Beruflich Dokumente
Kultur Dokumente
The Laryngoscope Volume 118 Issue 10 2008 (Doi 10.1097 - Mlg.0b013e31817d9cd5) Alfio Ferlito Alessandra Rinaldo - Is Radical Neck Dissection A Current Option For Neck Disease
Hochgeladen von
Ram Mohan0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
27 Ansichten2 Seitenmaking
Originaltitel
The Laryngoscope Volume 118 Issue 10 2008 [Doi 10.1097_mlg.0b013e31817d9cd5] Alfio Ferlito; Alessandra Rinaldo -- Is Radical Neck Dissection a Current Option for Neck Disease
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenmaking
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
27 Ansichten2 SeitenThe Laryngoscope Volume 118 Issue 10 2008 (Doi 10.1097 - Mlg.0b013e31817d9cd5) Alfio Ferlito Alessandra Rinaldo - Is Radical Neck Dissection A Current Option For Neck Disease
Hochgeladen von
Ram Mohanmaking
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 2
The Laryngoscope
Lippincott Williams & Wilkins
2008 The American Laryngological,
Rhinological and Otological Society, Inc.
Is Radical Neck Dissection a Current Option
for Neck Disease?
Alfio Ferlito, MD, FRCS, FACS; Alessandra Rinaldo, MD, FACS
For many years after the first description of a suc-
cessful en bloc neck dissection by the Polish surgeon Jaw-
dyn ski
1
in 1888, this procedure was the only operation
accepted for the surgical treatment of the neck in patients
with cancer of the head and neck staged N0 or otherwise.
The operation he described has come to be known as the
radical neck dissection (RND). This surgical procedure
was strongly advocated by Crile in the early 20th centu-
ry
24
and well established by Martin et al.
5
in the 1950s.
The term RND has been accepted by the Committee for
Neck Classification of the American Head and Neck Soci-
ety.
68
The Japan Neck Dissection Study Group recently
termed this surgical treatment as total neck dissection.
9
RND includes removal of all ipsilateral cervical
lymph node groups extending from the inferior border of
the mandible above, to the clavicle below, and from the
lateral border of the sternohyoid muscle, the hyoid bone,
and the contralateral anterior belly of the digastric muscle
anteriorly, to the anterior border of the trapezius muscle
posteriorly. It includes all lymph node groups from levels
I to V (the submental group, the submandibular group, the
upper jugular group, the middle jugular group, the lower
jugular group, and the posterior triangle group). The spi-
nal accessory nerve, the internal jugular vein, the sterno-
cleidomastoid muscle, the submandibular gland, the tail
of parotid gland, and the cervical plexus nerves are all
removed. RND does not include removal of the suboccipi-
tal nodes, periparotid nodes (except intraparotid nodes
located in the posterior aspect of the submandibular tri-
angle), buccinator nodes, retropharyngeal nodes, and mid-
line visceral (anterior compartment) nodes.
7
RND there-
fore is the dissection of all the lymph node levels and
sublevels of the lateral neck.
At present, conventional RND and modified RND
(MRND) are no longer indicated for elective neck dissec-
tion. The cancers of the head and neck do not involve all
levels and sublevels of the lateral neck. In particular,
RND is an overtreatment for N0 and Ndisease. Sublevel
IA is usually not involved in advanced tumors of the
larynx, hypopharynx, oropharynx, nasopharynx, parotid
gland, submandibular gland, thyroid gland, parathyroid
gland, trachea, and cervical esophagus. There is no pri-
mary cancer of the head and neck in which there is a high
risk for involvement of sublevels IA and IB, IIA and IIB,
VA and VB, and levels III and IV. In particular, the absence
of metastases in sublevel IA and/or in sublevel VB does not
justify a comprehensive dissection including levels I to V in
patients with primary cancer of the head and neck.
A strong trend exists in support of selective neck
dissection being implemented as an oncologically safe and
effective procedure for multiple N disease while limiting
morbidity.
The classic RND has been used for advanced-stage
nodal metastases from head and neck cancer followed by
adjuvant postoperative radiation therapy combined or not
with concomitant chemotherapy. The specific indications
were patients with N3 disease, extensive soft tissue dis-
ease either appreciated clinically or demonstrated radio-
logically. In cases with N3 neck disease, RND may not be
sufficient. These patients remain at the highest risk for
the development of local recurrence and distant metasta-
ses.
