Beruflich Dokumente
Kultur Dokumente
Diabetic Placenta: Ultrastructure and Morphometry of The Term Villi
Hochgeladen von
klapouschakOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Diabetic Placenta: Ultrastructure and Morphometry of The Term Villi
Hochgeladen von
klapouschakCopyright:
Verfügbare Formate
239
OBJECTIVE: To verify the ultrafine conformation of
term villi in diabetic and normal placentae. Villar dys-
maturity and chorangiosis are considered the most fre-
quent findings in diabetic placentae, but their histogene-
sis is still unclear.
STUDY DESIGN: We performed a morphometric study
of 38 term villi in 5 diabetic placentae and of 37 term villi
of 5 normal placentae in order to know the different ex-
tension of endothelial surface (VL), the maximum (D
max) and minimum (D min) distance of the vessels from
the basal membrane, as well as the exact thickness of basal
membrane (MT BM). The villi were examined with
transmission electron microscopy, and parameters were
automatically acquired with the iTEM software (Soft
Imaging System, Mnster, Germany).
RESULTS: VL results were statistically higher in dia-
betic placentae than in normal ones. Also D max and D
min were higher in diabetic disease. MT BM was not dif-
ferent in the two groups.
CONCLUSION: Our findings show that, in the pres-
ence of chorangiosis, the vessel surface in diabetic pla-
centae is higher than in normal group, but the vessels are
randomly distributed in term villi. The basal membrane
is not different in the two groups. Morphometric evalua-
tion seems to be more accurate using ultrafine samples.
(Anal Quant Cytopathol Histopathol 2012;34:239
247)
Keywords: diabetes, placenta, ultrastructure, villi.
Diabetes in pregnancy can lead to severe conse-
quences both for mother and fetus. Many studies
therefore aim to identify the macroscopic and his-
tological characteristics of the placenta during dia-
betes in order to correlate such variations with the
pathogenesis of the most common complications:
fetal macrosomia, sudden fetal death, onset of pre-
eclampsia.
Many of these studies have produced contrasting
results, although the features most often highlight-
ed in the literature include chorangiosis
1
and a vil-
lous immaturity, known as dysmaturity, featuring
enlarged villi with many capillaries often arranged
irregularly and not adjacent to the trophoblast.
2
Moreover, morphometric analysis has provided
unclear results. There are basically two key factors
Analytical and Quantitative Cytopathology and Histopathology
0884-6812/12/3405-0239/$18.00/0 Science Printers and Publishers, Inc.
Analytical and Quantitative Cytopathology and Histopathology
Diabetic Placenta
Ultrastructure and Morphometry of the Term Villi
Roberta Rossi, Ph.D., Giovanni Scillitani, Ph.D., Antonella Vimercati, M.D.,
Maria G. Fiore, M.D., Maria Mastrodonato, B.Sc., and Leonardo Resta, M.D.
From the Departments of Pathological Anatomy, of Biology, and of Obstetrics, Gynecology and Neonatology, University of Bari Aldo
Moro, Bari, Italy.
Dr. Rossi is Researcher, Department of Pathological Anatomy.
Drs. Scillitani and Mastrodonato are Aggregate Professors, Section of Animal and Environmental Biology, Department of Biology.
Dr. Vimercati is Aggregate Professor, Department of Obstetrics, Gynecology and Neonatology.
Dr. Fiore is Aggregate Professor, Department of Pathological Anatomy.
Dr. Resta is Professor, Department of Pathological Anatomy.
Address correspondence to: Leonardo Resta, M.D., Department of Pathological Anatomy, University of Bari Aldo Moro, Policlinico,
Pz. Giulio Cesare, 11, 70124 Bari, Italy (lresta@anatopat.uniba.it).
Financial Disclosure: The authors have no connection to any companies or products mentioned in this article.
A
R
T
I
C
L
E
S
underlying this lack of agreement: the pathogenetic
heterogeneity of the clinical entity diabetes in
pregnancy and the extreme heterogeneity of the
morphometric techniques used.
As is well known, diabetes can either develop
during pregnancy or be preexisting. Especially in
the latter case, at the onset of pregnancy the usual
complications may already be present, especially
vascular ones, with serious consequences for the
development of the placenta. The severity of the di-
abetes affects the evolution of the pregnancy. In this
regard, there is much debate over the definition of
diabetes mellitus: fasting plasma glucose levels >90
mg/dL and/or 2 hours postprandial plasma glu-
cose >130 mg/dL (glucose profile [GP]) or the
value measured in the glucose tolerance test, fol-
lowing oral administration of 100 g glucose (oral
glucose tolerance test [OGTT]), or a combination of
these two values. Finally, as diabetes is now fairly
well controlled among populations in developed
nations using pharmacological or insulin-based
treatment, many classic pregnancy complications
have become rare.
The aim of our study is to evaluate a small num-
ber of significant parameters in terms of the effi-
ciency of terminal vascularization by comparing
villi from normal placentae and those from diabetes
mellitus, using preparations observed under the
transmission electron microscope, in order to ob-
tain a more precise assessment.
Materials and Methods
In each case we examined a minimum of 3 and a
maximum of 5 samples, from which we selected
510 villi on the basis of the villi to be cut. The study
was carried out on 5 villous samples of diabetic pla-
centae and 5 of normal placentae.
The women with diabetes were from 2439 years
old. The gestational period ranged from 3941
weeks. These included 3 cases of type 1 diabetes
(one White class A and two class C) and 2 cases of
gestational diabetes. All of the patients were receiv-
ing insulin treatment, so their glucose profile in the
last weeks of pregnancy was fairly low (ranging
from 6576 to 108114 mg/dL). In 4 cases birth was
by cesarean section, with the remaining one by
vacuum extraction. Birth weight varied from 2900
4550 g. The infants were in good condition (Apgars
78), and only one child had a recto-cutaneous
fistula. The placentae weighed between 520 g and
850 g.
The 5 women with normal pregnancies ranged in
age from 3136 years and were in weeks 3641 of
pregnancy. Pregnancy had not been complicated
by any anomalies, especially as regards to glucose
values and arterial blood pressure. The newborn
infants were of normal weight (range, 27003050 g)
with Apgars of 710 in their first minute. Placenta
weight ranged from 430520 g.
Morphological Analysis
A full-thickness slice of the placenta was performed
immediately in the delivery room at the time of de-
livery, and some (n=57) 12 mm fragments ob-
tained from different areas of this slice were readily
fixed in 2.5% phosphate-buffered glutaraldehyde
(pH 7.4) for 4 hours. After repeated washings in
phosphate buffer, the samples were post-fixed in
1% phosphate-buffered OsO4 for another 2 hours.
They were then dehydrated and embedded in
epoxy resin.
