Beruflich Dokumente
Kultur Dokumente
Continuing Medical Education Examination-Facial Aesthetic Surgery The Hammock Platysmaplasty
Hochgeladen von
Nguyen Duong0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
34 Ansichten7 Seitenmedical examination
Originaltitel
Continuing Medical Education Examination—Facial Aesthetic Surgery the Hammock Platysmaplasty
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenmedical examination
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
34 Ansichten7 SeitenContinuing Medical Education Examination-Facial Aesthetic Surgery The Hammock Platysmaplasty
Hochgeladen von
Nguyen Duongmedical examination
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 7
Cont i nui ng Medi cal Educati on Exami nat i on- - Faci al
Aest het i c Sur ger y
The Hammock Platysinaplasty
Antoni o Fuent e del Campo, MD
L e a r n i n g Ob j e c t i v e s :
The reader is presumed to have a broad understanding of plastic surgical procedures and
concepts. After studying this article, the participant should be able to:
1. Better understand the mechanism of aging as it relates to the neck.
2. Conceptualize a limited incision platysmaplasty technique suitable for the aging neck
of mild to severe degree.
Physicians may earn 1 hour of Category 1 CME credit by successfully completing the
examination based on material covered in this article. The examination begins on page
253.
In this article, I describe the pertinent anatomy of the neck, the characteristics that define
a youthful-appearing neck, subsequent changes associated wi t h the aging neckline, and the
surgical procedure I am currently using for restoring the youthful appearance of the neck
through a submental approach. This procedure consists of overlapping the platysma mus-
cles (in "double-breasted" fashion) in the midline by use of lateral traction sutures
anchored to the periosteum and deep fascia of the contralateral mastoid region. In cases of
severe muscular laxity, the platysma muscles are partially sectioned horizontally at the
level of the hyoid bone, creating f our muscle flaps (extended procedure). This muscular
sectioning functionally elongates the abnormally shortened medial edge of the muscles.
The subsequent overlapping of these flaps permits deepening of the cervicomental angle.
The surgical procedure is performed exclusively through a submental approach, and
avoids the posterior traction of the platysma muscle. Its indications are described in detail.
Furthermore, the indications and procedures for a supplemental cervical approach in those
patients wi t h skin redundancy are discussed. My experience wi t h 43 consecutive patients is
presented, with a follow-up of 2 years and 9 months.
T
he aging process manifests itself in the neck in several ways, affecting neck vol-
ume, structure, and consistency. These changes are probably related to fat depo-
sition, muscular laxity, and poor skin tone, respectively. With regard to volume,
both preplatysmal and retroplatysmal fat must be evaluated and treated. Regarding
changes in contour and consistency, it is also necessary to determine whether the prob-
lem is related to the musculature, to the skin, or both, and each aspect must be treated
From the Division of Plastic and
Reconstructive Surgery, and t he
Plastic Craniomaxillofacial Surgery
Research Department of t he
Hospital "Dr. Manuel Gea
Gonzalez," Universidad Nacional
Autonoma de Mexico, Mexi co City,
Mexi co and the Craniofacial
Surgery Clinic of the Hospital
Infantil de Mexi co "Dr. Fredrico
Gomez," Mexi co City, Mexico.
Accepted for publication April 28,
1998.
Reprint requests: Antonio Fuente
del Campo, MD, Urbana no. 155-9
Col. Independencia, Mexi co City,
Mexico, D.F. 53830.
Copyright 1998 by t he American
Society for Aesthetic Plastic
Surgery, Inc.
190- 820X/ 98/ $5. 00 + 0
7 0 / 1 / 9 1 8 8 9
2 4 6 A E S T HE T I C SURGERY J OURNA L ~ J UL Y / A UGUS T 1 9 9 8
Figure 1. Submental approach for wide subcutaneous dissection and
dissection of the medial edges of the platysma. The sutures are placed
through the medial edges of the flaps at the level of the hyoid.
~ / t ~
/
@.
i "
Figure 2. Use of the custom-designed suture passer and the fixation of
"bridle" sutures to the mastoid region.
specifically. Current concepts of beauty dictate that the
face should project well-defined volumes, prominences,
and depressions. The submandibular line, which demar-
cates the separation between the face and the neck, runs
from one mastoid to the other, passing below the
mandible at the level of the hyoid. It should be well-
defined, establishing a cervicomental angle of 105 to 120
degrees. 1
The platysma is directed from its inferior origin on the
acromion and infraclavicular region upward and inward
toward its insertion on the inferior mandibular border.