10
The prognosis is usually poor. It is also important to
remember that a large number of patients with advanced
neck disease are not suitable candidates for aggressive
treatment because of their clinical status or associated
comorbidities and are, as a consequence, submitted to
radiation therapy alone.
10
Patients with advanced N stages are currently
treated initially with nonsurgical methods, usually with
concomitant combinations of chemotherapy and irradia-
tion. After the introduction of organ preservation strat-
egies, with various combinations using chemoradiother-
apy for definitive treatment of advanced locoregional
cancer of the larynx and pharynx, there is emerging trend
toward performing planned neck dissection for bulky cer-
vical lymphadenopathy. The regional disease control for
patients with persistent neck disease using selective and
superselective neck dissections for advanced N2 and N3
disease after concurrent chemoradiation is excellent.
1118
There is ample evidence in the literature that concom-
itant or concurrent radiochemotherapy can achieve
From the Department of Surgical Sciences, ENT Clinic, University
of Udine, Udine, Italy.
Editors Note: This Manuscript was accepted for publication April
24, 2008.
Send correspondence to Alfio Ferlito, MD, FRCS, FACS, Director of
the Department of Surgical Sciences, Professor and Chairman of the ENT
Clinic, University of Udine, Policlinico Universitario, Piazzale S. Maria
della Misericordia, I-33100 Udine, Italy. E-mail: a.ferlito@uniud.it
DOI: 10.1097/MLG.0b013e31817d9cd5
Laryngoscope 118: October 2008 Editorial
1717
good regional control in patients with advanced neck dis-
ease. However, the development of distant metastases
does remain a problem, despite the administration of sys-
temic therapy.
11
The technique of selective neck dissection has also
expanded to include removal of one or more of the non-
lymphatic structures routinely included in the MRND or
RND (i.e., sternocleidomastoid muscle, internal jugular
vein, spinal accessory nerve). The structures most fre-
quently sacrificed are the submandibular salivary gland
and the internal jugular vein.
19,20
Medina et al.
21
recently investigated the feasibility of
performing a single-level dissection in patients with
head and neck cancer treated with radiation therapy with
or without chemotherapy. The results confirmed the effec-
tiveness of selective neck dissection in the management of
residual disease in the neck.
The majority of patients who present squamous car-
cinoma in the neck with an unknown primary have N2 or
N3 neck disease, stage IV head and neck cancer. The
standard treatment choice has been RND followed by ra-
diation therapy; however, the current treatment is a com-
bination of chemoradiation therapy with neck dissection
reserved for salvage purposes. The usage of the RND, even
for advanced neck disease with unknown primary tumor,
is generally unnecessary because all the five neck levels
are rarely involved. At present, the use of RND has be-
come greatly limited and this surgical procedure is no
longer standard.
22
BIBLIOGRAPHY
1. Jawdyn ski F. Przypadek raka pierwotnego szyi. t.z. raka
skrzelowego Volkmanna. Wycie cie nowotworu wraz z
rezekcyja tetnicy szyjowej wspolnej i zyy szyjowej wewn-
etrznej. Wyzdrowienie. Gaz Lek 1888;8:530537, 554560,
582587.
2. Crile GW. On the surgical treatment of cancer of the head and
neck. With a summary of one hundred and twenty-one
operations performed upon one hundred and five patients.
Trans South Surg Gynecol Assoc 1905;18:108127.
3. Crile G. Excision of cancer of the head and neck. With
special reference to the plan of dissection based on one
hundred and thirty-two operations. JAMA 1906;47:
17801786.
4. Silver CE, Rinaldo A, Ferlito A. Criles neck dissection.
Laryngoscope 2007;117:19741977.
5. Martin H, Del Valle B, Ehrlich H, Cahan WG. Neck dissec-
tion. Cancer 1951;4:441499.
6. Robbins KT, Medina JE, Wolfe GT, Levine PA, Sessions RB,
Pruet CW. Standardizing neck dissection terminology. Of-
ficial report of the Academys Committee for Head and
Neck Surgery and Oncology. Arch Otolaryngol Head Neck
Surg 1991;117:601605.