The semithin sections, thickness 1 m, were
stained with toluidine blue borate. Four ultrathin
sections (5060 nm) per case were mounted on a
copper grid, then stained routinely with uranyl
acetate and lead citrate, and finally observed under
a Morgagni 268 transmission electron microscope
(TEM) (FEI Company, Hillsboro, Oregon, U.S.A.).
The remaining placenta was fixed in neutral
buffered formalin at pH 7 for 2448 hours. Six full-
thickness biopsies were taken from the maternal
and from the fetal surfaces (3 central and 3 periph-
eral), washed under running water, dehydrated
and embedded in paraffin using common histolog-
ical techniques. Five-mthick sections were de-
paraffined and stained with hematoxylin-eosin,
PAS and Massons trichrome stain. Some of the sec-
tions were incubated with CD34 for the study of vil-
lous vascularization.
Morphometric Analysis
Ultrastructural examination of each placenta sam-
ple under the TEM was used to randomly select the
terminal villi highlighted on each grid. Two digital-
ized images were acquired of each villus at magni-
fications of 1,800 and 4,400, respectively. A total
of 38 villi were studied in the group of diabetic
placentae, and 37 villi were studied in the control
group.
The morphometric measurements were carried
out using the Morgagni 268s built-in iTEM soft-
ware (Soft Imaging System, Mnster, Germany).
The parameters acquired were as follows: (1) inner
surface length of capillaries (VL), (2) minimum dis-
240 Analytical and Quantitative Cytopathology and Histopathology
Rossi et al
tance between the basement membrane of the out-
ermost capillary and the basement membrane of the
trophoblast (D MIN), (3) minimum distance be-
tween the basement membrane of the innermost
capillary and the basement membrane of the tro-
phoblast (D MAX) (Figure 1) and (4) mean thick-
ness of the trophoblast basement membrane (MT
BM).
The first 3 parameters were assessed using the
images with a magnification of 1,800, and the last
parameter using a magnification of 4,400. In addi-
tion to original magnification the program iTEM al-
lows the magnification to be increased to improve
accuracy via the function zoom.
VL was measured using the iTEM softwares
electronic pointer to trace the internal contour of the
vessel endothelium; once completed, the automatic
calibration carried out by the software when ac-
quiring the image provides the measurement in
microns. Five consecutive measurements were
carried out for each vessel, after which the mean
was calculated, in order to limit any measurement
errors.
D MIN (Figure 1) for the vessel closest to the
villus surface was measured using the softwares
dedicated function, indicating the two points re-
quired and leaving the software to carry out the
measurements automatically. Again, five consecu-
tive measurements for each vessel were carried out.
The measurements were carried out on more capil-
laries to find the one with minimum distance to BM.
The same technique was used to assess the maxi-
mum distance for the capillary furthest from the
villus surface. These measures also were found
comparing different capillaries (at least 10 measure-
ments).
MT BM was assessed using the 4,400 images. A
series of at least 10 measurements was carried out
for each villus using the softwares electronic point-
er and obtaining the corresponding values. In meas-
uring the thickness of the basement membrane, we
excluded areas subject to pathological submembra-
nous protein accumulation typically found in dia-
betic placentae.
Statistical Evaluation
Statistical analyses were performed for each vari-
able among single cases as well as between the
groups resulting from the pooling of all the data
from controls and diabetics, respectively. Details
and references about the tests can be found in
Riffenburgh.
3
Basic statistics (arithmetic mean,
variance, coefficient of variation) were computed
for each case as well as for pooled controls and
diabetic cases. Preliminary tests of departure from
normality (Shapiro-Wilk, Anderson-Darling) were
computed. Equality of variances among cases was
estimated by Levenes test. Comparisons of means
among cases for each variable were performed
by both parametric (ANOVA) and nonparametric
(Kruskal-Wallis) tests. Comparisons of means were
also performed between pooled control and dia-
betic groups by Students t test (parametric) and
Mann-Whitney U-test (nonparametric). Control
cases did not differ significantly for age of mother
or birth weight, whereas in the diabetic group some
differences were observed. In particular, cases 3
and 4 were between 24 and 27 years old compared
to >30 in the others, and birth weights in cases 2
and 3 were >4,000 g, compared to about 3,000 g
in the others. Thus, we tested with the aforesaid
methods whether these differences were significant
within the diabetic cases pooled by age and birth
weight prior to comparing them with the controls.
Means and related standard-error intervals for each
variable were plotted for visual comparisons be-
tween cases. For each analysis the value of the
estimated probability to reject the null hypothesis
was set to p<0.01.
Results
Morphological analysis showed that the normal
placentae contained mature intermediate villi and
Volume 34, Number 5/October 2012 241 Diabetic Placenta
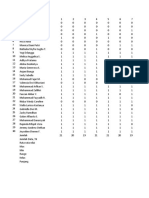
Figure 1 Ultrastructural appearance of term villous in diabetic
placenta. Several capillary vessels at different distances from
basal membrane are present. Arrows show the value of D MIN
and D MAX (minimum distance and maximum distance).
Original magnication 4,400.
regular terminal villi, with a normal connective
vascular stroma and maturation of the vasculosyn-
cytial membranes. The terminal villus usually con-
tained 24 capillaries, close to the trophoblast base-
ment membrane.
In diabetic placentae, mature intermediate villi
and terminal villi were sometimes found to be
thicker, with edematous stroma, having some ves-
sels with smaller diameters and distributed at vary-
ing distances from the surface of the villus.
Details on the quantity and distribution of the
capillary vessels in mature terminal intermediate
villi were more evident when assessing the prepa-
rations subject to immunohistochemical CD34 re-
action. Even smaller vessels became visible due to
the antibody reaction of the endothelia.
Basic statistics for each variable in single and
pooled cases are shown in Tables IIV, as well as the
tests for departure from normality and the associat-
ed probabilities. Mean values tended to be higher in
diabetics. Table V shows the results of Levenes test
for equality of variances. In general, data are dis-
tributed normally in the single cases but not in the
pooled ones (except for VL in controls). Variances
of VL and D MIN (pooled cases only) do not differ
significantly, whereas variance for D MAX is signif-
icantly higher in the diabetic and that for MT BM is
significantly higher in controls. Tests for significant
differences within diabetic cases pooled according
to mothers age and birth weight for each variable
(Table VI) did not reject the null hypothesis, the
probabilities associated with both t test and U test
being always >0.01. Thus, all the diabetic cases
were used in the following comparisons with the
controls. Table VII reports the results of tests for the
comparison of means. ANOVA and Kruskal-Wallis
agreed in finding significant differences among
single cases for VL, D MIN and D MAX, and no
differences for MT BM. In the comparisons between
pooled controls and diabetic cases, both Students t
test and Mann-Whitney U test found significant dif-
ferences for VL and D MAX and no differences for
MT BM, whereas they disagreed for D MIN, since
Mann-Whitney U test was significant, but not
Students t test. Figure 2 shows the plot of means
and standard errors in single and pooled cases for
each variable. In VL, D MIN and D MAX values for
controls tend to be lower, even if single cases in
controls can attain values similar to or higher than
diabetics (like controls 1 and 2 for VL and control 5
for D MIN). In MT BM no trends are seen, with val-
ues for controls and diabetics falling in about the
same range.