Its medial portion inserts over the medial third of an
oblique line along the external aspect of the mandibular
body. Its external aspect mixes with fibers of the depres-
sor anguli oris, the mentalis, the risorius of Santorini, and
the orbicularis otis muscle of the lips to terminate in the
skin of the oral commissure. 2 Along the midline of the
neck, platysmal fibers join or intermix below the menton
with the corresponding fibers from the contralateral side,
forming a reticular structure. The platysma muscle main-
tains an intimate relationship with the skin through a
network of aponeurotic reinforcements first described by
Bosse and Papillon 3 and later by Furnas 4 as "retaining
ligaments" (platysmoauricular, anterior platysmocuta-
neous, and mandibular ligaments). With the passage of
time, the platysma becomes detached from the deeper
planes. This muscular attenuation and the weight of the
soft tissue displaces the skin, giving it a convex, pendu-
lous, and flaccid appearance. The central aspects of the
Figure 3. Posterior traction of the "bridle sutures" to overlap the
platysma in "double-breasted fashion. "
paired muscles separate in the midline. Frequently, medi-
al bands appear, perhaps owing to vertical shortening of
the corresponding muscular fibers. McKinney s classifies
these bands in four different grades, from minimal to
severe. Establishing the grade of deformity has important
implications for planning the appropriate surgical treat-
ment.
A variety of procedures have been espoused for neck con-
tour restoration. Fatty excess may be corrected with lipo-
The Hammock Platysmaplasty AESTHETI C SURGERY JOURNAL - JULY/ AUGUST 1998 247
/
Figure 4. Tacking sutures for fixation of the platysma in its newly
overlapped position.
Figure 6. Overlapping of the superior platysmal flaps to restore con-
tour in the upper neck.
Figure 5. Sectioning of platysma at the level of the hyoid for treatment
of grade 1H and IV platysmal bands.
suction or directed excision. Redundant skin has been
addressed with retroauricular and cervical incisions, and
muscular laxity has been corrected by restoring the
platysma to its proper anatomic location.
Platysmaplasty has taken on many forms, including later-
al plication, 6 sectioning and flap rotation, 7 simple midline
suturing, 8,9 progressively tensioned midline sutures, 1
muscular Z-plasty, 11 resection of muscular "bridles, ''12
and suspension sutures. 13 Most of these procedures
require a cervical approach, necessitating wide incisions
even in patients in whom the fundamental problem is
muscular and does not require cutaneous resection. In
general, those procedures designed to be performed
through a single, submental incision are effective only in
patients with minor deformities. The progressive corset
plication 1 is an excellent procedure. However, in my
experience, it has drawbacks associated with muscular
bunching in the midline, causing extra volume in this
area, reducing the distance between the submental line
and the mental symphysis, and limiting the possibility of
achieving a slim neck. Also, with this procedure, some-
times I find it difficult to determine the right amount of
tension to apply to achieve a good result.
After weighing both the advantages and disadvantages of
these techniques, I have developed and implemented a
procedure over the past 3 years that uses a combination
of these principles. This hybrid approach results in suc-
cessful restoration of neck contour, with good functional,
muscular reconstruction solely through a minimal sub-
mental incision.
Surgical Procedure
This procedure is performed as ambulatory surgery under
local anesthesia with intravenous sedation or under gen-
eral anesthesia. During the procedure the neck is extend-
ed. I overlap the platysma in a "double-breasted" fashion
in the midneck to restore neck contour, using one of two
248 AESTHETI C SURGERY . J OURNAL - J ULY/ AUGUST 1998 Volume18, Number4
Figure 7. Bilateral traction of bridle sutures with subsequent tacking
sutures for fixation of the upper and lower platysmal flaps in their new
position.
Figure 8. A, Preoperative view of a 56-year-old female patient with
grade IH rhytidosis, prominent jowls, and platysmal bands. B,
Postoperative view at 18 months after endoscopic subperiosteal face lift,
blepharoplasty, and extended hammock platysmaplasty, ensuring ade-
quate coverage of thyroid cartilages.
variations: direct overlapping for grade I (minimal) and
grade II bands (moderate), and muscular Z-plasty
(extended procedure) for grade III (significant) and IV
(severe) deformities.