7. Robbins KT, Clayman G, Levine PA, et al. Neck dissection
classification update: revisions proposed by the American
Head and Neck Society and the American Academy of
Otolaryngology-Head and Neck Surgery. Arch Otolaryngol
Head Neck Surg 2002;128:751758.
8. Robbins KT, Shaha AR, Medina JE, et al. Consensus statement
on the classification and terminology of neck dissection. Arch
Otolaryngol Head Neck Surg. 2008;134:536538.
9. Hasegawa Y, Saikawa M, Hayasaki K, et al. A new classifi-
cation and nomenclature system for neck dissections: a
proposal by the Japan Neck Dissection Study Group
(JNDSG). Jpn J Head Neck Cancer 2005;31:7178.
10. Ferlito A, Silver CE, Shaha AR, Rinaldo A. Management of
N3 neck. Acta Otolaryngol 2002;122:230233.
11. Frank DK, Hu KS, Culliney BE, et al. Planned neck dissec-
tion after concomitant radiochemotherapy for advanced
head and neck cancer. Laryngoscope 2005;115:10151020.
12. Robbins KT, Wong FSH, Kumar P, et al. Efficacy of targeted
chemoradiation and planned selective neck dissection to control
bulky nodal disease in advanced head and neck cancer. Arch
Otolaryngol Head Neck Surg 1999;125:670675.
13. Stenson KM, Haraf DJ, Pelzer H, et al. The role of cervical
lymphadenectomy after aggressive concomitant chemora-
diotherapy: the feasibility of selective neck dissection. Arch
Otolaryngol Head Neck Surg 2000;126:950956.
14. Robbins KT, Doweck I, Samant S, Vieira F. Effectiveness of
superselective and selective neck dissection for advanced
nodal metastases after chemoradiation. Arch Otolaryngol
Head Neck Surg 2005;131:965969.
15. Robbins KT, Ferlito A, Suarez C, et al. Is there a role for selective
neck dissection after chemoradiation for head and neck cancer?
[Editorial]. J Am Coll Surg 2004;199:913916.
16. Robbins KT, Shannon K, Vieira F. Superselective neck dis-
section after chemoradiation: feasibility based on clinical
and pathologic comparisons. Arch Otolaryngol Head Neck
Surg 2007;133:486489.
17. Nouraei SA, Upile T, Al-Yaghchi C, et al. Role of planned
postchemoradiotherapy selective neck dissection in the
multimodality management of head and neck cancer. La-
ryngoscope 2008;118:797803.
18. Stenson KM, Huo D, Blair E, Cohen EE, Argiris A, Haraf DJ,
Vokes EE. Planned post-chemoradiation neck dissection: signif-
icance of radiation dose. Laryngoscope 2006;116:3336.
19. Pellitteri PK, Robbins KT, Neuman T. Expanded application
of selective neck dissection with regard to nodal status.
Head Neck 1997;19:260265.
20. Ferlito A, Rinaldo A, Silver CE, et al. Elective and therapeu-
tic selective neck dissection. Oral Oncol 2006;42:1425.
21. Medina JE, Vasan NR, Krempl GA. Management of the neck
after treatment with radiation with or without chemother-
apy. Curr Treat Options Oncol 2007;8:261264.
22. Ferlito A, Kowalski LP, Byers RM, et al. Is the standard
radical neck dissection no longer standard? [Guest Edito-
rial]. Acta Otolaryngol 2002;122:792795.