Discussion
The overall appearance of the diabetic placentae ob-
served are in agreement with previous findings in
the literature.
4-7
The most characteristic associated
condition is known as dysmaturity, a relative and
focal immaturity of the mature intermediate villi
with edema and swelling of the villi. Another
aspect of note is chorangiosis, i.e., the presence of
numerous tiny capillary vessels across the villous
cross-section surface, even at a certain distance
from the villous surface itself. Observation using
the CD34 immunohistochemical reaction without
doubt highlights the different number and location
of the vessels.
Various attempts at morphometric studies of the
diabetic placenta have been carried out using dif-
242 Analytical and Quantitative Cytopathology and Histopathology
Rossi et al
Table I Descriptive Statistics for the Variable VL
Case N Mean (minmax) Variance CV S-W A-D
Control 1 7 126.076 (62.110182.750) 1738.272 0.331 0.976 (0.939) 0.162 (>0.15)
Control 2 8 152.150 (96.460227.030) 2216.834 0.309 0.951 (0.716) 0.190 (>0.15)
Control 3 7 87.710 (43.400141.940) 1374.091 0.423 0.946 (0.697) 0.209 (>0.15)
Control 4 10 94.292 (50.310177.100) 1203.177 0.368 0.825 (0.029) 0.865 (0.016)
Control 5 5 52.694 (31.470103.480) 899.496 0.569 0.789 (0.066) 0.549 (0.075)
Controls (pooled) 37 105.948 (31.470227.030) 2399.956 0.462 0.962 (0.234) 0.439 (>0.15)
Diabetic 1 8 129.955 (49.560194.200) 2179.790 0.359 0.961 (0.824) 0.230 (>0.15)
Diabetic 2 8 133.530 (57.770165.800) 1480.844 0.288 0.841 (0.078) 0.560 (0.100)
Diabetic 3 7 171.284 (91.050359.550) 9846.827 0.579 0.841 (0.102) 0.497 (0.139)
Diabetic 4 7 127.561 (52.520182.820) 2484.713 0.391 0.949 (0.700) 0.207 (>0.15)
Diabetic 5 8 147.487 (58.790325.820) 6438.316 0.544 0.831 (0.082) 0.623 (0.061)
Diabetics (pooled) 38 141.571 (49.560359.550) 4165.018 0.456 0.876 (0.001) 1.106 (<0.01)
CV = coefcient of variation, N = sample size, min = minimum value recorded in the sample, max = maximum value recorded in the sample, S-W = Shapiro-
Wilk test for the normality of distribution (associated probability in brackets), A-D = probability associated with Anderson-Darling test for the normality of
distribution (associated probability in brackets).
ferent techniques, with contrasting results. In a
microphotographic and planimetric study, Bjrk
and Persson
8
demonstrated an increase in villus
ramification with corresponding increases in sur-
face area in diabetic placentae compared with nor-
mal ones. In a series of papers
9-11
differentiated by
White class, Teasdale showed an increase in the
parenchymal component in diabetic placentae and
a greater exchange surface area, especially in rela-
tion to fetal birth weight. This effect, rather than
arising from particular metabolic alterations, may
more simply be due to the placentas ability to
adapt to the greater nutritional needs of the fetus.
Substantially similar values were reported by Boyd
et al.
12
Using stereological studies, Mayhew et al
13
found that diabetic placentae have a more volumi-
nous capillary bed, showed a greater diameter and
area, and the vessels were longer. No differences in
stromal diffusion distance and villous diameter
were found for varying fetal weights and severity of
diabetes.
More recently, Jauniaux and Burton
14
studied 12
placentae from women with Type I diabetes and 10
control placentae, measuring the volume of the in-
termediate and terminal villi as well as that of the
intervillous space, the volume and surface area of
the capillaries, their length and diameter, the thick-
ness of the villous membrane and its diffusing
capacity. The methodology they used was inter-
section of test lines.
15
An increase in volume of the
mature intermediate and terminal villi has been
reported, as well as of their surface area and that of
the fetal capillaries. The basement membrane was
even thicker in the subgroup of patients with fetal
macrosomia. Calderon et al
16
studied 56 uncompli-
cated placentae, 51 with mild hyperglycemia, 59
Volume 34, Number 5/October 2012 243 Diabetic Placenta
Table II Descriptive Statistics for the Variable D MIN
Case N Mean (minmax) Variance CV S-W A-D
Control 1 7 0.781 (0.3001.320) 0.184 0.549 0.850 (0.123) 0.526 (0.115)
Control 2 8 0.480 (0.3300.720) 0.020 0.298 0.864 (0.132) 0.535 (0.116)
Control 3 7 0.476 (0.2000.770) 0.040 0.419 0.970 (0.896) 0.176 (>0.15)
Control 4 10 0.385 (0.1600.700) 0.031 0.459 0.908 (0.266) 0.473 (>0.15)
Control 5 5 1.666 (0.6203.230) 1.771 0.799 0.742 (0.025) 0.668 (0.032)
Controls (pooled) 37 0.671 (0.1603.230) 0.424 0.971 0.596 (0.000) 4.925 (<0.01)
Diabetic 1 8 1.339 (0.5203.070) 0.828 0.680 0.834 (0.065) 0.632 (0.062)
Diabetic 2 8 0.943 (0.6901.680) 0.107 0.348 0.753 (0.009) 0.876 (0.013)
Diabetic 3 7 0.836 (0.4301.640) 0.181 0.509 0.878 (0.219) 0.408 (>0.15)
Diabetic 4 7 0.549 (0.3000.980) 0.066 0.467 0.920 (0.428) 0.302 (>0.15)
Diabetic 5 8 0.730 (0.4401.020) 0.031 0.240 0.987 (0.986) 0.160 (>0.15)
Diabetics (pooled) 38 0.889 (0.3003.070) 0.295 0.611 0.755 (0.001) 2.786 (<0.01)
CV = coefcient of variation, N = sample size, min = minimum value recorded in the sample, max = maximum value recorded in the sample, S-W = Shapiro-
Wilk test for the normality of distribution (associated probability in brackets), A-D = probability associated with Anderson-Darling test for the normality of
distribution (associated probability in brackets).
