bewertungen
- Muscles of MasticationDokument8 SeitenMuscles of MasticationNaisi Naseem100% (1)
- Amberley Fernando: Bachelor of Science in Nutrition - Human Nutrition and Dietetics - GPA 4.0Dokument2 SeitenAmberley Fernando: Bachelor of Science in Nutrition - Human Nutrition and Dietetics - GPA 4.0api-354220446Noch keine Bewertungen
- Mnemonic Devices for Medical EducationDokument9 SeitenMnemonic Devices for Medical EducationJhey MalanyaonNoch keine Bewertungen
- KDIGO AKI Guideline DownloadDokument141 SeitenKDIGO AKI Guideline DownloadSandi AuliaNoch keine Bewertungen
- Concurrent Validity of Two Observer-Rated Alexithymia MeasuresDokument6 SeitenConcurrent Validity of Two Observer-Rated Alexithymia MeasuresLolo LoloNoch keine Bewertungen
- GNMK IMC 20152 A EPlex BrochureDokument4 SeitenGNMK IMC 20152 A EPlex BrochureBilgi KurumsalNoch keine Bewertungen
- AE403BIOMEDICALINSTRUMENTATIONDokument2 SeitenAE403BIOMEDICALINSTRUMENTATIONalwin sozaNoch keine Bewertungen
- 2013 Fluconazole Resistant Candida Albicans.22Dokument8 Seiten2013 Fluconazole Resistant Candida Albicans.22Kala SuvarnaNoch keine Bewertungen
- The Apgar ScoreDokument6 SeitenThe Apgar ScoretiuwangNoch keine Bewertungen
- Clinical MethodsDokument13 SeitenClinical MethodsHashimIdreesNoch keine Bewertungen
- ActonelDokument42 SeitenActonelSimon JonatanNoch keine Bewertungen
- Andre Hannah NursingresumeDokument1 SeiteAndre Hannah Nursingresumeapi-450112281Noch keine Bewertungen
- Dall Miles Surgical ProtocolDokument16 SeitenDall Miles Surgical Protocolfarnaz_2647334Noch keine Bewertungen
- A+P CHP 15 QuizDokument8 SeitenA+P CHP 15 QuizGennaroNoch keine Bewertungen
- 'NEXtCARE UAE - ASOAP FormDokument1 Seite'NEXtCARE UAE - ASOAP FormMohyee Eldin RagebNoch keine Bewertungen
- Smith Medical - H-1200 Fast Fluid WarmerDokument78 SeitenSmith Medical - H-1200 Fast Fluid WarmerVictor ȘchiopuNoch keine Bewertungen
- LFD 15 IudmcDokument2 SeitenLFD 15 IudmcMaria Elvira Abrogena DuadNoch keine Bewertungen
- StaphylococciDokument25 SeitenStaphylococcichikitsakNoch keine Bewertungen
- Topographical Relationship of The Greater Palatine Artery and The Palatal Spine. Significance For Periodontal SurgeryDokument13 SeitenTopographical Relationship of The Greater Palatine Artery and The Palatal Spine. Significance For Periodontal SurgerycristianNoch keine Bewertungen
- B Braun Ra - CatalogueDokument21 SeitenB Braun Ra - CatalogueDina Friance ManihurukNoch keine Bewertungen
- Laporan - Pendahuluan PJK FixDokument8 SeitenLaporan - Pendahuluan PJK FixNndaydnaNoch keine Bewertungen
- Relationship Between Patients Perceptions of Care.3Dokument9 SeitenRelationship Between Patients Perceptions of Care.3inno semuNoch keine Bewertungen
- Focus ChartingDokument46 SeitenFocus ChartingIsmail Alnemr100% (5)
- The Role of Dispensers in The Rational Use of DrugsDokument19 SeitenThe Role of Dispensers in The Rational Use of DrugsAci LusianaNoch keine Bewertungen
- Pediatric Fluid and Electrolyte AlterationsDokument51 SeitenPediatric Fluid and Electrolyte AlterationsMatthew Ryan100% (1)
- Psyche 4 AnxietyDokument37 SeitenPsyche 4 AnxietysimplyrosalynNoch keine Bewertungen
- Medical Massage ManualDokument3 SeitenMedical Massage ManualPeter Sosa100% (1)
- Igas Flow ChartDokument1 SeiteIgas Flow ChartYi Wei KoNoch keine Bewertungen