Laryngoscope 118: October 2008 Editorial
1718
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Links To Dental WebsitesDokument2 SeitenLinks To Dental WebsitesRam MohanNoch keine Bewertungen
- Indication of Radiotherapy After Neck DissectionDokument7 SeitenIndication of Radiotherapy After Neck DissectionKumaran Bagavathi RagavanNoch keine Bewertungen
- The Masseteric Nerve: A Versatile Power Source in Facial Animation TechniquesDokument6 SeitenThe Masseteric Nerve: A Versatile Power Source in Facial Animation TechniquesRam MohanNoch keine Bewertungen
- Case Presentation Pre OperativeDokument1 SeiteCase Presentation Pre OperativeRam MohanNoch keine Bewertungen
- Review of The Management of Chylous Fistula As A Complication of Neck DissectionDokument1 SeiteReview of The Management of Chylous Fistula As A Complication of Neck DissectionRam MohanNoch keine Bewertungen
- Journal of Oral and Maxillofacial Surgery Volume 40 Issue 11 1982 [Doi 10.1016_0278-2391(82)90145-8] Troxell, James B.; Fonseca, Raymond J.; Osbon, Donald B. -- A Retrospective Study of Alveolar Cleft GraftingDokument5 SeitenJournal of Oral and Maxillofacial Surgery Volume 40 Issue 11 1982 [Doi 10.1016_0278-2391(82)90145-8] Troxell, James B.; Fonseca, Raymond J.; Osbon, Donald B. -- A Retrospective Study of Alveolar Cleft GraftingRam MohanNoch keine Bewertungen
- Adjuvant AnalgesicsDokument1 SeiteAdjuvant AnalgesicsRam MohanNoch keine Bewertungen
- Human Stem Cells and Tooth Regeneration 2157 7633.1000e107Dokument2 SeitenHuman Stem Cells and Tooth Regeneration 2157 7633.1000e107Ram MohanNoch keine Bewertungen
- @@complications of Facial FracturesDokument5 Seiten@@complications of Facial FracturesRam MohanNoch keine Bewertungen
- Stem CellDokument9 SeitenStem CellMbew HadiNoch keine Bewertungen
- SD Article HJDokument9 SeitenSD Article HJRam MohanNoch keine Bewertungen
- New Text DocumentDokument1 SeiteNew Text DocumentRam MohanNoch keine Bewertungen
- S0901502713X00086 S0901502712004833 MainDokument4 SeitenS0901502713X00086 S0901502712004833 MainRam MohanNoch keine Bewertungen
- Role of Tissue Engineering in Oral and Maxillofacial Reconstruction: Findings of The 2005 AAOMS Research SummitDokument8 SeitenRole of Tissue Engineering in Oral and Maxillofacial Reconstruction: Findings of The 2005 AAOMS Research SummitRam MohanNoch keine Bewertungen
- New Text DocumentDokument1 SeiteNew Text DocumentRam MohanNoch keine Bewertungen
- Higher Algebra - Hall & KnightDokument593 SeitenHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Higher Algebra - Hall & KnightDokument593 SeitenHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Higher Algebra - Hall & KnightDokument593 SeitenHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Higher Algebra - Hall & KnightDokument593 SeitenHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- 13-Case Report - Pindborg TumorDokument2 Seiten13-Case Report - Pindborg TumorRam MohanNoch keine Bewertungen
- Apartheid in South AfricaDokument24 SeitenApartheid in South Africaapi-300093410100% (1)
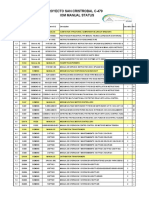
- Proyecto San Cristrobal C-479 Iom Manual StatusDokument18 SeitenProyecto San Cristrobal C-479 Iom Manual StatusAllen Marcelo Ballesteros LópezNoch keine Bewertungen
- Apply Study and Learning SkillsDokument58 SeitenApply Study and Learning SkillsSelf-DeveloperNoch keine Bewertungen
- Right To Freedom From Torture in NepalDokument323 SeitenRight To Freedom From Torture in NepalAnanta ChaliseNoch keine Bewertungen
- Klarna: Klarna A Company Valued To Be 5.5 Billion and 8 Most Valued Fintech Company in The WorldDokument1 SeiteKlarna: Klarna A Company Valued To Be 5.5 Billion and 8 Most Valued Fintech Company in The WorldChetan NarasannavarNoch keine Bewertungen