Table III Descriptive Statistics for the Variable D MAX
Case N Mean (minmax) Variance CV S-W A-D
Control 1 7 1.649 (0.8802.750) 0.306 0.336 0.797 (0.038) 0.848 (0.014)
Control 2 8 2.891 (0.5108.800) 11.467 1.171 0.713 (0.003) 1.097 (<0.01)
Control 3 7 1.534 (0.6603.280) 0.718 0.552 0.844 (0.108) 0.544 (0.102)
Control 4 10 2.370 (0.5404.580) 2.617 0.683 0.879 (0.127) 0.471 (>0.15)
Control 5 5 2.674 (0.7005.580) 5.500 0.877 0.791 (0.068) 0.562 (0.069)
Controls (pooled) 37 1.229 (0.5108.800) 3.956 0.892 0.780 (0.001) 2.704 (<0.01)
Diabetic 1 8 9.906 (3.22020.070) 29.405 0.547 0.949 (0.699) 0.242 (>0.15)
Diabetic 2 8 5.325 (1.15012.420) 21.135 0.863 0.813 (0.040) 0.684 (0.045)
Diabetic 3 7 5.131 (1.35018.710) 40.039 1.233 0.668 (0.002) 1.096 (<0.01)
Diabetic 4 7 2.704 (0.5105.470) 3.094 0.650 0.902 (0.300) 0.364 (>0.15)
Diabetic 5 8 5.049 (1.1009.340) 7.823 0.554 0.943 (0.669) 0.307 (>0.15)
Diabetics (pooled) 38 5.713 (0.51020.070) 23.743 0.367 0.847 (0.001) 1.871 (<0.01)
CV = coefcient of variation, N = sample size, min = minimum value recorded in the sample, max = maximum value recorded in the sample, S-W = Shapiro-
Wilk test for the normality of distribution (associated probability in brackets), A-D = probability associated to Anderson-Darling test for the normality of
distribution (associated probability in brackets).
with gestational diabetes and 41 with full-blown
diabetes. An image analyzer was used to measure
the total area of the terminal villi (in reality, mature
intermediate and terminal villi were measured), the
mean area and the density of the villi, the total and
mean areas of the vessels, and their number and
capillarization index (percentage of the villous area
occupied by the capillary area). The results of this
study showed an increase in the total area of the
villi only in the mild diabetes group. The capillar-
ization index was lower in full-blown diabetes and
less so in gestational diabetes.
The only study to have used both optical and
electron microscopy to perform morphometric
evaluation was by Pietryga et al.
17
They studied
32 placentae with diabetes of varying severity and
8 normal placentae. Whereas placentae in well-
controlled diabetes showed no significant alter-
ations, diabetic placentae with retarded intrauter-
ine growth showed thickening of the basement
membrane, endothelial proliferation, and reduction
in capillary surface area. By contrast, diabetic pla-
centae with macrosomia had only slight thickening
of the membrane and an increase in perivasal colla-
gen.
We used electron microscopy in this study as we
feel that the small size of the terminal villi means
that morphometric evaluation can be performed
only at the higher magnifications seen in ultrastruc-
ture. Comparison with results from the above
papers is therefore difficult, as these focused, either
intentionally
14
or unintentionally,
16,18
on both ma-
ture intermediate and terminal villi rather than on
terminal villi alone. In order to evaluate the capil-
laries involved in maternal-fetal exchange, a study
should be limited to the capillaries of the terminal
villi. The capillaries located in mature intermediate
villi are also involved in exchange but at a far lower
level and are difficult to evaluate.
In order to evaluate the effective exchange sur-
face area, we measured the inner surface of the cap-
illary, rather than its surface area, since a greater or
lesser degree of dilation does not affect transport of
material. We also feel that knowing the capillary
surface area is more important than knowing the
total surface area of the trophoblast, as not all of the
villous surface is involved in exchange: the areas of
trophoblast occupied by nuclei undergoing apopto-
sis (knots) and any that might be occupied by fibrin
are not relevant for placental function.
Again in order to evaluate organ efficiency, we
measured the minimum distance from the base-
ment membrane to the closest and to the farthest
vessels. One of the most controversial aspects of
diabetes-related chorangiosis is the apparently ran-
dom distribution of the vessels in relation to the
filtration membrane. Our results show that the min-
imum distance from the capillaries, both the closest
and the farthest from the basement membrane, is
244 Analytical and Quantitative Cytopathology and Histopathology
Rossi et al
Table IV Descriptive Statistics for the Variable MT BM
Case N Mean (minmax) Variance CV S-W A-D
Control 1 7 0.437 (0.1991.140) 0.109 0.753 0.744 (0.011) 0.807 (0.018)
Control 2 8 0.387 (0.0820.970) 0.092 0.786 0.903 (0.305) 0.350 (>0.15)
Control 3 7 0.442 (0.1810.780) 0.061 0.561 0.865 (0.166) 0.446 (>0.15)
Control 4 10 0.428 (0.1531.550) 0.238 1.142 0.611 (0.000) 1.898 (<0.01)
Control 5 5 0.392 (0.3070.457) 0.003 0.147 0.968 (0.865) 0.229 (>0.15)
Controls (pooled) 37 0.418 (0.0821.550) 0.107 0.781 0.794 (0.001) 2.569 (<0.01)
Diabetic 1 8 0.430 (0.2050.698) 0.032 0.419 0.904 (0.316) 0.416 (>0.15)
Diabetic 2 8 0.381 (0.2640.518) 0.007 0.213 0.986 (0.985) 0.138 (>0.15)
Diabetic 3 7 0.514 (0.2970.930) 0.058 0.469 0.854 (0.133) 0.500 (0.137)
Diabetic 4 7 0.384 (0.2600.730) 0.027 0.426 0.824 (0.051) 0.577 (0.089)
Diabetic 5 8 0.414 (0.3320.503) 0.004 0.146 0.929 (0.545) 0.309 (>0.15)
Diabetics (pooled) 38 0.423 (0.2050.930) 0.024 0.367 0.874 (0.001) 1.540 (<0.01)
CV = coefcient of variation, N = sample size, min = minimum value recorded in the sample, max = maximum value recorded in the sample, S-W = Shapiro-
Wilk test for the normality of distribution (associated probability in brackets), A-D = probability associated with Anderson-Darling test for the normality of dis-
tribution (associated probability in brackets).
Table V Probabilities Associated with Levenes Test for Equality
of Variances among Single and between Pooled Cases
(Controls Versus Diabetics)
Single cases Pooled cases
Variable Test p Value Test p Value
VL 1.874 0.072 0.351 0.555
D MIN 13.398 0.000 0.063 0.802
D MAX 4.095 0.000 18.369 0.000
MT BM 3.158 0.003 8.880 0.004
significantly greater in diabetic placentae and this
increases the diffusion distance of the vasculosyn-
cytial membrane.
Finally, we examined the thickness of the base-
ment membrane using a random measurement
repeated at high magnification, avoiding areas with
deposits of anomalous matter.
Parametric tests of comparisons among samples,
like ANOVA and Students t test, are more accurate
and precise than nonparametric tests, like Kruskal-
Wallis and Mann-Whitney U, when a variable has a
normal distribution and its variance is the same
across the cases; otherwise, the opposite holds
true.