In those patients in whom liposuction is indicated, I
begin with a 5 mm incision located 1 cm behind the sub-
mental line. With a 4 mm cannula, preplastysmal and
retroplastysmal fat are removed in both the submental
and the submandibular regions. I am careful to leave a
homogenous, thin layer of fat attached to the skin to
avoid the appearance of "leathery" skin that commonly
accompanies aggressive superficial suctioning. Once lipo-
suction is completed, the incision is enlarged to 3 cm, and
a thorough subcutaneous dissection is performed, com-
pleting the flap elevation that began with the blunt dis-
section performed with the liposuction cannula. In those
patients with jowls, further dissection is undertaken. A
wide subperiosteal dissection of the menton and the infe-
rior mandibular border is made either through the same
submental incision or through a supplemental inferior
vestibular approach, avoiding damage to the mental
nerve. This maneuver frees the insertions of the chin mus-
culature and indirectly frees the superomedial insertions
of the platysma. 14,1S Meticulous hemostasis is obtained
either with a long, insulated cautery (Colorado tip), or
with a similar insulated suction-cautery cannula that
offers the advantage of smoke extraction.
The location of the submandibular line should begin at
the hyoid, running upward toward the mastoids bilateral-
ly, and passing beneath the mandibular angle. Through
the submental incision, the entire medial edges of the
platysma muscles are approached, and their middle third
is dissected free from the deeper structures.
In the case of grade I and II bands, the medial border of
each muscle is drawn toward the midline with a 4-0
polyglactin stitch placed through it at the level of the sub-
mandibular line (Figure 1). Through a 1 cm bilateral
retroauricular slit incision, a custom-made, long, blunt,
curved needle is introduced to pass the sutures across the
neck. This needle is passed subcutaneously along the
length of what will be the new submandibular sulcus. On
one side, the needle is passed through to the midline exit-
ing through the submental incision. The ends of the pre-
viously placed platysmal suture from the contralateral
side are passed through the hole in the tip of the needle;
the needle is then drawn back through its tunnel (Figure
2). On the other side, the needle must pass through the
fibers of the ipsilateral platysma, continuing on deep to
the muscle to the midline. At this point, the contralateral
muscular suture is similarly drawn back through the
retroauricular incision. The two sutures are tightened,
overlapping the two muscles in the midline (Figure 3).
For the best results, it is convenient to previously calcu-
late the point of maximum desired superimposition
ahead of time by use of the calculation to estimate the
level at which the needle transfixes the platysma muscle
on the ipsilateral side.
The Hammock Platysmaplasty AESTHETI C SURGERY . JOURNAL ~ JULY/ AUGUST 1 998 249
\ . /
Figure 9. Incisions for redundant skin resection of the neck. A,
Cervical and retroauricular skin resection for grade III rhytidosis. B,
Additional, compensatory skin resection around the lobule.
The two sutures are drawn symmetrically upward in a
bridlelike fashion with moderate tension and are sutured
to the deep mastoid fascia and periosteum. This maneu-
ver permits relocation of the muscle and enables the sur-
geon to determine the best amount of traction and
muscular overlap necessary to obtain an aesthetically
pleasing neckline. Then, through the same submental
route, the free edge of the platysma, which overlies the
other one, is sutured to the deeper muscle with several 4-
0 polyglactin stitches (Figure 4). The intimate overlap-
ping of the two muscles allows a permanent scar to
develop after about 8 days, which prevents loss of con-
tour correction once the sutures dissolve. The submental
incision is closed with an intradermal running suture, and
the mastoid incisions are closed with a simple subcuticu-
lar 4-0 polyglactin stitch.
In grade III and IV platysmal bands, which manifest visi-
ble muscular shortening, I perform an extended proce-
dure. The muscles are sectioned horizontally from their
medial edge at the level of the hyoid (Figure 5). This sec-
tioning produces four triangular flaps; two are superolat-
erally based, and the other two are inferolaterally based.
These flaps are then fixed at their vertexes and over-
lapped with tension as previously described (Figure 6).