- Rapidjson Library ManualDokument79 SeitenRapidjson Library ManualSai Kumar KvNoch keine Bewertungen
- Correlation SecretDokument23 SeitenCorrelation SecretDavid100% (1)
- Systems Analysis and Design 11th Edition Tilley Test BankDokument15 SeitenSystems Analysis and Design 11th Edition Tilley Test Banksusanschroederoqdrkxtafn100% (15)
- Checklist of Requirements of Special Land Use PermitDokument1 SeiteChecklist of Requirements of Special Land Use PermitAnghelita ManaloNoch keine Bewertungen
- Ingrid Gross ResumeDokument3 SeitenIngrid Gross Resumeapi-438486704Noch keine Bewertungen
- Citibank Vs Hon ChuaDokument12 SeitenCitibank Vs Hon ChuaJA BedrioNoch keine Bewertungen
- PFASDokument8 SeitenPFAS王子瑜Noch keine Bewertungen
- 11 PJBUMI Digital Data Specialist DR NOOR AZLIZADokument7 Seiten11 PJBUMI Digital Data Specialist DR NOOR AZLIZAApexs GroupNoch keine Bewertungen
- Presbuteroi (Elders) and Episkopoi (Overseers) and Are Described in 1 Tim 3 and TitusDokument15 SeitenPresbuteroi (Elders) and Episkopoi (Overseers) and Are Described in 1 Tim 3 and TitusNimaro Brenda100% (1)
- Characteristics of Pop CultureDokument3 SeitenCharacteristics of Pop Culturekhimamad02Noch keine Bewertungen
- Manual de Utilizare ProSpray 3.20 Airless SpraypackDokument88 SeitenManual de Utilizare ProSpray 3.20 Airless Spraypackjohnny angeles ñiquenNoch keine Bewertungen
- ARCHESDokument10 SeitenARCHESCaroline MugureNoch keine Bewertungen
- 2beloved Lizzo PDFDokument1 Seite2beloved Lizzo PDFAntwerpQueerChoir AQCNoch keine Bewertungen
- 4h Thank You ProofDokument1 Seite4h Thank You Proofapi-362276606Noch keine Bewertungen
- Eva Karene Romero (Auth.) - Film and Democracy in Paraguay-Palgrave Macmillan (2016)Dokument178 SeitenEva Karene Romero (Auth.) - Film and Democracy in Paraguay-Palgrave Macmillan (2016)Gabriel O'HaraNoch keine Bewertungen
- Official Memo: From: To: CCDokument4 SeitenOfficial Memo: From: To: CCrobiNoch keine Bewertungen
- HARRISON 1993 - The Soviet Economy and Relations With The United States and Britain, 1941-45Dokument49 SeitenHARRISON 1993 - The Soviet Economy and Relations With The United States and Britain, 1941-45Floripondio19Noch keine Bewertungen
- Due Date: 29-12-2021: Fall 2021 MTH104: Sets and Logic Assignment No. 1 (Lectures # 16 To 18) Total Marks: 10Dokument3 SeitenDue Date: 29-12-2021: Fall 2021 MTH104: Sets and Logic Assignment No. 1 (Lectures # 16 To 18) Total Marks: 10manzoor ahmadNoch keine Bewertungen
- Ode To The West Wind Text and AnalysisDokument7 SeitenOde To The West Wind Text and AnalysisAbdullah HamzaNoch keine Bewertungen
- Net Present Value AnalysisDokument6 SeitenNet Present Value AnalysisAmna Khalid100% (1)
- PT3 Liste PDFDokument2 SeitenPT3 Liste PDFSiti KamalNoch keine Bewertungen
- Financial Accounting Theory Craig Deegan Chapter 7Dokument9 SeitenFinancial Accounting Theory Craig Deegan Chapter 7Sylvia Al-a'maNoch keine Bewertungen
- FCI - GST - Manual On Returns and PaymentsDokument30 SeitenFCI - GST - Manual On Returns and PaymentsAmber ChaturvediNoch keine Bewertungen
- Basic OmDokument242 SeitenBasic OmRAMESH KUMARNoch keine Bewertungen
- History of Architecture VI: Unit 1Dokument20 SeitenHistory of Architecture VI: Unit 1Srehari100% (1)














































![Journal of Oral and Maxillofacial Surgery Volume 40 Issue 11 1982 [Doi 10.1016_0278-2391(82)90145-8] Troxell, James B.; Fonseca, Raymond J.; Osbon, Donald B. -- A Retrospective Study of Alveolar Cleft Grafting](https://imgv2-1-f.scribdassets.com/img/document/235740563/149x198/e7f1765f1b/1407075026?v=1)