3
In our sample, parametric and nonparametric
tests are in general agreement in rejecting the null
hypothesis for variable VL and D MAX (due to
higher values attained by the diabetics) and accept-
ing it for MT BM, i.e., values do not differ between
controls and diabetics. As far as D MIN, parametric
and nonparametric tests among single cases reject
the null hypothesis, but for the pooled cases they do
not support the same conclusion. Having found a
significant departure from normality, we conclude
that the Mann-Whitney U test should be preferred
over Students t test, thus we reject the null hypoth-
esis and conclude that in diabetics values of D MIN
are significantly higher than controls. In conclusion,
it would seem that the diabetic condition increases
significantly the values of VL, D MIN and D MAX
in respect to controls, but those of MT BM do not
change.
The results of our study show that in diabetic
placentae, the capillary surface area is greater, per-
haps in relation to their numeric increase per villus.
The increase in capillarization in placental villi is
connected to oxygen saturation in the placental bed,
according to a well-known model used for pre-
eclampsia.
19,20
According to Desoye and Myatts
recent theory,
21
the maternal-fetal metabolic alter-
ations in pregnancies complicated by diabetes
cause intrauterine hypoxia and this leads to a com-
pensatory vascular proliferation. This hypothesis is
no doubt interesting, though two specific points
need to be highlighted. First of all, the distribution
and structure of the vessels in diabetic chorangiosis
seems to be very different from the hypervascular-
ization occurring in gestosis, in which there are
several small vessels per villus, often of equal di-
ameter with a narrow lumen and irregular profile.
22
On the other hand, if it is true that the mean inner
surface area of the vessels is higher in diabetic pla-
centae, the minimum distance of the closest and
farthest vessels from the basement membrane is
greater, and this could counteract the efficacy pro-
vided by the greater surface area. Finally, the thick-
ening of the endothelium which we observed, as
Volume 34, Number 5/October 2012 245 Diabetic Placenta
Table VI Statistical Tests for Equality of Means of Each Variable between Diabetic Cases Pooled for Mothers Age and Birth Weight
Mothers age Birth weight
p Value p Value p Value p Value
Variable t test (36 df) U test (1 df) t test (36 df) U test (1 df)
VL 0.568 0.468 162.000 0.483 0.734 0.535 149.000 0.856
D MIN 1.753 0.973 233.000 0.303 0.034 0.088 138.000 0.049
D MAX 1.785 0.632 247.500 0.310 0.484 0.083 206.500 0.016
MT BM 0.775 0.973 176.000 0.654 0.535 0.444 157.500 0.059
df = degrees of freedom, p value = probability value associated with each test, t test = value of Students t test, U test = value of Mann-Whitney U test.
Table VII Statistical Tests for Equality of Means of Each Variable among Single Cases and between Pooled Cases (Controls Versus
Diabetics)
Single cases Pooled cases
F-ratio K-W test t test U test
Variable (9 df) p Value (9 df) p Value (1 df) p Value (1 df) p Value
VL 2.673 0.010 22.340 0.008 7.221 0.009 457.000 0.009
D MIN 4.187 0.000 32.820 0.000 2.487 0.119 375.500 0.001
D MAX 3.816 0.001 24.268 0.004 16.269 0.000 311.500 0.000
MT BM 0.157 0.997 8.109 0.523 0.007 0.934 537.000 0.079
df = degrees of freedom, F-ratio = value of F-statistics in ANOVA, K-W test = value of Kruskal-Wallis test, p value = probability value associated with each test,
t test = value of Students t test, U test = value of Mann-Whitney U test.
highlighted also by other authors,
7,17
certainly does
not help to make maternal-fetal exchange more
efficient.
Our study was unable to confirm the thickening
of the trophoblast basement membrane that has
been reported by various other authors. We believe
that, in order to be as objective as possible, the thick-
ness of the basement membrane must be measured
at a sufficiently high magnification, such as those
provided by ultrastructural examination. This en-
sures that only the trophoblast membrane is meas-
ured and not the capillary membrane or the inter-
stitial space between the two structures or even the
immunocomplex protein deposits, which, accord-
246 Analytical and Quantitative Cytopathology and Histopathology
Rossi et al
Figure 2 Means (dots) and standard-error intervals (bars) for the variables VL (upper left), D MIN (upper right), D MAX (lower left), and
MT BM (lower right) for each case and for pooled cases. c1, c2, c3, c4 and c5 = single control cases; cm = pooled control case; d1, d2,
d3, d4 and d5 = single diabetic cases; dm = pooled diabetic case.
ing to Zybzhitskaia et al,
23
are widespread in dia-
betic placentae. The fact that the basement mem-
brane is substantially normal leads us to believe
that it is undamaged by the metabolic condition
and/or by any immune system Noxa present.
Conclusion
Our study, performed on diabetic and normal pla-
centae, showed a series of morphological and mor-
phometric anomalies in the placentae of women
with pregnancies complicated by hyperglycemia.
Mature intermediate and terminal villi very often
appeared swollen (dysmaturity) with the presence
of numerous small blood vessels with a random
distribution along the axis (chorangiosis). This was
highlighted especially by trichrome staining and
CD34 immunohistochemical reaction.
As well as confirming the noteworthy vascular-
ization features in the ultrastructure, in some cases
the study showed submembranous deposits of pro-
tein material, excessive vacuolization of the tropho-
blast with degenerative focal points, and regressive
and proliferative features of the endothelium.
Morphometric evaluation showed that the inner
surface area of the vessels in the villus was higher
in diabetic placentae, though this advantage was
cancelled out by the greater minimum distance
from the villous surface to the nearest and farthest
vessel. The mean thickness of the basement mem-
brane was the same in both study groups.
Taken together, these alterations can be interpret-
ed as an attempt by the diabetic placenta to com-
pensate for metabolic-hypoxic damage, which is
difficult to assess at a functional level.
Acknowledgments
The authors wish to thank Professor Peter Kauf-
mann
for reading the manuscript and giving im-
portant suggestions.