This partial muscular section perceptibly lengthens the
muscles, permitting ample overlap of their superior and
inferior portions. This provides excellent definition, con-
B
Figure 10. A, Preoperative view of a 58-year-old female patient with
grade IV rhytidosis, prominent jowls, and hanging neck. B, Postopera-
tive view at 14 months after endoscopic subperiosteal face lift,
blepharoplasty, cervical liposuction, suhperiosteal dissection of mental
area, and extended hammock pla~ysmaplasty.
Table. Complications
Submental cutaneous irregularities 7.0%
Small hematomas 4.7%
Skin rippling 2.3%
Partial relapse 2.3%
tour and support in the submental region and along the
submandibular area. The two inferior flaps are also over-
lapped to remodel the lower neck. As described for type I
and II bands, the procedure is completed by suturing the
free edges of the overlapped muscles (Figure 7). I do not
typically drain the wounds. They are protected after
surgery with an elastic garment that is worn continuously
for 1 week and intermittently thereafter for 2 weeks.
Results
I have used this procedure on 43 patients (35 women,
and 8 men), ranging in age from 35 to 66 years. Thirty-
two of the patients were treated exclusively through a
submental incision without removal of skin. With a max-
imum follow-up of 2 years and 9 months, I have
observed excellent long-term maintenance of the postop-
erative correction of neck contour. The best results were
observed in those cases in which the skin retained its
capacity to contract well (Figure 8). Complications have
been few; only two patients had small hematomas that
were readily drained during an office visit. In three other
250 AESTHETI C SURGERY JOURNAL - JULY/ AUGUST 1998 Volume18, Number4
Figure 11. A, Preoperative view of a 47-year-old obese female patient
with grade III rhytidosis, platysmal bands, heavy jowls and "marionette
lines. " B, Postoperative view at 6 months after mini-invasive subperios-
teal face lift, blepharoplasty, facial and cervical liposuction, subperios-
teal dissection of the mental area, and extended hammock platysma-
plasty. Note the improvement in the "marionette lines" and jowling.
patients areas of submental cutaneous adherence devel-
oped, resulting in temporarily visible irregularities. In one
case, lateral skin rippling occurred, most likely as a result
of insufficient subcutaneous dissection in this region
(Table). No other serious complications were encoun-
tered. There were no cases of neurovascular compromise
or recurrent deformity.
Discussion
This procedure avoids the posterior traction of the
platysma muscle common to many standard cervicoplas-
ty procedures. It allows excellent platysmal suspension
and intimate redraping of the muscle, elevating the deep
neck structures, such as the submandibular glands. The
tension applied to the muscle restores the muscular sup-
port of the neck, imparting adequate suspension without
the risk of central muscular diastasis, which may occur
with the posterolateral traction procedures.
The use of a bridle of suture or other foreign material to
give form to the neck does not change the fundamental
deformity, so that if the suture loosens or breaks, the cor-
rection is lost. The two bridle sutures that I use to relo-
cate the muscles permit the determination of the correct
amount of lateral traction and muscular overlap to
obtain an aesthetic and natural neck contour. Further-
more, the rest of the sutures placed along the borders of
the two overlapped muscles guarantee the permanence of
the muscular reconstruction without having to depend on
A
Figure 12. A, Preoperative view of a 38-year-old male patient. B,
Postoperative view 8 months after hammock platysmaplasty.
the bridle sutures for long-term results. I use delayed
absorption sutures because they need to last only long
enough to allow the cicatricial process to fuse the muscles
together. It is equally effective to use nonabsorbable
sutures such as nylon, but in my experience, these materi-
als can be palpable in thin-skinned patients. To avoid
skin irregularities, it is necessary to free the skin from the
underlying muscle, which permits muscle traction with-
out pulling on the skin.
The new contour of the neck with a deep submandibular
arch, which is obtained with this procedure, requires
more skin to cover it adequately. Thus in most cases
there is notably less skin redundancy, and in some cases,
the appearance of flaccidity disappears altogether. In
addition, the natural elasticity of the skin allows its redis-
tribution, redraping, and adherence to the muscles, so
that in most cases, skin resection is not necessary.