References
1. Ogino S, Redline RW: Villous capillary lesions of the pla-
centa: Distinctions between chorangioma, chorangiomato-
sis, and chorangiosis. Hum Pathol 2000;31:945954
2. Vogel M: Plakopatia diabetica. Virchows Arch Pathol Anat
1967;343:5163
3. Riffenburgh RH: Statistics in Medicine. Second edition.
Burlington, Mass, Elsevier Academic Press, 2006, pp 1672
4. Okudaira Y, Hirota K, Cohen S, Strauss L: Ultrastructure of
the human placenta in maternal diabetes mellitus. Lab Invest
1966;15:910926
5. Widmaier G: Zur ultrastruktur menschlicher placentazotten
beim diabetes mellitus. Arch Gynkol 1970;208:396409
6. Jones CJP, Fox H: Placental changes in gestational diabetes:
An ultrastructural study. Obstet Gynecol 1976;48:274280
7. Laurini RN, Visser GHA, van Ballegoodie E: Morphological
fetoplacental abnormalities despite well-controlled diabetic
pregnancy. Lancet 1984;1:800
8. Bjork O, Persson B: Villous structure in different parts of the
cotyledon in placentas of insulin-dependent diabetic wom-
en. Acta Obstet Gynecol Scand 1984;63:3743
9. Teasdale E: Histomorphometry of the placenta of the diabet-
ic women: Class A diabetes mellitus. Placenta 1981;2:241251
10. Teasdale E: Histomorphometry of the human placenta in
class B diabetes mellitus. Placenta 1983;4:112
11. Teasdale E: Histomorphometry of the human placenta in
class C diabetes mellitus. Placenta 1985;6:6981
12. Boyd PA, Scott A, Keeling JW: Quantitative structural stud-
ies on placenta from pregnancies complicated by diabetes
mellitus. Br J Obstet Gynaecol 1986;93:3135
13. Mayhew TM, Srensen FB, Klebe JG, Jackson MR: Growth
and maturation of villi in placentae from well-controlled di-
abetic women. Placenta 1994;15:5765
14. Jauniaux E, Burton GJ: Villous histomorphometry and pla-
cental bed biopsy investigation in Type 1 diabetic pregnan-
cies. Placenta 2006;27:468474
15. Mayhew TM, Burton GJ: Methodological problems in pla-
cental morphometry: Apologia for the use of stereology
based on sound sampling practice. Placenta 1988;9:565581
16. Calderon IM, Damasceno DC, Amorin RL, Costa RA, Brasil
MA, Rudge MV: Morphometric study of placental villi and
vessels in women with mild hyperglycemia or gestational or
overt diabetes. Diabetes Res Clin Pract 2007;78:6571
17. Pietryga M, Biczysko W, Wender-Ozegowska E, Brazert J,
Bieganska E, Biczysko R: Ultrastructural examination of the
placenta in pregnancy complicated by diabetes mellitus.
Ginekol Pol 2004;75:111118
18. Baurakiades E, Martins AP, Victor Moreschi N, Souza CD,
Abujamra K, Saito AO, Mecatti MC, Santos MG, Pimentel
CR, Silva LL, Cruz CR, de Noronha L: Histomorphometric
and immunohistochemical analysis of infectious agents, T-
cell subpopulations and inflammatory adhesion molecules
in placentas from HIV-seropositive pregnant women. Diagn
Pathol 2011;6:101
19. Kaufmann P, Kingdom JCP: Development of the vascular
system in the placenta. In Morphogenesis of Endothelium.
Edited by W Risau, GM Rubanyi. Amsterdam, Harwood
Academic Publishers, 2000, pp 255276
20. Barut F, Barut A, Gun BD, Kandemir NO, Harma MI, Harma
M, Aktunc E, Ozdamar SO: Intrauterine growth restriction
and placental angiogenesis. Diagn Pathol 2010;5:24
21. Desoye G, Myatt L: The placenta. In Diabetes in women:
Adolescence, Pregnancy, and Menopause. Edited by EA
Reece, DR Coustan, SG Gabbe. Third edition. Philadelphia,
Lippincott Williams & Wilkins, 2004, pp 147157
22. Resta L, Capobianco C, Marzullo A, Piscitelli D, Sanguedolce
F, Schena FP, Gesualdo L: Confocal laser scanning micro-
scope study of terminal villi vessel in normal term and pre-
eclamptic placentas. Placenta 2006;27:735739
23. Zybzhitskaia LB, Kosheleva NG, Semenov VV, Nazarova SI,
A lamazian EK: Placental changes in type 1 diabetes melli-
tus. Arkh Patol 2008;70:1417
Volume 34, Number 5/October 2012 247 Diabetic Placenta
Das könnte Ihnen auch gefallen
- Research Bio StratchDokument48 SeitenResearch Bio StratchJanuar Dwi YudhistiraNoch keine Bewertungen
- Application of Statistical Concepts in The Determination of Weight Variation in SamplesDokument3 SeitenApplication of Statistical Concepts in The Determination of Weight Variation in SamplesLope Santos IVNoch keine Bewertungen
- Hypothesis Testing Random MotorsDokument8 SeitenHypothesis Testing Random MotorsLinn ArshadNoch keine Bewertungen
- Sim Chapter 1-5Dokument69 SeitenSim Chapter 1-5Rommel Urbano YabisNoch keine Bewertungen
- LSS Cheat SheetsDokument29 SeitenLSS Cheat SheetsPaweł Szpynda100% (2)
- Ebook Ebook PDF Statistics For Psychology 6th Edition by Aron PH D Arthur PDFDokument41 SeitenEbook Ebook PDF Statistics For Psychology 6th Edition by Aron PH D Arthur PDFgearldine.paul661100% (34)
- Mir Ghani 2006Dokument4 SeitenMir Ghani 2006Sarly FebrianaNoch keine Bewertungen
- Final - Artic Ro Imf&Gd ModifDokument8 SeitenFinal - Artic Ro Imf&Gd ModifAnonymous eson90Noch keine Bewertungen
- DIC in Abruptio 2Dokument5 SeitenDIC in Abruptio 2HoneylynNoch keine Bewertungen
- Clinical Study Gene Expression of Leptin and Long Leptin Receptor Isoform in Endometriosis: A Case-Control StudyDokument38 SeitenClinical Study Gene Expression of Leptin and Long Leptin Receptor Isoform in Endometriosis: A Case-Control StudyAnthony ChandraNoch keine Bewertungen
- Thy Box Timo Munoz-Chapuli2015Dokument6 SeitenThy Box Timo Munoz-Chapuli2015PABLO ALBERTO SANCHEZ BARRERANoch keine Bewertungen
- Hum. Reprod.-2004-Carp-191-5Dokument5 SeitenHum. Reprod.-2004-Carp-191-5venkayammaNoch keine Bewertungen
- Kista OvariumDokument6 SeitenKista OvariumAde Gustina SiahaanNoch keine Bewertungen
- Efficacy and Safety of Indomethacin Therapy For PolyhydramniosDokument6 SeitenEfficacy and Safety of Indomethacin Therapy For PolyhydramniosdoctorkwekkwekNoch keine Bewertungen
- Amniocentesis Results and Retrospective Analysis Performed in The University ClinicDokument6 SeitenAmniocentesis Results and Retrospective Analysis Performed in The University ClinicCindy Denti PratikasariNoch keine Bewertungen
- Circulating Microparticles in Preeclampsia: Research ArticleDokument4 SeitenCirculating Microparticles in Preeclampsia: Research ArticleFahmi Nur ZamanNoch keine Bewertungen
- Stereological Analysis of Terminal Villi of The Placentas of Pregnant Woman With Sideropenic AnemiaDokument5 SeitenStereological Analysis of Terminal Villi of The Placentas of Pregnant Woman With Sideropenic Anemiasanbin007Noch keine Bewertungen
- Doppler en EctopicoDokument6 SeitenDoppler en EctopicoLuis Enrique Moscoso OrtizNoch keine Bewertungen
- Correlation of Myometrial Thickness and The Latency Interval of Women With Preterm Premature Rupture of The MembranesDokument6 SeitenCorrelation of Myometrial Thickness and The Latency Interval of Women With Preterm Premature Rupture of The MembranesstephaniedianNoch keine Bewertungen
- Cog NTDokument11 SeitenCog NTFabiolaQuijaiteNoch keine Bewertungen
- Sulfated Glycosaminoglycans of Periurethral Tissue in Pre-And Postmenopausal WomenDokument4 SeitenSulfated Glycosaminoglycans of Periurethral Tissue in Pre-And Postmenopausal WomenSheila Regina TizaNoch keine Bewertungen
- Pap Smear Accuracy For The Diagnosis of Cervical Precancerous LesionsDokument5 SeitenPap Smear Accuracy For The Diagnosis of Cervical Precancerous LesionsPahang Reforansa PutraNoch keine Bewertungen
- Thalassemic Mothers and Their Babies: AbstractDokument4 SeitenThalassemic Mothers and Their Babies: AbstractWahyu PermataNoch keine Bewertungen
- AMM V 27.07Dokument138 SeitenAMM V 27.07paul_calburean7899Noch keine Bewertungen
- Placental Pathology and Blood PressureDokument12 SeitenPlacental Pathology and Blood PressureEka PutraNoch keine Bewertungen
- C. Eckmann-Scholz, J. Mallek, A. Caliebe, S. HeidemannDokument2 SeitenC. Eckmann-Scholz, J. Mallek, A. Caliebe, S. HeidemannKeith Mark AlmarinesNoch keine Bewertungen
- Hamil AnggurDokument7 SeitenHamil AnggurIchunx MelissaNoch keine Bewertungen
- Monoamniotic Twin Pregnancies: Antenatal Management and Perinatal Results of 19 Consecutive CasesDokument6 SeitenMonoamniotic Twin Pregnancies: Antenatal Management and Perinatal Results of 19 Consecutive CasesNovd NovitaNoch keine Bewertungen
- Selective Feticide in Complicated Monochorionic Twin Pregnancies Using Ultrasound-Guided Bipolar Cord CoagulationDokument5 SeitenSelective Feticide in Complicated Monochorionic Twin Pregnancies Using Ultrasound-Guided Bipolar Cord CoagulationDesyHandayaniNoch keine Bewertungen
- Endometrial Thickness As A Predictor of Endometrial HyperplasiaDokument28 SeitenEndometrial Thickness As A Predictor of Endometrial HyperplasiaPirthi MannNoch keine Bewertungen
- Journal Pre-Proof: Journal of Pediatric and Adolescent GynecologyDokument18 SeitenJournal Pre-Proof: Journal of Pediatric and Adolescent GynecologyCorey WoodsNoch keine Bewertungen
- Ijph 41 92Dokument7 SeitenIjph 41 92Trung Kien VoNoch keine Bewertungen
- Comparison of The Rheologic Properties of Neonatal and Adult BloodDokument4 SeitenComparison of The Rheologic Properties of Neonatal and Adult BloodPrasad BorkarNoch keine Bewertungen
- Acta Obstet Gynecol Scand - 2019 - Litwinska - Ventriculo Amniotic Shunting For Severe Fetal VentriculomegalyDokument6 SeitenActa Obstet Gynecol Scand - 2019 - Litwinska - Ventriculo Amniotic Shunting For Severe Fetal VentriculomegalyApotik ApotekNoch keine Bewertungen
- Maternal Serum Leptin As A Marker of PreeclampsiaDokument6 SeitenMaternal Serum Leptin As A Marker of PreeclampsiaAlfa FebriandaNoch keine Bewertungen
- Bankoglu 2018Dokument8 SeitenBankoglu 2018Ronald Echeverria IbazetaNoch keine Bewertungen
- Prenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromaDokument5 SeitenPrenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromawitaNoch keine Bewertungen
- Marconi 2008Dokument6 SeitenMarconi 2008Sri HariNoch keine Bewertungen
- Cases With Ruptured Membranes That "Reseal": Gainesville, FloridaDokument7 SeitenCases With Ruptured Membranes That "Reseal": Gainesville, FloridaHòa HồNoch keine Bewertungen
- Aydin 2017Dokument7 SeitenAydin 2017Berry BancinNoch keine Bewertungen
- Early First-Trimester Trophoblast Volume in Pregnancies That Result in Live Birth or MiscarriageDokument8 SeitenEarly First-Trimester Trophoblast Volume in Pregnancies That Result in Live Birth or MiscarriageFebrinata MahadikaNoch keine Bewertungen
- Singleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalDokument6 SeitenSingleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalSarah SilaenNoch keine Bewertungen
- Prediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery DopplerDokument6 SeitenPrediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery Dopplerganesh reddyNoch keine Bewertungen
- Día Transfer. Labarta 1Dokument6 SeitenDía Transfer. Labarta 1AnaNoch keine Bewertungen
- V11n3oa04 PDFDokument6 SeitenV11n3oa04 PDFGohar Ali UsmanNoch keine Bewertungen
- Jurnal B.inggris AnakDokument14 SeitenJurnal B.inggris AnakLuciana LorenzaNoch keine Bewertungen
- DM & Carotid A. ThicknessDokument5 SeitenDM & Carotid A. ThicknessMohammed FareedNoch keine Bewertungen
- First Trimester Screening For AneuploidyDokument11 SeitenFirst Trimester Screening For AneuploidyRakhmad HidayatNoch keine Bewertungen
- LKI Perina HDI - 21102021Dokument37 SeitenLKI Perina HDI - 21102021ManusiaNoch keine Bewertungen
- Fat Cell Size, Insulin Sensitivity, and Inflammation in Obese ChildrenDokument6 SeitenFat Cell Size, Insulin Sensitivity, and Inflammation in Obese ChildrenwilmaNoch keine Bewertungen
- Fetal Biometei PDFDokument134 SeitenFetal Biometei PDFfariska amanizataNoch keine Bewertungen
- Statistical Analysis: Menstrual CyclesDokument3 SeitenStatistical Analysis: Menstrual Cyclesmihrullah.azimi1Noch keine Bewertungen