In general terms, this muscular correction achieves excel-
lent results in the contour of the neck, although there are
cases in which skin laxity (grade III rhytidosis) needs to
be corrected by drawing the skin upward and posteriorly
through a cervical and retroauricular incision. In these
cases, when the cutaneous traction causes bunching of
the skin around the lobule, the retroauricular incision is
generously extended downward and forward to permit
excess skin resection. It is important to ensure that this
incision does not violate the limits between the lobule
and the tragus, to avoid the scar becoming visible (Figure
9). In cases of severe skin redundancy (grade IV rhytido-
sis), which presents with skin redundancy extending
across the cheek, it is necessary to lengthen the incision
The Hammock Platysmaplasty AESTHETI C SURGERY JOURNAL ~ JULY/ AUGUST 1998 25"1
across the preauricular region. The need for cutaneous
resection depends on the aesthetic concept of the sur-
geon. But above all, it is the patient' s idea of a natural
result t hat should guide the surgeon. Many patients
choose t o avoid the cervical scar. Although in some cases
this implies leaving a certain cutaneous flaccidity, the
patients believe this result is more natural looking.
The hammock platysmaplasty procedure limits the need
for cervical incisions to a mi ni mum of cases. It can be
performed as an isolated procedure or as part of a full
face lift. It even permits cont our i mprovement of the neck
in those patients with promi nent t hyroi d cartilages. In
women it is i mport ant to ensure adequate coverage of the
t hyroi d cartilage, and not to apply excessive traction t o
the muscle flaps, to soften the neck' s cont our and to
avoid masculinizing its appearance (Figure 10). By free-
ing up the musculature of the ment on (and indirectly the
superomedial insertions of the platysma), centrally or lat-
erally directed tension acts on the lower cheek, improving
bot h the jowls and the "mari onet t e lines" (Figures 11
and 12).
Postoperative edema is moderat e, allowing the pr ompt
resumption of daily activities. This rapid resolution of
telltale surgical changes with minimal visible scarring
provides a very attractive procedure, particularly to male
patients, who may not have long hair to cover scars in
the post eri or cervical region.
Endoscopic technique is a versatile and powerful tool in
the plastic surgical armamentarium16; it permits a better
visualization of the surgical field t hrough a magnified
image on the moni t or and allows more directed assis-
tance from the scrub team. The hammock platysmaplasty
is equally easy to carry out under direct vision. Thus it is
as accessible to those who are comfort abl e with endo-
scopic techniques as to those who prefer a direct view of
the surgical field.
Re f e r e n c e s
1. Ellenbogen S, Karlin JV. Visual criteria for success in restoring t he
youthful neck. Plast Reconstr Surg 1980; 66: 826-37.
2. Cardoso de Castro C. The anatomy of t he platysma muscle. Plast
Reconstr Surg 1980; 66: 680-3.
3. Bosse JP, Papillon J. Surgical anatomy of t he SMAS at t he malar region.
In: Transactions of t he 9t h International Congress of Plastic and
Reconstructive Surgery. New York: McGraw-Hill, 1987:348-9.
4. Furnas DW. The retaining ligaments of t he cheek. Plast Reconstr Surg
1989; 83: 11-6.
5. McKinney P. The management of platysma bands. Plast Reconstr Surg
1996; 98: 999- 1006.
6. Guerrero Santos J, Espaillat G, Morales F. Muscular lifts in cervical
rhytidoplasty. Plast Reconstr Surg 1974; 54: 127-31.
7. Connell BF. Contouring t he neck in rhytidectomy by lipectomy and a
muscle sling. Plast Reconstr Surg 1978; 61: 376-83.
8. Souther SG, Vistnes LM. Medical approximation of t he platysma muscle
in the treatment of t he neck deformities. Plast Reconstr Surg
1981; 67: 607-13.
9. Cardoso de Castro C. The value of t he anatomical classification of t he
medial fibers of platysma muscle in cervical lifting. In: Transactions of
the 8t h International Congress of Plastic and Reconstructive Surgery.
Montreal: McGill University; 1983:515-6.
10. Feldman J. Corset platysmaplasty. Clin Plast Surg 1992; 19: 369.
11. Weisman PA. One surgeon's experience wi t h surgical contouring of t he
neck. Clin Plast Surg 1983; 10: 521.
12. Millard DR Jr., Garst WP, Beck RL, et al. Submental and submendibular
lipectomy in conjunction wi t h a face lift in t he male or female. Plast
Reconstr Surg 1972; 49: 385.
13. Giampapa VC, Di Bernardo BE. Neck contouring wi t h suture suspension
and liposuction: an alternative for t he early rhytidectomy candidate.
Aesthet Plast Surg 1995; 19: 217-23.
14. Fuente del Campo A. Face lift wi thout preauricular scars. Plast Reconstr
Surg 1993; 92: 642-53.
15. Fuente del Campo A. Subperiosteal face lift: open and endoscopic
approach. Aesthet Plast Surg 1995; 19: 149-60.
16. Fuente del Campo A. Facial rejuvenation: technique and rationale. In:
Fodor PB, Isse NG, eds. Endoscopically assisted aesthetic plastic
surgery. St. Louis: Mosby; 1996: 63-77.
2 5 2 A E S T H E T I C S U R G E R Y J O U R N A L ~ J U L Y / A U G U S T 1 9 9 8 Volume18, Number4
Das könnte Ihnen auch gefallen
- Surviving Cutaneous Melanoma. A Clinical Review of Follow-Up Practices, Surveillance, and Management of RecurrenceDokument14 SeitenSurviving Cutaneous Melanoma. A Clinical Review of Follow-Up Practices, Surveillance, and Management of RecurrenceNguyen DuongNoch keine Bewertungen
- New Tattoo Approaches in DermatologyDokument6 SeitenNew Tattoo Approaches in DermatologyNguyen DuongNoch keine Bewertungen
- Filler Placement and The Fat CompartmentsDokument14 SeitenFiller Placement and The Fat CompartmentsNguyen Duong100% (1)
- Innate and Intrinsic Antiviral Immunity in SkinDokument8 SeitenInnate and Intrinsic Antiviral Immunity in SkinNguyen DuongNoch keine Bewertungen
- Obstetrics and Gynecology-An Illustrated Colour TextDokument174 SeitenObstetrics and Gynecology-An Illustrated Colour TextAlina CiubotariuNoch keine Bewertungen
- Complications of Infantile HemangiomasDokument6 SeitenComplications of Infantile HemangiomasNguyen DuongNoch keine Bewertungen
- Efficacy and Safety of Intense Pulsed Light in Treatment of Melasma in Chinese PatientsDokument9 SeitenEfficacy and Safety of Intense Pulsed Light in Treatment of Melasma in Chinese PatientsNguyen DuongNoch keine Bewertungen
- 1,064-Nm Q-Switched Neodymium-Doped Yttrium Aluminum Garnet Laser and 1,550-Nm Fractionated Erbium-Doped Fiber Laser For The Treatment of Nevus of Ota in Fitzpatrick Skin Type IVDokument5 Seiten1,064-Nm Q-Switched Neodymium-Doped Yttrium Aluminum Garnet Laser and 1,550-Nm Fractionated Erbium-Doped Fiber Laser For The Treatment of Nevus of Ota in Fitzpatrick Skin Type IVNguyen Duong100% (1)
- Forehead Plasty For Facial RejuvenationDokument12 SeitenForehead Plasty For Facial RejuvenationNguyen DuongNoch keine Bewertungen
- Traditional AbdominoplastyDokument23 SeitenTraditional AbdominoplastyNguyen DuongNoch keine Bewertungen
- Aesthetic Facial ImplantsDokument21 SeitenAesthetic Facial ImplantsNguyen DuongNoch keine Bewertungen
- Endoscopic Forehead Lift. Technique and Case PresentationsDokument9 SeitenEndoscopic Forehead Lift. Technique and Case PresentationsNguyen DuongNoch keine Bewertungen
- One Hundred Cases of Endoscopic Brow LiftDokument5 SeitenOne Hundred Cases of Endoscopic Brow LiftNguyen DuongNoch keine Bewertungen
- Chapter 23 - Cosmetic Plastic SurgeryDokument24 SeitenChapter 23 - Cosmetic Plastic SurgeryNguyen DuongNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- A Study On Financial Performance of State Bank of India: April 2018Dokument6 SeitenA Study On Financial Performance of State Bank of India: April 2018priyankaNoch keine Bewertungen
- Assessment in The K To 12Dokument49 SeitenAssessment in The K To 12Alec Palcon JovenNoch keine Bewertungen