- 12 .Tyraskis2017Dokument31 Seiten12 .Tyraskis2017dw21541Noch keine Bewertungen
- Correcting Data For Case Mix in Stroke Medicine: Unplanned Deliveries, PillDokument2 SeitenCorrecting Data For Case Mix in Stroke Medicine: Unplanned Deliveries, PillNatanael SusantoNoch keine Bewertungen
- 2012 Article 61Dokument5 Seiten2012 Article 61Al MubartaNoch keine Bewertungen
- Perinatal Transient Myeloproliferative Disorder in Trisomy 21Dokument11 SeitenPerinatal Transient Myeloproliferative Disorder in Trisomy 21Carina SuarezNoch keine Bewertungen
- Dec24 16 PDFDokument8 SeitenDec24 16 PDFijasrjournalNoch keine Bewertungen
- Advancesinsurgeryfor Abdominalwalldefects: Gastroschisis and OmphaloceleDokument12 SeitenAdvancesinsurgeryfor Abdominalwalldefects: Gastroschisis and OmphaloceleSitti HazrinaNoch keine Bewertungen
- Fetal Macrocrania: Diagnosis, Delivery and Outcomes: Original ArticleDokument4 SeitenFetal Macrocrania: Diagnosis, Delivery and Outcomes: Original ArticleAndreas NatanNoch keine Bewertungen
- 140 140 1 PBDokument4 Seiten140 140 1 PBMina LelymanNoch keine Bewertungen
- MacroalbuminemiaDokument4 SeitenMacroalbuminemiailma_ilemNoch keine Bewertungen
- The Development and Validation of A Fast and Robust Dried Blood Spot Based Lipid Profiling Method To Study Infant Metabolism - 2014 - KoDokument8 SeitenThe Development and Validation of A Fast and Robust Dried Blood Spot Based Lipid Profiling Method To Study Infant Metabolism - 2014 - KomasurNoch keine Bewertungen
- AMM V 27.07Dokument138 SeitenAMM V 27.07Anonymous 5cHdazK6b100% (1)
- Hydatidiform Mole Vs PMDDokument6 SeitenHydatidiform Mole Vs PMDNADIANoch keine Bewertungen
- Placenta Changes in Pregnancy With Gestational Diabetes: R I G I N A L A P E RDokument6 SeitenPlacenta Changes in Pregnancy With Gestational Diabetes: R I G I N A L A P E RMayra PereiraNoch keine Bewertungen
- Diagnosis of Endometrial Biopsies and Curettings: A Practical ApproachVon EverandDiagnosis of Endometrial Biopsies and Curettings: A Practical ApproachNoch keine Bewertungen
- A Simple Introduction To Anova: Amemou Franck Elyse Yao, Kaleab Hailemariam Venkat KumarDokument20 SeitenA Simple Introduction To Anova: Amemou Franck Elyse Yao, Kaleab Hailemariam Venkat KumarKumar SaiNoch keine Bewertungen
- Reading, Responding, and Writing - Asep NurjaminDokument8 SeitenReading, Responding, and Writing - Asep NurjaminAnna Althofunnisa Mustafasya BarkahNoch keine Bewertungen
- The Effects of Shariah Board Composition On Islamic Equity Indices ' PerformanceDokument12 SeitenThe Effects of Shariah Board Composition On Islamic Equity Indices ' PerformanceGhulam NabiNoch keine Bewertungen
- Article ChildparentrelationmanpreetSKM PDFDokument11 SeitenArticle ChildparentrelationmanpreetSKM PDFannoynmus meiNoch keine Bewertungen
- Tugas Jurnal Bimkos - Uninus - 2022Dokument14 SeitenTugas Jurnal Bimkos - Uninus - 2022EyrashahiraNoch keine Bewertungen
- Unit 5 Exploratory Data Analysis (EDA)Dokument41 SeitenUnit 5 Exploratory Data Analysis (EDA)Shamie Singh100% (1)
- UF Forensic PharmChem ClinicalTox Syllabi Current CatalogDokument86 SeitenUF Forensic PharmChem ClinicalTox Syllabi Current CatalogcuamiNoch keine Bewertungen
- CHAPTER 3 ProbabilityDokument55 SeitenCHAPTER 3 Probabilityyahska1305Noch keine Bewertungen
- The Use of ICT in Teaching Geometry in Primary SchoolDokument14 SeitenThe Use of ICT in Teaching Geometry in Primary SchoolSyed Abdul Hakim Syed ZainuddinNoch keine Bewertungen
- Understanding Students Personalityto Detect Their Learning DifferencesDokument9 SeitenUnderstanding Students Personalityto Detect Their Learning DifferencesKatrine Visitacion Dela CruzNoch keine Bewertungen
- Shane R. Brady, PHD, Assistant Professor, University of OklahomaDokument16 SeitenShane R. Brady, PHD, Assistant Professor, University of OklahomaGrace Talamera-SandicoNoch keine Bewertungen
- Chapter 1 To 3 and Preliminaries 1Dokument34 SeitenChapter 1 To 3 and Preliminaries 1Emmanuelle CalleNoch keine Bewertungen
- SAINS Carin and SundDokument9 SeitenSAINS Carin and SundnopiNoch keine Bewertungen
- School Environment and Satisfaction With Schooling Among Primary School Pupils in Ondo State, NigeriaDokument5 SeitenSchool Environment and Satisfaction With Schooling Among Primary School Pupils in Ondo State, NigeriaWEIN LIMNoch keine Bewertungen
- MODULE 7 2 Hypothesis Testing CANVASDokument63 SeitenMODULE 7 2 Hypothesis Testing CANVASMary Charlin BendañaNoch keine Bewertungen
- Summative Test Week 5 10 Statistics and ProbabilityDokument4 SeitenSummative Test Week 5 10 Statistics and ProbabilityOliver NardoNoch keine Bewertungen
- Effect of Multimodal Instructional Approaches On Students Learning of Chemistry Concepts in Selected Colleges of EducationDokument8 SeitenEffect of Multimodal Instructional Approaches On Students Learning of Chemistry Concepts in Selected Colleges of EducationPremier Publishers100% (1)
- Discriminant AnalysisDokument70 SeitenDiscriminant Analysisanupam99276Noch keine Bewertungen
- Pillars of TQM Implementation in Manufacturing Organizationan Empirical StudyDokument14 SeitenPillars of TQM Implementation in Manufacturing Organizationan Empirical StudyIbrahimMustefaNoch keine Bewertungen
- Ken Black QA ch13Dokument56 SeitenKen Black QA ch13Rushabh Vora100% (1)
- Thailand 2020Dokument14 SeitenThailand 2020Chee Wei HuanNoch keine Bewertungen
- Classroom Management Strategies For Effective Teaching and Learning in Universities in Rivers State, NigeriaDokument23 SeitenClassroom Management Strategies For Effective Teaching and Learning in Universities in Rivers State, NigeriaGlobal Research and Development ServicesNoch keine Bewertungen
- EfektivitasDokument21 SeitenEfektivitasKohanaMiyukiNoch keine Bewertungen
- BIOA01 Formal Lab Report Template - F2022Dokument6 SeitenBIOA01 Formal Lab Report Template - F2022Brian MachariaNoch keine Bewertungen