- Clinical Practice EvalDokument17 SeitenClinical Practice Evalapi-712107767Noch keine Bewertungen
- (MCQ'S) Production Planning and ControlDokument5 Seiten(MCQ'S) Production Planning and ControlHVFTOOLS HVFNoch keine Bewertungen
- Adani LTDDokument12 SeitenAdani LTDcekedNoch keine Bewertungen
- Skin LesionDokument2 SeitenSkin Lesion_carido_Noch keine Bewertungen
- Compression Ratio PDFDokument6 SeitenCompression Ratio PDFRafael LuqueNoch keine Bewertungen
- Service Manual: Compact Disc ReceiverDokument130 SeitenService Manual: Compact Disc Receiverjose luisNoch keine Bewertungen
- Hanz I para Record ArDokument591 SeitenHanz I para Record ArJuanpeGarbayoNoch keine Bewertungen
- Uml Lab ManualDokument38 SeitenUml Lab ManualcomputerstudentNoch keine Bewertungen
- Implied Volatility Forecast and Option Trading STRDokument12 SeitenImplied Volatility Forecast and Option Trading STRK P LoNoch keine Bewertungen
- NCM 101 - Health Assessment SyllabusDokument2 SeitenNCM 101 - Health Assessment SyllabusRA100% (3)
- Post-Earthquake Report On Bamboo Structures and Recommendations For Reconstruction With Bamboo On The Ecuadorian CoastDokument36 SeitenPost-Earthquake Report On Bamboo Structures and Recommendations For Reconstruction With Bamboo On The Ecuadorian CoastRUENoch keine Bewertungen
- (The American Scholar Vol. 13 Iss. 4) John Dewey - The Problem of The Liberal Arts College (1944) (10.2307 - 41206764) - Libgen - LiDokument4 Seiten(The American Scholar Vol. 13 Iss. 4) John Dewey - The Problem of The Liberal Arts College (1944) (10.2307 - 41206764) - Libgen - LiDang Tuan DungNoch keine Bewertungen
- Chirp Induced Vortices PRA v1 HighlightedDokument9 SeitenChirp Induced Vortices PRA v1 HighlightedShooboNoch keine Bewertungen
- DLL 10-11Dokument5 SeitenDLL 10-11LORIBELLE MALDEPENANoch keine Bewertungen
- C 1891622Dokument199 SeitenC 1891622api-3729284Noch keine Bewertungen
- Basic Tools in Nutrition 1Dokument10 SeitenBasic Tools in Nutrition 1Khibul LimNoch keine Bewertungen
- Prof - Ed 5 Facilitating Learner Centered Teaching Module 5 Week 5Dokument5 SeitenProf - Ed 5 Facilitating Learner Centered Teaching Module 5 Week 5Leanne Lawrence BonaobraNoch keine Bewertungen
- Building Electrification Unit 03Dokument3 SeitenBuilding Electrification Unit 03SURAJ KUMARNoch keine Bewertungen
- List of CollegesDokument2 SeitenList of Collegesbipul pandeyNoch keine Bewertungen
- Aol Act 11 RandyDokument3 SeitenAol Act 11 RandyaksanaNoch keine Bewertungen
- CDP AT FINGER PIER - StudyDokument25 SeitenCDP AT FINGER PIER - Studyd_mazieroNoch keine Bewertungen
- MIT - Sip FundamentalsDokument13 SeitenMIT - Sip Fundamentalskoalla01Noch keine Bewertungen
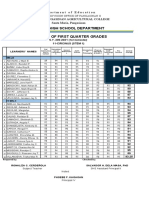
- Department of Education Senior High School 1st Quarter GradesDokument4 SeitenDepartment of Education Senior High School 1st Quarter GradesRonaliza CerdenolaNoch keine Bewertungen
- Wolfsdorf The Socratic Fallacy and The Epistimological Priority of Definitional KnowledgeDokument17 SeitenWolfsdorf The Socratic Fallacy and The Epistimological Priority of Definitional KnowledgeMaria SozopoulouNoch keine Bewertungen
- FWBD Mop 2019Dokument181 SeitenFWBD Mop 2019Aflkjael JamaelNoch keine Bewertungen
- Origin of NatyasastraDokument9 SeitenOrigin of NatyasastraArya V NairNoch keine Bewertungen
- Long-Term Contracts Loss AdjustmentDokument30 SeitenLong-Term Contracts Loss AdjustmentDina Adel DawoodNoch keine Bewertungen